Dr Rajiv Desai
An Educational Blog
REFRACTIVE ERROR
________________
REFRACTIVE ERROR:
________
Prologue:
Way back in 1973 when I was 12 years old and studying in 7th standard, I noticed that I could not read black-board from last bench. Initially I thought that everybody must be finding difficult to read black-board from last bench but it was not the case. Soon I visited eye doctor who found that I have refractive error and he prescribed -4 (minus 4) eyeglasses for me. Since then I have been wearing glasses. Refractive errors are usually present in the childhood and continue in the adult life. Unfortunately, they are not given much importance in our society which is evident from the fact that there is no effective system of pre-school visual examination of children either in the government sector or in the private sector. The earth was formed 4 billion years ago. Society has been around for about twenty thousand years. Spectacles (eyeglasses) did not appear until just over seven hundred years ago. Before that time, nearsighted youth endured a world that was clear only to within four to five feet from where they stood. Farsightedness and more specifically presbyopia (typically brought on by the aging process after the age of 40) affected almost everyone. Active, productive members of society had to stop working, writing, reading, and using their hands for skillful tasks at a relatively young age. Before the invention of spectacles to improve vision, society’s progress in culture, crafts, art, commerce, and science was severely limited! Even today worldwide half billion people suffer from poor vision because they do not have the eyeglasses they need. Their uncorrected refractive errors are a major cause of global disability and drastically reduce productivity, educational opportunities, and overall quality of life. The problem persists most prevalently in low-resource settings, even though prescription eyeglasses serve as a simple, effective, and largely affordable solution.
__________
__________
The figure below shows how billiard table will look if you have normal vision (Emmetropia):
_
The figure below shows how billiard table will look if you have Myopia (Near-sightedness):
Near objects are seen clearly but distant objects look blurred.
_
The figure below shows how billiard table will look if you have Hyperopia (Far-sightedness):
Near objects look blurred but distant object are seen clearly.
_
The figure below shows how billiard table will look if you have Astigmatism:
Both near and distant objects look blurred.
__________
“The art of making a pair of spectacles was an achievement of monumental significance for mankind that has had an incalculable impact. Although it has been relatively unknown to the general public, the evolution and development of spectacles over the past seven centuries qualifies as a long, significant, and quite fascinating journey through history, whose impact deserves to be better recognized and more widely appreciated.”
Professor Spencer Discala
__________
Interesting facts that you didn’t know:
1. About 30.8 million people purchase new glasses each year and yet few know about their production, history and life cycle.
2. Over one billion people in developing countries need eyeglasses but cannot afford them.
3. 25 percent of the global population needs eyeglasses.
4. 50 percent of children in institutions for the blind in Africa would be able to read normal or large print if they had eyeglasses.
5. The price for glasses in many African countries can exceed three months’ average salary. Despite this need, over four million pairs of eyeglasses are thrown away each year in North America.
6. The human eyeball weighs approximately one ounce.
7. Your eye blinks over 10,000,000 times a year
8. Just fewer than two primary school children in every ten wear glasses and three out of ten secondary school children wear glasses.
_________
Introduction to refractive error:
Vision:
Vision is the ability of some living beings to perceive, to distinguish and to interpret luminous stimuli. Vision is important on earth mainly in the terrestrial and in the superficial aquatic habitats because our planet is intensely exposed to sunlight and thus light and colors become distinguishing factors of objects present in the environment, even at distance. This distinction provided new survival strategies for the organisms, new protection mechanisms against external dangers, new ways to find food and to communicate with other individuals, new types of courting and reproduction behaviors, etc. That is, it created new possibilities of interaction with the surrounds and increased capacity to explore new ecological niches.
_
We see the objects because our brains need information about our environment for our behavior, actions and survival. Visual system uses light as an input of environmental information entering through our eyes and processed in brain. When light falls on an object, it is reflected and that reflected light enters eyes to fall on retina as visual perception to be interpreted by brain as visual information. In other words, you cannot see if there is no light or if the object is transparent which does not allow any reflection of light. It cannot be overemphasized that visual system sees every object two dimensionally (2D). We can see only that part of object that is facing us making 2D image on retina. The light rays reflected from objects enter eye in vertical, oblique and horizontal meridians to fall in retina to make 2D image. However, the environment is very large in size with multiple objects and eyes are very small, so these light rays must be bent (refracted) and focused on retina to get a clear 2D image on retina. That is the function of cornea and lens of the eye. Light entering the eye is bent, or “refracted”, as it passes through the cornea and the crystalline lens. The term “refractive error” is used to describe how accurately this light is focused on the retina to form a clear image. An eye that perfectly refracts the light coming from a distant object, to make a crisp focused image of it on the retina, does not have a refractive error and is referred to as “emmetropic” eye by eye care professionals. In the emmetropic (normally refracted) eye, entering light rays are focused on the retina by the cornea and the lens, creating a sharp image that is transmitted to the brain. The lens is elastic, more so in younger people. During accommodation, the ciliary muscles adjust lens shape to properly focus images. Refractive errors are failure of the eye to focus images sharply on the retina, causing blurred vision.
_
Let me start with basics:
We see objects in our environment because ambient light falls on object and reflected light rays from object enter our eyes. The source of light rays in our eyes is the point on object that reflects ambient light. Light spreads out from its source.
_
_
If the light rays are approaching the “source” they are converging and have positive vergence, if they are leaving the source they are diverging and have negative vergence, the further light travels from its source the less vergence it has, and if they travel far enough from the source (optical infinity) then the rays may eventually be considered parallel. Light from a distance greater than 20 feet or 6 meters is considered to be parallel. This is called Optical Infinity. However, true parallel light rays are rays that never meet. They have zero vergence.
_
_
The further the lens is from the source, the smaller the biggest angle between rays reaching the lens. In diagram above the rays with the maximum negative vergence describe a much wider angle for lens 1 than for lens 4. Lens 1 has the most negative vergence, since it is closest to the source. Lens 4 has the least vergence, since it is farthest from the source. As the lens moves to a distance of 6 meter, the vergence becomes almost zero and rays become almost parallel.
_
A pencil of light is a group of rays divergent from a single point on a light source. A beam of light is composed of the group of pencils originating from all of the points on a light source.
_
Large aperture will allow more divergent peripheral rays of pencil of light to pass through, as in fully open pupil. Normally, the full opening of the pupil admits light. It is the improper bending of the outermost rays in that pencil of light which causes refractive errors such as myopia, hyperopia, presbyopia (diminished focusing range with age) and astigmatism to be noticeable. Small pupil, by blocking these peripheral rays, and only letting into the eye those central rays, make any refractive error much less noticeable.
_
In a nutshell, a pencil of light from object is a group of divergent rays being reflected by the object. These divergent rays become less divergent as the object moves away from eye. At 6 meter the divergent rays appear parallel and these are so called parallel rays from distant objects entering eye. When object is near eye, the rays become more divergent and less parallel. The outermost (peripheral) rays from pencil of light are most divergent requiring most bending (refraction) to focus on retina and therefore most likely cause of refractive error. Near object would need far more bending than distance object as rays are more divergent. Small pupil will block outermost rays and therefore less bending required.
_
The figure above shows that so called parallel rays from distant objects (6 meter) are bent (refracted) by eye to focus on retina for clear image. However when object is near eye, these rays become divergent and focus behind retina. To bring these divergent rays back on retina, the eye must increase its refractive power i.e. accommodation for near objects.
_
Spherical aberration:
On top of figure above is a depiction of a perfect lens without spherical aberration: all incoming rays are focused in the focal point. The bottom example depicts a real lens with spherical surfaces, which produces spherical aberration: The different rays do not meet after the lens in one focal point. The further the rays are from the optical axis, the closer to the lens they intersect the optical axis. Spherical aberration is an optical effect observed in lens that occurs due to the increased refraction of light rays when they strike a lens near its edge, in comparison with those that strike nearer the centre. So is spherical aberration a contradiction to above discussion where peripheral rays are less refracted?
No.
See the figure again. It shows parallel rays meaning distant objects. However, as object moves closer to eye, these parallel rays become divergent. So even though there is slight over-convegence due to spherical aberration, divergent rays would need far more convergence to focus on retina and therefore slight spherical aberration would not correct it, resulting in peripheral outermost rays falling behind retina. Small pupil will help focus better image in both distant and near objects. For distant objects, it will reduce spherical aberration and for near objects, it will eliminate most diverging rays. In a nutshell, peripheral rays in distance vision would cause myopic defocus due to spherical aberration and peripheral rays in near vision would cause hyperopic defocus due to divergent rays. Since peripheral rays are blocked by small pupil or pinhole glasses (vide infra), both distance and near vision improves when pupil is small or when pinhole glasses are used.
________
The function of the eye is to see clearly the objects around us. The inability of the eye to accurately focus the rays of light coming from distance on the retina is called “Refractive Error”. This condition may be either because the eye is too short or long in length, or because the cornea or lens does not have the required refractive power. Like a camera, the human eye must be properly focused to see an image clearly. If light does not bend or refract correctly and focus directly on the retina, the result is blurred vision, or a refractive error. Refractive error refers to the mismatch between the optical components of the eye so that the retinal image is out of focus. It is correctable by wearing spectacles or contact lenses, assuming that the eye has not become amblyopic. The biggest concern is that a child who has uncorrected refractive error during the critical period development may become amblyopic. Fortunately, highly myopic (‘nearsighted’) children can hold objects very close and get a clear retinal image and the pediatric eye can also adjust considerably for hyperopia. However, if the two eyes have different uncorrected refractive errors, the potential for amblyopia in one eye is very high and bilateral amblyopia may accompany extreme refractive errors. Myopia usually starts in childhood and it progresses with age, generally leveling off in the late teens or early twenties.
______
______
The four most common refractive errors are:
•Myopia, or nearsightedness : clear vision close up but blurry in the distance
•Hyperopia, or farsightedness : clear vision in the distance but blurry close up
•Presbyopia : inability to focus close up as a result of aging
•Astigmatism : focus problems caused by the cornea
It is possible to have more than one refractive error, such as having both myopia and astigmatism.
_
_
Refractive error classification:
We know that the expression emmetropia is a conventional one and that in fact all normal human eyes have mild degrees of spherocylindrical errors or consist of a bitoric optical system, i.e. have principal meridians of relatively higher and lower powers at right angles. Let me explain in simple terms. The light rays must be refracted and focused on retina for clear image. When all light rays entering eyes are equally refracted (i.e. refracted in vertical, oblique and horizontal meridians) but focused before retina (myopia) or behind retina (hyperopia), we call it spherical refractive error. Pure myopia and pure hyperopia are spherical refractive error. When all light rays are unequally refracted in different meridians, we call is astigmatism, a cylindrical refractive error. Not only do light rays have to focus at the level of the retina (as opposed to in front or behind it) but also on a single point. This is achieved through the symmetry of the corneal and lens curvatures around their circumference. In astigmatism, variations in the symmetry of these curvatures (usually corneal) result in rays failing to focus on a single point. Obviously in astigmatism, no object will be clearly seen no matter the distance of object from eye. Remember, the terms spherical/cylindrical refractive error are used because lens made from glass sphere or glass cylinder is used to correct refractive error. In other words, spherical surface will bend light rays in all meridians equally to correct spherical refractive error and cylindrical surface will bend light rays in specific meridian perpendicular to axis of cylinder to correct cylindrical refractive error. Not to mention, two cylindrical surfaces of same dimensions at right angle to each other would make spherical surface. Not to mention, spherical or cylindrical does not mean 3D image. Remember, our visual system is meant for 2D image only.
_
An eye that has no refractive error when viewing distant objects is said to have emmetropia or be emmetropic meaning the eye is in a state in which it can focus parallel rays of light (light from distant objects) on the retina, without using any accommodation. A distant object in this case is defined as an object 6 meters or further away from the eye. This proves to be an evolutionary advantage by automatically focusing the eye on objects in the distance because it allows an individual to be alert in, say, a prey-predator situation. An eye that has refractive error when viewing distant objects is said to have ametropia or be ametropic. This eye, when not using accommodation, cannot focus parallel rays of light (light from distant objects) on the retina. The word “ametropia” can be used interchangeably with “refractive error” or “image formation defects.”
______
Myopia:
Also known as nearsightedness, myopia is the inability to see clearly at distance while objects at near are clear. In myopia the point of focus is in front of the retina because the cornea is too steeply curved, the axial length of the eye is too long, or both. Distant objects are blurred, but near objects can be seen clearly. Individuals will “squint” or move closer to the object they are viewing to see clearly. Myopia generally progresses into the late teens. Just as a child becomes taller or needs progressively larger shoes with increased body size through puberty, the eyes grow and lengthen as well. Therefore, an eye that is longer in infancy will proportionally lengthen or “worsen”. Therefore, myopic individuals are less likely to “grow out of” glasses. To correct myopia, a concave (minus) lens is used. It is also associated with an increased risk of retinal detachment, cataract formation and glaucoma.
_
Hyperopia:
Also known as farsightedness, hyperopia is the inability to see clearly at near, but there is also difficulty at distance. In hyperopia the point of focus is behind the retina because the cornea is too flatly curved, the axial length is too short, or both. In adults, both near and distant objects are blurred. Children and young adults with mild hyperopia may be able to see clearly because of their ability to accommodate. To correct hyperopia, a convex (plus) lens is used. It is actually normal for infants and young children to have mild degrees of hyperopia. As they grow and the eye becomes longer, this disappears. These children do not require correction with glasses. However, high degrees of hyperopia may create too much blur and lead to amblyopia, or a form of strabismus called accommodative esotropia. In such patients, glasses are necessary to properly focus the images, and sometimes to also straighten the eyes. Some hyperopic children may actually “grow out” of their glasses when they are older because of the eye growth mentioned above.
_
Astigmatism:
Astigmatism is an irregular shape of the refractive surfaces of the eye, most commonly the cornea but sometimes also the lens. Astigmatism can affect both distance and near vision and may be present alone, or with either hyperopia or myopia. In astigmatism, nonspherical (variable) curvature of the cornea or lens causes light rays of different orientations (e.g., vertical, oblique, horizontal) to focus at different points. To correct astigmatism, a cylindrical lens (a segment cut from a cylinder) is used. Cylindrical lenses have no refractive power along one axis and are concave or convex along the other axis.
_
Presbyopia:
Presbyopia is loss of the lens’ ability to change shape to focus on near objects due to aging. Typically, presbyopia becomes noticeable by the time a person reaches the early or mid 40s. A convex (plus) lens is used for correction when viewing near objects. These lenses may be supplied as separate glasses or built into a lens as bifocals or variable focus lenses.
_
Anisometropia:
Most children have similar readings in each eye. However, some may have very unequal eyes, with refractive error in one eye only, refractive error in both eyes but much stronger in one, or even different types of refractive error in each eye. This is known as anisometropia. Anisometropia is a significant difference between the refractive errors of the 2 eyes (usually > 3 diopters). Differing refractive states result in very slight differences in image sizes (aniseikonia refers to a difference in size or shape of images formed in the two eyes). Where the refractive difference is very small, this is imperceptible by the patient and not a problem. Where the effect is magnified due to a large refractive difference, the patient may experience diplopia, headaches, photophobia, reading difficulties, nausea, dizziness and general fatigue. It is for this reason that in childhood the brain suppresses one of the images and hence amblyopia develops in the eye where the image has been suppressed. These children are at risk of developing “lazy eye” or amblyopia in the eye with a higher refractive error. Therefore, glasses are extremely important not only to focus the image, but to prevent vision loss. These children are often not discovered until a later age, and often complain that they do not need glasses because they see well through one eye and seem to function normally even though they have poor vision in the other eye. Even after correction with eyeglasses, a difference in image size (aniseikonia) may persist; it can lead to difficulties with fusion of the 2 differently sized images and even to suppression of one of the images.
________
People who have always enjoyed clear vision at any distance start to hold the book further away and employ brighter light for comfortable close work as they grow older. The cornea and lens refract the incoming light rays to focus them on the retina at the back of the eye. In humans the cornea does some two-thirds and the lens one-third of this focusing. The power of the lens can be altered by changes in the shape of the lens — a process called accommodation. This allows a rapid change in focus, according to how near or distant is the object of regard. Better light increases the contrast between print and page, the associated contraction of the pupil increasing the depth of field. Unfortunately, focusing for near objects gradually reduces with age (presbyopia) and has to be helped by converging or convex lenses. The lens develops from the same layer of embryonic tissue that forms the skin (ectoderm). Both skin and the lens grow throughout our life. Skin is slowly shed or rubbed away and replaced, but the lens is confined within the fixed volume of the eyeball. As it grows it becomes more compact and stiffer, less able to assume greater convexity for near vision. Further compaction causes opacities to develop within the lens — cataract formation. When this causes significant interference with vision it is extracted surgically and replaced by an artificial intra-ocular lens (IOL). However, the IOL cannot accommodate for near vision, and glasses are still needed for reading.
_
With vision being our principal sensory contact with the environment, it is not surprising that uncorrected focusing can have significant influences, so much so that separate myopic and hyperopic personalities have been recognized. The myopic child can be introverted, studious, and solitary, with no interest in ball games or outdoor pursuits. ‘Short-sighted’ can be used as a derogatory term, implying an incomplete view, lacking in extent of intellectual outlook. As Disraeli put it, ‘so short-sighted are politicians in power’. The distinctive style of Impressionist painters has been attributed to myopia, and Cézanne, Degas, Pissarro, and Renoir were all known to be myopes. A survey of the teachers and pupils at the École des Beaux-Arts in Paris around the turn of the nineteenth century revealed 48% to be myopes, almost three times as many as in the general population.
_____
Importance of refractive errors:
•Refractive errors are important because they account for half the cases of avoidable vision impairment globally (153 million people).
•Undetected refractive errors in childhood may lead to behavioural problems and adversely affect social interaction and performance (academic or sporting) at school.
•It has been found that a minor reduction in vision has been associated with an increased risk of death and physical, social and emotional problems in people aged over 50 years.
•Under-corrected refractive error may account for up to 75% of all vision impairment in high-income countries.
Interventions to treat refractive errors (e.g., spectacles) are simple and cost-effective. However, global estimates indicate that more than 2.3 billion people in the world experience poor vision due to refractive error; of which 670 million people are considered visually impaired because they do not have access to corrective treatment.
_
Generally speaking, anyone can suffer from refractive error, however:
• Higher degrees of refractive error tend to run in families.
• Almost everyone gets presbyopia if they live long enough.
• Myopia is especially common in Asian peoples. It is a major cause of treatable visual disability in developing countries in Asia and other parts of the world.
• Myopia tends to begin in young people, at or before the age of puberty and tends to increase in degree until the age of about thirty, although this is variable.
• Hyperopia tends to appear as people age because younger people have a natural mechanism by which they adjust to it. As in presbyopia however, there comes a point at which the eye is no longer able to adjust and blur is noted.
_________
_________
Refraction and refractive index:
_
Refraction:
_
Refraction is the change in direction of propagation of a wave due to a change in its transmission medium. The phenomenon is mainly in governance to the law of conservation of energy and momentum. Due to change of medium, the phase velocity of the wave is changed but its frequency remains constant. This is most commonly observed when a wave passes from one medium to another at any angle other than 0° from the normal. Refraction of light is the most commonly observed phenomenon, but any type of wave can refract when it interacts with a medium, for example when sound waves pass from one medium into another or when water waves move into water of a different depth.
_
At the microscale, an electromagnetic wave’s phase velocity is slowed in a material because the electric field creates a disturbance in the charges of each atom (primarily the electrons) proportional to the electric susceptibility of the medium. (Similarly, the magnetic field creates a disturbance proportional to the magnetic susceptibility.) As the electromagnetic fields oscillate in the wave, the charges in the material will be “shaken” back and forth at the same frequency. The charges thus radiate their own electromagnetic wave that is at the same frequency, but usually with a phase delay, as the charges may move out of phase with the force driving them. The light wave traveling in the medium is the macroscopic superposition (sum) of all such contributions in the material: the original wave plus the waves radiated by all the moving charges. This wave is typically a wave with the same frequency but shorter wavelength than the original, leading to a slowing of the wave’s phase velocity. Most of the radiation from oscillating material charges will modify the incoming wave, changing its velocity. However, some net energy will be radiated in other directions or even at other frequencies.
_
Refractive index:
The speed of light is determined by the medium (material) through which the light is travelling. Light travels faster in a vacuum than it does in any other medium. Light changes speed as it passes from one medium to another. This is called refraction. The frequency of light does not change as it refracts. Refractive index of a material is a measure of the change in speed of light as it passes from a vacuum (or air as an approximation) into the material.
n = v1/v2
In the equation above, v1 is the speed of light in a vacuum. The bigger the refractive index the slower the light travels in that material i.e. the smaller v2 is.
__
When a ray of light is incident at normal incidence (at right angles) to the surface between two optical materials, the ray travels in a straight line. A ray travelling along the normal (perpendicular to the boundary) will change speed, but not direction.
_
When the ray is incident at any other angle, the ray changes direction as it refracts. That is why optic lenses are curved. It is the curvature of surface that bends light. Understanding of this concept led to the invention of lenses and the refracting telescope. The dotted line is the normal (perpendicular) to the surface. In refraction, calculation angles are always measured between rays and the normal. Angle of incidence is the angle between an incident ray and the normal. Angle of refraction is the angle between a refracted ray and the normal.
_
In the figure above, i is the angle of incidence and r is the angle of refraction.
_
The change in direction of a ray depends on the change in speed of the light and can be used to calculate refractive index. For the example above the refractive index n of the glass is given by:
_
_
Snell’s law states that for a given pair of media and a wave with a single frequency, the ratio of the sines of the angle of incidence θ1 and angle of refraction θ2 is equivalent to the ratio of phase velocities (v1 / v2) in the two media, or equivalently, to the opposite ratio of the indices of refraction (n2 / n1). Here n1 is 1 (refractive index of vacuum/air is one), hence refractive index of media is the ratio of the sines of the angle of incidence θ1 and angle of refraction θ2.
_
At the interface between two materials, the angle of refraction cannot be greater than 90°. When the angle of refraction is equal to 90°, the angle of incidence is called the critical angle. At any angle of incidence greater than the critical angle, the light cannot pass through the surface – it is all reflected.
_
The terms refraction and reflection describe two ways that waves, as of sound or light, change course upon encountering a boundary between two media. The media might consist of two different substances, such as glass and air, or a single substance in different states in different regions, such as air at different temperatures or densities in different layers. Reflection occurs, as in a mirror, when a wave encounters the boundary but does not pass into the second medium, instead immediately changing course and returning to the original medium, typically reflecting from the surface at the same angle at which it contacted it. Refraction occurs, as in a lens, when a wave passes from one medium into the second, deviating from the straight path it otherwise would have taken. The amount of deviation or “bending” depends on the indexes of refraction of each medium, determined by the relative speed of the wave in the two media. Waves entering a medium with a higher index of refraction are slowed, leaving the boundary and entering the second medium at a greater angle than the incident wave. Waves entering a medium with a lower index are accelerated and leave the boundary and enter the second medium at a lesser angle. Incident light waves tend to be fully reflected from a boundary met at a shallow angle; at a certain critical angle and at greater angles, some of the light is also refracted; looking at the surface of water from a boat, for instance, one can see down into the water only out to where the sight line reaches the critical angle with the surface. Light passing through a prism is mostly refracted, or bent, both when it enters the prism and again when it leaves the prism. Since the index of refraction in most substances also depends on the frequency of the wave, light of different colors is refracted by different amounts—hence the colorful rainbow effect of prisms. The boundary between media does not have to be abrupt for reflection or refraction to occur. On a hot day, the air directly over the surface of an asphalt road is warmer than the air higher up. Light travels more quickly in the lower region, so light coming down from the sky (from not too steep an angle) is refracted back up again, giving a “blue puddle” appearance to the asphalt—a mirage.
_
_
Dispersion:
In optics, dispersion is the phenomenon in which the phase velocity of a wave depends on its frequency. Chromatic dispersion is the change of index of refraction with wavelength. Generally the index decreases as wavelength increases, blue light traveling more slowly in the material than red light. Dispersion is the phenomenon which gives you the separation of colors in a prism. It also gives the generally undesirable chromatic aberration in lenses. Usually the dispersion of a material is characterized by measuring the index at the blue F line of hydrogen (486.1 nm), the yellow sodium D lines (589.3 nm), and the red hydrogen C line (656.3 nm). The dispersion is measured by a standard parameter known as Abbe’s number. Blue light travels more slowly than red light in transparent media. The effect of dispersion on the focal length of a lens can be examined by calculating the change in the focal length with wavelength. The table below starts with a biconvex lens designed to have a focal length of 10.0 cm for violet light (400 nm) in crown glass. The focal lengths shown are calculated from the lensmakers equation with radii of curvature 10.62 cm for both surfaces.
_
| Medium | Violet 400 nm |
Red 650 nm |
| Crown glass | 10.00 | 10.37 |
| Acrylic | 10.46 | 10.87 |
| Fused quartz | 11.30 | 11.58 |
_
In optics, one important and familiar consequence of dispersion is the change in the angle of refraction of different colors of light, as seen in the spectrum produced by a dispersive prism and in chromatic aberration of lenses. Design of compound achromatic lenses, in which chromatic aberration is largely cancelled, uses a quantification of a glass’s dispersion given by its Abbe number V, where lower Abbe numbers correspond to greater dispersion over the visible spectrum.
_
_
The indices of refraction of some common substances are given below. The values given are approximate and do not account for the small variation of index with light wavelength which is called dispersion.
| Material | n | Material | n |
| Vacuum | 1.000 | Ethyl alcohol | 1.362 |
| Air | 1.000277 | Glycerine | 1.473 |
| Water | 4/3 | Ice | 1.31 |
| Carbon disulfide | 1.63 | Polystyrene | 1.59 |
| Methylene iodide | 1.74 | Crown glass | 1.50-1.62 |
| Diamond | 2.417 | Flint glass | 1.57-1.75 |
_
In a nutshell, bending of light rays by a lens depends not only on its surface curvature and its material’s ability to bend (refract) light rays but also on frequency (or wave length) of incident light rays. Greater the wave length of light, lesser the bending of waves.
______
______
Anatomy and physiology of vision:
The eye is not a single frame snapshot camera. It is more like a video stream. The eye moves rapidly in small angular amounts and continually updates the image in one’s brain to “paint” the detail. We also have two eyes, and our brains combine the signals to increase the resolution further. We also typically move our eyes around the scene to gather more information. Because of these factors, the eye plus brain assembles a higher resolution image than possible with the number of photoreceptors in the retina.
_
Eye anatomy:
_
The eye is our organ of sight. The eye has a number of components which include but are not limited to the cornea, iris, pupil, lens, retina, macula, optic nerve, choroid and vitreous.
•Cornea: clear front window of the eye that transmits and focuses light into the eye.
•Iris: colored part of the eye that helps regulate the amount of light that enters
•Pupil: dark aperture in the iris that determines how much light is let into the eye
•Lens: transparent structure inside the eye that focuses light rays onto the retina
•Retina: nerve layer that lines the back of the eye, senses light, and creates electrical impulses that travel through the optic nerve to the brain
•Macula: small central area in the retina that contains special light-sensitive cells and allows us to see fine details clearly
•Optic nerve: connects the eye to the brain and carries the electrical impulses formed by the retina to the visual cortex of the brain
•Vitreous: clear, jelly-like substance that fills the middle of the eye
_
The eye is like a camera. The front of the eye is called the cornea. It is a clear structure that allows light into the eye, much like a watch crystal, and also begins the process of focusing the light. Inside the eye, behind the cornea, is the iris. This is the part of the eye which gives it color, such as blue or brown. The iris controls how much light enters the eye depending on the brightness of the environment. It does this by opening and closing the small hole in its center, the pupil. The functions of the pupil are to produce sharp images, especially in close work; to alter the depth of field; and to help regulate the amount of light striking the retina. Behind the iris and pupil is the focusing lens of the eye. This lens completes the focusing of light. It is flexible and allows the eye to focus at different distances. After passing through these structures at the front of the eye, the focused light forms an image on the retina, a layer of tissue on the back of the eye, analogous to the film of a camera. If the image is not focused on the retina correctly, then the image is blurred and a refractive error is present. The major components of the visual system can be broken up into visual acuity, depth perception, color sensitivity, and light sensitivity.
_
The visual system provides a supremely efficient means for the rapid assimilation of information from the environment to aid in the guidance of behavior. The act of seeing begins with the capture of images focused by the cornea and lens on a light-sensitive membrane in the back of the eye called the retina. The retina is actually part of the brain, banished to the periphery to serve as a transducer for the conversion of patterns of light energy into neuronal signals. Light is absorbed by photopigment in two types of receptors: rods and cones. The retina is a mosaic of two basic types of photoreceptors: rods, and cones. Rods are sensitive to blue-green light with peak sensitivity at a wavelength of 498 nm, and are used for vision under dark or dim conditions. There are three types of cones that give us our basic color vision: L-cones (red) with a peak sensitivity of 564 nm, M-cones (green) with a peak sensitivity of 533 nm, and S-cones (blue) with a peak sensitivity of 437 nm. Cones are highly concentrated in a region near the center of the retina called the fovea region. The maximum concentration of cones is roughly 180,000 per square mm in the fovea region and this density decreases rapidly outside of the fovea to a value of less than 5,000 per square mm. Note the blind spot caused by the optic nerve which is void of any photoreceptors. In the human retina there are 100 million rods and 5 million cones. The rods operate in dim (scotopic) illumination. The cones function under daylight (photopic) conditions. The cone system is specialized for color perception and high spatial resolution. The majority of cones are within the macula, the portion of the retina that serves the central 10° of vision. In the middle of the macula a small pit termed the fovea, packed exclusively with cones, provides the best visual acuity.
_
| Comparison of Peripheral and Foveal Retina | ||
| Property | Foveal Retina | Peripheral Retina |
| Threshold | Relatively high | Exquisitely low |
| Receptor distribution | Cones only | Rods and cones |
| Convergence | Limited or none in fovea; probably more elsewhere | Extensive |
| Illumination | Photopic (Daylight) | Scotopic (Night) |
| Functions | Central vision Color vision Detail vision |
Peripheral vision Achromatic vision Poor detail vision |
_
Photoreceptors hyperpolarize in response to light, activating bipolar, amacrine, and horizontal cells in the inner nuclear layer. After processing of photoreceptor responses by this complex retinal circuit, the flow of sensory information ultimately converges on a final common pathway: the ganglion cells. These cells translate the visual image impinging on the retina into a continuously varying barrage of action potentials that propagates along the primary optic pathway to visual centers within the brain. There are a million ganglion cells in each retina and hence a million fibers in each optic nerve.
_
Ganglion cell axons sweep along the inner surface of the retina in the nerve fiber layer, exit the eye at the optic disc, and travel through the optic nerve, optic chiasm, and optic tract to reach targets in the brain. The majority of fibers synapse on cells in the lateral geniculate body, a thalamic relay station. Cells in the lateral geniculate body project in turn to the primary visual cortex. This massive afferent retinogeniculocortical sensory pathway provides the neural substrate for visual perception. Although the lateral geniculate body is the main target of the retina, separate classes of ganglion cells project to other subcortical visual nuclei involved in different functions. Ganglion cells that mediate pupillary constriction and circadian rhythms are light sensitive owing to a novel visual pigment, melanopsin. Pupil responses are mediated by input to the pretectal olivary nuclei in the midbrain. The pretectal nuclei send their output to the Edinger-Westphal nuclei, which in turn provide parasympathetic innervation to the iris sphincter via an interneuron in the ciliary ganglion. Circadian rhythms are timed by a retinal projection to the suprachiasmatic nucleus. Visual orientation and eye movements are served by retinal input to the superior colliculus. Gaze stabilization and optokinetic reflexes are governed by a group of small retinal targets known collectively as the brainstem accessory optic system.
_
The eyes must be rotated constantly within their orbits to place and maintain targets of visual interest on the fovea. This activity, called foveation, or looking, is governed by an elaborate efferent motor system. Each eye is moved by six extraocular muscles that are supplied by cranial nerves from the oculomotor (III), trochlear (IV), and abducens (VI) nuclei. Activity in these ocular motor nuclei is coordinated by pontine and midbrain mechanisms for smooth pursuit, saccades, and gaze stabilization during head and body movements. Large regions of the frontal and parietooccipital cortex control these brainstem eye movement centers by providing descending supranuclear input.
_
The eye of humans and of most, if not all primates, has an area of central vision. This is the part we use when we read. Or when we focus on stuff. The number of visual receptors, and in particular, color visual receptors, is more crowded in the portion of the retina that resolves things for fine vision. Around that we have a ring of area which is less good at seeing color and fine detail. It has more rods than cones. If, for example, you are meteor watching, you are more likely to glimpse a meteor with your peripheral vision than you are with your central vision because peripheral vision is more sensitive to distinguishing light from dark. But you will then focus on the meteor because your peripheral visions isn’t any good at fine detail.
_
Let me discuss vision when observing stars on a night sky. The first stage is the optical imaging of the outside world on the retina. Light impinges on the mosaic of receptor sense cells, rods and cones, which covers the retinal surface without gaps or overlap, just like the detecting pixels in the film plane of digital cameras. Each receptor accepts all the light reaching it but acts as a unit, representing a single location in visual space. This compartmentalization sets a limit to the decision whether an image came from a single or a double star (resolution). For a percept of separately articulated stars to emerge, the images of the two must be wide enough apart to leave at least one intervening pixel relatively unstimulated between them. This defines the resolution limit and the basis of visual acuity.
_
The purpose of the eye-globe is to receive light from the outside world and transmit it to the brain for processing. There are two aspects to this function. In the first instance, the light rays have to be correctly focused on to the back of the eye. Then, this information has to be converted to electrochemical signals by the cells within the retina and transmitted to the brain. In optical physics, the term ‘refraction’ is used to describe the bending of light rays as they pass across a particular medium. Refraction – whether by natural eye tissue or of an artificial lens – is measured in dioptres (D) which describes the power that a structure has to focus parallel rays of light. The higher this value, the stronger it’s focusing ability. In the eye, refraction happens at the air/tear interface on the surface of the cornea (the most important site of ray refraction), by the cornea and by the lens. The accuracy of this process depends on:
•The integrity of these structures.
•The shapes of the cornea and lens.
•The depth of the anterior chamber of the eye.
•The length of the eye from front to back (the axial length).
These four elements change over time as the eye grows (e.g., axial length) and matures in later years (e.g., quality of tears which affects the air-tear interface). The emmetropic eye is able to achieve a perfect focus. Ametropia is the global term referring to any refractive error. Refractive development is influenced by both environmental and genetic factors.
_
Visual acuity:
Visual acuity is the term used to describe the smallest detail a person can see when looking straight at a stationary, high contrast (e.g. black on white) target in good lighting. The sharpness of our senses is defined by the finest detail we can discriminate. Visual acuity is measured by the smallest letters that can be distinguished on a chart and is governed by the anatomical spacing of the mosaic of sensory elements on the retina. Yet spatial distinctions can be made on a finer scale still: misalignment of borders can be detected with a precision up to 10 times better than visual acuity. This hyperacuity, transcending by far the size limits set by the retinal ‘pixels’, depends on sophisticated information processing in the brain. Visual acuity, the sharpness of the eye to fine detail, is a major component of a human’s visual system. It requires not only the muscles of the eye – the muscles of orbit and the ciliary muscles – to be able to focus on a particular object through contraction and relaxation, but other parts of the retina such of the fovea to project a clear image on the retina.
_
For the smallest point to be detected or the finest detail to be resolved, requires a good optical system and appropriately spaced detectors. Visual acuity (VA) is acuteness or clearness of vision. It depends on optical and neural factors, i.e., (i) the sharpness of the retinal focus within the eye, (ii) the intactness and functioning of the retina, and (iii) the sensitivity of the interpretative faculty of the brain. Visual acuity will be limited by one of these. Apart from these main limiting factors, visual acuity also depends on a number of factors including:
•Refractive error
•Size of the pupil
•Illumination
•Time of exposure of the target
•Area of the retina stimulated
•State of adaptation of the eye
•Eye movement
_
A common cause of low visual acuity is refractive error (ametropia), or errors in how the light is refracted in the eyeball. Causes of refractive errors include aberrations in the shape of the eyeball, the shape of the cornea, and reduced flexibility of the lens. In the case of pseudomyopia, the aberrations are caused by muscle spasms. Too high or too low refractive error (in relation to the length of the eyeball) is the cause of nearsightedness (myopia) or farsightedness (hyperopia) (normal refractive status is referred to as emmetropia). Other optical causes are astigmatism or more complex corneal irregularities. These anomalies can mostly be corrected by optical means (such as eyeglasses, contact lenses, laser surgery, etc.).
_
Neural factors that limit acuity are located in the retina or the brain (or the pathway leading there). Examples for the first are a detached retina and macular degeneration, to name just two. A common impairment amblyopia caused by incorrect nerve pathway function connecting eye with brain is involved. In some cases, low visual acuity is caused by brain damage, such as from traumatic brain injury or stroke. When optical factors are corrected for, acuity can be considered as being a measure of neural well-functioning.
_
Visual Field:
The human visual system does not just see the world in front of them, but is aware of things to the side and above and below them. This is called the visual field, and means that when we look straight head we are aware of things greater than 180 degrees horizontally, and approximately 70 degrees above and 80 degrees below us. We do not pay attention to all the things in our visual field at once, but select the important things to pay attention to. The visual field is very important for moving through environments and not being surprised by things coming from the side of our vision.
_
Contrast Sensitivity:
This is the ability of the visual system to detect subtle changes in contrast.
_
Crowding:
This is the ability of the visual system to interpret the visual environment and be able to pay attention to the things that matter within the environment, and perhaps visually ignore some other objects. This selective visual attention is important so we are not overwhelmed by all we ’see’. Some children with difficulties in visual processing can find complexity and crowding within visual scenes challenging.
_
Accommodation:
Accommodation is the adjustment of the refractive power of the lens of the eye to achieve an exact image of the object on the retina. This is the focusing ability of the eye. Accommodation is the ability of the eye to change the refractive power of the lens to automatically focus on objects at various distances. It is a complex constellation of sensory, neuromuscular and biophysical phenomena by which the overall refracting power of the eye changes rapidly to image objects at different viewing distances clearly on to the retina. The stimulus to accomodation is a blurred retinal image. It is part of the Near Reaction that involves accomodation along with convergence and pupillary constriction. The eye has a crystalline lens which can increase/decrease in power to ensure accurate focus for objects and different distances. The eye has internal eye muscles (ciliary muscles) which make the crystalline lens change shape. This process is called ocular accommodation and can only happen if the ciliary muscles are functioning normally and if the crystalline lens is intact and flexible. If the crystalline lens has been removed, is not positioned correctly, is rigid, or if the muscles are not functioning optimally, the eye may not be able to change focus to accommodate. Even when the crystalline lens and muscles are essentially normal, it can be difficult for some children to focus accurately or cannot sustain accurate accommodation. If the child also has an uncorrected hyperopic refractive error, this compounds the problem.
_
Tonic accommodation:
It is now well established that accommodation adopts an intermediate resting position in the absence of visual stimulation. It is also called dark focus of accommodation, or tonic accommodation, or resting state of accommodation. The reason for tonic accomodation is some basic residual accommodation, as stated by Leibowitz et al.: “the focus of the eye tends to return passively to an individually characteristic intermediate resting position or dark-focus whenever the stimulus to accommodation is degraded or when the quality of the image is independent of focus.” Tonic accommodation is the resting position of the accommodative system in the absence of compelling visual stimuli. It is generally reported to have a range of 0.50 D to 4.00 D, with a mean of approximately 1.50 D in adults. Tonic accommodation and its adaptation (how it changes after active accommodation) have attracted considerable interest in recent years as a putative risk factor for myopia and have been studied widely as a function of refractive error. An association between tonic accommodation, the resting accommodative position of the eye in the absence of a visually compelling stimulus, and refractive error has been reported in adults and children. In general, myopes have the lowest (or least myopic) levels of tonic accommodation. In early studies, it was shown that emmetropes had significantly higher (i.e., more myopic) values of tonic accommodation than did high myopes. Later, distinctions were drawn within the subgroup of myopia, and hyperopes were examined. Juvenile-onset myopes and emmetropes had similar tonic accommodation values, whereas hyperopes had higher tonic accommodation values, and adult-onset myopes had lower tonic accommodation values. Similar relations have been shown in children, with tonic accommodation values progressing from highest in hyperopes, to intermediate in emmetropes, to lowest in juvenile-onset myopes.
_
The definition of presbyopia is fluid because there is no standard distance for near work. The age at which patients seek help for presbyopic symptoms vary and it is not unusual to see patients even in their late forties, not wearing presbyopic lenses. This variability could be either real, due to variable preservation of accommodative ability or artifactual. Symptoms of presbyopia itself can be dependent on other factors like the amount of near work done, lighting conditions, corrected distance acuity etc. It is well known that the myopes seek help for presbyopic symptoms much later than the rest. It could be due to the fact that these individuals remove their glasses for near work; the under correction prescribed for myopes delays presbyopic symptoms; or myopes preserve their accommodation for longer periods. There is also a suggestion that near work and thereby increased accommodative effort or capability is a major factor in the development of simple myopia. Corrected hyperopes have a lower effective accommodation compared to emmetropes and will need near addition at a younger age. Hyperopes are thus more symptomatic earlier than emmetropes or myopes.
________
Focusing on retina:
In geometrical optics, a focus, also called an image point, is the point where light rays originating from a point on the object converge. An image, or image point or region, is in focus if light from object points is converged almost as much as possible in the image, and out of focus if light is not well converged.
_
Eye focusing ideally collects all light rays from a point on an object into a corresponding point on the retina.
Note that inverted image is formed on retina and brain interprets it as upright image. Since the crystalline lens is a convex spherical lens it forms inverted images on the retina (every converging lens forms inverted images). The inverted information follows through the optical nerves until the occipital cerebral cortex that contains the visual area of the brain. In the brain the interpretation of the image takes place and the inverted information is reverted.
_
The figure below shows image partially in focus and partially out of focus.
_
Range of focus:
You must understand how the normal eye functions. When viewing things in the distance (6 meter and beyond are optically equal), the normal eye is relaxed and focused. The light rays entering the eye are parallel, and the relaxed eye converges those parallel rays, bringing them into focus on the retina. When the eye shifts its gaze to anything inside 20 feet, the rays of light begin to diverge, or open up, which pushes the focal point to somewhere behind the normal relaxed eye [discussed vide supra]. The eye then has to accommodate, or shift focus, to keep the near object in focus. This happens when an internal muscle called the cilliary body activates and changes the shape of the crystalline lens that sits behind your pupil. This accommodation pulls the long-focused rays back into focus on the retina. And it all happens faster, and more fluidly than you can perceive, without conscious effort on your part. The normal eye uses about 2.50 diopters of accommodative power to see things at the normal reading distance (30 cm).
_
Just as camera has range of focus, eyes also have range of focus. Range of focus is a distance within which camera/eyes can make a clear image on film/retina. Normal eyes can see objects clearly between infinity (distance vision) and 30 cm (near vision). As discussed earlier, optical infinity is 6 meter (20 feet).
As you can see in the figure below, range of focus changes in refractive errors.
_
_
In myopia the near point and the far point of vision come closer. In hyperopia the near point becomes more distant and far point is in fact behind retina.
_
Far point and near point:
1. Far Point is the farthest an eye can see clearly. For emmetrope it is optical infinity or 20 feet (6 meter) as seen in the figure above. Far point is the point on the visual axis conjugate to the retina when accommodation is completely relaxed. Far point in 4.00D myope without glasses it is 25cm in front of the eye; 1.00D myope without glasses it is 1meter in front of the eye; 3.00D hyperope without glasses 33.3 cm behind the eye. When you give them corrective glasses, their far point would become 6 meter.
2. Near Point is the closest the eye can see clearly. In optics, the closest point at which an object can be brought into focus by the eye is called the eye’s near point. For emmetrope, it is 30 cm as seen in the figure above. Near point is the point conjugate to the retina when accommodation is maximally exerted. The near point is the sum of the power of the eye and accommodation. In other words, power for near point is sum of power for far point plus power of accommodation. An emmetrope with 10.00D of accommodation and a -4.00D error without glasses has a near point of 14.00D or 7.15cm in front of the eye.
3. A 50 year old with 2.00D of accommodation and a -1.00D error without glasses has a far point of 1 meter and a near point of 33.3 cm. With glasses on, the far point is infinity or 20 feet and the near point is 50cm in front of the eye. A +3.00D without glasses hyperope with 6.00D of accommodation has a far point of 33.3 cm behind the eye and a near point of 33.3 cm in front of the eye. With glasses on, the far point is infinity (6 meter) and the near point 16.6 cm.
4. To bring near point to 30 cm after correcting myopia/hyperopia/astigmatism, additional lens will be needed if accommodative power is less than 3 diopters.
5. Remember; a myope has too much plus in their eyes whereas a hyperope has too much minus. Accommodation power means addition of plus lens. Also diopter is inverse of focal length in meter (vide infra).
6. Amplitude of accommodation (AA) is the amount of accommodation exerted to move the focus from the far point to the near point. It decreases from childhood to 65 years. In humans, the total optical power of the relaxed eye is approximately 60 dioptres. The cornea accounts for approximately two thirds of this refractive power (about 40 dioptres) and the crystalline lens contributes the remaining third (about 20 dioptres). In focusing, the ciliary muscle contracts to reduce the tension or stress transferred to the lens by the suspensory ligaments. This results in increased convexity of the lens which in turn increases the optical power of the eye. As humans age, the amplitude of accommodation reduces from approximately 15 to 20 dioptres in the very young, to about 10 dioptres at age 25, to around 1 dioptre at 50 and over.
_
Evolutionary biologically, human eyes are tuned for distant vision in order to search for food and detect predators. Tens of thousands of years ago, there was no reading and no writing, so near vision (accommodation) was hardly used except for eating and sex. Therefore in humans, visual system is devised predominantly for distant vision and not near vision. Whenever myopia/ hyperopia/ astigmatism is measured and corrected, it is for distant vision. That means after correction by lens, far point will become infinity (6 meter). For near vision, additional correction is done to bring near point to 30 cm if accommodation power of eye is less than 3 diopters (<+3). Therefore the same corrective lens cannot be used for distant and near vision when myopia/hyperopia/astigmatism is associated with presbyopia, and hence bifocal or progressive lens is used.
_
Defocus:
In optics, defocus is the aberration in which an image is simply out of focus. This aberration is familiar to anyone who has used a camera, videocamera, microscope, telescope, or binoculars. Optically, defocus refers to a translation along the optical axis away from the plane or surface of best focus. In general, defocus reduces the sharpness and contrast of the image. What should be sharp, high-contrast edges in a scene become gradual transitions. Fine detail in the scene is blurred or even becomes invisible. Nearly all image-forming optical devices incorporate some form of focus adjustment to minimize defocus and maximize image quality. Any object placed out of range of focus of eyes will lead to defocus.
_
Refraction and the Eye:
Refraction is the phenomenon which makes image formation possible by the eye as well as by cameras and other systems of lenses. Most of that refraction in the eye takes place at the first surface, since the transition from the air into the cornea is the largest change in index of refraction which the light experiences. About 80% of the refraction occurs in the cornea and about 20% in the inner crystalline lens. While the inner lens is the smaller portion of the refraction, it is the total source of the ability to accommodate the focus of the eye for the viewing of close objects. For the normal eye, the inner lens can change the total focal length of the eye by 7-8%. Common eye defects are often called “refractive errors” and they can usually be corrected by relatively simple compensating lenses.
_
Refractive power of eye:
Although the eye consists of 14 optical components, total refraction of the eye is the product of only 6: corneal curvature, anterior chamber depth, thickness of the lens, anterior and posterior curvatures of the lens, and axial length. Corneal curvature, power of the crystalline lens, and axial length are believed to exert the greatest influence on ametropia. Several population studies have demonstrated that the values of each optical component are distributed in a normal binomial curve. The cornea contributes to approximately 2/3 of the refracting power of the eye along with the tear film. It contributes +43 diopters. The lens contributes to 1/3 of the refractive power of the eye (+ 20 diopters). By itself it is more powerful than the cornea as a convergent surface but because of less difference in indices of refraction between the aqueous versus the cornea, less convergence exists at the level of the lens. The total convergence power of the eye is 58.7D and not 43 + 20 = 63D due to the distance between the cornea and the lens (depth of the anterior chamber) that will subtract approximately 4D. This is the calculation of refractive power of eye with accommodation relaxed. However, when accommodation is exerted, refractive power of eye will increase depending on accommodation power.
_
Focal length of eye: axial length of eye:
The eye focuses on an object by bending all of the light rays from a single point on the observed object toward a single point on the retina. In the eyeball, light rays passing through the cornea are bent by its curvature toward the pupil. The lens flexes to change its curvature and finish the focusing process. When an object is located at infinity, the focal length, or the distance from the cornea to the retina, of a normal relaxed eye is about 22 mm. Stenstrom determined the axial length of the eyeball radiologically in 1,000 eyes. Although there was a slight tendency for longer axes to produce myopia and shorter axes to produce hyperopia, the length of the axes varied within the same limits in different types of refraction. Thus, if axial length remained constant, the different combinations of variable but normal measurements for the first three optical components could render a total refraction ranging from +6 to -9 diopters!
___________
__________
Lens:
A lens is a transmissive optical device which affects the focusing of a light beam through refraction. Lenses are solids made of some transparent material, with curved surfaces. A simple lens consists of a single piece of material, while a compound lens consists of several simple lenses (elements), usually along a common axis. Lenses are made from transparent materials such as glass, ground and polished to a desired shape. A lens can be used to focus light to form an image, unlike a prism which refracts light without focusing. Devices which similarly refract radiation other than visible light are also called lenses, such as microwave lenses or acoustic lenses. Lenses came into widespread use in Europe with the invention of spectacles, probably in Italy in the 1280s.This was the start of the optical industry of grinding and polishing lenses for spectacles, first in Venice and Florence in the thirteenth century, and later in the spectacle-making centers in both the Netherlands and Germany. Spectacle makers created improved types of lenses for the correction of vision based more on empirical knowledge gained from observing the effects of the lenses (probably without the knowledge of the rudimentary optical theory of the day).
_
Most lenses are spherical lenses: their two surfaces are parts of the surfaces of spheres. Each surface can be convex (bulging outwards from the lens), concave (depressed into the lens), or planar (flat). The line joining the centers of the spheres making up the lens surfaces is called the axis of the lens. Typically the lens axis passes through the physical centre of the lens, because of the way they are manufactured. Lenses may be cut or ground after manufacturing to give them a different shape or size. The lens axis may then not pass through the physical centre of the lens. Toric or sphero-cylindrical lenses have surfaces with two different radii of curvature in two orthogonal planes. They have a different focal power in different meridians. This forms an astigmatic lens. An example is eyeglass lenses that are used to correct astigmatism in someone’s eye. More complex are aspheric lenses. These are lenses where one or both surfaces have a shape that is neither spherical nor cylindrical. The more complicated shapes allow such lenses to form images with less aberration than standard simple lenses, but they are more difficult and expensive to produce.
_
Some terms used in connection with lenses:
_
Principal axis: A line which passes through the center of the lens, perpendicular to the lens surface. Lines X-Y in the diagrams above illustrate the principal axes of the lenses.
_
Optical centre: This is a point on the principal axis of a lens through which light passes without undergoing any deviation. In other words, a ray of light passing through the optical center will not change its direction. For thin lenses whose faces have the same curvature, this point, marked O in the diagram, is in the center of the lens.
_
Principal focus or focal point: This is a point, marked F in the diagram above, to which all rays parallel to the principal axis converge (in the case of a convex lens), or (in the case of a concave lens) from which the rays appear to diverge.
_
Focal length of lens: This is the distance between the optical centre and the principal focus. In the diagram above, it is the distance OF. For a thin double convex lens, refraction acts to focus all parallel rays to a point referred to as the principal focal point. The distance from the lens to that point is the principal focal length f of the lens. For a double concave lens where the rays are diverged, the principal focal length is the distance at which the back-projected rays would come together and it is given a negative sign. The lens strength in diopters is defined as the inverse of the focal length in meters. For a thick lens made from spherical surfaces, unequal refraction of light by different parts of the lens is called spherical aberration. The focal length for different wavelengths will also differ slightly, and this is called chromatic aberration. The principal focal length of a lens is determined by the index of refraction of the glass, the radii of curvature of the surfaces, and the medium in which the lens resides.
_
Principal focal plane: An imaginary plane located at the principal focus, perpendicular to the principal axis.
_
Lenses are classified by the curvature of the two optical surfaces. A lens is biconvex (or double convex, or just convex) if both surfaces are convex. If both surfaces have the same radius of curvature, the lens is equiconvex. A lens with two concave surfaces is biconcave (or just concave). If one of the surfaces is flat, the lens is plano-convex or plano-concave depending on the curvature of the other surface. A lens with one convex and one concave side is convex-concave or meniscus. It is this type of lens that is most commonly used in corrective lenses.
_
_
Plus lens:
If the lens is biconvex or plano-convex, a collimated beam of light passing through the lens will be converged (or focused) to a spot behind the lens. In this case, the lens is called a positive or converging lens. The distance from the lens to the spot is the focal length of the lens, which is commonly abbreviated f in diagrams and equations.
_
Minus lens:
If the lens is biconcave or plano-concave, a collimated beam of light passing through the lens is diverged (spread); the lens is thus called a negative or diverging lens. The beam after passing through the lens appears to be emanating from a particular point on the axis in front of the lens; the distance from this point to the lens is also known as the focal length, although it is negative with respect to the focal length of a converging lens.
_
Convex-concave (meniscus) lenses can be either positive or negative, depending on the relative curvatures of the two surfaces. A negative meniscus lens has a steeper concave surface and will be thinner at the centre than at the periphery. Conversely, a positive meniscus lens has a steeper convex surface and will be thicker at the centre than at the periphery. An ideal thin lens with two surfaces of equal curvature would have zero optical power, meaning that it would neither converge nor diverge light. All real lenses have nonzero thickness, however, which causes a real lens with identical curved surfaces to be slightly positive. To obtain exactly zero optical power, a meniscus lens must have slightly unequal curvatures to account for the effect of the lens’ thickness.
_
The reason that these plus and minus lenses are called spherical is that their surfaces are uniformly curved, like the surface of a sphere or round ball. [Further discussion on lenses later on in the article]
___
Diopter:
Diopter is a measurement of refractive power of lens or any refractive object (e.g. eyes). Diopter is also used to express the amount of nearsightedness (or farsightedness) a person has. Diopter is also used on the eyeglass prescription. See above figures of plus lens and minus lens. A plus lens converges parallel light rays to the principal focal point. The distance from the lens to that point is the principal focal length f of the lens. A minus lens diverges parallel light rays; the principal focal length is the distance at which the back-projected rays would come together. The refractive power of lens in diopter is the inverse of focal length in meters. If a lens was to focus light coming from optical infinity onto a point 2 meters away this would be a 1/2 diopter lens (1/2D = 2 meters). If the lens were to focus these rays at 50cm. this would be a 2 diopter lens [1/(1/2meters) = 2D]. This would be a stronger lens than the first. For plus or convex lens, diopter is assigned + sign (positive). For minus or concave lens, diopter is assigned – sign (negative). Positive diopter means converging rays and negative diopter means diverging rays.
_
Myopia (Nearsighted): The eye’s optical system needs to be about 59 diopters (D) to converge light onto the retina. If a particular eye system needs 60D to focus light on the retina but actually has 63D then you have a myopic eye. The amount of myopia here is easy to calculate: 63D – 60D = 3D of myopia. The eye will over-converge light by 3 diopters. The eye will need concave lens (minus lens) to correct over-convergence of light.
Hyperopia: The eye’s optical system needs to be about 59 diopters (D) to converge light onto the retina. If a particular eye needs 60D of power to focus light on the retina but actually has 57D then you have a hyperopic eye. The amount of hyperopia here is easy to calculate: 60D – 57D = 3D of hyperopia. The eye will under-converge light by 3 diopters. The eye will need convex lens (plus lens) to correct under-convergence of light.
_
-1 D corresponds with a focal distance of 1 m. People with myopia of -1.0 D can see still clearly at a distance of 1 m (at -2.0 D the distance is 0.5 m). The refractive power of the prescribed glasses is given in D with a minus in front. The nearsighted person who needs a -1 D lens to regain normal vision is said to have one diopter of myopia. A farsighted person would be said to have a refractive error of +1 D, +2 D, etc.
_
A nearsighted person who needs a –1.00 diopter lens can see objects at one metre clearly, but anything farther is blurred. Someone with a –2.00 diopter measurement requires a lens that is twice as powerful – so they can only see objects up to a 1/2 metre away clearly. A –3.00 lens would mean the person can only see a distance of up to 1/3 of a metre clearly, and so on. Most nearsighted people are in the range of -1.50 to -7.00 diopters, which is considered mild to moderate.
_
Convex lenses have positive dioptric value and are generally used to correct hyperopia (farsightedness) or to allow people with presbyopia (the limited accommodation of advancing age) to read at close range. Concave lenses have negative dioptric value and generally correct myopia (nearsightedness).
_
Diopters can be added together or subtracted from each other. In other words, three +1 D lenses are equal optically to one +3 D lens. A -4 D lens together with a +1 D lens is equivalent to a -3 D lens. The fact that optical powers are approximately additive enables an eye care professional to prescribe corrective lenses as a simple correction to the eye’s optical power, rather than doing a detailed analysis of the entire optical system (the eye and the lens). Optical power can also be used to adjust a basic prescription for reading. Thus an eye care professional, having determined that a myopic (nearsighted) person requires a basic correction of, say, −2 dioptres to restore normal distance vision, might then make a further prescription of ‘add 1’ for reading, to make up for lack of accommodation (ability to alter focus). This is the same as saying that −1 dioptre lenses are prescribed for reading.
_
The lenses used by the optical industry are usually made available in 0.25 D steps such as 1 D, 1.25 D, 1.5 D, 1.75 D, etc. Steps smaller than 0.25 D are seldom needed. Zero power lenses are called plano – that is, they are similar to window glass.
_
A prescription of -3 D means the far point is only 1/3 meter from the eyes. This 1/3 meter (33 1/3 centimeters) is the approximate distance at which most people hold a book. Expressed in another way, a -3 D myope (a person who needs -3 D lens for clear distance vision) who reads without glasses with the book held at 1/3 meter is reading without having to accommodate at all. The eyes are focused for distance. In theory, if the person never wore glasses, the myopia progression would stop at this amount since no accommodation is used. It is normally only the use of minus glasses that causes the myopia to increase beyond this amount (vide infra).
_
Refraction in Ophthalmology:
It is the determination of the optical state of the eye and the basis for prescribing glasses and contact lenses.
1. Ocular refraction:
The refraction of light produced by the media of the normal eye and resulting in the focusing of images upon the retina.
2. Binocular refraction:
A clinical procedure in which the subjective measurement of refraction of each eye is performed while both eyes are viewing a test. The visual examination is thus carried out under more natural conditions than when one eye is closed; the sizes of the pupils are similar and the accommodation-convergence relationship is maintained. There are various such methods; using polarized targets (e.g. Vectograph slides; Parallel-testing Infinity Balance test), using a septum (e.g. Turville Infinity Balance test), or fogging (e.g. Humphriss Immediate Contrast test). These methods give better results than refracting monocularly, especially in latent hyperopia, hyperopic anisometropia, pseudomyopia, cyclophoria, etc. and no additional step for binocular balancing is necessary.
3. Cycloplegic refraction:
Assessment of the refractive state of the eye when accommodation has been totally or partially paralysed by a cycloplegic (e.g. cyclopentolate 1% eyedrops, or atropine 0.5 or 1% ointment). This may be carried out in children to reveal the full extent of a hyperopia or in the initial assessment of accommodative esotropia, but only occasionally in adults as fogging methods usually suffice for them.
4. Double refraction:
The splitting of an incident ray into two (ordinary and extraordinary) by a birefringent medium.
5. Dynamic refraction:
Determination of the refractive state of the eye when accommodation is stimulated, as distinguished from static refraction which is the determination of the refractive state of the eye when accommodation is at rest or paralysed.
6. Laser refraction:
A method of subjective refraction in which the patient observes a slowly rotating drum, on the surface of which is perceived a speckle pattern resulting from illumination by a laser. The speckle pattern appears to move only when the eye is not focused for the fixation distance. If the perceived movement of the pattern is opposite to that of the drum, the eye is myopic and if the perceived movement of the pattern is in the same direction as the drum, the eye is hyperopic. Correction can be determined by placing a lens in front of the eye, which will neutralize the movement; at that point the eye is focused for the fixation distance. Astigmatism can be measured by rotating the drum in various meridians. The drum can be placed at infinity or at near (an allowance for the radius of curvature of the drum and the distance must then be made). This method can be useful for mass screening, especially children, as accommodation is not stimulated as much as with Snellen letters. It has been very useful as a research tool for accommodation studies where it is arranged as part of a Badal optometer.
7. Manifest refraction:
The refractive error or the process of determining it, when accommodation is at rest (but not paralysed).
8. Objective refraction:
Measurement of the refraction of the eye that is not based on the patient’s judgments, as when using an objective optometer or a retinoscope.
9. Subjective refraction:
Measurement of the refraction of the eye based on the patient’s judgments.
_
Significant refractive error:
< 6/12 in children in the better eye
< 6/18 in adults in the better eye
Myopia >= 0.50 Ds.[Ds means diopter spherical]
Astigmatism >= 1.50 Dcyl [Dcyl means diopter cylindrical]
Hyperopia >= 2.0 Ds (>=1.0 Ds in > 40 yrs)
Anisometropia >= 2.0 Ds (children)
____________
____________
History of refractive error and eyeglasses:
Refractive errors have been observed in the human race since antiquity. Indeed, the Emperor Nero was known to have observed the gladiator fights through an emerald. Historians debate the form of refractive error that afflicted the Roman emperor, since both concave and convex lenses were fashioned from glass or transparent gems during this period. Kepler was the first to define a form of ametropia when he identified myopia as a condition in 1611. At that time, he expressed the controversial belief that its cause lay in the accommodation and convergence required by near-work. This theory has been both supported and disputed by scholars for centuries.
_
___
No one really knows about the early history of image magnification. In ancient times, someone noticed that convex-shaped glass magnified images. Sometime between the year 1000 and 1250 crude technology began to develop regarding reading stones (simple magnifiers). English Franciscan Friar Roger Bacon (1220 -1292), in his 1268 ‘Opus Majus’, noted that letters could be seen better and larger when viewed through less than half a sphere of glass. Bacon’s experiments confirmed the principle of the convex (converging) lens, described by Alhazen (965-1038), “Father of modern optics”, Arabian mathematician, optician and astronomer at Cairo, and even earlier by the Greeks. Bacon recognized that this could assist weak eyes or the vision of aged persons. Early recorded evidence demonstrates that glasses first appeared in Pisa, Italy about the year 1286. Technically, they were formed from two primitive convex shaped glass/crystal stones. Each was surrounded by a frame and given a handle. These were then connected together through the ends of their handles by a rivet. They were not really an invention per se but instead a bright idea or “adaptation” of something used earlier – the simple glass stone magnifier. Essentially someone took two existing mounted stones and connected them with a rivet. Most likely, this first pair of glasses were invented by a lay person who wanted to keep the process a secret in order to make a profit. This individual was a true visionary (no pun intended). Two monks from the St. Catherine’s Monastery, Giordano da Rivalto and Alessandro della Spina, provide the earliest (primary source) documentation to support this fact. On Feb.23, 1306, Giordano mentioned them by stating in a sermon. “It is not yet twenty years since there was found the art of making eyeglasses which make for good vision, one of the best arts and most necessary that the world has.” He coined the word “Occhiale” (eyeglasses) and its use began to spread throughout Italy and Europe. Friar Spina’s 1313 obituary notice mentions, “When somebody else was the first to invent eyeglasses and was unwilling to communicate the invention to others, all by himself he made them and good-naturedly shared them with everybody.” Salvino D’Armato Degli Armati of Florence was at one time thought to be the inventor of eyeglasses but this claim has been proven to be totally false. Though roughly made, early spectacles were full of charm and rapidly became a symbol of wisdom and learning. Later glasses quickly became more technically sophisticated. One of the most important industries, the German spectacles industry, was formulated in 1535 with the issuance of regulations of the Nuremberg spectacle makers’ guild. In London in 1629, King Charles I granted a charter incorporating the Worshipful Company of Spectacle Makers. Unfortunately all of their earliest records were destroyed in the Great Fire of London in 1666 except for that charter. During most of the 17th century, Germany remained the center of spectacle making. Germans made the finest frames while the Italians made the highest quality lenses. The early lenses were still cloudy until manufacturing developed and flint was added to make the glass clearer. Genuine, original pre-1700 spectacles are exceedingly rare today and are highly treasured by museums and collectors alike. As the 20th century opened, eyeglass wearers emphasized style. The improved plastics in the early 1900’s heralded a new era in frame styling. During the 1930’s sunglasses became especially popular. By 1950, as described by Pierre Marly of France, spectacles had become a fashion accessory in Europe and North America. In Great Britain at that time, they were just starting to become an accessory. Eyeglass wearers demanded stylish, comfortable, and functional designs exhibiting both variety and elegance. They still do. Glasses have become an added refinement by which people can enhance their personality. Individuals can look smart and also discreet in a variety of designs and colors. In 1946, Vasco Ronchi of Florence stated “when it is all summed up, the fact remains that this world has found lenses on its nose without knowing whom to thank.” Bifocals (combining convex and concave lenses to correct both nearsightedness and farsightedness) were invented by Benjamin Franklin around 1775. Glasses with hinged arms were invented in 1752 by James Ayscough. Ayscough also made the first sunglasses (glasses with green- or blue-tinted lenses). A monocle is a type of corrective lens used to correct or enhance the vision in only one eye. It consists of a circular lens, generally with a wire ring around the circumference that can be attached to a string or wire. The other end of the string is then connected to the wearer’s clothing to avoid losing the monocle. Monocles were most prevalent in the late 19th century but are rarely worn today. This is due in large part to advances in optometry which allow for better measurement of refractive error, so that glasses and contact lenses can be prescribed with different strengths in each eye, and also in reaction to the stereotypes that became associated with them. Pince-nez is a style of glasses, popular in the 19th century, that are supported without earpieces, by pinching the bridge of the nose. The name comes from French pincer, “to pinch”, and nez, “nose”. Although pince-nez were used in Europe in the 15th, 16th, and 17th centuries, modern ones appeared in the 1840s and reached their peak popularity around 1880 to 1900.
_
The figure below depicts evolution of refractive error correction from spectacles to intraocular lens (IOL):
______
Refractive error in animals:
Some animals suffer from shortsightedness and have poor eyesight. In domestic animals, myopia, with or without astigmatism, occurs frequently. Whereas the rhinoceros may suffer from less-than-adequate eyesight, it generally survives by concentrating with its superior hearing and sense of smell. Some reports, however state that it can see better when focusing with one eye, particularly when walking, posturing, and combating. Myopia, with or without astigmatism, is the most common eye condition in horses. Several types of occlusion myopia have been recorded in tree shrews, macaques, cats and rats, deciphered from several animal-inducing myopia models. Preliminary laboratory investigations using retinoscopy of 240 dogs found myopic problems with varying degrees of refraction errors depending on the breed. In cases involving German Shepherd, Rottweiler and Miniature, the refraction errors were indicative of myopia. Nuclear sclerosis of the crystalline lens was noticed in older dogs. Levinsohn argues that the bending forward of the head and neck is an essential factor in the development of myopia. Experiments into newborn macaque monkeys have revealed that surgically fusing the eyelid for one year results in eye deterioration as the eye has not had a chance to grow and develop. Keeping monkeys in the dark for a similar period, however, does not lead to myopia. In 1996, Maurice and Mushin conducted tests on rabbits by raising their body temperatures and intraocular pressures (IOP) and noted that while younger rabbits were prone to developing myopia, older rabbits were not. Some tests have revealed that myopia in some animals can be improved with eye drops containing zinc, by increasing the activity of superoxide dismutase (SOD). The rhesus monkey’s vision amplitude reduction is noticeable in its second decade of life; however the condition does not impede normal functioning. Older rhesus monkeys have more difficulty accommodating this reduction in vision amplitude, encountering difficulty in focusing on objects at close range, even objects on the ground within an arm’s length. In Central Park Zoo, New York, several myopic animals have been reported, including a 39-year-old elephant, a Cape buffalo, and some monkeys. Young elephants and other animals are said to be myopia free. Pet dogs with progressive myopia have been reported.
__________
_________
Epidemiology of refractive error:
The global prevalence of refractive errors has been estimated from 800 million to 2.3 billion. Global estimates indicate that more than 2.3 billion people in the world suffer from poor vision due to refractive error (RE). REs are the most common forms of eye disorders that result in poor vision and have severe social and economic implications if uncorrected. A RE can simply be diagnosed, measured, and corrected with the aid of optical corrective approaches and devices such as spectacles and contact lenses or by refractive surgical procedures. Despite this, an estimated 670 million people worldwide do not have spectacles or have inadequate correction; 517 million have near vision impairment and 153 million have distance vision impairment. Of the 517 million people without spectacles for near vision correction, 410 million are prevented from performing near vision tasks and activities. Current data suggests that more than 90% of people with uncorrected RE, worldwide, reside in rural and low-income countries.
_
Myopia, the most common form of refractive error, has a prevalence of about 10-30% in most Western countries, but this figure is as high as 80% in parts of Asia. While presbyopia most often begins after 40 years of age in Western countries, studies have shown that it starts earlier and is more severe in Africa compared to Europe and North America. These studies have shown that in developing countries, more than 50% of adults older than 30 years suffer from presbyopia. Furthermore, presbyopia is more common and more severe in women than in men. The prevalence of astigmatism may be as high as 70 per cent, if all amounts are included, but is considered to decrease to 3 percent if the extent is limited to 1.25 diopters or more. Poor vision in children as a result of uncorrected refractive errors is a pressing public health concern in countries like China, where about six million children have such errors. In 2010, it was estimated that 123 million people had significant vision impairment (< 6/18 in the better eye) due to uncorrected refractive errors affecting distance vision, including at least eight million people with blindness (< 3/60 in the better eye). In addition, 517 million people were without adequate correction for functional presbyopia in 2005 estimate.
_
The figure below shows number of people with refractive error per 100,000 people in 2004 worldwide:
India, Bangladesh, Pakistan and china have highest number of people with refractive error.
_
In France, 39% of the population is estimated to suffer from myopia, 15% from astigmatism, 9% from hyperopia, and 26% to 30% from presbyopia. Myopia seems to be less common in Europe than in Asia, where 84% of the population in Hong Kong and Taiwan appear to be affected. Australian aborigines represent the other extreme, with less than 5% experiencing myopia. Hyperopia affects 9.9% of Americans, 11.6% of Western Europeans, and 5.8% of Australians aged 40 years or older. According to Matsumura, myopia is the most common ocular disorder in Japan, affecting, at some ages, 65.6% of individuals. In Brazil, hyperopia is the most frequent refractive error in children, varying between 60 and 70%, demonstrated in studies at the Campo Grande University Hospital, between 1996 and 1998. Some authors, in a sample of medical students in Singapore, discovered that 82% were myopic. In Norway as well as in Greece, myopia has also been the most common refractive error. Refractive errors affect approximately one third of persons 40 years or older in the United States and Western Europe, and one fifth of Australians in this age group. In the Western world some 15–20% of people are myopic and 40–50% hypermetropic, but in Japan and China 50–70% are myopic. The Jewish race has an excess of myopia, but Black African have more hyperopia than average.
_
A study found that myopia occurs more frequently in girls (7.4%) than in boys (5.1%) – p < 0.001. Hyperopia occurs more frequently in boys (19.6%) than in girls (18.2%) – p < 0.001. A slightly higher prevalence of astigmatism in girls (1.9%) than in boys (1.5%) was also observed (p > 0.05). Gender influences the occurrence of myopia and hyperopia in schoolchildren ranging from 6-18 years of age.
