Dr Rajiv Desai
An Educational Blog
SWEATING
SWEATING:
_____
_____
Prologue:
Sweating is an essential and natural biological process that starts soon after we are born. Sweat is a weak salt solution produced by the sweat glands of skin. These are distributed over the entire body but are most numerous on the palms and soles. Since the time of the ancient Greeks, the significance of sweating has been recognized, whereas our understanding of the mechanisms and controllers of sweating has largely developed during the past century. Heat dissipation is vital for our survival during exercise and heat stress. In humans, the primary mechanism of heat dissipation, particularly when ambient temperature is higher than skin temperature, is evaporative heat loss secondary to sweat secretion from sweat glands. Normally humans produce as much as one liter of sweat per day; however most of this evaporates as soon as it is produced so we don’t notice it. The body produces more sweat during exercise or in warmer environments in order to help cool us down. If a person exercised very hard in the heat they could produce up to 10 litres of sweat in a day. I have shown in my article ‘Heat Illness’ that evaporation of 1.36 ml of sweat per kg body weight is needed to reduce body temperature by 1 degree Celsius. Sweating is already discussed briefly in my articles ‘Heat Illness’, ‘Fever’ and ‘Clothing’. So what is the need to devote full article to sweating? In some people, the body’s mechanism for cooling itself is overactive — so overactive that they may sweat four or five times more than normal. When sweating is this extreme; it can be embarrassing, uncomfortable, anxiety-inducing, dangerous, and disabling. It often disrupts all aspects of a person’s life, from career choices and recreational activities to relationships, emotional well-being, and self-confidence. It can be associated with a significant quality of life burden from a psychological, emotional and social perspective. It has been called by some ‘the silent handicap’. Excessive sweat in the hands may make it impossible to play a musical instrument, allow handshake or pursue careers requiring contact with paper or electrical devices. Hands can be so sweaty that it becomes difficult to turn a doorknob or use a computer. On the other hand, biomarkers contained in sweat can give indications about the physical state of the body and these biomarkers can be accurately, non-invasively and continuously measured as an alternative to blood analysis. To discuss all these aspects of sweating, an entire article is needed.
________
Synonyms and abbreviations:
Euhirosis = normal sweating
Hyperhidrosis = abnormally excessive sweating
Hypohidrosis = abnormally reduced sweating
Anhidrosis = absent sweating
Axilla = armpit = underarm
Axillary = of armpit
Palmar = of hands
Plantar = of feet
ACh = acetyl choline
QSART = quantitative sudomotor axon reflex test
TST = thermoregulatory sweat test
ETS = endoscopic thoracic sympathectomy = video assisted thoracic sympathectomy (VATS)
ELS = endoscopic lumbar sympathectomy
BO = body odour
________
________
Human Skin:
Skin is not only the largest, but also, functionally, the most versatile organ of the human body. Human skin has complex properties and functions and is in a continuous change due to environmental, biochemical, and psychological factors. A vast amount of research has been published on different key functions of the skin, e.g. its barrier function or its role as a first-line immune response system. Although the regulation of body core temperature by sweating is one of these key tasks, comparatively few studies are available focussing on sweat glands or their biology.
_
Figure below shows schematically the human skin structure and important interactions with the environment.
_
The main functions of the skin are: protection (against mechanical, thermal, and chemical impacts, UV radiation, microorganisms etc.), repair and adaptation (self-healing and change in composition and structure when injured or exposed to stresses), sensation (through its mechanoreceptors, thermoreceptors and nociceptors) and temperature regulation (e.g. control of the sweating and perfusion rate). The skin is also responsible for the synthesis of vitamin D3 and the excretion of water, urea, ammonia and uric acid. Besides these functions, the appearance of the skin has important implications on social interaction providing information about the health, age, gender etc.
________
Heat generation and heat loss in humans and other animals:
_
Warm-blooded vs. cold blooded:
We humans are warm-blooded animals. In fact, with a few exceptions, all mammals and birds are warm-blooded, and all reptiles, insects, arachnids, amphibians and fish are cold-blooded. Warm-blooded creatures try to keep the inside of their bodies at a constant temperature. In other words, warm-blooded species tries to maintain core body temperature independent of environmental temperature. The human body has the remarkable capacity for regulating its core temperature somewhere between 98°F and 100°F when the ambient temperature is between approximately 68°F and 130°F. They do this by generating their own heat when they are in a cooler environment, and by cooling themselves when they are in a hotter environment. To generate heat, warm-blooded animals convert the food that they eat into energy. They have to eat a lot of food, compared with cold-blooded animals, to maintain a constant body temperature. Only a small amount of the food that a warm-blooded animal eats is converted into body mass. The rest is used to fuel a constant body temperature. Cold-blooded creatures take on the temperature of their surroundings. They are hot when their environment is hot and cold when their environment is cold. In hot environments, cold-blooded animals can have blood that is much warmer than warm-blooded animals. A cold-blooded animal can convert much more of its food into body mass compared with a warm-blooded animal. Mammals and birds require much more food & energy than do cold-blooded animals of the same weight.
_
When it comes to keeping cool, there are really three major mechanisms at play: evaporation, insulation, and metabolic regulation. Think of insulation like wearing white linen, or sitting under an umbrella on a sunny day. Animals that have adapted to living in desert climates, like camels, often develop thick coats of fur that serve to – perhaps counter-intuitively – prevent the transfer of heat from the environment to the animal. This occurs partially due to evaporative forces under the coat, and partially through reflection of direct sunlight. Metabolic regulation most of us are familiar with. It’s the urge to just lay around doing nothing on hot days. However, evaporative cooling is the method we’re most concerned with. During evaporation, water absorbs a tremendous amount of energy in order to break the powerful hydrogen bonds. In layman’s terms, it takes a lot of heat to make steam. Heat that gets used in the evaporative process is the heat dissipated by the body.
_
Heat generated by human body:
Out of total energy derived from food, about 20 percent is utilized for all metabolic processes and the remaining 80 percent is converted into heat to maintain the core temperature of human body. Irrespective of the work output, a human body continuously generates heat at a rate varying from about 100 Watts (e.g. for a sedentary person) to as high as 2000 Watts (e.g. a person doing strenuous exercise). Continuous heat generation is essential, as the temperature of the human body has to be maintained within a narrow range of temperature, irrespective of the external surroundings. The rate of metabolic heat production is primarily controlled by the rate of body activity. In general, the more physically active (physical exertion), the higher the metabolic rate and the higher metabolic rate will generate more heat which in turn will increase body temperature above normal unless extra-heat is dissipated.
_
Heat is exchanged with the environment by:
(1) Radiation occurs through electromagnetic waves in the form of infrared rays. At rest, radiation is the primary method of heat loss. Heat loss by radiation occurs by electromagnetic waves when someone is in an environment that is cooler than the body temperature. Therefore, if the ambient temperature is 60 deg F, and the body temperature is 98.6 deg F, the body radiates heat to the environment. No radiant heat gain or loss occurs when the temperature of surrounding objects is the same as the skin temperature (about 33°C).
(2) Convection occurs through water or air circulating across the skin. Convection is the process by which the body exchanges heat with the surrounding air. The body gains heat from hot air and loses heat to cold air which comes in contact with the skin. Convective heat exchange increases with increasing air speed and increased difference between air and skin temperature.
(3) By conduction, the body gains or loses heat when it comes into direct contact with hot or cold objects. It is a small amount as compared to other heat exchange modalities.
(4) By sweat evaporation:
_
Conduction, radiation and convection require a temperature gradient between the skin and its surroundings, and evaporation entails a water vapor pressure gradient. Excessive heat exposure constitutes a major stress for the organism. When environmental heat overwhelms the body’s heat-dissipating mechanisms, core temperature rises. An increase of less than 1 ºC is immediately detected by thermoreceptors disseminated through the skin, deep tissues and organs. The thermoreceptors convey the information to the hypothalamic thermoregulatory centre, which triggers two powerful responses to increase dissipation of heat: an active increase in skin blood flow and initiation of sweating (through cholinergic pathways). The cutaneous vasodilatation results in marked increases in blood flow to the skin and cardiac output, at the expense of other major systems. When the outdoor temperature is higher than the skin temperature, the only heat loss mechanism available is evaporation (sweating). Therefore, any factor that hampers evaporation, such as high ambient humidity, reduced air currents (no breeze, tight fitting clothes) or drugs with anticholinergic mechanisms, will result in a rise of body temperature that can culminate in life-threatening heatstroke or aggravate chronic medical conditions in vulnerable individuals. Evaporation proceeds more quickly and the cooling effect is more pronounced with high wind speeds and low relative humidity. In hot and humid workplaces, the cooling of the body due to sweat evaporation is limited by the capacity of the ambient air to accept additional moisture. In hot and dry workplaces, the cooling due to sweat evaporation is limited by the amount of sweat produced by the body. The body also exchanges small amounts of heat by breathing. Breathing exchanges heat because the respiratory system warms the inhaled air. When exhaled, this warmed air carries away some of the body’s heat. However, the amount of heat exchanged through breathing is normally small enough to be ignored in assessing the heat load on the body. Also, evaporation of insensible fluid from skin (trans-epithelial) & respiratory tract is also a mode of heat loss from the body each day but is not under regulatory control. Evaporation of sweat from the skin has a strong cooling effect, as we feel when we are sweaty and stand in front of a fan. On the other hand, if core body temperature falls below normal due to exposure to cold environment, this is also sensed by the hypothalamus and signals are sent to the cutaneous arteries (those supplying the skin) to constrict them. Warm blood is then retained deeper in the body and less heat is lost from the surface. If this is inadequate, then the brain activates shivering. Each muscle tremor in shivering releases heat energy and helps warm the body back toward its 37 degrees Celsius set point. In both cases, specialized neurons sense the abnormal body temperature and activate corrective negative feedback loops that return the temperature to normal. As a result, body temperature seldom goes more than 0.5 degrees Celsius above or below its set point.
_
Evaporative heat dissipation by sweating:
If part of a liquid evaporates, it cools the liquid remaining behind because it must extract the necessary heat of vaporization from that liquid in order to make the phase change to the gaseous state. It is therefore an important means of heat transfer in certain circumstances, such as the cooling of the human body when it is subjected to ambient temperatures above the normal body temperature. Because of the large heat of vaporization of water, the evaporation from a liquid surface is a very effective cooling mechanism. The human body makes use of evaporative cooling by perspiration to give off energy even when surrounded by a temperature higher than body temperature. When the ambient temperature is above body temperature, then radiation, conduction and convection all transfer heat into the body rather than out. Since there must be a net outward heat transfer, the only mechanisms left under those conditions are the evaporation of perspiration from the skin and the evaporative cooling from exhaled moisture.
_
The sweat water is having temperature of 33 degree Celsius, same as that of skin surface. At normal atmospheric pressure, water boils at 100°C, and 419 kJ (kilo-joules) of energy are required to heat 1 kg of water from 0°C to its boiling temperature of 100°C. So to raise temperature of 1 kg water from 33 to 100 degree Celsius, it will need approximate 281 kJ of energy. Another 2257 kJ of energy are required to convert 1 kg of water at 100°C into 1 kg of steam (latent heat of vaporization). So total 281 + 2257 = 2538 kilo-joules (604 Kilocalories) of energy required to vaporize 1 kg sweat from 33 degree C skin temperature to vapor. So when body evaporates 1 kg sweat from skin into vapor, 2538 kilo-joules/ 604 Kilocalories of energy lost. In other words, evaporation of 1g/minute of sweat is equivalent to 42Watts. Evaporation of 1 liter of sweat per hour means heat loss of 700 watts. As part of the physiological regulation of body temperature, the skin will begin to sweat almost precisely at 37°C and the perspiration will increase rapidly with increasing skin temperature. Guyton reports that a normal maximum perspiration rate is about 1.5 liters/hour, but that after 4 to 6 weeks of acclimatization in a tropical climate, it can reach 3.5 liters/hr! You would have to just sit around drinking constantly, just to keep from getting dehydrated! That maximum rate corresponds to a maximum cooling power of almost 2.4 kilowatts!
_
Lowering of body temperature occurs by process of heat loss via sweating and vasodilatation. Vasodilatation means blood vessels in periphery of body are dilated drawing away blood from internal organs to periphery (skin) promoting heat loss via skin. Vasodilatation can directly promote heat loss from skin by the processes of radiation, convection and conduction provided skin temperature is higher than ambient temperature. Skin blood flow can increase from approximately 0.2–0.5 L/min in normothermia to values exceeding 7–8 L/min hyperthermia. However, if the ambient temperature is higher than skin temperature, then, sweat evaporation is the only means of heat loss. The evaporation of sweat from skin takes away bodily heat promoting heat loss, thereby reducing temperature. So when you are exposed to hot environment, body maintains core temperature by vasodilatation and sweating. Heat produced by metabolic processes of body cannot be reduced in hot environment because these metabolic processes are essential for our survival.
_
Evaporation of 600 ml of insensible perspiration per day would lose 362 Kcal of heat in 24 hour but it occurs independently of heat regulation and maintenance of core body temperature. Therefore it is not considered along with evaporative cooling of body by sweating.
_
Sweating and humidity:
If air temperature is as warm as or warmer than the skin, blood brought to the body surface cannot lose its heat. Under these conditions, the heart continues to pump blood to the body surface, the sweat glands pour liquids containing electrolytes onto the surface of the skin and the evaporation of the sweat becomes the principal effective means of maintaining a constant body temperature. Sweating does not cool the body unless the moisture is removed from the skin by evaporation. Evaporation of sweat from the skin surface has a cooling effect due to the latent heat of evaporation of water. Hence, in hot weather, or when body heats up due to physical exertion, more sweat is produced. Typically, all of the sweat does not evaporate, but a part of it runs off your skin. After the sweat has been evaporated, the water vapor must move away from the skin in order that more evaporation can occur; which is dependent on speed of air movement around skin. The driving force for evaporation is the gradient of the water vapor pressure near the skin surface. Higher the humidity of air, greater will be vapor pressure in air, lesser will be the gradient of water vapor pressure at the skin surface and lesser will be sweat evaporation. Under conditions of high humidity, the evaporation of sweat from the skin is decreased and the body’s efforts to maintain an acceptable body temperature may be significantly impaired. During rainy season or conditions of high humidity, the relative humidity is on the higher side which means air cannot hold moisture further. In humid conditions where surrounding air cannot hold further water vapour, sweat evaporates slowly, if at all. As a result the body heats up and consequently we tend to sweat more. This explains why it feels so much hotter in high humidity. On the other hand, in a dry climate, evaporation happens very quickly, allowing a person to stay cooler. That’s why people talk about “a dry heat” being more pleasant, whereas when it’s hot and muggy (meaning humid), it’s far more miserable: there’s no way to cool off. In some dry areas, people even use what are called “swamp coolers” which consist of a fan blowing over filters that are constantly soaked with water. As long as water keeps being supplied, it can cool a house just by evaporation. They’re cheaper and use less power than a traditional air conditioner, but they only work in areas with dry air.
__
How does sweat cool the body even when the air is warmer than it?
Perspiration does not transfer heat to its surrounding air, at least not the kind of heat measurable by a thermometer. Rather, it absorbs the body’s heat and uses it to power the transformation of the moisture from liquid form into water vapor. The air will register increased humidity as the vapor is added to its composition, but it won’t increase in temperature. When the vapor later condenses back into liquid form, perhaps as dew or as part of a raincloud, all of this latent energy will be converted back into measurable heat and released into the environment. This state change requires a lot of energy – about 600 Kilocalories for each liter evaporated. By comparison, each Kcal contains enough energy to heat one liter of water by 1ºC. This means that every drop of water which evaporates absorbs enough energy to heat six drops from just above freezing to just under boiling! Evaporation requires the relative humidity of the air to be less than 100%; or, stated differently, the air’s temperature must be above the dew point, whereat vapor begins condensing into liquid form. If this condition is met, evaporation will occur regardless of whether a person’s environment is warmer or colder than their skin. The speed of sweat evaporation depends on many factors including relative humidity of air, speed of air over skin and temperature of skin & air. Evaporative heat loss by sweating would occur even if ambient temperature is lower than core body temperature although with lesser speed as lower ambient temperature will increase relative humidity of air.
___
Heat dissipation in animals:
In addition to higher primates (monkeys, apes and humans), horses are among the only other animals in the world that perspire profusely to evaporate heat through activating eccrine sweat glands —making them one of the few that could challenge humans in a marathon. Although sweating is found in a wide variety of mammals, relatively few (exceptions include humans and horses) produce large amounts of sweat in order to cool down. Non-primate mammals have eccrine sweat glands only on the palms and soles. Apocrine glands cover the rest of the body, though they are not as effective as humans’ in temperature regulation (with the exception of horses). Cats and dogs pant to cool by evaporation of water, while other species such as rodents have no physiological mechanism of thermoregulation and hence rely only on behavioral responses.
_
The hair of non-human mammals refers as “fur,” while humans are said to have hair, although hair and fur are chemically indistinguishable. One of the key differences between human hair and animal hair (fur) is the core of the hair follicle. In case of animals, the core allows for the coating of hair to provide excellent insulation from not only heat and cold, but also a fair amount of protection from rain as well. Along with these thermal regulating qualities, coarse nature of animal hair works as a great means of holding in cold or heat, as well as preventing rain and moisture. In contrast, human hair lacks this ability and does nothing to provide temperature regulation for the body. Fur is actually an insulator that serves as a barrier between the outside environment and the animal’s interior. It acts much like the vacuum barrier in a thermos. Thus in the winter the fur preserves the body heat and serves as a barrier to keep the cold out. In the summer it is a barrier to the outside heat. Unfortunately, in a continuously hot environment, once there is temperatures build up in the body, the fur then serves as an impediment to cooling since the heat then has a hard time dissipating through it.
_
Evaporative cooling is the only mechanism the warm blooded mammals have to reduce the body temperature especially if heat is produced in the body when undergoing physical actions or when the environmental temperature is much more than the body temperature. In those mammals where the body is covered by fur, panting is the major mechanism to cool the body. So sweating all over the body is found only in human beings as we have lost our fur during evolution and have only hair. Animals with few sweat glands, such as dogs, accomplish similar temperature regulation results by panting, which evaporates water from the moist lining of the oral cavity and pharynx. Panting is the primary avenue for evaporative heat loss in most non-sweating animals, dissipating as much as 95% of metabolic heat. Panting is dominated by an increased breathing frequency, with elevated evaporative heat loss occurring within the upper airways at frequencies as high as 200 breaths/min. Unlike sweating, panting requires the active participation of the animal involved to produce the air current. However for some animals, the mechanical energy required to pant can actually raise their core body temperature. At the same time, since the evaporation is occurring in the mouth, the act of panting acts locally to lower brain temperature. Another mechanism that dogs use to try to cool off in involves dilating or expanding blood vessels in their face and ears. If it is not too hot outside, this helps to cool the dog’s blood by causing it to flow closer to the surface of the skin. This mechanism works best if the overheating is due to exercise, rather than a high outside temperature.
_
Domestic animals have apocrine glands at the base of each hair follicle, but eccrine glands only in foot pads and snout. Their apocrine glands, like those in humans, produce an odorless oily milky secretion evolved not to evaporate and cool but rather coat and stick to hair so odor-causing bacteria can grow on it. Apocrine sweat of animals may contain pheromones for communication with other members of the species. Eccrine glands on their foot pads, like those on palms and soles of humans, did not evolve to cool either but rather increase friction and enhance grip.
________
The evolution of sweat glands:
Mammals have two kinds of sweat glands, apocrine and eccrine, which provide for thermal cooling. Researchers have rejected the suggestion that development of the eccrine gland occurred from the apocrine gland during the Tertiary geological period. The evidence strongly suggests that the two glands, depending on the presence or absence of fur, have equal and similar functions among mammals; apocrine glands are not primitive. However, there is a unique and remarkable thermal eccrine system in humans; researchers have suggested that this system evolved in concert with bipedalism and a smooth skin without fur. So loss of fur and walking on two legs coincided with thermal eccrine sweat gland system in humans. Humans aren’t the only animals with sweat glands, but we are one of the few species that produces large amounts of perspiration to cool off. While sweating might lead to awkward encounters on a hot day, some scientists think that it also gave us an evolutionary advantage. Daniel Lieberman, professor of Human Evolutionary Biology at Harvard University, argues that our ability to sweat let us run longer distances at faster speeds than other animals. This meant human could hunt game during the hottest parts of the day, when other predators were forced to rest. Other experts, such as anthropologist Nina Jablonski at Pennsylvania State University, say that sweating provided more efficient cooling that allowed us to evolve bigger, hotter brains.
______
______
Introduction to sweating:
_
Are sweating, perspiration and diaphoresis synonymous?
To perspire is to sweat. That’s the only definition. However, sweat has a lot of different meanings. One is in fact a synonym for perspire. “To expel through external pores.”
Sweat can also mean:
To condense atmospheric moisture:
1. To release moisture, as hay in the swath.
2. To ferment, as tobacco during curing.
Informal meaning:
1. To work long and hard.
2. To suffer much, as for a misdeed.
__
As nouns the difference between sweating and diaphoresis is that sweating is the production and evaporation of a watery fluid called sweat that is excreted by the sweat glands in the skin of mammals while diaphoresis is (physiology) perspiration, especially when profuse and medically induced.
_
Sensible and insensible perspiration:
There are two forms of perspiration: insensible perspiration and sensible perspiration. Insensible perspiration refers to the perspiration that happens before it is perceived or “sensed”. This is in contrast to sensible perspiration. Insensible perspiration occurs from both the skin (trans-epithelial) and respiratory tract as water vapor in expired air, and amounts to about 600 to 800 ml of water per day. It is not under regulatory control and accounts for the daily source of heat loss from the body. A small amount of sweat is continually excreted by the sweat glands in the skin. The portion that evaporates before it is observed may also be included by some as part of insensible perspiration. However to avoid confusion, any sweat secreted by sweat gland is perspiration. Sweating is perspiration. The term sensible perspiration ought to be deleted. The term insensible perspiration is obligatory water loss from skin (trans-epithelial) and respiratory tract. Even a small amount of sweat secreted round the clock which is not sensed by us is perspiration (sweating) and not insensible perspiration. The term insensible perspiration should be called obligatory evaporative water loss.
_
| Main Differences between Sweat and Insensible Water Loss | ||
| Sweat | Insensible Fluid | |
| Source | From specialised skin appendages called sweat glands | From skin (trans-epithelial) and respiratory tract |
| Solute loss | Yes, variable | None |
| Role | Body temperature regulation | Evaporation of insensible fluid is a source of heat loss from the body each day but is not under regulatory control. Cannot be prevented even if body wants to conserve heat. |
______
______
Definition of sweating:
Perspiration, also known as sweating is the production of fluids secreted by the sweat glands in the skin of mammals. Sweating is a function of the sweat glands which are present in the skin and widely distributed over the general body surface. Special microscopic glands (sweat glands) in the deep layer of the skin (the dermis) produce sweat by filtering fluid and salts out of the blood and secreting this fluid through small tubes in the skin (sweat ducts) that empty out into small pores at the top layer of the skin (the stratum corneum). Sweat glands are distributed over the entire body — except for the lips, nipples and external genital organs. The total number of sweat glands is somewhere between 2 and 4 million and only about 5% are active at the same time, indicating the enormous potential for sweat production. Three types of sweat glands can be found in humans: eccrine glands, apocrine glands and apoeccrine glands. The eccrine sweat glands are distributed over much of the body. In humans, sweating is primarily a means of thermoregulation, which is achieved by the water-rich secretion of the eccrine glands. Maximum sweat rates of an adult can be up to 2–4 liters per hour or 10–14 liters per day (10–15 g/min•m²), but is less in children prior to puberty. Evaporation of sweat from the skin surface has a cooling effect due to evaporative cooling. Hence, in hot weather, or when the individual’s muscles heat up due to exertion, more sweat is produced. “Normal” sweating can be as much as one liter of fluid per day, according to the National Institutes of Health (NIH, 2011). Children don’t start reaching those levels until puberty. We tend to sweat more in the afternoon than the morning because our metabolism increases over the course of the day generating heat. Lack of sweat or excessive sweating can cause problems. The absence of sweat can be dangerous because your risk of overheating increases. Excessive sweating may be more psychologically damaging than physically. About 3% of people say that they sweat excessively. Of course, we all sweat more when we are hot or anxious but excessive sweating may be partly caused by genes – 1 in 3 sufferers says that others in their family have the same problem. Sweating, accompanying hot flushes is common in women at the menopause. Occasionally, excessive sweating can signify a medical problem (such as an overactive thyroid gland). Antidepressant drugs can also cause sweating especially of the head and neck.
_
Apocrine glands are usually the culprits when it comes to most embarrassing sweating issues: Apocrine sweat glands, which are usually associated with hair follicles, continuously secrete a fatty sweat into the gland tubule. Emotional stress causes the tubule wall to contract, expelling the fatty secretion to the skin, where local bacteria break it down into odorous fatty acids. The fact that most of your apocrine glands are concentrated in your underarm region is why you only put deodorant under your arms and not all over your body. Your Eccrine glands, on the other hand, fire off when your body gets too hot and you need to cool down. Most of the wetness you feel when you work out or when you’re in a hot environment comes from these glands, but the there is much less odor.
_
Sweat is produced as a thermoregulatory response to heat, either from a rise in environmental temperature or endogenously from a rise in body temperature, e.g. during exercise. Evaporation of sweat from the skin causes cooling as long as the environmental humidity is not excessive. Thermoregulatory sweating occurs over the general body surface, while that which is associated with emotional states is seen mainly on the face, palms and feet. Sweating is a normal bodily function that serves to cool off and lubricate the skin, especially in areas that may rub against other areas of skin, such as under the arms, under the breasts, and between the legs. However, considerable differences in the sweating pattern, in response to various stimuli, are found between individuals. Sweating is abnormal when either too much (hyperhidrosis) or too little, or none (hypohidrosis or anhidrosis) is produced either generally or in particular regions of the body. Hypohidrosis is decreased sweating from whatever cause. Focal hyperhidrosis is increased or excessive sweating in certain regions such as the underarms, palms, soles, face or groin. Excessive sweating secondary to an underlying condition it is called secondary hyperhidrosis and usually involving the body as a whole (in which case it is called generalized hyperhidrosis). Hidromeiosis is a reduction in sweating that is due to blockages of sweat glands in humid conditions.
_
Sweat comes in two varieties: Active and passive:
Active sweating happens when you exercise, and it invigorates your body. Passive sweating, which has more of a therapeutic effect, happens when your core body temperature rises (usually because the air around you is hot, as in a traditional sauna or a steam room). The more advanced far infrared saunas are something else. They induce a passive sweat by heating the body directly, not just the air. In both active and passive sweating, your breath quickens, your circulation improves, and your metabolism speeds up. This combination of responses contributes to getting your body back to a normal temperature. In fact, temperature regulation is the most important benefit to sweating.
_______
The figure below shows sweating statistics:
_
Factors affecting sweating:
Besides hot weather, exercise and fever conditions, other factors affect sweating: People have an average of two to four million sweat glands. But how much sweat is released by each gland is determined by many factors, including gender, genetics, environmental conditions, age or your fitness level. A lot of it comes down to biological variation. If you examined two people—same height, sex and build—one might produce twice the volume of perspiration as the other. It could just be one person has more sweat glands. Everybody’s baseline is different, so it’s hard to say what amount of sweat is ‘healthy’.
1. Gender:
Men are sweatier than women, even when you take body size into account. Scientists tested volunteers in a laboratory mock-up of a sweltering car. Men lost 250 g of sweat per hour, which was 70 g more than the women. In general, males really do produce more sweat than females—approximately four times more per day. While both sexes have about the same number of sweat glands, because men are larger, they have more surface area to cool off, not to mention the hormonal variations that cause them to sweat more. A study published in the Journal of Experimental Physiology found that when physically fit men and women exercised intensely, the men produced more sweat—even though both sexes had the same number of active sweat glands. The study also followed unfit men and women and found that the unfit women perspired significantly less than their male counterparts. Women may be at a disadvantage when it comes to cooling off during heavy bouts of exercise or during hot conditions. Researchers have suggested an evolutionary reason for this: women carry less body fluid than men, and they may sweat less to prevent dehydration. For this reason, it may be advisable for women to take more precautions in extreme heat conditions or during long bouts of exercise.
2. Age:
Age-related factors can also affect the amount of sweat a person produces. As the skin changes during the aging process, the sweat glands produce less sweat. This can make it harder to cool off and may increase the risk of heat stroke.
3. Body Mass:
The higher a person’s body mass index (BMI), the more they sweat. If an individual weighs more, sweat rate is likely to increase because the body must exert more energy to function and there is more body mass to cool down.
4. Coffee, alcohol and smoking:
A hot coffee can encourage sweating. Caffeine has an effect on your central nervous system, causing you to sweat more. Caffeine, nicotine, and certain prescription drugs can stimulate the sweat glands. Alcohol increases your heart rate and dilates blood vessels in your skin, bringing blood to your skin’s surface. This in turn raises your skin temp, which can cause you to sweat more. Hot drinks raise your internal temperature, activating your body’s cooling mechanism.
5. Spicy Foods:
Eating spicy foods also triggers sweating. Spicy foods excite the receptors in the mucosa of the mouth that normally respond to heat. Those receptors are pain fibers, technically known as polymodal nociceptors… The central nervous system can be confused or fooled when these pain fibers are stimulated by a chemical, like that in chilli peppers, which triggers an ambiguous neural response. The central nervous system reacts to whatever the sensory system tells it is going on. Therefore, the pattern of activity from pain and warm nerve fibers triggers both the sensations and the physical reactions of heat, including vasodilation, sweating and flushing.
6. Fitness and sweating:
Over the past few decades, multiple studies have suggested that trained endurance athletes sweat sooner and produce more perspiration compared to untrained people. The trained runners are able to run faster and harder, creating more body heat and more sweat. The more fit you are, the more efficiently your body sweats. Research shows that the higher the VO2 max (and therefore fitness level) of a long-distance runner, the more quickly he starts to sweat and the more sweat he produces. This is a good thing, since sweating helps cool you down and enables you to lift, run, or cycle at a higher intensity for longer. Athletes sweat more than regular people because their bodies have become adept at keeping cool by increasing the amount they sweat. The difference between fit and unfit people has to do with each person’s capacity for heat generation. A high fitness level allows you to exercise at a higher workload, which generates more heat, which in turn leads to more sweat. When you start sweating earlier the body cools down faster, which releases extra body heat and allows you to work out harder for longer. Another theory suggests that during exercise, the body needs to pump more blood to the working muscles, which also stimulates the eccrine and apocrine glands. All these could have implications for everyone from military personnel in hot climates to elite athletes to anyone facing extreme heat and humidity – particularly in the face of global warming.
_
Making a few lifestyle changes can help prevent excessive sweating:
1. Avoid sweat triggers like spicy foods, caffeine, nicotine and alcohol.
2. Avoid synthetic fabrics and wear loose-fitting clothing.
3. Wear shoes and socks made from natural materials that draw moisture away from the feet like cotton, linen and bamboo.
4. Change your clothes regularly and wash and dry them properly to avoid body odor and sweat patches.
_
Causes of excessive sweating:
1. Physiological causes:
These include physical exertion, menopause, fever, spicy foods, and high environmental temperature. Strong emotions (anger, fear, anxiety etc.) and remembrance of past trauma can also trigger profuse sweating. Hormonal changes such as menopause, pregnancy, menstruation or puberty may stimulate sweating.
2. Pathological causes:
Diaphoresis (excessive sweating in a medical condition) may be associated with some abnormal conditions, such as hyperthyroidism and shock. If it is accompanied by unexplained weight loss or fever or by palpitations, shortness of breath, or chest discomfort, it suggests serious illness. Diaphoresis is also seen in an acute myocardial infarction (heart attack), from the increased firing of the sympathetic nervous system, and is frequent in serotonin syndrome. Diaphoresis can also be caused by many types of infections, often accompanied by fever and/or chills. Most infections can cause some degree of diaphoresis and it is a very common symptom in some serious infections such as malaria and tuberculosis. In addition, pneumothorax can cause diaphoresis with splinting of the chest wall. Neuroleptic malignant syndrome and other malignant diseases (e.g. leukemias) can also cause diaphoresis. Diabetics relying on insulin shots or oral medications may have low blood sugar (hypoglycemia), which can also cause diaphoresis. Drugs (including caffeine, morphine, alcohol, antidepressants and certain antipsychotics) may be causes, as well as withdrawal from alcohol, benzodiazepines, nonbenzodiazepines or narcotic painkiller dependencies. Sympathetic nervous system stimulants such as cocaine and amphetamines have also been associated with diaphoresis. Diaphoresis due to ectopic catecholamine is a classic symptom of a pheochromocytoma, a rare tumor of the adrenal gland. Acetylcholinesterase inhibitors (e.g. some insecticides) cause excessive acetyl choline at muscarinic receptors on sweat glands leading to diaphoresis. Mercury is well known for its use as a diaphoretic, and was widely used in the 19th and early 20th century by physicians to “purge” the body of an illness. However, due to the high toxicity of mercury, secondary symptoms would manifest, which were erroneously attributed to the former disease that was being treated with mercurials. Infantile acrodynia (childhood mercury poisoning) is characterized by excessive perspiration. A clinician should immediately consider acrodynia in an afebrile child who is sweating profusely. People who experience excessive sweating all over their body as a result of medical conditions or particular medications is called secondary hyperhidrosis. Diaphoresis is secondary hyperhidrosis due to a medical condition. Hyperhidrosis can produce up to five times more sweat than is normally required. Hyperhidrosis without known causes is primary hyperhidrosis.
_
Hot sweat and cold sweat:
Hot sweat:
Exposure to hot environment or exercise increase core body temperature and hot sweat is sweating to cool it down. When our bodies get hotter, we sweat to cool ourselves down. This is a normal bodily process called thermoregulation. Hot sweat is sweating to dissipate heat (thermoregulatory sweating) accompanied by dilatation of skin blood vessels.
_
Cold sweat:
Cold sweats aren’t caused by the cold, heat or exertion. The body normally produces sweat as a way to help keep cool. Sweating normally occurs with exertion such as when exercising or in high temperatures. However, there are other reasons for sweating. Sweating can be triggered by fear or anxiety, and this is often referred to as a cold sweat. It comes on suddenly and results in cool, damp skin. A nightmare during sleep can trigger a cold sweat, and people with prolonged stress or anxiety problems can experience sweating as a symptom. A patient suffering intense pain due to fractures, amputations, or even a migraine can experience cold sweats. Diaphoresis is a type of cold sweat. Cold sweat comes from the body’s response to stress, called the fight or flight response. Cold sweating is accompanied by vasoconstriction of skin blood vessels, hence the term cold sweat.
Treatment of Cold Sweats:
All medical conditions causing cold sweats have to be treated. Therapy with anti-anxiety medications can help manage your cold sweats and other anxiety symptoms. You can do a number of things to alleviate your cold sweats at home in a number of ways.
1. Relaxation:
Stress management techniques can be used to treat your cold sweats due to stress and anxiety. Physical activities such as jogging, yoga, breathing exercises or a warm bath can all help you relax. Slower breathing can help reduce panic and anxiety attacks and lead to a faster recovery. You can seek help from your physician if you are having a hard time coping with anxiety.
2. Change Sleeping Environment:
Use your thermostat to control the temperature in your bedroom to help reduce the incidence of cold sweats. If cold sweats occur during sleep, change the bedding and wear loose and comfortable sleep clothing.
3. Diet:
You can make changes to your diet to avoid consuming foods before bedtime that can trigger cold sweats. Avoid caffeine, alcohol, nicotine and spicy foods.
4. Be Productive:
When cold sweats occur, engage in an activity to keep your mind off of it and prevent further anxiety. Read or do a crossword puzzle.
________
Sweaty hands:
_
We use our hands every day, so palms damp with sweat can cause issues with everything from greeting people to handling objects. We often get sweaty palms in stressful situations, when we’re nervous or excited. This is because eccrine sweat glands are highly concentrated in the hands, forehead and feet. They’re connected to our sympathetic nervous system, which kicks in when we’re stressed. Some people who have hyperhidrosis, or excessive sweating, find they only sweat heavily on the palms of their hands. This condition is called palmar hyperhidrosis (vide infra). It may be present at birth, but mostly starts to occur in adolescence. For some people the problem goes away, while others experience it all their lives.
Here are some quick tips if you get sweaty palms:
• Wash your hands regularly. Unless they’re actually dirty, just using water is fine, as constantly washing with soap will dry your skin.
• Carry tissues with you and wipe your hands throughout the day.
• Pocket-size hand gels will help cleanse and dry when you can’t get to a sink.
• Talcum powder can help absorb sweat and give your hands a better grip, so grab a small container from the baby products aisle and keep it in your bag.
• Outside of winter, don’t resort to gloves to cover up sweaty palms – this will make your hands sweat more, as your skin won’t be able to breathe.
• Since stress can be a big factor in sweating, tackling the cause of your stress can sometimes help with symptoms like excessive sweaty hands.
_______
Sweaty feet:
_
Sweaty feet can cause problems for everyone. Our feet sweat because of heat and exercise, as well as stress. Some people’s feet naturally sweat more than others, but it doesn’t cause them any problems or discomfort. Changes during puberty, pregnancy and the menopause can also increase foot sweating. And people who stand all day for their job can find their feet sweat more. With other areas of the body, sweat can easily evaporate, but with feet it gets trapped between our toes and in socks and shoes. When sweat gets trapped, the bacteria that feed on our sweat release an unpleasant smell, causing foot odor or smelly feet, also known as bromohidrosis. This continues after we’ve removed our socks and shoes, especially if we put them in a dark place like a cupboard or drawer, where they can thrive. A very small percentage of people have excessive sweating, or hyperhidrosis, and some of them may find they only sweat heavily on their feet. This condition is called plantar hyperhidrosis (vide infra). For some people the problem goes away, while others experience it all their lives.
Here are some quick tips if you get sweaty feets:
• Sweat easily gets trapped in our feet and toes, so wash and dry them properly at least once a day.
• Socks made from natural fabrics like cotton or bamboo fibres are the best option, as they draw moisture away from the feet.
• Change your socks at least once a day.
• Wear shoes made from breathable materials, like canvas or leather. Sandals or flip-flops in the summer will help your feet breathe.
• Don’t wear the same pair of shoes every day, so they have time to dry out.
• For excessively sweaty feet, wipe surgical spirit between your toes after a shower or bath to help dry them out.
• Deodorising insoles and foot powders can help to absorb sweat and keep shoes fresh.
• Consider using a foot soap or deodorant – particularly in hot climates.
________
Baby sweating:
Common causes of Baby Sweating while Sleeping:
Some of the most common health conditions that could make your baby sweats while sleeping at night include the following:
1. Congenital Heart Disease: Babies who suffer from a congenital heart disease may sweat too much, particularly during the night. Babies with congenital heart disease may excessively sweat while eating and playing as well.
2. Sleep Apnea: Sleep apnea is another common cause of night sweats in babies. The condition makes the baby pause for at least 20 seconds while breathing. Hence, the infant’s body has to work excessively hard to breathe. Sleep apnea commonly affects premature babies. If your baby suffers from sleep apnea, he may also display other symptoms like bluish skin tone and wheezing along with night sweats.
3. Sudden Infant Death Syndrome: The other name for the condition is SIDS. It is related to ‘overheating’ of the body at night, which makes the baby fall into a deeper sleep. It will make waking up difficult for the baby.
4. Hyperhidrosis: If your baby is in a cool room and is still perspiring, he may be suffering from hyperhidrosis. A sweaty head, hands, and feet characterize this condition. It is not a serious health issue. You can easily deal with it by taking basic steps for sweat management.
_
Tips to deal with Night Sweats in Babies:
Following some simple steps can help you deal with baby sweating at night:
1. Keep the Room Temperature in Check:
The best way to deal with your baby’s night sweats is to keep the temperature of the room cool. You should keep your baby’s room between 60 degrees F and 70 degrees F. The basic idea to keep in mind is that if you are feeling hot, your baby is probably feeling hot too. So clear the unnecessary blankets and wraps from the baby’s crib to help him sleep comfortably.
2. Hydrate your Baby:
Make sure you hydrate your baby properly before putting him to bed every night to make up for the loss of fluids that could happen while sweating.
3. Dress him properly:
Dress up your baby in comfortable night clothing. A light sleeping gown in soft, breathable material should be the most comfortable attire at bedtime for your baby. Dress baby in the same amount of clothing you would be comfortable in without a blanket. Also, keep blankets, toys, sheets and bumpers out of the crib while your baby sleeps.
______
The functions of normal sweating:
1. Sweating is one of the ways we regulate our body temperature – humans rely on the evaporation of sweat to protect the body against a hot environment and dissipate internal heat during exercise or fever recovery.
2. Sweat helps to keep our skin moist. Moist skin assures fine tactile skills & pliability of the palms & soles. Continuous basal sweating is responsible to keep the skin smooth. If this balance is disrupted in the negative, one has the effect of dry, brittle or chapped skin. Sweat literally leaves your skin glistening.
