Dr Rajiv Desai
An Educational Blog
SELF MEASUREMENT OF BLOOD PRESSURE (SMBP):
SELF MEASUREMENT OF BLOOD PRESSURE (SMBP):
________
The figure above shows correct way to measure blood pressure at home.
_______
Prologue:
When the heart beats it generates a pressure in the arteries to pump blood around the body. In some people, the pressure generated is too high and this is called hypertension. Way back in 1981, Dr. R. C. Hansoti was head of cardiology department in Nair hospital, Mumbai and he was taking a clinic on hypertension for a group of medical students and I was one of the medical student attending his clinic. He asked a question to everybody: What are the symptoms of hypertension? Some said headache, some said giddiness and some said palpitation. When my turn came, I said hypertension has no symptoms. Dr. Hansoti was satisfied with my answer. He said that there is only one wise doctor among the crowd. I felt elated. Even today, I remember that incident. Most people aren’t aware that they have high blood pressure because there really are no symptoms. Death may be the first symptom of hypertension. That is why it’s been dubbed the silent killer. Untreated hypertension increases the risk of heart disease and stroke which are common causes of death worldwide. One in every three adults has high blood pressure. If you aren’t checking your blood pressure regularly, there’s no sure way to know if it’s within a healthy range. Often high blood pressure goes untreated until another medical condition arises or the individual goes in for a routine check-up. The only way to know that you have high blood pressure is to measure it clinically. There is no laboratory test or X-ray to detect hypertension. Approximately 100 years have passed since the legendary development by the Italian Riva Rocci to measure blood pressure by an upper arm cuff with the mercury manometer and since the first description of sound phenomena above the brachial artery by the Russian Korotkoff during upper arm compression. Blood pressure determination continues to be one of the most important measurements in all of clinical medicine and is still one of the most inaccurately performed. For decades, doctors and nurses used to measure blood pressure. Today, I will discuss self measurement of blood pressure (SMBP) by people themselves at their home/workplace/shopping mall.
______
Abbreviations and synonyms:
HT = hypertension
BP = blood pressure
SP = Systolic pressure =SBP
DP = Diastolic pressure = DBP
PP = Pulse pressure
MP = Mean pressure
SMBP = Self measurement (monitoring) of blood pressure [by patient or relative]
OMBP = Office (clinic) measurement (monitoring) of blood pressure [by doctor or nurse]
AMBP = Ambulatory measurement (monitoring) of blood pressure [by doctor or patient] = ABPM (ambulatory BP monitoring)
SMBP is also called HBPM (home blood pressure monitoring) or HBP (home BP); but since self measurement of blood pressure can be done outside home, I prefer SMBP over HBPM/HBP.
AOBP = automated office BP (BP taken in clinic with automated oscillometric validated device)
______
Note:
Self measurement of blood pressure (SMBP) is performed by adults only. There is no self measurement of blood pressure by children. If a child indeed has high/low blood pressure, it ought to be measured by doctor. Parents of hypertensive child can measure blood pressure of child at home provided they are trained and they have appropriate cuff size. In this article, blood pressure measurement means blood pressure measured by adults for adults, and arm means upper arm.
_______
The value of blood pressure among lay public:
My 27 years of experience as a physician tells me that blood pressure is highly overvalued physiological parameter by patients. Most lay public think that blood pressure is cornerstone of health. Tying the cuff and watching the mercury go up and down make them feel that the most vital parameter of their health is being investigated. The moment doctor says that BP is normal; they feel elated, happy and satisfied. Whether a person may be having a vertigo or terminal cancer, normal blood pressure assure them of wellbeing and good health. We doctors know that it is not true. You may have normal blood pressure during heart attack and die suddenly. On the other hand, your blood pressure may be elevated due to anxiety but you may be absolutely healthy. Paradoxically, there are many people having hypertension but never got BP measured as they have no symptoms. Also, there are many people who know that they have hypertension but refuse treatment as they have no symptoms. Also, there are many people who are on treatment for hypertension but their BP was never controlled. So lay public and BP have love-hate relationship.
_______
Introduction to SMBP:
Self measurement of blood pressure was introduced in the 1930s. A recent UK Primary Care survey showed 31% people self-measure blood pressure and out of them 60% self-measure at least monthly. In the USA, the use of self-BP monitoring is growing rapidly: Gallup polls suggest that the proportion of patients who report that they monitor their BP at home increased from 38% in 2000 to 55% in 2005. Because blood pressure monitors are now readily available and cheap (as little as £10; €11.8; $15), self monitoring is likely to increase—in the United States and Europe up to two thirds of people with hypertension do self-monitor. Home blood pressure monitoring is becoming increasingly important in the diagnosis and management of arterial hypertension. The rapid diffusion of this technique has been favoured by a number of factors, including technical progress and wider availability of SMBP devices, increasing awareness of the importance of regular BP monitoring, and recognition of the usefulness of SMBP by international hypertension management guidelines. Each person has roughly 100.000 single blood pressure values per day. That is why only regular measurements taken at the same daytime and over a longer period of time enable a useful evaluation of blood pressure values. Approximately one in three American adults have high blood pressure. Nearly third of adults with hypertension do not have their blood pressure under control. There is now a growing body of data that strategies in which anti-hypertensive therapy is titrated remotely by patients, as well as clinicians, using home blood pressure monitoring can be effective. As a result, connected blood pressure monitors could potentially have a meaningful impact on health outcomes.
_
The gold standard for clinical blood pressure measurement has always been readings taken by a trained health care provider using a mercury sphygmomanometer and the Korotkoff sound technique, but there is increasing evidence that this procedure may lead to the misclassification of large numbers of individuals as hypertensive and also to a failure to diagnose blood pressure that may be normal in the clinic setting but elevated at other times in some individuals. There are 3 main reasons for this: (1) inaccuracies in the methods, some of which are avoidable; (2) the inherent variability of blood pressure; and (3) the tendency for blood pressure to increase in the presence of a physician (the so-called white coat effect).
_
Numerous surveys have shown that physicians and other health care providers rarely follow established guidelines for blood pressure measurement; however, when they do, the readings correlate much more closely with more objective measures of blood pressure than the usual clinic readings. It is generally agreed that conventional clinic readings, when made correctly, are a surrogate marker for a patient’s true blood pressure, which is conceived as the average level over prolonged periods of time, and which is thought to be the most important component of blood pressure in determining its adverse effects. Usual clinic readings give a very poor estimate of this, not only because of poor technique but also because they typically only consist of 1 or 2 individual measurements, and the beat-to-beat blood pressure variability is such that a small number of readings can only give a crude estimate of the average level.
_
There is little point nowadays in simply classifying people as “hypertensive” or “non-hypertensive” purely on the basis of one blood pressure measurement – no matter by what means or how confidently it may have been made. For some applications (for example, in monitoring or researching the effect of antihypertensive medication on blood pressure) it is important to be confident about baselines and the changes that may occur with medication. For other applications such as assessing cardiovascular risk, additional factors are at least as important as the blood pressure measurement and choice of the means by which blood pressure is measured may be less critical.
_
There are potentially 3 measures of blood pressure that could contribute to the adverse effects of hypertension. The first is the average level, the second is the diurnal variation, and the third is the short-term variability. At the present time, the measure of blood pressure that is most clearly related to morbid events is the average level, although there is also evidence accumulating that suggests that hypertensive patients whose pressure remains high at night (nondippers) are at greater risk for cardiovascular morbidity than dippers. Less information is available for defining the clinical significance of blood pressure variability, although it has been suggested that it is a risk factor for cardiovascular morbidity.
_
The recognition of these limitations of the traditional clinic readings has led to two parallel developments: first, increasing use of measurements made out of the clinic, which avoids the unrepresentative nature of the clinic setting and also allows for increased numbers of readings to be taken; and second, the increased use of automated devices, which are being used both in and out of the office setting. This decreased reliance on traditional readings has been accelerated by the fact that mercury is being banned in many countries, although there is still uncertainty regarding what will replace it. The leading contenders are aneroid and oscillometric devices, both of which are being used with increasing frequency but have not been accepted as being as accurate as mercury.
_
High blood pressure is one of the most readily preventable causes of stroke and other cardiovascular complications. It can be easily detected, and most cases have no underlying detectable cause; the most effective way to reduce the associated risk is to reduce the blood pressure. Unlike many other common, chronic conditions, we have very effective ways of treating high blood pressure and we have clear evidence of the benefits of such interventions. However, despite a great deal of time and effort, hypertension is still underdiagnosed and undertreated. Furthermore, losses to follow up are high and are responsible for avoidable vascular deaths. Blood pressure is usually measured and monitored in the healthcare system by doctors or nurses in hospital outpatient departments and, increasingly, in primary care settings. New electronic devices have been introduced and validated in the clinical setting to replace the mercury sphygmomanometer and to overcome the large variations in measurement due to variability between observers. Ambulatory blood pressure monitoring is also being used more often to assess individuals’ blood pressures outside the clinical setting. Measuring blood pressure at home is becoming increasingly popular with both doctors and patients. Some national and international guidelines also recommend home monitoring in certain circumstances.
_
Hypertension is elevated blood pressure (BP) above 140 mm Hg systolic and 90 mm Hg diastolic when measured under standardized conditions. Hypertension can be a separate chronic medical condition estimated to be affecting a quarter of the world’s adult population, as well as a risk factor for other chronic and nonchronic patient groups. Traditional high-risk patient groups include diabetics, pregnant women with gestational diabetes or preeclampsia, and kidney disease patients. For chronic hypertensive patients, persistent hypertension is one of the key risk factors for strokes, heart attacks, heart and kidney failure, and other heart and circulatory diseases and increased mortality. Preeclampsia is the most common cause of maternal and fetal death. For gestational diabetes and preeclampsia patients, the accurate measurement of BP during pregnancy is one of the most important aspects of prenatal care. For kidney disease patients and diabetics, blood pressure should be kept below 130 mmHg systolic and 80 mm Hg diastolic to protect the kidneys from BP-induced damage. As there are usually no symptoms, frequent blood pressure controls are highly relevant for these high-risk groups. The level of the blood pressure is the main factor in the decision to start antihypertensive therapy and other interventions. It is thus vital that the measurements are obtained in a reliable manner. Measurements can be performed either at the clinic or in the home setting. In the clinical setting, patients often exhibit elevated blood pressure. It is believed that this is due to the anxiety some people experience during a visit to the clinic. This is known as the white coat effect and is reported to be affecting between 20% to 40% of all patients visiting a clinic. As a consequence, the current international guideline on BP measurement is to follow up on measurements obtained in the clinic using SMBP to negate the white coat effect.
________
History of BP measurement:
In the early 1700’s a British veterinarian demonstrated that blood was under pressure by inserting a tube into a horse’s artery and connecting it to a glass tube. He observed the blood rising in the vertical tube and concluded that it had pressure. It was not until 1847 that a human blood pressure was demonstrated but again by a catheter inserted directly into an artery. The blood would rise in the tube until the weight of the column of blood was equal to the pressure of the blood. Unfortunately, this required a tube 5 or 6 feet tall and, to be able to demonstrate hypertension, even 12 or 13 feet. Neither the invasive technique nor the huge column was practical. In 1881 Ritter von Basch developed a device to encircle the arm with pressure sufficient to obliterate the pulse in an artery beyond the cuff. Connected to a manometer (a pressure measuring device) one could read how much pressure was required to shut off the pulse. Intra-arterial measurement confirmed the accuracy. This method read only the systolic pressure. In 1896 Italian, Riva-Rocci, developed the prototype of the mercury sphygmomanometer used to this day. He reasoned that the very high column could be greatly shortened if a heavy liquid could be used. Fortunately, mercury (Hg) was available. A silvery liquid that is 13.6 times as heavy as water, mercury could shorten the column to less than a foot. Thus he connected the cuff wrapped around the arm to a glass column of mercury that showed the pressure in the cuff. The observer could then read how many millimeters of mercury were required to shut off the pulse below the cuff. The use of mercury is still the gold standard today and the millimeters of mercury still the units of pressure measurement (mm Hg) regardless of the type of apparatus used. A column of mercury of a specific height is a certain pressure no matter how you look at it. This design was brought to the United States by a neurosurgeon, Harvey Cushing, who was traveling through Italy at the time. Nikolai Korotkoff, who observed and described the sounds made by the heart pumping the blood beneath the cuff as it was deflated, made the final real advance in 1905. This required the use of a stethoscope to listen but was the first method to allow the diastolic pressure to be measured as well. In addition, the measurement of both systolic and diastolic pressures was more accurate and reliable than previous methods. It’s difficult to realize but we only began to take blood pressures about one hundred years ago. Thus the blood pressure unit of measurement today is still millimeters of mercury (mm Hg). The sounds we observe when taking a blood pressure are still called the Korotkoff sounds. This only requires the operator to deflate the cuff and observe at what pressure the Korotkoff sounds start and at what pressure they stop. These are the systolic and the diastolic pressures and are written for example as 120/80 or 120 over 80. Since Riva-Rocci invented indirect brachial cuff sphygmomanometry in 1896 and Korotkoff proposed the auscultatory method in 1905, the method for blood pressure (BP) measurements has remained essentially unchanged for the past 100 years. In 1969, Posey et al. identified mean BP on the basis of the cuff-oscillometric method. With subsequent theoretical and technical improvements, a newer method to determine systolic and diastolic BP was introduced to the cuff-oscillometric method. As a result, many of the automatic electronic sphygmomanometers available today have adopted this method, and those different from the auscultatory method have begun to be used in general clinical practice. Since the advent of indirect methods for sphygmomanometry, the past century has developed the practical and clinical sciences of hypertension. However, BP information necessary for the diagnosis and treatment of hypertension is still obtained essentially on the basis of casual measurements at the outpatient clinic (clinic BP). However, the reliability of clinic BP was called into question 40 years after the advent of indirect sphygmomanometry. In 1940, Ayman and Goldshine widely adopted the concept of self-BP measurements in the field of clinic BP measurements and demonstrated discrepancies between clinic BP and self-BP measurements. Bevan, in the United Kingdom, first reported the results of ambulatory BP monitoring using a direct arterial BP measurement method in 1969, and showed that human BP changes markedly with time. The quantity and quality of BP information vary greatly according to different methods, and the problem of interpreting clinic BP, which is obtained specifically in a medical environment, has been an issue in the clinical practice of hypertension during the past 50 years.
__________
Prevalence, harms and awareness of hypertension:
_
According to the National Health And Nutrition Examination Survey (NHANES), at least 65 million adult Americans, or nearly one-third of the US adult population, have hypertension, defined as a systolic blood pressure ≥140 mm Hg, diastolic blood pressure ≥90 mm Hg, and/or current use of antihypertensive medication. Another one-quarter of US adults have blood pressure in the “pre-hypertension” range, a systolic blood pressure of 120 to 139 mm Hg or diastolic blood pressure of 80 to 89 mm Hg, i.e., a level above normal yet below the hypertensive range. The prevalence of hypertension rises progressively with age, such that more than half of all Americans aged 65 years or older have hypertension.
_
The figure above shows prevalence of hypertension among adult population worldwide. It is estimated that one out of three adults has hypertension. Nearly 1 billion adults (more than a quarter of the world’s population) had hypertension in 2000 with a prevalence rate of 26.4 percent, and this is predicted to increase to 1.56 billion by 2025 and a prevalence rate of 29.2 percent. The prevalence rates in India are now almost comparable to those in the USA. While mean blood pressure has decreased in nearly all high-income countries, it has been stable or increasing in most African countries. Today, mean blood pressure remains very high in many African and some European countries. The prevalence of raised blood pressure in 2008 was highest in the WHO African Region at 36.8% (34.0–39.7).
__
Blood pressure levels, the rate of age-related increases in blood pressure, and the prevalence of hypertension vary among countries and among subpopulations within a country. Hypertension is present in all populations except for a small number of individuals living in primitive, culturally isolated societies. In industrialized societies, blood pressure increases steadily during the first two decades of life. In children and adolescents, blood pressure is associated with growth and maturation. Blood pressure “tracks” over time in children and between adolescence and young adulthood. Both environmental and genetic factors may contribute to regional and racial variations in blood pressure and hypertension prevalence. Studies of societies undergoing “acculturation” and studies of migrants from a less to a more urbanized setting indicate a profound environmental contribution to blood pressure. Obesity and weight gain are strong, independent risk factors for hypertension. It has been estimated that 60% of hypertensives are >20% overweight. Among populations, hypertension prevalence is related to dietary NaCl (salt) intake, and the age-related increase in blood pressure may be augmented by a high NaCl intake. Low dietary intakes of calcium and potassium also may contribute to the risk of hypertension. The urine sodium-to-potassium ratio is a stronger correlate of blood pressure than is either sodium or potassium alone. Alcohol consumption, psychosocial stress, and low levels of physical activity also may contribute to hypertension. Adoption, twin, and family studies document a significant heritable component to blood pressure levels and hypertension. Family studies controlling for a common environment indicate that blood pressure heritabilities are in the range 15–35%. In twin studies, heritability estimates of blood pressure are ~60% for males and 30–40% for females. High blood pressure before age 55 occurs 3.8 times more frequently among persons with a positive family history of hypertension. Despite improvements in the quality of health care and life expectancy, it is expected that the prevalence of hypertension will continue to rise worldwide.
_
Hypertension awareness:
_
From the above table, one can say that one third of adult population have HT in the U.S. Out of all hypertensive, one third are unaware that they have HT. Out of all hypertensive taking treatment, only one third are controlled.
_
40% of Adult Population Worldwide has Hypertension: 54 % of them unaware of hypertension:
Hypertension is truly a global epidemic, being highly prevalent in all communities worldwide, according to new data from the Prospective Urban Rural Epidemiology (PURE) study. Other findings show that awareness is very low and that once patients are aware, most are treated, but control is very poor. The prevalence of hypertension was lowest in lowest-income countries (around 30%) and highest in upper-middle-income economies (around 50%), with high-income and low-middle-income economies having an intermediate level (around 40%). Only 30% of the population had optimal blood pressure, with another 30% found to be in the pre-hypertension range. Of the 40% with hypertension, 46% of these individuals were aware of their condition, 40% were treated, but only 13% were controlled.
_
Risk and harm of hypertension:
_
The figure below shows that hypertension is the number one risk factor for death worldwide. Blood pressure is a powerful, consistent, and independent risk factor for cardiovascular disease and renal disease.
_
As per the World Health Statistics 2012, of the estimated 57 million global deaths in 2008, 36 million (63%) were due to noncommunicable diseases (NCDs). The largest proportion of NCD deaths is caused by cardiovascular diseases (48%). In terms of attributable deaths, raised blood pressure is one of the leading behavioral and physiological risk factor to which 13% of global deaths are attributed. Hypertension is reported to be the fourth contributor to premature death in developed countries and the seventh in developing countries. The World Health Organization ranks high BP as the third highest risk factor for burden of disease, highlighting the contribution of hypertension directly and indirectly to the development of numerous diseases. Hypertension has been identified as a major risk factor for cardiovascular disease, and is an important modifiable risk factor for coronary artery disease, stroke, peripheral vascular disease, congestive heart failure, and chronic kidney disease. The Global Burden of Diseases Study 2010 reported that hypertension is worldwide the leading risk factor for cardiovascular disease, causing 9.4 million deaths annually. Hypertension is a major contributor to the global morbidity burden with devastating downstream outcomes with heavy financial burden on scarce health resources.
_
Raised blood pressure is a major risk factor for coronary heart disease and ischemic as well as hemorrhagic stroke. Blood pressure levels have been shown to be positively and continuously related to the risk for stroke and coronary heart disease. In some age groups, the risk of cardiovascular disease doubles for each increment of 20/10 mmHg of blood pressure, starting as low as 115/75 mmHg. In addition to coronary heart diseases and stroke, complications of raised blood pressure include heart failure, peripheral vascular disease, renal impairment, retinal hemorrhage and visual impairment. Treating systolic blood pressure and diastolic blood pressure until they are less than 140/90 mmHg is associated with a reduction in cardiovascular complications. Effective control of blood pressure has been shown to significantly improve health outcomes and reduce mortality. Control of blood pressure has been shown to decrease the incidence of stroke by 35 to 40 percent, myocardial infarction by 20 to 25 percent and heart failure by more than 50 percent. A decrease of 5 mmHg in systolic BP is estimated to result in a 14 percent reduction in mortality due to stroke, a 9 percent reduction in mortality due to heart disease, and a 7 percent reduction in all-cause mortality.
_
The figure below shows correlation between HT and cardiovascular risk:
_
Data from numerous observational epidemiological studies provide persuasive evidence of the direct relationship between blood pressure and cardiovascular disease. In a recent meta-analysis that aggregated data across 61 prospective observational studies that together enrolled 958,074 adults, there were strong, direct relationships between average blood pressure and vascular mortality. These relationships were evident in middle-aged and older-aged individuals. Importantly, there was no evidence of a blood pressure threshold, that is, cardiovascular mortality increased progressively throughout the range of blood pressure, including the pre-hypertensive range. It has been estimated that ≈15% of blood pressure–related deaths from coronary heart disease occur in individuals with blood pressure in the pre-hypertensive range. Individual trials and meta-analyses of clinical trials have conclusively documented that antihypertensive drug therapy reduces the risk of cardiovascular events in hypertensive individuals. Such evidence provides strong evidence for current efforts to identify and treat individuals with hypertension and for parallel efforts to identify individuals with pre-hypertension, who are at risk for hypertension and blood pressure–related morbidity.
_______
Validity of self-reported hypertension:
Arterial hypertension is the main modifiable risk factor for coronary disease, cerebrovascular diseases, congestive cardiac insufficiency, and other cardiovascular diseases. The adequate treatment of arterial hypertension significantly reduces cardiovascular morbidity and mortality. Thus, knowledge of the distribution of hypertension among the population and the identification of vulnerable groups are of great interest to public health. To determine the prevalence of hypertension in the population is a complex task, which requires not only the measurement of arterial pressure, but also the verification of the use of medication for its control. Self-reported hypertension has been used in a number of health surveys, including the National Health and Nutrition Examination Survey (NHANES), in the United States, and the Pesquisa Nacional por Amostras de Domicílio (National Household Sample Survey – PNAD 98), in Brazil. The sensitivity and specificity of self reported hypertension found in various studies are about 71% and 90% respectively. Generally speaking, these results confirm the validity of self-reported hypertension among population. Since only 50 % hypertensives know that they have HT, SMBP by population at home would greatly increase HT detection, and consequently treatment and prevention of HT related morbidity and mortality.
________
Blood pressure measurement in low resource settings:
The treatment of hypertension has been associated with an approximate 40% reduction in the risk of stroke and 20% reduction in the risk of myocardial infarction. However, in developing countries the detection of major cardiovascular risk factors, such as hypertension, is often missed. Failure to identify hypertension is largely due to the unavailability of suitable blood pressure measurement devices and the limited attention paid to the techniques and procedures necessary to obtain accurate blood pressure readings.
_______
Basics of blood pressure:
The ejection of blood from the left ventricle of the heart into the aorta produces pulsatile blood pressure in arteries. Systolic blood pressure is the maximum pulsatile pressure and diastolic pressure is the minimum pulsatile pressure in the arteries, the minimum occurring just before the next ventricular contraction. Normal systolic/diastolic values are near 120/80 mmHg. Normal mean arterial pressure is about 95 mmHg.
_
Pressure pulse wave (pulse pressure wave):
Every heart beat generates pressure pulse wave transmitted over walls of aorta and major arteries.
_
The figure above shows aortic pulse pressure waveform. Systolic and diastolic pressures are the peak and trough of the waveform. Augmentation pressure is the additional pressure added to the forward wave by the reflected wave. The dicrotic notch represents closure of the aortic valve and is used to calculate ejection duration. Time to reflection is calculated as the time at the onset of the ejected pulse waveform to the onset of the reflected wave.
_
Energetics of flowing blood:
Because flowing blood has mass and velocity it has kinetic energy (KE). This KE is proportionate to the mean velocity squared (V2; from KE = ½ mV2). Furthermore, as the blood flows inside a vessel, pressure is exerted laterally against the walls of the vessel; this pressure represents the potential or pressure energy (PE). The total energy (E) of the blood flowing within the vessel, therefore, is the sum of the kinetic and potential energies (assuming no gravitational effects). Although pressure is normally considered as the driving force for blood flow, in reality it is the total energy that drives flow between two points (e.g., longitudinally along a blood vessel or across a heart valve). Throughout most of the cardiovascular system, KE is relatively low, so for practical purposes, it is stated that the pressure energy (PE) difference drives flow. Kinetic energy and pressure energy can be interconverted so that total energy remains unchanged. This is the basis of Bernoulli’s Principle. An interesting, yet practical application of Bernoulli’s Principle is found when blood pressure measurements are made from within the ascending aorta. The instantaneous blood pressure that is measured within the aorta will be very different depending upon how the pressure is measured. As illustrated in the figure below, if a catheter has an end-port (E) sensor that is facing the flowing stream of blood, it will measure a pressure that is significantly higher than the pressure measured by a side-port (S) sensor on the same catheter. The reason for the discrepancy is that the end-port measures the total energy of the flowing blood. As the flow stream “hits” the end of the catheter, the kinetic energy (which is high) is converted to potential (or pressure) energy, and added to the potential energy to equal the total energy. The side-port will not be “hit” by the flowing stream so kinetic energy is not converted to potential energy. The side-port sensor, therefore, only measures the potential energy, which is the lateral pressure acting on the walls of the aorta. The difference between the two types of pressure measurements can range from a few mmHg to more than 20 mmHg depending upon the peak velocity of the flowing blood within the aorta. So end pressure is higher than lateral pressure (blood pressure).
_
_
________
Regulation of blood pressure:
_
_
To provide a framework for understanding the pathogenesis of and treatment options for hypertensive disorders, it is useful to understand factors involved in the regulation of both normal and elevated arterial pressure. Cardiac output and peripheral resistance are the two determinants of arterial pressure. Cardiac output is determined by stroke volume and heart rate; stroke volume is related to myocardial contractility and to the size of the vascular compartment. Peripheral resistance is determined by functional and anatomic changes in small arteries (lumen diameter 100–400 micron) and arterioles. So any condition that increases cardiac output and/or peripheral resistance would increase blood pressure.
_
Blood is a fluid and fluid flows across pressure gradient. Blood pressure in arteries is higher than blood pressure in capillaries and blood pressure in capillaries is higher than blood pressure in veins. That is how blood flows from arteries to capillaries to veins. Blood pressure generates pressure gradient from heart to tissues and that is how tissues are perfused. When you are in shock with very low blood pressure, tissue perfusion is markedly reduced resulting in multi-organ failure and death if not treated.
________
Blood pressure measurement means arterial blood pressure measurement:
Blood pressure measurements have been part of the basic clinical examination since the earliest days of modern medicine. The origin of blood pressure is the pumping action of the heart, and its value depends on the relationship between cardiac output and peripheral resistance. Therefore, blood pressure is considered as one of the most important physiological variables with which to assess cardiovascular hemodynamics. Venous blood pressure is determined by vascular tone, blood volume, cardiac output, and the force of contraction of the chambers of the right side of the heart. Since venous blood pressure must be obtained invasively, the term blood pressure most commonly refers to arterial blood pressure, which is the pressure exerted on the arterial walls when blood flows through the arteries. The highest value of pressure, which occurs when the heart contracts and ejects blood to the arteries, is called the systolic pressure (SP). The diastolic pressure (DP) represents the lowest value occurring between the ejections of blood from the heart. Pulse pressure (PP) is the difference between SP and DP, i.e., PP = SP – DP.
The period from the end of one heart contraction to the end of the next is called the cardiac cycle. Mean pressure (MP) is the average pressure during a cardiac cycle. Mathematically, MP can be decided by integrating the blood pressure over time. When only SP and DP are available, MP is often estimated by an empirical formula:
MP = DP + PP/3
Note that this formula can be very inaccurate in some extreme situations. Although SP and DP are most often measured in the clinical setting, MP has particular importance in some situations, because it is the driving force of peripheral perfusion. SP and DP can vary significantly throughout the arterial system whereas MP is almost uniform in normal situations.
_
Unit of blood pressure measurement:
Pressure is force per unit area. Examples are pounds per square foot; newtons per square centimeter, tons per square yard, etc. Other units are atmospheres (atm) and Pascals (Pa).
One Pascal = 1 N/m2 = 10-5 Bars
Atmospheric pressure is the force per unit area exerted on a surface by the weight of air above that surface in the atmosphere of Earth (or that of another planet). In most circumstances atmospheric pressure is closely approximated by the hydrostatic pressure caused by the weight of air above the measurement point.
A pressure of 1 atm can also be stated as:
= 1.01325 bar
= 101325 pascal (Pa) or 101.325 kilopascal (kPa)
= 1013.25 millibars (mbar, also mb)
= 760 torr
≈ 760.001 mm-Hg (millimeter mercury), 0 °C
So atmospheric pressure is about 760 mm Hg at sea level.
That means our human body is subjected to 760 mm Hg pressure by atmosphere.
Same units are used for blood pressure.
Blood pressure means lateral pressure exerted by column of blood over wall of blood vessel (aorta and major arteries for arterial blood pressure). Normal blood pressure in an adult human is 120/80 mm Hg. 120 is systolic blood pressure when heart is in systole (contracting forcefully) and 80 is diastolic blood pressure when heart is in diastole (relaxing). It cannot be overemphasized that atmospheric pressure by air over our body acts on blood column as well as blood vessel wall and therefore whatever blood pressure we are measuring is the pressure over and above atmospheric pressure. The blood pressure measurements are “relative pressure”, meaning the figures that we state are above atmospheric pressure. When we say blood pressure is 100 mmHg, that really means 100 mmHg higher than atmospheric pressure. It’s a gauge pressure, not an absolute pressure. The corresponding absolute pressure would be about 760 + 100 mmHg. It is the atmospheric pressure that forces air into your lungs and compresses your body. That’s why it’s supposed that a human in space would have the air sucked out of them – there’s no pressure whatsoever to keep air in your lungs. Alternatively, when you go underwater, for every 33 feet you dive you’re being squeezed by an additional atmosphere of pressure. Deep water diving can cause extreme changes in blood pressure levels. The amount of atmospheric pressure is increased dramatically, due to the pressure exerted by the water over the swimmer. This increased pressure forces an increase of blood pressure, which can be extremely dangerous to anyone with high blood pressure. Individuals with blood pressure problems should consult their physician prior to any deep water diving excursion, to avoid serious risks to their health. Astronauts are individuals who spend long periods of time in space, without gravity and the pressure exerted by the atmosphere. The greater the length of time spent outside of the Earth’s atmosphere, the more likely that the astronaut will experience fainting episodes upon their return to Earth. It is theorized that the increased atmosphere pressure puts a higher demand on the heart and it cannot keep up, which makes the blood pressure lower, which results in fainting.
_
The gradual accumulation of mercury on the sea bed and the increasing use of accurate validated automatic sphygmomanometers that do not use mercury, or cumbersome, and frequently inaccurate, auscultation is leading to the gradual withdrawal of mercury sphygmomanometers. If a mercury column is no longer used to measure blood pressure, should we continue to use mm Hg or should we switch to kPa? Doctors feel comfortable with the conventional mm Hg and not Kilo-Pascal or Bars.
_______
Manometer:
A ‘manometer’ is an instrument that uses a column of liquid to measure pressure, although the term is often used nowadays to mean any pressure measuring instrument.
_
Sphygmomanometer:
The word comes from the Greek sphygmos meaning pulse, plus the scientific term manometer (pressure meter). A sphygmomanometer consists of an inflatable cuff, a measuring unit (the mercury manometer, or aneroid gauge), and a mechanism for inflation which may be a manually operated bulb & valve or a pump operated electrically. It is always used in conjunction with a means to determine at what pressure blood flow is just starting, and at what pressure it is unimpeded. Manual sphygmomanometers are used in conjunction with a stethoscope. The usual unit of measurement of blood pressure is millimeters of mercury (mmHg) as measured directly by a manual sphygmomanometer. You do not need stethoscope in automated sphygmomanometer, where cuff inflation is done by electrically operated pump; and you have either microphone-filter combination to detect korotkoff sound or you have oscillometric technique which obviates korotkoff sound altogether. When using semi-automatic blood pressure monitors for measuring blood pressure, the cuff is inflated by hand using a pumping bulb. The device deflates automatically. Beyond this the blood pressure is evaluated and calculated the same way as it is done by full-automatic devices.
________
Variability of blood pressure:
Blood pressure can vary widely as seen in the figure below.
The main value of self monitoring is that it can provide more precise estimates of the true underlying mean blood pressure than traditional clinic measurements. The table below shows the increased precision in mean systolic blood pressure gained from additional measurements for up to two weeks.
_
In order to obtain an accurate evaluation of the blood pressure value, the number of measurements should be increased
Indeed, many medical studies have showed that the higher the number of blood pressure measurements the more reliable the precision will be. So the ambulatory blood pressure measurement during 24 hours is currently used. The other technique consists of measuring the blood pressure only a few times during the day, for a few days in a row. Physicians committees have proved that at least 15 measurements were necessary to appreciate the real value of the blood pressure.
These measurements must be collected in the same conditions to have an optimal reliability.
_
No matter which measurement device is used, blood pressure is always a variable haemodynamic phenomenon. Modification of the factors that influence variability is not always possible, but we can minimize their effect. When optimum conditions are not possible, this should be noted with the reading. The table below shows factors that influences blood pressure variability.
_
Blood pressure generally is higher in the winter and lower in the summer. That’s because low temperatures cause your skin blood vessels to narrow (vasoconstriction) to conserve heat — which increases blood pressure because more pressure is needed to force blood through your narrowed veins and arteries.
_
The figure below shows typical BP fluctuations during a day:
_____
High blood pressure vs. hypertension:
Well, hypertension and high blood pressure are two terms that are almost used interchangeably. The common layman is expected to assume that both hypertension and high blood pressure are one and the same thing. And yes, they are correct because the two are really similar! Hence, in ordinary day-to-day usage, people can interchange “hypertension” for “high blood pressure” and vice versa. However, in the medical setup, the story seems to be different. If you’re in good health, your blood pressure will fluctuate during the day, depending on your stress level, how much caffeine you’ve had, whether you’re exerting yourself and so on. Taking your blood pressure when you’ve just heard that your house has been burgled, or after you’ve lost your job will show that you have high blood pressure. That’s not necessarily dangerous. Causes of reversible high blood pressure are pain, anxiety, agitation, hypoxia, hypercarbia and urinary bladder distention. Reversible high blood pressure is not hypertension. When your blood pressure stays high for a long time, you have hypertension. In the strictest sense, there should be a clear distinction between hypertension and high blood pressure. By definition, “hypertension” is a medical condition of the cardiovascular system that is often chronic in nature. It is characterized by a persistent elevation of the blood pressure. The prefix “hyper” means “high” so “hypertension” is the opposite of “hypotension” (low blood pressure). What you have is a number above which you have a defined diagnosis — at least that’s how we tend to do this in medicine. And the numbers actually mean risk — the higher the blood pressure, the greater the risk — and the interesting thing is the risk begins to occur even at relatively normal blood pressure readings. So the higher you go, the worse off you’re going to be, from a blood pressure point of view. You must also remember that certain medical conditions can cause reversible hypertension like anemia, thyrotoxicosis etc. You correct anemia and thyrotoxicosis, the BP will come down.
_____
Defining Hypertension:
_
_
From an epidemiologic perspective, there is no obvious level of blood pressure that defines hypertension. In adults, there is a continuous, incremental risk of cardiovascular disease, stroke, and renal disease across levels of both systolic and diastolic blood pressure. The Multiple Risk Factor Intervention Trial (MRFIT), which included >350,000 male participants, demonstrated a continuous and graded influence of both systolic and diastolic blood pressure on coronary heart disease mortality, extending down to systolic blood pressures of 120 mmHg. Similarly, results of a meta-analysis involving almost 1 million participants indicate that ischemic heart disease mortality, stroke mortality, and mortality from other vascular causes are directly related to the height of the blood pressure, beginning at 115/75 mmHg, without evidence of a threshold. Cardiovascular disease risk doubles for every 20-mmHg increase in systolic and 10-mmHg increase in diastolic pressure. Among older individuals, systolic blood pressure and pulse pressure are more powerful predictors of cardiovascular disease than is diastolic blood pressure.
_
Clinically, hypertension may be defined as that level of blood pressure at which the institution of therapy reduces blood pressure–related morbidity and mortality. Current clinical criteria for defining hypertension generally are based on the average of two or more seated blood pressure readings during each of two or more outpatient visits. A recent classification recommends blood pressure criteria for defining normal blood pressure, pre-hypertension, hypertension (stages I and II), and isolated systolic hypertension, which is a common occurrence among the elderly as seen in the table below.
_
Blood pressure classification:
| Blood Pressure Classification | Systolic, mmHg | Diastolic, mmHg |
| Normal | <120 | and <80 |
| Pre-hypertension | 120–139 | or 80–89 |
| Stage 1 hypertension | 140–159 | or 90–99 |
| Stage 2 hypertension | ≥160 | or ≥100 |
| Isolated systolic hypertension | >140 | and <90 |
_
_
In children and adolescents, hypertension generally is defined as systolic and/or diastolic blood pressure consistently >95th percentile for age, sex, and height. Blood pressures between the 90th and 95th percentiles are considered pre-hypertensive and are an indication for lifestyle interventions.
_
Fetal blood pressure:
In pregnancy, it is the fetal heart and not the mother’s heart that builds up the fetal blood pressure to drive its blood through the fetal circulation. The blood pressure in the fetal aorta is approximately 30 mm Hg at 20 weeks of gestation, and increases to approximately 45 mm Hg at 40 weeks of gestation.
The average blood pressure for full-term infants:
Systolic 65–95 mm Hg
Diastolic 30–60 mm Hg
Remember, as human ages from infancy to adulthood to elderly, BP steadily rises. Clinic BP of 140/90 mm Hg is a cut off value for adult above which anti-HT treatment is advised. It may be advised at 135/85 mm Hg if person has diabetes or chronic kidney disease.
_
The figure below shows discrepancy between office (clinic) measurement of blood pressure (OMBP) and self measurement of blood pressure (SMBP) at home:
For SMBP, cut off value is 135/85 mm Hg in contrast to OMBP cut off value 140/90 mm Hg.