_
As for the proportion of an entire population with refractive error, Daniel Etyale of the W.H.O. reported at a special session on refractive error at an International Agency for Prevention of Blindness meeting in 2001, that 5 -15 percent of children are considered to have refractive errors, the majority of which are uncorrected, and that there is currently a need for population based studies to ascertain these figures. Although Vision 2020 (the current W.H.O. global initiative) imposes a mandate to correct refractive errors, little infrastructure and few resources are available to accomplish the task of correcting refractive errors. Etyale noted that while access to general medical services is possible for about 25 percent of populations in developing countries, access to medical eye care, including refraction, could be obtained by only about 10 percent.
_
American statistics:
Approximately 148 million people (52% of the population) in the United States wear some form of corrective eyewear.
Approximately 34 million people in the United States wear contact lenses.
Approximately 1.8 million refractive surgery procedures are performed in 2002.
Approximately 63 million people in the United States are candidates for refractive surgery.
Laser in-situ keratomileusis (LASIK) accounts for approximately 95 percent of all refractive surgeries.
Photorefractive keratectomy (PRK) accounts for approximately five percent of refractive surgeries.
_
Increased myopia worldwide:
Studies of ethnic Chinese in Taiwan documented an increase in the prevalence and severity of myopia over two generations. Genetics alone are unlikely to account for such a rapid change, although one study has speculated that genetic factors do not preclude such a change. A study of successive cohorts of enlistees in the Israeli army showed a marked increase in prevalence of myopia over a 13-year period. A study in Finland showed that the prevalence of myopia doubled among teenagers and young adults over the course of the 20th century. A study comparing U.S. population-based estimates in 1971 to 1972 and 1999 to 2004 also found a marked increase in the prevalence of myopia, although the reasons for this increase could not be identified.
_
Presbyopia estimate:
1.04 billion people globally
517 million of whom had no spectacles or inadequate spectacles.
410 million prevented from performing near tasks in the way required.
94% from less and least-developed countries
_
Measurements of refractive errors of large numbers of individuals, when plotted graphically to show their relative incidence, lie on a sharply-peaked curve compared with a theoretically derived ‘normal’ or ‘Gaussian’ distribution curve. Ninety-eight per cent of all refractions in one series of cases lay between +4 and –4 dioptres, and the number of emmetropes (normals) was greater than anticipated. Furthermore, the mean refractive level was at some +2 dioptres of hyperopia in infants, moving towards +1 dioptre by 25 years of age, with a similar distribution of relative values at all ages. There appears to be a definite tendency towards normalization of refraction (emmetropization), which implies highly accurate and coordinated control of growth of the cornea, the lens, and the whole eyeball. Interestingly, when refractive errors are present they are often closely similar in the two eyes, even down to the degree and axes of any astigmatism. Occasionally there is a large difference between the focusing of the two eyes, making correction difficult and with profound implications for the development of normal binocular vision.
_
Global magnitude of visual impairment caused by uncorrected refractive errors in 2004:
Estimates of the prevalence of visual impairment caused by uncorrected refractive errors in 2004 have been determined at regional and global levels for people aged 5 years and over from recent published and unpublished surveys. The estimates were based on the prevalence of visual acuity of less than 6/18 in the better eye with the currently available refractive correction that could be improved to equal to or better than 6/18 by refraction or pinhole. A total of 153 million people (range of uncertainty: 123 million to 184 million) are estimated to be visually impaired from uncorrected refractive errors, of whom eight million are blind. This cause of visual impairment has been overlooked in previous estimates that were based on best-corrected vision. Combined with the 161 million people visually impaired estimated in 2002 according to best-corrected vision, 314 million people are visually impaired from all causes: uncorrected refractive errors become the main cause of low vision and the second cause of blindness.
_
Uncorrected refractive errors are the second cause of blindness after cataract and the main cause of low vision: overall, they are the cause of almost half of all visual impairment.
_
Another estimate:
An estimated 180 million people worldwide are visibly disabled, of whom nearly 45 million are blind, four out of five of them live in developing countries. One third of the world’s blind (about 15 million) are in SEAR (South East Asian region) and 50 % of world’s blind children live in this region. Blindness is one of the most significant social problems in India with uncorrected refractive errors as the second major cause accounting for 19.7% of blindness and low vision. In India Adolescents constitute 23-25 % of the population. Poor vision in childhood affects performance in school or at work and has a negative influence on the future life of the child. The prevalence of myopia is currently attracting worldwide attention as many recent studies report dramatic increases over the last 20 years. Moreover, planning of a youth’s career is very much dependent on the visual acuity, especially in jobs for navy, military, railways and aviation. This warrants early detection and treatment of refractive errors to prevent permanent disability. Diagnosis and treatment of these errors is relatively simple and is one of the easiest ways to reduce impaired vision. Children do not complain of defective vision, and may not even be aware of their problem. They adjust to the poor eyesight by sitting near the blackboard, holding the books closer to their eyes, squeezing the eyes and even avoiding work requiring visual concentration. This warrants early detection and treatment to prevent permanent disability.
________
Eye growth and emmetropization:
The refractive state of the eye is determined by refractive components (corneal power, lens power, anterior chamber depth, and axial length) which are interdependent rather than independent variables, and that the eye grows during the early years in life in such a manner that the refractive state tends towards emmetropia. The refractive state of the human eye is dependent on the balance of change in overall eye size and refractive components, namely, the cornea and crystalline lens. The axial length (AL) is the distance from the corneal surface to an interference peak corresponding to the retinal pigment epithelium/Bruch’s membrane, and this is expressed in millimeters. Majority of eye growth takes place in the first 18 months of life after which there is little change. Overall the changes in axial length appear to outweigh the progressive corneal flattening with age in normal eyes; the majority of axial length elongation takes place in the first three to 6 months of life and a gradual reducing rate of growth over the next two years, and by three years the adult eye size is attained. The cornea is the most powerful refracting surface of the optical system of the eye, accounting for two-thirds of the eye’s focusing power. Production of a sharp image at the retinal receptors requires corneal transparency and appropriate refractive power. The refractive power of the cornea depends on its curvature and the difference in refractive indexes between it and air. The interaction between axial length and corneal radius of curvature (CRC) has played a major role in the compensatory adjustments of the optical components of the eye towards attaining emmetropic state. The axial length-corneal radius (AL/CR) ratio has been shown to give a better correlation with refractive error than is obtained with axial length alone. The process operating to produce greater frequency of emmetropia than would be expected on the basis of chance alone is termed emmetropization. Emmetropization mechanism is disturbed if degraded visual images reach the retina. The cornea has an average radius of curvature of 7.80 mm with an instrument calibrated for index of refraction of 1.3375. The report of Llorente and colleagues showed that axial length was significantly higher in myopes than hyperopes. Chen et al. also reported that eyes with more myopic refractive error tended to have greater axial length. Numerous studies have shown that axial length and corneal radius of curvature are interdependent variables and that the true refractive state can be assessed based on axial length-corneal radius of curvature index expressed as AL/CRC ratio. Myopes have been shown to have higher AL/CRC ratio than emmetropes and hyperopes. The inverse relationship between axial length and corneal radius of curvature supports the mechanism of emmetropization described by Grosvenor. He asserted that as the axial length increases tending to bring about myopia, the cornea tend to flatten bringing a decrease in myopia. This mechanism brings about a greater frequency of emmetropia than is expected on the basis of chance alone. The inverse correlation between axial length and corneal radius of curvature demonstrates the eye’s ability to compensate for normal physiologically driven axial length changes.
_____
Natural history of refractive error:
The distribution of refractive errors changes with age. Newborns average 3.00 D of hyperopia. This may increase slightly in the first few months, but then it declines toward an average of 1.00 D of hyperopia by 1 year of age. Fewer than 5% of infants have more than 3.00 D of hyperopia at age 1 year. This shift toward emmetropia is a complex process that involves changes in the power of the refractive components of the eye, including thinning of the crystalline lens. Visual stimulation appears to play a role in this process. Myopia typically appears between 6 and 12 years of age, and the mean rate of progression is approximately 0.50 D per year, based on studies of mostly Caucasian children. A study reported that progression of myopia varied by ethnicity and by age of the child. For ethnic Chinese children, the rate of progression is higher. Astigmatism in children is commonly oriented with the steep axis vertical (“with the rule”). In older adults, astigmatism oriented with the steep meridian horizontally is more common (“against the rule”) and remains relatively stable in older adults, although one study found that the axis of astigmatism tended to shift against the rule over a 5-year period. Individuals with high refractive errors are more likely to develop pathologic ocular changes over time. Highly myopic patients have an increased incidence of progressive elongation of the eye with progressive retinal thinning, peripheral retinal degeneration, retinal detachment, cataract, and glaucoma. An increased risk of glaucoma and visual field defects with myopia has also been found. An increased risk of developing primary angle-closure glaucoma among individuals with hyperopia has been reported. Refractive changes in adults over the age of 40, over a 10 year period, are small (<0.5D) and dependant on age (mild hyperopia in 40s, mild myopia in 70s.) This may also be dependent on the presence of cataract, which may induce a myopic shift in refraction.
______
______
Symptoms of Refractive Errors:
• Children can have difficulty in reading small letters on the blackboard
• Some children squeeze their eyes while trying to see distant objects like blackboard, television etc.
• Children hold books close to their face while reading
• Children with myopia have defective vision for distance and clear vision for near.
• They can experience eye strain while trying to read for long hours.
• Some children with hyperopia can present with squint.
• Children can develop swellings on the lids due to constant rubbing of the eyes to see things clearly.
• Eye pain and headache may occur.
The child should be immediately brought to an ophthalmologist, if any one of the above symptoms is observed.
_
Blurred vision is the most common symptom of refractive errors.
Other symptoms may include:
•Double vision
•Haziness
•Glare or halos around bright lights
•Squinting
•Headaches
•Eye strain
___
Refractive error and headache:
Headache and refractive errors are very common conditions in the general population, and those with headache often attribute their pain to a visual problem. The International Headache Society (IHS) criteria for the classification of headache include an entity of headache associated with refractive errors (HARE), but indicate that its importance is widely overestimated. Headache associated with refractive errors was rarely identified in individuals with refractive errors. In those with chronic headache, proper correction of refractive errors significantly improved headache complaints and did so primarily by decreasing the frequency of headache episodes.
_
The International Headache Society’s diagnostic criteria for headache attributed to refractive errors:
A. Recurrent mild headache, frontal and in the eyes themselves, fulfilling criteria C and D
B. Uncorrected or miscorrected refractive error (e.g., hyperopia, astigmatism, presbyopia, wearing of incorrect glasses)
C. Headache and eye pain first develop in close temporal relation to the refractive error, are absent on awakening and aggravated by prolonged visual tasks at the distance or angle where vision is impaired
D. Headache and eye pain resolve within 7 days, and do not recur, after full correction of the refractive error
_
In 2002 Gil-Gouveia and Martins reported an association between hyperopia and HARE in healthy subjects with uncorrected or miscorrected RE compared with a control group. Although in the literature several possible ophthalmic causes for headache are mentioned, it remains unclear how to explain a possible causal relation. In 1966, Gordon et al. claimed that minor RE often caused more headache and symptoms of eyestrain than major RE. Ciliary muscle strain has also been suggested as possible source of headache. Another proposed mechanism is “brow furrowing,” implying that prolonged contraction of the brow, scalp, and neck muscles in an attempt to maintain a clear image results in headache.
_
My view:
Headache and refractive errors are very common conditions affecting everybody and therefore their association by chance is far more likely than causal relationship. After seeing thousands of headache patients over last 27 years of my medical practice, I assert that most of them did not have refractive error as their cause of headache although lot of them did have refractive error coincidentally. In fact most of them turned out to be common migraine or tension headache or depression; and many of them were prescribed glasses without any relief in headache. It is rare to find a patient who says that his/her chronic headache is completely relieved by wearing glasses. Exceptions are uncorrected hyperopia where use of constant accommodation power to see distant objects may lead to ciliary muscle strain and headache since the eye’s close focusing power is not designed to remain constantly activated; and severe anisometropia where differing refractive states result in large differences in image sizes formed in the two eyes resulting in prolonged contraction of the brow, scalp, and neck muscles in an attempt to maintain a clear image results in headache. The key word is an attempt by a person to improve vision resulting in headache. In other words, if somebody ignores poor vision, he/she will not get headache no matter whatever the refractive error. In other words, uneducated and unintelligent people are unlikely to get headache due to refractive error. The same logic cannot apply for other refractive error like astigmatism because no matter how much person attempts using accommodation or scalp/neck muscles, clear image is not formed on retina and therefore person will not persists in attempting and will not get headache.
___________
___________
Refractive errors in detail:
_
Myopia:
Myopia literally meaning “trying to see like a mole”, commonly known as near-sightedness (American English) and short-sightedness (British English), is a condition of the eye where the light that comes in does not directly focus on the retina but in front of it, causing the image that one sees when looking at a distant object to be out of focus, but in focus when looking at a close object. Myopia (nearsightedness) is an ocular disorder in which the optical power of the eye is too strong for the corresponding axial length. Light rays from an object at infinity entering a non-accommodating myopic eye are converged too strongly and focus in front of the retina. The far point of a myope is located in front of the eye, between the cornea and optical infinity. Visual acuity of an uncorrected myope will continue to decrease as objects are located further away from the far point and closer to optical infinity. Conversely, visual acuity is greater for objects located between the far point of the eye and the near point of accommodation. Myopia is a significant, prevalent disease in children with increasing rates of progression. With over 80 million reported myopic children worldwide there are considerable socioeconomical and public health concerns. Moreover, high myopia is associated with potentially blinding complications such as glaucoma, retinal detachment, and myopic macular degeneration.
__
Classification:
Borish and Duke-Elder classified myopia by cause:
•Axial myopia is attributed to an increase in the eye’s axial length.
•Refractive myopia is attributed to the condition of the refractive elements of the eye.
Borish further subclassified refractive myopia:
1. Curvature myopia is attributed to excessive, or increased, curvature of one or more of the refractive surfaces of the eye, especially the cornea. In those with Cohen syndrome, myopia appears to result from high corneal and lenticular power.
2. Index myopia is attributed to variation in the index of refraction of one or more of the ocular media.
_
Simple myopia:
It is just a variant of the normal and is not a major problem. Apart from the refractive error, no anatomical or functional complications of the ocular structures occur. The progression of myopia, more commonly happens during the growing phase of one’s life. The maximum growth happens between the ages of 12 and 20 years. Frequent change of glasses maybe required during these years and the myopic error usually stabilizes after the age of 20. Hence permanent surgical procedures like laser surgery have to be performed only after documented stabilization of the myopia.
Pathological (or progressive) myopia:
It is also called as degenerative myopia, as the name suggests is of a more serious nature a type of severe, progressive nearsightedness characterized by changes in the fundus of the eye, posterior staphyloma, and deficient corrected acuity. Refractive error is greater than -8.00 diopters, and axial length is greater than 32.5 mm. In pathological myopia the retina becomes very thin and is stretched at the periphery. The peripheral retina is at risk of developing tears or holes.
_
•Nocturnal myopia, also known as night or twilight myopia, is a condition in which the eye has a greater difficulty seeing in low-illumination areas, even though its daytime vision is normal. A pilot with 20/20 visual acuity in normal daylight may develop -0.50D to -0.75D. Essentially, the eye’s far point of an individual’s focus varies with the level of light. Night myopia is believed to be caused by pupils dilating to let more light in, which adds aberrations, resulting in becoming more near-sighted. Spherical aberration exacerbates myopia in low light (night myopia). In brighter conditions, the pupil constricts, blocking the more peripheral rays and minimizing the effect of spherical aberration. As the pupil enlarges, more peripheral rays enter the eye and the focus shifts anteriorly, making the patient slightly more myopic in low-light conditions. In general, the increase in overall wave aberration with pupil size has been reported to increase to approximately the second power of the pupil radius. This is because of the fact that most wave aberration is due to the 2nd order aberrations which have a square radius dependency. The effect of spherical aberration increases as the fourth power of the pupil diameter. Doubling pupil diameter increases spherical aberration 16 times. Thus, a small change in pupil size can cause a significant change in refraction. In dark adaptation the eye becomes more sensitive to shorter wave lengths (Purkinje shift- In the light-adapted eye the region of maximal brightness is in the yellow; in the dark adapted eye, the region of maximal brightness is in the green),and visual acuity depends on parafoveal blue cones. Shorter wavelengths come into focus in front of the retina, and this chromatic aberration accounts for some of the relative myopia that a normal eye experiences at night; much of the remainder is due to an increase in accommodative tone in the dark. A stronger prescription for myopic night drivers is often needed. Younger people are more likely to be affected by night myopia than the elderly.
•Pseudomyopia is the blurring of distance vision brought about by spasm of the ciliary muscle.
•Induced myopia, also known as acquired myopia, results from exposure to various pharmaceuticals, increases in glucose levels, nuclear sclerosis, oxygen toxicity (e.g., from diving or from oxygen and hyperbaric therapy) or other anomalous conditions. Elevation of blood-glucose levels can also cause edema (swelling) of the crystalline lens as a result of sorbitol (sugar alcohol) accumulating in the lens. This edema often causes temporary myopia (near-sightedness). The encircling bands used in the repair of retinal detachments may induce myopia by increasing the axial length of the eye.
•Index myopia is attributed to variation in the index of refraction of one or more of the ocular media. Cataracts may lead to index myopia.
•Form deprivation myopia occurs when the eyesight is deprived by limited illumination and vision range, or the eye is modified with artificial lenses or deprived of clear form vision. In lower vertebrates, this kind of myopia seems to be reversible within short periods of time. Myopia is often induced this way in various animal models to study the pathogenesis and mechanism of myopia development.
•Nearwork-induced transient myopia (NITM) is defined as short-term myopic far point shift immediately following a sustained near visual task. Some authors argue for a link between NITM and the development of permanent myopia.
•Instrument myopia is defined as over-accommodation when looking into an instrument such as a microscope.
_
Degree of myopia:
Myopia, which is measured in diopters by the strength or optical power of a corrective lens that focuses distant images on the retina, has also been classified by degree or severity:
•Low myopia usually describes myopia of −3.00 diopters or less.
•Medium myopia usually describes myopia between −3.00 and −6.00 diopters. Those with moderate amounts of myopia are more likely to have pigment dispersion syndrome or pigmentary glaucoma.
•High myopia usually describes myopia of −6.00 or more. People with high myopia are more likely to have retinal detachments and primary open angle glaucoma. They are also more likely to experience floaters, shadow-like shapes which appear singly or in clusters in the field of vision. Roughly 30% of myopes have high myopia.
_
Consequences of myopia:
Some basic pathological consequences of high myopia can be:
1. Retinal detachment:
2. Vitreous liquefaction and detachment:
3. Various Myopic maculopathies:
4. Posterior Staphyloma:
5. Glaucoma:
6. Cataract:
_
Treatment of myopia:
The standard treatment for myopia in children is glasses. A concave lens is used to diverge the light rays entering the eye and place the focal point on the retina.
Light rays exiting a concave lens have less positive vergence, placing the focal point on the retina. Myopia correction can be achieved by eyeglasse lenses, contact lenses, or refractive surgery.
_
Prognosis:
Patients with early onset and high myopia have a worse prognosis for long term visual acuity. These patients tend to have a higher rate of myopic progression with longer axial lengths. Patients with longer axial lengths are at a greater risk for developing myopic retinal degeneration and other associated pathology.
______
Hyperopia:
Hyperopia from the Greek word “hyper-metropia (a condition of over-measured sight) commonly known as being farsighted (American English) or longsighted (British English), is a defect of vision caused by an imperfection in the eye (often when the eyeball is too short or the lens cannot become round enough), causing difficulty focusing on near objects, and in extreme cases causing a sufferer to be unable to focus on objects at any distance. As an object moves toward the eye, the eye must increase its optical power to keep the image in focus on the retina. If the power of the cornea and lens is insufficient, as in hyperopia, the image will appear blurred. It is an ocular condition in which the refracting power of the eye causes light rays entering the eye to have a focal point that is posterior to the retina while accommodation is maintained in a state of relaxation. Visual acuity is better at far (e.g. 6 meters) distances than at near (e.g. 0.33 meters) distances. People with hyperopia can experience blurred vision, asthenopia, accommodative dysfunction, binocular dysfunction, amblyopia, and strabismus, another condition that frequently causes blurry near vision. Presbyopes who report good far vision typically experience blurry near vision because of a reduced accommodative amplitude brought about by natural aging changes with the crystalline lens. It is also sometimes referred to as farsightedness, since in otherwise normally-sighted persons it makes it more difficult to focus on near objects than on far objects. The causes of hyperopia are typically genetic and involve an eye that is too short or a cornea that is too flat, so that images focus at a point behind the retina. The opposite of hyperopia is myopia.
_
Significant hyperopia is defined as any degree of hyperopia sufficient to cause symptoms prompting clinical attention. Hyperopia may be classified by structure and/or function of the eye. Simple hyperopia is due to decreased axial length or decreased converging power of cornea, lens, and/or media (flattened cornea/decreased curvature, increased thickness of lens, etc.). Pathologic hyperopia is due to atypical development, trauma, or disease of the eye (i.e. cataract, microphthalmia, nanophthalmia, aniridia, etc.). Simple hyperopia is much more common than pathologic hyperopia. Decreased axial length is the most common etiology for hyperopia. Functional hyperopia is due to paralysis of accommodation. If affected, functional hyperopia is usually present at birth. Drugs, such as cycloplegics, can also cause a transient hyperopia. Hyperopia may also be categorized by the degree of refractive error: Low hyperopia is +2.00D or less, Moderate hyperopia ranges from +2.25 to +5.00D, and High hyperopia is +5.25D or more. High hyperopia may be associated with blurring of the optic disk margin, known as pseudopapilledema. It can be differentiated from true papilledema by the presence of normal caliber vasculature and normal appearing juxtaposed retina.
_
Hyperopia may also be classified by the role of accommodation to visual functioning. Facultative hyperopia is hyperopia that can be overcome by accommodation whereas Absolute hyperopia cannot be overcome by accommodation. Total hyperopia is the sum of Facultative and Absolute hyperopia. Hyperopia may also be categorized based upon the outcome of noncycloplegic and cycloplegic refractions. Manifest hyperopia is determined with noncycloplegic refraction whereas Latent hyperopia is determined with cycloplegic refraction. The magnitude of hyperopia is the sum of Manifest and Latent hyperopia. With aging, the accomodative power of the eye decreases. This will shift a hyperopic patient from latent hyperopia to greater degrees of absolute hyperopia.
_
Presentation:
Most commonly, the patient may experience decreased visual acuity or squinting at near distances. Strabismus, which is most commonly recognized in childhood, can be a sign of a concomitant hyperopia. Anisometropia may also be noted on visual acuity exam or red reflex testing. Accommodation typically enables younger patients to overcome facultative and latent hyperopia. Asthenopia (eye strain) and/or eye pain is commonly reported and is commonly associated with headaches due to close work such as reading, writing, or computer work. Accommodative dysfunction may result as the eye is no longer capable of accommodating to focus light onto the retina. Binocular dysfunction may also be a symptom of hyperopia.
_
In severe cases of hyperopia from birth, the brain has difficulty merging the images that each individual eye sees. This is because the images the brain receives from each eye are always blurred. A child with severe hyperopia has never seen objects in detail and might present with amblyopia or strabismus. If the brain never learns to see objects in detail, then there is a high chance that one eye will become dominant. The result is that the brain will block the impulses of the nondominant eye with resulting amblyopia or strabismus. In contrast, the child with myopia can see objects close to the eye in detail and does learn at an early age to see detail in objects. The child with hyperopia will typically stand close in front of a television. One would have expected that the child would stand far away because the child is hyperopic, but because the brain has never learned to see detailed lines and object contours the child sees objects blurred. While children with myopia learn to see sharp lines because they can see perfectly well very close to their eyes, the brain of a child with hyperopia cannot see sharp lines, so they stand right in front of the television to at least see blurred images. This blurred vision may also cause a child to develop a squint because the two eyes do not detect sharp lines which the brain can use to map the separate images of the two eyes together to form a single image. Each eye functions independently. So a child with hyperopia from birth presents with decreased visual perception. The parents of a child with hyperopia do not always realize that the child has a problem at an early age. A hyperopic child might have problems with catching a ball because of blurred vision and because of a decreased ability to see three-dimensional objects. The child will typically perform below average at school. As soon as a child starts identifying images, a parent might find that the child cannot see small objects or pictures. In many circumstances mild to moderate hyperopia can be mistaken for ADHD; or other learning and personality disorders. One coping mechanism many children subconsciously use is constant head and body movement to attempt to maintain focus. The incidence of hyperopia is correlated with lower IQ, educational attainment, and literacy. This is to be contrasted with myopia, which is associated with higher IQ and educational outcomes.
_
Treatment of hyperopia:
The standard, and safest, treatment for symptomatic hyperopia is corrective lenses. Mild hyperopia does not need treatment. Hyperopic correction can be achieved by glasses lenses, contact lenses, or refractive surgery. The lenses required to correct hyperopia are convex lenses that converge light rays entering the eye to bring the focal point of the eye onto the retina. Glasses lenses are tolerated better in babies and children. Contact lenses are typically not preferred until adolescence or later, however the decision is based on the responsibility level of the patient or caregiver. A survey of practitioners revealed a common threshold for treatment intervention of hyperopia was 3.00D to 5.00D of asymptomatic hyperopia in children at age. Refractive surgery is typically not preferred until the refractive error of the eye has stabilized and growth of the eye has stopped, which typically occurs in the third decade of life.
_
Complications and Prognosis of hyperopia:
Young children (ages 0-10) with uncomplicated low-to-moderate hyperopia usually do not require intervention. With aging, loss of accommodation causes visual acuity to decrease and hyperopia to worsen. Decreased quality of life is common with hyperopia. There may also be a decrease in the ability to learn and develop within normal limits when vision is poor. Hyperopia that is not fully compensated with accommodation will force the eye into convergence and an esotropia (crossed eyes) will develop. Amblyopia can be another complication of hyperopia. Monocular amblyopia or Binocular amblyopia may result. Levels greater than 1.00D of hyperopic anisometropia and 5.00D of isometric hyperopia are considered amblyogenic. Accommodative esotropia, acute angle closure glaucoma, and strabismus may also result from hyperopia.
____
Myopic versus hyperopic eyes: axial length, corneal shape and optical aberrations:
The main structural difference between hyperopic and myopic eyes is the axial length, which is higher for myopic eyes (Carney, Mainstone, & Henderson, 1997; Grosvenor & Scott, 1994; Mainstone et al., 1998; Strang et al., 1998). Cheng et al. (1992), using magnetic resonance for a small sample of eyes, showed that myopic eyes are larger in all three dimensions (i.e., equatorial, antero-posterior, and vertical axes). There are discrepancies across studies with respect to the corneal shape (both corneal radius of curvature [CR] or asphericity [Q]) and optical aberrations in myopic and hyperopic eyes. Myopic eyes have been found to have steeper corneas (Carney et al., 1997; Grosvenor & Goss, 1998), as opposed to flatter corneas in hyperopic eyes (Sheridan & Douthwaite, 1989). Some studies found significant correlations between CR and myopic (Carney et al., 1997) or hyperopic (Strang et al., 1998) refractive error, or significant differences across refractive groups (Sheridan & Douthwaite, 1989). However, other authors (Grosvenor & Goss, 1999; Mainstone et al., 1998) did not find a significant correlation between CR and refractive error. The axial length/corneal radius of curvature ratio (AL/CR) seems to be negatively correlated with refractive error stronger than CR itself in both hyperopes (Strang et al., 1998) and myopes (Grosvenor & Scott, 1994). Cross-sectional (Carney et al., 1997) and longitudinal (Horner, Soni, Vyas, & Himebaugh, 2000) studies show higher asphericity (less negative or even positive) with increasing myopia. However, this tendency, consistent with increased corneal spherical aberration in high myopes, is reduced when only low and moderate myopes are considered (Marcos, Barbero, & Llorente, 2002). For hyperopes, no correlation has been found between Q and refractive error (Budak, Khater, Friedman, Holladay, & Koch, 1999; Carkeet, Luo, Tong, Saw, & Tan, 2002; Mainstone et al., 1998; Sheridan & Douthwaite, 1989). However, Budak et al. (1999) reported more positive Q values for their moderately myopic eyes than those for their hyperopic eyes and those for their high myopic eyes.
_________
Refractive Errors and Age-related Macular Degeneration (AMD): A Systematic Review and Meta-Analysis: 2013:
Analysis of the 6 cross-sectional studies showed that hyperopia was associated with higher odds of prevalent AMD (pooled OR hyperopia vs. emmetropia: 1.16; 95% confidence interval [CI], 1.04–1.29) and that myopia was associated with lower odds of prevalent AMD (pooled OR myopia vs. emmetropia: 0.75; 95% CI, 0.61–0.92). Analysis from the 3 cohort studies showed nonsignificant associations. Analysis of the 5 cross-sectional and 2 cohort studies showed that each diopter increase in spherical equivalent was associated with increased odds of both prevalent (pooled OR, 1.09; 95% CI, 1.06–1.12) and incident (pooled HR, 1.06; 95% CI, 1.02–1.10) AMD. In 3 cross-sectional studies with data on axial length, each millimeter increase in axial length was associated with a decreased odd of prevalent AMD (pooled OR, 0.76; 95% CI, 0.69–0.85). In conclusion, Refractive error is associated with AMD, although a temporal relationship cannot be determined on the basis of current evidence. Ophthalmologists should be aware that risk of AMD clinically seems to vary by refractive status.
________
Simplified explanation of hyperopia vs. myopia vis-à-vis vision:
Farsighted (hyperopic) individuals have more trouble seeing up close than in the distance, usually because the light will only come to a point “behind” the fovea. In order to make the image clear, a hyperopic person will use their focusing system even out in the distance in order to make objects clear. This allows them to move the image onto the fovea. People that don’t have any farsightedness do not use any focus power to see in the distance clearly.
Example:
Let say a child has a refractive error of +2.00D but does not wear glasses. This means they use 2 units of focusing power in order to see clearly in the distance. However when you need to shift your focus to up close, like when reading a book (and for example sake, the book is held at about 16 inches), they must focus 2.5 units (Diopters) of focusing power that the book requires everyone to use, but additionally focus the 2 units of focusing power they already had to use in order to compensate for their refractive error in the distance. That is 4.5 units altogether, which puts a bigger strain on the visual system and can make it more difficult to work up close for activities such as reading with ease and comfort.
_
Nearsighted (myopic) individuals have trouble seeing clearly out in the far distance because the light comes to a point before it hits the fovea in the back of the eye. The light will only hit the fovea on objects that are closer. Without glasses, most individuals that are nearsighted exert less energy up close because their eye is preset to see clearly at near distances.
Example:
If you have a child with a refractive error of -2.00D without wearing glasses, this means their point of focus is at about 50 cm (1meter/2D=50cm). This means they can see clearly up to this point, but beyond it is blurry. If that child is holding their book at 40 cm, which takes 2.50D to read, they only have 0.50D to crank in to see the book clearly.
______
Astigmatism:
_
Astigmatism is a blurring of vision due to an irregular shape in the cornea or lens. In eyes without astigmatism, the cornea and lens have a more-or-less similar curvature in all directions. This allows light to be focused to a single point on the retina. People with astigmatism have more curvature in one direction, or meridian, than in another, so that light is not able to focus on a single point on the retina. This results in blurring of vision at all distances. Ophthalmic astigmatism is a refraction error of the eye in which there is a difference in degree of refraction in different meridians. It is typically characterized by an aspherical, non-figure of revolution cornea in which the corneal profile slope and refractive power in one meridian is less than that of the perpendicular axis. Astigmatism usually is caused by an irregularly shaped cornea. Instead of the cornea having a symmetrically round shape (like a baseball), it is shaped more like a football, with one meridian being significantly more curved than the meridian perpendicular to it.
_
Diagram above shows the shape of a normal cornea, and the elongated, football-shaped cornea of someone with astigmatism.
_
In astigmatism, the curvature of the optical system varies in different meridians thus refracting the incident light differently in those meridians. To understand what meridians are, think of the front of the eye like the face of a clock. A line connecting the 12 and 6 is one meridian; a line connecting the 3 and 9 is another. The steepest and flattest meridians of an eye with astigmatism are called the principal meridians.
_
In an eye with astigmatism, light fails to come to a single focus on the retina to produce clear vision. Instead, multiple focus points occur, either in front of the retina or behind it (or both). Astigmatism usually causes vision to be blurred or distorted to some degree at all distances. An optical system with astigmatism is one where rays that propagate in two perpendicular planes have different focus. If an optical system with astigmatism is used to form an image of a cross, the vertical and horizontal lines will be in sharp focus at two different distances. Astigmatism causes difficulties in seeing fine detail. Symptoms of uncorrected astigmatism are eye strain and headaches, especially after reading or other prolonged visual tasks. Squinting also is a very common symptom. In some cases, astigmatism is caused by the shape of the lens inside the eye. This is called lenticular astigmatism, to differentiate it from more common the corneal astigmatism. Rubbing of eyes is associated with increase in astigmatism, avoid rubbing.
_
Types of astigmatism:
With—the—rule astigmatism: the vertical meridian is steeper
Against-the-rule astigmatism: the horizontal meridian is steeper
Regular astigmatism: Principle meridians are 90 degrees apart
Irregular astigmatism: Principle meridians are not 90 degrees apart. This type of astigmatism cannot be completely corrected by spectacles and may need contact lenses e.g.: corneal scarring, keratoconus.
_
Astigmatism is also classified based on focus of the principal meridians:
With accommodation relaxed:
•Simple astigmatism
◦Simple hyperopic astigmatism – first focal line is on retina, while the second is located behind the retina.
◦Simple myopic astigmatism – first focal line is in front of the retina, while the second is on the retina.
•Compound astigmatism
◦Compound hyperopic astigmatism – both focal lines are located behind the retina.
◦Compound myopic astigmatism – both focal lines are located in front of the retina.
•Mixed astigmatism – focal lines are on both sides of the retina (straddling the retina)
__
In with-the-rule astigmatism, a minus cylinder is placed in the horizontal axis to correct the refractive error (or a plus cylinder in the vertical axis). Adding a minus cylinder in the horizontal axis makes the vertical axis “less steep” which makes both axes equally “steep”. In against-the-rule astigmatism, a plus cylinder is added in the horizontal axis (or a minus cylinder in the vertical axis). Children tend to have with-the-rule astigmatism and elderly people tend to have against-the-rule astigmatism. Axis is always recorded as an angle in degrees, between 0 and 180 degrees in a counter-clockwise direction. Both 0 and 180 degrees lie on a horizontal line at the level of the centre of the pupil, and as seen by an observer, 0 lies on the left of both the eyes of the patient. [As seen by the patient, 0 lies on the right of both eyes]
______
Presbyopia:
Presbyopia (from Greek meaning trying to see as old men do) is a condition associated with aging in which the eye exhibits a progressively diminished ability to focus on near objects. Presbyopia is the irreversible loss of the accommodative ability of the eye that occurs due to aging. Accommodation refers to the ability of the eye to increase its refractive power of the crystalline lens in order to focus near objects on the retina. The first signs of presbyopia – eyestrain, difficulty seeing in dim light, problems focusing on small objects and/or fine print – are usually first noticed between the ages of 40 and 50. The ability to focus on near objects declines throughout life, from an accommodation of about 20 dioptres (ability to focus at 50 mm away) in a child, to 10 dioptres at age 25 (100 mm), and levels off at 0.5 to 1 dioptre at age 60 (ability to focus down to 1–2 meters only). This decline occurs as a natural result of aging and will ultimately affect any person reaching advanced enough age. Presbyopia’s exact mechanisms are not fully understood; research evidence most strongly supports a loss of elasticity of the crystalline lens, although changes in the lens’ curvature from continual growth and loss of power of the ciliary muscles (the muscles that bend and straighten the lens) have also been postulated as its cause. In presbyopia, the visual input to the cortex is limited by the optics of the eye. High spatial frequencies (fine details) are attenuated. Thus, at near, the visual acuity and contrast sensitivity of uncorrected presbyopes is lower than normal. Since contrast is important in driving neural responses in the visual cortex, the consequence of a blurred input may result in weaker and slower neuronal responses in the visual cortex, leading to degraded letter identification and reduced reading abilities.
_
_
The expected, maximum, and minimum amplitudes of accommodation in diopters (D) for a corrected patient of a given age can be estimated using Hofstetter’s formulas:
Expected amplitude (D) = 18.5 – 0.3 x (age in years),
Maximum amplitude (D) = 25 – 0.4 x (age in years),
Minimum amplitude (D) = 15 – 0.25 x (age in years).
_
Presentation:
Gradual onset of blurred near vision is often the first presenting symptom of presbyopia. The severity of accommodative loss at the time of presentation varies based on the visual needs of the individual. Those who utilize near vision in daily activities frequently complain of impairment earlier. Other symptoms commonly experienced include squinting, headaches secondary to eye strain, increased light requirement, and need to work from progressively greater distances. Diplopia can also result from presbyopia and is thought to be associated with increasing exophoria and decreased vergence amplitude seen frequently in presbyopic patients. The first symptoms most people notice are difficulty reading fine print, particularly in low light conditions, eyestrain when reading for long periods, blur at near or momentarily blurred vision when transitioning between viewing distances. Many extreme presbyopes complain that their arms have become “too short” to hold reading material at a comfortable distance. Presbyopia symptoms, like other focus defects, become much less noticeable in bright sunlight due to the action of the iris closing to a smaller diameter. As with any lens, increasing the focal ratio of the lens increases depth of field by reducing the level of blur of out-of-focus objects (compare the effect of aperture on depth of field in photography). A delayed onset of seeking correction for presbyopia has been found among those with certain professions and those with miotic pupils. In particular, farmers and homemakers seek correction later, whereas service workers and construction workers seek eyesight correction earlier. Scuba divers with interest in underwater photography may notice presbyopic changes while diving before they recognize the symptoms in their normal routines due to the near focus in low light conditions.
_
There is some confusion in articles and even textbooks over how the focusing mechanism of the eye actually works. In the classic book, Eye and Brain by Gregory, for example, the lens is said to be suspended by a membrane, the ‘zonula’, which holds it under tension. The tension is released, by contraction of the ciliary muscle, to allow the lens to become more round, for close vision. This implies the ciliary muscle, which is outside the zonula, must be circumferential, contracting like a sphincter, to slacken the tension of the zonula pulling outwards on the lens. This is consistent with the fact that our eyes seem to be in the ‘relaxed’ state when focusing at infinity, and also explains why no amount of effort seems to enable a myopic person to see farther away.
_
Diagnosis of presbyopia:
Corrected near and distance visual acuity testing allows for evaluation of a patients’ refractive error as well as their functional capacity at near distances. Uncorrected or under-corrected myopes will typically have less difficulty with near vision while the difficulties will be exacerbated in patients with uncorrected hyperopia. Refraction will provide a baseline distance correction to which the near value will be added to provide optical correction for presbyopia. Near lens prescription can be determined by adding plus power over the distance correction until clear near vision is achieved. Performing this monocularly will yield a higher value by eliminating variation caused by convergence accommodation. Near retinoscopy will provide an objective measurement of the required optical power for clear near vision. Intermediate distance testing may also be warranted for patients with mid-range visual needs (i.e. computers) and advanced presbyopia.
_
Management:
The safest and least invasive management of presbyopia consists of corrective glasses lenses either as a separate set of reading glasses, contact lenses, bifocals, or progressive lenses.
_
Interaction with myopia:
Many people with myopia (near-sightedness) can read comfortably without eyeglasses or contact lenses even after age 40. However, their myopia does not disappear and the long-distance visual challenges remain. Myopes considering refractive surgery are advised that surgically correcting their nearsightedness may be a disadvantage after age 40, when the eyes become presbyopic and lose their ability to accommodate or change focus, because they will then need to use glasses for reading. Myopes with astigmatism find near vision better, though not perfect, without glasses or contact lenses when presbyopia sets in, but the more astigmatism, the poorer their uncorrected near vision.
_
Monovision:
An alternative way to deal with presbyopia is called monovision. In monovision, your dominant eye is given a distance prescription, while your other eye is given a near prescription. Contact lens practitioners have used monovision for years. Refractive surgeons use it as well. While monovision can decrease your need for reading glasses, it can take some getting used to. Monovision can hinder depth perception, and you may not feel comfortable driving or reading for extended periods without glasses to bring both your eyes into optimal focus. If you’ve never experienced monovision, try it with contact lenses first to make sure you’re comfortable with it. If you are, your eye surgeon can give you permanent monovision LASIK or other refractive surgery. Monovision does not work well for spectacles, since the user will not always look through the optical centers of the lenses, causing double images. That problem is not present with contacts or laser surgery.
_
Exercises:
Available treatment programs based upon exercising the ciliary muscles have not proven effective.
_
Surgically implanted corneal inlays are another treatment option for presbyopia. Corneal inlays typically are implanted in the nondominant eye to minimize impact to binocular uncorrected distance vision. They seek to improve near vision in one of three ways: The Flexivue Microlens (Presbia) changes the central refractive index, the Kamra (AcuFocus) increases the depth of focus through the use of a pinhole, and the Vue+ (Revision Optics) reshapes the central cornea.
_
Brain image processing enhancement:
Scientists’ understanding of the ability of the adult brain to change, termed neuroplasticity, has been vastly advanced during the last 20 years, giving rise to solutions based on perceptual learning. Perceptual learning, standing for repeated practice on a demanding task, improves visual skills by enhancing the image processing in the brain. Several great achievements in this field include FDA-approved solutions for severe visual problems such as amblyopia, loss of vision resulting from a stroke, and others. Academic research on perceptual learning has been published in leading academic journals, including Nature, Science, PNAS, Vision Research and others, including studies showing improved visual performance in presbyopes. Improvements in visual functions following perceptual learning are achieved without changing the optical characteristics of the presbyopic eye, implying enough retained plasticity in the aging brain to offset the natural biological deterioration of the eyes. Thus, the unavoidable deterioration of the eyes with age can be compensated by boosting the speed and quality of image processing in the visual cortex of the brain.
_________
Non-presbyopic Accommodation problems:
Accommodation is the process whereby changes come about in order to increase the refractive power of the eye and enable near vision. There are three aspects to it: the eyes converge, pupil size reduces and the crystalline lens changes shape and position.
Accommodative insufficiency:
•Description – this effectively describes a premature form of presbyopia. The exact problem is not clearly understood but is probably neuronal in origin. It is found in a number of neurological conditions, such as encephalitis and closed head trauma. It is also seen in patients with current or past debilitating illness and it may be induced by certain medications (e.g., parasympatholytics and tranquilising drugs). It is characterised by an inability to maintain binocular alignment as an object comes nearer to a patient. This condition is relatively common (3% to 5% of the population) and particularly affects individuals who have high visual demands (a lot of close work such as teenagers, college and others studying), in periods of illness, anxiety or fatigue.
•Patient perspective – initially, patients may complain of asthenopia – the vague discomfort associated with using the eyes (headache, ‘eye strain’, brow ache), particularly when trying to accommodate. Ultimately, near vision becomes blurred or there is diplopia associated with bringing objects closer. Symptoms vary from mild to severe but are few or absent in distant vision.
•Correction – treatment is very successful with corrective lenses or exercises for the eyes involving the near point of convergence. Very occasionally, there is a role for pharmacological agents. Any underlying condition needs to be addressed.
Accommodative excess:
•Description – this arises as a result of ciliary muscle spasm which may arise from ocular disease (e.g., iridocyclitis), drugs used to treat ocular disease (e.g., anticholinesterases used in the treatment of glaucoma) or it may arise due to uncorrected refractive errors (usually hyperopia). It can also occur after prolonged periods of close work.
•Patient perspective – the symptoms characteristically include headache, brow ache, variable blurring of distance vision and an unusually close near point.
•Correction – lenses and eye exercises are prescribed but, occasionally, the patient may need pharmaceutical help too (e.g., cycloplegics).
_____
Anisometropia [discussed vide supra]:
Anisometropia is the condition in which the two eyes have unequal refractive power. Each eye can be nearsighted (myopia), farsighted (hyperopia) or a combination of both, which is called antimetropia. Generally a difference in power of two diopters or more is the accepted threshold to label the condition anisometropia. In certain types of anisometropia, the visual cortex of the brain will not use both eyes together (binocular vision), and will instead suppress the central vision of one of the eyes. If this occurs often enough during the first 10 years of life while the visual cortex is developing, it can result in amblyopia, a condition where even when correcting the refractive error properly, the person is still not correctable to 20/20. Estimated 6% of subjects aged 6 to 18 have anisometropia.
_
Management of anisometropia:
Spectacle correction:
For those with large degrees of anisometropia, spectacle correction may cause the person to experience a difference in image magnification between the two eyes (aniseikonia) which could also prevent the development of good binocular vision. This can make it very difficult to wear glasses without symptoms such as headaches and eyestrain. However, the earlier the condition is treated, the easier it is to adjust to glasses. It is possible for spectacle lenses to be made which can adjust the image sizes presented to the eye to be approximately equal. These are called iseikonic lenses. In practice though, this is rarely ever done. If the difference between the eyes is up to 3 diopters, iseikonic lenses can compensate. At a difference of 3 diopters the lenses would however be very visibly different – one lens would need to be at least 3mm thicker and have a base curve increased by 7.5 spheres.
Contact lenses:
The usual recommendation for those needing iseikonic correction is to wear contact lenses. The effect of vertex distance is removed and the effect of center thickness is also almost removed, meaning there is minimal and likely unnoticeable image size difference. This is a good solution for those who can tolerate contact lenses.
Refractive surgery:
Refractive surgery causes only minimal size differences, similarly as contact lenses. In a study performed on 53 children who had amblyopia due to anisometropia, surgical correction of the anisometropia followed by strabismus surgery if required led to improved visual acuity and even to stereopsis in many of the children.
_
Aniseikonia:
- Patients with aniseikonia view one image as a different size in each of their eyes.
- The difference in size of the images between the two eyes is measured as a percentage e.g. an image may be seen 10% larger in the left eye than the right eye.
- Aniseikonia is thought to be noticeable to the patient when the difference between eyes is 3-5%.
- Aniseikonia may be caused by a difference in the two eyes such as their length or power of refraction.
- Patients may present with: head/eye pain, double vision, nausea and dizziness, photophobia and reading problems.
- Aniseikonia can be managed in a variety of ways with contact lenses, glasses and intraocular lenses. The best choice will vary for each individual.
- Causes are many:
- Anisometropia : Commonest cause
- Aphakia: This is the absence of a lens, commonly due to congenital cataract extraction or trauma.
- Astigmatism
- Stereopsis: This is a difficulty with being able to perceive depth of objects, and patients with this problem are slightly more likely to develop aniseikonia.
- Strabismus: This is malalignment of the eyes.
- Amblyopia (‘lazy eye’)
_
Aphakia:
Aphakia is the absence of a lens resulting from a birth defect, eye injury, or eye surgery for removal of a cataract. If a person has had a lens removed to treat cataracts but has not had a lens implant, objects look blurred at any distance.
___________
Differential diagnosis of refractive errors:
Patients with refractive errors often complain of defective vision, tiredness of eyes and headache. Even though refractive errors is the most common causative factor for defective vision, other organic causes such as the following should be examined and ruled out by a comprehensive eye examination.
i. Cataract
ii. Retinal disorders
iii. Optic nerve pathology
iv. Glaucoma
v. Other media opacities
It should be once again emphasized that estimation of refractive errors should be a part of a complete ophthalmic evaluation. In addition, other causes of headache like sinusitis or migraine should be suspected especially when there are complaints of recurrent headache in the setting of a normal refractive status.
__________
Synopsis refractive error:
_________
_________
Research, animal experiments and studies on causes of refractive error:
_
_
There is strong evidence that the development of myopia in humans is influenced by both genetic makeup and environmental factors. Up to 80% of the variation in refractive error in humans may be explained by genetic factors (Hammond, Snieder, Gilbert, & Spector, 2001), and the number of myopic parents significantly increases the odds of children becoming myopic (Pacella et al., 1999). Evidence of environmental influence comes from a rapid increase in the prevalence of myopia in certain populations (Lam et al., 1994; Young et al., 1969) or in certain sub-groups of the population (McBrien & Adams, 1997; Zylbermann, Landau, & Berson, 1993), as well as an association of myopia with near work (Mutti, Mitchell, Moeschberger, Jones, & Zadnik, 2002). However, the relative importance of genetic makeup and environmental factors is still a matter of controversy.
_
Hereditary factors:
Controversy exists over the exact etiology of ametropia. However, most investigators agree that heredity is an important component. Early studies delineated pedigrees that supported autosomal dominant, autosomal recessive, and X-linked recessive inheritance patterns. Multifactorial inheritance has also been proposed. Several authors suggest that heredity does not play a role in the development of refractive errors. Many investigators noted that high ametropias were transmitted differently than low ametropias and were often associated with other ocular anomalies. Individual ocular components are not considered in many of these studies. A school of thought exists which believes that myopia is caused by genetic predisposition and exposure to risk factors. There have been up to 8 susceptibility loci identified, for example MYP 3(Chromosome: 12; Location: 12q21-q23), MYP 11 (Chromosome: 4; Location: 4q22-q27) which are autosomal dominant, MYP1 (Chromosome: X; Location: Xq28) and OPEM (Chromosome: X). A review of literature will show that there are numerous studies with contradicting results regarding the causes and risk factors of myopia. In this context, it is justified if one says that there still seems a lot to be resolved regarding the cause of myopia.
_
Genome-wide meta-analyses of multiancestry cohorts identify multiple new susceptibility loci for refractive error and myopia: 2013 study:
Refractive error is the most common eye disorder worldwide and is a prominent cause of blindness. Myopia affects over 30% of Western populations and up to 80% of Asians. The CREAM consortium conducted genome-wide meta-analyses, including 37,382 individuals from 27 studies of European ancestry and 8,376 from 5 Asian cohorts. Authors identified 16 new loci for refractive error in individuals of European ancestry, of which 8 were shared with Asians. Combined analysis identified 8 additional associated loci. The new loci include candidate genes with functions in neurotransmission (GRIA4), ion transport (KCNQ5), retinoic acid metabolism (RDH5), extracellular matrix remodeling (LAMA2 and BMP2) and eye development (SIX6 and PRSS56). Authors also confirmed previously reported associations with GJD2 and RASGRF1. Risk score analysis using associated SNPs showed a tenfold increased risk of myopia for individuals carrying the highest genetic load. The results, based on a large meta-analysis across independent multiancestry studies, considerably advance understanding of the mechanisms involved in refractive error and myopia.
_
Refractive errors of all types can be inherited in a simple mendelian fashion in some families. Even in such families, however, the degree of ametropia may vary widely among affected individuals. Clues to underlying pathogenetic mechanisms may come from genetic defects elucidated in disorders that feature refractive errors, such as Stickler syndrome. At present if a high refractive error is present, an associated syndrome should be sought. If the refractive error appears to be isolated, signs of other ocular disorders should be sought. A careful family history may reveal the inheritance pattern of isolated refractive errors for a given family. If none is apparent, patients must be informed that while simple mendelian frequencies cannot be given, cases of X-linked, autosomal recessive and autosomal dominant transmission have been reported for almost every type of refractive error and cannot be ruled out for a single individual. Myopes in particular tend to have myopic children, and hyperopes, especially those with esophorias, may impart an increased risk of esotropia to their offspring. The relationship between astigmatism and keratoconus is being elucidated. In all eye conditions early recognition and treatment in childhood help make normal vision possible, and early examination may prevent amblyopia in those with a family history of refractive errors.
_
Myopia as a symptom of genetic disorders:
The Online Mendelian Inheritance in Man (OMIM) database has listed 261 genetic disorders in which myopia is one of the symptoms. Myopia may be present in heritable connective tissue disorders such as: Knobloch syndrome (OMIM 267750); Marfan syndrome (OMIM 154700); and Stickler syndrome (type 1, OMIM 108300; type 2, OMIM 604841). Myopia has also been reported in X-linked disorders caused by mutations in loci involved in retinal photoreceptor function (NYX, RP2, MYP1) such as: autosomal recessive congenital stationary night blindness (CSNB; OMIM 310500); retinitis pigmentosa 2 (RP2; OMIM 312600); Bornholm eye disease (OMIM 310460). Many genes that have been associated with refractive error are clustered into common biological networks involved in connective tissue growth and extracellular matrix organization. Although a large number of chromosomal localisations have been associated with myopia (MYP1-MYP17), few specific genes have been identified.
_
Twin studies:
Twin studies have been used in an effort to further delineate the influence of multiple factors on the heredity of refractive errors. In classic twin research, monozygotic (MZ) twins share identical genetic material and, if raised together, the same environment. Dizygotic (DZ) twins, on the other hand, only share one fourth of their genetic material but do share the same environment if raised together. Concordance rates in both groups are analyzed for the trait under study. If the concordance rate of a trait in MZ twins approaches 100%, while the same rate in DZ twins is significantly less, then genetic transmission is likely. When the concordance rates between MZ and DZ twins do not differ significantly, environmental influences and other random factors assume greater importance in the etiology of the trait under study. Jablonski was the first to recognize the importance of twin studies in ametropia. In 1922, he reported his findings in 28 pairs of MZ twins and 23 pairs of DZ twins. Jablonski found essentially the same refraction in each member of a MZ twin pair. Rarely did the refraction differ more than 0.5 D. In the DZ twins, however, no concordance was noted. To identify trends in inheritance of refractive errors through twin studies, Waardenberg reviewed the findings of several other investigators and found a high concordance for hyperopia and low to moderate myopia in MZ twins. He reported on 300 pairs of MZ and 225 pairs of DZ twins. High myopia was excluded from the study. Ninety percent of the MZ twin pairs had less than 1-D difference in refraction. The DZ twins were discordant. Occasional discordance was found in MZ twin pairs. The differences between MZ twin pairs tended to decrease with age, while the differences between DZ twin pairs tended to increase with age. Weekers and colleagues examined 14 MZ twin pairs and 14 DZ twin pairs and found results that were similar to those reported by Waardenberg. Hyperopia and astigmatism were very similar in the MZ twin pairs. High myopia, however, showed wide variations. Conflicting results have been reported by Otsuka, who examined 295 pairs of twins and found no significant difference in refractive error correlation between MZ and DZ twins. Orth reported differences in refraction between MZ twins. In one MZ twin pair with identical optical components, one twin had a refraction of -24.00 Sphere/ -25.00 sphere while the other was emmetropic. Several twin studies were able to document good concordance in MZ twin pairs despite differences in environment. Lisch examined a MZ pair with identical myopia despite the fact that one twin had a job involving constant close work while the other did not. Jancke and Holste compared 72 MZ twin pairs with 68 DZ twin pairs and found similar refractions in MZ twins despite the fact that one member of each twin pair engaged in strenuous near-work while the other twin did not. Sorsby and co-workers studied 78 MZ twin pairs, 40 DZ twin pairs, and 48 unrelated pairs. Their criteria for concordance was agreement of refraction within 0.50 D. They found concordance was not equally good for all refractive states in the MZ twin pairs. Concordance was high for refractions near emmetropia but not so high for larger refractive errors. Low to moderate astigmatism (0.75–2.0 D) exhibited a high incidence of concordance in the MZ twin pairs. DZ twin pairs and the control pairs both exhibited poor concordance for this level of astigmatism, All pairs showed poor concordance with higher degrees of astigmatism (greater than 2.00 D). Sorsby and co-workers then went on to investigate the separate components of refraction in each of the pairs. Generally, there was an incidence of concordance of 70% to 80% for most of the components of refraction in the MZ twin pairs. Only slight concordance for components of refraction was found in the DZ twin and control pairs. Thus, twin studies have shown heredity to be an important factor in determining refraction.
_
Myopia twin studies:
Investigations into the cause of myopia have engendered more passionate debate than those into all other forms of ametropia combined. Twin studies have helped to establish the hereditary nature of myopia. In general, investigators make a distinction between low and moderate myopia (up to -6 D) and high myopia (greater than -6 D). A large number of twin studies of low to moderate myopia have been published. The majority show a high degree of concordance in MZ twin pairs when compared with DZ twin pairs. However, occasional examples of discordance between MZ twin pairs have also been reported. Concordance rates for myopia in MZ twin pairs have been observed to decrease as the degree of myopia in creases. In addition, the number of twin studies dealing with MZ twins with high myopia is much smaller. However, good concordance has been noted in several studies of high myopia in MZ twins. Although twin studies establish heredity as an important factor in the etiology of myopia, there is very little consensus as to the exact mode of inheritance of myopia.
_
Hyperopia twin studies:
The comparative ophthalmology studies of Kardo Sysoeff have shown that hyperopia is the most frequent refraction found in mammals, birds, reptiles, amphibians, and fish. Degree of hyperopia is higher in the smaller animals. Generally, the more highly developed animals tend toward lower degrees of hyperopia. The most frequent refraction in humans is a low degree of hyperopia. The hereditary character of hyperopia has been demonstrated by numerous twin studies. This hyperopic concordance in MZ twins tends to persist unchanged throughout life. Environmental factors apparently do not exert a great influence. Differences in inheritance patterns have been encountered in persons with different degrees of hyperopia. Low hyperopes (up to +6 D) exhibit different inheritance patterns than high hyperopes (over +6 D). In addition, highly hyperopic eyes have an increased incidence of pathologic associations. Low hyperopia can be considered a variation within the normal limits of the binomial distribution. Most authors propose an autosomal dominant pattern of inheritance. High hyperopia, on the other hand, is rather uncommon. Most extreme forms, often associated with abnormalities of the eye such as microcornea, can be classified as microphthalmia. Most studies demonstrate an autosomal recessive pattern of genetic transmission. Consanguinity of parents has been found frequently. Rarely, autosomal dominant transmission has been reported. Several inherited and sporadic syndromes are associated with hyperopia.
_
A strong case can be made for the view that refractive error is determined genetically. An international team of scientists led by King’s College London has discovered 24 new genes that cause refractive errors and myopia. The new genes include those which function in brain and eye tissue signaling, the structure of the eye, and eye development. The genes lead to a high risk of myopia and carriers of the high-risk genes had a tenfold increased risk. Parents who have myopia tend to have children with myopia. The prevalence of myopia in children with two parents with myopia is 30% to 40%, decreasing to 20% to 25% in children with one parent with myopia and to less than 10% in children with no parents with myopia. An increasing number of parents with myopia significantly elevates the odds of being myopic, with an odds ratio of 5.09 reported for having two versus no parents with myopia. Monozygotic twins tend to resemble each other in refractive error more than do dizygotic twins. Heritabilities for refractive error calculated from twin data are typically very high, on the order of 0.82 or greater. Refractive error and the axial length of children’s eyes are more closely related to parental refractive error than to children’s near-work habits. To date, genetic loci have been associated with pathologic myopia but not with juvenile myopia.
_
Both genetic and environmental factors responsible for myopia:
The percentage of myopes in the human population has increased dramatically in the last decades, reaching near epidemic proportions in some countries. In Asian industrial centers (e.g., Hong Kong, Singapore), the prevalence approaches 75% of the population depending on age and occupation (Rosenfield & Gilmartin, 1999). It is estimated that the number of myopes worldwide will increase from 1.6 billion today to 2.5 billion by 2020. Much attention is being devoted to counteracting this problem, as myopia can be associated with economic and pathological consequences such as cataract, glaucoma, choroidal neovascularization, and retinal detachment (Saw, Katz, Schein, Chew, & Chan, 1996). The mechanism underlying the development of myopia in the postnatal years is unknown. However, in humans, both genetic (Kurtz et al., 2007; Mutti, Mitchell, Moeschberger, Jones, & Zadnik, 2002; Pacella et al., 1999; Saw et al., 2005) and environmental factors (Konstantopoulos, Yadegarfar, & Elgohary, 2008; Mutti et al., 2002; Saw et al., 2001) contribute to the disorder.
_
Myopia in East Asia:
Myopia has emerged as a major health issue in east Asia, because of its increasingly high prevalence in the past few decades (now 80–90% in school-leavers), and because of the sight-threatening pathologies associated with high myopia, which now affects 10–20% of those completing secondary schooling in this part of the world. Similar, but less marked, changes are occurring in other parts of the world. The higher prevalence of myopia in East Asian cities seems to be associated with increasing educational pressures, combined with life-style changes, which have reduced the time children spend outside. There is in fact strong evidence for rapid, environmentally induced change in the prevalence of myopia, associated with increased education and urbanisation. These environmental impacts have been found in all major branches of the human family, defined in modern molecular terms, with the exception of the Pacific Islanders, where the evidence is too limited to draw conclusions. The idea that populations of East Asian origin have an intrinsically higher prevalence of myopia is not supported by the very low prevalence reported for them in rural areas, and by the high prevalence of myopia reported for Indians in Singapore. A propensity to develop myopia in “myopigenic” environments thus appears to be a common human characteristic. There are no reported major genes for school myopia, although there are several genes associated with high myopia. Any genetic contribution to ethnic differences may be small. However, to what extent many genes of small effect and gene-environment interactions contribute to variations in school myopia within populations remains to be established. There are promising optical and pharmacological interventions for preventing the development of myopia or slowing its progression, which require further validation, and promising vision-sparing treatments for pathological myopia.
_
Why rise in myopia worldwide?
90% of Taiwanese are myopic. The odd thing is that only 70% of mainland Chinese are myopic. The majority of Taiwanese are ethnically Southern Chinese so the difference does not appear to be genetic. A study showed that between the 1950’s and the 1970’s the incidence of myopia in the Inuit increased dramatically. Not just doubled or tripled but a four- to eightfold-increase. Obviously, schooling, and the change of lifestyle associated with it—going from a people who would move from location to location depending on what time of year it was and whether it was time to fish, or to hunt, for example—is physically changing the structure of the eye. Young and co-workers studied 508 Eskimo subjects and found myopia rarely in parents and grandparents. However, 58% of the children were myopic. This was attributed to the introduction of Western-style education during the past generation. There’s a study comparing children of Chinese ethnicity in Singapore with children of Chinese ethnicity in Australia. In Singapore there was a 29.1% rate of myopia and in Australia it was 3.3%. They found that those in Singapore spent around 4 hours per week outdoors compared to around 14 hours in Australia. There are also a lot of correlations with harsh studying environments which seem to be the case in countries like Taiwan and China where the pressure is high.
_
Environmental Risk Factors:
In stupid to the genetic predisposition of refractive error, there is a correlation between environmental factors and the risk of developing myopia. Myopia has been observed in individuals with visually intensive occupations. Reading has also been found to be a predictor of myopia in children. It has been reported that children with myopia spent significantly more time reading than non-myopic children who spent more time playing outdoors. Socioeconomic status and higher levels of education have also been reported to be a risk factor for myopia.
_
Animal and human studies:
To examine the role played by environment in the development of myopia, animal models have been employed. Many of these animal studies focus on the induction of myopia by artificial manipulation of the environment. The earliest report of an animal model for myopia was made in 1929 when Levensohn137 reported the induction of myopia in macaque monkeys enclosed in a box with their heads held horizontally and extended beyond a table. His results were disputed by subsequent authors. Young went on to induce myopia in monkeys exposed to a restricted visual space. Wiesel and associates serendipitously found myopia in visually deprived macaque monkeys in their investigations on amblyopia and monocular visual deprivation. Wiesel and Raviola went on to show that unilateral lid suture produced high degrees of myopia in macaque monkeys. The degree of myopia was related to the age of the monkey at the time of the lid suture and the duration of the experiment. Axial length and equatorial diameter were increased while the anterior segment was essentially unchanged. However, when lid-sutured monkeys were raised in the dark, axial lengths and refractions were normal. The mechanism of induction of myopia was believed to be reduction in patterned retinal images. To confirm this theory, corneal opacities were then caused in monkeys by injection of a fine suspension of polystyrene beads. This also increased the axial length, while leaving the anterior segment unchanged, thus confirming the investigator’s suspicions. Other investigators have documented a similar arrest of emmetropization with disruption of vision. Clinical models of vision deprivation myopia have also been reported. Unilateral birth injuries of the cornea have been observed to progress toward myopia. Myopia and increased axial length have been observed in persons with corneal opacities. A unilateral posterior subcapsular cataract was noted to be associated with axial myopia in the affected eye in one of a pair of MZ twins. Von Noorden and Lewis reported on 10 patients with unilateral aphakia. In 7 of these patients, the affected eye demonstrated an axial myopia. Robb described orbital and adnexal hemangiomas associated with unilateral ametropia, usually high myopia, in young children. Hoyt and co-workers have found a similar association of axial myopia in neonatal lid closure from a variety of causes. Rabin and associates found unilateral myopia in association with several monocular visual anomalies. They also reported bilateral myopia in several patients with binocular anomalies. These clinical observations confirm the findings of experimental models of myopia-visual deprivation can produce myopia by interrupting the emmetropization process.
_
The refractive development of the eye is under the influence of a feedback mechanism known as emmetropization where optical defocus guides the growth of the eye so that there is no refractive error (Hung, Crawford & Smith, 1995; Schaeffel, Glasser & Howland, 1988; Troilo & Wallman, 1991). This requires that the visual system is able to distinguish between myopic defocus (where the optical image is formed in front of the retina) from hyperopic defocus (where the image plane is behind the retina). When the primate emmetropic eye is deprived of form vision by degrading the optical image, it becomes myopic (Raviola & Weisel, 1977; Wallman & McFadden, 1995) and restoring an undegraded image results in a growth of the eye towards emmetropia again. A similar response has been found in most (but not all) species examined. Although there is general agreement that growth of the young human eye is regulated by an emmetropization mechanism, refractive errors occur in between 20% of the adult population in European populations, and up to 80% of the population in some Asian countries. The reason for this anomaly is not clear, as the retinal image is defocused in myopes rather than degraded. Possibly the error detection system in these individuals is flawed, or the eye may be growing towards an ‘‘incorrect’’ zero (Medina, 1987).
_
Near work:
Of all the issues surrounding myopia in children, there is probably none so contentious yet crucial as understanding the relative contributions of environment—primarily near work—and heredity. Several clinical studies have documented an association between myopia and higher levels of children’s near work. Level of education is often used as a surrogate measure for near work with more myopia among the more educated. Researchers in Asia point to their rigorous schooling system and the long hours children spend studying as being responsible for the high rates of myopia in Asia, rates that may be on the increase. Support for an important role for near work also comes from animal studies that have demonstrated the plasticity of refractive error in response to environmental stimuli. Neonatal chicks, tree shrews, or monkeys experience increased ocular growth and become myopic or less hyperopic after wearing minus lenses, presumably to compensate for the hyperopic defocus produced by these lenses. Hyperopic defocus from a deficient accommodative response in juvenile myopes is theorized to be the connection between near work in human myopia and the minus lens results from animal studies. One of the most unexpected results of the chicken studies was that imposed defocus was compensated even if the connection of the eye to the brain was disrupted by cutting the optic nerve. Even though the baseline refraction of the eye without optic nerve moved to more hyperopia, suggesting general growth inhibition, negative lenses still caused axial elongation, and positive lenses growth inhibition on top of the new baseline refraction. These results suggest that the retina releases factors to control the growth of the underlying sclera. Furthermore, they show that the retina can make a distinction between positive and negative defocus. The current environmental model derived from these clinical and experimental studies is that exposure to hyperopic defocus from accommodative lag during prolonged near work leads to excessive growth of the eye and a myopic refractive error. Both human and animal studies point toward the hypothesis that reducing defocus in children may slow myopia progression. The hypothesis that progressing myopes have greater defocus than nonmyopic children and increased defocus may produce axial elongation has led to two clinical trials. Enrollment is complete in both trials, and results are scheduled to become available in several years.
_
The figure below shows that hyperopic defocus leads to myopia as confirmed by animal & human studies:
_
Accommodation and Accommodative lag:
Accommodation is a significant covariant of reading and near work and as a result, several studies have focused on the association between accommodation, accommodative lag and myopic progression. A study in 2004 by Gwiazda et al. demonstrated that children with higher degrees of myopia also had increased accommodative lag. The children enrolled in the study were already myopic and although a correlation between myopia and accommodative lag can be assumed, it does not represent a causative relationship. More recent studies have shown opposite results to those of Gwianda et al. In 2006 Mutti et al. showed no changes in accommodative lag prior to the onset of myopia, moreover accommodative lag was only documented in children after the onset of myopia. The authors speculate that accommodative lag may be a consequence rather than a cause of myopia and is unlikely a predictive factor. This was further supported in 2008 by Weizhong et al who showed no significant relationship between accommodative lag and myopic progression. The notion that accommodation is good—because it clears the image of nearby objects, allowing them to be seen clearly and also removing a stimulus for axial elongation. The notion is also consistent with the correlation of myopia with intensive schoolwork. Accommodation requires effort (contraction of the ciliary muscle), and the lag of accommodation may increase over many hours of near work. The association between extensive near work and myopia is merely an association between a condition (near work) that tends to produce accommodation. It does not imply that the act of accommodation causes myopia. The data from animal experiments and from children suggest the contrary—that accommodation is good because it prevents excessive defocus.
_
The Ciliary Body and Refractive Error:
All studies have shown that the ciliary body tends to be thicker in patients with myopia as compared to emmetropic or hyperopic patients. A well-known association exists between accommodative dysfunction and myopia development in children. Multiple studies have reported that children with myopia have higher accommodative convergence per diopter of accommodation (AC/A) ratios than children without myopia, and higher AC/A ratios appear in these children prior to the onset of myopia. Additionally, accommodative lag has also been associated with myopia development. Whether or not these accommodative problems are a cause or an effect of myopia is a hotly debated topic. Certainly, we can speculate that the ciliary muscle is a prime candidate for a source of accommodative lag. The ciliary muscle is, of course, the muscle that generates accommodation. I hypothesize that thick ciliary body is due to persistent near-work.
_
My view:
Evolutionary biologically our eyes are tuned for constant distant vision and occasional near vision using accommodation power. Prolonged near work leads to constant accommodation use. Constant accommodation increases refractive power of eye persistently rather than intermittently. Thick ciliary body in myopic children points to constant accommodation overuse due to persistent near-work. Persistent increase in refractive power tricks retina into believing that eyes are trying to compensate for hyperopic defocus. This illusory hyperopic defocus stimulate retina to secrete growth factors for sclera to increase axial length of eye producing compensatory myopia. Constant accommodation is sufficient to cause central and paraxial rays to fall on fovea but not sufficient for peripheral rays from near objects to focus on retina as they would need far more refraction (bending) and therefore these peripheral rays will fall behind retina causing peripheral hyperopic defocus. This peripheral hypeopic defocus also causes axial elongation of eye resulting in compensatory myopia (vide infra). Although accommodative pupillary reflex causes pupil constriction to block peripheral rays momentarily, constant accommodation leads to retinal adaptation and accommodative papillary reflex is abolished allowing peripheral rays to enter eyes. Compensatory Myopia will make distant vision blurred but near vision easy with less strain on accommodation. In other words, persistent near work leads eye changes to make eyes suitable for constant near vision i.e. myopia. Therefore children must be encouraged to intermittent vision breaks in between near work activities to dissipate constant accommodation.
_
Prevention of Myopia Progression with Atropine:
A study show inhibition of myopia development in three groups of children in Taiwan, who received eye drops every evening with different concentrations of atropine. Note that all concentrations used inhibited myopia. In the case of 0.5% solution (green crosses), there was even an initial regression of myopia. The burning question of how cholinergic antagonists can inhibit axial eye growth in a variety of vertebrates (chick, rhesus monkey, human) remains unanswered. In the case of atropine, currently still the most effective drug against myopia, at least five different target tissues have been identified (summarized by Wallman and Winawer). The sclera defines the shape and size of the globe and was therefore always at the center of interest in myopia research. In an attempt to identify targets for pharmacological intervention of myopia, its metabolism has been extensively studied in the recent years. Atropine prevents progression of myopia not because it paralyses accommodation but by direct inhibitory effect on scleral metabolism.
_
Illumination and myopia:
To avoid myopia, one should read in bright light that decreases pupil diameter and increases depth of focus, thus reducing defocus. Good illumination is highly recommended especially for near work – as Feldkaemper et al. stated: “Because the experiments show that the eye becomes more sensitive to image degradation at low light, the human eye may also be more prone to develop myopia if the light levels are low during extended periods of near work.” And Ashby et al. confirmed: “… results, in conjunction with recent epidemiologic findings, suggest that daily exposure to high light levels may have a protective effect against the development of school-age myopia in children.”