3. Generalized sweating cools the body when intense physical activity is expected. Sweating of the body during stress help us escape from enemies if they try to grab us and sweating of hands can improve grip to hold objects. Excessive hand sweating may have opposite effect but we are discussing functions of normal sweating.
4. Sweat from some areas of the body contains scents (‘pheromones’) that send secret signals to other people.
5. Sweat contains a natural antibiotic, dermicidin that helps to destroy bacteria on the skin.
6. Sweat is responsible for up to 7% of daily elimination of urea. The concentration of urea in the sweat is 22.2 mmol/L, which is 3.6 times that in serum.
________
________
Physiology of sweating:
_
History of sweat gland physiology:
The first description of sweating dates back to the ancient Greeks. In Aristotle’s writings entitled Parts of Animals, as translated by Peck, he summarized their understanding of sweating as follows: “The blood vessels get progressively smaller as they go on until their channel is too small for the blood to pass through. But although the blood cannot get through them, the residue of the fluid moisture, which we call sweat can do so, and this happens when the body is thoroughly heated and the blood vessels are open widely at their mouth.” Although in the 1600s the basic sweat gland duct was described, the existence of a sweat gland was not accepted until the 1800s. Furthermore, the importance of sweating for thermoregulation was not fully recognized until the 20th century. Especially noteworthy is Kuno’s monograph published in 1934 as The Physiology of Human Perspiration, and later updated as “Human Perspiration”, which at that time provided the most comprehensive review of sweating. Subsequently, many researchers have studied the physiology of sweating toward a greater understanding of the mechanisms and controllers of sweating.
_
The regulation of body core temperature is crucial for survival; constant body core temperatures above 40°C result in protein denaturation and cell death, finally leading to multiple organ failure. Thus, the down-regulation of body core temperature under conditions of high environmental temperature or under physiological stress is the most important role of perspiration. With the onset of sweat secretion, thermal energy is released by the evaporation of water from the skin surface, and skin and body core temperatures are lowered. Other stimuli for perspiration, which are less well understood, are emotional stress or consumption of spicy food as seen in the figure below.
_
Control cycle of thermoregulation in humans:
Changes in body core temperature and skin temperature are driving forces for thermoregulation. These changes, caused by physical exercise/movement energy, metabolic rates and ambient temperature, are detected by local thermoreceptors and further processed in the hypothalamus as the principal centre of thermoregulation. T-set is at 37 degree Celsius i.e. hypothalamic set point for core temperature, anything above will stimulate sweating. High skin temperature reduces the hypothalamic set point for sweating and increases the gain of the hypothalamic feedback system in response to variations in core temperature. Overall, however, the sweating response to a rise in hypothalamic (‘core’) temperature is much larger than the response to the same increase in average skin temperature. This brain region is also influenced by emotional and gustatory stimuli like, e.g. stress or spicy food. Thermoregulatory sweating and skin blood circulation finally lead to the reduction of skin temperature as well as body core temperature.
_
Sweating is a physiological and vital process. Basically two types of sweating exist: thermoregulatory and emotional sweating. They are controlled by different centers: thermo regulatory sweating is regulated predominantly by the hypothalamus, emotional sweating predominantly by the limbic system. Enhanced sweating, called hyperhidrosis, can be generalized or focal. Primary focal hyperhidrosis is the most common type and affects the axillae, hands, feet, and face—areas principally involved in emotional sweating. Secondary hyperhidrosis develops due to dysfunction of the central or peripheral nervous system. The peripheral nerve innervation of sweat glands is through sympathetic C fibers releasing acetylcholine which particularly binds to the M3 muscarinic receptor to trigger sweat production. The number of glands depends on an intact peripheral sympathetic innervation, together with average experienced environmental temperature and humidity, particularly during childhood. Emotional sweating arises from signals emanating from the amygdala, prefrontal cortex, insula and cingulum, then passing along the same routes as for hypothalamic autonomic sweat innervation. In contrast to temperature-related sweating, emotional sweating leads to vasoconstriction of blood vessels in the dermis, unlike raised temperature which leads to sweating and vasodilation (hence the cold sweat with emotion). However, the distinction between temperature and emotional sweating is not absolute, with each influencing the other.
__
Autonomous nervous system (ANS) and sweating:
The ANS plays a crucial role in the maintenance of homeostasis and functions without conscious, voluntary control. The regulation of blood pressure, gastrointestinal responses to food, contraction of the urinary bladder, focusing of the eyes, and thermoregulation are just a few of the many homeostatic functions regulated by the ANS. The ANS is composed of two anatomically and functionally distinct divisions, the sympathetic nervous system (SNS) and the parasympathetic nervous system (PNS). Both systems are tonically active. In other words, they provide some degree of nervous input to a given tissue at all times. Therefore, the frequency of discharge of neurons in both systems can either increase or decrease. As a result, tissue activity may be either enhanced or inhibited. This characteristic of the ANS improves its ability to more precisely regulate a tissue’s function. Without tonic activity, nervous input to a tissue could only increase. Many tissues are innervated by both systems. Because the sympathetic system and the parasympathetic system typically have opposing effects on a given tissue, increasing the activity of one system while simultaneously decreasing the activity of the other results in very rapid and precise control of a tissue’s function. Several distinguishing features of these 2 divisions of the ANS are summarized in table below:
_
Distinguishing Features of the Sympathetic and Parasympathetic Systems:
_
Sympathetic Division:
The preganglionic neurons of the sympathetic system arise from the thoracic and lumbar regions of the spinal cord (segments T1 through L2). Most of these preganglionic axons are short and synapse with postganglionic neurons within ganglia found in the sympathetic ganglion chains. These ganglion chains run parallel immediately along either side of the spinal cord.
_
Parasympathetic Division:
The preganglionic neurons of the parasympathetic system arise from several nuclei of the brainstem and from the sacral region of the spinal cord (segments S2-S4). The axons of the preganglionic neurons are quite long compared to those of the sympathetic system and synapse with postganglionic neurons within terminal ganglia which are close to or embedded within the effector tissues. The axons of the postganglionic neurons, which are very short, then provide input to the cells of that effector tissue.
_
Neurotransmitters of the Autonomic Nervous System
The two most common neurotransmitters released by neurons of the ANS are acetylcholine and norepinephrine. Neurotransmitters are synthesized in the axon varicosities and stored in vesicles for subsequent release. Several distinguishing features of these neurotransmitters are summarized in table below. Nerve fibers that release acetylcholine are referred to as cholinergic fibers. These include all preganglionic fibers of the ANS, both sympathetic and parasympathetic systems; all postganglionic fibers of the parasympathetic system; and sympathetic postganglionic fibers innervating sweat glands. Nerve fibers that release norepinephrine are referred to as adrenergic fibers. Most sympathetic postganglionic fibers release norepinephrine.
_
Distinguishing Features of Neurotransmitters of the Autonomic Nervous System:
Acetylcholine (ACh) is the preganglionic neurotransmitter for both divisions of the ANS as well as the postganglionic neurotransmitter of the parasympathetic neurons; the preganglionic receptors are nicotinic, and the postganglionic are muscarinic in type. Norepinephrine (NE) is the neurotransmitter of the postganglionic sympathetic neurons, except for cholinergic neurons innervating the eccrine sweat glands.
_
The sympathetic nervous system is most active when you are in an emergency, exercising, or an exciting or embarrassing situation. It is often referred to as the “fight-or-flight” system. It increases the heart rate, blood pressure, and blood glucose levels. It also dilates the bronchioles of the lungs, and dilates the blood vessels of the skeletal muscles. This nervous system enables the body to cope rapidly with situations. The parasympathetic nervous system is active when the body is resting. It is referred to as the “resting-and-digesting” system. It conserves your body’s energy by slowing the heart rate. It also promotes digestion. Sympathetic is the “fight or flight” response and the parasympathetic is the “rest and digest” responses. Sweat glands are innervated by sympathetic post-ganglionic fibers that release acetyl choline at nerve ending rather than usual norepinephrine. I would call it sympathetic cholinergic nerves. The vast majority of sweat glands in the body are innervated by sympathetic “cholinergic” neurons. Sympathetic postganglionic neurons usually secrete norepinephrine and are named sympathetic adrenergic neurons. However, when sympathetic postganglionic neurons innervate sweat glands they secrete acetylcholine and hence are termed sympathetic “cholinergic” neurons. Sweat glands, piloerector muscles and some blood vessels are innervated by sympathetic cholinergic neurons. Many activities that stimulate the nervous system, such as strong smells, spicy foods, increased air temperatures, exercise, high emotional excitement, stress or nervousness may cause attacks of excessive sweating through sympathetic nerve over activity.
_
The function of the sweat glands and circulation of the skin is regulated by the sympathetic nervous system. Several feedback loops exist to ensure regulation:
•Most important are thermoregulatory afferents consisting of afferent somatosensory and central thermosensitive neurons.
•The thermoregulatory efferents are sudomotor, vasomotor, and motor efferents.
•The central regulatory center is situated mainly in the hypothalamus.
•In the periphery, the amount of secreted sweat is regulated mainly via skin temperature by postganglionic sudomotor fibers innervating sweat glands.
_
Central mechanisms:
An increase in core body temperature—e.g., because of thermogenesis, mostly muscle activity—and skin temperature—e.g., because of sun irradiation—stimulates temperature receptors and thus thermosensory afferents. Receptors of heat and cold are situated in the skin and viscera, which pass impulses via Ad and C fibers to the central nervous system. Central thermosensitive neurons are situated in the spinal cord, the brain stem (reticular formation, raphe nucleus), and the hypothalamus (preoptic nucleus of the anterior hypothalamus). The hypothalamus is the integration center of all thermosensory afferents. Its function is to regulate the body temperature to a level of 37 degrees Celsius. Depending on the degree of agreement of target temperature and actual temperature, thermogenesis—through muscle tremor and cutaneous vasoconstriction—or release of heat—through sweating and cutaneous vasodilatation—is induced. Numerous other factors of influence—such as hormones, affect, oxygen saturation, and plasma osmolality—also influence thermoregulation and therefore sweating. Progesterone raises the body temperature and lowers the rate of sweating, whereas estrogen has the opposite effect. So changes in progesterone and estrogen levels cause sweating. The sweating rate also falls in case of hypovolemia and a rise in plasma osmolality; it rises as a result of increased oxygen saturation.
_
Peripheral mechanisms:
The sweat glands are innervated sympathetically by postganglionic fibers. The fibers in question are sympathetic C fibers. The released peripheral transmitter is—in contrast to vasomotor efferents—acetylcholine, which binds to postsynaptically localized M3 muscarinic receptors of the eccrine glands and triggers sweat production. The sweat glands, whose purpose is thermoregulation, are situated all over the entire body surface; the palms of the hands and the soles of the feet have relatively more glands. The number of functioning eccrine glands depends on the one hand on intact peripheral innervation and on the other hand on environmental conditions (climate) during early childhood. On the periphery, the rate of sweating is regulated by skin temperature and circulation: a rise in skin temperature increases the rate of sweating, cooling down reduces it. Peripheral and central mechanisms can influence each other mutually. It is thus not surprising that in thermoregulation, there are no linear but complex associations between sweat production on the one hand and body and skin temperature on the other hand. This also partly explains the great variability of sweating between individuals.
_
Given the challenges of identifying neural tracks in humans, the exact neurological pathways responsible for sweating are not entirely understood. Evidence from animal studies suggests that efferent signals from the preoptic hypothalamus travel via the tegmentum of the pons and the medullary raphe regions to the intermediolateral cell column of the spinal cord. In the spinal cord, neurons emerge from the ventral horn, pass through the white ramus communicans, and then synapse in the sympathetic ganglia. Postganglionic nonmyelinated C fibers pass through the gray ramus communicans, combine with peripheral nerves and travel to sweat glands. Sympathetic nerve terminals cluster mainly around the secretory coil of the sweat gland, but a few projections extend to the sweat duct.
_
Direct recording of postganglionic skin sympathetic nerve activity (SSNA) is possible in humans and much of the early work in this area was performed by Wallin and colleagues. This technique permits the assessment of the neural signal responsible for sweating, as well as cutaneous vascular and perhaps pilomotor responses. Because of the potential for the integrated skin sympathetic recording to contain neural signals innervating these differing efferent structures, caution must be taken when trying to link the skin neural signal to a particular efferent event (e.g., sweating, cutaneous vasoconstriction, etc.). Nevertheless, during heat stress, SSNA is partially synchronized with galvanic skin response (an index of sweating) and pulsatile sweat expulsion, and ∼80% of SSNA bursts have been reported to be synchronized with pulsatile sweat expulsion. These observations suggest that a large fraction of the recorded skin sympathetic neural signal in heat stressed subjects is sudomotor in nature.
_
Note: In Latin sudor, means “sweat”. So nerves that innervate sweat gland are known as sudomotor nerves.
_
Acetylcholine is the primary neurotransmitter released from cholinergic sudomotor nerves and binds to muscarinic receptors on the eccrine sweat gland, although sweating can also occur via exogenous administration of α- or β-adrenergic agonists. The sympathetic nerves distributed to sweat glands consist of large numbers of cholinergic terminals and a few adrenergic terminals. The effect of these adrenergic terminals in causing sweating is minimal given that exogenous administration of adrenergic agents will cause only minimal sweating relative to acetylcholine administration, the latter of which is the primary neurotransmitter causing sweating. Nevertheless, the observation that local and systemic administration of atropine (a muscarinic-receptor antagonist) greatly attenuates or abolishes sweating during a thermal challenge or during exogenous administration of acetylcholine or its analogs strongly suggests that thermoregulatory sweating primarily occurs through stimulation of muscarinic receptors. Released acetylcholine is rapidly hydrolyzed by acetylcholinesterase, and this response may be one of a number of mechanisms by which sweat rate is regulated. Immunochemistry studies have identified a number of possible peptide neuromodulators (e.g., vasoactive intestinal polypeptide, calcitonin gene-related peptide) in and around cholinergic sudomotor nerve terminals and eccrine sweat glands. Although some evidence is present, the precise role of these peptides in modulating sweating remains unclear.
_
When acetylcholine binds to muscarinic receptors on the sweat gland, intracellular Ca2+ concentrations increase. This results in an increase in the permeability of K+ and Cl− channels, which initiates the release of an isotonic precursor fluid from the secretory cells. This precursor fluid is much like plasma but is devoid of proteins. In a noteworthy series of in vitro studies, Sato collected sweat samples from an isolated secretory coil and from the sweat duct and found that the solution from the duct was hypotonic relative to the secretory coil. These and a number of earlier observations led to the conclusion that, as the fluid travels up the duct toward the surface of the skin, sodium and chloride are reabsorbed, resulting in sweat on the skin’s surface being hypotonic relative to plasma. However, when the rate of sweat production is elevated, as occurs during exercise or heat stress, ion reabsorption mechanisms can be overwhelmed due to the large quantity of sweat secreted into the duct, resulting in higher ion losses. Thus the sodium content in sweat on the skin’s surface is greatly influenced by sweat rate.
_
In addition to a central neural drive for sweating, sweating can also be initiated by an axon reflex. Exogenous administration of acetylcholine, or its analogues, not only directly stimulates muscarinic receptors on sweat glands, but also activates an axon reflex via stimulation of axonal nicotinic receptors. The neural impulse due to the activated axon terminal is thought to travel antidromically to a branch-point, and then travel orthodromically to other nerve terminals, culminating in the release of acetylcholine. Thus not only the central drive from thermoregulatory center but also local mechanisms (e.g., perhaps endogenous acetylcholine stimulation of the axon reflex) can contribute to the modulation of sweating. Acetylcholine released from cholinergic nerves is rapidly hydrolyzed by acetylcholinesterase. Thus acetylcholinesterase is capable of modulating sweat rate during low to moderate sweating activity but its effectiveness is greatly reduced when sweat rate is substantially increased. Consistent with this finding, elevations in sweat rate occur earlier with exogenous methacholine than with acetylcholine administration, given the reduced cholinesterase susceptibility of methacholine.
_
The neurotransmitter(s) responsible for active cutaneous vasodilation has yet to be fully elucidated, although neuropeptides such as calcitonin gene-related peptide (CGRP), vasoactive intestinal polypeptide (VIP), and substance P as well as nitric oxide (NO) have been implicated. Although acetylcholine is the primary neurotransmitter responsible for sweat secretion, enhanced sweating due to local administration of VIP, CGRP, or NO suggest that these peptides as well as NO may contribute to the overall modulation of sweating during a thermal challenge. Aquaporins (AQPs) are a family of membrane water channel proteins. Given that AQP proteins have been identified in human sweat glands, coupled with findings that botulinum toxin inhibits water permeability via AQP-dependent mechanisms, botulinum toxin, which is recognized to abolish sweating, may do so via pre- and post- cholinergic synaptic mechanisms; although botulinum toxin is considered primarily as a pre-synaptic inhibitor of neurotransmission. Recently, Shibasaki et al. found that local administration of botulinum toxin in human skin completely blocked the sweating response to exogenous acetylcholine, lending support to a post-synaptic mechanism by which botulinum toxin can abolish sweating. Future studies are warranted to identify the precise mechanism(s) by which botulinum toxin blocks sweating independent of inhibition of cholinergic neurotransmission.
_
Emotional sweating:
The second type of sweating is emotional sweating. This serves as a physical “feedback” signal in emotionally affecting sensory, cognitive, and behaviorally relevant processes. Further, it maintains the trophic functions of the sensorily important palms and soles. This type of sweating is regulated by the neocortical and limbic centers. The responsible centers are currently not exactly defined, but the amygdala, prefrontal cortex, insular cortex, and cingulum seem to have a major role. The preganglionic and postganglionic (spinal and peripheral) pathways are the same as in thermoregulatory sweating. However—by contrast to thermoregulation, which affects hirsute skin—emotion, stress, or other stimuli mainly stimulate sweat glands in the face, the axillae, the palms, and the soles of the feet. Another difference is the simultaneous activation of the vasomotors. Stress induces vasoconstriction, whereas thermoregulatory sweating is accompanied by vasodilatation. It needs to be borne in mind, however, that the distinction between thermoregulatory and emotional sweating is not an absolute distinction; they have been shown to mutually influence one another. However, the distinction makes the physiology of sweating easier to explain and both types can be examined in a differentiated manner.
_
Gustatory sweating:
Under certain conditions, sweat secretion can be induced by ingestion, which can be explained by a direct or indirect thermal effect. First, ingestion causes an increase in metabolism, leading to elevated body temperature and thermal sweating. Second, hot and spicy food is able to induce a mild form of gustatory sweating, which is confined to the face, the scalp and the neck. This reaction is believed to be driven by the substance capsaicin, which binds to warmth sensors in the oral cavity leading to a thermoregulatory response. On the other hand, gustatory sweating describes a pathological state, referred to as Frey’s syndrome, which follows parotid surgery and affects the area of the cheek. It is assumed that this unilateral form of gustatory sweating results from disruption of parasympathetic secretomotor fibres. These later anastomose with sudomotor sympathetic fibres of the skin, thereby gaining control of sweat gland activity. Aside from Frey’s syndrome, gustatory sweating is a rare complication in diabetic patients with autonomic neuropathy.
_
Are sweat glands parasympathetic or sympathetic?
Sweat is sympathetic but an exception – Ach (acetyl choline) is released as a post-synaptic neurotransmitter rather than Adrenaline/Noradrenaline. Eliciting a parasympathetic response will not stimulate these neurons and therefore sweating is not a parasympathetic effect. However, as post-synaptic sweat glands contain Muscarinic receptors and not adrenoceptors, the administration of a non-selective Muscarinic agonist would result in both a parasympathetic response such as constriction of the pupil or decreased heart rate as well as sweating due to the activation of these sympathetic post-synaptic MAChR in the sweat glands. Atropine would reduce all parasympathetic responses and stop sweating.
________
________
Glands:
Generally speaking, exocrine glands are duct glands i.e.; these glands are provided with ducts to transport their secretions; whereas endocrine glands are ductless glands i.e.; they release their secretions directly into blood stream. Endocrine, or ductless glands (e.g., pituitary, thyroid, adrenal) secrete substances known as hormones directly into the bloodstream rather than through ducts. Exocrine glands (e.g., salivary, sweat, lacrimal) discharge their products through ducts. Pancreas has both exocrine glands (pancreatic digestive juice) and endocrine glands (release insulin).
_
Exocrine glands secrete their products through a duct onto an outer surface of the body, such as the skin or the human gastrointestinal tract. Secretion is directly onto the apical surface. The glands in this group can be divided into three groups:
1. Apocrine glands: a portion of the secreting cell’s body is lost during secretion. E.g. mammary gland, sweat gland of arm pit & pubic region,
2. Holocrine glands: the entire cell disintegrates to secrete its substances e.g., sebaceous gland, meibomiun & zeis gland.
3. Merocrine glands: cells secrete their substances by exocytosis (e.g., mucous and serous glands). Also called “eccrine” glands. E.g. most sweat gland of humans, goblet cells, salivary gland, tear gland, intestinal glands.
_
Three types of exocrine glands:
_____
Sweat glands:
Sweat glands are also known as sudoriferous or sudoriparous glands from Latin sudor, meaning “sweat”. Sweat glands are cutaneous appendages like hair follicles or sebaceous glands. Cutaneous glands are exocrine glands, as the secretion is released via a duct to the outer skin surface. The embryonic development of the glands begins with an ingrowth of the epithelial surface, when the epithelial cells begin to form the duct and the gland with differentiated cells. The sweat gland is a long, coiled, hollow tube of cells. The coiled part in the dermis is where sweat is made, and the long part is a duct that connects the gland to the opening or pore on the skins’s outer surface. Sweat glands are coiled tubular systems. Although they are usually perceived as distinct single entities, there is evidence that the coils of two eccrine glands may also occur convoluted within each other; these structures might easily be mistaken as one large coil with two or more ducts to the surface. Nerve cells from the sympathetic nervous system are connected to the sweat glands. Human sweat glands are generally divided into three types, the apocrine, the apoeccrine and the eccrine gland. Eccrine sweat glands are distributed over nearly the entire body surface. Sweat glands become identifiable in the palm and sole of the feet in the 16th fetal wk, and in the 22nd wk or later sweat glands are identifiable on the rest of the body. Eccrine sweat glands already exist at birth and can be found over the whole body surface with only two exceptions: lips and glans penis. The number of sweat glands in humans varies greatly, ranging from 1.6 to 4.0 million, with the density of eccrine sweat glands associated with thermoregulation (i.e., precluding glands on the palms of the hands and soles of the feet) being the greatest on the forehead, followed by the upper limbs, and finally the trunk and lower limbs. The structure of the eccrine sweat gland consists of a bulbous secretory coil leading to a duct. The secretory coil is located in the lower dermis, and the duct extends through the dermal layer and opens directly onto the skin surface. The uncoiled dimension of the secretory portion of the gland approximates 30–50 μm in diameter and 2–5 mm in length. If one sweat gland were uncoiled and stretched out, it would be approximately 50 inches (127 centimeters) in length. Collectively, the sweat glands are 2,000 miles (3,218 kilometers) in length. The size of the adult secretory coil ranges from 1 to 8 × 10−3 mm3. There is a positive correlation between the size of an individual sweat gland and the maximal sweat rate of that gland. Apocrine sweat glands are the ones in the armpits (axilla) and the anal-genital area. They are larger than eccrine glands and they normally end in hairs rather than pores. Also, they do not do anything until puberty. There is also a third type of sweat gland, first discovered in 1987. It’s only been found in the same places that apocrine glands show up, but because researchers couldn’t classify them as apocrine or eccrine, they became known as apoeccrine glands. Some think that they are eccrine glands that become somehow modified during puberty.
_
Eccrine and apocrine sweat glands:
Apocrine glands are found mainly in the armpits and near the anus. We each have about 1 million of these glands. They are really scent glands. The sweat that comes from them has a particular smell in each person, and probably includes ‘pheromone’ scents that send messages to other people. Eccrine glands are responsible for sweating when we are hot. We each have about 3 million of these glands. Every 1 cm2 of the back has about 60 sweat glands. On the palms and soles, there are about 600 glands per cm2.
__
Humans have up to four million sweat glands distributed over the body, of which about three million are eccrine sweat glands. Eccrine glands secrete an odorless, clear fluid that is hypotonic to plasma and that serves to aid in the regulation of body temperature by allowing heat loss by evaporation. If you sweat excessively, it is not because you have too many sweat glands or that they are abnormally large. It is probably because there is a lot of activity in the tiny nerves that control them. Apocrine sweat glands are located in limited areas—the axilla and urogenital regions—and produce a thick, odorless fluid that undergoes bacterial decomposition, leading to substances with strong odors. These scent glands become active during puberty and secrete a viscous fluid. They are responsible for an individual’s “personal,” occasionally unpleasant, odor. The ratio of apocrine to eccrine glands is one to one in the axillae and one to ten elsewhere. The secretory portion of eccrine glands produce an ultrafiltrate that is then processed by cells lining the duct portion, where reabsorption of sodium occurred, leading to hypotonic sweat and conserving electrolytes. An acclimatized person can produce up to several liters of sweat per hour and ten liters per day. For nonhuman species, apocrine sweat provides pheromone signalling that is important in mating, parenting, and other interactions; it is unclear what the role is for apocrine sweat in humans. There are also mixed sweat glands called apoeccrine glands, found in human axillary and perianal areas. These glands develop during puberty from eccrine precursors. The function of this type of gland and its role in the pathophysiology of hyperhidrosis is unknown, but in some patients, up to 45% of the axillary sweat glands were of this type. In addition, in vitro studies have shown the apoeccrine gland to secrete sweat at a sevenfold higher rate than the eccrine gland does. In vitro sweat production by the apoeccrine gland was stimulated by epinephrine and methacholine.
_
Both eccrine and apocrine sweat glands are innervated by postganglionic sympathetic fibers. For eccrine glands, the major neurotransmitter is acetylcholine, and for apocrine glands, catecholamines are the major neurotransmitters. Spinal cord segments from T2 to T8 provide innervation to the skin of the upper limbs, from T2 to T4 to the skin of the face, from T4 to T12 to the skin of the trunk, and from T10 to L2 to the skin of the lower limbs. The thermoregulatory center in the hypothalamus controls body temperature by regulating eccrine sweat output and blood flow to the skin. This center responds not only to changes in core body temperature but also to hormones, endogenous pyrogens, physical activity, and emotions. Both emotional and physical activities are thought to affect the thermoregulatory center via the limbic system. The sweat glands on the palms and soles appear to be activated primarily by emotional stimuli rather than thermoregulatory change, while axillary sweating is stimulated by both thermoregulatory changes as well as emotional stimuli. Since palmar and plantar glands do not differ from sweat glands in other areas with respect to morphology, innervation, and neurotransmitter response, one theory suggests that there is a distinct hypothalamic thermoregulatory center that controls sweating in the palms and soles and sometimes in the axillae. Differing from the regulatory center that controls sweating in other areas, this center is thought to receive input exclusively from the cortex and to be unresponsive to temperature changes. Supporting this theory is the finding that emotional sweating is not seen during sleep or sedation. Emotional sweating is thought to be an atavistic function that was important when hunting animals or fighting enemies. Physiologic amounts of sweat on the palms and soles can improve friction by controlling the humidity of the stratum corneum, leading to an improved grip. Generalized sweating cools the body when intense physical activity is expected. In addition, increased eccrine sweat output in the axillae produced by emotional stimuli will allow natural odors from prior apocrine gland secretion to aerosolize and function as pheromone signals.
__
| Differences Between Eccrine & Apocrine Sweat Glands | ||
| Eccrine Glands | Apocrine Glands | |
| Overall diameter of secretory coil | 500-700 µm | 800 µm |
| Diameter of individual secretory tubule | 30-40 µm | 80-100 µm |
| Composition of secretory unit | single layer, mixed clear cells & dark cells | single layer columnar cells |
| Composition of ductal epithelium | two or more layers of cuboidal cells | double layer of cuboidal cells |
| Duct opens to | skin surface | hair follicle, sometimes nearby skin surface |
_
Eccrine sweat glands produce a clear, odorless substance, consisting primarily of water and NaCl. NaCl is reabsorbed in the duct to reduce salt loss, but is dysfunctional in cystic fibrosis thus producing salty sweat. They are active in thermoregulation by providing cooling from water evaporation of sweat secreted by the glands on the body surface and emotional induced sweating (anxiety, fear, stress, and pain). The white sediment in otherwise colorless eccrine secretions is caused by evaporation that increases the concentration of salts. The basic function of the sweat duct is the reabsorption of ions from primary sweat, having an almost isotonic sodium chloride concentration when entering the duct. During the process of reabsorption, sodium moves passively into the ductal cells via sodium channels on the apical membrane. This process is driven by a Na/K-ATPase on the basolateral membrane, pumping sodium from the ductal cells into the interstitial fluid. The chloride channel cystic fibrosis transmembrane conductance regulator (CFTR), which is abundantly expressed in the human reabsorptive duct, is composed of a major part of the electrical conductance for chloride and is acutely regulated by protein kinase A-dependent phosphorylation. Mutations in the CFTR gene lead to cystic fibrosis (CF), a clinical condition in which ductal electrolyte reabsorption is highly affected, leading to increased sweat chloride levels. This is why sweat testing is a relevant tool for CF diagnosis. Recent studies led to the identification of anion exchangers, carbonic anhydrases II and vacuolar proton pumps (V-H+-ATPase) in ductal cells, providing evidence for the existence of a second chloride reabsorption mechanism that proceeds as proton-driven active transport, allowing chloride reabsorption also under low luminal chloride concentrations.
Eccrine Sweat Glands Disorders include:
1. Hyperhidrosis Causes: emotional, neurologic, infectious, neoplastic
2. Hypohidrosis or anhidrosis: Acquired: neuropathy Congenital: hypohidrotic ectodermal dysplasia
3. Sweat retention: Miliaria (prickly heat)
_
Apocrine glands already exist at birth but do not become active until puberty. Apocrine glands are restricted to hairy body areas, as they open and secrete into the hair canal. For this reason, apocrine glands can only be found in the axilla, mammary, perineal and genital region. Apocrine Sweat glands primarily reside in your armpits and your genital regions. They produce a thicker, oily, odorless, fluid that gets released into your hair follicles. Bacteria that reside on your skin break down this fluid and the result is the odor we smell when we don’t shower regularly. In mammals, this oily fluid is thought by some to act as a pheromone to attract a mate, or act as a warning signal to other mammals. Apocrine sweat glands respond to emotional stimuli such as anxiety, pain or sexual arousal. Apocrine secretion takes place as apical budding-off from the luminal cells and is under adrenergic control, via adrenaline and noradrenaline. The fluid secreted by the apocrine sweat gland is an oily, odourless substance, containing proteins, lipids and steroids. However, it cannot be excluded that apocrine secretions are mixed with sebum, as both, apocrine and sebaceous glands open into the hair follicle. Recently, it was shown that two apocrine proteins, referred to as apocrine secretion odour-binding proteins 1 and 2 (ASOB1 and ASOB2) function as carrier proteins for volatile odour molecules, e.g. (E)-3-methyl-2-hexenoic acid, which are linked as amino acid conjugates and are subsequently released by bacterial enzymes. ASOB2 was shown to be identical with the lipocalin apolipoprotein D. ASOB1 shares homology to the α-chain of apolipoprotein J. As in other species, lipocalins serve as carrier proteins for pheromones; an analogous function has been suggested for ASOB1/2. Recent studies of Natsch et al. led to the purification of a Zn2+-dependent aminoacylase from Corynebacteria, which was shown to mediate the release of (E)-3-methyl-2-hexenoic acid and 3-hydroxy-3-methyl-hexanoic acid, a chemically related compound, from their glutamine-conjugated precursors. Moreover, several odoriferous sulfanylalkanols were identified as axillary odour components, that are presumably released from cysteine conjugates. A respective cystathione-β-lyase has been cloned from an axillary isolate of Corynebacterium striatum.
_
The figure below shows that in childhood, we have eccrine and eccrine-like sweat glands, and during adolescence apocrine and apoeccrine sweat glands develop:
_
Sweat gland density for different body parts by different researchers:
This table below shows sweat gland density (in square centimeter) for different body regions that have been assessed by direct and indirect counting techniques in the 1970s, 1980s, 1990s, and recently. Note the broad variations of sweat gland numbers, e.g. in the armpit, the face or the chest.
| Region | Wilke et al. | Sato et al. | Fiedler et al. | IFSCC Monograph |
| Palms | 644 | 600–700 | 620 ± 120 | 370 |
| Forearm | 134 | 108 | 225 ± 25 | 155 |
| Abdomen | 127 | – | 190 ± 5 | – |
| Upper arm | 90 | 108 | 150 ± 20 | – |
| Armpit | 68 | ∼100 | 400 ± 50 | 90–200 |
| Thigh | 57 | – | 120 ± 10 | 80 |
| Face | 59 | 181 | 360 ± 20 | 175 |
| Chest | 20 | – | 175 ± 30 | – |
| Back | – | 64 | 160 ± 30 | 60–100 |
_________
_________
Mechanism of sweat production and secretion:
The cell membranes lining the sweat gland act as “salt pumps.” When messages from the central nervous system trigger the membranes to push negatively charged chloride ions out, they drag positively charged sodium ions with them, maintaining a neutral charge in the sweat duct. The insides of the cells become less salty than their exteriors. This imbalance draws water through the cell membranes into the sweat duct, until the sodium and chloride concentrations again match; as a result, the cells shrink until they can replenish themselves by pulling in water and salt from interstitial fluid. The process repeats to create more and more sweat. On the other hand, measuring levels of sodium and chloride in sweat is essential in diagnosing cystic fibrosis. The cells lining the upper portion of the sweat ducts normally reabsorb most of the salt that is produced by the sweat creation. But for patients with cystic fibrosis, the cells that handle that reabsorption don’t work properly.
_
When the eccrine sweat gland is stimulated, the cells secrete a fluid (primary secretion) that is similar to plasma — that is, it is mostly water and it has high concentrations of sodium and chloride and a low concentration of potassium — but without the proteins and fatty acids that are normally found in plasma. The source of this fluid is the spaces between the cells (interstitial spaces), which get the fluid from the blood vessels (capillaries) in the dermis. This fluid travels from the coiled portion up through the straight duct as seen in the figure above. What happens in the straight duct depends upon the rate of sweat production or flow:
•Low sweat production (rest, cool temperature) — Cells in the straight duct reabsorb most of the sodium and chlorine from the fluid. This happens because there is enough time for reabsorption. In addition, water is reabsorbed osmotically. So not much sweat reaches the outside. Also, the composition of this sweat is significantly different from the primary secretion. There is not as much sodium and chloride, and there is more potassium.
•High sweat production (exercise, hot temperature) — Cells in the straight portion do not have enough time to reabsorb all of sodium and chloride from the primary secretion. So, a lot of sweat makes it to the surface of the skin and the composition is close to, but not exactly like the primary secretion. The sodium and chloride concentrations are about half as much, and potassium is about 20 percent higher.
_
Sweat is produced in apocrine sweat glands in the same way. However, the sweat from apocrine glands also contains proteins and fatty acids, which make it thicker and give it a milkier or yellowish color. This is why underarm stains in clothing appear yellowish. Sweat itself has no odor, but when bacteria on the skin and hair metabolize the proteins and fatty acids, they produce an unpleasant odor. This is why deodorants and antiperspirants are applied to the underarms instead of the whole body. The maximum volume of sweat that a person who is not adapted to a hot climate can produce is about one liter per hour. Amazingly, if you move to a hot climate such as the American desert southwest or the tropics, your ability to produce sweat will increase to about two to three liters per hour within about six weeks! This appears to be the maximum amount that you can produce.
________
Composition of sweat:
Eccrine sweat can vary in composition, depending on hydration, exercise, state of health and region of the body. Besides water, which accounts for 99% of eccrine sweat, further components are sodium, chloride, potassium, calcium, magnesium, lactate, ammonia, amino acids, urea and bicarbonate. Eccrine sweat is clear, odourless, hypo-osmotic relative to plasma having pH from 4 to 6.8. In addition, several proteins and peptides, e.g. cysteine proteinases, DNAse I, lysozyme, Zn-α2-glycoprotein, cysteine-rich secretory protein-3 and dermcidin have been identified in eccrine sweat. Some of these, like dermcidin (DCD), an antimicrobial peptide, that is expressed constitutively in eccrine sweat glands, are believed to play a role in innate host defence mechanisms. Recently, it was shown that sweating leads to a reduction in bacteria on the skin of healthy subjects, but not in patients with atopic dermatitis having reduced DCD concentrations in eccrine sweat. On the other hand, the apocrine sweat has a pH of 6 to 7.5; it contains water, proteins, carbohydrate waste material, lipids, and steroids. The sweat is oily, cloudy, viscous, and originally odorless; it gains odor upon decomposition by bacteria. Because both apocrine glands and sebaceous glands open into the hair follicle, apocrine sweat is mixed with sebum.
_
Sweat is not pure water; it always contains a small amount (0.2–1%) of solute. Mineral composition varies with the individual, their acclimatisation to heat, exercise and sweating, the particular stress source (sauna, etc.), the duration of sweating, and the composition of minerals in the body. An indication of the minerals content is sodium (0.9 gram/liter), potassium (0.2 g/l), calcium (0.015 g/l), and magnesium (0.0013 g/l). Also many other trace elements are excreted in sweat, again an indication of their concentration is (although measurements can vary fifteen fold) zinc (0.4 milligrams/liter), copper (0.3–0.8 mg/l), iron (1 mg/l), chromium (0.1 mg/l), nickel (0.05 mg/l), and lead (0.05 mg/l). When a person moves from a cold climate to a hot climate, adaptive changes occur in the sweating mechanisms of the person. This process is referred to as acclimatisation: the maximum rate of sweating increases and its solute composition decreases. The volume of water lost in sweat daily is highly variable, ranging from 100 to 8,000 mL/day. The solute loss can be as much as 350 mmol/day (or 90 mmol/day acclimatised) of sodium under the most extreme conditions. During average intensity exercise, sweat losses can average up to 2 litres of water/hour. In a cool climate and in the absence of exercise, sodium loss can be very low (less than 5 mmols/day). Sodium concentration in sweat is 30-65 mmol/l, depending on the degree of acclimatisation.
_
Reference values of Na(+) and Cl(-) concentrations in adult sweat:
The results of the investigations to reference values for Na(+)- and Cl(-)-concentrations in sweat of adults are as follows: The normal range of electrolyte values in sweat in adults is up to 70 mmol/l (Na+) and 55 mmol/l (Cl-) respectively in infants (40 mmol/l for Na+ and Cl-). There are no sex and age differences. Adults with chronic bronchitis and bronchiectasis don’t show different results in comparison with healthy persons. Adults with cystic fibrosis have significantly increased sweat electrolyte concentrations (90-120 mmol/l). Variations in the electrolyte values of a day or of a month are important and much higher than the analytical one.
_
During sweating, salt is lost at about 4 g per litre (1 g per litre in acclimatised persons). As a normal diet provides 8–14 g of salt per day, a normal diet is often sufficient.
_
The excretion of trace metals in human sweat:
The concentrations of zinc, copper, iron, nickel, cadmium, lead, manganese, sodium and chloride in the sweat of six males and three females were determined after collections utilizing a total body washdown technique. From the results, sweat appears to be an important excretory pathway for zinc and copper. The mean concentrations of nickel and cadmium in sweat were higher than those reported for urine, that of lead was similar to urine. The loss of manganese in sweat is significant. Levels of zinc and iron were lower in sweat from females, possibly reflecting compensation for menstrual and other losses.
_
Uric acid and urea in human sweat: a 2002 study:
The present study investigated whether thermal sweating may relieve elevated concentrations of serum uric acid or urea. Concentrations of uric acid and urea were measured in the sweat of sixteen male volunteers, who were treated with external heat after one hour of intense physical exercise. The same analytes were also measured in their urine and serum samples. Furthermore, creatinine and some electrolytes were determined in these specimens. The results show that the concentration of uric acid in the sweat is 24.5 micromol/L, which is only 6.3% of that in serum. The concentration of urea in the sweat is 22.2 mmol/L, which is 3.6 times that in serum. The results indicate that sweat uric acid concentration is quite minimal, and the estimated total uric acid excretion per day in normal physiological range is insignificant. However, the level of sweat urea was found at a much higher concentration than the serum level. No correlation could be established between the level of uric acid in sweat and in serum. There was also no correlation between the level of urea in sweat and that in serum. These results suggest it would not be effective to relieve the elevated serum uric acid concentration by thermal sweating when the renal excretion of uric acid is partly compromised. Nevertheless, the potential of urea excretion via profuse sweating is apparent particularly when the kidneys are damaged or their function is impaired. These findings also suggest that persons who take vigorous exercise or are exposed to hot environments should be well advised to drink adequate fluids since heavy sweating excretes only minimal uric acid, accompanied by significant diminution of urinary output and diminished urinary excretions of uric acid, which may induce elevated levels of serum uric acid.
