Dr Rajiv Desai
An Educational Blog
HEAT ILLNESS
HEAT ILLNESS:
_
Prologue:
Heat stroke is not new to the medical community. In 24 B.C., Roman soldiers with heat stroke were instructed to drink olive oil and wine while rubbing both liquids on the body. In the 1500s, physicians recommended stimulating friction and bloodletting to “release the heat”. In the 18th century, the cause of heat stroke was once thought to be drinking cold water. Patients would receive the diagnosis of “hurt by drinking cold water.” Amazingly, public pumps were posted with signs warning about the risk of sudden death from drinking cold water. Today, heat illness is the number one weather killer in the world and kills more people every year than tornadoes, hurricanes, flooding and lightening. Heat illness is more common in poor & middle class people than rich people because air-conditioners are beyond the reach of majority of middle class people (especially in developing countries) and all poor people. On the top of it, in my view, heat illness is commonly missed by patients, relatives and doctors. I remember a Saudi gentleman driving a car without air-conditioning for hundreds of kilometers in very hot Saudi summer brought to hospital with weakness, vomiting & high temperature; and was diagnosed as a case of fever by emergency doctor. It was impending heat stroke.
_
Seasons:
Seasons result from the yearly revolution of the Earth around the Sun (minor contribution) and the tilt of the Earth’s axis relative to the plane of revolution (major contribution). The Earth’s axis is tilted from perpendicular to the plane of the ecliptic by 23.5°. This tilting is what gives us the four seasons of the year – spring, summer, autumn (fall) and winter. Since the axis is tilted, different parts of the globe are oriented towards the Sun at different times of the year. Summer is warmer than winter (in each hemisphere) because the Sun’s rays hit the Earth at a more direct angle during summer than during winter and also because the days are much longer than the nights during the summer. During the winter, the Sun’s rays hit the Earth at an extreme angle, and the days are very short. These effects are due to the tilt of the Earth’s axis. During May, June and July, the northern hemisphere is exposed to more direct sunlight because the hemisphere faces the sun. The same is true of the southern hemisphere in November, December and January. When it is summer in the southern hemisphere it is winter in the northern hemisphere, and vice versa. It is the tilt of the Earth that causes the Sun to be higher in the sky during the summer months which increases the solar flux. The solstices are days when the Sun reaches its farthest northern and southern declinations. For the year 2011, the winter solstice occurs on December 22 and marks the beginning of winter (this is the shortest day of the year) and the summer solstice occurs on June 21 and marks the beginning of summer (this is the longest day of the year). However, there exists a variable seasonal lag meaning that the meteorological start of the season, which is based on average temperature patterns, occurs several weeks later than the start of the astronomical season. According to meteorologists, summer extends for the whole months of June, July, and August in the northern hemisphere and the whole months of December, January, and February in the southern hemisphere. In southern and Southeast Asia, where the monsoon occurs, summer is more generally defined as lasting from March to May/early June, their warmest time of the year, ending with the onset of the monsoon rains.
_
Climate change (global warming) and health:
Global warming is the current rise in the average temperature of Earth’s oceans and atmosphere. During the 20th century, global surface temperature increased by about 0.74 °C (1.33 °F) and it is projected that global surface temperature is likely to rise 1.1 to 6.4 °C (2.0 to 11.5 °F) by 2100. It would be speculative to assume that the cooling mechanisms developed by human body over evolution of millions of years to dissipate extra-heat, will in fact work, when global warming causes increase in ambient temperature by 1 to 2 degree Celsius over 50 years. Sufficient to say that our body would not have developed newer mechanism to dissipate extra-heat of global warming and therefore our existing heat dissipation mechanisms would be overloaded and can be overwhelmed by global warming.
_
Climate change threatens far more than our environment. It has already led to the spread of infectious diseases and respiratory ailments across the globe and contributed to thousands of deaths through heat waves and other extreme weather events. Malaria, Lyme disease, and cholera, as well as food shortages and malnutrition, are all becoming increased risks with steadily rising temperatures. Even slight increases in temperature – a couple of degrees – can broaden the habitat of pests that cause infectious diseases, from malaria in Kenya to Lyme disease in Maine. Pests also target wildlife, wiping out forests and increasing the risk of fires, such as in the Rockies and Cascades, where it used to be too cool for those pests to venture to high altitudes. A WHO report estimated that an additional 150,000 people were dying every year from global warming – mainly from malnutrition, diarrhoea and malaria. Another result of a changing climate: heat and carbon dioxide magnify the effects of asthma and allergies, particularly in cities where more and more children are developing respiratory problems.
_
Climate change is leading to variations in weather patterns and an apparent increase in extreme weather events, including heat-waves. And a combination of heat waves — such as the one that killed fifteen thousands Russians last summer (2010) — and droughts not only causes immediate local health crises, but also threatens global public health by destroying crops and driving up food prices. The heat-waves have led to a rise in related mortality but the adverse health effects of hot weather and heat-waves are largely preventable. Prevention requires a portfolio of actions at different levels, including meteorological early warning systems, timely public and medical advice, improvements to housing and urban planning, and ensuring that health care and social systems are ready to act. These actions can be integrated into a defined heat–health action plan.
__
Population health outcomes of hot weather and heat waves depend upon the level of exposure (frequency, severity and duration), the size of the exposed population and the population sensitivity. It is therefore not surprising that the relationship between daily weather and health varies between populations and between studies. For a given city or region there is a general pattern of increase in the number of daily deaths above and below an optimum range of temperatures.
_
Are we warm-blooded?
We humans are warm-blooded animals. In fact, with a few exceptions, all mammals and birds are warm-blooded, and all reptiles, insects, arachnids, amphibians and fish are cold-blooded. Warm-blooded creatures try to keep the inside of their bodies at a constant temperature. In other words, warm-blooded species tries to maintain core body temperature independent of environmental temperature. The human body has the remarkable capacity for regulating its core temperature somewhere between 98°F and 100°F when the ambient temperature is between approximately 68°F and 130°F. They do this by generating their own heat when they are in a cooler environment, and by cooling themselves when they are in a hotter environment. To generate heat, warm-blooded animals convert the food that they eat into energy. They have to eat a lot of food, compared with cold-blooded animals, to maintain a constant body temperature. Only a small amount of the food that a warm-blooded animal eats is converted into body mass. The rest is used to fuel a constant body temperature. Cold-blooded creatures take on the temperature of their surroundings. They are hot when their environment is hot and cold when their environment is cold. In hot environments, cold-blooded animals can have blood that is much warmer than warm-blooded animals. A cold-blooded animal can convert much more of its food into body mass compared with a warm-blooded animal. Mammals and birds require much more food & energy than do cold-blooded animals of the same weight.
_
Heat generated by human body:
Out of total energy derived from food, about 20 percent is utilized for all metabolic processes and the remaining 80 percent is converted into heat to maintain the core temperature of human body. Irrespective of the work output, a human body continuously generates heat at a rate varying from about 100 Watts (e.g. for a sedentary person) to as high as 2000 Watts (e.g. a person doing strenuous exercise). Continuous heat generation is essential, as the temperature of the human body has to be maintained within a narrow range of temperature, irrespective of the external surroundings. The rate of metabolic heat production is primarily controlled by the rate of body activity. In general, the more physically active (physical exertion), the higher the metabolic rate and the higher metabolic rate will generate more heat which in turn will increase body temperature above normal unless extra-heat is dissipated. Other factors which influence an individual’s metabolic rate include: body weight, sex, age and state of health. The metabolic rate is normally measured in the unit “Met”. A Met is defined as the metabolic rate per unit area of a sedentary person and is found to be equal to about 58.2 W/m2. This is also known as “basal metabolic rate”. When the metabolic rate is about 1 Met (58.2 W/m2), there is neither body cooling nor body heating at an operative temperature of about 25.5 deg C for light clothed person. That means that when Met is higher, more heat is generated necessitating heat dissipation to prevent core temperature rising. The resting individual has metabolic rate of 0.7 met, light work 1.2 met, walking 2 met and wrestling 7 met. The total heat generated rate by body is given in following formula.
Where A is the surface area of the body in square-meter and QG is total heat generated in watts. For example, a normal adult with 1.7 square-meter body area is walking (2 met) that will generate heat of 197.8 watts.
_
Body temperature:
Is this the correct way to measure body temperature?
An axillary temperature is when your armpit (axilla) is used to check your temperature. No reputed textbook of medicine advocates axillary temperature measurements. This is because axilla (armpit) is exposed to air and hence its temperature is influenced by air temperature. Axillary temperature should be read after 5 minutes but nobody waits for 5 minutes. Even under ideal conditions, an armpit (axillary) temperature is usually 0.5°F (0.3°C) to 1°F (0.6°C) lower than an oral temperature. So when you are taking axillary temperature, you are going to miss many cases of fever and heat illnesses. To counteract it, nurses add 1 degree to the temperature they get from armpit for a more accurate reading but it is unscientific to say the least. Nonetheless, the sorry state of affairs in India, I have seen many nurses & doctors taking axillary temperature and nobody objects to it.
_
While measuring the temperature, make sure that the patient hasn’t just had a bath or has been exercising. This could give a wrong temperature reading. Improper placement of the thermometer or removing it too quickly, could also give a faulty thermometer reading. Oral or rectal temperature should be measured. For oral temperature measurement, with your mouth open, put the tip of thermometer under your tongue. Close your lips gently around the thermometer. Avoid using mercury thermometer because if thermometer breaks, mercury may be swallowed or absorbed. A child younger than 5 years may bite the thermometer, breaking it in their mouth. So take rectal temperature in children below 5 years. There is a perception that axillary temperature should be taken in infants as it is too dangerous to take oral or rectal temperature. Taking oral temperature may be dangerous in infants for the risk of breaking thermometer in mouth but the same cannot be said about rectal temperature. Rectal temperature measurement is safer than previously suggested as perforation has occurred in less than one in two million measurements. Also, when used in hospital to detect high temperature, axillary temperature had a sensitivity of 73% compared with rectal temperature. This is too insensitive for accurate detection of an infant’s high temperature. Therefore, if an infant’s temperature needs to be taken, rectal temperature should be used. If heat stroke is suspected, always take rectal temperature in all age groups.
_
Different parts of the body have different temperatures. Core temperature is the temperature of structures deep within the body, as opposed to peripheral (surface) temperature such as that of the skin. The skin is the largest organ in the human body. It protects the body from the sun’s rays. It also keeps body (core) temperature normal (37 °C). Skin temperature depends on air temperature and time spent in that environment. Such weather factors as wind chill and humidity cause changes in skin temperature. The normal temperature of skin is about 33 °C or 91 °F. The flow of energy to and from the skin determines our sense of hot and cold. Heat flows from higher to lower temperature, so the human skin will not drop below that of surrounding air, regardless of wind. If a person goes in a warm room and his skin temperature was cooler than the air, then his skin temperature would rise. The opposite would happen in a cold room and warm skin temperature. The person’s skin temperature would decrease. Humans fight air temperature by becoming warm or cold. When warm, they sweat. When cold, they get chills. On a trip during a windy and snowy day, a man recorded his skin temperature from different parts of body while climbing a mountain. The skin temperature of his toe was about 15 °C. At the same time, the skin temperature of his chest was 32 °C. This proves that different parts of body can have different skin temperatures. The skin over chest is closer to core of body while skin over toes is far away from core of body.
_
Rectal and vaginal measurements, or measurements taken directly inside the body cavity, are typically slightly higher than oral measurements, and oral measurements are somewhat higher than skin temperature. Temperature examination in the rectum is the traditional gold standard measurement used to estimate core temperature. Rectal temperatures are generally 0.4°C (0.7°F) higher than oral readings. Lower oral readings are probably attributable to mouth breathing, a particularly important factor in patients with respiratory infections and rapid breathing. Also, oral temperature is affected by hot or cold drink taken just before measurement. Lower-esophageal temperatures closely reflect core temperature. Tympanic (ear) thermometer measurements, although convenient, may be more variable than directly determined oral or rectal values. Ear thermometers measure eardrum temperature using infrared sensors. The blood supply to the tympanic membrane is shared with the brain. However, this method of measuring body temperature is not as accurate as rectal measurement and has a low sensitivity for fevers, missing three or four out of every ten fevers in children. Ear temperature measurement may be acceptable for observing trends in body temperature but it is less useful in consistently identifying fevers.
_
The commonly accepted average core body temperature (taken internally) is 37.0 °C (98.6 °F). The typical oral (under the tongue) measurement is slightly cooler, at 36.8±0.7 °C, or 98.2±1.3 °F, with low levels at 6 a.m. and high levels at 4–6 p.m. Normal daily temperature variation is typically 0.5°C (0.9°F). In some individuals recovering from a febrile illness, daily variation can be as great as 1.0°C. During a febrile illness, diurnal variations are usually maintained, but at higher levels. Daily temperature swings do not occur in patients with hyperthermia. It is observed that when the core temperature is between 35 to 39oC, the body experiences only a mild discomfort. When the temperature is lower than 35oC or higher than 39oC, then people suffer major loss in efficiency. It becomes lethal when the temperature falls below 31oC or rises above 43oC.
_
| Core temperature (rectal, esophageal, etc.) | |
| Normal | 36.5–37.5 °C (98–100 °F) |
| Hypothermia | <35.0 °C (95.0 °F) |
| Fever | >37.5–38.3 °C (100–101 °F) |
| Hyperthermia | >37.5–38.3 °C (100–101 °F) |
| Hyperpyrexia | >41.5 °C (>106.7 °F) |
| Note: The difference between fever and hyperthermia is the mechanism | |
_
Thermoregulation:
Body temperature is controlled by the hypothalamus in our brain. Neurons in both the preoptic anterior hypothalamus and the posterior hypothalamus receive two kinds of signals: one from peripheral nerves that reflect warmth/cold receptors and the other from the temperature of the blood bathing the region. These two types of signals are integrated by the thermoregulatory center of the hypothalamus (thermostat) to maintain normal temperature. In a neural environment, the metabolic rates of humans consistently produce more heat than is necessary to maintain the core body temperature of 37 degree C. A normal body temperature is ordinarily maintained, despite environmental variations, because the hypothalamic thermoregulatory center balances the excess heat production derived from metabolic activities from muscles & liver with heat dissipation from skin & lungs.
_
Elevated body temperature occurs due to process of heat conservation (vasoconstriction) and heat production (shivering and increased metabolic activity). Vasoconstriction means blood vessels in the periphery of body are constricted, shunting away blood form periphery (skin) to the internal organs. The person feels cold. This process can increase body temperature by 1-2 degree C. Vasoconstriction can directly prevent heat loss from skin by reducing heat loss via radiation, convection and conduction. Shivering, which increases heat production from muscles, can increases temperature further. Heat productions from liver also contribute. Human behavior of putting on more clothing/bedding can also help raise temperature by reducing heat loss from skin. So when you are exposed to cold environment, body maintains core temperature by vasoconstriction, increased heat production and behavioral changes.
_
Lowering of body temperature occurs by process of heat loss via sweating and vasodilatation. Vasodilatation means blood vessels in periphery of body are dilated drawing away blood from internal organs to periphery (skin) promoting heat loss via skin. Vasodilatation can directly promote heat loss from skin by the processes of radiation, convection and conduction provided skin temperature is higher than ambient temperature. Skin blood flow can increase from approximately 0.2–0.5 L/min in normothermia to values exceeding 7–8 L/min hyperthermia. However, if the ambient temperature is higher than skin temperature, then, sweat evaporation is the only means of heat loss. The evaporation of sweat from skin takes away bodily heat promoting heat loss, thereby reducing temperature. So when you are exposed to hot environment, body maintains core temperature by vasodilatation and sweating. Heat produced by metabolic processes of body can not be reduced in hot environment because these metabolic processes are essential for our survival.
_
The healthy human body maintains its internal temperature around 37°C. Variations, usually of less than 1°C, occur with the time of the day, level of physical activity or emotional state. A change of body temperature exceeding 1°C occurs only during illness or when environmental conditions surpass the body’s ability to cope with extreme temperatures. As the environment warms-up, the body tends to warm-up as well. The body’s internal “thermostat” maintains a constant inner body temperature by pumping more blood to the skin and by increasing sweat production. In this way, the body increases the rate of heat loss to balance the heat burden created by the environment. In a very hot environment, the rate of “heat gain” exceeds the rate of “heat loss” and the body temperature begins to rise. A rise in the body temperature results in heat illnesses.