_
White-Coat Hypertension (WCH) or Isolated Office (Clinic) Hypertension:
_
_
Most patients have a higher level of anxiety, and therefore higher blood pressure, in the physician’s office or clinic than in their normal environment (as revealed by ambulatory monitoring or home blood pressure measurements), a phenomenon commonly called the white-coat effect. Several factors can increase this effect, such as observer-patient interaction during the measurement. The effect tends to be greatest in the initial measurement, but can persist through multiple readings by the doctor or nurse during the same visit. Whether the white-coat effect is due purely to patient anxiety about an office visit or to a conditioned response has been a point of interest in clinical studies. Regardless, it may result in the misdiagnosis of hypertension or in overestimation of the severity of hypertension and may lead to overly aggressive therapy. Antihypertensive treatment may be unnecessary in the absence of concurrent cardiovascular risk factors. “White-coat hypertension” or “isolated office hypertension” is the condition in which a patient who is not on antihypertensive drug therapy has persistently elevated blood pressure in the clinic or office (> 140/90 mm Hg) but normal daytime ambulatory blood pressure (< 135/85 mm Hg). Since patients may have an elevated reading when seen for a first office visit, at least several visits are required to establish the diagnosis. Multiple studies have suggested that white-coat hypertension may account for 20% to 25% of the hypertensive population, particularly in older patients, mainly women. Both white-coat hypertension and the white-coat effect can be avoided by using an automatic and programmable device that can take multiple readings after the clinician leaves the examination room. Its magnitude can be reduced (but not eliminated) by the use of stationary oscillometric devices that automatically determine and analyze a series of blood pressures over 15 to 20 minutes with the patient in a quiet environment in the office or clinic. Other health risk factors are often present and should be treated accordingly. In some patients, WCH may progress to definite sustained hypertension, and all need to be followed-up indefinitely with office and out-of-office measurements of blood pressure. Treatment with antihypertensive drugs may lower the office blood pressure but does not change the ambulatory measurement. This pattern of findings suggests that drug treatment of WCH is less beneficial than treatment of sustained hypertension. The so-called white coat hypertension may be associated with an increased risk of target organ damage (e.g., left ventricular hypertrophy, carotid atherosclerosis, overall cardiovascular morbidity), although to a lesser extent than in individuals with elevated office and ambulatory readings.
_
A survey showed that 96% of primary care physicians habitually use a cuff size too small, adding to the difficulty in making an informed diagnosis. For such reasons, white coat hypertension cannot be diagnosed with a standard clinical visit. Ambulatory blood pressure monitoring and patient self-measurement using a home blood pressure monitoring device is being increasingly used to differentiate those with white coat hypertension or experiencing the white coat effect from those with chronic hypertension. Ambulatory monitoring has been found to be the more practical and reliable method in detecting patients with white coat hypertension and for the prediction of target organ damage. Even as such, the diagnosis and treatment of white coat hypertension remains controversial.
_
Masked Hypertension or Isolated Ambulatory Hypertension:
Somewhat less frequent than WCH but more problematic to detect is the converse condition of normal blood pressure in the office and elevated blood pressures elsewhere, e.g., at work or at home. Lifestyle can contribute to this, e.g., alcohol, tobacco, caffeine consumption, and physical activity away from the clinic. Target organ damage is related to the more prolonged elevations in pressure away from the physician’s office and the presence of such when the blood pressure is normal in the office can be a clue. There is also some evidence that such patients are at increased risk.
_
So in a nutshell, adult population is divided in four groups: true hypertensive, true normotensive, white coat HT and masked HT:
_____
Pseudo-hypertension:
When the peripheral muscular arteries become very rigid from advanced (often calcified) arteriosclerosis, the cuff has to be at a higher pressure to compress them. Rarely, usually in elderly patients or those with longstanding diabetes or chronic renal failure, it may be very difficult to do so. The brachial or radial artery may be palpated distal to the fully inflated cuff in these instances (positive Osler sign). The patients may be overdosed with antihypertensive medications inadvertently, resulting in orthostatic hypotension and other side effects. When suspected, an intra-arterial radial artery blood pressure can be obtained for verification. The Osler maneuver is not a reliable screen for pseudo-hypertension. The maneuver is performed by assessing the palpability of the pulseless radial or brachial artery distal to a point of occlusion of the artery manually or by cuff pressure. It was present in 7.2% of 3387 persons older than 59 years screened for the Systolic Hypertension in the Elderly Program (SHEP) study—more common in men, those found to be hypertensive, and those with a history of stroke. However, the Osler maneuver may be positive in the absence of pseudo-hypertension in one-third of hospitalized elderly subjects.
______
Orthostatic or Postural Hypotension:
Orthostatic hypotension is defined as a reduction of systolic blood pressure of at least 20 mm Hg or 10 mm Hg in diastolic blood pressure within 3 minutes of quiet standing. An alternative method is to detect a similar fall during head-up tilt at 60 degrees. This may be asymptomatic or accompanied by symptoms of lightheadedness, faintness, dizziness, blurred vision, neck ache, and cognitive impairment. Factors affecting this response to posture include food ingestion, time of day, medications, ambient temperature, hydration, deconditioning, standing after vigorous exercise, and age. If chronic, the fall of blood pressure may be part of pure autonomic failure, multiple system atrophy, associated with Parkinsonism or a complication of diabetes, multiple myeloma, and other dysautonomias. Patients with autonomic failure exhibit a disabling failure of control of many autonomic functions. The major life-limiting failure is inability to control the level of blood pressure, especially in those patients with orthostatic hypotension who concomitantly have supine hypertension. In these patients, there are great and swift changes in pressure so that the patients faint because of profound hypotension on standing and have very severe hypertension when supine during the night. Often the heart rate is fixed as well. The supine hypertension subjects them to life-threatening target organ damage such as left ventricular hypertrophy, coronary heart disease, flash pulmonary edema, heart failure, renal failure, stroke, and sudden death (presumably caused by central apnea or cardiac arrhythmias).
_______
Measurement of blood pressure:
_
Flow chart of blood pressure measurement is depicted in the figure below:
_
Location where BP is measured: clinic (office), home or ambulatory:
There are three clinical settings where blood pressure is measured. These are in an office (clinic) setting – office measurement of blood pressure (OMBP), an ambulatory setting – ambulatory measurement of blood pressure (AMBP) and at home –self measurement of blood pressure measurement (SMBP). SMBP can be done even outside home at work place or shopping mall etc.
_
_
The measurement of blood pressure is the commonest procedure carried out by doctors and nurses. The correct method of blood pressure measurement is crucial, particularly in patients with hypertension. There is marked intrinsic variability of blood pressure such that an observer even if careful and meticulous in adhering to recommended guidelines, obtain a value which will not be the same from one moment to the next or from one occasion to another. A failure to recognize such variability may result in a patient being falsely labeled as hypertensive or even normotensive and consequently being treated unnecessarily or not being treated.
_
Although the monitoring of antihypertensive treatment is usually performed using blood pressure readings made in the physician’s office and having a blood pressure check is by far the most common reason for visiting a physician, it is neither a reliable nor an efficient process. Thus, physician’s measurements are often inaccurate as a result of poor technique, often unrepresentative because of the white coat effect, and rarely include more than three readings made at any one visit. It is often not appreciated how big variations in blood pressure can be when measured in the clinic. In a study conducted by Armitage and Rose in 10 normotensive subjects, two readings were taken on 20 occasions over a 6-wk period by a single trained observer. The authors concluded that “the clinician should recognize that the patient whose diastolic pressure has fallen 25 mm from the last occasion has not necessarily changed in health at all; or, if he is receiving hypotensive therapy, that there has not necessarily been any response to treatment.” In addition, blood pressure can decrease by 10 mmHg or more within the time of a single visit if the patient rests, as shown by Alam and Smirk in 1943. There is also a practical limitation to the number or frequency of clinic visits that can be made by the patient, who may have to take time off work to make the visit. The potential utility of hypertensive patients having their blood pressures measured at home, either by using self-monitoring or by having a family member make the measurements, was first demonstrated in l940 by Ayman and Goldshine. They demonstrated that home blood pressures could be 30 or 40 mmHg lower than the physicians’ readings and that these differences might persist over a period of 6 month. Self monitoring has the theoretical advantage of being able to overcome the two main limitations of clinic readings: the small number of readings that can be taken and the white coat effect. It provides a simple and cost-effective means for obtaining a large number of readings, which are at least representative of the natural environment in which patients spend a major part of their day.
_
It is not uncommon for blood pressure to be much higher in a doctor’s office than in an out of office setting, the difference being referred to as “white coat effect”. Furthermore, considerably large amount of data indicates that out of office blood pressure whether recorded via ambulatory measurements or self at home is a better predictor of outcome than that measured by a doctor in a clinical setting. The normal values for the SMBP and AMBP are lower than the OMBP. The cut off blood pressure levels for the three settings are as follows:
Office Blood Pressure: 140/90mm Hg
Home Blood pressure: 135/85 mm Hg
Ambulatory Blood Pressure: Mean Daytime 135/85 mm Hg
Mean Night time 120/70 mm Hg
The diagnosis of hypertension in clinic setting is made if repeated measurements performed on three separate occasions when the systolic blood pressure is equal or greater than 140 mm Hg and the diastolic blood pressure is equal or greater than 90 mm Hg taken over a period of two months.
_
Problem with office (clinic) BP:
The accurate measurement of blood pressure (BP) remains the most important technique for evaluating hypertension and its consequences, and there is increasing evidence that the traditional office BP measurement procedure may yield inadequate or misleading estimates of a patient’s true BP status. The limitations of office BP measurement arise from at least four sources: 1) the inherent variability of BP coupled with the small number of readings that are typically taken in the doctor’s office, 2) poor technique (e.g., terminal digit preference, rapid cuff deflation, improper cuff, and bladder size), 3) the white coat effect and 4) the masked effect. Nearly 70 years ago there were observations made that office BP can vary by as much as 25 mm Hg between visits. The solution to this dilemma is potentially two-fold: by improving the office BP technique (e.g., using accurate validated automated monitors that can take multiple readings), and by using out-of-office monitoring to supplement the BP values taken in the clinical environment.
_
Out-of-office monitoring takes two forms at the present time: self (or home), and ambulatory BP monitoring. While both modalities have been available for 30 years, only now are they finding their way into routine clinical practice. The use of self-BP monitoring (also referred to as home BP monitoring) as an adjunct to office BP monitoring has been recommended by several national and international guidelines for the management of hypertension, including the European Society of Hypertension, the American Society of Hypertension (ASH), the American Heart Association (AHA), the British Hypertension Society, the European Society of Hypertension, the Japanese Hypertension Society, the World Health Organization – International Society of Hypertension, and the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7).
_
The practice and epidemiology of hypertension still depend entirely on BP information obtained in a medical environment (clinic BP/BP at a health examination), resulting in the accumulation of a great quantity of data about BP in a medical environment. For this reason, clinic BP remains the gold standard for the diagnosis and treatment of hypertension. However, data regarding AMBP or self-BP measurements at home (home BP) have also been accumulating for the past 30 years, and BP information, other than clinic BP, has been shown to have greater clinical significance than clinic BP. Many of these findings are the result of clinical and epidemiological studies. Essentially, as AMBP and home BP are accompanied by qualitative improvements and quantitative increases in information compared with clinic BP, they are considered to have greater clinical significance. For example, in AMBP by an indirect method widely used today, BP values can be obtained every 15 or 30 min on a particular day. Therefore, 50–100 BP values can be measured in the time course of one day. On the other hand, with home BP measurements, BP values are obtained at least at 2 time points in a day, that is, morning and evening, providing time-related BP information at 60 time points in a month. In addition to such definite increases in the quantity of information, BP information as a function of time leads to qualitative improvements. The application of the cuff-oscillometric method to sphygmomanometric devices associated with recent improvements in electronic technology and the clinical utilization of AMBP and home BP measurements are a paradigm shift in the history of the diagnosis and treatment of hypertension by indirect BP measurements.
_
Home blood pressure and average 24-h ambulatory blood pressure measurements are generally lower than clinic blood pressures. Because ambulatory blood pressure recordings yield multiple readings throughout the day and night, they provide a more comprehensive assessment of the vascular burden of hypertension than do a limited number of office readings. Increasing evidence suggests that home blood pressures, including 24-h blood pressure recordings, more reliably predict target organ damage than do office blood pressures. Blood pressure tends to be higher in the early morning hours, soon after waking, than at other times of day. Myocardial infarction and stroke are more common in the early morning hours. Nighttime blood pressures are generally 10–20% lower than daytime blood pressures, and an attenuated nighttime blood pressure “dip” is associated with increased cardiovascular disease risk. Recommended criteria for a diagnosis of hypertension are average awake blood pressure 135/85 mmHg and asleep blood pressure 120/70 mmHg. These levels approximate a clinic blood pressure of 140/90 mmHg.
_
_
How should we handle the difference between home and clinic readings?
Most home measurements of blood pressure are lower than those taken by a health professional in the office— a meta-analysis found that they differed by 6.9/4.9mm Hg and the difference varied with age and treatment. The British Hypertension Society suggests a “correction” factor in the order of 10/5 mm Hg. In one trial where antihypertensive drugs were titrated by someone who was blinded to whether the blood pressure results were from home or office readings, the home monitored group had worse blood pressure control because of lower prescription of all classes of drugs. This may have resulted from failure to account for the difference between home and office blood pressures. A systemic review aimed at ascertaining a diagnostic cut-off for hypertension for home measurements— defined as an office equivalent of 140/90 mm Hg— identified different thresholds of self monitored pressures of between 129/84 mm Hg and 137/89 mm Hg, depending on the method of comparison used. Recommendations from the US and Europe have settled on a threshold of 135/85 mm Hg. No studies have assessed morbidity and mortality outcomes from treating to a lower “home target,” but because home blood pressure is systematically lower than office readings it seems appropriate to adopt such a strategy.
______
Technique of BP measurement: direct or indirect:
_
Indirect Blood Pressure Measurement
Indirect measurement is often called noninvasive measurement because the body is not entered in the process. The upper arm, containing the brachial artery, is the most common site for indirect measurement because of its closeness to the heart and convenience of measurement, although many other sites may have been used, such as forearm or radial artery, finger, etc. Distal sites such as the wrist, although convenient to use, may give much higher systolic pressure than brachial or central sites as a result of the phenomena of impedance mismatch and reflective waves. An occlusive cuff is normally placed over the upper arm and is inflated to a pressure greater than the systolic blood pressure. The cuff is then gradually deflated, while a detector system simultaneously employed determines the point at which the blood flow is restored to the limb. The detector system does not need to be a sophisticated electronic device. It may be as simple as manual palpation of the radial pulse. The most commonly used indirect methods are auscultation and oscillometry.
Auscultatory Method:
The auscultatory method most commonly employs a mercury column, an occlusive cuff, and a stethoscope. The stethoscope is placed over the blood vessel for auscultation of the Korotkoff sounds, which defines both SP and DP. The Korotkoff sounds are mainly generated by the pulse wave propagating through the brachial artery. The Korotkoff sounds consist of five distinct phases. The onset of Phase I Korotkoff sounds (first appearance of clear, repetitive, tapping sounds) signifies SP and the onset of Phase V Korotkoff sounds (sounds disappear completely) often defines DP. Observers may differ greatly in their interpretation of the Korotkoff sounds. Simple mechanical error can occur in the form of air leaks or obstruction in the cuff, coupling tubing, or Bourdon gage. Mercury can leak from a column gage system. In spite of the errors inherent in such simple systems, more mechanically complex systems have come into use. The impetus for the development of more elaborate detectors has come from the advantage of reproducibility from observer to observer and the convenience of automated operation. Examples of this improved instrumentation include sensors using plethysmographic principles, pulse-wave velocity sensors, and audible as well as ultrasonic microphones. The readings by auscultation do not always correspond to those of intra-arterial pressure. The differences are more pronounced in certain special occasions such as obesity, pregnancy, arteriosclerosis, shock, etc. Experience with the auscultation method has also shown that determination of DP is often more difficult and less reliable than SP. However, the situation is different for the oscillometric method where oscillations caused by the pressure pulse amplitude are interpreted for SP and DP according to empirical rules.
Oscillometric Method:
In recent years, electronic pressure and pulse monitors based on oscillometry have become popular for their simplicity of use and reliability. The principle of blood pressure measurement using the oscillometric technique is dependent on the transmission of intra-arterial pulsation to the occluding cuff surrounding the limb. An approach using this technique could start with a cuff placed around the upper arm and rapidly inflated to about 30 mmHg above the systolic blood pressure, occluding blood flow in the brachial artery. The pressure in the cuff is measured by a sensor. The pressure is then gradually decreased, often in steps, such as 5 to 8 mmHg. The oscillometric signal is detected and processed at each step of pressure. The cuff pressure can also be deflated linearly in a similar fashion as the conventional auscultatory method. Arterial pressure oscillations are superimposed on the cuff pressure when the blood vessel is no longer fully occluded. Separation of the superimposed oscillations from the cuff pressure is accomplished by filters that extract the corresponding signals. Signal sampling is carried out at a rate determined by the pulse or heart rate. The oscillation amplitudes are most often used with an empirical algorithm to estimate SP and DP. Unlike the Korotkoff sounds, the pressure oscillations are detectable throughout the whole measurement, even at cuff pressures higher than SP or lower than DP. Since many oscillometric devices use empirically fixed algorithms, variance of measurement can be large across a wide range of blood pressures. Significantly, however, MP is determined by the lowest cuff pressure of maximum oscillations and has been strongly supported by many clinical validations.
_
_
How to diagnose Blood Pressure without a Blood Pressure Cuff:
Physicians normally use a blood pressure cuff, but patients can approximate their own blood pressures without a cuff.
Step 1:
Feel for a pulse at one of the carotid arteries. These arteries run through the neck, on either side of the voice box, or larynx. A palpable carotid pulse means the individual in question has a systolic, or pumping, pressure of 60-70 mmHg.
Step 2:
Feel for a pulse at one of the femoral arteries. These arteries are the major vessels that deliver blood to the tissues of the leg, and they run from the abdomen through each thigh. The femoral pulse is easiest to palpate in the crease between the thigh and the abdomen, a few inches to either side of the midline. Since the femoral artery is further from the heart than the carotid artery, blood pressure is lower in the femoral artery. Palpable femoral arteries mean the patient has at least a systolic pressure of 70-80 mmHg.
Step 3:
Feel for a pulse at one of the radial arteries. These run along the underside of the arm near the two bones of the forearm. It’s easiest to find the radial pulse by placing the fingers on the underside of the forearm before the arm meets the wrist, closer to the thumb side of the arm. Palpable radial pulses indicate that the patient has a systolic pressure of more than 80 mmHg. Because the radial artery is smaller than the femoral artery and is higher on the body, blood pressure must be higher than 80 mmHg for a pulse to reach the radial artery.
Warnings:
A 2000 article in the “British Medical Journal” notes that palpation-based blood pressure assessments may overestimate blood pressure slightly. Also, feel for pulses gently–overly compressing arteries can cause damage to tissues and may make it impossible to feel a pulse.
______
Direct Blood Pressure Measurement:
Direct measurement is also called invasive measurement because bodily entry is made. For direct arterial blood pressure measurement an artery is cannulated. The equipment and procedure require proper setup, calibration, operation, and maintenance. Such a system yields blood pressures dependent upon the location of the catheter tip in the vascular system. It is particularly useful for continuous determination of pressure changes at any instant in dynamic circumstances. When massive blood loss is anticipated, powerful cardiovascular medications are suddenly administered, or a patient is induced to general anesthesia, continuous monitoring of blood pressures becomes vital. Most commonly used sites to make continuous observations are the brachial and radial arteries. The femoral or other sites may be used as points of entry to sample pressures at different locations inside the arterial tree, or even the left ventricle of the heart. Entry through the venous side of the circulation allows checks of pressures in the central veins close to the heart, the right atrium, the right ventricle, and the pulmonary artery. A catheter with a balloon tip carried by blood flow into smaller branches of the pulmonary artery can occlude flow in the artery from the right ventricle so that the tip of the catheter reads the pressure of the left atrium, just downstream. These procedures are very complex and there is always concern of risk of hazard as opposed to benefit. Invasive access to a systemic artery involves considerable handling of a patient. The longer a catheter stays in a vessel, the more likely an associated thrombus will form. The Allen’s test can be performed by pressing on one of the two main arteries at the wrist when the fist is clenched, then opening the hand to see if blanching indicates inadequate perfusion by the other artery. However, it has proved an equivocal predictor of possible ischemia. In the newborn, when the arterial catheter is inserted through an umbilical artery, there is a particular hazard of infection and thrombosis, since thrombosis from the catheter tip in the aorta can occlude the arterial supply to vital abdominal organs. Some of the recognized contraindications and complications include poor collateral flow, severe hemorrhage diathesis, occlusive arterial disease, arterial spasm, and hematoma formation. In spite of well-studied potential problems, direct blood pressure measurement is generally accepted as the gold standard of arterial pressure recording and presents the only satisfactory alternative when conventional cuff techniques are not successful. This also confers the benefit of continuous access to the artery for monitoring gas tension and blood sampling for biochemical tests. It also has the advantage of assessing cyclic variations and beat-to-beat changes of pressure continuously, and permits assessment of short-term variations. Other exceptional cases where this method may also be employed include cases where the pressure is very high, but the patient does not exhibit any symptoms. This may be a case of calcified arteries, in which case, the pressure will not be recorded accurately with the help of a sphygmomanometer and a stethoscope.
_____
Blood pressure measurements in routine clinical practice:
Repeated office blood pressure measurements are mandatory in clinical practice to characterize precisely the blood-pressure-related cardiovascular risk of individual subjects. Precise recommendations are available to ensure standardized accurate measurements (O’Brien et al. 2003, Parati et al. 2008a), which until now have been obtained in most cases through the auscultatory technique making use of mercury or aneroid sphygmomanometers. Given the fact that aneroid manometers easily lose calibration, mercury manometers have been, until now, the recommended tools for auscultatory blood pressure readings, on which the conventional management of hypertensive patients has been based over the last 60-70 years. In more recent years an increasing use of home blood pressure monitoring and 24-hour ambulatory blood pressure monitoring has been observed (both based on oscillometric blood pressure measurements), aimed at complementing the information provided by office blood pressure measurements. This is based on the evidence of a stronger prognostic value of 24-hour ambulatory and home blood pressure monitoring as compared to isolated office readings (Parati et al. 2008b, Parati et al. 2009b, Verdecchia et al. 2009). A slow progressive increase in the use of oscillometric blood pressure measuring devices at the time of the office visit has been recently observed, although auscultatory readings are still preferred by physicians in most countries.
_
Reliable measurements of blood pressure depend on attention to the details of the technique and conditions of the measurement. Proper training of observers, positioning of the patient, and selection of cuff size are essential. Owing to recent regulations preventing the use of mercury because of concerns about its potential toxicity, most office measurements are made with aneroid sphygmomanometers or with oscillometric devices in western nations. These instruments should be calibrated periodically, and their accuracy confirmed. Before the blood pressure measurement is taken, the individual should be seated quietly in a chair (not the exam table) with feet on the floor for 5 min in a private, quiet setting with a comfortable room temperature. At least two measurements should be made. The center of the cuff should be at heart level, and the width of the bladder cuff should equal at least 40% of the arm circumference; the length of the cuff bladder should be enough to encircle at least 80% of the arm circumference. It is important to pay attention to cuff placement, stethoscope placement, and the rate of deflation of the cuff (2 mmHg/s). Systolic blood pressure is the first of at least two regular “tapping” Korotkoff sounds, and diastolic blood pressure is the point at which the last regular Korotkoff sound is heard. In current practice, a diagnosis of hypertension generally is based on seated, office measurements. Currently available ambulatory monitors are fully automated, use the oscillometric technique, and typically are programmed to take readings every 15–30 min. Twenty-four-hour ambulatory blood pressure monitoring more reliably predicts cardiovascular disease risk than do office measurements. However, ambulatory monitoring is not used routinely in clinical practice and generally is reserved for patients in whom white coat hypertension is suspected. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) has also recommended ambulatory monitoring for treatment resistance, symptomatic hypotension, autonomic failure, and episodic hypertension.
_______
Factors affecting blood pressure measurement:
It is important to be aware of the factors that affect blood pressure measurement:
(1) The technical skills of the observer;
(2) The inherent variability of blood pressure;
(3) The accuracy of the device, including its limitations and applications;
(4) The difficulty in measuring blood pressure in some special groups, e.g. the elderly, patients with arrhythmias, patients with a large arm, children, pregnant women.
The most important element in using auscultatory methods is the observer. All observers need adequate training in listening and recognising the correct sounds. Most common sources of error in many reports are mostly due to the observer, including poor hearing, difficulty/failure in interpreting the Korotkoff sounds and lack of concentration. Most serious errors involve the interpretation of the Korotkoff sounds and recognising diastolic pressure. Observers may be influenced by the subjects. For example, observers tend to be reluctant in diagnosing young healthy subjects as hypertensive or obese older persons as normotensive when the blood pressure is around 140/90 mmHg (systolic/diastolic blood pressure) resulting in a tendency to under read in the first case and over estimate in the latter. Observer-related issues include: prejudice and bias such as threshold avoidance; terminal digit preference; fast deflation, etc. (Beevers et al. 2001).
______
Location of Measurement vis-à-vis body part—Arm, Wrist, and Finger:
The standard location for blood pressure measurement is the upper arm, with the stethoscope at the elbow crease over the brachial artery, although there are several other sites where it can be performed. Monitors that measure pressure at the wrist and fingers have become popular, but it is important to realize that the systolic and diastolic pressures vary substantially in different parts of the arterial tree. In general, the systolic pressure increases in more distal arteries, whereas the diastolic pressure decreases. Mean arterial pressure falls by only 1 to 2 mm Hg between the aorta and peripheral arteries. Moreover, during the measurement, it is very important to place the site of measurement at the level of the heart because gravity is also another source of error. Indeed, if the subject takes its blood pressure upright, with an outstretched arm along the body, the blood pressure measured at the level of the arm could be raised on an average of 3 millimeters of mercury, whereas if it is measured at the level of the wrist, this increase could be of 15 millimeters of mercury, compared to the blood pressure measured in the aorta!
_
Three techniques of measuring blood pressure using a cuff: palpatory, auscultatory and oscillometric:
Blood pressure is measured noninvasively by occluding a major artery (typically the brachial artery in the arm) with an external pneumatic cuff. When the pressure in the cuff is higher than the blood pressure inside the artery, the artery collapses. As the pressure in the external cuff is slowly decreased by venting through a bleed valve, cuff pressure drops below systolic blood pressure, and blood will begin to spurt through the artery. These spurts cause the artery in the cuffed region to expand with each pulse and also cause the famous characteristic sounds called Korotkoff sounds. The pressure in the cuff when blood first passes through the cuffed region of the artery is an estimate of systolic pressure. The pressure in the cuff when blood first starts to flow continuously is an estimate of diastolic pressure. There are several ways to detect pulsatile blood flow as the cuff is deflated: palpation, auscultation over the artery with a stethoscope to hear the Korotkoff sounds, and recording cuff pressure oscillations. These correspond to the three main techniques for measuring blood pressure using a cuff.
_
Palpatory method using pneumatic cuff:
The brachial artery should be palpated while the cuff is rapidly inflated to about 30 mmHg above the point at which the pulse disappears; the cuff is then slowly deflated, and the observer notes the pressure at which the pulse reappears. This is the approximate level of the systolic pressure. Palpatory estimation is important, because phase I sounds sometimes disappear as pressure is reduced and reappear at a lower level (the auscultatory gap), resulting in systolic pressure being underestimated unless already determined by palpation. The palpatory technique is useful in patients in whom auscultatory endpoints may be difficult to judge accurately: for example, pregnant women, patients in shock or those taking exercise.
_
The radial artery is often used for palpatory estimation of the systolic pressure, but by using the brachial artery the observer also establishes its location before auscultation. In the palpatory method, the appearance of a distal pulse indicates that cuff pressure has just fallen below systolic arterial pressure.
_
Note:
Palpatory method must precede auscultatory method of BP determination by manual manometers using auscultatory technique.
________
Actual manual measurement of BP by auscultatory method:
_
_
The auscultatory method has been the mainstay of clinical blood pressure measurement for as long as blood pressure has been measured but is gradually being supplanted by other techniques that are more suited to automated measurement. The Auscultatory Method involves—Mercury, Aneroid, and Hybrid Sphygmomanometers. It is surprising that nearly 100 years after it was first discovered, and the subsequent recognition of its limited accuracy, the Korotkoff technique for measuring blood pressure has continued to be used without any substantial improvement. The brachial artery is occluded by a cuff placed around the upper arm and inflated to above systolic pressure. As it is gradually deflated, pulsatile blood flow is re-established and accompanied by sounds that can be detected by a stethoscope held over the artery just below the cuff. Traditionally, the sounds have been classified as 5 phases: phase I, appearance of clear tapping sounds corresponding to the appearance of a palpable pulse; phase II, sounds become softer and longer; phase III, sounds become crisper and louder; phase IV, sounds become muffled and softer; and phase V, sounds disappear completely. The fifth phase is thus recorded as the last audible sound. The sounds are thought to originate from a combination of turbulent blood flow and oscillations of the arterial wall. There is agreement that the onset of phase I corresponds to systolic pressure but tends to underestimate the systolic pressure recorded by direct intra-arterial measurement. The disappearance of sounds (phase V) corresponds to diastolic pressure but tends to occur before diastolic pressure determined by direct intra-arterial measurement. No clinical significance has been attached to phases II and III.
_
The Korotkoff sound method tends to give values for systolic pressure that are lower than the true intra-arterial pressure, and diastolic values that are higher. The range of discrepancies is quite striking: One author commented that the difference between the 2 methods might be as much as 25 mm Hg in some individuals. There has been disagreement in the past as to whether phase IV or V of the Korotkoff sounds should be used for recording diastolic pressure, but phase IV tends to be even higher than phase V when compared against the true intra-arterial diastolic pressure and is more difficult to identify than phase V. There is now general consensus that the fifth phase should be used, except in situations in which the disappearance of sounds cannot reliably be determined because sounds are audible even after complete deflation of the cuff, for example, in pregnant women, patients with arteriovenous fistulas (e.g., for hemodialysis), and aortic insufficiency. Most of the large-scale clinical trials that have evaluated the benefits of treating hypertension have used the fifth phase.
_
Auscultatory gap:
In older patients with a wide pulse pressure, the Korotkoff sounds may become inaudible between systolic and diastolic pressure, and reappear as cuff deflation is continued. This phenomenon is known as the auscultatory gap. In some cases, this may occur because of fluctuations of intra-arterial pressure and is most likely to occur in subjects with target organ damage. The auscultatory gap often can be eliminated by elevating the arm overhead for 30 seconds before inflating the cuff and then bringing the arm to the usual position to continue in the measurement. This maneuver reduces vascular volume in the limb and improves inflow to enhance the Korotkoff sounds. You can also approximate systolic BP by palpatory method and then inflate cuff 30 mm Hg above it and then deflate at 2mm/sec rate to determine accurate BP. By this way, you can avoid mistake of underestimating systolic BP due to auscultatory gap. The auscultatory gap is not an issue with nonauscultatory methods.
_
Measurement of BP manually by mercury sphygmomanometer:
_
Stethoscope:
A stethoscope should be of a high quality, with clean, well-fitting earpieces. The American Heart Association recommends using the bell of the stethoscope over the brachial artery, rather than placing the diaphragm over the antecubital fossa, on the basis that the bell is most suited to the auscultation of low-pitched sounds, such as the Korotkoff sounds. However, it probably does not matter much if the bell or diaphragm is used in routine blood pressure measurement, provided the stethoscope is placed over the palpated brachial artery in the antecubital fossa. As the diaphragm covers a greater area and is easier to hold than a bell, it is reasonable to recommend it for routine clinical measurement of blood pressure.
_
Position of manometer:
The observer should take care about positioning the manometer:
• The manometer should be no further than 1 meter away, so that the scale can be read easily.
• The mercury column should be vertical (some models are designed with a tilt) and at eye level. This is achieved most effectively with stand-mounted models, which can be easily adjusted to suit the height of the observer.
• The mercury manometer has a vertical scale and errors will occur unless the eye is kept close to the level of the meniscus. The aneroid scale is a composite of vertical and horizontal divisions and numbers, and must be viewed straight-on, with the eye on a line perpendicular to the centre of the face of the gauge.
_
Placing the cuff:
The cuff should be wrapped round the arm, ensuring that the bladder dimensions are accurate. If the bladder does not completely encircle the arm, its centre must be over the brachial artery. The rubber tubes from the bladder are usually placed inferiorly, often at the site of the brachial artery, but it is now recommended that they should be placed superiorly or, with completely encircling bladders, posteriorly, so that the antecubital fossa is easily accessible for auscultation. The lower edge of the cuff should be 2–3 cm above the point of brachial artery pulsation.
_
1. The patient should be relaxed and seated, preferably for several minutes, (at least 5 minutes). Ideally, patients should not take caffeine-containing beverages or smoke for two hours before blood pressure is measured.
2. Ideally, patients should not exercise within half an hour of the measurement being taken (National Nutrition Survey User’s Guide).
3. Use a mercury sphygmomanometer. All other sphygmomanometers should be calibrated regularly against mercury sphygmomanometers to ensure accuracy.
4. Bladder length should be at least 80%, and width at least 40% of the circumference of the mid-upper arm. If the Velcro on the cuff is not totally attached, the cuff is probably too small.
5. Wrap cuff snugly around upper arm, with the centre of the bladder of the cuff positioned over the brachial artery and the lower border of the cuff about 2 cm above the bend of the elbow.
6. Ensure cuff is at heart level, whatever the position of the patient.
7. Palpate the brachial pulse of the arm in which the blood pressure is being measured.
8. Inflate cuff to the pressure at which the brachial pulse disappears and note this value. Deflate cuff, wait 30 seconds.
9. Place the stethoscope gently over the brachial artery at the point of maximal pulsation; a bell endpiece gives better sound reproduction, but in clinical practice a diaphragm is easier to secure with the fingers of one hand, and covers a larger area. The stethoscope should be held firmly and evenly but without excessive pressure, as too much pressure may distort the artery, producing sounds below diastolic pressure. The stethoscope endpiece should not touch the clothing, cuff or rubber tubes, to avoid friction sounds.
10. The cuff should then be inflated rapidly to about 30 mmHg above the palpated systolic pressure and deflated at a rate of 2–3 mmHg per pulse beat (or per second), during which the auscultatory phenomena described below will be heard.
11. For recording the systolic reading, use phase I Korotkoff (the first appearance of sound). For diastolic pressure, use phase V Korotkoff (disappearance of sound).
12. When all sounds have disappeared, the cuff should be deflated rapidly and completely to prevent venous congestion of the arm before the measurements is repeated.
13. Wait for 30 seconds before repeating the procedure in the same arm. Average the readings. If the first two readings differ by more than 6 mm Hg systolic or if initial readings are high, take several readings after five minutes of quiet rest. I recommend ignoring the first reading altogether. Blood pressure should be taken at least once in both arms and the higher pressure subsequently used.
14. Leaving the cuff partially inflated for too long will fill the venous system and make the sounds difficult to hear. To avoid venous congestion, it is recommended that at least 30 seconds should elapse between readings. Conversely, if the sounds are difficult to hear initially, the veins can be emptied and the sound magnified if the patient raises the arm over the head with the cuff deflated. Milk the forearm down and inflate the cuff while the arm is still raised. Then quickly return the arm to the usual position and take the reading.
15. In the case of arrhythmias, additional readings may be required to estimate the average systolic and diastolic pressure. Isolated extra beats should be ignored. Note the rhythm and pulse rate.
_
The phases of sound during gradual deflation of cuff over brachial artery are shown in the table below and they were first described by Nicolai Korotkoff and later elaborated by Witold Ettinger.
_
Diastolic dilemma:
For many years, recommendations on blood pressure measurement have been equivocal as to the diastolic endpoint – the so-called ‘diastolic dilemma’. Phase IV (muffling) may coincide with, or be as much as, 10 mmHg greater than phase V (disappearance), but usually the difference is less than 5 mmHg. There has been resistance to general acceptance of the silent endpoint until recently, because the silent endpoint can be considerably below the muffling of sounds in some groups of patients, such as children, pregnant women, or anaemic or elderly patients. In some patients, sounds may even be audible when cuff pressure is deflated to zero. There is now a general consensus that disappearance of sounds (phase V) should be taken as diastolic pressure (as originally recommended by Korotkoff in 1910). When the Korotkoff sounds persist down to zero, muffling of sounds (phase IV) should be recorded for diastolic pressure, and a note made to this effect.
_
Inflation/Deflation System:
Indirect blood pressure measurement requires that occlusion of the brachial artery is produced by gradual inflation and deflation of an appropriately sized cuff. The tubing from the device to the cuff must be of sufficient length (70 cm or more) to allow for its function in the office setting. Successful inflation and deflation requires an airtight system; ongoing inspection and maintenance of the tubing for deterioration of the rubber (cracking) and the release valve are required. In my experience, air leakage from rubber tubing and bladder in cuff is the most common malfunction of manometer resulting in incorrect BP measurement.
_
Points to be noted while recording blood pressure:
The following points should be recorded with the blood pressure measurement [made to the nearest 2 mmHg without rounding-off to the nearest 5 or 10 mmHg (digit preference)]:
(i) position of the individual – lying, sitting or standing
(ii) the arm in which the measurement will be made– right or left
(iii) blood pressure in both arms on first attendance
(iv) arm circumference and inflatable bladder size
(v) phases IV and V for diastolic blood pressure
(vi) an auscultatory gap if present
(vii) state of the individual – e.g. anxious, relaxed
(viii) time of drug ingestion.
_
Effects of Body Position:
Blood pressure measurement is most commonly made in either the sitting or the supine position, but the two positions give different measurements. It is widely accepted that diastolic pressure measured while sitting is higher than when measured supine (by ≈5 mm Hg), although there is less agreement about systolic pressure. When the arm position is meticulously adjusted so that the cuff is at the level of the right atrium in both positions, the systolic pressure has been reported to be 8 mm Hg higher in the supine than the upright position. In the supine position, the right atrium is approximately halfway between the bed and the level of the sternum; thus, if the arm is resting on the bed, it will be below heart level. For this reason, when measurements are taken in the supine position the arm should be supported with a pillow. In the sitting position, the right atrium level is the midpoint of the sternum or the fourth intercostal space. Other considerations include the position of the back and legs. If the back is not supported (as when the patient is seated on an examination table as opposed to a chair), the diastolic pressure may be increased by 6 mm Hg. Crossing the legs may raise systolic pressure by 2 to 8 mm Hg.
_
Effects of Arm Position:
The position of the arm can have a major influence when the blood pressure is measured; if the upper arm is below the level of the right atrium (when the arm is hanging down while in the sitting position), the readings will be too high. Similarly, if the arm is above the heart level, the readings will be too low. These differences can be attributed to the effects of hydrostatic pressure and may be 10 mm Hg or more, or 2 mm Hg for every inch above or below the heart level. Hydrostatic pressure is the pressure exerted by a fluid at equilibrium at a given point within the fluid, due to the force of gravity. Hydrostatic pressure increases in proportion to depth measured from the surface because of the increasing weight of fluid exerting downward force from above. The gravity affects blood pressure via hydrostatic forces (e.g. during standing).