_
Average and Champion Sweat Rates:
How much do we sweat? An average person sweats between 0.8 to 1.4 liters per hour during exercise. The highest recorded sweat rate for an athlete in an exercise situation is 3.7 liters per hour, recorded by Alberto Salazar while preparing for the 1984 Summer Olympics. The highest human sweat rate recorded is 5 liters per hour measured on a resting body exposed to a hot environment. At rest, the skin blood flow was maximum and not competing with exercising muscles.
_
Calculate Your Sweat Rate:
The easiest way to measure your sweat rate is to weigh yourself without clothes on before exercising for one hour. After an hour of exercise, return home, strip down and weigh yourself again. Assuming you did not use the toilet or consume any fluids during exercise, your weight loss is your sweat rate. For each kilogram of lost weight, you lost one liter of fluid.
_
Sweat rate as indicator of health:
Physical stimuli and emotional stress-induced sweat secretions in the human palm and forehead: a 1997 study:
When sweating is induced by emotional or physical stimuli, the observation of the behavior of active sweat glands and measurement of the sweat rate are useful for the estimation of the degree of emotional stress on humans. When a loud sound was produced behind the subject’s head, a periodical damped oscillation of sweating was observed. This sweat secretion may correlate with how a human being absorbs a big surprise stimulus. The differences of the time lag for starting to secrete sweat from sweat glands may correlate with the performance of the nervous system and/or the difference of body condition with and without stress. An intake of caffeine stimulates the central nervous system, and it rises basic, mental and thermal perspiration. The degree of physical stimuli given is amplified by the dose of caffeine, and sweating becomes 1.5–2 times greater compared to that without the dose. This study shows that sweat rate can be used as a good indicator for the state of body conditions.
__________
Thermoregulatory sweating:
Thermoregulatory sweating involves eccrine sweat glands that are distributed over almost the whole body surface. Along with vasodilatation in the skin, thermoregulatory sweating serves as a system for temperature reduction under heat stress conditions. Failure of this mechanism can lead to hyperthermia and death. Sweat gland activity is directly controlled by the central nervous system with the hypothalamus as the principal centre of thermoregulation. This centre responds not only to changes in core body temperature but also to hormones, endogenous pyrogens, physical activity, and emotions. The central drive for thermoregulatory sweating is described as the sum of internal body temperature and mean skin temperature, whereas the influence of the first exceeds the second by a factor of 10. Moreover, the sweat rate is affected by local thermal skin conditions – an augmentation of local skin temperature leads to increased sweating. However, the mechanism by which this reaction is controlled remains unclear; it could be explained with both, a greater release of neurotransmitters and an increased sensitivity of sweat glands to a given neurotransmitter during conditions of higher local skin temperature. In addition to skin and body temperature, thermoregulatory sweating is affected by many other internal factors like gender, physical fitness, menstrual cycle and circadian rhythm as well as external factors like air humidity.
__
Nadel and colleagues were among the first to directly access the relationship between the increase in sweat rate relative to dynamic increases in internal temperature in humans. Later, this concept was confirmed in monkeys in which direct measures of brain temperature were obtained while sweating was assessed by Smiles et al. They concluded that sweating is primarily controlled by central brain temperature and secondarily affected by mean skin temperature. Given these findings, sweating responses are now commonly characterized by the internal or mean body temperature threshold for the onset of sweating, as well as the slope of the relationship between the elevation in sweating and the elevation in internal or mean body temperature as seen in the figure below, as eloquently outlined in the reviews by Gisolfi and Wenger. An increase in the internal or mean body temperature threshold for the onset of sweating and/or an attenuation of the elevation in sweating relative to the elevation in internal or mean body temperature is recognized as impaired sweating responsiveness.
__
The figure above shows the effect of mean skin temperature on the relationship between sweat rate and internal temperature. Initially, as internal temperature increases, sweating does not occur. However, after a threshold is surpassed, the increase in sweat rate parallels the rise in internal temperature, and this threshold can be shifted by mean skin temperature.
_
Humans have the capability of producing a tremendous amount of sweat during prolonged exercise in the heat. For example, the highest reported sweat rate was >3 l/h, although average maximum sweat rates for humans are ∼1.4 l/h. These high rates of sweating cannot be maintained for prolonged periods of time, given findings that 4–6 h of heat exposure decreases the rate of sweating. When sweating is reduced during prolonged heat stress or exercise, the mechanism for this event, despite sustained elevations in internal temperature, is not entirely clear, although both central and peripheral factors have been implicated. For example, dehydration (i.e., hypohydration and elevated plasma osmolality) inhibits sweating primarily through central mechanisms. However, dehydration does not explain decreases in sweating during prolonged exposure to hyperthermic conditions when individuals are adequately hydrated. Under these conditions, decreases in sweat rate may be due to the skin being wet for prolonged periods of time, which can swell the keratinized layer around the sweat duct, thereby mechanically occluding the ducts and reducing sweat secretion.
_
Acclimatization and sweating:
Acclimatisation refers to the increased ability of a person to reduce heat strain due to experience of exposure to heat. It takes two forms: behavioural and physiological. Behavioural acclimatisation is most effective and is mainly gained in the context of the heat exposure. If we go to a hot climate, we soon learn to drink appropriately and keep out of the sun. Physiological acclimatisation involves adjustments to our ability to thermoregulate and allow a greater capacity for and more efficient vasodilatation and in particular, sweating. When people become exposed to heat they increase their ability to sweat. With repeated exposure to hyperthermic environmental conditions, sweat rate is elevated for a given internal temperature, coupled with a decreased sodium concentration in the sweat. Thus, although heat acclimated individuals sweat more, there is less sodium in that sweat. Detailed examination of the effects of heat acclimation on sweating responses show that this exposure decreases the internal temperature threshold for the onset of sweating, resulting in a greater cooling capacity through sweating for a given internal temperature. In addition, Ogawa et al. observed that the number of sweat expulsions per minute, which may be indicative of sudomotor neural activity, increased after heat acclimation, suggesting that heat acclimation may alter central modulation of the sweating response. The maximum rate of sweating increases and its solute composition decreases. From 1 liter sweat production per hour in a non-acclimated individual, an acclimated individual can produce 2 liter of sweat per hour. This adjustment to heat, under normal circumstances, usually takes about 5 to 7 days, during which time the body will undergo a series of changes that will make continued exposure to heat more endurable. On the first day of work in a hot environment, the body temperature, pulse rate, and general discomfort will be higher. With each succeeding daily exposure, all of these responses will gradually decrease, while the sweat rate will increase. When the body becomes acclimated to the heat, the person will find it possible to perform work with less strain and distress. Gradual exposure to heat gives the body time to become accustomed to higher environmental temperatures. Heat disorders in general are more likely to occur among workers who have not been given time to adjust to working in the heat or among workers who have been away from hot environments and who have gotten accustomed to lower temperatures. Hot weather conditions of the summer are likely to affect the worker who is not acclimatized to heat. Be aware that any sudden change in temperature, such as an early summer heat wave, will be stressful to your body. You will have a greater tolerance for heat if you limit your physical activity until you become accustomed to the heat. If you travel to a hotter climate, allow several days to become acclimatized before attempting any vigorous exercise, and work up to it gradually.
__
Non-thermal modifier of sweating:
Sweating from eccrine glands is essential for thermoregulation during heat stress and/or exercise. On the surface, it may appear that control of sweating is simplistic in that people sweat when they are heat stressed. However, like so many physiological systems, this view is not comprehensive, and there are a number of factors that alter the magnitude and composition of sweat as seen in the figure below. These factors should be viewed as fine tuners of the sweating response to form a balance between temperature regulation and nonthermal stressors imposed by the condition (i.e., exercise, dehydration, etc.).
_
The figure above shows schematic illustration of possible nonthermal modifiers of sweating including factors associated with exercise (i.e., central command and muscle mechano- and metaboreceptors), baroreflexes (carotid, aortic, and cardiopulmonary baroreceptors), and osmoreceptors. Arrows indicate neural connections between osmoregulatory, thermoregulatory, and cardiovascular centers.
_________
Exercise and sweating:
Exercise produces heat. Prevention of overheating occurs by transfer of heat to the skin by vasodilation of the cutaneous circulation, and by the cooling effect of evaporation of sweat. Exercise creates an increase in body temperature, which is cooled by sweating. If your body isn’t properly hydrated, it is not able to properly cool itself. Sweat rates of 2 to 3 litres/hour can be expected during short periods of hard exercise in the heat, and an excess of 1.5-2 litres/hour during endurance events. Even in cooler conditions losses are appreciable. During a football game on a cool day (10 deg. C), players can lose up to two litres of sweat, and runners are estimated to lose around 1.2 litres/hour at 6 minute/mile pace on a cool, dry day (double this amount on a hot, humid day). Additionally, fluid is lost via moisture in exhaled air. Except in extreme circumstances, blood Na levels are maintained during exercise. Sweat is mainly composed of water, and Na losses in sweat represent a small fraction of total body content and are readily replaced afterwards by normal food. Unless fluid losses are replaced by drinks, sweating causes progressive depletion of circulating blood volume, commonly called dehydration and a thickening of blood (increased viscosity). This places a strain on the cardiovascular system, with a rise in heart rate in order to maintain adequate blood flow to exercising muscles and vital organs. As blood volume depletes, blood flow to the skin is reduced. As a result, sweating decreases and heat dissipation from the skin is impaired, causing body core temperature to rise, potentially leading to heat stress, collapse and even death. Even low levels of dehydration have physiological consequences. A loss of 2% bodyweight (just 1kg for a 50kg person) causes an increase in perceived effort and is claimed to reduce performance by 10-20%. A fluid loss exceeding 3-5% bodyweight reduces aerobic exercise performance noticeably and impairs reaction time, judgement, concentration and decision making – vital elements in all sports, from pole-vaulting to football. A particular issue for boxers is that dehydration increases risk of brain injury.
_
The person at rest will generate heat of 1 kcal/kg/hr and the person doing significant physical exertion (exercise) will generate heat of 10 Kcal/kg/hr raising body temperature significantly, had no heat dissipation mechanism existed. But since sweating exists as heat dissipation mechanism, the amount of which is dependent on acclimatization, non-acclimated person doing exertion is most likely to be affected by heat illness and acclimated person at rest is least likely to be affected by heat illness, provided ambient temperature & relative humidity are same for both persons. Also, in dry environment & with maximum efficiency, sweating can maximally dispose of 604 Kcal of heat by evaporating 1 liter sweat in 1 hour and if a man having weight of 80 kg is doing strenuous work generating 800 Kcal heat per hour, he cannot dispose of extra-heat despite maximum sweating especially in hot weather when heat loss through convection & radiation is negligible. Such a person is vulnerable to heat illness despite adequate sweating, merely on the basis of strenuous work.
_
You should never wear ‘Makeup’ while working out:
Makeup impedes the egress of the sweat, causing blockages and breakouts. When you wipe off the sweat, you drive the makeup into the open pores. The most important time to clean your face is before you work out, because when you perspire, you tend to wipe your skin, which means you rub in not only your makeup but also the grime, dirt and oils that were there. The oil and particles can clog pores, which open with excessive perspiration, causing inflammatory papules and pustules. Clogged pores and sweat are a breeding ground for bacteria and breakouts. Take off makeup before exercise to prevent clogging your pores with a mix of sweat, dirt, oils and dead skin cells. Stay fresh and dry by showering after exercise and make sure you dry yourself properly to prevent bacteria-causing body odor.
_
Do you have to sweat in order to burn calories? Is sweat the sign of a good workout?
Sweating is definitely a sign that your body is working hard: The more intense the activity, the more heat your muscles produce, and the more you sweat. However, just because you’re sweating, does not mean you are burning calories. Just because you’re not sweating doesn’t mean you’re not burning calories. Caloric burn depends on the intensity and duration of the exercise. The environment plays a big role in how much you sweat. If you exercise in an air-conditioned room, you will not sweat so much because body will cool by conduction, convection and radiation, and whatever you sweat will evaporate fast as air-conditioner reduces humidity of air. Your body can easily cool the heat generated by your exercise. Exercising in a hot and humid room will just exhaust you faster, and you won’t burn as many calories because you will stop working out sooner. On the same note, when you go into a sauna, you’re not burning calories – you are merely sweating. Any weight loss incurred is likely to be water-loss from perspiration, and will be regained as soon as you drink fluids. Sweating is simply a way to cool your body so you don’t overheat. Some people prefer to workout in ways that make them sweat, because they feel like they’ve worked hard. Other folks like to sweat because it’s cleansing, and releases toxins from their body. So now we know, a good workout and a good sweat do not go hand in hand. Different people have different numbers of sweat glands, so even a brisk walk to the mailbox can trigger sweat production in some women. Remember that not everyone sweats the same amount, and sweat can evaporate quickly, especially if you’re exercising outdoors on a nice, breezy day or inside in an air-conditioned gym.
_
Does sweating protect me from overheating?
Not necessarily. In order for sweat to cool us down, it needs to evaporate into the air, and humidity makes that difficult. For this reason, experts warn against overdoing it at hot-yoga studios; when exercising outdoors on a hot, humid day with little-to-no wind; or when sitting in a steam room. The sweating itself isn’t dangerous, but humid environments can make it ineffective. You will still sweat a lot! But sweat beading up on your skin and rolling off onto the ground is not helping you to regulate temperature.
_
Does a fan actually cool objects down, or only humans, by evaporating their sweat?
The fan blows air across your body or for that matter any object at a higher velocity. This increases the forced convection coefficient of air. The convection coefficient is determined experimentally to depend on many factors like temperature, velocity, density and other fluid properties. But the main point is it depends on velocity. Now if the air is still, forced convection does not occur and natural convection is solely responsible for heat transfer. The natural convection coefficient is lower than forced convection and it depends solely on temperature difference. The fan, by increasing velocity of flow, increases forced convection of air and aids heat transfer in the medium. So, it should work on inanimate objects as well by carrying away the heat.
The speed of sweat water evaporation depends on many factors, namely;
– Relative Humidity of the air
– Temperature of the air and the water
– Surface area of the water
– Velocity of air over the water
Evaporation of sweat from the skin surface has a cooling effect due to the latent heat of evaporation of water. Hence, in hot weather, or when body heats up due to physical exertion, more sweat is produced. Typically, all of the sweat does not evaporate, but a part of it runs off your skin. After the sweat has been evaporated, the water vapor must move away from the skin in order that more evaporation can occur; which is dependent on speed of air movement around skin. Fan increases velocity of air over skin and thereby increases speed of evaporation.
So fan cool you down by two mechanisms:
1) increased forced convection of air which aids heat transfer and
2) increased sweat evaporation.
Thus if you are sweating, you cool at a higher rate under a fan. Objects not sweating will cool too, only at a lower rate. Of course, if ambient temperature is more than body temperature, convective heat transfer will be reversed and the only way you cool is by sweating and inanimate objects would become as hot as ambient temperature. Use fan only when windows are open otherwise fan will circulate hot air around you.
_________
Clothing and sweating:
Clothes act as a barrier for transfer of heat and moisture (water vapor and liquid water) between skin and atmosphere in either direction. The type of fiber, the type of fabric construction and the type of garment construction will determine the thermoregulatory ability of clothing. The science of clothing is based on premise that clothes for hot weather would assist in transferring heat and evaporated sweat out of body into atmosphere; clothes for cold weather would assist in retaining body heat and preventing wind-chill; and clothes for monsoon will prevent entry of moisture from atmosphere into skin. Various researchers conducted various studies of different clothing and their effect on thermoregulation. Overall, these experiments indicate that people wearing polyester fibers (non-breathable, non-absorbent) in hot environments tend to have higher body temperatures, sweat more, and experience greater discomfort than those wearing cotton or wool. Some fabrics, as polyester and nylon, conserve the heat and create more perspiration, as contrasted with, for example, cotton, linen and silk. Those who sweat a lot should avoid wearing pure cotton clothing in hot summer. Any clothing that is breathable and also having wicking property will be ideal in hot weather. Loose fitting, light colored, single layer, sleeveless, poly-cotton fabric (65 % cotton with 35 % microfiber wicking polyester) clothes would be ideal in summer. Perspiration-absorbing, Quick-drying New Fabric is a high-performance sportswear material with a refreshing touch and easy wearability which eliminates the perspiration-induced stickiness and clinginess of traditional materials. By scientifically analyzing the movement of water through materials, research effort created a technology which applies the principles of capillary transport to the structure of knitwear to absorb, move, disperse and evaporate perspiration from the skin, thus providing a refreshing feel during exercise. Perspiration-absorbing, Quick-drying New Fabric has gained an excellent reputation for its properties in golf-wear and athletics wear.
_______
Fever and sweating:
In fever, the hypothalamic thermostat becomes set at a higher temperature. The normal blood temperature is therefore sensed as being too low, and temperature-raising mechanisms come into action, accounting for initial pallor and shivering. When the hypothalamic set point is again reset downwards (due to reduction in pyrogens or use of antipyretics), the processes of heat loss through vasodilatation and sweating are initiated. Loss of heat by sweating and vasodilatation continues until the blood temperature at the hypothalamic level matches the lower setting.
_
Myth: Sweat out a fever to recover fast.
Fact: The old adage “sweating out a fever” is incorrect. This is a common fever belief, and unfortunately, it’s misguided. It’s the increase in internal body temperature of a fever that helps fight viral and bacterial infections, not sweating. So, piling on excessive layers of wool blankets and looking for beads of sweat isn’t the right approach. On the other hand, bundling your child in blankets or dressing him or her in lots of clothes may actually raise the fever and cause hyperpyrexia. Dress your child in light clothing, keep the room temperature cool and have him or her sleep with only a sheet or light blanket. The focus during a fever should be on making a person more comfortable. Blankets are fine if they make a person more comfortable, but the goal should be comfort, not sweat.
_______
Sweating and emotions:
Emotional sweating:
Emotional sweating is a physical reaction to emotive stimuli like stress, anxiety, fear and pain that can occur over the whole body surface, but is most evident on palms, soles and in the axillary region. Unlike thermoregulatory sweating, emotional sweating arises independently of ambient temperature and decreases during sleep and relaxation. When emotional stress causes a reaction from your sympathetic nervous system, it primarily affects the Eccrine glands on your face, palms, soles of your feet, and in your armpits. It also causes your skin vessels to constrict. The prevailing theory is that this is a very efficient way to cause several reactions using the same pathways and glands. Emotional sweating is thought to be an atavistic function that was important when hunting animals or fighting enemies. Physiologic amounts of sweat on the palms and soles can improve friction by controlling the humidity of the stratum corneum, leading to an improved grip. Generalized sweating cools the body when intense physical activity is expected. In addition, increased eccrine sweat output in the axillae [armpit] produced by emotional stimuli will allow natural odors from prior apocrine gland secretion to aerosolize and function as pheromone signals. When you’re stressed, you sweat from both the odor sweat glands and the water sweat glands. But the odor sweat glands get a head start which means that as soon as you start to feel stressed, you could be emitting a scent that’s detectable by others. A study published in the journal PLoS One showed changes in brain activity when participants were exposed to the sweat of other people in an emotionally tense situation—in this study’s case, skydivers. The participants had a subsequent chemical reaction to the sweat, which caused them to become more alert to potential threats, and display higher levels of vigilance. The purpose of stress-triggered sweat mostly remains a mystery, but now scientists are piecing together new clues about the role it might play in the way people function. Although most of us try to avoid sweating in public, some scientists believe it has an evolutionary role in sending warning signals to people around us. The body odor of a stranger provokes the brain to negatively interpret social stimuli, even friendly facial expressions, recent research has shown. Meanwhile, the scent of a family member can help calm a person who is under stress, according another study. Emotional sweating of palms and soles already occurs in babies. Evolved as a fleeing reaction in different mammals, palmoplantar sweating increases friction and thus prevents slipping during running or climbing in stressful situations. Investigations of Kerrassidis indicate that sweating of palms and soles is mainly induced by emotive stimuli, not by high ambient temperature. Like thermoregulatory sweating, emotional palmar and plantar sweating involves eccrine sweat glands that are typically activated by cholinergic fibres of the sympathetic nervous system.
_____
Why does anxiety cause excessive sweating?
There are four main reasons why anxiety can cause excessive sweating:
1. Anxiety (behaving anxiously) activates the stress response, which causes the body to increase perspiration:
2. Stress-response hyperstimulation (an overly stressed body) can cause erratic sensations and symptoms, including involuntary episodes of sweating.
3. Stress-response hyperstimulation can intensify our perception of, and reaction to, danger.
4. Reacting to, or being anxious about, your excessive sweating can cause additional stress responses, which can create and/or aggravate stress caused symptoms, including excessive sweating. Containing your anxiousness and keeping yourself calm can prevent unnecessary stress responses and their effects.
_
How to get rid of excessive sweating during anxiety?
•Relaxed breathing – can help calm down the body and nervous system, which can make them less reactive and help bring an end to an active stress response. Relaxed breathing also helps reduce stress. The less stressed your body is, the less likely it will produce involuntary symptoms, such as episodes of excessive sweating.
•Contain your anxious thinking – can reduce the frequency and degree of stress responses, which can also calm down an overly reactive body and nervous system.
•Visualize being calm and relaxed – calming yourself down can keep your body and nervous system from over reacting, and sometimes from misbehaving due to stress-response hyperstimulation.
•Passive acceptance – passively accepting this symptom in the short term reduces stress, and reducing stress helps the nervous system to calm down and become less reactive. The less reactive you are to excessive sweating, the better off you’ll be.
•Reduce your body’s stress – reducing the body’s stress is an important part of overcoming symptoms of stress-response hyperstimulation. Again, the less stressed your body becomes, the less likely it will produce involuntary symptoms of stress, including excessive sweating.
•Get regular good sleep – regular good sleep can play an important role in keeping the body calm, relaxed, and unstressed, and reduce stress-caused symptoms, such as excessive sweating.
•Avoid stimulants – since stimulants can irritate the nervous system, eliminating them can help the nervous system be calmer, thus less reactive.
•Wear less restrictive clothing – less restrictive clothing can help cool the body and hide wetness from excessive sweating.
•Wear clothes that breathe – can help cool the body, which can prevent episodes of excessive sweating.
•Be sure to keep your body hydrated – this can help prevent the body from becoming dehydrated due to many episodes of excessive sweating.
______
Excessive sweating and flushing:
What happens when you flush or blush? To answer this question we need to briefly consider the very extensive network of tiny blood vessels that are embedded in the skin. Each of these blood vessels contains smooth muscle in its walls. When we are cold the smooth muscle in the walls of the superficial blood vessels contracts which reduces the volume of blood passing through those vessels. This is referred to as vasoconstriction. This is a heat conservation measure that diverts warm blood from the surface of the body to the core. That is the reason why the surface of the skin looks white and feels cold when the ambient temperature is low while at the same time the core body temperature remains normal. In contrast, when the smooth muscle in the blood vessels relaxes the diameter of the vessel increases and the volume of blood passing through the blood vessel also increases. This is referred to as vasodilation. In this situation the skin feels warm and may have a pink or red colour. Vasodilation and vasoconstriction are both controlled by the ANS (autonomic nervous system), which means that both of these functions are outside of voluntary control. Vasodilatation is the physiological mechanism that produces flushing or blushing. Sweating is also controlled by the ANS and the cause of hyperhidrosis has been traced to over activity in the sympathetic component, as opposed to the parasympathetic component, of the ANS. Thermoregulatory sweating is accompanied by skin vasodilation. It is important with both of these embarrassing problems to exclude the possibility that the person might be suffering from an underlying condition that is giving rise to the sweating or flushing. For example, some people sweat excessively because they are obese or they may be suffering from an overactive thyroid gland. Such people may have sweating with flushing. The menopause is another obvious cause of both flushing and sweating. Flushing and sweating can also be prominent physical symptoms associated with the mental health condition known as social phobia. Finally it needs to be emphasised that flushing is almost never due to a serious medical condition with one notable exception, which is the rare condition known as carcinoid syndrome.
Medication causing flushing:
Medication may also give rise to flushing. The list of possible culprits includes various hormonal treatments for prostate cancer; gylceryl trinitrate, which is used in the treatment of angina; tamoxifen, which is used in the treatment of breast cancer; raloxifene, which is used for treating osteoporosis; calcium channel blockers, which are used to treat high blood pressure and chlorpropamide, which is used for treating diabetes and can cause flushing if the person takes alcohol concurrently.
_
Blushing:
Blushing is the reddening of a person’s face due to psychological reasons. It is normally involuntary and triggered by emotional stress, such as that associated with embarrassment, anger, or romantic stimulation. Severe blushing is common in people who suffer social anxiety in which the person experiences extreme and persistent anxiety in social and performance situations. Blushing is generally distinguished, despite a close physiological relation, from flushing, which is more intensive and extends over more of the body, and seldom has a mental source. Evidence for skin vasodilation mechanisms was reported by Mellander and his colleagues. Alpha-adrenergic blockade with phentolamine had no influence on the amount of blushing in frequent or in infrequent blushers, indicating that release of sympathetic vasoconstrictor tone does not substantially influence blushing. This result was expected since vasoconstrictor tone in the facial area is known to be generally low. Beta-adrenergic blockade with propranolol on the other hand decreased blushing in both frequent and infrequent blushers. This suggests stimulation of beta adrenergic receptors in skin blood vessels caused blushing. Although flushing and blushing are similar, flushing is accompanied by sweating and usually physical in origin while blushing is not accompanied by sweating and psychological in origin.
_
A young woman blushing and covering her face:
Note no sweating while blushing:
______
______
Sudden, Severe Sweating:
Numerous conditions may cause sudden, severe perspiration. Sudden and severe sweating may indicate a serious underlying health condition or disorder. If you perspire for no apparent reason, visit your physician for an evaluation.
1. Hyperthyroidism:
Common signs and symptoms associated with hyperthyroidism include sudden and severe sweating, unexplained weight loss, elevated heart rate, increased appetite, nervousness, anxiety and irritability, increased heat sensitivity, difficulty sleeping, fatigue, weight loss and muscle weakness.
2. Panic Attack:
A panic attack is a common cause of sudden, severe perspiration. This condition causes a sudden bout of intense fear that manifests for no apparent reason. Panic attacks often cause extreme physical reactions. Common signs and symptoms associated with a panic attack include excessive sweating, the feeling of impending doom, elevated heart rate, trembling, shortness of breath, nausea, abdominal cramping, chest pain and dizziness.
3. Heart Attack (acute myocardial infarction):
Common signs and symptoms associated with a heart attack include sudden, severe sweating; chest pain, pain that radiates to the jaw, teeth, shoulder, arm and back, shortness of breath, fainting, nausea and vomiting. Sweating during physical activity or in hot weather is healthy. But when individuals begin perspiring while experiencing discomfort in their chest, arm, neck or jaw — with little or no exertion — it could be the onset of a heart attack. Sweating may be a key variable in the symptom cluster prompting individuals to seek treatment. But the research could not determine whether sweating is an indication of a more serious heart attack.
4. Hypoglycemia (low blood sugar): Symptoms of hypoglycemia include hunger, tremors, sweating, confusion, palpitation, anxiety and dizziness. Diabetic on treatment may get hypoglycemia due to missed meals or excess medications.
______
______
Sweating benefits:
Sweating is a natural, essential body process designed to help your body stay cool. But some may wonder whether it’s beneficial to encourage your body to sweat more for reasons beyond temperature control. The New York Times recently published an article that concluded “sweating, per se, provides no health benefits” aside from preventing overheating, but many other experts, believe there’s far more to the story than this. Aside from its temperature-regulating effect, sweating has been shown in recent studies to excrete toxins, including arsenic, mercury, lead, and cadmium, as well as rev up circulation and clear the pores. Still, many experts contend that perspiration’s key benefit is preventing overheating — not ridding our bodies of unwanted pollution — noting that sweat’s detoxification powers are mild compared with that of our kidneys and livers. Researchers have found that exercise is not the only way to reap these rewards — saunas can be a part of your sweat-inducing regimen. Infrared saunas, in particular, which heat the body without warming the surrounding air, can provide such benefits as improved circulation and pain relief. Scientists are exploring the use of this therapy in treating health issues like rheumatoid arthritis and high blood pressure. Sweating is the body’s built-in mechanism for keeping cool, but some experts believe that, because it opens up and unclogs the pores, perspiration is also a secret weapon for keeping our skin looking its best. However, if that’s true, then why does sweat sometimes seem to aggravate conditions like acne and eczema? When you work up a sweat, is that healthy glow really healthy? The answer to this question isn’t a simple “yes” or “no”. For one thing, the process of perspiring itself causes your pores to open up as the sweat makes its way through layers of skin to the surface. Many aestheticians actually use steam during facials to achieve this same effect, so they can prep the skin for deep cleaning and extractions. Sweat also may play a role in fending off foreign substances. Some recent studies — including one conducted at Eberhard-Karls-University at Tubingen in Germany — suggest that perspiration contains a natural antibiotic known as Dermcidin. Dermcidin can help kill bacteria, including E. coli and Staphylococcus aureus, on the skin’s surface. But here’s the catch: Leaving sweat untended to for too long can end up doing more harm than good because it can lead to conditions like miliaria. More commonly known as prickly rash or heat rash, miliaria occurs when the eccrine glands become blocked, which results in a series of red bumps. Your best bet for keeping your pores clean and unclogged is to always wash your face and body as soon as possible after sweating. If your skin is easily irritated, you should probably change sweaty clothes and sheets right away, too. Sweating can help lessen breakouts by flushing out clogged pores. When you sweat, your pores open up, and dirt and oil that are congesting them are washed away. Here’s where the timing issue comes in. Even though this debris is flushed out of the pores, it still sits on the skin until the face and/or body is properly washed. Wait too long, and all that dirt can re-clog your pores. So to ensure your sweat is working for you and not against you, make sure to shower as soon as you’ve finished working out or come in from the heat. Don’t have time for a shower? Try carrying around some baby wipes or cleansing cloths to wipe skin clean after your pores have been purged. So maybe the answer to whether sweat is your skin’s friend or foe isn’t a simple one, but at least now you know a trick to keep it on your side: Let perspiration take its natural course, but once it’s made its way to the surface, make sure to follow up immediately with proper cleaning and care.
____
The figure below summarises non-thermoregulatory sweat benefits:
____
Let me go in detail about non-thermoregulatory sweat benefits:
_
1. Germ Fighters:
While studying proteins involved in skin cancer, a team of researchers discovered a potent natural antibiotic called dermcidin. The researchers learned that sweat glands constantly excrete this antibiotic. Persistent skin washing can remove this natural protective barrier. Though a long shower after a hot sweaty day sounds perfect, it may limit your defence against germs. University of California researcher Tomas Ganz notes that bacteria thrive in hot, moist conditions. Dermcidin can limit what thrives on our skin, reducing our risk of infection. But Ganz cautions that being sweaty all the time does not guarantee protection: It depends on how much dermcidin a person exudes. Dermcidin is an antimicrobial peptide with a broad spectrum of activity that is expressed in eccrine sweat glands and secreted into sweat. These peptides are positively charged and attract negatively charged bacterial, enter the membranes of bacteria, and break them down. In the average healthy person, research shows that sweating leads to a reduction of viable bacteria on your skin surface, which may lower your risk of skin infections. In fact, one study suggested that people with atopic dermatitis, who have recurrent bacterial or viral skin infections, may be lacking dermcidin in their sweat, which may impair the innate defence system in human skin. A 2013 study published in the Proceedings of the National Academy of Sciences proved dermcidin is a highly effective tool to fight not only tuberculosis germs but other dangerous bugs. The researchers believe these natural substances are more effective in the long-term than traditional antibiotics because germs are not capable of quickly developing resistance to them. The natural antibiotic is naturally activated in salty, slightly acidic sweat.
_
2. Healing Powers:
University of Michigan researchers discovered that sweat glands play a role in the wound-healing process, including recovery from scrapes, burns, and ulcers. In a study published in the American Journal of Pathology, Laure Rittié, Research Assistant Professor of Dermatology, notes that sweat glands are understudied and that they may hold the secret to speeding up wound repair. The study found that eccrine glands store an important reservoir of adult stem cells that can quickly take action when a wound occurs. Rittié explains that sweat glands are understudied because they are unique to humans and not present in animals, which are commonly studied in laboratories.
_
3. Happiness and pain relief:
The act of sweating alone doesn’t ward off bad moods, but a good sweat in the gym or outdoors increases endorphin levels – those feel-good hormones that contribute to a runner’s high. Endorphins are related to positive mood and an enhanced sense of overall well-being. The proof is in the smiles after the sweat! Those exercise endorphins not only stimulate your brain’s mood enhancers, they also are natural pain relievers.
_
4. Prevents kidney stones:
One unexpected benefit from sweating is actually a great preventative method against kidney stones. As your body temperature rises, your body will automatically perspire to release a salty liquid from your sweat glands to help cool you down. This salt would otherwise enter your kidneys, where it would assist in the creation of painful kidney stones. The theory is that the more you sweat out the salt, the less chance it has entering your kidneys. Research has also shown that people who exercise, and therefore sweat more, have a lower risk of kidney stones. People who sweat more also tend to drink more water, which is another way to lower your risk of kidney stones. A study presented at the 2013 American Urological Association conference in San Diego, Calif., found even walking for a couple of hours a week could cut the risk for developing kidney stones. Mild to moderate activity changes the way the body handles nutrients and fluids that affect stone formation. Sweating helps flush out the system more efficiently because it demands more hydration from the body.
_
5. Toxin excretion in sweat:
Sweating has long been known as a source of bodily, if not also spiritual “cleansing.” But until recently, very little ‘scientific’ confirmation existed proving that using heat and/or exercise to facilitate perspiration-induced detoxification actually works the way that many natural health advocates claim. With the Rise of Biomedicine and its so-called ‘evidence-based’ model of determining what is true and thereby legal to practice, this conspicuous lack of clinical proof has resulted in a veritable inquisition against those who claim that bodily detoxification through sweating is anything more than a form of ‘quackery.’ Your skin is a major organ of elimination, but many people do not sweat on a regular basis. The use of sweating as a form of detoxification is downplayed by modern medicine, yet it has been valued as a form of cleansing since ancient times.
_
A 2011 study published in the journal Archives of Environmental and Contamination Toxicology found many toxic elements appeared to be excreted through sweat. Induced sweating appears to be a potential method for the elimination of many toxic elements from the human body. Researchers believe sweat analysis could be considered as an additional method for the monitoring of toxic elements in humans rather than just blood and/or urine testing.
_
Why Blood and Urine Analysis may fail to reveal the Problem:
A 2012 meta-analysis was published in the Journal of Public and Environmental Health. The study titled, “Arsenic, cadmium, lead, and mercury in sweat: a systematic review,” was performed by researchers from the Children’s Hospital of Eastern Ontario Research Institute, Ontario, Canada, and was based on a review of 24 studies on toxicant levels in the sweat. The researchers discovered the following:
In individuals with higher exposure or body burden, sweat generally exceeded plasma or urine concentrations, and dermal could match or surpass urinary daily excretion.
1. Arsenic dermal excretion was several fold higher in arsenic-exposed individuals than in unexposed controls.
2. Cadmium was more concentrated in sweat than in blood plasma.
3. Sweat lead was associated with high-molecular-weight molecules, and in an interventional study, levels were higher with endurance compared with intensive exercise.
4. Mercury levels normalized with repeated saunas in a case report.
The review found that toxins including arsenic, cadmium, lead, and mercury are excreted in sweat and noted: “Sweating is not only observed to enhance excretion of the toxic elements of interest in this paper, but also may increase excretion of diverse toxicants, as observed in New York rescue workers, or in particular persistent flame retardants and bisphenol-A (BPA). …Optimizing the potential of sweating as a therapeutic excretory mechanism merits further research.” The researchers concluded, “Sweating deserves consideration for toxic element detoxification.”
_
Counter-view:
Perspiration is not used for detoxification.
A common misbelief and misinterpretation is that sweating is useful for the excretion of toxic agents and purification. Toxic agents are solely filtered and excreted by the kidneys or the liver. Only in rare cases, when both organs are severely affected by illness, the body would use the skin to emit harmful substances (e.g. yellow jaundice). Scientists know that human sweat may contain minimal traces of urinic substances from time to time but the amount is very minuscule – it could never be used for an efficient excretion of bodily waste products. Some toxins such as mercury create legitimate concerns. But there’s no evidence that you sweat out heavy metals. Donald Smith, a professor of environmental toxicology at UC Santa Cruz, explains: “Almost all toxic metals in the body are excreted through urine or feces. Less than 1% are lost through sweat. In other words, you’ll do far more detoxifying in the bathroom than you ever could in a sauna.” Regarding the specific claims made for sauna detox, Smith has one word: “Baloney.”
_
6. Lower Blood Pressure:
While losing too much sodium by sweating can be problematic if you’re eating a low-sodium diet, excreting some sodium through sweat can actually help offset a higher sodium diet. Because high-sodium diet can cause high blood pressure and increase your risk for heart disease, sweating can help lower high blood pressure. The School of Medicine and Public Health at the University of Wisconsin-Madison reports that sauna-induced sweating is a healthy way to reduce high blood pressure, as long as you abide by recommendations of 15 to 30 minutes of sauna use three or four days per week. Exercise-induced sweating also helps keep blood pressure in check.
_
7. Axillary sweat and pheromones: Sweat may play a role in nonverbal human communication:
While humans are highly dependent upon visual cues, when in close proximity smells also play a role in sociosexual behaviors. Pheromones are so subtle that we are not consciously aware of smelling them. An inherent difficulty in studying human pheromones is the need for cleanliness and odorlessness in human participants. Experiments have focused on three classes of putative human pheromones: axillary steroids, vaginal aliphatic acids, and stimulators of the vomeronasal organ. Several studies have been conducted that have reached different conclusions, but some pheromone effects seen in other mammals are definitely present in humans. Many contradictory studies failed important aspects of pheromone experiments, such as common odor or musk control, so these studies are disregarded. Although exact conclusions differ, most studies have found that human sweat or putative pheromones increase physiological arousal, one way or another. Pheromone like compounds are believed to be secreted via axillary (armpit) glands called apocrine glands, which create a nutritional environment for bacteria. The compounds can be further affected by the microbial flora, which may separate compounds to enable their transmission or make the steroid pheromones more odorous (Hays, 2003). There are differences between men and women in the types of glands, secretions and even microbial flora present in the axillary environment, suggesting a sex-specific role. Most of these glands do not become active until after puberty, suggesting a role in sexual communication. (Hays, 2003) Pheromone-like compounds are also found in salivary, seminal and urine secretions, but studies tend to focus on the most accessible: axillary sweat. Various studies have suggested that pheromones can communicate information about genetic compatibility, sexual orientation, emotions and gender by affecting humans unconsciously and physically. Reproduction is the most important aspect when it comes to being a successful species, comparable only, perhaps, to survival. Of course it makes sense, then, that there are mechanisms beyond our control that urge us not only to procreate, but with mates that will result in the most successful offspring. The “sweaty-T-shirt study,” for example, conducted by Swiss biologist Claus Wedekind in 1995, found that women rated most pleasant the scent of men whose genes were most unlike their own, ensuring a stronger immune system for their offspring. Sweat can also speak poorly of us: Research published in PLOS ONE in 2013 shows that women’s stress sweat can make men perceive them as less confident, competent, and trustworthy; in other words less biologically suitable for procreation. And a report published in Psychological Science finds that we can detect other people’s emotions, thanks to sweat. In fact, researchers from Utrecht University in the Netherlands suspect that sweat’s scent actually makes emotions contagious. In the study, underarm sweat was collected from men as they watched scary scenes from The Shining and gross-out clips from the TV show Jackass. When women smelled the “fear sweat” samples, they opened their eyes wide and had a frightened expression. When they smelled the “disgust sweat,” they grimaced.