Notes:
This argument is very convincing, as every photographer knows that high levels of illumination results in sharper pictures with a higher contrast. Moreover, reduced image quality was made responsible for myopia, and therefore low levels of illumination will favor myopia.
_
Urbanization:
There are several studies that have reported urbanization as a potential determinant of physiologic myopia. Many studies that have shown an association between increased myopia in urban areas as compared to rural areas are confounded by variables such as level of education, IQ, socioeconomic status, near related activities and outdoor exposure. In 2008, a Polish study of 2206 students found that children living in the city had a two-fold increase in the rate of myopia when compared to children living in rural areas. Although they were able to show a correlation between urbanization and myopia, the authors did not control for the above mentioned co-variants and a causative relationship cannot be assumed.
_
Evolutionary explanations:
There are two main theories for the ultimate evolutionary cause for myopia with implications in evolutionary medicine. They both stem back to mismatch theory, which is the idea that the environment to which the human body was adapted over millions of years does not match our current environment. The transition from the hunter-gatherer lifestyle to the modern Western lifestyle has facilitated the development of chronic, noninfectious diseases such as myopia. Studies of modern hunter-gatherer populations in Africa and Inuit populations in the Arctic point to environmental factors as the leading cause of myopia. In ancestral populations, myopic genes would have been strongly selected against because of the survival disadvantage they caused.
_
“Visual stimuli” hypothesis:
Although not mutually exclusive with the other hypotheses presented, the visual stimuli hypothesis adds another layer of mismatch to explain the modern prevalence of myopia. There is evidence that lack of normal visual stimuli causes improper development of the eyeball. In this case, “normal” refers to the environmental stimuli that the eyeball evolved for over hundreds of millions of years. These stimuli would include diverse natural environments—the ocean, the jungle, the forest, and the savannah plains, among other dynamic visually exciting environments. Modern humans who spend most of their time indoors, in dimly or fluorescently lit buildings are not giving their eyes the appropriate stimuli to which they had evolved and may contribute to the development of myopia. Experiments where animals such as kittens and monkeys had their eyes sewn shut for long periods of time also show eyeball elongation, demonstrating that complete lack of stimuli also causes improper growth trajectories of the eyeball. Further research shows that people, and children especially, who spend more time doing physical activity and outdoor activity have lower rates of myopia, relating the increased magnitude and complexity of the visual stimuli encountered during these types of activities.
_
“Screen sightedness” by SmartPhones and Tablet-PCs:
As there is a connection between accommodation effort and myopia, it is obvious that the recent and extensive use of smartphones and small tablet PCs with their small fonts and a resulting close reading distance will have a strong negative impact on the onset and progression of myopia. Allamby reported some warning facts about the extensive use of smartphones and small tablet PCs: “… there has been a 35 per cent increase in the number of people with advancing myopia (short sightedness) since the launch of smartphones in 1997. He has warned the problem could increase by 50 per cent in the next ten years.” And “… the average smartphone user holds the handset 30 cm from their face – with some people holding it just 18cm away – compared to newspapers and books, which are held 40cm away from the eyes.”
_
Contact Lenses:
Numerous experiences and experiments of ophthalmologists have shown that wearing RGP (rigid gas permeable) contact lenses instead of glasses can slow down the progression of myopia substantially. New studies, however, denied this. This positive effect has not been claimed for soft contact lenses and silicone hydrogel lenses. In contrast, it was found that a switch from glasses to soft contact lenses increased the progression of myopia substantially, also adding a greater change in near-point phoria and a steepening of the corneal curvature. Walline et al. reported: “The RGP wearers’ myopia progressed less than that of the SCL [soft contact lens] wearers. The corneal curvature of the SCL wearers steepened more than that of the RGP wearers, but the axial growth was not significantly different between the groups.” Jiminez R et al. stated: “The higher accommodative lags found in this study with SCL could indicate that prolonged use of SCL in near tasks may provoke a continuous hyperopic retinal defocus, a risk factor for the onset and progression of myopia, as indicated in numerous studies.” The amount of oxygen transmitted through the lens appears to have an impact too, Blacker found: “… low-Dk/t hydrogel contact lens wearers [myopia] increasing more during the study.” As an explanation for the inconsistent results, flaws in the design of the studies were made responsible. In a summary of randomized controlled trials no evidence of positive effects of contact lenses (RGP) were found.
_
Peripheral vision in development of refractive error:
In Texas, as part of mankind’s continuing attempts to improve the quality of life of all animals everywhere, especially in labs, a researcher has found that if you fit baby monkeys with goggles that distort their vision, you can make them nearsighted. You can take those goggles that you fit on monkeys, and black out the center so that the monkeys are seeing only with their peripheral vision. Or you can leave such a small portion of the goggles clear that the monkey never gets a chance to use its peripheral vision. Myopia, it turns out, is more likely when the monkey can’t use its peripheral vision. On the one hand, the peripheral retina can contribute to emmetropizing responses and to ametropias produced by an abnormal visual experience. On the other hand, unrestricted central vision is not sufficient to ensure normal refractive development, and the fovea is not essential for emmetropizing responses. Several lines of evidence suggest that peripheral vision can influence refractive development. First, peripheral retinal mechanisms are sensitive to moderately high spatial frequencies and to the effects of optical defocus. Although resolution acuity declines dramatically with eccentricity, detection acuity remains high at substantial eccentricities and is strongly influenced by optical defocus. For example, at 20° eccentricities, grating detection acuity is between 12 and 20 cyc/deg (four times better than resolution acuity) and 1.0 D of defocus can reduce peripheral detection acuity by approximately 50%. In this respect, detection acuity probably provides a better estimate of the spatial characteristics of the mechanisms that mediate emmetropization than resolution acuity because the emmetropization process is not orientation sensitive. Regardless, high visual acuity is not an absolute requirement for emmetropization, because there is ample evidence that emmetropization operates very effectively in animals with much lower visual acuities than humans (e.g., tree shrews have grating acuities of ~2 cyc/deg). Second, studies in birds and tree shrews have demonstrated that eye growth is regulated by local retinal mechanisms that integrate visual signals over spatially restricted areas across the retina and that alterations in peripheral vision can have a significant impact on eye shape and potentially on axial length for the central retina. Recent studies have shown that the peripheral refraction of the eye might play a role in the progression or the onset of myopia. Relative to the fovea, it was found that a more hyperopic refractive error exists in the horizontal peripheral visual field than exists in emmetropic or hyperopic eyes during distance viewing (Atchison, Pritchard, & Schmid, 2006; Mutti, Sholtz, Friedman, & Zadnik, 2000; Seidemann, Schaeffel, Guirao, Lopez-Gil, & Artal, 2002). These studies suggest peripheral hyperopic defocus encourages excessive axial eye growth and the progression of foveal myopia. This hypothesis was further supported in animal studies involving macaque monkeys. Depriving the peripheral retina of form vision in infant monkeys produces foveal axial myopia (Smith, Kee, Ramamirtham, Qiao-Grider, & Hung, 2005) while laser ablation of the fovea does not prevent emmetropization in infant monkeys (Smith et al., 2007), indicating that the peripheral retina is a sufficient, and perhaps dominant, regulator of the emmetropization process.
_
Current research interest is centered heavily around the influence of peripheral refraction on myopic progression. First reported by Hoogerheide et al., in their investigation of myopic pilots, Smith et al. have since provided compelling evidence in primates that manipulation of peripheral retinal focus can dramatically affect the eye’s axial elongation. Peripheral refraction refers to the focal point of off-axis light rays incident to the eye when on-axis light rays are focused on the fovea.
_
Figure above shows location of myopic (red lines) and hyperopic (blue lines) off axis defocus image shells when foveal fixation (black lines) is maintained for on-axis distant objects.
_
Whereas emmetropes and hyperopes typically exhibit peripheral myopia (off-axis peripheral rays focused in front of the retina), children who become myopic have been shown to demonstrate relative peripheral hyperopia (peripheral rays focused behind the retina) from two years prior to the onset of myopia, and maintained through to five years of post-myopia follow up. Peripheral myopia in emmetropes and hyperopes for distant objects occurs due to spherical aberration and increase in curvature of field for peripheral rays. However myopes have peripheral hyperopia due to excessive near-work where objects near eyes throw divergent rays needing far mare refraction resulting in hyperopic defocus. Now whether near-work caused myopia or whether myopes do lot of near-work is matter of debate. Based on research findings, the current theory is that peripheral hyperopia is a driving factor towards myopic progression. If this is the case, then correcting or inducing peripheral myopia should lead to a reduction in the rate of myopic progression.
__
Reconciliation of genetic and environmental theories:
Two hypotheses may reconcile these divergent views. The first is a theory of inherited environment. The tendency for myopia to run in families may be due to a shared intense near-work environment within a family, rather than because of shared genes. Parents with myopia would pass on their own academic standards or love of reading to their children rather than passing on a myopic refractive error itself. The same argument would apply to twin data. Monozygotic twins may share a more similar environment, as well as identical genes, than do dizygotic twins, perhaps falsely inflating estimates of heritability. Another theory that may reconcile genetic and environmental evidence is that there is a genetic susceptibility to the effects of environment. Modification of the risk of near work by parental history of myopia should be detectable as a statistical interaction, with near work having the strongest association with myopia when there are two parents with myopia and the weakest association when there are no parents with myopia. Further complicating the task of unraveling the role of near work is the association between myopia and intellectual ability. Children with myopia tend to have higher intelligence test scores and higher achievement test scores, with better vocabularies and grades in school, than do nonmyopes. It is conceivable that children with a special aptitude for schoolwork may be inclined to engage in more near work over a longer time. Perhaps a child’s cognitive skills are more closely related to refractive error than is near-work behavior. This association also underscores the difficulty in using the highest level of education achieved as a surrogate for near work. Brighter children are more likely to do more near work and to pursue higher education. Untangling the relative importance of near work, heredity, and intellectual ability is impossible without assessing all three factors in the same subjects.
_______
Prevention of myopia and reduction of progression of myopia:
Most myopic refractive errors develop and progress during childhood and adolescence. Treatments proposed to prevent or reduce the progression of myopia include optical correction, use of cycloplegic eyedrops, contact lenses, and visual training. A Cochrane review of interventions to slow progression of myopia in children found positive effects of antimuscarinic eyedrops, which have undesirable side effects or are not commercially available, and lesser effect of multifocal eyeglasses. Reduction of peripheral hyperopic defocus may be the mechanism by which these interventions are effective. Information about the effects of nutritional changes on the progression of myopia is largely anecdotal and no scientifically valid studies are available. Studies have shown that intensive near work may be a contributing factor for myopia and myopic progression. Many authors have speculated that accommodating during near work may be contributing to the progression and development of myopia. Both refractive and pharmocological methods of eliminating accommodative demands while participating in near work have been investigated.
_
Reading Glasses:
These are glasses with convex lenses that are used only for reading. By making the light rays less divergent, these glasses reduce the amount of accommodation required and lessen the likelihood of a ciliary spasm developing. If strong enough lenses are selected, all the accommodation can be eliminated and the eyes will be completely focused for distance. The book is normally held at about a distance of one-third meter from the eyes. Since a +3 D lens has a focal length of one-third meter, if it is placed in front of the eye, it will make the diverging rays become parallel before entering the eye. Thus, this eye can read without accommodation. This is called reading at the far point.
_
Fogging technique:
Now suppose that the book is pushed just a little farther away from the eyes so that it becomes a little blurred. Now the eye is receiving converging rays, something which does not normally occur in everyday life. Only optical lenses make this possible. Notice that the lens of the eye is fully relaxed and cannot relax further. The rays are therefore bent too much and come to a focus slightly in front of the retina. The result is a slightly blurred image. This is called the blurred image or fogging technique because it purposely makes the vision a little blurred or foggy. This technique is especially useful in relaxing a ciliary spasm that is already present. The use of the fogging technique creates an active relaxation of the ciliary muscle and thus has a greater effect on relaxing a ciliary spasm than could be accomplished by merely eliminating the accommodation (with no fogging). The reason for this is that the ciliary muscle is composed of two separate sets of fibers. The circular fibers are obviously used to tighten the muscle and increase the accommodation. The radial fibers are used by the eye to relax the muscle and decrease the accommodation. This has been given the term negative accommodation. Thus, the fogging technique forces the ciliary spasm to relax, as the eyes attempt to see the blurred image clearly. However, most doctors who prescribe reading glasses do not give an add that will eliminate all of the accommodation. They may prescribe an add of only +1 D, +1.5 D, or +2 D. The reason for this is that many children have difficulty “accepting” a large add. That is, the add causes some “side effects” in the form of various vision problems. This drawback of reading glasses is due to the fact that there is a strong linkage in the human visual system between accommodation and convergence (turning the eyes inward when looking at something close). As a viewed object approaches the eyes, accommodation and convergence increase in proportion to each other. Over thousands of years, the brain has learned that this is the normal situation. Consequently, accommodation stimulates convergence and vice versa. Thus, if we converge without accommodating the appropriate amount, or if we accommodate without converging the appropriate amount, problems can develop. This close relationship between accommodation and convergence is upset when reading glasses are used to eliminate the accommodation for reading. Since the eyes must still converge on the book, an unnatural situation is created. The result can be eye fatigue, double vision, or other types of fusion problems. That is, the two images can no longer be fused together without discomfort. Normal binocular vision is interfered with. For this reason, the book should be held as far as possible from the eyes to reduce the amount of convergence needed. This problem can also be partially overcome by prescribing a prismatic component in the reading glasses to reduce the amount of convergence required. These prisms are placed with the bases toward the nose and are called base-in prisms.
_
Bifocals:
The reading glasses just described have what are called single-vision lenses. This means that the same correction is ground over the entire surface of the lens. Any lens having more than one power ground on its surface is a multifocal lens. A lens with two powers is called a bifocal lens. Reading glasses can be provided in a bifocal form, with the upper segment used for distance and the lower segment used for reading. In this manner, the schoolchild can look up at the blackboard without having to remove the glasses. The statements made above about upsetting the accommodation/convergence relationship also apply here when looking through the lower segment. The success of bifocals has been shown in a very interesting and significant study prepared by Francis Young and Kenneth Oakley. Oakley’s practice consisted of both Caucasian families and Native American families. Because of differences in reading habits, life style, etc., the results for the two groups were tabulated separately. The children were between six and fifteen years old and their refractive error was recorded over several years. The annual rate of increase for the Native Americans is more than three times higher for the control group than for the bifocal group. Among the Caucasians, the annual rate of increase is twenty times higher for the control group than for the bifocal group. The wide difference between Native Americans and Caucasians in this study is discussed by the authors at the conclusion of their paper: The Native American subjects generally read less and less intensively than the Caucasian subjects. They also tend to drop out of school earlier and do not wear their bifocals as compulsively as do the Caucasian subjects. Since the Native American bifocal wearers do not use their bifocals as consistently as the Caucasian subjects, the bifocals should be less effective, which they apparently are. On the other hand, since the Native American subjects do less reading, the control subjects should show lower rates of progression, which they do. Thus, the reading variable alone could account for the differences found between the two groups. Since even under these conditions the bifocals seem to have a significant effect on the annual rates of progression and clearly have a significant effect on the Caucasian subjects who follow the instructions better and also do more reading, the bifocals seem to be a relatively effective means of controlling the progression of myopia. Here is a method which can reduce the rate of myopia progression to a fraction of what it would otherwise be.
_
Progressive lenses:
Many studies have investigated the effect of decreasing accommodation in myopic patients using single vision, bifocal and multifocal lenses. In 2003, the Correction of Myopia Evaluation Trial (COMET) studied the effects of progressive additional lenses (PALs) and single vision lenses (SVLs) in 469 myopic children. Their preliminary data showed a slowing of myopic progression by a statistically small amount during the first year of PALs when compared to SVLs. The authors concluded that it did not warrant a change in clinical practice. There is significant debate over the efficacy and long term outcome of bifocals for the prevention of myopic progression. A recent study in 2010 by Cheng et al. studied the effects of bifocals and prismatic bifocal spectacles on myopic progression in Chinese Canadian children. The authors showed a greater reduction of myopic progression and axial enlongation at two years for children in bifocals and prismatic bifocals as compared to the SVLs group. Unfortunately, the study did not provide long-term follow-up data.
_
Overall, the use of plus glasses (for non-myopes) or plus additions (for myopes) for extensive near work (best with appropriate prism) offers an easy first step to prevent further progression of shortsightedness, or to prevent shortsightedness at all. And still more logical, you must keep a proper distance for reading – even with plus additions, the more distant the paper the better. A larger distance has the same effect as a plus addition.
Therefore, always take care to avoid excessive accommodation, e.g.
– By a general undercorrection of glasses/contacts and the use of additional glasses for perfect distant viewing, or
– By full correction of glasses/contacts and the use of plus glasses for near work, or
– By bifocals/progressives
_
Atropine and Pirenzepine:
Accommodation can be inhibited by using an eyedrop that contains a muscarinic receptor antagonist. Atropine and pirenzepine have been the focus of studies investigating pharmocologic prevention of myopic progression. Although previous studies have reported decreased myopic progression rates with atropine eyedrops, ophthalmologists have been reluctant to initiate treatment due to poor follow-up data, risk of atropine toxicity and symptoms of photophobia. A study in 2009 by Tong et al. published a placebo-controlled, randomized, double-masked follow-up study to evaluate the effect of myopia progression after cessation of atropine therapy. The authors found a reduction in myopic progression after 2 years of atropine therapy when compared to the placebo group, however during the follow-up year the atropine group had significantly higher progression rates. Due to the significant rebound of myopia after cessation of treatment and the previously mentioned risks, many clinicians do not advocate using cycloplegic eyedrops for treating myopic progression. Other potential disadvantages include the possible need for bifocal or multifocal eyeglasses (depending on the concentration of atropine administered), photosensitivity and glare, and the inconvenience of using daily eyedrops. Pirenzepine is another muscarinic receptor antagonist, and unlike atropine it is relatively selective for the M1 receptor and less likely to cause cycloplegia and mydriasis. Two similar studies invested the efficacy of Pirenzepine using multicenter, double-masked, placebo-controlled treatment trials. A 50% reduction in myopic progression was shown in patients that used 2% pirenzepine gel in 2005 by Tan et al. and again in 2008 by Siatkowsi et al. Both studies showed an excellent safety profile with significantly less side effects than seen with atropine. Currently there are no long term follow-up data on pirenzepine. Cyclopentolate 1% administered nightly was evaluated in one study in school children in Taiwan. It was found to slow the rate of progression of myopia compared with controls (mean myopic progression of -0.60 D/year compared with -0.90 D/year, which is statistically significant), but not as much as atropine did (mean myopic progression of -0.20 D/year).
_
Overnight Contact lenses:
A highly controversial treatment modality for retarding myopic progression is the use of overnight rigid contact lenses (orthokeratology). [vide infra] These lenses temporarily change the refractive state of the eye by applying pressure to the cornea, creating a non-physiological shape. There are currently no large studies that have shown a benefit to overnight rigid contact lenses. There are several studies that suggest temporary benefits of orthokeratology, however due to small sample size and no long term follow up data, these studies remain inconclusive. In 2003 Katz et al. performed a large randomized trial of 298 Singaporean children that showed that myopic progression was not reduced with overnight contact lens wear and the authors concluded that there is no apparent benefit to orthokeratology for the treatment of myopic progression. There are potential sight-threatening and devastating risks associated with overnight contact lens wear and numerous reports of corneal infection and scarring have been published.
_
Contact lens control of peripheral refraction:
Contact lenses rotate with the eye to provide a consistent retinal focus, so overcome a number of the problems associated with spectacle lenses. Contact lenses provide better refraction to off-axis peripheral rays to reduce peripheral hyperopic defocus. Multifocal contact lenses with concentric distance and +2D near add zones of vision would eliminate peripheral hyperopic defocus while focusing near objects, resulting in preventing progression of myopia. Researchers and eye doctors are finding that conventional or modified multifocal soft contact lenses are effective tools for myopia control. In 2010, researchers from Australia, China and the United States presented data from a study of experimental myopia control contact lenses worn by Chinese schoolchildren for six months. The contacts had a special dual-focus multifocal design with full corrective power in the center of the lens and less power in the periphery. Participants were between the ages of 7 and 14 at the onset and had -0.75 to -3.50 diopters (D) of myopia, with no more than 0.50 D of astigmatism. A total of 65 children wore the experimental multifocal contacts, and 50 children wore eyeglasses. After six months, the children wearing the multifocal contact lenses had 54 percent less progression of their myopia than the children wearing eyeglasses. In June 2011, researchers in New Zealand reported on a comparison of an experimental multifocal soft contact lens and conventional soft lenses for myopia control in children. A total of 40 nearsighted children ages 11 to 14 participated in the study. The children wore the multifocal contact lens on one randomly assigned eye and a conventional soft contact lens on the fellow eye for 10 months, then switched the lenses to the opposite eye for another 10 months. In 70 percent of the children, myopia progression was reduced by 30 percent or more in the eye wearing the experimental multifocal contact lens in both 10-month periods of the study. In November 2013, researchers in the U.S. published the results of a two-year study that revealed nearsighted children who wore multifocal soft contact lenses on a daily basis had 50 percent less progression of their myopia, compared with similarly nearsighted children who wore regular soft contact lenses for two years. Children participating in the study ranged in age from 8 to 11 years and had -1.00 to -6.00 D of myopia at the time of enrollment.
_
Outdoor activity:
The positive effect of outdoor activity for reducing myopic progression has been documented in numerous studies. Physical activity, sports, and low accommodative demands have been postulated as the cause of this protective effect. The Sydney Myopia Study in 2008 demonstrated a significant reduction in the prevalence of myopia in children who spent more time outdoors. After adjusting for time spent on near work, parental refractive error and ethnicity, they showed that increased time spent outdoors, rather than physical activity was associated with less myopia. The authors of the article suggest that light intensity when outdoors may be the contributing factor, by increasing depth of field and decreasing image blur. They also comment on the possible effects of light on the release of dopamine from the retina which is an eye growth inhibitor. Although the nature of this protective factor has yet to be determined, outdoor activity does appear to have positive effects for slowing myopic progression.
_
Preventing myopia through changing habits of reading and near work:
It should be obvious that there are essentially only two ways to prevent myopia. Either 1) give up all reading and close work, at least until adulthood is reached, or 2) arrange to do the close work in such a manner that the eyes can remain relaxed and focused for distance. The first of these alternatives is hardly practical, and is becoming even less so as time goes on because of the increasing amounts of close work that our modern society requires. We obviously must teach our children to read. However, we should abandon the increasingly prevalent practice of teaching children to read even before they start school. Many parents do this without realizing the visual harm they are doing. This just starts the child down the myopia road sooner than necessary. The eyes of preschool children respond very readily to the stress of close work by developing myopia. In addition, the child will be reading for a greater number of years before reaching adulthood, and there is thus more time for a greater amount of myopia to develop. Age six is early enough to start teaching children to read. Many children spend over three-fourths of their working hours concentrating on things at close range. This is a totally unnatural use of the eyes. This leaves us with the second alternative, and there are a number of things which can be done in this area.
1. Reading Distance:
The book or other material should be held as far from the eyes as possible. The distance from the elbow to the knuckles of the hand has been suggested as the minimum working distance. If the book can he propped up beyond arm’s reach and read in this manner, this is even better. If you own or can afford to buy a projector that can project the pages of a book onto a screen across the room, this is better yet. In fact, this type of projector should be in every schoolroom and used by the teacher as much as possible in preference to asking the students to read from their books. If you ever watch a group of schoolchildren studying or writing, and pay particular attention to the distance between their eyes and their desks, you will note that many of them literally have their noses in their work. When reading, the child should look up and into the distance momentarily at the end of each paragraph, or at least at the end of each page, to relax the eyes. Ideally, the chair should be placed to enable looking out a window or across the room when looking up. If a book is lying on the desk in front of a child, the top of the book is obviously further from the eyes than the bottom of the book. This means that as the child reads down the page an increasing amount of accommodation will be required. If the book is lying flat on the table, as much as 3 D more of accommodation will be needed to read the bottom of the page than is needed to read the top. It is better to support the book on a slant board so that the pages are more perpendicular to the line of sight and the bottom of the book is farther away as seen in the figure below. The angle between table and book should be fifty or sixty degrees. It is possible to make or buy an elevating desk with a surface that can be raised to various angles and locked in position for this purpose.
_
_
When a conventional desk is used (or when an elevating desk is in the horizontal position for writing), it is important that the desk surface not be too high for the child. This unavoidably puts the work too close to the eyes. Raising the chair is one way of overcoming this problem. Some people feel that small print in books contributes to the development of myopia but this is not really true. Only if the book is held closer to the eyes than it would otherwise be (because the small print is harder to see) can it be said that small print contributes to the myopia. For this reason, the print in children’s books should be large enough that the child does not need to hold the book too close. Small print can be boring and tiring to the eyes but it does not cause myopia. It is the distance from the eyes to the book which is of most importance.
_
2. Posture:
Reading should not be permitted while a child is lying on the floor or lying in bed. This usually places the eyes too close to the reading material. The elbows should not be rested on the desk or table when reading or writing since this creates a posture which usually causes the head to bend forward too close to the work. A child who habitually reads while lying on the left side will probably develop more myopia in the left eye than in the right eye, because the left eye is closer to the book. If the right side is used, the right eye will probably develop more myopia. It is the job of the schools as well as the parents to teach proper reading posture and proper reading distance to the children. Teachers should remind their pupils daily about the proper use of the eyes and proper posture. At present, this valuable information and training is being universally ignored.
_
3. Lighting:
Good lighting is extremely important in myopia prevention. Use as much light as possible when reading, as long as it does not cause glare or discomfort. Most people tend to use far too little light for their close work. Ceiling lighting is usually insufficient. Get a desk lamp that can be adjusted for different positions so that it can be placed to shine as much light as possible on the book. If the lamp is of the incandescent type, choose a bulb with as high a wattage as the lamp manufacturer permits without danger of overheating the lamp. Our eyes were meant to be used in daylight, so we should sit by a window or outdoors in the sunlight to read whenever possible. It is rare to find indoor illumination that comes anywhere near approaching the intensity of natural sunlight. Good lighting causes the pupil of the eye to become smaller, requiring less accommodation. In addition, good lighting eliminates the need to hold the book close. The indiscriminate use of sunglasses or tinted lenses of any kind should be avoided for the same reason, at least when doing close work.
_
4. Television Viewing:
Watching TV does not cause myopia unless the child sits so close that it becomes a close task. A child should be permitted no closer to the TV set than six feet. Draw a line on the floor if necessary. If the child persists in sitting too close, turn off the set. Another solution would be to place a portable TV set on a high piece of furniture so that the screen cannot be seen except from a proper distance.
_
5. Illness:
When confined to bed, it is common for the sick person to be provided with books, games, etc., to relieve the boredom of confinement. In addition, illumination in the sickroom is often poor. This environment can contribute to a rapid development of myopia, particularly in children. It is possible that the eyes somehow become temporarily weakened so that they more easily become myopic from excessive close work. Or, it may merely be that too much close work is being done in a darkened environment. In any case, if close work is prohibited when a child is ill, there will be little risk of myopia developing. Watching television should be encouraged in preference to reading.
_
While the proper close-work habits described above are beneficial, they are seldom sufficient to prevent or halt myopia in children who have the tendency to develop it. The amount of close work done by children in our modern society is just too much to be counteracted by any halfway measures. More strenuous measures are nearly always needed in order to prevent accommodation to a greater extent and for longer periods of time.
_
Visual training:
Visual training purported to reduce myopia includes exercises such as near-far focusing change activities. There are no scientifically acceptable studies that document that these treatments are clinically effective, and, therefore, this therapy is not recommended.
_
Myopter:
Using the instrument for as much close work as possible prevents myopia while keeping the eyes in normal balance, which eyeglasses cannot do. The Myopter is not a “crutch” but should be considered as a protective device. It protects the eyes from a harmful environment (an unnatural amount of close work) in much the same manner that gloves protect our hands and shoes protect our feet. If a person uses the instrument for all prolonged close work, myopia will be prevented in nearly every case. Because it is impractical for many people to use the instrument for all close work, it is usually recommended for use in combination with other preventive aids. As a totally new instrument, it naturally looks a little strange to some people who see it in use for the first time, especially if they don’t understand its function. Keep in mind that even ordinary eyeglasses looked strange when they first came into use, but now no one thinks there is anything unusual about them. The appearance of the Myopter viewer will become familiar in the same manner. The current model of the Myopter is a sleeker version of the original and eliminates the temples and elastic straps. It is held on the head with a Velcro band that is offered in various colors. The development of the Myopter viewer was based upon the belief that acquired myopia is caused by an excessive amount of close work, resulting in a ciliary muscle spasm (or, in other words, a change in the relaxation level of accommodation), followed by an increase in axial length. The instrument does not merely treat symptoms, but instead attempts to eliminate the cause. Since actually eliminating or greatly reducing close work is difficult in our modern literate society, it seemed logical to place an optical system before the eyes that would simulate distance vision to the greatest extent possible whenever close work was to be done. The Myopter viewer is an instrument with a lightweight plastic housing containing lenses and mirrors, and it is worn instead of glasses for close work. Light coming from the viewed object enters the single opening at the front of the viewer and is split by a beam-splitter into two identical parts. A beam-splitter is a mirror with a special coating which only reflects half of the light which strikes its surface. Thus half of the incoming light is reflected 90 deg at the beam-splitter, and is again reflected 90deg by a mirror into the left eye. The other half of the light passes through the beam-splitter and is reflected by two other mirrors into the right eye. The two beams emerging from the instrument are parallel, and the axes of the eyes must also be parallel. Convergence is eliminated and each eye therefore sees an identical picture.
________
The most important tools to prevent onset and progression of myopia would be:
• Reduction of accommodative and convergence stress e.g. via reading with appropriate distance only or via appropriate undercorrection for reading. Wearing plus glasses for a few minutes a few times per day can block the onset of myopia
• Maintain a permanent good image quality, e.g. via good illumination, and by proper correction for distant viewing. Avoid long-term undercorrection with respect to the respective viewing distance.
• Strengthening of the connective tissue, e.g. via optimized nutrition which helps to prevent degradation, which might be caused by local effects (e.g. via poor image quality) or by systemic processes.
• Outdoor activities can compensate for accommodative stress, can contribute to a sufficient supply of vitamin D, and, e.g., the outdoor illumination can have a positive effect on the day-night rhythm.
• Physical exercises help to reduce stress, increase blood circulation and NO metabolism.
• Keep a healthy sleep-time / wake-time rhythm.
_
_
_
_
Summary of Randomized Trials to Slow Progression of Myopia:
Walline et al. went through numerous medical dadabases to summarize randomized trials about the question, which treatment slows down the progression of myopia. Their result: ” Undercorrection of myopia [note: permanent undercorrection] was found to increase myopia progression slightly in two studies; children who were undercorrected progressed on average 0.15 D (95% confidence interval (CI) -0.29 to 0.00) more than the fully corrected SVLs wearers at one year. Rigid gas permeable contact lenses (RGPCLs) were found to have no evidence of effect on myopic eye growth in two studies (no meta-analysis due to heterogeneity between studies). Progressive addition lenses (PALs), reported in four studies, and bifocal spectacles, reported in four studies, were found to yield a small slowing of myopia progression. For seven studies with quantitative data at one year, children wearing multifocal lenses, either PALs or bifocals, progressed on average 0.16 D (95% CI 0.07 to 0.25) less than children wearing SVLs. The largest positive effects for slowing myopia progression were exhibited by anti-muscarinic medications. At one year, children receiving pirenzepine gel (two studies), cyclopentolate eye drops (one study), or atropine eye drops (two studies) showed significantly less myopic progression compared with children receiving placebo (mean differences (MD) 0.31 (95% CI 0.17 to 0.44), 0.34 (95% CI 0.08 to 0.60), and 0.80 (95% CI 0.70 to 0.90), respectively)”.
___________
__________
Refractive error in children:
Refractive error is an optical defect, intrinsic to the eye which prevents light from being brought to a single point focus on the retina, thus reducing vision. Refractive error remains one of the primary causes of visual impairment in children worldwide. Childhood blindness and visual impairment are as important and perhaps more devastating and disabling than adult onset blindness, because of the long span of life and their permanent effects on the developing eyes. Refractive errors and more particularly myopia, place a substantial burden on the individual and society. School-age children constitute a particularly vulnerable group where uncorrected refractive errors may have a dramatic impact on learning capability and educational potential.
_
Epidemiology:
Population-based studies attempt to determine the prevalence of untreated refractive error and its disability. In the United States, an estimated 5–7% of preschool children have significant refractive errors and 1–4% have amblyopia. Recent studies have reported a substantial amount of refractive visual impairment in pediatric populations around the world, including 10.4% in a predominantly Caucasian Australian 12-year-old population, 11.2% in a rural Chinese population, 9.8% in an urban Chilean sample, and 20.2% and 21.3% in Malaysian and urban Chinese populations, respectively. Prevalence of visual impairment in children varies from as low as 2.72% in South Africa to as high as 15.8% in Chile.
_
The World Health Organization classifies people as visually impaired (acuity worse than 6/18 using a Snellen chart), severely visually impaired (worse than 6/60), or blind (worse than 3/60). Using these definitions, about two per 1000 children in high income countries and around four per 1000 children in low income countries have some degree of visual impairment. Many have disorders of the eye or brain that are present from birth or early childhood and all will experience substantial effects on their development together with educational challenges and curtailed occupational and social prospects. Poor vision is a major barrier to achieving a healthy and educationally sustaining school environment for children in many regions of the world. The world’s leading and most easily remedied cause of poor vision among children is refractive error. Spectacles provide a safe and inexpensive solution to this problem. Nonetheless, a WHO supported series of studies among schoolchildren in Africa, Latin America, and Asia has shown that 10% of children in the developing world require refractive correction. Among secondary schoolchildren in rural China, 60% require spectacles, but two thirds of these are not currently benefiting from appropriate vision correction because of a failure to own or wear spectacles or because they wear spectacles that fail to provide adequate vision. Among Chinese secondary schoolchildren, over 95% of poor vision (≤6/12 in either eye) is caused by inadequately corrected refractive error. For India, the range is 61-82%. Myopia (“near sightedness”) is the most common refractive error among school aged children and is strongly associated with self reported poor visual function in this group. Correction of even modest amounts of myopia improves children’s visual function. Various barriers, however, prevent many children with refractive error from attaining optimum vision and achieving the classroom success envisioned by the WHO and Unesco initiatives. These include the cost of spectacles, concern about cosmetic appearance, and an inadequate understanding of the benefits of refractive correction among children, parents, and teachers. An important problem in many areas, though, is lack of access to refractive services capable of providing accurate spectacles.
_
Child’s vision is essential for successful learning in school. When the vision suffers, pupil’s routine schoolwork and day to day activities also get affected. Vision problems prevail in common among school-age kids. The reasons are many viz. Unhygienic living conditions, malnourishment and the alluring media influence like television, computer games and diminishing parental care etc. The students are not mature enough to point out the deficiency at the early stage or the parents have no idea on the gradually developing vision problem. This results in tiredness, distraction, headache and a few other disorders. Children who have been affected could not concentrate on studies or on any other curricular or extracurricular or recreational activities.
_
Vision screening is effective in identifying children who can benefit from refractive correction. Current means of correcting vision in children detected by such programs, however, are resource intensive. Subjective refraction by a trained professional, the current standard of care, depends on local availability of skilled practitioners. Those few studies that have examined the issue suggest that resource poor areas often fall short of the WHO recommended standard for 2010 of one refractionist per 100 000 population. Diagnosis of significant refractive errors in children remains a diagnostic and public health dilemma. Treatment of amblyogenic hyperopia, astigmatism, anisometropia and myopia can prevent legal blindness and vision loss. The difficulty remains how to screen large numbers of children in a timely and cost-efficient way. Traditional vision screening methods using eye charts in children aged 3–5 years requires their cooperation as well as proficiency in testing by the examiner. Alternative methods such as autorefraction and photoscreening have been developed to address the difficulties in screening young children. Automated refraction requires access to expensive machines, which must be adequately maintained and calibrated. Retinoscopy is a less expensive technology potentially suitable for use in the developing world, but the need for rigorous training has limited its use there. Accuracy of automated and retinoscopic refraction in children depends on paralysis of accommodation (the ability to focus on near objects) with cycloplegic drugs, which also dilate the pupil. Accommodation will otherwise produce a falsely myopic refractive power in children and less effective in identifying hyperopia because of the high accommodative capacity overcoming hyperopic refractive error. A comparison between non-cycloplegic and cycloplegic autorefraction showed that noncycloplegic measurements generally result in too high minus diopters, Zhao et al. reported. Also in true myopes, the omission of cycloplegic agents can contribute to the progression of myopia because the prescribed glasses can be too strong, which causes a further progression of myopia. These preparations must be maintained under sterile conditions and can be associated with unwanted side effects and refusal of services. Cycloplegic refraction has the obvious advantage of dilating the pupil, making subsequent ophthalmoscopy much easier. On the other hand, a widely dilated pupil gives rise to aberrations that can make retinoscopy more difficult. It is not always possible to ensure equality of cycloplegia in the two eyes, especially if the child has been reluctant to open his/her eyes during instillation, so the binocular balance of the final prescription may be suspect. Cycloplegia prevents postrefraction assessment of ocular motility, accommodation and near functions. It is, of course, an invasive technique that is uncomfortable or even distressing for the child.
_
Estimating visual acuity in children:
The newborn’s visual acuity is approximately 20/400, developing to 20/20 well after the age of six in most children, according to a study published in 2009. The measurement of visual acuity in infants, pre-verbal children and special populations (for instance, handicapped individuals) is not always possible with a letter chart. For these populations, specialised testing is necessary. As a basic examination step, one must check whether visual stimuli can be fixated, centered and followed. More formal testing using preferential looking techniques use Teller acuity cards (presented by a technician from behind a window in the wall) to check whether the child is more visually attentive to a random presentation of vertical or horizontal gratings on one side compared with a blank page on the other side — the bars become progressively finer or closer together, and the endpoint is noted when the child in its adult carer’s lap equally prefers the two sides. Another popular technique is electro-physiologic testing using visual evoked (cortical) potentials (VEPs or VECPs), which can be used to estimate visual acuity in doubtful cases and expected severe vision loss cases like Leber’s congenital amaurosis.
_
Nonverbal child (up to 1 year):
Estimating visual acuity in a non verbal child is a challenge. It should comprise of assessing the following parameters.
1. The assessment for this age involves evaluation of ocular fixation and following to appropriate visual stimuli: for an infant under 4 months of age, the examiner’s face or the parent’s face is used as a target. For older infants, appropriate toys can be used to induce fixation. Attempts should be made to assess the quality of the fixation response (central, eccentric, steady, unsteady, maintained) to the targets used. Even a subtle difference in the ocular fixation response of an infant with an otherwise normal eye examination requires monitoring to evaluate the presence or development of amblyopia.
2. Ability to fixate a light held at 33cm.is assessed
3. Blink reflex in response to sound is observed.
_
Verbal but preliterate child (1 to 5 year):
Preschool going children can be assessed by either of the following methods.
1. Ability to locate small objects (cake decorations).
2. Marble game test; in which child is asked to place marbles in holes of a card.
3. Illiterate E-card test.
4. Sheridan Gardiner (S-G) test.
Literate child (>5 year) and adults:
These patients can be checked using a regular Snellen’s visual acuity chart. In illiterate people, Landolt C chart or a tumbling E chart may be used. Near vision testing can be performed using a Jeager chart.
__
The American Academy of Ophthalmology publishes the guidelines (see table below) for prescribing spectacles in children. However, the table carries the following important note: These values were generated by consensus and are based solely on professional experience and clinical impressions, because there are no scientifically rigorous published data for guidance. Individual practitioners will have very different opinions about what level of refractive error requires correction.
_
Let’s begin by thinking about what we expect to be the benefits of refractive correction in children. These are minimising the risk of defects such as strabismus and amblyopia, providing good visual function with a clear retinal image and improving binocular function (including straightening squint). Animal studies would suggest that correcting refractive errors at a young age is likely to impede emmetropisation, (in effect ‘fooling the eyes into thinking they are already emmetropic’) and one study with children supports this. On the other hand, the Cambridge longitudinal study showed that spectacle correction (in this case a partial correction – more of this later) did not influence the final level of refractive error compared to an uncorrected control group, although the corrected group were slower in achieving emmetropisation.
_
Refraction in young children changes rapidly, in the usual case in the direction of emmetropisation. A single measure of refractive error, unless extreme or anisometropic, is not a useful indicator of the need for correction. Monitoring refractive error at regular intervals will allow the optometrist to distinguish between eyes that are emmetropising (low risk of defects) and eyes that are not (high risk of defects). If a child is in the high risk category, then correction for refractive error is probably beneficial. Hyperopia in children may be compensated by active accommodation, but it is not sufficient to assume this. Practitioners should measure accommodation routinely and use this to determine the need for and the amount of a hypermetropic correction, rather than rely on consensus tables or usual practice. Myopia should be corrected by school age, (earlier if marked, or if the child has distance interests) and be fully corrected for distance. Accommodation can be measured to determine whether spectacles may be worn for near tasks. Finally, the refractive error cannot be considered in isolation. Binocular vision status and visual acuity without and with a refractive correction will, of course, contribute to our decision making, as will family history, and the wishes of both parent and child.
_
Myopia:
Myopic refractive errors, if symmetrical may be corrected by taking the child’s visual needs in account since there is only a minimal risk of associated amblyopia. As per the guidelines from the American Academy of Ophthalmology up to 3.00 D of myopia may not require correction in age group of 2-3 years as most of the objects that the very young child is interested in does not require fine resolution. In children up to 6 years, up to 1.5 D of myopia may not need to corrected given their largely desk based work but full correction should be prescribed for older children. Contrary to popular belief, undercorrection of myopic refractive error should be avoided as it may lead to blurred vision and may increase progression of myopia. In cases of myopia associated with a large exophoria or intermittent exotropia, a full time pre-scription of the full myopia correction is required; some cases may even require an intentional overcorrection to stimulate accommodative convergence to control an intermittent exodeviation, particularly in patients with a high AC/A (accommodative convergence/accommodation) ratio. Some cases of high exophoria or long standing Intermittent exotropia could present as pseudomyopia as an attempt to maintain fusion by use of accommodative convergence. In such cases the aim of treatment is to relax accommodation by use of cycloplegic agents and thereafter treat the underlying strabismus.
Hyperopia:
Uncorrected hyperopia can produce accommodative esotropia and amblyopia (strabismic or refractive) but the threshold for management is not clearly defined. Moderate hyperopia,(not associated with strabismus, if left un-corrected will probably not degrade visual acuity in young children. However, owing to the greater risk of associated strabismus and amblyopia, hyperopic refractive error more than 3.5 to 4 D should be corrected especially if there is a poorly controlled phoria or a family history of strabismus and /or amblyopia. Full correction in the nonstrabismic child should be avoided as it blurs visual acuity at distance and hinders compliance .However, when strabismus is present, full cycloplegic hyperopic correction has to be given. Children with bilateral high hyperopia with isometropic amblyopia usually do not have a manifest esotropia since they make no attempts to accommodate. In such cases though the child may not be able to tolerate the full correction in the first instance, partial optical correction is strongly discouraged; since the child could now make use of accommodation in order to overcome the remaining uncorrected hyperopia. These cases warrant a full optical correction.
Astigmatism:
It is known that up to 1.5 D of meridional symmetric astigmatic error is non-amblyogenic and therefore spectacles need not be prescribed in preverbal children. However it is well accepted that oblique astigmatism is more amblyogenic even with less magnitude. In school going children, a cycloplegic refraction followed by comparison between BCVA (best corrected visual acuity) with uncorrected VA will help in deciding whether or not to prescribe spectacles. Some patients may be able to use accommodation to obtain a fairly focused retinal image in moderate astigmatism. In other children, the full cylinder that can be tolerated should be prescribed. Spherical equivalent can be prescribed in compound myopic or hyperopic astigmatism.
Anisometropia:
Anisometropia can be a very powerful amblyogenic factor. In most cases, mild and moderate levels of anisometropia do not cause amblyopia. However, children with family history of amblyopia and patients with hyperopic anisometropia are more vulnerable. The threshold for treating anisometropia is recommended to be > 1.5 D. In hyperopic anisometropia with amblyopia, a symmetric reduction of hyperopia of up to 1.5D of spherical hyperopia should be done. However, if strabismus is also present, hyperopia has to be fully corrected. In cases of myopic anisometropia, a difference of 3-4 D usually does not result in amblyopia. The less myopic eye fixes for far (unless more than 3 Dioptres) and the more myopic eye is used for near fixation, thus allowing use of both the eyes. At higher levels, glasses may not be tolerated due to aneiseikonia and contact lenses are preferable, but many children are intolerant to them. Refractive laser surgery could be a viable option in such cases. Usually, in anisometropic amblyopia, the dominant fellow eye has good visual acuity, and therefore there is no incentive to wear glasses. In such cases spectacle compliance is often difficult and needs to be forced.
________
________
Difference between an Ophthalmologist, Optometrist and Optician:
Your sight depends on seeing the right eye doctor at the right time. When it’s time to “get your eyes checked,” make sure you are seeing the right eye care professional for your needs. Ophthalmologists, optometrists and opticians each play an important role in providing eye care to consumers. But the levels of training and expertise are quite different for each type of provider. Here’s a quick look at the three types of eye care providers:
Ophthalmologist:
An ophthalmologist — Eye M.D/M.S — is a medical doctor who specializes in eye and vision care. Ophthalmologists differ from optometrists and opticians in their levels of training and in what they can diagnose and treat. As a medical doctor who has completed college and at least eight years of additional medical training, an ophthalmologist is licensed to practice medicine and surgery. An ophthalmologist diagnoses and treats all eye diseases, performs eye surgery and prescribes and fits eyeglasses and contact lenses to correct vision problems. Many ophthalmologists are also involved in scientific research on the causes and cures for eye diseases and vision disorders. An ophthalmologist is a specialist who is qualified by lengthy medical education, training and experience to diagnose, treat and manage all eye and visual systems and is licensed by a state regulatory board to practice medicine and surgery. An ophthalmologist is a medically trained specialist who can deliver total eye care: primary, secondary and tertiary (i.e., vision services, contact lenses, eye examinations, medical eye care and surgical eye care), diagnose general diseases of the body and treat ocular manifestations of systemic diseases.
Optometrist:
Optometrists are healthcare professionals who provide primary vision care ranging from sight testing and correction to the diagnosis, treatment, and management of vision changes. An optometrist is not a medical doctor. An optometrist receives a doctor of optometry (OD) degree after completing four years of optometry school, preceded by three years or more years of college. They are licensed to practice optometry, which primarily involves performing eye exams and vision tests, prescribing and dispensing corrective lenses, detecting certain eye abnormalities, and prescribing medications for certain eye diseases. They are state licensed to examine the eyes and to determine the presence of vision problems. Optometrists determine visual acuity and prescribe spectacles, contact lenses and eye exercises. Optometrists may perform all services listed under the definition of an optician. Some states permit optometrists to give limited treatments of some eye conditions.
Optician:
Opticians are technicians trained to design, verify and fit eyeglass lenses and frames, contact lenses, and other devices to correct eyesight. They use prescriptions supplied by ophthalmologists or optometrists, but do not test vision or write prescriptions for visual correction. Opticians are not permitted to diagnose or treat eye diseases. The opticians’ functions include prescription analysis and interpretation; determination of the lens forms best suited to the wearers needs; the preparation and delivery of work orders for the grinding of lenses and the fabrication of eye wear, the verification of the finished ophthalmic products; and the adjustment, replacement, repair and reproduction of previously prepared ophthalmic lenses, frames and other specially fabricated ophthalmic devices.
________
________
Diagnosis and measurement of refractive error:
This test is performed by an ophthalmologist or optometrist. Both of these professionals are often called “eye doctor.” In approaching a patient with reduced vision, the first step is to decide whether refractive error is responsible. In emmetropia, parallel rays from infinity are focused perfectly on the retina. Sadly, this condition is enjoyed by only a minority of the population. In myopia, the globe is too long, and light rays come to a focal point in front of the retina. Near objects can be seen clearly, but distant objects require a diverging lens in front of the eye. In hyperopia, the globe is too short, and hence a converging lens is used to supplement the refractive power of the eye. In astigmatism, the corneal surface is not perfectly spherical, necessitating a cylindrical corrective lens. With the onset of middle age, presbyopia develops as the lens within the eye becomes unable to increase its refractive power to accommodate on near objects. To compensate for presbyopia, an emmetropic patient must use reading glasses. A patient already wearing glasses for distance correction usually switches to bifocals. The only exception is a myopic patient, who may achieve clear vision at near simply by removing glasses containing the distance prescription. Refractive errors usually develop slowly and remain stable after adolescence, except in unusual circumstances. For example, the acute onset of diabetes mellitus can produce sudden myopia because of lens edema induced by hyperglycemia. Testing vision through a pinhole aperture (pinhole glasses) is a useful way to screen quickly for refractive error. If visual acuity is better through a pinhole than it is with the unaided eye, the patient needs refraction to obtain best corrected visual acuity.
_
Detection of refractive error:
Refractive error can be detected through routine examination of patients who present to clinics, or through vision screening of the population at large. The former approach may work satisfactorily in developed countries, but the latter is necessary in developing countries because a large majority of the population does not have access to reasonable quality eye care services. Vision screening is most commonly carried out on schoolchildren, which is a valuable method of identifying potentially treatable ocular abnormalities, including blindness due to refractive error and related amblyopia. School screening is performed in various ways, including simple visual acuity assessment by school teachers or paramedical professionals, and by using computers to assess vision. In developing countries, school teachers have been most commonly used for vision screening of schoolchildren. In recent years, vision screening has also included preschool children. However, current understanding of the natural history of refractive error and amblyopia is incomplete, thus limiting the prophylactic potential of early screening of preschool-age children. Since in developed countries the majority of children attend schools or preschools, it is relatively easier to reach them by vision screening programs. However, in developing countries many children do not attend school, and they are therefore missed by vision screening programs conducted in schools. This problem can be overcome by the community vision screening approach.
_
Provision of services to individuals who need them after being identified through vision screening is as important as the vision screening itself. Provision of affordable, reasonable-quality spectacles is crucial for the effective delivery of eye care services. The emphasis in such vision screening programs should not only be on the number of people screened, but also on the number who experience substantial improvement of vision with spectacles. Aphakia after cataract surgery is also a significant cause of blindness in developing countries since many individuals with aphakia do not obtain adequate spectacles or lose them and do not have them replaced. These difficulties can be addressed, on the whole, through provision of cataract surgery with intraocular lens implantation, which would reduce the chances of blindness due to aphakia. In addition, provision of adequate refractive services for those with aphakia has to be tied with cataract blindness programs.
_
Refraction means refractive correction:
Assessment of a refractive error can only really be done via the process of refraction (generally carried out by an optometrist). In clinical ophthalmology, ‘refraction’ is actually an abbreviation for ‘refractive correction’ and it refers to the process by which the best possible visual acuity can be obtained for a patient. Vision defects caused by refractive error can be distinguished from other problems using a pinhole occluder, which will improve vision only in the case of refractive error.
Refraction has three objectives:
•It measures the patient’s refractive error.
•It determines the optical correction required for focusing on distant and close objects.
•It provides the patient with appropriate corrective spectacles/lenses.
_
Refraction has several components to it:
•Objective refraction: this uses a special instrument (retinoscope) devised to determine the approximate nature of the patient’s refractive error (e.g., myopia, astigmatism) and does not require any input from the patient.
•Subjective refraction: this uses a series of lenses to refine the measurement of the refractive error. It requires active patient participation and therefore is difficult to perform in patients with limited communication (e.g., pre-verbal children).
•Binocular balancing: this final step ensures that accommodation and distant viewing are balanced in both eyes.
_
Who should be tested?
Healthy adults who are not experiencing vision problems should have a refraction test every three to five years. Children should have a refraction test every one to two years, starting at no later than three years of age. If you currently wear prescription glasses or contact lenses, you should have a refraction test every one to two years. This will allow your doctor to figure out what prescription is necessary as your eyes change. If you are having problems with your vision between exams, you should see your eye doctor for another refraction test. Individuals who have diabetes should have an eye examination every year. Individuals over 40 or those with a family history of glaucoma should also have a refraction test every year. Glaucoma occurs when pressure builds up in the eye, damaging the retina and the optic nerve. Regular exams will help your eye doctor to screen for glaucoma and other eye conditions associated with aging, and if possible, treat them early.
_
Subjective measurement of visual acuity: subjective refraction:
Visual acuity is the eye’s ability to detect fine details and is the quantitative measure of the eye’s ability to see an in-focus image at a certain distance. Visual acuity is typically measured while fixating, i.e. as a measure of central (or foveal) vision, for the reason that it is highest there. However, acuity in peripheral vision can be of equal (or sometimes higher) importance in everyday life. Acuity declines towards the periphery in an inverse-linear (i.e. hyperbolic) fashion. Distance visual acuity is usually measured in a dimly lit room, typically at 20 feet (6 meters), as the patient looks at a chart with lines of high-contrast characters. Distance acuity should be measured separately for each eye with current correction. Near acuity is usually measured while the patient looks at a well-lit reading card of high-contrast characters held at a specified near working distance, typically 14 inches or 36 centimeters.
_
Eye chart:
An eye chart is a chart used to measure visual acuity. Types of eye charts include the logMAR chart, Snellen chart, Landolt C, E chart, Lea test, Golovin–Sivtsev table and the Jaeger chart.
_
_
Snellen chart:
A standard eye chart is necessary to make comparisons and to record people’s visual acuity. The most common chart used in most doctors’ offices is the Snellen eye chart. In 1862, a Dutch Ophthalmologist, Dr. Hermann Snellen, devised this eye chart. He determined that there was a relationship between the sizes of certain letters viewed at certain distance. The Snellen eye chart has a series of letters or letters and numbers, with the largest at the top. As the person being tested reads down the chart, the letters gradually become smaller. Many other versions of this chart are used for people who cannot read the alphabet. The Tumbling E chart has the capital letter “E” facing in different directions and the person being tested must determine which direction the “E” is pointing, up, down, left, or right. A Broken Wheel vision test is one that can be used for children or those who cannot read the alphabet and the person being tested must tell which card has the broken wheels on the pictured car. Another type of eye chart that can be used is a picture chart with common pictures of different sizes. In research, another chart, the ETDRS chart, has become the standard. The Snellen fractions, 20/20, 20/30, etc., are measures of sharpness of sight. They relate to the ability to identify small letters with high contrast at a specified distance. They give no information about seeing larger objects and objects with poor contrast (such as steps and curbs); it also does not inform us as to whether or not meaning is obtained from visual input, how much effort is needed to see clearly or singly, and whether or not vision is less efficient when using both eyes as opposed to each eye individually. In short, visual acuity measures only the smallest detail we can see; it does not represent the quality of vision in general. If a subject needs letters (or symbols) that are twice as large or twice as close as those that can just be seen by a standard eye, visual acuity is said to be 1/2 (or an equivalent fractional value, such as 20/40, 6/12, etc.). If the magnification need is 5x, visual acuity is 1/5 (20/100, 6/30, etc.), and so on. The standard definition of normal visual acuity (20/20 or 6/6 vision) is the ability to resolve a spatial pattern separated by a visual angle of one minute of arc. The terms 20/20 and 6/6 are derived from standardized sized objects that can be seen by a “person of normal vision” at the specified distance. For example, if one can see at a distance of 20 ft an object that normally can be seen at 20 ft, then one has 20/20 vision. If one can see at 20 ft what a normal person can see at 40 ft, then one has 20/40 vision. Put another way, suppose you have trouble seeing objects at a distance and you can only see out to 20 ft what a person with normal vision can see out to 200 feet, then you have 20/200 vision. The 6/6 terminology is more commonly used in Europe and Australia, and represents the distance in meters. So 20/20 scale is in feet and 6/6 scale is in meters. Contrary to popular belief, 20/20 is not actually normal or average, let alone perfect acuity. Snellen established it as a reference standard. Normal acuity in healthy adults is one or two lines better. Average acuity in a population sample does not drop to the 20/20 level until age 60 or 70. This explains the existence of the two lines smaller than 20/20: 20/15 and 20/10. The 20/40 letters are twice the size of 20/20 letters; however, it does not mean 50% vision since 20/20 sounds like it is one half of 20/40. If 20/20 is considered 100% visual efficiency, 20/40 visual acuity is 85% efficient. When checking visual acuity, one eye is covered at a time and the vision of each eye is recorded separately, as well as both eyes together.
_
Snellen Chart:
Usually the 20/20 line of letters is fourth from the bottom, with 20/15, 20/10 and 20/5 below that. Healthy young observers have a binocular acuity superior to 20/20; the limit of acuity in the unaided human eye is around 20/10–20/8 (6/3–6/2.4), although 20/8.9 was the highest score recorded in a study of some US professional athletes. Not many people have 20/10 or better visual acuity, but many animals do, especially birds of prey such as hawks, which have been estimated to have an acuity of 20/5 or even better. In this respect, their vision is much better than human eyesight.
_
The traditional Snellen chart is printed with eleven lines of block letters. The first line consists of one very large letter, which may be one of several letters, for example E, H, or N. Subsequent rows have increasing numbers of letters that decrease in size. A person taking the test covers one eye from 20 ft. away, and reads aloud the letters of each row, beginning at the top. The smallest row that can be read accurately indicates the visual acuity in that eye. Symbols on an acuity chart are formally known as “optotypes”. In the case of the traditional Snellen chart, the optotypes have the appearance of block letters, and are intended to be seen and read as letters. They are not, however, letters from any ordinary typographer’s font. They have a particular, simple geometry in which:
•the thickness of the lines equals the thickness of the white spaces between lines and the thickness of the gap in the letter “C”
•the height and width of the optotype (letter) is five times the thickness of the line.
Only the ten Sloan letters C, D, E, F, L, N, O, P, T, Z are used in the traditional Snellen chart. The perception of five out of six letters (or similar ratio) is judged to be the Snellen fraction. Wall-mounted Snellen charts are inexpensive and are sometimes used for approximate assessment of vision, e.g. in a primary-care physician’s office. Whenever acuity must be assessed carefully (as in an eye doctor’s examination), or where there is a possibility that the examinee might attempt to deceive the examiner (as in a motor vehicle license office), equipment is used that can present the letters in a variety of randomized patterns.
_
Snellen fraction:
Visual acuity = Distance at which test is made / distance at which the smallest optotype identified subtends an angle of 5 arcminutes.
Snellen defined “standard vision” as the ability to recognize one of his optotypes when it subtended 5 minutes of arc. Thus the optotype can only be recognized if the person viewing it can discriminate a spatial pattern separated by a visual angle of 1 minute of arc. The standard definition of normal visual acuity (20/20 vision) is the ability to resolve a spatial pattern separated by a visual angle of one minute of arc. Since one degree contains sixty minutes, a visual angle of one minute of arc is 1/60 of a degree. The spatial resolution limit is derived from the fact that one degree of a scene is projected across 288µm of the retina by the eye’s lens. In this 288µm, there are 120 color sensing cone cells packed. Thus, if more than 120 alternating white and black lines are crowded side-by-side in a single degree of viewing space, they will appear as a single gray mass to the human eye. With a little trigonometry, it is possible to calculate the resolution of the eye at a specific distance away from the lens of the eye. In the most familiar acuity test, a Snellen chart is placed at a standard distance: 20 ft in the US, or 6 meters in the rest of the world. At this distance, the symbols on the line representing “normal” acuity subtend an angle of five minutes of arc, and the thickness of the lines and of the spaces between the lines subtends one minute of arc. This line, designated 20/20 (US) or 6/6 (rest of world), is the smallest line that a person with normal acuity can read at a distance of 20 ft. Three lines above, the letters have twice the dimensions of those on the 20/20 line. The chart is at a distance of 20 ft, but a person with normal acuity could be expected to read these letters at a distance of 40 ft. This line is designated by the ratio 20/40. If this is the smallest line a person can read, the person’s acuity is “20/40,” meaning in a very rough kind of way that this person needs to approach to a distance of 20 ft to read letters that a person with normal acuity could read at 40 ft. At 20 ft, the letters on the 20/20 line should subtend 5 minutes of arc (such that the limbs of the letters subtend 1 minute of arc), which means that the chart should be sized such that these letters are 8.86 mm tall and the topmost (20/200) “E” should be 88.6 mm tall. Putting it another way, the eye should be at a distance 68.75 times the height of the top (20/200) letter. Outside of the US, the standard chart distance is 6 m, normal acuity is designated 6/6, and other acuities are expressed as ratios with a numerator of 6. Many rooms do not have 6 m available, and either a half-size chart subtending the same angles at 3 m, or a reversed chart projected and viewed by a mirror is used. Acuity charts are used during many kinds of vision examinations, such as “refracting” the eye to determine the best eyeglass prescription. During such examinations, acuity ratios are never mentioned.
_
While visual acuity charts are usually designed for use at 6 meters or 20 feet, there is often also a need to test a subject’s vision at near or occupational tasks (like reading or computer use). For these situations near-point charts have been created.
_
The largest letter on an eye chart often represents an acuity of 20/200 (6/60), the value that is considered “legally blind.” Some individuals with moderate myopia may not be able to read the large E without glasses, but have no problem reading the 20/20 line or 20/15 line with glasses. By contrast, legally blind individuals have a visual acuity of 20/200 (6/60) or less when using the best corrective lens. In the United States you are considered “legally blind” if your best-corrected visual acuity (meaning, your best distance vision with eyeglasses or contact lenses) is 20/200 or worse. To get a driver’s license in most of the United States, your best-corrected visual acuity must be at least 20/40.
_
The Snellen chart is used to test acuity at a distance of 6 m (20 ft). For convenience, a scale version of the Snellen chart called the Rosenbaum card is held at 36 cm (14 in.) from the patient as seen in the figure below:
The Rosenbaum card is a miniature, scale version of the Snellen chart for testing visual acuity at near. When the visual acuity is recorded, the Snellen distance equivalent should bear a notation indicating that vision was tested at near, not at 6 m (20 ft). Patients who need reading glasses because of presbyopia must wear them for accurate testing with the Rosenbaum card.
_
Eye Chart Limitations:
Eye charts measure visual acuity only, so they are just one part of a complete eye exam. They do help your eye doctor figure out whether you need prescription eyeglasses or contact lenses for your distance vision. But eye charts don’t measure your peripheral vision, depth perception, color perception or ability to perceive contrast. Also, they don’t measure items related to the health of your eyes, such as your eye fluid pressure, how dry your eyes are or whether your retinas are in good shape.
_
Snellen Metric conversion:
If a patient sees 20/200, the smallest letter that they can see at 20 feet could be seen by a normal eye at 200 feet. This is the Snellen Acuity. In Metric Acuity, 20/200 equals 6/60. The conversion is that 20 feet equals approximately 6 meters (actually 6.096).
_
For people who have worse than 20/400 vision, a different eye chart can be used that measures beyond 20/400 vision, or, for the most accurate measurements, a Low Vision Chart can be moved closer to the patient to measure the smallest letter that they can see at a lesser distance. It is common to record vision worse than 20/400 as Count Fingers (CF at a certain number of feet), Hand Motion (HM at a certain number of feet), Light Perception (LP), or No Light Perception (NLP). The conversion of Snellen Acuity to Count Fingers Acuity is as follows:
| 20/800 20/1000 20/1143 20/1333 20/1600 20/2000 20/2666 20/4000 20/8000 |
CF10′ (Count Fingers at ten feet) CF 8′ CF 7′ CF 6′ CF 5′ CF 4′ CF 3′ CF 2′ CF 1′ |
_
Prescriptions for eyeglasses are measured in diopters. The measurement starts at zero (“plano”), with four quarters to a diopter: 0.25 (a quarter diopter), 0.50 (one half a diopter), 0.75 (3/4 of a diopter), and 1.00 (one diopter). The higher the numbers, the higher (stronger) the prescription.
Here are estimates for the approximate correction needed for each line seen on the Snellen chart:
| Snellen20/10 20/15 20/20 20/30 20/40 20/50 20/100 20/200 |
Estimated prescriptionPlano (zero) Plano Plano to -0.25 -0.50 -0.75 -1.00 to -1.25 -1.75 to -2.00 -2.00 to -2.50 |
This estimation works best for myopia (nearsightedness) because hyperopic (farsighted) people can focus and compensate for a certain amount of their prescription. The Snellen fractions cannot be used for ordering a pair of glasses or contacts that will correct a person’s vision.
_
Normal vision vs. normal visual acuity:
Visual acuity depends upon how accurately light is focused on the retina, the integrity of the eye’s neural elements, and the interpretative faculty of the brain. Normal visual acuity (in central, i.e. foveal vision) is frequently considered to be what was defined by Hermann Snellen as the ability to recognize an optotype when it subtended 5 minutes of arc, that is Snellen’s chart 20/20 feet, 6/6 meter, 1.00 decimal or 0.0 logMAR (Logarithm of the Minimum Angle of Resolution). In young humans, the average visual acuity of a healthy, emmetropic eye (or ametropic eye with correction) is approximately 20/16 to 20/12, so it is inaccurate to refer to 20/20 visual acuity as “perfect” vision. 20/20 is the visual acuity needed to discriminate two contours separated by 1 arc minute—about 1/16 of an inch at 20 feet. This is because a 20/20 letter, E for example, has three limbs and two spaces in between them, giving 5 different detailed areas. The ability to resolve this therefore requires 1/5 of the letter’s total size, which in this case would be 1 minute (visual angle). The significance of the 20/20 standard can best be thought of as the lower limit of normal or as a screening cutoff. When used as a screening test, subjects that reach this level need no further investigation, even though the average visual acuity with a healthy visual system is typically better. Some people may suffer from other visual problems, such as color blindness, reduced contrast, mild amblyopia, cerebral visual impairments, inability to track fast-moving objects, or one of many other visual impairments and still have normal visual acuity. Thus, normal visual acuity by no means implies normal vision. The reason visual acuity is very widely used is that it is easily measured, its reduction (after correction) often indicates some disturbance, and that it often corresponds with the normal daily activities a person can handle, and evaluates their impairment to do them (even though there is heavy debate on that).
_
Does 20/20 [6/6] mean perfect vision?
No, it only indicates how sharp your vision is. Peripheral vision (the area of vision around you), eye coordination, depth perception, color vision and focusing ability all contribute to your overall visual ability.
_
Although most normal eyes should have a corrected acuity of 20/20 to 20/25 or better, it may not be possible to achieve this level of acuity in patients with high refractive errors, even with optimal refraction. For a subset of patients, this might be due to the minification produced by high myopic correction at the spectacle plane. In other cases, refractive amblyopia may be the cause. However, a pathologic basis for reduced best-corrected visual acuity (BCVA) should be sought. A suddenly acquired refractive change may signal a systemic or local disease, or a drug or medication effect. Excellent visual acuity does not preclude serious eye disease; therefore, all patients should have a comprehensive medical eye evaluation at the recommended intervals.
_
Phoropter or trial frame refraction:
_
_
A subjective refraction requires responses from the patient. Your eye care professional may use a phoropter or a trial frame to measure your subjective refractive error to determine your eyeglass prescription. Typically, you will sit behind the phoropter or wear a trial frame and look at an eye chart. Your eye care professional will change lenses and other settings while asking you for feedback on which set of lenses give you the best vision. While the automated refractor and the retinoscope provide an objective estimate of refractive error, the phoropter will further refine the refraction and provide a subjective measure of visual acuity. The phoropter is a machine in which patients look through lenses while reading a visual acuity chart. The doctor positions different lenses in front of the patient’s eyes until the patient states that they see the clearest. In other words, the patient repeatedly answers questions about which lens gives the best vision. For this reason, the phoropter is not often used on young children.
_
Distance refraction should be performed with accommodation relaxed. This may be accomplished by using manifest (noncycloplegic) refraction with fogging or other techniques to minimize accommodation with care not to provide excess minus power correction to the patient. In some cases, especially in younger patients, a cycloplegic refraction can be useful. Near vision should be measured in each eye before cycloplegia for patients with high hyperopia, presbyopia, or complaints about near vision. If the patient is presbyopic, the near- vision add is determined at the reading or working distance preferred by the patient.
_
Objective measurement of refractive error: Objective Refraction:
An objective refraction is a refraction obtained without receiving any feedback from the patient. An objective refraction is obtained by using different instruments. Your doctor will use a retinoscope or auto-refractor to measure your refraction without asking for subjective responses from you.
_
Retinoscopy:
One of the most common instruments used for objective refraction is the retinoscope. Retinoscopy (also called skiascopy) is a technique to objectively determine the refractive error of the eye (farsighted, nearsighted, astigmatism) and the need for glasses. The test can be quick, easy, reliably accurate and requires minimal cooperation from the patient. Retinoscopy is a technique to obtain an objective measurement of the refractive error of a patient’s eyes. The examiner uses a retinoscope to shine light into the patient’s eye and observes the reflection (reflex) off the patient’s retina. While moving the streak or spot of light across the pupil the examiner observes the relative movement of the reflex; then uses a phoropter or manually places lenses over the eye (using a trial frame and trial lenses) to “neutralize” the reflex.
_
The examination is conducted in a dark room, at a distance of 1 meter from the patient’s eye. A hand held instrument called a retinoscope projects a beam of light into the eye as seen in the figure above. When the light is moved vertically and horizontally across the eye, the examiner observes the movement of the red reflex from the retina. If there is no movement at all, it means that there is no refraction error. A movement in the direction of the beam of light indicates hyperopia, and a movement in the opposite direction indicates myopia. The reflection’s movement speed is also an important indicator. The slower the movement is, the more significant the refraction error is. The examiner then introduces lenses in front of the eye until the movement is neutralized. The power of the lens required to neutralize the movement is the refractive error of the eye and indicates the lens strength needed to optimize vision with spectacles and/or contact lenses.
_
Retinoscopy is used to determine refractive error in children, developmentally delayed adults, or in individuals whose behavior limits the ability to cooperate. It is especially useful in very young children and infants. Retinoscopy is particularly useful in prescribing corrective lenses for patients who are unable to undergo a subjective refraction that requires a judgment and response from the patient (such as children or those with severe intellectual disabilities or communication problems). In most tests however, it is used as a basis for further refinement by subjective refraction. It is also used to evaluate accommodative ability of the eye and detect latent hyperopia.
_
Photoretinoscopy:
The oculomotor triad comprising ocular accommodation, vergence, and pupil size is essential to seeing a clear, single, luminance intensity controlled image of the outside world. Continuous measurement of the oculomotor system is needed to understand further conditions such as ocular neurological effects and their progression, the potential of multifocal intraocular lenses, and the efficacy of orthoptic training. Although many techniques have been devised to measure accommodation continuously over the past two decades, photoretinoscopy is unique in enabling the measurement of accommodation, vergence, and pupil size in both eyes simultaneously, objectively, remotely (typically the camera is placed 1 meter from the eyes) and continuously.
_
Photorefraction:
Photorefraction is described as retinoscopy based videorefraction method to determine refractive state from a distance of a meter or more without cycloplegia. Photorefraction method is preferred by Kennedy and Schmidt et al to screen children or children who would not otherwise cooperate with objective pediatric vision screening methods; however its reliability and accuracy has been questioned. Other commercial devices that have used this measurement principle include: iScreen Vision, MTI PS-100 Photoscreener, PlusOptix S08 Auto- Refractor/Photoscreener (Previous models were PowerRefractor and Plusoptix S04, current version is S09), Right Medical Retinomax Autorefractor, Visiscreen OSS-C, Welch Allyn SureSight Autorefractor, Fortune Optical VRB-100 videophotorefractor. Various studies suggest that non-cycloplegic photorefraction has reasonable accuracy and repeatability compared with cycloplegic retinoscopy and subjective refraction. However, in a study it was demonstrated that accommodation may not be completely neutralized. It may be especially important in children who have high accommodative reserve.