_
Other physiological factors that may influence the blood pressure during the measurement process include muscle tension. If the arm is held up by the patient (as opposed to being supported by the observer), the isometric exercise will raise the pressure. BP should be measured by keeping the arm cuff at heart level, with extension of the lower arm, and relaxation of the arm by means of a supporting pillow.
_
Cuff:
A soft arm cuff is usually recommended. In subjects with standard proportions, a hard plastic cuff is also applicable. In subjects with excessively thick or thin arms, large cuffs or small cuffs, respectively, should be used.
A) Site for cuff:
The cuff oscillometric principle is applicable to any site where an arterial pulse is available. However, the standard site for BP measurements is the upper arm, and several issues arise when BP is measured at sites other than the upper arm. At present, three types of electrical devices for home BP measurements are commercially available: the arm-cuff device, the wrist-cuff device and the finger-cuff device. In 1999, 7 million of these electrical devices were produced in the Far East (including Japan, Korea and Taiwan). Of those, 35% were wrist-cuff devices. Previously, finger-cuff devices commanded a considerable portion of the market share owing to their convenience and ease of use. However, it is now known that finger BP is physiologically different from brachial BP, and issues of vasospasm in the winter season as well as hydrostatic pressure differences are inevitable. Therefore, manufacturers have decreased production of finger-cuff devices and extensively increased production of wrist-cuff devices. In Japan wrist-cuff devices have 35% of the market share, and in Germany they possess almost half of the market share. Wrist-cuff devices are much easier to handle and more portable, but have several serious shortcomings. The most important issue is the necessity for correction of the hydrostatic pressure. The reference level for BP measurements is the right atrium. When the measurement site is 10 cm below the right atrium, SP and DP are measured as 7 mm Hg higher than at the level of the right atrium, and vice versa. Therefore, instructions for the wrist-cuff device indicate that the wrist must be kept at heart level. However, it is uncertain whether general users can accurately recognize where the heart level is. For example, the apex of the heart is sometimes determined as the heart level, but it is actually 5–10 cm lower than the right atrium, resulting in a 3.5–7-mm Hg higher BP reading compared with a measurement taken at the right atrium level. A 10-cm difference from the right atrium level easily and frequently occurs in usual settings. This difference may have serious implications for public health policies as well as clinical practice. In this situation, when the wrist is settled on the chest at the site of the heart in the supine position, the wrist is sometimes laid at a level 5–10 cm higher than that of the heart level, leading to lower BP measurements by 3.5–7 mm Hg than BP measurements at the right atrium. This issue also applies to the arm-cuff device, and adequate instruction is necessary when home BP is measured by the arm-cuff device. Even after appropriate correction of the hydrostatic pressure in the wrist-cuff device, another issue remains concerning the anatomy of the wrist. At the wrist, the radial and ulnar arteries are surrounded by the radial bone, ulnar bone and several long tendons, including the long palmar tendon. Therefore, even a sufficient excess of cuff pressure over arterial pressure does not necessarily occlude these arteries completely. Measurements are also influenced by flexion and hyperextension of the wrist. As a result, wrist-cuff devices sometimes provide erroneous readings, especially for SP. At present, the wrist-cuff device is inappropriate as a tool for clinical decision making. Recently, a wrist-cuff device that does not work unless the device is at the heart level has been developed, but even such devices do not overcome this anatomical issue. However, the wrist-cuff device has a certain merit in terms of convenience. Arm-cuff devices also have some shortcomings, such as application to a thick arm, the relationship between the cuff and clothes and the position of the arm cuff in relation to the elbow joint. The wrist-cuff device can overcome these shortcomings. However, I recommend the use of an arm-cuff device operated under standard measurement procedures.
B) Type of Cuff:
At present, soft cuffs and hard plastic cuffs are available for automatic arm-cuff devices for home BP measurements. In individuals with thick arms, a hard plastic cuff does not necessarily fit the arm, resulting in erroneous measurements. Thus, a soft cuff is more suitable, but in certain subjects a hard plastic cuff is convenient and measures BP accurately. Among cuff-oscillometric devices, the width and length of the cuff bladder differ among producers. This is permitted by the American Association for Medical Instrumentation (AAMI) and the American National Standard Institute Inc. (ANSI) as a prerequisite, provided that cuff pressure is transmitted to the artery and can occlude the brachial artery completely. In individuals with excessively thick or thin arms, the use of large or small cuffs, respectively, is recommended.
_
The inflation of the cuff:
An insufficient inflation leads to an undervaluation of the systolic blood pressure, i.e. the maximal blood pressure. The solution for the self-measurement device is based on an automatic system of inflation of the cuff. Many self-measurement devices of the blood pressure inflate the cuff up to 180 millimeters of mercury and then deflate it gradually. If this pressure is lower than the systolic blood pressure, then the device inflates the cuff again until the pressure is above the systolic blood pressure. Many self-measurement devices of the blood pressure have a possibility of presetting the maximal level of the pressure, such as 140, 170, 200 and 240 millimeters of mercury. Thus, when the cuff inflates with 140 millimeters of mercury and that the systolic blood pressure is 190 millimeters of mercury, the cuff inflates again with 170 and then 200 millimeters of mercury. The very sophisticated devices inflate their cuff gradually, hear the noises at the level of the artery at the same time and stop the inflation as soon as the blood pressure measured by the device exceeds the systolic blood pressure.
_
The deflating of the cuff:
The deflating must be very meticulous in order not to make an error of measurement of the blood pressure. If the deflating is too fast, the systolic blood pressure may be underestimated whereas the diastolic blood pressure may be over-estimated. The best self-measurement devices use a deflating programmed at a speed of 2 millimeters of mercury per second. Other devices use a deflating programmed on the heart pulsations, but they are valid only when the patient heart rate is between 60 and 80 per minute.
_
Differences between the Two Arms:
Several studies have compared the blood pressure measured in both arms, mostly using the auscultatory technique. Almost all have reported finding differences, but there is no clear pattern; thus, the difference does not appear to be determined by whether the subject is right- or left-handed. One of the largest studies was conducted in 400 subjects using simultaneous measurements with oscillometric devices, which found no systematic differences between the 2 arms, but 20% of subjects had differences of >10 mm Hg. Although these findings are disturbing, it is not clear to what extent the differences were consistent and reproducible, as opposed to being the result of inherent blood pressure variability. Nevertheless, it is recommended that blood pressure should be checked in both arms at the first examination. This may be helpful in detecting coarctation of the aorta and upper extremity arterial obstruction. When there is a consistent inter-arm difference, the arm with the higher pressure should be used. In women who have had a mastectomy, blood pressure can be measured in both arms unless there is lymphedema. Self-BP measurements at home, however, are usually performed using the non-dominant arm. When an apparent difference in BP is observed between the arms in a clinical setting, the arm showing the higher BP should be used for self-BP measurements. To provide consistent results, the same arm should always be used for self-BP measurements.
_
Cuff Size:
_
The figure below differentiates between cuff and bladder. Whenever we talk of cuff size, we actually mean bladder size.
_
Von Recklinghausen in 1901 recognized that Riva Rocci’s device for determination of accurate systolic blood pressure by palpation had a significant flaw, its 5-cm-width cuff. Multiple authors have shown that the error in blood pressure measurement is larger when the cuff is too small relative to the patient’s arm circumference than when it is too large. Previous epidemiological data from Britain and Ireland had suggested that arm circumferences of >34 cm were uncommon. Data from NHANES III and NHANES 2000 have shown the opposite in the United States. In the United States during the period from 1988 to 2000, there has been a significant increase in mean arm circumference and an increase in the frequency of arm circumferences of >33 cm was found because of increasing weight in the American population. This should not be surprising, because the prevalence of obesity in the United States has increased from 22.9% in NHANES III (1988 to 1994) to >30% in 2000. Similar data regarding the increased frequency of larger arm circumferences were also found in a study of a referral practice of hypertensive subjects, in which a striking 61% of 430 subjects had an arm circumference of ≥33 cm. Recognition of the increasing need for the “large adult” cuff, or even the thigh cuff, for accurate blood pressure measurement is critical, because frequently in practice only the standard adult size has been demonstrated to be available. More importantly, it has been demonstrated that the most frequent error in measuring blood pressure in the outpatient clinic is “miscuffing,” with undercuffing large arms accounting for 84% of the “miscuffings.”
_
_
_
The “ideal” cuff should have a bladder length that is 80% and a width that is at least 40% of arm circumference (a length-to-width ratio of 2:1). A recent study comparing intra-arterial and auscultatory blood pressure concluded that the error is minimized with a cuff width of 46% of the arm circumference. For the large adult and thigh cuffs, the ideal width ratio of 46% of arm circumference is not practical, because it would result in a width of 20 cm and 24 cm, respectively. These widths would give a cuff that would not be clinically usable for most patients, so for the larger cuffs, a less than ideal ratio of width to arm circumference must be accepted. In practice, bladder width is easily appreciated by the clinician but bladder length often is not, because the bladder is enclosed in the cuff. To further complicate the issue for clinicians, there are no standards for manufacturers of different sizes of blood pressure cuff. This has led to significant differences in which arm circumferences are accurately measured by individual manufacturers’ standard adult and large adult cuffs.
_
_
Individual cuffs should be labeled with the ranges of arm circumferences, to which they can be correctly applied, preferably by having lines that show whether the cuff size is appropriate when it is wrapped around the arm. In patients with morbid obesity, one will encounter very large arm circumferences with short upper arm length. This geometry often cannot be correctly cuffed, even with the thigh cuff. In this circumstance, the clinician may measure blood pressure from a cuff placed on the forearm and listening for sounds over the radial artery (although this may overestimate systolic blood pressure) or use a validated wrist blood pressure monitor held at the level of the heart.
_
_
Cuff Placement and Stethoscope:
Cuff placement must be preceded by selection of the appropriate cuff size for the subject’s arm circumference. The observer must first palpate the brachial artery in the antecubital fossa and place the midline of the bladder of the cuff (commonly marked on the cuff by the manufacturer) so that it is over the arterial pulsation over the patient’s bare upper arm. The sleeve should not be rolled up such that it has a tourniquet effect above the blood pressure cuff. On the other hand, applying the cuff over clothes is similar to the undercuffing error and will lead to overestimation of blood pressure. The lower end of the cuff should be 2 to 3 cm above the antecubital fossa to allow room for placement of the stethoscope. However, if a cuff that leaves such space has a bladder length that does not sufficiently encircle the arm (at least 80%), a larger cuff should be used, recognizing that if the cuff touches the stethoscope, artifactual noise will be generated. The cuff is then pulled snugly around the bare upper arm. Neither the observer nor the patient should talk during the measurement. Phase 1 (systolic) and phase 5 (diastolic) Korotkoff sounds are best heard using the bell of the stethoscope over the palpated brachial artery in the antecubital fossa, although some studies have shown that there is little difference when using the bell or the diaphragm. The key to good measurement is the use of a high-quality stethoscope with short tubing, because inexpensive models may lack good tonal transmission properties required for accurate auscultatory measurement.
_
The clinician must also interpret BP measurement entries with some caution. One study showed that as many as 20% of logbook entries were incorrect or fictitious. My patients of government hospitals told me that many times nurses do not take blood pressure and write fictitious BP on the indoor case sheets.
__
Number of measurements at clinic:
Because of the variability of measurements of casual blood pressure, decisions based on single measurements will result in erroneous diagnosis and inappropriate management. Reliability of measurement is improved if repeated measurements are made. At least two measurements at 1 min intervals should be taken carefully at each visit, with a repeat measurement if there is uncertainty or distraction; it is best to make a few carefully taken measurements rather than taking a number of hurried measurements.
_
American Heart Association Guidelines for In-Clinic Blood Pressure Measurement:
| Recommendation | Comments |
| Patient should be seated comfortably, with back supported, legs uncrossed, and upper arm bared. | Diastolic pressure is higher in the seated position, whereas systolic pressure is higher in the supine position. |
| An unsupported back may increase diastolic pressure; crossing the legs may increase systolic pressure. | |
| Patient’s arm should be supported at heart level. | If the upper arm is below the level of the right atrium, the readings will be too high; if the upper arm is above heart level, the readings will be too low. |
| If the arm is unsupported and held up by the patient, pressure will be higher. | |
| Cuff bladder should encircle 80 percent or more of the patient’s arm circumference. | An undersized cuff increases errors in measurement. |
| Mercury column should be deflated at 2 to3 mm per second. | Deflation rates greater than 2 mm per second can cause the systolic pressure to appear lower and the diastolic pressure to appear higher. |
| The first and last audible sounds should be recorded as systolic and diastolic pressure, respectively. Measurements should be given to the nearest 2 mm Hg. | |
| Neither the patient nor the person taking the measurement should talk during the procedure. | Talking during the procedure may cause deviations in the measurement. |
_______
Auscultatory method using microphone:
Mercury and aneroid sphygmomanometers require the use of a stethoscope to hear the sounds over the brachial artery. Sometimes, a microphone has been integrated into the cuff to obtain an automatic device. Unfortunately, this device is not always highly reliable because of the dexterity needed in their handling and the reduction in the precision of the cuff with time. Nevertheless, this device has not currently been abandoned.
______
Automated device:
Very often, the self-measurement devices for blood pressure are automatic, i.e. the patient just has to press on a button to begin the inflation. These automated devices use electric pump to inflate pneumatic cuff. Many devices are even equipped with a special program that can measure the blood pressure 3 times in a row. Most of automated devices use oscillometric technique to determine BP but you can have an automated device using auscultatory technique employing microphone-filter system to detect korotkoff sounds but these devices are now obsolete.
_
The Oscillometric Technique:
_
_
They measure systolic and diastolic pressures by oscillometric detection, using a piezoelectric pressure sensor and electronic components including a microprocessor. They do not measure systolic and diastolic pressures directly, per se, but calculate them from the mean pressure and empirical statistical oscillometric parameters. In the oscillometric method the cuff pressure is high pass filtered to extract the small oscillations at the cardiac frequency and the envelope of these oscillations is computed, for example as the area obtained by integrating each pulse. These oscillations in cuff pressure increase in amplitude as cuff pressure falls between systolic and mean arterial pressure. The oscillations then decrease in amplitude as cuff pressure falls below mean arterial pressure. The corresponding oscillation envelope function is interpreted by computer aided analysis to extract estimates of blood pressure. The point of maximal oscillations corresponds closely to mean arterial pressure. Points on the envelope corresponding to systolic and diastolic pressure, however, are less well established. Frequently a version of the maximum amplitude algorithm is used to estimate systolic and diastolic pressure values. The point of maximal oscillations is used to divide the envelope into rising and falling phases. Then characteristic ratios or fractions of the peak amplitude are used to find points corresponding to systolic pressure on the rising phase of the envelope and to diastolic pressure on the falling phase of the envelope. Current algorithms for oscillometric blood pressure implemented in commercial devices may be quite valid but are closely held trade secrets and cannot be independently validated.
_
One advantage of the method is that no transducer need be placed over the brachial artery, so that placement of the cuff is not critical. Other potential advantages of the oscillometric method for ambulatory monitoring are that it is less susceptible to external noise (but not to low-frequency mechanical vibration), and that the cuff can be removed and replaced by the patient, for example, to take a shower. The main problem with the technique is that the amplitude of the oscillations depends on several factors other than blood pressure, most importantly the stiffness of the arteries. Thus, in older people with stiff arteries and wide pulse pressures the mean arterial pressure may be significantly underestimated. The algorithms used for detecting systolic and diastolic pressures are different from one device to another and are not divulged by the manufacturers. The differences between devices has been dramatically shown by studies using simulated pressure waves, in which a systolic pressure of 120 mm Hg was registered as low as 110 and as high as 125 mm Hg by different devices. Another disadvantage is that such recorders do not work well during physical activity, when there may be considerable movement artifact. Additionally, the bladders deflate at a manufacturer-specific “bleed rate,” which assumes a regular pulse between bleed steps as part of the algorithms used to determine systolic and diastolic pressure.
_
It is a simple technique, effective and validated by many medical societies. This technique can be easily automated, and can be used as a self-measurement device by a great number of patients with high blood pressure. Currently, the majority of the self-measurement devices for blood pressure use this technique and the devices are generally reliable. The oscillometric technique has been used successfully in ambulatory blood pressure monitors and home monitors. Comparisons of several different commercial models with intra-arterial and Korotkoff sound measurements have shown generally good agreement, but the results have been better with ambulatory monitors than with the cheaper devices marketed for home use. Oscillometric devices are also now available for taking multiple measurements in a clinic setting.
_
Oscillometric vs. auscultatory:
There are a number of physiological and pathological states that may influence the ability of an oscillometric device to obtain an equivalent reading to a mercury sphygmomanometer. Oscillometric measurements are dependent on movement, and changes in the amplitude of this movement, in the artery, and therefore maybe altered. Oscillometric measurements cannot be relied on in patients with arrhythmias, or some valvular heart disease such as aortic incompetence. Other patients with altered vascular compliance, such as diabetics, or the elderly, could have less accurate blood pressure readings using oscillometric measurement. Changes in vascular compliance may also be confounded by oedema, intravascular volume, hyperdynamic circulation and by changes in cardiac output such as pre-eclampsia, in which oscillometric readings frequently underestimate the blood pressure. Although the accuracy and reproducibility of Korotokov sounds in these disease states are not known, listening to the Korotkoff sounds remains the technique in which current knowledge of indirect blood pressure is determined, and therefore, the auscultatory method of blood pressure is recommended in such populations.
_
Are oscillometric measurements reliable?
Oscillometric monitoring requires the recording of pressure pulses in the cuff which arise through volume pulses of the artery. The course of the pulse pressure curve is recorded as the so called ‘pulse oscillogram’. By referring to the pulse amplitudes, an envelope curve is provided. The maximum of this oscillation envelope curve corresponds to the mean arterial pressure. Both systolic and diastolic blood pressures are determined from the shape of the envelope curve by means of a micro-computer. The underlying algorithms are specific for the respective commercial instruments. They are well guarded secrets of the manufacturers. Users generally will not be informed about changes in the use of algorithms. In addition to the algorithms and the quality of the electromechanical pressure transducer, further errors can influence the measurement accuracy of oscillometric devices. The recording of the oscillation pattern significantly depends on the anatomical position, elasticity and size of the artery. In addition, the size, histo-anatomy and distribution of the surrounding tissue affect the accuracy. This is particularly true for the circumference of the measurement site. Basically, the device calibration depends on the application site (upper arm, wrist, finger). Changes of the vascular wall elasticity and arteriosclerotic vascular changes also affect the course and pattern of the pulse oscillogram. Finally, oscillations are also dependent on the size and material of the cuff and of pressure tube connections. The impact of these physiological-anatomical and technical factors on the device-specific oscillometric measurement accuracy requires a critical review of the measurement accuracy by referring to an adequately sized patient sample. Unfortunately, such evaluation is not mandatory for all markets. For example, according to the European standard (EN1060 1-3) the CE (European Conformity Mark) identification does not include such a mandatory clinical evaluation of the measurement accuracy; an omission, which is not commonly known by prescribing practitioners or users of the instruments. Therefore, only a small proportion of automated devices on the market have been qualified by clinical evaluations according to generally accepted protocols of an independent institution or scientific society such as the British Hypertension Society (BHS), the Deutsche Hochdruckliga [German Hypertension Society (test seal)], the American Association for the Advancement of Medical Instrumentation (AAMI) or according to the DIN58130. Due to the unsatisfactory number of sufficiently evaluated instruments, a proposal to simplify the evaluation procedure has been made by the ESH Working Group on Blood Pressure Monitoring. Further efforts are currently under discussion to standardize the underlying clinical protocols imposing an obligatory regulation in order to carry out such evaluations (EN standard 1060, part 4). Successfully evaluated devices may not guarantee a specific monitoring accuracy for all kinds of users. Therefore, in addition to the general exclusion of patients suffering from frequent cardiac arrhythmia (in particular atrial fibrillation) a comparative monitoring including the standard Korotkoff method is urgently required to evaluate the individual monitoring accuracy of a device for each single user. Clinical evaluation studies demonstrate that the measurement accuracy in wrist type devices is significantly lower compared with upper arm monitoring devices. The wrist-type device market-share in Germany is ∼60–80% despite the fact that the evaluation according to the ‘test seal protocol’ (Deutsche Hochdruckliga) has only been passed by one of 13 tested wrist devices.
_
Doppler ultrasound to detect brachial BP:
Doppler ultrasound is based on the Doppler phenomenon. The frequency of sound waves varies depending on the speed of the sound transmitter in relation to the sound receiver. Doppler devices transmit a sound wave that is reflected by flowing erythrocytes, and the shift in frequency is detected. Frequency shift can be detected only for blood flow greater than 6 cm/sec. Doppler ultrasound is commonly used for the measurement of blood pressure in low-flow states, evaluation of lower extremity peripheral perfusion, and assessment of fetal heart sounds after the first trimester of pregnancy. Doppler’s sensitivity allows detection of systolic blood pressure down to 30 mm Hg in the evaluation of a patient in shock. Devices incorporating this technique use an ultrasound transmitter and receiver placed over the brachial artery under a sphygmomanometer cuff. As the cuff is deflated, the movement of the arterial wall at systolic pressure causes a Doppler phase shift in the reflected ultrasound, and diastolic pressure is recorded as the point at which diminution of arterial motion occurs. Another variation of this method detects the onset of blood flow, which has been found to be of particular value for measuring systolic pressure in infants and children. In patients with very faint Korotkoff sounds (for example those with muscular atrophy), placing a Doppler probe over the brachial artery may help to detect the systolic pressure, and the same technique can be used for measuring the ankle–arm index, in which the systolic pressures in the brachial artery and the posterior tibial artery are compared to obtain an index of peripheral arterial disease.
___________
Shortcoming of traditional brachial artery compression:
The occlusion by the cuff – applied in the majority of indirect blood-pressure meters – changes the biomechanical properties of the arteries resulting in a change in the systolic and diastolic values. The occlusion of the brachial artery influences the local value of blood-pressure. In other words, the measurement changes the parameter to be measured. The change in blood-pressure is different in different parts of the body. The change caused by the inflation of the cuff is different from person to person. Even the same person can react to the occlusion differently. The widely used devices determine the momentarily value of blood-pressure. This results in an unpredictable error. According to BHS and AAMI the reference blood-pressure value is also determined by using a cuff. As a result of the occlusion the reference value can also be biased. Presently available devices also neglect the variation caused by breathing. This can be as high as 10 Hg mm in the systolic pressure. The aim of the research work has been to increase the accuracy and reproducibility of the indirect, cuff-based blood pressure measurement with monitors using the Pulse Wave Velocity (PWV) principle. The importance of all this is that brachial BP can be unreliable, especially in young people whose more flexible blood vessel walls can give misleadingly high blood pressure, leading to unnecessary medical interventions. Conversely, old people with stiffer blood vessels may give a misleadingly low reading of brachial BP, disguising dangerous high blood pressure which can be a precursor to heart attack or stroke.
________
The Pulse Wave Velocity (PWV) principle:
Since the 1990s a novel family of techniques based on the so-called pulse wave velocity (PWV) principle has been developed. These techniques rely on the fact that the velocity at which an arterial pressure pulse travels along the arterial tree depends, among others, on the underlying blood pressure. Accordingly, after a calibration maneuver, these techniques provide indirect estimates of blood pressure by translating PWV values into blood pressure values. The main advantage of these techniques is that it is possible to measure PWV values of a subject continuously (beat-by-beat), without medical supervision, and without the need of inflating brachial cuffs. PWV-based techniques are still in the research domain and are not adapted to clinical settings. Non-intrusive blood pressure monitoring are either the pulse wave velocity (PWV) or the inverse – pulse transit time (PTT). In general the PTT refers to the time it takes a pulse wave to travel between two arterial sites. PTT varies inversely with blood pressure changes and can be used to develop cuffless and continuous blood pressure measurement. There are a number of different sophisticated pulse transit time measurement techniques such as the Ultrasound Doppler, arterial tonometry, and the so called “two point” PPG method (Smith et al. 1999; Kanda et al. 2000; Lykogeorgakis 2002). However, the simplest and most convenient method is to compute PTT as a temporal difference between the R wave in an electrocardiogram (ECG) and the beginning of the following pulse wave measured by photoplethysmography (Lutter et al. 2002; Kazanavicius et al. 2003).
_
PPG:
Photoplethysmography (PPG) is a simple and low-cost optical technique that can be used to detect blood volume changes in the microvascular bed of tissue. It is often used non-invasively to make measurements at the skin surface. The PPG waveform comprises a pulsatile physiological waveform attributed to cardiac synchronous changes in the blood volume with each heart beat, and is superimposed on a slowly varying baseline with various lower frequency components attributed to respiration, sympathetic nervous system activity and thermoregulation. Although the origins of the components of the PPG signal are not fully understood, it is generally accepted that they can provide valuable information about the cardiovascular system. A PPG is often obtained by using a pulse oximeter which illuminates the skin and measures changes in light absorption. The change in volume caused by the pressure pulse is detected by illuminating the skin with the light from a light-emitting diode (LED) and then measuring the amount of light either transmitted or reflected to a photodiode. Each cardiac cycle appears as a peak. Blood pressure measuring method using PPG signal is the one of many non-invasive blood pressure methods. We can estimate blood pressure using wrist cuff and wrist PPG signal. During the deflation of the wrist cuff pressure, the PPG pulse appears at certain point that is similar to Korotkoff sound. After the pulse appeared, the morphology of PPG pulses was changed into the certain shape. So, we use these points to estimate the blood pressure.
_
The Finger Cuff Method of Penaz: The Photoplethysmographic (PPG) method:
This interesting method was first developed by Penaz and works on the principle of the “unloaded arterial wall.” Arterial pulsation in a finger is detected by a photoplethysmograph under a pressure cuff. The output of the plethysmograph is used to drive a servo-loop, which rapidly changes the cuff pressure to keep the output constant, so that the artery is held in a partially opened state. The oscillations of pressure in the cuff are measured and have been found to resemble the intra-arterial pressure wave in most subjects. This method gives an accurate estimate of the changes of systolic and diastolic pressure, although both may be underestimated (or overestimated in some subjects) when compared with brachial artery pressures; the cuff can be kept inflated for up to 2 hours. It is now commercially available as the Finometer (formerly Finapres) and Portapres recorders, and has been validated in several studies against intra-arterial pressures. The Portapres enables readings to be taken over 24 hours while the subjects are ambulatory, although it is somewhat cumbersome. The PPG signal helps to measure the systolic pressure directly unlike the oscillometric method that measures the mean pressure and gives only an estimate for the systolic and diastolic pressures. The additional information gained by monitoring the PPG signal before and during slow inflation provides more accurate results than conventional indirect methods and assures that the cuff pressure only slightly (by less than 10 Hg mm) exceed the systolic pressure. The PPG signal also indicates if the cuff is placed or inflated improperly. Some tests have revealed that the photoplethysmographic method was not reliable, not only because of the measuring site of the blood pressure, but also because of the bad quality of the blood pressure data collected. Besides photoplethysmography (PPG), piezoplethysmography and volume pressure recording are also used in various noninvasive blood pressure (NIBP) techniques for measuring the BP.
_
Ultrasound Technique:
Researchers have demonstrated that Doppler ultrasound can be used to measure aortic PWV in a reliable and reproducible way. In addition, B-mode ultrasound provides an anatomical image that can increase the precision of measurements (for example, using the carotid or femoral bifurcation as a reference). This method has the further advantages of shorter performance time, short learning curve and the absence of anatomical limitations, which are especially pronounced in the carotid artery. The versatility of ultrasound also permits to explore simultaneously other pathologies such as plaques or blockages in the carotid and femoral territories as well as to assess intima-media thickness.
_
Tonometry:
The principle of this technique is that when an artery is partially compressed or splinted against a bone, the pulsations are proportional to the intra-arterial pressure. This has been developed for measurement of the blood pressure at the wrist, because the radial artery lies just over the radius bone. However, the transducer needs to be situated directly over the center of the artery; hence, the signal is very position-sensitive. This has been dealt with by using an array of transducers placed across the artery. Although the technique has been developed for beat-to-beat monitoring of the wrist blood pressure, it requires calibration in each patient and is not suitable for routine clinical use.
_
Applantion tonometry for BP measurement:
Another application is applanation tonometry, in which a single transducer is held manually over the radial artery to record the pressure waveform while systolic and diastolic pressures are measured from the brachial artery. This technique has been used to estimate central aortic pressure. The rationale for this is that the arterial pressure at the level of the aortic root is different from the brachial artery pressure, and that this difference varies according to a number of physiological and pathological variables. Central aortic pressure is a better predictor of cardiovascular outcome than peripheral pressure and peripherally obtained blood pressure does not accurately reflect central pressure because of pressure amplification. Lastly, antihypertensive medications have differing effects on central pressures despite similar reductions in brachial blood pressure. Applanation tonometry can overcome the limitations of peripheral pressure by determining the shape of the aortic waveform from the radial artery. Waveform analysis not only indicates central systolic and diastolic pressure but also determines the influence of pulse wave reflection on the central pressure waveform. It can serve as a useful adjunct to brachial blood pressure measurements in initiating and monitoring hypertensive treatment, in observing the hemodynamic effects of atherosclerotic risk factors, and in predicting cardiovascular outcomes and events. Radial artery applanation tonometry is a noninvasive, reproducible, and affordable technology that can be used in conjunction with peripherally obtained blood pressure to guide patient management. The shape of the pressure waveform in the arterial tree is determined by a combination of the incident wave and the wave reflected from the periphery. In hypertensive subjects and subjects with stiff arteries, the systolic pressure wave in the aorta and brachial artery is augmented by a late systolic peak, which can be attributed to wave reflection and which is not seen in more peripheral arteries such as the radial artery. Using Fourier analysis, it is possible to derive the central aortic pressure waveform from the radial artery trace. However, comparisons with directly recorded aortic pressure made during cardiac catheterization have shown considerable scatter between the estimated and true values, so the technique cannot yet be recommended for routine clinical practice.
_______
BP measurement devices: BP monitors:
_
_
Auscultatory arm devices:
1. Mercury Sphygmomanometers:
The mercury sphygmomanometer has always been regarded as the gold standard for clinical measurement of blood pressure, but this situation is likely to change in the near future. The design of mercury sphygmomanometers has changed little over the past 50 years, except that modern versions are less likely to spill mercury if dropped. In principle, there is less to go wrong with mercury sphygmomanometers than with other devices, and one of the unique features is that the simplicity of the design means that there is negligible difference in the accuracy of different brands, which certainly does not apply to any other type of manometer. However, this should not be any cause for complacency. One hospital survey found that 21% of devices had technical problems that would limit their accuracy, whereas another found >50% to be defective. The random zero sphygmomanometer was designed to eliminate observer bias but is no longer available.
_
2. Aneroid Sphygmomanometers:
In these devices, the pressure is registered by a mechanical system of metal bellows that expands as the cuff pressure increases and a series of levers that register the pressure on a circular scale. This type of system does not necessarily maintain its stability over time, particularly if handled roughly. They therefore are inherently less accurate than mercury sphygmomanometers and require calibrating at regular intervals. Recent developments in the design of aneroid devices may make them less susceptible to mechanical damage when dropped. Wall-mounted devices may be less susceptible to trauma and, hence, more accurate than mobile devices. The accuracy of the manometers varies greatly from one manufacturer to another. Thus, 4 surveys conducted in hospitals in the past 10 years have examined the accuracy of the aneroid devices and have shown significant inaccuracies ranging from 1% to 44%. The few studies that have been conducted with aneroid devices have focused on the accuracy of the pressure registering system as opposed to the degree of observer error, which is likely to be higher with the small dials used in many of the devices.
_
3. Hybrid Sphygmomanometers:
Devices have been developed that combine some of the features of both electronic and auscultatory devices, and are referred to as “hybrid” sphygmomanometers. The key feature is that the mercury column is replaced by an electronic pressure gauge, such as are used in oscillometric devices. Blood pressure is taken in the same way as with a mercury or aneroid device, by an observer using a stethoscope and listening for the Korotkoff sounds. The cuff pressure can be displayed as a simulated mercury column, as a digital readout, or as a simulated aneroid display. In one version, the cuff is deflated in the normal way, and when systolic and diastolic pressure are heard a button next to the deflation knob is pressed, which freezes the digital display to show systolic and diastolic pressures. This has the potential of minimizing terminal digit preference, which is a major source of error with mercury and aneroid devices. The hybrid sphygmomanometer has the potential to become a replacement for mercury, because it combines some of the best features of both mercury and electronic devices at any rate until the latter become accurate enough to be used without individual validation.
_
Selection of an accurate device:
An accurate device is fundamental to all measurements of blood pressure. If the device is inaccurate, attention to the detail of measurement methods is of little relevance. The accuracy of devices for measurement of blood pressure should not be judged on the sole basis of claims from manufacturers, which can be extravagant. Instead devices should be validated according to international protocols in peer reviewed journals. Understandably, many are skeptical about the accuracy of SMBP devices. The American Association for the Advancement of Medical Instrumentation and the British Hypertension Society has established the 2 standard protocols for instrument accuracy. Given the multitude of products available, few have been subjected to the rigorous standards of independent testing. The European Society of Hypertension found only 5 out of 23 tested devices worthy of recommendation. The investigators noted that all the recommended devices measured BP in the upper arm. They advised against the less accurate wrist and finger devices, as these can be subject to inaccuracies from peripheral vasoconstriction and errors in positioning in respect to heart-level placement.
_
Mercury sphygmomanometers:
The mercury-containing sphygmomanometer should not be viewed as an absolute standard. It is however, with all its faults as an indirect blood pressure determination, the method used to establish our current knowledge. Since Riva-Rocci’s times mercury sphygmomanometers associated with the occlusion-auscultatory technique have been used in clinical and epidemiological studies on hypertension. They represent the cornerstone for cardiovascular disease prognosis and prevention, as well as in the daily clinical management of patients with high blood pressure. As a result of this time- honoured use, blood pressure values are still quantified in mmHg both in current practice and in research, and doctors keep watching the mercury column as the most faithful indicator of the blood pressure levels in their patients. A commonly perceived advantage of mercury manometers lies in the fact that, when they are well maintained, they offer “absolute” measurements of blood pressure, and represent a “gold standard” reference technique used to validate all other methods which provide information on blood pressure levels in mmHg without using a mercury column. The blood pressure measurement based on the mercury sphygmomanometer is an indirect blood pressure determination, and is difficult to perfectly mimic with other techniques unrelated to auscultation of Korotkoff sounds. The high-density of liquid mercury metal provides an acceptable short length of the rising column for visualization of the pressure in the cuff. Therefore, the mercury column in a sphygmomanometer is used as a simple, gravity-based unit. When properly maintained and serviced and when used by knowledgeable trained health professionals, it can give accurate indirect measurements of both systolic and diastolic pressure. Currently it is considered to be the most accurate technique (O’Brien et al. 2003). A complete mercury sphygmomanometer requires a cuff, bladder, tubing and a rubber bulb, and should be maintained in good condition and serviced regularly according to the manufacturers’ instructions. Mercury sphygmomanometers are easily checked and maintained, but great care should be taken when handling mercury.
_
Limitations of mercury sphygmomanometer:
Despite its widespread availability for almost a century, there can be major problems with the use of mercury sphygmomanometers in clinical practice. Reports from hospitals and family practices have suggested that many mercury sphygmomanometers are defective because of poor maintenance (Beevers and Morgan 1993, Burke et al. 1982, Feher et al. 1992, Gillespie and Curzio 1998, Hutchinson et al. 1994, Markandu et al. 2000, Wingfield et al. 1996). Moreover, several studies have shown that there is a lack of knowledge of the technical aspects of the actual blood pressure measurement in both doctors and nurses and other health care professionals who use the mercury sphygmomanometers. The reports also suggest that the technique of blood pressure measurement is not applied very well. Additionally, there is a lack of knowledge of the appropriate blood pressure equipment and how to maintain the devices so that they are calibrated and in pristine condition. One should be aware of the fact that issues of maintenance are a factor for every blood pressure measurement device.
_
There are several other limitations of using the auscultatory method which affect both mercury and aneroid manometers:
1. Terminal digit preference: Tendency of the observer to round off the number to their choosing e.g. 144/96 mmHg as 140/100 mmHg or 150/90 mmHg (systolic/diastolic blood pressure). This is the zero preference. The observer finds it easier to read the prominent larger 10 mmHg markings instead of the smaller, 2 mmHg markings.
2. Errors may occur when the manometer is not kept vertical, and the device is rested on the side of the bed or, having it tilted against the pillow. This is an issue when the device is being used at the patient’s bedside, not when used for public- health monitoring.
3. Inflation/deflation system: Another important limitation to consider is the performance of the inflation/deflation system and of the occluding bladder encased in a cuff, and proper application of auscultation with a stethoscope. Those issues apply to all blood pressure measuring devices using the auscultatory method. The inflation/deflation system consists of an inflating and deflating mechanism connected by rubber tubing to an occluding bladder. The standard mercury sphygmomanometers used in clinical practice are operated manually, with inflation being effected by means of a bulb compressed by hand and deflation by means of a release valve, which is also controlled by hand. The pump and control valve are connected to the inflatable bladder and thence to the sphygmomanometer by rubber tubing. Leaks from cracked or perished rubber make accurate measurement of blood pressure difficult because the fall of the mercury cannot be controlled. The length of tubing between the cuff and the manometer should be at least 70 cm and that between the inflation source and the cuff should be at least 30 cm. Connections should be airtight and easily disconnected.
4. Oxidisation of the mercury is another very common occurrence, which can increase with time and make the columns difficult to read.
5. The markings on the column also fade with time, again making it impossible to read accurately.
6. Environmental concerns regarding mercury mean that there is no long-term future for these devices. These concerns have led to the imposition of bans in some European countries and supply in the UK is now restricted to healthcare use.
_
________
Automated oscillometric devices:
• Automated (spot-check) arm device:
This includes an electronic monitor with a pressure sensor, a digital display and an upper arm cuff. An electrically-driven pump raises the pressure in the cuff. Devices may have a user-adjustable set inflation pressure or they will automatically inflate to the appropriate level, usually about 30mmHg above an estimated systolic reading. When started, the device automatically inflates, then deflates the cuff and displays the systolic and diastolic values. The pulse rate may also be displayed. These devices may also have a ‘memory’ facility which stores the last measurement and previous readings. They are battery powered.