_
The normal human body temperature range (36.1–37.8 ºC) is maintained by the hypothalamus which constantly regulates heat gain and heat loss. The main source of heat gain is the body’s own internal heat called metabolic heat. It is generated within the body by the biochemical processes that keep us alive and by the energy we use in physical activity.
Heat is exchanged with the environment by:
(1) Radiation occurs through electromagnetic waves in the form of infrared rays. At rest, radiation is the primary method of heat loss. Heat loss by radiation occurs by electromagnetic waves when someone is in an environment that is cooler than the body temperature. Therefore, if the ambient temperature is 60 deg F, and the body temperature is 98.6 deg F, the body radiates heat to the environment, including buildings, trees, etc. Radiation is the process by which the body gains heat from surrounding hot objects, such as hot metal, furnaces or steam pipes, and loses heat to cold objects, such as chilled metallic surfaces, without contact with them. No radiant heat gain or loss occurs when the temperature of surrounding objects is the same as the skin temperature (about 33°C).
_
(2) Convection occurs through water or air circulating across the skin. Convection is the process by which the body exchanges heat with the surrounding air. The body gains heat from hot air and loses heat to cold air which comes in contact with the skin. Convective heat exchange increases with increasing air speed and increased difference between air and skin temperature.
_
(3) By conduction, the body gains or loses heat when it comes into direct contact with hot or cold objects. It is a small amount as compared to other heat exchange modalities.
_
(4) Evaporation of sweat.
_
Conduction, radiation and convection require a temperature gradient between the skin and its surroundings, and evaporation entails a water vapor pressure gradient. Excessive heat exposure constitutes a major stress for the organism but particularly for the cardiovascular system. When environmental heat overwhelms the body’s heat-dissipating mechanisms, core temperature rises. An increase of less than 1 ºC is immediately detected by thermoreceptors disseminated through the skin, deep tissues and organs. The thermoreceptors convey the information to the hypothalamic thermoregulatory centre, which triggers two powerful responses to increase dissipation of heat: an active increase in skin blood flow and initiation of sweating (through cholinergic pathways). The cutaneous vasodilatation results in marked increases in blood flow to the skin and cardiac output, at the expense of other major systems. When the outdoor temperature is higher than the skin temperature, the only heat loss mechanism available is evaporation (sweating). Therefore, any factor that hampers evaporation, such as high ambient humidity, reduced air currents (no breeze, tight fitting clothes) or drugs with anticholinergic mechanisms, will result in a rise of body temperature that can culminate in life-threatening heatstroke or aggravate chronic medical conditions in vulnerable individuals. Evaporation proceeds more quickly and the cooling effect is more pronounced with high wind speeds and low relative humidity. In hot and humid workplaces, the cooling of the body due to sweat evaporation is limited by the capacity of the ambient air to accept additional moisture. In hot and dry workplaces, the cooling due to sweat evaporation is limited by the amount of sweat produced by the body. The body also exchanges small amounts of heat by breathing. Breathing exchanges heat because the respiratory system warms the inhaled air. When exhaled, this warmed air carries away some of the body’s heat. However, the amount of heat exchanged through breathing is normally small enough to be ignored in assessing the heat load on the body. Also, evaporation of insensible fluid from skin (trans-epithelial) & respiratory tract is a major source of heat loss from the body each day but is not under regulatory control.
_
Under control of thermoregulatory mechanisms, sweating begins almost precisely at a skin temperature of 37°C and increases rapidly as the skin temperature rises above this value. The heat production of the body under these conditions remains almost constant as the skin temperature rises. If the skin temperature drops below 37°C, a variety of responses are initiated to conserve the heat in the body and to increase heat production. These include
1) Vasoconstriction to decrease the flow of heat to the skin.
2) Cessation of sweating.
3) Shivering to increase heat production in the muscles.
4) Secretion of norepinephrine, epinephrine, and thyroxine to increase heat production.
_
Heat Balance equation
Body Heat = Metabolism + [+/- conduction +/- radiation +/- convection – evaporation]
Note:
Conduction, convection and radiation modes of heat transfer proceeds only form higher temperature to lower temperature. If the skin temperature is higher than ambient temperature, heat will be lost from body to environment through these 3 modes. If the ambient temperature is higher than skin temperature, then, heat will be gained by body through these 3 modes. Sweat evaporation is a one way traffic. Heat is always lost from body to environment through sweat evaporation. Unless the person has more heat than can be eliminated by radiation and convection, evaporation (through perspiration) is not required and conduction is negligible. A sedentary person at neutral condition loses about 40 % of heat by evaporation, about 30 % by convection and 30 % by radiation. However, this proportion may change with other factors. The process of sweating itself consumes energy but it is negligible in quantity and therefore not considered.
__
Sweat:
Sweating is controlled from a center in the hypothalamus where thermosensitive neurones are located. The heat regulatory function of the hypothalamus is affected by inputs from temperature receptors in the skin. High skin temperature reduces the hypothalamic set point for sweating and increases the gain of the hypothalamic feedback system in response to variations in core temperature. Overall though, the sweating response to a rise in hypothalamic temperature (‘core temp’) is much larger than the response to the same increase in average skin temperature. The volume of water lost in sweat daily is highly variable, ranging from 100 to 8,000 ml/day. It is made almost completely of water, with tiny amounts of other chemicals like ammonia, urea, salts, and sugar. The solute loss can be as much as 350 mmol/day (or 90 mmol/day acclimatized) of sodium under the most extreme conditions. In a cool climate and in the absence of exercise, sodium loss can be very low (less than 5 mmols/day). Sodium concentration in sweat is 30-65 mmol/l, depending on the degree of acclimatization. In humans, sweat is hypo-osmotic relative to plasma. In general, emotionally induced sweating is restricted to palms, soles, armpits, and sometimes the forehead, while physical heat-induced sweating occurs throughout the body. Individuals with heat exposure can require from 5 to 13 liters of water per day depending upon the type of work they do. Salt consumption should be slightly increased to compensate for loses due to sweating. However, an average American/Indian diet contains excess salt anyway, so salt tablets are unnecessary and may indeed be harmful. Horses and humans are two of the few animals capable of sweating. Animals with few sweat glands, such as dogs, accomplish similar temperature regulation results by panting, which evaporates water from the moist lining of the oral cavity and pharynx. The adult human body can maximally produce 1 to 2 liters of perspiration every hour to cool it. If there’s not enough fluid or the heat overwhelms the body, the person develops a heat related illness.
_
Do humans pant?
Panting is the primary avenue for evaporative heat loss in most non-sweating animals, dissipating as much as 95% of metabolic heat. Panting is dominated by an increased breathing frequency, with elevated evaporative heat loss occurring within the upper airways at frequencies as high as 200 breaths/min. Humans have an extremely powerful sweating response, and while the coexistence in humans of hyperthermia and hyperventilation has been known for almost 100 years; ventilatory heat losses generally constitute a small portion of total heat loss during thermal stress. Contrary to the situation in panting species where there is no clear threshold body temperature for the onset of hyperventilation; a change in respiration occurs in humans (hyperthermic hyperventilation) only when core body temperature has risen to a threshold value; once a threshold temperature is exceeded, hyperventilation ensues. This threshold is significantly higher than the threshold temperatures for both the onset of sweating and increase in cutaneous blood flow, demonstrating that the respiratory response to hyperthermia is a part of the usual group of thermolytic reflexes to cool down brain. Most heat exchange takes place at the nasal epithelial lining, and venous drainage can be directed to a special network of arteries at the base of the brain whereby countercurrent heat transfer can occur, which results in selective brain cooling.
_
Evaporation of sweat from the skin surface has a cooling effect due to the latent heat of evaporation of water. Hence, in hot weather, or when body heats up due to physical exertion, more sweat is produced. Typically, all of the sweat does not evaporate, but a part of it runs off your skin. After the sweat has been evaporated, the water vapor must move away from the skin in order that more evaporation can occur; which is dependent on speed of air movement around skin. The driving force for evaporation is the gradient of the water vapor pressure near the skin surface. The water vapor pressure is that part of the total pressure of the air which is caused by the molecules of water vapor in it. The maximum driving force is the difference between the vapor pressure of water at skin temperature and the vapor pressure in the air as a whole. Remember, vapor pressure of water is different from vapor pressure in air (vide infra). Higher the humidity of air, greater will be vapor pressure in air, lesser will be the gradient of water vapor pressure at the skin surface and lesser will be sweat evaporation.
_
If air temperature is as warm as or warmer than the skin, blood brought to the body surface cannot lose its heat. Under these conditions, the heart continues to pump blood to the body surface, the sweat glands pour liquids containing electrolytes onto the surface of the skin and the evaporation of the sweat becomes the principal effective means of maintaining a constant body temperature. Sweating does not cool the body unless the moisture is removed from the skin by evaporation. Under conditions of high humidity, the evaporation of sweat from the skin is decreased and the body’s efforts to maintain an acceptable body temperature may be significantly impaired.
_
Ratio of body surface area to body mass (weight);
Assuming all other factors same, the heat transfer between environment and human body is proportional to the surface area of the body, while the heat generated by the body is proportional to its mass. Greater the mass of human body, more heat will be generated. Greater the surface area, more heat will be lost through radiation, conduction and convection if environmental temperature is less than body temperature which is the case in many parts of worlds in all seasons. However, in other parts of world, during summer, the environmental temperature is higher than body temperature. Again, greater surface area will be advantageous as more heat can be lost via sweating. The ratio of body surface area to body mass is crucial in determining body response to environmental temperature changes. A commonly accepted view in human physiology literature is that a high surface to mass ratio is beneficial in the heat. This is based on the concept that body surface determines heat loss capacity for dry and evaporative heat loss (together with skin temperature and sweat rate) and that body mass determines the amount of heat producing tissues. However when sweat evaporation was limited, as e.g. in hot humid climates, this higher ratio would not be advantageous. In cold climates, greater the exposed surface area, greater the loss of heat and therefore energy. Humans in cold climates need to conserve as much energy as possible. A low surface area to mass ratio helps to conserve heat and will be advantageous in cold climate. In warm climates, the opposite is true. We will overheat quickly if we have a low surface area to mass ratio. Therefore, humans in warm climates need to have high surface area to mass ratios so as to help them lose heat. In a nutshell, it simply means there is a characteristic ratio of body surface area to body mass that generally correlates with climate. For example, Fur or Tutsi people of Africa (warm climate) release body heat more readily because their ratio is high. However, Eskimos and Inuit (cold climate) have a lower ratio and therefore retain body heat.
_
Greater the ratio of surface area to mass, advantageous in summer and disadvantageous in winter.
Lesser the ratio of surface area to mass, advantageous in winter and disadvantageous in summer.
_
Body surface area (BSA):
The human body is considered to be a cylinder with uniform heat generation and dissipation. The surface area over which the heat dissipation takes place is given by an empirical equation, called as Du Bois Equation. This equation expresses the surface area as a function of the mass and height of the human being.
_
Average BSA is generally taken to be 1.73 m² for an adult.
| Average BSA values | ||
| Neonate (Newborn) | 0.25 | m² |
| Child 2 years | 0.5 | m² |
| Child 9 years | 1.07 | m² |
| Child 10 years | 1.14 | m² |
| Child 12-13 years | 1.33 | m² |
| For men | 1.9 | m² |
| For women | 1.6 | m² |
_
All formula of BSA contains height and weight of an individual and therefore ratio of surface area to mass (weight) is more dependent on height than weight. So comparison of the height of two individual will roughly compare the ratios of surface areas to mass of the same two individuals irrespective of their weights. In other words, greater the height of an individual, greater will be his ability to dissipate heat.
__
Humidity and relative humidity (RH):
The term humidity describes the fact that the atmosphere does contain water vapor. The amount of humidity found in air varies depending on many factors. Absolute humidity on a volume basis is the mass of water in the unit volume of air. The most common units are grams per cubic meter. Absolute humidity ranges from 0 grams per cubic meter in dry air to 30 grams per cubic meter when the vapor is saturated at 30 °C. Relative humidity is defined as the ratio of the partial pressure of water vapor (in a gaseous mixture of air and water vapor) to the saturated vapor pressure of water vapor at a given temperature. In other words, relative humidity is the amount of water vapor in the air at a specific temperature compared to the maximum water vapor that the air is able to hold without it condensing, at that given temperature. Relative humidity is expressed as a percentage and is calculated in the following manner:
Where PG [H2O] is the partial pressure of water vapor in the given air; PS [H2O] is the partial pressure of the saturated water vapor at that temperature of the air; and RH is relative humidity at that temperature.
Note: In a gas mixture having water vapor e.g. air, the vapor pressure is synonymous with the partial pressure exerted by vapor. Since air contains predominantly nitrogen gas and oxygen gas, the atmospheric pressure of air is the sum total of partial pressures of nitrogen, oxygen, water vapor and partial pressures of other gases. Therefore the term ‘vapor pressure’ and ‘partial pressure of water vapor’ can be used interchangeably as far as air (atmosphere) is concerned.
_
In other words, Relative humidity (RH) is the amount of moisture in the air compared to what the air can “hold” at that temperature. When the air can’t “hold” all the moisture, then it condenses as dew. The dewpoint temperature is the temperature at which the air can no longer hold all of its water vapor, and some of the water vapor must condense into liquid water. The dew point is always lower than (or equal to) the air temperature. Relative humidity of 100% indicates the dew point is equal to the current temperature and the air is maximally saturated with water. Air with a relative humidity of 50% contains half of the water vapor it could hold at a particular temperature. The picture below shows concept of relative humidity (RH).
The yellow circle is the amount of water vapor, the air can maximally hold at that temperature and the blue circle is the amount of water vapor, the air is actually holding at that temperature.
_
The capacity of the air to hold moisture is proportional to ambient temperature; warm air can hold more moisture than cold air. Basically heat loss through sweating is inversely proportional to RH. So when we are in hot weather with warm air as in heat waves, higher RH will reduce efficiency of sweat mediated heat loss and therefore we are more prone to heat illness despite sweating. However, in a proscribed space e.g., a room, as warm air in it is cooled; the capacity of the air to hold moisture in that room thus decreases reducing RH. So the best thing to do in heat waves is to remain indoor in cool room.
_
Radiant temperature:
We all know air temperature but less known and equally important is mean radiant temperature. All objects emit radiant energy at a level proportional to their temperature. Thus, when we are in a room, we radiate out to all surfaces and objects and they radiate back. The mean radiant temperature is a measure of the radiative effects arising in a room from all objects and surfaces. Large cold surfaces such as cold walls or windows can greatly reduce the mean radiant temperature of a room, causing significant thermal discomfort. For example, a poorly insulated home has cold interior walls, and bodies within its rooms continually lose heat to these cold surfaces. To compensate, room air temperature must be raised significantly, even as high as 27 degree C, before occupants feel comfortable. The complex interaction of air temperature, mean radiant temperature, air velocity and humidity makes up the human thermal environment.
_
Heat wave:
The above picture shows temperature difference in Europe form the average during the European heat wave of 2003.
The heat wave as defined by the World Meteorological Organization is when the daily maximum temperature of more than five consecutive days exceeds the average maximum temperature by 5 Celsius degrees (9 Fahrenheit degrees), the normal period being 1961–1990. Temperatures that people from a hotter climate consider normal can be termed a heat wave in a cooler area if they are outside the normal climate pattern for that area. The term is applied both to routine weather variations and to extraordinary spells of heat which may occur only once a century. Severe heat waves have caused catastrophic crop failures, thousands of deaths from hyperthermia, and widespread power outages due to increased use of air conditioning. Near the summer solstice, long days & high sun would create warm conditions. In the summer, within an area of high pressure with little or no rain or clouds, the air and the ground easily heats to excess. A static high pressure area can impose a very persistent heat wave. A heat wave may be accompanied by high humidity increasing heat index (vide infra).