_
Auto-refraction, auto-refractor and refractometry:
Cycloplegic retinoscopy and subjective refraction is still the gold standard for measuring refractive error in children. But, cycloplegia usage take more time and causes patient discomfort. Therefore, autorefractometers have become widely used to determine the objective refractive status. Modern autorefractometers are standard clinical instruments that generally use Scheiner’s double pinhole principle (e.g. Topcon RM-8000B, Topcon Corporation- Tokyo, Japan) or retinoscopy based infrared video refraction method (e.g. Plusoptix S08 – Plusoptix GmbH, Nuremberg, Germany). In addition, few autorefractometers work on slightly different principals. Such as, Grand Seiko/Shin-Nippon (Grand Seiko Co., Ltd., Fukuyama, Japan) works on the principal of imaging the magnification of a shape reflected from the retina and Canon R-1 (Canon Inc., Tokyo, Japan) works on position of the peak intensity of light as a lens passed through three beams of light reflected off the retina. Currently, some videorefractors were presented by manufacturers as non-cycloplegic autorefractometers called as photoscreener.
_
Refractometry is the method of determining refractive error using an optical device refractometer. For this examination, the ophthalmologist employs a computer-assisted instrument called an automatic refractometer. Computerized automatic refractometers contain infrared light, fixation point and Badel optometer. During the examination, you will be asked to rest your chin on the refractometer’s chin rest while the instrument takes three consecutive measurements of each of your eyes. While seated with your chin in a stabilizing chinrest, you’ll be asked to focus on an image or point of light. The autorefractor automatically determines the correction needed to place your “focus point” on top of the retina, the light-sensitive area at the back of the eye responsible for correctly processing images. The measurement taken by an autorefractor can be translated into a prescription for eyeglasses. Refractometry is quick, painless, and very accurate.
_
Auto-refractor:
_
An auto-refractor is a computerized instrument that shines light into your eye. The light travels through the front part of your eye to the back part of your eye, then back again. The information bounces back to the instrument, giving an objective measurement of your refractive error. Auto-refractors are quick and easy to use, and require no feedback from you.
_
Shack–Hartmann wavefront sensor and its inverse can also be used to characterize eye aberrations in a higher level of resolution and accuracy.
_
Cycloplegic refraction:
Cycloplegic refraction is done by applying a cycloplegic agent to the eye (atropine, cyclopentolate or tropicamide) to paralyze the ciliary muscle so that the absolute refractive error can be measured. It is helpful to detect latent hyperopia in children compensating their hyperopia by accommodation. All children, below the age of 15 years should be refracted only after applying cycloplegics to neutralize the effects of accomadation, to identify accomadative spasm and to diagnose strabismus of accomadative aetiology. A significant difference between manifest and cycloplegic refraction is frequent in children; in adults, a substantial difference between manifest and cycloplegic refraction may require a post-cycloplegic dynamic refraction on a subsequent day where the cycloplegic refraction is used to guide the final manifest prescription. The post-cycloplegic refraction is performed when full accommodation has returned.
_
It has been stated that accommodation has a prominent effect on refraction and affects the spherical equivalent values of school-age children. Wesson et al. took measurements with and without cycloplegia (with cyclopentolate) on infants using the retinoscopy method and found the measurements with cycloplegia to be 2.12 D more hypermetropic. Saunders and Westall performed a similar study with infants and children and found that the refractive error values were approximately 0.39 D more hypermetropic with cycloplegia. In another study, Broghi and Rouse obtained results that were an average of 0.5-0.75 D more hypermetropic in patients of ages varying between 3.6 and 10 years with cycloplegia. Fotedar et al. compared pre- and postcycloplegic autorefraction in 6- and 12-year-old children and found the mean spherical equivalent difference between these measurements to be 0.84 D more hypermetropic in the 12-year-old children and 1.18 D more hypermetropic in the 6-year-old children with cycloplegia.
_
Reliability of Cycloplegic Autorefractor Measurements to determine Spherical and Astigmatic Refractive Errors in Young Children: 2007 study:
Conventional cycloplegic retinoscopy is widely used method to determine the refractive errors in patients of all age groups. Ophthalmologists and opticians in India are increasingly using Non-cycloplegic autorefractor measurements to determine refractive errors in patients of all age groups. Their reliability is questionable especially in young children. This study is an attempt to determine the reliability of cycloplegic automated refractor measurements as an effective substitute for conventional cycloplegic retinoscopy in young children. It is a prospective study involving 200 school children aged 8 to 15 years. They were evaluated for refractive errors over a period of one year. Visual acuity is tested using Snellen’s acuity chart. Automated refraction was performed prior to the administration of cycloplegics. It is followed by cycloplegic conventional retinoscopy and cycloplegic autorefraction. 4% lignocaine topical drops were used to minimise the irritation with cyclopentolate eye drops. 1% cyclopentolate eye drops was used for the purpose. Cyclopentolate eye drops were administered at 0 minutes, after 5 minutes and after 20 minutes. The pupillary reflex and dilatation were inspected at 35 minutes from the first drop of administration. After adequate papillary dilatation (6 mm or more), cycloplegic conventional retinoscopy followed by cycloplegic autorefraction was performed. The study concluded that Cycloplegic Autorefraction spherical and cylindrical measurements can be substituted for conventional cycloplegic retinoscopy in young children. It is even better than conventional cycloplegic retinoscopy for cylindrical axis measurements. The least reliable measure was non-cycloplegic auto refraction. Despite the cost of equipment, autorefraction with cycloplegia can be comparable to conventional cycloplegic retinoscopy in accuracy in children, can be run by an ophthalmic technician and therefore eliminates the ophthalmologist’s examination time required for retinoscopy. Autorefraction without cycloplegia cannot substitute for the conventional cycloplegic retinoscopy in young children.
_
Confusion about the word refractometer:
An auto-refractor or automated refractor or auto-refractometer is a computer-controlled machine used during an eye examination to provide an objective measurement of a person’s refractive error and prescription for glasses or contact lenses. A refractometer is also a laboratory or field device for the measurement of an index of refraction (refractometry). The index of refraction is calculated from Snell’s law and can be calculated from the composition of the material using the Gladstone–Dale relation. Automatic refractometers automatically measure the refractive index of a sample. The automatic measurement of the refractive index of the sample is based on the determination of the critical angle of total reflection. There are four main types of refractometers: traditional handheld refractometers, digital handheld refractometers, laboratory or Abbe refractometers, and inline process refractometers. There is also the Rayleigh Refractometer used (typically) for measuring the refractive indices of gases. An Abbe refractometer is a bench-top device for the high-precision measurement of an index of refraction. To avoid confusion, I suggest the word Autorefractor for determination of refractive error of eye while Refractometer for determination of refractive index of eyeglass lens.
_
Spectacle lens refractive index verification:
There are several methods for assessing the refractive index. Measuring the lens thickness difference from centre to edge and using calculations to determine the refractive index has merit but is likely to lack accuracy, as this ignores the effect of base curve. Other methods involve measurement of lens curvature and lens power. The development of different materials suitable for manufacturing spectacle lenses has presented the dispensing optician with a problem: how can materials be identified? Whereas glass and plastics materials are easily distinguishable, any further classification is difficult without more detailed examination.
Knowledge of the refractive index of a spectacle lens is desirable:
•Where spectacles are to be replicated
•Following a change in prescription, where the same refractive index is to be dispensed and no record is available of the original
•Where only one lens is to be replaced
•As part of the general verification process.
It is possible to estimate the refractive index of a spectacle lens by using equipment readily available in any optical practice. That is lensmeter.
_
Lensmeter:
_
A lensmeter or lensometer, also known as a focimeter or vertometer, is an ophthalmic instrument. It is mainly used by optometrists and opticians to verify the correct prescription in a pair of eyeglasses, to properly orient and mark uncut lenses, and to confirm the correct mounting of lenses in spectacle frames. Lensmeters can also verify the power of contact lenses, if a special lens support is used. The parameters appraised by a lensmeter are the values specified by an ophthalmologist or optometrist on the patient’s prescription: sphere, cylinder, axis, add, and in some cases, prism. The lensmeter is also used to check the accuracy of progressive lenses, and is often capable of marking the lens center and various other measurements critical to proper performance of the lens. It may also be used prior to an eye examination to obtain the last prescription the patient was given, in order to expedite the subsequent examination.
__
Tests for astigmatism:
A number of tests are used by ophthalmologists and optometrists during eye examinations to determine the presence of astigmatism and to quantify its amount and axis. A Snellen chart or other eye charts may initially reveal reduced visual acuity. A keratometer may be used to measure the curvature of the steepest and flattest meridians in the cornea’s front surface. Corneal topography may also be used to obtain a more accurate representation of the cornea’s shape. An autorefractor or retinoscopy may provide an objective estimate of the eye’s refractive error and the use of Jackson cross cylinders in a phoropter or trial frame may be used to subjectively refine those measurements. An alternative technique with the phoropter requires the use of a “clock dial” or “sunburst” chart to determine the astigmatic axis and power. A keratometer may also be used to estimate astigmatism by finding the difference in power between the two primary meridians of the cornea. Javal’s rule can then be used to compute the estimate of astigmatism. Another rarely used refraction technique involves the use of a stenopaic slit (a thin slit aperture) where the refraction is determined in specific meridians – this technique is particularly useful in cases where the patient has a high degree of astigmatism or in refracting patients with irregular astigmatism.
_
Keratometry:
A keratometer, also known as a ophthalmometer, is a diagnostic instrument for measuring the curvature of the anterior surface of the cornea, particularly for assessing the extent and axis of astigmatism. It was invented by the German physiologist Hermann von Helmholtz in 1851, although an earlier model was developed in 1796 by Jesse Ramsden and Everard Home. A keratometer uses the relationship between object size (O), image size (I), the distance between the reflective surface and the object (d), and the radius of the reflective surface (R). The Javal-Schiotz keratometer is a two position instrument which uses a fixed image and doubling size and adjustable object size to determine the radius of curvature of the reflective surface. It uses two self illuminated mires (the object), one a red square, the other a green staircase design, which are held on a circumferential track in order to maintain a fixed distance from the eye. In order to get repeatable, accurate measurements, it is important that the instrument stays focused. It uses the Scheiner principle, common in autofocus devices, in which the converging reflected rays coming towards the eyepiece are viewed through (at least) two separate symmetrical apertures. The Bausch and Lomb Keratometer is a one position keratometer that gives readings in dioptric form. It differs from the Javal-Schiotz in that object size is fixed, image size is the manipulable variable. The reflected rays are passed through a Scheiner disc with 4 apertures – As there are two prisms, each aligned perpendicular to the other, the major and minor axis powers can be measured independently without adjusting the orientation of the instrument.
_
Corneal topography:
Corneal topography, also known as photokeratoscopy or videokeratography, is a non-invasive medical imaging technique for mapping the surface curvature of the cornea, the outer structure of the eye. Since the cornea is normally responsible for some 70% of the eye’s refractive power, its topography is of critical importance in determining the quality of vision and corneal health. The three-dimensional map is therefore a valuable aid to the examining ophthalmologist or optometrist and can assist in the diagnosis and treatment of a number of conditions; in planning cataract surgery and intraocular lens (IOL) implantation (plano or toric IOLs); in planning refractive surgery such as LASIK, and evaluating its results; or in assessing the fit of contact lenses. A development of keratoscopy, corneal topography extends the measurement range from the four points a few millimeters apart that is offered by keratometry to a grid of thousands of points covering the entire cornea. The procedure is carried out in seconds and is completely painless.
_
NETRA: Refraction Test on a Mobile Phone:
It is an interactive, portable, and inexpensive solution for estimating refractive errors in the human eye. Using this platform, a new range of interactivity is created for measuring several parameters of the human eye, such as refractive errors, focal range, and focusing speed.
_
Netra:
_
Netra is a $2 clip-on eyepiece that goes on top of a cell phone. The user looks through this eye piece and interactively aligns the displayed patterns by clicking the buttons. The number of clicks required to bring the patterns into alignment indicates the refractive error. This optometry solution combines inexpensive optical elements and interactive software components to create a new portable and inexpensive device that mimics (and replaces) the expensive laser-based Shack-Hartmann wavefront aberrometers.
__________
__________
Eyeglass lens and contact lens prescription:
Correcting for nearsightedness or farsightedness is called a spherical correction, because it is correcting in all the directions equally. Myopia and hyperopia are corrected with spherical lenses. Concave lenses are used to treat myopia; they are minus or divergent. Convex lenses are used to treat hyperopia; they are plus or convergent. Astigmatism is treated with cylindrical lenses. Many people have astigmatism, which means that their nearsightedness or farsightedness is not the same in all directions. This is because their corneas are not perfectly round, but stretched irregularly, like a cylinder (or the back of a spoon). Astigmatism makes vision blurry at any distance. When your eye doctor corrects for astigmatism, it is called a cylindrical correction. It is called cylindrical because it has no curve (or power) in one direction, and maximum power at a 90-degree angle to the original direction. The term “cylinder” means that this lens power added to correct astigmatism is not spherical, but instead is shaped so that one meridian has no added curvature (axis of cylinder), and the meridian perpendicular to this “no added power” meridian contains the maximum power and lens curvature to correct astigmatism. The number in the cylinder column may be preceded with a minus sign (for the correction of nearsighted astigmatism) or a plus sign (for farsighted astigmatism). The other thing is; our two eyes can be very different in terms of refractive error. We may have astigmatism and some nearsightedness in one eye, and even more nearsightedness but no astigmatism in the other, for example. Rarely do people need exactly the same correction for both of their eyes.
_
Understanding Astigmatism:
It is due to a distortion of the cornea and/or lens.
The refracting power is not uniform in all meridians
The principal meridians are the meridians of greatest and least refracting powers
The amount of astigmatism is equal to the difference in refracting power of the two principal meridians
_
Light rays passing through the top of the spherical lens would be bent just as much as rays passing through the bottom or sides of the lens. The figure below shows an eye where the horizontal lens curvature is greater than the vertical. It can be seen that while the rays passing through the sides of the lens come to a focus on the retina (as in the top view), the rays passing through the top and bottom of the lens do not (as in the side view). If this eye was to accommodate so that the top and bottom rays come to a focus on the retina, then the rays coming through the sides of the lens would fall short of the retina. In other words, there is no way for the eye to focus all the rays on the retina at the same time.
_
_
Usually the astigmatism is not great enough to cause poor vision or to require the use of corrective lenses. When astigmatism is corrected, it is done with the use of cylindrical lenses as opposed to spherical lenses.
A concave cylindrical lens is shown in top, and a convex cylindrical lens in bottom of the figure. Line AB indicates the axis of the lens. Note that rays passing through the axis are not bent. When both a cylindrical and spherical correction are needed, they are ground on the same lens. The location of the axis of a cylindrical lens must he specified when it is placed before the eye. Cylindrical refraction or bending of light rays in one meridian is always perpendicular to axis.
_
Figure below shows the usual method of designating the angle of the axis.
A similar notation is used for each eye. The observer is facing the eyeglass wearer and the zero is at the observer’s left. The scale is read below the horizontal line with 90 deg at the bottom and 180 deg at the right. As an example, if a cylindrical lens was placed with its axis along line AB, it would be at an angle of 70 deg.
_
Eyeglass (spectacle) lens prescription:
Corrective lens prescriptions have 3 numbers. The first number is the power (magnitude) of spherical correction required (minus for myopia; plus for hyperopia). The second number is the power of cylindrical correction required (plus or minus). The third number is the axis of the cylinder. As an example, a prescription for a person with myopic astigmatism may read -4.50 + 2.50 × 90, and a prescription for a person with hyperopic astigmatism may read +3.00 + 1.50 × 180.
_
Let’s look at a sample eyeglass prescription. Note however that eyeglass prescriptions can vary in how they are written, so yours may not look exactly like this example.
_
The term “O.D.” stands for oculus dexter and means right eye. The term “O.S.” stands for oculus sinister and means left eye. If both of the eyes have the same prescription, it can also be written O.U. The term O.U. stands for oculus uterque and means it applies to both eyes. Some prescriptions are written with R.E. for right eye and L.E. for left eye, and I will use this terminology in the descriptions that follow.
Here is one complicated prescription:
R.E. -3.50
L.E. -2.50 -1.00 x 90o
The right eye requires only a -3.50 spherical lens. However, the left eye requires a -2.50 spherical lens coupled with a -1.00 cylindrical lens with its axis at an angle (denoted by the symbol “x”) of 90o. Both corrections are ground on the same lens. This astigmatic correction at 90o tells us that the sides of the lens of the eye are more myopic than the top and bottom so that more power is needed at the sides. By adding -2.50 and -1.00 together we get -3.50, indicating that the sides of the lens of the left eye are just as myopic as the entire lens of the right eye. If necessary, a prismatic correction can also be added to the prescription.
_
The patient with a prescription of -1.25/-1.00 x 180 has a refractive error requiring a 1.25 D lens to correct the myopic element and a 1.00 D lens to correct the astigmatic element (at 180° which tells the optometrist in which plane the astigmatism lies). If the prescription was 0.00/-2.00 x 180, the patient has some astigmatism but no myopia or hyperopia. Understanding refraction and prescriptions can be tricky but having some sense of what is being indicated can be helpful when considering the patient’s problem.
_
Add:
If the glasses are for near or intermediate work, the respective increments in the add boxes of the prescription must be added to the sphere powers of the distance listing. If you have a column called Add in your prescription, this is for bifocals. The “add” is usually additional diopters of strength that are added onto your usual prescription in the lower portion of the lens.
_
Sphere power, cylinder power and add power always appear in diopters. They are in decimal form and generally are written in quarter-diopter (0.25 D) increments. Axis values are whole numbers from 1 to 180 and signify only a meridional location, not a power.
_
You should now be able to read a simple eyeglass prescription and better understand what is happening to your eyes or your child’s eyes. If you already have a pair of glasses and you want to know what the prescription is for them, you don’t have to return to the doctor who prescribed them. Take them to any optician’s shop and the prescription can be determined by testing them on a special machine knows as lensmeter.
_
There is also a simple test that you can do yourself to determine whether your glasses are of the plus or minus type. Remove your glasses and hold them a short distance in front of you. Look through one of the lenses at an object across the room. Then move your glasses up and down or sideways. If the viewed object moves in the same direction as the lens, the lens is minus. If the viewed object moves in the opposite direction, the lens is plus. If the direction of movement is not readily apparent it is possible that the difficulty is due to an astigmatic correction in the lens.
__
Transposition of lens prescription:
See table 1 and table 2 for understanding transposition:
| Table 1. suitable format | |||||
| Typical eye prescription extract for a person in highest spherical power notation. |
|||||
| Distance. | Sphere | Cylinder | Axis | ||
| Right eye, (O.D) | +6.5 | -1.5 | 95 | ||
| Left eye, (O.S.) | +5.5 | -1 | 85 | ||
| Intermediate. | Add | ||||
| Right eye, (O.D) | +1 | ||||
| Left eye, (O.S.) | +1.25 | ||||
| Near | Add | ||||
| Right eye, (O.D) | +1.5 | ||||
| Left eye, (O.S.) | +1.75 | ||||
| Table 2. unsuitable format | |||||
| The same eye prescription for a person in the more unusual notation. |
|||||
| Distance. | Sphere | Cylinder | Axis | ||
| Right eye, (O.D) | +5 | +1.5 | 5 | ||
| Left eye, (O.S.) | +4.5 | +1 | 175 | ||
| Intermediate. | Add | ||||
| Right eye, (O.D) | +1 | ||||
| Left eye, (O.S.) | +1.25 | ||||
| Near | Add | ||||
| Right eye, (O.D) | +1.5 | ||||
| Left eye, (O.S.) | +1.75 | ||||
_
Two fictitious prescriptions have been produced in Tables 1 and 2. These make glasses that are identical, though they look quite different in their number content. The typical of format used throughout the world is the version in Table 1. Notice that both lenses in the prescription in Table 1 have higher Sphere values that the ones in Table 2. When an optician encounters a prescription that is not in the format of highest spherical power he simply transposes it. The method used is called flat transposition, and it consists of just a few simple sums.
_
Transposing the Format:
To transpose from (-) cylinder to (±) cylinder
A. add the cylindrical power to the spherical power
B. reverse the sign of the cylinder
C. add 90 degrees to the axis
_
Another task that your optician would take for granted is the modifying of the distance prescription for near or intermediate use. For voucher checking this just involves adding some numbers so it has been included also. Refer again to the prescription in Table 1. The main data of interest here describe the powers of the correction lenses. In fact powers are expressed in diopter. Because diopter values can be added directly, opticians prefer these to the difficulty of adding focal lengths. The focal lengths are the reciprocals of diopter. The figures seen in the Sphere, Cylinder, and Add boxes of the prescription are all power values; they are used by the optician to work out the details of lens grinding. Large power values also tell him that more material and more work will be needed to grind the lenses.
_
Some of the main prescription ideas are these:
•There are shorthand methods to express lens prescriptions
+6.5 -1.5 X 95 RIGHT
+5.5 -1 X 85 LEFT
•The Sphere column describes the uniform curvature of each lens. It is quite common for the left and right eyes to need different corrections. These curvature components can best be imagined as if they were sliced from the surface of a sphere.
•The Cylinder column is not always used. Only those with astigmatism will have these entries. When this is the case, these figures describe the extent to which the eyes’ functions deviate from the true spheres. These too are often different for each eye.
•The signs for the various lens powers can differ and negative and positive powers relate to divergent and convergent lens behaviour respectively.
•The Add values are power increments. These are added to their respective sphere figures for reading glasses (near), or for screen viewing glasses (intermediate). These increments are invariably positive and as such their signs are often missing.
•The Axis entry states the angle for the cylinder function. It tells the optician the angle from the horizontal at which to add the cylindrical compensation. These often differ for each eye.
_
In a nutshell:
1. Inspect the prescription to make sure that both lenses in the distance eye prescription are written in the format of highest spherical power. If they are not, then transpose them so that they both are.
2. Add the respective sphere increments if the glasses are for near or intermediate use, to make a new prescription.
_
Spherical lens:
+ means convex lens and DS means diopter spherical
_
Cylindrical lens:
-4.00X180 means concave cylinder with axis 180 meaning perpendicular to 180 i.e. at 90 degree or in vertical meridian lens is concave meaning eye has steep cornea in vertical meridian to be corrected by -4 cylinder.
_
Spherocylindrical lens:
+3 spherical with -1 at 180 deg means +3 spherical and 90 deg/vertical meridian -1 meaning +2 in vertical meridian.
__
Single vision prescription:
Single Vision prescriptions are for patients who have trouble seeing either near or far (but not both). The prescription has no value in the ADD column.
Bifocal/progressive vision prescription:
Bifocal prescriptions are for patients who have trouble seeing both near and far. The prescription has a value in the ADD column. You will only have an ADD measurement if you wear bifocal/progressives lenses. ADD corrections are almost always the same number for both eyes. If you happen to see the letters PAL(progressive additive lens) next to one of the numbers, or written elsewhere on your prescription, this means your doctor indicated that you will need a different ADD correction for progressive bifocals versus lined bifocals.
_
Prismatic Lenses:
Prismatic lenses are used in eyeglasses, not to change the focus of light rays, but to change their direction.
_
Figure above shows a simplified form of a prismatic lens. Note that the parallel rays entering the left side of this lens are still essentially parallel when leaving the right side. If the eye is located on the right side of the lens, the dotted lines show where the eye believes the rays are coming from. The viewed object thus appears to be higher than it actually is. Light rays are always bent toward the base or thick portion of the prism. The viewed object thus appears to be displaced toward the apex or top of the prism.
_
Prism correction:
Sometimes an image that one eye sees is not in line with what the one other eye sees, and so creates an impression of two images instead of only one. A lens which includes some amount of prism correction, will displace the viewed image, as seen by that eye, toward a direction so as to bring that image into proper binocular sync with the image that is viewed by the other eye. This prism correction is used to treat muscular imbalance or other conditions that cause errors in eye orientation, such as double-vision. Prism correction is measured in prism dioptres. A prescription that specifies prism correction will also specify the “base”, which is the direction of displacement. . Four abbreviations are used for prism direction: BU = base up; BD = base down; BI = base in (toward the wearer’s nose); BO = base out (toward the wearer’s ear). Whether a patient needs this type of correction or not is determined by the Pola-test (a test for the evaluation of binocular vision). Prism correction is commonly specified in prism dioptres, a unit of angular measurement that is loosely related to the dioptre. The prism dioptre of a lens is equal to one hundred times the tangent of the angle by which it displaces an image seen through the lens. Prism dioptre is represented by the Greek symbol delta (Δ). A prism of power 1Δ would produce 1 unit of displacement for an object held 100 units from the prism. Thus a prism of 1Δ would produce 1 cm visible displacement at 100 cm; 2Δ would produce 2 cm displacement at 100 cm, and so on.
________
How to read your Contact Lens Prescription:
To make a point consider this, “your eye glasses are at the minimum distance of 12mm from your eyes whereas your contact lenses rest on your eyes directly”. How can you expect your prescriptions to be the same for the both medical devices? The numbers for the refraction of the glasses and for the refraction of the contact lenses are different, especially for higher grades of myopia.
_
_
Additionally, the refractive power of the tear-liquid filled gap between the cornea and the contact lens has to be considered. For a flat fitted lens, this gap acts as an additional minus lens. The power of this additional lens can be between zero D for a lens fitted exactly to the cornea and – 1.00 D for rather flat fitted lenses and has to be considered when determining the power of the final lens: A change of 0.05 mm in the BCR (Base Curve Radius), or BOZR (Back Optic Zone Radius) results in a change of 0.25 D of the lens system, i.e. a lens that is 0.05 mm flatter has in effect – 0.25 D more refractive power.
_
Contact lens prescription:
A prescription for glasses is different than a prescription for contact lenses although they can be similar. A contact lens comes in direct contact with the cornea, which is the clear covering over the front surface of the eye. For this reason, there are additional measurements needed for fitting a contact lens and these need to be included in the prescription.
– the curvature of the cornea
– the diameter of the cornea
_
Base Curve (BC):
The curvature of the cornea is measured to determine the exact curvature (base curve) of the inside surface of the contact lens. This ensures the lens fits the shape of the eye providing optimum vision and comfort.
Diameter:
The lens diameter (DIA) specifies the overall size of the lens and, along with the base curve, determines how the lens fits. In most cases, the diameter of soft contact lenses ranges from 13.5 to 14.5 mm, and the diameter of rigid gas permeable (GP) contacts ranges from 8.5 to 9.5 mm.
Lens brand or material:
The lens brand and material also must be specified on a contact lens prescription, because each lens material has a specific degree of oxygen permeability (“breathability”). This is especially important if you want extended wear contact lenses or you occasionally fall asleep while wearing your contacts.
Expiration date:
Generally, a contact lens Rx is valid for one year. You will need to revisit your eye doctor when your prescription expires, for a checkup of the health of your eyes before you can purchase additional lenses. Eyeglass prescriptions are regulated under state law in the U.S, and most expire after two years.
_
Here is a typical contact lens prescription:
| RE | LE | |
| PWR | -1.25 | -2.00 |
| BC | 8.7 | 8.7 |
| DIA | 14 | 14 |
| CYL | -2.25 | -2.25 |
| AXIS | 160 | 160 |
| ADD | 1.75 | 1.75 |
| COLOR | Blue | Blue |
_
Toric (Astigmatism correcting):
Some patients require lenses that are toric or astigmatism correcting. Prescriptions for these types of lenses will also contain two additional numbers that relate to the correction of the astigmatism. These two numbers are usually separated by an “X” and read as “times”, they are indicated with the following symbols/abbreviations.
CYL – Cylinder (usually a number between -4.00 and +4.00)
AX – Axis (usually a number between 0 and 180)
Bifocal or Multifocal:
A smaller minority of patients require lenses that are bifocal or multifocal. Prescriptions for these types of lenses will contain an additional number with the following symbol/abbreviation.
ADD – Also known as “Add Power” or “Extra Strength”
_
A contact lens prescription can be the same as a prescription for glasses when:
– The prescription is a lower power, i.e.: -4.00 to +4.00 and
– There is absolutely no astigmatism present.
If you have any astigmatism or require a lens power greater than +/-4.00, the parameters of the contact lens can change.
– If you have astigmatism under 0.50, a spherical lens should be prescribed.
– Astigmatism of 0.50 to 0.75 can be effectively corrected with an aspheric lens.
– Astigmatism greater than 1.00 should be managed with a toric lens.
If your prescription power for glasses is greater than +/-4.00, you should see a difference in the power of your contact lens prescription. A quick way to estimate is to look at any prescription over 4 diopter, and subtract 0.25 diopter for every two diopter of increase. That means -10 diopter glasses would need -9.25 contact and +10 diopter glasses would need +9.25 contact.
___________
___________
Treatment of refractive error:
Rationale for treatment:
The major reasons for treating refractive errors are to improve a patient’s visual acuity, visual function, and visual comfort. It may be desirable to correct a very small error in one patient, whereas another patient may function well with no ill effects when the same very small refractive error is not corrected. Patients with moderate to high refractive errors generally require correction to achieve satisfactory vision. Other reasons for treatment include enhancing binocular vision (e.g., for driver safety), controlling strabismus (e.g., accommodative esotropia), and, on a societal level, preventing economic productivity loss associated with uncorrected refractive error. In some cases of unilateral refractive amblyopia it appears that there is a treatment benefit from refractive correction alone. Where amblyopia persists there is evidence that adding occlusion may further improves vision. In patients beyond visual maturity, uncorrected refractive errors do not result in amblyopia. At any age, uncorrected refractive errors do not lead to structural ocular damage or to worsening of the refractive status.
_
Who manages refractive errors?
These may be managed by optometrists (specialists in the diagnosis and management of refractive errors), orthoptists (specialists in ocular motility problems and assessment of refractive errors in very young children) or ophthalmologists (medically qualified physicians or surgeons). There are 3 ways of managing refractive errors.
1. Spectacles (eyeglasses or simply glasses):
Spectacles are the simplest, safest and most cost-effective way or managing refractive errors. Spectacle Lenses may be spheres, cylinders or a mixture of both. Spherical lenses are characterised by a constant curvature over the entire surface and may be convex (converge light rays, known as plus lenses) or concave (diverge light rays, known as minus lenses). Cylindrical lenses have focusing powers in one meridian only, the orientation of which depends on the patient’s problem. The power of a spectacle lens can be measured using an instrument known as a lensmeter. Lenses may have one or more refractive components to them, the latter being known as multifocal lenses. The power needed for each component can be assessed and prescribed separately.
2. Contact lenses:
Contact lenses work on the same principle as spectacle lenses but the space between the lens and the anterior surface of the cornea is reduced to the tear film alone.
3. Surgical correction (refractive surgery):
This may entail microsurgery (such as lens implants) or laser treatment to the cornea.
_
Most refractive errors are easily treatable by appropriate refractive correction. However, high refractive error in childhood may lead to amblyopia, resulting in permanent vision loss if it is not corrected during early childhood. Refractive correction can be by spectacles, contact lenses, or refractive surgery. Spectacles are the most commonly used form of refractive correction since they are the most inexpensive and the simplest of the three options; as such, they are the most appropriate treatment for refractive error in developing countries. However, all three forms of treatment for refractive error are relatively easily available and more affordable to individuals in developed countries.
_
Corrective lenses, whether as glasses or contact lenses, are necessary for children with refractive errors to correct vision and ensure that a child will achieve the best vision as possible as an adult. An important thing to understand about glasses is that they do not change the eyes. In other words, they do not “get rid” of the problem, or make it worse. However, amblyopia or “lazy eye” can get worse if a child does not use prescribed glasses. The need for updated glasses over time in children is caused by eye growth.
_
Treatment in developing countries:
The approach to dealing with refractive error in poorer countries is fairly straightforward. Detection of refractive error as a cause of poor vision, including the use of school screening, needs to become part of comprehensive eye care delivery. Training of non-medical staff in the ordering of appropriate glasses is part of the human resource development needed in all eye care programs. Glasses can be provided to all who need them if they are sourced from appropriate manufacturers and a system is developed to make them reliably, consistently and cheaply available within communities. Provision of spectacles is currently a challenge in many developing countries because of issues related to availability and affordability. There are often inequities in the availability of spectacles between urban and rural areas. Different strategies have been tried to increase the availability and affordability of reasonable-quality spectacles, with varying degrees of success. These include manufacturing low-cost spectacles in developing countries using trained staff, an approach that has been tried in Africa and Asia, use of ready-made spectacles with spherical correction for refractive errors, and provision of spectacles at cost price to the poor. Much work still needs to be carried out to optimize the logistics necessary to provide spectacles to all those who would otherwise be blind without them.
_
Do myopic need to permanent undercorrection for slowing progression of myopia?
Permanent undercorrection instead of undercorrection for Near Work only:
Permanent overcorrection is increasing myopia without any doubt. Many propose a permanent undercorrection. The studies show contradictory results. To answer the question whether full correction or undercorrection are more suitable to reduce the progression of myopia, schoolchildren were fitted with glasses where one eye was fully corrected for distance and the other eye was undercorrected by up to 2.00 D (monovision). As a result, Phillips found: “All children accommodated to read with the distance corrected (dominant) eye. Thus, the near corrected eye experienced myopic defocus at all levels of accommodation. Myopia progression in the near corrected eyes was significantly slower than in the distance corrected eyes and ..suggesting that sustained myopic defocus slows axial elongation of the human eye.” Myopia has traditionally been slightly undercorrected with the weakest negative lens that permitted good acuity. However, there are almost no data in the literature to suggest that undercorrection may be beneficial, other than Tokoro and Kabe. This study was not very well designed since treatments were mixed (atropine treatment and undercorrection by 1D in ten children, compared to 13 fully corrected children). Nevertheless, it was confirmed by Goss that the undercorrected group progressed more slowly (–0.54 D per year) compared to the fully corrected group (–0.75D per year; p<0.001). More recently, a better designed study was conducted in Malaysia. Full correction was given to 47 children (aged 9–13) and 47 children were intentionally undercorrected by 0.75D. In this study, the fully corrected group progressed more slowly (–0.77D per year) than the undercorrected group (–1.01D per year; difference about 20%, p<0.01). In both groups, the average progression of myopia was strikingly high. Although the second study should be more trustworthy, three additional points have to be kept in mind: (1) even with full correction at the time the glasses were prescribed, all children were undercorrected already after a few weeks due to the generally high myopia progression, (2) most myopic subjects have observed that their progression is restarted once new spectacles were prescribed, (3) that undercorrected eyes have a faster progression does not fit with what has been learned from animal models. Undercorrection should have a similar optical effect as wearing a positive lens and, accordingly, should generate a strong inhibitory signal for axial eye growth. On the other hand, overcorrection would be comparable to wearing an additional negative lens and should stimulate myopia progression. Overcorrection by 1–2D has been used in 4-year-old children as a potential therapy for intermittent exotropia .However, myopia progression was not enhanced in the overcorrected group (on average about 2.5 D progression over the following 6 years). Similar results were reported by Vasudevan et al: ‘Under-correction of myopia produced a small but progressively greater degree of myopic progression than did full correction’. Chung et al. wrote: ‘Although we have shown that a general undercorrection of the myopia tends to accelerate the progression of myopia, it is significant that a full distance correction for myopia, taken in conjunction with a progressive reading addition, reduces the progression of myopia’. Until there is a definite answer to the question about permanent undercorrection, the conclusion is that it is best for the eye
• to have permanently a clear focus
• to avoid excessive accommodation load.
Obviously, bifocals are matching these conditions best, but it appears to be hard to make use of this concept, as there are some ophthalmologists, optometrists and opticians, who do not like to apply this concept, and these bifocals are not so easy to fit properly. Therefore a solution without these bifocals is to use glasses with proper distance correction permanently, but to exchange them for glasses with a plus addition for longer time near work like reading, doing homework, making handicrafts, writing tests in school etc. Very careful determination of the right refraction is therefore an extremely important issue.
_
Nearpoint Stress:
Near point stress is literally stress on the visual system due to near work. Our visual system is ideally set for use at greater distances (like in the past when people had to hunt and gather and watch for bad things in the bushes) and not really designed to do a huge amount of detailed, near work. The need to look at near targets for long periods of time did not start happening until industrialism. In today’s world most of us spend a great deal of time working at close range, children and adults alike. Think about your average day; how much time do you spend reading, writing or working on a computer? Add to this time many hobbies like playing an instrument where you must read music, sewing, tye flies for fishing, pleasure reading, computer games, internet surfing, handheld gaming and a host of others. Increasing numbers of people are spending greater amounts of time working up close. All this time spent at near without allowing our eyes to relax the way they were meant to, often translates into overworking the visual system. Nearpoint stress may display itself as generalized eye fatigue, headaches, transient blurred vision (distance or near), or poor ability to concentrate on tasks up close. Often there are no consistent physical signs of near point stress, since people compensate in a variety of ways, so it is often overlooked. The muscles in your focusing system are often “clenched” in this position for hours and we call this an accommodative spasm. Practice good visual hygiene to minimize the effects of near point stress. If you must sit and do a lot of nearwork, every 15 minutes give yourself 15-20 seconds to look in the distance, out the window or across the classroom or office at an object far away. It should ideally be a distance greater than 20 feet. Make sure the object is as clear as you can make it during these 15-20 seconds before resuming your work. Children and adults alike should practice these techniques, teachers can call for “eye stretching” breaks during class time and parents can do the same when their children are studying or engaged in other near point activities. Remember, the best thing to minimize near point stress is having an efficient and flexible visual system.
_______
Eyeglasses and contact lenses: Introduction:
Eyeglasses and contact lenses are devices that correct refractive errors in vision. Eyeglass lenses are mounted in frames worn on the face, sitting mostly on the ears and nose, so that the lenses are positioned in front of the eyes. Contact lenses appear to be worn in direct contact with the cornea, but they actually float on a layer of tears that separates them from the cornea. A contact lens is a corrective, cosmetic, or therapeutic lens usually placed on the cornea of the eye. Glasses or spectacles are frames bearing lenses worn in front of the eyes, normally for vision correction, eye protection, or for protection from UV rays. The purpose of eyeglasses and contact lenses is to correct or improve the vision of people with nearsightedness (myopia), farsightedness (hyperopia), presbyopia, and astigmatism. Though contact lenses can be worn for up to 14 hours a day, one needs to switch to the traditional spectacles once the 14 hours run out. A new category of contact lenses which are disposable on a daily basis, offer comfort for over 14 hours. Contact lenses should be worn for the shortest period of time since it has a few hazards related to it. Spectacles have no upper limit for their usage. People allergic to certain plastics should not wear contact lenses or eyeglass frames or lenses manufactured from that type of plastic. People allergic to nickel should not wear Flexon frames. People at risk of being in accidents that might shatter glass lenses should wear plastic lenses, preferably polycarbonate. Lenses made from polycarbonate, the same type of plastic used for the space shuttle windshield, are about 50 times stronger than other lens materials. Also, people at risk of receiving electric shock should avoid metal frames. People employed in certain occupations may be prohibited from wearing contact lenses, or may be required to wear safety eyewear over the contact lenses. Some occupations, such as construction or auto repair, may require safety lenses and safety frames. Physicians and employers should be consulted for recommendations.
______
Eyeglasses (spectacles) [colloquially glasses]:
Eyeglasses or spectacles are instrument or device for aiding and correcting defective sight. Eyeglasses usually consist of a pair of lenses mounted in a frame to hold them in position before the eyes. Spectacles or glasses are used to correct disorders like myopia, hyperopia, astigmatism and presbyopia. Eyeglasses may be ancient in their origin but they are more popular than ever, despite recent innovations in contact lenses and vision correction surgery. Some people need reading glasses to correct their hyperopia and mild presbyopia conditions. Progressive and bifocal lenses used in glasses are used to treat both long sightedness and short sightedness. Progressive lenses differ from bifocals as they do not have a line or a visible demarcation differentiating between lenses when the user shifts from one lens to another.
• Safety glasses are also manufactured, where their primary motive is to protect the eye from flying debris. They are made from a variety of shatter-resistant glasses and need to be 1 mm thick at their thinnest point.
• Sunglasses are also another type of eye glasses that are used to provide protection against harsh visible light and UV light. They can be made with prescription or without it and are darkened to serve their purpose.
• Another popular type of eye glasses are the 3D glasses. These enable the wearer to view images that are specially prepared for 3D viewing.
Bioptics are those glasses that are used by people with severe eyesight impairment.
_
Eyeglasses are the simplest and safest means of correcting a refractive error; therefore, eyeglasses should be considered before contact lenses or refractive surgery. A patient’s eyeglasses and refraction should be evaluated whenever visual symptoms develop. Optimal eyeglass correction for higher refractive errors requires precision in fitting, especially with respect to the position of the optical center of each lens relative to the pupil. High-index lenses, which reduce the lens thickness and weight, are useful in correcting high refractive errors and providing increased comfort and better cosmetic appearance. When hyperopia is accompanied by esotropia, eyeglasses may be required to control the strabismus or to improve fusion. If minus lenses improve fusion in intermittent exotropia, eyeglass correction may be indicated even if the patient is not myopic. A nonrefractive, yet important, indication for eyeglasses is to protect the eyes from accidental injury. Safety glasses or eye protectors are strongly recommended for individuals involved in certain sports (e.g., racquetball, squash) and hazardous activities in which there is risk of flying particles (e.g., using hammers, saws, weed trimmers). They are also recommended for all individuals with good vision in only one eye. When ocular protection is the foremost consideration, polycarbonate plastic is the material of choice because it is much more impact resistant than regular plastic or hardened glass. Depending on the activity, frames with side protection may be important.
_
By far the commonest used correction for refractive errors are spectacles. An optometrist performs either a subjective or an objective assessment of your vision and prescribes the lenses (and even dispenses) you will need for your refractive error.
The advantages of using spectacles:
1. Cost effective
2. Freely available even in remote places
3. Can be worn and removed easily
4. Can be cleaned easily
_
The disadvantages:
1. Difficult to handle for children and sports persons
2. Misplaced or lost easily
3. Accidental breakage and “scratching” more common
4. Provided limited field of peripheral vision
5. Peripheral distortion specially in high powered lenses
6. “Heavy” to wear specially in high powered lenses
7. Some persons are prone to dermatitis over the bridge of the nose (contact dermatitis)
8. Some persons find it difficult to adjust to bifocals, trifocals and multifocals
9. Social stigma specially in children
_
How often should I change my glasses?
Generally an eyeglass prescription is good for a year, sometimes longer. Some circumstances may lead to a need for new glasses at a shorter interval. They include:
•Increasing nearsightedness in the teen years
•Presbyopia in midlife
•Developing cataracts
•Surgery
•Onset of diabetes
_
Difficulties and complications of eyeglass wear:
A variety of factors related to lenses and frames may cause difficulties in wearing eyeglasses. These include:
◦Incorrect prescription
◦Base curve and location of the cylinder on the front or back surface
◦Bifocal power and segment position (height and size)
◦Tint
◦Anisometropia (if large)
◦Prisms or prism effects
◦Pantoscopic tilt
◦Centration of lenses with respect to the pupil
◦Vertex distance
◦Size of frame and fit
◦Contact sensitivity to frame material
◦Change in lens material
In addition, the lenses in the eyeglasses can cause spherical and chromatic aberrations as well as lens distortions, including magnification (hyperopic lenses) and minification (myopic lenses).
_____
Eyeglass lens:
Lenses work by changing the direction of light so that images come into focus on the retina. The greater the index of refraction of the lens material and the greater the difference in the curvature between the two surfaces of the lens, the greater the change in direction of light that passes through it, and the greater the correction. Lenses can be unifocal, with one correction for all distances, or they can be correct for more than one distance (multifocal). One type of multifocal, the bifocal, has an area of the lens (usually at the bottom) that corrects for nearby objects (about 14 in from the eyes); the remainder of the lens corrects for distant objects (about 20 ft from the eyes). Another type of multifocal, a trifocal, has an area in-between that corrects for intermediate distances (usually about 28 in). Conventional bifocals and trifocals have visible lines between the areas of different correction; however, lenses where the correction gradually changes from one area to the other, without visible lines, have been available since the 1970s. Such lenses are sometimes called progressives or no-line bifocals. To be suitable for eyeglass lenses, a material must be transparent, without bubbles, and have a high index of refraction. The greater the index of refraction, the thinner the lens can be. Lenses are made from either glass or plastic (hard resin). The advantage of plastic is that it is lightweight and more impact resistant than glass. The advantage of glass is that it is scratch resistant and provides the clearest possible vision. Lenses today are more commonly made from plastic. Glass lenses are breakable and are about twice as heavy as plastic ones; however, they are more resistant to scratches. Plastic lenses scratch more easily, even with scratch-resistant coatings, but they are much lighter, less likely to break, and can be treated with ultraviolet filters and antiglare coatings.
_
Eyeglass lenses correct refractive errors by focusing light directly on the retina. The type of lens depends on the type and severity of the refractive error. The strength of a lens (i.e., its refractive power) is measured in optical units called diopters. This measurement indicates how much refractive power the lens must have to focus images directly on the retina. The higher the diopter, the stronger the lens!
The type of refractive error determines the lens’s shape:
• A concave (minus) lens is used to correct myopia (nearsightedness).
• A convex (plus) lens is used to correct hyperopia (farsightedness).
• A cylinder lens is frequently used to correct astigmatism, which is caused by distortions in the shape of the lens or cornea, the cylinder lens has two refractive powers on one lens. One power is placed over the entire lens and the other is oriented in one direction. This corrects the scattered pattern in which light enters the eye and creates one focal point on the retina.
_
Single vision lens (SVL):
Single vision lenses correct for only one distance. If they correct for far distance, the person must accommodate to see clearly up close. If the person cannot accommodate, they may need a separate pair of single vision glasses for near distances, or else use a multifocal lens.
_
Reading glass:
Reading glass has single vision lens that correct for only near vision (reading).
_
Single vision lenses correct for only distance or near vision. Patients with presbyopia or other disorders of accommodation often benefit from corrections for both distance and near vision. Infrequently, prism and base curve values may also be specified to correct for binocular vision disorders.
_
Multifocal Lenses
People that have more than one refractive error may require two pairs of eyeglasses or glasses with multifocal lenses. Multifocal lenses contain two or more vision-correcting prescriptions.
• Bifocals are the most common type of multifocal lenses. The lens is split in two sections; the upper part is for distance vision and the lower part for near vision.
_
• Trifocals have a third section used for middle distance vision
_
Varifocal or progressive lenses:
Varifocal lenses, also known as progressive lenses, are used for correcting presbyopia but unlike bifocal lenses have no visible dividing lines between the different corrections. Instead, they have a graduated section in which the power of the lens progresses smoothly from one prescription to the other, allowing the wearer to see clearly at all distances. They are characterised by a gradient of increasing lens power, added to the wearer’s correction for the other refractive errors. The gradient starts at the wearer’s distance prescription, at the top of the lens and reaches a maximum addition power, or the full reading addition, at the bottom of the lens. A range of varifocal designs is available depending on your lifestyle and occupation. Lens technology means that there are many different designs and materials to choose from. Your optometrist or dispensing optician will be able to advise you on the best lenses to suit your individual requirements. Progressive Lenses have no visible lines and provide a smooth gradual progression of power from distance vision on top through intermediate vision to near vision on bottom. Progressives have multiple focal areas unlike lined bifocals or trifocals which have only two or three. Progressive lenses are sometimes referred to as “no-line” bifocals because there is no noticeable line dividing the different prescriptions. There is a continuous change in magnification from the upper portion of the lens to the lower portion of the lens.
_
Plano:
Some people with good natural eyesight like to wear eyeglasses as a style accessory, or want to change the appearance of their eyes using novelty contact lenses. For these people, no power or acuity correction is required. Some may need a prescription in one lens in their spectacles, but not in the other. In this case the lens is simply a placeholder that does nothing, with equal parallel curved surfaces. This is referred to as a plano lens.
_
Adjustable focus:
Adjustable or variable focus dynamically adjusts focal length to allow clear vision at any distance. It is especially useful for treating the loss of accommodation common in presbyopia. “Adjustable focus eyewear” are glasses that can change their strength at the turn of a dial, depending on what activity you’re using them for. The Oxford-based company specialises in “adjustable focus eyewear” – glasses that can change their strength at the turn of a dial, depending on what activity you’re using them for. Around 600,000 pairs have been bought around the world in almost four years. The “Adlens Adjustables” are based on technology from the 1960s developed by the Nobel prize-winning physicist Luis Alvarez. The distinctive lens system on the glasses is made up of two polycarbonate plates on each eye which slide across each other by twisting the dials at each side. Where the plates sit determines the strength of the lenses. With this you can have [glasses for the] computer, reading, reading in bed [and] different lighting. Adlens has marketed the glasses as a temporary measure for when prescription glasses are lost or broken and for those with diabetes who see changes in their vision as blood levels fluctuate. Any fears that the self-diagnosis may damage the eye are unfounded as per the makers of the glasses. The visual system is really good at detecting discomfort and if, particularly on this product, if you turn it in and you get it wrong, you will feel it. If you go too far, you will feel your eye straining and you can very easily turn in the other direction.
__
Lens geometry:
Radius of Curvature of lens:
Before we can fully understand the thickness of a lens, we need to understand the geometry of a lens surface. A typical spherical lens surface is simply a section of a sphere. The curvature of a spherical lens surface is dictated by its radius of curvature, which controls how “steep” or “flat” the surface is. The larger the radius of curvature, the flatter the curvature of the surface. Conversely, the shorter the radius of curvature, the steeper the curvature of the surface. The radius of curvature of a surface is inversely proportional to its surface power. This means that, as the radius of curvature increases, the surface power decreases. Conversely, as the radius of curvature decreases, the surface power increases. This simply means that steeper surfaces produce stronger surface powers than flatter surfaces. For instance, the radius of a 6.00 diopter surface is twice as long as the radius of a 12.00 diopter surface. The relationship between the power of a surface, in diopters, and its radius of curvature, in meters, is given by:
Surface Power = (Refractive Index – 1) ÷ Radius
For example, consider a lens surface with an 83.2 mm (0.0832 m) radius of curvature, ground onto hard resin, which has a refractive index of 1.499. The surface power is equal to (1.499 – 1) ÷ 0.0832 = 6.00 D.
_
A lens is little more than two surfaces in a lens material separated by a finite amount of center or edge thickness. Note that “center” in these cases refers to the optical center of the lens, which is the point of zero prismatic effect. The power of each surface contributes to the total focal power of the lens. In fact, the total focal power of the lens, which is the capacity of a lens to add either convergence or divergence to incident waves of light, is simply the net effect of its two surfaces.
Focal Power:
The ability of a lens to refract and focus light—by either converging or diverging it—is referred to as its focal power or refractive power. The focal power of a lens is simply equal to the net effect of its front and back surfaces. When a refractionist writes a prescription for an ophthalmic lens, he/she is specifying the focal power of the lens.
The focal power of a lens, in diopters, is therefore given very nearly by:
Focal Power = Front Surface Power + Back Surface Power
For example, consider a lens with a 6.00 D front curve and a -4.00 D back curve. The focal power (P) is equal to F + B = 6.00 + (-4.00) = +2.00 D.
* This is an approximation to keep our math simple; the formula becomes a bit more complex when lens thickness is considered.
_
Lens Form:
_
The relationship between the front and back surface curves of a lens is referred to as the lens form (or lens profile). A lens with a given focal power can be produced by many different lens forms, as long as the sum of the front and back surface powers remains constant—or at least nearly so (neglecting thickness). A given lens power can be produced with an almost endless variety of lens forms, as long as the sum of the front and back surface powers remains equal to the desired focal power. Historically, spectacle lenses fall into either one of two general categories of lens form:
•Bent lenses: Modern lens form are generally bent, or meniscus—which means “crescent-shaped.” Bent lenses use convex front curves and concave back curves.
•Flat lenses: The earliest lens forms were flat. For plus lenses, flat lenses use either convex curves for both the front and back (i.e., bi-convex lenses), or one convex curve and one plano (plano) curve (i.e., plano-convex lenses). For minus lenses, flat lenses use either concave curves for both the front and back (i.e., bi-concave lenses), or one concave curve and one plano (plano) curve (i.e., plano-concave lenses).
_
Modern ophthalmic lenses are generally meniscus—or “crescent-shaped”—in form. This means that they typically have a convex front surface (i.e., positive power) and a concave back surface (i.e., negative power). Because focal power is the net effect of both surfaces, you can make three general statements concerning the relationship between the front and back surfaces and the thickness of the lens:
•Plus lenses: When the positive (convex) front surface is stronger than the negative (concave) back surface, the lens is generally a plus lens. The sagitta (or height) of the curve will be higher with stronger surface powers, which means that the convex front surface will be the highest surface. Consequently, by necessity, a plus lens will generally be thicker at the center and thinner at the edge.
•Minus lenses: When the negative (concave) back surface is stronger than the positive (convex) front surface, the net power of the two surfaces is negative and the lens is generally a minus lens. This means that the concave back surface will be the highest surface. Consequently, by necessity, a minus lens will generally be thicker at the edge and thinner at the center.
•Plano lenses: When the positive (convex) front surface is equal to the negative (concave) back surface, the net power of the two surfaces is essentially zero and the lens is usually a plano lens. Consequently, by necessity, a plano lens will generally have roughly the same thickness at both the center and the edge.
_
_
Focal power: As the magnitude (plus or minus) of the focal power increases, the maximum lens thickness also increases—and vice versa.
•Refractive index: As the refractive index of the lens material decreases, the maximum lens thickness increases—and vice versa.
•Lens diameter: As the size of the lens blank increases, the maximum lens thickness increases (rapidly)—and vice versa.
_
Minimizing lens thickness:
•Use of small frame sizes
•Centration.
•Refractive index. Use of high-index lens materials
•Aspheric lens designs usage
•Use of high-index lens materials
•Use of edge treatments and modifications
_
The figure below shows as refractive index of lens increases, thickness decreases:
_
Because the maximum edge thickness of a minus lens is more obvious to the wearer (and others) than the maximum center thickness of a plus lens, myopes (nearsighted wearers) are often more concerned with lens thickness. High index lenses are thinner and lighter as thinner edges require less lens material, which reduces the overall weight of the lenses.
_
_
Aspheric Lens Designs (flatter lens):
The use of special, non-spherical surfaces, referred to as aspheric surfaces, allows lens designers to flatten a lens form in order to improve cosmesis, without sacrificing opical performance. Flattening the form of a lens with a spherical base curve from traditional “best form” recommendations will result in significant optical errors—or lens aberrations—in the periphery of the lens, including oblique astigmatism. However, the lens aberrations produced by using flattened lens forms are neutralized by the surface astigmatism of the aspheric design. While aspheric lenses do not necessarily provide better vision than traditional lenses in lower powers, they do provide equivalent vision in a flatter, thinner, and lighter lens. However, in high plus prescriptions—above roughly +8.00 D—aspheric lens designs can provide considerably better vision than spherical base curves in any form.
_
Aspheric lenses allow lens designers to produce lenses that are considerably flatter, thinner, and lighter in weight than conventional (i.e., “best form”) lenses. Aspheric surfaces produce thinner lenses for two reasons:
•Aspheric lenses generally use flatter front curves, which reduce the center thickness in plus lenses and the edge thickness in minus lenses.
•The geometry of an aspheric surface also provides additional thickness reduction. Some aspheric lenses are even designed solely for cosmesis, and actually use more asphericity than what is optically required. This produces a thinner lens at the expense of reduced optical performance.
Aspheric base curves free lens designers from the constraints of conventional (best form) lenses—which use simple spherical base curves. Lenses can be made flatter, thinner, and lighter, while maintaining the same excellent optical performance. Moreover, aspheric lenses are essential in high plus prescriptions, since traditional spherical lens designs cannot eliminate lens aberrations in this prescription range.
_
The key benefits of aspheric lenses compared to spherical lenses are listed in the table below.
The combination of an aspheric design with high-index lens materials creates a lens that is noticeably slimmer, thinner and lighter than conventional glass or plastic lenses.
_
The figure below shows that flatter lens (aspheric lens) fits securely in a frame:
_
Flatter lens forms provide the following mechanical and cosmetic benefits:
•Flatter (less “bulge”)
•Thinner center thickness (plus) or edge thickness (minus)
•Lighter in weight
•Less magnification (or minification)
•Better frame retention (in plus powers)
____
Atoric Lens Design:
Each prescription power requires a unique front curve or lens design in order to achieve optimal optics. A single, rotationally-symmetrical lens surface cannot completely eliminate the power errors produced simultaneously by both principal meridians of sphero-cylindrical lenses with cylinder power. Consequently, standard best form and aspheric lens designs with prescribed cylinder power represent an optical compromise. Lenses must therefore be designed to optimize peripheral optical performance for either the sphere power meridian, the cylinder power meridian, or some power in between the two. It is possible, however, to eliminate the power errors associated with both the sphere power and cylinder power meridians of sphero-cylindrical lenses using a non-rotationally-symmetrical surface in which the asphericity varies from meridian to meridian. Atoric surfaces have two planes of symmetry corresponding to the principal meridians of the lens, each with a unique amount of asphericity to minimize the peripheral optical aberrations that would otherwise occur through that power meridian. Unlike the change in curvature away from the center of an aspheric lens surface, which remains the same through every radial meridian of the lens, the change in curvature away from the center of an atoric lens surface varies from meridian to meridian. Since any atoricity is most often applied to the toric surface of the lens, atoric can be thought of as a departure from a standard toric surface, just as aspheric refers to a departure from a spherical surface. When the prescription calls for significant cylinder power, the field of clear vision is often restricted through one or more planes of the lens, since a traditional base curve or aspheric lens design can only correct the optical aberrations associated with one power meridian. Atoric lens designs, on the ohter hand, provide unrestricted fields of clear vision, regardless of the power meridian of the lens, since the optical aberrations associated with each power meridian are corrected individually.
_
______
Types of corrective lenses:
1. Spherical lenses: All have equal curvatures in all meridians.
A. Convex, (+) lenses or convergent lenses are used for the correction of hyperopia, presbyopia and aphakia. They make objects look larger in size.
B. Concave, (-) lenses or divergent lenses are used for the correction of myopia. They make objects look smaller in size.
2. Cylindrical or toric lenses:
One meridian is curved more than all the other ones. They are used to correct astigmatism.
3. Prisms:
A prism is an optical device composed of 2 refracting surfaces that are inclined toward one another. It has an apex and a base. It refracts light toward its base whereas an object seen through a prism appears deviated toward the apex of the prism. It does not change the size of an object. Prisms are used to correct strabismus.
_
Components of a sphero-cylindrical correction:
Sphere component:
Every corrective lens prescription includes a spherical correction in diopters. Convergent powers are positive (e.g., +4.00 D) and condense light to correct for farsightedness (hyperopia) or allow the patient to read more comfortably (see presbyopia and binocular vision disorders). Divergent powers are negative (e.g., −3.75 D) and spread out light to correct for nearsightedness (myopia). If neither convergence nor divergence is required in the prescription, “plano” is used to denote a refractive power of zero. The term “sphere” comes from the concept that the basic geometry of a corrective lens is a series of curved surfaces that are sections of spheres. These surfaces can be modified as needed to generate more complex corrections by using more complex geometry. The “cylinder” and “axis” components specify how a particular lens is different from a lens composed of purely spherical surfaces.
Cylinder component:
If a patient has astigmatism, he needs a toric lens to see clearly. The geometry of a toric lens focuses light differently in different meridians. For example, a toric lens, when rotated correctly, could focus a horizontal line to a series of points at one focal distance while focusing a vertical line to a separate focal plane. The power of a toric lens can be specified by describing how the cylinder (the meridian that is most different from the spherical power) differs from the spherical power. Power evenly transitions between the two powers as you move from the meridian with the most convergence to the meridian with the least convergence or most divergence. For regular toric lenses, these powers are perpendicular to each other and their location relative to vertical and horizontal are specified by the axis component. There are two different conventions for indicating the amount of cylinder: “plus cylinder notation” and “minus cylinder notation”. In the former, the cylinder power is a number of diopters more convergent than the sphere power. That means the spherical power describes the most divergent meridian and the cylindrical component describes the most convergent. In the latter, the cylinder power is a number of diopters more divergent than the sphere component. Thus the sphere power describes the most convergent meridian and the cylinder component describes the most divergent. Europe typically follows the plus cylinder convention while the US typically follows the minus cylinder convention. Minus cylinder notation is also more common in Asia, although either style may be encountered there. There is no difference in these forms of notation and it is easy to convert between them: simply add the sphere and cylinder numbers together to produce the converted sphere—then change the sign of the cylinder number. For example a lens with a vertical power of -3.75 and a horizontal power of -2.25 could be specified as either -2.25, -1.50 or -3.75, +1.50. [vide supra transposition]
Axis component:
The axis defines the location of the sphere and cylinder powers. The name “axis” comes from the concept of generating a cylinder by rotating a one line around an axis. The curve of that cylinder is 90° from that axis of rotation. When dealing with toric lenses, the axis defines the orientation of the steepest and flattest curvatures relative to horizontal and vertical. The “3 o’clock” position is defined as zero, and the 90th meridian is a vertical line. A horizontal line passes through both zero and the 180th meridians. By convention, a horizontal axis is recorded as 180. In a typical toric lens, the flattest and steepest curvatures are separated by 90°. As a result, the axis of the cylinder is also the meridian containing the sphere power. The cylinder power, as defined above is the power that is most different from the sphere power. Because they are defined relative to each other, it is important to know if the lens is being described in minus cylinder notation, where the sphere power is the most convergent / least divergent power. When using plus cylinder notation, the opposite is true.
_
If the lens is spherical (there is no cylinder component) then there is no need for an axis. A prescription like this is written with D.S. (diopters sphere) after the spherical power (e.g., −3.00 D.S.).
In a nutshell:
•correction power is measured in diopters
•by convention, an axis of 90° is vertical, 0° or 180° are horizontal
•if the cylinder power is positive, the lens is most convergent 90° from the axis
•if the cylinder power is negative, the lens is most divergent 90° from the axis
•if the cylinder power is zero (D.S.), the lens is spherical and has the same power in every meridian
Sample prescription:
So, a prescription of −1.00 +0.25 x 180 describes a lens that has a horizontal power of −1.00 D and a vertical power of −0.75.
________
Ways to reduce the weight and thickness of spectacle lenses, in approximate order of importance are these:
•Choose spectacle frames with small lenses; that is to say, so that the longest measurement across the lens at any angle is as short as possible. This gives the greatest advantage of all.
•Choose a frame that allows the pupil to occupy the exact middle point of the lens.
•Choose a lens as near round as possible. These are less commonly found than other shapes.
•Choose as high a refractive index for the lens material as cost permits.
It is not always possible to follow the above points, because of the rarity of such frames, and the need for more pleasing appearance. However, these are the main factors to consider if ever it should become necessary and possible to do so.
______
Eyeglass lens material:
_
Here are popular eyeglass lens materials, arranged in order of refractive index and lens thickness (pretty good indicators of cost). Except for the crown glass, these are all plastic materials.
| Lens Material | Refractive Index | Abbe Value | Key Features and Benefits |
| High-index plastics | 1.70 to 1.74 | 36 (1.70) 33 (1.74) |
The thinnest lenses available. Block 100 percent UV. Lightweight. |
| High-index plastics | 1.60 to 1.67 | 36 (1.60) 32 (1.67) |
Thin and lightweight. Block 100 percent UV. Less costly than 1.70-1.74 high-index lenses. |
| Tribrid | 1.60 | 41 | Thin and lightweight. Significantly more impact-resistant than CR-39 plastic and high-index plastic lenses (except polycarbonate and Trivex). Higher Abbe value than polycarbonate. Downside: Not yet available in a wide variety of lens designs. |
| Polycarbonate | 1.586 | 30 | Superior impact resistance. Blocks 100 percent UV. Lighter than high-index plastic lenses. |
| Trivex | 1.54 | 45 | Superior impact resistance. Blocks 100 percent UV. Higher Abbe value than polycarbonate. Lightest lens material available. |
| CR-39 plastic | 1.498 | 58 | Excellent optics. Low cost. Downside: thickness. |
| Crown glass | 1.523 | 59 | Excellent optics. Low cost. Downsides: heavy, breakable. |
___
___
Glass Lenses:
| PROS | CONS |
|
|
____
Plastic Lenses:
| PROS | CONS |
|
|
_______
Why plastic is preferred
Most modern spectacle lenses are made from plastic as opposed to glass. Glass lenses, whilst providing excellent optical clarity and scratch resistance, are heavy to wear and potentially hazardous as they are subject to shattering.
Plastic lenses provide spectacle wearers with many advantages:
• excellent clarity of vision
• light and comfortable to wear
• impact resistance
Your optometrist will recommend the type of lens material ideal for you, taking into account your visual requirements, lifestyle, cosmetic considerations and frame choice.
______
High-Powered Lenses:
As the power of a spectacle lens increases, the optical and mechanical issues associated with lens power also increase. For prescription powers stronger than ±4.00 diopters, the fit and design of the lens become especially critical due to the sensitivity of these higher powers to changes in lens design or position. This means that great care must be taken when fitting and dispensing high-powered lenses in order to ensure maximum optical performance and visual comfort for the wearer. The following factors should be considered when fitting and dispensing high-powered lenses:
•Magnification and field of view. The magnification produced by plus lenses results in a relatively small field of view through the spectacle lens. This magnification also results in the unappealing “bug-eye” effect visible to others. Keeping the vertex distance of the lenses as short as possible and using a flatter, aspheric lens design will minimize magnification and its related effects.
•Lens reflections. The thick edges of high minus lenses produce internal reflections, known as power rings, which are visible to others and exacerbate the apparent thickness of the lens. An anti-reflection coating will eliminate these annoying reflections and also improve the overall appearance of the lens.
•Optical aberrations. High-powered lenses are subject to greater optical aberrations in the periphery of the lens than low-powered lenses, including oblique astigmatism and chromatic aberration. Therefore, proper base curve selection in critical in order to ensure that the wearer enjoys a wide field of clear vision. Lens materials with high Abbe values are also highly recommended.
•Vertex distance. As the vertex distance—or distance from the back surface of the lens to the cornea of the eye—changes, the power of the lens as perceived by the wearer effectively changes as well. Increasing the vertex distance, for instance, increases the effective power of a plus lens and decreases the effective power of a minus lens. In some cases the refractionist may note a refracted vertex distance, which is the vertex distance of the trial lenses used during the examination. If the fitted vertex distance of the actual frame differs from the refracted vertex distance, the ordered powers of the lens should be adjusted accordingly.
•Lens tilt. Any excessive lens tilt, including pantoscopic tilt (that is, lens tilt toward the cheek) and face-form tilt (that is, “wrap”), will also induce a form of oblique astigmatism due to lens tilt. The oblique astigmatism induced by lens tilt can be minimized by ensuring that the optical axis of the lens passes through the center of rotation (C) of the eye. We can accomplish this by manipulating the relationship between the pantoscopic tilt and the height (H) of the wearer’s pupil center above the optical center (OC) of the lens according to Martin’s rule of tilt, which states that you should ensure 1 mm of Optical Center Drop (H) for Every 2° of Pantoscopic Tilt. You can also compensate for the effect by changing the ordered powers of the lens.
____
Image size in eyeglass correction:
Retinal image size is determined by many factors. The size and position of the object being viewed affects the characteristics of the light entering the system. Corrective lenses affect these characteristics and are used commonly to correct refractive error. The optics of the eye including its refractive power and axial length also play a major role in retinal image size. In uncorrected axial ametropia, the “basic” retinal image is smaller in hyperopia and larger in myopia than that in emmetropia by about 2 per cent for every diopter of error. In corrected axial ametropia, the retinal image is the same size in all three conditions. In refractive ametropia, the “basic” retinal image is smaller in hyperopia and larger in myopia than that in emmetropia by about 0.5 per cent for every diopter of error. The correcting lens makes the retinal image larger in hyperopia and smaller in myopia than that in emmetropia by about 1.7 to 1.6 per cent for every diopter of correction. These features place the refractive hyperope and the axial myope in a more favoured condition for effective seeing.
_____
Lens Aberrations:
The principal impetus behind lens form selection is optical performance. Base curves are typically chosen to provide a wide field of clear vision. It turns out that the form of a lens will have a significant impact on the clarity of peripheral vision experienced by the wearer. Although vision through the center of a lens will be relatively sharp no matter what the form, vision through the periphery of a lens will vary greatly as a function of lens form. Peripheral vision generally requires the wearer to look away from the optical center of the lens. As a result, the wearer’s line of sight makes an angle to optical axis of the lens, which is the imaginary line passing through the optical center. Consequently, we often refer to the peripheral performance of a spectacle lens as its off-axis or off-center performance. During peripheral and dynamic vision, the line of sight makes an angle to the optical axis of up to 30° or more as the wearer observes objects in the visual field. When the incident rays of light make larger and larger angles to the optical axis, incident rays of light are no longer brought to a single point focus at the desired focal point of the lens. This error in focus is referred to as a lens aberration.
_
You can also think of a lens aberration as the failure of a lens, which has otherwise been made correctly, to produce a sharp focus at the desired focal point of the lens as the eye rotates behind it in order to view objects in the periphery. The focal power of the lens is prescribed to produce a focus at the far-point of the eye. The far-point (FP) of the eye is conjugate to the retina, meaning that rays of light from a lens that come to a focus at the far-point will also be brought to a focus at the retina once refracted by the eye. Hence, the far-point represents the ideal focal plane of the spectacle lens. As the eye rotates vertically and horizontally behind the lens, the far-point moves with the eye at a fixed distance from its center of rotation (C). This movement describes an imaginary spherical surface, known as the far-point sphere, which represents the ideal locus of focal points for the lens as the eye rotates to look through it. Lens aberrations result when light refracted by a lens fails to come to a focus at the far-point sphere.
_
Lens aberrations act as errors in power from the desired prescription, and can degrade the image quality produced by the lens as the wearer gazes away from—or obliquely to—its optical axis. There are six different lens aberrations that can affect the quality of peripheral vision through a spectacle lens:
•Oblique Astigmatism
•Power Error
•Spherical Aberration
•Coma
•Distortion
•Chromatic Aberration
_
Lens induced oblique astigmatism:
As the eye shifts its gaze from looking through the optical center of the corrective lens, the lens induced astigmatism value increases. In a spherical lens, especially one with a strong correction whose base curve is not in the best spherical form, such increases can significantly impact the clarity of vision in the periphery. As corrective power increases, even optimally designed lenses will have distortion that can be noticed by a user. This particularly affects individuals that use the off-axis areas of their lenses for visually demanding tasks. For individuals sensitive to lens errors, the best way to eliminate lens induced aberrations is to use contact lenses. Contacts eliminate all these aberrations since the lens then moves with the eye.
_
Chromatic aberration: [discussed vide supra]
Chromatic aberration, is a consequence of the dispersive properties of the actual lens material, and is not a function of lens design. Chromatic dispersion is a result of the fact that colors of light with shorter wavelengths, like blue, travel more slowly through most transparent materials than colors with longer wavelengths, like red. Therefore, blue light generally has a higher refractive index than red light. However, this is usually only a concern for certain high-index lens materials, since the differences in refractive index between colors is more dramatic.
_
The figure above shows close-up of color shifting through corner of eyeglasses. The light and dark borders visible between color swatches do not exist. Of all of the properties of a particular lens material, the one that most closely relates to its optical performance is its dispersion, which is specified by the Abbe number. Lower Abbe numbers result in the presence of chromatic aberration (i.e., color fringes above/below or to the left/right of a high contrast object), especially in larger lens sizes and stronger prescriptions (±4D or greater). Generally, lower Abbe numbers are a property of mid and higher index lenses that cannot be avoided, regardless of the material used. The Abbe number for a material at a particular refractive index formulation is usually specified as its Abbe value. In practice, a change from 30 to 32 Abbe will not have a practically noticeable benefit, but a change from 30 to 47 could be beneficial for users with strong prescriptions that move their eyes and look ‘off-axis’ of optical center of the lens. Abbe values even as high as that of (Vd≤45) produce chromatic aberrations which can be perceptible to a user in lenses larger than 40 mm in diameter and especially in strengths that are in excess of ±4D. At ±8D even glass (Vd≤58) produces chromatic aberration that can be noticed by a user. Chromatic aberration is independent of the lens being of spherical, aspheric, or atoric design. Color fringing can make accurate drawing and painting difficult for users of strong eyeglass prescriptions. Strongly near-sighted wearers of contact lenses do not experience chromatic aberration because the lens moves with the cornea and always stays centered in the middle of the wearer’s gaze.