• Wrist device:
This includes an electronic monitor with a pressure sensor, an electrically-driven pump attached to a wrist cuff. Function is similar to the automated (spot-check) device above. Battery powered. Wrist monitors have the advantages of being smaller than the arm devices and can be used in obese people, because the wrist diameter is little affected by obesity. A potential problem with wrist monitors is the systematic error introduced by the hydrostatic effect of differences in the position of the wrist relative to the heart. This can be avoided if the wrist is always at heart level when the readings are taken, but there is no way of knowing retrospectively whether this was performed when a series of readings are reviewed. Devices are now available that will only record a measurement when the monitor is held at heart level.
• Finger device:
A new invention that has come is the finger blood pressure monitor. The finger monitor is the latest technology that helps measure the blood pressure almost instantly in the most non-invasive way possible. This is a tiny digital device that works on batteries and consists of an electric monitor and a sensor. There is a small finger compartment where the index finger of the person needs to be placed. Within a matter of seconds, the sensor reads the blood pressure in the finger and gives you the reading. This device is small and portable and hence, is preferred for regular monitoring in individuals, especially when the person is constantly on the go. Uses oscillometric, pulse-wave or plethysmographic methods for measurement. Finger monitors have so far been found to be inaccurate and are not recommended.
• Spot-check non-invasive blood pressure (NIBP) monitor:
This is a more sophisticated version of the automated device above and is designed for routine clinical assessment. There may be an option to measure additional vital signs, such as oxygen saturation in the finger pulse (SpO2) and body temperature. Mains and battery powered.
• Automatic-cycling non-invasive blood pressure (NIBP) monitor:
This is similar to the spot-check NIBP monitor, but with the addition of an automatic-cycling facility to record a patient’s blood pressure at set time intervals. These are designed for bed-side monitoring in a clinical environment where repetitive monitoring of patients and an alarm function is required. These devices may incorporate the ability to measure additional vital signs. The alarm limits can usually be set to alert nursing staff when one or more of the measured patient parameters exceed the pre-set limits. Mains and battery powered.
• Multi-parameter patient monitors:
These are designed for use in critical care wards and operating theatres and monitor a range of vital signs including blood pressure. May be possible to communicate with a Central Monitoring Station via Ethernet or Wi-Fi.
• Ambulatory blood pressure monitor:
This includes an upper arm cuff and an electronic monitor with a pressure sensor and an electrically-driven pump that attaches to the patient’s belt. The unit is programmed to record the patient’s blood pressure at pre-defined intervals over a 24-hour period during normal activities and stores the data for future analysis. Battery powered. Uses electronic auscultatory and oscillometric techniques.
________
Automated non-auscultatory (oscillometric) devices:
There is an ever-increasing market for oscillometric blood pressure devices that have also increased home surveillance such as self-measurement and ambulatory/24hr monitoring. Home blood pressure measurement has been shown to be more reproducible than office blood pressure measurement (Stergiou et al. 2002) more predictive of cardiovascular events (Bobrie et al. 2004, Ohkubo et al. 2004) and reliable when used by non-clinicians (Nordmann et al. 1999). The out-of-office measurements are effective at removing the white-coat effect (Parati et al. 2003) particularly when using an averaging mode (Wilton et al. 2007). Telemonitoring enables the patient to transmit home measurements directly to the clinician’s computer for further analysis, potentially enhancing early identification, reducing hospital visits (Pare et al. 2007) and improving the degree of blood pressure control also in general practice (Parati et al. 2009a).
_
Automated devices are generally intended for use on the upper arm, but finger and wrist devices are also available. Few of these latter devices have been shown to be accurate according to independent accuracy assessments; only a small minority of wrist devices assessed achieved an acceptable accuracy (five in total) (O’Brien and Atkins 2007). Wrist devices are sensitive to errors related to positioning of the wrist at heart level, and some devices have position sensors. Very few of the wrist devices have passed clinical validation after independent assessment (Altunkan et al. 2006, Nolly et al. 2004). However, even the validated wrist devices with position sensors appear to give significantly different blood pressure values than arm devices in a large proportion of hypertensive patients (Stergiou et al. 2008d), while in an earlier study no such differences were observed (Cuckson et al. 2004). The European Society of Hypertension Guidelines state the preference of arm over wrist oscillometric devices (O’Brien et al. 2003, Parati et al. 2008b). No finger device has yet achieved the established validation standards (Elvan-Taspinar et al. 2003, Schutte et al. 2004).
_
An accurate automated sphygmomanometer capable of providing printouts of systolic, diastolic and mean blood pressure, together with heart rate and the time and date of measurement, should eliminate errors of interpretation and abolish observer bias and terminal digit preference. Moreover, the need for elaborate training of observers would no longer be necessary, although a period of instruction and assessment of proficiency in using the automated device will always be necessary. Another advantage of automated measurement is the ability of such devices to store data for later analysis (Parati G et al. 2008b). This development is in fact taking place, and a number of long-term outcome studies are using automated technology to measure blood pressure instead of the traditional mercury ‘gold standard’. For example, in the large Anglo–Scandinavian Cardiac Outcome Trial, the validated Omron HEM-705CP automated monitor was used including thousands of patients followed for about five years (Dahlöf et al. 2005, Hansson et al. 1998, Yusuf et al. 2008).
_
The table below shows advantages of current automated oscillometric devices:
_
Automated blood pressure measurement will eliminate the observer errors associated with the use of the manual auscultatory technique such as terminal digit preference, threshold avoidance, observer prejudice, rapid deflation etc. (Beevers et al. 2001). However, clinically significant differences exist between measurements obtained through automation compared to auscultation in many devices. Automated device accuracy is not only device dependent, but also user dependent. As these devices are more likely to be used by untrained individuals, errors related to selecting correct cuff size and taking the recommended arm position, ensuring no movement or talking during device measurement, or allowing for sufficient rest before measurements may be more pronounced than mercury sphygmomanometers. Various guidelines have been published for the correct use of automated devices with specific methodologies advocated (Chobanian et al. 2003, O’Brien et al. 2003, Parati et al. 2008a), but are not as established as training for auscultatory blood pressure measurement. Automated devices have accuracy limitations in special groups such as those with vascular damage that influences the oscillometric signal: these include patients with diabetes, arrhythmias or pre-eclampsia, and the elderly. This is related to arterial/vascular changes in these patients, which are likely to influence the recording of pressure waves by the device.
_
__________
Which is the best BP measurement device?
_
Is the mercury sphygmomanometer still ‘the gold standard’ of blood pressure monitoring?
It is undisputed that the mercury sphygmomanometer has the highest accuracy, with a high degree of technical agreement between devices of different producers. This ensures worldwide comparability of values measured with this method. Specific advantages of mercury-based manometer devices are the simple technique and a simple baseline correction. Nevertheless, several studies have reported on insufficient maintenance and calibration of mercury sphygmomanometers used in the clinical setting and in general practice. A check of the devices in a major teaching hospital showed that only 5% of the investigated instruments had been properly serviced while an inspection in general practices of an English district found that only ∼30% of the devices had been properly maintained. Regular maintenance intervals are infrequently met. Despite the relatively simple principle of the technique, instrument inspections disclosed defects in the manometers, cuffs and tubing systems of more than 50% of the mercury manometers in use: the defects had an impact on the correctness of the readings. This means that sufficient measurement accuracy is ensured only by devices which undergo regular technical evaluation and calibration at least on a yearly basis. Restrictions of the use of mercury in medical devices have already been imposed in the Netherlands and Sweden. This was felt to be necessary to avoid occupational health hazards and environmental contamination. This raises the question of whether mercury sphygmomanometers should still be used as standard devices for measuring blood pressure.
_
Are aneroid manometers a first-choice alternative?
Aneroid sphygmomanometers are the most commonly used alternative devices for measuring blood pressure in the clinical setting and in general practice. Instead of transferring pressure to a mercury column, they are designed to transfer the detected pressure via a mechanical system and an elastic expansion chamber to a gauge needle. The devices are characterized by their handy design and even portability. The mechanism is, however, highly sensitive towards any mechanical strain. It can be easily damaged by any mechanical impact, mainly the result of accidental falls or pushes; accuracy can also decrease over time during clinical use. This may result in both calibration errors (which are often not immediately apparent) and baseline shifts. In addition, the technical design differs widely between models from different manufacturers. Dependent on the kind of application of these devices, instrument evaluation studies demonstrated technical defects or unacceptable measurement inaccuracy in up to 60% of the devices that had been evaluated. Reading errors occur more frequently in the range of high blood pressure values where aneroid manometers tend to underestimate the blood pressure of the patient. Portable instruments, in particular, show a higher technical failure rate. In general practices the percentage of regularly serviced and recalibrated instruments is sometimes below 5%. If, however, aneroid manometers receive regular technical maintenance, their measurement accuracy is identical to the standard mercury manometer devices. This has been tested for wall-mounted instruments. Therefore, only devices which undergo a regular (half-) yearly technical inspection including recalibration ensure a reliable measurement accuracy. Under these circumstances they can be adopted as a potential alternative to mercury sphygmomanometers. However, as a result of the widespread lack of such checks, one must unfortunately assume that the percentage of erroneous measurements is high. In particular, this applies to devices in which the manometer is not cuff-integrated, since the latter can act as a ‘shock protection’. The new development of a mechanical gear free sphygmomanometer (Durashock, Welch-Allyn) apparently combines the advantage of a handy design with lesser susceptibility to shock and impact. The calibration stability is therefore higher than for aneroid manometers.
_
Is the automated sphygmomanometer the better alternative?
It must be conceded that electronic blood pressure measurement devices have numerous advantages. They are small, compact and relatively inexpensive. It is recommended that automated devices should be subjected to independent validation for accuracy. To this end, various assessment protocols are available from the Association of Advanced Medical Instrumentation, the British Hypertension Society and the European Society for Hypertension. Indeed, several studies have shown that the best models perform well in comparison to their manual counterparts. They contain no mercury and hence, there is no concern regarding safety. They are also simple to use and most importantly, remove the huge user-bias which exists with mercury sphygmomanometers.
_
_
Problems with automated devices:
The advent of accurate oscillometric devices, however welcome, is not without problems. First, oscillometric devices have been notorious for their inaccuracy in the past, although more accurate devices are now appearing on the market. Secondly, most of the available oscillometric devices were designed for self-measurement of blood pressure by patients, and it should not be assumed that they will be suitable for clinical use, or that they will remain accurate with use, although some are being used successfully in hospital practice. Thirdly, oscillometric techniques cannot measure blood pressure accurately in all situations, particularly in patients with pre-eclampsia, arrhythmias such as atrial fibrillation, and there are also individuals in whom these devices cannot measure blood pressure, for reasons that are not always apparent (Stergiou et al. 2009a, Van Popele et al. 2000). All alternative blood pressure measurement devices need to be clinically validated in clinical protocols against the current gold standard of the mercury sphygmomanometer, until an alternative device is developed and recognised as such. Several international protocols, such as the ISO protocol, the British Hypertension Society (BHS) and the European Society of Hypertension (ESH) International Protocol are available for such a clinical validation. A list of validated oscillometric devices is available on dedicated websites, such as the British Hypertension Society as well as other national learned societies.
_
Accuracy and reliability of wrist-cuff devices for self-measurement of blood pressure: a 2014 study:
Self-measurement of blood pressure (BP) might offer some advantages in diagnosis and therapeutic evaluation and in patient management of hypertension. Recently, wrist-cuff devices for self-measurement of BP have gained more than one-third of the world market share. In this study, authors validated wrist-cuff devices and compared the results between wrist- and arm-cuff devices. The factors affecting the accuracy of wrist-cuff devices were also studied. The research group assessed the validity of automated blood pressure measuring device consisted of 13 institutes in Japan, which validated two wrist-cuff devices (WC-1 and WC-2) and two arm-cuff devices (AC-1 and AC-2). They used a crossover method, where the comparison was done between auscultation, by two observers by means of a double stethoscope on one arm and the device on the opposite arm or wrist. The results suggest that wrist-cuff devices in the present form are inadequate for self-measurement of blood pressure and, thus, are inadequate for general use or clinical and practical use. However, there is much possibility in wrist-cuff device and the accuracy and reliability of wrist-cuff device are warranted by an improvement of technology.
_
You can see that most wrist cuff devices have questionable recommendation:
_
Synopsis of BP devices:
________
Validation of the devices and monitors for BP measurement:
In order to guarantee a good quality of the measurement, the self-measurement device must be validated by independent organizations or experts in blood pressure measurement. For the moment, there is no regulation control concerning this type of device worldwide. Thus, the quality of the self-measurement devices is very unequal, and only very few are currently validated. There are two reasons for validation of the device. The first is to confirm whether the type of device is clinically applicable for BP measurements in the general population, and the other is to confirm whether the device can accurately and properly measure BP in individual. Home measurement devices should be validated before use and at regular intervals (essentially once a year) during use.
_
All monitors in clinical use should be tested for accuracy. All oscillometric automated monitors that provide read-outs of systolic and diastolic pressure should be subjected by independent investigators to formal validation protocols. The original 2 protocols that gained the widest acceptance were developed by the Association for the Advancement of Medical Instrumentation (AAMI) in 1987 and the British Hypertension Society (BHS) in 1990, with revisions to both in 1993, and to AAMI in 2002. These required testing of a device by 2 trained human observers in 85 subjects, which made validation studies difficult to perform. One consequence of this has been that there are still many devices on the market that have never been adequately validated. More recently, an international group of experts who are members of the European Society of Hypertension Working Group on Blood Pressure Monitoring has produced an International Protocol that could replace the 2 earlier versions and is easier to perform. Briefly, it requires comparison of the device readings (4 in all) alternating with 5 mercury readings taken by 2 trained observers. Devices are recommended for approval if both systolic and diastolic readings taken are at least within 5 mm Hg of each other for at least 50% of readings. It is recommended that only those devices that have passed this or similar tests should be used in practice. However, the fact that a device passed a validation test does not mean that it will provide accurate readings in all patients. There can be substantial numbers of individual subjects in whom the error is consistently >5 mm Hg with a device that has achieved a passing grade. This may be more likely to occur in elderly or diabetic patients. For this reason, it is recommended that each oscillometric monitor should be validated on each patient before the readings are accepted. No formal protocol has yet been developed for doing this, but if sequential readings are taken with a mercury sphygmomanometer and the device, then major inaccuracies can be detected. Another problem is that manufacturers may change the model number after a device has been tested without indicating whether the measurement algorithm has also been changed. Users should also be aware that some automated non-invasive blood pressure monitors may have been validated by reference to intra-arterial measurements. There can be differences in readings between these devices and those validated by reference to non-invasive (sphygmomanometric) measurements.
_
In the interest of continuous technologic improvement, there should be a positive and close interaction between the validation centers and the manufacturers of the devices. Protocols should not restrict such exchange. For instance, after a negative stage 1 result of a validation, the manufacturer should have the possibility to adjust the device and resubmit it within a given time span, with the overall target of an improved performance of the instrumentation and a better product at the end. Only if such possibility is waived, or the modified device fails the study criteria, a negative publication should be the consequence to document that the device has failed and is not recommended for health care purposes.
_
With manual devices, such as mercury and aneroid monitors, it is recommended that the accuracy of the pressure registration mechanism be checked. In the case of mercury sphygmomanometers, this involves checking that the upper curve of the meniscus of the mercury column is at 0 mm Hg, that the column is free of dirt, and that it rises and falls freely during cuff inflation and deflation. Aneroid devices or other nonmercury devices should be checked by connecting the manometer to a mercury column or an electronic testing device with a Y-tube. The needle should rest at the zero point before the cuff is inflated and should register a reading that is within 4 mm Hg of the mercury column when the cuff is inflated to pressures of 100 and 200 mm Hg. The needle should return to zero after deflation.
__________
Automated BP recording in clinic:
Manual BP measurement is accurate when there is strict adherence to a BP measurement protocol, but readings might still be subject to “white-coat effect” and are often higher than BP measurements taken outside of the office setting. In the real world of everyday practice, physician and patient factors such as conversation during BP readings, recording of only a single BP reading, no antecedent period of rest before BP measurement, rapid deflation of the cuff, and digit preference with rounding off of readings to 0 or 5 all adversely affect the accuracy of manual BP measurement. The net result is a reading in routine clinical practice that is on average 9/6 mm Hg higher than BP taken in accordance with standardized guidelines for BP measurement in a research setting. Consequently, routine manual office BP has come to be regarded as an inferior method for diagnosing and managing hypertension. Even when performed properly in research studies, manual BP measurement is a relatively poor predictor of cardiovascular risk related to BP status compared with methods of out-of-office BP measurement such as 24-hour ambulatory BP monitoring (AMBP) or home BP measurement.
_
There is now an alternative to manual office BP measurement—automated office BP (AOBP). Automated oscillometric devices have recently been used in large-scale clinical trials and in population studies including the current National Health and Nutrition Education Survey. By incorporating validated, fully automated BP recorders into clinical practice, it is possible to improve the quality and accuracy of BP measurement in the office while eliminating most, if not all of the white coat response. AOBP involves the use of a fully automated, oscillometric sphygmomanometer to obtain multiple BP readings while the patient rests alone in a quiet room. Studies in community-based, primary care settings, in patients referred for 24-hour AMBP, and in patients referred to a hypertension specialist have all shown that AOBP can virtually eliminate the white coat response with AOBP readings being similar to the mean awake ambulatory BP. AOBP has other advantages over manual BP measurement. Multiple readings can be taken without a health professional being present, thus saving valuable time of office personnel for other tasks. Unlike manual BP, AOBP readings are similar when taken in the office and in nontreatment settings such as an AMBP unit. Multiple AOBP readings can be taken as frequently as every 1 minute, from the start of one reading to the start of the next. Finally, the cutpoint for normal BP vs. hypertension for AOBP (135/85 mm Hg) is similar to values for both awake ambulatory BP and home BP.
_
A recent reevaluation of the cutpoint for a normal manual BP reading in routine practice has raised further questions about the use of the mercury sphygmomanometer. The traditional value of 140/90 mm Hg for defining hypertension was derived from carefully measured BP readings taken in the context of research studies or by specially trained health professionals in population surveys and in other similar research settings. However, manual BP measurement in routine office practice is usually not performed in accordance with recommended guidelines despite intensive efforts during recent decades on the part of organizations such as the American Heart Association to improve the quality of manual BP measurement in the community. In the “real world,” manual BP readings are of relatively poor quality and accuracy, often exhibit digit preference (rounding off to the nearest zero), have little or no correlation with target organ damage, and show a weak correlation with the awake ambulatory BP, a gold standard for determining future risk of cardiovascular events in relation to BP status. The net result is a “real world” cutpoint for manual BP/hypertension which is closer to 150/95 mm Hg instead of 140/90 mm Hg with about 25% of the patients exhibiting a clinically important white coat response, leading to possible overtreatment or inappropriate treatment of hypertension. Whereas, intensive education of physicians and other health professionals to improve the quality of BP measurement in routine practice has met with little success, the replacement of manual recorders such as the mercury sphygmomanometer with AOBP is relatively inexpensive, requires minimal training, and will make accurate BP measurement much less dependent on the expertise and training of the person recording the BP.
_________
Self measurement of blood pressure (SMBP):
Self measurement (monitoring) of blood pressure is when a person (or carer) measures their own blood pressure outside the clinic—at home, in the workplace, or elsewhere. Self monitoring allows multiple measurements and therefore provides a more precise measure of “true” blood pressure and information about variability in blood pressure. Many investigators have found differences between blood pressure values obtained by health care professionals in a clinic and automated, self-determined measures obtained at home, the latter being on average about 8/4 mm Hg lower. The correlation between measurements at home and in the clinic has been reported to be as low as 0.21 for diastolic blood pressure. In line with these low correlations Padfield and colleagues reported that the sensitivity and specificity of self-determined measures in diagnosing hypertension when compared with pressures measured in the clinic were 73% and 86% respectively. This finding assumes that the clinic pressures constitute a gold standard, which may not be the case. Thus is raised the issue of which readings, home or clinic, are more valid. Studies have demonstrated that blood pressure measurements obtained at home can be highly reproducible. Reproducibility of readings is essential for accuracy, and these studies are therefore reassuring. Furthermore, Gould and colleagues found that the accuracy of self-determined readings at home and of professionally taken readings at the clinic were similar, as determined by intra-arterial pressures. However, the overriding issue here is the validity of self-determined measures of blood pressure in decisions about the diagnosis of hypertension and whether treatment should be initiated.
_
Effective management of BP has been shown to dramatically decrease the incidence of stroke, heart attack, and heart failure. However, hypertension is usually a lifelong condition, and long-term adherence to lifestyle modification (such as smoking cessation, regular exercise, and weight loss) and medication treatment remains a challenge in the management of hypertension. Thus an increasing focus has been placed on developing strategies that can improve adherence and result in satisfactory BP control with the goal of improving health outcomes for hypertensive patients. One such proposed method is self-measured blood pressure (SMBP) monitoring. SMBP refers to the regular self-measurement of a patient’s BP at home or elsewhere outside the office or clinic setting. However, while patient self-participation in chronic disease management appears promising, the sustainability and clinical impact of this strategy remain uncertain. Also its impact on health care utilization is uncertain, since it may replace office visits for BP checks but may increase overall intensity of surveillance and treatment.
_
Self-monitoring of blood pressure has been advocated as an adjunct to diagnosis, particularly for the detection of white coat hypertension (defined as pressure that is persistently high when measured at the clinic but normal when measured elsewhere.) Although there have been studies of home blood pressure monitoring as part of the management of treated hypertension, there have been few of self-monitoring as an adjunct to diagnosis and the initiation of therapy. Unfortunately, there is little information on the distribution of self-monitored pressures in the normotensive population, and there have been no prospective studies assessing the relation between level of self-monitored blood pressure and incidence of major illness or death from cardiovascular disease. The evidence from less rigorous cross-sectional assessments of monitoring at home and at the clinic is conflicting. Julius and colleagues have found that patients with high readings at the clinic and lower ones on self-assessment have hypertensive target-organ findings and cardiovascular risk factors similar to those of patients with sustained borderline elevation of blood pressure both at the clinic and at home. However, other investigators have found higher correlations of electrocardiographically determined left ventricular hypertrophy with self-determined blood pressure readings than with casual office readings and higher correlations of echocardiographically determined left ventricular mass with blood pressure readings taken at home than with those taken at the clinic.
_
Given the consequences of both false-negative and false-positive diagnoses, the inaccuracy of many devices for the self-determination of blood pressure and the potential value of additional measurements in a patient s home, the accuracy of self-monitoring should be studied further and its value in diagnosis determined for those with mild elevations in blood pressure at the clinic. If patients are asked to measure their blood pressure at home it is important that their equipment and technique be checked by health care professionals to ensure accuracy. Mercury sphygmomanometers are the most accurate and dependable devices and can be purchased for home use, but they are more difficult to master than the semi-automated or automated devices that are widely available. Mercury devices should likely not be suggested for patients with young children at home in view of the possibility of a mercury spill. Patients with difficulty hearing or seeing should only be asked to use automated devices if someone else in the home can assist them. Some sphygmomanometers of all types are accurate, but most nonmercury devices are not. It is important that patients use the correct cuff size for their arm circumference. Thus, the given recommendations for blood pressure determination apply to the use of automated devices if they are found to be as accurate as mercury devices.
________
Home BP:
Home BP is information obtained under a non-medical setting and essentially by self-measurement. With home BP measurements, time-related BP information can be obtained over a long period. On the basis of these characteristics, home BP provides the information indispensable for the diagnosis of white-coat hypertension, masked hypertension or early-morning hypertension. The frequency of white-coat hypertension based on home BP measurements has been reported to be 38–58% in cohorts of the general population, 15% in untreated patients with hypertension and 12–19% in hypertensive patients being treated. The frequency of masked hypertension based on home BP is reported to be about 10% in cohorts of the general population and 11–33% in hypertensive patients under treatment. Also, some home BP-measuring devices provide BP information during sleep at night. Moreover, home BP measurements are used as a means to average BP over a long period of time and, thus, are used as a means to transform essentially highly variable BP values into stable BP information in the form of averaged BP. This is applied to BP measurements for pregnant women and children. Many studies have also reported the usefulness of home BP measurements for the diagnosis and treatment of hypertension in dialysis patients and diabetic patients, in whom daily management of BP mediates critical results on their outcome.
_
Home blood pressure monitoring has been shown to be feasible; acceptable to patients, nurses, and doctors in general practice; and more suitable for the screening of “white coat” hypertension than ambulatory blood pressure monitoring. The white coat effect is important in the diagnosis and treatment of hypertension, even in a primary care setting, and is not a research artefact. Either repeated measurements by health professionals or ambulatory or home measurements may substantially improve estimates of blood pressure and management and control of hypertension. Home blood pressure measurements are the most acceptable method to patients and are preferred to either readings in the clinic or ambulatory monitoring. They provide accurate blood pressure measurements in most patients, although some patients of low educational level may have poor reporting accuracy. Finally, blood pressure monitoring at home might help to improve awareness and concordance, and thus overall effective management.
_
Morning hypertension, and morning and evening home BP:
Although there is no precise definition of morning hypertension, a condition with a specifically high BP after waking early in the morning may be referred to as morning hypertension. According to the absolute values of home BP or AMBP, a value of greater than or equal to135/85 mm Hg in the morning, for example, may be regarded as morning hypertension; however, the value in the morning must be higher than that in the evening to confirm that BP is high specifically in the morning. Morning hypertension may be the result of one of two patterns of diurnal BP changes. One is the morning surge, which is a rapid elevation in BP around awakening from a low nocturnal level. The other is high BP in the morning observed in non-dippers, who show no normal nocturnal decrease in BP, or risers, who show nighttime elevations in BP. Both patterns are considered to be possible risk factors of cardiovascular diseases. Those who exhibit large morning–evening differences in BP have marked target organ damage, such as left ventricular hypertrophy. However, home BP measured in the evening also has a high prognostic significance.
_
Nighttime BP during SMBP:
During sleep at night, BP is usually measured by AMBP. Recently, home BP-measuring devices capable of monitoring BP during sleep at night have been developed, and their performance has been close or equal to that of AMBP. Using a home BP-monitoring device, BP during sleep is measured once or twice during the night, although the frequency of measurement can be preset freely, and is therefore able to capture the BP in relation to the quality of sleep at the time of the measurement. Recently, midnight BP and diurnal changes in BP, as well as morning BP, have become of interest because of their relationships with target organ damage and prognosis. Decreases of 10–20% in nocturnal BP compared with daytime BP are classified as a normal pattern of diurnal changes (dipper), decreases of 0–10% as a no-nocturnal-dip type (non-dipper), elevations in BP during the nighttime compared with the daytime as a nocturnal elevation type (riser), and decreases of greater than or equal to20% in nocturnal BP as an excessive decrease type (extreme dipper). The prognosis has been poor in non-dippers and risers. In non-dippers and risers, hypertensive target organ damage, such as asymptomatic lacunar infarction, left ventricular hypertrophy and microalbuminuria, are observed more frequently than in dippers. Prospective studies have shown that the risk of cardiovascular diseases is higher in non-dippers than in dippers. According to the results of the Ohasama study, the risk of cardiovascular diseases is high in non-dippers even if they are normotensive. Therefore, the clinical significance of nocturnal BP is attracting interest. The results of a large-scale intervention study and an international collaborative study of observation studies show that low nighttime and low daytime BP are considered to improve the prognosis of patients. For the future, a wide application of home BP-measuring devices is expected to evaluate the BP during sleep at night in relation to the quality of sleep and to diurnal changes in BP.
________
Most suitable device for SMBP:
Arm-cuff devices based on the cuff-oscillometric method validated on the basis of the auscultation method are recommended for home BP measurements.
Why?
Previously, mercury column manometers or aneroid manometers, in conjunction with the auscultation method, have been used for home BP measurements. However, these manometers, especially aneroid manometers, are sometimes unreliable and inaccurate. Mercury column manometers are cumbersome and cause environmental pollution. Furthermore, the auscultation method involves a subjective decision and a complex technique, and technical instruction and training are necessary to perform an accurate auscultation. For all these reasons, previous devices for home BP measurements were not widely accepted and, consequently, not widely distributed. In the 1960s, electrical devices based on the microphone method were introduced for home BP measurements. However, because of the mechanical properties of the microphone, these devices were costly and subject to frequent malfunctions. The microphone method also had an inherent shortcoming in determining the phase V Korotkoff sound making determination of diastolic BP inaccurate. Thus, microphone devices for home BP measurements were not widely distributed. During this period, theoretical analysis of the cuff-oscillometric principle advanced extensively. In 1969, Posey et al. discovered that the maximum oscillation of intra-cuff pressure was nearly identical to the mean arterial BP, and the cuff-oscillometric principle was originally introduced as a method of determining mean arterial BP. Several experimental studies revealed that SBP and DBP could be estimated from the pattern of the gradual increase and decrease in cuff oscillation during cuff-pressure deflation. This basic algorithm has been improved by including procedures to correctly approximate the characteristic changes in cuff oscillation to the phase I and phase V Korotkoff sounds, and now almost all electrical devices for home BP measurements are based on the cuff-oscillometric principle. However, the different properties of the Korotkoff sounds and cuff oscillation led to an unavoidable difference in BP values between the two methods. Nevertheless, devices based on the cuff-oscillometric principle have become the norm for home BP measurements because of their simple mechanical properties, requiring only measurements in cuff-pressure changes. Therefore, these devices incorporate only a pressure sensor. Such a simple mechanism makes the device less troublesome and cheaper. The cuff-oscillometric device has another advantage when compared with the microphone device, in that surrounding noise does not interfere with BP measurements. More accurate BP values in patients with atrial fibrillation or arrhythmia are also available by cuff-oscillometric devices when compared with the Korotkoff sound method, as ectopically large or small pulses are averaged by the algorithm. Such factors encourage the production and distribution of cuff-oscillometric devices for home BP measurements. However, it is remarkable that sphygmomanometers used in the clinical setting have been changing from the Korotkoff sound method to cuff-oscillometric devices without much difficulty.
_
Although the mercury column sphygmomanometer with auscultation is becoming obsolete, the gold standard for clinical practice is still the Korotkoff sound method using a mercury column sphygmomanometer. Almost all epidemiological and clinical studies on hypertension have been based on casual-clinic BP measured by the Korotkoff sound method. Therefore, clinical and epidemiological information obtained using the cuff-oscillometric principle needs to be validated by the accumulation of data. Various manufacturers of devices using the cuff-oscillometric principle may use different algorithms, leading to differences among devices in BP measurements from a single subject. In practice, the accuracy of automatic devices is determined by comparison with the auscultation method, and no other standard method is currently available for this purpose. The issue here is the subjectivity and the possible inaccuracy of auscultation when the auscultation method is used as a standard. To exclude the shortcomings of the auscultation method, equipment based on objective methods should be developed for the calibration of automatic devices, in which the Korotkoff sound signal is treated with an established algorithm, and cuff-oscillometric devices are validated from this standard equipment. Objective and accurate evaluation of these automatic devices is a prerequisite for the authorization of cuff-oscillometric devices for home BP measurements. The accumulation of clinical and epidemiological data obtained by authorized cuff-oscillometric devices may finally validate such devices as tools for clinical decision making. As BP measurements in a clinical setting are now mostly obtained by cuff-oscillometric devices, the necessary data will be accumulated soon.
_
Choosing a Home Blood Pressure Monitor:
Here are some other tips to follow when shopping for a blood pressure monitor.
1. Choose a validated monitor:
Make sure the monitor has been tested, validated and approved by the Association for the Advancement of Medical Instrumentation, the British Hypertension Society and the International Protocol for the Validation of Automated BP Measuring Devices.
2. Ensure the monitor is suitable for your special needs:
When selecting a blood pressure monitor for the elderly, pregnant women or children, make sure it is validated for these conditions.
3. Make sure the cuff fits:
Children and adults with smaller or larger than average-sized arms may need special-sized cuffs. They are available in some pharmacies, from medical supply companies and by direct order from companies that sell blood pressure cuffs. Measure around your upper arm and choose a monitor that comes with the correct size cuff.
__
________
Why is home monitoring important?
1. Charting provides a “time-lapse picture”:
Your healthcare provider will want an accurate picture of the situation inside your arteries. One measurement taken at the doctor’s office is like a snapshot. It tells what your blood pressure is at that moment. Since there are no symptoms for HT and no way to sense fluctuations in blood pressure, measuring is the only way to get the facts. Readings can vary throughout the day and can be temporarily influenced by factors such as emotions, diet and medication. A record of readings taken over time can provide you and your healthcare provider a clearer picture of your blood pressure. It can be like a time-lapse picture or movie, providing information on what is happening with your blood pressure over time.
2. Charting can help eliminate false readings:
Some people experience anxiety when at a doctor’s office, which leads to temporarily higher readings. This condition is known as “white-coat hypertension.” At the other extreme, some individuals have normal readings in a professional’s office but elevated readings outside the office. This condition is often referred to as “reverse white-coat hypertension” or “masked hypertension.” Such false readings can lead to over-diagnosis or misdiagnosis of HT. Self-measurement at home is good to reveal whether your blood pressure reading in the doctor’s office is correct.
_
Who should home monitor?
Home monitoring may be especially useful for:
1. Patients starting HT treatment to determine its effectiveness
2. Patients requiring closer monitoring than intermittent office visits provide, especially individuals with coronary heart disease, diabetes and/or kidney disease
3. Pregnant women since preeclampsia or pregnancy-induced hypertension can develop rapidly
4. People who have some high readings at the doctor’s office, to rule out white-coat hypertension and confirm true HBP
5. Elderly patients, because the white-coat effect increases progressively with age
6. People suspected of having masked hypertension
_
_
_
Why do I need to monitor my blood pressure at home?
Monitoring your blood pressure at home offers several benefits. It can:
1. Help make an early diagnosis of high blood pressure. If you have pre-hypertension, or another condition that could contribute to high blood pressure, such as diabetes or kidney problems, home blood pressure monitoring could help your doctor diagnose high blood pressure earlier than if you have only infrequent blood pressure readings in the doctor’s office.
2. Help track your treatment. Home blood pressure monitoring can help people of all ages keep track of their condition including children and teenagers who have high blood pressure. Self-monitoring provides important information between visits to your doctor. The only way to know whether your lifestyle changes or your medications are working is to check your blood pressure regularly. Keeping track of changes can help you and your health care team make decisions about your ongoing treatment strategy, such as adjusting dosages or changing medications.
3. Encourage better control. Taking your own blood pressure measurements can result in better blood pressure control. You gain a stronger sense of responsibility for your health, and you may be even more motivated to control your blood pressure with an improved diet, physical activity and proper medication use.
4. Cut your health care costs. Home monitoring may cut down on the number of visits you need to make to your doctor or clinic. This can reduce your overall health care costs, lower your travel expenses and save in lost wages.
5. Check if your blood pressure is different outside the doctor’s office. Your doctor may suspect that your blood pressure goes up due to the anxiety associated with being at the doctor’s office, but is otherwise normal — a condition called white coat hypertension. Monitoring blood pressure at home or work, where that kind of anxiety won’t cause those spikes, can help see if you have true high blood pressure or simply white coat hypertension.
6. Home and workplace monitoring may also help when the opposite occurs — your blood pressure seems fine at the doctor’s office, but is elevated elsewhere. This kind of high blood pressure, sometimes called masked hypertension, is more common in women and those who have cardiovascular risk factors, such as obesity, high blood cholesterol and high blood sugar.
_
Diagnostic threshold for hypertension in SMBP:
________
Schedule of SMBP:
A systematic review found little evidence to determine how many readings are appropriate, with considerable variation in recommendations in the literature. There is disagreement between guidelines for SMBP at home:
(i) The European Society of Hypertension and the 2012 Canadian Hypertension Education Program recommend duplicate SMBPs in the morning and evening;
(ii) The American Society of Hypertension recommends triplicate SMBPs;
(iii) The Japanese Society of Hypertension recommends at least one SMBP.
The 1st SMBP in a triplicate tends to be higher than the 2nd and 3rd. The differences are quite small. They amount, on average, to 3 – 4 mmHg for systolic BP, 1 mmHg for diastolic and 1 – 2 mmHg for the heart rate.
__
Blood pressure varies throughout the day and drugs are typically taken in the morning. This usually results in peaks and troughs during the day, so it has been recommended that blood pressure is measured in the morning and the evening. Japanese data suggest that blood pressure measured in the morning correlates best with end organ damage, but these findings may be confounded by Japanese customs such as taking hot baths in the evening. Current guidelines for SBPM recommend that in untreated patients there should be an initial 7-day measurement period with 2 readings taken in the morning and in the evening at predefined times (6 am–9 am and 6 pm–9 pm). The average of day 2 through 7 values should be taken as reference for the follow-up period. Once treatment is initiated, SBPM should be used exactly as in the pre-treatment phase and the readings should preferably be taken at trough, i.e., before drug intake in case of once-daily administration. When changes in treatment occur, the averages of the SBPM values measured over 2 weeks should be used to assess BP control. It follows that many BP readings should be collected that may create some problems for interpretations. For reasons of time and practicality, doctors are reluctant to calculate the average of tens or even hundreds of values and thus they usually make a cursory inspection of patients’ reports. In addition, there is experimental evidence that many patients tend to manipulate the BP reports, excluding those values that do not seem appropriate to them. Current international guidelines do not provide specific recommendations on how to solve these problems.
_
Long term monitoring for people on stable treatment:
Data from the PROGRESS trial (Perindopril Protection against Recurrent Stroke study) indicate that true changes in blood pressure occur slowly, and that for patients on stable medication a reasonable time frame for remeasurement would be every six to 12 months (Keenan K, Hayen A, Neal BC, Irwig L, 2008). Although the PROGRESS trial looked at office measurements of blood pressure, this estimate is probably valid for patients who self monitor. However, I think we need more studies to determine how frequently SMBP done for patients on long term stable treatment.
_
A study was done to determine frequency of SMBP by patents:
__________
Correct way for SMBP:
1. Only measure when being relaxed. Take a rest for approximately two to three minutes before each measurement. Sit relaxed in an upright position. Even desk work increases the blood pressure by 6mm Hg (systolic value) and 5mm Hg (diastolic value) on average.
2. A full bladder causes an increase in blood pressure of approx. 10mm Hg.
3. Check both a proper cuff size and a proper fit of the cuff. The cuff should be at the level of right atrium.
4. Don’t talk and move during the measurement. Talking elevates your values by 17/13 mm Hg.
5. A repeated measurement should be started not earlier than a minute after the prior measurement.
6. Change therapy only after consulting your physician.
7. In some people, there is a significant difference in blood pressure numbers between their right and left arm. Although the reason for this is unclear, guidelines recommend that blood pressure be measured in both arms at the initial consultation. If there is a significant difference between the two readings, the arm with the higher reading should be used for future monitoring.