_
Axillary sweat actually carries emotional messages:
It turns out that emotion-induced sweating is an important tool for communication. In fact, the scents that we detect in sweat can tell us a lot about how others are feeling. In one experiment, a quintet of Utrecht University psychologists collected sweat samples from 10 men as they watched videos designed to evoke feelings of fear (excerpts from The Shining) or disgust (excerpts from MTV’s Jackass). In order to avoid odour contamination, the volunteers agreed to forego smelly foods, alcohol, smoking, and “excessive exercise” for two days prior to their sweat donation session. Then, 36 women were asked to see whether they could detect any emotional cues hidden in the sweat samples. The researchers found that when women were exposed to fear-derived sweat samples, their own facial expressions suggested fear as well. And when they were exposed to disgust-based sweat samples, their faces mirrored that emotion too. (Sweat collection pads that remained unused served as controls; these didn’t cause the participants to show any predictable sort of facial expression.) That suggested to the researchers that sweat appears to be an effective means of transmitting an emotional state from one person to another. Importantly, the facial expressions the women made while sniffing the sweat were completely independent of their subjective perceptions of the odours’ pleasantness or intensity. So they might show a look of disgust even if they reported a particular sweat sample as smelling pleasant. Similar patterns have also been seen in other experiments. In 2006, Rice University psychologists discovered that women exposed to sweat samples collected from fearful donors (this time the sweat came from both men and women) performed better on a word association task than women exposed to sweat produced by people watching neutral videos, or by sweat pads that contained no sweat at all. The fear-related cues gave them a heightened awareness of their environment. And in 2012, psychologists and psychiatrists from the State University of New York extracted sweat from the t-shirts of 64 donors. Half of the donors jumped out of an aeroplane for the first time, while the other half exercised really hard. People who sniffed the sweat of scared skydivers became aroused in response to angry faces, but also to neutral and ambiguous ones. Psychologists refer to it as vigilance; the free-fall-invoked sweat induced participants to pay attention to whatever possible subtle social cues that they might otherwise have overlooked. Those who sniffed the sweat of exhausted exercisers only became more alert when viewing angry faces, as would be expected under any circumstance. Yet another experiment conducted by German psychologists and neuroscientists found that sweat from anxious men (who participated in a high ropes course) caused women to make riskier decisions – after spending more time deliberating on their choices – in a computer game designed to assess risk-taking behaviours. None of these studies indicate whether people are aware that other people’s sweat has altered their own cognition or behaviour, but they do suggest that sweat might, in some cases at least, communicate important information about our internal mental states. They also suggest that we use the information contained in other people’s sweat to better understand our surroundings. Perhaps that’s not surprising. Our species may be adapted to verbal and linguistic communication, but language is a fairly new item in our social toolkit. It seems reasonable to imagine that our ancestors took advantage of the olfactory data constantly flowing into their noses – and that they passed the skill down to us. Indeed, people seem better able to identify emotions in virtual humans on a computer screen when the animated characters visibly perspire. And not only that, but the addition of sweat seems to allow people to perceive the intensity of a displayed emotion. Sweat, in other words, isn’t just a smelly signal, but a visual one too. Sweat, in the end, is more than just the body’s air conditioning system. It just might be an emotional weather vane as well, a tool used for broadcasting our innermost feelings to our friends and family.
_
8. Sweating prompts Heart Attack Care:
Sweating may be a Key Factor in Heart Attack Victims’ seeking of Treatment:
Sweating appears to be the symptom that prompts more people suffering a heart attack to get to the hospital, researchers have discovered. Heart attack patients often deny symptoms, [thereby] delaying treatment, but those who sweat are more likely to seek treatment earlier, according to Catherine Ryan, PhD, RN, project coordinator of medical-surgical nursing in the department of nursing at the University of Illinois at Chicago. Remember earlier the treatment better is the outcome in heart attack.
_
9. Sweating and acne:
Sweat’s basic function is to keep you cool when the body begins to heat up, which is actually accomplished when the sweat evaporates off your skin. Meanwhile, the oil which every acne patient needs to reduce is sebum. Sebum is made up of various oils like squalene, triglycerides, and wax esters. It has a completely different function to sweat; its main job is to lubricate your skin and prevent it from being damaged by outside forces such as sunlight. It is sebum, not sweat, that is largely responsible for acne. Possibly the reason why so many people get confused is that both sweat and sebum increase on a hot day; sweat to keep you cool, and sebum to provide additional lubrication “defences”. Nevertheless, the two are completely different and you should never confuse them. Sweat is very rarely a cause of acne. Dermcidin in sweat kills acne bacteria. But what does that mean for people who are prone to acne? It might help, but it doesn’t necessarily hurt, say the experts at the Children’s Hospital of Colorado (CHC). Sweat in itself neither fights acne nor causes it; but the increased blood flow, unclogging of pores from sweating, and stress reduction that result from exercise may all benefit the acne sufferer, says the CHC. Your pores open up when you sweat and that releases the build-up inside them. Sweat purges the body of toxins that can clog pores and plague the skin with pimples and blemishes. These skin benefits only apply to mild or moderate sweating. Excessive sweating can actually predispose individuals to skin infections such as warts and tinea. Eczema and rashes occur more often in people with hyperhidrosis.
________
Sweating and weight loss:
Most people associate a good, hard sweat with excessive calorie burning. That’s why those who aspire to lose weight drive themselves to perspire to lose weight. Burning calories and sweating are related activities, so it’s understandable why one has become synonymous with the other. Yet when you’re sweating a river during intense exercise, it isn’t the sweat that is burning away all those calories. Sweat happens. Throughout every day of your life, you exude a watery blend of urea and salts from your pores. Most people presume that when you sweat, you lose weight. It’s true that when you sweat, you shed some weight. However, most of the weight you lose is water weight, and you regain that as soon as you rehydrate. Any real weight loss that occurs when you sweat happens because of what you are doing that makes you sweat, and not because of the sweating. You can lose weight sweating, but don’t let that confuse you into thinking that you’re burning calories and fat weight. Sweat comes from water in your body. When you get those sweat glands going, you’ll definitely lose some weight, but it will all be water weight. When you drink water after an intense workout, your body will soak it up like a dry sponge, causing you to gain back the weight you sweated off. According to the Scientific American website, a 300-lb. football player loses an average of 3 percent of his body weight during a football game. This results in a loss of 1.08 gallons of fluid. While it may appear that the sweating caused a significant weight loss, the water weight that you lose during exercise is immediately returned afterward when you rehydrate. A number of sweating devices such as sauna belts claim to increase the number of calories that you burn. These claims are generally based on the assumption that the added heat increases your body’s metabolic rate, resulting in an overall acceleration of the number of calories your body burns in a natural state. These claims are largely untested, however, and have not been proven in peer-reviewed studies. According to the Military Fitness Center, excessive sweating has no useful purpose in weight loss. It may also lead to a number of health problems such as heatstroke, extreme loss of electrolytes, kidney damage and cardiovascular-related emergencies. You should always hydrate yourself before and after any vigorous exercise, and should maintain a healthy level of electrolytes by consuming healthy amounts of fresh fruits and vegetables.
_
How many calories are burned by sweating itself?
When you’re involved in a heart-pumping workout, your body’s core temperature starts to heat up. It is the work that you’re engaging in that eats up calories; sweating is just a side effect of the workout. It’s your body’s reaction to the rise in temperature, an attempt to cool itself down by releasing the heat through your pores in the form of moisture. That moisture cools you as it evaporates from your skin. Sweating isn’t completely non-productive, however, when it comes to burning calories. In the 2008 book “The Fiber 35 Diet,” Brenda Watson writes that “the body uses 0.568 calorie to evaporate 1 gram of sweat,” meaning that the act of sweating, separate from the activity that causes sweating, actually does contribute to calorie burning, although it’s in an extremely minuscule amount. In other words, evaporation of one liter sweat causes loss of only ½ Kcal by the act of sweating.
_
Myth of Sweat Suits:
For decades, many people have used sweat suits, garbage bags or saunas in order to lose weight quickly. You will lose weight in the form of sweat, which is water and electrolytes, but you will gain it back as soon as you eat again or drink water. This myth seems to have spread through the wrestling, boxing, and other sports gyms where guys need to lose a few pounds in order to make a weight class. But sweating excessively has no useful purpose in health weight loss. The dangers of sweating to lose weight are severe — they include overheating (heatstroke), extreme loss of electrolytes (kidney damage/death), and other cardiovascular related emergencies.
_
Hyperhidrosis and weight loss:
There is no evidence that hyperhidrosis cause any hyper metabolic situation in which patients can lose weight because of excessive sweating. Although some of the sweat of hyperhidrosis runs off; some of them may be evaporated leading to unintended heat loss and so food energy will be utilized for generation of this unintended heat loss resulting in minor weight loss provided diet, metabolism and physical activity remain same. For example, if you have 4 liters of non-thermal excessive sweat in a day and half is run off, still it will lead to body inadvertently losing 1200 Kcal energy from evaporating 2 liters of non-thermal sweat per day, which has to be supplied by burning 0.3 pound of fat as to lose one pound of fat you need to create a deficit of 3,500 calories. In other words, people who have hyperhidrosis may lose weight unless they eat extra or reduce physical activity. This is because some of the excessive non-thermal sweat may evaporate leading to unintended heat loss from body resulting in increased caloric expenditure of body.
________
Sweating in a sauna:
The act of sweating to improve your health is an extremely old one. The Romans, the Aboriginals, and the Russians have all used saunas and steam baths for medicinal purposes during their history. The Finns have always been particularly obsessed with the idea. Centuries ago they used to light a fire underneath rocks to create smoke, and then they would throw buckets of water on top to turn it to steam. Then they would close off the room with wood and sit around in a makeshift sauna. The smart idea these civilisations had was that sweating helps to remove toxins and other impurities from the human body. Many people choose to enjoy a few minutes in a sauna every once in a while, to relax and to get a good sweat going. The difference between an infrared sauna and the traditional Finnish-style saunas is that the latter heats you up from the outside in, like an oven. The infrared sauna heats you from the inside out, raising your body’s core temperature and resulting in a deeper, more cleansing sweat. It’s said that using an infrared sauna will cause you to produce a sweat that is composed of 20 percent toxins, compared to only 3 percent toxins by using a traditional sauna. Recent research has even shown that regular sauna use correlates to a reduced risk of death from any cause, including lethal cardiovascular events. Men who used the sauna (Finnish-style, dry heat sauna) seven times per week cut their risk of death from fatal heart problems in half, compared to those who only used it once each week. One mechanism for this beneficial effect is thought to be related to the fact that sauna therapy places stress on your heart and body similar to that of exercise. Keep in mind that sweating, especially heavy sweating, will cause your body to lose valuable fluids and electrolytes. Be sure to stay well hydrated if you’ve been sweating heavily and replace your water loss by drinking water.
_
Health Benefits of a Sauna:
Sweat Toxins Out:
Sweat does more than regulate body temperature. Many of the tens of thousands of man-made chemicals in our environment make their way into our food, water and air. There are ways to get rid of stored toxins, and one of them is sweating. Sweating mobilizes toxins stored in the fat and enhances their elimination. If you’ve ever been around a heavy smoker or drinker, you know they reek of nicotine or alcohol—it literally pours out of their skin in their sweat. The same is true, although less obvious, of other toxins. Here’s where a sauna comes in. On an average day, your eccrine glands put out about a liter of sweat. But when you hang out in a sauna, they pump out that much in 15 minutes.
Study of 9/11 Rescue Workers:
One of the most recent studies of this program is the New York Rescue Workers Detoxification Project. When the World Trade Center buildings collapsed on September 11, 2001, massive amounts of toxins were released, and the firemen, policemen, and other rescue and cleanup workers bore the brunt of this environmental disaster. As you might expect, acute respiratory distress was common in this group. However, over the subsequent weeks and months, a significant number of these individuals experienced a wide range of health issues, including gastrointestinal complaints, worsening pulmonary problems, depression, irritability and cognitive disorders. From September 2002 through September 2005, more than 500 of these rescue workers, the majority of them firefighters between the ages of 35 and 45, completed this sauna detox program, and the results were astounding.
Before Treatment (which averaged 33 days):
•They missed a median of 2.1 days of work per month,
•Had 4.4 days of limited activity,
•Symptom severity scores—which rated 10 systems, including skin, respiratory, emotional, cognitive and musculoskeletal—were high,
•And half of the participants were taking drugs to manage their symptoms.
After Treatment:
•The number of days of missed work or limited activity fell to 0.2,
•Symptom scores dropped dramatically,
•And 84 percent of participants had discontinued all their drugs because their symptoms had cleared up.
•They also had significant improvements in thyroid function, balance, reaction time and even IQ!
_
Cardiovascular Benefits of a Sauna:
The benefits of a sauna extend beyond detoxification; it’s also good for your heart. Sitting in a sauna has effects akin to mild exercise. The heart gets a gentle workout while the heat of the sauna dilates the capillaries and improves blood flow. In a study published in the Journal of the American College of Cardiology, 15 minutes in a sauna a day for 14 days improved the function of the endothelial cells lining the arteries by 40 percent. Japanese researchers have found that sitting in a sauna is particularly helpful for congestive heart failure. After taking daily saunas for four weeks, 13 of 15 patients with serious heart failure had significant decreases in blood pressure and improvements in ejection fraction (a measure of the heart’s pumping ability), exercise tolerance and oxygen uptake.
_
Additional Benefits of a Sauna:
Other conditions for which sauna is proving to be helpful include:
•Chronic fatigue
•Mild depression
•Rheumatoid arthritis
•Musculoskeletal pain
•Skin conditions
And don’t forget this very important point: Sauna just makes you feel good.
_
Acclimatization through sauna:
In fact, the concept of “hyperthermic conditioning,” or acclimating yourself to heat independent of aerobic physical activity through sauna use, has been shown to boost exercise endurance. It does this by inducing adaptations in your body that make it easier for you to perform when your body temperature is elevated. Stated another way: as your body is subjected to heat stress, it gradually becomes acclimated to the heat, prompting a number of beneficial changes and adaptations.
These adaptations include:
•Increased plasma volume
•Increased blood flow to your heart and muscles (boosting athletic endurance)
•Increased muscle mass due to greater levels of heat-shock proteins and human growth hormone (HGH)
Sauna use combined with exercise may lead to even greater, synergistic increases in HGH as well as brain-derived neurotrophic factor (BDNF), which can prompt the generation of new brain cells.
_
A quick overview of dangers of the Sauna:
• Overheating (heat exhaustion and heat stroke)
• Dehydration
• Using the sauna while drinking or after drinking alcohol
• Depleting your electrolytes or minerals through sweating
It is, as well, not recommended to use the sauna during an acute illness or injury where it may interfere with the natural healing process. For example, it is recommended to avoid sauna use during the first 48 hours of an acute sprain-type injury.
_
Avoid sauna use completely in the case of:
• Stroke (type caused by bleeding into the brain)
• Severe aortic stenosis
• Recent myocardial infarction (heart attack)
• Unstable angina pectoris
• Lupus erythematosus, if you are on steroids (interferes with blood circulation)
• Brain tumors
• Multiple sclerosis
• Silicone implants
_
Sauna suit:
Sauna suit is a garment made from waterproof fabric designed to make the wearer sweat profusely and they are typically made of PVC or coated nylon cloth. A sauna suit is commonly worn during physical exercise as an aid to weight loss, for example by boxers, MMA fighters or wrestlers, who wish to qualify for a specific weight class. The body temperature elevation and the profuse sweating induced by wearing the suit cause a rapid loss in body weight by loss of water. Because of this dehydration effect, sauna suits should be used with great caution. Sauna suits are also worn for body wrapping in some health spas. The wearer is first wrapped in bandages saturated with mineral and/or herbal preparations and then covered with a sauna suit. The objective of this process is to enable the wearer to “sweat out toxins”; however there is little scientific evidence to support the effectiveness of this practice. Sauna suits are often worn specifically for such sweat excretion rather for exercise or weight loss. A medical use for a sauna suit is in the treatment of psoriasis, an inflammation of the skin causing itchiness and discomfort. The symptoms of psoriasis can be relieved by use of ointments and by keeping the skin moist. The wearing of a sauna suit helps to retain skin moisture and to prevent the ointment from leaking out and staining other clothing, furniture or bedding. In medical literature, a sauna suit is also called an “occlusion suit”.
________
Sweat therapy:
Sweat therapy is the combination of group counselling/psychotherapy with group sweating. Group sweating is social interaction while experiencing psychophysiological responses to heat exposure. Group sweating has strong cultural validity as it has existed throughout the world for thousands of years to promote well-being. Examples include the Finnish Sauna, the Russian Banya (sauna), the American Indian Sweat lodge Ceremony, the Islamic Hammam, the Japanese Mushi-Buro or Sentō, and the African Sifutu. Group sweating has been used for various physical and mental purposes for thousands of years. It has been asserted that the potential health benefits of regular participation in Native American sweat lodges are numerous, but that there is a scarcity of research about the practice. Colmant and Eason (2009) introduced a theoretical model to describe how sweat rituals operate to deliver positive effects to mind, body and spirit. The theoretical model proposes five factors that reciprocally interact to produce the positive effects of sweat rituals: cultural priming, exercise, self-regulation, metaphorical contextual elements, and interpersonal factors.
_________
Diseases of the sweat glands include:
1. Fox-Fordyce disease
The apocrine sweat glands become inflamed, causing a persistent, itchy rash, usually in the axillae and pubic areas.
2. Frey’s Syndrome
If the auriculotemporal nerve is damaged (most often as a result of a Parotidectomy), excess sweat can be produced in the rear of the cheek area (just below the ear) in response to stimuli that cause salivation.
3. Heatstroke
When the eccrine glands become exhausted and unable to secrete sweat, Heatstroke can lead to fatal hyperthermia (extreme rise in body temperature).
4. Hyperhidrosis (vide infra) is a pathological, excessive sweating that can be either generalized or localized (focal hyperhidrosis); focal hyperhidrosis occurs most often on the palms, soles, face, scalp and axillae. Hyperhidrosis is usually brought on by emotional or thermal stress, but it can also occur or with little to no stimulus. Local (or asymmetrical) hyperhidrosis is said to be caused by problems in the sympathetic nervous system: either lesions or nerve inflammation. Hyperhidrosis can also be caused by trench foot or encephalitis.
5. Miliaria rubia (vide infra):
Also called prickly heat, Miliaria rubia is the rupture of sweat glands and migration of sweat to other tissues. In hot environments, the skin’s horny layer can expand due to sweat retention, blocking the ducts of eccrine sweat glands. The glands, still stimulated by high temperatures, continue to secrete. Sweat builds up in the duct, causing enough pressure to rupture the duct where it meets the epidermis. Sweat also escapes the duct to adjacent tissues (a process called miliaria). Hypohidrosis then follows miliaria (post-miliarial hypohidrosis).
Osmidrosis:
Often called bromhidrosis (vide infra), especially in combination with hyperhidrosis. Osmidrosis is excessive odor from apocrine sweat glands (which are overactive in the axillae). Osmidrosis is thought to be caused by changes in the apocrine gland structure rather than changes in the bacteria that act on sweat.
_
Tumors:
Sweat gland tumors include:
Acrospiroma
Aggressive digital papillary adenocarcinoma
Apocrine gland carcinoma
Ceruminoma
Cutaneous myoepithelioma
Cylindroma
Eccrine carcinoma
Hidradenoma papilliferum
Hidrocystoma
Microcystic adnexal carcinoma
Mucinous carcinoma
Papillary eccrine adenoma
Syringadenoma papilliferum
Syringofibroadenoma
Syringoma
Adenolipomas are lipomas associated with eccrine sweat glands.
_
As signs in other illnesses:
Many diseases cause sweat gland dysfunction:
1. Acromegaly, a result of excess growth hormone, causes the size of sweat glands increase, which leads to thicker skin.
2. Aquagenic wrinkling of the palms, in which white papules develop on the palms after exposure to water, can sometimes come with abnormal aquaporin 5 in the sweat glands.
3. Cystic fibrosis can be diagnosed by a sweat test, as the disease causes the sweat glands ducts to reabsorb less chloride, leading to higher concentrations of chloride in the secreted sweat.
4. Ectodermal dysplasia can present a lack of sweat glands.
5. Fabry disease, characterized by excess globotriaosylceramide (GL3), causes a decrease in sweat gland function due to GL3 deposits in the eccrine glands.
6. GM1 gangliosidoses, characterized by abnormal lipid storage, leads to vacuolization in eccrine sweat gland cells.
7. Hunter syndrome can include metachromin granules and mucin in the cytoplasm of the eccrine sweat gland cells.
8. Hypothyroidism’s low levels of thyroid hormone lead to decreased secretions from sweat glands; the result is dry, coarse skin.
9. Kearns–Sayre syndrome, a disease of the mitochondria, involves abnormal mitochondria in eccrine sweat glands.
10. Lafora disease is a rare genetic disorder marked by the presence of abnormal polyglucosan deposits. These “Lafora bodies” appear in the ducts of sweat glands, as well as the myoepithelial cells of apocrine glands.
11. Lichen striatus, a self-limited eruption of small, slightly scaly papules, includes a lymphoid infiltrate around eccrine sweat glands.
12. Metachromatic leukodystrophy, a lysosomal storage disease, leads to the accumulation of lipopigments and lysosomal residual bodies in the epithelial cells of sweat glands.
13. Neuronal ceroid lipofuscinosis causes abnormal deposits of lipopigment in sweat gland epithelial cells (among other places).
14. Neutral lipid storage disease includes abnormal lipid deposits in cells, including those of the sweat gland.
15. Newmann–Pick type C, another lipid storage disease, includes abnormal lipid storage in sweat glands.
16. Schindler disease causes cytoplasmic vacuoles that appear to be empty or contain filamentous material to manifest in eccrine sweat gland cells.
17. Small fiber peripheral neuropathy can damage the nerves that control the sweat glands. The sweat gland nerve fiber density test can diagnose this condition.
__________
__________
Introduction to hyperhidrosis:
Hyperhidrosis is sweating that is more than required to maintain normal thermal regulation. Excessive sweating is when you sweat more than you might expect based on the surrounding temperature or your activity level or stress. There is only a thin line between increased sweating and Hyperhidrosis, the medical term for abnormal excessive sweating. If you’re sweating so much that it makes you uncomfortable and affects your social life, schooling, or job, that’s when we would consider it a problem. About 3 percent of the world’s population has hyperhidrosis, which causes someone to sweat a lot — four to five times as much as the average person. People with excessive sweating (hyperhidrosis) sweat profusely, and some sweat almost constantly. Although people with a fever or those exposed to very warm environments sweat, people with excessive sweating tend to sweat even without these circumstances. Hyperhidrosis is excessive sweating, which can be focal or diffuse and has multiple causes.
_
In humans, sweating is induced by heat or exercise and is part of thermoregulation. Primary hyperhidrosis is defined as excessive, uncontrollable sweating without any discernible cause. While it most commonly affects the armpits, feet, and hands, it is possible for someone to experience this condition over their whole body. The face is another common area for hyperhidrosis to be an issue. Severely affected patients have skin maceration and secondary microbial infections; their clothes may be drenched, especially from axillary hyperhidrosis; and they may be socially stigmatized. Primary hyperhidrosis, while not life threatening, is certainly life altering. The extreme embarrassment as well as actual functional impairment can be devastating. Those affected experience substantial impairments in terms of the social and professional environments because of increased sweat production, and the resultant subjective perception of illness at the individual level may be substantial. Millions of people are affected by this condition, but more than half never receive treatment due to embarrassment or lack of awareness. While primary hyperhidrosis appears to have a genetic component, secondary hyperhidrosis can result from an underlying condition, such as lymphoma, hyperthyroidism, or diabetes, or as a side effect of medication.
_
Classification of hyperhidrosis:
Hyperhidrosis can be localised or generalised:
• Localised hyperhidrosis (focal hyperhidrosis) affects armpits, palms, soles, face or other sites
• Generalised hyperhidrosis affects most or all of the body
_
Primary hyperhidrosis:
• Starts in childhood or adolescence
•May persist lifelong, or improve with age
•There may be a family history
•Tends to involve armpits, palms and or soles symmetrically
•Sweating usually reduces at night, and disappears during sleep
Experts are not certain why excessive sweating during sleep is not common for people with primary hyperhidrosis.
Secondary hyperhidrosis:
•Less common than primary hyperhidrosis, can present at any age
•More likely to be generalised but can be localized and asymmetric
•Can occur at night or during sleep.
•Due to infection, endocrine, drugs, cancer or neurological conditions
_
The latest diagnosis codes for hyperhidrosis are:
ICD-10 Codes (Effective Oct. 1, 2015)
L74.5 – Focal Hyperhidrosis
L74.51 – Primary Focal Hyperhidrosis
L74.510 – Axilla
L74.511 – Face
L74.512 – Palms
L74.513 – Soles
L74.519 – Unspecified
L74.52 – Secondary Focal Hyperhidrosis
L74.8 – Other Eccrine Sweat Disorders
L74.9 – Eccrine Sweat Disorder Unspecified
_
Pathophysiology of hyperhidrosis:
Sweat glands in patients with hyperhidrosis are not histopathologically different from those in normal patients, nor is there an increase in the number or size of glands. The condition is caused by hyperfunction of the sweat glands rather than hypertrophy. Patients with primary hyperhidrosis have a higher-than-normal basal level of sweat production as well as an increased response to normal stimuli such as emotional or physical stress. There is evidence that these patients have a reduced threshold for emotional sweating but have normal thermoregulatory and drug-induced sweating. Other clinicians report that patients may be hyperreactive to thermal stimuli. Although emotional stimuli are involved in primary hyperhidrosis, Stolman observes that it is a physiologic disorder as opposed to a psychological disease. One of the underlying mechanisms for a lowered threshold and exaggerated response in hyperhidrosis patients may be excessive sympathetic activity. Patients with palmoplantar hyperhidrosis showed less reflex bradycardia in response to Valsalva maneuver or facial immersion than healthy controls but a higher degree of vasoconstriction in response to finger immersion in cold water. This study suggested that increased sympathetic activity through the T2-T3 ganglia causes palmar hyperhidrosis. There is a vicious cycle that can occur with excessive palmar and plantar sweating—the evaporative cooling of the skin increases sympathetic outflow through reflex action, in turn increasing sweat output. If there is generalized sympathetic overactivity in primary hyperhidrosis, catecholamine levels in patients could be predicted to be elevated. However, a study of plasma catecholamine levels in patients before and after thoracic sympathectomy found preoperative norepinephrine and epinephrine levels to be normal. After sympathectomy, the norepinephrine level fell but epinephrine was unchanged. It was thus concluded that primary hyperhidrosis is more likely due to sympathetic overactivity in the upper dorsal ganglia. Cardiac autonomic response was studied in patients with primary focal hyperhidrosis and healthy controls using spectral analysis of heart rate variability. Interestingly, there were no differences between groups in the low-frequency band that represents sympathetic cardiac innervation, but the high-frequency band representative of parasympathetic innervation did show differences. These results led the investigators to suggest that primary hyperhidrosis may involve a more complex dysfunction of the autonomic nervous system than previously thought, involving parasympathetic pathway differences as well.
_
Epidemiology:
People of all ages and genders can be affected by hyperhidrosis. This condition affects millions of people around the world (approximately 3 percent of the population), but because of lack of awareness and understanding that there are treatments for the condition, more than half of these people are never diagnosed or treated for their symptoms. It is estimated that the incidence of focal hyperhidrosis may be as high as 2.8% of the population of the United States. It affects men and women equally, and most commonly occurs among people aged 25–64 years, though some may have been affected since early childhood. About 30–50% of people have another family member afflicted, implying a genetic predisposition.
_
Prevalence of hyperhidrosis in the U.S.
_
The mean age of onset of primary hyperhidrosis is youth:
_
Hyperhidrosis Facts:
•Hyperhidrosis affects 3 % of the world’s population.
•Family genetic history is believed to play a major role in hyperhidrosis.
•The most common areas hyperhidrosis, the hands, feet and armpits.
•No known difference for those affected with regard to race or gender.
•Higher percentages in certain geographic regions (Taiwan, Philippines, etc.).
•Hyperhidrosis can negatively affect people both socially and functionally.
•Historically doctors have underestimated and/or misunderstood hyperhidrosis.
_
Common triggers include heat, exercise, fever, feeling anxious, and certain foods. Foods and beverages that are common triggers contain:
-Monosodium glutamate (MSG).
-Caffeine (chocolate, coffee, tea).
-Hot sauce.
-Spices such as curry or cumin.
-Alcohol.
_
Hyperhidrosis affect quality of life:
Hyperhidrosis is not a serious or life-threatening condition, although it often interferes with normal, daily activities and affects a person’s quality of life. Severe, chronic sweating may make the affected skin white, wrinkled, and cracked, often causing the area to become red and inflamed. Hyperhidrosis often requires medical care. In fact, about one-third of people with focal hyperhidrosis describe their symptoms as significantly affecting their quality of life.
_
_
Quality of life: Primary Axillary Hyperhidrosis:
Less confident 72%
Unhappy/depressed 49%
Change type of leisure activities 45%
Frustrated with daily activities 30%
Miss outings/events 25%
Decrease time in leisure activities 19%
Quality of Life: Primary Palmar Hyperhidrosis:
Interference with daily tasks 95%
Social embarrassment 90%
Psychological difficulties 40%
_______
Focal hyperhidrosis:
Excessive sweating may affect the entire surface of the skin but is often limited to certain parts of the body (called focal excessive sweating). The parts most often affected are the palms of the hands, soles of the feet, forehead, and armpits. Sweating in these areas is usually caused by anxiety, excitement, anger, or fear. Although such sweating is a normal response, people with excessive sweating sweat profusely and under conditions that do not cause sweating in most people. Primary focal hyperhidrosis develops “idiopathically” in otherwise healthy persons. The onset is mostly in puberty. Altogether, some 3% of the population suffer from hyperhidrosis, 51% of these from focal axillary hyperhidrosis. There does seem to be a genetic predisposition because 30% to 65% of patients have a positive family history. Primary hyperhidrosis affects mainly the axillae, but the feet, hands, and face can also be affected; often, several areas are affected. Changes in sweat gland morphology are not observed. Hyperhidrosis is a complex dysfunction of the sympathetic and parasympathetic nervous system. Patients are often subject to severe psychosocial problems. They often avoid shaking hands or have unwanted sweat patches under their arms. Secondary focal hyperhidrosis is the result of central or peripheral neuronal defects. Peripheral causes are neuropathies—e.g., diabetic neuropathy. In this scenario, sweating may be peripherally increased at the onset of a polyneuropathy and may disappear as nerve damage progresses. In a scenario of a chronic neurogenic inflammation—such as the complex regional pain syndrome—hyperhidrosis is often found at the extremity that is affected. After cerebral infarctions or hemorrhages, the failure of cortical inhibitory centers leads to hyperhidrosis contralaterally to the lesion. After spinal lesions, sweating is reduced ipsilaterally or may even be completely absent, so that compensatory hyperhidrosis develops on the remaining body parts. Often, patients experience the absence of sweating as less disruptive than the compensatory increase in sweating in other areas. In posttraumatic syringomyelia, hyperhidrosis in the affected area may be one of the first symptoms. Special forms of focal hyperhidrosis include the Harlequin syndrome and Frey’s syndrome. In Harlequin syndrome, erythema and hyperhidrosis develop unilaterally. Usually, this is compensatory, increased sweating in contralateral anhidrosis owing to damage to the sympathetic efferent. Harlequin syndrome can be caused by central (brain stem) or peripheral damage to the sympathetic pathways. Frey’s syndrome—focal gustatory sweating (sweating during eating/drinking, especially of hot foods)—may develop after operations, if tumors are present, or in patients with lesions of the parotid salivary gland with damage to the facial nerve.
_
Studies showing genetic predisposition in primary focal hyperhidrosis:
1. Ann Surg 1994
Retrospective questionnaire following ETS for primary hyperhidrosis, 270/323 patients responded, 31.5% reported positive family history (FH).
2. Vasc Surg 2002
Controlled prospective study of patients with primary hyperhidrosis presenting for ETS, 49/58 patients responded to detailed FH questionnaire: 65% reported + FH (0.28 risk offspring, 0.14 risk parents), Concluded gene present in 5% of population with 25% penetrance.
3. In 2006, researchers at Saga University in Japan reported that primary palmar hyperhidrosis maps to gene locus 14q11.2–q13.
__
Primary Focal Hyperhidrosis is a separate and unique disease:
1. Bilateral & symmetric
2. Axilla, palms, soles, craniofacial
3. Onset in childhood and adolescence
4. Significant impact on quality of life
5. Effective therapies
_
Diagnosis of Primary Focal Hyperhidrosis:
Focal, visible, excessive sweating of at least 6 months duration without apparent cause with at least two of the following characteristics:
1. Bilateral and relatively symmetric
2. Impairs daily activities
3. Frequency of at least one episode per week
4. Age of onset less than 25 years
5. Positive family history
6. Cessation of focal sweating during sleep
_
What is the impact of excessive sweating?
Hyperhidrosis is embarrassing and interferes with many daily activities.
Axillary hyperhidrosis:
•Clothing becomes damp, stained and must be changed several times a day
•Wet skin folds are prone to chafing, irritant dermatitis and infection
_
Palmar hyperhidrosis:
• Slippery hands lead to avoidance of hand shaking
• Marks left on paper and fabrics
•Difficulty in writing neatly
•Malfunction of electronic equipment such as keypads and trackpads
•Prone to blistering type of hand dermatitis (pompholyx)
_
Plantar hyperhidrosis:
•Affects soles of the feet
•Unpleasant smell
•Ruined footwear
•Prone to blistering type of dermatitis (pompholyx)
•Prone to secondary infection (tinea pedis, pitted keratolysis)
________
Causes of hyperhidrosis:
_
Some causes of secondary generalized hyperhidrosis:
| Type | Examples |
| Hormonal (endocrine) disorders | An overactive thyroid gland (hyperthyroidism), low blood sugar levels (hypoglycemia), and certain pituitary gland disorders or use of drugs that affect pituitary gland function |
| Drugs | Antidepressants, aspirin and other nonsteroidal anti-inflammatory drugs (NSAIDs), some drugs for diabetes, caffeine, theophylline:: Withdrawal from opioids |
| Nervous system disorders | Injuries, dysfunction of the autonomic nervous system, and damage to certain nerves by cancer |
| Cancer* | Lymphoma and leukemia |
| Infections* | Tuberculosis, heart infection (endocarditis), and severe fungal infections of the entire body |
| Other | Flushing and diarrhoea that occurs in people who have certain disorders (carcinoid syndrome), pregnancy, menopause, and anxiety |
*Causes primarily night sweats.
_____
Night sweat:
Night sweats, also known as sleep hyperhidrosis, is the occurrence of excessive sweating during sleep. The person may or may not also suffer from excessive perspiration while awake. One of the most common causes of night sweats in women over 40 is the hormonal changes related to menopause. This is a very common occurrence during the menopause transition years and while annoying, it is not necessarily dangerous or a sign of underlying disease. While night sweats might be relatively harmless, it can also be a sign of a serious underlying disease. It is important to distinguish night sweats due to medical causes from those that occur simply because the sleep environment is too warm, either because the bedroom is unusually hot or because there are too many covers on the bed. Night sweats caused by a medical condition or infection can be described as “severe hot flashes occurring at night that can drench sleepwear and sheets, which are not related to the environment.” Some of the underlying medical conditions and infections that cause these severe night sweats can be life-threatening and should promptly be investigated by a medical practitioner. Night sweats are a common outpatient complaint, yet literature on the subject is scarce. Tuberculosis and lymphoma are diseases in which night sweats are a dominant symptom, but these are infrequently found to be the cause of night sweats in modern practice. While these diseases remain important diagnostic considerations in patients with night sweats, other diagnoses to consider include human immunodeficiency virus, gastroesophageal reflux disease, obstructive sleep apnea, hyperthyroidism, hypoglycemia, and several less common diseases. Antihypertensives, antipyretics, other medications, and drugs of abuse such as alcohol and heroin may cause night sweats.
_
In one study of 2,267 people visiting primary care physicians, 41% said they experience night sweats. While not a type of primary focal hyperhidrosis, night sweats often occur in secondary generalized hyperhidrosis. Your body uses sweat to reduce your core temperature when it spikes above a threshold called the thermoneutral zone, research suggests. Lots of things push your body temp into this zone, from use of heavy blankets to inflammatory processes inside your body when you have an infection or cancer. Some research into night sweats even suggests that these inflammatory mediators periodically spike during the night. What’s more, several other conditions can impact your sympathetic nervous system, your sweat glands, or other factors that influence your body’s ability to regulate its temperature. Another theory about night sweats might apply to healthy guys: People who work out may be conditioned to sweat at lower temperatures than expected, Dr. Mold and his colleagues posited in their study review. It’s not clear whether this could lead to night sweats, but one study in Human Kinetics did find that night sweats can be a sign of overtraining.
_
Prevention and treatment of night sweat:
Medications are also a common cause of night sweats. Frequent culprits are antidepressants, other psychiatric medicines, hormone therapy, and medications taken to decrease the level of sugar (glucose) in your blood. Even medicine taken to lower fever (aspirin, acetaminophen) can lead to sweating. So can cortisone, prednisone, and prednisolone. Remember flushing is different from night sweats. Flushing is redness of the skin, typically of the neck and cheeks that is sometimes confused with night sweats. There are a number of drugs that can cause flushing including: niacin, tamoxifen, hydralazine, nitroglycerine, and sildenafil (Viagra). If you suffer from night sweats, talk to your doctor about it, especially if the night sweats are accompanied by a fever or other symptoms such as unexplained weight loss. There is usually an underlying medical condition that needs to be addressed. Tell your doctor about any medications you take, including over-the-counter and herbal or “natural” supplements or vitamins. The treatment of choice for night sweats depends upon the underlying cause such as correcting hormone irregularities, adjusting medications, and attending to contributing factors. Medications known as anticholinergic agents may help reduce sweating. These should only be taken under the advice of a health care professional.
_
There are things you can do to make bedtime more comfortable.
1. Sleep in an air-conditioned room or use a fan
2. Sleep in a cool environment with light, breathable, non-synthetic nightclothes and sheets
3. Apply a clinical strength antiperspirant to the parts of the body that are most sweaty; underarms, hands, feet, hairline, back, chest or groin. Your sweat glands are less active at night, so applying antiperspirant to clean, dry skin before bed will allow it to work while you sleep and into the next day.
4. Avoid alcohol, caffeine, spicy foods, and eating 2-3 hours before going to bed
5. Practice relaxation breathing exercises prior to bed and after waking with a night sweat
6. Get adequate daily exercise
7. Maintain a normal weight
8. Drink plenty of water during the day
Night sweats are a common annoyance usually associated with sleeping in warmer than ideal conditions. However, persons with drenching night sweats or a change in their pattern of sweating should pursue a medical evaluation.
_____
Gustatory sweating:
Sweating is a normal physiologic function controlled by sympathetic cholinergic pathways. Thermoregulation is the priority of this autonomic function. There are several conditions where sweating activity is inappropriate, ranging from hyperhidrosis to anhidrosis. Gustatory sweating itself is a unique entity characterized by profuse sweating of the face, scalp, and neck during or immediately after ingestion of food or drink. Caffeine, alcohol, onions, garlic and capsaicin are sweat triggers in humans. No specific foods are consistently related to symptoms and reactions are variable. This occurrence may be a source of embarrassment to patients and, in diabetic patients, may disturb eating patterns and thus impair glycemic control. Gustatory sweating can be very distressing because the mere idea of food can make a patient’s face drenched with sweat. And because much of life’s business (friendships, romances, networking, and celebrations) is conducted at mealtime, gustatory sweating can have extensive social, economic, and emotional implications. There are a few different reasons why we sweat when we eat, although researchers haven’t yet pinned down a tried-and-true cause. But they have found two types of triggers for gustatory sweating: physiologic and nonphysiologic. Physiologic reasons for sweating when we eat include hot temperatures, hot foods and spicy foods — things that raise your body temperature enough to signal the sympathetic nervous system to turn down the heat. Nonphysiologic reasons for gustatory sweating include medical causes such as Parkinson’s disease, nerve damage associated with diabetes, viruses that have neurologic complications including herpes zoster (also known as shingles) and nerve damage from surgery — things that cause the nervous system to have a communication breakdown. Nonphysiologic forms include the auriculotemporal (Frey’s) syndrome and diabetic gustatory sweating. Gustatory sweating is most commonly a result of damage to a nerve that goes to the parotid gland, the large salivary gland in the cheek. In this setting, referred to as Frey syndrome, the sweating is usually on one side of the head. Gustatory sweating is also a rare complication of diabetes mellitus. In this case sweating may occur on both sides of the head, with mild or substantial severity.
_
Frey syndrome:
Frey’s syndrome results from surgical or traumatic damage to the auriculotemporal nerve as it passes through the parotid gland. In this case, symptoms are localized unilaterally to the distribution of the affected nerve. Frey’s syndrome is not uncommon in certain surgical arenas, since it occurs in up to 60% of patients having parotidectomy with facial-nerve dissection. Many cases of gustatory sweating show up after surgery or trauma to a parotid gland. Most people have a pair of parotid glands, one located on each side of the face, below and in front of the external ear. The parotid glands are the body’s largest salivary glands. Saliva is a fluid secreted by salivary glands to aid chewing, swallowing, and digestion of food. Saliva is produced in preparation for eating (like when you are thinking about a delicious meal) as well as during chewing. If a parotid gland is damaged or if surgery to a parotid is required (damage can occur due to inflammation, infection, and tumors can require surgery), then related nerves may become damaged or may regenerate from such damage in a way that causes them to become “mixed up” and/or “intertwined”. The result is that when a person is supposed to salivate, he or she may also sweat and experience facial flushing. This combination of sweating and flushing related to parotid trauma is called Frey’s syndrome. Usually Frey’s syndrome affects just one side of the face. Taste buds appear to be related to triggering symptoms, since placing food directly into the stomach does not evoke sweating.