_
Curvature of field:
Curvature of field causes a planar object to project a curved (nonplanar) image. It can be thought of as arising from a “power error” for rays at a large angle. Those rays see then lens as having an effectively smaller diameter and an effectively higher power, forming the image of the off axis points closer to the lens.
__________
__________
Free-form Design:
‘A new technology that could change the way you see—forever.’
Called ‘free-form’ these lenses are Aspheric. However using the latest free-form technology, they are cut using a digital design manufacturing process that takes into consideration over 40,000 points across the lens enabling lenses to be produced with 0.01D power accuracy. This gives lens designers the ability to reduce lens aberrations even more than they are using conventional lens design and processing techniques. Lighter and thinner than standard lenses they provide exceptional night/low light vision reducing glare and halo effects from car headlights. They also offer exceptional contrast perception sharpening vision and improved colour rendition providing brighter and more intense colours. While everyone can benefit to a certain extent from free-form lenses, since these lenses are usually made with more aberration & distortion control and improved power accuracy, individuals with higher eyeglass prescriptions will notice greater benefits than people with only mild prescriptions. They also benefit people with complex prescriptions and those that select frames with higher base curve lenses which are more complex to produce. Free form lenses can ensure they will provide good vision across the whole curvature of the lens and avoid the optical distortions that can occur in the periphery area of vision with standard lenses.
_
The free-form digital progressive lens is the most popular one these days. They have many advantages over normal progressives.
1. Compared with regular progressives, it offers up to 20% larger areas of clear vision, better color perception, better peripheral vision and minimal distortion.
2. It also provides better control of image distortion, providing unprecedented levels of optical clarity.
3. It offers quicker adaptation thanks to optimal design ergonomics that fully respect the routine movements of new progressive wearers and wearers of progressive lenses with a different design.
_
What should I know about lens colours?
Lenses can be clear, tinted, photochromic or polarized. Each type offers various levels of ultraviolet protection, including no protection (even when colored). Do not be fooled by the color of the lenses.
_
The Coating of the Glass:
Without a coating, there would be very disturbing reflections on the surface of the glass, for example making the eyes “invisible” to other people, and which create reflections of light which are very disturbing during night driving. For organic glasses there is another reason for coating: The relatively soft surface has to be protected from getting scratched too easily. Overall, up to ten layers have to be brought to the lens, and significant differences in quality (and price) can be found for lenses from different manufacturers, and for different product lines of the same manufacturer.
_
AR (anti-reflective) Coating:
All lens materials block some light from passing through the lens. This light reflects back from the lens surface, causing distractions and reducing the clarity of night vision. Conventional glass or plastic lenses reflect about 8 percent of light that otherwise would reach the eye. High-index lenses reflect up to 50 percent more light than conventional glass or plastic lenses. For the best vision and appearance, it’s a good idea to have an anti-reflective lens coating (AR coating) applied to high-index lenses. AR-coated high-index lenses transmit up to 99.5 percent of light to the eye for optimum vision. And because AR coating virtually eliminates lens reflections, it makes high-index lenses appear nearly invisible, so others see your eyes, not your lenses. Also, studies have shown that eyeglass lenses with anti-reflective coatings provide sharper night vision with less glare — a real advantage for night drivers.
_
Scratch-Resistant Coatings:
Not all eyeglass lenses are scratch proof or even scratch resistant – not even those made of glass. Treating lenses with a clear, hard coating, front and back, makes both plastic and glass lenses more impervious to scratches. Hard-coated, scratch-resistant eyeglasses are also perfect for kids. Nearly all high-index lenses (including polycarbonate) come with a factory-applied scratch-resistant coating for added durability. This coating is optional for regular plastic lenses. However, to safeguard your eyewear investment, scratch-resistant coating should be considered for all eyeglass lenses. The only exception is glass lenses, which are naturally hard and scratch-resistant. To further protect your eyeglasses from scratches, keep them in a protective case when you’re not wearing them. Also, never clean your lenses without first rinsing them with water or an approved cleaning solution. Rubbing a dry, dusty or dirty lens with a cleaning cloth or towel can cause scratches, even if the lens is treated with a scratch-resistant coating.
_
UV Treatment keeps your eyes Safe:
Ultraviolet (UV) treatment of eyeglass lenses blocks the rays of the sun and prevents them from harming your eyes in the same way sunscreen blocks the rays that damage your skin. Constant exposure of your eyes to the ultraviolet rays of the sun may eventually cause retinal damage, cataracts, and other eye problems. Almost all high index lenses have a built-in 100% UV protection feature. But with regular plastic lenses, a lens treatment is required for these lenses to block all UV rays. This UV treatment does not change the appearance of the lenses and is quite inexpensive.
_
Tinted lenses:
Sometimes a light or dark hint of color on the eyeglass lens can be beneficial to aid in vision. For example, a yellow tint may increase contrast and a gray tint may not alter color perception with sunglasses. A light tint can also hide the signs of aging around the eyes.
_
Mirror coatings:
If you are looking for a purely cosmetic lens that allows the eyes to be hidden from view, then this is the coating for you. Mirror coatings come in a variety of colors such as silver, gold, and blue. Mirrored lenses, having a metallic, partially reflective coating on the outer surface, combined with a tinted glass lens, are an alternative to polarization for UV protection, improving contrast when depth perception is important such as seeing moguls and ice while skiing or snowboarding. The mirrored lens reflects glare to protect the eyes, but improves the ability to see contrasts, and mirrored lenses of different colors can expand the range of fashion styles.
__
Multi-coated lenses:
Multi-coated lenses incorporate a combination of coatings – anti-reflection, scratch-resistant, water repellent and ultraviolet protected – to combine to improve the properties of your glasses.
____
Goggles (safety glasses):
Goggles or safety glasses are forms of protective eyewear that usually enclose or protect the area surrounding the eye in order to prevent particulates, water or chemicals from striking the eyes. These are special eyewear systems designed for protecting the eye from excessive heat, dust, light, harmful rays, or impact. They are used in chemistry laboratories and in woodworking. They are often used in snow sports as well, and in swimming. Goggles are often worn when using power tools such as drills or chainsaws to prevent flying particles from damaging the eyes. This eyewear is suitable for people working in extremes of environment like welders, bikers, those living in extremes of weather, those handling harmful chemicals etc. Many types of goggles are available as prescription goggles for those with vision problems.
____
Sunglasses:
Looking at the sun may not only cause headache and distort your vision temporarily, but it can also cause permanent eye damage. Any exposure to sunlight adds to the cumulative effects of ultraviolet radiation on your eyes. UV exposure has been linked to eye disorders such as macular degeneration, solar retinitis, and corneal dystrophies. The most dangerous time for sun gazing is during a solar eclipse. The brightness of the sun is hidden; but the dangerous invisible rays that permanently burn your eyes are not reduced. You should never look at a welder without the appropriate eye protection because light from this process can damage your eyes and/or foreign matter can get into your eyes. As always, it is best to wear eye protection or sunglasses to protect your eyes as much as possible.
_
Sunglasses or sun glasses are a form of protective eyewear designed primarily to prevent bright sunlight and high-energy visible light from damaging or discomforting the eyes. They can sometimes also function as a visual aid, as variously termed spectacles or glasses exist, featuring lenses that are colored, polarized or darkened. Healthcare professionals recommend eye protection whenever the sun comes out to protect the eyes from ultraviolet radiation (UV) and blue light, which can cause several serious eye problems. Its usage is mandatory immediately after some surgical procedures such as IntraLASIK and recommended for a certain time period in dusty areas, when leaving the house and in front of a TV screen or computer monitor after LASEK. Sunglasses have long been associated with celebrities and film actors primarily from a desire to mask their identity. Since the 1940s sunglasses have been popular as a fashion accessory, especially on the beach.
_
Medical experts advise the public on the importance of wearing sunglasses to protect the eyes from UV; for adequate protection, experts recommend sunglasses that reflect or filter out 99-100% of UVA and UVB light, with wavelengths up to 400 nm. Sunglasses which meet this requirement are often labeled as “UV400.” This is slightly more protection than the widely used standard of the European Union, which requires that 95% of the radiation up to only 380 nm must be reflected or filtered out. Sunglasses are not sufficient to protect the eyes against permanent harm from looking directly at the Sun, even during a solar eclipse.
_
Though it is important to always look for labels when buying sunglasses to protect you from UV rays, you should also recognize the 3 categories of sunglasses that comply with industry standards and know what they mean in terms of UV protection.
1. Cosmetic Sunglasses- Have lightly lenses that are good for use in sunlight that is not too harsh. These glasses block 0-60% of visible light and UVA rays, and between 87-5 and 95% of UVB rays. Not recommended for daylight driving.
2. General Purpose Sunglasses- Block From 60-92% of visible light and UVA rays, and between 95 and 99% of UVB rays. Good for driving and recommended for use in harsh sunlight.
3. Special Purpose Sunglasses- Block up to 97% of visible light and up to 98.5% of UVA rays. Suitable for prolonged sun exposure, but are not recommended for driving.
____
Photochromic lenses:
Photochromic lenses are lenses that darken on exposure to specific types of light, most commonly ultraviolet (UV) radiation. Once the light source is removed (for example by walking indoors), the lenses will gradually return to their clear state. Photochromic lenses may be made of glass, polycarbonate, or another plastic. Photochromatic lenses contain millions of molecules of silver chloride or another silver halide embedded within them. These molecules are transparent to visible light in the absence of ultraviolet rays, which is normal for artificial lighting. When exposed to ultraviolet (UV) rays, as in direct sunlight, the molecules undergo a chemical process that causes them to change shape and absorb portions of the visible light, causing the lenses to darken. This process is reversible; once the lens is removed from strong sources of UV rays, the silver compounds return to a state which allows all light through. The reason these lenses darken in sunlight but not indoors under artificial light, is that room light does not contain the UV (short wavelength light) found in sunlight. Automobile windows also block UV so these lenses would darken less in a car. Typically, photochromic lenses darken substantially in response to UV light in less than one minute, and then continue to darken very slightly over the next fifteen minutes. The lenses fade back to clear along a similar pattern. The lenses will begin to clear as soon as they are away from UV light, and will be noticeably lighter within two minutes and mostly clear within five minutes. However, it normally takes more than fifteen minutes for the lenses to completely fade to their non-exposed state. A report by the Institute of Ophthalmology at the University College London has suggested that even in dark conditions photochromic lenses can absorb up to 20% of ambient light.
_
Polarized sunglasses:
Polarized sunglasses have been popular for years with boaters and fishermen who need to reduce reflected glare from the water surrounding them. But now that many others who spend time outdoors have discovered the benefits of polarized lenses, interest in these types of sunglasses has soared. Besides boaters, outdoor enthusiasts who benefit the most from polarized sunglasses include skiers, bikers, golfers and joggers, all who may enjoy a clearer view along with elimination of glare. These sunglasses can be used for driving and, in fact, can reduce glare from a long, flat surface such as the hood of the car or the road’s surface. Polarized sunglasses also can be worn indoors by light-sensitive people, including post-cataract surgery patients and those continually exposed to bright light through windows. Light reflected from surfaces such as a flat road or smooth water generally is horizontally polarized. This means that, instead of light being scattered in all directions in more usual ways, reflected light generally travels in a more horizontally oriented direction. This creates an annoying and sometimes dangerous intensity of light that we experience as glare. Polarized sunglasses reduce glare reflected off of roads, bodies of water, snow, and other horizontal surfaces. Polarized sunglasses cut glare and haze so your eyes are more comfortable and you can see better.
_
Polarized lenses contain a special filter that blocks this type of intense reflected light, reducing glare. Though polarized sunglasses improve comfort and visibility, you will encounter some instances when these lenses may not be advisable. One example is downhill skiing, where you don’t want to block light reflecting off icy patches because this alerts skiers to hazards they are approaching. In addition, polarized lenses may reduce the visibility of images produced by liquid crystal displays (LCDs) or light-emitting diode displays (LEDs) found on the dashboards of some cars or in other places such as the digital screens on automatic teller machines and self-service gas pumps. With polarized lenses, you also may be unable to see your cell phone or GPS device. Boaters and pilots also have reported similar problems when viewing LCD displays on instrument panels, which can be a crucial issue when it comes to making split-second decisions based strictly on information displayed on a panel. Polarized bifocal sunglasses or progressive lenses are examples of options for the presbyope who also likes outdoor sports. And polarized photochromic lenses, which change from dark outside to light inside, may be right for the light-sensitive person who frequently is in and out of the sun on any given day. Whether you spend your time waterskiing or boating, in-line skating or mountain biking, driving or jogging, polarized sunglasses may be the right choice to help you enjoy your life outdoors.
_
Using pinholes as sunglasses:
A serious limitation of ordinary sunglasses that is not obvious to the average user is that they degrade the vision in two ways. The obvious way is that they reduce the amount of light entering the eye, making everything darker and harder to see. The less obvious way is that any refractive error (nearsightedness, farsightedness, astigmatism) is made worse. This happens because the pupil becomes wider to compensate for the loss of light when the glasses are put on. And the wider the pupil, the more any refractive error contributes to poor vision. This is a simple thing for anyone to verify. Of course, one answer to this problem is to buy expensive prescription sunglasses. And new glasses must be purchased whenever there is a substantial change in the vision. Conventional, hole-type pinhole glasses also reduce the brightness of the sun, just like sunglasses. But they do so by creating a smaller pupil which improves the vision. This is also a simple thing to verify. Just put on a pair of pinholes on a sunny day and see how the brightness of the sun is reduced. One drawback of this solution is that the glasses have no ultraviolet protection. But the most extraordinary use of pinholes in place of ordinary sunglasses is with the new smooth-lens pinholes. In addition to the light reduction that is provided by the small holes, the lenses have built-in UV protection. So you get a sunglass effect and better vision at the same time with no need for expensive prescription sunglasses. Smooth-lens pinholes are really the ultimate in eyewear. They are inexpensive, stylish, improve visual acuity, function as sunglasses, can be used indoors or outdoors, and can last a lifetime.
_____
Among the most popular eyeglass lenses and lens treatments prescribed today are:
Aspheric lenses, which are not perfectly rounded on the surface, recently have been designed as a way to correct for small distortions in vision that can be associated with more traditional lenses. These types of designs also make lenses thinner and lighter. High-index materials also are associated with thinner, lighter lenses, because of the more efficient way this special plastic refracts light to help you achieve focus. Because less plastic is needed with high-index materials, lens thickness is reduced. Wavefront technology lenses are fabricated based on very precise measurements of the way light travels through your eye, which helps sharpen visual clarity. Polycarbonate and Trivex lenses are thinner, lighter and up to 10 times more impact-resistant than regular plastic lenses, making them the perfect choice for safety glasses, sports eyewear and eyeglasses for children and active adults. Photochromic lenses have chemical coatings or special internal changes allowing them to quickly darken in bright conditions, and quickly return to normal in ordinary indoor lighting or at night. Polarized lenses diminish glare from flat, reflective surfaces (like water) and also reduce eye fatigue. Anti-reflective coating is a popular add-on for lenses. AR (anti-reflective) coating can dramatically improve the look and comfort of your glasses by reducing distracting lens reflections that interfere with eye contact and make your lenses look thicker. AR-coated lenses also reduce glare and allow more light into your eyes for better night vision.
_________
Eyeglass frames:
Frames can be made from metal or plastic, and they can be rimless. There is an almost unlimited variety of shapes, colors, and sizes. The type and degree of refractive correction in the lens determine to some extent the type of frame most suitable. Some lenses are too thick to fit in metal rims, and some large-correction prescriptions are best suited to frames with small-area lenses. Rimless frames are the least noticeable type, and they are lightweight because the nosepiece and temples are attached directly to the lenses, eliminating the weight of the rims. They tend to not be as sturdy as frames with rims, so they are not a good choice for people who frequently remove their glasses and put them on again. They are also not very suitable for lenses that correct a high degree of farsightedness, because such lenses are thin at the edges. Metal frames are less noticeable than plastic, and they are lightweight.
_
The patient should have the distance between the eyes (PD) measured, so that the optical centers of the lenses will be in front of the patient’s pupils. Bifocal heights also have to be measured with the chosen frame in place and adjusted on the patient. Again, this is so the lenses will be positioned correctly. If not positioned correctly, the patient may experience eyestrain or other problems. It’s also important to keep in mind that some frames just aren’t right for certain types of lenses. Progressive lenses, for example, often don’t work well in today’s smaller, stylish frames. And it’s best to choose a small, symmetrical frame that centers on your eyes if you have a high prescription. It is a very good idea to consider your lens selection first before buying frames.
_
The types of frames can be broadly classified into Metal and Plastic Frames.
_
Matching Eyeglass Frames to Face Shapes:
You should consider three main points when choosing an eyeglass frame for your face shape:
1. Eyewear should repeat your personal best feature (such as a blue frame to match blue eyes).
2. The frame shape should contrast with your face shape.
3. The frame size should be in scale with your face size.
_
The correct fit:
_
_
The size of your frames can affect the look of the glasses on your face and how comfortable they are to wear:
•The top edge of the frames should be no higher than the line of your eyebrows.
•The bridge design and position is the key to a comfortable fit.
•The lower edge of the frames should not sit on your cheeks, even when you smile, so that they don’t rub or irritate.
•The size should be in proportion to your face – if you have a small face, don’t choose large glasses.
•The width of the frames should not be wider than the overall width of your face at the temples.
_
Interpupillary Distance:
The distance between the patient’s pupils is called the interpupillary distance and is sometimes abbreviated PD (pupillary distance). The PD is measured with a millimeter rule. The resulting measurement is called the binocular PD. Depending on the size of your head and face, PD figures vary from anywhere from around 40 to 80 millimeters. The binocular PD is shown in the figure below:
Generally, adults have a PD within the range of 54-68 mm, while children have a PD within the range of 41-55 mm.
_
A more accurate method of measurement recommended today is corneal reflection. It involves measuring the distance from the pupil, using light reflected from the cornea, to the center of the nose where the center of the frame bridge rests. This measurement is called the monocular PD. If the monocular PD has been given on an order, then the laboratory will be given a value for each eye. The instrument used to measure the corneal reflection is called the corneal reflection pupillometer (also known as CRP).
_
Frame size:
_
_
To find a frame of your size, you must first know the measurements of the frame that you require. In order to do that, please refer to the figure above and measure it accordingly. If you wear glasses and have a pair handy already, first check the inner side of the temples (arms) of those glasses. Usually, there are some numbers listed on them.
For Example, it says: Brand Model 52/18 135 or 52 18-135, it refers to the following measurements.
a) 52 – Lens Width
b) 18 – Nose Bridge
c) 135 – Temple size
_
Though not shown on your glasses, an important measurement is the Frame Width. This is the horizontal distance between the centers of the two dowel screws that secure the sides. As a general rule this can be calculated by taking the lens diameter x 2, add the bridge width and add on 6mm to cover the hinge extensions for both end pieces.
_
Important Tips:
•Most important measurement is the Total Width.
•You may neglect height and width of lenses but make sure to find a frame with the accurate total width as required.
•The other measurements (Nose bridge & Temple size) should also be close to your requirements.
•Frame measurements are listed in mm (millimeters).
_
PD and frame size matching:
When considering frames, the idea is generally to have your pupils centered in the lenses. This isn’t always possible because frames come in size increments that may not correspond to your exact PD or you may simply want larger-sized frames, in which case your pupils will be more toward the inner edges of the lenses. To figure the distance between the lens centers on a particular frame, just add the lens width and the bridge width figures. So, a 50-22 frame would have lens centers 50 + 22 = 72 millimeters apart. If your PD is close to 72, then your pupils would be centered in the frames! Again, having your PD isn’t really necessary when ordering frames, but its one more measurement that can be handy in considering frame sizes. If the distance between the optical centers of both lenses is same as PD, it is best match. The whole point of getting a PD (papillary distance) measurement is to have the optical center of the lens centered in front of the eye. If it is decentered, that induces prism that is not prescribed and unnecessary and it will create double vision and focusing problems. Optician can also tailor match by making you wear frame with dummy lenses. Then mark center of your pupils on dummy lenses when you have focused on distant object. When real lenses are cut, it will be such that their optical center will be overlying pupils.
Glasses will need Adjustment:
Please don’t expect your glasses to fit perfectly without a little adjustment. Many opticians do small adjustments free of charge. Cable temples are flexible and with a little adjustment at home or by your optician, they form to fit your face properly and comfortably. For adjustments to plastic and aluminum frames, an optician warms up the frame and bends it a little to fit your head.
__________
Care and cleaning of eyeglasses:
Any lens material will scratch over time depending on what they’re exposed to and what accidents may occur. Dust and dirt particles will accumulate on your glasses over time. Facial oils and the environment around you apply a sticky layer of substance to the glasses that quickly attracts dust and dirt particles. The particles get trapped in various places on your glasses which include the groove between the frame and lens, around the nose pad area and generally any area that isn’t reached during normal cleaning. The best solution is proper preventive care of eye glasses, whether they are made of plastic or glass. Storing eye glasses in a sturdy, cushioned eyeglass case is the first step in prevention of scratches. This means the eye glasses should never be placed in a pocket or purse without a protective covering. Never use facial tissues or paper towels to clean lenses, as these products will scratch the lenses. Clean lenses every day with soapy water and dry with a soft, clean cloth, preferably one made for that purpose. Do not clean with soaps containing anti-bacterial products or hand creams. Know that some products including household cleaners, acetone (nail polish remover), perfume, and hairspray can harm lens coatings. Never wipe your lenses when they are dry otherwise your lenses will scratch. Never clean glasses dry, no matter what material you use. Liquids act as a lubricant, and help reduce friction, and the risk of scratching. Water works great, although there are spray cleaners you can buy from most optical places (usually made of water and mild detergent or a miniscule amount of alcohol).
_
The best way to clean your glasses is to run them under lukewarm water and put a tiny drop of dishwashing detergent on the tip of your fingers to create lather on the lens. Then rinse with warm water, and dry with a clean, soft cotton cloth. Once lenses are scraped up, there is no way to buff that scratch out. Attempting to clean glasses when dry only exacerbates the problem, since a wet surface is slicker than a dry one. Soap, warm water and a dry cloth are all you need, once a day, to keep glasses optimally clean and functional. Natural oils from your hands, eyelashes and face can lead to a lot of buildup each day, reducing lenses’ effectiveness. Leaving spectacles on a sink or vanity, where hair spray and perfume can fly through the air, adds to the residue. You wash glasses every morning, paying special attention to the frames and earpieces, where hair product and makeup tend to rub off. Whatever you do, don’t use the most handy form of water to clean your lenses. Some people use spit, but don’t. Though dirty glasses won’t cause an eye infection, saliva is not the best hygiene method, and it just won’t work very well. You probably even know that’s the wrong way to clean glasses, but you do it anyway. But you don’t need special sprays and microfiber cloth to clean glasses the right way. You only need kitchen soap and a normal cotton cloth. Soap, warm water and a dry cloth are all you need, once a day, to keep glasses optimally clean and functional.
_
Most people think buying scratch-resistant eye glasses means never having to deal with scratched lenses, but with improper care, all lenses will scratch, even those made of glass. When lens scratches begin to interfere with vision, people may ask their eye care professional how best to remove them. They are usually told the scratches cannot be removed and new lenses are necessary. Although this is especially true for glass lenses, plastic lens scratches can sometimes be repaired by some do-it-yourself remedies. The most popular remedy for plastic lens scratches is a glass-etching product called Armor Etch. Armor Etch removes the anti-glare and anti-scratch coatings on plastic lenses, leaving the original plastic lens intact. Because it is a glass-etching chemical, it does not affect plastic but must not be used on glass lenses. Other abrasive products like cleansers also remove the lens coatings without harming the original plastic lens beneath. Care must be taken to not change the thickness of the surface as it is cleaned and polished. Any product or procedure that changes the surface of an eyeglass lens can also change the refraction and effectiveness of that lens.
_
If you use tissues or your shirtsleeve to clean your eyeglass or sunglass lenses, you’re not doing your eyewear any favors. Those materials can scratch the lenses and generally don’t do a very good cleaning job anyway.
_
Peeps:
_
Peeps is a new device designed to clean meticulously and conveniently, with carbon technology and without using a spray.
First you use the retractable goat-hair brush to remove dust and abrasive particles from the lenses. This light brushing is meant to reduce the possibility of scratching the lens or its anti-reflective coating. Then you slide the arms out from the holder and clean with circular motions. To remove any smudges, you simply breathe on the surface and repeat. When you slide the arms back into the holder, the carbon on the cleaning tips is replenished.
_
A further point to note is that should your child have large eyelashes, please tell the consulting ophthalmologist of the same so that while prescribing glasses the consultant dispenses a pair of lenses which are ‘clear off eyelashes’. Usually a good manufacturer of spectacles would be also be able to make the suitable pair of glasses if that person is informed about the long eyelashes while ordering the item. If the eyelashes get constantly brushed against the glasses, there is increased watering of the eyes, the glasses get dirty, the wearer becomes irritated and the visual capability gets impaired enough to render the wearing of the spectacles useless.
_____
How to choose right spectacle and right lenses:
_
Thinning out Thick Eyeglasses:
There are many options available to reduce the appearance of thick eyeglass lenses. Thick lenses not only are cosmetically unappealing but they also add to the weight of the glasses, making the eyeglasses uncomfortable.
1. High Index Lenses:
Eyeglass lenses are able to correct vision because they refract, or bend, light as it passes through the lens. The amount of refraction that is needed to provide good vision is determined by your eyeglass prescription. The stronger your prescription, the thicker the lens required. Fortunately, there is a variety of plastic lens material that has been created to bend light more efficiently than conventional plastic lenses. This means less material is required to correct your vision. Less material means thinner and lighter lenses for you. There are many choices when it comes to high index lenses. Conventional plastic has an index of refraction of 1.50. The choices for high index lenses range from 1.53 to 1.74, the latter being the thinnest and lightest lens. Your eyeglass prescription determines what kind of material is the best choice for you. It is best to rely on the professional advice from your eye doctor and your optician as to which index is ideal for you.
2. Eye Glass Frame Choice:
Eyeglass frames come in all shapes and sizes. The “A” measurement is a measurement of the horizontal distance of each lens from temple to bridge. The “B” measurement is of the vertical distance of each lens from top to bottom. As the lens power increases, the curve and thickness is increased, specifically as you move toward the edge of the lens. By selecting a frame with reduced ‘A’ or ‘B’ or both measurements, lens edge thickness is reduced. It is also a good idea to get a frame made of thicker metal or plastic. The frame thickness can hide some of the lens edge. The resulting appearance is less edge apparent from the side view of the frame.
_
Points to note when choosing Eyeglasses Frames:
1. Severity of refractive errors: Students with severe refractive errors may choose plastic frames as they are thick enough to cover the edge of the thick lenses for a better look.
2. Width of the face: The size of the frames should match the size of the face and the head. The larger the frames, the bigger and heavier the lenses will be. However, smaller frames mean smaller peripheral vision.
3. Width of the head: The width of the frame should be similar to that of the head so that the arms will not press against the head nor too far from the head.
4. Distance between the eye and the ear: The length of the arm should match the distance between the eye and the ear. Arms that are either too long or too short are uncomfortable.
5. Height of the bridge: Students with flat nose should choose frames with nose pads because these can fix the position of the frame and prevent it from sliding down and being too close to the face, so that it is more comfortable.
6. Habit of removing the eyeglasses with one hand: Students who are accustomed to removing their eyeglasses with one hand should choose frames with spring hinges. These are not easily distorted and damage is usually milder.
7. Style of the eyeglasses: Students may refuse to wear eyeglasses if they don’t like the style. Thus, when choosing the eyeglasses, parents should discuss with their children and make sure they accept the need to wear glasses and agree with the style chosen.
_
Points to note when choosing Lenses:
1. Students should choose plastic lenses because glass lenses may break during accidents and cause eye injury.
2. Should get used to cleaning the lenses with appropriate lens cloth instead of tissues, shirts or other materials so as to avoid scratching the lens.
3. If the anti-reflective coating comes off, the lens will look worse than ordinary uncoated lens and the vision will be affected.
4. To address the weakness of being easily scratched, a scratch-resistant film can be coated to the surface of plastic lenses, though the effect is not ideal and the surface of the lenses are still not as hard as glass lenses.
5.I f the lenses are severely scratched, they should be replaced as soon as possible to avoid the vision being affected.
_
Choosing Eyeglass Lenses: By Prescription:
When selecting eyeglasses, your prescription plays an important role in determining which frames and lenses are the best choices.
If you are very nearsighted:
•Choose a frame with a small eye-size (the size of the openings in the frame for the lenses). A large eye-size will make your lenses thicker and heavier. A smaller eye-size will make them thinner and lighter.
•Choose a high index lens material. High index lenses are thinner and lighter than regular plastic or glass lenses.
•Get eyeglass lenses with an anti-reflective (AR) coating. Eliminating lens reflections will make your lenses look thinner, and provide better vision when driving at night.
_
If you are very farsighted:
•Choose a smaller frame. A frame with a smaller eye-size will reduce the thickness of your lenses and the overall weight of your eyewear.
•Choose an “aspheric” lens. An aspheric lens design will make your lenses flatter and reduce unwanted magnification that can give you that “bug-eye” look with regular lenses with a high prescription for farsightedness. Aspheric lenses also provide better peripheral vision if you are farsighted.
•Avoid rimless frame designs. Lenses for farsightedness sometimes have to be made thicker to fit in this type of frame.
_
If you have high astigmatism:
•Choose a smaller frame to reduce lens thickness and avoid peripheral lens distortions.
•Ask your optician about “atoric” lenses, which may provide better optics for clearer, more comfortable vision.
_
Allergy to eyeglass frames and lenses:
Although contact dermatitis from eyeglass frames is uncommon, occasionally it may be encountered. Various substances may cause allergic contact dermatitis, including metals, cosmetics, plastics, rubber, solvents, antioxidants, dyes, and waxes, some of which can be found in the average eyeglass frame. Recently, it has been determined that plasticizers, UV stabilizers and nickel are the most common allergens. One common allergy is a nickel allergy. This causes a rash in the area that comes in contact with the glasses. If you have an allergy to nickel you should try to purchase plastic frames or frames made of titanium. Titanium glasses are the best choice for people with allergies, but if it does not work for you then try the plastic glasses. Stainless steel glasses also work for people with a nickel allergy. Another common problem involves the nose pads. These are usually made out of silicone. The main indicator of a specific nose pad allergy would be that the rash is focused around your nose where the pads touch your face. These can be replaced with vinyl nose pads, and any eyeglasses shop can special order the correct pads for your glasses. Another option is to look for frames that do not use nose pads. However, if you have an allergy to the metal, this might not be the best option for you to consider. Some people may have reactions to the chemical coatings that are on the lenses of the glasses. A sign of this would be constant eye irritation, and no reaction on your ears or along your temples. If this is the case, you may consider ordering glasses without the additional coatings added to them. This would mean avoiding the scratch resistant and glare blocker coatings. You may also try to find someone that will make glasses for you from actual glass. Another option for dealing with allergies to eyeglasses is to consider using contact lenses for the majority of each day. Contacts will allow you to avoid using the frames at all. However, this is not a practical suggestion for everyone.
________
Self correction of refractive error among young people in rural China: results of cross sectional investigation: 2011 study:
Adjustable devices offer a novel approach to vision correction in areas with few resources. Some, such as the focometer, are capable only of measuring but not correcting refractive error. Adjustable spectacles not only allow the user to adjust the power of each lens independently to achieve optimal vision but can also be worn as a corrective device. This potentially allows refractive correction programs to occur entirely within the classroom and without the need for specialised professionals. Most published studies on adjustable spectacles have been carried out on adults and have suggested that good vision can be achieved. Though visual acuity was slightly worse with self refraction than automated or subjective refraction, acuity was excellent in nearly all these young people with inadequately corrected refractive error at baseline. Inaccurate power was less common with self refraction than automated refraction. Self refraction could decrease the requirement for scarce trained personnel, expensive devices, and cycloplegia in children’s vision programs in rural China.
______
Pinhole glasses:
_
Pinhole glasses are not made of glass at all but of an opaque substance such as metal or plastic. The user looks through any of the many small holes in the material. These holes have the effect of reducing the width of the bundle of diverging rays (called a “pencil of light”) coming from each point on the viewed object. Normally, the full opening of the pupil admits light. It is the improper bending of the outermost rays in that pencil of light which causes refractive errors such as myopia, hyperopia (farsightedness), presbyopia (diminished focusing range with age) and astigmatism to be noticeable. Pinholes can bring about clearer vision in all these conditions. By blocking these peripheral rays, and only letting into the eye those rays which pass through the central portion of the pupil, any refractive error in the lens or cornea is not noticed as much. The pupil may be wide open, but only the central portion is receiving light. The improvement in visual acuity can be striking.
_
Figure below shows an eye with a pinhole lens in front of it. You will see that the eye does not need to deal with the rays that would need the most bending since they are blocked by the lens. It is said that Scheiner first described this effect in 1573. Those who are familiar with cameras will recognize that this is the same principle used to increase the depth of focus by decreasing the aperture. Pinhole glasses also operate by this principle.
_
An easy way to demonstrate this is to make a fist and put it up to one eye while closing the other eye. Open the fist just enough to create a small hole to look through. If you have a refractive error, you should see clearer this way. This same improvement in the vision takes place when someone squints to see more clearly. The upper and lower eyelids cut off the rays that would normally enter the top and bottom of the pupil and the vision improves somewhat. Since there is no similar way to cut off rays entering the sides of the pupil, these rays still contribute to the blurred vision. Looking through pinhole glasses instead of squinting cuts off the peripheral rays from all sides. Since the glasses are so close to the eye, the material between the holes is greatly out of focus and is not as disturbing as one might think. After a period of getting used to the glasses, the brain tends to ignore the presence of the material. Also of interest is that the farther away the viewed object is, the less the pinholes are noticed. The honeycomb effect of the holes is more noticeable when viewing a book held close to the eyes, because the eyes are focused just a short distance in front of the glasses. When looking at a distant TV, however, the holes are hardly visible at all since the eyes are focused much farther away. Also, because of the distance, you can view the entire TV screen through one hole, an obvious benefit. The native people of Alaska have long used this principle by wearing glasses with narrow slits to look through, thus blocking out much of the glare from the sunshine reflecting off the snow and ice. Anyone who remains in this environment for long periods during the summer without protection can suffer from snow blindness. This painful condition forces the person to discontinue the use of the eyes until healing can take place.
_
Some advantages that pinholes have over prescription glasses:
As we get into our 40’s and 50’s and presbyopia (inability to focus close) develops, pinholes provide a simple and inexpensive solution for reading or other close work. Bifocals or trifocals are designed to provide a clear image only at fixed distances. Pinholes provide an improved image at ‘all’ distances. Multi-focal lenses provide a continuously variable curve that is supposed to give good vision at all distances. In reality, the distortion on either side of the center line is considerable and often too great for comfortable use. Pinholes eliminate this problem. There is no need to continually throw away old glasses and buy new, stronger ones. Unless the pinholes break, they can be used an entire lifetime. Some people find glasses unsuitable because the refractive error in each eye is not the same. Pinholes are ideal for such people because these glasses do not require a similar refractive error in each eye. There is a pincushion effect when looking through the edges of prescription glasses. That is, straight lines appear curved. This disturbing effect does not occur with pinholes. When you lay prescription glasses down improperly, they can easily get scratched at the center of the lens, the very area you have to look through. Scratching pinholes has no effect on their performance. Pinholes do not have to be cleaned of fingerprints and other marks that affect vision. Many people who have had corneal surgery find that their night vision has permanently deteriorated. Glare is a problem. They see halos and “starbursts” around lights. Even in normal home lighting they have problems so that they get in the habit of turning on as many lights as possible in order to get a small pupil and reduce the visual problems. Pinholes, either conventional or Snap-ons, can deliver the same small pupil without increasing the electric bill. Children with special needs often use only their peripheral vision, and pinhole glasses help them concentrate on detail better. It has been found that the pinhole glasses help improve acuity and central macular vision. One nationwide organization that deals in child development uses them on a regular basis for this purpose. Aniridia is the complete or partial absence of the iris; polycoria is having more than one pupil in a single iris; and albinism is the lack of normal pigmentation. All of these abnormalities may be aided with pinhole lenses. Many people with cataracts see better through pinholes. A cataract is one or more opacities in the lens that do not allow the light to pass through properly but instead cause it to scatter. By cutting off the peripheral rays, pinholes can reduce some of this scattering and improve the vision.
_
Myopia prevention:
When a person’s eye has become abnormally long due to excessive close work, the outermost rays come to a focus in front of the retina and cause the blurred vision. Imagine for a moment the common situation where a child begins to develop myopia and can’t see the board in school clearly. The usual solution of giving the child minus lenses is disastrous as for near vision accommodation will be stressed worsening myopia. But suppose the child has a pair of pinholes and puts them on just to look at the board. A large area of the board can be seen through just one hole. The cost and the risk involved with minus lenses has been avoided entirely. Suppose the child also leaves them on when reading or looking at a computer screen. This could help greatly in preventing myopia since the accommodative effort is reduced. For those children whose natural farsightedness has diminished to around +0.5 diopters and are on the verge of moving into myopia, sitting down at the school desk and putting on the pinholes should be almost simultaneous events. Many children might need nothing more than this to insure that they do not develop myopia. Schoolteachers should have several pairs on hand to lend to the students who have difficulty seeing the board.
_
Limitations of pinhole glasses:
One limitation of pinhole glasses is that blocking some of the light makes it more important than usual to have good lighting on the viewed object, even though the sharper image greatly compensates for the diminished light. When looking at television this is not a problem since the set makes its own light. When reading, a good lamp should be provided nearby. Another limitation is that peripheral vision is diminished, so they should not be used for driving or similar activities involving motion. As with any glasses, even sunglasses, they should not be used to stare at the sun, thinking that no harm can be done. Pinholes cannot replace prescription glasses in every situation. People with over 6 diopters of myopia will probably not find pinholes useful, because pinholes cannot eliminate all of the blur. And just as it would be risky to wear ordinary glasses in situations where they could be broken and damage the eyes, there are situations where using pinholes instead of prescription glasses is not advisable. Use common sense and only wear the pinholes when the limited view does not pose a risk. One group that should not use pinholes, or any glasses that reduce accommodation (focusing effort), is young people who are very farsighted. These people need to accommodate as much as possible in order to reduce their farsightedness to a lower level. This is nature’s dynamic method of refining visual acuity in the growing youngster and it should not be defeated. One possible drawback of the multiple pinhole array is that it will often be impossible for the two central sight lines of a person’s eyes to be perfectly aligned on a single object through two corresponding holes. This makes it impossible to have normal binocular vision with normal convergence and probably accounts for many of the experiences of strain and headache reported by a few users.
_______
3D glasses:
The illusion of three dimensions on a two dimensional surface can be created by providing each eye with different visual information. 3D glasses create the illusion of three dimensions by filtering a signal containing information for both eyes. The signal, often light reflected off a movie screen or emitted from an electronic display, is filtered so that each eye receives a slightly different image. The filters only work for the type of signal they were designed for. Anaglyph 3D glasses have a different colored filter for each eye, typically red and blue or red and green. A polarized 3D system on the other hand uses polarized filters. Polarized 3D glasses allow for color 3D, while the red-blue lenses produce an image with distorted coloration. An active shutter 3D system uses electronic shutters. Head-mounted displays can filter the signal electronically and then transmit light directly into the viewers eyes. Anaglyph and polarized glasses are distributed to audiences at 3D movies. Polarized and active shutter glasses are used with many home theaters. Head-mounted displays are used by a single person, but the input signal can be shared between multiple units.
_
Eyeglasses with adaptive focus:
_
_
The end is nigh for bifocals, and not a moment too soon. Optical scientists at the University of Arizona have developed new switchable, flat, liquid crystal diffractive eyeglass lenses that can adaptively change their focusing power. The new technology will open the way for a new generation of “smart” eyeglasses with built-in automatic focus. In the foreseeable future, with this technology, you won’t change prescription eyeglasses but will have your eyes tested and the optician will dial in a new prescription into the specs you already own. “Right now, in our prototype, you switch the lenses on or off to change focus,” said Nasser Peyghambarian, chair of photonics and lasers in UA’s College of Optical Sciences and professor of optical sciences, materials science and engineering. “But ultimately this will act just like your automatic camera: Eyeglass lenses will know where to focus just like your auto-focusing camera does.” The novel lenses focus electroactively. They are basically two pieces of flat glass spaced five microns apart. Five microns is an incredibly small space — roughly one-twentieth the diameter of a human hair. The space is filled with liquid crystal — the same kind of stuff in your laptop’s liquid crystal display. The flat glass is coated with an even thinner layer (one-tenth micron) of indium tin oxide, or ITO, which is a transparent electrode. Unlike electrodes made of aluminum or gold, ITO transmits most of the light that hits it. The transparent electrodes are patterned in a circular array over the area of the lens. The circular pattern is created through photolithography, an extremely precise technique that processes with light and chemicals. Applying less than two volts to the circuit changes the orientation of the liquid crystal molecules, and that changes the optical path length through the lens. It takes only about 1.8 volts to change the index of refraction so that light refocuses. The result is a flat piece of glass that acts like a lens. The scientists first tested the imaging properties of the lens on a model human eye, then built prototype eyeglasses that real humans tested. The clinical results agreed with the model eye test. Their tests showed that distance vision was no way impaired when the glasses were switched off and enabled close-up vision when switched on. These flat lenses are highly promising to replace conventional area division refractive, multi-focal spectacle lenses used by presbyopes. Estimates are that 93 percent of the world’s population over age 45 have the condition called “presbyopia,” where an aging person’s eye lens loses flexibility and therefore, its ability to shift focus from distant to near objects. Presbyopes will be some of the first to benefit from the UA research. Electroactively focusing eyeglasses will revolutionize the $50 billion worldwide vision care industry. Their major step in creating state-of-the-art liquid crystal diffractive lenses will have applications beyond vision care, the scientists predict. Tools with switchable lens elements would be valuable in dentistry, for example.
__________
__________
Contact lenses:
_
A contact lens, or simply contact, is a thin lens placed directly on the surface of the eye. Contact lenses are considered medical devices and can be worn to correct vision, or for cosmetic or therapeutic reasons. They are designed to rest on the cornea, the clear outer surface of the eye, and are held in place mainly by sticking on to the tear film that covers the front of the eye. As the eyelid blinks, it glides over the surface of the contact lens and causes it to move slightly. This movement allows the tears to provide enough lubrication to the cornea, as well as flush away any debris between the cornea and the contact lens. Most lenses are coming with a substantial UV blocking capability; this should never be considered, however, as a substitute for wearing sunglasses.
_
Not everyone is able to wear contact lenses for numerous reasons, which include:
•frequent eye infections;
•allergy eyes; and
•dry eye due to insufficient tear production.
You should also take into account your daily surroundings when considering contact lenses. For example, if you work in an environment that is dusty or where you are exposed to chemical fumes, you may be advised not to wear contact lenses. Also, if you work or live in an environment that is exceptionally dry due to heating or air conditioning, you may find wearing contact lenses uncomfortable.
_
In 2004, it was estimated that 125 million people (2%) use contact lenses worldwide, including 28 to 38 million in the United States. In 2010, worldwide contact lens market was estimated at $6.1 billion, while the U.S. soft lens market is estimated at $2.1 billion. Some have estimated that the global market will reach $11.7 billion by 2015. As of 2010, the average age of contact lens wearers globally was 31 years old and two thirds of wearers were female. People choose to wear contact lenses for many reasons. Aesthetics and cosmetics are often motivating factors for people who would like to avoid wearing glasses or would like to change the appearance of their eyes. Other people wear contacts for functional or optical reasons. When compared with spectacles, contact lenses typically provide better peripheral vision, and do not collect moisture such as rain, snow, condensation, or sweat. This makes them ideal for sports and other outdoor activities. Contact lens wearers can also wear sunglasses, goggles, or other eyewear of their choice without having to fit them with prescription lenses or worry about compatibility with glasses. Additionally, there are conditions such as keratoconus and aniseikonia that are typically corrected better by contacts than by glasses.
__
Eyeglasses are situated away from the eyes whereas contact lenses sit directly on the eyes. Unlike eyeglasses, contact lenses do not move around, and the distance between contact and eye remains a constant as well as the clarity of your sight. Eyeglasses also have a tendency to get dirty and scratched, which also impairs your vision. Along with the clarity and consistency of your vision, you will also notice how much more enhanced your peripheral vision is. Contact lenses cover your entire eye, and if your eyesight is pretty impaired, eyeglasses will limit your peripheral vision because they only correct your vision through the lenses; they don’t wrap around your whole face. This means that anything appearing in the periphery of your line of sight can be difficult to spot and even more difficult to recognize and focus on. On the other hand, contacts take time to get accustomed to; require more measurements for fitting; require many follow-up visits to the eye doctor; can lead to complications such as infections and corneal damage; and may not correct astigmatism as well as eyeglasses, especially if the astigmatism is severe. Probably one of the greatest benefits to wearing contact lenses is that there aren’t any weather conditions that can affect or limit your ability to function. Rain and cold weather can cause eyeglasses to fog up or distort vision with the moisture. With contact lenses, you don’t have to worry about your lenses fogging up or the moisture affecting your vision. When it’s time for sunglasses, all you have to worry about is finding a pair that accommodates you and your look. Having to buy and carry around a pair of prescription sunglasses to protect your eyes from the sun can be cumbersome and very frustrating. Contacts are in the eye and are basically the same protection against the elements as the eyes themselves. Some people prefer wearing contact lenses for the aesthetic appeal of not having something on their face. Many individuals have memories of being picked on as a child and called names such as “four-eyes.” Switching from glasses to contact lenses might enhance the self-esteem substantially, especially for children and older girls. Others would rather not advertise they need corrective lenses to help them see better. And then there are others who choose to wear contact lenses to discreetly change their eye color. Whatever the reason, the advancement in technology of the contact lens has grown incredibly. They are much safer and easier to wear.
_
Image size vis-à-vis contact lens and eyeglass:
Contact lenses are necessary when there is a substantial difference in the refraction of both eyes, because with glasses the difference of both images on the retina is too large to result in one combined image. A person who is switching from glasses to contact lenses experiences a magnification of the image on the retina. Table below compares the image size on the retina for people with glasses and for people with contact lenses. (Image size for contact lenses is rather similar to emmetropic people).
_
_
As the accuracy of vision is, among others, determined by the “granularity” of the retina for higher grades of myopia, a smaller image results in poorer vision. Additionally it was found that contact lenses improved the contrast sensitivity for high myopes (more than – 6.25D). Contact lenses have an additional advantage in being able to limit the increase in refractive errors. Since they are placed on the cornea and are essentially able to reshape the cornea so that the incoming rays of light are correctly focussed, they have been found to have some beneficial effect in the long run. An attractive alternative to spectacles for correcting refractive errors, contact lenses are also used for various therapeutic, pharmacological and cosmetic procedures. Modern contact lenses are polymers which are relatively safe, non-toxic and non-allergic. Since the cornea derives its oxygen supply mainly from the atmosphere, placing a lens on its surface can compromise its intake starving the cornea of oxygen. Newer lenses however, allow oxygen to pass through them to the cornea.
_
Advantages of a contact lens:
1. A contact lens provides a larger field of vision than spectacles and a better range of mobility. Hence it is ideally suited for sportspersons and people engaged in outdoor physical activities.
2. In people with high refractive error in one eye alone, spectacles will produce double vision due to the image size discrepancy. Contact lenses can be used for such people.
3. Cosmetically, they offer an advantage over spectacles.
4. Apart from correcting refractive errors, contact lenses are also used to deliver drugs to the eyes and to treat corneal diseases.
5. Nowadays contact lenses are also available in various colors and can be used by people even with normal vision for the cosmetic appeal.
6. Overcome peripheral distortions in spectacles specially if the power requirement is high
7. The only form of correction for irregular corneal surfaces (irregular astigmatism) and mild corneal scars
_
The Disadvantages of contact lenses:
1. Require more maintenance (or meticulous maintenance)
2. Chances of infection in the eye are more common if cleanliness is inadequate
3. Require better hand-eye co-ordination while wearing
4. Cannot be used without supervision by children and mentally handicapped
5. More chance of injury to the eye in case of an accident especially with hard and semisoft lenses
6. Cannot be “over-worn” (most lenses have a wearing time of 12-14 hours/day)
7. Uncomfortable to use in dusty, humid, or polluted environments, or in the presence of chemical fumes, etc.
8. Costlier than spectacles
____
Relative Contraindications of contact lens use:
The use of contact lenses to correct refractive errors may not be advisable when there is significant eyelid, tear film, or ocular surface abnormalities related to any of the following:
◦Keratoconjunctivitis sicca
◦Blepharoconjunctivitis
◦Acne rosacea
◦Conjunctival cicatrization
◦Corneal exposure
◦Neurotrophic keratitis
◦Other corneal abnormalities
Other relative contraindications include the following:
◦Use of topical corticosteroids
◦Inflammation of the anterior segment
◦Presence of a filtering bleb
◦Poor hygiene
◦Certain environmental or work settings e.g., dust, volatile chemicals
◦History of corneal complications related to contact lens
◦Limited dexterity
◦Inability to understand the risks and responsibilities involved
______
Specific Weight and Refractive Index:
These two parameters are sometimes expected to be important – mainly for contact lenses of higher grades of Diopter because of a higher volume of the optical part: A heavier lens (i.e. of higher specific weight and lower refractive index) might have more a tendency to move downward, i.e. centration is more likely to become a problem. Detailed analysis and experiments, however, have shown that “the lens mass is not a significant predictor of lens dynamics.” More important is the center of gravity of the lens. Carney et al. stated that “… lenses with a center of gravity location further behind the lens vertex show better stability.” The center of gravity is shifted into this direction by an increasing diameter, decreasing lens thickness (and increasing negative power and increasing lens curvature, but these two are determined already for other reasons). Anyway, a lower weight of the lens can be achieved by manufacturing it from a material with lower specific weight, with minimal center thickness (depending on the specific material), or by a specific lens cut called lenticulation.
_
The geometrical parameters are:
Diameter of the Lens (DIA):
Typical diameters of hard RGP lenses are between 9.00 mm and 10.50 mm; the selected size depends e.g. on the diameter of the iris, and the position of the upper eyelid, i.e. whether the upper edge of the lens should stay covered by the lid (“lid attachment”) or not (“interpalpebral”). It was noted, “High powers require larger diameters for lens stability because the heavier lens may sink down if it is not caught by the eyelid.” Generally, lens diameters above 9.5 mm were found to be more comfortable. Typical diameters of soft lenses are between 13 mm and 15 mm. Astonishingly, a report found that oxygen uptake increased with increasing diameter of hard lenses (and their typical diameter). A large diameter of a hard lens may create, however, problems for fitting, if no aspheric design is used.
_
Base Curve Radius (BC/BCR, or Back Optic Zone Radius BOZR):
This very important number determines the fit of the lens on the cornea, and it is for hard RGP lenses between 6.50 mm and 9.00 mm; this radius is available with a granularity of 0.1 mm or better of 0.05 mm. A lens manufacturer, which delivers 0.05 mm granularity, should be preferred, because this allows a more accurate fitting of the lens – especially if the selected lens material is rather rigid. For soft lenses, the exact fit to the cornea is by far less important, because due to their flexibility they can adjust to the radius of the cornea. Very often soft lenses are coming with one radius of about 8.6 mm only; sometimes there is a choice between numbers like 8.4 mm, 8.7 mm, and 9.00 mm. Sometimes the curvature of the cornea is not described by its radius in mm, but by its corresponding Diopter number.
The formula for conversion is:
D = 337.5/R
where D is the Base Curve Radius in Diopter, and R is the Base Curve Radius in mm.
Because of the lens built by the tear-liquid between cornea and contact lens, a transition to a flatter lens than the previous lens results in a lens with less Diopter (weaker power), whereas a transition to a steeper lens results in a lens with stronger power.
0.05 mm change in BCR corresponds to about 0.25 Diopter.
_
Center Thickness:
The thickness of the lenses in the center is between about 0.08 mm and 0.15 mm for hard lenses and between about 0.04 mm and 0.15 for soft lenses. The thickness of the lens has not only an impact on the oxygen transmission, but also on the flexibility of the lens: To avoid in certain cases a warping of the hard lens, a lens with increased thickness is provided.
_
Back Optic Zone Diameter (BOZD or OZ):
The back optic zone is the area, which has the “right” optic without any disturbing optical effect of the aspheric design, or a secondary curve. This diameter should be not too small for good vision.
_
The thesis to avoid any avoidable accommodative load for the eye leads to these trade off recommendations for contact lens wearers:
• Have fully correcting contact lenses but wear additional plus glasses for extensive near work, or
• Have under-correcting contact lenses but wear additional minus glasses for perfect vision for far (e.g. for driving).
• Be aware that the power of contact lenses is lower than that of the respective glasses.
_
Presbyopia and contact lens:
For presbyopia, the contact lenses are required to replace the accommodation of the human lens, i.e. to offer focus as well for near objects as well as for distant objects, as with bifocal glasses. Wearers of glasses accommodate less and have lower convergence demands than emmetropes or wearers of contact lenses, i.e. myopic people wearing contact lenses should be affected by presbyopia more early than myopic people, which are wearing glasses. There are some different concepts to handle presbyopia with contact lenses. Generally, there are two groups of systems, i.e. for alternating vision, where an image is produced either for distant view or near view, and simultaneous vision, where the evaluation of the different images is done in the brain. In any case, it will take a while until the patient is used to the new vision.
_
Specific contact lenses for presbyopia:
1. The optical zone of the lens is split into an upper section for distant focusing and a lower section for near focusing (alternating vision). A problem is that the lens has to be kept in the right rotational and vertical position. The lens is difficult to fit, and is normally fitted flat.
2. The optical zone of the lens is split into a center section for distant focusing and a peripheral section for near focusing (simultaneous vision). This lens is fitted more on the steeper side to have the lens properly centered. When the aperture of the iris is small, e.g. at bright light, near focusing may be a problem. As with all methods which are using simultaneous vision, the contrast of the images is reduced.
Notes:
– The steep fitting, which is necessary to keep the movement of the lens at a minimum, might create a problem particularly for older people whose amount of tear liquid is frequently reduced.
– As with older age the ability to see in the dark and the contrast sensitivity fades generally, every optical device which increases these handicaps is problematic, especially when this device is worn permanently, i.e. when there is no way to improve the vision when needed, like for driving at night.
3. Into the optical zone of the lens fine microscopic steps are inserted. These steps create via diffraction two focus points – one for distant vision and one for near vision (simultaneous vision). An exactly centered position, and the aperture of the iris is not as important as in the method described on top. The reduction of the contrast, however, is similar.
In general, the visual performance of rigid gas permeable contact lenses was better than the performance of soft contact lenses.
4. Other methods to cope with presbyopia are:
Monovision:
The lens of one eye is adjusted for distant vision; the lens of the other eye is adjusted for near vision. This method is less expensive, and easier to fit than the previous methods. Good success rates have been reported for this method. For driving (especially night driving) the use of additional glasses, which compensate for the undercorrection of one eye, is recommended. Especially for reading additions that were not greater than 2.50 D the visual results were reported to be quite satisfying.
__________
Types of contact lenses:
Contact lenses can be classified in many different ways. Contact lenses can be separated by their primary function, material, wear schedule (how long a lens can be worn before removing it), and replacement schedule (how long before a lens needs to be discarded).
_
Functions:
1. Corrective contact lenses:
Corrective contact lenses are designed to improve vision, most commonly by correcting refractive error. This is done by directly focusing the light so that it enters the eye with the proper power for clear vision. Recently, there has been renewed interest in orthokeratology, the correction of myopia by deliberate overnight flattening of the corneal epithelium, leaving the eye without a refractive error during the day. A spherical contact lens bends light evenly in every direction (horizontally, vertically, etc.). They are typically used to correct myopia and hyperoipa. A toric contact lens has a different focusing power horizontally than it does vertically, and as a result can correct for astigmatism. Some spherical rigid lenses can also correct for astigmatism. Because a toric lens must have the proper orientation to correct for a person’s astigmatism, a toric contact lens must have additional design characteristics to prevent the lens from rotating away from the ideal alignment. This can be done by weighting the bottom of the lens or by using other physical characteristics to rotate the lens back into position. Some toric contact lenses have marks or etchings that can assist the eye doctor in fitting the lens. The first disposable toric lenses were introduced in 2000 by Vistakon. The correction of presbyopia discussed vide supra.
_
For those with certain color deficiencies, a red-tinted “X-Chrom” contact lens may be used. Although the lens does not restore normal color vision, it allows some colorblind individuals to distinguish colors better. Red-filtering contact lenses can also be an option for the extreme light sensitivity in some visual deficiencies such as achromatopsia. ChromaGen lenses have been used and these have been shown to have some limitations with vision at night although otherwise producing significant improvements in color vision. Magnification is another area being researched for future contact lens applications. The embedding of telescopic lenses and electronic components suggests that future uses of contact lenses may become extremely diverse. However, there are still barriers that prevent the transition of these technologies from research and development to practical application and commercial availability.
_
2. Cosmetic contact lenses:
A cosmetic contact lens is designed to change the appearance of the eye. These lenses may also correct refractive error. Although many brands of contact lenses are lightly tinted to make them easier to handle, cosmetic lenses worn to change the color of the eye are far less common, accounting for only 3% of contact lens fits in 2004. All individuals who would like to wear cosmetic lenses should have a contact lens examination with an eye doctor prior to first use, and if used long-term, regular aftercare examinations, in order to avoid potentially blinding complications. Cosmetic lenses can be used to drastically alter the appearance of the eye, as seen in the entertainment industry. Scleral lenses that cover the white part of the eye (i.e., sclera) are used in many theatrical applications. These lenses are typically custom made for a specific production and as a result have very limited availability to the general public. As with any cosmetic lens, if the design changes the clarity of the center of the lens, the lens may interfere with vision. A new trend in Japan, South Korea and China is the circle contact lens. Circle lenses extend the appearance of the iris onto the sclera by having a dark tinted area surrounding the iris. The result is the appearance of a bigger, wider iris, a look reminiscent of dolls’ eyes. Cosmetic lenses can have more direct medical applications. For example, some lenses can restore the appearance and, to some extent the function, of a damaged or missing iris.
__
3.Therapeutic contact lenses:
Therapeutic contact lenses are also available in the market and have healing properties. These lenses can help an injured or diseased cornea to recover slowly. They are also used to correct disorders like bullous keratopathy, dry eyes, corneal ulcers and erosion, keratitis, corneal edema, descemetocele, corneal ectasis, Mooren’s ulcer, anterior corneal dystrophy, and neurotrophic keratoconjunctivitis.
_
Types of contact lens by material used:
There are basically three types of contact lenses:
1. Soft contact lens:
These are well flexible lenses made of a polymer called HEMA (Hydroxy Ethyl Metha Acrylate). They are very comfortable to wear and permit oxygen to reach the cornea.
_
2. Semi soft lenses or Rigid Gas Permeable Lenses (RGP/GP):
These lenses are made from special materials like Cellulose or Silicon acrylate. They are less flexible than soft contact lenses but allow some oxygen to pass through the cornea. Though less comfortable than soft lenses, they can be used to correct steep corneas and high astigmatism.
_
_
_
3. Hard contact lenses:
Made of a polymer called PMMA (Poly Methyl Metha Acrylate), hard lenses are least flexible and permit almost no oxygen to pass through to the cornea. The advantage of a hard contact lens is its durability.
_
Contact lenses rest on a thin layer of tearfilm on the front surface of the eye (the cornea). Various derivatives of Acrylic material are used in the manufacture of contact lenses. The most commonly used contact lenses now a days are the soft lenses, though semisoft (gas permeable lenses) are indicated occasionally. Both soft lenses and semisoft lenses are gas permeable, that is, they allow the cornea to “breathe” through the lenses, making them more comfortable to wear.
_
Comparison of RGP lens vs. soft lens:
| RGP Contacts | Soft Lenses | |
| Oxygen Delivery | GP contacts are made of special materials that allow your eyes to breathe. Oxygen is absolutely necessary to the health of your eyes. | Some soft contact lenses just don’t allow enough oxygen to get through to your eyes. This can lead to corneal problems. |
| Visual Acuity | GP contacts have superior optics. Since they’re firm, they retain their shape better when you blink, so your eyes don’t have to refocus as much. And they are superb for astigmatism or bifocal needs. | When you blink, soft lenses are more likely to distort; your eyes must then refocus, which can be annoying if you’re reading, or detrimental to your performance if you’re driving or participating in sports. |
| Initial Comfort | GP contact lenses require a short adaptation period. | Soft lenses are comfortable from just about the moment you put them on. |
| Long-Term Comfort | GP contacts require almost no water to maintain their shape, so they won’t pull the moisture away from your eyes. | After a few hours of wear, water-absorbing soft lenses can dry out your eyes, making them itchy and tired. |
| Durability | GP contacts are made of a firm plastic, so they don’t scratch or tear. And they stay clear over time. | Made of a gel-like plastic, soft lenses are easy to tear. And protein deposit buildup clouds the lenses over time. |
| Deposit Resistance | Their smooth finish and lack of water retention mean they harbor fewer protein deposits from your tear film. This is healthier and more comfortable for your eyes. | Since soft lenses absorb more of your tears, they are more likely to contain protein deposits from your tears and harbor bacteria. More deposits are scratchy, too. |
| Value | GP contacts are much less expensive to maintain; also, they last longer so you don’t have to spend as much on replacements. | Soft lenses require significant spending on cleaning supplies; and they don’t last as long, so you buy new lenses more often. |
As you can see, initial comfort is the only area where soft lenses excel over GP contacts. But once you get used to them, GP contacts are comfortable, more durable, easier and less expensive to care for, healthier, and provide crisper vision.
_
Wear schedule:
A “daily wear” (DW) contact lens is designed to be worn for one day and removed prior to sleeping. An “extended wear” (EW) contact lens is designed for continuous overnight wear, typically for up to 6 consecutive nights. Newer materials, such as silicone hydrogels, allow for even longer wear periods of up to 30 consecutive nights; these longer-wear lenses are often referred to as “continuous wear” (CW). Extended and continuous wear contact lenses can be worn overnight because of their high oxygen permeability. While awake, the eyes are typically open, allowing oxygen from the air to dissolve into the tears and pass through the lens to the cornea. While asleep, oxygen is supplied from the blood vessels in the back of the eyelid. A lens that interferes with the passage of oxygen to the cornea can cause corneal hypoxia which can result in many complications, including a corneal ulcer, which has the potential to permanently decrease vision. Extended and continuous wear contact lenses typically allow for the transfer of 5–6 times more oxygen than conventional soft lenses, allowing the eye to remain healthy, even when the eyelid is closed. Wearing lenses designed for daily wear overnight has an increased risk for corneal infections, corneal ulcers, and corneal neovascularization. The most common complication of extended wear lenses is giant papillary conjunctivitis (GPC), sometimes associated with a poorly fitting contact lens.
_
Replacement schedule:
The contact lenses are often categorized by their replacement schedule. Single use lenses (typically called 1-day or daily disposable) are discarded after one use. Because they do not have to stand up to the wear and tear of repeated uses, single use lenses can be made thinner and lighter. This can improve the comfort of the lens. Lenses replaced frequently gather fewer deposits of allergens and germs, making these lenses preferable for patients that have ocular allergies or are prone to infection. Single-use lenses are also useful for people who wear contacts infrequently, or when losing a lens is likely or not easily replaced (such as when on vacation). They are also considered useful for children, because no cleaning or disinfecting are needed, leading to improved compliance. Other disposable contact lenses are designed for two-week or 4-week replacement. Quarterly or annual lenses, which used to be very common, have been discontinued by manufacturers. Rigid gas permeable lenses are very durable and may last for several years without the need for replacement. PMMA hard lenses were very durable, and were commonly worn for 5 to 10 years, but had other drawbacks. Lenses with different replacement schedules can be made of the same material. Although the materials are the same, differences in the manufacturing processes determines if the resulting lens will be a “daily disposable” lens or a lens recommended for two-week or 4-week replacement.
_
Wear and care of contact lens:
There are some things you should keep in mind before deciding on contact lenses. Contact lenses – with the exception of daily disposable lenses – require regular cleaning and disinfection. Although this process only takes a few minutes, a lot of people do not bother doing it. The most common eye problems encountered by contact lens users are excess tearing, itching, burning, sensitivity to light, dryness and occasional blurred or distorted vision. These conditions may be worsened by improper care or cleaning of contact lenses and increase the risk of developing an eye infection. Clinical studies suggest that the extended use of contact lenses, particularly overnight, seriously increases the risk of developing corneal ulcers, also known as ulcerative keratitis. An ulcer can scar the cornea in a day or two, leading to permanent scarring or even blindness. Many eye doctors advise their patients not to use extended-wear contact lenses for this reason. Some problems caused by contact lens wear use do not produce symptoms, but may still harm the eye. For this reason regular examinations by an eye doctor are recommended.
_
The Basics of Soft Contact Lens Care: Clean, Rinse and Disinfect:
1. Wash your hands so that you don’t transfer dirt and germs to your eye. Try to avoid moisturizing soaps, as they are not good for contact lenses. Dry your hands with a lint-free towel.
2. Remove one lens and clean it with the recommended solution. Cleaning removes eye-produced buildup, cosmetics and other debris that impairs lens comfort. The FDA recommends that you rub the lens in the palm of your hand with a few drops of solution, even if you are using a “no-rub” product.
3. Rinse the lens again to remove the loosened debris, making sure to take as long as the package directs: Rinsing is an important step.
4. Place the lens in your clean lens case or lens holder and fill with fresh solution; don’t “top off” your old solution. Disinfecting kills microorganisms on the lens. Disinfection time varies from product to product; check the package for details.
5. Repeat steps two through four for your other lens.
_
While cleaning them does remove some protein, it can still build up on your lenses and make them uncomfortable. That’s why the longer you wear lenses before replacing them, the more likely you are to need a protein remover. For example, if you wear disposables, you probably won’t need one; but if you wear the kind of lenses that are replaced only once or twice a year, you definitely will. Products for removing protein include enzymatic cleaner and daily protein removal liquids.
Eye dryness and irritation:
Use contact lens eye drops to lubricate your eyes and rewet your lenses.
Eye sensitivity and allergies:
A small percentage of lens wearers develop an eye allergy to the chemicals present in contact lens solutions. If this is the case with you, you don’t need an additional product: You just need to switch products to those marked “preservative-free.”
_
Cleaning, Rinsing and Disinfecting Solutions:
Saline solution is for rinsing and storing contact lenses, when you’re using a heat or UV disinfection system. You also may need it for use with enzymatic cleaning tablets or cleaning/disinfecting devices. Never use saline products for cleaning and disinfection. Daily cleaner is for cleaning your contact lenses. You place a few drops in the palm of your hand and carefully rub the lens for as long as directed, usually around 20 seconds, making sure to clean both sides. Use other products for rinsing and disinfection. Multipurpose solution is for cleaning, rinsing, disinfecting and storing your contact lenses. Clean your lenses as you would with daily cleaner, then rinse (as long as directed) and disinfect, all with the same solution; or rinse the lenses twice, then place them in the clean lens case with solution to clean and disinfect. When you are ready to wear the lenses, rinse them again. With multipurpose solutions, no other lens care products are necessary.
_
Hydrogen peroxide solution is for cleaning, disinfecting, rinsing and storing your contact lenses. With this product, you place your lenses in the provided basket and rinse them, then place the basket in its cup and fill the cup with solution to clean and disinfect your lenses. Some lens holders for hydrogen peroxide systems have a built-in neutralizer (to convert the hydrogen peroxide to water, so it doesn’t sting your eyes), but with others you need to add a neutralizing tablet. After the disinfection and neutralizing step is completed, you can remove the lenses from the case and put them on. Never rinse your contacts with hydrogen peroxide solution and apply them directly to your eyes without completing the entire disinfecting and neutralizing step. Doing so can cause a painful chemical injury to the eye. Cleaning/disinfecting devices will, as you would expect, both clean and disinfect your contact lenses. Depending on how the brand is designed, cleaning is accomplished with either ultrasonic waves or subsonic agitation, whereas disinfection occurs via multipurpose solution or ultraviolet light.
_
Contact Lens Care Must-Knows:
Regardless of which care regimen or brands you use, remember:
• Never touch solution bottle tips to any surface, including your body: this can cause contamination of the solution.
• Avoid getting tap water on your contact lenses and accessories, as it can carry a microorganism called Acanthamoeba that causes serious eye infections.
• Remember to clean your contact lens accessories (lens case, cleaning/disinfecting devices, enzymatic cleaner vials and so on) as directed.
• Lens cases should be rinsed with hot tap water and dried when not in use. (Because Acanthamoeba cysts may be present in tap water and can survive for years after drying, some eye doctors recommend using only contact lens disinfecting or multipurpose solution for this step.)
• Recent studies suggest that wiping your case with a clean tissue and/or placing it upside-down on another clean tissue may be additional good steps in keeping bacteria biofilms off the case.
• Throw out your contact lens case once a month, or as directed, to reduce your risk of infection.
Most importantly, clean and disinfect your contact lenses once a day. If you wear extended wear contacts, clean and disinfect the lenses as soon as you remove them, unless they are designed to be discarded immediately after use. Not only will your eyes be safer and healthier, but your contact lenses will be more comfortable to wear, too.
_
How to put on contacts:
1. Wash your hands.
You want to ensure you don’t accidentally carry any dust, germs, or makeup to your contact lens as that could irritate your eyes. Also, use plain soap without any heavy moisturizers or perfumes. Rinse well and dry your hands. Again, this is to prevent transmitting anything unwanted to your eyes.
2. Start with the same eye every time.
Your contact lenses specifically fit each eye, left or right. Like your shoes, you can’t mix the two interchangeably. Since your contacts will look identical out of the box, starting with your right eye if you’re right handed, or your left eye if you’re left handed, and doing this every time you insert your contacts will help you keep which is which straight in your mind. This is the easy way to put contacts in for the first time, which is what we want.
3. Scoop out the lens carefully.
Place the lens on your index finger. Look at it. Is it curved upward, like a bowl? If so, great! You’re almost there. Just clean it with contact lens solution and you’re ready to put in the contacts and get on with your day. Remember, before inserting your contact lens into your eye, use a contact cleansing solution to cleanse thoroughly.
4. Hold your eyelid and insert your contact lens.
Just use your free hand to hold up your eyelid and insert the lens. Many choose to look away as the contact lens goes onto the eye. You can do this, or you’re free to look straight at the lens, too. Either way is fine.
5. Blink!
That’s right. Blink naturally and maybe take a look in the mirror. If everything feels and looks fine, you’re done.
6. After inserting your contacts into your eyes, empty your contact case and rinse thoroughly with warm water, and allow it to air dry.
_
Aftercare:
Contact lens wearers must be examined periodically by their eye doctors to make sure that the lenses fit properly and that there is no infection. Infection and lenses that do not fit properly can damage the cornea. Patients can be allergic to certain solutions that are used to clean or lubricate the lenses. For that reason, patients should not randomly switch products without speaking with their doctor. Contact lens wearers should seek immediate attention if they experience eye pain, a burning sensation, red eyes, intolerable sensitivity to light, cloudy vision, or an inability to keep the eyes open. To avoid infection, it is important for contact lens wearers to exactly follow their instructions for lens insertion and removal, as well as cleaning. Soft contact lens wearers should never use tap water to rinse their lenses or to make up solutions. All contact lens wearers should also always have a pair of glasses and a carrying case for their contacts with them, in case the contacts have to be removed due to eye irritation.
_
Patient education:
When contact lenses are initially prescribed and dispensed, patients should be trained and supervised in contact lens insertion and removal. Contact lens cleaning and disinfection should be carefully explained, because improper care may be associated with complications of contact lens wear. Patients should be instructed that rubbing is an important part of the cleaning step before disinfection for any lens that is to be reworn. Hydrogen peroxide systems may be superior to preserved disinfecting solutions in reducing pathogen binding and cysticidal disinfection, but they require more complex care regimens. Patients should be instructed to use only sterile products that are commercially prepared specifically for contact lens care and to replace these at the intervals recommended by the manufacturers. Specifically, patients should be instructed not to rinse contact lenses or lens cases with nonsterile water (e.g., tap water, bottled water). Patients should also be instructed to clean and replace contact lens cases frequently, because they can be a source of lens contamination. Patients should be instructed to replace the solution in contact lens cases each time the lenses are disinfected (i.e., the old solution should not be topped off). Patients should be made aware that using contact lenses can be associated with the development of ocular problems, including corneal infections that may threaten vision, and that overnight wear of contact lenses is associated with an increased risk of these corneal infections. This increased risk of corneal infections with overnight contact lens wear should be discussed with patients who are considering this modality of vision correction. If patients choose overnight wear, they should be instructed to use only lenses specifically approved for extended wear. Swimming with contact lenses has been associated with the development of Acanthamoeba keratitis, and showering with lenses seems to be part of a pattern of risk. Patients should be instructed to minimize water contact when wearing contact lenses and informed of the risks of wearing contact lenses while swimming, in a hot tub, or showering.