_
| Checklist for correct use of automated home blood pressure monitoring machine | ||
| 1 | Do not use caffeine products 30 minutes before measuring BP | |
| 2 | Do not use tobacco products 30 minutes before measuring BP | |
| 3 | Do not use alcohol products 30 minutes before measuring BP | |
| 4 | No exercise 30 minutes before measurement of BP | |
| 5 | Rest for 5 minutes before the first reading is to be taken and patient should be relaxed as measurement is taking place | |
| 6 | No full bladder before measuring BP | |
| 7 | Appropriate cuff size: the bladder length should be 80% of arm circumference | |
| 8 | Appropriate cuff size: the bladder width should be at least 40% of arm circumference (i.e. a length-to-width ratio of 2:1) | |
| 9 | Sit in a comfortable position, with legs and ankles uncrossed, and back and arm supported | |
| 10 | All clothing that covers the location of cuff placement should be removed. Long sleeves should not be rolled up to avoid tourniquet effect | |
| 11 | Wrap the correctly sized cuff smoothly and snugly around the upper part of the bare arm | |
| 12 | The cuff should fit snugly, but there should be enough room to slip one fingertip under the cuff | |
| 13 | The lower end of the cuff should be 2–3 cm above the antecubital fossa | |
| 14 | The middle of the cuff on the upper arm should be at the level of the right atrium (the midpoint of the sternum) | |
| 15 | No talking during BP measurement | |
| 16 | No moving during BP measurement | |
| 17 | A minimum of two readings should be taken at intervals of at least 1 minute, and the average of those readings should be used to represent the patient’s BP | |
| 18 | If there is a >5 mmHg difference between the first and second readings, an additional two readings should be obtained, and then the average of these multiple readings should be used (ask patient if it is not applicable during the patient demonstration) | |
| 19 | Properly record the BP reading in the log book | |
_
________
Patient education:
People should be aware of the main causes of inaccuracy in measurement, which can be divided into three broad categories—patient factors, technique and measurer factors, and device inaccuracy. Talking (increase of 17/13 mm Hg in one study) or crossing of legs (increase of 7/2 mm Hg in another study) during measurement and arm position (increase or decrease of 8 mm Hg for every 10 cm above or below heart level) can significantly alter measurements. Education regarding disclosure of results is important because studies have shown that up to 20% of readings are not divulged to healthcare professionals.
_
________
Which patients may not benefit from self monitoring?
To date, trials of self monitoring have studied people who are willing to monitor themselves, so the question remains whether self monitoring should be recommended for all. People with an absolute contraindication for self monitoring are rare and include those in whom it is impossible to measure indirect blood pressure accurately (such as amputees). The evidence for self monitoring in pregnant women, children, and those with vascular problems such as Raynaud’s disease is sparse, and self monitoring should be undertaken with caution in these groups. Atrial fibrillation, which may affect the accuracy of oscillometric algorithms in automated monitors, may be problematic, although evidence indicates that accurate readings are possible with standard models. People with conditions that might preclude self monitoring, such as dementia or stroke, may need the help of a carer. Increased anxiety is often quoted as a problem in self measurement, and anecdotally some people seem not to cope with self monitoring. Studies that have looked for increased anxiety resulting from self monitoring have been negative, but this may reflect the population studied.
_
____
When to consult doctor in SMBP:
The following table represents the values (units mmHg) supplied by the World Health Organisation (WHO):
| Range | Systolic | Diastolic | Recommendation |
| blood pressure to low | < 100 | < 60 | Consult your doctor |
| blood pressure optimum | 100 – 120 | 60 – 80 | Self-check |
| blood pressure normal | 120 – 130 | 80 – 85 | Self-check |
| blood pressure slightly high | 130 – 140 | 85 – 90 | Consult your doctor |
| blood pressure to high | 140 – 160 | 90 – 100 | Seek medical advice |
| blood pressure far too high | 160 – 180 | 100 – 110 | Seek medical advice |
| blood pressure dangerously high | > 180 | > 110 | Urgently seek medical advice! |
It is recommended that you record your blood pressure values frequently and discuss them with your doctor. If your systolic values are frequently above 140 and/or the diastolic values above 90, you should consult your doctor. It is normal that blood pressure values are sometimes higher and lower and there is no need to worry if the results are sometimes higher than the above limits. But if your pressure is above the limits in most cases, you should consult your doctor!
___________
What is the value of self monitoring in diagnosis and prognosis?
Faster diagnosis:
Trials have shown that morbidity and mortality are significantly lower in people whose blood pressure is reduced earlier rather than later. The British Hypertension Society recommends that hypertension is diagnosed by using a series of office blood pressure readings taken over one to 12 weeks, depending on the blood pressure level. Self monitoring can provide more precise data in a much shorter time.
Improved accuracy:
Self monitoring can improve diagnostic and predictive accuracy. A large cohort study in Japan showed that self monitoring predicted the risk of stroke better than office readings. In this study, risk of stroke increased 29% (95% confidence interval 16% to 44%) for each 10 mm Hg increase in home systolic readings versus 9%(0%to 18%) for office readings. The predictive value of home measurement improved with the number of measurements, with the best predictive value being seen with 25 measurements. Another large cohort study used an upper limit for normality of 135/85 mm Hg for self monitoring and found that each 10 mm Hg increase above this was associated with a 17% increase in risk of cardiovascular disease, even when office blood pressure was normal.
Reduced risk:
Self monitoring avoids two situations where office readings can mislead—white coat hypertension, where out of home readings are normal but office readings are raised, and masked hypertension, where the opposite is the case. Risk of death from cardiovascular disease increases progressively from normal readings at home and in the office, to white coat hypertension, then masked hypertension, and finally increased readings at home and in the office. Furthermore, one large cohort study found that the prognosis for masked hypertension was similar to that for uncontrolled office hypertension. People with masked hypertension are rarely identified, and self monitoring may be particularly helpful for this group, especially if it is used as a screening tool for people with high-normal office readings.
______
SMBP: from measurement to control:
How does self monitoring reduce blood pressure?
Better adjustment of antihypertensive drugs:
Doctors do not always treat patients with documented raised blood pressure even though antihypertensives are known to reduce blood pressure and the risk of cardiac disease. Self monitoring of blood pressure may lead patients to discuss their blood pressure with their doctor and this may encourage appropriate prescription of antihypertensives.
Improved compliance with scheduled treatment:
Self monitoring makes patients more aware of their blood pressure level; this might increase their illness perceptions and subsequent health behaviours and therefore improve adherence to drugs. Of 11 randomised controlled trials of self monitoring that reported measures of treatment adherence, six showed a statistically significant improvement in adherence, but in five of these six trials self monitoring was part of a complex intervention. These trials must be treated cautiously because pill counting was often used to measure compliance as opposed to more reliable methods.
Improved non-pharmacological interventions:
Self monitoring may lead to improvements in health behaviours, such as diet and exercise, that help reduce blood pressure. A randomised controlled trial found significant changes in body mass index at six and12 months in a self monitoring group compared with controls. A reduction in alcohol intake was also seen at six but not 12 months. No effect was seen on self reported physical activity or salt intake.
Habituation to measurement:
Repeated measurement of blood pressure lowers blood pressure readings. Presumably this is because people habituate to the measurement process and show less of an alarm response when the cuff is inflated. However, results of a randomised trial of self monitoring that included ambulatory monitoring as an outcome measure supported the conclusions of a previous review implying that habituation to measurement was not the reason for the lowering of blood pressure in self monitoring.
____
Self-measured home blood pressure in predicting ambulatory hypertension:
Physicians are commonly uncertain whether a person with office blood pressure (BP) around 140/90 mm Hg actually has hypertension. This is primarily because of BP variability. One approach is to perform self-measured home BP and determine if home BP is elevated. There is a general agreement that if home BP is ≥135/85 mm Hg, then antihypertensive therapy may be commenced. However, some persons with home BP below this cut-off will have ambulatory hypertension. Researchers therefore prospectively studied the role of home BP in predicting ambulatory hypertension in persons with stage 1 and borderline hypertension. They studied in a cross-sectional way home and ambulatory BP in a group of 48 patients with at least two elevated office BP readings. The group was free of antihypertensive drug therapy for at least 4 weeks and performed 7 days of standardized self-BP measurements at home. They examined the relationships of the three BP methods and also defined a threshold (using receiver operating curves) for home BP that captures 80% of ambulatory hypertensives (awake BP ≥135/85 mm Hg). Office systolic BP (145 ± 13 mm Hg) was significantly higher than awake (139 ± 12 mm Hg, P = 0.013) and home (132 ± 11 mm Hg, P <0.001) BP. Office diastolic BP (88 ± 4 mm Hg) was higher than home diastolic BP (80 ± 8 mm Hg, P < 0.001) but not different from awake diastolic BP (88 ± 8 mm Hg, P = 0.10). Home BP had a higher correlation (compared with office BP) with ambulatory BP. The home BP-based white coat effect correlated with ambulatory BP-based white coat effect (r = 0.83, P = 0.001 for systolic BP; r = 0.68, P = 0.001 for diastolic BP). The threshold for home BP of 80% sensitivity in capturing ambulatory hypertension was 125/76 mm Hg. The preliminary data suggest that a lower self-monitored home BP threshold should be used (to exclude ambulatory hypertension) in patients with borderline office hypertension.
_______
SMBP in special circumstances and groups:
Certain groups of people merit special consideration for the measurement of blood pressure—because of age, body habitus, or disturbances of blood pressure related to hemodynamic alterations in the cardiovascular system. Home BP, measured by patients themselves over a long period, is widely used for the management of chronic diseases in which BP control has a critical role for the prognosis. The AHA/ASH/PCNA joint statement and ESH Guidelines for home BP measurements emphasize the importance of home BP measurements in the management of diabetes mellitus, pregnancy, children and renal diseases. Now I will discuss special populations vis-à-vis SMBP:
_
Elderly Patients:
Elderly patients are more likely to have WCH, isolated systolic hypertension, and pseudohypertension. Blood pressure should be measured while seated, 2 or more times at each visit, and the readings should be averaged. Blood pressure should also be taken in the standing position routinely because the elderly may have postural hypotension. Hypotension is more common in diabetic patients. It is frequently noticed by patients on arising in the morning, after meals, and when standing up quickly. Self-measurements can be quite helpful when considering changes in dosage of antihypertensive medications. Ambulatory blood pressure monitoring, sometimes coupled with Holter recordings of ECGs, can help elucidate some symptoms such as episodic faintness and nocturnal dyspnea. A study found that elderly have a relatively poor understanding of their blood pressure readings and targets, but a subset was considerably more knowledgeable and potentially suited to be more involved in blood pressure self-management.
_
Pulseless Syndromes:
Rarely, patients present with occlusive arterial disease in the major arteries to all 4 limbs (e.g., Takayasu arteritis, giant cell arteritis, or atherosclerosis) so that a reliable blood pressure cannot be obtained from any limb. In this situation, if a carotid artery is normal, it is possible to obtain retinal artery systolic pressure and use the nomogram in reverse to estimate the brachial pressure (oculoplethysmography), but this procedure and the measurement of retinal artery pressures are not generally available. If a central intra-arterial blood pressure can be obtained, a differential in pressure from a noninvasive method can be established and used as a correction factor.
_
Arrhythmias:
When the cardiac rhythm is very irregular, the cardiac output and blood pressure varies greatly from beat to beat. There is considerable inter-observer and intra-observer error. Estimating blood pressure from Korotkoff sounds is a guess at best; there are no generally accepted guidelines. The blood pressure should be measured several times and the average value used. Automated devices frequently are inaccurate for single observations in the presence of atrial fibrillation, for example, and should be validated in each subject before use. However prolonged (2 to 24 hours) ambulatory observations do provide data similar to that in subjects with normal cardiac rhythm. Sometimes, an intra-arterial blood pressure is necessary to get a baseline for comparison. If severe regular bradycardia is present (e.g., 40 to 50 bpm), deflation should be slower than usual to prevent underestimation of systolic and overestimation of diastolic blood pressure. Hypertension and atrial fibrillation (AF) often coexist and are strong risk factors for stroke.
_
Blood Pressure Measurement in Atrial Fibrillation: NICE Hypertension Guideline Update 2011:
Because automated devices may not measure blood pressure accurately if there is pulse irregularity (for example, due to atrial fibrillation), palpate the radial or brachial pulse before measuring blood pressure. If pulse irregularity is present, measure blood pressure manually using direct auscultation over the brachial artery.
_
Automated blood pressure measurement in atrial fibrillation: a systematic review and meta-analysis:
The measurement of blood pressure in atrial fibrillation is considered as difficult and uncertain, and current guidelines recommend the use of the auscultatory method. The accuracy of automated blood pressure monitors in atrial fibrillation remains controversial. A systematic review and meta-analysis was performed of studies comparing automated (oscillometric or automated Korotkoff) versus manual auscultatory blood pressure measurements (mercury or aneroid sphygmomanometer) in patients with sustained atrial fibrillation. Twelve validations were analyzed (566 patients; five home, three ambulatory and three office devices). The meta-analysis found that these monitors appear to be accurate in measuring SBP but not DBP. Given that atrial fibrillation is common in the elderly, in whom systolic hypertension is more common and important than diastolic hypertension, automated monitors appear to be appropriate for self-home but not for office measurement.
_
An embedded algorithm for the detection of asymptomatic AF during routine automated BP measurement with high diagnostic accuracy has been developed and appears to be a useful screening tool for elderly hypertensives.
_
Obese people:
The association between obesity and hypertension has been confirmed in many epidemiological studies. Obesity may affect the accuracy of measurement of blood pressure in children, young and elderly people, and pregnant women. The relation of arm circumference to bladder dimensions is particularly important. If the bladder is too short, blood pressure will be overestimated—“cuff hypertension”—and if it is too long, blood pressure may be underestimated. The increasing prevalence of the metabolic syndrome, of which hypertension is a major component, means that accurate measurement of blood pressure increasingly becomes important. Today, modern automatic devices can overcome the problem of miscuffing in patients with large arms as a result of a special software algorithm that can provide accurate BP readings over a wide range of arm circumferences when coupled with a single cuff of standard dimensions. A tronco-conical–shaped cuff may be a key component of this instrumentation because it fits better on large, conical arms. In fact, the use of an inappropriately small rectangular cuff can be the source of large errors when BP is measured with the oscillometric method, in which measured cuff pressure oscillations are a reflection of the entire artery volume change under the cuff and does not involve the central section only. Instead of brachial artery, radial artery is more suitable for SMBP of obese people by listening for Korotkoff sounds over the radial artery, using a Doppler probe, or using an oscillometric device. Whether validated wrist BP monitors can be an appropriate solution for very obese patients should also be established. Unfortunately, there is no available evidence to show that BP measured with upper arm oscillometric devices or wrist monitors is reliable in the obese population. Assessment of BP in obese individuals is further complicated by the fact that the discrepancies between office and out-of-office BPs are more pronounced in this group than in the nonobese segment of the population. Prospective trials designed to specifically evaluate whether BP measured with automatic devices in obese patients can predict cardiovascular events as accurately as BP measured with the traditional auscultatory technique will shed light on this controversial issue.
_
Children:
_
_
Pregnant Women:
Hypertension is the most common medical disorder of pregnancy and occurs in 10% to 12% of all pregnancies. The detection of elevated blood pressure during pregnancy is one of the major aspects of optimal antenatal care; thus, accurate measurement of blood pressure is essential. Changes in BP during pregnancy are markedly affected by the season. Seasons are important for the diagnosis of hypertension during pregnancy and preeclampsia. Mercury sphygmomanometry continues to be the recommended method for blood pressure measurement during pregnancy. Blood pressure should be obtained in the seated position. Measurement of blood pressure in the left lateral recumbency, on the left arm, does not differ substantially from blood pressure that is recorded in the sitting position. Therefore, the left lateral recumbency position is a reasonable alternative, particularly during labor. If the patient’s upper arm circumference is 33 cm or greater, a large blood pressure cuff should be used. In the past, there had been some question as to whether the fourth (K4) or fifth (K5) Korotkoff sound should be used to define the diastolic blood pressure. The International Society for the Study of Hypertension in Pregnancy currently recommends using K5 for the measurement of diastolic blood pressure in pregnancy. When sounds are audible with the cuff deflated, K4 should be used. It is recognized that alternatives to mercury devices may be necessary in the future, and a small number of automated blood pressure recorders have been validated for use in pregnancy. Self-monitoring may be useful in evaluating blood pressure changes during pregnancy.
_
_
Studies have found that home BP monitoring is the optimal method for the early detection of and early preventive intervention in preeclampsia and eclampsia. White-coat hypertension has also been frequently detected by home BP measurements in pregnant women.
_
Patients who take antihypertensive drugs:
In patients who take antihypertensive drugs, the timing of measurement may have a substantial influence on the blood pressure. The time of taking antihypertensive drugs should be noted.
_
Blood pressure in patients who are exercising:
Systolic blood pressure increases with increasing dynamic work as a result of increasing cardiac output, whereas diastolic pressure usually remains about the same or moderately lower. An exaggerated blood pressure response during exercise may predict development of future hypertension.
_
Diabetes mellitus and hypertension:
Individuals with diabetes are at great risk for cardiovascular disease. Part of this increased risk is because of hypertension. There is a very high incidence of hypertension in patients with diabetes. One survey estimated that 54.8% of Caucasians, 60.4% of African Americans, and 65.3% of Mexican Americans who had diabetes also had hypertension. Several trials have also demonstrated the importance of blood pressure–lowering in hypertensive patients with diabetes. Two of the most significant of these trials were the United Kingdom Prospective Diabetes Study (UKPDS) and the Hypertension Optimal Treatment (HOT) study. The HOT study reported a 51% reduction in cardiac events in the diabetes subpopulation (n = 1,501) who were randomized to the more intensive blood pressure arm (goal: diastolic blood pressure of 80 vs. 90 mmHg). The UKPDS reported significant reductions in its intensive blood pressure arm (mean result: 144/82 vs. 154/87 mmHg in the standard arm) in all diabetes-related endpoints, deaths, stroke, and microvascular endpoints. Currently, the American Diabetes Association (ADA) recommends a blood pressure goal of < 130/80 mmHg. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) also recommends a blood pressure goal of < 130/80 mmHg for patients with diabetes. The International Diabetes Federation has recommended the use of home BP for the management of BP in diabetic patients. The J-HOME Study reported that home BP was greater than or equal to130/80 mm Hg in 7% of diabetic patients in whom clinic BP was controlled under 130/80 mm Hg. Home BP in the morning has been reported to more accurately reflect target organ damage than clinic BP in diabetic patients. Management of patients on the basis of telemedicine in co-operation with nurses, where home BP is used as an index, has been reported to have led to a more rapid control of BP in diabetic patients.
_
Renal diseases (chronic kidney disease, dialysis):
Renal diseases are often accompanied by hypertension, and hypertension is the greatest risk factor for the progression of nephropathy. In the general population, the risk of chronic kidney disease has been reported to be high in patients with masked hypertension, as determined by home BP measurements. In patients undergoing dialysis, the greatest prognostic factor is the presence of cerebro- and cardiovascular complications, and the management of hypertension is extremely important. However, BP measured at the dialysis center fluctuates widely, and has been reported to not accurately reflect the outcome. Home BP is known to more closely reflect the usual BP of dialysis patients. In addition, home BP measurements in dialysis patients have been shown to improve the state of BP control.
_
Some unresolved issues in special populations vis-à-vis SMBP:
__________
Clinical significance and application of home BP:
1. Home BP is highly reproducible.
2. Home BP has a greater prognostic value than clinic BP.
3. Home BP is extremely effective for the evaluation of drug effects and their duration.
4. Home BP can also be used for telemedicine.
5. The introduction of home BP to the diagnosis and treatment of hypertension facilitates long-term BP control.
6. Home BP measurements improve the adherence to medications and medical consultations.
7. Home BP can detect seasonal variations and long-term changes in BP.
8. Home BP is essential for the diagnosis of white-coat hypertension and masked hypertension.
9. Home BP measurements detect morning hypertension, and nighttime BP during sleep can also be obtained with certain devices.
10. Home BP is particularly important for the diagnosis and treatment of hypertension in diabetes mellitus, pregnancy, children and renal diseases.
11. Home BP has a great effect on the medical economy.
__________
Efficacy and utility of SMBP:
Although clinic blood pressure (BP) measurement still remains the cornerstone hypertension management, the broad availability of electronic BP measurement devices has led to their widespread adoption. Home BP monitoring is now uniformly advocated for the evaluation and management of hypertension. This is so because BP control among treated hypertensives remains poor, and it is believed that home BP monitoring can improve hypertension control. This improvement may be attributable to both better adherence with antihypertensive therapy and detection and treatment of masked hypertension. Further, in contrast to clinic BP measurement, which is associated with a white coat effect, home BP monitoring may reduce white coat effect and may obviate unnecessary therapy. In addition to improving hypertension control, home BP is superior to clinic BP in predicting cardiovascular prognosis and end-stage renal disease.
_
SMBP and target organ damage:
_
Several studies have indicated that the correlation between echocardiographically determined LVH and blood pressure is better for home than for clinic readings as shown in the table above. Home blood pressure has also been related to other measures of target organ damage. It has been reported to correlate more closely than clinic blood pressure with microalbuminuria and carotid artery interomedial thickness.
_
SMBP and prognosis:
_
_
The table below shows various studies that link high BP measured at home to morbidity and mortality:
_
Masked HT detected only by SMBP has high hazard ratio similar to sustained HT.
__________
Self-monitoring for the evaluation of antihypertensive treatment:
When patients are having their antihypertensive medication initiated or changed, it is necessary to measure their blood pressure on repeated occasions. Self-monitoring is ideal for this purpose, because it can obviate the need for many clinic visits. It has the additional advantage of avoiding the biases inherent in clinic pressure measurements. More frequent measures might increase compliance with antihypertensive medications. The validity of using home readings for monitoring the effects of treatment on blood pressure has been well established in a number of studies that have compared the response to treatment evaluated by clinic, home, and ambulatory pressures. Despite the general parallelism between clinic and home blood pressure during treatment, there may be considerable discrepancy between the two in individual patients. Thus, in a study of 393 patients treated with trandolapril, the correlation coefficient between the clinic and home pressure response, while highly significant, was only 0.36. The slope of the line was also rather shallow, indicating that a decrease of 20 mmHg in clinic pressure is on average associated with a decrease in home pressure of only 10 mmHg. Other studies have shown that drug treatment lowers clinic blood pressure more than home blood pressure; in a study of 760 hypertensives treated with diltiazem 300 mg the clinic blood pressure fell by 20/13 mmHg and the home blood pressure by 11/8 mmHg. In another study losartan lowered clinic blood pressure by 17/13 mmHg and home blood pressure by 7/5; trandolapril lowered clinic blood pressure by 17/13 and home blood pressure by 7/5; changes of AMBP were closer to the changes of home blood pressure. It is well recognized that drug treatment also lowers ambulatory blood pressure less than clinic blood pressure. One study has looked at the effects of exercise training on clinic and home blood pressure. Clinic blood pressure fell by 13/8 mmHg in the experimental group and 6/1 mmHg in the controls, whereas home blood pressures fell by 6/3 and 1/–1, respectively. Home monitoring is also ideal for evaluating the time course of the treatment response.
_
Self-Measurement of Blood Pressure at Home reduces the need for Antihypertensive Drugs: A Randomized, Controlled Trial:
It is still uncertain whether one can safely base treatment decisions on self-measurement of blood pressure. In the present study, authors investigated whether antihypertensive treatment based on self-measurement of blood pressure leads to the use of less medication without the loss of blood pressure control. they randomly assigned 430 hypertensive patients to receive treatment either on the basis of self-measured pressures (n=216) or office pressures (OPs; n=214). During 1-year follow-up, blood pressure was measured by office measurement (10 visits), ambulatory monitoring (start and end), and self-measurement (8 times, self-pressure group only). In addition, drug use, associated costs, and degree of target organ damage (echocardiography and microalbuminuria) were assessed. The self-pressure group used less medication than the OP group (1.47 versus 2.48 drug steps; P<0.001) with lower costs ($3222 versus $4420 per 100 patients per month; P<0.001) but without significant differences in systolic and diastolic OP values (1.6/1.0 mm Hg; P=0.25/0.20), in changes in left ventricular mass index (−6.5 g/m2 versus −5.6 g/m2; P=0.72), or in median urinary microalbumin concentration (−1.7 versus −1.5 mg per 24 hours; P=0.87). Nevertheless, 24-hour ambulatory blood pressure values at the end of the trial were higher in the self-pressure than in the OP group: 125.9 versus 123.8 mm Hg (P<0.05) for systolic and 77.2 versus 76.1 mm Hg (P<0.05) for diastolic blood pressure. These data show that self-measurement leads to less medication use than office blood pressure measurement without leading to significant differences in OP values or target organ damage. Ambulatory values, however, remain slightly elevated for the self-pressure group.
_
THOP trial 2004:
The appropriateness of home BP measurement to guide antihypertensive treatment has been tested in another large-scale randomized trial: the THOP (Treatment of Hypertension Based on Home or Office Blood Pressure) trial. The THOP trial showed that adjustment of antihypertensive treatment based on home BP instead of office BP led to less intensive drug treatment and marginally lower costs but also to less BP control, with no differences in general well-being or left ventricular mass . Home BP monitoring also contributed to the identification of patients with white-coat hypertension. Author’s findings support a strategy in which both home monitoring and 24-hour ambulatory monitoring can be “complementary” to conventional office BP measurement. The findings also “highlight the need for prospective studies to establish the normal range of home BP, including the operational thresholds at which drug treatment should be instituted or can be discontinued. Until such prospective data become available,” they conclude, “management of hypertension exclusively based on home BP cannot be recommended.” Well, we have come a long way from 2004 to 2014.
_
The figure below shows advantages of SMBP over OMBP for antihypertensive treatment trials:
___________
___________
Now I will go through various clinical trials on SMBP in chronological order:
_
Blood pressure control by home monitoring: meta-analysis of randomised trials: 2004
1359 people with essential hypertension allocated to home blood pressure monitoring and 1355 allocated to the “control” group seen in the healthcare system for 2-36 months participated in the study. The meta-analysis of 18 randomised controlled clinical trials found that “self” blood pressure monitoring at home results in better blood pressure control and greater achievement of blood pressure targets than “usual” blood pressure monitoring in the healthcare system. The size of the difference is rather small from the clinical viewpoint: 2.2/1.9 mm Hg (when allowing for publication bias), with 10% greater proportion on target. However, this may represent an adjunctive useful improvement in management of hypertension likely to contribute to a better outlook for cardiovascular events. The main inclusion criterion in the study was that participants had undertaken blood pressure monitoring at home either by themselves or with the aid of a family member. As this is the likely scenario for implementation in a population setting, the results of our meta-analysis could be applicable to the general population of people with mild to moderate essential hypertension.
Implications
What is already known on this topic:
Blood pressure is usually measured and monitored in the healthcare system by health professionals. With the introduction and validation of new electronic devices, self blood pressure monitoring at home is becoming increasingly popular. No evidence exists as to whether use of home monitoring is associated with better control of high blood pressure.
What this study adds:
Patients who monitor their blood pressure at home have a lower “clinic” blood pressure than those whose blood pressure is monitored in the healthcare system. A greater proportion of them also achieve blood pressure targets when assessed in the clinic.
Authors conclude that blood pressure monitoring by patients at home is associated with better blood pressure values and improved control of hypertension than usual blood pressure monitoring in the healthcare system. As home blood pressure monitoring is now feasible, acceptable to patients, and reliable for most of them, it could be considered as a useful, though adjunctive, practice to involve patients more closely in the management of their own blood pressure and help to manage their hypertension more effectively.
_______
Relationship between the Frequency of Blood Pressure Self-Measurement and Blood Pressure Reduction With Antihypertensive Therapy: 2006:
OLMETEL was conducted between February and October 2003 in 27 clinical practices in Germany. Patients adhering to the instructions for SMBP (at least two measurements daily) had a higher response to antihypertensive treatment with olmesartan medoxomil than those who were not adherent to these instructions. One explanation for the observed phenomenon is that patients who meticulously follow the instructions for SMBP may equally meticulously follow their physicians’ recommendation for antihypertensive drug intake, or vice versa. This means that once the physician is dealing with an a priori compliant patient, it may not necessarily make a difference whether the patient uses SMBP to achieve the intended effect concerning BP-lowering since the number of SMBP recordings are just an indicator of good compliance. Similarly, other authors have concluded that physicians should recommend home BP measurement to patients being treated with antihypertensive drugs because there is the possibility that home BP measurement might improve medication compliance. On the other hand there is strong support for the notion that self-measurement per se increases compliance with antihypertensive therapy. This has been demonstrated in the Self-Measurement for the Assessment of the Response to Trandolapril study that was performed in general practice and enrolled 1710 patients. Furthermore, not only did SMBP increase compliance compared with usual management, it also resulted in fewer clinic visits. The assumption that self-measurement increases compliance is also supported by other studies using home telemonitoring that showed that the mean arterial pressure reduction in the telemedical patient group was superior to that observed in the usual care group (in whom an increase in mean arterial pressure was observed). Whether SMBPs per se resulted in improved compliance with antihypertensive therapy or whether the number of recordings was an indicator of already existing compliance remains to be determined. Furthermore, a number of at least five BP home readings per week was identified as being able to correctly predict response to olmesartan medoxomil treatment. Non-adherence to drug intake is one of the most common causes of treatment-resistant hypertension. Patients’ non-adherence to therapy is increased by misunderstanding of the condition or treatment, denial of illness because of lack of symptoms or perception of drugs as symbols of ill health, lack of patient involvement in the care plan, or unexpected adverse effects of medications. Therefore, any means to improve patient compliance should be welcome. Using BP telemonitoring not only may improve compliance but has also been proven to be a very useful tool in the assessment and follow-up of BP in hypertensive patients.
__________
Changes in Home Versus Clinic Blood Pressure With Antihypertensive Treatments: A Meta-Analysis 2008:
The main findings of this meta-analyses are as follows: (1) the changes produced by antihypertensive drug treatments in home BP were 20% smaller than those of clinic BP, and the changes in clinic BP were linearly related to those of home BP; (2) the difference in the BP reduction between clinic and home BP were attributable to the difference in the baseline BP levels; (3) the changes in home SBP were intermediate between the changes of clinic and ambulatory SBPs (including 24-hour SBP, daytime SBP, and nighttime SBP); and (4) the differing effects on clinic and home BP were similar for calcium channel blockers, angiotensin converting enzyme inhibitors, and angiotensin II receptor blockers, and also for placebo or control groups. Final conclusion is that the reduction of home BP produced by antihypertensive drug treatment is about 80% of the magnitude of the reduction of clinic BP.
________
Does self-monitoring reduce blood pressure?
Meta-analysis with meta-regression of randomized controlled trials 2010:
Randomised controlled trials (RCTs) that compared self measurement of blood pressure without professional intervention against usual care (not including patient self-monitoring) were eligible for inclusion in the review. Eligible studies had to report self measurement blood pressure and independently measured blood pressure (either systolic or diastolic office pressure or ambulatory monitoring expressed as mean daytime ambulatory pressure). Where reported, included studies assessed automated (40%), manual (20%), digital/electronic (20%) and semi-automated (8%) measurement devices. Four studies made no adjustment for self-measured readings and six made adjustments (usually 5/5mmHg); the other studies did not report any information regarding adjustments. Control groups were mostly usual or routine care; three studies used drug treatment as a control. Most of the included studies reported a target office blood pressure of 140/85-95mmHg. Authors’ concluded that self-monitoring of blood pressure in adults reduced blood pressure by a small but significant amount. Evidence of significant heterogeneity could not be explained by meta-regression.
______
Home Blood Pressure Monitoring in the Diagnosis and Treatment of Hypertension: A Systematic Review: 2010:
Sixteen studies in untreated and treated subjects assessed the diagnostic ability of SMBP by taking AMBP as reference. Seven randomized studies compared SMBP vs. office measurements or AMBP for treatment adjustment, whereas many studies compared SMBP with office measurements in assessing the antihypertensive drug effects. Several studies with different design investigated the role of SMBP vs. office measurements in improving patients’ compliance with treatment and hypertension control rates. The evidence on the cost-effectiveness of SMBP is limited. The studies reviewed consistently showed moderate diagnostic agreement between SMBP and AMBP, and superiority of SMBP compared to office measurements in diagnosing uncontrolled hypertension, assessing antihypertensive drug effects and improving patients’ compliance and hypertension control. Preliminary evidence suggests that SMBP has the potential for cost savings. There is conclusive evidence that SMBP is useful for the initial diagnosis and the long-term follow-up of treated hypertension. These data are useful for the optimal application of SMBP, which is widely used in clinical practice. More studies on the co-steffectiveness of SMBP are needed.
______
Role of Home Blood Pressure Monitoring in Overcoming Therapeutic Inertia and Improving Hypertension Control:
A Systematic Review and Meta-Analysis 2011:
Authors conclude that a small but significant improvement for all BPs, systolic, diastolic, or mean, results when home BP monitoring is used. However, simply monitoring home BP is of little value if the patients or their physicians do not act on the results. When home BP monitoring is accompanied by specific programs to treat elevated BP, such as through titration of antihypertensive drugs, it can result in more meaningful change in BP. Compared with no program to titrate antihypertensive therapy, programs that incorporate a strategy of antihypertensive therapy, such as through telemonitoring, may provide even better hypertension control. Larger studies are warranted among hemodialysis patients, for whom this strategy may be particularly beneficial.
_______
Sensitivity and specificity in the diagnosis of hypertension with different methods: 2011:
OBJECTIVE: To evaluate sensitivity and specificity of different protocols for blood pressure measurement for the diagnosis of hypertension in adults.
METHODS: Cross-sectional study conducted in a non-probabilistic sample of 250 public servants of both sexes aged 35 to 74 years in Vitória, southeastern Brazil, between 2008 and 2010. The participants had their blood pressure measured using three different methods: clinic measurement, self-measured and 24-hour ambulatory measurement. They were all interviewed to obtain sociodemographic information and had their anthropometric data (weight, height, waist circumference) collected. Clinic measurement and self-measured were analyzed against the gold standard ambulatory measurement. Measures of diagnostic performance (sensitivity, specificity, accuracy and positive and negative predictive values) were calculated. The Bland & Altman method was used to evaluate agreement between ambulatory measurement (standard deviation for daytime measurements) and self-measured (standard deviation of four measurements). A 5% significance level was used for all analyses.
RESULTS: Self-measured blood pressure showed higher sensitivity (S=84%, 95%CI 75;93) and overall accuracy (0.817, p<0.001) in the diagnosis of hypertension than clinic measurement (S=79%, 95%CI 73;86, and overall accuracy=0.815, p<0.001). Despite the strong correlation with daytime ambulatory measurement values (r=0.843, p<0.001), self-measured values did not show good agreement with daytime systolic ambulatory values (bias=5.82, 95%CI 4.49;7.15). Seven (2.8%) cases of white coat hypertension, 26 (10.4%) of masked hypertension and 46 (18.4%) of white-coat effect were identified.
CONCLUSIONS: The study shows that self-measured blood pressure has higher sensitivity than clinic measurement to identify true hypertension. The negative predictive values found confirm the superiority of self-measured when compared to clinic in identifying truly normotensive individuals. However, clinic measurement cannot be replaced with self-measured, as it is still the most reliable method for the diagnosis of hypertension.
________
Cardiovascular outcomes in the trial of antihypertensive therapy guided by self-measured home blood pressure: 2012:
The multicenter Hypertension Objective Treatment Based on Measurement by Electrical Devices of Blood Pressure (HOMED-BP; 2001–2010) trial involved 3518 patients (50% women; mean age 59.6 years) with an untreated systolic/diastolic HBP of 135–179/85–119 mm Hg. In a 2 × 3 design, patients were randomized to usual control (125–134/80–84 mm Hg (UC)) vs. tight control (<125/<80 mm Hg (TC)) of SMBP and to initiation of drug treatment with angiotensin converting enzyme inhibitors, angiotensin receptor blockers or calcium channel blockers.
1. In the study, 3518 hypertensive subjects were followed for up to 10 years by 300 general practitioners. This study showed that SMBP was used without difficulty and was readily accepted by practitioners and patients
2. The assessment of nocturnal BP is of major clinical relevance because of its demonstrated prognostic value. The Ohasama study investigators developed an SMBP device that can monitor nocturnal BP during sleep. Such devices are now used in epidemiological surveys, large-scale intervention trials and clinical pharmacology studies in Japan.
3. Although there was no difference among the groups in a 2 × 3 study design, the risk of the primary endpoint independently increased by 41% and 47% for a 1 s.d. increase in baseline and follow-up systolic HBP, respectively, in all patients combined. The 5-year risk was <1% if the on-treatment systolic HBP was 131.6 mm Hg. The HOMED-BP study proved the feasibility of adjusting antihypertensive drug treatment based on HBP and suggested that a systolic HBP level of 130 mm Hg should be an achievable and safe target.
4. More recently, the HOMED-BP proved that adjusting antihypertensive drug treatment on the basis of blood pressure values collected through HBPT is feasible and effective for maintaining an optimal target blood pressure level and optimal antihypertensive medication
_______
How hypertensive patients in the rural areas use home blood pressure monitoring and its relationship with medication adherence: A primary care survey in China: 2013:
Despite an increasing popularity of home blood pressure monitoring (HBPM) over the last few decades, little is known about HBPM use among hypertensive patients in the rural areas. A cross-sectional survey including 318 hypertensive patients was conducted in a rural community in Beijing, China, in 2012. Participants were mainly recruited from a community health clinic and completed the questionnaires assessing HBPM usage. Binary logistic regression models were used for the analysis of medication adherence with age, gender, level of education marital status, perceived health status, duration of hypertension, HBPM use, and frequency of performing BP measurement. Among the total population, 78 (24.5%) reported currently use of HBPM. Only 5.1% of the HBPM users cited doctor’s advice as the reason for using HBPM. Analysis of the risk factors of poor medication adherence by multivariable modeling indicated significant associations between the duration of hypertension (adjusted OR, 3.31; 95% CI, 1.91-5.72; P < 0.001), frequency of performing BP measurements (adjusted OR, 2.33; 95% CI, 1.42-3.83; P < 0.001) and medication adherence. Authors found that most use of HBPM was without the involvement of a doctor or nurse. Further study is required to understand if HBPM is effective and the role of health professionals in its use for improved hypertension control.