_
Recently torrid weather continued to bake North Indian plains as mercury soared over 46 deg C in parts of Rajasthan and Uttar Pradesh and the humidity oscillated between 25 per cent and 56 per cent. Such high ambient temperature would definitely initiate heat illnesses among people. When these unusually hot weather conditions last longer than 2 days, the number of heat illnesses usually increases. This is due to several factors, such as progressive body fluid deficit, loss of appetite (and possible salt deficit), buildup of heat in living and work areas, and breakdown of air-conditioning equipment. Therefore, it is advisable to make a special effort to adhere rigorously to the preventive measures during these extended hot spells (vide infra) and to avoid any unnecessary or unusual stressful activity. Sufficient sleep and good nutrition are important for maintaining a high level of heat tolerance.
_
Fever versus hyperthermia:
Fever is an elevation of body temperature that exceeds the normal daily variation and occurs in conjunction with an increase in the hypothalamic set point- for example, from 37 to 39 degree C. This shift of the set point from normothermic to febrile levels is similar to resetting of a thermostat in the AC of your home. On the other hand, hyperthermia means unchanged set point of hypothalamus in conjunction with an uncontrolled increase in body temperature that exceeds the body’s ability to lose heat. Hyperpyrexia is the temperature > 41.5°C (> 106.7°F) which can occur with severe infections, but more commonly occurs with central nervous system (CNS) hemorrhages or hyperthermia.
_
The above picture shows summary of the differences between hyperthermia, hypothermia, and fever.
Hyperthermia: Characterized on the left: Normal body temperature (thermoregulatory set-point) is shown in green, while the hyperthermic temperature is shown in red. As can be seen, hyperthermia can be conceptualized as an increase above the thermoregulatory set-point.
Hypothermia: Characterized in the center: Normal body temperature is shown in green, while the hypothermic temperature is shown in blue. As can be seen, hypothermia can be conceptualized as a decrease below the thermoregulatory set-point.
Fever: Characterized on the right: Normal body temperature is shown in green. It reads “New Normal” because the thermoregulatory set-point has risen. This has caused what was the normal body temperature (in blue) to be considered hypothermic.
_
It is important to distinguish between fever and hyperthermia. Hyperthermia can be rapidly fatal and characteristically does not respond to antipyretics. There is no rapid way to make this distinction. Hyperthermia is often diagnosed on the basis of events immediately preceding elevation of core temperature for example history of heat exposure and treatment with drugs that interfere with thermoregulation. In addition to clinical history, physical aspects of some forms of hyperthermia may alert the clinician. Hot, dry skin is a typical sign of hyperthermia. The skin may become red and hot as blood vessels dilate in an attempt to increase heat dissipation, sometimes leading to swollen lips. An inability to cool the body through perspiration causes the skin to feel dry. Other signs and symptoms vary depending on the cause. Antipyretics do not reduce elevated temperature in hyperthermia.
_
Heat stress:
“Heat stress” is the net (overall) heat burden on the body from the combination of the body heat generated while working, environmental sources (air temperature, humidity, air movement, radiation from the sun or hot surfaces/sources) and clothing requirements. In foundries, steel mills, bakeries, smelters, glass factories, and furnaces, extremely hot or molten material is the main source of heat. In outdoor occupations, such as construction, road repair, open-pit mining and agriculture, summer sunshine is the main source of heat. In laundries, restaurant kitchens, and canneries, high humidity adds to the heat burden. In all instances, the cause of heat stress is a working environment which can potentially overwhelm the body’s ability to deal with heat. Most people feel comfortable when the air temperature is between 20°C and 27°C and the when relative humidity ranges from 35 to 60%. When air temperature or humidity is higher, people feel uncomfortable. Such situations do not cause harm as long as the body can adjust and cope with the additional heat. Very hot environments can overwhelm the body’s coping mechanisms leading to a variety of serious and possibly fatal conditions.
_
The most widely used heat stress index is the wet bulb globe temperature (WBGT) index. The WBGT is a composite temperature used to estimate the effect of temperature, humidity, wind speed (wind chill) and solar radiation on humans. It is used by industrial hygienists, athletes, and the military to determine appropriate exposure levels to high temperatures. This method is the most accurate and practical way to evaluate the potential threat of heat related illness in industry.
_
In moderately hot environments, the body “goes to work” to get rid of excess heat so it can maintain its normal body temperature. The heart rate increases to pump more blood through outer body parts and skin so that excess heat is lost to the environment, and sweating occurs. These changes impose additional demands on the body. Changes in blood flow and excessive sweating reduce a person’s ability to do physical and mental work. When the environmental temperature rises above 30°C, it may interfere with the performance of mental tasks. Heat can also lead to accidents resulting from the slipperiness of sweaty palms and to accidental contact with hot surfaces. As a worker moves from a cold to a hot environment, fogging of eye glasses can briefly obscure vision, presenting a safety hazard.
_
Under conditions of high humidity, the evaporation of sweat from the skin is decreased and the body’s efforts to maintain an acceptable body temperature may be significantly impaired. These conditions adversely affect an individual’s ability to work in the hot environment. With so much blood going to the external surface of the body, relatively less goes to the active muscles, the brain, and other internal organs; strength declines; and fatigue occurs sooner than it would otherwise. Alertness and mental capacity also may be affected. Very high body temperatures may damage the brain or other vital organs directly. Several factors affect the body’s ability to cool itself during extremely hot weather besides humidity including old age, youth (age 0-4), obesity, fever, dehydration, heart disease, mental illness, poor circulation, sunburn, prescription drug use and alcohol use.
_
Gender difference of heat tolerance:
Several studies comparing the heat tolerances of men and women have concluded that women are generally less heat tolerant than men. While this difference seems to diminish when such comparisons take into account cardiovascular fitness, body size and acclimatization, women have a lower sweat rate than men of equal fitness, size and acclimatization. Laboratory experiments have shown that women may be more tolerant of heat under humid conditions, but slightly less tolerant than men under dry conditions.
_
Acclimatization:
Humans are, to a large extent, capable of adjusting to the heat. When a person moves from a cold climate to a hot climate, adaptive changes occur in their sweating mechanism. These are referred to as acclimatization. The maximum rate of sweating increases and its solute composition decreases. From 1 liter sweat production per hour in a non-acclimated individual, an acclimated individual can produce 2 liter of sweat per hour. This adjustment to heat, under normal circumstances, usually takes about 5 to 7 days, during which time the body will undergo a series of changes that will make continued exposure to heat more endurable. On the first day of work in a hot environment, the body temperature, pulse rate, and general discomfort will be higher. With each succeeding daily exposure, all of these responses will gradually decrease, while the sweat rate will increase. When the body becomes acclimated to the heat, the person will find it possible to perform work with less strain and distress. Gradual exposure to heat gives the body time to become accustomed to higher environmental temperatures. Heat disorders in general are more likely to occur among workers who have not been given time to adjust to working in the heat or among workers who have been away from hot environments and who have gotten accustomed to lower temperatures. Hot weather conditions of the summer are likely to affect the worker who is not acclimatized to heat. Be aware that any sudden change in temperature, such as an early summer heat wave, will be stressful to your body. You will have a greater tolerance for heat if you limit your physical activity until you become accustomed to the heat. If you travel to a hotter climate, allow several days to become acclimatized before attempting any vigorous exercise, and work up to it gradually.
_
Vulnerable population for heat illness:
Heat-waves and hot weather can kill and also aggravate existing health conditions. Health effects can appear in all age groups and as a result of a wide range of factors; however, some people are more at risk of heat-related illness and death than others.
1) Elderly population: A comprehensive literature review showed that the elderly (and the very elderly) constitute the largest defined group at risk of dying due to a heat-wave. Elderly people with dementia are particularly at risk. Ageing decreases tolerance to heat: thirst is sensed late, the sweating reaction is delayed and the number of sweat glands is reduced. The elderly often suffer from co-morbidity, physical and cognitive impairment and need to take multiple medications. Elderly persons are at increased risk for heat-related illnesses because of their limited cardiovascular reserves, preexisting illness, and use of many medications that may affect their volume status or sweating ability. In addition, elderly people who are unable to care for themselves are at increased risk for heatstroke, presumably because of their inability to control their environment.
_
2) Infants and children are sensitive to the effects of high temperatures because their metabolism differs from the metabolism in adults. They also rely on others to regulate their thermal environments and provide adequate fluid intake. Information and advice should thus be addressed to their carers. Infants and children are also at risk for heat illness due to inefficient sweating. Even though, infants & children have a greater ratio of body surface area to body mass as compared to adults, they are more vulnerable to heat illness due to inefficient sweating, higher metabolism and dependence on others for fluid intake.
_
3) Virtually all chronic diseases present a risk of death/illness due to heat and, since the elderly are more likely to have a chronic medical condition, this is another reason why they are at increased risk. Medical conditions where the evidence is strongest are psychiatric disorders, depression, diabetes, pulmonary, cardiovascular and cerebrovascular conditions. There are several reasons why people with chronic diseases are at increased risk during heat-waves.
A) Any disease that leads to an inability to increase cardiac output, such as cardiovascular disease, will increase the susceptibility to heatstroke and/or cardiovascular failure and death, as thermoregulation during severe heat stress requires a healthy cardiovascular system.
B) Peripheral vascular disease, often caused by diabetes or atherosclerosis, may increase the risk of severe heat illness, as it may be hard to increase the blood supply to the skin.
C) Diarrhoea or febrile illness, particularly in children, and pre-existing renal or metabolic diseases may increase the risk of heat-related illness and death because these may be associated with excessive fluid loss and dehydration.
D) Chronic diseases which affect the number and/or function of sweat glands, such as diabetes, scleroderma and cystic fibrosis, can increase the risk of hyperthermia and heatstroke. Psoriasis, burns and eczema can also affect heat illness.
E) Any disease or condition that confines someone to bed and reduces their ability to care for themselves or to leave home daily also increases the risk. This is because of a general reduction in the ability to make an appropriate behavioral response to heat.
The table below shows medical conditions which increases risk of dying in a heat wave.
_
4) Medications can also aggravate heat illness. The risk for heat-related illness and death may increase among people using the following drugs:
(A) Psychotropics, which affect psychic function, behavior, or experience (e.g. haloperidol or chlorpromazine);
(B) Medications for Parkinson’s disease, because they can inhibit perspiration;
(C) Tranquilizers such as phenothiazines, butyrophenones, and thiozanthenes;
(D) Diuretic medications or “water pills” that affect fluid balance in the body.
Many medications can directly affect the central and peripheral mechanisms of thermoregulation, namely the thermoregulatory centre or afferent and efferent pathways, sweating, cutaneous vasodilatation, and/or cardiac output and thereby affect heat elimination. A simple non-prescription cough/cold remedy containing anti-histaminic agent can reduce sweating due to its anticholinergic effect. Some medications place you at a greater risk of heatstroke and other heat-related conditions because they affect your body’s ability to stay hydrated and respond to heat. Be especially careful in hot weather if you take medications that narrow your blood vessels (vasoconstrictors), regulate your blood pressure by blocking adrenaline (beta blockers), rid your body of sodium and water (diuretics), or reduce psychiatric symptoms (antidepressants or antipsychotics). Additionally stimulants, such as amphetamines and cocaine, increase your body’s heat production, making you more vulnerable to heatstroke. Vasodilators, such as nitrates and calcium channel blockers, can theoretically cause low blood pressure in people who tend to be dehydrated during excessive heat exposure, particularly the elderly. Dehydration and changes in blood volume distribution can also increase medication toxicity and/or decrease the efficacy by influencing drug levels, drug kinetics and excretion and, hence the pharmacological activity. This includes drugs with a narrow therapeutic index. Finally, storage of drugs at high ambient temperatures can adversely affect their efficacy, as most manufactured drugs are licensed for storage at temperatures up to 25 °C. This is particularly important for emergency drugs used by practitioners including antibiotics, adrenalins, analgesics and sedatives.
_
5) It may be that socioeconomic status, including ethnicity, occupation and education, is linked to heat-related health effects as mainly shown in several studies from the United States. Social isolation may also indicate higher vulnerability to the health effects of heat and increased social contact may be a protective factor. The effects of social isolation or the role of social networks in coping with hazards is, however, no straightforward and requires further research. The existing information on possible linkages between social and socioeconomic indicators and heat–health effects may still show important indications as to which population groups to include in targeted interventions. Needless to say that poor people can not afford air-conditioning and even fans in many developing countries. Also, access to water is lacking among these poor people and therefore deaths due to heat illness are quite a reality among poor people.
_
6) Many occupations require people to work in hot conditions, irrespective of the weather, and need effective management systems for ensuring health and safety. Air temperature, radiant temperature, air velocity, humidity, clothing and activity are recognized as factors that interact to determine heat stress. Anyone having to work outside in hot weather without appropriate protection, particularly if this involves heavy physical activity, is at increased risk of suffering health effects from heat. Protective clothing, particularly for workers in the emergency services, may become a dangerous hazard. Therefore, certain occupational groups need to be informed about possible measures to prevent heat stress, how to recognize heat stress, heat exhaustion and heatstroke, and what to do.
_
7) Obese population: People who are overweight may be prone to heat sickness because of their tendency to retain more body heat.
_
8) Genetic response to heat stress: To some degree, the way your body responds to extreme heat is determined by genetics. Researchers believe that your genes may play a vital role in determining how your body will respond in extremely hot conditions.
_
Heat illness:
Heat illness means illness due to increased heat energy in our body manifested by increased core temperature without change in hypothalamic set-point. Increased heat energy in our body is due to increased heat gain and/or reduced heat loss. Our bodies have a natural mechanism of regulating the body temperature through sweat and emitting heat through skin. This mechanism helps our body temperature to stay normal. However, this mechanism may fail if our body is exposed to extreme conditions like high temperature and/or high humidity level. In such cases, the body fails to cool down and its temperature builds up to unnatural and harmful levels. This condition is called heat illness. Mild to moderate heat-related health problems include heat rash, heat tetany, heat oedema, heat syncope, heat cramps and heat exhaustion while severe heat illness means heat stroke. Heat illness can also occur with normal or subnormal ambient temperature by increased heat production in the body (e.g. physical exertion, metabolic conditions) or reduced heat loss from the body (e.g. high humidity, anticholinergic drugs).
_
1) Heat rash: Heat rash, also known as prickly heat, is a maculopapular rash accompanied by acute inflammation and blocked sweat ducts. The sweat ducts may become dilated and may eventually rupture, producing small pruritic vesicles on an erythematous base. Heat rash affects areas of the body covered by tight clothing. When profuse sweating is covered by tight clothing, sweat ducts get blocked. It is an itching rash in warm environment (itching usually responds to antihistamines). If prolonged, it can develop into chronic dermatitis or a secondary bacterial infection. Treatment includes staying in cool environment and frequent showers. Keep affected area dry. It is advisable to wear loose-fitting clothing in the heat to prevent hear rash.
_
2) Heat tetany (hyperventilation and heat stress) is usually related to short periods of stress in intense heat environments. Symptoms may include hyperventilation, respiratory problems, numbness or tingling, or muscle spasms. Hyperventilation leads to hypocapnia, and hypocapnia leads to respiratory alkalosis, and alkalosis causes increased binding of calcium to albumin, thus decreasing free calcium despite normal total calcium level in blood. Treatment includes removing the affected person from the heat and slowing the breathing pattern.
_
3) Heat cramps are muscle contractions, usually in the gastrocnemius or hamstring muscles (muscles at the back of the calves or thighs). These contractions are forceful and painful. Heat cramps are muscle spasms that result from loss of large amount of salt and water through exercise. Besides calf muscles, heat cramps are associated with cramping in the abdomen and arms. Frequently, they don’t occur until sometime later, especially at night or when relaxing. Heavy sweating causes heat cramps, especially when the water is replaced without replacing salt. The mechanism is considered to be extra-cellular sodium depletion as a result of persistent sweating, exacerbated by replacement of water but not salt. Although heat cramps can be quite painful, they usually don’t result in permanent damage. Gently massage or apply pressure to cramping muscles. Symptoms usually respond rapidly to rehydration with oral rehydration salts or intravenous normal saline. In order to prevent them, one may drink electrolyte solutions such as sports drinks during exercise.