_
Diabetic Gustatory Sweating:
Diabetic gustatory sweating is a specific thermoregulatory disturbance directly related to oral intake. Some gustatory sweating is normal, especially after you eat spicy foods, but in diabetes, it’s often profuse, inappropriate or unexpected sweating. The American Diabetes Association reports that cheese and chocolate are two of the most common causes of such sweating. Pickles, vinegar, fresh fruit, salty foods and alcohol may also trigger gustatory sweating. Although the precise prevalence of gustatory sweating in diabetes is unknown, it is documented much less commonly than surgical causes. This may be due in part to less frequent occurrence but is likely compounded by underrecognition and underreporting. Diagnosis of diabetic gustatory sweating relies on a high level of suspicion in an appropriate clinical setting. This phenomenon is bilateral and is seen in long-standing diabetes with complications and other signs of dysautonomia. Scientists aren’t sure why gustatory sweating happens with diabetics. But the condition has been linked to complications such as nerve and kidney damage, as well as poorly controlled blood sugar. In a “Diabetic Medicine” study, 69 percent of the diabetics who reported gustatory sweating had nephropathy, or kidney damage; 36 percent had neuropathy or nerve damage. Chewing activates the sweating, and the condition is marked by sweating about the face, scalp and neck. No data suggest that level of glycemic control is related to severity of symptoms, though autonomic dysfunction in general is related to the level of metabolic stability. In patients with renal insufficiency, gustatory sweating has been reversed with renal transplantation, though it occurs in the absence of diabetic nephropathy as well. While no single test confirms the diagnosis of diabetic gustatory sweating, supporting evidence may be obtained by documenting the presence and distribution of diaphoresis. The increased moisture should appear during or after eating and be restricted to the head and neck region. This may be documented by application of a variety of indicator substances, including iodine starch and cobalt chloride strips.
_
Treatment of diabetic gustatory sweating has drawn on experience from surgical cases of Frey’s syndrome. These approaches focus on symptomatic relief only and have no documented impact on the course of the syndrome or directly on glycemic control. Tight glycemic control also does not reverse existing dysautonomia. Several systemic therapies have been used with varying degrees of success. Oral anticholinergic agents, including scopolamine, oxybutynin, propantheline, and glycopyrrolate, have improved symptoms; however, concurrent illnesses and adverse reactions, including mouth dryness, constipation, potential worsening of gastroparesis, and confusion, limit the use of systemic therapies. Clonidine has also been used with some success but is also limited by side effects such as dry mouth and hypotension. Such intolerability led to the investigation of nonsystemic approaches. Noting the efficacy of oral antimuscarinic agents, several investigators have used topical glycopyrrolate. This quaternary ammonium compound has been shown to significantly decrease the incidence, severity, and frequency of sweating with eating and is tolerated well. Botulinum toxin has been used for gustatory sweating, though in most literature it is limited to use in unilateral, surgical-related cases. Botulinum toxin injections can provide “a couple of years” of relief from gustatory sweating. This is a much longer duration of effectiveness than is typically seen when Botox is used to treat other forms of hyperhidrosis. (Please note, Botulinum toxin has not been approved by the FDA for the treatment of gustatory sweating or Frey’s syndrome so this is an “off-label” use of the medication. Off-label uses of medications are, however, very common.) In cases in which more conservative measures have failed and symptoms are disabling, surgery may be done; however, tympanic neurectomy or subdermal fascia grafts are invasive, difficult procedures and have varying and often temporary, efficacy.
______
Alcohol related sweating:
A number of people after a round of alcoholic drinks complain about sweating. There is indeed a close relation between alcohol and sweating. While some people experience excessive sweating after drinking alcohol, some might experience it as a withdrawal symptom. Also, some people have a condition called alcohol intolerance, wherein they cannot tolerate even slight amounts of alcohol and end up with symptoms like excessive sweating and gastrointestinal distress.
_
Sweating after drinking alcohol is common, because alcohol has a tendency to dilate the vessels in the skin. Therefore, after consumption of alcohol, it is not uncommon to experience hot flashes. Skin vasodilation leads to an increase in skin temperature. To keep the body temperature at its optimum, the body releases sweat. Alcohol is rapidly metabolised in liver generating 7 Kcal energy from 1 gram alcohol. This alcohol metabolism generates heat. The other reason behind excessive sweating after alcohol consumption is the body’s activation sympathetic nervous system due to alcohol per se or alcohol induced hypoglycemia. Drinking a small amount of alcohol at a slow rate may not induce perspiration, but drinking large amounts may lead to accumulation of the substance that may continue to dilate vessels after drinking, causing night sweats. Excessive perspiration at night or night sweats are commonly accompanied by hot flashes. Night sweats related to alcohol consumption is prevalent in individuals suffering from alcohol dependence. However, binge drinking on occasion may also cause this symptom even when one is not addicted to alcohol. Some people however, cannot tolerate even small amounts of alcohol. This condition, known as alcohol intolerance, may be due to a lack of aldehyde dehydrogenase, an enzyme necessary to break down alcohol. Symptoms include skin flushing, excessive sweating and gastrointestinal distress. It is commonly seen among women and people of Asian descent.
____
Nicotine and sweating:
Add to the list of complaints against cigarettes is their propensity to make you sweat. Acetylcholine (ACh) is the preganglionic neurotransmitter for both divisions of the ANS and preganglionic receptors are nicotinic. Since nicotine itself is a nicotinic acetylcholine receptor agonist, nicotine in your smoke will stimulate sweating.
____
Common Drugs/Medications known to cause sweeting:
Sweating can be a side effect of several types of prescription and over-the-counter drugs. Although sweating is a known side effect of the medications, in most cases only a small percentage of people using the medicines experience undue sweating (in some cases less than 1%). Blood pressure tablets, pain medication, antibiotics, cancer treatments, anti-depressants, gastrointestinal, dermatology, diabetes and hormone drugs can all make you sweat more. If excessive sweating side effects of medication – or withdrawing from medication – are concerning you, see your doctor for advice before making any changes.
_____
Sweating and illnesses:
Infection and cancer are common causes of sweating. Infection can give you a high temperature and your body sweats to try and reduce it. Treating the infection can control or stop the sweating. Night sweats and excessive sweating during the day can be indicators of diabetes, cancer, tuberculosis, HIV/AIDS, some infections, hormonal disorders and gastro-oesophageal reflux disease. If you’ve recently had surgery, anaesthetic side effects are another example of what causes cold sweats and chills. The types of cancer that sometimes cause sweating include
•Non Hodgkin lymphoma and Hodgkin lymphoma – the sweats usually happen at night but can be any time
•Carcinoid tumours – sweating is a symptom of carcinoid syndrome
•Leukaemia
•Mesothelioma
•Bone cancer
•Liver cancer
People with advanced cancer of any type may also have sweating. Researchers at St Christopher’s Hospice in London found that at least 16 out of every 100 people (16%) with advanced cancer have this symptom.
_
Sweating and Diabetes mellitus:
1. Diabetic neuropathy and sweating:
Given that sweating is under autonomic control, abnormalities in people with advanced diabetes should not be surprising. Dysautonomia is strongly related to duration and overall control of diabetes and portends an overall poor prognosis. Extremes of anhidrosis and hyperhidrosis occur in 10% to 75% of people with diabetic autonomic neuropathy. Upper body “compensotory hyperhidrosis” is observed in patients with peripheral neuropathy with distal anhidrosis. This is unrelated to eating or drinking. If the nerves that control sweat glands are damaged, they may not be able to activate the sweat glands and produce sweat. This inability to sweat is called anhidrosis. One study published in Mayo Clinic Proceedings found that 94 percent of patients with diabetic neuropathy had abnormalities in sweating. People who cannot sweat often have trouble regulating their body temperature, because sweat helps the body to cool down. As a result, diabetic patients with anhidrosis may easily become overheated in warm temperatures or after physical exertion. Some patients with diabetic neuropathy actually experience the opposite effect when the nerves that control the sweat glands are damaged; they sweat too much, reports the University Of Washington Department Of Medicine. Diabetic neuropathy has been linked to excess sweating, particular at night or while eating. Some patients may wake up in the middle of the night because their sheets are drenched in sweat, which is sometimes referred to as soaking night sweats.
2. Heavy sweating is often linked to low blood glucose levels known as hypoglycemia. When blood glucose levels plummet, it triggers a “fight or flight “response from your body. As a result, your sympathetic nervous system gets excited. This can lead to heavy sweating as well as shakiness and anxiety. It is important to get your blood sugar back to normal as soon as possible to alleviate this sweating.
3. Another reason for heavy sweating is hyperthyroidism, a metabolic condition that people with diabetes may be prone to. The combination of diabetes and hyperthyroidism can worsen diabetes symptoms and lead to further complications. It is important to seek treatment immediately.
4. People with diabetes have an increased risk of developing cardiovascular disease and having a stroke. This risk may be increased when a person with diabetes is overweight or obese. Heart failure, heart attack or a stroke can cause excessive sweating.
5. Diabetic Gustatory Sweating is already discussed vide supra.
_____
Sweating vis-à-vis menses, pregnancy, postpartum and menopause:
Some women experience post ovulation symptom of night sweats and hot flashes after few days of ovulation. This is due to changes in the progesterone hormone levels and progesterone levels tend to be very high during ovulation. Surely night sweats can be one of the initial symptoms of being pregnant. However, night sweats can occur in women who is approaching menopause too. But pregnancy night sweats are accompanied with several other pregnancy symptoms. Night sweats usually happens in pregnant women during the first trimester of pregnancy. Pregnant women may experience night sweats as early as 2 to 3 weeks of pregnancy or during the latter part of the pregnancy. Sometimes some women may not experience night sweat symptoms in their early pregnancies. Night sweats during pregnancy are caused due to rapid fluctuation of female hormone estrogen. It’s common to perspire a lot in the weeks after giving birth, especially at night. Sweating is one of the ways your body gets rid of the extra water you retained during pregnancy. It’s possible that the dramatic drop in estrogen that occurs right after delivery also contributes to post-partum sweating. Although postpartum sweating is completely normal, if it’s accompanied by a fever, you might have an infection. Increased sweating can also be a sign of other problems, such as an overactive thyroid gland. Check with your healthcare provider if you have a fever or think your sweating is excessive.
_
Vasomotor symptoms (VMS), commonly called hot flashes or flushes (HFs) and night sweats, are the menopausal symptoms for which women seek treatment during menopause most often. Around 70% of women experience hot flashes during menopause. The ‘flush’ itself can last from 30 seconds to 30 minutes. VMS are a form of temperature dysfunction that occurs due to changes in gonadal hormones. Normally, core body temperature (CBT) remains within a specific range, oscillating with daily circadian rhythms. Physiological processes that conserve and dissipate heat are responsible for maintaining CBT, and tight regulation is important for maintenance of optimal internal organ function. Disruption of this tightly controlled temperature circuit results in exaggerated heat-loss responses and presents as VMS. The mechanistic role related to changes in gonadal hormones associated with VMS is not understood. Hormone therapy is the most effective treatment for VMS and other menopausal symptoms. Estrogens are known potent neuromodulators of numerous neuronal circuits throughout the central nervous system. Changing estrogen levels during menopause may impact multiple components involved in maintaining temperature homeostasis.
_
Specific Treatment of hot flashes and sweating in menopause:
•hormone replacement therapy using the lowest dose necessary for the shortest period
•drugs approved to treat depression, which can also reduce hot flashes in some cases
•gabapentin, which is used to treat nerve pain can also lessen hot flashes
•clonidine, which is a blood pressure drug that can reduce hot flashes
•paroxetine, which is an antidepressant drug meant specifically to stop hot flashes
_______
Signs and symptoms of hyperhidrosis:
Areas that produce excessive sweat usually appear pink or white, but, in severe cases, may appear cracked, scaly, and soft. Sometimes the area becomes red and inflamed. The area may emit a foul odor (bromhidrosis) due to the breakdown of sweat by bacteria and yeasts that normally live on the skin. Medications that are used for other treatments and diet will also affect odor. Medical conditions like kidney failure and diabetic ketoacidosis will have the same effect. Clothing may also become soaked with sweat. People who sweat excessively are frequently anxious about their condition, and it may lead to social withdrawal. This anxiety may make the sweating worse.
_
You may be asked details about your sweating, such as:
•Location: Does it occur on your face, palms, or armpits, or all over the body?
•Time pattern: Does it occur at night? Did it begin suddenly?
•Triggers: Does the sweating occur when you are reminded of something that upsets you (such as a traumatic event)?
•Other symptoms: Weight loss, pounding heartbeat, cold or clammy hands, fever, lack of appetite.
_
Armpits sweating:
In case of Primary Hyperhidrosis affecting the armpits, it’s often young adults complaining of sweat marks on their clothes under their arms since their teens. They avoid colourful and white clothes and prefer dark clothes to not show the marks; they feel ashamed and lose their confidence as they are wrongly convinced that the excessive sweating under the arms is associated with excessive body odours. They bring extra clothes at school or at work to change during the day.
Hand sweating:
It can also affect the hands, usually noted when the child learned to write at the age of 5; the pen slipped out the hand; they made wet mark on the paper when writing. Then these children don’t dare holding hands of their friends at primary school and later on avoid social contacts; it can also affect professional manual skills.
Feet Sweating:
The excessive sweating of the feet is usually well tolerated in winter where the socks in the shoes absorb the sweat. The worst is in summer when ladies try to wear open sandals, in particular with some heels; the sweaty wet feet slip out and make walking hazardous.
Facial sweating:
Facial sweating is also very distressing. The sweat can drip from the scalp or the forehead along the face, the cheeks and the nose and in back of the neck leaving the hair wet.
_
Signs of Hyperhidrosis:
1. Visible sweat when no physical exertion or excessive heat is present
2. Interfering with daily activities (for example, sweaty palms make it difficult to open doors)
3. Soft, peeling skin from continued moisture
4. Frequent skin infections, such as athlete’s foot or jock itch
__
When to see a doctor:
Excessive sweating can be a symptom of other, very serious conditions. Call your doctor right away if you experience:
•sweating and weight loss
•sweating that occurs with a fever, chest pain, shortness of breath, and rapid heartbeat
•sweating that is prolonged and unexplained
•Sweating disrupts your daily routine
•You suddenly begin to sweat more than usual
•You experience night sweats for no apparent reason
Make it a point to mention to your doctor the medicines you are taking, including over-the-counter drugs and supplements, when you seek consultation.
_
Key Points of hyperhidrosis:
• Asymmetric hyperhidrosis suggests a neurologic cause.
• Although diffuse sweating is usually normal, consider cancer, infection, and endocrine disorders.
• Obtain laboratory tests to determine systemic causes based on clinical findings
______
Diagnosis of hyperhidrosis:
Doctors usually base the diagnosis of excessive sweating on the person’s history and a physical examination. Occasionally, they may apply substances to the skin that makes small amounts of sweat visible. Doctors may also do blood tests and hormone screenings to detect other disorders.
_
1. Especially in focal sweating disorders, Minor’s starch iodine test is appropriate. Iodine solution (1%–5%) is applied to a dry surface, followed by a sprinkling of starch. The iodine and starch interact in the presence of sweat, leaving purplish sediment. The distribution pattern of the color (or absence of it) often allows conclusions about the cause of the focal sweating disorder. A starch iodine test is used to outline the area of excessive sweating.
_
The photo shows Minor’s starch iodine test on forehead. The right side of forehead shows unmistakable hyperhidrosis, indicated by the area stained purple. The left forehead was treated with botulinum toxin and shows no signs of sweating.
_
_
2. The amount of sweat can be determined by using quantitative sudometry. The amount of sweat released can be measured with a plexiglas capsule and continuous air stream—either the spontaneously released sweat or after stimulation, for example by using iontophoresis of acetylcholine (quantitative sudomotor axon reflex test, QSART).
_
3. The extent of hyperhidrosis can be measured gravimetrically as the rate of sweat production (expressed in milligrams per minute). To quantify axillary sweating, gravimetry is a particularly suitable test. Filter paper that has been weighed beforehand is inserted into the axilla for a defined time period (60 sec or 5 min) and then weighed again. The difference corresponds to the amount of sweat released in mg/time. Unequivocal normative values do not exist; axillary hyperhidrosis is defined as an amount of released sweat of >50 mg/min. On the palm of the hand, values >20 mg/min are considered pathological.
_
4. Water-vapor analysis performed with the use of a detector over a flat skin surface after the injection of methacholine, this is the most accurate method of measuring maximal sweat production, but it is not feasible in the axillae.
_
5. The Thermoregulatory Sweat Test (TST):
Similar to the starch-iodine test, this test uses a special powder that’s sensitive to moisture. The powder changes color in areas where there is excessive sweating. TST tests for reflex sweating by elevating general body temperature. Signals then pass to the hypothalamus and travel via the intermediolateral cell column, sympathetic chain and postganglionic sudomotor nerves to the sweat glands. A material which changes colour when mixed with sweat, such as alizarin red, corn starch or sodium carbonate is applied to the skin of the unclothed subject who is then placed in a cabinet or room with heaters which raise the air temperature to 44 to 50 degC with a constant humidity. Normally, when the temperature rises by 1degC above baseline (temperature to above 38 degC), uniform sweating is seen over the entire body, with characteristic areas of the body displaying either increased or decreased amounts of sweat production. When exposed to heat people who do not have hyperhidrosis tend not to sweat excessively in the palms of their hands, as opposed to patients with hyperhidrosis who do. This test helps the doctor determine the severity of the condition, as well as making a more accurate diagnosis. This can then be quantified by photographing the body areas and digitizing the change in colour or appearance of the test powder.
_
Another test available to pinpoint the areas of sweating and estimate the severity of your condition include Skin conductance test.
______
Laboratory tests in hyperhidrosis:
Laboratory tests, such as thyroid function tests, blood glucose and uric acid level measurements, and urine samples are performed to rule out more serious medical conditions that may be associated with excessive sweating. Your doctor may order blood or urine tests to determine if the excessive sweating is caused by another medical condition, such as an overactive thyroid (hyperthyroidism) or low blood sugar (hypoglycemia).
_______
Visual scale for the quantification of hyperhidrosis:
The figure above shows visual scale for the quantification of hyperhidrosis that measures or quantifies hyperhidrosis clinically with a visual scale on the basis of drawings, ranging from being drier than normal to having the worst possible level of hyperhidrosis. In addition, the presentation of hyperhidrosis is quantified, whether it is generalized or localized, and the type of body distribution as seen in the figure below.
_
In most cases, patients with hyperhidrosis have unpleasant sensory and emotional experiences in the social sphere, experiences that are difficult to express to physicians in a simple way and to be understood by society. In contrast, assessing and quantifying hyperhidrosis clinically is not an easy task. Sakiyama et al. described a quantitative assessment of the intensity of palmar and plantar sweating in patients with primary palmoplantar hyperhidrosis. A measuring device will certainly add to improving the quantification of hyperhidrosis during clinical assessment. This is because the clinical presentation of hyperhidrosis varies widely from person to person, although there is a certain pattern of presentation in localized hyperhidrosis. It is assumed that this is due in part to the large anatomical variation in the sympathetic chain and also to the fact that the sympathetic nervous system shows a metameric distribution that is not so precise, which makes it difficult to be mapped as dermatomes. Physiologically, there is great variability in sweat production, which depends on environmental heat, seasons, physical exertion, stress, and even circadian cycle. Therefore, it is of the utmost importance that the patient guide us and quantify the areas that should be demarcated, thereby providing a strong foundation for reasoning about the choice of clinical or surgical treatment of hyperhidrosis.
_
What is the outlook for hyperhidrosis?
Localised primary hyperhidrosis tends to improve with age. The outlook for secondary localised or generalised hyperhidrosis depends on the cause.
_______
Discolored Perspiration:
Discolored perspiration can be unsightly, embarrassing and expensive to remove from your clothing. There are many different causes of sweat discoloration, and therefore different treatments and solutions for the problem. It is relatively rare, but possible, for discolored perspiration to be a symptom of poison exposure or another health problem, so consult your doctor for medical advice.
Poisons:
Chemical poisoning may cause discolored perspiration. A study carried out at the University of Auckland, New Zealand, reported in the July 2001 issue of the “International Journal of Occupational and Environmental Health,” indicated that timber workers exposed to pentachlorophenol (PCP) in the course of their work displayed symptoms and syndromes including discolored and foul-smelling sweat.
_
Chromhidrosis:
Chromhidrosis (also referred to as “colored sweat”) is a rare condition characterized by the secretion of colored sweat. It is caused by the deposition of lipofuscin in the sweat glands. Cases of red, blue, green, yellow, pink, and black sweat have been reported. Usually chromhidrosis affects the apocrine glands, mainly on the face and underarms. A limited number of treatment options exist, including regular application of Capsaicin cream and prolonged relief may be provided by botulinum toxin treatment. Chromogenic pigments produced by bacteria (Corynebacterium in particular) are implicated in this condition but their exact role still requires careful microbiological elucidation. Chromhidrosis of the eccrine glands is rare, it occurs mainly after the ingestion of certain dyes or drugs. Chromhidrosis must be differentiated from another condition, called pseudochromhidrosis, where clear sweat is produced and mixes with a coloring agent when it reaches the skin. The classic case most often cited is the blue sweat found on copper miners — the mineral mixes with the sweat on the skin, causing the pigmentation. The case literature on pseudochromhidrosis generally ends with a disappearance of the symptoms when the patient discontinues the product or activity that led to them.
_
Orange sweat:
_
Differential diagnosis of Chromhidrosis:
• Hyperbilirubinemia
• Pseudomonas infection
• Bleeding diathesis
• Alkaptonuria
• Addison’s disease
• Hemochromatosis
______
Hematohidrosis:
Hematohidrosis (also called blood sweat) is a very rare condition in which a human sweats blood. Hematohidrosis is a condition in which capillary blood vessels that feed the sweat glands rupture, causing them to exude blood, occurring under conditions of extreme physical or emotional stress. Manonukul et al. proposed the term “hematofolliculohidrosis” because it appeared along with sweat-like fluid and the blood exuded via the follicular canals.
_
Bloody sweat:
_
Various causative factors have been suggested by Holoubek, like component of systemic disease, vicarious menstruation, excessive exertion, psychogenic, psychogenic purpura, and unknown cause. Acute fear and intense mental contemplation are the most frequent causes, as reported in six cases in men condemned to execution, a case occurring during the London blitz, a case involving fear of being raped, a case of fear of a storm while sailing, etc. The etiopathogenesis according to Dr. Frederick Zugibe is that multiple blood vessels which are present in a net-like form around the sweat gland dilate to the point of rupture due to severe anxiety. The blood goes into the sweat glands, which push it along with sweat to the surface, presenting as droplets of blood mixed with sweat. The extravasated blood has identical cell components as that of peripheral blood. The severe mental anxiety activates the sympathetic nervous system to invoke the stress-fight or flight reaction to such a degree as to cause haemorrhage of the vessels supplying the sweat glands into the ducts of the sweat glands. Effect on the body is weakness and mild to moderate dehydration from the severe anxiety and both blood and sweat loss. Manonukul et al. has recently proposed that there may be some defects in the dermis causing stromal weakness. These defects will communicate with vascular spaces in the dermis and they will eventually dilate and enlarge as blood-filled spaces when the blood comes in. After that, they will exude the blood out by either via follicular canals or directly on to the skin surface and this will occur whenever the positive pressure inside is enough. Afterwards, they will collapse leaving no scar. This phenomenon acts like a balloon, waxes and wanes and thus explains why these bleedings are sometimes intermittent and self-limiting. Immediate biopsy is important because a late biopsy, after these spaces collapse, will not help in identifying them. Skin pathohistological study by Zhang et al. revealed some intradermal bleeding and emphraxised (obstructed) capillaries. No abnormality was found in sweat glands, hair follicles, and sebaceous glands. They concluded that pathological basis for hematohidrosis might be a distinctive vasculitis. The condition is very rare but there are reports in medical literature of successful treatment with beta blockers (propranolol 10 mg) with significant reduction in the frequency of spontaneous blood oozing. The successful use of beta blockers supports the theory that the condition is induced by stress and anxiety yet this etiology is not established yet as the high prevalence of stress and anxiety in the modern era did not change the incidence of this extremely rare disease, suggesting that other co-abnormality also play a key role in this disease. Atropine sulfate transdermal patches have also been used successfully.
_____
_____
Complications and disadvantages of excessive sweating:
Excessive sweating is uncontrollable, embarrassing and not anticipated. People with hyperhidrosis never get used to it and continue to suffer throughout their lives. Complications are rarely medically serious; they include significant psychological distress, as well as skin problems:
1. Social, emotional and psychological strains:
Excessive sweating causes serious mental problems. More than 35 % of people with sweat problems say their symptoms are intolerable or barely tolerable. They avoid social and professional opportunities because of embarrassment. Many report difficulties in their romantic lives because of excessive sweating. Excessive sweating can affect the patient’s self-confidence, job, and relationships. It might eventually control and undermine their ability to enjoy life. Some individuals may become anxious, emotionally stressed, socially withdrawn, and even depressed. Excess perspiration has aesthetic, relational, psychological and even professional consequences. In addition, the anxiety caused by perspiration worsens the production of sweat. On average, a person with hyperhidrosis seeks medical help after living with the condition for 9 years. It is important to spread the word that the symptoms of excessive sweating can be effectively treated.
_
2. Maceration (fishy skin):
The softening and whitening of skin that is kept constantly wet. The mushy, peeling skin can lead to other skin conditions including eczema, which are usually mild but annoying.
_
3. Skin/nail Infections:
Tinea cruris (Jock itch):
An itching fungal infection in the folds of the groin. Heavy sweating around one’s private parts creates a continuous moist environment – the perfect climate for mycosis.
Tinea pedis (Athlete’s foot):
Athlete’s foot is a fungal infection of the feet. The fungus thrives in moist conditions, mostly in between the toes or on the sole.
Warts and bacterial infections:
Damp skin, permanently soaked from sweating can allow easier entry for bacteria and viruses that cause all kinds of skin infections and warts. A prominent wart is the Verruca plantaris, the plantar wart that grows vice versa – into the skin.
Hidradenitis suppurativa (HS):
The apocrine glands can occasionally get diseased or infected, and may lead to a condition known as hidradenitis suppurativa, which is a serious medical condition that may require antibiotics or surgery to cure the disorder. Hidradenitis suppurativa (HS) is a common (though rarely diagnosed), chronic skin disease characterized by clusters of abscesses or subcutaneous boil-like “infections” (oftentimes free of actual bacteria) that most commonly affects apocrine sweat gland bearing areas, such as the underarms, under the breasts, inner thighs, groin and buttocks. The disease is not contagious. There are indications that it is hereditary among certain ethnic groups and autoimmune in nature. Onset is most common in the late teens and early 20’s. HS outbreaks are painful in tender areas and may persist for years with interspersed periods of inflammation, often culminating in sudden drainage of pus. This process often forms open wounds that will not heal and frequently leads to significant scarring. For unknown reasons, people with HS develop plugging of their apocrine glands. Incision and drainage procedures may provide symptomatic relief. HS flares may be triggered by emotional/erotic stress, sweating, hormonal changes, heat and humidity, and the condition is exacerbated by friction from clothing.
_
4. Bromhidrosis (foul body odour):
Sweat itself does not smell bad. It’s the fatty acids skin bacteria create when they decompose the salty fluid. The sweat in the underarm and genital areas is most prone to create body odour. Smelly feet are feared too.
_
5. Heat rash (prickly heat, miliaria):
An itchy, red skin rash that often causes a stinging or prickling sensation. Heat rash develops when sweat ducts become blocked and perspiration is trapped under the skin. This causes irritation and results in the rash.
_
6. Dehydration:
Dehydration can occur if excessive sweating reaches 10 litres per day. When the water in the sweat evaporates, it leaves the salts (sodium, chloride and potassium) behind on your skin, which is why your skin tastes salty. The loss of excessive amounts of salt and water from your body can quickly dehydrate you, which can lead to circulatory problems, kidney failure and heat stroke. So, it is important to drink plenty of fluids when you exercise or are outside in high temperatures. Sports drinks contain some salts to replace those lost in the sweat.
_
7. Clothing issues:
Excessive sweat often stains and ruins clothing.
______
Body odour (BO) = Sweat odour
Apocrine glands are found typically under our armpits and groin. They grow and begin to function after puberty. Apocrine glands secrete a milky type of sweat, the main ingredient of which is water, along with proteins, lipids, fatty acids, cholesterols and iron-containing salts. When all that sweat encounters the bacteria brimming on your skin, odors start to rise. The bacteria break down the sweat and generate smelly by-products. In humans, the formation of body odors is mainly caused by skin glands excretions and bacterial activity. Between the different types of skin glands, the human body odor is primarily the result of the apocrine sweat glands, which secrete the majority of chemical compounds needed for the skin flora to metabolize it into odorant substances. This happens mostly in the axillary (armpit) region, although the gland can also be found in the areola, anogenital region, and around the navel. In humans the armpit regions seem more important than the genital region for body odor which may be related to human bipedalism. The genital and armpit regions also contain springy hairs which help diffuse body odors. The main components of human axillary odor are unsaturated or hydroxylated branched fatty acids with E-3M2H (E-3-methyl-2-hexenoic acid) and HMHA (3-hydroxy-3-methyl-hexanoic acid), sulfanylalkanols and particularly 3M3SH (3-methyl-3-sulfanylhexan-1-ol), and the odoriferous steroids androstenone (5α-androst-16-en-3-one) and androstenol (5α-androst-16-en-3α-ol). E-3M2H is bound and carried by two apocrine secretion odor-binding proteins, ASOB1 and ASOB2, to the skin surface. Body odor is influenced by the actions of the skin flora, including members of Corynebacterium, which manufacture enzymes called lipases that break down the lipids in sweat to create smaller molecules like butyric acid. Staphylococcus hominis is also known for producing thioalcohol compounds that contribute to odors. These smaller molecules smell, and give body odor its characteristic aroma. Propionic acid (propanoic acid) is present in many sweat samples. This acid is a breakdown product of some amino acids by propionibacteria, which thrive in the ducts of adolescent and adult sebaceous glands. Because propionic acid is chemically similar to acetic acid with similar characteristics including odor, body odors may be identified as having a vinegar-like smell by certain people. Isovaleric acid (3-methyl butanoic acid) is the other source of body odor as a result of actions of the bacteria Staphylococcus epidermidis, which is also present in several strong cheese types.
_
The primary cause of strong-smelling perspiration is bacterial flora. Sweat is naturally odorless, but when it reaches the skin’s surface, bacteria that normally live on the skin digest sweat and excrete the strong-smelling waste associated with smelly sweat. Bacteria break down the sweat produced by the apocrine sweat glands. Eccrine sweat is made up, mostly, of water and certain salts. Apocrine sweat is a thicker, milky colored sweat that contains fats. Human perspiration is largely odorless until it is fermented by bacteria that thrive in hot, humid environments. The human underarm is among the most consistently warm areas on the surface of the human body, and sweat glands provide moisture, which when excreted, has a vital cooling effect. When adult armpits are washed with alkaline pH soap, the skin loses its acid mantle (pH 4.5 – 6), raising the skin pH and disrupting the skin barrier. As many bacteria thrive in this elevated pH environment, this makes the skin susceptible to bacterial colonization. The bacteria feed on the sweat from the apocrine glands and on dead skin and hair cells, releasing trans-3-Methyl-2-hexenoic acid in their waste, which is the primary cause of body odor.
_
Factors such as food, drink, and diseases can affect body odor. Certain foods and beverages can increase the odor in sweat. Strong-smelling foods, such as onions, garlic, curry and other strong spices can make sweat smell. Likewise, caffeine, alcohol and tobacco smells can be excreted through sweat. Certain diseases can cause perspiration to smell strong. Diabetes, for instance, produces an acetone-like smell because the body either has low stores of insulin or is insulin-resistant. Without insulin, the body does not process sugar and begins to burn its own fat instead, and kidney diseases, too, can produce strong-smelling sweat. An individual’s body odor is also influenced by lifestyle, sex, genetics, and medication. The sweat of identical twins smells the same, according to a study published in Journal of the Royal Society Interface, even when they don’t eat the same foods. Trimethylaminuria (TMAU), also known as fish odor syndrome or fish malodor syndrome, is a rare metabolic disorder where Trimethylamine is released in the person’s sweat, urine, and breath, giving off a strong fishy odor or strong body odor.
_
The following suggestions may help you cope with sweating and body odor:
•Use antiperspirant. Nonprescription antiperspirants contain aluminum-based compounds that temporarily block the sweat pore. This reduces the amount of sweat that reaches your skin. This type of product may help with minor hyperhidrosis.
•Bathe daily. Regular bathing helps keep the number of bacteria on your skin in check. Dry yourself thoroughly, especially between the toes and under the arms.
•Choose shoes and socks made of natural materials. Shoes made of natural materials, such as leather, can help prevent sweaty feet by allowing your feet to breathe. When you’re active, moisture-wicking athletic socks are a good choice.
•Rotate your shoes. Shoes won’t completely dry overnight, so try not to wear the same pair two days in a row.
•Change your socks often. Change socks or hose once or twice a day, drying your feet thoroughly each time. You may want to try pantyhose with cotton soles. Use over-the-counter foot powders to help absorb sweat.
•Air your feet. Go barefoot when you can, or at least slip out of your shoes now and then.
•Choose clothing to suit your activity. Generally, wear natural fabrics, such as cotton, wool and silk, which allow your skin to breathe. When you exercise, you might prefer fabrics designed to wick moisture away from your skin.
•Try relaxation techniques. Consider relaxation techniques such as yoga, meditation and biofeedback. These can help you learn to control the stress that triggers sweating.
__
Bromhidrosis (foul body odour):
Osmidrosis or bromhidrosis is defined by a foul odor due to a water-rich environment that supports bacteria, which is caused by an abnormal increase in perspiration (hyperhidrosis). This can be particularly strong when it happens in the axillary region (underarms). In this case, the condition may be referred to an axillary osmidrosis. Bromhidrosis is a condition of abnormal or offensive body odour, to a large extent determined by apocrine gland secretion, although other sources may play a role. Sudoriferous (sweat) glands are divided into two types: apocrine and eccrine. There is some cross-over. Apocrine bromhidrosis is the most common type of bromhidrosis and results from bacterial breakdown of apocrine sweat, essentially all within the armpit area. Fatty acids and ammonia are the major products of bacterial breakdown and the odour has been described as pungent, rancid, musty or “sour and sweet”.
_
Apocrine bromhidrosis
1. Possibly associated with a positive family history
2. Only occurs after puberty, as the apocrine glands are not active until puberty is reached
3. More common in men than women, which may be a reflection of greater apocrine gland activity in men than in women
4. Skin usually appears normal except when bromhidrosis is associated with concomitant skin condition such as erythrasma.
5. Corynebacterium species are the most common bacteria found in the armpit and have been shown to produce the offensively smelling fatty acids.
_
Eccrine bromhidrosis:
1. Occurs in all races
2. May be rarely caused by metabolic disorders, e.g. amino acid disturbances (trimethylaminuria [fish odour syndrome]), sweaty feet syndrome, odour of cat syndrome
3. Possibly caused by ingestion of certain foods or medications
4. Bromhidrosis caused by bacterial degradation of the skin protein keratin may be associated with maceration and a thick mat of moist keratin present on the skin
5. The role of excessive eccrine secretion (hyperhidrosis) in causing bromhidrosis is unclear. It may promote the spread of apocrine sweat and cause further bacterial overgrowth and decomposition, or it may improve the symptoms of bromhidrosis by flushing away the more smelly apocrine sweat.
_
One distinction the clinician must be aware of is the difference between the true bromhidrosis patient and the bromhidrosiphobic individual. Bromhidrosiphobic patients have a morbid dread of bodily odours and their sensory delusions can be an early warning sign of schizophrenia.
_
Treatment for bromhidrosis:
The two main factors to consider when treating bromhidrosis are to:
1. Keep the number of naturally occurring skin bacteria to a minimum
2. Keep skin in the area, namely the armpit in apocrine bromhidrosis, as dry as possible
Improved hygiene and topical therapy are the main treatment options for mild cases of bromhidrosis and may include the following.
1. Washing the underarm at least twice daily with germicidal soap
2. Regular shaving of underarm hair to prevent accumulation of bacteria and sweat on hair shafts
3. Prompt removal of sweaty clothing
4. Try anti-odour anti-microbial socks and other garments impregnated with silver or copper
5. Use of topical deodorants
6. Treatment of coexisting skin conditions such as intertrigo, erythrasma and trichomycosis axillaris
7. Electrolysis to remove hair shaft and follicle
8. If hyperhidrosis is a contributing factor, this needs to be treated first
9. Bromhidrosis may be treated with a glycine-soja sterocomplex topical agent, which has shown encouraging results on both the intensity and quality of odor in patients with bromhidrosis.
_
Stress does actually make us sweat in a specific way that can increase body odor. Apocrine sweat is released when we’re stressed or upset, and is very conducive to bacteria throwing a sweat-based pool party. So if you’re finding yourself smelling strange after long, anguished meetings, you’re not cracking up; your body’s reacting to the heightened stress levels.
_
Why do certain clothes smell worse than others after we sweat?
A study published in the journal Applied and Environmental Microbiology shows that polyester apparel is much stinkier than cotton clothing after a hard workout, because it is less absorbent and promotes odor-causing bacteria. Polyester was a source for micrococcus enrichment, which was not seen on cotton. Micrococci are known for their enzymatic capacity to degrade fatty acids and amino acids into volatile malodorous compounds. These microbes are also an important reason why polyester is stinkier after exercise. Like natural cotton, wool can help you avoid a smelly clothes hamper. While wool will permit microbial growth, it breeds mostly nonodorous bacteria.
_
Does shaving your armpits reduce sweating and sweat odour?
Unfortunately, shaving your armpits won’t make you sweat less because the practice doesn’t affect the glands that produce perspiration. The apocrine glands that produce sweat are under the skin and not in the hair itself. These glands will continue to produce perspiration even when the hair is shaved down to skin level. The perspiration will continue to leak out of the hair’s openings, even if there are fewer openings because the hair is shorter or shaved down to the skin. However, shaving armpit hair can help reduce body odor. Regular shaving of underarm hair prevents accumulation of bacteria and sweat on hair shafts. Also, because hair is porous, it readily absorbs odors.
Counter-view:
Underarm hair whisks the moisture away from the skin and aids in keeping the skin dry enough to prevent or diminish bacterial colonization. The hair is less susceptible to bacterial growth and therefore is ideal for preventing the bacterial odor.
______
Heat rash:
Miliaria also called “sweat rash”, “heat rash” or “prickly heat” is a skin disease marked by small and itchy rashes. Miliaria is a common ailment in hot and humid conditions, such as in the tropics and during the summer season. Heat rash can be prevented by staying in cool areas and wearing loose clothing. Although it affects people of all ages, it is especially common in children and infants due to their underdeveloped sweat glands. Adults usually develop heat rash in skin folds and where clothing causes friction. In infants, the rash is mainly found on the neck, shoulders and chest. It can also show up in the armpits, elbow creases and groin. Miliaria arises from obstruction of the sweat ducts. It is commonest in hot, humid conditions but may occur in desert regions. It affects up to 30% of people exposed to these climatic conditions. However, there is a striking variation in individual susceptibility. Very young infants are especially prone to it. Miliaria may begin within a few days of arrival in a tropical climate but is maximal after 2-5 months. In hospital, miliaria is typically seen on the backs of people who are lying for prolonged periods in bed, particularly when they are sweating from an infection, heart attack or chemotherapy, or have been immobilized by a stroke, head injury or orthopaedic operation.
_
Pathophysiology of heat rash:
Heat rash begins with excessive perspiration, usually in a hot, humid environment. The perspiration makes it easier for dead skin cells and bacteria on the skin to block the sweat glands, forming a barrier and trapping sweat beneath the skin, where it builds up, causing the characteristic bumps. As the bumps burst and sweat is released, there may be a prickly, or stinging sensation that gives this condition its name. Miliaria occurs when the sweat gland ducts get plugged due to dead skin cells or bacteria such as Staphylococcus epidermidis, a common bacterium that occurs on the skin which is also associated with acne. The glands, still stimulated by high temperatures, continue to secrete. Sweat builds up in the duct, causing enough pressure to rupture the duct where it meets the epidermis. Sweat also escapes the duct to adjacent tissues (a process called miliaria). The trapped sweat leads to irritation (prickling), itching and to a rash of very small blisters, usually in a localized area of the skin. Heat rashes are more common in places with hot, humid climates because people sweat more. Intense exercise associated with lots of sweating may cause a heat rash, especially if the clothing worn does not allow adequate air circulation. Newborns, infants, the elderly, and obese individuals with large areas with skin-on-skin contact areas (for example, a large overlapping area of abdominal fat) are at risk for developing heat rash. They all are especially at risk if they are immobile for long periods of time and parts of the skin aren’t exposed to circulating air, which results in the inability of the sweat ducts to “breathe” (evaporative cooling).