_______
Self-Measured Blood Pressure Monitoring: Comparative Effectiveness:
Systemic review of 52 comparative studies in 2013:
The primary objective of this review is to evaluate whether the use of SMBP monitoring influences outcomes in adults and children with hypertension, and to what extent these changes in outcomes can be attributable to the use of self-monitoring devices alone or the use of SMBP plus additional support or attention. The intention of this report is to inform physicians’ decision making as to whether to encourage the use of SMBP monitoring alone or along with additional support, and to assist health care policymakers and payers with decisions regarding coverage and promotion of SMBP monitoring. This review identified 52 comparative studies that examined the impact of SMBP with or without additional support in the management of hypertension. Overall, the benefit of SMBP for BP reduction appears to be modest and is not consistent across studies. Authors examined the role of additional support in combination with SMBP by setting up comparisons as: (1) SMBP alone versus usual care; (2) SMBP plus additional support versus usual care; and (3) SMBP plus additional support versus SMBP with no additional support or less intense additional support. Twenty-four trials compared SMBP alone versus usual care. Meta-analysis showed a statistically significant reduction in clinic SBP and DBP (SBP/DBP 3.1/ 2.0 mmHg) at 6 months but not at 12 months. Only one RCT reported follow up beyond 12 months; findings indicated significant reductions in SBP and DBP at 24 months in favor of SMBP. The comparison of SMBP plus additional support versus usual care was examined in 24 studies, with 11 of 21 randomized trials and 2 of 3 nonrandomized studies reporting a statistically significant benefit in BP reduction favoring SMBP plus additional support. Four studies provided results after 12 months. Twelve trials compared SMBP plus additional support (or more intense additional support) versus SMBP without additional support (or plus less intense additional support). Only four of these trials reported a significantly greater reduction in BP in the SMBP plus additional (or more intense) support groups. Two studies provided results beyond 12 months. Both reported findings that were non-significant or of uncertain statistical significance. Tracking blood pressure at home helped patients with hypertension keep it under control, at least over the short term, a meta-analysis determined. Pooled study results pointed to 3.9/2.4 mm Hg lower blood pressure on average with self-monitoring at 6 months compared with usual care based on in-clinic monitoring alone. That impact would be clinically relevant on a population level if they were sustained over time. For example, a decrease of 2 or 5 mm Hg in systolic blood pressure in the population has been estimated to result in mortality reductions of 6% or 14% due to stroke, 4% or 9% due to chronic heart disease, and 3% or 7% due to all causes. While the impact of home monitoring alone fizzled to a non-significant 1.5/0.8 mm Hg reduction by 12 months, additional support, like education or counseling, kept the effect going. SMBP with or without additional support may confer a small benefit in BP control compared with usual care, but the BP effect beyond 12 months and the attendant long-term clinical consequences remain unclear. Given clinical heterogeneity and limited head to head comparisons, the evidence limits authors’ ability to draw definitive conclusions about the incremental effect of any specific additional support. Future research should standardize patient inclusion criteria, BP treatment targets for home BP, and SMBP and additional support protocols to maximize the interpretability and applicability of SMBP trials. For the current report, authors reviewed 52 published studies in which patients monitored their blood pressure with and without assistance. Such help ranged from educational materials to contact with a nurse or pharmacist or counseling over the telephone. They found some evidence that monitoring blood pressure at home improved control at six months, but not at 12 months. When patients got help, either through educational material or direct contact with medical professionals, home monitoring improved blood pressure control at both six and 12 months. From this data, authors concluded that home blood pressure monitoring is effective in the short term.
________
Self-Monitoring Blood Pressure lowers Cardiovascular Risk in Hypertension: Self-Monitoring of BP reduces Hypertension and Stroke Risk: 2014:
After participating in a self-management program, hypertensive patients at high risk for cardiovascular disease had lower systolic blood pressure compared to those who received standard care, according to the results of the Phase III TASMIN-SR trial published August 27, 2014, in JAMA. Researchers from the University of Oxford in the United Kingdom studied 552 patients aged at least 35 years with hypertension and a history of stroke, coronary heart disease, diabetes, or chronic kidney disease. The patients had baseline blood pressures of at least 130/80 mm Hg and were treated at 59 primary care practices across the United Kingdom between March 2011 and January 2013. Those in the intervention group were instructed to monitor their own blood pressures using an individualized self-titration algorithm, while those assigned to the control group received usual care, which included seeing their clinician for routine blood pressure measurements and receiving medication adjustments as necessary. Although the previous Phase II TASMINH2 trial deemed this method effective, the research team “wanted to develop the intervention and trial it in higher risk patients,” lead study author Richard J. McManus, PhD, FRCGP said. At baseline, the blood pressure of the intervention group was 143.1/80.5 mm Hg, which was similar to the 143.6/79.5 mm Hg baseline blood pressure of the control group. Although average systolic blood pressure decreased in both groups after 12 months, a more significant decline was found in the intervention group, as the researchers recorded a mean blood pressure of 128.2/73.8 mm Hg in the intervention group, compared to a mean blood pressure of 137.8/76.3 mm Hg in the control group. Based on readings received, the interventional group adjusted their own medication levels. Mean blood pressure at the beginning of the trial for self-monitoring patients was 143.1/80.5 mm Hg; after 12 months, that figure dropped to 128.2/73.8. For patients in the control group, mean blood-pressure prior to the start of the project was 143.6/79.5; afterward, it fell to 137.8/76.3. The study authors noted the results were comparable in all subgroups and no excessive adverse events were observed. “We thought that older patients with more comorbidities might not do as well as younger patients, but, in fact, we got better results: 9.2 mm Hg difference versus 5.4 mm Hg difference in systolic blood pressure in TASMIN-SR versus the TASMINH2 trial,” Dr. McManus said when asked about the study’s surprising findings. As a result, the researchers concluded self-monitoring is a viable option for the long-term treatment of hypertension in patients with high cardiovascular disease risk. “A group of high-risk individuals…are able to self-monitor and self-titrate antihypertensive treatment following a pre-specified algorithm developed with their family physician and that, in doing so, they achieved a clinically significant reduction in systolic and diastolic blood pressure without an increase in adverse events,” the study authors wrote. “This is a population with the most to gain in terms of reducing future cardiovascular events from the optimized blood pressure control.” Thus, Dr. McManus urged health care professionals to “consider self-management as an effective approach for lowering blood pressure safely” in patients with “above-target blood pressure and cardiovascular comorbidity.” Patients at risk for hypertension and stroke that self-monitor and make adjustments to medication from home could reduce their risk of stroke by 30% and significantly lower their blood pressure after 12 months, according to a recent study.
__________
Blood pressure self-monitoring could save tens of thousands of unnecessary deaths every year: A study:
Experts say that despite the availability of effective drugs, controlling high blood pressure in health centers and GP practices is poor because of infrequent monitoring and reluctance by doctors to increase medication (therapeutic inertia). Often patients do not take their drugs properly.
1. Portable system allows people to send their readings to medical staff
2. Doctors check figures and can contact the patient to discuss their health
3. Trial found significant drop in blood pressure among people using system
4. Each year there are 62,000 unnecessary deaths in the UK due to poor blood pressure control
SMBP overcomes therapeutic inertia and improves patient compliance, control BP and saves life.
__________
__________
Negative reports about SMBP:
Blood Pressure Monitoring Kiosks aren’t for Everyone: FDA warning:
Convenience can come with tradeoffs. The next time you put your arm in the cuff at a kiosk that measures blood pressure, you could get an inaccurate reading unless the cuff is your size. Correct cuff size is a critical factor in measuring blood pressure. Using a too-small cuff will result in an artificially high blood pressure reading; a too-large cuff may not work at all or result in an inaccurately low blood pressure reading. The Food and Drug Administration (FDA) is advising consumers that blood pressure cuffs on public kiosks don’t fit everyone and might not be accurate for every user. These desk-like kiosks for checking blood pressure are available in many public places—pharmacies, grocery and retail stores, gyms, airports, hair salons and even cafeterias. They are easily accessible and easy to use. But it’s misleading to think that the devices are appropriate for everybody. They are not one-size-fits-all. Other factors, including how someone uses a device, might cause an inaccurate reading. The user might not have placed the cuff on his arm properly or might not be sitting properly. These things will affect accuracy. That’s why people shouldn’t overreact to any one reading from a kiosk. Hypertension isn’t diagnosed solely based on one reading. Inaccurate blood pressure measurements can lead to the misdiagnosis of hypertension or hypotension (low blood pressure), and people who need medical care might not seek it because they are misled by those inaccurate readings.
_
Blood Pressure Self-Measurement in the Obstetric Waiting Room:
Authors observed 81 pregnant diabetics’ ability to correctly self-measure in the waiting room during a 4-week observational descriptive study. Specifically, they investigated the level of patient adherence to six recommendations with which patients are instructed to comply in order to obtain a reliable blood pressure reading. They found that the patients did not adhere to given instructions when performing blood pressure self-measurement in the waiting room. None of the 81 patients adhered to all six investigated recommendations, while around a quarter adhered to five out of six of the recommendations. The majority followed four or fewer of the recommendations. Results indicate that unsupervised self-measurement of blood pressure is not a reliable method. Thus, there is a need for increased staff presence and patient training or, alternatively, for introducing improved technology support. This could include context-aware patient adherence aids and clinical decision support systems for automatically validating self-measured data based on e-health and telemedicine technology.
__________
Blood pressure measurements in epidemiological/observational studies:
Very comprehensive research on population blood pressure exists throughout the world. These studies are essential for defining hypertension prevalence, awareness and treatment in any geographical region/country. A change in population blood pressure of 2 mmHg in systolic blood pressure translates to a change in stroke mortality of ten percent and coronary heart disease mortality of seven percent (Lewington et al. 2002). Therefore, data on progression from normotension to prehypertension and hypertension are very important in epidemiological research. The data have documented that prehypertension carries an increased risk for cardiovascular morbidity and mortality, and a high risk for progression to sustained hypertension (Hansen et al. 2007a, Julius et al. 2006). In this respect, changes from normotension to prehypertension are as important as the observation of hypertension itself. Reliable data are heavily dependent on blood pressure measurements carried out meticulously by properly trained personnel and with precise equipment. For this, adherence to a standardised technique over time is crucial. Findings of changes in population blood pressure are only meaningful if they are ascertained to be true differences and not related to a change in methods applied. Nearly all results on population blood pressure have been obtained by the use of a standard mercury sphygmomanometer by well-trained health personnel (Cutler et al. 2008). Despite this, the readings are not without observer bias and end-digit preference. In an attempt to minimise observer bias and end-digit preference, a number of highly recognized epidemiological research institutions have used the Random Zero Mercury Sphygmomanometer, where the reader has to subtract a random chosen magnitude of mmHg (from 0 to 20 mmHg) at the very end of the measurement. Despite minimising observer bias, the equipment has been shown to slightly underestimate the “true” blood pressure level as obtained by the use of a standard mercury manometer (Yang et al. 2008). Another approach that has been employed is the “London School of Hygiene Sphygmomanometer” (Andersen and Jensen 2007) where the reader is blinded to the mercury column but has to tap a button when they hear the first and the last Korotkov sounds (phase 1 and phase 5). In recent years, 24-hour ambulatory blood pressure measurements have been introduced in population studies and comprehensive databases have been constructed, e.g. the Idaco Database on population studies with contributions from many parts of the world (Hansen et al. 2007b). All these studies have convincingly shown that 24-hour ambulatory blood pressure measurements determined with oscillometric devices (at approximately 80 readings over 24 hours), are superior for prediction of cardiovascular morbidity and mortality as compared to a few measurements of blood pressure performed in clinical conditions with a standard mercury sphygmomanometer. In almost all these studies, although not exclusively, the comparator has been the standard mercury sphygmomanometer (Hansen et al. 2007b). Research into normal values for home blood pressure and the prognostic implication is less comprehensive. This research has been almost exclusively carried out with automatic oscillometric devices, with measurements being compared to the mercury sphygmomanometer. Data are accumulating showing that the predictive prognostic value of a certain number of home blood pressure readings is superior to a single or a few blood pressure readings performed in a clinic using a mercury sphygmomanometer (Sega et al. 2005). The home readings are a reflection of more precise estimation of the actual blood pressure levels over many readings as compared to few readings in the clinical setting. So far, comparisons of measurements obtained with mercury sphygmomanometer versus oscillometric automatic devices, obtained in the same clinical setting for determination of population blood pressure and prognostic implications, are missing. However, in the Pamela Study, three clinic readings with a mercury sphygmomanometer were compared to two home blood pressure oscillometric readings (Sega et al. 2005). As expected, the clinical readings were somewhat higher, but the prognostic implication was not that much different. In long-term outcome clinical trials, usually running for three to five years, mercury sphygmomanometers have been used as the gold standard for office blood pressure measurement. In some recent trials (the HOT Study, the ASCOT Study and the OnTarget Study) automatic oscillometric devices were used (Dahlöf et al. 2005, Hansson et al. 1998, Yusuf et al. 2008). In some of these studies it was shown that small differences in measured blood pressure already can have an impact on cardiovascular diseases. There is rapidly growing information on normal values and the prognostic implications of 24 hour ambulatory blood pressure measurements with oscillometric devices, while knowledge on self/home blood pressure measurements with oscillometric devices is less substantial. So far, a direct comparison between clinic blood pressure and prognostic implication based on measurements carried out with mercury sphygmomanometer and those with automatic oscillometric devices is lacking. In conclusion, the vast majority of information on population blood pressure (secular trends, progression to hypertension and prognostic implications, and also the benefits from treatment-induced blood pressure reduction in terms of cardiovascular events prevention) has so far been obtained with the use of mercury sphygmomanometers. Reliable data on changes in population blood pressure level, incidence and prevalence of hypertension, awareness and treatment, derived from follow-up studies are dependent on the use of consistent and trustworthy methods. It can be expected that epidemiological/observational studies in the future will comprise repetitive blood pressure measurements at home carried out with well-calibrated, well-validated automatic oscillometric equipment. For the moment, mercury sphygmomanometers are essential for such validation of newly developed blood pressure measurement devices. Otherwise, the conclusions based on the results of long–term epidemiological studies on changes in population blood pressure may be seriously jeopardized.
___________
SMBP and telemonitoring:
BP measurement and monitoring are critical for BP management. Traditionally, BP measurement has been performed by physicians or nurses in office-based care settings. Office BP measurements are subject to error related to the patient’s reaction to the measurement procedure, a phenomenon known as the ‘‘white coat effect.’’ Measurement of BP at home is not impacted by this effect and can therefore provide more stable and reproducible BP measures, which can be of greater prognostic value. In addition, home BP measurements have been shown to reflect true BP more reliably than office readings and to correlate better with end-organ damage. Moreover, home BP measurement has the added value of providing clinically relevant information between office visits and, therefore, can be a more consistent source of information to help manage BP and associated risks. Therefore, hypertension management guidelines recommend home or ‘‘self’’ BP monitoring (SMBP) in the management of hypertension. SMBP can be manually measured and recorded by the patient or electronically transmitted to a healthcare provider. The technological advances in BP telemonitoring have been brought about by the availability of valid and easy-to-use BP devices that use automated oscillometric tools. Further, the technology allows automatic transmission of BP data to primary care providers. Several studies have demonstrated the feasibility, accuracy, patient compliance, and satisfaction with BP telemonitoring in managing hypertension.
_
Systemic review of 15 studies on BP telemonitoring:
Authors searched five databases (PubMed, CINAHL, PsycINFO, EMBASE, and ProQuest) from 1995 to September 2009 to collect evidence on the impact of blood pressure (BP) telemonitoring on BP control and other outcomes in telemonitoring studies targeting patients with hypertension as a primary diagnosis. Fifteen articles met their review criteria. Authors found that BP telemonitoring resulted in reduction of BP in all but two studies; systolic BP declined by 3.9 to 13.0mm Hg and diastolic BP declined by 2.0 to 8.0mm Hg across these studies. These magnitudes of effect are comparable to those observed in efficacy trials of some antihypertensive drugs. Although BP control was the primary outcome of these studies, some included secondary outcomes such as healthcare utilization cost. Evidence of the benefits of BP telemonitoring on these secondary outcomes is less robust. Compliance with BP telemonitoring among patients was favorable, but compliance among participating healthcare providers was not well documented. This systemic review of 15 studies concluded that home BP telemonitoring is feasible in the management of hypertension.
_
Effects of BP self measurement and telemedicine communication on physician prescribing habits: 2012:
This was a secondary analysis of a telemedicine trial of 241 patients with uncontrolled hypertension (BP >150/90 mmHg). Patient from two large medical centers were recruited and randomized to usual care (control group-C, N=121) or Telemedicine with usual care (T, N=120). The T group was provided a digital sphygmomanometer and training, along with CVD risk reduction counseling. They were instructed to report their BP, HR, weight, steps/day, and tobacco use twice weekly for 6 months. All patients had baseline and 6-month follow-up visits. Monthly reports on blood pressure and treatment guidelines were provided to both the patient and physician in the T group. At the end of the study, patients’ anti-hypertensive medications were compared to their baseline therapy. Patients in the telemedicine group were more likely to be prescribed more anti-hypertensive medications during the study. This may indicate that patient involvement in self-reporting via telemedicine changes the information available to the physician in such a way that leads to more appropriate and effective pharmacotherapy, better blood pressure control, and overall reduction in cardiovascular risk.
_
Two Model Hypertension Care:
_
Telemonitoring of home BP is the most effective way to lower Blood Pressure: 2013:
Patients with uncontrolled blood pressure can significantly improve their health using a new self-monitoring system called telemonitoring that can be used at home, according to a new study in the British Medical Journal (BMJ). The research showed that patients with this condition, which is usually difficult to treat with drugs alone, can greatly benefit from this portable system which enables them to record and send their own blood pressure readings straight to doctors in real-time. These figures are then checked online by doctors and nurses who contact patients if they need to discuss their health and treatment with them. Over the previous 15 years, systems similar to this have been tested on a small scale, however, this study is the first to observe incorporating use in frontline primary care, the experts, from the University of Edinburg, explained. Patients who used telemonitoring required more medical time and attention, compared to those who did not use it, the results also showed. The patients who used telemonitoring experienced a bigger reduction in their blood pressure than those who did not use it. “The drop in blood pressure was helped mainly by encouraging doctors to prescribe and patients to accept more prescriptions of anti-high blood pressure drugs,” the authors pointed out. On the other hand, telemonitoring use had little effect on people’s lifestyle changes, including weight control and salt consumption. Although effective drugs are available, controlling high blood pressure in health centers and GP practices – monitoring is insufficient, and clinicians are unwilling to increase treatment. Patients who do not take their medication as they should can also experience complications because their blood pressure will remain high. Professor Brian McKinstry, of the University of Edinburgh’s Centre for Population Health Sciences, concluded: “We found that the use of supported telemonitoring in patients who manage their high blood pressure at home produces important reductions in blood pressure. We believe that telemonitoring has the potential to be implemented in many healthcare settings. Before this happens however, we would recommend testing it out on a much larger scale so that we can see that the reduction in blood pressure over six months can be achieved in the longer term and that it is cost effective.”
_________
In a nutshell, what do all studies on SMBP find?
_
Home BP and prognosis:
The prognostic significance of home BP has been reported to be comparable to, or slightly better than, that of AMBP. The high prognostic significance of home BP is considered to be derived from the stability of BP information. Evidence has also shown that home BP reflects target organ damage with similar or higher reliability than AMBP. AMBP provides data on short-term BP variability every 15–30 min, and these values are reported to have prognostic significance. The day-to-day variability of BP detected by home BP measurements has also been reported to predict the risk of cerebrovascular and cardiovascular diseases. Heart rate measured simultaneously with home BP also has a prognostic significance.
_
Home BP and clinical pharmacology of antihypertensive drugs:
As home BP provides a stable mean value and ensures high reproducibility, it is extremely effective for the evaluation of drug effects and their duration. Home BP eliminates the placebo effect and records the responses to antihypertensive drugs more accurately than AMBP, and, as such, is considered optimal for evaluating the effects of antihypertensive drugs. Consequently, home BP reduces the number of subjects necessary for the evaluation of drug effects compared with AMBP, and markedly reduces the number necessary when compared with clinic BP. Evaluation of the duration of drug effects has been considered possible by the use of the trough/peak (T/P) ratio based on AMBP. However, as the reproducibility of AMBP is not always adequate, the reproducibility of the T/P ratio is also unsatisfactory. It has recently been reported that the morning/evening (M/E) or evening/morning (E/M) ratio obtained from home BP measurements is very effective in evaluating the duration of drug effects.
_
Home BP and telemedicine:
With the advance of devices for home BP measurements, BP values have begun to be stored as electronic data. As a result, such data have been transmitted via telephone lines or the internet, and are widely used for decision making and clinical pharmacological evaluations. Improvements in BP control by means of such telemedicine have been reported.
_
Home BP and BP control:
The Japanese and International guidelines recognize home BP measurements as an optimal tool for long-term BP control. The introduction of home BP measurements in the diagnosis and treatment of hypertension facilitates the attainment of a goal BP compared with BP management based on clinic BP alone. By implementing antihypertensive therapy according to home BP, the goal BP can be achieved sooner. BP control has been reported to be improved by combining home BP measurements with behavioral therapy. Home BP measurements also reduce the frequency of clinic consultations and elevate the participation rate to medical treatment. As home BP is measured and interpreted by the patients themselves, the possibility of self-regulation of antihypertensive medication according to home BP has become relevant in hypertension management.
_
Home BP and adherence:
Home BP measurements require an active commitment by the patients themselves in medical care and health management, and results in a marked improvement in the adherence to medication. High adherence to home BP measurements has also been reported to improve BP control. Patients with high adherence to home BP measurements have also shown high adherence to exercise or dietary intervention.
_
Home BP and seasonal changes in BP:
Unlike AMBP, home BP is effective in evaluating long-term changes in BP. For example, home BP can detect seasonal variations in BP. The monitoring of seasonal changes in home BP facilitates the titration of antihypertensive drugs.
_
Home BP and physiological & pathophysiological conditions:
Home BP can detect slight changes in BP mediated by modifications in lifestyle or by exposure to stress, as well as small changes in BP in response to antihypertensive drugs. For example, home BP can detect the depressor effect caused by the intake of fruits and vegetables in a population or by physical training, the hypertensive response to passive smoking in a population, the relationship with the longevity of parents and low BP in children, the relationship of combinations of hypertension candidate genes with the incidence of hypertension and so on. In a crossover study of calcium supplementation assessed by office, home and ambulatory BPs, the small reduction in BP was significant only for home BP. Serial measurements of home BP also detected time-related biphasic changes in morning and evening BPs with alcohol consumption and restriction in hypertensive patients. Therefore, home BP measurements provide an excellent index for the evaluation of BP changes in individuals and for the comparison of BP among individuals and groups. In particular, the reliability and precision of BP as a phenotype are determinants of the results of gene-related studies, and home BP is considered to be extremely useful in such studies.
_
Home BP detects morning hypertension, a risk factor for cardiovascular events:
Patients on antihypertensive medication who have high blood pressure (SBP >145 mmHg) in the morning, as measured with home monitoring kits, are at increased risk of cardiovascular events, even if their clinic measurement is acceptable, researchers have found.
_________
Ambulatory measurement of blood pressure (AMBP):
_
Ambulatory BP measurement:
_
Ambulatory measurement of blood pressure monitoring (AMBP) involves measuring blood pressure (BP) at regular intervals (usually every 20–30 minutes) over a 24-hour period while you carry on with normal daily activities. AMBP has the additional advantage of measuring your BP during sleep and it is now known that night time BP may give much valuable information. Your AMBP is measured with a small monitor, worn in a pouch on a belt, and the monitor is connected to a cuff on your upper arm. This cuff inflates and deflates regularly measuring the systolic (upper) and the diastolic (lower) blood pressure as well as your average blood pressure and heart rate. AMBP is safe and free of complications, apart from occasional discomfort when the cuff is inflating. Occasionally there may be slight bruising of the arm. Modern machines are light, quiet and easy to wear but can sometimes disturb sleep.
_
Upper limit of normal ambulatory blood pressure monitoring values:
Normal ambulatory blood pressure during the day is <135/85 mm Hg and <120/70 mm Hg at night. Levels above 135/85 mm Hg during the day and 125/75 mm Hg at night should be considered as abnormal.
_
Dippers and non-dippers:
1. Blood pressure will fall at night in normotensive individuals. People who undergo this normal physiological change are described as ‘dippers’.
2. In ‘non-dippers’ the blood pressure remains high, i.e. less than 10% lower than daytime average. There is also the phenomenon of ‘reverse dippers’ whose blood pressure actually rises at night. Both these conditions have also been reported to be associated with a poor outcome.
_
The diagnosis and management of hypertension has traditionally been based on blood pressure measurements taken in the office. However, the inherent variability of blood pressure and its susceptibility to transient emotional influences in normotensive and hypertensive people undermine the ability of conventional clinical measurement to accurately reflect the usual level of blood pressure in some people. In contrast to other means of blood pressure assessment, including self-assessment, ambulatory monitoring provides information automatically and noninvasively about the effects of blood pressure load over time and under the various circumstances during which blood pressure is not usually measured (including work and sleep). Whereas self-assessments at home usually provide periodic measurements over many days and weeks, ambulatory monitoring provides numerous measurements over a period of hours, up to a day. Thus, the sampling of a person s blood pressure provided by the two means is quite different. Although the accuracy of ambulatory monitoring is less than optimum, technical errors are relatively small compared with errors in the estimate of true pressure based on a small number of clinic readings and can be minimized if a standard protocol is followed, including calibration with a mercury sphygmomanometer immediately before and after the readings are taken. It is important to note that even with excellent calibration there is substantial variability in the results of ambulatory monitoring when repeated after an interval of 2 to 8 weeks. Thus, monitoring may need to be done repeatedly to provide an average measure of a person s usual ambulatory blood pressure. The devices currently available vary in their reliability and accuracy. Reference values for ambulatory monitoring in normotensive subjects are available from recent studies: daytime pressures range from 101/62 to 143/90 mm Hg, and a daytime average of 135/84 mm Hg corresponds to a clinic-based cut-off of 140/90 mm Hg. In view of the generally lower pressures obtained with ambulatory monitoring than at the clinic, patients with an average blood pressure of more than 135/84 mm Hg on ambulatory monitoring and without target-organ damage should be followed closely for the development of higher pressures or target-organ damage. To date, ambulatory blood pressure monitoring has been primarily a research tool and has not had an established clinical role in the diagnosis and management of hypertension. Nevertheless, some clinical problems are better elucidated by this technique than by casual blood pressure readings, and ambulatory monitoring is being used increasingly in clinical decision making. Its most important clinical application is the detection of white-coat hypertension. Estimates of the prevalence of this syndrome vary from 20% to 39%. Other clinical situations in which ambulatory monitoring might be of diagnostic value include borderline hypertension with target-organ involvement, episodic hypertension and resistant hypertension. Many studies have shown a closer correlation of target-organ involvement (particularly left ventricular hypertrophy) with pressures obtained through ambulatory monitoring than with those obtained at the clinic, and there is also evidence that left ventricular hypertrophy occurs much less frequently in patients with white-coat hypertension than in those with confirmed essential hypertension. Other studies have shown that pressures obtained from ambulatory monitoring at work and the percentage of daily blood pressure loads correlate more strongly with left ventricular hypertrophy than do pressures measured at the clinic. The results of ambulatory blood pressure monitoring also appear to be a more potent predictor of cardiovascular disease and death in patients with hypertension than are casual blood pressure readings. However, the evidence concerning the value of ambulatory blood pressure monitoring is not complete in some respects, and some procedural issues make its use less than straightforward. The main clinical trials of the benefits of lowering blood pressure have used measurements taken at the office or clinic to establish the diagnosis of hypertension and to gauge the effects of treatment. Ambulatory monitoring as a substitute has not been tested in studies large enough to determine whether it provides a better measure of diagnosis or of risk reduction. There are other factors to be considered: ambulatory monitoring devices are expensive (in terms of both equipment and personnel costs) in comparison with the usual sphygmomanometers, they are error-prone and need careful calibration, they are inconvenient for patients, few centers can provide them, there is enough variability in the measurements they provide for the same patient from time to time that more than one monitoring session may be needed, and the service is not approved for reimbursement by government health insurance plans in some countries. Thus, it is premature to recommend the widespread application of ambulatory monitoring for the diagnosis of patients with mild hypertension.
_
Ambulatory blood pressure monitoring has been found to be clinically useful only in the following settings: to identify non-dippers and white-coat hypertension, evaluate drug resistant hypertension, episodic hypertension, evaluate antihypertensive drugs and in individuals with hypotensive episodes while on antihypertensive medication. However, this procedure should not be used indiscriminately in the routine work-up of a hypertensive patient because of its high cost.
___
AMBP and cardiovascular outcomes:
Several studies have demonstrated the prognostic benefit of AMBP, with evidence that 24-hour daytime or nighttime average BP values correlate with subclinical organ damage more closely than office values. The Ohasama study – the first study to address the prognostic value of AMBP – reported a greater association between ambulatory BP and CV mortality than office BP. Clement et al showed that for the same clinical systolic BP, CV prognosis was worsened (incidence of CV events multiplied by two to three) when 24-hour systolic BP was >135 mmHg. In the SYST-EUR (Systolic Hypertension in Europe) study, ambulatory but not clinical BP was shown to predict CV mortality during follow-up; higher 24-hour BP was associated with total, cardiac, and cerebrovascular events in untreated hypertensives.
_
AMBP for evaluating pharmacological treatment of hypertension:
To reduce CV risk of patients with hypertension, antihypertensive agents should provide effective, sustained, and smooth BP reduction throughout the 24-hour dosing period. AMBP has drastically improved the ability to assess the efficacy of antihypertensive drugs in both clinical trials and medical practice. Greater reproducibility, lack of placebo effect, and absence of an alerting-dependent BP response make AMBP the ideal tool to quantify the antihypertensive effect of new drugs in clinical trials, as well as drug combinations or nonpharmacological measures. It also makes it possible to compare the ability of different drugs or doses to provide smooth and consistent reductions in BP using indices such as trough-to-peak ratio and smoothness index.
_
Relative effectiveness of clinic and home blood pressure monitoring compared with ambulatory blood pressure monitoring in diagnosis of hypertension: systematic review:
The 20 eligible studies used various thresholds for the diagnosis of hypertension, and only seven studies (clinic) and three studies (home) could be directly compared with ambulatory monitoring. Compared with ambulatory monitoring thresholds of 135/85 mm Hg, clinic measurements over 140/90 mm Hg had mean sensitivity and specificity of 74.6% (95% confidence interval 60.7% to 84.8%) and 74.6% (47.9% to 90.4%), respectively, whereas home measurements over 135/85 mm Hg had mean sensitivity and specificity of 85.7% (78.0% to 91.0%) and 62.4% (48.0% to 75.0%). Neither clinic nor home measurement had sufficient sensitivity or specificity to be recommended as a single diagnostic test. If ambulatory monitoring is taken as the reference standard, then treatment decisions based on clinic or home blood pressure alone might result in substantial overdiagnosis. Ambulatory monitoring before the start of lifelong drug treatment might lead to more appropriate targeting of treatment, particularly around the diagnostic threshold. This review has shown that neither clinic nor home measurements of blood pressure are sufficiently specific or sensitive in the diagnosis of hypertension. Authors included 20 studies with 5683 patients that compared different methods of diagnosing hypertension in diverse populations with a range of thresholds applied. In the nine studies that used similar diagnostic thresholds and were included in the meta-analysis (two comparing home with ambulatory measurement only, six comparing clinic with ambulatory measurement only, and one study comparing all three methods), neither clinic nor home measurement could be unequivocally recommended as a single diagnostic test. Clinic measurement, the current reference in most clinical work and guidelines, performed poorly in comparison with ambulatory measurement, and, given that clinic measurements are also least predictive in terms of cardiovascular outcome, this is not reassuring for daily practice. Home monitoring provided better sensitivity and might be suitable for ruling out hypertension given its relative ease of use and availability compared with ambulatory monitoring. In the case of clinic measurement, the removal of studies with a mean blood pressure in the normotensive range reduced specificity still further. This has profound implications for the management of hypertension, suggesting that ambulatory monitoring might lead to more appropriate targeting of treatment rather than starting patients on lifelong antihypertensive treatment on the basis of clinic measurements alone, as currently recommended. In clinical practice, this will be particularly important near the threshold for diagnosis, where most errors in categorisation will occur if ambulatory monitoring is not used.
What is already known on this topic:
Hypertension is traditionally diagnosed after measurement of blood pressure in a clinic, but ambulatory and home measurements correlate better with outcome.
What this study adds:
Compared with ambulatory monitoring, neither clinic nor home measurements have sufficient sensitivity or specificity to be recommended as a single diagnostic test. If the prevalence of hypertension in a screened population was 30%, there would only be a 56% chance that a positive diagnosis with clinic measurement would be correct compared with using ambulatory measurement. More widespread use of ambulatory blood pressure for the diagnosis of hypertension would result in more appropriately targeted treatment.
_
Cost saving ambulatory BP monitoring (ABPM):
In 2011, British doctors began using ABPM as a confirmatory test on nearly every patient suspected of having hypertension. The change occurred after Britain’s National Institute for Health and Clinical Excellence concluded that ABPM was the most accurate and cost-effective option for clinching the diagnosis. An analysis published in the medical journal, the Lancet, projected that new approach will save Britain’s National Health Service $15 million over the first five years since it was adopted, mainly by avoiding treatment for those with white coat hypertension.
_____
Downside to ambulatory blood pressure monitoring:
1. It is not universally available although this is improving.
2. It requires specialist training.
3. Some patients find inflation of the cuff unbearable.
4. Sleep disturbance.
5. Bruising where the cuff is located.
6. Background noise may lead to interference (less with oscillometric methods).
7. Poor technique and arrhythmias may cause poor readings.
8. There is some evidence that SMBP may be better than AMBP for predicting cardiovascular risk at every level below severe hypertension (≥160/≥100 mm Hg). However, these findings need to be confirmed by larger trials.
___________
Advantages and limitations of SMBP vis-à-vis OMBP and AMBP:
_
Blood pressure measured by any technique outside of the physician’s office tends to have lower values. In six studies comparing SMBP and OMBP, a consistently lower blood pressure by SMBP (SBP 5.4 ± 17.7 mm Hg and DBP 1.5 ± 6.3 mm Hg) was demonstrated. Three studies comparing AMBP and SMBP show similar daytime blood pressure results. While AMBP is the gold standard for the determination of WCH, SMBP is comparable to AMBP for prevalence of WCH. A systematic review including six comparisons of SMBP and AMBP found that blood pressures over the criterion of 135/85 mmHg were obtained more frequently\ overall with SMBPs. However, in the three studies with the largest numbers of SMBPs (29 to 56), the average AMBPs were higher than the SMBPs, to a lesser or greater degree.
_
__
The advantages of using SMBP monitoring to manage hypertension are:
1. Avoiding under-treatment of hypertension — SMBP monitoring can provide more frequent BP measurements. If transmitted to the health care provider, this can permit more rapid adjustments in antihypertensive medication and more effective BP control.
2. Enhancing patient self-participation in disease management and adherence to lifestyle and pharmacological interventions — long-term adherence to lifestyle modification strategies and antihypertensive medication is a key challenge in hypertension management. SMBP monitoring may help address this challenge by enhancing patient participation in disease management.
3. Avoiding overtreatment in patients with lower BP outside the clinic than in it — SMBP may be useful in identifying individuals with white coat hypertension, orthostatic BP changes, or hypotensive episodes from medication and thereby prevent overtreatment in these individuals.
4. Another advantage of the self-measurement devices to control the blood pressure when symptoms appear. Self-measurement of the blood pressure device makes it possible to control the blood pressure when symptoms appear like faintness, a loss of consciousness (symptoms of hypotension), headaches, a nosebleed or neurological symptoms (confusion, agitation….). A high or low blood pressure measured on the device can thus induce a consultation in the physician office or in the emergency service in the hospital.
__
_
SMBP reliability:
The reliability of the patient recording of the blood pressure measurement is critical if this technique is to be trusted. Patients consistently misreport the results of the monitor when patient manual recordings are compared to a device that stored readings unbeknownst to the patient. Patient reports had mean differences in blood pressure of at least 10 mm Hg for SBP and 5 mm Hg for DBP compared to stored readings. In another study, 36% of patients underreported and 9% overreported blood pressure readings. Log books also had phantom readings noted; conversely, patients failed to report measurements that were taken and stored. Similar findings were observed with other monitoring technologies such as glucometers for diabetic patients and for recording metered dose inhaler usage in asthmatic patients. Thus, objective recording of the data is strongly advised. SMBP is a useful adjunct to OMBP measurement with properly validated monitors, can be performed by many patients, and is consistent with the goal of self-management.
_
Limitations of SMBP monitors:
Position: The cuff and the monitor should be at the same level of the heart; otherwise the reading has to be adjusted due to the difference in height. This is especially true for wrist cuff blood pressure monitors.
Patient Movement: Measurements will be unreliable or cannot be performed if the patient is moving, shivering or having convulsions. These motions may interfere with the detection of the arterial pressure pulses. In addition, the measurement time will be prolonged.
Cardiac Arrhythmia: Measurements will be unreliable and may not be possible due to irregular heartbeats caused by cardiac arrhythmia.
Rapid pressure change: If the arterial pulse pressure changes rapidly during measurement, the blood pressure monitor would not be able to obtain a good reading.
Severe Shock: When the patient is in severe shock or having hypothermia, blood flow would be reduced resulting in weak pulses. The weak signal may lead to inaccurate readings.
Heart rate: If the heart beats too fast (>240bpm) or too slow (<40bpm), measurement would be difficult.
_
Limitations of SMBP:
_______
Similarities between SMBP and AMBP:
_
_
The most important common denominator of SMBP and AMBP is the fact that they both provide out-of-office BP values, i.e., BP values obtained in the patient’s “natural” environment. Thus, these values are basically devoid of the alarm reaction associated with office BP measurement, responsible for the white coat effect. Another important common advantage of AMBP and SMBP is that, when current recommendations are followed, they both make use of automated, validated oscillometric devices. This makes the obtained BP values operator independent, thus avoiding some common limitations affecting office measurements. Importantly, the application of these techniques is possible in a vast majority of cases, the two most relevant exceptions including important arrhythmias, e.g., frequent extrasystoles or atrial fibrillation, where oscillometric measurements are unreliable, and obesity with extremely large arm circumference and/or conical shaped arms, where fitting an appropriate cuff may be difficult. In the latter case the use of wrist devices for SMBP might possibly be justified, whereas otherwise upper arm devices should always be preferred. The above advantages, together with the ability of SMBP and AMBP to provide a much larger number of values than office BP measurements, result in more stable estimates of the prevailing BP in a given subject, reflecting the actual BP burden on cardiac and vascular targets more precisely than office readings. This has not only methodological but also clinical relevance, as documented by a number of studies showing the prognostic superiority of SMBP or AMBP over isolated office BP measurement. These observations are further reinforced by the demonstration that a worse prognosis characterizes subjects with normal office and elevated out-of-office BP, assessed by either SMBP or AMBP (masked hypertension), than subjects with normal out-of-office but elevated office BP (white coat or isolated office hypertension).