_
4) Heat edema: Heat edema presents as a transient swelling of the hands, feet, and ankles and is generally secondary to increased aldosterone secretion, which enhances sodium & water retention. When combined with peripheral vasodilatation and venous stasis, the excess fluid accumulates in the dependent areas of the extremities. The heat edema usually resolves within several days after the patient becomes acclimated to the warmer environment. No treatment is required, although wearing support stocking and elevating the affected legs with help minimize the edema. Diuretics are not indicated.
_
5) Heat syncope: Heat syncope is related to heat exposure that produces orthostatic hypotension. This hypotension can precipitate a near-syncopal episode. Heat syncope is believed to result from intense sweating, which leads to dehydration, followed by peripheral vasodilatation and reduced venous blood return in the face of decreased vasomotor control. The patient should be brought into a cool room and given supine position with elevated legs to increase venous return. Management of heat syncope consists of cooling and rehydration of the patient using oral rehydration therapy (sport drinks) or isotonic IV fluids. People who experience heat syncope should avoid standing in the heat for long periods of time. They should move to a cooler environment and lie down if they recognize the initial symptoms. Wearing support stockings and engaging in deep knee-bending movements can help promote venous blood return.
_
6) Heat exhaustion: Heat exhaustion occurs with prolonged exertion in hot and humid weather, profuse sweating and inadequate salt & water replacement. There is an elevation of core temperature between 37 to 40 degree C. Heat exhaustion is considered by experts to be the forerunner of heat stroke. It may even resemble heat stroke, with the difference being that the neurologic function remains intact. Heat exhaustion is marked by excessive dehydration and electrolyte depletion. Symptoms may include headache, nausea, vomiting, dizziness, malaise, and myalgia. Heat exhaustion is caused by the loss of large amounts of fluid by sweating, sometimes with excessive loss of salt. A worker suffering from heat exhaustion still sweats but experiences extreme weakness or fatigue, giddiness, nausea, or headache. The clinical signs include heavy sweating, rapid breathing and a fast, weak pulse. The skin is clammy and moist, the complexion is pale or flushed, and the body temperature may be occasionally normal or only slightly elevated. So normal body temperature (due to profuse sweating) does not rule out heat exhaustion. In most cases, treatment involves having the victim rest in a cool place and drinks plenty of oral rehydration solutions or intravenous normal saline. Up to 5 liters of positive fluid balance is required in first 24 hours. Victims with mild cases of heat exhaustion usually recover spontaneously with this treatment. Those with severe cases or with high core temperatures need active evaporation cooling using tepid sprays and fanning. There are no known permanent effects. Untreated, heat exhaustion may progress to heat stroke.
_
7) Heat stroke means core body temperature of greater than 40 °C (104 °F) due lack of thermoregulation (vide infra). This is distinct from fever, where there is a physiological increase in the temperature set point of the body.
_
First aid to victims of heat illnesses:
_
| Condition | Symptoms | First Aid |
| Sunburn | Skin redness and pain, possible swelling, blisters, fever, headaches | Take a shower using soap to remove oils that may block pores, preventing the body from cooling naturally. Apply dry, sterile dressings to any blisters, and get medical attention. |
| Heat Cramps | Painful spasms, usually in leg and abdominal muscles; heavy sweating | Get the victim to a cooler location. Lightly stretch and gently massage affected muscles to relieve spasms. Give sips of up to a half glass of cool water every 15 minutes or sports drink. (Do not give liquids with caffeine or alcohol.) Discontinue liquids, if victim is nauseated. |
| Heat Exhaustion | Heavy sweating but skin may be cool, pale, or flushed. Weak pulse. Normal body temperature is possible, but temperature will likely rise. Fainting or dizziness, nausea, vomiting, exhaustion, and headaches are possible. | Get victim to lie down in a cool place. Loosen or remove clothing. Apply cool, wet clothes. Fan or move victim to air-conditioned place. Give sips of water if victim is conscious. Be sure water is consumed slowly. Give half glass of cool water every 15 minutes. Discontinue water if victim is nauseated. Seek immediate medical attention. |
| Heat Stroke ( a medical emergency) |
High body temperature (105+); hot, red, dry skin; rapid, weak pulse; and rapid shallow breathing. Victim will probably not sweat unless victim was sweating from recent strenuous activity. Possible unconsciousness. | Get the victim to a hospital immediately. Delay can be fatal. Move victim to a cooler environment. Removing clothing. Try a cool bath, sponging, or wet sheet to reduce body temperature. Watch for breathing problems. Use extreme caution. Use fans and air conditioners. No fluid by mouth. |
_
Heat stroke (HS):
Heat stroke is the most severe form of the heat-related illnesses and is defined as a core body temperature higher than 40°C (104°F) associated with neurologic dysfunction due to lack of thermoregulation. Heat stroke becomes commonplace during periods of sustained high temperature and humidity. Sweating is absent from 84%–100% of those affected. Two forms of heat strokes exist.
1) Exertional heat stroke (EHS) generally occurs in young individuals who engage in strenuous physical activity for a prolonged period of time in a hot environment. EHS can happen in young people without health problems or medications, most often in athletes and military recruits. EHS results from increased heat production, which overwhelms the body’s ability to dissipate heat.
2) Classic heat stroke or nonexertional heat stroke (NEHS) more commonly affects sedentary elderly individuals, persons who are chronically ill and very young persons. NEHS occurs during environmental heat waves and is more common in areas that have not experienced a heat wave in many years. Classic heat stroke occurs because of failure of the body’s heat dissipating mechanisms. Substances that inhibit cooling and cause dehydration such as alcohol, caffeine, stimulants, medications, and age related physiological changes predispose to so-called “classic” heat stroke (NEHS). The chronically ill and elderly are often taking prescription medications (e.g., diuretics, anticholinergics, antipsychotics, and antihypertensives) that interfere with the body’s ability to dissipate heat.
_
Both types of heatstroke are associated with a high morbidity and mortality, especially when therapy is delayed. A combination of the two types is frequently seen. Women are at lower risk of EHS probably due to lower muscle bulk, effects of estrogens and a lower threshold for activation of thermoregulatory reflexes. With the influence of global warming, it is predicted that the incidence of heatstroke cases and fatalities will also become more prevalent. Because behavioral responses are important in the management of temperature elevations, heat strokes may be entirely preventable.
_
Pathophysiology of heat stroke:
Despite wide variations in ambient temperatures, humans and other mammals can maintain a constant body temperature by balancing heat gain with heat loss. When heat gain overwhelms the body’s mechanisms of heat loss, the body temperature rises, and a major heat illness ensues. Excessive heat denatures proteins, destabilizes phospholipids and lipoproteins, and liquefies membrane lipids; leading to cardiovascular collapse, multiorgan failure, and ultimately death. Generally speaking, heat directly influences the body on a cellular level by interfering with cellular processes along with denaturing proteins and cellular membranes. In turn, an array of inflammatory cytokines and heat shock proteins (HSPs) (HSP-70 in particular, which allows the cell to endure the stress of its environment) are produced. If the stress continues, the cell will succumb to the stress (apoptosis) and die. Certain preexisting factors such as age, genetic makeup, and the non-acclimated individual may allow progression from heat stress to heat stroke, multiorgan-dysfunction syndrome (MODS), and ultimately death. Progression to heatstroke may occur through thermoregulatory failure, an amplified acute-phase response, and alterations in the expression of HSPs. The exact temperature at which cardiovascular collapse occurs varies among individuals because coexisting disease, drugs, and other factors may contribute to or delay organ dysfunction. Full recovery has been observed in patients with temperatures as high as 46°C, and death has occurred in patients with much lower temperatures. Temperatures exceeding 106°F or 41.1°C generally are catastrophic and require immediate aggressive therapy.
_
Heat may be acquired by a number of different mechanisms. At rest, basal metabolic processes produce approximately 80 kcal of heat per hour or 1 kcal/kg/h. These mechanisms can raise the body temperature by 1.1°C/hr if the heat dissipating mechanisms are nonfunctional. Strenuous physical activity can increase heat production more than 10-fold to levels exceeding 800 kcal/h which necessitates a greater need for heat dissipation to prevent body becoming overheated. If both the ambient temperature and the humidity are high, it becomes difficult for the body to dissipate heat – and body temperature may rise. If body temperature becomes too high, hyperthermia may result. Similarly fever, shivering, tremors, convulsions, thyrotoxicosis, sepsis, sympathomimetic drugs, and many other conditions can increase heat production, thereby increasing body temperature. The body also can acquire heat from the environment through some of the same mechanisms involved in heat dissipation including conduction, convection, and radiation. These mechanisms occur at the level of the skin and require a properly functioning skin surface, sweat glands, and autonomic nervous system, but they also may be manipulated by behavioral responses. The efficacy of radiation as a means of heat transfer depends on the angle of the sun, the season, and the presence of clouds, among other factors. For example, during summer, lying down in the sun can result in a heat gain of up to150 kcal/h.
_
Maximum sweating in non-acclimated person is 1 liter per hour and in acclimated person is 2 liter per hour. The person at rest will generate heat of 1 kcal/kg/hr and the person doing significant physical exertion (exercise) will generate heat of 10 Kcal/kg/hr raising body temperature significantly, had no heat dissipation mechanism existed. But since sweating exists as heat dissipation mechanism, the amount of which is dependent on acclimatization, non-acclimated person doing exertion is most likely to be affected by heat illness and acclimated person at rest is least likely to be affected by heat illness, provided ambient temperature & relative humidity are same for both persons. Also, in dry environment & with maximum efficiency, sweating can maximally dispose of 604 Kcal of heat by evaporating 1 liter sweat in 1 hour and if a man having weight of 80 kg is doing strenuous work generating 800 Kcal heat per hour, he cannot dispose of extra-heat despite maximum sweating especially in hot weather when heat loss through convection & radiation is negligible. Such a person is vulnerable to heat illness despite adequate sweating, merely on the basis of strenuous work.
_
In a simplified model, thermosensors located in the skin, muscles, and spinal cord send information regarding the body temperature to the anterior hypothalamus, where the information is processed and appropriate physiologic and behavioral responses are generated. Physiologic responses to heat include an increase in the blood flow to the skin (as much as 8 L/min), which is the major heat-dissipating organ; dilatation of the peripheral venous system; and stimulation of the eccrine sweat glands to produce more sweat.
_
As the major heat-dissipating organ, the skin can transfer heat to the environment through conduction, convection, radiation, and evaporation. Radiation is the most important mechanism of heat transfer at rest in temperate climates, accounting for 65% of heat dissipation, and it can be modulated by clothing. At high ambient temperatures, conduction becomes the least important of the 4 mechanisms, while evaporation, which refers to the conversion of a liquid to a gaseous phase, becomes the most effective mechanism of heat loss. The efficacy of evaporation as a mechanism of heat loss depends on the condition of the skin and sweat glands, the function of the lung, ambient temperature, humidity, air movement, and whether or not the person is acclimated to the high temperatures. For example, evaporation does not occur when the ambient humidity exceeds 75% and is less effective in individuals who are not acclimated. Acclimatization to hot environments usually occurs over 7-10 days and enables individuals to reduce the threshold at which sweating begins, increase sweat production, and increase the capacity of the sweat glands to reabsorb sweat sodium, thereby increasing the efficiency of heat dissipation.
_
When heat gain exceeds heat loss, the body temperature rises. Classic heatstroke occurs in individuals who lack the capacity to modulate the environment (e.g., infants, elderly individuals, individuals who are chronically ill). Furthermore, elderly persons and patients with diminished cardiovascular reserves are unable to generate and cope with the physiologic responses to heat stress and, therefore, are at risk of heat stroke. Patients with skin diseases and those taking medications that interfere with sweating also are at increased risk for heat stroke because they are unable to dissipate heat adequately. Additionally, the redistribution of blood flow to the periphery, coupled with the loss of fluids and electrolytes in sweat, place a tremendous burden on the heart, which ultimately may fail to maintain an adequate cardiac output, leading to additional morbidity and mortality. Factors that interfere with heat dissipation include an inadequate intravascular volume, cardiovascular dysfunction, and abnormal skin. Additionally, high ambient temperatures, high ambient humidity, and many drugs can interfere with heat dissipation, resulting in a major heat illness. Similarly, hypothalamic dysfunction may alter temperature regulation and may result in an unchecked rise in temperature and heat illness.
_
Clinical manifestation of heat stroke:
Heat stroke is typically seen as hyperthermia exceeding 40°C and anhidrosis (no sweating) associated with an altered sensorium. However, when a patient is allowed to cool down prior to measurement of the temperature (as may occur during transportation in a cool ambulance or evaluation in an emergency department), the measured temperature may be much lower than 40°C, making the temperature criterion relative. Similarly, some patients may retain the ability to sweat, removing anhidrosis as a criterion for the diagnosis of heatstroke. Therefore, strict adherence to the definition is not advised because it may result in dangerous delays in diagnosis and therapy.
_
EHS is characterized by hyperthermia, diaphoresis ( profuse sweating), and an altered sensorium, which may manifest suddenly during extreme physical exertion in a hot environment. A number of symptoms (e.g., abdominal and muscular cramping, nausea, vomiting, diarrhea, headache, dizziness, dyspnea, weakness) commonly precede the heatstroke and may remain unrecognized. Syncope and loss of consciousness also are observed commonly before the development of EHS. EHS commonly is observed in young, healthy individuals (e.g., athletes, firefighters, military personnel) who, while engaging in strenuous physical activity, overwhelm their thermoregulatory system and become hyperthermic. Because their ability to sweat remains intact, patients with EHS are able to cool down after cessation of physical activity and may present for medical attention with temperatures well below 41°C. Despite education and preventative measures, EHS is still the third most common cause of death among high school students. Risk factors that increase the likelihood of heat-related illnesses include a preceding viral infection, dehydration, fatigue, obesity, lack of sleep, poor physical fitness, and lack of acclimatization. Although lack of acclimatization is a risk factor for heatstroke, EHS also can occur in acclimatized individuals who are subjected to moderately intense exercise. EHS also may occur because of increased motor activity due to drug use, such as cocaine and amphetamines, and as a complication of status epilepticus.
_
NEHS is characterized by hyperthermia, anhidrosis, and an altered sensorium, which develop suddenly after a period of prolonged elevations in ambient temperatures (i.e., heat waves). Core body temperatures greater than 41°C are diagnostic, although heatstroke may occur with lower core body temperatures. Numerous CNS symptoms, ranging from minor irritability to delusions, irrational behavior, hallucinations, and coma have been described. Anhidrosis due to cessation of sweating is a late occurrence in heatstroke and may not be present when patients are examined. Other CNS symptoms include hallucinations, seizures, cranial nerve abnormalities, cerebellar dysfunction, and opisthotonus. Patients with NEHS initially may exhibit a hyperdynamic circulatory state, but, in severe cases, hypodynamic states may be noted. Classic heatstroke most commonly occurs during episodes of prolonged elevations in ambient temperatures. It affects people who are unable to control their environment and water intake (e.g., infants, elderly persons, individuals who are chronically ill), people with reduced cardiovascular reserve (e.g., elderly persons, patients with chronic cardiovascular illnesses), and people with impaired sweating (e.g., patients with skin disease, patients ingesting anticholinergic and psychiatric drugs). In addition, infants have an immature thermoregulatory system, and elderly persons have impaired perception of changes in body and ambient temperatures and a decreased capacity to sweat.
_
Heat stroke symptoms include:
1) High body temperature. A body temperature of 104 F (40 C) or higher is the main sign of heatstroke.
2) A lack of sweating. In heat stroke brought on by hot weather, your skin will feel hot and dry to the touch. However, in heat stroke brought on by strenuous exercise, your skin usually feels moist.
3) Flushed skin. Your skin may turn red due to increased blood flow.
4) Rapid breathing. Your breathing may become rapid and shallow.
5) Racing heart rate and weak pulse. Your pulse rate may significantly increase because heat stress places a tremendous burden on your heart to help cool your body.
6) Headache. You may experience a throbbing headache.
7) Neurological symptoms. You may have seizures, lose consciousness, slip into a coma, hallucinate, or have difficulty speaking or understanding what others are saying.
8) Muscle cramps or weakness. Your muscles may feel tender or cramped in the early stages of heatstroke, but may later go rigid or limp.