_
It is uncertain why some people get heat rashes and others don’t. The sweat gland ducts can become blocked if excessive sweating occurs, and that sweat is not allowed to evaporate from a specific area. Some examples of how blockage may occur include the following:
1. Creases in the skin like the neck, armpit, or groin have skin touching adjacent skin, which makes it difficult for air to circulate, and prevents sweat evaporation.
2. Tight clothing that prevents sweat evaporation.
3. Bundling up in heavy clothing or sheets. This may occur when a person tries to keep warm in wintertime or when chilled because of an illness with fever.
4. Heavy creams or lotions can clog sweat ducts.
5. Babies have immature sweat glands that aren’t able to efficiently remove the sweat they produce. They can develop heat rash if they are exposed to warm weather, are overdressed, excessively bundled, or have a fever.
6. Heat rash may occur as a side effect of some medications (for example clonidine).
_
What does heat rash look like?
The appearance of the heat rash depends upon where the excess sweat gets deposited in the skin. Tiny blisters that look like small beads of sweat are seen if the sweat is blocked at the most superficial layers of the skin where the sweat duct opens on the skin surface. Called miliaria crystallina, it has no symptoms other than these “sweat bubbles.” Classic heat rash or miliaria rubra occurs if the sweat causes inflammation in the deeper layers of the epidermis. Like any other inflammation, the area becomes red (and therefore the name rubra = red) and the blisters become slightly larger. Because the sweat ducts are blocked and don’t deliver sweat to the skin’s surface, the area involved is dry and can be irritated, itchy, and sore. This rash is also called prickly heat. Occasionally, the fluid-containing sacs (vesicles) of miliaria rubra become inflamed and pus-filled (pustular). This form is called miliaria pustulosa. Less commonly, after repeated episodes of prickly heat, the heat rash may inflame the deeper layer of the skin called the dermis, and cause miliaria profunda. This rash is made up of larger, harder bumps that are more skin colored. The rash begins almost immediately after exercise, and again no sweat can be found on the affected areas. Rarely, this type of heat rash may be potentially dangerous if enough skin is involved, since the lack of sweating can lead to heat-related illnesses like heat cramps, heat exhaustion, or heat stroke. Hypohidrosis then follows miliaria (post-miliarial hypohidrosis).
_
How can heat rash be prevented?
Prevention is the most important treatment for heat rash; by allowing the skin to be exposed to circulating air, the potential for sweat ducts to become blocked and the glands to become inflamed decreases. In other words, allow sweat to perform its evaporative cooling function will prevent heat rash. It is important not to bundle newborns and infants too tightly so that air can get to the skin, but it also is important to keep them warm enough. It is important to move individuals who are immobile (for example, some elderly, those with paralysis, or are weak) so all parts of the body can be exposed to fresh air. Of course, keeping the skin cool on hot days is also an important preventive measure to reduce excessive sweating.
Other strategies to prevent heat rash include:
•Avoid exercising in hot, humid weather
•Wear loose clothing made of breathable fabrics like cotton
•Use air conditioning
•Keep the skin clean with frequent baths or showers to prevent sweat glands from becoming clogged
•Reduce the amount of overlapping skin-on-skin (fat or weight loss)
_
Treating prickly heat:
Prickly heat is not a serious condition and rarely requires any specific treatment. The rash usually disappears after a few days. However, there are several things you can do to ease your symptoms:
1. Avoid excessive heat and humidity – if you need to go outside, spend time in the shade or take a small fan with you. Further exposure to the heat will cause you to sweat more and may make your rash worse. Drink plenty of fluids to avoid dehydration, especially in hot weather.
2. Wear loose cotton clothing – avoid wearing synthetic fibres, such as polyester and nylon, which trap heat easier than natural fibres.
3. Avoid further sweating. Keep your skin cool – a cool bath or shower will cool you down, soothe your skin and help prevent further sweating. Staying in an air-conditioned room for a few hours a day will also provide considerable relief. You can also use a cold compress, but don’t leave it on the skin for longer than 20 minutes. Cool water compresses and good ventilation will soothe inflamed areas.
4. Prickly heat powder is a talc admixture containing drying milk proteins (Labilin) and Triclosan to fight the infection. These include cooling menthol to help alleviate difficulty getting to sleep. This is an effective treatment—the powder stays on the skin longer and treats bacteria dispersed into bed linens, providing a reasonably dry refuge area for healing. Regular talcum powder will not reduce the rash but can alleviate burning and itching.
5. Calamine is probably as effective as anything for relief of discomfort, but because of its drying effect an emollient may subsequently be required.
6. For more marked cases, mild topical steroids often give reasonable relief of symptoms while natural resolution of the condition is awaited.
7. Antiseptics and antistaphylococcal antibiotics can combat bacterial overgrowth. Caution should be used with oil-based preparations (ointments and oily creams as opposed to water-based or aqueous lotions) that may increase blockage to the sweat glands and prolong duration of illness.
_
What is the prognosis for heat rash?
Heat rash or prickly heat tends to be self-limiting and gets better once the skin cools and is allowed to breathe. Prevention by not allowing heat to accumulate in body areas, followed by cooling the skin are the most common ways to obtain the best prognosis for heat rash.
______
Cholinergic urticaria (CU):
Cholinergic urticaria is one of the inducible forms of urticaria. Cholinergic urticaria is also sometimes called sweat urticaria. In the case of cholinergic urticaria wheals and itchiness occur in response to exercise, bathing, staying in a heated environment, or emotional stress. Cholinergic urticaria is not an uncommon disease and is one of the more common forms of urticaria. It affects both sexes, indeed particularly young people between the age of 15 and 25. According to a recent study more than one in ten of the 15 to 25-year olds suffer from cholinergic urticaria. Cholinergic urticaria often involves the formation of small pinpoint wheals that are typically surrounded by a larger reddened part of the skin. In most cases the skin changes occur within 2 to 20 minutes after the onset of sweating, generally starting on the neck and the upper part of the body. The patient often first notes itchiness or prickliness or burning of the skin. Once the body cools down again, the wheals disappear without a trace within minutes or hours. In mild cases only a few wheals appear, particularly on the upper body. In severe cases the entire body may be affected. Fortunately cholinergic urticaria rarely involves serious symptoms like angioedema (= swellings deep down in the skin), breathing difficulties, nausea, headaches or vascular collapse.
Causes:
Sweat hypersensitivity
Acquired anhidrosis and/or hypohidrosis
Idiopathic
_
Sweat hypersensitivity:
This subtype of CU refers to those who are hypersensitive to their own sweat. Diagnosis is made by injecting autologous (the person’s own) sweat into the skin. The hives are observed to coincide with perspiration points of sweating. Tanaka et al. found that the sweat hyper-sensitivities of CU and atopic dermatitis seem to be virtually the same, and therefore, the sweat-induced histamine release from basophils may also be mediated by a specific IgE for sweat in atopic dermatitis as well as CU. Rapid desensitization protocol using autologous sweat my help. Forced perspiration by excessive body warming (hot bath or exercise) used daily may reduce the symptoms through exhaustion of inflammatory mediators. This non-pharmacological treatment is contraindicated in those with CU as a result of hypohidrosis. Antihistamines are a commonly prescribed first-line treatment for conventional urticaria, but its effectiveness in the treatment of CU is rather limited in most cases. Some research suggests that first-generation antihistamines with anticholinergic properties such as diphenhydramine are most successful at treating CU. Ketotifen is both an antihistamine and also a mast cell stabiliser. In some cases it revealed a good effect in connection with cholinergic urticaria, even in patients who do not respond to other antihistamines. Due to the sedative effect ketotifen is, however, a second option drug and should only be administered in exceptional cases. Anticholinergics like Clidinium bromide and butylscopolamine bromide were successfully used for cholinergic urticaria. These drugs lead to reduced sweat production, flares, bloating, disturbed vision, palpitation (tachycardia) and a dry mouth may occur as unwanted side effects. Long-term surveys or studies with a greater number of patients are not available for this drug. In individual cases successful therapy was described using propranolol (Beta-Blocker), maprotiline (tetracyclic antidepressant with antihistaminic effect) and chlordiazepoxide (benzodiazepine).
_
Acquired anhidrosis and/or hypohidrosis:
This subtype of CU refers to those who have abnormally reduced sweating. Failure of the topical indicator to undergo a colour change during thermoregulatory sweat testing can indicate anhidrosis and/or hypohidrosis. A skin biopsy may reveal cellular infiltrates in sweat glands or ducts. Patients have severe heat intolerance (e.g., nausea, dizziness, and headache), and tingling, pricking, pinchy or burning pain over the entire body on exposure to hot environments or prolonged exercise which improve after cooling the body. It occurs in the absence of any causative skin, metabolic, or neurological disorders.
Pathophysiology:
The wheals, hypohidrosis, and pain seems to result from the low expression levels of acetylcholinesterase (AchE) and cholinergic receptor muscarinic 3 (CHRM3) in the eccrine gland epithelial cells. Activation of CD4+ and CD8+ T cell populations may be responsible for exerting a downmodulatory effect on the AchE and CHRM3 expressions.
_
Diagram above shows the overflow of acetylcholine to adjacent mast cells.
_
Treatment of CU with hypohidrosis:
First-line treatment is Steroid pulse therapy (methylprednisolone). In the absence of sweat, cold-water sprays and wet towels can be used increase the evaporative loss of heat from the skin. Shifting to cooler or air-conditioned environments when necessary can also reduce discomfort. In the event of severe hyperthermia (body temperature >106 °F/41 °C), drastic measures such as immersion in ice-cold water are necessary to prevent irreversible brain damage.
____
Sweating and hair loss:
Do you know sweat can actually cause hair loss? Surprised!! Yes, it is true. Well, often people have this mind-set that sweating more is good for health. But that’s not true at all. Though sweating is a healthy mechanism in dissipating excess heat from the body, however, excess sweating can be harmful to the hair and scalp due to lactic acid content in the sweat. There are studies that have shown that when the lactic acid in the sweat mixes with the keratin in the hair it leads to damage and hair loss. This is one reason why to a certain extent you might feel loss of hair when you are sweating or just after that. The damage caused lactic acid becomes evident at first when dry, brittle, weak hair is observed. In addition to damaging the hair, the lactic acid in sweat may cause inflammation, which is strongly believed to have a direct impact on hair growth, due to the restriction of blood supply to the hair (and therefore nutrient supply). While some studies suggest that lactic acid in sweat affect keratin and result in hair loss, most other studies claim that sweat itself does not cause any harm to your hair. But at the same time, poor hair hygiene along with excessive sweating will make the situation different. Scalp is a surface where dead skin cells accumulate over time. If scalp is not washed regularly, oil, sweat and dead skin cells together can cause dandruff and skin infections which in turn result in hair loss. Also when sweat mixes with flakes on the scalp it can block the pores and make the hair follicles inactive. The salt build-up after sweat evaporation also blocks these pores. This can also lead to hair loss to quite an extent.
_
How to avoid hair loss with sweating?
1. In hot and humid conditions, wash your hair more often to remove sweat, oil, and dirt and car for them.
2. Use clean cold water to wash your hair. Use a mild and pH balanced shampoo. Maintain good hair hygiene in summers as you sweat more in this season. But frequent use of warm water or aggressive use of shampoo may lead to a dry itchy scalp.
3. Brushing your hair will not only increase air circulation, but will encourage blood flow to the scalp there by increasing hair growth.
4. Keep your hair loose. Avoid tying up hair too tight. Avoid tight hairstyles or ponytails that can prevent the sweat from evaporating and trigger it to get accumulated with the dirt and oil in the scalp and thus cause hair loss. Keep the hair loose to enhance passing of air. After exercising, keep your hair loose so that it has room to breathe.
5. Steaming removes sweat and oil from the scalp and opens all clogged pores of your hair follicles.
_____
Excessive sweating and social anxiety:
Excessive sweating is a symptom of social anxiety. If you do not sweat profusely when by yourself, and should you find your perspiration to be caused by exposure to the possibility of negatively judged by other people, you may have social anxiety. People who are anxious may experience sweating on their face, palms or under their arm pits. Unfortunately, excessive sweating may be apparent to others. Facial sweating may be distressing for males and females. However, women who wear makeup may have an additional problem of makeup running due to their profuse perspiration. Sweaty palms may be embarrassing when one is required to hold or shake hands. Underarm sweat may leave visible patches on one’s clothes. People with profuse sweating consider their perspiration is shameful and that they will be unfavourably evaluated because of it. Excessive sweating sufferers worry that people will believe they are lying, unwell, nervous or weak and therefore will not want to associated with them. Embarrassment and fear of sweating can lead to sufferers leading restricted lives; avoiding some social scenarios completely or developing subtle avoidance behaviours such as:
•wearing their hair over their face rather than pulling it back into a pony tail or having some other face revealing hairstyle
•wiping their hands and face
•routinely carrying cold drinks with them
•choosing to wear garments which they consider are less likely to show perspiration
•excessive use of antiperspirants
•avoiding garments which fit snugly under the arms
•avoiding wearing synthetic fabrics
•changing their clothes several times per day
•having the air-conditioning on high
•wearing insufficient clothing for the climate
•avoiding shaking or holding hands because of sweaty palms
The hyperhidrosis sufferer may worry they will perspire in a particular social setting and this anticipatory anxiety heightens the problem. People who have anxiety about sweating profusely try to hide and/or control their perspiration and their efforts to do so only maintain and exacerbate the problem. It is important for people to try to overcome their feelings of shame and embarrassment and stop going to extreme lengths to hide or prevent perspiration. Your efforts to conceal and/or prevent sweating are causing disruption to your life and can be a bigger handicap than the perspiration itself.
Hyperhidrosis sufferers need to focus on two facts:
•People may not register that you’re sweating
•Should someone observe you are perspiring, they may not judge you badly for doing so.
For example, a marketing executive is giving a presentation in a work context about his product. He may be exhibiting facial sweating but his audience could interpret that positively, believing that he is very passionate and enthused about his product.
_
The figure above shows positive feedback loop of sweating and anxiety. Excessive sweating leads to anxiety on the presumption that they will be unfavourably evaluated because of it. Anxiety will provoke further sweating due to activation of sympathetic nervous system.
_____
Sweat stains:
_
Sweat itself is clear, but when sweat patches get on your clothes and dry, the salt, proteins and oils in your sweat may leave a residue. This usually disappears with normal machine washing. Sweat stain problems occur if the sweat patches are left to dry and not washed for a long time, or if there’s a build-up of antiperspirant or deodorant product mixed in. Over time, the aluminium in the product and the salt in your sweat combine to form a yellow sweat stain, making it harder to remove with normal washing. You may have to use special stain remover. Dark colors like navy and black won’t show wet stains that badly, and neither will very light colors like white. Grays, blues, and bright colors are the worst options for hiding sweat.
How to prevent sweat stains:
1. Wear loose clothing made of natural fibres like cotton, linen and wool. This will allow your sweat to evaporate more easily.
2. Make sure your antiperspirant deodorant is dry before dressing or use a ‘dry on application’ product like an aerosol.
3. Don’t use too much product, as this can lead to build-up and cause yellow sweat stains.
4. Wear a breathable undershirt to absorb sweat before it reaches the outer layer of your clothing.
____
Sweating sickness:
Sweating sickness, also known as “English sweating sickness” was a mysterious and highly contagious disease that struck England, and later continental Europe, in a series of epidemics beginning in 1485. The last outbreak occurred in 1551, after which the disease apparently vanished. The onset of symptoms was dramatic and sudden, with death often occurring within hours. Though its cause remains unknown, it has been suggested that an unknown species of Hantavirus was responsible for the outbreak. The disease began very suddenly with a sense of apprehension, followed by cold shivers (sometimes very violent), giddiness, headache and severe pains in the neck, shoulders and limbs, with great exhaustion. After the cold stage, which might last from half an hour to three hours, the hot and sweating stage followed. The characteristic sweat broke out suddenly without any obvious cause. Accompanying the sweat, or after was a sense of heat, headache, delirium, rapid pulse, and intense thirst. Palpitation and pain in the heart were frequent symptoms. No skin eruptions were noted by observers including Caius. In the final stages, there was either general exhaustion and collapse, or an irresistible urge to sleep.
________
________
Treatment of hyperhidrosis:
In order to decrease general sweating, one has to cut down the nerve impulses to the sweat glands, cut down on the acetylcholine, destroy the glands, or block off their ducts, so that the sweat cannot flow out onto the skin. One of the main ways to cut down sweating is to use a medicine on the surface of the skin to cause the sweat to thicken and plug up the ducts, which is how the antiperspirants that are often used under the arms to decrease underarm sweat and odor work. These usually contain aluminium metal salts, such as aluminium chloride, which have to be frequently reapplied, or else the clumps in the ducts will get dissolved, unblocking the ducts and permitting sweating. The sweat glands themselves can be destroyed, but since they are so small and numerous, and are located deep in the skin, methods such as electrolysis (which uses electric currents to destroy the hair roots) are not very practical. If only a particular area of the skin, such as the underarms, is causing sweating problems, there have been some reports on the use of liposuction to remove the apocrine sweat glands there. Various conservative and surgical treatments exist for hyperhidrosis. Conservative treatment options are the local application of aluminium chloride, tap water iontophoresis, and the intracutaneous injection of botulinum toxin. If other treatments are not effective, various surgical procedures to control severe sweating may be tried. Excessive sweating limited to the armpits is sometimes treated by removing the sweat glands via surgery or liposuction. Excessive sweating limited to the palms can be treated by a procedure called endoscopic transthoracic sympathectomy, in which the nerves leading to the sweat glands are cut. However, surgery can cause permanent complications such as phantom sweating (a sensation of sweating, but no sweat exists), compensatory sweating (increased sweating in untreated parts of the body), gustatory sweating, nerve pain, and Horner syndrome. Systemic drugs (e.g. anticholinergic substances) can be used in the treatment of generalized hyperhidrosis.
_
Treatment of hyperhidrosis include following measures:
1. General measures
2. Topical applications
3. Drug treatment
4. Tap water Iontophoresis
5. Botulinum toxin injection
6. Surgical removal of axillary sweat glands including microwave and laser treatment
7. Sympathectomy
8. Cognitive behavioural treatment
9. Alternative medicine
_
1. General measures:
Don’t wear heavy clothes that will trap sweat. Instead, wear light, breathable fabrics such as cotton and silk. Bring along an extra shirt when you know you’ll be exercising or outdoors in the heat. Your feet can sweat too, so wear socks that wick moisture away from them (merino wool and polypro are good choices). Shower or bathe every day using an antibacterial soap to control the bacteria that can inhabit your sweaty skin and cause odors. Dry yourself completely afterward, and before applying antiperspirant. Use underarm liners and shoe inserts to absorb sweat so it doesn’t ruin your clothes or starts to smell. Change clothing and footwear when damp. Change your socks regularly, twice or three times a day if you have to. Avoid synthetic fibers. Socks containing silver or copper reduce infection and odour. Use absorbent insoles in shoes and replace them frequently. Besides hot outdoor temperatures or a killer workout, emotions (such as feeling stressed during a job interview) can also make you sweat. Anything you can do to decrease your anxiety, such as deep breathing or other relaxation techniques, will decrease the potential stimulation of neurotransmitters that can then stimulate your sweat glands. Absorbents like talc, starch and other powders may be applied to absorb excessive sweat. Armpit shields are pads worn in the armpit to protect a garment from perspiration. The sanitary towels for your armpits stick onto your armpits, the product claims to stop you getting sweat patches. They claim to absorb your excess sweat for up to eight hours.
_
Some foods, beverages and habits encourage the body to sweat more ought to be avoided.
-Spicy foods
-Garlic and onion – these also make body odor worse, as do strong spices like curry.
-Caffeine
-Alcohol
-Nicotine (tobacco products)
___
2. Topical applications:
Antiperspirants and deodorants:
Deodorant targets the bacteria that hang around your armpits. Ingredients like triclosan in deodorants make the skin in your underarm too salty or acidic to support the indigenous bacteria that are meant to thrive there. Without any bacteria to feast on the proteins and fats delivered through your sweat, no smell is produced. Antiperspirants cut down on body odor using the exact opposite principle: They actually keep you from sweating. Without any sweat, the bacteria found in abundance in your underarms don’t have anything to eat. Most antiperspirants have some of the same ingredients found in deodorants that kill bacteria as a failsafe. Their main function, however, is to keep you from perspiring. They do this through ingredients like aluminum and zirconium, which plug the sweat glands found in your underarms. When you apply antiperspirant, it’s literally no sweat. Antiperspirants and deodorants come in four main categories: stick, aerosol, clinical soft solid and roll-on. Sticks are a solid block and have the largest application surface, making them good for heavy perspiration. Aerosol is a spray format that goes on instantly dry. Clinical soft solids allow for precise application, while moisturizing your skin and delivering advanced sweat protection. Roll-ons are easy to apply and provide basic wetness protection. In the United States, the Food and Drug Administration classifies and regulates most deodorants as cosmetics, but classifies antiperspirants as over-the-counter drugs.
_
Excessive sweating can be controlled to some degree with commercial antiperspirants. However, stronger treatment is often needed, especially for the palms, soles, armpits, or genital area. A prescription-strength aluminum chloride solution may help. At night, the person first dries the sweaty area and then applies the solution. In the morning, the person washes the area. Sweat production is at its lowest at night, giving the active ingredients in antiperspirants a better chance to get into your pores and block perspiration in the morning. Its okay to reapply in the morning, but don’t worry about the product washing away in the shower because the ingredients have already penetrated your sweat ducts. At the start of treatment, the person must apply the solution several times until the sweating is controlled. Then an application once or twice a week is sufficient to maintain relief for as long as necessary. The solution should not be applied to inflamed, broken, wet, or recently shaved skin. Sometimes doctors give the person an anticholinergic drug (such as glycopyrrolate or oxybutynin) to take before applying the solution to prevent sweat from washing the aluminum chloride away. Your hands, feet, face, back, chest, and even groin have high concentrations of sweat glands. Gliding or spraying antiperspirants on these areas can help keep you dry, but skip sensitive areas such as your face or private parts. Deodorants are applied only in armpits as apocrine sweat of axilla is mainly responsible for body odour.
_
The figure below shows deodorants applied to axilla (armpits):
_
Antiperspirants usually contain aluminum or zirconian as active ingredients, both of which, upon contact with water, will physically clog the sweat glands and stop them from producing sweat. Antiperspirants are most effective when applied to very dry skin. If you apply them in the morning right before you head out, or right after you get out of the shower, you’ll likely already be sweating or have wet underarms. If the skin’s surface is wet, the chemical reaction that forms from the aluminum will happen on the surface of the skin instead of in the pores, preventing the sweat glands from getting blocked. Instead apply these products at night when sweat production is at its lowest. Even when you shower the next morning, the antiperspirant will still be effective, since it can last for a few days. Then, after your shower, if you want a scent, you can apply a deodorant for fragrance. Aluminium-based complexes react with the electrolytes in the sweat to form a gel plug in the duct of the sweat gland. The plugs prevent the gland from excreting liquid and are removed over time by the natural sloughing of the skin. The metal salts work in another way to prevent sweat from reaching the surface of the skin: the aluminium salts interact with the keratin fibrils in the sweat ducts and form a physical plug that prevents sweat from reaching the skin’s surface. Aluminium salts also have a slight astringent effect on the pores; causing them to contract, further preventing sweat from reaching the surface of the skin. The blockage of a large number of sweat glands reduces the amount of sweat produced in the underarms, though this may vary from person to person. Aluminum salts for topical use are added to many freely available antiperspirants, mostly at concentrations of 1% to 2%. Medications contain aluminum chloride in concentrations of up to 15% to 25%. Repeated daily applications are necessary. Side effects include skin irritations, burning or stabbing dysesthesias. Though there are concerns amongst some people that the aluminum salts in antiperspirants may cause Alzheimer’s disease or breast cancer, both the Alzheimer’s Association and the National Cancer Institute report that no scientific evidence has linked antiperspirants to either disease.
_
Heat rash occurs due to blocked sweating and antiperspirants also block sweating, so does antiperspirant cause heat rash?
No.
Heat rash begins with excessive perspiration, usually in a hot, humid environment and the skin is not exposed to circulating air resulting in the inability of the sweat ducts to “breathe” (evaporative cooling) due to tight clothing or immobility; which makes it easier for dead skin cells and bacteria on the skin to block the sweat glands, forming a barrier and trapping sweat beneath the skin, where it builds up, causing the characteristic bumps. Antiperspirants contain aluminium salts and aluminium-based complexes react with the electrolytes in the sweat to form a gel plug in the duct of the sweat gland. The plugs prevent the gland from excreting liquid and are removed over time by the natural sloughing of the skin. The aluminium salts interact with the keratin fibrils in the sweat ducts and form a physical plug that prevents sweat from reaching the skin’s surface. Aluminium salts also have a slight astringent effect on the pores; causing them to contract, further preventing sweat from reaching the surface of the skin; all these reduce sweat production. So sweat is blocked in sweat gland even before it has an opportunity to come to surface to mix with dead skin cells and bacteria. In fact, antiperspirants containing aluminium salts can stop your sweat, which can help prevent heat rash.
_
Other Topical applications:
Topical agents for hyperhidrosis therapy include topical anticholinergics, boric acid, 2-5% tannic acid solutions, resorcinol, potassium permanganate, formaldehyde (which may cause sensitization ), glutaraldehyde, and methenamine. All of these agents are limited by staining, contact sensitization, irritancy, or limited effectiveness. Astringent external substances such as formaldehyde or glutaldehyde are used only to a limited extent as they may cause allergic reactions and local skin irritations. In cases of gustatory sweating (in diabetes or Frey’s syndrome), 0.5% glycopyrrholate, an anticholinergic substance, may be applied topically. Generally, topical applications are suitable only for cases of focal hyperhidrosis. Topical glycopyrrolate application may be effective and safe for the treatment of excessive facial sweating in primary craniofacial and secondary gustatory hyperhidrosis following sympathectomy.
_
3. Drug treatment
Systemic agents used to treat hyperhidrosis include anticholinergic medications. Anticholinergics such as propantheline bromide, glycopyrrolate, oxybutynin, and benztropine are effective because the preglandular neurotransmitter for sweat secretion is acetylcholine (although the sympathetic nervous system innervates the eccrine sweat glands). Many medical professionals and hyperhidrosis patients experience great success with anticholinergic therapy. Anticholinergics have not, however, been studied in controlled clinical trials specifically for hyperhidrosis. Their FDA approval is, on the other hand, based on studies involving other medical conditions. Their use for hyperhidrosis is thus “off-label”. Of course, it is common for medications to be used “off-label” and a substantial safe history of off-label use of these meds has helped many doctors to feel confident about them. Some anticholinergics, such as glycopyrrolate and oxybutynin, have even been found to be safe in young children. The use of anticholinergics may be unappealing because their adverse effect profile includes mydriasis, blurry vision, dry mouth and eyes, difficulty with micturition, and constipation. A newer study (published in 2015) reported a potential link between the development of dementia and long-term, high-level anticholinergic use by people age 65 and older. When taking anticholingerics, the body may have more difficulty keeping itself cool with the sweat mechanism ‘turned off.’ Therefore, athletes, people who participate in sports, people who work outdoors and anyone who may potentially cause themselves injury by becoming overheated must use extra care when considering these treatments. Patients or parents of children taking the medication must remain aware of temperature, water intake, exertion, and any symptoms of overheating such as pale skin, dizziness, muscle cramping, weakness, headache, and nausea.
_
Oxybutynin chloride is a weak cholinergic blocker. It has 1/3 and 1/25 propantheline power atropine, its spasmolytic effect was 2 times higher than that of the first and 10 times of that of the latter. Oxybutynin is readily absorbed from the gastrointestinal tract, reaching peak effect between 3 and 6 h after intake and its action lasts from 6 to 10 h, reaching 24 hours in slow-release preparations. It is metabolized by the cytochrome P450 enzyme systems, particularly CYP3A4, with a half-life of 2 to 3 h. The lower dose of oxybutynin is 5 mg at night before bed. Thus, the patient does not present side effects of the drug. Generally, the effective dose requires taking 15 mg per day, tid 5 mg fractionated during the day. However, increasing the dose should be gradual so as to provide adherence to treatment. Propantheline dose is 15–30 mg up to three times daily. Only one randomized, placebo-controlled, double-blind study exists that shows a positive effect of methanthelinium bromide 50 mg twice a day in axillary hyperhidrosis, but not palmar hyperhidrosis. The effectiveness of scopolamine and propantheline has been documented in individual case reports only. Here is another promising use for oral anticholinergic medications. Some physicians and their patients have had great success treating sweaty palms and sweaty feet by adding a crushed anticholinergic tablet to the water used during iontophoresis.
_
There are other oral medications besides anticholinergics that are successful in treating patients with specific types of hyperhidrosis, as well. Beta blockers (propranolol) and benzodiazepines work by “blocking” the physical manifestations of anxiety. These meds act on the central nervous system and are best for patients who experience episodic or event-driven hyperhidrosis (such as excessive sweating brought on by job interviews or presentations). Side effects limit their long-term use. For instance, benzodiazepines can be habit-forming and many patients cannot tolerate the sedative effects caused by both of these drug therapies. There have also been single-case or small samples of patients with specific types of hyperhidrosis who responded to a variety of other oral medications. Agents such as Clonidine, indomethacin, gabapentin, calcium channel blockers and multiple others have shown effectiveness in very specific cases of hyperhidrosis. Antidepressant drugs such as amitriptyline and paroxetine, as well as antihypertensive drugs such as beta blockers, calcium channel antagonists (diltiazem), alpha antagonists (phentolamine), and alpha-2 agonists (clonidine) have been described in single case reports as merely slightly to moderately effective. Clonidine in particular is thought to be more effective for menopause-related hyperhidrosis or hyperhidrosis secondary to antidepressants. Fludrocortisone 0.3 mg daily has been used to control sweating in quadriplegics with orthostatic hypotension.
_
Oral hyperhidrosis medications are best suited for patients with certain types of excessive sweating such as excessive facial sweating (cranio-facial hyperhidrosis), generalized hyperhidrosis, and those who have not had success using other first-line therapies such as clinical strength antiperspirants, iontophoresis, Botulinum toxin, or a combination of these. People who have compensatory sweating from ETS surgery, sweat over a large body area (such as the back), need temporary relief from sweating every once in a while for a special event (such as a performance or presentation), or have excessive sweating secondary to a medication or medical condition may also find success with oral medications.
_
4. Tap water Iontophoresis:
Tap water iontophoresis is the method of choice for the initial treatment of palmar and plantar hyperhidrosis because of its low side effect profile and effectiveness. The hands or feet are immersed into water or moist electrodes are applied. The standard therapy consists of continuous direct current; alternatively, pulsed direct current can be used, which is easier to handle but probably slightly less effective. In palmoplantar hyperhidrosis, the daily treatment of each palm or sole for 30 minutes at 15-20 mA with tap water iontophoresis is effective. Intact skin can endure 0.2-mA/cm2 galvanic current without negative consequences, and as much as 20-25 mA per palm may be tolerated. Numerous agents have been used to induce hypohidrosis, including tap water and anticholinergics; however, treatment with anticholinergic iontophoresis is more effective than tap water iontophoresis. The assumed mechanism of action is a reversible disruption of the ion transport in the secretory tangle of the sweat glands, possibly owing to accumulation of protons in the sweat gland ducts. This therapy is effective in up to 81% of patients but is very time consuming; initially it should be administered at least three times per week. In the maintenance phase, one session per week should be sufficient. Iontophoresis must not be used in pregnant women or patients with pacemakers. Side effects include erythema, local burning pain, and blistering.
_
Method:
The treatment consists in placing the hands and/or the feet in flat containers which are partially filled with water and have electrodes and cables connected to a DC generator. The intensity of the current is increased with a knob until a slight tingling sensation is felt. For the armpits and other parts of the body, there are special electrodes available (electrode pads of absorbent material) that have to be soaked in water before use. Tap water seems to be an ideal conducting fluid, better even than saline for the purpose of inhibiting the sweat glands, despite saline being a better conductor. Only exceptionally, in areas with tap water of extremely low conductivity (almost no mineral content), half a teaspoon of bicarbonate can be added to 1 liter of water in order to improve conductivity. Each treatment lasts around 15-30 minutes. In the beginning, it should be performed daily or every 2 days over a period of 1-2 weeks until the sweating stops. The duration of dryness varies from person to person and can last for several days, up to 3-4 weeks. Once the moisture reappears, a maintenance treatment should be carried out. Some patients undergo treatment regularly once a week as a preventive measure.
_
Here are some important tips:
•If possible, learn how to use iontophoresis effectively in a clinical office from a trained health professional before trying it at home.
•Expect to feel a mild tingling sensation during iontophoresis.
•Know that the electric current used during iontophoresis is not strong enough to cause a harmful shock but it could startle you, so don’t remove your hands or feet from the water during treatment.
•Don’t use iontophoresis if you are pregnant, have a pacemaker, have a substantial metal implant in the current path (such as a joint replacement), or have a cardiac condition or epilepsy.
•Remove jewellery before iontophoresis treatments.
•Cover scratches, tender cuticles, and nicks in your skin with a petroleum jelly (like Vaseline) before treatment. If redness occurs at the water line, cover that area with petroleum jelly, too. Keep in mind that petroleum jelly is, however, a barrier to iontophoresis, so apply it only as necessary.
•Treat any post-treatment, mild skin irritation or redness with 1% hydrocortisone cream.
•Talk to your doctor if the treatment doesn’t seem to be working. Adding baking soda or a prescription medicine (anticholinergic) to the water can help.
•If excessive dryness occurs, use a moisturizer after treatment sessions.
______
Therapies that have been shown to reduce the rate of sweat production include iontophoresis, topical application of aluminum chloride, and administration of anticholinergic agents and beta-blockers. For axillary hyperhidrosis, however, iontophoresis is cumbersome: several times a week, wet sponges wrapped around metal electrodes must be inserted into each armpit for 20 minutes and a low-voltage current applied to the skin, producing a stinging sensation. Application of aluminum chloride is often discontinued because of skin irritation. Anticholinergic agents and beta-blockers may have substantial side effects.
______
5. Botulinum toxin injection:
Injection of botulinum toxin is the most effective nonsurgical therapy for focal hyperhidrosis. Botulinum toxin type A can be injected directly into the armpits, palms, or forehead to inactivate the nerves that trigger sweating. It prevents sweating for about 5 months depending on the dose. Botulinum toxin is a highly effective neurotoxin that is formed by the anaerobic bacterium Clostridium botulinum. Botulinum toxin is injected intradermally and inhibits the release of acetylcholine from the sudomotor synapses. Diffusion of the toxin and inhibition of acetylcholine release from the presynaptic terminals of the sudomotor nerves seems to be the underlying mechanism producing anhidrosis after botulinum toxin A injections. However local administration of botulinum toxin in human skin completely blocked the sweating response to exogenous acetylcholine, lending support to a post-synaptic mechanism by which botulinum toxin can abolish sweating. The duration of its effect depends on the location and the preparation used and is 4 to 7 months, until the sudomotor nerve fibers have regrown. Initially, botulinum toxin was used to treat muscular dystonias, such as blepharospasm or torticollis. In the meantime, however, it has been licensed for use in axillary hyperhidrosis. The preparations are very costly, however, and several injections are necessary, which may be painful. The main side effect, especially when injected into the hand, is paralysis of the hand muscles. Therapeutic failure owing to antibody formation is possible but extremely rare. A 2008 study found botulinum toxin type A to be more effective than topical 20% aluminum chloride for the treatment of moderate-to-severe primary focal axillary hyperhidrosis.
_
Research demonstrates that treating excessive sweating of the armpits, hands, feet, head and face (craniofacial), and other relatively small body areas (like under the breasts) with botulinum toxin A is safe and effective. When used to treat underarm excessive sweating, Botulinum toxin A has been shown to result in an 82-87% decrease in sweating. Results start to be noticeable approximately 2 to 4 days after treatment with the full effects usually noted within 2 weeks. Dryness typically lasts 4 to 12 months but some studies have found it can last as long as 14 months. Additional statistics from published research studies have shown that repeated treatment with botulinum toxin A is safe and effective for hyperhidrosis and consistently results in meaningful, long-lasting improvements in an excessive sweating patient’s symptoms, daily functioning, and quality of life. Botulinum toxin A treatment for hyperhidrosis has also been scientifically proven to improve on-the-job productivity. While sweating is an essential body function for temperature-control, localized body areas house only a small percentage of the body’s sweat glands (the underarms, for instance, are home to less than 2% of the body’s sweat glands.) The temporary cessation of these sweat glands’ functioning, therefore, has little to do with body thermoregulation. Compensatory sweating (sweating on other body parts, common after ETS surgery) has not been found to be a concern. In the case of palmar (hand) excessive sweating, research shows that Botulinum toxin A is 80-90% effective. Repeat injections are needed after 6 months. Botulinum toxin A injections work well on the head and face but the injection technique requires skill, so patients should seek an experienced practitioner. A potential side effect of Botulinum toxin A injections in the face as a treatment for sweating is asymmetry, particularly of the forehead. This can happen if some of the Botulinum toxin A diffuses into the facial muscles. Such asymmetry, however, is always temporary and can, if necessary, be balanced-out by additional Botulinum toxin A injections. Botulinum toxin A can also be used for plantar hyperhidrosis (excessive sweating of the feet) but patients report more pain during plantar injections and statistics indicate the treatment is less effective than when used for other body sites; indeed, some data suggests that 50% patients are dissatisfied with the results.
_
Intradermal botulinum toxin injections for the treatment of palmar hyperhidrosis:
For palmar hyperhidrosis, intradermal injections spaced about 1–2 cm apart seem to give the best results. About 2 units of botulinum toxin A are injected per site as required, with a total dose of 100 units for each palm. The main limitation is that most patients find the injections painful and may require regional anesthesia via median, ulnar and radial nerve blocks at the wrist level. A similar technique and dosage of botulinum toxin A is used for the treatment of plantar hyperhidrosis, requiring regional nerve blocks of posterior tibial and sural nerves for anesthesia. Other methods of reducing the pain of injections have included high-intensity vibration devices, cool packs and liquid nitrogen spray, all with variable results.
_
Intradermal botulinum toxin injections for the treatment of axillary hyperhidrosis:
Focal axillary hyperhidrosis is treated with 50–200 units of botulinum toxin A per axilla. The usual starting dose is 50 units per axilla. The drug is injected intradermally using a 13-mm-long 30-gauge needle. Injections are done in a grid-like pattern in order to cover the entire affected area, with injection sites generally 1–2 cm apart. There is no difference in efficacy of botulinum toxin A in the treatment of axillary hyperhidrosis when administered by subcutaneous or intradermal injection, but intradermal injections are reported to be more painful. The subcutaneous injection technique requires further study for validation of the results.
_
Safety information:
Botulinum toxin A may cause serious side effects that can be life threatening. Call your doctor or get medical help right away if you have any of these problems any time (hours to weeks) after injection of Botulinum toxin A:
•Problems swallowing, speaking, or breathing, due to weakening of associated muscles, can be severe and result in loss of life. You are at the highest risk if these problems are pre-existing before injection. Swallowing problems may last for several months.
•Spread of toxin effects. The effect of botulinum toxin may affect areas away from the injection site and cause serious symptoms including: loss of strength and all-over muscle weakness, double vision, blurred vision and drooping eyelids, hoarseness or change or loss of voice (dysphonia), trouble saying words clearly (dysarthria), loss of bladder control, trouble breathing, trouble swallowing. If this happens, do not drive a car, operate machinery, or do other dangerous activities
There has not been a confirmed serious case of spread of toxin effect away from the injection site when Botulinum toxin A has been used at the recommended dose to treat severe underarm sweating.
_______
Therapeutic algorithm for axillary and palmar/plantar hyperhidrosis:
_
Synergy of Techniques:
Botulinum, iontophoresis, and aluminium formulations may act synergistically and be used in combination for palmar and plantar hyperhidrosis. In some patients, a combination of iontophoresis, aluminium preparations and botulinum injection may therefore lead to a greater effect than any individually. This may then allow less frequent injections to be given with a consequent reduction in side effects and cost.
_
Evidence-Based Review of the Nonsurgical Management of Hyperhidrosis: a 2008 study:
The most common nonsurgical modern treatments for hyperhidrosis include topical treatments such as aluminum chloride, iontophoresis (usually with tap water), oral medications such as anticholinergics, and botulinum toxin type A. Topical treatments should always be first-line therapy. For those for whom such treatment fails, iontophoresis is typically recommended for those who have palmar or plantar hyperhidrosis, whereas botulinum toxin is often considered as first- or second-line therapy for severe axillary hyperhidrosis. Oral anticholinergics are considered after failure of all other nonsurgical treatments.