_
Differences between AMBP and SMBP:
Notwithstanding the above similarities, there are major differences between SMBP and AMBP that importantly influence their possible clinical and research applications. One of the key issues is the economic aspect of using either SMBP or AMBP. Although the price of validated AMBP devices has fallen considerably over the last years, making them more easily and widely available, still, the costs of the system and its maintenance remain relatively high, unquestionably higher than those of SMBP. This is of particular relevance when promoting BP monitoring in low-resource settings, where the prevalence of hypertension is increasing and the limited availability of economic resources does not allow costly equipment to be considered in a population setting. Thus, should SMBP and AMBP provide equivalent clinical information, the former technique would have to be preferred on the background of the possibility to reduce patients’ management costs. Admittedly, however, AMBP has a number of clinically relevant features that are not directly available with SMBP, which makes the former approach not easily replaceable by the latter. One of the peculiar advantages of AMBP lies in its ability to provide a series of frequent and automated BP measurements throughout the 24 hours, which makes AMBP, at variance from SMBP, capable to dynamically assess BP changes over relatively short periods of time. This might have clinical implications in light of the evidence supporting the adverse prognostic relevance of specific patterns of BP variability over 24 hours, including reduced nocturnal BP fall, increased short-term BP variability, and possibly also an excessive morning BP surge. Nevertheless, the actual clinical usefulness of assessing these dynamic BP features remains controversial because of the lack of universally accepted normal reference values for their interpretation, lack of well-defined interventions able to counteract their adverse effects, and missing evidence that their modification by treatment may significantly reduce cardiovascular risk.
_
Final position of SMBP vis-à-vis AMBP:
The current position is that SMBP and AMBP should coexist and be used as complementary tools, providing different information on a subject’s BP status. However, SMBP may be a valid alternative to AMBP in many cases, possibly even in settings where AMBP is currently considered the method of choice, e.g., identification of isolated office hypertension and of masked hypertension, clinical evaluation of BP variability, and assessment of antihypertensive drug coverage. In fact, in clinical practice, SMBP is increasingly replacing AMBP, with use of the former being recommended in all treated hypertensive subjects by recent guidelines, a recommendation that cannot apply to AMBP. This is because SMBP is an ideal first-line tool because of its low cost, high availability, and easy application. It may also be the most reasonable option for the initial assessment of untreated subjects, in whom white coat or masked hypertension is suspected, i.e., those with highly variable office BP, with office BP close to diagnostic thresholds, with isolated out-of-office BP values discrepant from office BP, with evidence of organ damage contrasting with office BP findings, etc. Moreover, SMBP is clearly the tool of choice in monitoring BP control in treated subjects over extended periods of time, also because it has the particular advantage of promoting a better therapeutic adherence.
_
Recent studies showed that home blood pressure monitoring is as accurate as a 24-hour ambulatory monitoring in determining blood pressure levels. Researchers at the University of Turku, Finland studied 98 patients with untreated hypertension. They compared patients using a home blood pressure device and those wearing a 24-hour ambulatory monitor. Researcher Dr. Niiranen said that “home blood pressure measurement can be used effectively for guiding anti-hypertensive treatment”. Dr. Stergiou added that home tracking of blood pressure “is more convenient and also less costly than ambulatory monitoring.”
__
Schema of SMBP and AMBP:
A schema showing how both self/home and ambulatory BP measurements may be used in clinical practice is shown in the figure below. Self-BP monitoring may be used as an initial step to evaluate the out-of-office BP, and if AMBP is available it is most helpful in cases where the self/home BP is borderline (between 125/75 mm Hg and 135/85 mmHg). The target BP for self/home BP is usually 135/85 mm Hg for those whose target office BP is 140/90 mm Hg and 125/75 to 130/80 mm Hg for those whose target office BP is 130/80 mm Hg. Equivalent values for ambulatory BP in low risk hypertensive patients are 130/80 mm Hg for 24-hour BP, 135/85 mm Hg for the awake BP, and 125/75 mm Hg for the sleep BP.
_
The figure above shows that practical use of self/home BP monitoring and AMBP in clinical practice.
_______
Patient assessment strategy for HT vis-à-vis OMBP, SMBP and AMBP:
Patients frequently note that their SMBP is lower than the office-measured blood pressure (OMBP). A number of investigators have studied this difference and confirmed the observation. Combining a number of studies, SMBP is typically lower than OMBP by 8.1 mm Hg systolic and 5.6 mm Hg diastolic. In addition, the upper limit of normal for SMBP is 130 to 135 mm Hg systolic and 80 to 85 mm Hg diastolic. Readings above these limits should be considered abnormal. Finding the proper role for SMBP in standard clinical practice has been a challenge. Numerous organizations have clinical guidelines for the diagnosis and treatment of hypertension, but typically only have brief mention of SMBP. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) recommends OMBP for diagnosis and treatment of hypertension, and designates SMBP as an adjunct for the monitoring of therapy. The American Heart Association recommends OMBP with a mercury sphygmomanometer. They recognized SMBP as an emerging force but also relegate it to a supplementary role. Currently most authorities view SMBP as a supplement to OMBP. SMBP will likely gain wider clinical acceptance as more research outcomes become available. Treatment can be started without confirmation of elevated office BP in patients with high office BP and target organ damage, or a high cardiovascular risk profile. In patients with raised office BP but without target organ damage (white-coat hypertension), or with normal office BP but unexplained target organ damage (masked hypertension), ambulatory or home BP monitoring or both must be used to confirm the diagnosis. Few longitudinal studies have addressed the long-term prognostic meaning of home BP measurement. Until more prospective data become available, management of hypertension exclusively based on self-measurement of BP at home cannot be recommended.
_
_______
Cost-effectiveness of home monitoring: A study:
There is some evidence that self-monitoring may be cost-effective. In a randomized study conducted by the Kaiser Permanente Medical Care Program in San Francisco, 430 patients with mild hypertension, most of whom were taking antihypertensive medications, were randomized either to a usual care group or to use self-monitoring. Their technique was checked by clinic staff, and they were asked to measure their blood pressure twice weekly and to send in a record of their readings every month. At the end of 1 yr the costs of care (which included physician visits, telephone calls, and laboratory tests) were 29% lower and blood pressure control slightly better in the self-monitoring group. The vast majority of both patients and their physicians considered that the self-monitoring procedure was worthwhile. The authors estimated that the annual cost of self-monitoring was $28 per year (in 1992 dollars), which assumed a depreciation of a $50 monitor over 5 yr, $10 for training (also depreciated), $1 for blood pressure reporting, and $6 for follow-up to enhance compliance. Combining this estimate with their study results led to an estimated cost saving per patient of $20 per year. Projecting these numbers on a national level, they estimated that about 15 million hypertensive patients in the United States are candidates for self-monitoring and that 20 of the 69 million annual hypertension related physician visits could be saved, with a cost saving of $300 million per year. These numbers seem very optimistic, but they clearly establish the potential for cost saving.
_
Effects of home BP on the medical economy:
The introduction of SMBP into the diagnosis and treatment of hypertension has been shown to have a strong effect on the medical economy. In fact, in Japan, where home BP-measuring devices are already used by most hypertensive patients, the introduction of home BP into the care of hypertension has resulted in a decrease in annual medical expenditure of about 1 trillion yen. This decrease has been mediated primarily by screening for white-coat hypertension and masked hypertension. As a result of large-scale intervention studies, the introduction of home BP has also been reported to lead to a reduction in medical expenditure via a decrease in the amount of drugs used.
______
Innovation and research in BP measuring technology:
_
Techniques for Self-Measurement of Blood Pressure (SMBP): Limitations and Needs for Future Research:
SMBP improves the overall management of hypertension provided it is implemented with methodologic care. This concerns especially the accuracy and technical requirements of blood pressure measuring devices that should be validated according to internationally accepted protocols. The use of memory-equipped automatic home monitors is strongly recommended because they reduce observer bias, avoid patients’ misreporting, and allow fully automatic analysis by software. For current use, simple software should be worked out that allow for analysis of readings in an objective manner. Miscuffing is also a frequent source of measurement error in obese arms when oscillometric devices are used. Modern automatic devices can overcome this problem because of special software algorithms that can provide accurate measurements over a wide range of arm circumferences when coupled with a single cuff of standard dimensions. Tronco-conical–shaped cuffs are a key component of this instrumentation because they better fit on large conical arms frequently present in obese individuals. Semi-rigid cuffs should be increasingly used because they ensure that the proper amount of tension is applied without the intervention of the user. Continuous technology improvement of instrumentation for SBPM can be achieved through close cooperation between manufacturers and validation centers.
_
Wireless Blood Pressure Monitor:
_
Easy and precise self-measurement of your blood pressure with your smartphone:
_
Simply slip on the cuff, turn on the Wireless Blood Pressure Monitor and the Health Mate app will automatically launch. Following a brief set of instructions, you will be ready to take your blood pressure. Because it makes more sense to track your blood pressure over time, the Health Mate app stores all your BP readings, syncs with the Withings Health Cloud and creates an easy to understand chart. The app gives you an instant color feedback based on the World Health Organization’s official standards for a quick and simple blood pressure tracking experience. The Wireless Blood Pressure Monitor’s results have scientific value: it is compliant with European medical device regulations and has received clearance from the Food and Drug Administration (FDA) in the USA. It is also medically approved in Canada, Australia and New Zealand. The Wireless Blood Pressure Monitor works with all iOS 5.0 or higher devices, and with Android 4.0 or higher stmartphones and tablets using Bluetooth connectivity or your smartphone’s cable. Now you can check your blood pressure using your iPhone or iPad with two products that make it easy to download an app onto your iOS device, put on a blood pressure cuff, tap the touchscreen, and soon you have a blood pressure reading that you can track every day. They’re quick and reasonably priced.
_
Considerations for Future Development of Cuff and Bladders:
There is a need for devices that make use of cuffs and bladders with appropriate characteristics. Manufacturers should pay special attention to the size and shape of the bladders and to the material used for cuffs. Semi-rigid cuffs should be increasingly used for self-BP measurement because they ensure that the proper amount of tension is applied for placement of the cuff. Elderly persons in particular often have problems in wrapping the cuff correctly around the arm. With cuffs made of soft material, it is more difficult for the user to apply the optimal amount of tension, and this may result in improper wrapping. Placing a flexible compliant laminate in the cuff, with an amount of tension pre-set by the manufacturer, may provide accurate BP measurements without the intervention of the user. Devices for clinical use may have soft cuffs because the BP measurement is performed under the supervision of health care personnel. Soft cuffs also have better durability, are less bulky, and are lower in cost. However, the use of conically shaped bladders in small cuffs may be preferable if they have to be applied on large arms. The appropriate slant angle for conical cuffs should be calculated from the arm characteristics in large samples, with arm circumferences ranging from 22 cm to 50 cm. Cylindrical and conical bladders of different size and shape should be constructed and compared in the various arm size classes, studying the influence of sex, age, adiposity, and BP level. Cuffs of soft and rigid material containing the same type of bladders should be compared either under the supervision of the clinician or by the patient at home. This would allow physicians to ascertain whether semi-rigid cuffs are more reliable than soft cuffs in real-life situations.
______
Atrial Fibrillation: The WatchBP device:
Atrial fibrillation (AF) is the most common cardiac arrhythmia. It affects over one percent of the general UK population and is related to one fifth of all strokes (European Heart Rhythm et al. 2010).
The WatchBP device:
The WatchBP Home is an automated blood pressure monitor with an implemented AF detection system. When a GP or Patient measures blood pressure using the WatchBP, the device automatically screens for AF without any extra effort. As a simple explanation, the algorithm of the device calculates the irregularity index (SD divided by mean) based on interval times between heartbeats and if the irregularity index is above a certain threshold value a patient is diagnosed as having AF. If a patient performs self-measurements at home and the WatchBP Home detects AF, it gives a warning that a visit to the GP is required. The systems’ accuracy has been investigated in several scientific studies and showed high diagnostic accuracy (Stergiou et al. 2009; Wiesel et al. 2009). Although, the WatchBP device has never been directly compared to pulse palpation for AF screening, results from different clinical studies consistently show a higher diagnostic accuracy for the WatchBP (Stergiou et al. 2009; Wiesel et al. 2009) device than for pulse palpation as compared to the gold standard: a 12-lead ECG assessed by a consultant (Hobbs et al., 2005, Morgan and Mant, 2002, Somerville et al., 2000, Sudlow et al., 1998). Based on the results of the SAFE study the AF detector of the WatchBP monitor shows an even higher rate of accuracy for the detection of AF than a GP or nurse using a 12-lead ECG system (Hobbs et al. 2005) as compared to a 12-lead ECG assessment by a consultant.
_
Context Classification during Blood Pressure: Sensor Chair:
Self-Measurement using the Sensor Seat and the Audio Classification Device:
Blood pressure self-measurement requires the patient to follow a range of recommendations. Patients must remain silent during measurements, be seated correctly with back support and legs uncrossed, and must have rested at least 5 minutes prior to taking the measurement. Current blood pressure devices cannot verify whether the patient has followed these recommendations or not. As a result, the data quality of BP measurements could be biased. Researchers present a proof-of-concept demonstration prototype that uses audio context classification for detecting speech during the measurement process, as well as a sensor seat for measuring patient posture and activity before and during the SMBP process.
_
A Wristwatch that monitors Blood Pressure without cuff:
Now a new wireless monitor from Hewlett-Packard and a Singapore company called Healthstats aims to make it much easier for patients and doctors to monitor blood pressure. The device, which has the size and look of a wristwatch, can monitor pressure continuously—which provides a much more accurate picture than infrequent readings in the doctor’s office. Until now, the only way to do such continuous monitoring has been with a cumbersome inflatable cuff for the arm or wrist. The new monitor comes with related software designed to keep patients and doctors informed of the wearer’s vital signs, including blood pressure. Data is transmitted from the device to the user’s cell phone, and then to the cloud, where clinicians can review it. Patients and their doctors can view 24-hour graphs of blood pressure, and the system can sound alerts when it detects abnormalities in pressure or other measures. Unlike standard equipment, the Healthstats device relies on a sensor that rests against radial artery in the wrist and detects the shape of the pressure wave as blood flows through it. (The device is first calibrated with a standard blood pressure monitor.) Together with algorithms they have developed, the indices can be processed to get heart rate, diastolic and systolic pressure, and other measures.
_
Healthstats CEO Dr.Ting Choon Meng with his BPro blood pressure monitor wristwatches.
_
A revolutionary method to estimate aortic blood pressure:
With regard to the variation between central aortic and brachial pressures, it is assumed that the mean arterial and diastolic pressure remains largely unchanged from aortic root to brachial artery, and that it is variation in amplification of the pulsatile pressure component, namely, systolic pressure, that accounts for the central-to-brachial pressure differences. Thus, focus has been on the accurate derivation of central aortic systolic pressure (CASP). For more than a hundred years, blood pressure has been measured in largely the same way. You’ve probably experienced it yourself: your doctor will inflate a cuff around your upper arm, temporarily interrupting the flood of blood in your brachial artery. From this, they will take a reading of the pressure when your heart beats (systolic pressure) and when it is between beats (diastolic pressure) – which is why blood pressure (BP) is given as ‘this number over that number’. But this is not ideal because blood pressure is amplified as it travels away from the heart. It has been known for a long time that the pressure in the large vessels close to the heart (e.g. the aorta) is lower than the corresponding pressure on the arm. This may seem surprising but it is due to amplification of the pressure wave as it moves away from the heart to the arm. A way was needed to eliminate the amplification that increases the pressure in the arm so that we could get back to the original central aortic pressure. To do this mathematical modeling is used, similar to the kind of modeling that is undertaken to remove distortion of waves in many other applications. The process acts like a filter, filtering out the amplified portion of the pulse wave to reveal the central aortic pressure. Being able to measure blood pressure near the heart, specifically in the aorta – called ‘central aortic systolic pressure’ or CASP – is important because this is where high blood pressure can cause damage. But obviously your aorta is much harder to reach than your upper arm, what with that whole rib cage and so on. It can be done – but only using a surgical procedure. Clearly what is needed is some way to measure CASP indirectly using blood vessels we can actually get at. Now, if the relationship between brachial BP and CASP was constant, there would be no problem – you could just use a multiplication factor. But the ratio between the two measurements varies not only between individuals but also within each person as they get older and their artery walls become stiffer. The new approach, developed by scientists at the University of Leicester, uses technology invented by Singapore-based medical device company HealthSTATS International: a device worn on the wrist which can accurately record a patient’s pulse. Not just the pulse rate but the actual pulse wave. In short, your pulse wave provides enough data to be able to determine your aortic blood pressure from a measurement of your brachial blood pressure – without having to cut you up or poke anything into you. The sensor records a pulse wave at the wrist at the same time that blood pressure is measured in the arm. The data is then used to mathematically compute the CASP. The process takes only a few minutes more than conventional measurements. The non-invasive procedure uses a device which not only looks like a wristwatch and is worn like a wristwatch but, in some versions, actually is a wristwatch. A carefully positioned pad presses on the radial artery on the inside of your wrist; it’s a bit tight but not uncomfortable. Wearing this device for 24 hours provides an average which flattens out pulse-raising factors such as excitement or exercise. Working with colleagues from HealthSTATS, the Leicester researchers have built up an extensive collection of patient data from which they have derived an effective algorithm for calculating CASP. Direct comparison with traditional CASP measurements obtained using the old-fashioned, invasive method shows a 99% correlation. The results of all this research have now been published in the prestigious Journal of the American College of Cardiology. It is worth stressing that the new system is not designed to replace the old inflatable cuff that we all know and love; you need the cuff and the wristwatch to calculate CASP (although you don’t need to wear the cuff for 24 hours). What it will do is let doctors measure CASP much more easily; you could potentially have your aortic blood pressure measured by your GP. The importance of all this is that brachial BP can be unreliable, especially in young people whose more flexible blood vessel walls can give misleadingly high blood pressure, leading to unnecessary medical interventions. Conversely, old people with stiffer blood vessels may give a misleadingly low reading of brachial BP, disguising dangerous high blood pressure which can be a precursor to heart attack or stroke. It may be some time before this technology reaches the majority of patients but the scientists hope that you see it soon because you’ll be helping them determine whether CASP really can become the standard measurement for blood pressure. And that could save lives. The device looks like a normal blood pressure monitor, with one important difference. There is an additional strap attached to the monitor that is placed around the wrist. This contains the sensor that captures the pulse wave. Once the blood pressure cuff and wrist strap are in place – a button is pressed which blows up the cuff like a normal blood pressure measurement, but also captures the pulse wave at the wrist. The device contains the program that we developed that uses the blood pressure and the pulse wave form to derive central aortic pressure. The pulse sensor has also been incorporated into the strap of a wrist watch that allows ambulatory measurements of blood pressure to be recorded day and night.
_
In this approach, radial artery waveform is obtained by noninvasive tonometry. In this method, the radial waveform is usually calibrated to brachial blood pressure, measured using standard sphygmomanometry, thereby generating a calibrated radial artery pressure waveform (RAPWF). Mathematical generalized transfer functions (GTFs) in the frequency or time domain have then been used to derive central aortic pressures and related aortic hemodynamic indices from the RAPWF. This method has, however, been criticized because of concerns that it may not be appropriate to apply a GTF generated in 1 cohort of patients to all patients with different disease states, at different ages, and receiving different treatments, and so forth. Nevertheless, applying a GTF to the RAPWF remains the most commonly used method for the noninvasive assessment of central aortic pressure indices. More recently, an alternative approach to estimating CASP from the RAPWF has been proposed. This requires the accurate identification of an inflection point on the RAPWF that is said to correspond to the superimposition of the peak of the reflected wave onto the outgoing pressure wave. Numerous recent studies have suggested that this inflection point, so-called SBP2, corresponds to the peak CASP and is a reasonably accurate way of noninvasively assessing CASP, without the need to apply a GTF. In another method, a simple approach for the accurate estimation of CASP in humans utilizes an n-point moving average (NPMA).
_______
Frequently Asked Questions (FAQ) about SMBP:
1. Will I get the same reading each time I use my Blood Pressure Monitor?
No. Blood pressure is not a static value but changes with each heartbeat, even in rest condition. Both the upper blood pressure value (systolic B.P.) and the lower blood pressure value (diastolic B.P.) vary by 5 to 10 mmHg with each heartbeat in healthy individuals. These variations may be considerably greater in the event of certain cardiovascular disorders. Insufficient rest condition is the most frequent reason for improper use in self-administered blood pressure measurement. A resting time of at least 5 minutes should therefore be chosen before commencing blood pressure measurement. Deliberate movements, muscle activities, coughing, sneezing and psychological demands such as speaking, listening and watching (e.g. TV ) may lead to false readings when measuring blood pressure. Measurements should therefore be carried out under conditions of complete rest and without any distraction. Cardiac rhythm disorders can cause inaccurate readings or may result in measurement failure. These cardiac rhythm disorders may occur without the self-user being aware of them.
_
2. Why are my home readings different from my doctor’s readings?
Many factors affect blood pressure including the anxiousness of a doctor’s visit. When the blood pressure is measured in a hospital, it may be 25 to 30 mmHg higher than when measured at home. This is because you are tense at the hospital and relaxed at home. It is important to know your stable normal blood pressure at home. If your doctor is using automated oscillometric device on you and takes multiple readings, your clinic BP would be close to your home BP.
_
3. Are manual inflate monitors (semi-automated) as accurate as automatic inflate monitors?
Yes. Both models comply with the same accuracy standards. The only difference is the way the cuff is inflated.
_
4. How often and when should I measure my blood pressure?
It is recommended that you consult with your health care professional for the time and frequency that is best suited for you. It is important to take your readings at similar times and conditions on a day-to-day basis. This will allow for reliable comparisons of your readings. Initially take BP twice a day, morning and evening with two recording at each time.
_
5. What happens if I do not place the cuff at heart level?
If the cuff is not at heart level, readings will be affected producing either higher or lower measurements.
_
6. Which arm should I use to take my blood pressure?
It is suggested to consult with your health care professional to determine which arm is best for you to use. For home monitoring, non-dominant arm is used to measure blood pressure. Ideally, both arms must be used for first BP measurements. The arm with higher BP is then used for daily BP recording. The same arm should be used for all future readings to ensure reliable comparisons.
_
7. Can I use my blood pressure monitor while exercising and also in moving vehicles?
The oscillometric method of blood pressure monitoring requires quiet, stable conditions. Movement, vibrations or other activity will interfere with the reading and likely cause an error or inaccurate reading.
_
8. When the cuff deflates, you get an error message. What does this mean?
An error message (EE) can appear for various reasons:
• Incorrect cuff placement
• Movement or talking during measurement
• Over or under inflation of cuff
• Not waiting long enough between subsequent measurements
_
9. Why is the pressure close to the heart, i.e. in the central aortic pressure, different from the pressure that is measured in the arm using a conventional blood pressure device?
It has been known for a long time that the pressure in the large vessels close to the heart (e.g. the aorta) is lower than the corresponding pressure on the arm. This may seem surprising but it is due to amplification of the pressure wave as it moves away from the heart to the arm. If this amplification was fixed, then measuring pressure in the arm would always be a good measure of pressure in the aorta – but it is not fixed. The amplification of the pressure wave as it moves from the heart to the arm can vary with ageing, disease of the blood vessels and with medication. This means that the pressure we measure routinely in the arm is not always a good predictor of the pressure in the large arteries which we call central aortic pressure. This is important because the central aortic pressure is the true pressure that the heart, the brain and other major organs actually sees and as such, is likely to be a better indicator of the pressure that can cause damage if it is too high. Another interesting aspect of this pressure amplification is that it is paradoxically greater in younger people with healthy arteries. This means that some people with a high blood pressure when measured in their arm may actually have a completely normal central aortic pressure. This amplification effect is greatest for systolic pressure and can result in a difference between central systolic aortic pressure and systolic pressure in the arm as great as 30mmHg. So the only way to really know what the central aortic pressure is, is to actually measure it in some way.
________
________
The moral of the story:
_
1. When we use the tem blood pressure (BP) we mean arterial blood pressure, which is lateral pressure exerted by column of flowing blood over wall of arteries (aorta and major arteries).
_
2. Hypertension (HT) is not synonymous with high blood pressure even though both terms are used interchangeably. Hypertension is persistent and irreversible elevation of blood pressure over a longer period of time above a level where only treatment reduces blood pressure and where treatment does more good than harm. Transient and reversible elevation of blood pressure is not hypertension.
_
3. About 40 % of world’s adult population has hypertension. Out of all hypertensives, half do not know that they have hypertension, 40% are treated, but only 13% are controlled.
_
4. Among all risk factors for death worldwide due to non-communicable diseases, hypertension is number one risk factor for death and it carries greater risk than smoking, diabetes and obesity.
_
5. Hypertension is one of the most readily preventable causes of heart disease and stroke. High blood pressure can be easily detected and we have very effective ways of treating high blood pressure and we have clear evidence of the benefits of such interventions. A decrease of 5 mmHg in systolic BP is estimated to result in a 14 percent reduction in mortality due to stroke, a 9 percent reduction in mortality due to heart disease, and a 7 percent reduction in all-cause mortality.
_
6. Each person has roughly 100,000 single blood pressure values per day as every heart beat generates pressure pulse wave. Also, blood pressure varies widely due to multiple factors. That is why higher the number of blood pressure measurements, greater the accuracy of blood pressure value. Physicians committees have proved that at least 15 measurements are necessary to determine true blood pressure.
_
7. Assuming that doctor is measuring blood pressure using correct technique and validated device in clinic (office BP), yet frequently patient gets incorrect BP readings because they typically only consist of 1 or 2 individual measurements; the inherent variability of blood pressure; and the tendency for blood pressure to increase in the presence of a physician (the so-called white coat effect).
_
8. A survey showed that 96% of primary care physicians habitually use a cuff size too small resulting in getting higher BP than actual BP. Other poor techniques shown by doctors are terminal digit preference, threshold avoidance, observer prejudice, rapid cuff deflation and absence of approximation of systolic BP by palpatory method. So a “real world” cut off point by manual clinic BP measurement (office BP) for hypertension is closer to 150/95 mm Hg instead of 140/90 mm Hg.
_
9. Studies on the so called gold standard for clinical measurement of blood pressure by mercury sphygmomanometer found that about 20 to 50 % of mercury sphygmomanometers have technical flaws affecting accuracy of BP measurement. A check of the devices in a major teaching hospital showed that only 5% of the investigated instruments had been properly serviced.
_
10. Instrument evaluation studies demonstrated technical defects or unacceptable measurement inaccuracy in up to 60% of the aneroid devices that had been evaluated.
_
11. The Korotkoff sound method tends to give values for systolic pressure that are lower than the true intra-arterial pressure, and diastolic values that are higher. The range of discrepancies is quite striking: one author commented that the difference between the two methods might be as much as 25 mm Hg in some individuals.
_
12. In my experience, air leakage from rubber tubing and bladder in cuff is the most common malfunction of any sphygmomanometer resulting in incorrect BP readings.
_
13. Appropriate size bladder in cuff and position of cuff at mid-right atrium level are the two most important technical points while measuring BP by auscultatory or oscillometric technique. In the sitting position, the mid-right atrium level is the midpoint of the sternum or the fourth intercostal space. In the supine position, the mid-right atrium is approximately halfway between the bed and the level of the sternum; so when measurements are taken in the supine position the arm should be supported with a pillow.
_
14. The sleeve should not be rolled up such that it has a tourniquet effect above the blood pressure cuff. On the other hand, applying the cuff over clothes is similar to the undercuffing error and will lead to overestimation of blood pressure.
_
15. Talking (increase of 17/13 mm Hg) or crossing of legs (increase of 7/2 mm Hg) during measurement and arm position (increase or decrease of 8 mm Hg for every 10 cm below or above mid-right atrium level) can significantly alter BP measurements. A full urinary bladder causes an increase in blood pressure of approximate10mm Hg.
_
16. Even when performed properly in research studies, office measurement of blood pressure (OMBP) is a relatively poor predictor of cardiovascular risk related to BP status compared with methods of out-of-office BP measurement such as 24-hour ambulatory measurement of blood pressure (AMBP) or self measurement of blood pressure (SMBP) at home.
_
17. Automated oscillometric blood pressure measurement eliminates observer errors associated with the use of the manual auscultatory technique such as terminal digit preference, threshold avoidance, observer prejudice, rapid deflation etc.
_
18. In the United States and Europe, up to two thirds of people with hypertension do self-monitor.
_
19. SMBP has qualitative improvement and quantitative increase in information compared with clinic BP and such improvised data has greater significance. Self-measured blood pressure has higher sensitivity and higher accuracy than clinic measurement to identify true hypertension. Home blood pressure is better correlated with target organ damage and adverse prognosis than clinic BP. On the other hand, the reliability of the patient doing SMBP is poor. About half of patients consistently misreport monitor readings. Simply monitoring home BP is of little value if the patients or their physicians do not act on the results.
_
20. AMBP has higher sensitivity and specificity for diagnosis of hypertension compared to both SMBP and OMBP. However, SMBP is an ideal first-line tool over AMBP because of its low cost, high availability, easy application, and because it has the particular advantage of promoting a better therapeutic adherence. Also, SMBP had a higher correlation (compared with OMBP) with AMBP.
_
21. SMBP can detect white coat hypertension and obviate unnecessary therapy. SMBP can also detect masked hypertension missed by doctor at clinic leading to better treatment of hypertension.
_
22. Automated oscillometric upper arm validated devices are best for SMBP. Self-BP measurements at home are usually performed using the non-dominant arm. When an apparent difference in BP is observed between the arms in a clinical setting, the arm showing the higher BP should be used for self-BP measurements. To provide consistent results, the same arm should always be used for self-BP measurements. For the beginner, I recommend duplicate SMBPs in the morning and evening. Duplicate means two readings at 1 minute interval.
_
23. Oscillometric wrist cuff devices for BP measurement are not recommended due to; 1) wrist is not held at mid-right atrium level, 2) radial and ulnar arteries are not completely occluded by sufficient pressure in cuff, 3) flexion and hyperextension at wrist influences BP, and 4) overestimation of systolic pressure occurs. Only in obesity with extremely large arm circumference and/or conical shaped arms, where fitting an appropriate cuff may be difficult, the use of wrist devices for SMBP might possibly be justified.
_
24. Finger BP is physiologically different from brachial BP, and issues of vasospasm in the winter season as well as hydrostatic pressure differences are inevitable. Therefore, oscillometric finger-cuff devices are no longer recommended.
_
25. SMBP is typically lower than OMBP by 8.1 mm Hg systolic and 5.6 mm Hg diastolic.
_
26. As far as cut off value for hypertension is concerned in adults; SMBP, awake AMBP and AOBP (automated office BP) are same; i.e. 135/85 mm Hg.
_
27. SMBP leads to faster diagnosis of hypertension, better accuracy of diagnosis of hypertension, greater control of hypertension, overcomes therapeutic inertia (reluctance by doctors to increase medication), improves patient compliance and reduces risks of hypertension. Blood pressure self-monitoring could save hypertensive population from thousands of unnecessary deaths every year.
_
28. Morning hypertension and non-reduction in nocturnal BP (non-dipper) correlate highly with target organ damage and both are missed in office BP measurement. AMBP and newer SMBP devices can pick up both.
_
29. SMBP can be done for high risk groups including children, pregnant women, elderly, obese, diabetic, chronic kidney disease, and even atrial fibrillation.
_
30. Most studies have shown that drug treatment for hypertension lowers clinic blood pressure more than home blood pressure and since home blood pressure is highly correlated with target organ damage and adverse prognosis, SMBP is far better than OMBP for evaluating efficacy of anti-hypertensive treatment.
_
31. Home blood pressure monitoring can save costs in health care since it lowers the number of clinic visits compared to conventional treatment of hypertension. Home BP has also been reported to lead to a reduction in medical expenditure via a decrease in the amount of drugs used.
_
32. Telemonitoring of home BP with physician leads to more appropriate and effective pharmacotherapy, better blood pressure control, and overall reduction in cardiovascular risk.
_
33. The biggest drawback of traditional brachial artery occlusion devices (auscultatory or oscillometric) is the occlusion of the brachial artery influences the local value of blood-pressure. In other words, the measurement changes the parameter to be measured. So we do need other technique to measure BP without occlusion of brachial artery. The pulse wave velocity (PWV) principle rely on the fact that the velocity at which an arterial pressure pulse travels along the arterial tree depends, among others, on the underlying blood pressure. Accordingly, after a calibration maneuver, these techniques provide indirect estimates of blood pressure by translating PWV values into blood pressure values. Innovative wrist watch device relies on a sensor that rests against radial artery in the wrist and detects the shape and velocity of the pressure pulse wave as blood flows through it. The device is first calibrated with a standard blood pressure monitor. Together with algorithms developed, the indices can be processed to get heart rate, diastolic and systolic pressure, and other measures. Now people can use wrist watch SMBP device using PWV principle. Using Fourier analysis, it is possible to derive the central aortic pressure waveform from the radial artery trace. However, comparisons with directly recorded aortic pressure made during cardiac catheterization have shown considerable scatter between the estimated and true values, so the technique cannot be recommended for estimating central aortic pressure.
_
34. Central aortic pressure is a better predictor of cardiovascular outcome than peripheral pressure and peripherally obtained blood pressure does not accurately reflect central pressure because of pressure amplification. Also antihypertensive medications have differing effects on central aortic pressure despite similar reductions in brachial blood pressure. Brachial BP can be unreliable, especially in young people whose more flexible blood vessel walls can give misleadingly high blood pressure, leading to unnecessary medical interventions. Conversely, old people with stiffer blood vessels may give a misleadingly low reading of brachial BP, disguising dangerous high blood pressure which can be a precursor to heart attack or stroke. In an innovative technique, radial artery sensor records a pulse wave at the wrist, and at the same time blood pressure is measured in the upper arm by conventional way. The data is then used to mathematically compute central aortic pressure. The process takes a few minutes more than conventional measurements. Direct comparison with traditional central aortic measurements obtained using the old-fashioned, invasive method shows a 99% correlation. All you need is a wrist watch device which records radial artery pressure pulse wave & a conventional upper arm BP monitor, and you can estimate your central aortic pressure at home.
_
35. The sensitivity and specificity of self reported hypertension found by SMBP is about 71% and 90% respectively. These results confirm the validity of self-reported hypertension among population. Since one out of three adults have hypertension worldwide and since out of all hypertensives, only half are aware that they have hypertension; these so called healthy people (unaware about hypertension) can measure BP randomly at home to detect hypertension in them and report to their doctor thereby save their lives from death. I therefore recommend that every home should have automated oscillometric SMBP device and if this recommendation is accepted by people, thousands of lives from so called healthy population would be saved worldwide every year.
___________
___________
Dr. Rajiv Desai. MD.
October 2, 2014
________
Postscript:
When most doctors and nurses cannot measure BP accurately, can we expect lay public to measure it accurately? This article is written to help people measure their own BP at home in most accurate way and adjust drug treatment accordingly in consultation with their doctors to save their lives. I urge doctors to possess two devices, mercury sphygmomanometer (regularly serviced) and automated oscillometric device (validated) in their clinic and take BP of every patient on both devices. In my view, ideal BP measurement device is still elusive.
_
Footnote:
I never understood why we inflate cuff, occlude brachial artery and then slowly release cuff air and then measure systolic pressure with first korotkoff sound and diastolic pressure with last korotkoff sound. Can we do the reverse? Slowly inflate brachial artery cuff and first sound heard is diastolic pressure and then keep on slowly inflating cuff till last sound heard which is systolic pressure. Well, I could not find any literature / reference on “Reverse Korotkoff Sounds”. If anybody knows it, please drop me an email.