_
Causes of heat stroke:
Increased heat production:
A) Increased metabolism
1) Infections
2) Sepsis
3) Encephalitis
4) Stimulant drugs: Stimulant drugs, including cocaine and amphetamines, can generate excessive amounts of heat by increasing metabolism and motor activity through the stimulatory effects of dopamine, serotonin, and norepinephrine.
5) Thyroid storm
6) Drug withdrawal
_
B) Increased muscular activity
1) Exercise: Strenuous exercise and status epilepticus can increase heat production 10-fold and, when uninterrupted, can overwhelm the body’s heat-dissipating mechanisms, leading to dangerous rises in body temperature.
2) Convulsions
3) Tetanus
4) Strychnine poisoning
5) Sympathomimetics
6) Drug withdrawal
7) Thyroid storm
_
Neuroleptic malignant syndrome and malignant hyperthermia:
Neuroleptic malignant syndrome (NMS) is a syndrome of hyperthermia, autonomic dysregulation, and extrapyramidal side effects caused by neuroleptic agents (e.g., haloperidol). Neuroleptic malignant syndrome appears to be caused by inhibition of central dopamine receptors in the hypothalamus, resulting in increased heat generation and decreased heat dissipation. NMS is basically an idiosyncratic reaction characterized by hyperthermia, altered mental status, muscle rigidity, and autonomic instability and appears to be due to excessive contraction of muscles. Malignant hyperthermia is a hyperthermic and systemic response to halothane and other inhalational anesthetics in patients with genetic abnormality. Malignant hyperthermia occurs in individuals with an inherited abnormality of skeletal-muscle sarcoplasmic reticulum that causes a rapid increase in intracellular calcium levels in response to halothane and other inhalational anesthetics or to succinylcholine. In contrast to heat stroke, malignant hyperthermia is believed to be induced by a decreased ability of the sarcoplasmic reticulum to retain calcium, resulting in sustained muscle contraction.
_
Decreased heat loss:
A) Reduced sweating
1) Dermatologic diseases
2) Drugs
3) Burns
_
B) Reduced CNS responses
1) Advanced age
2) Toddlers and infants
3) Alcohol
4) Barbiturates
5) Other sedatives
_
C) Reduced cardiovascular reserve
1) Elderly persons
2) Beta-blockers
3) Calcium channel blockers
4) Diuretics
5) Cardiovascular drugs that interfere with the cardiovascular responses to heat and, therefore, can interfere with heat loss.
_
D) Drugs
1) Anticholinergics
2) Neuroleptics
3) Antihistamines
_
E) Exogenous factors
1) High ambient temperatures
2) High ambient humidity
_
F) Reduced ability to acclimatize
1) Children and toddlers
2) Elderly persons
3) Diuretic use
4) Hypokalemia
_
G) Reduced behavioral responsiveness: Infants, patients who are bedridden, and patients who are chronically ill are at risk for heat stroke because they are unable to control their environment and water intake. To compound matters, co-morbidities and poly-pharmacy in the elderly can compromise their recovery.
_
Investigations in heat stroke:
Laboratory investigation of heat stroke include arterial blood gases with electrolytes, glucose, renal function tests, liver function tests, muscle enzymes, CBC, urinalysis etc. other tests include ECG, CT brain and chest radiograph.
_
Differential diagnosis:
Differential diagnosis of heat stroke includes delirium, delirium tremens, diabetic ketoacidosis, uremic encephalopathy, hepatic encephalopathy, hyperthyroidism, meningitis, Neuroleptic Malignant Syndrome, Malignant Hyperthermia, tetanus, cocaine toxicity, phencyclidine toxicity, salicylate toxicity, cerebral malaria etc. Each of these possible diagnosis have distinguishing features that may help to differentiate one from another. However, establishing the correct diagnosis is a challenge in the setting of an obtunded emergency patient who gives no history and where there may be limited access to any past medical or drug history.
_
What should lay people do if they see anybody with warning symptoms of heat stroke before hospitalizing him?
1) Get the victim to a shady area.
2) Cool the victim rapidly, using whatever methods you can. For example, immerse the victim in a tub of cool water; place the person in a cool shower; spray the victim with cool water from a garden hose; sponge the person with cool water; or if the humidity is low, wrap the victim in a cool, wet sheet and fan him or her vigorously.
3) Monitor body temperature and continue cooling efforts until the body temperature drops to 101-102°F.
4) Do not give the victim alcohol or coffee to drink.
5) Do not give the victim any fluids to drink as his consciousness is impaired resulting in aspiration of fluids.
6) Get medical assistance as soon as possible.
_
Medical treatment of heat stroke:
Heat stroke is a medical emergency. Rapid reduction of the core body temperature is the cornerstone of treatment because the duration of hyperthermia is the primary determinant of outcome. Except for the mildest cases, patients diagnosed with EHS or NEHS should be admitted to the hospital for at least 48 hours to monitor for complications. Once heatstroke is suspected, cooling must begin immediately and must be continued during the patient’s resuscitation. Controversy still exists over what therapeutic modality is most effective in the treatment of heatstroke; however, the basic premise of rapidly lowering the core temperature to about 39°C (avoid overshooting and rebound hyperthermia) remains the primary goal. Various studies have shown that the conduction method of cooling was found to be more efficacious in young, active adults with EHS. Removal of restrictive clothing and spraying water on the body, covering the patient with ice water soaked sheets, or placing ice packs in the axillae and groin may reduce the patient’s temperature significantly. The goal of treatment is to reduce the temperature by at least 0.2°C/min to approximately 39°C. Active external cooling generally is halted at 39°C to prevent overshooting, which can result in iatrogenic hypothermia.
_
Cold-water immersion (CWI) or Ice-water immersion is an extremely effective method of rapidly reducing core body temperature and traditionally was the most frequently recommended method. The increased thermal conductivity of ice water can reduce core body temperature to less than 39°C in approximately 20-40 minutes. The practice has been criticized recently. Theoretically, the ice water, which may be extremely uncomfortable to patients who are awake, can cause subcutaneous vasoconstriction, preventing the transfer of heat via conduction. Ice water also increases shivering, which in turn increases internal heat production. Other reasons for the recent criticisms include difficulty monitoring and resuscitating patients. This line of criticism has reached the medical community, including athletic trainers, team physicians, emergency department physicians, emergency medical technicians, registered nurses, first aid-trained coaches, and others. However, scientific evidence strongly refutes this criticism. Evidence from basic physiological studies looking at the effect of CWI on cooling rates in hyperthermic individuals and treatment of actual EHS victims clearly shows that CWI has cooling rates superior to any other known modality. Recently, evaporative techniques have been touted to be as effective as CWI techniques without the practical difficulties. However, data on the efficacy of this method are limited. Evaporative body heat loss may be accomplished by removing all of the patient’s clothes and intermittently spraying the patient’s body with tap water while a powerful fan blows across the body, allowing the heat to evaporate. A number of other cooling techniques have been suggested, but none has proven superior to or equal to cold-water immersion or evaporative techniques.
_
Various studies have shown that the cooling rates of hyperthermic individuals during CWI are consistently about 0.16 to 0.2°C/minute. A scientific study found that the cooling rates were nearly identical between ice-water immersion (5.15 ± 0.20°C) and cold-water immersion (14.03 ± 0.28°C) and the cooling rate is 0.16 ± 0.01°C reduction in core temperature every minute. It is far greater than reported cooling rates for other modes of cooling: passive cooling (0.054°C/min), 6 cold packs placed on large arteries of the neck, axillae, and groin (0.049°C/min), body covered with 24 to 48 cold packs (0.074°C/min), evaporative cooling in which water was splashed onto the body and evaporated by a compressed air spray (0.081°C/min), evaporative cooling plus 6 cold packs (0.086°C/min), and whole-body immersion at 25°C (0.075°C/min).
_
The results of various studies on cooling rates in humans and dogs by various methods are depicted in table below:
_
Monitor core temperature continuously by rectal probe as oral or tympanic membrane temperature may be inaccurate. If any treatments to lower your body temperature makes you shiver, your doctor may give you a muscle relaxant, such as a benzodiazepine. Shivering increases your body temperature, making treatment less effective. Supportive treatment includes oxygen, endotracheal intubation & assisted ventilation, replacement of fluids, electrolytes & glucose; judicious use of benzodiazepines, treatment of shock, treatment of rhabdomyolysis, ICU cares etc. If treated swiftly, 90% of people with heat stroke survive. If not, the survival rate is as low as 20% among vulnerable people such as the elderly. Complications of heat stroke may include renal and hepatic failure, disseminated intravascular coagulation, rhabdomyolysis and adult respiratory distress syndrome.
_
Antipyretics (e.g., acetaminophen [paracetamol], aspirin, and other nonsteroidal anti-inflammatory agents) have no role in the treatment of heat stroke because antipyretics interrupt the change in the hypothalamic set point caused by pyrogens. They are not expected to work on a healthy hypothalamus that has been overloaded, as in the case of heat stroke. In this situation, antipyretics actually may be harmful in patients who develop hepatic, hematologic, and renal complications because they may aggravate bleeding tendencies. Dantrolene has been studied as a possible pharmacological option in the treatment of hyperthermia and heatstroke, but at present, it has not been proven to be efficacious in clinical trials.
_
Heat waves, heat strokes and mortality:
Heat stroke is fatal in 10–50% of all cases and may lead to neurological morbidity in 20–30% of patients. Researchers say that the majority of heat-related deaths occur in urban areas where stagnant air and poor ventilation are common. It is still under-reported, as causes of death have been attributed instead to cardiovascular and respiratory diseases. Heat illness as an increased risk of death, was found among individuals with pre-existing illnesses, for example, heart disease, cerebrovascular disease, respiratory diseases, blood and metabolic/endocrine gland disorders, cardiopulmonary and genitourinary disorders. Heat stroke is the second leading cause of death among young athletes. An estimated 10,000 people perished in the 1980 United States heat wave and drought, which impacted the central and eastern United States. In the European heat wave of 2003, around 35,000 people died of it. Much of the heat was concentrated in France, where nearly 15,000 people died. Heat-related deaths and illness are preventable, yet annually many people succumb to extreme heat. In the United States, heat waves claim more lives each year than all other weather-related exposures combined (hurricanes, tornadoes, floods, and lightening). About 400 people in the US die from heat illnesses every year but if there’s a major heat wave, the number of deaths can increase to over 1500 people. In the UK, heat related mortality is estimated to be at around 40 cases per million population annually. The highest incidence of heat illness of 45 to 1300 per 100,000 population is reported from Saudi Arabia. The incidence can rise when customs or beliefs cause groups of people to be exposed to the heat for long periods of time such as Hajj, the annual Muslim pilgrimage in Saudi Arabia. The statistics of heat related mortality from developing countries of Africa and Asia is lacking but I assume it to be far greater than the U.S. In India, HS occurs frequently in areas of Northern and Western India but precise statistics is lacking.
_
Children and pets in cars:
If you ever park outside during the summer months, your car will heat up quickly. Heat coming in through the windows is absorbed by the interior, and the glass acts as an insulator. The temperature in your car get up to 200 degrees, depending on the temperature outside, the kind of vehicle you have, and how long it has been in the sun. Even in cool temperatures, cars can heat up to dangerous temperatures very quickly. The temperature can raise to 135 degrees in less than ten minutes, which can cause death to children or pets. Even with the windows cracked open, interior temperatures can rise almost 20 degrees Fahrenheit within the first 10 minutes. Anyone left inside is at risk for serious heat-related illnesses or even death. Children, elderly, or disabled individuals left alone in a vehicle are at particular risk of succumbing to heat stroke, even with windows partially open. As these groups of individuals may not be able to express discomfort verbally (or audibly, inside a closed car), their plight may not be immediately noticed by others in the vicinity. Pets are even more susceptible than humans to heat stroke in cars, as dogs (the animals usually involved), cats and many other animals cannot produce whole body sweat. Dogs cool themselves by panting and by sweating through their paws. If they have only overheated air to breathe, animals can collapse, suffer brain damage and possibly die of heat stroke. Non-guide dogs are prohibited from being brought into many establishments, and opening a vehicle window sufficiently may present an escape opportunity or bite hazard. Leaving the pet at home with plenty of water on hot days is recommended instead, or, if a dog must be brought along, tied up outside the destination and provided with a full water bowl. Always park car in the shade and use tinted window glass or place sunshades on the inside of the windshield. Never leave children, elderly, disabled and pets in a parked car even with windows partially open.
_
Working in hot environment:
From iron workers to pastry bakers, people work in a wide variety of hot or hot and humid environments. Being uncomfortable is not the major problem with working in high temperature and humidity. Workers who are suddenly exposed to working in a hot environment face additional and generally avoidable hazards to their safety and health. Certain safety problems are common to hot environments. Heat tends to promote accidents due to the slipperiness of sweaty palms, dizziness, or the fogging of safety glasses. Wherever there exists molten metal hot surfaces, steam, etc., the possibility of burns from accidental contact also exists. Aside from these obvious dangers, the frequency of accidents, in general appears to be higher in hot environments than in more moderate environmental conditions. One reason is that working in a hot environment lowers the mental alertness and physical performance of an individual. Increased body temperature and physical discomfort promote irritability, anger, and other emotional states which sometimes cause workers to overlook safety procedures or to divert attention from hazardous tasks.
_
People working in industry, military and first responders must wear Personal Protective Equipment (PPE) to protect themselves from hazardous threats such as chemical agents, gases, fire, small arms and even Improvised Explosive Devices (IEDs). This PPE can include a range of hazmat suits, firefighting turnout gear, body armor and bomb suits, among many other forms. Depending on its design, PPE often ‘encapsulates’ the wearer from a threat and creates what is known as a microclimate, due to an increase in thermal resistance and decrease in vapor permeability. As a person performs physical work, the body’s natural method of thermoregulation (i.e., sweating) becomes ineffective. This is compounded by increased work rates, high ambient temperatures and humidity levels, and direct exposure to the sun. The net effect is that protection from one or more environmental threats inadvertently brings on the threat of heat stress. In situations demanding prolonged wearing protective equipment, a personal cooling system is required as a matter of health and safety. A variety of active or passive technology-mediated personal cooling systems exist which can be categorized by their power sources and whether they are man or vehicle-mounted. For example, active liquid systems operate on the basis of chilling water and circulating it through a garment that cools the skin surface area that it covers through conduction. This type of system has proven successful in certain Military, Law Enforcement and Industrial applications.
_
Efforts to reduce heat stress in hot working environment:
1) Many industries have attempted to reduce the hazards of heat stress by introducing engineering controls, training workers in the recognition and prevention of heat stress, and implementing work-rest cycles.
2) Lessen work duration & frequency by providing adequate rest time. Take more breaks in extreme heat and humidity. Schedule heavy work during the coolest parts of day.
3) Providing cool rest areas in hot work environments considerably reduces the stress of working in those environments. Take breaks in the shade or a cool area when possible.
4) In the course of a day’s work in the heat, a worker may produce as much as 2 to 3 gallons of sweat. Because so many heat disorders involve excessive dehydration of the body, it is essential that water intake during the workday be about equal to the amount of sweat produced. Most workers exposed to hot conditions drink less fluid than needed because of an insufficient thirst drive. A worker, therefore, should not depend on thirst to signal when and how much to drink. Instead, the worker should drink 5 to 7 ounces of fluids every 15 to 20 minutes to replenish the necessary fluids in the body.
5) Heat acclimatized workers lose much less salt in their sweat than do workers who are not adjusted to the heat. The average American/Indian diet contains sufficient salt for acclimatized workers even when sweat production is high. If, for some reason, salt replacement is required, the best way to compensate for the loss is to add a little extra salt to the food. Salt tablets should not be used.
6) Clothing inhibits the transfer of heat between the body and the surrounding environment. Therefore, in jobs where the air temperature is lower than skin temperature, wearing clothing reduces the body’s ability to lose heat into the air. When air temperature is higher than skin temperature, clothing helps to prevent the transfer of heat from the air to the body. However, this advantage may be nullified if the clothes interfere with the evaporation of sweat. In dry climates, adequate evaporation of sweat is seldom a problem; protective clothing could be an advantage to the worker. However, during hot & humid climate, protective clothing may increase the risk of heat illness. Wear light-colored, loose-fitting, breathable clothing such as cotton. Avoid non-breathing synthetic clothing.