___________
Complication and long term effects of contact lens:
Wearing contact lenses increases the risk of corneal damage and eye infections. Contact lenses are generally safe as long as they are used correctly. Complications due to contact lens wear affect roughly 5% of contact lens wearers each year. Improper use of contact lenses may affect the eyelid, the conjunctiva, and the various layers of the cornea. Poor lens care can lead to infections by various microorganisms including bacteria, fungi, and Acanthamoeba. Many complications arise when lenses are worn not as prescribed (improper wear schedule or lens replacement). Sleeping in lenses not designed or approved for extended wear is a common cause of complications. Many people go too long before replacing their lenses, wearing lenses designed for 1, 14, or 30 days of wear for multiple months or years. While this does save on the cost of lenses, it risks permanent damage to the eye and loss of sight. Mishandling of contact lenses can also cause problems. Corneal abrasions can increase the chances of infection. When combined with improper cleaning and disinfection of the lens, the risk of infection further increases. Decreased corneal sensitivity following extended contact lens wear may cause a patient to miss some of the earliest symptoms of such complications. The way contact lenses interact with the natural tear layer is a major factor in determining lens comfort and visual clarity. People that suffer from dry eyes are particularly vulnerable to discomfort and episodes of brief blurry vision. Proper lens selection can minimize these effects for some patients. Long-term wear (over 5 years) of contact lenses may decrease the entire corneal thickness and increase the corneal curvature and surface irregularity.
_
It was estimated that the probability for microbial keratitis (disease of the cornea) is about 3-fold for daily-wear soft lenses, and about 20 fold for extended wear soft lenses, compared with daily-wear hard RGP lenses. Other authors claim that this rate is mainly a matter of proper fitting and maintenance. The time for recovery was reported to be substantially shorter for incidents with hard RGP lenses than for soft lenses. Additionally, it was reported that the corneas of RGP wearers contained less bacteria. Therefore, it was reported that most of the people could not wear their soft lenses any more after 15 years. Those who wear the lenses overnight have a risk of eye infection 10 to 15 times that of users who insert and remove the lenses daily. Lenses for continuous wear – like for 30 nights and days – with very high oxygen transmissibility are available as RGP lenses and as soft lenses. As with normal lenses, it was found that RGP lenses for continuous wear showed fewer adverse events, especially fewer bacterial infections. People, who use lenses for continuous wear should do so under the strict control of an experienced practitioner, who follows established guidelines. A survey among members of the Contact Lens Section of the American Academy of Optometry showed that among these professionals RGP lenses were rated superior to soft lenses in most respects, especially quality of vision, eye health, ease of care/handling, and deposit resistance. Therefore the tradeoff appears to be to choose between a
• More healthy, but maybe a little bit less comfortable lens – the hard RGP lens, and a
• More comfortable, but maybe somewhat less healthy lens – the soft lens.
The new lenses made of silicon hydrogel can eliminate the disadvantages of the low oxygen transmissibility of the traditional soft lenses. Problems with microbial infections can still exist in a few cases, however, especially with extended wear. The fitting process of these silicon hydrogel lenses appears to be more demanding than the fitting of conventional soft lenses.
__
Oxygen transmission:
One of the major factors that causes contact lens complications is that the lens is a barrier to oxygen. The cornea needs a supply of oxygen to function and it normally gets that oxygen from the surrounding air while awake and from the blood vessels in the back of the eyelid while asleep. The most prominent risks associated with long-term, chronic low oxygen to the cornea include corneal neovascularization, increased epithelial permeability, bacterial adherence, microcysts, corneal edema, endothelial polymegethism and potential increase in myopia. That is why much of the research into the latest soft and rigid contact lens materials has centered around improving oxygen transmission through the lens. Limited oxygen supply for the cornea (hypoxia) is a central problem for all contact lenses. The swelling of the cornea occurs at night even without any lens, because of the coverage by the lid. Clearly, these tiny damages are making the cornea more vulnerable to bacterial and fungal infections. Due to this hypoxia at night it is recommended, to wait in the morning some 15 minutes before putting the lenses in to the eye to allow the cornea to recover from the lack of oxygen.
_
Effects of long-term contact lens wear on the cornea:
Long-term contact lens use can lead to alterations in corneal thickness, stromal thickness, curvature, corneal sensitivity, cell density, and epithelial oxygen uptake, etc. Other changes may include the formation of epithelial vacuoles and microcysts (containing cellular debris) as well as the emergence of polymegethism in the corneal endothelium. Decreased corneal sensitivity, vision loss, and photophobia have also been observed in patients who have worn contact lens for an extended period of time. Many contact lens-induced changes in corneal structure are reversible if contact lenses are removed for an extended period of time. Increases in corneal curvature are thought to be caused by corneal thinning-induced ectasia. Two explanations have been proposed for contact lens-induced stromal thinning. It is thought that contact lens-induced edema may inhibit stroma tissue synthesis. Alternatively, contact lens-induced hypoxia may trigger a lactic acid buildup that leads to the erosion of stromal tissue. The mechanism behind contact lens-induced polymegethism is unknown, though it is also thought to be a byproduct of corneal edema and epithelial hypoxia. It is thought that constant adhesion of contact lenses to the cornea may lead to adaptation to mechanical stimuli, thus decreasing corneal sensitivity to tactile stimuli. A proposed explanation for the reduced sensitivity is the induced quiescence of free nerve endings following long term corneal exposure to contact lenses.
_______
The Spectrum of Soft Lens induced changes in Refractive Error:
Increases in myopia or ‘myopic shifts’ during both daily and extended wear with traditional soft lenses have been reported since the 1970’s. Some of these myopic shifts are less than -0.50 diopters and are usually considered too small to be of much clinical relevance. However significant increases in myopia up to and over 1 D have also been observed. Soon after the release of silicone hydrogel lenses, there were several anecdotal reports of large hyperopic shifts in silicone hydrogel lens wearers. These unexpected results stimulated researchers to characterise the spectrum of changes in refractive error with soft lens wear, and to better understand why such changes occur. Generally the myopic shift associated with traditional soft lens wear is attributed to lens-induced hypoxia. It is well established that traditional hydrogel lens materials fail to deliver oxygen to the cornea at levels sufficient to avoid hypoxic consequences, particularly during overnight wear. The corneal oedema that results from low Dk soft lens wear is thought to modify corneal shape and induce changes in corneal curvature and refractive index that bring about the increase in total refractive power of the eye. Another possible cause for the changes in refractive error seen with silicone hydrogels may be related to pressure-induced changes in corneal shape. The central cornea is flattened by the relatively stiff silicone hydrogel materials leading to an ‘orthokeratology’-like effect. This hypothesis is supported by the fact that central corneal flattening is typically observed during silicone hydrogel wear. It also follows that these effects would be more pronounced in prolate corneas and/or with increasing lens central thickness which occurs with high hyperopic corrections. Given that the amount of refractive change measured with silicone hydrogels is more than 0.50 diopters in approximately 30% of cases and can be as high as 1.00 diopter in 5% of cases, significant visual complaints may develop if the refractive change is allowed to persist undetected.
Practitioners would therefore be wise to adopt the following practices:
• Full refraction should be undertaken before and regularly reviewed in the initial weeks/months following the initial fitting of soft silicone hydrogel lenses.
• Corneal topography and/or central corneal thickness measurements should be included whenever possible. Keratometry is required as a minimum.
• Early follow-up visits should be scheduled in high risk cases such as high hyperopes.
• Subjects should be advised to return for follow-up should they experience any unusual visual symptoms.
_______
Contact lens and orthokeratology (ortho-k):
The formal definition of orthokeratology is “the reduction or elimination of refractive anomalies and binocular dysfunctions by the programmed application of contact lenses.” In simple terms, this means using overnight rigid contact lenses to change the shape of the cornea of the eye, and it is especially applicable to myopic eyes. The majority of people who undergo orthokeratology are myopes. Very few are hyperopes. There are also a substantial number of people who use the method to treat astigmatism. When worn only at night, they have been found to slow down eye growth by more than 50% compared to soft lenses and glasses, according to studies by Drs. Jeffrey Walline, Pauline Cho, and Helen Swarbrick. Another study, published in November 2014 in the journal Ophthalmology, found no eye growth over a one-year period in eyes wearing overnight orthokeratology lenses. In the study, participants used traditional daytime-wear GP lenses in one eye — which did exhibit growth during the study period — and orthokeratology lenses in the other. These designs reshape the front surface of the eye (the cornea) and reduce existing myopia in qualified candidates when worn at night only, allowing wearers the freedom of not wearing contacts or glasses during the day.
_
Figure above shows an eye with a contact lens. Note that the contact lens is flatter than the cornea. The difference in curvature is greatly exaggerated for clarity. It is easy to visualize from this diagram that if the cornea conforms to the contact over a period of time it will have become flatter. Then with the contact removed, the rays of light entering the eye will be bent less at the cornea than they were before the cornea was changed. These rays of light will thus come to a focus farther back in the eye, making the eye less myopic. Naturally, hard contacts (RGP), rather than soft contacts, have to be used since soft contacts would conform to the cornea – the opposite of what is intended. After the cornea has been flattened a sufficient amount (a process that can take months or even years, depending on the initial amount of myopia), clear unaided vision is achieved. In the usual treatment, the eyes are examined every six weeks or so, and as the cornea changes a different set of lenses is prescribed. The patient may receive five or six pairs the first year, three or four the second year, and two or three the third year. The cost for the complete treatment may be several thousand dollars. There are other drawbacks to orthokeratology in addition to its expense: it does not eliminate the cause of the myopia, and the results are usually not permanent. This means that after clear unaided vision is attained, it is usually necessary to wear retainer lenses for part of the day. These are lenses that help retain the improvement that has occurred, to prevent the cornea from drifting hack toward its original shape. They are essentially the same as the lenses which the patient has been wearing for the treatment. They are just worn less often.
_
Orthokeratology should not be used in beginning myopia when the myopia is caused only by a ciliary spasm. Instead, spastic myopia should be eliminated as quickly as possible by the teaching of proper close-work habits and by the use of preventive aids to inhibit the accommodation for close work. If the cause of the acquired myopia is ignored, flattening of the cornea could be nearly as detrimental as the prescription of concave lenses, since both actions, by decreasing the convergence of the light rays entering the lens of the eye, make it necessary for the lens to accommodate more when focusing on an object at any given distance. This increased accommodation could aggravate the ciliary spasm and result in a further elongation of the eye, which will make necessary a further flattening of the cornea by continued orthokeratology treatment – the same vicious circle that concave lenses create. In adults, when the myopia progression has ceased, the above statement may not apply, but it does apply to children. What is the sense of flattening the cornea to move the point of focus further back in the eye while we permit the eye to continue lengthening because of excessive close work? The word orthokeratology comes from ortho, meaning correct or proper, and keratology, meaning having to do with the cornea. It thus means forming the cornea to a correct shape. This is certainly an accurate definition of what happens when a highly astigmatic cornea is made less astigmatic, but in the treatment of myopia it is somewhat of a misnomer. Most myopes have normal corneas. Orthokeratology is actually used to produce an abnormally shaped cornea to compensate for the abnormally long eye which has been produced by an abnormal amount of close work. It is difficult to suppress the thought that this is going about things in an abnormal way.
_
Latest research on contact lenses:
_
Therapeutic soft lenses:
Soft lenses are often used in the treatment and management of non-refractive disorders of the eye. A bandage contact lens protects an injured or diseased cornea from the constant rubbing of blinking eyelids thereby allowing it to heal. They are used in the treatment of conditions including bullous keratopathy, dry eyes, corneal abrasions and erosion, keratitis, corneal edema, descemetocele, corneal ectasis, Mooren’s ulcer, anterior corneal dystrophy, and neurotrophic keratoconjunctivitis. Contact lenses that deliver drugs to the eye have also been developed.
Contacts release Anesthesia to Eyes of Post-Surgery Patients:
Scientists have developed a contact lens that releases anesthesia to the eye for post-surgery pain relief. The contacts can be particularly effective for patients who undergo PRK (photorefractive keratectomy), in which the healing process can take days, weeks or even months. Currently, medicated eye drops are used after laser eye surgery, and patients typically use the drops every few hours for several days. Compared to the LASIK procedure, PRK has a longer period of pain following surgery, and PRK patients receive a “bandage” contact lens to help the eye heal. A team of scientists found that anesthesia can continually release from the lens for a full day and up to seven days when vitamin E is added to the lens. Without vitamin E, the lens can release anesthesia for only less than two hours. The scientists stated that the vitamin E loaded silicone contact lens could act as a bandage contact lens as well as deliver pain medication following laser eye surgery. The study was reported in the American Chemical Society’s journal Langmuir.
_
Bionic contact lens:
A recent area of research is in the field of bionic lenses. Bionic lenses are visual displays that include built-in electric circuits and light-emitting diodes and can harvest radio waves for their electric power. Bionic lenses can display information beamed from a mobile device overcoming the small display size problem. The technology involves embedding nano and microscale electronic devices in lenses. These lenses will also need to have an array of microlenses to focus the image so that it appears suspended in front of the wearer’s eyes. The lens could also serve as a head-up display for pilots or gamers.
_
Magnetic contact lenses:
Tracking eye movements can let a computer know when someone is paying attention and identify exactly what they are interested in, but it’s also a tricky business. Most systems work by using a camera and image recognition software to identify a person’s pupils and work out the direction of their gaze. In real-life situations, however, tracking systems can be easily confused by rapid head movement or spectacles. Now, the Office of Naval Research is looking for better ways of tracking eyes in the hope of developing military applications, such as tracking a fighter pilot’s gaze. So it has a funded James DiCarlo, a neuroscientist at the Massachusetts Institute of Technology in Cambridge, US, to develop a magnetic contact lens. A soldier would wear the lenses and a magnetic sensor attached to the side of his or her head. The sensor picks up any changes in the local magnetic field and works out how the wearer’s eyes are moving. The system should work regardless of head orientation and movement, lighting conditions or “face furniture” such as goggles or glasses. The team says the magnetic lenses could also let disabled people control equipment such as wheelchairs.
_
Scleral lenses:
A scleral lens is a large, firm, oxygen permeable lens that rests on the sclera and creates a tear-filled vault over the cornea. The cause of this unique positioning is usually relevant to a specific patient, whose cornea may be too sensitive to support the lens directly. Although several kinds of scleral lenses are available in the United States, the Boston prosthesis is arguably the most well-known. According to the foundation’s Web site, their lens is “an oxygen permeable optical shell that fits under the lids and over the front surface of the eye.” It fits on the sclera and immerses the eye in a pool of artificial tears. “The fluid reservoir of the device masks the distorted surface of the cornea to improve vision and provides a protective cushion that reduces pain and photosensitivity caused by inflamed and irritated corneas and dry eyes,” according to the Web site. Scleral lenses can be used in patients who are otherwise contact-lens intolerant. Scleral lenses may be used to improve vision and reduce pain and light sensitivity for people suffering from growing number of disorders or injuries to the eye, such as severe dry eye syndrome (Kerotanconjuctivis sicca), microphthalmia, keratoconus, corneal ectasia, Stevens–Johnson syndrome, Sjögren’s syndrome, aniridia, neurotrophic keratitis (aneasthetic corneas), complications post-LASIK, high order Aberrations of the eye, complications post-corneal transplant and pellucid degeneration. Injuries to the eye such as surgical complications, distorted corneal implants, as well as chemical and burn injuries also may be treated by the use of scleral lenses.
_
Contact lens with telescope:
Swiss researchers have unveiled a first-of-its-kind telescopic contact lens, giving hope to millions suffering from low vision and age-related macular degeneration (AMD) a better and stronger vision. Swiss researchers are developing contact lenses that contain tiny telescopes to boost vision and zoom in and out with the wink of an eye but not blinks. The new, 1.55 millimeter-thick contact lens contains an extremely thin, reflective telescope, which is activated by winks. The device magnifies objects 2.8 times, meaning AMD patients can read more easily and better recognize faces and objects with its help. Small mirrors within bounce light around, expanding the perceived size of objects and magnifying the view, so it’s like looking through low magnification binoculars. The team has also developed a novel method of electronically switching the wearer’s view between normal, unmagnified vision and telescopic. This switching functionality is crucial for the lenses to be widely useful for non-AMD sufferers, who will be able to have magnification “on demand”. In the system, electronic glasses use a small light source and light detector to recognise winks and ignore blinks. The wearer winks the right eye for magnification and left eye for normal vision. The combination of the telescopic contact lenses and optional blink-controlled eyewear represent a huge leap in functionality and usability in vision aid devices and a major feat for optics research. The contacts are made using large, rigid “scleral lenses,” unlike the soft contacts most people wear, but are nonetheless safe and comfortable. Since eyes need a steady supply of oxygen, the team has spent the last couple of years making the lenses more breathable – which is a critical requirement. To achieve oxygen permeability, they are incorporating tiny air channels roughly 0.1mm wide within the lens to allow oxygen to flow around and underneath the complex and normally impermeable optical structures to get to the cornea. The results are improving as the mechanical and manufacturing processes are refined and better understood.
__________
__________
Refractive surgery
Techniques that correct for refractive error in the eye have undergone dramatic evolution. The cornea is the easiest place to place a correction, so most techniques have focused on modifying the shape of the cornea.
_
Keratoplasty:
Keratoplasty is a technique for correction of refractive eye errors. These are carried out by making a series of precise cuts under anaesthesia on the cornea, in order to reshape it. The fundamental principle on which this procedure was based upon was that it was the loss of the round shape and correct curvature of the cornea that leads to errors of refraction. Initially the cuts on the cornea were made by hand using a very thin surgical blade. If the surgeon were to make too deep a cut on the cornea, it would have caused clouding of the cornea and ultimately loss of vision. This was precisely the reason why it was more known for the failures rather than due to the successes. Then came the age of lasers and further understanding of the procedure and principles and techniques involved in it. Today, the eye surgeon can make careful calculations about the degree of correction required and use computers to guide a laser ray to make the cuts. Since the length of the rays can be made extremely precisely, there is practically no danger of cutting too deep. Moreover, with computer-driven cutting, extremely precise cutting of the cornea is possible. For most refractive errors, excimer laser surgery has replaced radial and astigmatic keratotomy because of its ability to remedy precisely a wider range of refractive errors. Computerized topography and computerized aberrometry can be used preoperatively to determine the best procedure and postoperatively to determine whether additional correction might be needed. The topographic apparatus measures the true elevation of each portion of the cornea and gives the surgeon an accurate picture of the corneal surface. The aberrometers measure the total refractive error of the eye and can be synchronized with an excimer laser system to correct higher-order aberrations. The modern excimer laser system can minimize new higher order aberrations that would otherwise be induced by the refractive corneal laser procedure. New topography-guided ablations have been used around the world. Lens exchange procedures and introduction of an intraocular lens to augment the natural lens of the eye are also assuming a greater role in correcting refractive errors. Many of the new intraocular lenses have aspheric (nonspherical) optics that further reduce higher order aberrations that might otherwise be seen after cataract and refractive lens exchange procedures.
_
The term “refractive surgery” describes various elective procedures that modify the refractive status of the eye. Procedures that involve altering the cornea are collectively referred to as keratorefractive surgery, refractive keratoplasty, or corneal refractive surgery. Other refractive surgery procedures include the placement of an intraocular lens (IOL) implant, either in front of the crystalline lens (phakic IOL) or in place of the crystalline lens (refractive lens exchange). Refractive surgery may be considered when a patient wishes to be less dependent on eyeglasses or contact lenses, or when there are occupational or cosmetic reasons not to wear eyeglasses. Keratorefractive surgery can be applied to a broad range of refractive errors, but in some circumstances, the surgeon may consider an intraocular procedure. Laser assisted in situ keratomileusis (LASIK) is the most commonly performed refractive surgery worldwide. Good visual results, quick rehabilitation and negligible complication rates have been the main reasons for the widespread acceptance rate of this procedure. Patients should be informed that there is a risk for night vision symptoms after keratorefractive surgery. Most studies of conventional and wavefront-guided LASIK have not shown a relationship between the diameter of the low light pupil and night vision symptoms postoperatively.
_
A comprehensive medical eye evaluation should be performed before any refractive surgery procedure. The refractive surgery examination should include the following elements:
◦Distance visual acuity with and without correction
◦Manifest and, when appropriate, cycloplegic refraction
◦Computerized corneal topography
◦Central corneal thickness measurement
◦Evaluation of tear film and ocular surface
◦Evaluation of ocular motility and alignment
_
Before refractive surgery, corneal topography should be evaluated for evidence of irregular astigmatism, corneal warpage, or abnormalities suggestive of keratoconus or other corneal ectasias. All of these conditions may be associated with unpredictable refractive outcomes, and keratoconus and the ectasias may be associated with ectasia progression following keratorefractive surgery. When considering intraocular refractive surgery, measurement of corneal topography is important to assess the optical characteristics of the cornea. It is also relevant if a keratorefractive surgical procedure is necessary to optimize the refractive result after the lens surgery or for toric intraocular lens implantation.
_
People who usually should not have refractive surgery include those who have
•A change in their eyeglass or contact lens prescription in the past year
•An autoimmune or connective tissue disease
•Eye disease
•Keratoconus (cone-shaped corneas)
•Severe dry eyes
•Poor wound healing
Additional people who usually should not have refractive surgery are those who are
•Taking certain drugs (for example, isotretinoin or amiodarone)
•Younger than 18 (with a few exceptions)
_
Ocular limitations to refractive surgery:
_
| Factors indicating poor candidate for laser eye surgery: |
| Major illness or autoimmune disease. |
| Eye problems other than needing glasses. |
| A vision prescription that has changed in the past year. |
| Needing a very high prescription (thick glasses) or a very minor one. |
| Pupils that are extra large in dim conditions. |
| Thin corneas. |
| Very dry eyes. |
_
Today, various options in vision correction surgery include the following:
•radial keratotomy (RK)
•laser vision correction
•photorefractive keratotomy (PRK)
•laser in situ keratomileusis (LASIK)
•femtosecond laser-assisted LASIK (iLASIK)
•laser thermal keratoplasty (LTK)
•conductive keratoplasty (CK)
•intracorneal ring segments (ICR)
•phakic intraocular lens implants
•PRELEX (presbyopic refractive lens exchange) or clear lens extraction
_
Conductive keratoplasty:
Conductive keratoplasty (CK) is a type of refractive surgery that uses radio waves to adjust the contour of the cornea by shrinking the corneal collagen around it. It is used to treat mild to moderate hyperopia. It is a non-invasive alternative to other types of eye surgery. It uses the same principles of Laser Thermokeratoplasty (LTK) and Radial Keratocoagulation, although the former uses holmium laser and the latter a 700° Celsius needle to correct hyperopia.
_
Laser refractive surgery:
LASIK is an acronym for “laser assisted in situ keratomileusis” (in situ means “in place” and keratomileusis means “shaping the cornea”). Conventional LASIK can correct short sight, long sight and astigmatism, accounting for around 95 per cent of refractive error. Wavefront LASIK tackles the remaining 5 per cent of defects and many consider that it offers better results. PRK and LASEK are alternatives – the recovery period is longer than for LASIK, but might be safer if your cornea is relatively thin. LASIK combines delicate surgical procedures and laser treatment. First, eye surgeons surgically create a “flap” of corneal tissue less than a third the thickness of a human hair, and lift the flap to one side. They then apply laser energy to reshape the cornea according to carefully calculated measurements. When treating nearsightedness, the laser is used to decrease the cornea’s relative curvature. When treating farsightedness, the cornea’s relative curvature is increased. They then reposition the corneal flap. A naturally-adhering bandage, the flap helps to improve results and speed recovery. LASIK may be used for nearsightedness, nearsightedness plus astigmatism, farsightedness, and farsightedness plus astigmatism. In PRK, or photorefractive keratectomy, eye surgeons apply the laser directly to the cornea according to carefully calculated measurements, without creating a flap. For nearsightedness, decrease the relative curvature; for farsightedness increase the relative curvature. At the conclusion of the procedure they place a transparent “bandage” contact lens over the cornea to promote healing. PRK is presently used to treat nearsightedness, nearsightedness plus astigmatism, farsightedness, and farsightedness plus astigmatism. In LASEK, or laser epithelial keratomileusis, alcohol is used to separate the outermost layer of the cornea to create and move aside a sheet of cells, a third the thickness of a LASIK flap. Eye surgeons then apply the laser to reshape the cornea. For nearsightedness decrease the relative curvature; for farsightedness increase the relative curvature. At the conclusion of the procedure, replace the sheet of cells and cover the cornea with a transparent “bandage” contact lens to promote healing. LASEK is presently used to treat nearsightedness, nearsightedness plus astigmatism, farsightedness, and farsightedness plus astigmatism. LASEK is reserved for patients who have thin corneas, are at risk of occupational damage to the eye, are reluctant to have a LASIK flap, or have corneal disease that precludes the LASIK procedure.
_____
Intraocular lens (IOL) for refractive error correction:
Phakia is the presence of the natural crystalline lenses.
•Aphakia is the absence of the natural crystalline lens. The aphakic state is usually due to surgery to remove a cataractous lens, but post surgical aphakia is rare nowadays because of the ubiquity of intraocular lenses. Rarely, aphakia can be post-traumatic or congenital in nature.
•Pseudophakia is the substitution of the natural crystalline lens with an IOL, as is often done after cataract extraction or to correct refractive error.
The root of these words comes from the Greek word phakos ‘lens’.
Phakic IOLs are implanted without removal of the patient’s original crystalline lens, and this is performed solely to correct refractive error in the presence of a clear crystalline lens.
Aphakic IOLs generally refer to lenses implanted secondarily in an eye already aphakic from previous surgery or trauma some time ago.
Pseudophakic IOLs refer to lenses implanted during cataract surgery, as a sequential step after removal of the cataractous lens of the patient
_
Intraocular lens:
An intraocular lens (IOL) is a lens implanted in the eye used to treat cataracts or myopia. The most common type of IOL is the pseudophakic IOL. These are implanted during cataract surgery, after the cloudy crystalline lens (otherwise known as a cataract) has been removed. The pseudophakic IOL replaces the original crystalline lens, and provides the light focusing function originally undertaken by the crystalline lens. The second type of IOL, more commonly known as a phakic intraocular lens (PIOL), is a lens which is placed over the existing natural lens, and is used in refractive surgery to change the eye’s optical power as a treatment for myopia or nearsightedness. IOLs usually consist of a small plastic lens with plastic side struts, called haptics, to hold the lens in place within the capsular bag inside the eye. IOLs were traditionally made of an inflexible material (PMMA), although this has largely been superseded by the use of flexible materials. Most IOLs fitted today are fixed monofocal lenses matched to distance vision. However, other types are available, such as multifocal IOLs which provide the patient with multiple-focused vision at far and reading distance, and adaptive IOLs which provide the patient with limited visual accommodation. IOL implantation carries several risks associated with eye surgeries, such as infection, loosening of the lens, lens rotation, inflammation and night time halos, but a systematic review of studies has determined that the procedure is safer than conventional laser eye treatment. Though IOLs enable many patients to have reduced dependence on glasses, most patients still rely on glasses for certain activities, such as reading.
_
Refractive lens replacement:
For people who are severely farsighted or severely nearsighted, an alternative approach is replacement of their natural lens with an artificial lens of a more appropriate power. This procedure is useful for anyone who is beginning to develop distortions in the lens of the eye, especially patients over fifty years of age. This is essentially the same as cataract surgery, an operation that has been perfected over the years. This approach is logical for patients who are beginning to develop a cataract or who are within the cataract age group. In patients with extremely high refractive errors, it is often the only choice. “Standard” single vision intraocular lenses focus at just one distance. Such lenses can provide an increased range of focus when both eyes are used together as in monovision technique. With monovision, near focus with one eye and a distance focus with the other eye can be combined to reduce dependence on glasses. However the recent development of intraocular lenses which actually focus for far and near can allow the patient to use both eyes for distance and both eyes for near. Bausch & Lomb’s Crystalens® actually changes position and shape to provide a clear focus at different distances. It utilizes the natural focusing muscle (ciliary muscle) of the eye to provide a continuous focus from far to near by inducing a forward movement and optical arching of the lens implant. This lens usually allows adequate focusing for reading vision. About 10% of patients do not focus adequately to read fine print without a reading glass, but they still obtain good distance and intermediate vision without correction. There are also several varieties of bifocal intraocular lenses which present the retina simultaneously with several focused images for different distances and the patient’s brain chooses the appropriate image to obtain well-focused vision. One of the newest lenses of this variety is Abbott Medical Optics’s Tecnis Multifocal Lens®. These lenses (and the above-mentioned Crystalens) also have an aspheric surface to minimize higher order aberrations and improve vision.
_
Phakic intraocular lens (PIOL) implantation:
A special intraocular lens is placed either in front of or behind the iris so that it works with the eye’s natural lens to bend the light rays more appropriately. This type of lens implant can correct very high degrees of myopia, and is particularly beneficial to younger patients since it allows them to retain the ability to focus near with their natural lens. Some uncommon problems, such as cataract formation, have been reported. Cataract formation in itself is not difficult to deal with regular cataract surgery if this becomes necessary. Two types of PIOLs have been approved by FDA. The VisianICL (Visian Implantable Collamer Lens), (FDA approved in 2004), produced by Staar Surgical Company and Artisan Myopia lens (FDA approved in 2004), produced by Ophtec USA Inc. The VisianICL is made of collamer, a biocompatible material, and the Artisan is a plastic lens.
_
Some of the risks found so far during a three-year study of the PIOL are:
•a yearly loss of 1.8% of the endothelial cells,
•0.6% risk of retinal detachment,
•0.6% risk of cataract (other studies have shown a risk of 0.5 – 1.0%),
•0.4% risk of corneal swelling.
Other risks include:
•0.03 – 0.05% eye infection risk, which in worst case can lead to blindness.
•glaucoma,
•astigmatism,
•remaining near or far sightedness,
•rotation of the lens inside the eye within one or two days after surgery.
One of the causes of the risks above is that the lens can rotate inside the eye, if the PIOL is too short if the eye was incorrectly measured, or because the sulcus has a slightly oval shape (the height is slightly smaller than the width). Toric IOLs must be powered and aligned inside the eye on a meridian that corrects the patient’s preexisting astigmatism. Again, these lenses can rotate inside the eye postoperatively, or be placed incorrectly by the operating surgeon. Either way, the patient’s preexisting astigmatism may not be corrected completely or may even increase. When IOLs are implanted in the aphakic patient—either after clear lensectomy for the correction of refractive error or after cataract extraction to restore eyesight—astigmatism in these patients is mainly attributable to the cornea. The surgeon can ascertain the astigmatic, or steepest, meridian in a number of ways, including manifest refraction or corneal topography. Manifest refraction is the familiar test where the eye doctor rotates various lenses in front of the eye, asking the patient, “Which is better (or clearer), this one or this one?” Corneal topography is considered a more quantitative test, and for purposes of aligning a toric IOL, most surgeons use a measurement called simulated keratometry (SimK), which is calculated by the internal programming of the corneal topography machine, to determine the astigmatic meridian on the surface of the cornea. The astigmatic meridian can also be identified using corneal wavefront technology or paraxial curvature matching.
_
Intracorneal Lens (Permavision):
This is a procedure where lenses can be implanter inserted under a flap in the cornea. These lenses are called PermaVision lenses which are made of optically clear Nutrapore. The lenses will permanently reshape the outer surface of the eye to make the eye focus properly. Nutrapore material is very similar to the cornea in its ability to pass nutrients, fluids, focus, hold water, and remain clear. The similarity of Nutrapore to the cornea is what makes the PermaVision procedure possible. Nutrapore can be precisely formed into crescent-shaped discs and rings to correct farsightedness or nearsightedness. Unlike LASIK, which corrects nearsightedness by removing tissue, the PermaVision lens is added to the eye. This makes the surgical procedure predictable, adjustable and removable should changes be needed later.
_
Corneal Transplants:
Corneal transplant is done to improve visual acuity by replacing the opaque or distorted host tissue by clear healthy donor tissue. The most common indication in this category is pseudophakic bullous keratopathy, followed by keratoconus, corneal degeneration, keratoglobus and dystrophy, as well as scarring due to keratitis and trauma.
_
Artificial Cornea:
An implanted biocompatible polymer might be used one day to modify the refractive properties of the cornea. Xie et al. stated that artificial corneas “…have the potential to become an alternative to spectacles and contact lenses for the correction of refractive error.” There are three different types of implants discussed: an implant that sits on the surface (i.e. replaces a segment of the epithelium, synthetic onlay), an implant that sits inside the cornea (i.e. in the stroma, synthetic inlay), and an implant, which replaces a full segment of the cornea (i.e. replaces a segment of the epithelium, the stroma and the endothelium).
_
Pediatric refractive surgery:
Although official guidelines state that the minimum age for refractive procedures should be 18 to 21 years, increased attention has been given to the surgical treatment of anisometropic amblyopia and high refractive errors in children who are noncompliant with standard optical correction by spectacles or contact lenses. The fundamental issue is that it is not possible to improve vision or restore stereopsis when the child is beyond the age of cortical visual maturity. Therefore, when needed, surgery should be performed and should be performed early. The sooner the treatment, the more chances we have to prevent amblyopia. Several studies have shown a poor compliance with spectacles or contact lenses in children with unilateral high myopia. On the other hand, if untreated, the different refractive power in the two eyes inevitably leads to lack of stereopsis and amblyopia.
_____
Pros and cons of refractive surgery:
People contemplating refractive surgery should discuss the potential benefits and risks with an ophthalmic surgeon who is well regarded by the medical and optometric communities. As with any type of surgery, complications can occur. With corneal procedures, it is not unusual for patients to experience flare around lights at night, especially younger patients who have large pupils. Undercorrection or overcorrection may occur with any procedure and may necessitate a second “enhancement” procedure. Sometimes glasses may be required even after this surgery, and rarely, corneal irregularity may require use of contact lenses. In many cases, LASIK surgery may be used to refine the result of lens exchange surgery.
_
With LASIK, complications in the cutting of the corneal flap can lead to corneal irregularity. Rarely, wrinkles occur in the cap, requiring lifting and refloating of the cap, and sometimes corneal epithelial tissue grows under it and has to be removed. The excimer laser ablation itself could be off-center, resulting in reduced vision, halos around lights, and astigmatism. Newer scanning-spot excimer lasers enable greater accuracy of treatment and prevention and correction of higher-order optical distortions. Newer highly accurate tracking systems make decentration of laser treatment much less likely.
_
Lens exchange surgery carries with it the possibility of any complication that could occur with cataract surgery, such as infection, bleeding, and retinal detachment. These are rare nowadays, and, whereas in the past lens replacement surgery caused the patient to lose the ability to focus for near, newer focusing lenses remedy this problem. Two special advantages of lens exchange surgery are that the patient will not develop further refractive changes in the lens as he ages and the patient will never develop a cataract.
_
Satisfaction with modern refractive surgery is very high, and complications are rare. Most patients do well, gaining a whole new world of freedom from dependence on eyeglasses or contact lenses. Even so, the risk involved may not justify the use of surgery if adequate vision and comfort can be achieved with eyeglasses or contact lenses. Individuals who wish to explore the possibility of refractive surgery should seek a qualified eye surgeon who is thoroughly experienced in a wide variety of procedures.
_
Complications occur in less than 5 per cent of cases, but make sure your consultant outlines all the risks. Flap complications with LASIK arise in 0-4 per cent of cases, but can usually be corrected with little or no loss of vision. Some people have a problem with dry eyes in the months after surgery and artificial tear supplements might be needed in the long term. Many patients have experienced glare or halo effects when night driving, particularly just after treatment. This is more likely in cases of higher correction that has been made, but is rarely severe. In rare cases, excessive thinning of the eye wall can cause the shape of the eye to be unstable after treatment. Severe loss of vision is very unusual, but some patients could require corneal surgery or hard contact lenses to restore vision. Most of these complications may be prevented by a thorough pre-operative examination of the prospective patients.
_
What are the risks of LASIK?
_
_
LASIK has been shown to be a very effective procedure, and most patients are very happy with their vision following the procedure. However, like any surgical procedure, LASIK does come with some risks. In order for you to decide whether LASIK surgery is right for you, you need to be aware of potential risks and complications and weigh these carefully before proceeding with surgery.
1. You may be over-corrected or under-corrected. Most patients are satisfied with their vision after a single treatment, but in some cases, you may not achieve quality vision initially and need a second surgery, called an enhancement, to sharpen your vision. Patients with more extreme prescriptions are at higher risk for needing an enhancement. This enhancement cannot be performed for many months after your initial surgery to allow for your eyes to heal appropriately from the first surgery and for your eyeglass prescription to stabilize. In some rare cases, you may not be able to have an enhancement if your corneas are too thin or abnormally shaped after surgery.
2. You may still need glasses or contact lenses after surgery to achieve your best vision. This is extremely rare for the average person; however, it is something you should discuss with your surgeon. In addition, if both of your eyes are corrected for good distance vision, you will still need glasses for close work when presbyopia develops as a part of normal aging process.
3. Your results may not be permanent. Although uncommon, some patients do experience a regression of their desired treatment effect many years after the surgery. This is more common in patients with hyperopia, or farsightedness. Those who need reading glasses are especially prone to having changes in their vision after LASIK surgery. If regression does occur, it may be possible for you to have an additional surgery many years after your initial LASIK.
4. You may experience visual aberrations, especially in low light. Visual effects that can occur with LASIK and decrease visual quality include: anisometropia (difference in refractive power between the two eyes), aniseikonia (difference in image size between the two eyes), double vision, hazy vision, fluctuating vision during the day and from day to day, increased sensitivity to light, glare, shadows, and seeing halos around lights. These visual aberrations are extremely unusual; however, they may be incapacitating for some time and may not ever go away completely.
5. Dry eye symptoms may persist or get worse. Most people experience some dry-eye symptoms immediately after surgery. In some cases, people may develop worsening of dry-eye symptoms, such as burning and redness, or even decreased vision, after surgery. This condition is occasionally permanent and may require medication to improve tear production or punctal plugs, which temporarily close off the drainage system for tears.
6. You may lose vision. Rarely, LASIK may result in worse vision that cannot be corrected with glasses or contact lenses. This could result from flap-related complications, equipment malfunction, infection, scarring, or extreme changes in corneal shape postoperatively.
_
Lasik eye surgery found imperfect, even dangerous:
Lasik eye surgery, where vision defects are cured with lasers, has a high success rate. However, anyone who undergoes the procedure must carefully weigh the risks. Those for whom the procedure fails must wear several glasses afterwards and suffer ailments. The complications, experts warn, are life changing. The results of bad eye laser surgery include the necessitating of several glasses for both near and far-sighted vision, dry eyes and blurring of light sources at night. It’s hard to imagine patients taking a similarly relaxed approach to any other kind of surgery, says Professor David Gartry, who since 1989 has performed more than 20,000 laser eye procedures. Laser eye surgery, he says, has become the victim of “an unhappy marriage between big business and medicine.” The procedure has been saddled with hard-sell tactics and “terribly unprofessional and serving only to trivialize the surgery.” Most importantly, according to Professor Gartry, is just who is doing the surgery. At the absolute minimum, people should find out who the surgeon is and their qualifications. They should also insist on talking to the surgeon before the procedure.
_
How common are LASIK complications?
The safety and effectiveness of LASIK surgery continues to improve, thanks to increasingly sophisticated technology, surgical skill and optimal patient selection. Complications generally were more common in the early years of LASIK, when studies in the late 1990s indicated that up to 5 percent of people undergoing laser vision correction experienced some type of problem. These days, this number is under 1 percent for serious complications. A worldwide review of LASIK published in 2009 showed that more than 95 percent of people who had LASIK surgery between 1995 and 2003 were satisfied with their outcome. Public confidence in LASIK has grown in recent years due to the solid success rate of LASIK surgery outcomes. The U.S. military also has adopted widespread use of laser eye surgery to decrease reliance of troops on corrective eyewear. As of 2008, more than 224,000 military personnel had undergone laser vision correction. Since the procedure first was introduced in the military in 2000, researchers have conducted more than 45 studies regarding safety and effectiveness of LASIK and other procedures. LASIK outcomes have been overwhelmingly positive. Most military patients see 20/20 or better after the procedure without corrective eyewear, and the rate of complications has been very low. According to one study, only one in 112,500 patients required medical disability retirement due to complications from laser vision correction during this eight-year period. In another study, 100 percent of pilots and other aircraft personnel from the U.S. Navy and U.S. Marine Corps who underwent custom (wavefront-guided) LASIK attained 20/20 uncorrected visual acuity within two weeks after surgery. When questioned about their satisfaction one month after surgery, 95 percent of these patients said the procedure was helpful to their effectiveness, and 100 percent said they would recommend it to other aviators. Study results were presented at the 2008 ASCRS annual meeting. Laser eye surgery has successfully treated millions of patients and has high patient satisfaction rates. However, as with any surgery, LASIK involves potential complications. It is important for you to weigh the benefits and risks before choosing to go ahead with surgery.
______
______
Eyeglasses (spectacles) vs. contact lens vs. refractive surgery:
When deciding between contact lenses or eyeglasses to correct your vision, how do you know which is best for you? Whether you choose to wear eyeglasses or contact lenses for vision correction mostly depends on personal preferences. Lifestyle, comfort, convenience, budget and aesthetics should all factor into your decision-making process. Before deciding between contacts and glasses, keep in mind that one is not necessarily better than the other; each has its pros and cons in terms of vision, ease of use and eye health. Eyeglasses offer many benefits over contact lenses. They require very little cleaning and maintenance, you don’t need to touch your eyes to wear them (decreasing your risk for eye infections), and glasses are cheaper than contact lenses in the long run since they don’t need to be replaced as often. Glasses also can act as an extension of your personality and make a great fashion statement! That being said, contact lenses have many advantages over glasses. Contacts sit directly on your eye, so vision, particularly peripheral vision, is unobstructed. You can participate in sports and outdoor activities without fear of eyeglasses getting in the way, falling off or breaking. You can even change the color of your eyes with color contact lenses.
_
Do glasses worsen myopia?
Glasses may have the potential to make the eyes worse, as they increase the accommodation needed by the eyes to focus. Evidence of this can be seen when people with higher prescriptions have a harder time with activities like reading because their eyes grow tired faster. Stronger prescriptions require a higher accommodation by the eyes to focus through them, which can, over time, worsen eyesight, requiring yet another prescription, in a continuous but quickening cycle. However, the eyestrain caused by not wearing glasses when they are needed can also be a risk factor. The best way to avoid needing new lenses is by reducing the amount of near work, which forces the eyes into a continuous near-focusing position that eventually causes or increases myopia, by taking frequent breaks from near work, and by only wearing glasses when they are needed. Reading glasses can also be worn during near work to decrease the strain on the eye, especially when already wearing corrective lenses, as they work in the opposite fashion to normal lenses. Using this practice may have the potential to prevent near-sightedness or slow its progression. Contact lenses of equivalent prescription may not result in the same effect as eyeglasses, as they are closer to the eyes and may require less accommodation.
_
Once children have matured enough to handle the responsibility, then contact lenses may be an option. Most ophthalmologists agree that patients should be in their pre-teen or early teenage years before considering contact lenses; however the decision is made for each patient based on their level of maturity. In special circumstances, refractive surgery may be indicated for children with neurological impairment, neurobehavioural issues, facial deformities (craniofacial, hemifacial microsomia, ear deformity) or severe anisometropia that render it impossible for glasses wear. Although contact lenses are usually the secondary treatment option for children with developmental anomalies, there are concerns for infection, mishandling, and expense. Refractive surgery for the general population is usually only indicated once the patient has stopped growing which generally occurs in the late teens to early twenties.
_
Discuss with your eye doctor the following factors when choosing your corrective vision path:
• Age
• Cost
• Individual preference
• Lifestyle
• Occupation
• Other health conditions
• Severity and type of refractive error
It is also important to weigh the pros and cons between your options to help guide you to the most comfortable fit for your lifestyle.
________
________
Refractive Error Treatments comparison:
| Type of correction | Advantages | Disadvantages |
| Eyeglasses |
|
|
| Contact lenses |
|
|
| Surgery |
|
|
______
______
Residual refractive errors:
Residual refractive errors are the differences between the intended refractive correction and the actual refractive correction. Refractive surgeons generally aim for 20/20 vision (good vision without glasses or contacts). But many people don’t wind up with perfect 20/20 vision. There are numerous types of residual refractive errors. Most people who do not achieve 20/20 vision after the first surgery have several options. They can wear glasses or contact lenses to correct the remaining refractive error, or they can choose to undergo additional surgery to correct the residual refractive error (provided their corneas have enough thickness to allow the removal of more tissue). Additional surgery usually comes with a risk level similar to the original surgery. Some people can achieve 20/20 vision on a high contrast eye chart but still have horrible vision. If the area of correction placed on the eye is smaller than the pupil, one may experience glare, arcing, starbursts and/or halos (commonly called “GASH”). Others are left with a “bumpy cornea” (called “irregular astigmatism” and/or “higher order aberrations” (HOAs) that cause the light to scatter as it enters the cornea. When this happens, the patient will see multiple images with each eye. There is no reliable surgical fix for these problems at this time, although technology continues to advance. Since glasses and soft contact lenses usually cannot mask these problems, gas permeable rigid contact lenses (RGP) are the only option for this group of patients. Fitting prosthetic RGPs after refractive surgery can be challenging (due to the changed curvature of the cornea) and not everyone is able to wear these lenses successfully. There are also other types of residual refractive errors. The commonest being residual refractive error after Cataract surgery. In analysing refractive outcomes of cataract surgery, it is important not just to consider the percentage of cases falling within ±1 dioptre of the intended refractive result, but also look at whether there is a systematic tendency for the results to be more myopic or hyperopic than intended (in which case the constant for the intraocular lens model may need to be modified), and to consider the cases with a refractive outcome more than 2 dioptres away from the intended result. Outlying results are not necessarily due to human error or faulty equipment. The formulae used to estimate intraocular lens power do not achieve an accurate prediction in a small proportion of eyes, however carefully the measurements are made. However, where a “refractive surprise” occurs, biometry should be repeated to look for any inaccuracy in the preoperative measurements. This situation, however should be distinguished from a “wrong lens” incident where an intraocular lens other than the one intended was implanted. For toric lenses, rotating the lens may fix the issue.
_
The most common postoperative cataract surgical problems result from refractive inaccuracies. Lack of precision in biometric analysis, inadequate selection of the IOL power, limitations of the calculation formulas, or intraoperative IOL positional errors may contribute to unexpected refractive errors and visual outcomes after uneventful cataract surgery. IOL exchange, piggyback lens implantation, and laser vision correction (LASIK) are reasonable alternatives to reduce postoperative ametropia and improve patient satisfaction.
___________
Dopamine treatment:
Dopamine is a major neurotransmitter in the retina involved in signal transmission in the visual system. In the retinal inner nuclear layer, a dopaminergic neuronal network has been visualized in amacrine cells. Also, retinal dopamine is involved in the regulation of electrical coupling between horizontal cells and the retinomotor movement of photoreceptor cells. Also dopamine participates in visually guided eye growth regulation. Possible treatments involving dopamine in preventing a decrease in visual acuity have been shown to be successful in the past. L-Dopa treatment in children with amblyopia showed an improvement in visual acuity. In rabbits, injections of dopamine prevented the myopic shift and axial elongation typically associated with FDM (Form-deprived myopia). In guinea pigs, systemic L-dopa has been shown to inhibit the myopic shift associated with FDM, and has compensated for the drop in retinal dopamine levels. These experiments show promise in treating myopia in humans.
________
What Are Low-Vision Aids?
Aids for coping with vision loss (referred to as low-vision aids) can be an enormous help to people with only partial vision. Low-vision aids for reading, writing, watching television, and engaging in outdoor activities include the following:
•Large-print books
•Large-numbered telephones, clocks, watches, and thermometers
•Closed-circuit television to magnify objects
•Electronic “talking” clocks and other “talking” devices
•Computer programs that can scan text and then produce larger text or read the text out loud
•Light filters to improve contrast
•Color-coded pill boxes
•Handheld magnifying glasses
•Glare-reducing sunglasses
•Handheld binoculars
___________
Visual Training for Refractive Errors:
Vision training consists of a variety of programs designed to enhance visual efficiency and processing. Vision training, or orthoptics, typically addresses how well both eyes work together. Eye exercises may include, muscle relaxation techniques, biofeedback, eye patches, eye massages, the use of under-corrected prescription lenses, and/or nutritional supplements. Training is most often provided by an optometrist. After going through many studies, no evidence is found that visual training 1) has any effect on the progression of myopia; 2) improves visual function for patients with hyperopia or astigmatism; or 3) improves vision lost through disease processes, such as age-related macular degeneration, glaucoma, or diabetic retinopathy.
___________
___________
Computer glasses:
Computer vision syndrome (CVS):
According to the American Optometric Association (AOA), the most frequent health complaints among computer workers are vision-related. Studies indicate that 50 to 90 percent of computer users suffer from visual symptoms of computer vision syndrome. With more and more of us using a computer at work, CVS is becoming a major public health issue. The AOA reports that a survey of optometrists found that approximately 10 million eye exams are performed annually in the United States due to vision problems related to computer use. Many people experience eye strain from using a computer for long periods. This has been given the name Computer Vision Syndrome and consists of such problems as fatigue, headache, dry eyes, eyestrain, blurred vision and double vision. This has been attributed to glare from overhead lights, glare from the screen, poor contrast, reflections, poor lighting, squinting, infrequent blinking resulting in dry eyes, focusing close for long periods of time, ultraviolet light or “radiation” from the screen, inadequate screen resolution, etc. Also, letters on a computer screen consist of round pixels of light that form letters which are not sharply defined on the edges, different from the solid lines of normal print. This can create difficulty for the brain to accurately control focusing effort, resulting in blurred vision. The eye can tend to constantly shift its focus from the print to a point farther away and back again, causing fatigue.
_
Many computer users do need a pair of glasses for their computer work that is different from the glasses they use for their other common visual needs. In other cases, they may have a vision disorder that would not otherwise require correction if they weren’t performing a demanding visual job such as at the computer. Even people with excellent unaided vision could need glasses just for computer use. These are called “computer glasses”. Computer eyeglass lenses are generally not suitable for driving or regular wear.
_
CVS and Worker Productivity:
A study conducted by the University of Alabama at Birmingham (UAB) School of Optometry examined the relationship between the vision of computer workers and their productivity in the workplace. Studies suggest that increased productivity more than justifies the cost of computer glasses.
This study found:
•A direct correlation between proper vision correction and productivity. This relationship particularly is evident with complex and/or repetitive computer tasks such as data entry.
•A direct correlation between proper vision correction and the time required for a computer worker to perform a task. Computer-related tasks took much longer when the subjects wore glasses with less than the optimum correction.
•Reduced productivity even among computer users who were unaware they had vision problems. Computer users with small refractive errors may not notice any vision discomfort. But without proper vision correction, their performance on a specific task can suffer significantly — by as much as 20 percent.
The data strongly suggest that improving the visual status of workers using computers results in greater productivity in the workplace, as well as improved visual comfort. According to the UAB study, the economic benefit to employers of providing computer eyewear to their employees can be determined by measuring the average gain in productivity for computer workers over a one-year period, and dividing this productivity gain by the costs associated with the eyewear. The study confirms that investing in optimal computer eyewear for employees results in a significant cost-benefit ratio.
_
Why Computer Glasses?
Computer glasses differ from regular eyeglasses or reading glasses in a number of ways to optimize your eyesight when viewing your computer screen. Computer glasses include special lens coatings to reduce glare and a tint designed to eliminate eye strain. Computer screens usually are positioned 20 to 26 inches from the user’s eyes. This is considered the intermediate zone of vision — closer than driving (“distance”) vision, but farther away than reading (“near”) vision. Most young people wear eyeglasses to correct their distance vision. Reading glasses are prescribed to correct near vision only. And bifocals prescribed for those over age 40 with presbyopia correct only near and far. Even trifocals and progressive lenses (which do have some lens power for intermediate vision) often don’t have a large enough intermediate zone for comfortable computer work. Without computer eyeglasses, many computer users often end up with blurred vision, eye strain, and headaches — the hallmark symptoms of computer vision syndrome. Worse still, many people try to compensate for their blurred vision by leaning forward, or by tipping their head to look through the bottom portion of their glasses. Both of these actions can result in a sore neck, sore shoulders and a sore back. Though they sometimes are called “computer reading glasses,” it’s best to call eyewear designed specifically for computer use “computer glasses” or “computer eyeglasses” to distinguish them from conventional reading glasses. Computer glasses put the optimum lens power for viewing your computer screen right where you need it for a clear, wide field of view without the need for excessive focusing effort or unhealthful postures.
_
The simplest computer glasses have single vision lenses with a modified lens power prescribed to give the most comfortable vision at the user’s computer screen. This lens power relaxes the amount of accommodation required to keep objects in focus at the distance of the computer screen and provides the largest field of view. Single vision computer glasses reduce the risk of eye strain, blurred vision and unnatural posture that can cause neck and back pain, and can be used comfortably by young and old computer users alike. Another popular lens design for computer glasses is the occupational progressive lens — a no-line multifocal that corrects near, intermediate, and, up to a point, distance vision. It has a larger intermediate zone than regular progressive lenses for more comfortable vision at the computer. But this leaves less lens area for distance vision. So these lenses are not recommended for driving or other significant distance vision tasks. Other lenses used for computer glasses include occupational bifocal and trifocal lenses. These lined multifocal lenses have larger zones for intermediate and near vision than regular bifocals and trifocals, and the position of the intermediate and near zones can be customized for your particular computer vision needs.
_
Lens Coatings and Tints:
For maximum viewing comfort, the lenses of your computer glasses should include anti-reflective coating. Sometimes called anti-glare treatment, anti-reflective (AR) coatings eliminate reflections of light from the front and back surfaces of your lenses that can cause eye strain. Some eye doctors recommend adding a light tint to computer glasses to reduce glare caused by harsh overhead lighting and to enhance contrast. Tinted computer lenses also are recommended to block short-wavelength, “blue” light emitted from computer screens that is associated with glare and eye strain.
____
A pair of computer glasses should include:
•The prescription measured at the computer working distance
•The appropriate lens type for the patient
•A computer tint
•A UV tint
•An anti-reflective (AR) coating
•Prism, if needed
_____
Are Computer Glasses effective?
Whether or not computer glasses will be worth it and work for you is subjective, because factors include your visual abilities and computer usage, work environmental conditions, and your viewing habits. Computer eyewear does not necessarily prevent eye strain in an already optimized environment. Also, the range that the eyes can sweep from one side to the other is maximized without any eyewear. The frame edges limit this range of motion and may actually hinder people more who are not getting much benefit from wearing the glasses. Also eyeglasses get smudges which can interfere with vision as well. However, if you experience eyestrain, they are probably worth it. Eyeglasses with the premium anti-reflective coating help to ensure that your vision remains clear by keeping dust, fingerprints, etc. from appearing on your lenses. You will also want to look for glasses that include a small bump which will provide just enough of a boost in power, that the print on screen becomes slightly larger, thus decreasing eye strain. In addition, most computer glasses can help increase contrast, which makes it easier for your eyes to focus on a computer screen. A few studies back this up. A clinical study/survey by New York University College of Medicine of 121 patients, for example, found that 69% of them preferred AR-coated lenses over non-coated ones and reported lower pain or vision problems due to glare. 79% of them chose Transition lenses (the kinds that adapt to light) over clear ones.
_
Computer eye strain relief measures:
1. Use proper lighting:
Eye strain often is caused by excessively bright light either from outdoor sunlight coming in through a window or from harsh interior lighting. When you use a computer, your ambient lighting should be about half as bright as that typically found in most offices. Eliminate exterior light by closing drapes, shades or blinds. Reduce interior lighting by using fewer light bulbs or fluorescent tubes, or use lower intensity bulbs and tubes. If possible, position your computer monitor or screen so windows are to the side, instead of in front or behind it.
2. Minimize glare:
Glare on walls and finished surfaces, as well as reflections on your computer screen also can cause computer eye strain. Consider installing an anti-glare screen on your monitor and, if possible, paint bright white walls a darker color with a matte finish. Again, cover the windows. If you wear glasses, purchase lenses with anti-reflective (AR) coating. AR coating reduces glare by minimizing the amount of light reflecting off the front and back surfaces of your eyeglass lenses.
3. Upgrade your display:
LCD screens are easier on the eyes and usually have an anti-reflective surface. Old-fashioned CRT screens can cause a noticeable “flicker” of images, which is a major cause of computer eye strain. Even if this flicker is imperceptible, it still can contribute to eye strain and fatigue during computer work. Choose a relatively large display. For a desktop computer, select a display that has a diagonal screen size of at least 19 inches.
4. Adjust your computer display settings:
Adjusting the display settings of your computer can help reduce eye strain and fatigue. Generally, these adjustments are beneficial:
•Brightness. Adjust the brightness of the display so it’s approximately the same as the brightness of your surrounding workstation. As a test, look at the white background of this Web page. If it looks like a light source, it’s too bright. If it seems dull and gray, it may be too dark.
•Text size and contrast. Adjust the text size and contrast for comfort, especially when reading or composing long documents. Usually, black print on a white background is the best combination for comfort.
•Color temperature. This is a technical term used to describe the spectrum of visible light emitted by a color display. Blue light is short-wavelength visible light that is associated with more eye strain than longer wavelength hues, such as orange and red. Reducing the color temperature of your display lowers the amount of blue light emitted by a color display for better long-term viewing comfort.
5. Blink more often:
Blinking is very important when working at a computer; blinking moistens your eyes to prevent dryness and irritation. When working at a computer, people blink less frequently — about one-third as often as they normally do — and many blinks performed during computer work are only partial lid closures, according to studies. Tears coating the eye evaporate more rapidly during long non-blinking phases and this can cause dry eyes. Also, the air in many office environments is dry, which can increase how quickly your tears evaporate, placing you at greater risk for dry eye problems. If you experience dry eye symptoms, ask your eye doctor about artificial tears for use during the day. To reduce your risk of dry eyes during computer use, try this exercise: Every 20 minutes, blink 10 times by closing your eyes as if falling asleep (very slowly). This will help rewet your eyes.
6. Exercise your eyes:
Another cause of computer eye strain is focusing fatigue. To reduce your risk of tiring your eyes by constantly focusing on your screen, look away from your computer at least every 20 minutes and gaze at a distant object (at least 20 feet away) for at least 20 seconds. Some eye doctors call this the “20-20-20 rule.” Looking far away relaxes the focusing muscle inside the eye to reduce fatigue. Another exercise is to look far away at an object for 10-15 seconds, then gaze at something up close for 10-15 seconds. Then look back at the distant object. Do this 10 times. This exercise reduces the risk of your eyes’ focusing ability to “lock up” (a condition called accommodative spasm) after prolonged computer work. Both of these exercises will reduce your risk of computer eye strain. Also, remember to blink frequently during the exercises to reduce your risk of computer-related dry eye.
_
Pinhole glasses to relieve CVS:
It would seem that pinhole glasses offer as good a solution to this problem. Glare from above or the sides is reduced by looking through the holes. The depth of field increases. Also, the focusing effort, or accommodation, is reduced, just as if you put on a weak pair of reading glasses. This also reduces the possibility of developing myopia from the constant close work, in those who are prone to do so. Ultraviolet, or other forms of radiation, have been shown to be of no consequence.
_
Do Contact Lens wearers have more Computer Vision Problems? 2014 study:
Because so many computer users wear contact lenses, researchers in Spain recently reviewed published studies to see if contact lens wear increases the risk of computer vision problems or causes a worsening of computer vision syndrome. The investigators found 114 studies written in English or Spanish and published from 2003 to 2013 that referenced both contact lenses and computer use. They chose six studies for final analysis. All six revealed that contact lens wearers were more likely to have computer vision syndrome symptoms than individuals who wore eyeglasses only or did not need corrective lenses. Prevalence of symptoms ranged from 17 to 95 percent among contact lens wearers and 10 to 58 percent among non-wearers. Also, contact lens wearers were four times more likely to have dry eyes during or after computer use, compared with non-wearers. Silicone hydrogel contact lenses were associated with more comfort than regular soft lenses among computer users. The study authors concluded that, during computer use, contact lens wearers suffer more eye discomfort and visual disturbances than non-wearers. But they also stated that, due to the small number of studies included in their analysis and the non-conclusive nature of some findings, more research is needed to determine the best type of contact lenses for computer users and how the lenses should be used. A report of the study was published in the March/April 2014 issue of the journal Revista Espanola de Salud Publica.
_______
_______
Refractive error in other disorders: cataract, glaucoma, diabetes, pregnancy etc
_
Refractive error and glaucoma:
If you are nearsighted (myopic), you are at an increased risk of developing open-angle glaucoma. If you are farsighted (hyperopic), you are at an increased risk of developing closed-angle glaucoma.
_
Refractive error and cataract:
It is well known that nuclear cataract can cause a myopic shift in some cases. This change accounts for the “second sight of the elderly” in which the myopic shift provides normal reading ability without the need for spectacles, although distance vision worsens. On the other hand, high myopia may lead to cataract. The effect of cortical and posterior subcapsular (PSC) cataract on refractive error is less clear. Planter suggested that cortical opacity can induce significant hyperopic shifts, but this claim has not been repeated. Review papers have suggested that cortical opacity can induce astigmatic changes.
_
Ocular changes during pregnancy:
Pregnancy is often associated with ocular changes. Most of them are specifically associated with the pregnancy itself, rare disturb the normal visual function and are transient in nature. The ocular effects of pregnancy may be divided into physiologic changes, pathologic conditions or modifications of pre-existing conditions. Pregnancy is associated with changes in corneal sensitivity and thickness, decreased tolerance to contact lenses, decreased intraocular pressure, can affect refractive error. Pathologic conditions reported to develop during pregnancy include hypertensive and vascular disorders, central serous chorioretinopathy, uveal melanoma and others. The most significant modified pre-existing condition is diabetes mellitus. Pregnant women are at increased risk for the progression of preexisting proliferative diabetic retinopathy, and diabetic women should see an ophthalmologist before pregnancy or early in the first trimester. Ocular changes associated with pregnancy are transient and most tend to resolve postpartum, with values returning to near pre-pregnant state.
_
Refractive error in diabetes mellitus:
Diabetes mellitus is one of the systemic diseases that has ocular manifestation. Hyperglycemia is the most frequently observed sign of diabetes and is considered the etiological source of diabetes complication both in the body and in the eye. Changes in refraction are very common in diabetes. Transient refractive changes have been reported during periods of hyperglycemia, or falling blood glucose level during intensive glycemic control. Myopia has been reported to developing hyperglycemia and that following therapy, there is a hyperopic shift. Other studies however reported a shift in the hyperopic direction during periods of hyperglycemia. Transient cataracts have also been reported in many cases of acute increase or reduction in blood glucose concentration in diabetic patients. Optometrists as primary eye care providers come in contact frequently with patients presenting with ocular manifestations of systemic diseases. Ability to identify these manifestations and the condition causing them will place the clinician in a better position to manage, offer counsel or refer for appropriate treatment. Lens abnormalities have been suggested as a cause of refraction error in diabetic patients. Excess glucose in the lens is converted to sorbitol during hyperglycemia. Sorbitol is poorly permeable and accumulates in the lens. When blood glucose reduces, the difference in osmotic pressure results in the influx of water from the aqueous humour into the lens, causing lenticular swelling. However, an increase in lens thickness would promote myopic changes through increase of refractive power, which seems to be contradictory with the observation of hyperopic changes when plasma glucose reduces. The hypothesis is that lens cortex hydration following the influx of water from the aqueous humour results in the decrease of refractive power, which might be involved in the development of transient hyperopic change. The morphological change of the lens is minor. It is important to note that blurred vision during hyperglycemia also can be caused by factors other than refractive changes. For instance, changes in metabolism can also lead to alterations in media transparency and autofluorescence. In addition, tear film instability secondary to increased tear osmolarity can reduce visual acuity in patients with poorly controlled diabetes. Both corneal and lens autofluorescence are higher in the diabetic population than in healthy control groups because of fluorophore accumulation in the cornea and lens of diabetic patients, which is increased in proportion to the level of glycemic control. The concentration of glucose in aqueous humor increased along with glucose levels when there was a breakdown of the blood-aqueous barrier, giving rise to autofluorescence. Although many of the studies cited above noted refractive shifts in hyperglycemic subjects, bear in mind that only a few found significant changes in refractive error, and the effect tends to be transient. The physiology of the anterior segment and chamber––and their relationship to refractive error during hyperglycemia––still need to be studied in greater detail, but the prevailing theory seems to be that hyperopia might result from intraocular alternations of the lens that change its thickness and hence its refractive index. A thorough review of the literature suggests that is it more likely that hyperopia rather than myopia occurs in cases of uncontrolled diabetes. Greater understanding of the predisposing factors and mechanisms would improve our ability to properly manage these cases. Patients may require frequent changes of spectacles in the presence of persistently high hyperglycemia. Consequently, optometrists are advised to delay the prescription of new glasses as long as possible until stabilization of refraction (and glucose levels) is noted; potential benchmarks of stabilization to consider are an HbA1C below 7.5% and casual in-office blood glucose of less than 180mg/dl. We must also educate our patients about the causal relationship between poor blood glucose control and the risk of severe retinopathy as well as significant vision loss.
_
Can Myopia delay Diabetic Retinopathy (DR)?
High myopia is associated with progressive elongation of the globe, resulting in a variety of fundus changes that lead to visual impairment, including lacquer cracks in Bruch’s membrane, choroidal neovascularization and chorioretinal atrophy. Increased axial elongation in myopes may also lead to mechanical stretching and thinning of the choroid and retinal pigment epithelium, resulting in posterior staphyloma. Myopic refractive error and longer axial length are associated with narrower retinal arterioles and venules, less tortuous arterioles and increased branching coefficients in both arterioles and venules. This reduces retinal blood flow and, as a result, can potentially decrease the risk of DR development. Complete posterior vitreous detachment (CPVD) was more frequently noted in myopic eyes and this finding was associated with reduced progression of neovascularization. There are some clinic- and population-based studies showing that myopia—especially higher myopia—has a protective effect against DR. Both of the population-based studies, the Wisconsin Epidemiologic Study of Diabetic Retinopathy (WESDR) and Singapore Malay Eye Study (SiMES), suggested that high myopia reduces the progression of DR. Even though high myopia may be associated with an increased risk of ocular complications, it can act as a protective factor that forestalls proliferative DR.
_
Keratoconus:
Keratoconus, or “conical cornea” (from kerato- cornea and conus cone), is a degenerative non-inflammatory disorder of the eye in which the cornea thins and changes shape to become more conical than its normal parabolic curve.
•Keratoconus can cause the vision to become distorted quite badly, with multiple images, streaking and sensitivity to light, all often reported.
•Keratoconus is an unpredictable and as yet incompletely understood disease, and the course of its progression following diagnosis is uncertain.
•The associated deterioration in vision, if in both eyes, can affect the person’s ability to, for example, legally drive a car. It does not however lead to blindness.
•Further progression of the disease may lead to a need for surgery. There is no known cure for keratoconus, nor can its natural progression be significantly arrested, but it can be successfully managed with little or no impairment to the quality of life.
•With current methods using contact lens or intra corneal ring segments, only refractive error can be corrected, but it has little effect on the progression of keratoconus. To strengthen the weakened cornea, Corneal Collagen Cross linking is done which causes regression of the disease.
________
________
Uncorrected refractive error (URE), refractive error blindness and amblyopia:
Global estimates indicate that more than 2.3 billion people in the world suffer from poor vision due to refractive error (RE). REs are the most common forms of eye disorders that result in poor vision and have severe social and economic implications if uncorrected. A RE can simply be diagnosed, measured, and corrected with the aid of optical corrective approaches and devices such as spectacles and contact lenses or by refractive surgical procedures. Despite this, an estimated 670 million people worldwide do not have spectacles or have inadequate correction; 517 million have near vision impairment and 153 million have distance vision impairment. Of the 517 million people without spectacles for near vision correction, 410 million are prevented from performing near vision tasks and activities. Current data suggests that more than 90% of people with uncorrected RE, worldwide, reside in rural and low-income countries. The global initiative to eliminate avoidable blindness by the year 2020 (VISION 2020: the Right to Sight) has included RE as one of its five priority eye diseases, following epidemiological studies that have highlighted the escalating estimates of RE prevalence. Previous World Health Organization (WHO) categories of visual impairment refer to best corrected visual acuity in the better eye rather than presenting visual acuity. However, the establishment of the WHO Refractive Error Working Group, the inclusion on the task force of VISION 2020 of national and international NonGovernmental Development Organizations (NGDOs) and professional bodies focusing on REs, and a series of population-based studies on RE in children, has catapulted RE interventions to the center stage of blindness prevention. Resnikoff et al. in 2004 reviewed a series of published and unpublished surveys on uncorrected REs. While in the past the emphasis in the presentation of RE data was on best corrected vision, Resnikoff et al. addressed the category of presenting vision. The latter has been found to be a more accurate indicator of the relevance and challenge of RE as a global public health problem and can thus accurately quantify the need for services.
_
_
WHO revealed the magnitude of the problem on World Sight Day, October 12, 2006, when it released its findings about the prevalence of uncorrected refractive error: 153 million people are either blind or visually impaired due to uncorrected distance refractive error. The World Health Organization estimates that 153 million people have vision worse than 20/60 due to uncorrected refractive error, with the burden of disease greatest in developing countries. Globally, uncorrected refractive error accounts for 42% of persons with visual impairment worse than 20/60 and 18% of persons with vision worse than 20/400, making it the leading cause of visual impairment and second leading cause of blindness. The global burden of refractive error increases when presbyopia is taken into account. An estimated 1.04 billion people are estimated to have presbyopia, and nearly half of these do not wear presbyopic correction. Uncorrected presbyopia causes visual impairment for 410 million people worldwide, with the vast majority of cases (94%) occurring in developing countries. These results reveal the enormity of the problem. This common form of visual impairment can no longer be ignored as a target for urgent action. Adding the number of people who are blind and visually impaired due to uncorrected refractive error to those blind and visually impaired due to eye disease has virtually doubled the figures for the global burden of blindness and visual impairment. Those with presbyopia who cannot get access to spectacles may number over 500 million people.
_
Recent data suggest that a large number of people are blind in different parts of the world due to high refractive error because they are not using appropriate refractive correction. Refractive error as a cause of blindness has been recognized only recently with the increasing use of presenting visual acuity for defining blindness. Refractive error as a cause of blindness has not received much attention because many definitions of blindness have been based on best-corrected distance visual acuity, including the definition used in the International Statistical Classification of Diseases and Related Health Problems. However, in many parts of the world refractive error would become the second largest cause of treatable blindness after cataract if blindness were defined on the basis of presenting distance visual acuity. Refractive error is also one of the most common causes of visual impairment. In addition to blindness due to naturally occurring high refractive error, inadequate refractive correction of aphakia after cataract surgery is also a significant cause of blindness in developing countries. Blindness due to refractive error in any population suggests that eye care services in general in that population are inadequate since treatment of refractive error is perhaps the simplest and most effective form of eye care.
_
Visual impairment:
To assess the extent of visual impairment caused by uncorrected refractive errors, estimates need to be based on “presenting” vision, i.e. visual acuity obtained with currently available refractive correction, if any. Thus, presenting vision, as opposed to best-corrected vision, provides the prevalence of visual impairment that could be improved simply by appropriate corrective refraction. Basing the definition of visual impairment on presenting vision extends the current definition to one that characterizes visual impairment faced by people in day-to-day activities. Presenting vision is defined by the visual acuity in the better eye using currently available refractive correction, if any (i.e. person wearing his spectacles/contacts if any). Best-corrected vision is the visual acuity in the better eye achieved by subjects tested with pinhole or refraction (person given best refractive correction by eye doctor). Visual impairment caused by uncorrected or inadequately corrected refractive errors is defined as visual acuity of less than 6/18 (20/60) in the better eye that could be improved to equal to or better than 6/18 by refraction or pinhole.