_
Treatment of hyperhidrosis is divided into local, systemic and surgical:
________
6. Surgical removal of axillary sweat glands including microwave and laser treatment:
Overactive sweat glands in the armpits may be removed by several methods, usually under local anaesthetic.
•Tumescent liposuction (sucking them out): Subcutaneous liposuction is another means of removing the eccrine sweat glands responsible for axillary hyperhidrosis. Compared with classic surgical excision, this modality results in less disruption to the overlying skin, resulting in smaller surgical scars and a diminished area of hair loss. Ultrasound Power-Assisted Tumescent Liposuction with curettage is better than Tumescent Liposuction.
• Subcutaneous curettage (scraping them out)
• Microwave thermolysis (approved by FDA in 2011)
•Subdermal Nd:YAG laser
• Surgery to cut out the sweat gland-bearing skin of the armpits. If a large area needs to be removed, it may be repaired using a skin graft. Surgical excision of the affected area (identified with iodine starch testing) removes the appropriate sweat glands, thereby eliminating sweating. This technique is particularly useful in axillary hyperhidrosis.
__
Microwave Thermolysis for Excessive Sweating:
The system works by directing energy at the sweat glands in the underarm. This procedure uses electromagnetic energy to destroy the sweat glands in your armpit. By destroying the sweat glands in the underarm, excessive sweating in that area stops immediately. While the sweat glands are being eliminated through electromagnetic technology, the top layers of the skin are simultaneously cooled and protected. Sweat glands are not believed to grow back after treatment so the effect can be seen almost immediately and results are lasting. For best results, two procedures spaced three months apart are recommended. Common and minor side effects include underarm swelling, redness, and tenderness lasting for several days. Numbness and tingling can occur in the upper arm or armpit and may last for about 5 weeks. Only 2% of the sweat glands in the body are located in the underarm area, so destroying them in this area does not affect the body’s ability to cool. Before the procedure, your doctor will numb the underarm area. Then your underarm skin is lifted into the system and microwave energy is directed to the sweat glands. The procedure typically takes an hour and involves no incisions or cuts; you should not feel any discomfort. In April 2012, clinical data from the University of British Columbia showed that microwave thermolysis was successful in reducing underarm sweat in over 90% of patients. The average sweat reduction was 82%. Patients rated their satisfaction with the treatment at 90% and at the 12-month follow-up visit, 90.3% had at least a 50% reduction in axillary sweat from baseline. The device tested provided efficacious and durable treatment for axillary hyperhidrosis. The treatment of primary axillary hyperhidrosis can be rewarding using noninvasive microwave technology. Because the microwaves preferentially target the region of skin where the sweat glands reside, leading to localized thermolysis of the sweat glands, patients can now benefit from permanent targeted sweat reduction. The microwave treatment has been shown to be safe and effective in >6000 procedures to date.
_
Laser thermolysis:
The treatment of axillary hyperhidrosis using the 1064-nm Nd-YAG laser was found to be effective and safe in a pilot trial. You may be familiar with the use of laser therapy to treat varicose veins, to perform delicate eye surgery, and to remove skin lesions. But did you know that lasers are also used to treat excessive sweating (hyperhidrosis) of the underarms (axilla)? A laser can be focused into a very narrow beam, enabling physicians to target specific body structures without injuring surrounding tissue. This makes laser therapy both powerful and precise – much more precise, in fact, than more traditional surgical tools. The heat from lasers also helps to reduce infection risks and to seal blood vessels to help prevent bleeding. Laser procedures can thus be done faster with quicker recovery than some other types of procedures, and most are performed in a doctor’s office on an outpatient basis – meaning you can go home, or even back to work, soon after your treatment is over. For the treatment of underarm sweating, lasers are useful in that they can precisely target, heat, and destroy the sweat glands, which are primarily found in a specific layer of tissue under the skin of the underarms. Tiny incisions (often so small they don’t even require a stitch) are made in the underarms to allow the laser tool to be passed under the skin. The procedure usually takes less than an hour to complete. In two studies, following a total of 33 patients over the course of six months, a single laser treatment session was shown to significantly reduce underarm sweating. The patients in the study received local numbing (anesthesia) to the underarms to minimize discomfort during the procedure. Side effects included swelling, bruising, and numbness, but these symptoms resolved after 1 to 2 weeks. Follow-up observations showed that both the eccrine glands (the sweat glands that produce clear, odorless, watery sweat) and the apocrine glands (the sweat glands that produce fatty sweat that becomes pungent when broken down by the skin’s normal bacteria) in the underarms had been ablated (or destroyed) by the laser treatment. Measurements taken six months after the treatment showed that underarm sweating was reduced by approximately 78%. Sweat glands are not believed to regenerate (or regrow) after they have been destroyed so the benefits of laser treatment for excessive sweating are commonly regarded as permanent.
_
7. Sympathectomy:
_
The principle of sympathectomy is to interrupt the nerve tracks and nodes (ganglia) which transmit the signals to the sweat glands. Basically, this can be achieved for all locations in the body, but only the nerve nodes responsible for the sweat glands of the palms and the face are accessible without the need for a major surgical procedure. Sympathectomy has been used as a permanent effective treatment since 1920. Usually, it is reserved for the final treatment option. Sympathectomy involves the surgical destruction of the ganglia responsible for hyperhidrosis. The second (T2) and third (T3) thoracic ganglia are responsible for palmar hyperhidrosis, the fourth (T4) thoracic ganglia controls axillary hyperhidrosis, and the first (T1) thoracic ganglia controls facial hyperhidrosis. Two surgical approaches are available: an open approach and a newer endoscopic approach. Open approaches include bilateral upper dorsal sympathectomy via the supraclavicular approach and percutaneous radiofrequency upper thoracic sympathectomy. The endoscopic approach has become favored because of its improvements in terms of complications, surgical scars, and surgical times. With this method the specialized surgeon enters the thoracic cavity and disrupts the sympathetic chain responsible for excessive hand sweating. This is an outpatient procedure and the patient can go home the same day. Endoscopic thoracic sympathectomy (ETS) is an effective treatment for hyperhidrosis; in one study, immediate positive results occurred in 832 (98%) of 850 patients. After a 31-month average follow-up, symptoms recurred in 17 patients. Improved quality of life has been described for upper limb hyperhidrosis after treatment with limited endoscopic thoracic sympathetic block at T4. Numerous complications are associated with this endoscopic treatment option; these include compensatory sweating (induction of sweating in previously unaffected areas of the body), gustatory sweating, pneumothorax, intercostal neuralgia, Horner syndrome, recurrence of hyperhidrosis, and the sequelae of general anesthetic use. Of 850 patients who underwent endoscopic transthoracic sympathectomy, 55% had compensatory sweating (mostly on the trunk), and 36% had gustatory sweating. In a similar study of 72 patients who underwent transthoracic endoscopic sympathectomy (T2 or T2 and T3) for palmar hyperhidrosis, the success rate was 93%; compensatory sweating occurred in an overwhelming 99% of patients within 1 month after surgery, and gustatory sweating occurred in 17%. The overall occurrence of severe compensatory hyperhidrosis was reduced after T3 ganglionectomy as opposed to ganglionectomies performed at all other levels. T4 ganglion interruption for palmar hyperhidrosis is an effective approach that can simultaneously minimize the rate of compensatory hyperhidrosis. Thus, T4 sympathectomy may be an effective cure. Its rate of compensatory hyperhidrosis appears to be remarkably low compared with T2 sympathetic ganglionic interruption. An effective treatment for such compensatory sweating is the intradermal injection of botulinum toxin. Li et al reported on minimizing endoscopic thoracic sympathectomy for hyperhidrosis of the palms using the skin temperature of the palms and Doppler-guided blood flow analysis as aids. Video-assisted thoracic sympathectomy may be preferable to no treatment for children with palmar hyperhidrosis and a poor quality of life.
_
Today, the treatment of choice for moderate to severe palmar and facial hyperhidrosis (but also axillary, especially if combined with palmar sweating) is ETS. This minimal-invasive endoscopic technique has been developed in recent years in a few hospitals in Europe, superseding Conventional Thoracic Sympathectomy, a very traumatic procedure performed in the past. The endoscopic technique is very safe, if performed by a surgeon experienced in this type of procedure, and leads to definitive cure in nearly 100% of patients, leaving only a minimal scar in the armpit. ETS is considered a last resort because it frequently causes serious, irreversible compensatory sweating (excessive sweating on large areas of the body or all over) as well as other debilitating effects such as extreme hypotension, arrhythmia, and heat intolerance. In fact, most physicians do not recommend ETS surgery because of the serious negative side effects of the procedure.
_
Pathophysiology of compensatory hyperhidrosis:
The sweat regulatory center in hypothalamus is in the preoptic area. Its sympathetic efferent discharges must be controlled by feedback negative or positive from the sympathetic afferent pathways. The sympathectomy in T2 block the feedback negative afferent stimuli to the hypothalamus, since section practically sever all afferent pathways, and would stimulate compensatory hyperhidrosis in the periphery due to the continuous release of efferent stimulation by the hypothalamus. The sympathectomy below this level cut a smaller number of afferent, avoiding blocking of the feedback and decreasing compensatory hyperhidrosis.
_
Endoscopic lumbar Sympathectomy (ELS) for feet sweating:
For excessive foot sweating a new procedure known as lumbar sympathectomy was developed since about 2005. With this procedure people who suffer specifically from excessive foot sweating or did not get enough relief via the ETS procedure, get relief with a high degree of success 98-99%. It’s important to note that the majority of people with hyperhidrosis have it in both the hands and feet. For this reason it is more common for people who had surgery for their hands then want the surgery for their feet. Why the hands first? Typically excessive hand sweating appears in the younger age group and is more socially and functionally troubling to people than their feet. However excessive foot sweating can be as severe as hand sweating, sometimes worse. Problems in everyday life such as social and functional settings can be difficult. Shoes can be ruined, sandals cannot be worn, heels can be too difficult to wear, and foot odor and fungal infection can become problematic. It can lead to marital problems as well as difficulties at the work place. The long term success rate of ETS for foot sweating is only 15-20% while ELS has a much higher success rate of 98%. Excessive armpit sweating that appears by itself (without hand and foot sweating) can be addressed, after all conservative methods have failed, with microwave or laser ablation and suction curettage on outpatient basis with the success rate of about 85%.
_____
Synopsis of hyperhidrosis treatment:
_____
8. Cognitive Behavioural Therapy (CBT) for Hyperhidrosis:
Cognitive behavioural therapy challenges the client’s beliefs as to how others perceive excessive perspiration. A CBT therapist may question the client’s beliefs about how apparent the sweating is. For instance, perspiration often feels worse than it appears. A therapist may give you video evidence of how intensely (or not) you sweat in feared social/performance situations. CBT also entails having the client confront the interpersonal and/or performance scenarios where they fear sweating. Therapy may also involve behavioural experiments where the sufferer deliberately draws people’s attention to his excessive sweating, so he gets the opportunity to see how people really do react to his perspiration. The sweating sufferer is likely to find that other people are not as judgemental of his sweating as he has always assumed them to be. If the person’s anxiety about excessive sweating subsides so will the problem. Another component of treatment may be attention training. If excessive sweating sufferers can focus their attention more effectively on their environment, rather than being self-focussed they may perspire less. Psychological treatment may entail learning relaxation strategies such as slow breathing.
_
Psychotherapy:
It has very limited effect in the majority of patients. Psychological problems are in most cases a consequence of hyperhidrosis, not the cause. Hence, psychiatric or psychopharmacologic therapy cannot cure this disorder; at most it may help the patient to accept living with the problem.
_
9. Alternative medicine:
Many patients, disappointed by the treatment offered by their doctors, have tried different methods of alternative therapy including homoeopathy, massage, acupuncture and phytotherapeutic drugs, in almost all cases without noticeable improvement. Alternative therapies to treat hyperhidrosis may include herbal substances such as sage tea or sage tablets, chamomile, valerian root, and St. John’s Wort. Acupuncture, biofeedback, hypnosis, and relaxation techniques have also been suggested as potential treatments. Currently there is little research to recommend such alternative therapies but this doesn’t discount their potential.
_________
_________
Anhidrosis/Hypohidrosis:
Reduced sweating is called hypohidrosis, if there is partial loss of sweating, or anhidrosis if there is complete lack of sweating. Anhidrosis happens when your sweat glands stop working. It may be caused by nerve damage, burns, certain medications, genetics, or dehydration. If anhidrosis affects only a small area of your body, it’s typically not harmful. If you can’t sweat from a large area of your body, however, it’s wise to seek professional counsel. Lack of sweating may create problems of temperature control and lead to steep rises in body temperature during hot weather. Occasionally, this can be life threatening.
_
Causes of anhidrosis include:
Nerve Damage:
Injuries to the nerves that help control some of the involuntary functions of the autonomic nervous system (which regulates your internal organs, sweat glands, and blood pressure, for instance) can interfere with the activity of your sweat glands. Such nerve damage may be caused by a number of medical problems including B-vitamin deficiency, diabetes, and alcoholism.
Skin Injures:
Injuries to the skin and sweat glands can also cause anhidrosis. Such injuries can occur due to major third-degree burns from fire, chemicals, electricity, medication overdose, and poisonings. Skin disorders that inflame the skin can also affect your sweat glands. These include psoriasis, exfoliative dermatitis, heat rash, scleroderma and ichthyosis.
Clogged Ducts:
Skin diseases and conditions that can block or clog sweat ducts (a problem called poral occlusion) are the most common causes of anhidrosis. This is, by the way, how antiperspirants work, albeit on a localized and temporary basis.
Certain Drugs/Medications:
In particular, antipsychotic medications used to treat serious mental disorders may interfere with normal functioning of the sweat glands. Also, medications with anticholinergic properties and calcium-channel blockers may cause anhidrosis.
An Inherited Condition:
It’s rare but some people are born without sweat glands. Males with hypohidrotic ectodermal dysplasia, for instance, suffer from this problem and are therefore at high risk of death from overheating (hyperthermia), especially in hot environments.
Dehydration:
This occurs when you don’t have enough water in your body to carry on normal functions. You can easily become dehydrated when you work or exercise in hot weather and don’t drink enough fluids to replace what you’ve lost through perspiration. People age 65 and older, infants, and children are more prone to heat stress, which can contribute to anhidrosis. Other common causes of dehydration include persistent vomiting or diarrhea or the use of medications that increase the flow of urine (diuretics). If these problems last long enough, a person can eventually lose so much fluid that he or she is no longer able to sweat. Signs and symptoms of dehydration include thirst, weakness, and confusion. Severe dehydration can be fatal, particularly in older adults and children.
_
Anhidrosis may be from abnormalities of the glands themselves, or more typically the nerve pathways which innervate the glands. When the decrease in sweating is primarily in the hands and feet (distal anhidrosis), the cause is most likely to be a peripheral neuropathy such as diabetes. Amyloid is another common cause. In more advanced cases of amyloid and diabetic neuropathies, the anhidrosis may also have a preganglionic component. When the loss of sweating is generalized, the causes may either be central (e.g. MSA or multiple system atrophy or idiopathic orthostatic hypotension) or peripheral (e.g. acute panautonomic neuropathy). When the loss of sweating is throughout the body but with relative sparing of hands and feet, a central cause is most likely, such as MSA or primary autonomic failure. A peripheral nerve abnormality may lead to abnormal sweating in the distribution of that peripheral nerve. Thus, trauma or inflammation of an isolated root, trunk, or nerve may lead to a patch of altered sweating. The nerve pathways from the hypothalamus to the periphery travel on one side of the nervous system and therefore a lesion within this pathway will lead to hemi-anhidrosis, i.e., loss of sweating on one side of the body only. The individual nerves within this pathway do not form a tight well-defined bundle and therefore the decrease in sweating is typically patchy. Local skin pathology may also lead to altered sweating through direct destruction of glands or blocking of their ducts. In these cases or in focal nerve lesions, there may be a compensatory increase in sweating from neighboring normal sweat glands.
_
Tests and diagnosis:
Your doctor is likely to suspect anhidrosis based on your signs and symptoms, your medical history, and a physical exam. But you may need certain tests to confirm the diagnosis. These include:
1. TST and QSART: Sweating is induced by release of acetyl choline (ACh) from sympathetic postganglionic fibers. The quantitative sudomotor axon reflex test (QSART) is a measure of regional autonomic function mediated by ACh-induced sweating i.e. stimulation by using iontophoresis of acetylcholine. A reduced or absent response indicates a lesion of the postganglionic sudomotor axon. For example, sweating may be reduced in the feet as a result of distal polyneuropathy (e.g., diabetes). The thermoregulatory sweat test (TST) is a qualitative measure of regional sweat production in response to an elevation of body temperature under controlled conditions. An indicator powder placed on the anterior surface of the body changes color with sweat production during temperature elevation. The pattern of color changes is a measure of regional sweat secretion. A postganglionic lesion is present if both QSART and TST show absent sweating. In a preganglionic lesion, QSART is normal but TST shows anhidrosis.
2. Skin biopsy. In some cases, your doctor might request a biopsy of the area suspected of anhidrosis. For this test, skin cells and sometimes sweat glands are removed for examination under a microscope.
3. The silastic sweat imprint test measures where you sweat.
4. Sympathetic Skin Testing: Typically, a pair of electrodes 1 cm apart is applied to the thighs, hand, or foot. A stimulus is then applied such as a loud noise, electric shock, or cough, this then typically leading to a brief change in sweating and therefore electrical conductivity. In conditions with marked loss of sweating the response may be lost, but beyond this the method is not very useful because of the extreme variability in the response, both between patients and when testing the individual on repeated occasions. It is thus not useful for quantification of degree of sweating.
_
If there is a danger of overheating, take the following measures:
•Take a cool shower or sit in a bathtub with cool water
•Drink plenty of fluids
•Stay in a cool environment
•Move slowly
•Do not perform heavy exercise
_
Treatments and drugs:
Anhidrosis that affects a small part of your body usually isn’t a problem and doesn’t need treatment. But large areas of decreased perspiration can be life-threatening. Treatments may depend on the condition that’s causing the anhidrosis.
________
________
Sweat diagnostics and sweat devices:
Sweat diagnostics is an emerging non-invasive technique used to provide insights to the health of the human body. Common sweat diagnostic tests include testing for cystic fibrosis and illicit drugs. Most testing of human sweat is in reference to the eccrine sweat gland which in contrast to the apocrine sweat gland, has a lower composition of oils. Although sweat is mostly water, there are many solutes which are found in sweat that have at least some relation to biomarkers found in blood. These include: sodium (Na+), chloride (Cl-), potassium (K+), ammonium (NH4+), alcohols, lactate, peptides & proteins. Development of devices, sensing techniques and biomarker identification in sweat continues to be an expanding field for medical diagnostics and athletics applications.
___
Sweat test and cystic fibrosis (CF):
With “Quantitative Pilocarpine Iontophoresis Sweat Test” (QPIT), a relatively small area of 30–40 cm2 usually on the volar surface of the forearm, was stimulated to secrete sweat by iontophoresing a potent sweat secretagoque (usually pilocarpine) through the skin for a few minutes, after which sweat from the stimulated area was collected hermetically for about 30 min and analyzed for Cl−. After extensive investigations of other related conditions, Cl− concentrations in the sweat greater than 60 mEq/l were deemed to be characteristic of CF. The rule holds especially well in the paediatric population where, normally, sweat contains <40 mEq/l. The rule does not hold so well among adults, especially at high sweat rates. After nearly 50 years, the sweat test remains the foremost test in the differential diagnosis of CF to date. The sweat gland taught us that the most efficient, expedient test for diagnosing CF was to measure the concentration of Cl− in a small sample of pharmacologically induced sweat.
___
Sweat, the cooling system of your body, is made almost completely of water, with tiny amounts of other chemicals, including ammonia, urea, salts, and sugar. Remarkably, these chemicals along with the small molecules and peptides they contain can reveal what is going on inside your body. For this reason, scientists are trying to harness sweat through some form of wearable technology and turn it into a new way to measure and monitor your immediate health. Sweat contains a trove of medical information and can provide it in almost real time. Since long doctors have been extracting fluids from our bodies in order to evaluate some aspect of our health. How many blood tests, urine tests, or saliva tests have you undergone in your life? Sweat is a vastly untapped bio-fluid for human performance monitoring. For some time now, researchers have been exploring ideas and technologies that might continuously monitor a given biomarker and so open a window on the status of our overall health, in the manner, say, of a diabetic who daily tests her blood sugar levels. Because of its non-invasive (and therefore painless) possibilities, researchers began to focus their efforts on using sweat as fuel. Specifically, researchers envision a wearable gadget that stimulates and collects sweat via a patch about the size of a band-aid, and then analyzes it using your smartphone. Researchers have discovered that perspiration may carry far more information and may be easier to stimulate, gather, and analyze than previously thought. Researchers began to look for a convenient way to monitor an airman’s response to disease, medication, diet, injury, stress, and other physical changes during both training and missions. In that quest, they developed patches that stimulate and measure sweat and then wirelessly relay data derived from it to a smartphone. In 2013 the U.S. Air Force accelerated the commercialization of biomonitoring devices such as sweat sensors.
_
What’s in Sweat?
Biomarkers contained in sweat can give indications about the physical state of the body. They include electrolytes, metabolites, proteins, and amino acids. Here’s a sampling:
Electrolytes:
•Sodium
•Chloride
•Potassium
•Calcium
Metabolites:
•Lactate
•Creatinine
•Glucose
•Uric acid
Small Molecules:
•Amino acids
•DHEA
•Cortisol
Proteins:
•Interleukins
•Tumor necrosis factor
•Neuropeptides
Electrolytes are by far the easiest component of sweat to measure. But metabolites—like lactate, creatinine, and glucose—shouldn’t be too much harder. The lactate level is a great indicator of a person’s ability to cope during rigorous exercise or while on life support. Lactate, or lactic acid, is a by-product of burning glucose without oxygen. Therefore, when the body is not getting enough oxygen, it generates more lactate. Higher concentrations of creatinine and urea indicate an unhealthy kidney struggling to clear waste products from the body. In people with chronic kidney disease, so much urea is excreted with sweat that the accumulation of urea makes the skin look frosted. And glucose monitoring, of course, is key to managing diabetes. As yet, researchers have not found a way to predict exact blood levels by measuring these metabolites in sweat. So using sweat to monitor glucose levels, as desirable as that would be, is still out of reach. Researchers have understood the richness of the information carried in sweat for some 50 years, but they have been unable to take advantage of it because of the difficulty of collecting, transporting, and analyzing the samples. With the many recent advances in sensing, computing, and wearable technology providing inspiration—and with more than a little perspiration in the laboratory—we are on the verge of a true revolution in wearable diagnostics.
_
Correlation between sweat glucose and blood glucose in subjects with diabetes: 2012 study:
Sweat contains glucose that can accurately reflect blood glucose. However, skin surface glucose can confound these measurements. A perfusion method was used to rapidly harvest sweat from forearm sites on human subjects. The sweat samples were analyzed for glucose by high-performance liquid chromatography methods and compared with the results obtained with a blood glucose meter. The results of 23 different studies of seven individual subjects with diabetes show a strong correlation between sweat glucose and blood glucose. Sweat glucose, when properly harvested to prevent contamination from other sources on the skin’s surface, can accurately reflect blood glucose levels. However, it is not clear whether the glucose-detecting sensors would work continuously for long periods of time, or whether the patch would work well if the wearer sweated a lot due to exercise/hot weather.
_
Chemical analysis of human sweat may become an effective method of monitoring drug use over extended periods, according to NIDA researchers. Sweat, collected over several days or weeks in patches worn on the skin, is a sensitive indicator of heroin and cocaine use, according to Division of Intramural Research investigators at NIDA’s Addiction Research Center in Baltimore. The current standard test for evidence of drug use is urinalysis. But most drugs of abuse are cleared from urine within 2 to 3 days, meaning that urine screening must be performed two to three times a week to effectively monitor drug use on a continuing basis. Previous research has determined that residues of a number of drugs can be detected in human sweat, including alcohol, amphetamine, cocaine, heroin, morphine, methadone, methamphetamine, and phencyclidine (PCP).
_
Portable sweat devices include patches and tattoos.
Patches:
Patches have been demonstrated to be a promising detection platform for sweat diagnostics. Simple, long-term collection devices which check for drugs of abuse or alcohol are already on the market and operate on the following principle: a user applies the patch which then collects sweat over a period of hours or days, then the patch is analysed which are accurate but the suffer the drawback in lack of continuous measurements and high costs. For example, drugs of abuse and alcohol sweat testing. More recently, several startup companies such as have begun developing products targeted towards the consumer, healthcare and athletics market for sweat diagnostics. Ultimately, it is the hope that these devices will have the ability to detect changes in human physiology within minutes without the need for repeated sample collection and analysis.
Temporary tattoos:
Temporary tattoo-based sweat diagnostic tools have been demonstrated by Dr. Joseph Wang’s group from University of California, San Diego. Their work includes sweat diagnostics for sodium, lactate, ammonium, pH and biofuel opportunities.
_
Sweat monitoring to prevent heat illness in athletes:
Formed in late 2013, Eccrine Systems is developing non-invasive, disposable, electronic patches that measure and transmit real-time data about human sweat. Sweat derived from eccrine glands in human skin contains valuable information about physiological performance and dysfunction. Importantly, sweat data can be captured discreetly and non-invasively. Captured data can be transmitted securely in real-time to remote systems where the relationship among measured sweat molecules can be automatically integrated with other biometric data and interpreted as to its physiological relevance. Results can then be translated into alerts, actions, and reports. The short term goal is to dramatically reduce the occurrence of heat-related issues for athletes as they affect both safety and performance. Long-term goal is to create a ‘human dashboard’ that will allow athletes at all levels to see what’s going on inside. Our bodies broadcast all sorts of warnings and indicators that signal declined performance, muscle cramps, and a laundry list of other issues that result from dehydration. Eccrine’s ability to translate sweat data with accuracy and chronological assurance will enable a true paradigm shift in the monitoring of human physiological performance and dysfunction across a wide spectrum of high value applications for medicine, industry, and sport.
_
To maximize training and endurance, athletes need wearables that do more than count steps and track workouts. Answering the call, Kenzen has released the industry’s most complete smart patch wearable to track everything from basic fitness to real time monitoring of an athlete’s hydration, lactic acid and glucose levels. Called the ECHO H2, the wearable is a combination reusable sensor and disposable smart patch that utilizes one bead of sweat for real-time analysis. Alerts to adjust workouts are sent to a user’s smart device. If you are in the middle of your run and your lactic acid build-up is nearing critical levels, the sensor will detect it, send a signal to the app, and your phone or watch will alert you. It will give you instructions to slow your pace and let your muscles recover, so that you can continue your workout. ECHO and the H2 get you farther because the lactic acid doesn’t get a chance to build up to painful levels that would force you to quit.
_
Tattoo-Based Wearable Electrochemical Devices: Review 2015:
This article provides an overview of the recent advances in the field of skin-worn tattoo-based wearable electrochemical devices, including electrolyte and metabolite sensors, biofuel cells and batteries. Temporary tattoos are attractive platforms for fabricating skin-worn devices. Body-compliant wearable electrochemical devices on temporary tattoos couple highly favorable substrate-skin elasticity with an attractive electrochemical performance. For example, tattoo-based “skin-like” sensors can be used for real-time non-invasive analysis of key electrolytes and metabolites, leading to remarkable sensing capabilities. Continued progress has been made also towards developing skin-worn flexible energy harvesting and storage devices to power wearable health monitors and other devices. Key requirements and challenges that confront researchers in this exciting area of skin-worn electrochemical devices are discussed.
_
A Temporary Tattoo to track your workout and charge your Phone:
Scientists have invented a biosensor that can monitor exercise and store electricity. Researchers have developed a battery in the form of a temporary tattoo that can monitor your workout and even make electricity from your sweat. Eventually, biobatteries like this may be able to charge your watch, heart monitor, or smartphone. Wenzhao Jia from the University of California San Diego presented the research at the 248th National Meeting & Exposition of the American Chemical Society in San Francisco. The device has a sensor printed onto it that detects lactate, a chemical present in sweat that rises during strenuous training regimens. In the future, biotattoos may be a convenient tool for doctors who need to supervise athletes and average joes who want to monitor their own fitness.
_
Non-invasive and accurate access of biomarkers remains a holy grail of the biomedical community. Human eccrine sweat is a surprisingly biomarker-rich fluid which is gaining increasing attention. This is especially true in applications of continuous bio-monitoring where other biofluids prove more challenging, if not impossible. The concept of using sweat for non-invasive access to biomarkers and solutes in blood is far from new, with large volumes of clinical work showing promising results as far back as the 1940s and 1950s. However, outside of cystic fibrosis (CF) diagnostics for increased sweat chloride levels and testing for the metabolites of illicit drugs, sweat remains relegated mainly to the lab and clinic. Both the significant opportunities and frustrations with sweat as a diagnostic tool are succinctly summarized by Bravo and Castro: “The main limitations of sweat as clinical sample are the difficulty to produce enough sweat for analysis, sample evaporation, lack of appropriate sampling devices, need for a trained staff… normalization of the sampled volume.” In part, many of these issues are now being resolved by bringing low-cost wearable sensors into nearly immediate contact with sweat as it emerges onto skin. This not only improves convenience and eliminates evaporative issues causing misleading increases in biomarker concentrations but also it is powerful as many biomarkers in collected biofluids degrade in as little as 10–20 min. Wearables can also easily measure the change in sweat generation rate by skin impedance. However, sweat generation rate does not predict actual biomarker sampling intervals without a detailed microfluidic and transport model between the sweat glands and sensors.
__
Sweat sensor:
_
More recently, numerous studies have identified the plausibility of sweat as an alternative to blood analysis. In the recent years sweat testing developed a noninvasive monitoring of drug exposure in various contexts as criminal justice, employment and outpatient clinical settings for various xenobiotics especially cocaine metabolites, opiates, cannabis and amphetamines. The technique can be applied to situations such as workplace drug testing, drivers, doping or prenatal diagnosis. The potential substitution for sweat versus blood analysis has many potential benefits. For example, sweat can be: extracted in a non-invasive manner via iontophoresis of cholinergic agonist, extracted with little-to-no pain; and monitored continuously. There are downfalls to the technology, however. For example, demonstration of successful and reliable sweat extraction and analysis on a cohesive device has yet to be demonstrated. Furthermore, although some biomarker partitioning mechanisms are well-understood and well-studied, partitioning of other useful biomarkers (cytokines, peptides, etc.) are less understood.
_
Wearable sweat sensor monitors your perspiration:
Until now, sweat sensors have typically involved patches that are removed for subsequent chemical analysis by separate, non-wearable machines. The current device is wearable, it provides continuous data streams, and it measures multiple biomarkers simultaneously.
_
Researchers in the US have developed what they claim is the first standalone electronic sensor that provides continuous, non-invasive monitoring of multiple biochemicals contained in perspiration. Human sweat contains physiologically rich information, thus making it an attractive body fluid for non-invasive wearable sensors. Researchers have developed a fully integrated system that simultaneously and selectively measures multiple sweat analytes, and wirelessly transmits the processed data to a smartphone. A flexible, wearable sensor that can measure perspiration is promising to reveal the secrets in your sweat. The device, developed by a team at UC Berkeley, can measure metabolites and electrolytes, calibrate data based on temperature and then sync the results to a smartphone in real time. Researchers say that it is the “first fully integrated electronic system that can provide continuous, non-invasive monitoring of multiple biochemicals in sweat”. Writing in Nature, the team say the sensor could be used to warn users of problems including fatigue, dehydration and high body temperature. According to the researchers, the metabolites and electrolytes contained in human sweat say a lot about the health of a person, and could help replace invasive means of examining one’s wellbeing. The prototype includes five sensors on an array connected to a flexible circuit board. The array of sensors measures metabolites (glucose and lactate) and electrolytes (sodium and potassium), and also monitors skin temperature, while the circuit board analyses the data collected and can transmit it to other devices. The potential complexity of the array means it could also one day be used as a serious clinical tool to help physicians and scientists keep tabs on a range of biochemical secretions from patients, athletes, and perhaps even astronauts. The fact that the device can be worn constantly also means it’s capable of collecting a much broader and less interrupted stream of health data, compared to the isolated measurements doctors might otherwise only be able to record during infrequent patient visits to their GP.
_
Sweat meter measure swear rate:
The sweat meter was originally designed to diagnose hyperhidrosis, a nasty disease that causes sufferers to sweat excessively. Sweating has two causes. The best known is thermal sweat. When it’s hot, the body reacts by secreting sweat on the surface of the skin. The perspiration needs energy to evaporate. This cools the skin down. The second type of sweat is emotionally controlled and occurs primarily in the palm. The palm has more than 600 sweat glands per square centimeter. This is the highest density of sweat glands in the body. Although emotionally controlled sweat can be unnoticeable, it can have a great impact on measurements, even when you’re only calculating a few difficult math problems in your head. The sweat meter sends a small electrical current through the outer part of the skin, into the sweat glands and out onto the surface again. This layer of skin, which consists of dead horn cells which poor conductors of electricity. On the other hand, sweat is a good conductor of electricity. Sweat is made up of saltwater. As is known, saltwater conducts electricity. The conductivity of the skin increases, therefore, when the sweat pores are filled with sweat. Over the past year, several medical research institutes have expressed an interest in the sweat meter.
1. Athletes and stress. The sweat meter can be used to see how upset or excited you are.
2. Chronic Fatigue Syndrome. Vegard Bruun Wyller, chief physician at the Paediatric Cardiology Department at Oslo University Hospital and associate professor at the University of Oslo tests the sweat meter on children with chronic fatigue syndrome (ME). Even when ME patients rest quietly and should be relaxed, their bodies behave as though they are persistently stressed. Many complain of sweating.
3. Detect hypoglycemia:
Sweat meter could alert diabetes patients about low blood sugar:
It is known that diabetic patients change their sweat pattern when their blood sugar levels are too low. Some diabetic patients receive no warning before they pass out from low blood sugar. A modern sweat meter could alert patients in time. A sweat meter developed at the University of Oslo and the National Hospital can send a discreet alert – via a mobile phone – before a patient suffers an attack due to low blood sugar. The advantage of the sweat meter is that the patient doesn’t have to prick themselves. All you need to do is paste an electrode on your skin. The device is able to measure sweat activity continuously, providing an indication of whether the patient is about to experience low blood sugar. It can communicate directly or via a smartphone. The warning system will then not be very bothersome for the patient.
_____
_____
Sweat Research:
Researchers developed artificial skin capable of sweating:
Japanese scientists were able to develop and grow dermal tissue that behaves just like normal skin; the team performed the development of the organ and managed to test it successfully on mice. This new artificial skin is expected to bring a new degree of relief to scarring, skin diseases and burn victims. But one of the unforeseen advantages of the skin developed by the RIKEN Center for Developmental Biology is that it is able to grow hair, as it was published in the journal Science Advances. The tissue was developed by using stem cells, which are able to be worked upon until they can replicate any cell located within our organism. The cells were originally taken from the cells of lab mice and they were reprogrammed to become embryonic stem cells. Besides being able to have hair follicles, secrete oil and produce sweat, the skin developed by RIKEN has the three characteristic layers of the human skin. The experiment allows for further development in the areas of regenerative therapy and it displays possibilities of creating fully functional organs for clinical treatment. But there is still some resistance on whether to test the artificial skin on humans. The theory is that human skin substitutes should be created with human cells. The scientists need to figure out how to develop and obtain the same results by using human stem cells instead of mice’s. The team predicts that they still have a long way to go in creating artificial human skin, but they are aiming toward generating organs in a laboratory environment in order to assist patients that may need a transplant, so they do not have to rely on a donor. But yet, recreating skin is a big step in this area of research as it is the largest organ in the body, able to regulate temperature and protect inner and outer organs from the environment and possible infection. Regular grafted skin cannot connect to muscles, it is not able to sweat, and subsequently, it cannot regulate temperature effectively. As of now, the most widely-discussed application of the artificial skin developed by RIKEN is to be used as a test surface for cosmetics. This will reduce the test procedures that are still made on animals by many cosmetics companies. But one of the most interesting uses of the RIKEN artificial skin is to treat baldness, as 9 out of 10 males and 5 out of 10 women suffer from a certain degree of baldness in some point of their lives. It is a matter of time until cosmetic applications of RIKEN skin become available to the public to treat ailments such as baldness and hypohidrosis.
_____
_____
My theory on sweating:
Evolutionary biologically, first parasympathetic system evolved followed by evolution of sympathetic system. Parasympathetic system maintains homeostasis (rest and digestion) and sympathetic system faces challenges (fight or flight). You can face challenges successfully only if your systems are functioning optimally. So for using sympathetic nervous system facing challenge, parasympathetic system ought to be optimally tunes. It is wrong to say that sympathetic system and parasympathetic system oppose each other. They work balancing each other. Goal of autonomous nervous system is survival independent of consciousness. That is why it regulates blood pressure, heart rate, sleep, bladder & bowel function, focussing of eyes, sexual functions and thermoregulation. Efficient cooling mechanism by sweating allowed human ancestors to run longer distances at faster speeds than other animals and development of bigger hotter brain. In other words, sweating allowed development of stronger and intelligent humans. That is why sympathetic and parasympathetic nervous systems unite by having cholinergic sympathetic nerve endings.
_
The table below shows that alfa-1 adrenoceptor cause vasoconstriction and beta-2 adrenoceptor cause vasodilation:
Epinephrine (adrenaline) reacts with both α- and β-adrenoreceptors, causing vasoconstriction and vasodilation, respectively. Although α receptors are less sensitive to epinephrine, when activated, they override the vasodilation mediated by β-adrenoreceptors because there are more peripheral α1 receptors than β 2 adrenoreceptors. The result is that high levels of circulating epinephrine cause vasoconstriction. At lower levels of circulating epinephrine, β 2 adrenoreceptor stimulation dominates, producing vasodilation followed by decrease of peripheral vascular resistance.
_
Although sympathetic nervous system generally cause vasoconstriction and raise blood pressure, under certain circumstances, it causes vasodilation e.g. thermal sweating (skin vasodilation) and exercise (muscle vasodilation). During exercise/hot environment, beta 2 stimulation will cause vasodilatation of skin vessels along with sweating for heat loss and vasodilatation of muscles to give oxygen and nutrients. During shock, alfa 1 stimulation will try to increase blood pressure, so we have pallor due to skin vasoconstriction with sweating. During winter, reduced sweating with alfa 1 stimulation reduces blood supply to skin to conserve heat. So we feel cold, pale with dry skin. In other words, there are differential sympathetic pathways mediating sweating vis-à-vis vasoconstriction or vasodilatation.
_
| Skin vasodilation | Skin vasoconstriction | Skin blood vessels unaffected | |
| Sweating | Hot sweat (heat, exercise) | Cold sweat (anxiety, pain, fear, shock) | Apocrine sweat (sexual arousal) |
| No sweating | Blushes (romance) | Cold weather | Routine life |
Note: All different types of permutations and combination are possible. For example, if you suffer heart attack in cold weather, you will sweat; if you are anxious in romantic situation, you will blush with sweating. During menopause, woman gets flushes (vasodilation) with sweating which is cold sweat although cold sweat is generally accompanied by vasoconstriction. All these suggest differential neuronal pathways for handling different situations.
__
There are two types of sweating:
1. Classical sweating
2. Non-classical sweating
_
Classical sweating is meant for promoting heat loss to maintain core body temperature as all enzymatical reactions in body are temperature dependent. Classical sweating is always accompanied by vasodilation of skin blood vessels as it brings warm blood from core of body to surface carrying body heat which is dissipated by sweating.
Three causes of classical sweating:
1. Heat (hot weather) increases core body temperature by conduction, convection and radiation
2. Exercise increases core body temperature by heat generated in muscles
3. Fever transiently increases core body temperature to respond to infection/injury
In other words, classical sweating ensures survival by promoting heat loss taking help of vasodilatation of skin blood vessels. Nerve fibers for classical sweating arise from hypothalamus and travel to sweat glands and skin blood vessels by sympathetic nerves. Acetylcholine is released at muscarinic receptors on sweat glands and nor-epinephrine is released on beta-2 adrenoceptors on vascular smooth muscles for vasodilatation of skin blood vessels.
_
Non-classical sweating is not for heat loss and hence not accompanied by skin vasodilatation but in fact may be accompanied by vasoconstriction of skin blood vessels.