_
Sports and heat:
Although the condition is relatively rare, EHS incidence rate is as high as 1 in 1000 at some athletic events. Heat-related illnesses have claimed the lives of nearly 40 U.S. football players since 1995. It’s also important to be sensible about how much you exert yourself in hot weather. The hotter and more humid it is, the harder it will be for you to get rid of excess heat. The clothing you wear makes a difference too. The less clothing you have on, and the lighter that clothing is, the easier you can cool off. Football players are notoriously prone to heat illness, since football uniforms cover nearly the whole body, and since football practice usually begins in late summer when the temperature outside is highest. The majority of serious heat illness cases occur during the first four days of summer football practice, according to the American College of Sports Medicine. This is because most players aren’t used to the heat, are unprepared for the intensity of practice, and are not used to exerting themselves while wearing equipment.
_
Exercising in heat, for any population, places unusual demands on the human body’s thermoregulatory centers. Heat production during exercise is 10 to 15 times greater than at rest and is sufficient to raise core body temperature 1°C every 5 minutes if are no thermoregulatory adjustments. This generated heat, in addition to ambient heat from the external environment, must be offset by the body’s multiple mechanisms for heat dissipation to avoid hyperthermia. These cooling mechanisms include conduction, convection, evaporation and radiation. As ambient temperature rises above 20°C, the contributions of conduction, convection, and particularly radiation, become increasingly insignificant, with the bulk of heat dissipation in the patient resulting from evaporation as. In hot dry conditions, evaporation contributes for as much as 98% of dissipated heat. Anything that limits evaporation such as high humidity or dehydration will have profound effects on physiological function, athletic performance and risk for heat illness in the exercising patient. The athletic performance suffers considerably with even 2 to 3 % dehydration due to rise in core body temperature. Dehydration, with fluid loss occasionally as high as 6–10% of bodyweight, appears to be one of the most common risk factors for heat illness in athletes exercising in the heat. Core body temperature has been shown to rise an additional 0.15–0.2°C for every 1% of bodyweight lost to dehydration during exercise. To help prevent dehydration, consuming 400 to 600 ml (13 to 20 ounces) of cold water before exercising in the heat is recommended. The American College of Sports Medicine recommends approximately 250 ml of fluid (eight and one-half ounces) for every 10 to 15 minutes of activity.
_
Guidelines for sportsmen and athletes who are going to exert in heat:
1) Allow time for heat acclimatization. Increases in the duration or intensity of physical activity should be gradual. This process can take up to 14 days to complete.
2) Take breaks. Be sure to include adequate rest between exercise regimens.
3) Hydrate. Drink plenty of water or sports drinks before, during and after outdoor activities. Urine that is darker in color is a key warning sign of dehydration.
4) Time it right. Whenever possible, exercise during the early morning or late evening when the temperatures are cooler.
5) The highest risk for heat stroke occurs in the first few days of training in hot weather. The largest and fattest athletes are the most heat-sensitive.
6) Off the field, never skip meals, get plenty of fluids and salt, avoid alcohol, stay cool when you can, and get plenty of sleep.
7) After a workout, drink 1 liter of fluid for every pound of weight lost.
8) Know when to quit. Fever or other pre-existing illnesses can make a person more susceptible to heat related conditions.
_
An ice sock is a sock filled with ice, used by cyclists participating in long-distance rides to avoid overheating. A white athletic sock is filled with ice, which the cyclist drapes around his/her neck. This is a low-cost and effective method to keep the cyclist’s temperature in check and prevent overheating.
_
Sports drinks are beverages that may contain carbohydrates, minerals, electrolytes, and flavoring that intended to replenish water and electrolytes lost through sweating during exercise. Young athletes participating in vigorous, prolonged activities should be discouraged from using sports drinks outside of those activities because of their high caloric content. When not exercising, plain water and not commercial drinks, is the best source of hydration for children & adolescents according to an American Academy of Pediatrics report in ‘Pediatrics’.
_
Interaction between heat and air pollution:
Air pollution is often worse during a heat-wave. Because hot weather and air pollution often coincide, it can be difficult to separate the effects of the two exposures. Two main pollutants are particularly relevant during heat: ozone and PM10 (particulate matter with diameter under 10 microns). Ozone levels are highest outdoors, while PM10 also penetrates indoors. One possibility is that the effects of heat and air pollution are essentially equivalent to the effect of the two exposures occurring separately (an additive effect). Alternatively, it is plausible that there might be a greater than additive effect of simultaneous exposures to air pollution and heat (a synergistic effect). There is increasing evidence for a synergistic effect on mortality by co-existence of high temperatures and ozone concentrations. Several studies (from Europe, the United States and Canada) have found that the effects of ozone are higher during the summer. This may be explained by the higher ozone concentrations that occur during summer combined with a nonlinear response; or by a higher population exposure, as people spend more time outdoors in summer; or by an interactive effect. Similarly, the effects of heat-wave days on mortality are greater on days with high PM10 levels. The same was not found for other pollutants such as black smoke, NO2 (nitrogen dioxide) or SO2 (sulfur dioxide). The fact that, in contrast to ozone exposure, the interaction here seems to affect the elderly as well, might be explained by the high penetration of PM10 indoors. From these findings, it seems necessary that every effort should be made to keep levels of ozone and particulates as low as possible during hot weather and perhaps to integrate the monitoring and warning systems for air pollution with those for heat.
_
Chronic heat illness:
Certain kidney, liver, heart, digestive system, central nervous system and skin illnesses are thought by some researchers to be linked to long-term heat exposure. However, the evidence supporting these associations is not conclusive. Chronic heat exhaustion, sleep disturbances and susceptibility to minor injuries & sicknesses have all been attributed to the possible effects of prolonged exposure to heat. The lens of the eye is particularly vulnerable to radiation produced by red-hot metallic objects (infrared radiation) because it has no heat sensors and lacks blood vessels to carry heat away. Glass blowers and furnace-men have developed cataracts after many years of exposure to radiation from hot objects. Foundry workers, blacksmiths and oven operators are also exposed to possibly eye-damaging infrared radiation. In men, repeatedly raising testicular temperature 3 to 5°C decreases sperm counts. There is no conclusive evidence of reduced fertility among heat-exposed women. There are no adequate data from which conclusions can be drawn regarding the reproductive effects of occupational heat exposure at currently accepted exposure limits.
_
Sequelae (consequences) of heat stroke survivors:
It is widely believed that heat stroke leads only rarely to permanent deficits and the convalescence is almost complete. However, a study found the contrary. American researchers from the University of Chicago Medical Centre followed 58 subjects chosen from more than 3,000 patients with heat-related conditions who were admitted to Chicago area hospitals between July 12 and July 20, 1995. All 58 subjects experienced symptoms of near-fatal heat stroke. Each was interviewed at the time of their discharge from the hospital, with a follow up interview scheduled one year later. Almost a full quarter of the subjects died within the year; most of them within the first three months. All of the remaining survivors suffered some amount of brain and nervous system impairment. Approximately half were diagnosed with kidney problems and blood clots, while 10 percent of the group experienced malfunction of the lungs due to inflammation. After taking into account each subject’s health conditions before hospitalization, all of these side effects were judged to be a direct result of heat stroke. Perhaps the most significant finding was that age was not a factor among the subjects who died, in spite of the fact that the elderly are generally at greater risk of suffering heat stroke. Subjects ranged in age from 25 to 95, with the average age of the group being around 67. The study also recognized the fact that because of overcrowded conditions in all of the participating hospitals during this crisis, the immediate care – which is critical – was not as comprehensive as it should have been, underlining how important it is to quickly seek medical attention when the first signs occur.
_
Heat index (HI):
The heat index is a measure of how hot it feels based on temperature and humidity. The heat index is the “APPARENT TEMPERATURE” that describes the combined effect of high air temperature and high humidity. The higher this combination, the more difficult it is for the body to cool itself. If you work outdoors, it is critical that you remain aware of the heat index and take the appropriate precautions. Our bodies dissipate heat by varying the rate and depth of blood circulation, by evaporating water through the skin (sweat); and as a last resort, by hyperthermic hyperventilation (simulating panting) when blood is heated well above 98.6°F. Sweating cools the body through evaporation by using body heat as latent heat of water evaporation. However, high relative humidity retards evaporation, robbing the body of its ability to cool itself. When the relative humidity is high, the evaporation rate is reduced, so heat is removed from the body at a lower rate causing it to retain more heat than it would in dry air. Measurements have been taken based on subjective descriptions of how hot subjects feel for a given temperature and humidity, allowing an index to be made which relates one temperature and humidity combination to another at a higher temperature in drier air. When heat gain exceeds the level the body can remove, body temperature begins to rise, and heat related illnesses and disorders may develop. A heat index of 90°F or higher is risky and it is important to stay cool. The National weather service of every country will issue heat advisories or heat warnings based on the heat index. The chart below shows the HI that corresponds to the actual air temperature and relative humidity. (This chart is based upon shady, light wind conditions). Exposure to direct sunlight can increase the HI by up to 15°F. (Due to the nature of the heat index calculation, the values in the tables below have an error +/- 1.3F.)
_
Since high humidity reduces your body’s ability to get rid of excess heat by sweating, for a given air temperature, higher the humidity, higher the apparent temperature, or heat index. For example, if the air temperature is 86 degrees Fahrenheit (or 30 degrees Celsius), but the relative humidity is 50 percent, the apparent temperature will be about 88 degrees Fahrenheit (31 degrees Celsius). That may not sound like a huge difference… but if the humidity is 90 percent, the heat index will be 105 degrees Fahrenheit (40.7 degrees Celsius). In other words, your body will have to sweat as much to get rid of extra heat at 86 degrees Fahrenheit in 90 percent humidity as it would in a dry desert at 105 degrees Fahrenheit. People tend to feel most comfortable at a relative humidity of about 45 percent.
_
The formula for calculating heat index from ambient temperature and relative humidity is depicted below.
_
Remember, damp basement wall and floors, excessive boiling when cooking and laundry hung up to dry can cause high humidity in your home which can reduce efficiency of evaporative heat loss via sweating. Basement floors and walls should be treated with efficient waterproofing. Kitchen exhaust fan used while cooking is helpful. At least close kitchen door to the rest of house and open window slightly for ventilation. Windows in laundry room should be opened for ventilation when laundering or keep wet cloths outside home for drying. Bathroom door should be closed and window ventilation provided after hot showers. All these measures will reduce humidity in your home.
_
Educating people:
Education is the single most important tool for the prevention of heat stroke. The media, public education, public health programs, and athlete safety programs can play a pivotal role in increasing the public’s awareness of the dangers of heat during heat waves and advising the public on methods of remaining cool. Similarly, drinking fluids on schedule (and not based only on thirst), frequent cooling breaks, and frequent visits to air-conditioned places are very important because even short stays in an air-conditioned environment may drastically reduce the incidence of heatstroke. The best way to prevent dehydration is to observe color of urine. If urine is dark yellow, you are dehydrated. Keep on drinking fluids to maintain color of urine watery. Recognition of host risk factors and modification of behavior (e.g., limiting alcohol and drug intake and the use of medications and drugs that interfere with heat dissipation) and physical activity also will prevent heatstroke.
_
Recommendations for public during heat waves:
A) Keep your home cool:
During the day, close windows and shutters which are facing the sun and open those away from sun to let fresh air in. Open windows and shutters at night when the outside temperature is lower, if safe to do so. If your residence is air conditioned, close the doors and windows. Electric fans may provide relief, but when the temperature is above 35 °C, fans may not prevent heat-related illness. Use fan only when windows are open otherwise fan will circulate hot air around you. Air conditioning is the strongest protective factor against heat-related illness. Exposure to air conditioning for even a few hours a day will reduce the risk for heat-related illness. If you do not have air-conditioner at home, then, consider visiting a shopping mall or public library (having AC) for a few hours. People can reduce their risk for heat-related illness by spending time in public facilities that are air-conditioned. Have a plan for what to do if the power goes out.
_
B) Keep out of the heat.
If air-conditioning is not available, stay out of the direct sunshine. Move to the coolest room in the home, especially at night. Avoid going outside during the hottest time of the day. Schedule outdoor activities for cooler times of the day, before 10:00 AM and after 6:00 PM. If you must go outdoors, be sure to apply sunscreen 30 minutes prior to going out and continue to reapply according to the package directions. Sunburn affects your body’s ability to cool itself and causes a loss of body fluids. It also causes pain and damages the skin. Avoid strenuous physical activity during daylight hours in hot weather. Stay in the shade. It’s also a good idea to carry an umbrella. Do not leave children or animals in a parked vehicle (vide supra).
_
C) Keep the body cool and hydrated.
Take a cool shower or bath. If you’re outdoors and nowhere near shelter; soaking in a cool pond or stream also help bring your temperature down. Alternatives include cold packs and wraps, towels, sponging, foot baths, etc. Wear lightweight, loose fitting, light-colored clothes of natural materials. In environments that are not only hot but also humid, it is important to recognize that humidity reduces the degree to which the body can lose heat by evaporation. In such environments, it helps to wear light clothing such as cotton in light colors that is pervious to sweat but impervious to radiant heat from the sun. This minimizes the gaining of radiant heat, while allowing as much evaporation to occur as the environment will allow. Clothing such as plastic fabrics that are impermeable to sweat and thus do not facilitate heat loss through evaporation, can actually contribute to heat stress. Light-colored clothing fosters radiation because some light waves from the sun are reflected away from light surfaces. Darker colors absorb heat, so wearing dark colored clothing is not recommended during hot weather. If you go outside, wear a wide brimmed hat or cap and sunglasses. Wide-brimmed hats in light colors keep the sun from warming the head & neck and sunglasses block the powerful radiation from hurting the eyes. Also, vents on a hat will allow perspiration to cool the head. Drink regularly fluids. In hot weather people need to drink plenty of liquids to replace fluids lost from sweating. Thirst is not a reliable sign that a person needs fluids. A better indicator is the color of urine. A dark yellow color may indicate dehydration. It is debatable whether water or sports drinks are more effective to regain fluids; however, drinking only water without ingesting any salts may lead to a condition known as hyponatremia, or low sodium. By sweating and urination, humans lose salts, which need to be replaced along with fluids. However, average American/Indian diet contains excess salt and therefore salt replacement is not necessary in most cases. Do not take salt tablets because excessive sodium intake causes dehydration as it causes water to be drawn from the body’s cells. Orange juice is very good because it contains lot of potassium which is also lost in profuse sweating. Avoid drinks containing alcohol/ high-sugar/caffeine because they will actually cause you to lose more fluid through urine and may worsen dehydration. Also avoid very cold drinks, because they can cause stomach cramps. If your doctor generally limits the amount of fluid you drink or you are on diuretics, ask him how much you should drink while the weather is hot. Avoid hot foods and heavy meals—they add heat to your body. Even people that stay mostly indoors all day should drink at least 2 liters of water per day. Folks that spend time outdoors should drink 1 to 2 liters per hour that they are outdoors. People that do strenuous activity outdoors should be very careful- your body can lose up to 2 to 3 liters of water per hour during strenuous activity.
_
D) Get informed.
Listen to local news and weather channels or contact your local public health department during extreme heat conditions for health and safety updates.
_
E) Help others.
If you’re with someone who’s experiencing heat-related symptoms, cool the person by covering him or her with damp sheets or by spraying with cool water. Direct air onto the person with a fan. If anyone you know is at risk, help them to get advice and support. Elderly or sick people living alone should be visited at least daily. If the person is taking medication, check with the treating doctor how they can influence the thermoregulation and the fluid balance.
_
F) If you have a health problem:
Keep medicines below 25 °C or in the fridge (read the storage instructions on the packaging). Seek medical advice if you are suffering from a chronic medical condition or taking multiple medications.