_
_
Blindness:
Blindness is defined either in terms of best-corrected distance visual acuity (the most appropriate refractive correction) or presenting distance visual acuity (the individual’s current refractive correction) in the better eye. The latter definition permits assessment of blindness due to refractive error, whereas the former does not. An individual may qualify as ‘not blind’ because their vision improves with refractive correction. However, in their daily living, their vision may be poor enough, due to uncorrected or under-corrected refractive error, that they qualify as ‘blind’ when measured according to their presenting visual acuity. Best-corrected visual acuity excludes uncorrected refractive error as a cause of visual impairment, leading to substantial underestimation of the total visual impairment burden by about 38%. Although a large amount of data are available on the prevalence of blindness in different parts of the world, data on the prevalence of blindness due to refractive error are not readily available because the presenting distance visual acuity definition is not always used. Also of importance in the definition of blindness is the level of visual acuity that is applied. Visual acuity levels of <3/60 or <6/60 in the better eye have been commonly used to define blindness in different parts of world. WHO defines blindness as visual acuity <3/60 in a better eye. Visual acuity levels <6/60 (20/200) have been used to define blindness, for example in the USA. The cut-off level of visual impairment to define blindness in the International Statistical Classification of Diseases is visual acuity less than 3/60 in the better eye, but with increasing human development the visual acuity requirements are also increasing, suggesting that a level less than 6/60 be used to define blindness.
_
Blindness: Presenting distance vision worse than 6/60 (20/200) in the better eye
Low vision: Presenting distance vision worse than 6/18 (20/60), but at least 6/60, in the better eye
Vision impairment: Presenting distance vision worse than 6/18 in the better eye (being the combination of low vision and blindness)
_
What does “Legally Blind” mean?
Legal blindness is defined in 2 ways.
First, if the vision in the better eye is 20/200 (6/60) or less with corrective lenses (glasses or contacts), the person is considered legally blind. Second, someone whose peripheral vision is reduced to 20 degrees or less in the better eye is also considered to be legally blind. (A person with normal peripheral vision has 140 degrees or greater of peripheral vision.)
_
Refractive error blindness:
Even though the treatment of refractive error is simple and successful, the condition is still responsible for a significant amount of blindness in both developing and developed countries. Refractive error is also one of the leading causes of visual impairment in different parts of the world. The burden of blindness due to refractive error, in terms of blind-person-years, is even more significant than the numbers indicate since refractive error blindness mostly starts at a young age and probably causes significant economic and social burden to societies. Recent data from India suggest that, in terms of blind-person-years among the individuals who are blind currently, the burden on society due to refractive error blindness is about twice that due to cataract blindness.
_
Refractive error blindness prevalence:
With blindness defined as a presenting distance visual acuity <3/60 in the better eye, the prevalence of blindness due to refractive error has been reported to be as high as 0.20% in Pakistan and India, for all age groups in the population considered together. If blindness is defined as presenting distance visual acuity <6/60 in the better eye, the prevalence of blindness due to refractive error in an Indian population was reported to be 0.36%, including 0.06% from amblyopia resulting from high uncorrected refractive error. These data suggest that about 1 of every 280 people in the study population were blind from uncorrected or inadequately corrected refractive error or from refractive error-related amblyopia. A high prevalence of refractive error blindness (0.59%) was found among a population of Chinese over-50-years using the definition of presenting distance visual acuity <6/60 in the better eye. With this definition, the prevalence of blindness due to refractive error among those aged >40 years in an Indian study population was reported to be quite high (1.06%). With blindness defined as a presenting visual acuity <6/60 in the better eye, the prevalence of refractive error blindness in the USA among individuals aged >40 years has been reported to 0.33% among Blacks and 0.24% among Whites. It must be kept in mind, however, that if only older age groups are considered, the prevalence of refractive error blindness is likely to be higher because of cumulative effects, than that for all age groups taken together. The available data suggest that in India and China blindness due to natural refractive error is more common than that due to aphakia, whereas blindness due to aphakia is more common in some African countries. Studies carried out in schools for the blind have also reported blindness due to refractive error. For example, uncorrected myopia and aphakia were responsible for 3% of the blindness among blind-school children in Zimbabwe, while uncorrected aphakia and amblyopia were responsible for 5.1% of the blindness among blind-school children in India. Although data on refractive error blindness have only recently started to become available, evidence suggests that blindness due to uncorrected or undercorrected high refractive error is a significant problem in developing and developed countries alike. Recent data suggest that there has been an increase in the prevalence of myopia in some parts of the world over the past few decades. The reasons for this are not clear but this trend could result in a higher prevalence of high myopia which, if not adequately corrected, could result in an increase in the number of people who are blind due to refractive error.
_
Global Vision Impairment and Blindness due to Uncorrected Refractive Error:
A Systematic Review and Meta-Analysis – 2014:
Based on the Global Burden of Disease Study 2010 and ongoing literature research, authors examined how many people were affected by moderate and severe vision impairment (MSVI; presenting visual acuity <6/18, ≥3/60) and blindness (presenting visual acuity <3/60) due to uncorrected refractive error. In 2010, uncorrected refractive error was the leading cause of vision impairment and the second leading cause of blindness worldwide, affecting a total of 108 million people. Uncorrected refractive error ranks as one of the leading public health challenges in eye care.
_
The Evolution of Uncorrected Refractive Error as a Major Public Health Issue:
Uncorrected refractive error has only recently (2006) been formally recognised as a significant cause of blindness and the major cause of impaired vision in the world. It is now known that over 625 million people have uncorrected refractive error (for distance and near vision), simply because of a lack of an eye examination and appropriate spectacles. Accumulating evidence indicates that myopic macular degeneration (MMD) is a major cause of vision impairment and blindness – but this contribution of MMD to blindness prevalence is yet to be recognized by the World Health Organization (WHO) and national research bodies such as the US National Eye Institute (NEI). In 2010, there were an estimated 1.7 billion myopes worldwide – predicted to increase to around 2.2 billion by 2020 – with a small but significant percentage of those affected likely to progress to high myopia. High myopia significantly increases the risk of blinding conditions such as MMD, glaucoma and cataract and in some population amblyopia.
_
The figure below shows correlation between myopia prevalence and prevalence of URE:
_
Impact of refractive error blindness:
Blindness due to uncorrected or inadequately corrected natural refractive error starts at a younger age than cataract, which manifests itself in old age. If the impact of blindness due to refractive error is considered in terms of blind-person-years, a person becoming blind due to refractive error at a young age, and which is not corrected, would suffer many more years of blindness than a person becoming blind from cataract in old age and would place a greater socioeconomic burden on society. In the Indian state of Andhra Pradesh, among the individuals who are blind currently, the total number of blind-person-years suffered over their lifetime by those blind due to refractive error was estimated to be about twice that suffered by those blind due to cataract. Blindness due to natural refractive error can hinder education, personality development, and career opportunities, in addition to causing an economic burden on society. Visual impairment from uncorrected refractive errors can have immediate and long-term consequences in children and adults, such as lost educational and employment opportunities, lost economic gain for individuals, families and societies, and impaired quality of life. Uncorrected refractive errors can hamper performance at school, reduce employability and productivity, and generally impair quality of life. Yet the correction of refractive errors with appropriate spectacles is among the most cost-effective interventions in eye health care. The impact of blindness from myopia may be different from that from hyperopia, since those blind due to myopia are likely to have better near vision than those who are so due to hyperopia. Though there are no data available on the economic loss as a result of blindness due to natural refractive errors, it would not be unreasonable to assume that it is probably significant since a large proportion of those affected are in the economically productive age group. However, this burden of economic loss may vary with the type of refractive error. Since aphakia is a cause of blindness among older age groups, the economic loss associated with it is likely to be less than that associated with blindness due to myopia and hyperopia.
_
Reasons why refractive errors remain uncorrected:
Various factors are responsible for refractive errors remaining uncorrected: lack of awareness and recognition of the problem at personal and family level, as well as at community and public health level; lack of screening; non-availability of and/or inability to afford refractive services for testing; insufficient provision of affordable corrective lenses; and cultural disincentives to compliance.
______
Amblyopia:
Amblyopia is a Greek word, which means “dullness of vision”. In ophthalmology, it defines as reduced visual acuity that could not be explained by the effect of any abnormality in the eye. Amblyopia is a decrease in the child’s vision that can happen even when there is no problem with the structure of the eye. The decrease in vision results when one or both eyes send a blurry image to the brain. The brain then “learns” to only see blurry with that eye, even when glasses are used. Only children can get amblyopia. If it is not treated, it can cause permanent loss of vision. Amblyopia is the most common reason of unilateral visual impairment in children and juvenile, which is most often detected through routine vision screening programs. There are 3 main causes of early visual impairment, which lead to amblyopia including strabismus, anisometropia or high bilateral refractive errors (isometropia) and visual deprivation. Amblyopia is a developmental problem in the brain, not any intrinsic, organic neurological problem in the eyeball (although organic problems can lead to amblyopia which can continue to exist after the organic problem has resolved by medical intervention). The part of the brain receiving images from the affected eye is not stimulated properly and does not develop to its full visual potential. This has been confirmed by direct brain examination. David H. Hubel and Torsten Wiesel won the Nobel Prize in Physiology or Medicine in 1981 for their work in showing the extent of the damage to ocular dominance columns produced in kittens by sufficient visual deprivation during the so-called “critical period.” The maximum “critical period” in humans is from birth to two years old.
_
Anisometropia:
Anisometropia is the most common reason of amblyopia, which occurs due to uncorrected asymmetrical refractive error between the two eyes. Uncorrected anisometropia induces blurry image in one eye and unusual binocular interaction by producing different images on the fovea. Normal appearance of anisometropic child and good visual performance of dominant eye delay the diagnosis of amblyopia. The level of anisometropia, which leads to amblyopia, has been studied in different literature. In conclusion, anisohyperopia of more than 1 diopter, anisomyopia of more than 2 diopters and anisoastigmatism of more than 1.5 diopter may produce amblyopia. The amount of anisometropia has a direct connection with the severity of amblyopia .Successful visual outcome with traditional amblyopia therapy for anisometropia of more than 4 diopter has been reported.
_
Treatment of amblyopia:
The treatment of anisometropic amblyopia includes correction of the refractive errors by spectacles or contact lenses with patching of the dominant eye.
Spectacles:
Even today, spectacles are the most common treatment for anisometropic amblyopia. However, it has limitations in full optical correction of high anisometropic refractive errors. Anisokonia means dissimilar image size. Aniseikonia of more than 5% to 6% (typically present with 3 or more diopters of anisometropia) cannot be well tolerated. While performing the patching therapy, children can tolerate spectacles. However, once the patching is finished, the great aniseikonia occurs and the child cannot tolerate spectacle with full dioptric correction in their binocular state. Furthermore, in eccentric gazes, thick lenses can induce prismatic effects. Both of these reasons create binocular image unfused and disrupt binocular fusion. Anisometropic glasses of more than 2 to 3 diopters are also cosmetically problematic when corrected by spectacle due to different magnification of the hyperopic lens or minification effect of the myopic lens.
Contact lenses:
Alternate treatment for anisometropic amblyopia is the use of contact lenses. Contact lenses eliminate all disadvantages of spectacles with better quality of vision and contrast sensitivity. In spite of these benefits, contact lenses have some disadvantages such as the difficulty of insertion and removing, being time-consuming for parents, risk of microbial keratitis and comparatively high expenses. Because children are usually disregarded to hygiene, they are at higher risk of infections than adults who use contact lenses.
Occlusion, penalization:
Even though it is a common need to correct the anisometropic amblyopia, but further amblyopia treatment is regularly necessary. This extra treatment contains occlusion therapy, optical or pharmacologic penalization with cycloplegic agents or the combination of these procedures are used in children in whom the correction of refractive error cannot improve visual acuity. Most of the time occlusion therapy does not associated with any complaint. Atropine penalization has some disadvantages containing photosensitivity and anticholinergic effect. In comparison, optical penalization that utilizes a lens to blur visual acuity in the dominant eye is an accepted method. Considerable psychosocial pressure connected to amblyopia therapy has been reported by these children and their parents during the treatment period. Even in adults that have a history of amblyopia treatment in early years, psychosocial difficulties related to the previous amblyopia therapy were reported that have negatively affected behavior in places such as work, school and other social relations.
Eyepatch:
An eyepatch or eye pad is a small patch that is worn in front of one eye. It may be a cloth patch attached around the head by an elastic band or by a string, an adhesive bandage, or a plastic device which is clipped to a pair of glasses. It is often worn by people to cover a lost or injured eye, but it also has a therapeutic use in children for the treatment of amblyopia. Eye patching is used in the orthoptic management of children at risk of lazy eye (amblyopia), especially strabismic or anisometropic amblyopia. These conditions can cause visual suppression of areas of the dissimilar images by the brain such as to avoid diplopia, resulting in a loss of visual acuity in the suppressed eye and in extreme cases in blindness in an otherwise functional eye. Patching the good eye forces the amblyopic eye to function, thereby causing vision in that eye to be retained. A study provided evidence that children treated for amblyopia with eye patching had lower self-perception of social acceptance. It has been pointed out that the penalization of one eye by means of patching or atropine drops does not provide the conditions that are necessary in order to develop or improve binocular vision. Recently, efforts have been made to propose alternative treatments of amblyopia that do allow for the improvement of binocular sight, for example using binasal occlusion or partially frosted spectacles in place of any eye patch, using alternating occlusion goggles or using methods of perceptual learning based on video games or virtual reality games for enhancing binocular vision.
Neutral Density Filter:
A recent study by PEDIG analyzed the efficacy of Bangerter filters for the treatment of moderate amblyopia as compared to part-time patching. The authors found that after 24 weeks of treatment, the mean visual acuity improvement in the patching group was only half a line better than the Bangerter filter group. The study also included a questionnaire to assess the negative impact of each treatment modality. They found that the Bangerter filter was a less disruptive treatment option for both the child and family. The authors concluded that the Bangerter filter is effective for treating moderate amblyopia and may be a useful alternative for patients with poor patching compliance. It is important to mention that patients with minimal refractive error in their non-amblyopic eye will likely look over their glasses. These patients will likely not respond as well to Bangerter filter treatment.
Refractive surgery:
Refractive surgery is a reasonable option in the treatment of children with refractive anisometropic amblyopia, especially in patients who cannot tolerate spectacle or contact lenses. Both laser in situ keratomileusis (LASIK) and photorefractive keratectomy (PRK) have been well established in adults for correction of refractive errors. Refractive surgery through excimer laser has been useful in children as well as in particular cases with amblyopia due to high myopic anisometropia. Refractive methods that may be useful in children are PRK, LASIK and laser epithelial keratomileusis (LASEK). PRK and LASIK have been the most widely studied among the excimer laser procedures. Most of the ophthalmologists have suggested LASIK and PRK for children younger than two years old.
_
The other experimental method that treats amblyopia in adults and children is the use of medication for example levodopa, carbidopa and citicoline that can enhance dopaminergic neurotransmission in the brain. These methods can improve visual acuity mildly but unfortunately, the improvement was not persistent after the discontinuing of the medication.
_
Refractive-error-related amblyopia:
It is generally believed that blindness due to refractive-error-related amblyopia is not a significant problem. However, recent data from India suggest that this needs to be reconsidered. For example, in a population-based study in the Indian state of Andhra Pradesh, 0.06% of the population was blind due to refractive-error-related amblyopia. These data suggest that in the study population, 20% of those who had a high enough refractive error to be blind had developed dense amblyopia resulting in irreversible blindness. Blindness due to amblyopia resulting from uncorrected high refractive error may therefore not be insignificant, at least in some populations. Refractive amblyopia occurs before the age of cortical visual maturity.
_______
_______
Refractive error and learning in school:
The child’s vision is essential to his success in school. When his vision suffers, chances are his schoolwork does too. Vision problems are common among school-age kids. According to Prevent Blindness America, one in four school-age children have vision problems that, if left untreated, can affect learning ability, personality and adjustment in school. School-age children also spend a lot of time in recreational activities that require good vision. After-school team sports or playing in the backyard aren’t as fun if you can’t see well. Low vision is characterized reduced ability to perform many daily activities, such as recognizing people in the street, reading blackboards, writing at the same speed as peers, and playing with friends.
_
Refractive error and quality of life:
If visual impairment is left untreated, there is a greater risk of functional decline, social isolation, falls, hip fractures, accidents, and mortality. Refractive error reduces vision-related quality of life. In a British study, persons with myopia of 10.00 D or more had significantly worse vision-related quality of life compared with persons with less severe myopia. An Australian study found that individuals with myopia of 0.50 D or more reported worse vision-related quality of life measures compared with emmetropes. In a European study, more than half of pseudophakic patients who wore eyeglasses after cataract surgery would be willing to pay more than €0.50 per day to be free from wearing eyeglasses. Vision-related quality of life has been assessed for several refractive error treatments. In one study, contact lens wearers had a higher vision-related quality of life than eyeglass wearers. Patients undergoing refractive surgery are generally pleased with their decision, and a systematic review estimated that 95% of patients undergoing LASIK were satisfied with their outcome.
_
Without appropriate optical correction, millions of children are losing educational opportunities and adults are excluded from productive working lives, with severe economic and social consequences. Individuals and families are frequently pushed into a cycle of deepening poverty because of their inability to see well.
_
Refractive error and personality:
Studies of the relationships of personality style and ametropia have suffered from some basic problems and disagreement. The different researchers have all used many different personality probes that are not necessarily equal. Additionally, the tests may not have been looking at the attributes that clinicians associate with the various ametropias. What are the attributes associated with myopia? Myopes seem to have a profile that makes them: worry, depress, fear and they are lent to withdrawn-ness, a sedentary lifestyle, a detailed analytical nature, and a higher degree of desire for inter-personal relations. Angi and Rupelo described their myopic population as “sufferers”. What are the attributes associated with hyperopia? The candidates for adverse hyperopia are more likely to be: assertive, alarmable and hot-reacting; action-oriented; global analytical approach. These and a higher degree of goal, problem and task-orientedness would seem to predispose one for progressive hyperopia. There are individuals who mix these: they will do the opposite of one or the other, but statistics should prove an association of the above factors, generally speaking. The problem is to get personality inventories that are accurate in measuring the qualities being looked for. Researchers before Van Alphen’s seminal paper – and since – have asserted a relationship between anxiety and myopia. Just how to sort out what kind of, and how much, anxiety is required to trip the pre-myope into the active distortion is the problem before researchers now.
_
_______
_______
Refractive error and intelligence:
There is a widely held perception amongst many researchers and the community that, generally, myopes tend to have superior intelligence quotients (IQs) than emmetropes. The link between myopia and high intelligence has been independently investigated by a number of studies performed in countries as diverse as Singapore, Israel, the United States, the Czech Republic and New Zealand. While the first study conducted on this subject was performed in 1955 by Young, it was not until 1958 that Nadell and Hirsch demonstrated a strong positive correlation between these two factors. The results of all major studies undertaken since Young’s initial study are summarised in Table below.
_
Summary of study results linking myopia and high intelligence.
| Study | Country | Number of subjects |
Age (years) | Range of myopia | Intelligence test performed | IQ | Test/school results |
Significance level |
|
|
||||||||
| Young 1955 | USA | 633 | 6–17 | Not specified | Stanford-Binet | Average | N/A | < 0.001 CC = −0.19 |
|
|
||||||||
| Nadell and Hirsch 1958 | USA | 414 | 14–18 | Not specified | CTMM | Higher | N/A | > 0.1 |
|
|
||||||||
| Hirsch 1959 | USA | 554 | 6–17 | Not specified | Stanford-Binet CTMM |
Higher | N/A | < 0.001 |
|
|
||||||||
| Young 1963 | USA | 251 | 5–17 | Not specified | Stanford-Binet CTMM |
Average | Higher | CC = −0.11/0.10 CC = −0.17/0.21 |
|
|
||||||||
| Grosvenor 1970 | New Zealand | 707 | 11–13 | ≥−1.00 D | Otis Test | Higher | Higher | > 0.05 (versus emmetropes) < 0.05 (versus hyperopes) |
|
|
||||||||
| Karlsson 1976 | USA | 2527 | 17-18 | Not specified | Lorge-Thorndike IQ Test CTMM |
Higher | Higher | < 0.001 |
|
|
||||||||
| C. P. Benbow and R. M. Benbow 1984 | USA | 416 | 13 | Not specified | Scholastic Aptitude Test | Higher | Higher | < 0.05 |
|
|
||||||||
| Rosner and Belkin 1987 | Israel | 157 748 | 17–19 | ≤6/7.5 VA | Verbal Otis Test, Raven Matrix Test | Higher | Higher | Strongly positive association |
|
|
||||||||
| Williams et al., 1988 | New Zealand | 537 | 7–11 | ≥−0.5 D | WISC-R IQ Test Burt Word Reading Test |
Higher | Higher | < 0.05 |
|
|
||||||||
| Teasdale et al., 1988 | Denmark | 15 834 | 18 | ≥−0.25 D to ≤−7.5 D | Group IQ Scores Educational levels |
Higher | Higher | < 0.001 |
|
|
||||||||
| Dolezalova and Mottlova 1995 | Czech Republic | 225 | 14–18 | Unknown | School test scores | Higher | Higher | Unknown |
|
|
||||||||
| Saw et al., 2004 | Singapore | 1204 | 10–12 | ≥−0.5 D | Raven Matrix Test | Higher | N/A | < 0.05 |
|
|
||||||||
| Saw et al., 2006 | Singapore | 994 | 7–9 | ≥−0.5 D | Raven Matrix Test | Higher | Higher | < 0.05 |
|
|
||||||||
| Dirani et al., 2010 | Singapore | 1143 | 9-10 | ≥−0.5 D | Raven Matrix Test | Average | Average | > 0.38 (9-year-olds) > 0.27 (10-year-olds) |
|
|
||||||||
| Akrami et al., 2012 | Iran | 137 | 10–14 | ≥−0.5 D | Unspecified school tests | Average | N/A | = 0.465 |
CC: correlation coefficient.
_
A number of studies have shown higher incidence of myopia with the level of education, literacy and the levels of IQ (Intelligence Quotient). This has been attributed to the “near work” or studying/ reading habits of the subjects. The previous observation has been buffeted by a possible converse: Hyperopic children have lesser IQ and fewer scholastic achievements. Regarding IQ there have been several theories: IQ testing is near work and hence lesser strain for the myopes. Conversely, myopes have are more voracious readers and hence have better IQ‟s. Still another theory is that the pleiotropic genes affect the size of the brain and the eyes simultaneously. A study has found that there is no significant association between the number of hours spent reading and the presence of a refractive error (91.3 % of subjects with a refractive error are myopes). This particular finding can be construed to be in concord, at least in part, with two most recent studies that myopia may be associated with higher IQ independent of the number of hours read. Contrary to observation with reading, authors have found an association with of the presence of a refractive error with the average number of hours spent watching television per day. There has been a widespread campaign all over the world to reduce television watching in children, citing the fact that fifty years ago myopia was hardly seen and now about 1.6 billion people world over suffer with this affliction – a trend that is concurrent with the rise of the television, initially, and the computer, later on, to be pervasive domestically.
_
In 1959 Hirsch examined four hypotheses concerning the relationship between intelligence test scores and refractive errors:
1. According to the first hypothesis myopia is an overdevelopment of the eye just as hyperopia is an underdevelopment, and ocular and cerebral development are related.
2. A second hypothesis assumes that intelligence test scores may be influenced by the amount of reading which a child does. The myopic child, better adapted for reading than for playing games, might do more reading and, hence, obtain a better intelligence test score: the hyperopic child, on the other hand, handicapped to some degree in reading, might read less, and, hence, make a lower score.
3. According to the third hypothesis the intelligence rather than refraction might determine the amount of reading done. The more intelligent child may read more, and thus become more myopic. The less intelligent child, on the other hand, might read less and, hence, avoid becoming myopic.
4. A fourth hypothesis implies that the hyperopic child, maintaining accommodation with difficulty, is certainly at a disadvantage, just as the myopic child, requiring little or no accommodation, will be ideally situated to perform well in this test situation. In taking the test, a premium is placed upon the ability to perceive fine detail efficiently, thus giving the myope an advantage.
Hirsch concluded that the fourth hypothesis, which was supported by his own data, seemed the most probable. In a later period Young rejected the idea that there was a relationship between refractive state and intelligence, but favored the idea of a relationship between reading ability and intelligence.
_
From time to time, reports are published showing that myopes score higher than nonmyopes on intelligence tests and concluding that myopes are thus more intelligent than the rest of the population. These researchers usually go on to say that this proves that myopia is inherited since intelligence is largely inherited. They have even gone so far as to claim that the gene that lengthens the eyeball also stimulates the brain. Such a statement is indicative of the length to which some people will go to justify their claim that myopia is inherited. If those people who inherit a high intelligence also inherit myopia along with it, then it should be possible to select the most intelligent individuals from a group of primitive illiterates and find considerable myopia in these individuals. The fact is that in illiterate societies almost no one is myopic. Where then is this inherited myopia? It obviously does not exist. These researchers seem to be totally ignorant of the numerous studies which have shown repeatedly that myopes score higher than nonmyopes on intelligence tests because of their better reading ability and not because they are gifted with higher intelligence. Several papers on this subject have been written by Francis A. Young, former Director of the Primate Research Center at Washington State University.
_
Use-Abuse theory:
As the “use-abuse theory” states that many aspects of our modern environment involve near work, which strains our eyes. Examples include reading and looking at pixelated screens of computers and phones for long periods of time. A majority of people in the developed world spend most, if not all, of their days doing tasks defined as “close work”, steadily building up a pressure in the eye, as the ciliary fibers that focus the eye are constantly contracting in an effort to follow words on a page. This is especially exacerbated in children whose eyes are still developing; their eyes may grow permanently elongated and myopic. This hypothesis helps elucidate why some associations between myopia, intelligence, and education were made in some studies in the 20th century. People who have more access to education likely read much more and likely score higher on intelligence tests, therefore creating a spurious association between intelligence and myopia. This spurious association further explains the social and geographical patterns and trends in rates of myopia worldwide. Some trends include Africans and people of African descent having lower rates of myopia while Asians and people of Jewish descent have higher rates of myopia, perhaps due to differential education opportunities.
_
Wearing glass to appear learned:
Many studies have also shown that people who wear glasses appear more intelligent to others – and are more likely to find work. A survey by the British College of Optometrists found that one third of Brits thought glasses made someone look more professional and 43 per cent believed they made people look more intelligent. NYMag even reported back in 2011 that defence lawyers in the US were telling their clients to wear glasses in court because they’d appear ‘less menacing’ and more trustworthy in court. Lawyer Harvey Slovis said: ‘I’ve tried cases where there’s been a tremendous amount of evidence, but my client wore glasses and got acquitted.’ So, to conclude, people who wear glasses are officially more learned than those who don’t. And, even if you don’t need to wear them, if you’ve got a crucial job interview or court appearance, a nice pair of frames might make all the difference.
_______
_______
Refractive error, eyeglasses and social stigma:
Facial distortion and social stigma:
Eyeglasses for a high-diopter nearsighted or farsighted person cause a visible distortion of their face as seen by other people, in the apparent size of the eyes and facial features visible through the eyeglasses.
•For extreme nearsightedness the eyes appear small and sunken into the face, and the sides of the skull can be visible through the lens. This gives the wearer the appearance of having a very large or fat head in contrast with their eyes.
•For extreme farsightedness the eyes appear very large on the face, making the wearer’s head seem too small.
Either situation can result in social stigma for children and adults, due to the effect of these facial distortions on others’ perception of their attractiveness. Contact lenses are sometimes preferred because they do not present these distortions. Aspheric/atoric eyeglass design can also reduce minification and magnification of the eye for observers at some angles.
_
Tweens and Teens perceive eyeglasses as socially unacceptable:
Who are tweens? According to Wikipedia, they are youths, usually between the ages of 8 and 12. These young people go through a transitional phase of self-awareness and discovery, peer pressure and social acceptance as they develop their independence and interact with others. At that stage, adding eyeglasses with their associated social stigma can be an overwhelming experience. Alternatively, adjunct contact lenses can provide tweens with additional benefits beyond simple vision correction for refractive errors. A literature overview by the Faculty of Social and Behavioral Sciences at the University of Amsterdam showed that wearing eyeglasses negatively impacted how children felt about their physical appearance because of negative stereotyping by peers. In a study of 585 tweens and teens, eyeglasses were also perceived as socially unacceptable, while contact lenses were the preferred ‘eye correction choice’ for school, sports activities and hanging out with friends. When should practitioners start introducing contact lenses to tweens? In the Children & Contact Lenses study conducted by the American Optometric Association, more than half (51 per cent) of 576 optometrists surveyed felt that 10 to 12 years of age was appropriate, while 12 per cent felt that ages eight to nine were suitable. Among tweens, emotional and social behaviour varies, so the question of when they should start wearing contact lenses is often not a matter of age. Rather, factors such as interest, motivation, hygiene, maturity and sense of responsibility in adhering to the care and wearing schedule will determine a tween’s suitability and probability of success. The three-year multi-site Adolescent and Child Health Initiative to Encourage Vision Empowerment (ACHIEVE) Study from the Ohio State University College of Optometry revealed that myopic contact lens-wearing tweens felt significantly better about their physical appearance, social acceptance and athletic abilities than did tweens who wore eyeglasses. They also felt more confident about their academic performance if they initially disliked their eyeglasses. A follow-up study concluded that tweens over the age of 10 who played sports, those who were motivated to wear contacts, and those who disliked wearing eyeglasses were the best candidates for contact lens wear. But can tweens handle contact lens care and wear once they pass the initial screening process? Several studies have supported the belief that tweens as young as eight are able to insert, remove and independently care for and wear contact lenses successfully. Similarly, the Contact Lenses In Pediatrics (CLIP) study of 84 tweens and 85 teens (13 to 17) showed that tweens were as compliant with contact lens care and wear instructions as teens.
__
The figure below shows reasons for not wearing eyeglasses despite low vision:
_
Girls are particularly vulnerable to social and psychological distress vis-à-vis eyeglasses:
A study revealed that a large percentage of respondents (35%) were teased for using glasses. It was generally the peers who had a negative attitude and even the victimized children with refractive errors who were using spectacles. 3% even faced extreme rejection in the form of being declined for marriage, only because they wore glasses and 31% respondents were ready to hide their glasses to avoid rejection before marriage. An attitude like this could result in serious problems like psychosocial maladjustment, anxiety, depressive feelings, loneliness, lowered self-esteem and behavioural problems. 52% of the respondents considered spectacles to be a cosmetic blemish especially the females (56.6%). A study which was conducted in Pakistan too demonstrated this fact. The main reason for the discontinuation of spectacle wear in women was given as community pressure and cosmetic factors. These women reported that they had to face social pressure often, not only in terms of appearance but also because of the perception that their children could inherit their visual impairment. In another study, 10.5% respondents were ashamed or embarrassed by their spectacles. 27% felt that only intelligent people used spectacles. This brought to light the need to change their perspective towards the use of spectacles through the proper dissemination of knowledge and information. 14% of the respondents in our study said that they would refuse to marry a person who had a refractive error. This was despite them having a good educational background and awareness regarding various cosmetically acceptable options. This brings to light the deep rooted stigma which is associated with refractive errors and with spectacles which are used in their correction. This is a paradox considering the high literacy level and also the increased awareness of the option of refractive surgeries in our study.
_
_
Ignorance about eyeglasses:
The most common misconception in our society is that wearing glasses means you have defective eyes. The truth is if you can see properly after wearing glasses, you have good eyes. A study demonstrated well known fact about stigmas attached with spectacles uses. Among various obstacles in the use of spectacles for refractive error, important ones were the belief that continuous use of glasses would progressively increase severity of refractive error, spectacles use can harm the eyes, difficulty in doing manual work and it prevents normalization of eyes. Similar results were obtained in others, Indian and international studies. In south India study conducted by Sheetal Savor et al highlighted similar stigmas. In study among secondary school students in Tanzania parental concern about the safety of spectacles use was evaluated. The spectacle damaging the eye was a significant obstacle to spectacle use in the Nigerian study. In a study which was conducted in Pakistan, 69 per cent of the people thought that using spectacles would cause their vision to deteriorate, they therefore tried to avoid it. In studies on Chinese children, a common reason for not wearing spectacles was the belief that spectacles weakened the eyes.
________
Refractive error in vehicle drivers:
A considerably high number of drivers are in lack of optimal visual acuity. Vision is one of the most important sensory factors in driving accounting for about 95% of all sensory requirements. Other abilities required for driving include mental ability, motor ability and compensatory abilities. One of the most important and frequently used visual function tests is visual acuity. Visual acuity is therefore the most widely used criterion for determining eligibility for driving. Although commercial drivers know that poor vision is related to road traffic accidents (RTAs), only a few had ever had any eye examination. The relationship between visual function (visual acuity, visual field, colour vision etc.) and road traffic accidents (RTAs) have been equivocal. Some studies have found no association between the impairment of visual function and the occurrence of RTAs. Others on the other hand have reported a relationship. Refractive error is a commonly reported ocular morbidity among drivers. It is commonly observed that majority of commercial vehicle drivers with refractive error do not wear the spectacle correction while driving. Consistent with many studies, Ghana study shows that 12.1% of commercial drivers had a visual acuity below the visual acuity requirement for eligibility to drive in Ghana (VA = 6/9). This is comparable to 11.5% commercial inner-city vehicle drivers in Nigeria, 9.1% reported by McMoli and Ogunmekan and 8% reported for Australian drivers. A 2013 Indian study found that out of 140 truck drivers screened, the number of truck drivers with visual acuity 6/6 (normal vision) was 100 (71.43%) while the drivers with refractive errors were 40 (28.57%). Of the 40 truck drivers with refractive errors; 11 were having myopia, 20 hyperopia, and nine were found to have astigmatism. In the entire study, 44 truck drivers were found to have presbyopia. These findings underscore the fact that some commercial drivers who fail to meet the stipulated criteria for eligibility to drive do obtain licenses to drive. Of more significance is that many of those who fail this criteria have moderate to severe visual impairment. The major reported barriers to eyeglass use included ignorance of visual status, not having time to visit the eye clinic, cost of care and fear. For driving, the laws vary by state, but most states require a corrected acuity of 6/12 (20/40) in at least one eye for unrestricted privileges. Patients with a homonymous hemianopia should not drive.
________
Refractive error and economy:
Numerous studies worldwide have affirmed that the prevalence of uncorrected refractive error (RE) is influenced by strong socio-economic factors. Moreover, uncorrected RE, now a public health problem in India and other low- and middle-income countries, may impact the learning abilities of children. The impact of uncorrected REs are 2-fold, as not only do strong socio-economic factors such as poverty and the inability to access treatment influence the correction of a RE, but uncorrected RE can also contribute to the individuals and their families’ socio-economic status. Visually impairing REs have been observed to have extensive social and economic impact, for example, limiting educational and employment opportunities of economically active persons, healthy individuals, and communities. Smith et al. indicated in their article on the global burden of uncorrected RE, that the global economy loses $202 billion annually as a result of lost productivity due to uncorrected RE. To overcome this problem, they suggest that prescribed spectacles should be provided to those with correctable refractive conditions which in turn may result in a net economic gain. A relatively small investment (compared to the cost) of a one-off investment of US$20 billion in human resource development (with an upper estimate of $28 billion) and establishing and providing vision care for 5 years would save the global economy US$202 billion annually.
_
Cost Effectiveness of refractive error treatments:
Each year, over 27 million outpatient visits in the United States are devoted to assessment and treatment of refractive error. Moreover, refractive error accounts for one-third of the $16.24 billion in direct medical costs spent on vision disorders each year in the United States. Worldwide, the burden of uncorrected refractive error has substantial economic repercussions, with conservative analyses estimating a societal cost of $202 billion in lost productivity. A net economic gain would result from treatment of uncorrected refractive error if eyeglasses could be provided to each individual for less than $1000. At the individual level, several cost-effectiveness studies have compared refractive surgery to contact lenses. Although the results depend on the assumptions used in the models, these studies have generally found that refractive surgery has higher up-front costs compared with contact lenses but becomes more cost-effective in the long term. The long-term cost savings for refractive surgery results from fewer doctors’ appointments and fewer prescriptions for contact lenses or eyeglasses. Similarly, toric IOLs were shown to be more cost-effective than conventional IOLs, mostly because toric lenses reduced long-term costs of postoperative contact lenses or eyeglasses. More research on the cost-effectiveness of various treatments for refractive error would be helpful for insurers as well as for clinicians counseling their patients on services not covered by health insurance.
_______
_______
Research in management of refractive error:
_
Training the brain to overcome the effect of aging on the human eye: a 2012 study:
Presbyopia causes near vision to degrade with age, affecting virtually everyone over the age of 50. Presbyopia has multiple negative effects on the quality of vision and the quality of life, due to limitations on daily activities – in particular, reading. In addition presbyopia results in reduced near visual acuity, reduced contrast sensitivity, and slower processing speed. Currently available solutions, such as optical corrections, are not ideal for all daily activities. Here authors show that perceptual learning (repeated practice on a demanding visual task) results in improved visual performance in presbyopes, enabling them to overcome and/or delay some of the disabilities imposed by the aging eye. This improvement was achieved without changing the optical characteristics of the eye. The results suggest that the aging brain retains enough plasticity to overcome the natural biological deterioration with age.
_
Refractive errors and their effects on visual evoked potentials:
Visual evoked potentials (VEPs) reflect electrical phenomena occurring during the visual processing and are a graphic illustration of the cerebral electrical potentials generated by the occipital cortex evoked by a defined visual stimulus. Therefore, VEPs can be used both in research and in clinical practice to elucidate the function of the visual system. It is known that the technical and physiological factors such as pupil diameter, refractive errors (REs), type of stimulus, age and sex, electrode position and anatomical variations may affect VEP. It is assumed that RE cause defocus. Defocusing may affect the VEP, which if allowed to persist, can result in corresponding neurological changes. The RE blur the stimulus and cause defocus, which lead to significant changes in VEP (P100 latency and amplitude) in the presence of RE. As per authors perspective, among the REs, VEPs seem to be more affected by myopia than hyperopia. However, the principal cause in both is the degree of defocusing of the image produced by the RE.
__________
__________
Wavefront approach to refractive errors of eye:
In physics, a wavefront is the locus of points having the same phase: a propagation of a line in 1D, a curve in 2D or a surface for a wave in 3D. A wavefront in optics is a surface over which an optical disturbance has a constant phase. Rays and wavefronts are two mutually complementary approaches to light propagation. Wavefronts are always perpendicular to the rays.
_
Every point source of light emits spherical wavefronts and every point on the wavefront is considered a new point source. The sunlight strikes the earth with a spherical wavefront that has a radius of about 150 million kilometers. For many purposes, such a wavefront can be considered planar. The simplest form of a wavefront is the plane wave, where the rays are parallel to one another. In other words, distant objects emit/reflect plane wavefronts (parallel rays).
_
A lens can be used to change the shape of wavefronts. Here, plane wavefronts become spherical after going through the lens.
_
For light to converge to a perfect point, the wavefront emerging from the optical system must be a perfect sphere centered on the image point. The distance in micrometers between the actual wavefront and the ideal wavefront is the wavefront aberration, which is the standard method of showing the aberrations of the eye. Therefore, aberrations of the eye are the difference between two surfaces: the ideal and the actual wavefront.
_
The figure below shows myopic defocus:
_
_
The myopic defocus seen in the figure above is depicted as wavefront aberration three dimensionally in micrometers:
_
_
Figure below shows pupil size in millimeter and myopic defocus wavefront aberration:
Small pupil would block peripheral wavefronts having greater aberration reducing myopic defocus.
_
Zernike Polynomials:
In mathematics, the Zernike polynomials are a sequence of polynomials that are orthogonal on the unit disk. Named after optical physicist Frits Zernike, winner of the 1953 Nobel Prize in Physics, and the inventor of phase contrast microscopy, they play an important role in beam optics. In optometry and ophthalmology, Zernike polynomials are used to describe aberrations of the cornea or lens from an ideal spherical shape, which result in refraction errors. The most common method of classifying the shapes of aberration maps is to consider each map as the sum of fundamental shapes or basis functions of Zernike polynomials. Each aberration may be positive or negative in value and induces predictable alterations in the image quality. Because there is no limit to the number of terms that may be used by Zernike polynomials, vision scientists use the first 15 polynomials, based on the fact that they are enough to obtain a highly accurate description of the most common aberrations found in human eye. Among these the most important Zernike coefficients affecting visual quality are coma, spherical aberration, and trefoil.
_
_
Aberration of normal eyes:
In normal population the dominant aberrations are the ordinary second-order spherocylindrical focus errors, which are called refractive errors. Low Order Aberrations includes Myopia (positive defocus), hyperopia (negative defocus), and regular astigmatism. Other lower-order aberrations are non- visually significant aberrations known as first order aberrations, such as prisms and zero-order aberrations (piston). Low order aberrations account for approximately 90% of the overall wave aberration in the eye. There are numerous higher-order aberrations, of which only spherical aberration, coma and trefoil are of clinical interest. Higher order aberrations (HOA) are a relatively small component, comprising about 10% of the eye’s total aberration. Many techniques for measuring the eye’s aberrations have been described. The most common technique is Shack-Hartmann aberrometry. In this approach, a weak laser source is directed into the eye and the reflection off the retina is sampled and processed. Other methods include Tscherning systems, ray tracing and Skiascopy methods.
_
Management of wavefront aberrations:
Low order aberrations (hyperopia, Myopia and regular astigmatism), are correctable by eyeglasses, soft contact lenses and refractive surgery. Neither spectacles nor soft contact lenses nor routine keratorefractive surgery adequately corrects high order aberrations. Significant high order aberration usually requires a rigid gas-permeable contact lens for optimal visual rehabilitation.
_
Customized Wavefront-guided refractive corneal laser treatments are designed to reduce existing aberrations and to help prevent the creation of new aberrations. The wavefront map of the eye may be transferred to a Lasik system and enable the surgeon to treat the aberration. Perfect alignment of the treatment and the pupil on which the Wavefront is measured is required, which is usually achieved through iris feature detection. An efficient eye tracking system and small spot size laser is necessary for treatment. Wavefront customization of ablation increases the depth of ablation because additional corneal tissue must be ablated to compensate for the high order aberrations. Actual results with Wavefront guided LASIK showed that not only it cannot remove HOA but also the optical aberrations are increased. However, the amount of increase in aberrations is less than conventional Lasik. Corneal optical aberrations after photorefractive keratectomy with a larger ablation zone and a transition zone are less pronounced and more physiologic than those associated with first-generation (5 mm) ablations with no transition zone. Aspherical intraocular lenses (IOLs) have been used clinically to compensate for positive corneal spherical aberrations. Although Aspherical IOLs may give better contrast sensitivity, it is doubtful, whether they have a beneficial effect on distance visual acuity. Conventional (not Aspherical) IOLs give better depth of focus and better near vision. The reason for improved depth of focus in conventional lenses is linked to residual spherical aberration. The small improvement in depth of focus with the conventional IOLs enhances uncorrected near vision and contribute to reading ability. Wavefront customized lenses can be used in eyeglasses. Based on Wavefront map of the eye and with the use of laser, a lens is shaped to compensate for the aberrations of the eye and then put in the eyeglasses. Ultraviolet Laser can alter the refractive index of curtain lens materials such as epoxy polymer on a point by point basis in order to generate the desired refractive profile. Wavefront customized contact lenses can theoretically correct HOA. The rotation and decentration reduces the predictability of this method.
_
Automatic eyeglasses prescriptions:
New technology in aberrometers means ophthalmologists and others can accurately measure refractive error and other abnormalities in the eye’s optics. But these instruments cannot use these measurements to predict visual acuity, or how well a person can actually see. Usually, ophthalmologists and optometrists rely on a patient’s ability to identify characters on an eye chart to determine visual clarity. It is possible to routinely measure the aberrations of the human eye, but there is as yet no established metric that relates aberrations to visual acuity. Today we have automated objective measurement of visual acuity and of automated prescription of sphero-cylindrical corrections. However, it has been shown that correcting the spherical and cylindrical components of the aberrations does not provide best acuity. Thus, these automated procedures must await a more sophisticated metric that can predict acuity from an arbitrary set of aberrations. A study published by the Association for Research in Vision and Ophthalmology (ARVO) evaluates the performance of several simple metrics that predict visual acuity from wavefront aberrations — the eye measurements provided by an aberrometer. A group of researchers developed a model that successfully predicts visual acuity using both wavefront aberrations and simulations of the complex task of identifying individual letters from the widely used Sloan letter set. They then designed a simple metric that performs as well as the more elaborate model. The metric could be used internationally. The same metric, because of its generality, can predict acuity measured with other symbol sets, such as Chinese characters. With this metric, the aberrometer will be able to give direct predictions of visual acuity, and could also provide an automatic optimal refractive prescription for the patient.
__________
_________
Now I will discuss the most controversial aspects of eyeglasses:
Do eyeglasses weaken your eyesight or improve your eyesight on long run? Or no effect on eyesight?
First I will present conventional view that eyeglasses do not weaken eyesight.
Many people believe that the longer you wear spectacles the worse your eyesight becomes.
But are they right?
There are lots of reasons why people don’t always wear their glasses. They might dislike the way they look, get teased or simply feel more comfortable without them. Beyond comfort and aesthetics, though, some fear that wearing glasses too often will weaken their eyesight, and that they will increasingly rely on them more often than when first worn. A study from Nigeria published in 2013 found 64% of students believed that wearing glasses can damage eyes. Research in the Indian state of Karnataka put the figure at 30%, and in Pakistan 69% of people feel the same way. In Brazil, even medical staff believed that your eyes would gradually get weaker as a consequence of wearing glasses.
Is there any evidence to suggest they are right?
Few trials have been conducted on the prolonged effect of wearing glasses. And from what we know there’s no persuasive evidence that wearing reading glasses affects your eyesight. Why then do so many people become convinced, anecdotally, that glasses have made their eyesight worse? People may gradually find themselves more and more dependent on their specs, but it’s because their lenses have continued to deteriorate with age. So people find themselves needing their glasses more often, leading them to conclude that the glasses must have made their sight worse, where in fact, there’s no causal relationship. Whether or not you choose to wear your reading glasses will make no difference to your eyesight in the long run although if you have to strain your eyes to read, you might get headaches or find that your eyes feel sore. However, the situation is not the same with children. Not wearing the right glasses, or any glasses at all if they are needed, can have a long-term impact. For decades it was thought that deliberately under-correcting for short-sightedness – by giving children weaker glasses than they really needed – might slow down the elongation of the eyeball over time and thus slow down the progression of myopia. The idea was that if you wear glasses to allow you to see clearly in the distance, your eyeball tries to elongate itself when you focus on a close object in order to see it properly. But a trial conducted in Malaysia in 2002 proved this hypothesis was so wrong it had to be halted a year early. A group of 94 children with myopia were randomised at the toss of coin either to wear the correct glasses for their prescription, or to wear glasses that left them slightly short-sighted. When the study began the children were between the ages of nine and 14, and for the next two years the length of their eyeballs were measured at regular intervals. Contrary to an earlier, smaller study from the 1960s, the children who wore the weaker glasses showed a greater elongation of the eyeball over time. In other words their eyesight was gradually getting worse. Also Cochrane review from 2011 of studies of interventions in children with myopia concluded that the limited evidence available suggests it is better to give children the correct glasses, rather than deliberately trying to under-prescribe. There’s no suggestion that wearing the correct glasses will make their eyesight worse than not wearing them at all. In fact the longest-ever study of the progression of myopia, which has just published its 23-year findings suggests the contrary. Back in 1983 a group of children in Finland with myopia were randomised to various conditions, including reading without spectacles. Their myopia progressed a little faster than those who wore their glasses continuously. After the initial three years of the study, they were all advised to wear glasses all the time. Twenty years on, there was no difference between the groups. The benefits of wearing glasses if you’re a child who needs them, are clear. Children’s eyes need to learn to see, so if they don’t have the right glasses they can develop so-called “lazy-eye” or amblyopia because they’ve never had a sharp image on their retina. The correct prescription has also been shown to improve your reading speed and reduce the risk of developing a squint. While there are plenty of reasons to choose not to wear glasses, the fear that you might be damaging your eyesight isn’t one of them.
________
Now I present the contrary view. Wearing eyeglasses in fact worsen myopia and increases chance of myopic complications:
Is correct prescription of distance vision harmful in myopia?
Myopia myth declares that myopia or nearsightedness is inherited from one’s parents, and that there is nothing to be done about it but to wear glasses or submit to corneal surgery. We are told by the optometrists and ophthalmologists to whom we go for help with our vision problems, as well as by state and federal public health services, to expect that the myopia will get steadily worse, requiring stronger lenses, until we reach adulthood when the myopia will stabilize. The fact is that myopia is not inherited. It develops because of the unnatural way we use our eyes, and in nearly every case it can be prevented. This acquired myopia is caused by the excessive amount of reading and other close work that our modern society demands. It is estimated that approximately one-third of the United States population suffers from myopia and needs glasses for clear distance vision. It is significant that in the fifth or sixth grades, only about five percent of the children are myopic, but that the percentage increases steadily through the school years until at the graduate level over fifty percent are myopic. Moreover, fully two-thirds of the graduate honor students are myopic. How can this possibly be considered normal? Is it not strange that more parents do not ask for a logical reason why their children, normal in every other way, should suddenly suffer from failing vision at such an early age? Yet we do not find young children in such numbers suffering from deterioration of their senses of hearing, smell, taste, and touch. Why just vision? The obvious reason is that our vision is being used in a manner drastically different from the use for which nature has prepared it. Compare this high incidence of myopia with illiterate, primitive societies where almost no one is nearsighted. It is not inaccurate to speak of the situation as an epidemic of myopia, and it will continue to increase until the proper action is taken. It used to be common to see myopia develop around age nine, but it is now becoming common in youngsters five or six years old, because children are learning to read at an earlier age. Many children, while still under ten years of age, have myopia that has progressed to the point where they would be classified as legally blind if they did not have eyeglasses to correct their vision.
_
Assume that a child has just begun to become nearsighted. This means that the ciliary muscle spasm, which has been useful in reducing the infantile farsightedness to zero, is now threatening to cause the eye to continue to elongate and become permanently myopic. The most natural way to relax the spasm, return the vision to normal, and prevent overelongation is to have the child give up all close work and take up activities which only require distance vision. This prescription, since it would mean not going to school and not learning to read, is clearly impractical in our modern society. Other methods must be found that will “fool” the eyes so that the close work can be done with the eyes focused for distance.
_
_
Figure above shows a myopic eye in which the amount of myopia is exaggerated for the purpose of illustration. Because of the ciliary spasm, the lens cannot relax sufficiently to enable the parallel rays from a distant object to come to a focus on the retina. The object appears blurred. The child is taken to the doctor and fitted with a pair of minus lenses. Figure below shows what happens.
_
_
These glasses cause the parallel rays to diverge just enough so that the eye can focus them on the retina. They make the eye feel (with regard to focusing effort, at least) that the viewed object is actually closer than it is. In fact, if you follow the dotted lines, you will see that point F is where the viewed object appears to be. In this example, F is also the focal point of the lens. Minus lenses thus move the world closer to the eyes. Note that with these lenses, there is no longer any way that the eye can receive parallel rays. All light rays are diverging to a greater or lesser extent. Since the cause of myopia is too much close work, it is obvious that such glasses, by moving everything closer, will aggravate the condition. Most of the damage occurs when such glasses are used for reading. Many people use their distance glasses for reading even though they could read without them, merely because the eye specialist has never advised against it. There are also many people who must use their glasses for reading because their myopia has progressed to the point that if they remove their glasses they will find that even the book is blurred. Their far point or limit of clear vision is not far enough to reach the book.
_
_
Figure above shows what happens when these minus lenses are used for reading. The book, actually located at B, now appears to be at A. Now the eye, instead of focusing on the book at B, must accommodate more and focus at A. This simple fact explains why such glasses are so harmful. A vicious cycle now develops. The minus glasses bring everything closer, making increased accommodation necessary. The increased accommodation causes further lengthening of the eye with the resulting need for even stronger glasses. Many children find they need stronger glasses as often as once a year. If minus lenses were never prescribed, the myopia would only increase to the point where the usual close work could be done without the need for accommodation. There it would cease at a moderate amount, perhaps 3 diopters. The present, almost universal, practice of allowing a child to read with concave “distance” glasses is ruining the vision of millions of children.
_
_
Figure above shows very approximately the percentage of myopic persons at various ages in the United States. It is easy to see that the great increase in myopia begins during the early school years. When the school years are completed, the increase levels off. The reason is that if a person is going to develop myopia, it will usually have developed by the time adulthood is reached. Also, it is during the juvenile years, when the eyes are most flexible, that prolonged close work has the most damaging effect on the lengthening of the eyes. In adulthood, the coats of the eyes seem to lose much of their flexibility and do not stretch as readily in most people. It should be remembered, though, that a small number of people do find their myopia increasing through adulthood. If a myopic child is given minus lenses to read with for, say, one-half hour, the distance vision after removing the glasses is often found to be appreciably worse than before. The vision can be tested before and after the experiment by using an ordinary wall chart. In other words, the eyes have adapted to the minus lenses by temporarily becoming more myopic. If this type of eye abuse is continued long enough, the distance vision will be permanently damaged.
_
Lighting and myopia:
Reading with distance lenses obviously tends to make the vision get worse, particularly in children. If the reading is done under conditions of poor lighting, the vision will generally deteriorate faster than if good lighting is used. The following diagrams will make clear why this is so.
_
_
Figure above represents an eye where the pupil is very large (as it would automatically become under poor lighting), and the entire lens is being used to receive light rays. It is apparent that those rays farthest from the center of the lens must be bent more than those close to the center. In fact, the ray of light passing through the center of the lens does not have to be bent at all.
_
_
Now look at figure above, which represents an eye that is being used under a high amount of illumination. The iris has contracted, making the pupil quite small. The periphery, or outer portion of the lens, is not being used. The only light rays passing through the lens are those near the center, which require little bending, while the most divergent rays do not reach the lens at all. What this means is that the eye does not need to accommodate nearly as much when viewing an object in bright light as it does in poor light. It has long been recognized that the brighter the illumination, the less the accommodation. This is extremely important to the myope, since excessive accommodation is at the heart of the myopia problem. It is common for parents to tell their children not to read in poor light, but there are very few people who have any idea about exactly how the eyes might be harmed by poor light.
_
Is conventional wisdom wrong in correcting refractive error by glasses?
As things now stand, nearsighted children are given minus lenses and farsighted children are given plus lenses. Both are wrong and are worse than giving no lenses at all. Minus lenses accelerate the harmful elongation of the nearsighted eye, and plus lenses hinder the proper elongation of the farsighted eye. Minus lenses are stimulants to eyes that are in need of accommodative relaxation. Plus lenses are relaxants to eyes that are in need of accommodative stimulation. There are those who say, “How will the myopic child see if we don’t prescribe glasses?” This shows a lack of imagination. Children do not need clear distance vision for outside activities or around the house. About the only place where there is a problem is in school. If blind students can earn college degrees, surely we can make arrangements so that myopic children can see the blackboard without resorting to glasses. They can be allowed to sit in the front rows, the teacher can write larger, the blackboard can be better lighted, they can use pinhole glasses, etc. There is no harm or discomfort to a child if the blurred distance vision is uncorrected. It can only be beneficial. There are, in fact, many myopes who aren’t even aware of their problem. They think it is normal for distant objects to be a little blurred. It is also a fact that many doctors “overcorrect” for myopia. Instead of prescribing lenses that give 20/20 vision, they prescribe lenses that are even stronger and give 20/15 vision. This can only make the myopia get worse faster. Actually, even a person with normal vision will seem to see better through a weak minus lens. White seems to appear whiter and black blacker. This certainly does not mean that such a correction is needed or desirable. Unbelievable as it may seem, many myopic children are told by their doctors that if they wear glasses or contacts all of the time their eyes will get better, or at least not get worse. This is totally false. Because of this type of erroneous advice, people actually believe that glasses “save” eyes. The truth is that minus glasses destroy myopic eyes. It may surprise you to learn that many eye doctors act according to the philosophy that there is nothing wrong with wearing glasses. They reason that glasses do not cause much inconvenience, that they are so common these days that no one looks strange wearing them, and that so many types and fashions are available that glasses can actually “improve your looks.” In addition, one hears the argument that some nearsighted people (if they are lucky enough to develop just the right amount of nearsightedness) merely need to remove their glasses to read after they reach the age when non-nearsighted people must put on reading glasses to read (a condition called presbyopia). By reasoning or rationalizing in this manner, they can go about their business of prescribing glasses for young and old with no disturbance to their conscience and without concerning themselves about anyone’s vision getting worse because of the eye doctor’s actions.
_
The dangers of increasing myopia:
Most people are already aware of the most obvious drawbacks of having to wear glasses, such as distortion, reduced field of view, expense, poor appearance, inconvenience, reduced vision because of dirt or rain on the glasses, etc. However, they are not aware of the more serious results of increasing myopia. Let us look at some of these more serious problems.
1. Floaters:
In the nonmyopic eye, the vitreous chamber normally contains only a semi-solid, jelly-like substance called the vitreous body. Since the vitreous body fills the space between the lens and the retina, it provides solid support for the retina.
As myopia develops and the eye becomes longer than normal, the volume of the vitreous chamber becomes greater. Since the vitreous body is more firmly attached to the lens than to the retina, the support it provides for the retina becomes diminished. The vitreous becomes more watery, further decreasing retinal support. These changes, coupled with the stretching of the retina, make retinal detachment more likely in the myope than the nonmyope. Because of this watery substance in the vitreous chamber, myopes are more likely than nonmyopes to be disturbed by floaters. These are odd-shaped spots that appear to float and jump around in the field of vision, particularly when looking at a white surface and making sudden eye movements. These particles are located in the vitreous chamber. They may have been present from birth and can occur in both myopic and nonmyopic eyes. Others may develop during the myopic elongation of the eye. Usually, the floaters are not a cause for concern and they may not even be noticed most of the time. However, the watery vitreous of myopic eyes enables the particles to move around more easily, and they are thus more noticeable and disturbing than in nonmyopic eyes. People who ask their doctors about the “spots” they sometimes see are usually not told that the problem frequently arises only because myopia has been allowed to develop. Furthermore, if the floaters are increasing in number, this could be a sign that the myopia has progressed to the point where degenerative processes are taking place at the surface of the retina, and the particles of material resulting from this degeneration are leaving the retina and passing into the watery vitreous. A large number of floaters can thus be a sign that a retinal detachment is about to occur.
2. Retinal detachment and macular degeneration:
By far the worst thing wrong with the wearing of glasses by myopes is the increased risk of serious eye problems in later years. The lack of preventive measures coupled with the prescription of stronger and stronger lenses causes the eye to stretch more than it was ever designed to do. The eye is capable of continuing this lengthening process until it literally tears itself apart! Of the three layers at the rear of the eye, the sclera (the outermost layer) and the choroid (the middle layer) are fairly elastic and can withstand considerable stretching without damage. However, the retina (the innermost layer) is fragile and relatively inelastic and will tear loose from its attachment to the choroid if the eye is stretched too much. This can happen slowly or spontaneously, as the result of a blow to the eye or head. Any overelongation of the eye increases the risk of retinal detachment in later years. Methods are available to try to reattach the retina, but they are generally unsatisfactory. Even if a successful reattachment is made, further elongation of the eye can result in a second detachment. Even if retinal detachment does not occur, high myopes are prone to various forms of deterioration at the rear of the eye (that is, to various forms of macular degeneration) resulting from the abnormal stresses caused by the elongation. Because of this stretching, the sclera can, in extreme cases, be reduced to one-quarter or less of its original thickness. At some point during the enlargement of the eye, a pathological state begins to develop. That is, we are no longer dealing with a case of simple myopia, but with a diseased eye. Among the main changes are generalized atrophy of the retina and choroid, and degeneration at the point where the optic nerve leaves the eye and in the macular area (where the fovea is located). Hemorrhages can occur at various places. Because of the atrophy at the fovea, central vision begins to be lost. Macular degeneration can also be caused by clogged arteries to the eye, resulting from atherosclerosis which is due to too much fat in the diet. Similar mechanical and degenerative changes occur in the vitreous. Since the vitreous has become quite watery, large floating spots of degenerative material can be easily seen. The tearing and hemorrhaging of the retina lead to retinal detachment, allowing the watery vitreous to flow between the retina and choroid. The watery condition of the vitreous thus aggravates the tendency toward detached retina. If actual detachment does not occur, the degenerative changes can progress slowly until no useful vision remains. In either case, blindness often results. Large numbers of people lose their sight each year due to these complications of high myopia. The British Government lists myopia as the third most frequent cause of blindness, after diabetes and congenital defects. Retinal detachment is not to be confused with vitreous detachment, a condition where the vitreous body pulls loose from its attachment to the retina at the back of the eye. This happens to many people as they age and is generally not cause for concern. Momentary flashes of light are frequently seen off to the side when the eyes are moved, particularly at night, as this takes place. These flashes are thought to be due to the vitreous body putting momentary tension on the retina. They diminish in time.
3. Problems after cataract surgery:
It is not widely known among the public that cataract surgery, by its drastic alteration of the tissues and of the hydraulic forces inside the eye, predisposes that eye to tearing or detachment of the retina. The typical person who suffers through two cataract operations, believing that they will result in clear vision from then on, is totally ignorant of the fact that the operations can set up conditions that frequently result in serious retinal problems a few years later. While this situation is bad enough for the nonmyopic patient, a considerably worse situation exists for the moderate or high myope. The eye that has become overelongated and myopic from years of using concave lenses is predisposed to retinal deterioration even before cataract surgery. If the lens of such an eye is removed, this tendency is increased even further. A high myope facing cataract surgery has little to be optimistic about. The fact that so many people develop cataracts is yet another reason why myopia must be prevented in our children. They will then have a better chance of avoiding blindness if a cataract operation should ever be required. Even a small amount of myopia, if allowed to develop, unnecessarily increases the already present danger of retinal problems in those who undergo cataract surgery
_
High myopia can be a tragic affair, and the earlier that concave glasses are put on a child the more years there will be ahead for the myopia to develop serious complications. There is obviously a great deal wrong with being nearsighted, and those who claim otherwise are doing the public a disservice. Bringing these disquieting facts into the open is not a pleasant task. Many people don’t want to hear about such things. Nevertheless, you cannot protect yourself from harm without being made aware of the danger.
______
My view:
After listening to both sides of the story, I conclude that:
1. Failure to give full distance correction to myopic children may result in amblyopia and refractive error induced ambyopia is not uncommon.
2. Full distance correction glasses to children/teens may worsen myopia as they are inadvertently going to use the same glasses for near vision (e.g. reading/computer/smartphone).
3. I suggest that every child/adolescent myopic be given glasses having both distance and near vision correction (bifocal/progressive).
_______
_______
Can’t find your glasses?
It has happened with me many times that I can’t find my glasses. With -6D myopia, without glasses my distance vision blurred. Those of us without 20/20 vision suffer from a catch-22 that can be extremely aggravating: If you can’t find your glasses, you can’t see, but if you can’t see, you can’t find your glasses. How many collective hours have we all spent searching for those frames? But our days of squinting to see and blindly feeling around to find our glasses are over. There is incredibly simple, yet genius idea: Use your smartphone’s camera as a magnifying glass. If there is any item that we use more than our glasses, it would be our smart phones, and if those get lost, at least they make noise. Sure, this is no cure for visual impairments, and it won’t be as handy for those who are so near-sighted that they can’t even see the screen of their phone, but for the vast majority of us, it’s a golden trick for when we find ourselves glasses-less, but still need to see something. Seriously, take your glasses off right now and try reading this, or the clock, or something that you can’t see clearly, then use your smart phone to look at it. There is another way which I used frequently. Always keep another pair of glasses at a fixed secure place. When you can’t find your glasses, wear secure glasses and search for primary glasses. In event your primary glasses are broken; wear secure glasses till new glasses are made. Nowadays smart tracking devices are available to find misplaced glasses. Small attachment for the glasses are available that can connect to mobile devices through an app for easy tracking of misplaced glasses. The clip connects via Bluetooth to a smartphone app or keychain. When activated, the clip beeps to help locate the glasses.
_______
_______
True or false:
_
Babies can see at birth.
False.
At birth, baby sees only in black and white and shades of gray. Nerve cells in their retina and brain that control vision are not fully developed. Also, a newborn infant’s eyes don’t have the ability to accommodate (focus on near objects). It just takes time. Despite these visual limitations, studies show that within a few days after birth, infants prefer looking at an image of their mother’s face to that of a stranger.
_
Wearing the wrong kind of eyeglasses damages your eyes.
True.
Poorly corrected refractive errors in childhood can cause amblyopia. When myopic child/adolescent uses distance corrected minus glasses for reading for long hours, it may worsen myopia.
_
Reading in dim light is harmful to your eyes.
True.
Bright light decreases pupil diameter and increases depth of focus by blocking peripheral rays that need more refraction, thus reducing defocus. Also, eye does not need to accommodate nearly as much when viewing an object in bright light as it does in poor light. Less accommodation strain means less eye strain and less progression of myopia. The eye’s far point of an individual’s focus varies with the level of light; poor lighting will bring far point closer to eye and make eye myopic.
_
Using computers can damage your eyes.
True.
Too much near work strains accommodation and accommodation overload can worsen myopia. About 50 to 90 percent of computer users suffer from visual symptoms of computer vision syndrome. Computer users can prevent or reduce computer vision syndrome by proper lighting, minimizing glare, upgrading and adjusting computer display and exercising eyes including blinking more often. To reduce your risk of tiring your eyes by constantly focusing on your screen, look away from your computer at least every 20 minutes and gaze at a distant object (at least 20 feet away) for at least 20 seconds. Some eye doctors call this the “20-20-20 rule.” Looking far away relaxes the focusing muscle inside the eye to reduce fatigue.
_
Sitting close to the television can damage children’s eyes.
False.
Refractive errors occur because of variations in size and curvature of the eyeball and not due to nutritional deficiency or watching TV. Watching TV does not cause myopia unless the child sits so close that it becomes a close task. A child should be permitted no closer to the TV set than six feet. Instead of watching TV in a dark room, a well-lit room with white light is ideal. Children with nearsightedness (myopia) sometimes sit close to the television in order to see the images more clearly.
_
Reading too much will harm eyes.
False.
You need good illumination and good near vision for reading. The book or other material should be held as far from the eyes as possible. The distance from the elbow to the knuckles of the hand has been suggested as the minimum working distance. When reading, the child should look up and into the distance momentarily at the end of each paragraph, or at least at the end of each page, to relax the eyes.
_
Eating carrots improves your vision and reduce need for glasses.
False.
Carrots do contain vitamin A, which is good for the eyes. However it cannot correct refractive error.
_
Wearing glasses makes your myopia worse.
Half-true.
Studies have demonstrated that wearing glasses to provide clear vision for distance seeing does not cause more nearsightedness. However these lenses are not optimum for near vision and should be removed or a bifocal should be put in the glasses. Constant use of lenses for distance vision for near work may worsen myopia in children and adolescents. Optometrists who test both far and near vision should advise when removing glasses or a bifocal is appropriate for reading and other close work.
_
Over the counter reading glasses can harm your eyes:
False.
Like gray hair and a slowing metabolism, needing to use reading glasses is one of the unwelcome signs of middle age. After about age forty, the lens of the eye becomes more rigid which makes it harder to focus on close objects. This condition is called Presbyopia. Most drugstores nowadays carry readers. The American Academy of Ophthalmology says that over the counter reading glasses are perfectly safe if you don’t need corrective lenses for distance. For the best results, you try on different powers (labeled 1.0 for weakest to 4.0 for strongest) while reading something held at a distance of 14-16 inches.
_
Having 20/20 (6/6) vision means that the eyes are perfect.
False.
The term 20/20 (6/6) denotes good sharpness of central vision at distance. But other types of vision-such as peripheral vision, night vision, depth perception, eye coordination, near vision or color vision etc might be imperfect. Some potentially blinding eye disease such as glaucoma or diabetic retinopathy can take years to develop. During this time, they are harming parts of the inner eye, but the central vision can remain unaffected.
_
An eye examination is necessary only if you’re having problems.
False.
Everyone should follow proper eye healthcare, which includes regular eye exams, whether or not you are having any noticeable signs of problems. Children should be tested at birth, at 6 months of age, before entering school and periodically throughout the school years. For adults, the frequency depends on your doctor’s advice and may be every two years or more often. If you have diabetes or an eye disease, you should go every year for a comprehensive eye exam.
_
Wearing contact lenses too long can harm your eyes.
True.
Wearing contact lenses for too long can cause protein to build up on the surface of the eyeball, which can block oxygen circulation to the eye. Common problems that can result from leaving contacts in for too long include corneal ulcers, bacterial or fungal infections, and irritation caused by oxygen deprivation. Those who wear the lenses overnight have a risk of eye infection 10 to 15 times that of users who insert and remove the lenses daily. It was estimated that the probability for microbial keratitis is about 3-fold for daily-wear soft lenses, and about 20 fold for extended wear soft lenses, compared with daily-wear hard RGP lenses.
_
Contact lenses can prevent progression of myopia.
Half-true.
Orthokeratology means using the use of overnight rigid contact lenses to change the shape of the cornea of the eye, and it is especially applicable to myopic eyes. It may help some myopes. There are potential sight-threatening and devastating risks associated with overnight contact lens wear and numerous reports of corneal infection and scarring have been published. There are also a substantial number of people who use this method to treat astigmatism. Contact lenses rotate with the eye to provide a consistent retinal focus, so overcome a number of the problems associated with spectacle lenses. Contact lenses provide better refraction to off-axis peripheral rays to reduce peripheral hyperopic defocus. Multifocal contact lenses with special dual-focus multifocal design with full corrective power in the center of the lens and less power in the periphery would eliminate peripheral hyperopic defocus while focusing for near objects, resulting in prevention of progression of myopia.
_
Eye exercises can improve your vision.
Half-true.
Unfortunately, there is little eye exercises can do to improve your vision. They can be used by children to help with a condition called convergence insufficiency in which the eyes cannot focus on close objects easily. For adults, focusing difficulties and convergence can be improved with eye exercises although this does take a lot of time and effort. Eye exercises promoted as helping people get rid of glasses, known as the Bates method, have no scientific backing. As we age our vision naturally deteriorates and exercises will not reverse that. However, exercises may help you learn to use the vision you have more effectively. Someone with macular degeneration may be helped if they practice looking through other parts of the eye. Children must be encouraged to intermittent vision breaks in between prolonged near work activities (reading) to dissipate constant accommodation by focusing on distant objects every 15 minutes for 20 seconds to prevent progression of myopia.
_
Refractive error changes at night.
True.
At night the pupil is very large (as it would automatically become under poor lighting), and the entire lens is being used to receive light rays. Spherical aberration would increase as parallel peripheral rays from distant objects would fall before retina and divergent peripheral rays from near objects would fall behind retina as they need more bending. Chromatic aberration would worsen at night as dark adaptation would make shorter wave length rays fall before retina. Also, poor lighting leads to increased accommodation and eye strain. Small refractive errors can cause big symptoms particularly at night. The wider the pupil, the more any refractive error contributes to poor vision. The eye’s far point of an individual’s focus varies with the level of light. Individuals complaining of nighttime driving problems commonly experience a significant change in refractive error when the pupil dilates in low-light conditions. A pilot with 20/20 visual acuity in normal daylight may develop -0.50D to -0.75D at night. This change is difficult to measure with the conventional phoropter-based refraction, as it requires that the patient be refracted in nighttime conditions. As a result, most eyeglass wearers with nighttime vision problems do not receive a meaningful correction for poor night vision. Proper distance correction with adding an anti-reflective coating can help. A stronger prescription for myopic night drivers is often needed. The most common reason for haloes and reflections is a dirty windscreen (both inside and out) and scratched or dirty spectacle lens.