_

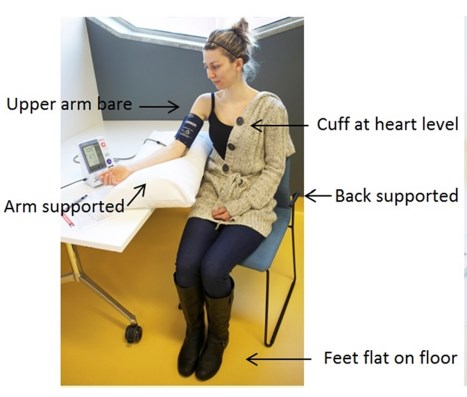
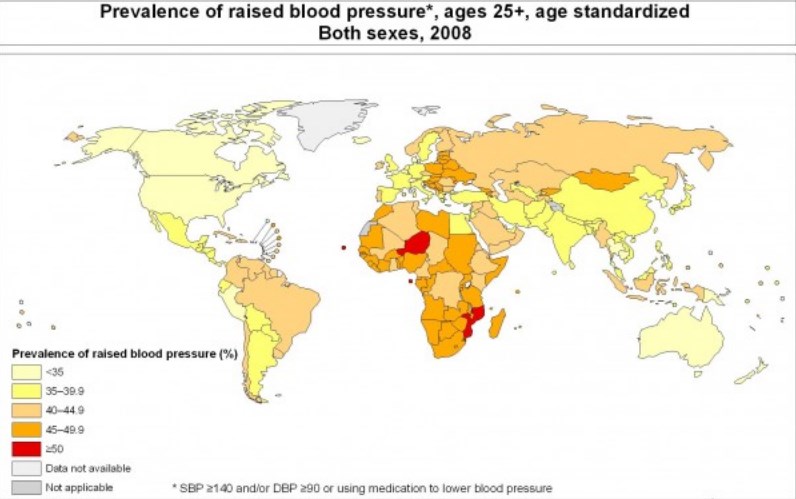
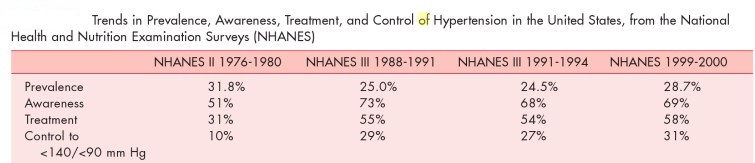
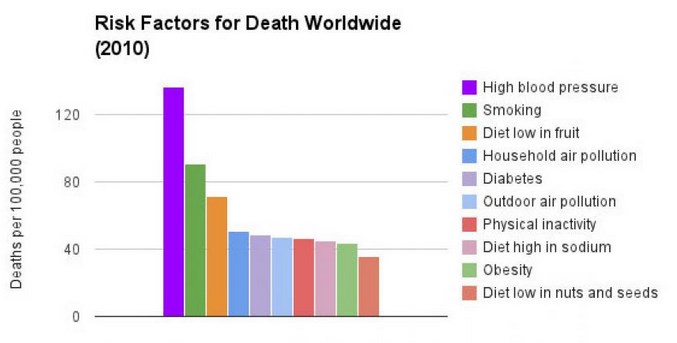
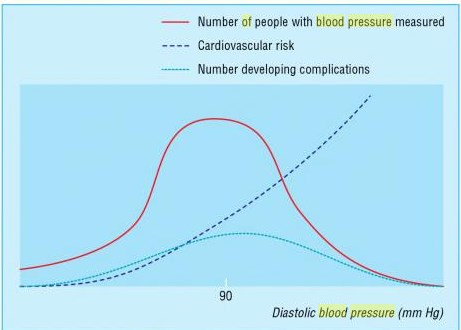
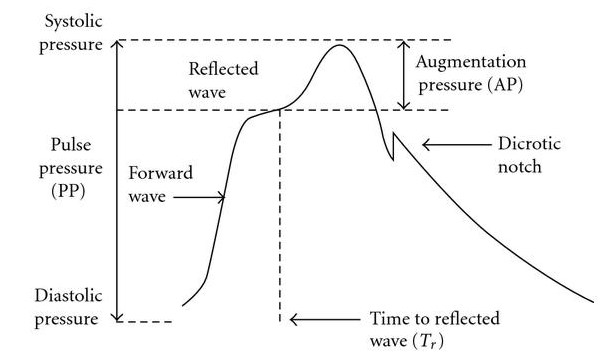
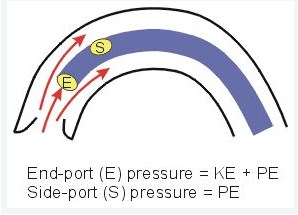
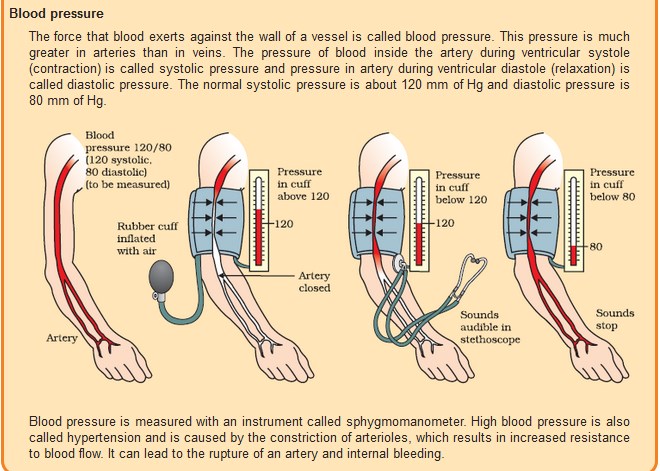
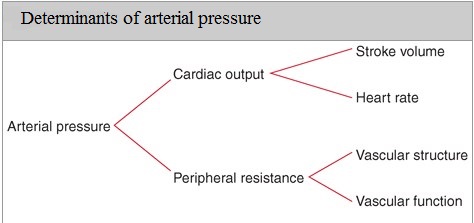
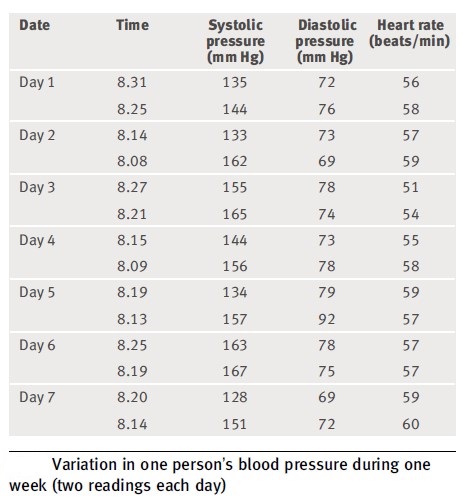
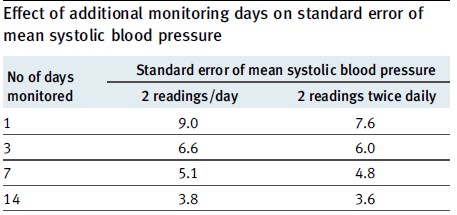
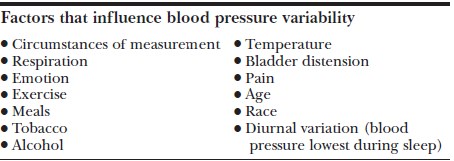
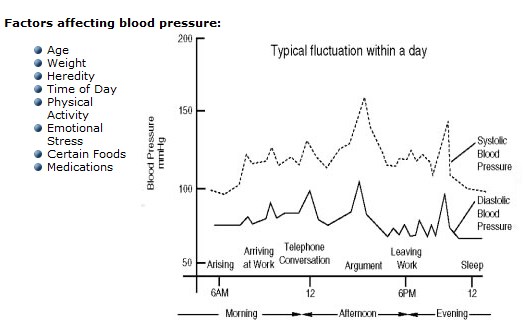
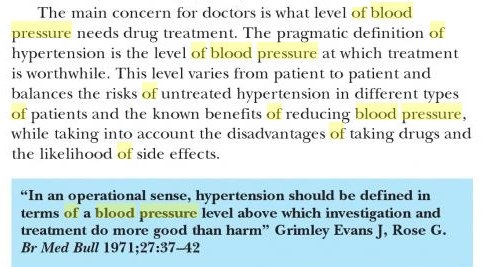
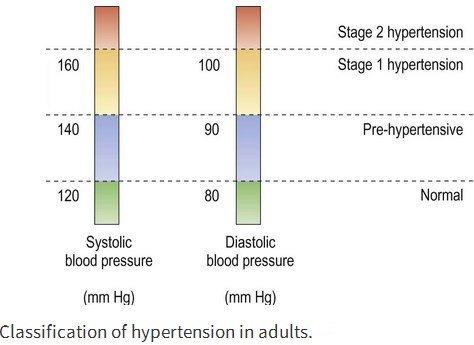
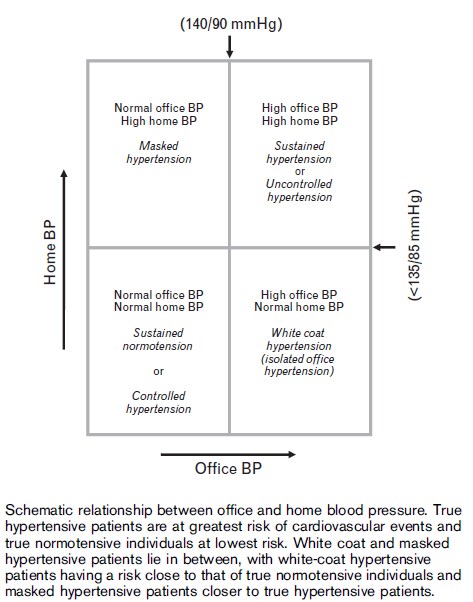
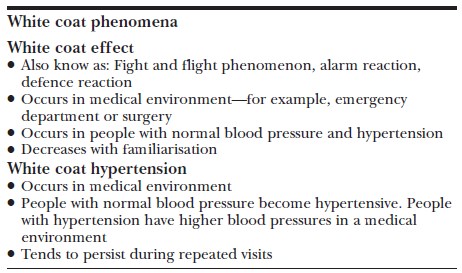
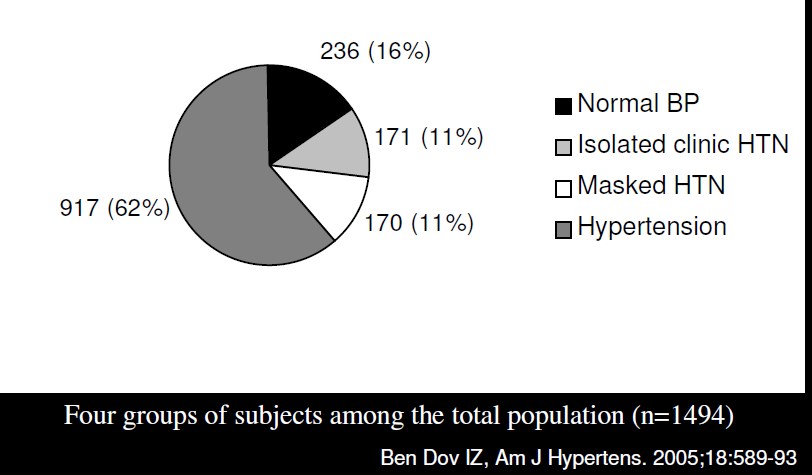
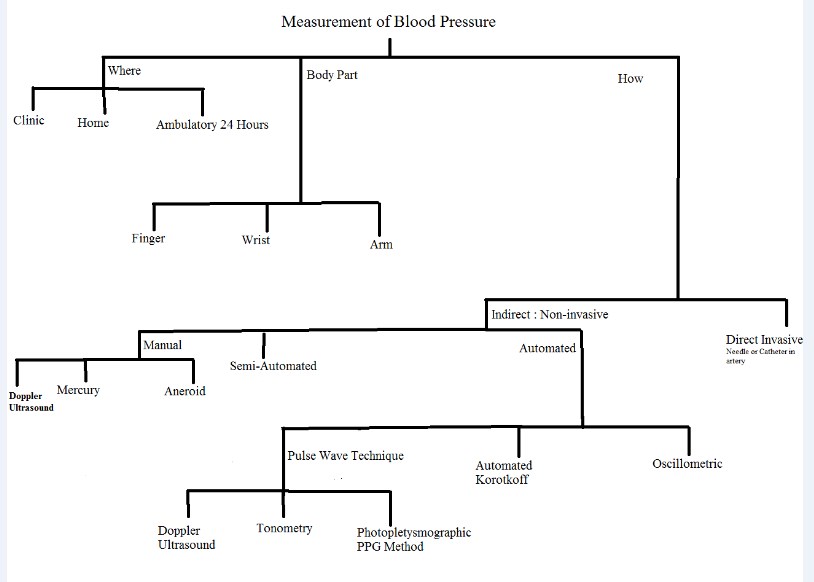
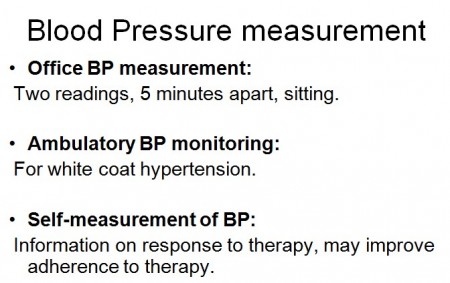
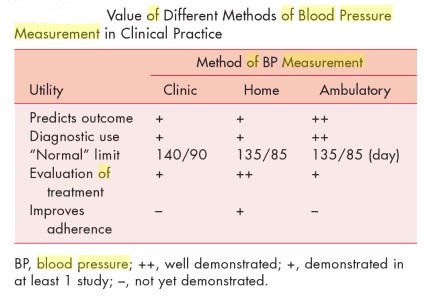
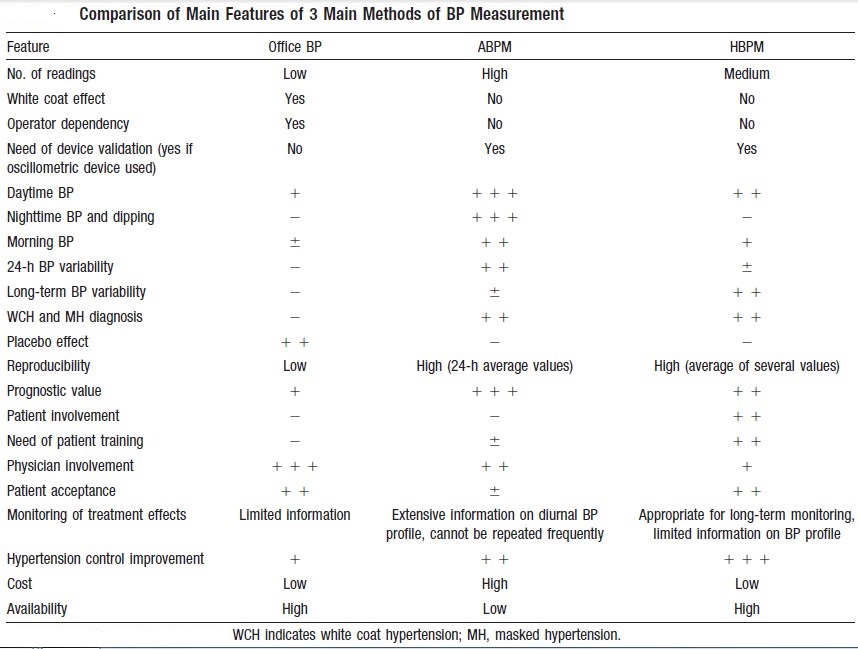
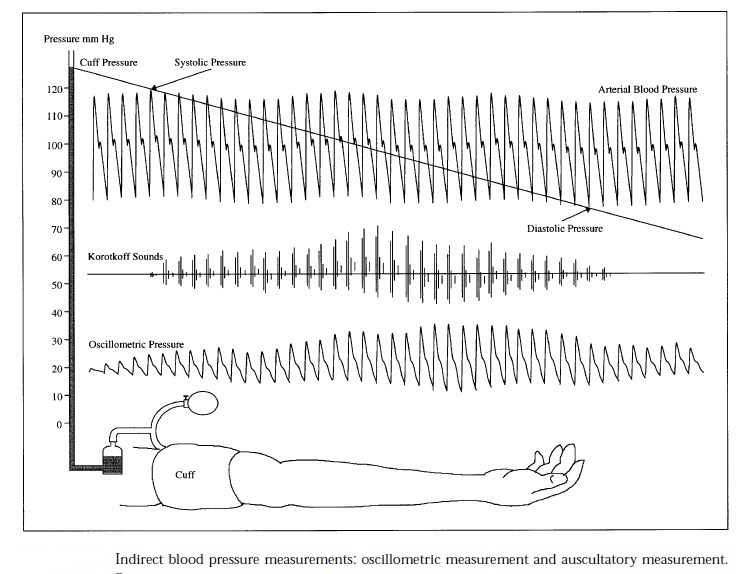
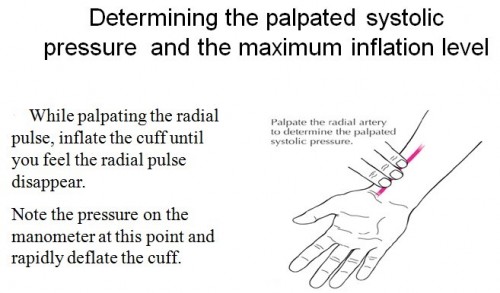
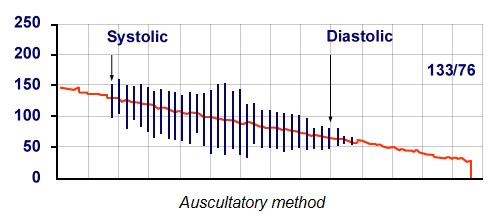
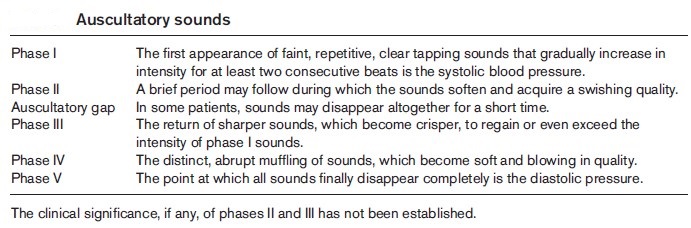
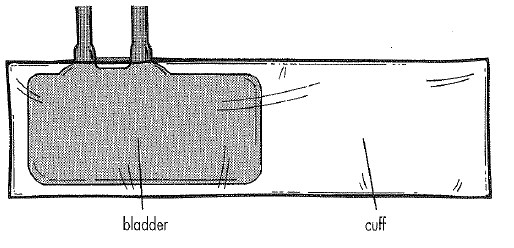

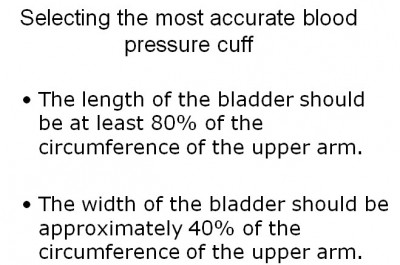
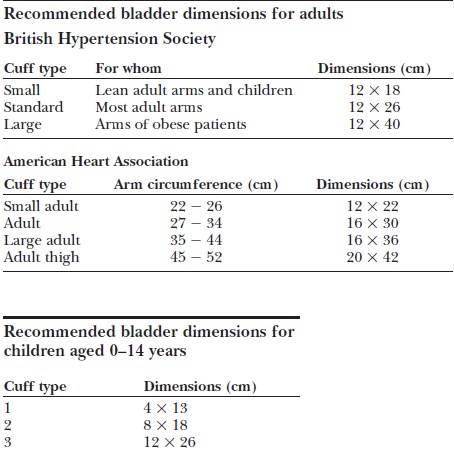
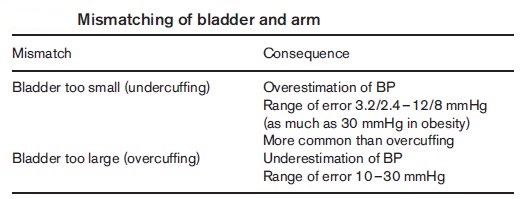
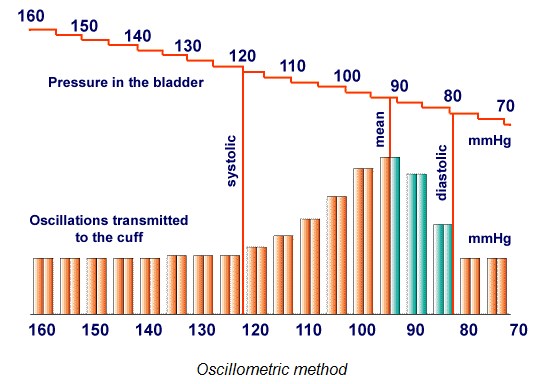
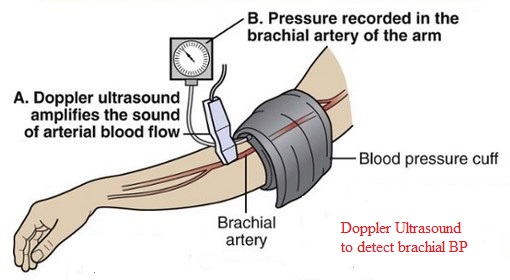
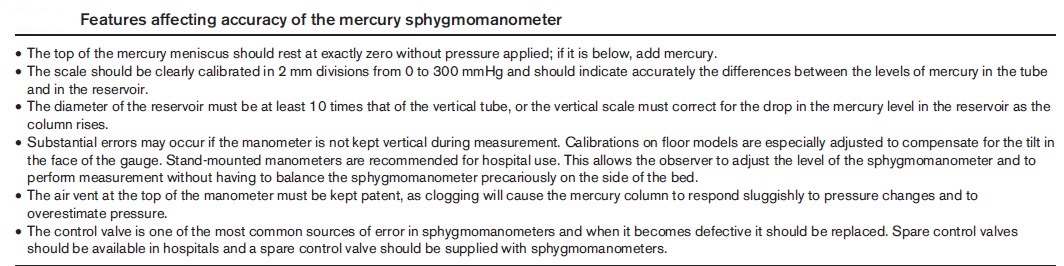
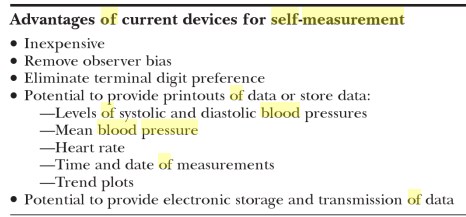
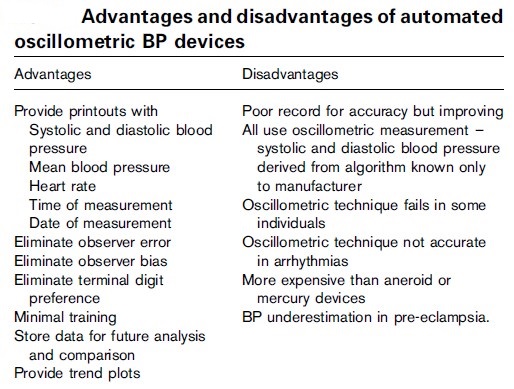
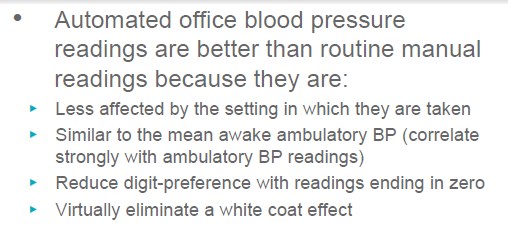
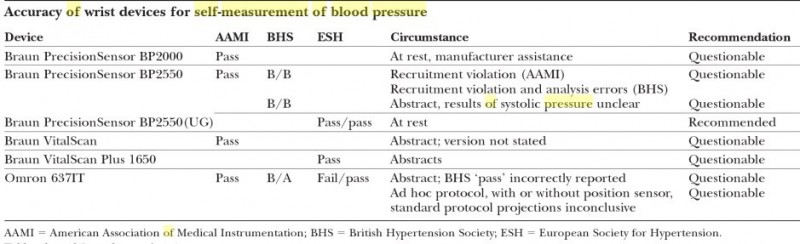
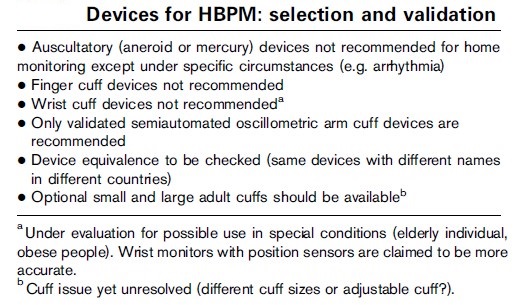
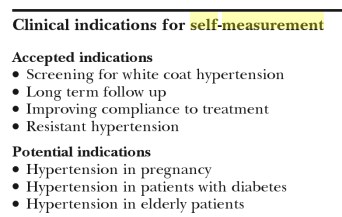
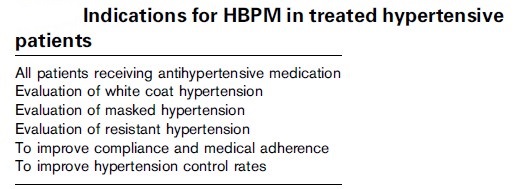
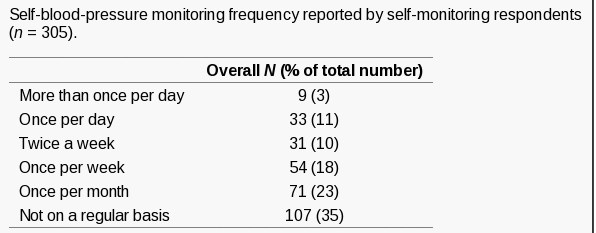

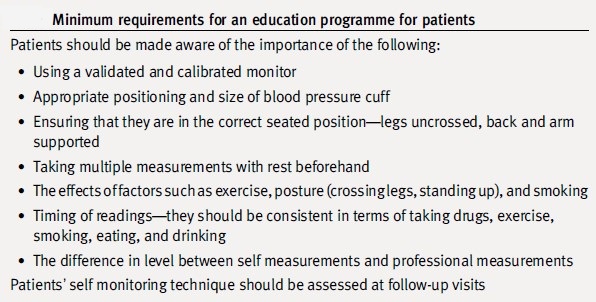
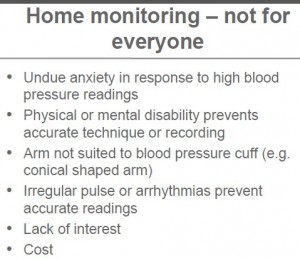
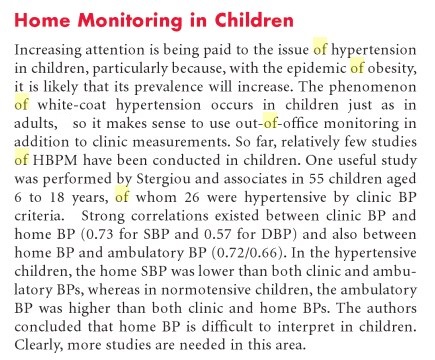
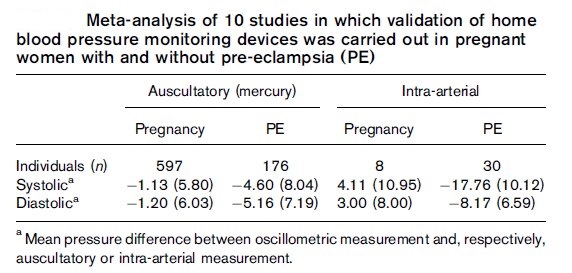
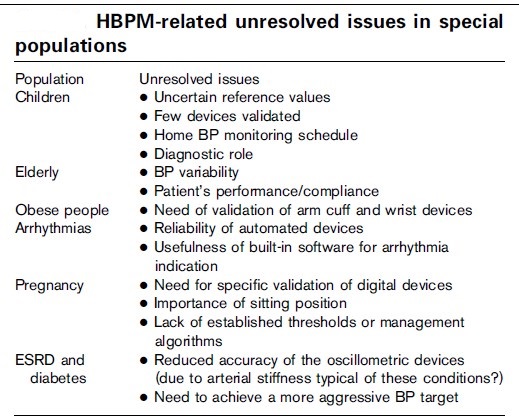
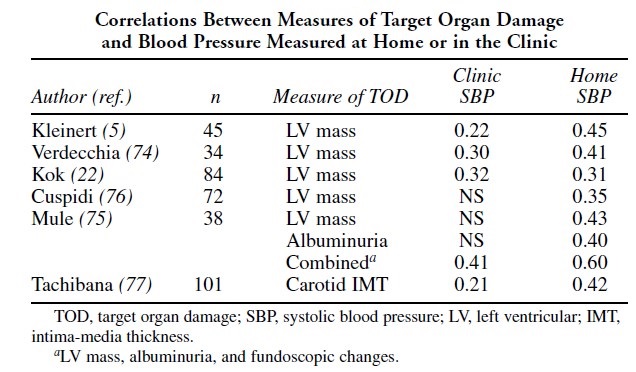
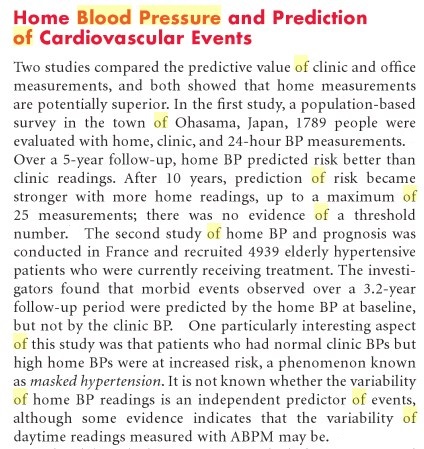
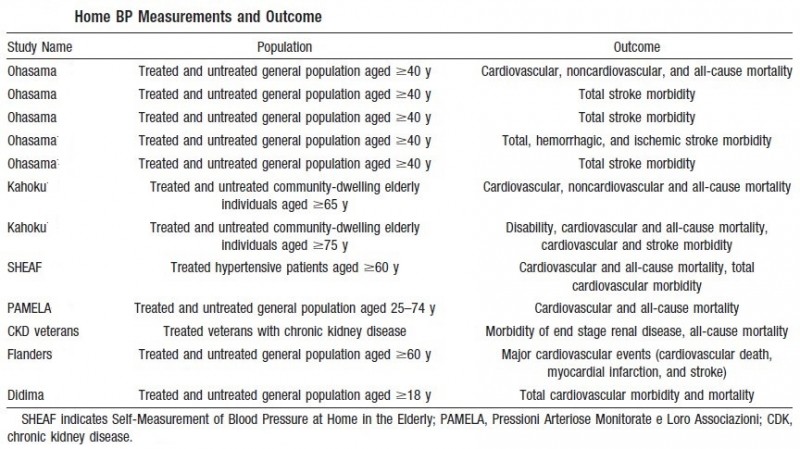
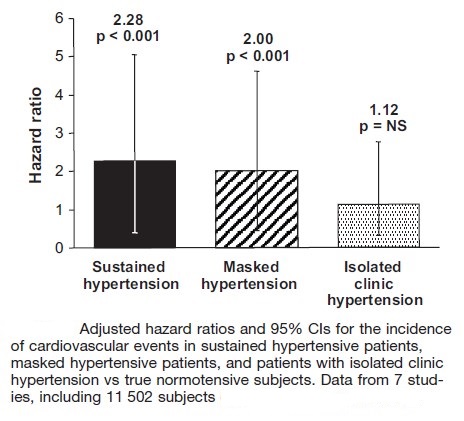
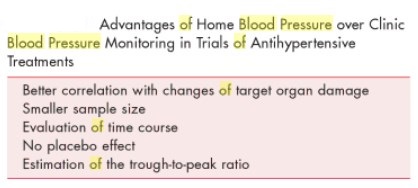
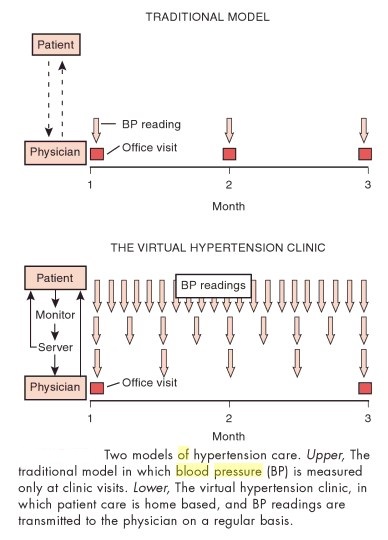
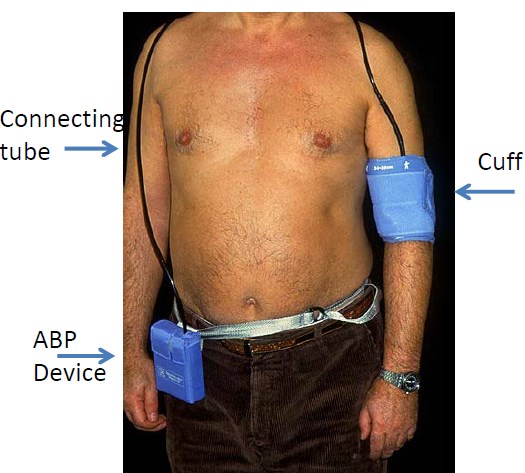
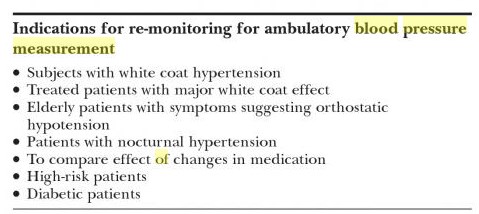
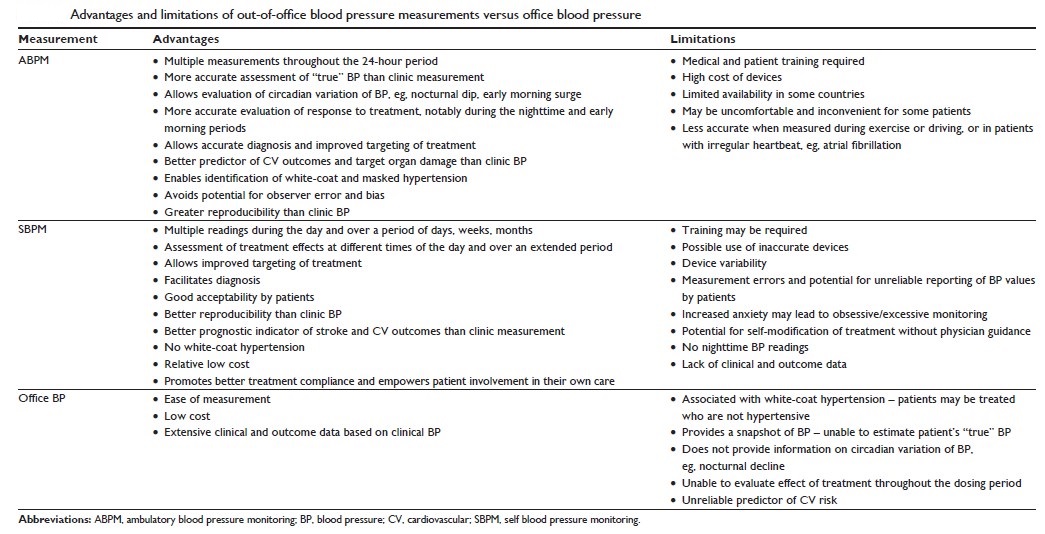
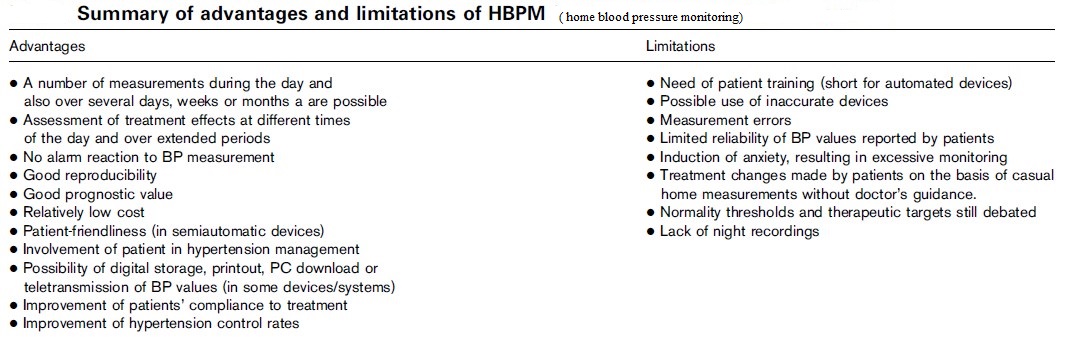
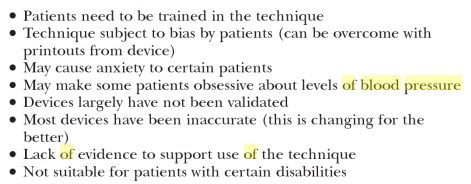
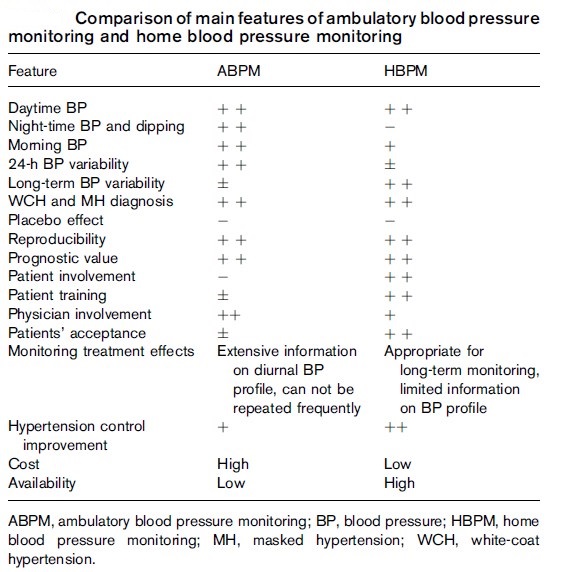
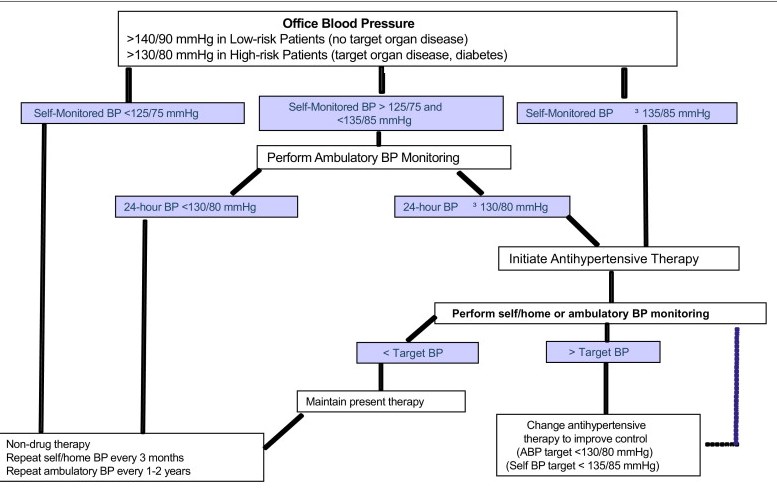
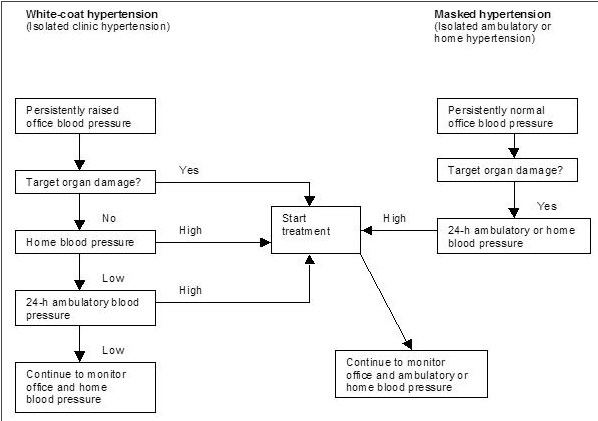

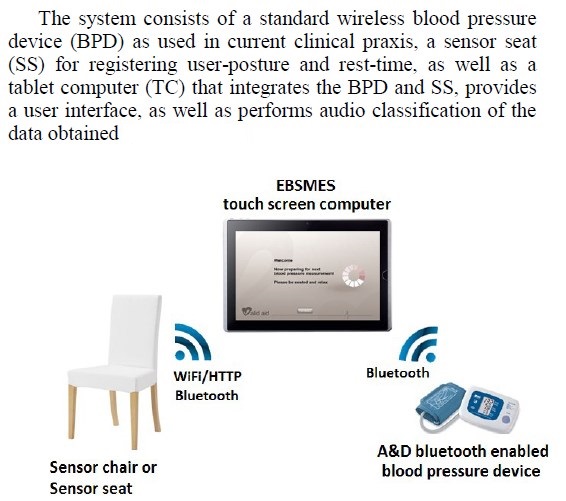

Thanks very interesting blog!|
I blog often and I truly thank you for your information. Your article has really peaked my interest. I’m going to take a note of your site and keep checking for new details about once per week. I subscribed to your Feed too.
“I’m not that much of a internet reader to be honest but your blogs really nice, keep it up! I’ll go ahead and bookmark your site to come back later on. All the best”