_
G) If you or others feel unwell:
Try to get help if you feel dizzy, weak, anxious or have intense thirst and headache; move to a cool place as soon as possible and measure your body temperature. Drink some water or fruit juice to rehydrate. Rest immediately in a cool place if you have painful muscular spasms, most often in the legs, arms or abdomen, in many cases after sustained exercise during very hot weather. Drink oral rehydration solutions containing electrolytes. Medical attention is needed if heat cramps are sustained for more than one hour. Consult your medical doctor if you feel unusual symptoms or if symptoms persist. If one of your family members or people you assist presents with hot dry skin and delirium, convulsions and/or unconsciousness call the doctor/ambulance immediately. While waiting for the doctor/ambulance move him/her to a cool place and put him/her in a horizontal position and elevate legs and hips, remove clothing and initiate external cooling, such as with cold packs on the neck, axillae and groin, continuous fanning and spraying the skin with tepid water. Measure the body temperature. Do not give aspirin or paracetamol. Position unconscious person on his side.
_
“DO NOT” of heat illness:
1) DO NOT underestimate the seriousness of heat illness, especially if the person is a child, elderly, or injured.
2) DO NOT give the person medications that are used to treat fever (such as aspirin or acetaminophen [paracetamol]). They will not help, and they may be harmful.
3) DO NOT give the person salt tablets.
4) DO NOT give the person liquids that contain alcohol or high sugar or caffeine as they speed up dehydration. They will also interfere with the body’s ability to control its internal temperature.
5) DO NOT use alcohol rubs on the person’s skin.
6) DO NOT give the person anything by mouth (not even salted drinks) if the person is vomiting or unconscious.
_
How to avoid heat stroke in infants and children?
1) Never leave a child in a closed, parked vehicle, not even for a minute.
2) Make sure babies and children drink plenty of fluids. If you are thirsty, chances are your little ones could also use a beverage. Avoid beverages with caffeine, or a large amount of sugar.
3) Avoid bundling infants in heavy blankets or clothing. Like adults, babies need to air out in order to cool down.
4) During the hottest hours of the day, keep children indoors in an air-conditioned environment as much as possible. Families without air conditioning should pull shades over the windows and use room fans.
_
I have discussed in the prologue of this article how a G.P. misdiagnosed fever for heat illness.
A pro-active approach by GPs – What GPs should know and do:
1) Understand the thermoregulatory and haemodynamic responses to excessive heat exposure.
2) The most important point in arriving at the diagnosis of heat illness is high index of suspicion by G.P. and obtaining careful history regarding exposure to heat and/or strenuous exertion.
3) Understand the mechanisms of heat illnesses, their clinical manifestations, diagnosis and treatment.
4) Recognize early signs of heat stroke, which is a medical emergency.
5) Initiate proper cooling and resuscitative measures.
6) Be aware of the risk and protective factors in heat-wave-related illness.
7) Identify the patients at risk and encourage proper education regarding heat illnesses and their prevention; education of guardians of the old and infirm and infants is also important.
8) Include a pre-summer medical assessment and advice relevant to heat into routine care for people with chronic disease (reduction of heat exposure, fluid intake, medication etc).
9) Be aware of the potential side-effects of the medicines prescribed and adjust dose, if necessary, during hot weather and heat-waves.
10) Make decisions on an individual basis, since there are – according to current knowledge – no standards or formal advice for alteration in medications during hot weather.
11) Be aware that high temperatures can adversely affect the efficacy of drugs, as most manufactured drugs are licensed for storage at temperatures up to 25 °C; ensure that emergency drugs are stored and transported at proper temperature.
12) Be prepared to monitor drug therapy and fluid intake, especially in the old and infirm and those with advanced cardiac diseases.
_
It is interesting to know that even though our bodies need to be a warm 98.6 degrees F (37 deg C) to function properly, sitting in a room of 98.6 degrees F would for most of us, be extremely uncomfortable. This is so because our body consistently produces more heat than it requires to maintain core temperature and all the times we are losing heat through convection, radiation and sweat evaporation to environment. When room temperature is same as body temperature, heat loss through convection and radiation becomes nil and body gets heated up, making us feel uncomfortable.
_
Is AC really helpful to world?
Ensure that responses to heat-waves do not exacerbate the problem of climate change. This is an important and heat-wave-specific principle. It would be easy to assume that the solution is widespread use of air conditioning (AC) and there is little doubt that air conditioning can be protective for vulnerable populations. However, air conditioning is energy intensive and adds to greenhouse gas emissions; and there are many ways of adapting the environment & buildings, and protecting individuals that are not energy intensive. Also, air-conditioning exhaust is nothing but a very hot air and if thousands of ACs are working simultaneously, it will also increase environmental temperature. So air-conditioning on massive scale will contribute to global warming primarily by increasing green house gas emissions due to electricity consumption and secondary to warming environment directly through hot air emissions. The global warming leads to increases heat waves which leads to increased use of air-conditioning and consequently a vicious cycle is established due to air-conditioning on massive scale.
_
Can we do something to moderate summer heat through nature?
Picture below shows trees as Nature’s air-conditioner.
Higher temperatures are recorded in urban areas compared with rural areas due to roofs and asphalt pavements baked by the sun. Warmer air hovers above city rooftops and streets with fewer trees, extending upwards as much as a mile. These Urban “heat islands” cause heat illnesses and also consume tremendous electricity. Trees are the nature’s air-conditioner. Urban street trees help to cool cities by providing shade to lower surface air temperatures. Trees also release water into the air from their leaves – a process called “transpiration” which cools the air. Temperatures in the shade are 20 to 45°F cooler than un-shaded areas. Transpiration alone reduces peak summer temperatures by 2 to 9°F. Maintaining existing street trees and planting more are simple, cost-effective strategies to mitigate urban heat islands effects.
_
Heat stroke in trees?
I discussed trees as nature’s air-conditioner for humans but can trees themselves get heat stroke?
Heat stroke in trees means heat loads have been extreme and caused damage or death of trees. Hot temperatures can injure and kill living tree systems. A thermal death threshold is reached at approximately 115°F. The thermal death threshold varies depending upon the duration of hot temperatures, the absolute highest temperature reached, tissue age, thermal mass, water content of tissue, and ability of the tree to make adjustments to temperature changes. Trees dissipate heat by long-wave radiation, convection of heat into the air, and transpiration (water loss from leaves). Transpiration is a major mechanism for dissipation of tree heat loads. Trees can dissipate tremendous heat loads if allowed to function normally and with adequate soil moisture. However in extreme hot weather; many of the old, young, and soil-limited trees get damaged. The best treatment of heat stroke in trees is watering of trees. The best way to prevent heat stroke in trees is to plant native trees which are heat-resistant.
_
My theory of ‘simulated sweating’ for prevention of heat illness:
_
The small calorie or gram calorie (symbol: cal) approximates the energy needed to increase the temperature of 1 gram of water by 1 °C. This is about 4.2 joules. The large calorie, kilogram calorie, dietary calorie or food calorie (symbol: Kcal) approximates the energy needed to increase the temperature of 1 kilogram of water by 1 °C. This is exactly 1000 small calories or about 4.2 kilojoules (KJ). Assuming an adult human body is 80 kg in weight, having surface area of 1.7 square meters and having core temperature of 37 degree C. The specific heat of human body on average is 0.82 kcal/kg/ degree Celsius. So to raise temperature of 80 kg human body by 1 degree Celsius, it will need 65.6 Kcal energy equivalent to 275.52 kilo-joules of energy. In other words, it will need 3.44 Kilo-joules of energy per kilogram body weight to raise temperature of human body by 1 degree C. Conversely, if 275.52 kilo-joules of energy is taken out of 80 kg body through evaporation of sweat water, the body temperature will fall by one degree Celsius. In other words, you have to take out 3.44 kilo-joules/kg body weight of heat energy from human body to reduce body temperature by 1 degree C.
_
The sweat water is having temperature of 33 degree Celsius, same as that of skin surface. At normal atmospheric pressure, water boils at 100°C, and 419 kJ of energy are required to heat 1 kg of water from 0°C to its boiling temperature of 100°C. So to raise temperature of 1 kg water from 33 to 100 degree Celsius, it will need approximate 281 kilo-joules of energy. Another 2257 kJ of energy are required to convert 1 kg of water at 100°C into 1 kg of steam (latent heat of vaporization). So total 281 + 2257 = 2538 kilo-joules (604 Kilocalories) of energy required to vaporize 1 kg sweat from 33 degree C skin temperature to vapor. So when body loses 1 kg sweat from skin into vapor, 2538 kilo-joules of energy lost. [The evaporation of 1g/minute of sweat is equivalent to 42Watts]. Since 275.52 kilo-joules of energy taken out of 80 kg human will reduce body temperature by 1 degree Celsius; it amounts to 0.1085 kg of sweat evaporated. In other words, 108.5 ml of sweat evaporation can reduce body temperature by 1 deg C in 80 kg human. Since specific heat of body and energy required to vaporize sweat are constant, it would mean that about 1.36 ml of sweat evaporation per kg body weight is required to reduce body temperature by 1 degree Celsius. This is the magic figure for heat loss via sweating. The same magic figure can be arrived by direct calculations. Since specific heat of human body is 0.82 Kcal/Kg/Celsius and since 1 liter of evaporation of sweat causes loss of 604 Kcal of heat from body, it would come to evaporation of 1.36 ml of sweat per kg body weight to lose sufficient heat to reduce body temperature by 1 degree Celsius.
_
One example is sufficient. Your body weight is 60 kg, you are at rest and ambient temperature is 47 deg C. If there is no mechanism of heat dissipation and heat production is constant, your body temperature will rise at a rate of 4.4 degree C per hour. This is calculated from complex equations of heat transfer for convective heat (QC) and radiative heat (QR) in an ‘average person’ in the formula depicted below.
Where QC is heat transferred to body by convection in watts, QR is heat transferred to body by radiation in watts, AT is ambient temperature in Celsius and BT is body temperature in Celsius and V is speed of air surrounding skin in m/s.
QC + QR = total heat received by body from environment when ambient temperature is greater than body temperature.
_
If ambient temperature is 47 degree C and your temperature is 37 deg C, your body of 60 kg will receive 182 watts heat energy from environment through convection & radiation, which comes to 156 Kcal/ hour. Also, at the rate of 1 Kcal/kg/hr, your body of 60 kg will generate heat of 60 Kcal/hr from basal metabolism at rest. So the total heat gain of body is 156 + 60 = 216 Kcal/hr. Since your body weight is 60 kg and since specific heat of body is 0.82 Kcal/kg/C, it will need 49 Kcal to raise body temperature by 1 degree C; and hence 216 Kcal/hr will raise body temperature by 4.4 degree C every hour. So if you are 60 kg in weight and exposed to ambient temperature of 47 deg C, your core temperature will rise by 4.4 deg C every hour if you do not sweat. You need 1.36 ml sweat evaporation per kg body weight to reduce body temperature by 1 degree C. Hence you will need 359 ml of sweat evaporated every hour to maintain core temperature to 37 deg C. Remember, 359 ml of sweat evaporation is not the same as 359 ml of sweat secreted as all sweat never evaporate. Remember, speed of sweat evaporation depends on body surface area, relative humidity of environment and speed of air surrounding skin. Tall person will evaporate sweat faster than short person despite having same body weight because of large surface area of tall person. A well ventilated room with fan will evaporate sweat faster than a room without fan. The rate limiting step of sweat evaporation is relative humidity (RH). Sweat evaporation is inversely proportional to RH. At RH higher than 75 %, there will be negligible sweat evaporation.
_
Your body doesn’t know about the humidity; it produces sweat to regulate your temperature. You feel more sweat when it is humid because it doesn’t evaporate that fast, but you sweat as much when the air is dry. So the perception of sweating is higher in humid conditions but the cooling is less. The cooling effect of evaporation of sweat is greater the more completely sweat evaporates. When humidity is more, the evaporation of sweat is inhibited or blocked completely. The reason is that because air is already very saturated with water vapor, it can not hold more water vapor and therefore sweat can’t evaporate. Sweat that beads up and rolls off doesn’t function in the cooling process. However, this “futile sweat” does deplete the body of vital water and salt. As dehydration progresses cooling become more difficult. Performance drops and heat injury becomes a real threat. Deaths have occurred when the air temperature was less than 75 degrees F (24 degrees C) but the relative humidity (RH) was above 95%.
_
Now in the above example, ambient temperature is 47 degree C and as discussed before, warmer the air, greater is the humidity and therefore at such high ambient temperature, it is not uncommon to have humidity of about 60 % or more which will reduce efficiency of heat loss via sweating. Since efficiency of heat loss via sweating is reduced, thermo-receptors of skin will record higher temperature and through hypothalamus, further sweating is stimulated. So even though 359 ml of sweat is already secreted every hour, it is not enough, therefore you actually sweat far more than 359 ml every hour to maintain core temperature and even that will not work. You can not sustain such a sweating rate long and you can not maintain core temperature long and therefore your body will be gradually dehydrated and develop heat illness. However, if you have RH of 20 % or less, then majority of sweat will evaporate and core body temperature will be maintained provided you keep on replenishing fluids and electrolytes.
_
Speed of evaporation:
On a molecular level, there is no strict boundary between the liquid state and the vapor state. All liquids have a tendency to evaporate, and vice versa, all gases have a tendency to condense back to their liquid form. The vapor pressure of liquid is an indication of a liquid’s evaporation rate. It relates to the tendency of particles to escape from the liquid phase into vapor phase. A liquid with a high vapor pressure at normal temperatures is often referred to as volatile. Vapor pressure of liquid is the pressure of a vapor in thermodynamic equilibrium with its liquid phase in a closed system. We all know that water evaporates from ocean surface to form clouds in the sky. We all know that when water boils at 100 deg C, it is converted into vapor. Basic difference between evaporation and boiling is that evaporation is the vaporization that occurs at the surface of liquid while boiling is the vaporization that occurs throughout the liquid. Evaporation rates generally have an inverse relationship to boiling points; i.e. the higher the boiling point, the lower the rate of evaporation. Evaporation of water occurs at a temperature far below boiling point of water. On average, the molecules in a glass of water do not have enough heat energy to escape from the liquid. When the molecules collide, they transfer energy to each other in varying degrees, based on how they collide. Sometimes the transfer is so one-sided for a molecule near the surface that it ends up with enough energy to escape. For molecules of a liquid to evaporate, they must be located near the surface, be moving in the proper direction, and have sufficient kinetic energy to overcome liquid-phase intermolecular forces. Only a small proportion of the molecules meet these criteria, so the rate of evaporation is limited. Since the kinetic energy of a molecule is proportional to its temperature, evaporation proceeds more quickly at higher temperatures. As the faster-moving molecules escape, the remaining molecules have lower average kinetic energy, and the temperature of the liquid, thus, decreases. This phenomenon is also called evaporative cooling. This is why evaporating sweat cools the human body. The vapor pressure of a liquid (water) is defined as the pressure exerted by the molecules that escapes from the liquid to form a separate vapor phase above the liquid surface. Vapor pressure of water depends on temperature. Higher the temperature, greater is the kinetic energy of water molecules, greater is the collision of molecules, greater is the energy transferred to surface molecules, greater is the number of surface molecules escape from liquid phase into vapor phase and greater will be vapor pressure of water. So more water evaporates from ocean having 30 deg C surface temperature than having 20 deg C surface temperature. Of course at boiling point, at temperature of 100 deg C, vapor pressure of water will be equal to atmospheric pressure and hence all water will be converted into vapor. But below boiling point, the speed of evaporation of water depends on many factors, namely;
– Relative Humidity of the air
– Temperature of the air and the water
– Surface area of the water
– Velocity of air over the water
This is why sprays evaporate faster (large surface area), clothes dry faster on windy days (higher velocity of air), you feel hotter on a humid day (your sweat does not evaporate as easily) and you will see more steam from a hot cup of coffee than cold one (higher temperature).
_
A typical equation for the rate (speed) of water (sweat) evaporation in kg/second/square meter is:
(Pw-Pa) x (0.089 + 0.0782V)/Y
Where Pw is the vapor pressure of water at skin temperature, Pa is the partial pressure of vapor in air, V is the velocity of the air over the water (sweat) in m/s and Y is the latent heat of vaporization of water. Pressures should be in kPa. So, the speed of water (sweat) evaporation could be practically anything depending on these conditions. This is only one of the formulas but many others are also available but none of them are exact because there are plenty of variables in water evaporation and it is difficult to put down all variables in an equation form.