____________
____________
The moral of the story:
_
Note:
Spectacles = eyeglasses = glasses
Contact lenses = contacts
LASIK = laser assisted in situ keratomileusis (in situ means in place and keratomileusis means shaping the cornea)
_
1. Refractive error is the failure of the eye to focus images sharply on the retina causing blurred vision. An image is in focus when almost all light rays from point on object are converged into a corresponding point on retina to make image. Refractive error is the most common eye disorder worldwide. Refractive errors except presbyopia begin in childhood, progress over childhood & adolescence, and get stabilized in adulthood; having direct correlation with growth of eye ball, and the coats of the eyes seem to lose much of their flexibility and do not stretch readily in adulthood.
_
2. Two in every ten primary school children and three in every ten secondary school children wear glasses.
_
3. Myopia is the most common form of refractive error and affects over 30% of Western populations and up to 80% of Asians. In 2010, there were an estimated 1.7 billion myopes worldwide – predicted to increase to around 2.2 billion by 2020.
_
4. The bending (refraction) of light rays by any optic lens depends on 3 factors:
a) Its surface curvature, greater the curvature, greater refraction; concave curvature will diverge rays and convex curvature will converge rays; flat surface no refraction.
b) Its material, higher refractive index, greater refraction assuming air with refractive index 1 is the preceding medium; otherwise ratio of refractive indices of two media
c) The wave length of incoming light rays, greater the wave length of light, lesser the bending of rays. This chromatic dispersion is determined by Abbe number; higher the Abbe number, lesser is the dispersion of visible light.
_
5. When all light rays entering eyes are equally refracted (i.e. refracted in vertical, oblique and horizontal meridians) but focused before retina (myopia) or behind retina (hyperopia), we call it spherical refractive error. Myopia and hyperopia are spherical refractive error. When all light rays are unequally refracted in different meridians, we call is astigmatism, a cylindrical refractive error. Not only do light rays have to focus at the level of the retina (as opposed to in front or behind it) but also on a single point. This is achieved through the symmetry of the corneal and lens curvatures around their circumference. In astigmatism, variations in the symmetry of these curvatures (usually corneal) result in rays failing to focus on a single point. It is possible to have more than one refractive error, such as having both myopia and astigmatism. Testing vision through a pinhole aperture is a useful way to screen quickly for refractive error. If visual acuity is better through a pinhole than it is with the unaided eye, the patient needs refraction (refractive correction) to obtain best corrected visual acuity (BCVA).
_
6. Range of focus is the distance between far point and near point wherein if objects are placed, clear images will be focused on retina. Far point is the farthest an eye can see clearly with accommodation relaxed. Near Point is the closest the eye can see clearly exerting accommodation fully. For normal adult eyes, far point is optical infinity (6 meter) and near point is 30 cm. Near point varies from 5 cm in infancy to 10 cm in young adult to 1 meter in middle age due to change in amplitude of accommodation. The eye’s far point of an individual’s focus varies with the level of light. Poor lighting will bring far point closer to eye.
_
7. Accommodation refers to the ability of the eye to increase its refractive power of the natural crystalline lens in order to focus near objects on the retina. The accommodation (near point) response is consensual (i.e., it involves the actions of the muscles of both eyes). The stimulus to accommodation is a blurred retinal image. It is part of the ‘Near Reaction’ that involves accommodation along with convergence and pupillary constriction. Papillary constriction increases depth of focus by blocking peripheral rays that need more refraction and reduce defocus. Convergence means eyes rotate towards each other around their vertical axis to keep the object’s image focused on the foveae of the two eyes to obtain single binocular vision. Amplitude of accommodation is the amount of accommodation exerted to move the focus from the far point to the near point. The ability to focus on near objects declines throughout life, from an accommodation of about 20 diopter (ability to focus at 5 cm away) in a child, to 10 diopter at age 25 (10 cm), and levels off at 0.5 to 1 diopter at age 60 (ability to focus down to 1–2 meters only). Presbyopia is the irreversible loss of the accommodative ability of the eye that occurs due to aging.
_
8. Whenever myopia/ hyperopia/ astigmatism is measured and corrected, it is for distance vision. That means after correction by lens, far point will become infinity (6 meter). Power for near point is sum of power for far point plus power of accommodation. For near vision, additional correction is done to bring near point to 30 cm if accommodation power of eye is less than 3 diopter (<+3). Therefore the same corrective lens cannot be used for distance and near vision when myopia/hyperopia/astigmatism is associated with presbyopia, and hence bifocal or progressive lens is used.
_
9. A nearsighted person (myopic) who needs a –1.00 diopter lens can see objects at one metre clearly, but anything farther is blurred. His far point is at 1 meter but he cannot clearly see beyond it. A farsighted person (hyperopic) who needs a +1.00 diopter lens has far point at 1 meter behind eyes and he has to use accommodative power constantly to see any distant object. When 1 diopter myopia/hyperopia is corrected by concave/convex lens, far point would become 6 meter for both. In other words, both can see objects clearly at 6 meter distance with relaxed accommodation. Remember; a myope has too much plus in their eyes whereas a hyperope has too much minus. Accommodation power means addition of plus lens.
_
10. The total refractive power of eye is approximately 60 diopter with accommodation at rest to focus image on retina from distant objects. When it is more than 60D, we call it myopia (i.e. the optical power of the eye is too strong for the corresponding axial length). When it is less than 60D, we call it hyperopia (i.e. the optical power of the eye is too weak for the corresponding axial length). In myopic eye, parallel light rays from distant objects (> 6 meter) will make image before retina. However, near objects throw divergent rays on eyes and therefore will focus well on retina naming the condition as near sightedness. In hyperopic eye, parallel light rays from distant objects (>6 meter) will make image behind retina and will need constant accommodation to focus image on retina resulting in difficult distant vision. As near objects are throwing divergent rays, it will focus far behind retina causing blurring of vision despite accommodation. It would be wrong to name it as far sightedness as distance vision is difficult and constant use of accommodation leads to eye strain and other complications. Remember; both for myopia & hyperopia, refractive error is same in all meridians as opposed to astigmatism where there is differential refraction in different meridians. Astigmatic eye cannot focus image on retina no matter whether object is moved near or far and no matter whether accommodation is exerted or not.
_
11. Headache and refractive errors are very common conditions affecting everybody and therefore their association by chance is far more likely than causal relationship. After seeing thousands of headache patients over last 27 years of my medical practice, I assert that most of them did not have refractive error as their cause of headache although lot of them did have refractive error coincidentally. In fact most of them turned out to be common migraine or tension headache or depression; and many of them were prescribed glasses without any relief in headache. It is rare to find a patient who says that his/her chronic headache is completely relieved by wearing glasses. Exceptions are uncorrected hyperopia where use of constant accommodation power to see distant objects may lead to ciliary muscle strain and headache since the eye’s close focusing power is not designed to remain constantly activated; and high anisometropia where differing refractive states result in large differences in image sizes formed in the two eyes resulting in prolonged contraction of the brow, scalp, and neck muscles in an attempt to maintain a clear image results in headache. The key word is an attempt by a person to improve vision resulting in headache. In other words, if somebody ignores poor vision, he/she will not get headache no matter whatever the refractive error. In other words, uneducated and unintelligent people are unlikely to get headache due to refractive error. The same logic cannot apply for other refractive error like astigmatism because no matter how much person attempts using accommodation or scalp/neck muscles, clear image is not formed on retina and therefore person will not persists in attempting and will not get headache.
_
12. Even though strong case can be made for the view that refractive error is determined genetically; animal and human studies show that visual deprivation during childhood produce myopia by interrupting the emmetropization process. The refractive development of the eye is under the influence of a feedback mechanism known as emmetropization where optical defocus guides the growth of the eye so that there is no refractive error. This is so as the retina can make a distinction between positive and negative defocus and in response retina releases factors to control the growth of the underlying sclera leading to change in axial length of eye.
_
13. Evolutionary biologically our eyes are tuned for constant distance (far) vision and occasional near vision using accommodation power. Prolonged near work (reading, schooling, computer work, smartphones use, indoor activities etc) leads to constant accommodation use. Constant accommodation increases refractive power of eye persistently rather than intermittently. Thick ciliary body in myopic children points to constant accommodation overuse due to persistent near-work. Persistent increase in refractive power tricks retina into believing that eyes are trying to compensate for hyperopic defocus. This illusory hyperopic defocus stimulate retina to secrete growth factors for sclera to increase axial length of eye producing compensatory myopia during childhood. Constant accommodation is sufficient to cause central and paraxial rays to fall on fovea but not sufficient for peripheral rays from near objects to focus on retina as these diverging rays would need far more refraction (bending) and therefore these peripheral rays will fall behind retina causing peripheral hyperopic defocus. This peripheral hyperopic defocus also causes axial elongation of eye resulting in compensatory myopia. Although accommodative pupillary reflex causes pupil constriction to block peripheral rays momentarily, constant accommodation leads to retinal adaptation and accommodative papillary reflex is abolished allowing peripheral rays to enter eyes. Compensatory Myopia will make distant vision blurred but near vision easy with less strain on accommodation. In other words, persistent near work leads eye changes to make eyes suitable for constant near vision i.e. myopia. Persistent near-work in childhood (schooling, reading, indoor activities, computers, smartphones etc) and bad reading habits do precipitate myopia and worsen myopia irrespective of genetic factors. Therefore children must be encouraged to intermittent vision breaks in between prolonged near work activities (reading) to dissipate constant accommodation by focusing on distant objects (at least 20 feet away) every 15 minutes for 20 seconds. The use of plus glasses (for non-myopes) or plus additions (for myopes) for extensive near work incorporated as reading glasses, bifocals and progressive lenses reduce accommodative efforts, makes person read at far point and prevent progression of myopia. In other words, all normal children without refractive error must use reading glasses for prolonged reading/near work to prevent future development of myopia. Prescribing minus lenses for distance correction in myopic children may worsen myopia as they use the same lens for prolonged near-work including reading. All myopic children/adolescents/adults should have full myopia correction for distance vision and additional plus lens (bifocal, progressive or separate reading glasses) for near vision. There is no rational for permanent under-correction of myopia.
_
14. Remember; in illiterate primitive societies myopia is rare. Among Australian Aborigines, less than 5% had myopia. Now there appears to have been a significant shift toward myopia in Australian Aborigines due to modest amount of formal education representing an increase in schooling and near work. A study on Eskimo subjects found myopia rarely in parents and grandparents. However, 58% of the children were myopic. This was attributed to the introduction of Western-style education during the past generation. So although genetic factors are relevant in myopia, prolonged near-work is the most important environmental factor for myopia.
_
15. Peripheral rays in distance vision would cause myopic defocus due to spherical aberration and increase in curvature of field for peripheral rays; and peripheral rays in near vision would cause hyperopic defocus due to divergent rays. Since peripheral rays are blocked by small pupil or pinhole glasses, both distance and near vision improves when pupil is small or when pinhole glasses are used.
_
16. Good illumination (lighting) decreases pupil diameter and blocks peripheral rays resulting in better distance and near vision. Eyes do not need to accommodate nearly as much when viewing an object in bright light as it does in poor light. Also good lighting eliminates the need to hold the book close. Poor illumination leads to defocus, poor image quality, eye’s far point brought closer to eye and excessive accommodation; stimulating retina to release factors for sclera growth and development of myopia.
Note:
Pupillary constriction and dilation occurs primarily because of the light reflex and accommodation reflex. The light reflex refers to constriction that occurs due to intense light and dilation that occurs with dim light. The accommodation reflex results in changes when the two eyes work together to focus on near object. In dim light/night, full pupil dilatation occurs to allow more light to enter and more peripheral rays need more bending to focus near objects resulting in increased accommodation but this increased accommodation cannot cause pupil constriction as light is dim.
_
17. Although sunglasses offer protection against ultraviolet radiation (UV) by blocking UV rays, they also block substantial visible light which degrade the vision in two ways. The obvious way is that they reduce the amount of light entering the eye, making everything darker and harder to see. The less obvious way is that any refractive error (myopia, hyperopia, astigmatism) is made worse. This happens because the pupil becomes wider to compensate for the loss of light when these sunglasses are put on. And wider the pupil, more peripheral rays enter the eye and more any refractive error contributes to poor vision.
_
18. Because of strong accommodation power of 10-20 diopter in children, distance visual acuity testing (6 meter) without cycloplegia (paralysis of accommodation) would result in over-diagnosis of myopia and under-diagnosis of hyperopia. Normal child will be labeled as myopic and hyperopic child will be labeled as normal. Refraction in young children changes rapidly in the usual case in the direction of emmetropisation. A single measure of refractive error, unless extreme or anisometropic, is not a useful indicator of the need for correction. Unwise correction of refractive errors at a young age is likely to impede emmetropization. Even in true myopes, the omission of cycloplegic agents can contribute to the progression of myopia because the prescribed glasses can be too strong, which causes a further progression of myopia.
_
19. Cycloplegic retinoscopy and subjective refraction is still the gold standard for measuring refractive error in children. However, cycloplegic autorefraction can be substituted for conventional cycloplegic retinoscopy.
_
20. Measurement of visual acuity is the minimum distance between two points, which are clearly seen as separate points, at a standard distance from the observer. Humans with normal visual acuity can distinguish two points separated by an angle of one minute of arc. Visual acuity test using eye chart (e.g. Snellen chart) is a screening test to determine refractive error of eye. Distance visual acuity of non-accommodated eye of 20/20 (6/6) does not mean normal vision. It only indicates that your eyes are able to detect fine detail of objects at 20 feet (6 meter) distance using your central vision. Peripheral vision, eye coordination, depth perception, night vision, color vision and focusing ability cannot be determined by eye charts. Also potentially blinding eye disease such as glaucoma or diabetic retinopathy can take years to develop and during this time, they are harming parts of the inner eye, but the central vision can remain unaffected.
_
21. Glass lenses are breakable but scratch resistant and provide the clearest possible vision. Plastic lenses scratch more easily but much lighter, less likely to break and less prone to glare.
_
22. Best spectacle lenses are thinner (high refractive index), lighter (plastic) and flatter (aspheric) than previously available spherical glass lenses.
_
23. Free-form lenses are not only aspheric but are cut using a digital design manufacturing process that takes into consideration over 40,000 points across the lens enabling lenses to be produced with 0.01D power accuracy. Lighter and thinner than standard lenses they provide exceptional night/low light vision reducing glare and halo effects from car headlights. It also reduces lens aberrations to provide good vision across the whole curvature of the lens and avoid the optical distortions that can occur in the periphery area of vision with standard lenses.
_
24. Frames are chosen for looks, style, fashion and comfort. However, proper frames can improve vision. The vertex distance is distance from the back surface of the spectacle lens to the cornea of the eye. Increasing the vertex distance increases the effective power of a plus lens and decreases the effective power of a minus lens. Keeping the vertex distance of the lenses as short as possible will minimize magnification and its related effects. A frame with a smaller eye-size not only reduces thickness of your lenses and overall weight of your eyewear but also reduce lens aberrations especially in high prescriptions. A frame having optical center of lens corresponding to the center of pupil in both eyes will give best corrected vision. Frame should be chosen such that the optical center of your eyeglass lenses (the part that gives you the truest vision) should be directly in front of your pupils. The whole point of getting a PD (papillary distance) measurement is to have the optical center of the lens centered in front of the eye. If it is decentered, it induces prism that is unnecessary and it will create double vision and focusing problems.
_
25. Spectacles must be cleaned every day morning paying attention not only to lenses but also to the frames and earpieces, by running it under lukewarm water, cleaning with lather of mild household soap and then rinsing with lukewarm water, and drying with a clean, soft cotton cloth or clean micro-fiber cloth. Never wipe your lenses when they are dry otherwise your lenses will scratch. Avoid facial tissues or paper towels to clean lenses, as these products may scratch the lenses.
_
26. The biggest advantage of contact lens over spectacles (glasses) is the image size of contact lens is larger than spectacles similar to emmetropic eyes resulting in greater accuracy of vision. Contact lenses also provide better peripheral vision compared to spectacles. Unlike eyeglasses, contact lenses do not move around, and the distance between contact and eye remains a constant resulting in consistency of vision. Another benefit to wearing contact lenses is that there aren’t any weather conditions that can affect or limit your ability to function. Rain and cold weather can cause eyeglasses to fog up or distort vision with the moisture. Multifocal soft contact lenses have an additional advantage in being able to limit the increase in myopia.
_
27. Initial comfort is the only area where soft contact lenses excel over RGP (rigid gas permeable) contacts. RGP lenses are rated superior to soft lenses in most respects, especially quality of vision, eye health, ease of care/handling, durability and deposit resistance.
_
28. Clean and disinfect your contact lenses once a day. If you wear extended wear contacts, clean and disinfect the lenses as soon as you remove them unless they are disposable.
_
29. Patient education about care, wear and replacement of contact lens is the most important factor in contact lens use.
_
30. Wearing contact lenses increases the risk of corneal damage and eye infections. Complications due to contact lens wear affect roughly 5% of contact lens wearers each year. Long-term contact lens use can lead to increased corneal stromal thinning, increased corneal curvature and reduced corneal sensitivity.
_
31. If adequate vision and comfort can be achieved with eyeglasses or contact lenses; the risks and the imperfections involved with laser eye surgery does not justify the use of it. There is a tendency to trivialize LASIK as an “easy”, “completely machine dependent”, “anyone can do it” procedure. However, LASIK is a professional service and significant qualitative differences can and do exist among professionals. Who is doing laser eye surgery is the most important factor in reducing risks and imperfections. Laser eye surgery is highly recommended for military to decrease reliance of troops on corrective eyewear.
_
32. No lens (spectacle or contact) will ever refract all light rays as certain amount of rays will always be reflected or diffracted and therefore number of rays entering an unaided eye will always be more. This effect will be more pronounced in dim light or night as light rays are anyway scant; and therefore person with refractive error using any lens will never see as good as normal eye especially in dim light or night; not to mention that dim light/night worsen all refractive errors. If you are doing any job where work in dim light or night is on regular basis (commercial driver, pilot, security forces etc), the best option to correct any refractive error is laser eye surgery provided it is done with perfection without any complications.
_
33. Whether to wear eyeglasses or contact lenses or undergo laser eye surgery for correction of refractive error not only depends on the type & severity of refractive error, eye conditions, age, coexisting systemic diseases, but also depends on occupation, lifestyle, comfort, convenience, social stigma, budget and aesthetics.
_
34. Extreme myopia leads to minification (small eyes) and extreme hyperopia leads to magnification (large eyes) of eyeglass wearer’s eyes for observers resulting in social stigma and it can be avoided by wearing eyeglasses having aspheric/atoric lenses or wearing contact lenses.
_
35. Wearing eyeglasses by girls is still a stigma in some parts of the world (India, Pakistan) where girls are rejected for marriages as eyeglasses spoil their looks, and they are perceived to have weak eyes which will be passed on to their children.
_
36. About 50 to 90 percent of computer users suffer from visual symptoms of computer vision syndrome. Contact lens wearers are more likely to have computer vision syndrome symptoms than individuals who wear eyeglasses only or do not need corrective lenses.
_
37. Symptoms of computer vision syndrome include fatigue, headache, dry eyes, eyestrain, blurred vision and double vision while working on computer. If you do not have symptoms of computer vision syndrome, there is no need for computer glasses.
_
38. Computer users can prevent or reduce computer vision syndrome by proper lighting, minimizing glare, upgrading and adjusting computer display and exercising eyes including blinking more often.
_
39. Common eyeglasses correct either distance vision or near vision or both, but computer glasses correct intermediate zone of vision closer than driving (“distance”) vision, but farther away than reading (“near”) vision. Progressive lenses do have some lens power for intermediate vision and I myself use this intermediate zone for hours of computer work. If you are emmetropic (no refractive error), then use single vision computer glasses having lens power less than reading glass to relax the amount of accommodation required to keep objects in focus at the distance of the computer screen and provide the largest field of view. All computer glasses ought to have anti-reflective (AR) coatings to eliminate glare and may be lightly tinted to enhance contrast and block “blue” light emitted from computer screens that is associated with glare and eye strain.
_
40. New glasses must not be prescribed to correct refractive error when diabetes mellitus is uncontrolled as high blood sugar will change the refractive index of natural lens, alter media transparency and cause autofluorescence of lens/cornea resulting in fluctuation of refractive error needing frequent changes of glasses.
_
41. A wavefront in optics is a surface over which an optical disturbance has a constant phase. Rays and wavefronts are two mutually complementary approaches to light propagation. Wavefronts are always perpendicular to the rays. Refractive errors may be considered as low order aberrations of wavefronts that account for approximately 90% of the overall wavefront aberration in the eye. The most common technique to determine wavefront map of eye is Shack-Hartmann aberrometry. Wavefront customized lenses can be used in eyeglasses. Based on wavefront map of the eye and with the use of laser, a lens is shaped to compensate for the aberrations of the eye and then put in the eyeglasses. Wavefront customized contact lenses can theoretically correct high order aberrations like spherical aberration. Customized wavefront-guided refractive corneal laser treatments are designed to reduce existing aberrations and to help prevent the creation of new aberrations although wavefront guided LASIK failed to correct spherical aberration.
_
42. A revolutionary technology of electroactively focusing liquid crystal diffractive spectacle lenses will know where to focus and adaptively change their focusing power opening the way for a new generation of “smart” eyeglasses with built-in automatic focus; just like your auto-focusing camera.
_
43. Large numbers of people become blind each year due to complications of high myopia like macular degeneration and retinal detachment due to mechanical stretching and thinning of retina due to increased axial elongation (eye globe elongation). These complications would occur independent of correction of myopia and should not be confused with reversible blindness due to uncorrected refractive error; although uncorrected refractive error may lead to amblyopia resulting in irreversible blindness in childhood.
_
44. Best-corrected vision is visual acuity obtained with the best possible refractive correction. Presenting vision is visual acuity obtained with currently available refractive correction, if any. We are not living in ideal world where everyone has best corrected visual acuity. Best-corrected visual acuity excludes uncorrected refractive error as a cause of visual impairment, leading to substantial underestimation of the total visual impairment burden by about 38%. An individual may qualify as ‘not blind’ because their vision improves with refractive correction. However, in their daily living, their vision may be poor enough, due to uncorrected or under-corrected refractive error, that they qualify as ‘blind’ when measured according to their presenting visual acuity. Therefore, blindness is defined as presenting distance vision worse than 6/60 (20/200) in the better eye. Low vision is presenting distance vision worse than 6/18 (20/60), but at least 6/60 in the better eye. Vision impairment is presenting distance vision worse than 6/18 in the better eye (being the combination of low vision and blindness). Vision impairment caused by uncorrected or inadequately corrected refractive errors is defined as presenting visual acuity of less than 6/18 (20/60) in the better eye that could be improved to equal to or better than 6/18 by refraction or pinhole.
_
45. One of every 280 people in India (and other developing nations) is blind from uncorrected or inadequately corrected refractive error and it would be still higher if only old people are considered. Uncorrected refractive error is the second leading cause of blindness worldwide next to cataract. More than 2.3 billion people in the world have refractive error. Spectacles provide a safe and inexpensive solution to this problem. Nonetheless, estimated 670 million people worldwide do not have spectacles or have inadequate correction. Uncorrected refractive errors lead to visual impairment, which leads to limited education & employment, which leads to adverse socio-economic consequences, which leads to poverty and poor quality of life. Poverty and poor education prevents correction of refractive error. So we end up in a society of people having poor quality of life for generations. Poverty may be a cause of poor eye health and poor eye health may lead to or deepen poverty. The cycle of poverty and poor eye health will not end unless strong interventions and programs are implemented.
_
46. The global economy loses $202 billion annually as a result of lost productivity due to uncorrected refractive error.
_
47. There is a positive association between myopia and high intelligence. Whether myopes have better reading ability due to little strain on accommodation resulting in higher intelligence or whether myopes are gifted with higher intelligence or whether intelligent child reads more and become myopic or whether myopia is associated with higher intelligence independent of the number of hours read or whether intelligent parents would pass on intelligence to their child and additionally intense near-work environment of intelligent parents would also be shared by child resulting in intelligent myopic child; are matters of debate and research to untangle the relative importance of near work, heredity, and intellectual ability in the same subjects. Moreover, people who wear glasses appear intelligent & learned to others.
_
48. Uncorrected refractive errors do cause poverty, poor education and economy loss; and if myopes are indeed more intelligent, then refractive correction of myopia worldwide will lead to far better poverty eradication, far better education and far greater economy gains as higher intelligence is utilized by better vision.
__________
__________
Dr. Rajiv Desai. MD.
March 26, 2015
_________
Postscript:
One of the greatest inventions of all times is spectacles (glasses). Thousands of philosophers, monks, mathematicians, physicists, scientists, microscopists, astronomers, and chemists have all played vital role in developing this instrument. All their knowledge, expertise and hard work over 700 years cannot be integrated into one article; nonetheless I made a sincere attempt to do it. We are living in a world where cricketers and bollywood actors are eulogized by crowds; this article would serve as a breath of fresh air.
_________






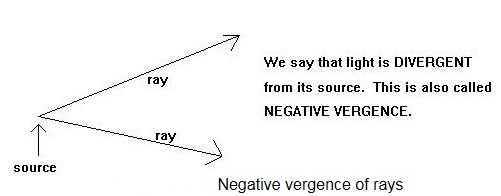
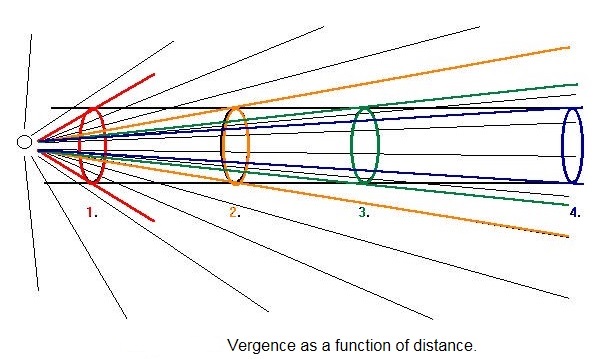
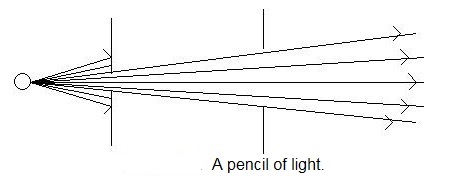
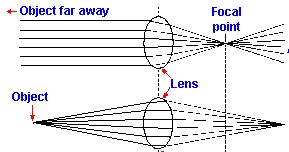
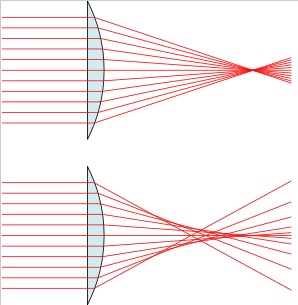
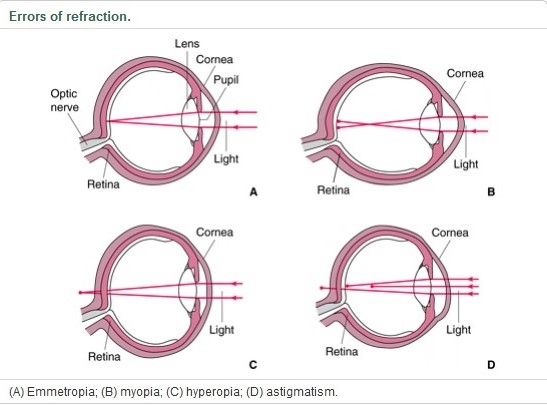
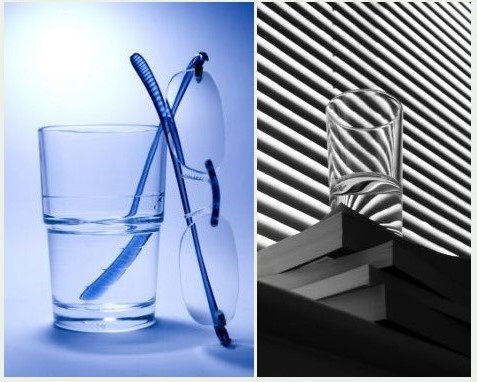
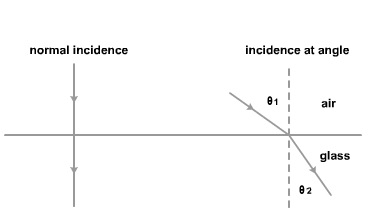
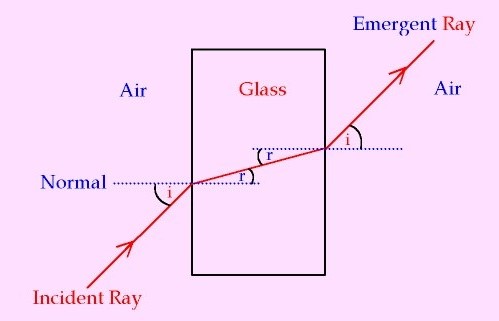

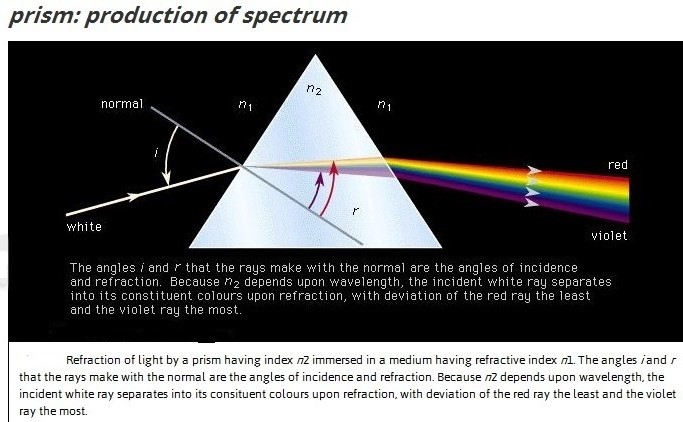
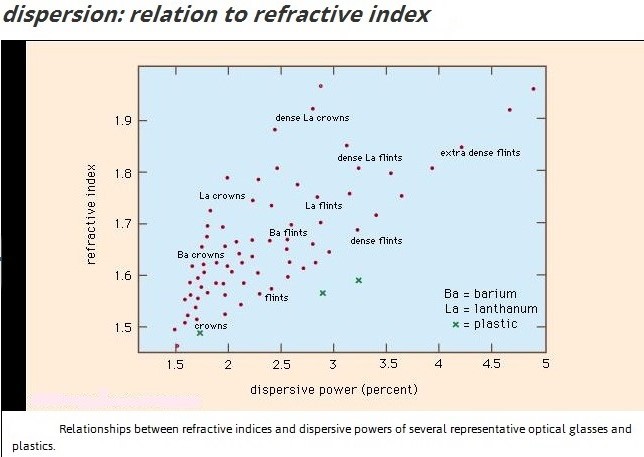
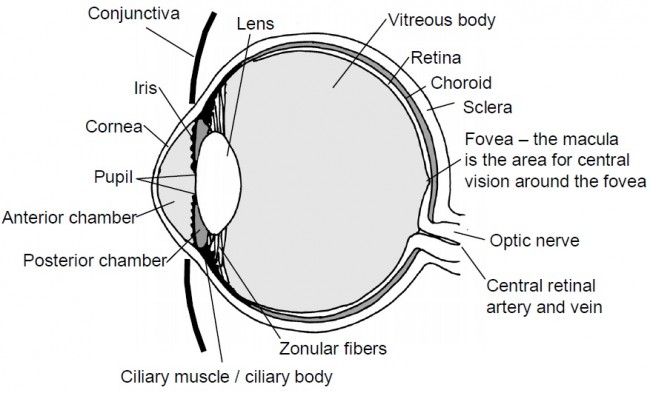
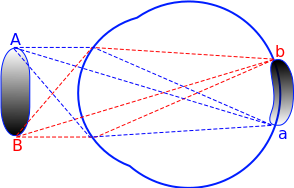
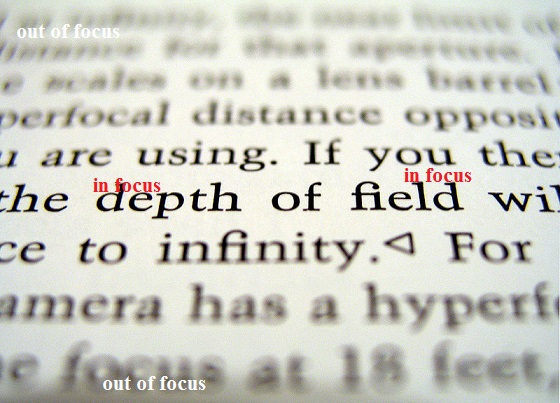
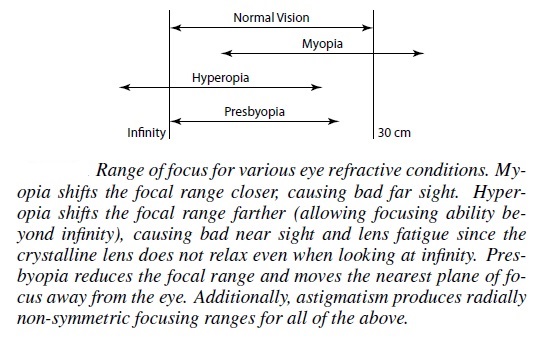
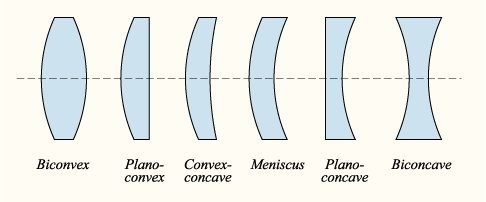
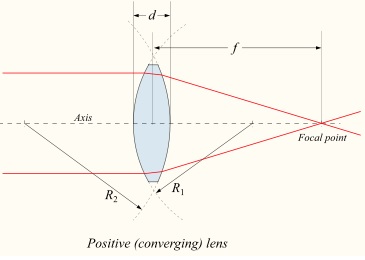
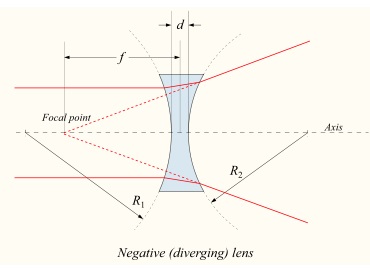
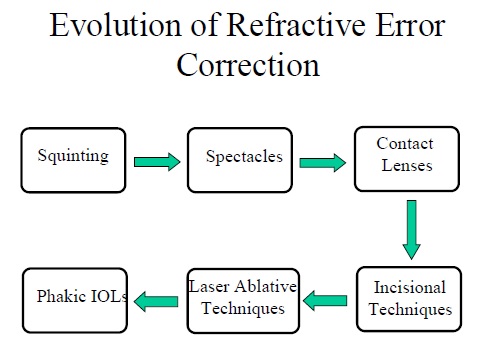
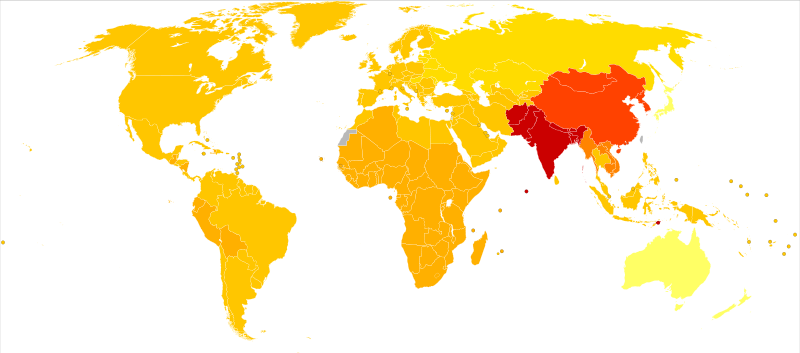
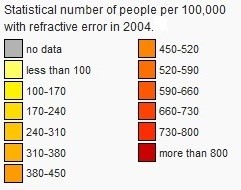
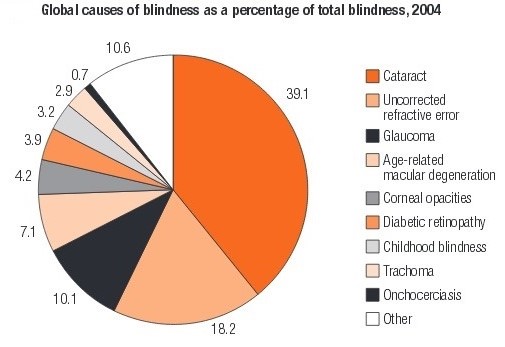
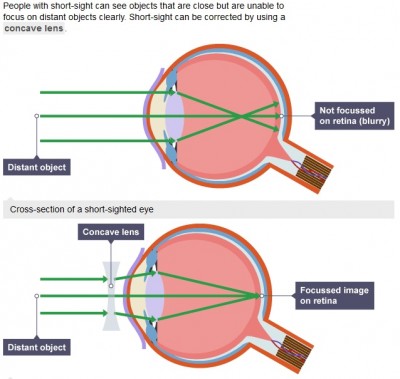
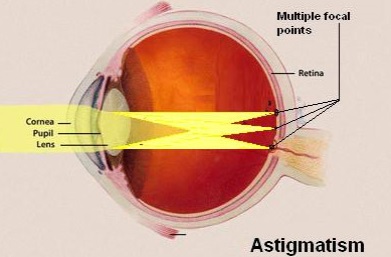
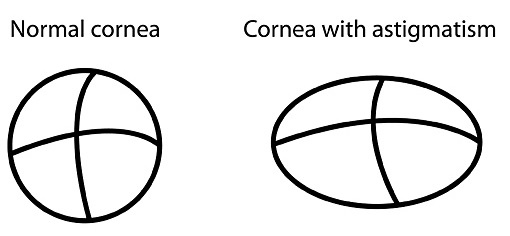
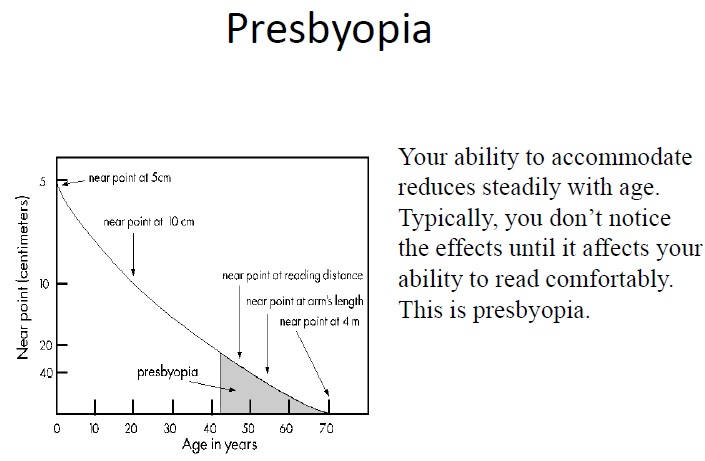
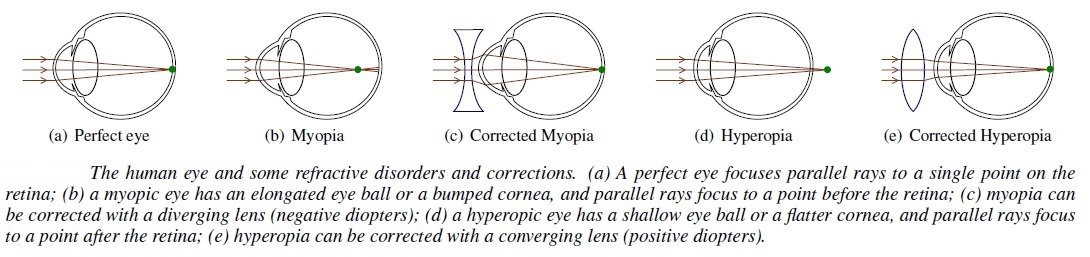
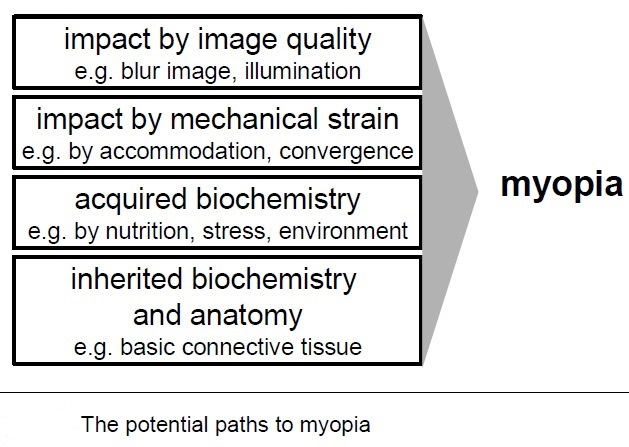
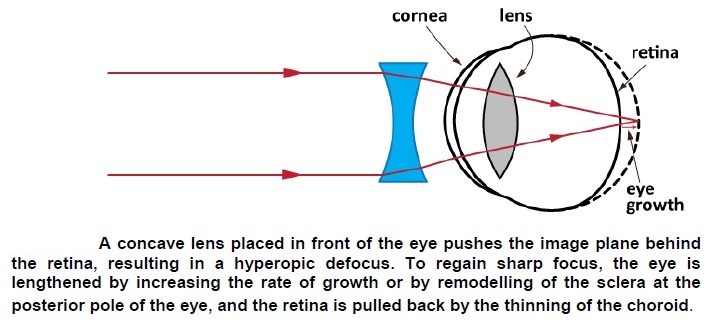
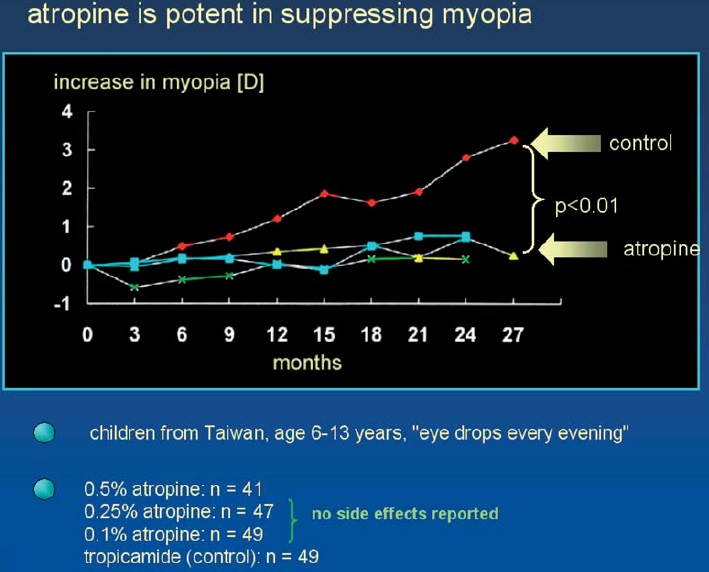
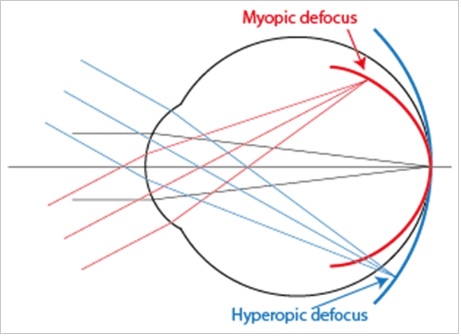

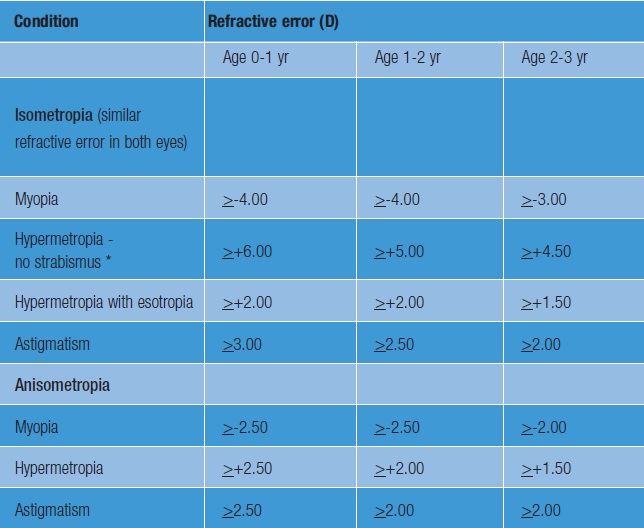
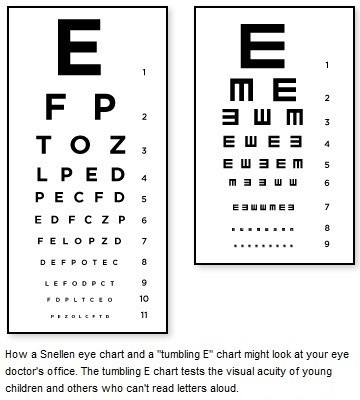
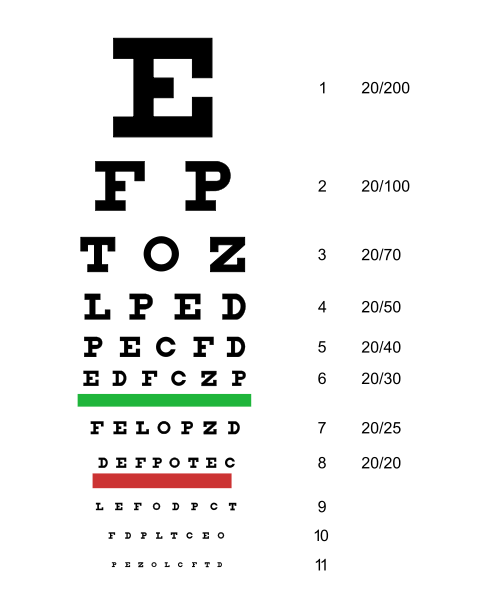
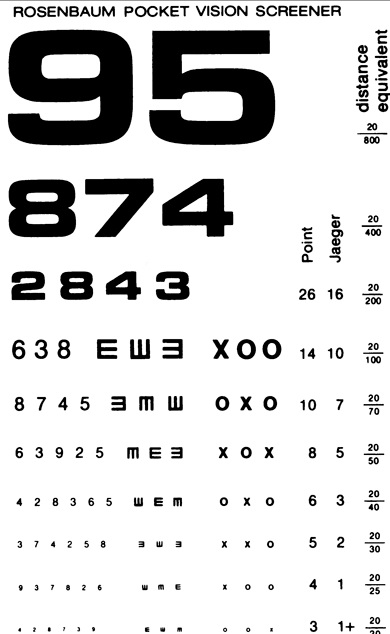
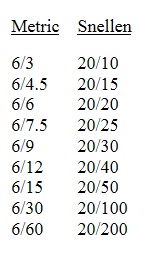
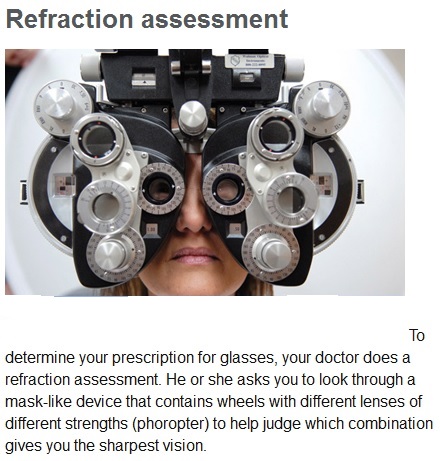
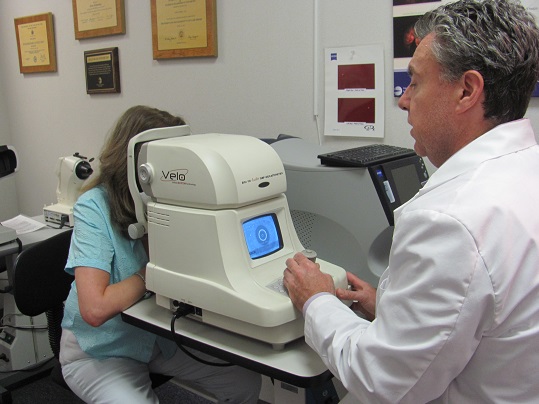

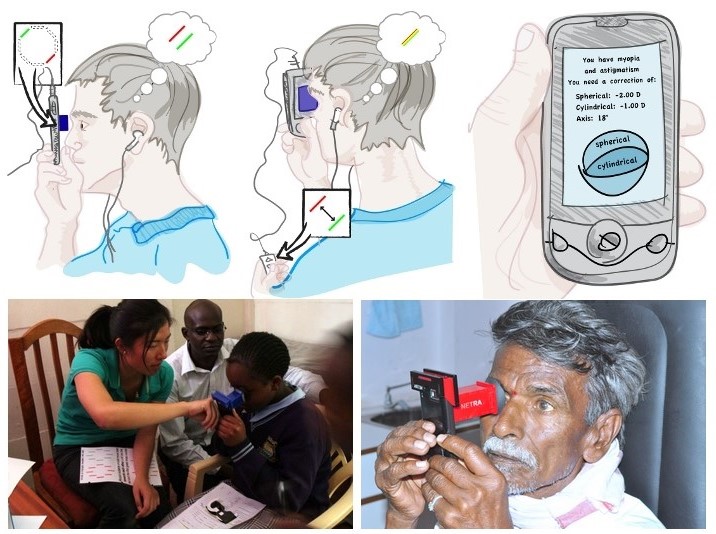
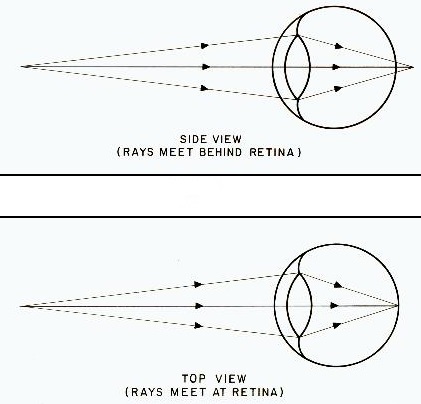
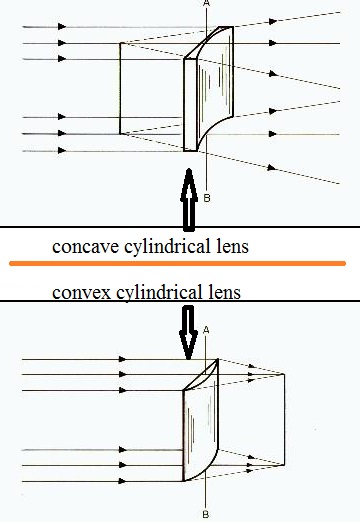
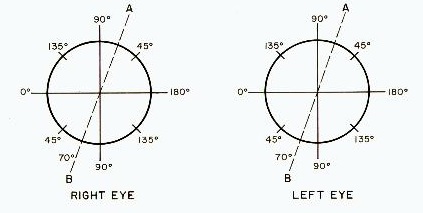
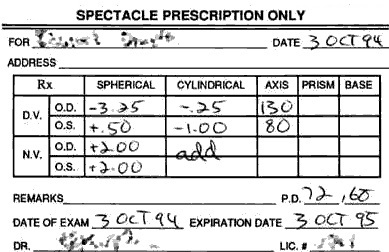
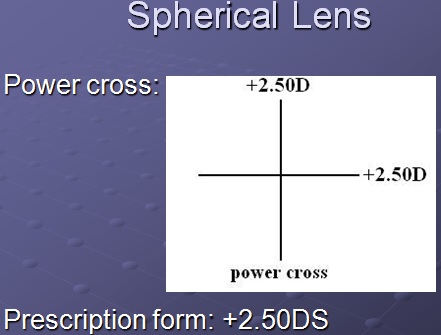
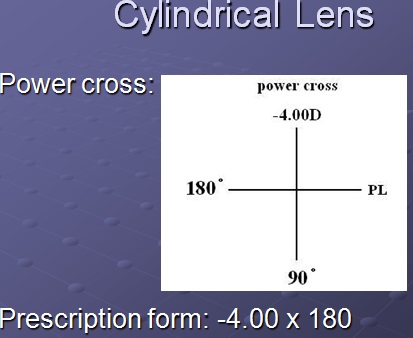
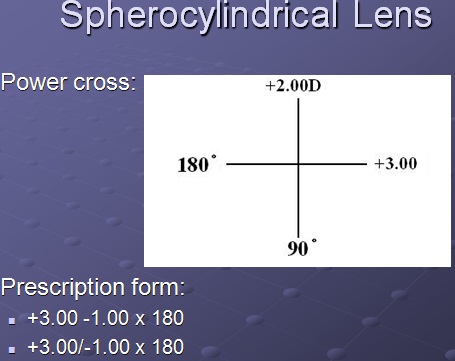
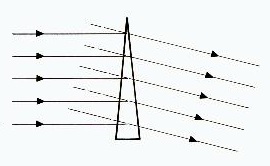



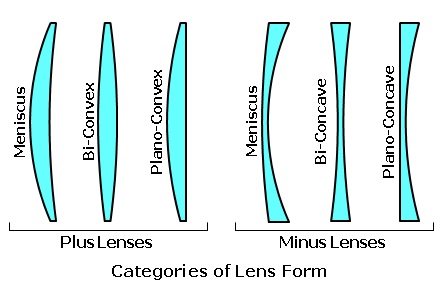
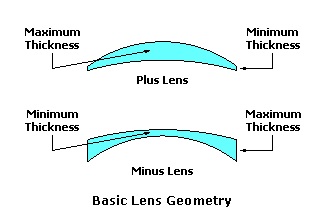
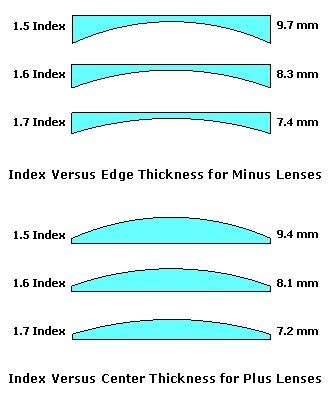
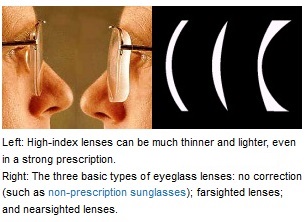
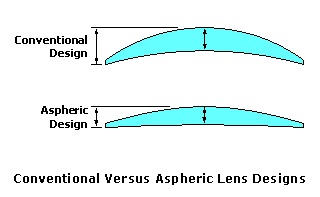
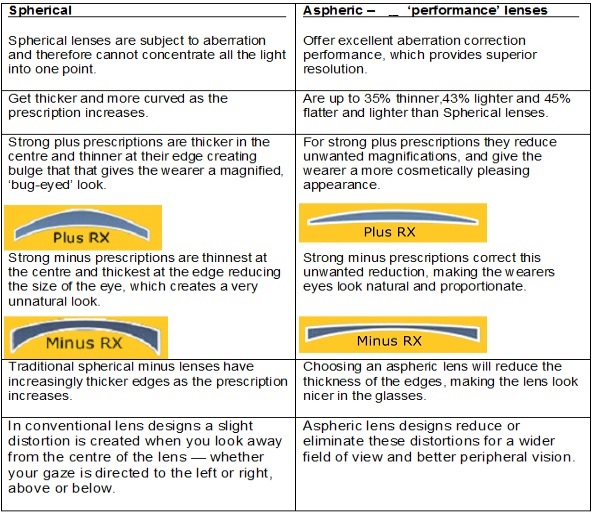
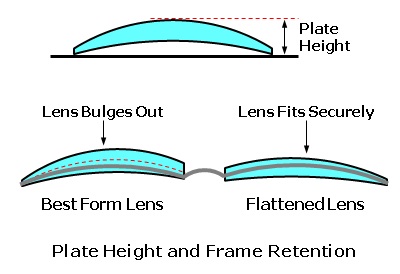
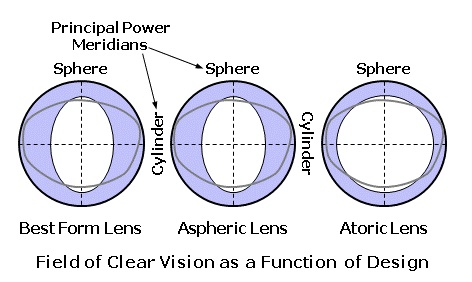

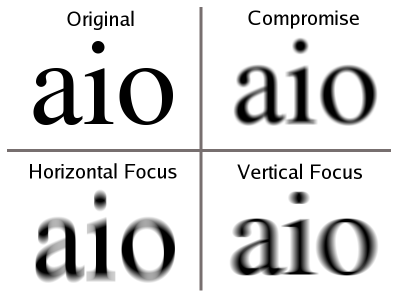
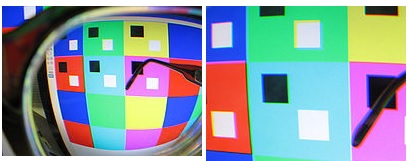
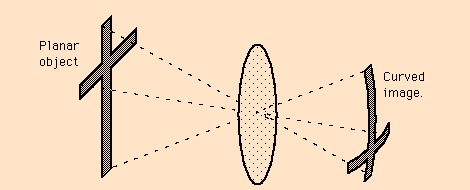
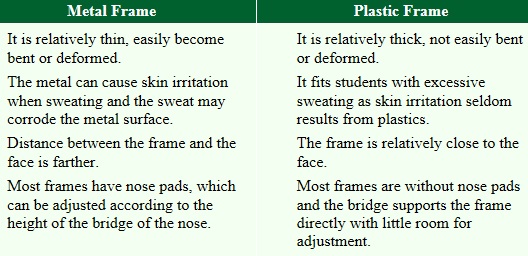
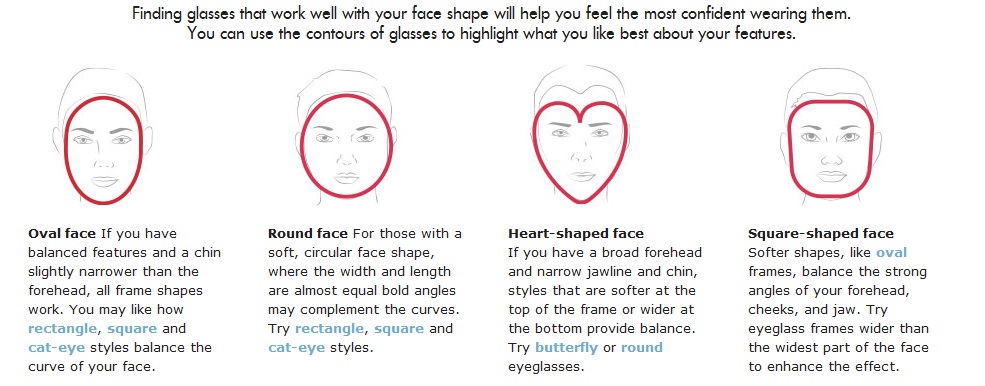
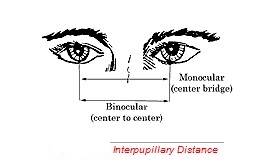
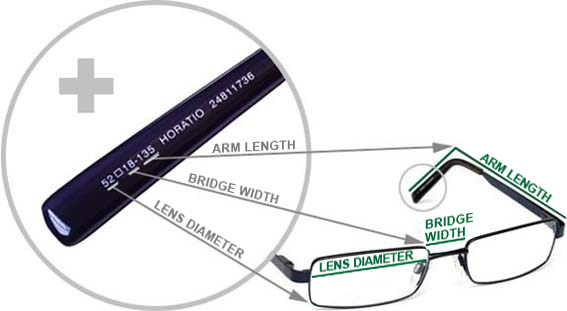



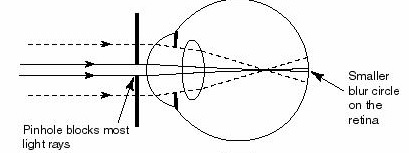
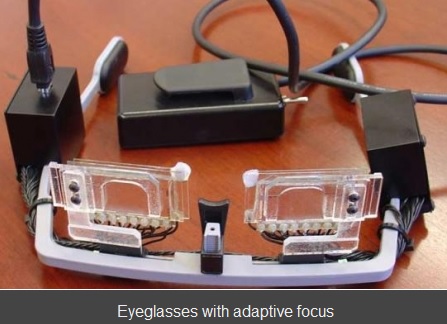

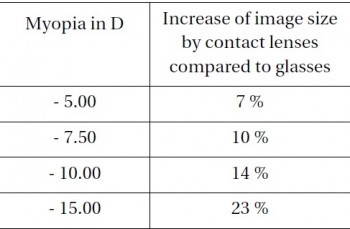


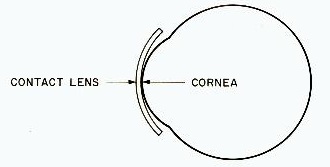
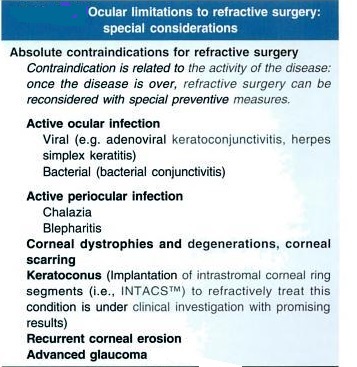
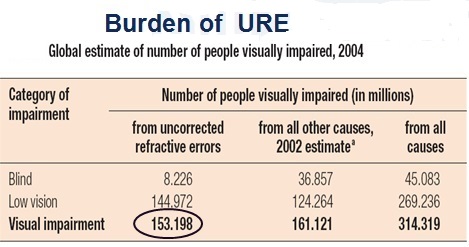
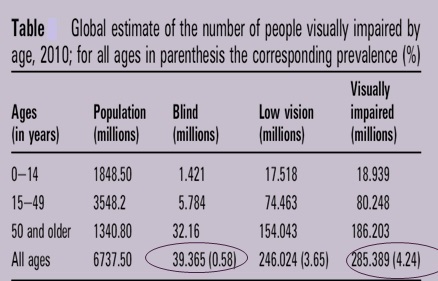
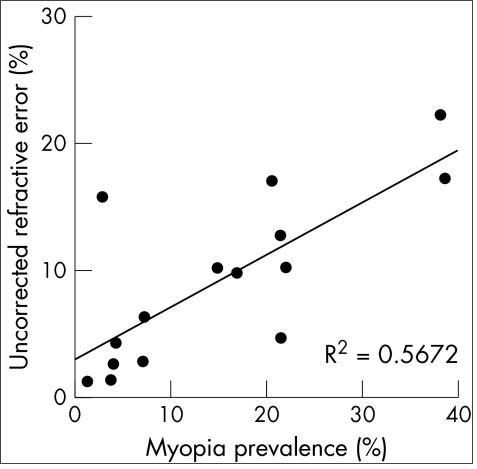
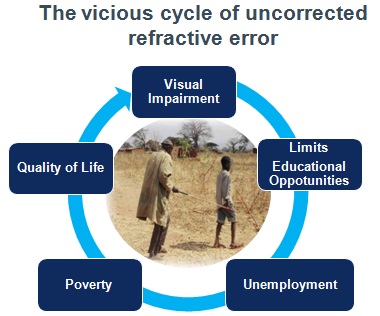
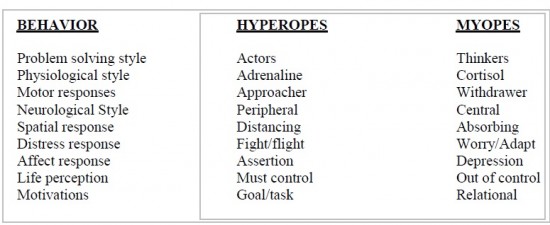
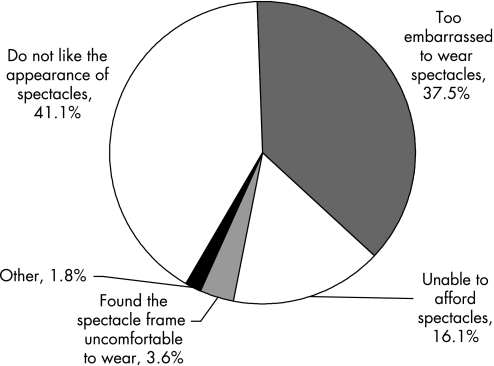
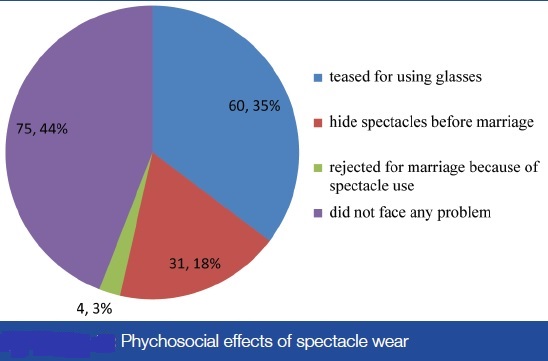
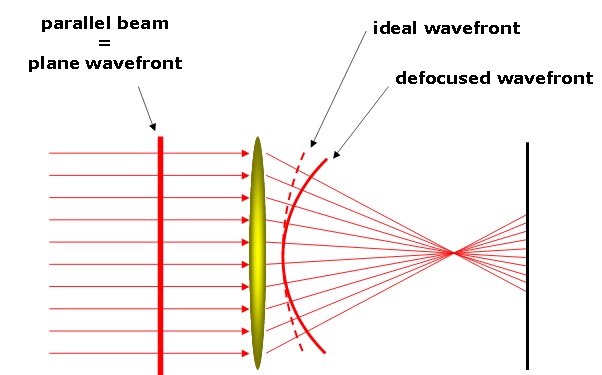
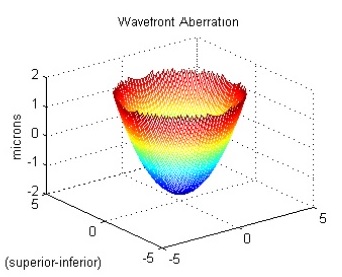
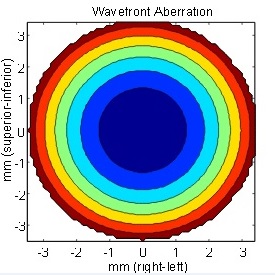
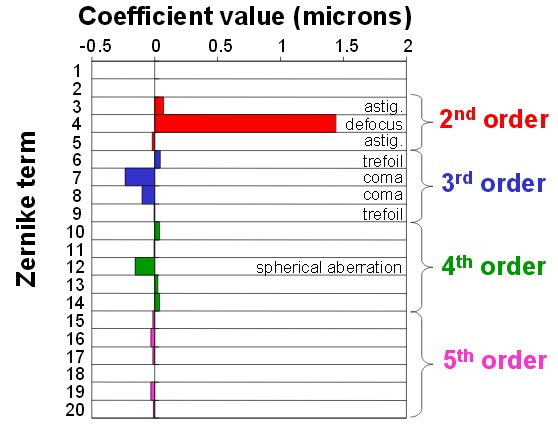
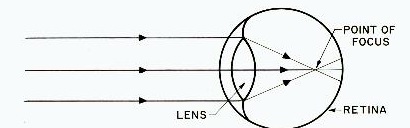
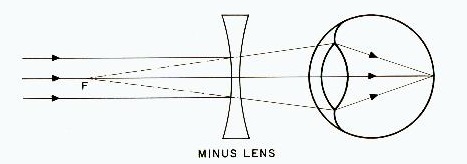
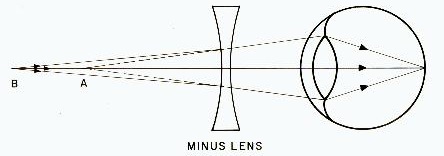
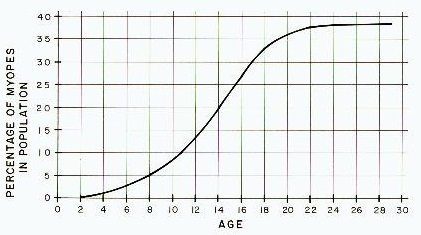
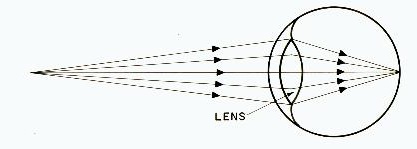
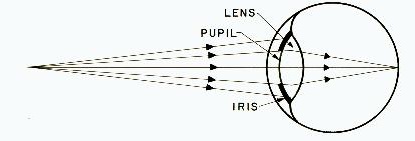
I was able to find good advice from your content.
Hi, I do think this is an excellent web site. I stumbledupon it 😉 I’m going to return once again since i have book-marked it. Money and freedom is the best way to change, may you be rich and continue to guide other people.
With havin so much written content do you ever run into any issues of plagorism or copyright violation? My site has a lot of exclusive content I’ve either authored myself or outsourced but it seems a lot of it is popping it up all over the web without my permission. Do you know any ways to help protect against content from being ripped off? I’d truly appreciate it.|
Great beat ! I would like to apprentice while you amend your web site, how can i subscribe for a blog website? The account helped me a acceptable deal. I had been a little bit acquainted of this your broadcast offered bright clear concept
Way cool! Some extremely valid points! I appreciate you penning this write-up and the rest of the website is extremely good.
I disagree with some of the conclusions, but it’s an interesting read nonetheless.
Wow, great blog post.Really thank you! Will read on…
Say, you got a nice blog.Thanks Again. Fantastic.
Greetings! This is my first comment here so I just wanted to give a quick shout out and say I genuinely enjoy reading through your blog posts. Can you recommend any other blogs/websites/forums that deal with the same subjects? Thanks!|
Appreciate you sharing, great post. Great.
This amazingness is a life changer!
What’s up, yes this piece of writing is truly nice and I have learned lot of things from it about blogging. thanks.
This is one awesome article.Much thanks again. Want more.
I really liked your blog. Cool.
Hello, after reading this amazing paragraph i am too cheerful to sharemy experience here with mates.
Highly energetic blog, I loved that a lot. Will there be a part 2?
Your article has proven useful to me.visit us at : https://www.lordophthal.com/
I couldn’t agree more- except I could!1!1! Haha
Wow! Thank you! I constantly wanted to write on my blog something like that. Can I include a portion of your post to my blog?
Thanks for the auspicious writeup. It in reality was a entertainment account it.
Glance complex to far brought agreeable from you!
By the way, how can we communicate?
I have read a few of the articles on your website now, and I really like your style of blogging. I added it to my favorites blog site list and will be checking back soon. Please check out my site as well and let me know what you think.
Everything is very open with a really clear explanation of the challenges. It was really informative. Your website is useful. Thanks for sharing!
I’m a retired MD in the US and wish I could get CME for your post, it is very educational. My question: does the increased corneal curve of myopia increase the angle of peripheral vision (axial eye size held constant)?
I simply could not go away your site prior to suggesting that
I actually loved the usual information a person supply to your
visitors? Is going to be back steadily in order to check up on new posts
I am impressed with this website , real I am a big fan .
Hi there, You have done a great job. I’ll certainly
digg it and personally suggest to my friends. I am confident they will be benefited
from this site.
Thanks for finally talking about >REFRACTIVE ERROR – Dr
Rajiv Desai <Liked it!
{Hello Dear, are you actually visiting this site on a regular basis, if so afterward you will definitely get nice experience.
Good write-up, I’m normal visitor of one’s website, maintain up the excellent operate, and It’s going to be a regular visitor for a long time.
Sometimes the better to simply take a stride back as well as recognize that not everybody gives your own beliefs
“A round of applause for your post.Thanks Again. Cool.”
Sounds certainly well thought out. Would it be ok to submit one or two questions? It’s just that..I can think of some other points that synergize with this.
Wow! This can be one particular of the most useful blogs We have ever arrive across on this subject. Basically Great. I am also a specialist in this topic so I can understand your effort.
Excellent article! We are linking to this particularly great article on our site. Keep up the good writing.
I like the nuance in this article, although I would like to see extra detail from you at some point.
This entry could detail so much more 🙁 Will you update it in the future?|
Quite well said, but a touch appeasing. Why?|
Is it okay if I ask you to elaborate? Could you show an additional example? Thanks!|