Causes of non-classical sweating
1. Reduced tissue perfusion e.g. shock, heart attack,
2. Facing severe challenge, stress response e.g. fight/flight
3. Attract mate/repel enemy
4. Emotional reaction
Here sweating functions to improve hand grip, cool down body in preparation to fight/flight, release odour to attract mate/repel enemy etc. As you can see that improved hand grip and cooling body help fight/flight reaction. Attracting mate for reproduction help propagate species. In other words, non-classical sweating also helps survival just like classical sweating. Only the neural connections differ. Most non-classical sweating have skin vasoconstriction accompanied by sweating. The nerve fibers arise from pre-frontal cortex and limbic system, travel down via sympathetic nervous system (bypassing hypothalamic thermoregulatory center) to release acetyl choline on muscarinic receptors of sweat glands but release nor-epinephrine on alfa-1 receptors of smooth muscles of skin blood vessels causing vasoconstriction. Dissipating excess heat is not the intention but lubricating skin, releasing pheromones, cooling the body and raising blood pressure is intention. If you see a patient in shock or heart attack, he will be sweating with pallor, skin vasoconstriction will pull blood in central circulation to improve blood pressure and perfuse vital organs during crisis; sweating will cool down body to prepare for adversity, just as radiator in car cool down car engine. Apocrine sweat glands are innervated by sympathetic post-ganglionic adrenergic nerves and apocrine sweat contain pheromones-like substances to attract mate for reproduction and therefore apocrine sweat neural pathways have no connection to skin blood vessels. When you’re sexually aroused, you sweat from both apocrine and eccrine sweat glands so that increased eccrine sweat output in the axillae will allow pheromones from apocrine gland secretion to aerosolize and function as pheromone signals to attract mates. Remember, reproduction ensures survival of genes and species.
_
Sweat glands and most vascular smooth muscles have only sympathetic innervation. The observation that patients with anhidrotic ectodermal dysplasia, who lack sweat glands, also fail to actively dilate skin vessels during heat stress and the close relationship between sweat production and vasodilator skin sympathetic nerve activity (SSNA) suggests that the sudomotor nerves and vasodilator nerves could well be same; but profuse sweating with vasoconstriction in shock or heart attack proves otherwise. Local application of atropine to skin abolished sweating completely, but it did not abolish active vasodilation during heat stress, ruling out role of acetylcholine in vasodilation. An intradermal dose of botulinum toxin, taken up by cholinergic nerve terminals and interrupting the release of all neurotransmitters from those terminals, completely abolished both cutaneous active vasodilation and sweating in the treated area of skin could well be due to some blockage of beta-2 adrenergic nerve terminals on skin vascular smooth muscle. Beta-adrenergic blockade with propranolol decreased blushing (skin vasodilation) due to blocking of beta-2 adrenoceptors. Also, the side effect of propranolol is peripheral vasoconstriction by blocking beta2 adrenoceptors which cause vasodilation. All these prove differential sympathetic neuronal pathways innervating sweat glands and skin blood vessels differentially rather than single sudomotor vasodilator pathway.
_
In a nutshell, sweating is a survival mechanism either by losing excess heat or even without it. Either way it helps survival and differential sympathetic neuronal pathways exist innervating sweat glands with/without either vasodilation or vasoconstriction to handle different situations to ensure survival in different adverse conditions which could be thermal or non-thermal.
_______
_______
The moral of the story:
1. Evolutionary biologically, loss of fur and walking on two legs caused thermal eccrine sweat gland system to evolve in human ancestors. Efficient cooling mechanism by sweating allowed human ancestors to run longer distances at faster speeds than other animals and development of bigger hotter brain. In other words, sweating allowed development of stronger and intelligent humans. That is why sympathetic and parasympathetic nervous systems unite by having cholinergic sympathetic nerve endings.
_
2. Sweating is synonymous with perspiration. Obligatory evaporative water loss (insensible perspiration) is water loss from skin (trans-epithelial) and respiratory tract (water vapor in exhaled air), and amounts to about 600 to 800 ml of water evaporated. It is not under regulatory control and accounts for daily heat loss from body independent of heat regulation. Diaphoresis is excessive sweating in a medical condition.
_
3. Sweating is the production of watery fluid by the microscopic sweat glands in the skin. Between 2 and 4 million sweat glands are distributed over the entire human skin (except for the lips, nipples and external genital organs) but only about 5% are active at the same time, indicating the enormous potential for sweat production. Normal sweating can be as much as one liter of fluid per day in an adult. Continuous basal sweating is responsible to keep the skin smooth, moist and glistening. Basal sweat secreted at rest in cool environment is almost water with little electrolytes. Thermoregulatory sweat contain water with sodium & chloride about half of plasma (4 gms/liter) but reduces to1 gm/liter in an acclimated person. From 1 liter sweat production per hour in a non-acclimated individual, an acclimated individual can produce 2 liter of sweat per hour but with lesser sodium in that sweat. Maximum sweat rates of an adult can be up to 2–4 liters per hour or 10–14 liters per day. As normal diet provides 8–14 gms of salt per day, it is often sufficient to compensate for sweat salt loss. So when you experience excessive sweating due to any cause, you must drink sufficient water to prevent dehydration. The word ‘Sweating’ means eccrine gland sweating unless specified otherwise and eccrine sweat glands become active soon after birth. The volume of fluid from apocrine sweating is very low.
_
4. Eccrine sweat glands are affiliated to sympathetic nervous system which is designed to cope up with stress, emergency, embarrassment, exercise or adverse environment thermal or non-thermal. Sympathetic postganglionic neurons usually secrete norepinephrine and are named sympathetic adrenergic neurons. However, when sympathetic postganglionic neurons innervate sweat glands they secrete acetylcholine and hence are termed sympathetic “cholinergic” neurons. In other words, sweat glands are innervated by sympathetic cholinergic nerves. Many activities such as spicy foods, hot weather, exercise, high emotional excitement, stress or nervousness may cause attacks of excessive sweating through sympathetic nerve over activity.
_
5. Hot sweat is sweating to dissipate heat (thermoregulatory sweating due to hot weather, exercise and fever) accompanied by dilation of skin blood vessels and occurs over the general body surface. Cold sweat is neither due to cold nor to dissipate heat. Cold sweat is body’s response to stress called the fight or flight response. Cold sweat could be due to emotions (anxiety, fear), stress, pain or medical conditions (diaphoresis). Cold sweating occurs mainly in the face, the axillae, the palms, and the soles of the feet; accompanied by vasoconstriction of skin blood vessels, hence the term cold sweat. Sweating of palms and soles is mainly induced by emotional stimuli independent of ambient temperature and decreases during sleep and relaxation. Both hot and cold sweat are secreted by eccrine sweat glands under stimulation of sympathetic cholinergic nerves, and although hot and cold sweat are distinct, they do influence each another.
_
6. Human body continuously generates heat at a rate varying from about 100 Watts (e.g. for a sedentary person) to as high as 2000 Watts (e.g. a person doing strenuous exercise) by converting 80 % of food energy into heat. To maintain core body temperature within a narrow range between 98°F and 100°F temperature, continuous heat generation is essential because body is constantly losing heat by conduction, convection, radiation, exhaled breath, insensible perspiration and basal sweat evaporation as ambient temperature is usually lower than core body temperature. However, when ambient temperature is higher than core body temperature, body gains heat by conduction, convection and radiation; and sweat evaporation is the only mode of heat loss to maintain core body temperature as heat generation from metabolic processes cannot be halted. Evaporation of sweat from the skin surface has a cooling effect due to the latent heat of evaporation of water. The evaporation of sweat water from the skin surface uses body’s heat consequently lowering skin and body core temperatures. The regulation of body core temperature is crucial for survival; constant body core temperatures above 40°C result in protein denaturation and cell death. [In fever, core body temperatures does rise above 40°C but only transiently and it is brought down by sweating] Sweating is accompanied by vasodilation of skin blood vessels that brings core body heat to skin surface to be dissipated by sweat evaporation. About 604 Kcal of heat energy is lost by evaporation of 1 liter of sweat in dry environment & with maximum efficiency. In other words, evaporation of 1gm/minute of sweat is equivalent to 42Watts. Remember all of the sweat does not evaporate, but a part of it runs off your skin. The speed of sweat evaporation is directly proportional to speed of air over skin and inversely proportional to relative humidity of air over skin. Evaporative heat loss by sweating would occur even if ambient temperature is much lower than core body temperature albeit with lesser speed of evaporation as lower ambient temperature will increase relative humidity of air; and with half sweat rate than on a hot, humid day. Of course while exercising in air-conditioned room, speed of sweat evaporation will be faster as air-conditioner reduces humidity. Vasodilation of skin blood vessels per se can promote heat loss by bringing core body heat to surface to be dissipated by conduction, convection and radiation provided ambient temperature is lower than core body temperature. However for efficient and speedy cooling, sweating and skin vasodilation go hand in hand when body wants to lose heat irrespective of ambient temperature.
_
7. Fan cools you down by two mechanisms: first, increased forced convection of air which aids heat transfer and second, increased sweat evaporation. Thus if you are sweating, you cool at a higher rate under a fan than without fan. Objects not sweating will cool too, only at a lower rate. Of course, if ambient temperature is more than body temperature, convective heat transfer will be reversed and the only way you cool is by sweating and inanimate objects would become as hot as ambient temperature. Under such circumstance, use fan when windows are open otherwise fan will circulate hot air around you.
_
8. Women sweat only 25 % of men and are at a disadvantage when it comes to cooling off during heavy bouts of exercise or during hot conditions.
_
9. The more physically fit you are, the more efficiently your body sweats.
_
10. Sweating is a way to cool your body so you don’t overheat during exercise but a good workout and a good sweat do not go hand in hand.
_
11. In hot weather, loose fitting, light colored, single layer and sleeveless clothing made up of fabric that is breathable and also having wicking property will assist in transferring heat and evaporate sweat out of body into atmosphere.
_
12. Makeup impedes the egress of the sweat, causing blockages and breakouts. Take off makeup before exercise to prevent clogging your skin pores with a mix of sweat, dirt, oils and dead skin cells.
_
13. Sudden and severe sweating may indicate a serious underlying health condition like hyperthyroidism, panic attack, heart attack or hypoglycemia.
_
14. Non-thermoregulatory benefits of sweat includes skin disinfection, wound healing, provide fine tactile skills & pliability of the palms & soles, reduce risk of kidney stones, excretion of urea, sexual attraction/repulsion due to pheromone-like substances in apocrine sweat, reduce acne and early treatment of heart attack. However, excessive sweating can negate sweating benefits e.g. sweating of hands can improve grip to hold objects but excessive hand sweating may have opposite effect. Sweating can open up skin pores but excessive sweating can clog skin pores by sweat water, debris, dead skin cells and bacteria. Sweating reduces acne but excessive sweating makes skin prone to infections. Apocrine axillary sweat contains pheromone-like substances to attract mates but excessive apocrine sweat leads to foul body odour repelling mates.
_
15. One should not mix up exercise benefits with sweat benefits. For example, weight loss and happiness & pain relief due to release of endorphins are exercise benefits and not sweat benefits. One can exercise in air-conditioned room with little sweating yet avail all benefits of exercise. Exercise in hot weather may precipitate heat illness despite profuse sweating negating all exercise benefits.
_
16. Body burns only 0.5 Kcal for evaporation of 1 liter sweat and therefore sweating per se does not cause weight loss but it is the exercise that caused sweating leads to weight loss. Whatever weight loss occurred due to sweating is mere water loss which will be regained when person drinks water. In fact dangers of sweating to lose weight are grave including dehydration, heat illness, kidney damage and cardiovascular emergencies. However, people who have hyperhidrosis may lose weight unless they eat extra or reduce physical activity. This is because some of the excessive non-thermal sweat may evaporate leading to unintended heat loss from body resulting in increased caloric expenditure of body.
_
17. There is some evidence to show that sweating in ‘sauna’ on regular basis would remove toxins, improve cardiovascular health, reduce risk of death and leads to heat acclimatization. The danger of ‘sauna’ includes overheating and dehydration.
_
18. Hyperhidrosis (abnormally excessive sweating) is when you sweat more than you might expect based on the surrounding temperature or your activity level or stress. About 3 percent of the world’s population has hyperhidrosis, which causes someone to sweat a lot — four to five times as much as the average person. More than half of these people are never diagnosed or treated for their symptoms due to lack of awareness about the condition and its treatment. On average, a person with hyperhidrosis seeks medical help after living with the condition for 9 years. Hyperhidrosis means eccrine sweat hyperhidrosis unless specified otherwise.
_
19. Primary focal hyperhidrosis, the most common type affecting the axillae, hands, feet, and face (areas principally involved in emotional sweating) is bilaterally symmetrical, familial, begins in youth and significantly affect quality of life. Although emotional stimuli are involved in primary focal hyperhidrosis, it is a physiologic disorder and not a psychological disorder, caused by sympathetic overactivity in the upper thoracic sympathetic ganglia. Excessive sweating during sleep is not common for people with primary focal hyperhidrosis. Axillary hyperhidrosis has been defined as greater than 50 mg per minute of sweat. Palmar hyperhidrosis has been defined as greater than 20 mg per minute of sweat. Asymmetric hyperhidrosis suggests a neurologic cause. Although diffuse generalized sweating is usually normal, consider cancer, infection, drug-induced, neurological conditions, substance abuse and endocrine disorders.
__
20. Excessive sweating has aesthetic, relational, psychological, medical and even professional consequences.
_
21. There is a vicious cycle of sweating and anxiety. Excessive sweating leads to anxiety on the presumption that they will be unfavourably evaluated because of it. Anxiety will provoke further sweating due to activation of sympathetic nervous system.
_
22. Best way to prevent prickly heat (heat rash) is to keep body cool to prevent excessive sweating and allow evaporation of sweat by air circulation around skin.
_
23. Excessive scalp sweating coupled with poor hair hygiene can cause hair loss.
_
24. Topical treatments with clinical strength antiperspirants containing aluminium chloride 15 to 25 % should always be first-line therapy for all types of hyperhidrosis except facial hyperhidrosis. For those for whom such treatment fails, iontophoresis is typically recommended for those who have palmar or plantar hyperhidrosis, whereas botulinum toxin is often considered as first- or second-line therapy for severe axillary hyperhidrosis. Oral medications are best suited for patients with certain types of excessive sweating such as excessive facial sweating, generalized hyperhidrosis, and those who have not had success using other first-line therapies. Excessive armpit sweating that appears by itself (without hand and foot sweating) can be treated after all conservative methods have failed with either microwave thermolysis or laser ablation or suction curettage of sweat glands. When all conservative or surgical treatment have failed or unfeasible or contraindicated; the last resort for severe palmar, facial and axillary especially if combined with palmar hyperhidrosis is ETS (endoscopic thoracic sympathectomy). The last resort for severe plantar hyperhidrosis is ELS (endoscopic lumbar sympathectomy).
_
25. Anhidrosis is absence of sweating. It may be caused by nerve damage, burns, skin disease, certain medications, genetics, or dehydration. If you can’t sweat from a large area of your body, you may develop heat stroke when exposed to hot weather or heavy exercise. Excessive sweating in a normal person during exercise/hot weather may lead to dehydration and consequently anhidrosis. Extensive heat rash can also lead to anhidrosis. In other words, anhidrosis can cause heat illness and heat illness by itself can cause anhidrosis.
_
26. Apocrine sweat glands are located in limited areas—the axilla and urogenital regions, become active at puberty and respond to emotional stimuli such as anxiety, pain or sexual arousal. Apocrine sweat glands are innervated by sympathetic post-ganglionic adrenergic nerves and apocrine sweat give each human its characteristic odour due to metabolism of its odorant substances by skin bacteria. The sweat of identical twins smells the same even when they don’t eat the same foods. Apocrine sweat contains pheromones-like substances for non-verbal communication pertaining to sexual attraction/repulsion with intention to procreate better offspring and also carries emotional messages. Don’t mix up body odour and pheromones although apocrine axillary sweat is responsible for both. Pheromones are so subtle that we are not consciously aware of smelling them while body odour (good or foul) is consciously perceived. Apocrine sweat does not take part in thermoregulation. Remember, when you’re sexually aroused, you sweat from both the odor sweat glands (apocrine) and the water sweat glands (eccrine). Increased eccrine sweat output in the axillae produced by sexual arousal will allow pheromones secreted from apocrine glands to aerosolize and function as pheromone signals.
_
27. Apocrine hyperhidrosis cause foul body odour. The role of eccrine hyperhidrosis in causing foul body odour is unclear. It may promote the spread of apocrine sweat and cause further bacterial overgrowth and decomposition, or it may improve foul body odour by flushing away the more smelly apocrine sweat. You may get foul body odour without hyperhidrosis when odorants from blood are released in sweat; for example, food (onions, garlic), drinks (alcohol, caffeine), smoking and diseases (liver failure, kidney failure, diabetics); although some of these conditions can produce eccrine hyperhidrosis.
_
28. Eccrine sweat is a bio-fluid containing plenty of biomarkers which can be measured in almost real time, non-invasively and accurately, for human health and physiological performance monitoring, as an alternative to blood analysis, in patients, athletes, pilots and perhaps even astronauts.
_
29. Researchers have not found a way to predict exact blood glucose by measuring glucose in sweat. Only when sweat is properly harvested to prevent contamination from other sources on the skin’s surface, it accurately reflects blood glucose levels. It is not clear whether the glucose-detecting sensors would work continuously for long periods of time, or whether the sensor would work well if the wearer sweated a lot due to exercise/hot weather. So using sweat to monitor glucose levels in diabetics is still out of reach. However sweat meter can alert diabetic patient in time of impending hypoglycemia by detecting increased sweating even before it is noticeable.
_
30. Wearable sweat sensors can prevent heat illness by detecting dehydration earlier in hot weather/exercise; prevent muscle cramps in athletes by measuring lactates, monitor kidney functions by measuring urea level and detect legal/ illegal drugs among athletes (doping), drug addicts and drivers.
_
31. Sweating is a survival mechanism either by promoting heat loss or even without it. That is why differential sympathetic neuronal pathways exists innervating sweat glands with/without either vasodilation or vasoconstriction to handle different situations to ensure survival in different adverse conditions which could be thermal or non-thermal.
_______
Dr. Rajiv Desai. MD.
April 14, 2016
_______
Postscript:
Traditionally doctors have underestimated and/or misunderstood excessive sweating. This article is written to create awareness about excessive sweating among lay people as well doctors.
______


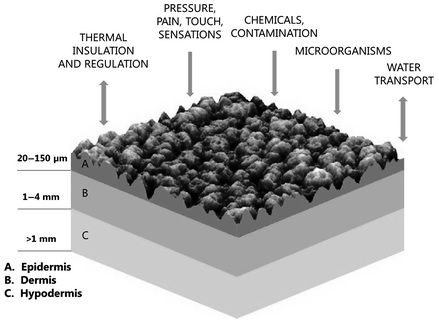
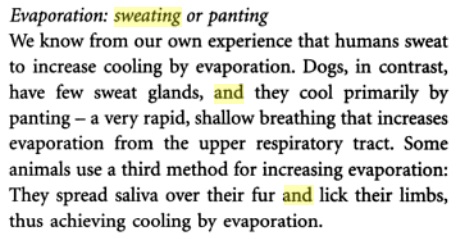
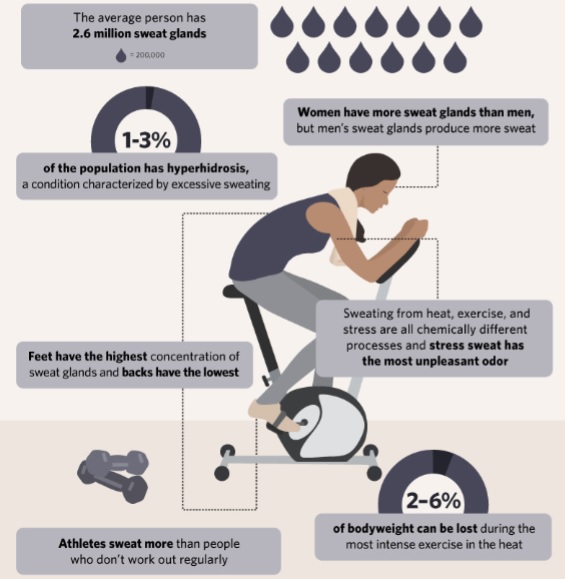


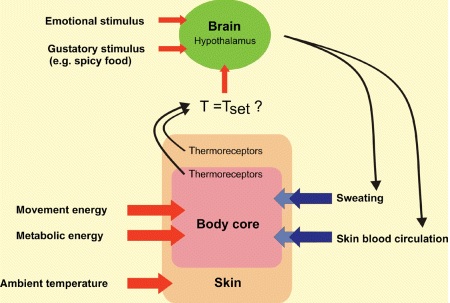
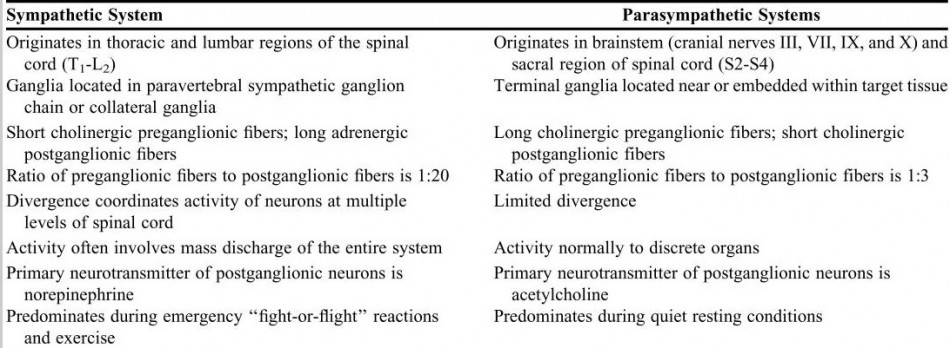
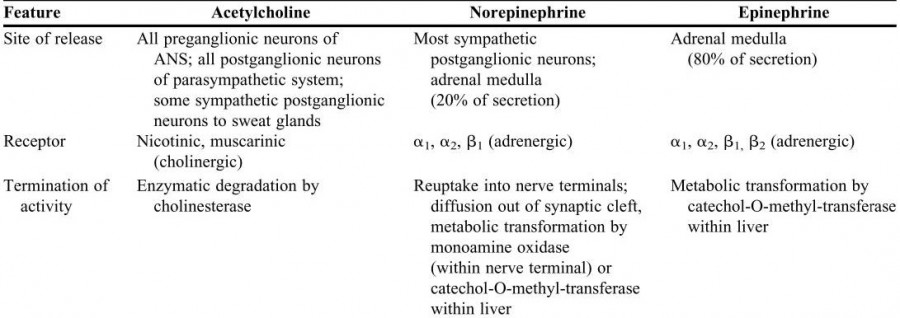
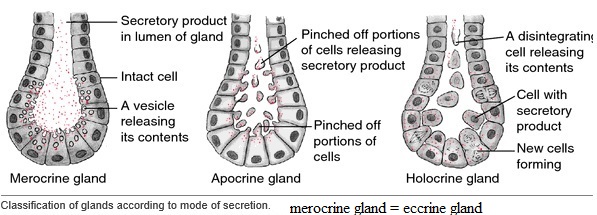
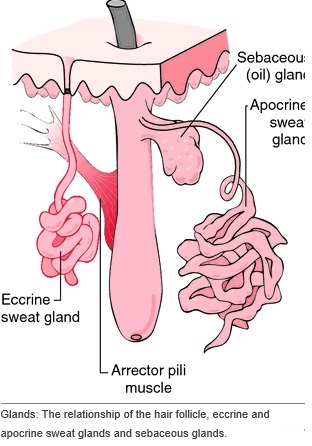
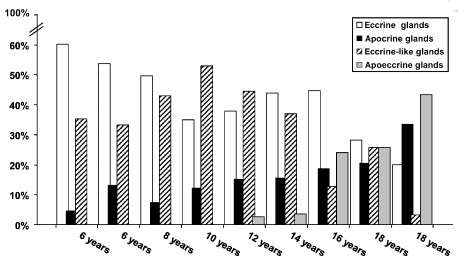
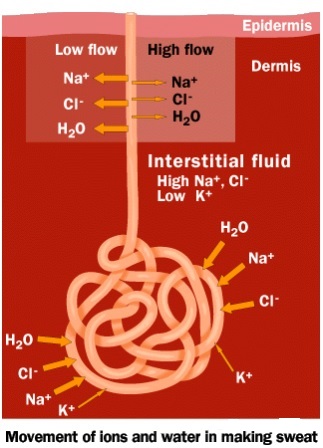
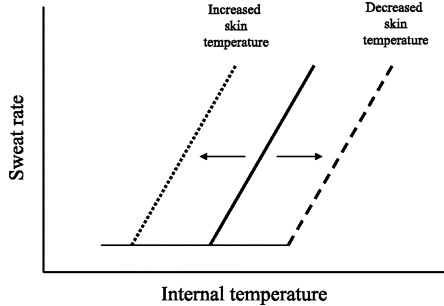
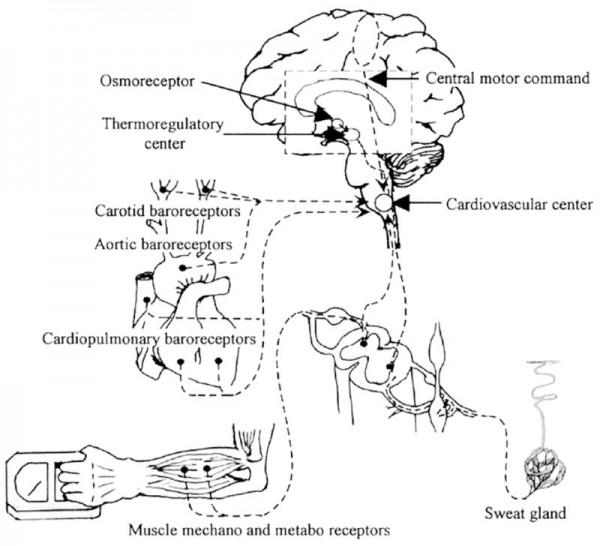

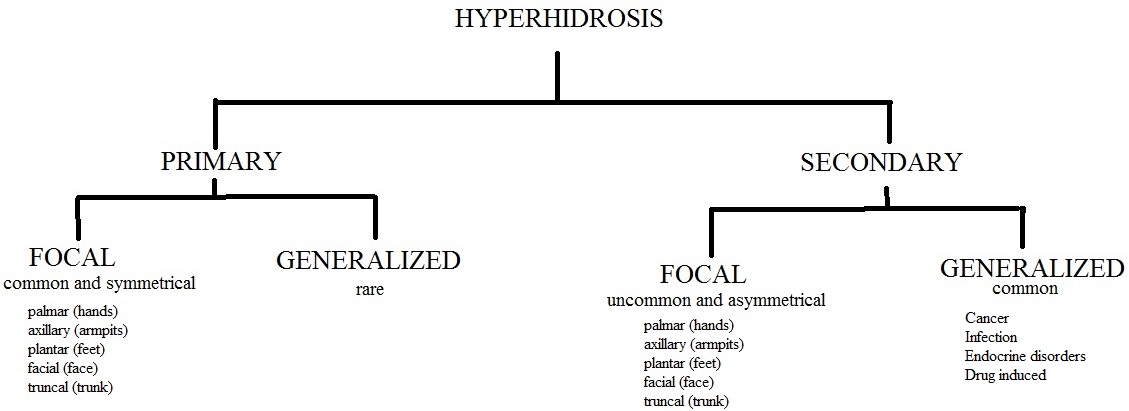
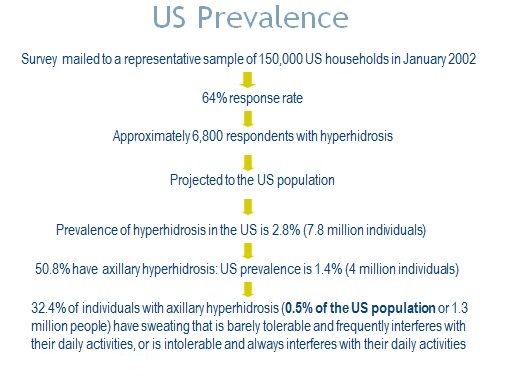
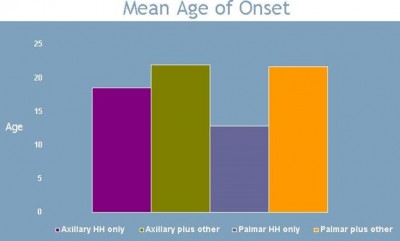
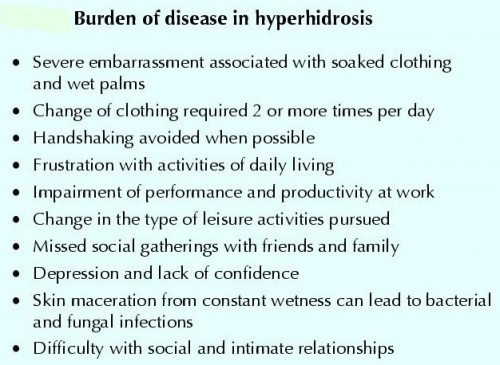

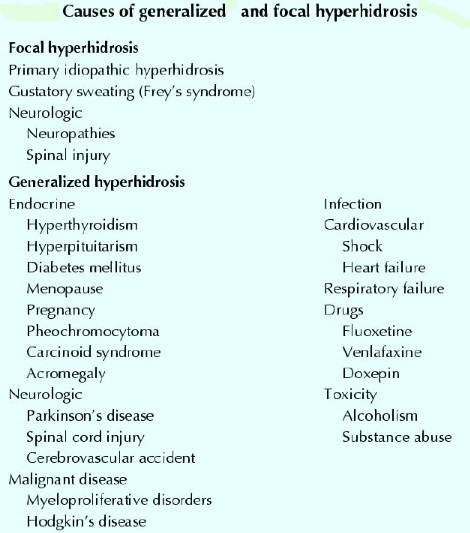


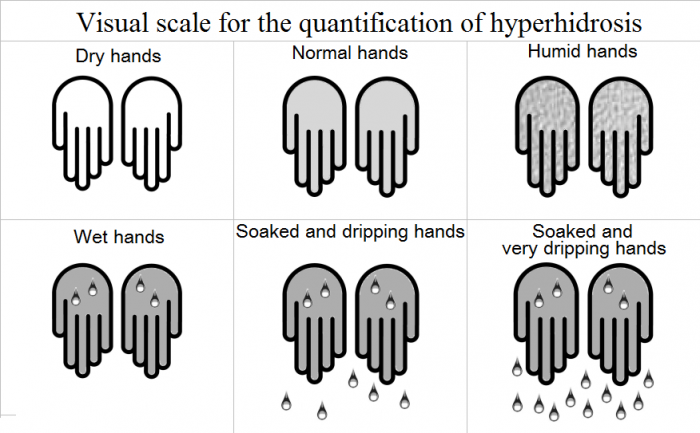
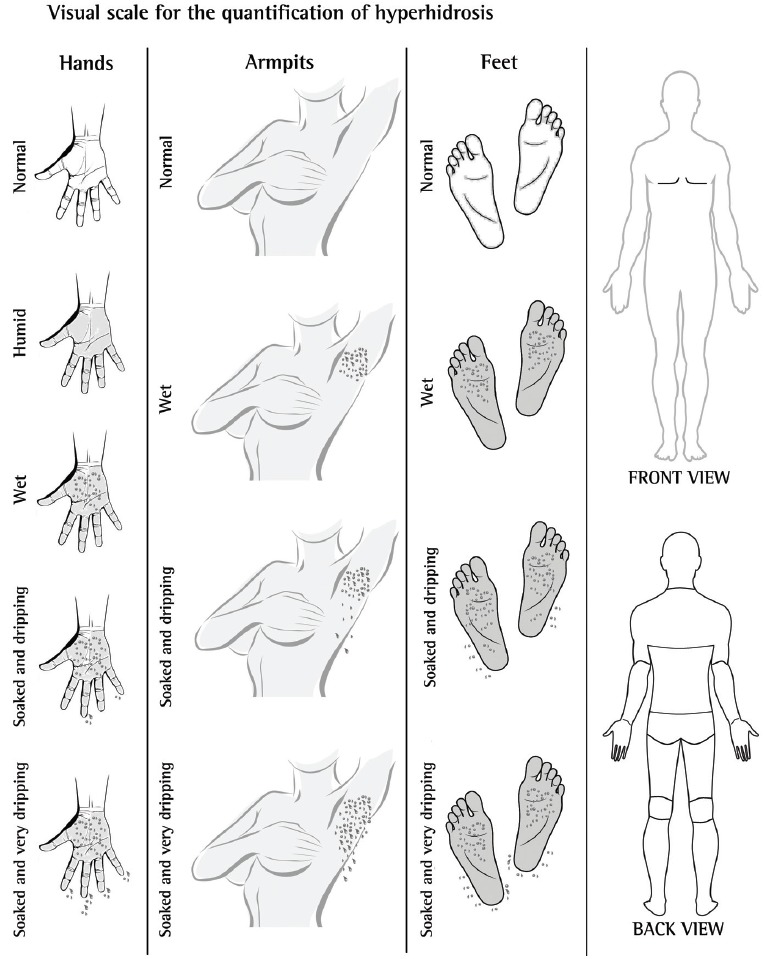


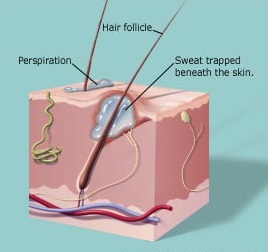


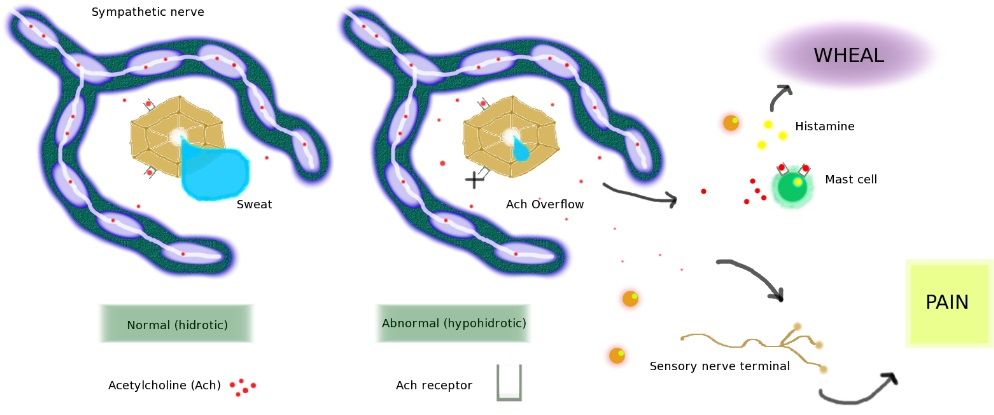
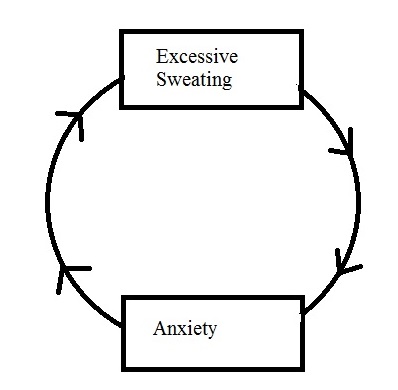

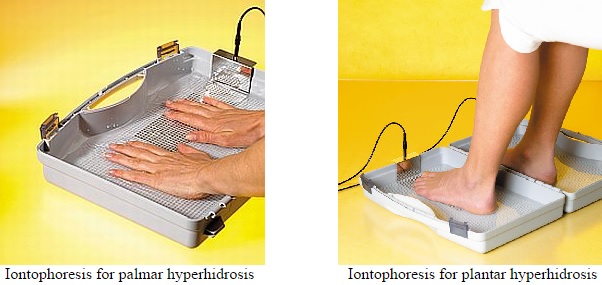

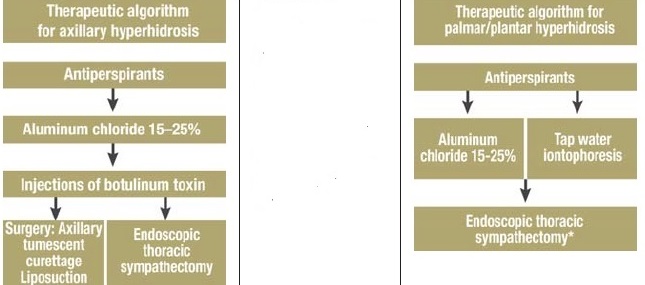
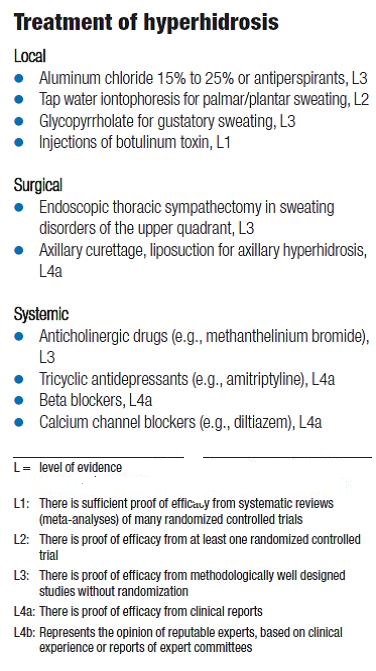
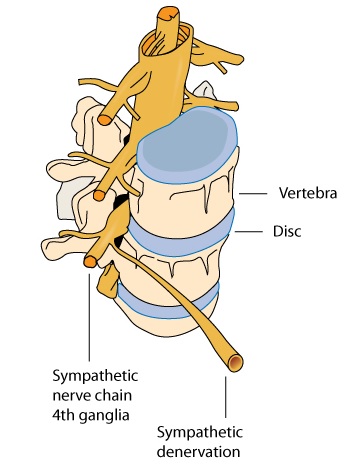
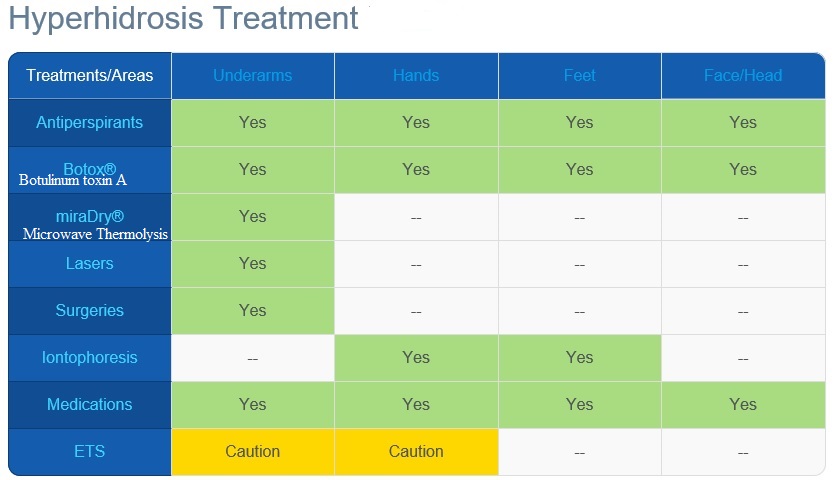
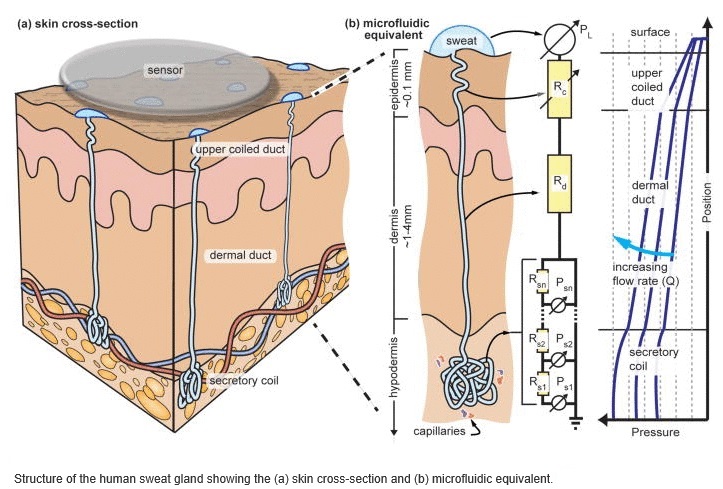

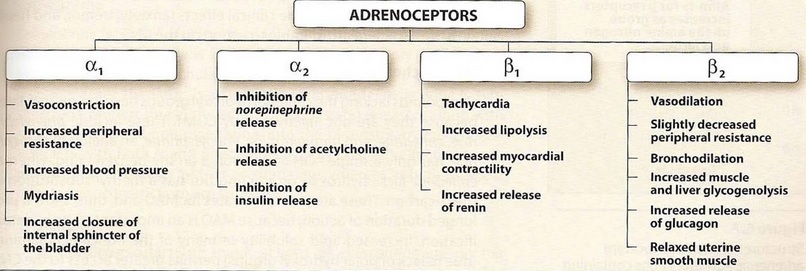
If you want to improve your experience simply keep visiting this web site and be updated with the most recent gossip posted here.|
Hi, all is going fine here and ofcourse every one is sharing data, that’s genuinely fine, keep up writing.|
Amazingness will certainly alter the means you live and also function .
Incredible advantages for you, friends and family that continue providing.
Itís hard to find knowledgeable people about this subject, but you seem like you know what youíre talking about! Thanks