_
Most of the factors in the heat gain and/or heat loss are not under our control. We can not change high ambient temperature unless we plant trees on massive scale. When ambient temperature is higher than body temperature as in hot weather or heat waves, heat loss from body via convection & radiation is nil and in fact there may be heat gain instead of heat loss. We can not change relative humidity unless we buy a dehumidifier which will work in a close environment like home but useless outdoors. We can not change our body surface area. We can increase speed of air surrounding skin by fan but even that will not work if ambient temperature is > 35 deg C. We can not avoid going outdoor during summer as we need to work to earn livelihood. We can not reduce metabolic heat production because these metabolic processes are essential for survival. We have to take tablets for many co-existent illnesses for our well-being. Most of the middle class people in developing countries and all poor people can not afford air-conditioning. So the only factor left in our hand is to increase water intake so that sweat loss of water is compensated. As I doctor I can say that most of my patients can not drink more water even though they are warned of adverse consequences of dehydration. Most people can not drink 2 to 3 liter water in a matter of 2 to 3 hours when they are facing hot weather outdoor. So basically, in hot weather & heat waves, we are at the receiving end of a zero sum game.
_
The concept of simulated sweating is designed for middle class and poor class people who can not afford air conditioner, who do not have access to plenty of water and who are vulnerable to heat illness due to lifestyle & occupation. Simulated sweating is recommended when a person feels uncomfortable due to heat and/or when a person is likely to acquire heat illness.
_
Simulated sweating is similar to the evaporative technique used in management of heat stroke by spraying person’s body with tap water while a powerful fan blows across the body, allowing the heat to evaporate. This can be used by common people to prevent heat illness especially those who cannot afford air-conditioner. Just sit below fan unclothed and wet body surface with tap water. Body heat will evaporate water on skin and fan will circulate air around body to reduce humidity around skin surface because evaporated water from skin will form a layer of humid air around body which will prevent further evaporation. The fan will bring fresh air around skin and replace evaporated vapor containing air. Also, higher surrounding air velocity increases evaporative heat loss from the body. By this simple inexpensive way, most heat illness can be prevented during heat waves. The water on skin will work as simulated sweating and circulation of air around skin by fan will prevent humidity around skin surface to rise.
_
The same principle can be used to cool down your building in summer. Just throw water on terrace & walls, and as it evaporates, the building will cool down. The stronger the breeze, the faster the evaporation rate and the cooler you feel in your home.
_
Various studies have shown that in the dry environment and at a maximum efficiency, sweating can dissipate 604 kilocalories of energy per hour, requiring evaporation of about 1 liter of sweat in an adult. Even though you may be acclimated person producing 2 liters of sweat every hour, all sweat is never evaporated and a significant amount dribbles down the skin. An experienced marathon runner can evaporate more than 2 liter of sweat per hour but it is an exception and such physiological adaptation is not possible for common people. Hence 1 liter per hour or 16 ml per minute or 160 ml every 10 minutes is the maximum an adult human can evaporate by sweating.
_
Is simulated sweating more efficient in heat dissipation than natural sweating ?
Yes.
Simulated sweat is only water while natural sweat has salt dissolved in it. Sodium concentration in sweat is 30 to 65 mmol/l, depending on the degree of acclimatization. Higher the acclimatization, lesser the sodium concentration. Salt is what we call a nonvolatile substance. This means that it will not easily evaporate. Water is a slightly volatile substance, meaning that if left standing it will evaporate (go from the liquid to the gas phase).When we have pure water, there is nothing to prevent it from evaporating. That is, on the surface of the water there are only water molecules, and we know that evaporation takes place on the surface. When we have saltwater, the surface now contains both salt and water. Salt does not like to evaporate (because it is nonvolatile), so it will stay in the solution. The water will still evaporate, but not as quickly because now salt takes up part of the surface area at the top of the solution. Since the water molecules in salt water don’t have as much surface area to evaporate from as the water molecules in pure water, the water in salt water will take longer to evaporate. We can also look at the forces between the salt and water in saltwater. We call these as intermolecular forces and they result from the attraction of the positive and negative parts of a water molecule to the positive and negative ions in salt. Salt is made up of ions, which are just atoms with either a positive or negative charge. This charge comes about when an atom has more or less electrons than it does protons. Sodium and chloride ions make up salt, and when we put salt in water, these ions separate from each other (we call this dissociation) and the salt dissolves. The chloride ions, which are negatively charged, are attracted to the partial positive charge on the hydrogen atoms in a water molecule while the positively charged sodium ions are attracted to the partial negative charge on the oxygen atom in a water molecule. When the water in saltwater tries to evaporate it has a harder time because now it has sodium and chloride ions holding it back. Remember that salt doesn’t like to evaporate so it tries to keep the water in the solution, too. In order for the water in saltwater to evaporate it needs more energy than pure water, so it will take a longer time to evaporate. Pure water, on the other hand, does not have to worry about intermolecular forces with ions. It does have something we call “hydrogen bonding,” which is basically a weak force between the negative and positively charged parts of a water molecule, but hydrogen bonding is not as strong as the forces between the water and ions in saltwater. So in a nutshell, greater the salt content of water, lesser is the speed of evaporation. Therefore, the acclimated person who has sweat secretion with lower salt concentration evaporates sweat faster than non-acclimated person. Also, volume of sweat secretion is higher in acclimated person than non-acclimated person and so heat dissipation by acclimated person is far higher than non-acclimated person. Simulated sweat (water) has no salt in it as compared to natural sweat and therefore water evaporation rate and heat dissipation rate is higher with simulated sweating than natural sweating for the same volume. Also, the volume of simulated sweating is independent of any bodily factors while natural sweating is dependent on many factors including hydration of body. Therefore total heal loss by simulated sweating will always be more than natural sweating.
_
All you have to do is to apply 160 ml of tap or stored water (20 to 30 deg C) over your skin surface every 10 minutes (for adults) and let it evaporate under a fan. This will work just like sweating but without causing dehydration and electrolyte loss. Since 1.36 ml/kg of sweat evaporation reduces body temperature by 1 degree C, 160 ml of tap water evaporation will reduce body temperature by 2 degree C in 60 kg person and by 1.5 degree C in 80 kg person within 10 minutes. This cooling rate is possible only if all 160 ml of water is evaporated in 10 minutes but anything less will reduce cooling rate. Since the process can be repeated every 10 minutes, body temperature can be reduced by several degrees C in an hour. You should not apply more than 160 ml of water every 10 minutes as excess water will be wasted and not evaporated. Experts say that bath with cool water will help but I disagree. First, you need lot of water for bath which is not possible in many developing countries especially in summer when many wells go dry. Second, you take a bath for 10 minutes and then come out. So body is allowed to cool for 10 minutes and again back to square one. My technique uses only small amount of water every 10 minutes and therefore saves water. Also, cooling will continue as long as you wish till core temperature is brought to normal. Also, the technique will work when your sweating is blocked due to any reason including drugs & dehydration. Also, you do not have to drink plenty of water to replenish water loss from sweating. In fact, application of tap or stored water (20 to 30 deg C) on skin will reduce skin temperature to less than 30 deg C instantly, which will reduce hypothalamic drive for sweating and conserve water & electrolytes in body during heat waves & hot weather. In event, you do not have even a fan or electricity is unavailable, a piece of cardboard or newspaper or magazine can be used manually to circulate air around you. Before advent of electricity, people were using hand-held-fans in summer to evaporate sweat.
_
Common people with common sense would suggest why simulated sweating? Why not apply ice on skin? Evaporation of 1ml of water has been shown to dissipate seven times as much heat as melting 1gm of ice. This is because latent heat of water evaporation is seven times greater than latent heat of ice melting. So evaporation of water from skin in simulated sweating is far better than melting of ice on skin. Ice-water immersion for treatment of heat stroke is recommended because it is a medical emergency and we want to rapidly cool down core temperature to save life and such rapidity is achieved by conductive heat loss through contact with ice or ice-water. Simulated sweating is not for treatment of heat stroke but to prevent it. However, if ice or ice-water is not available, then simulated sweating can be used even for treatment of heat stroke. Simulated sweating will be inefficient to lose heat if relative humidity of air is very high.
_
Simulated sweating is different from tepid water (lukewarm water) sponging as in the case of high grade fever. During fever, tepid water sponging is done to cause vasodilatation of skin blood vessels so that heat is lost from skin through convection & radiation. On the other hand, during hot weather & heat waves, body tries to lose heat by vasodilatation of skin blood vessels but fails as ambient temperature is higher than skin temperature and therefore heat loss through convection & radiation is nil, and the only way to lose heat is to evaporate water from skin surface.
_
I strongly recommend simulated sweating for all people who are at the risk of heat illness especially sportsmen (athletes, footballers etc), elderly, persons suffering from chronic diseases taking various medications, children, workers in hot environments, and poor & middle class people living in hot environment especially in developing world. Instead of getting heat illness, better prevent it. The best way to prevent heat illness in hot weather & heat waves is by simulated sweating.
_
The moral of the story:
1) One of the most under-reported cause of death in the world is heat illness because majority of deaths due to heat illnesses are attributed to other co-existent diseases.
_
2) Heat illnesses are easily preventable and readily treatable.
_
3) Tips to avoiding heat illness include: rely not on thirst; drink water on schedule; favor sports drinks during exercise; monitor weight; watch urine color; shun caffeine, alcohol and high sugar beverages; stay out of the sun; check up on relatives and neighbors; and know the early warning signs of heat illness.
_
4) Ice-water immersion or cold-water immersion is the best method for rapid cooling of body in heat stroke.
_
5) There is a vicious cycle of air-conditioning on massive scale contributing to global warming, which in turn leads to heat waves, which leads to more air-conditioning.
_
6) Plant more native trees to increase transpiration (evaporation of water from leaves) to reduce ambient temperature.
_
7) Evaporation of 1.36 ml of sweat per kg body weight is needed to reduce body temperature by 1 degree Celsius.
_
8) The best way to prevent heat illness in hot weather & heat waves is simulated sweating. Soaking skin surface by 160 ml of tap or stored water (20 to 30 degree C) every 10 minutes in adults under fan in a well ventilated place is simulated sweating; which help cool down the body by losing heat through water evaporation to prevent heal illness especially in high risk populations and populations who can not afford air-conditioning. The cooling can be continued till the person feels comfortable and/or core temperature is brought down to 37 deg Celsius.
______________________________________________________________________________________
Dr. Rajiv Desai. MD.
June 13, 2011
_____________________________________________________________________________
Postscript:
Socio-economic factors are responsible for many diseases including malnutrition, infectious diseases, alcoholism, smoking and heat illnesses. When a patient comes to a doctor for treatment, the buck stops at a doctor but the buck should have stopped at government & media. In India, one third of population live below poverty line who do not have access to electric fan & sufficient water; and therefore vulnerable to heat illness. Every year, thousands die due to heat illness in India but neither government & media have any statistics of it nor are they concerned about it.


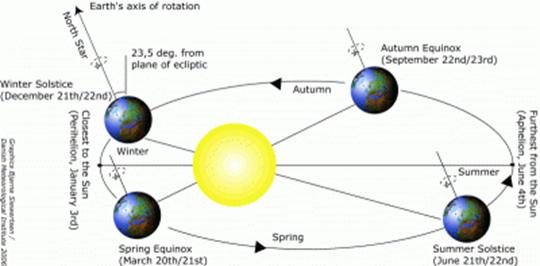
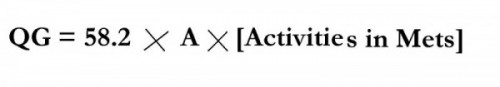

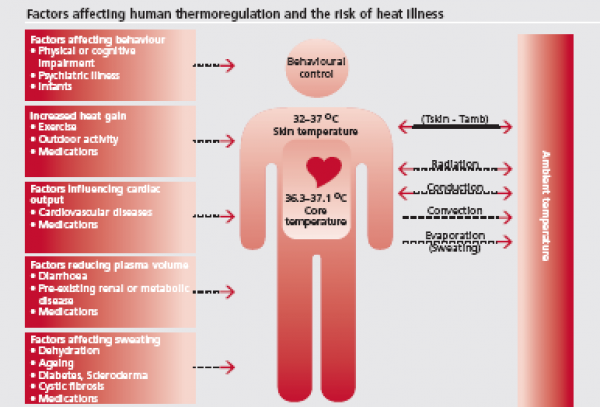
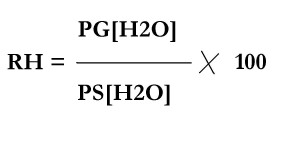
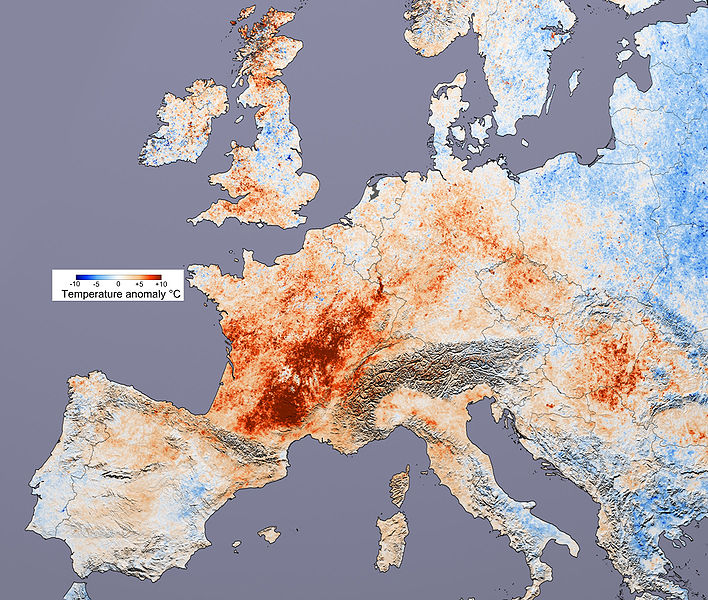
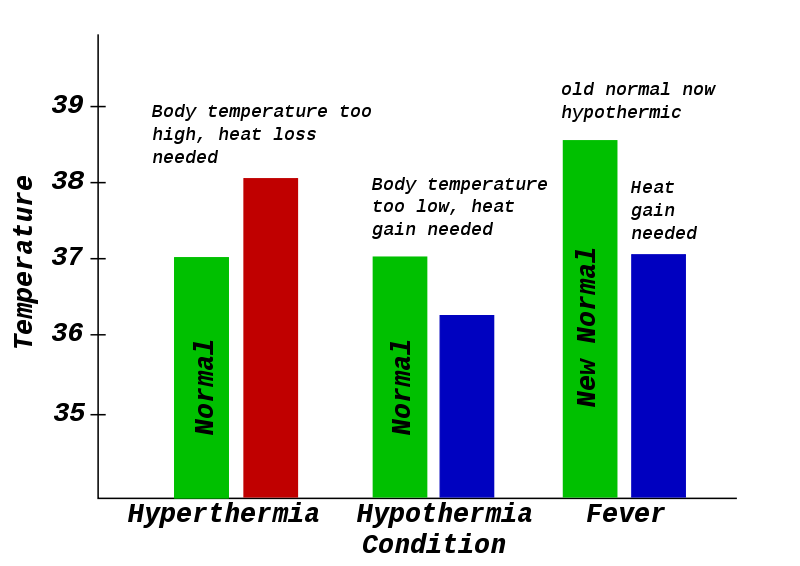
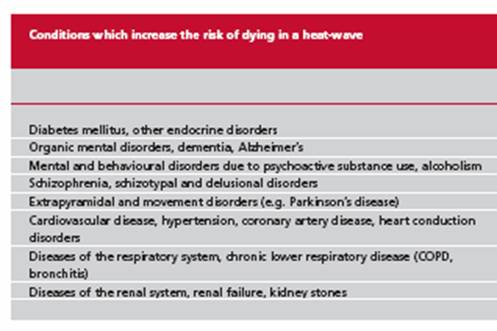



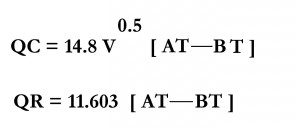
I am actually happy to read this website posts which carries lots of helpful facts, thanks for providing these kinds of data.|
Awesome article post.Really looking forward to read more. Keep writing.
Very good article.Really thank you! Keep writing.