Dr Rajiv Desai
An Educational Blog
PULSE OXIMETRY
PULSE OXIMETRY
_____
Prologue:
All of us know how important oxygen is for our survival. Hypoxia means low oxygen supply and/or utilization by organ or tissue. Hypoxemia means low oxygen content of arterial blood. Hypoxaemia invariably leads to hypoxia but hypoxia can occur even without hypoxaemia. Arterial blood oxygen saturation is now considered the 5th vital sign, joining: temperature, respiratory rate, heart rate and blood pressure. Hypoxemia can be present before recognizable signs of respiratory distress become evident and the traditional sign of circumoral cyanosis is a late indicator of decreased oxygenation. Blood gas analysis was for many years the only available method of detecting hypoxemia in critically ill patients, but this technique is painful, has potential complications, and does not provide immediate or continuous data. Pulse oximetry is an objective estimation of oxygenation, and it is simple, reliable, and accurate when used appropriately. It has the unique advantage of continuously monitoring the saturation of haemoglobin with oxygen, easily and noninvasively, providing a measure of cardio-respiratory function. Pulse oximetry is arguably the greatest advance in patient monitoring since electrocardiography. Hypoxaemia is commonly found in all aspects of medical practice and is a major cause of organ dysfunction and death. Since its introduction into clinical use in the 1980s, pulse oximeters have become ubiquitous clinical monitoring devices used throughout medical practice from operating theatres and intensive care units to outpatient departments and general practice clinics. However, clinically relevant principles and inherent limitations of pulse oximetry are not always well understood by health care professionals. Most of us have a thermometer, blood pressure cuff, or glucometer at home to track specific health concerns. We are just learning how helpful pulse oximeters are at home. The pulse oximeter is inexpensive and very easy to use as a trending tool for families at home.
______
Abbreviation and synonyms:
O2 = Oxygen
CO2 = Carbon dioxide
CO = Carbon monoxide
PaO2 = partial pressure of oxygen in arterial blood expressed in mm Hg.
SaO2 = Oxygen saturation of hemoglobin in arterial blood measured by ABG/Co-oximetry expressed as percentage
SpO2 = Oxygen saturation of hemoglobin in arterial blood measured by a pulse oximeter expressed as percentage
CaO2 = Oxygen content of arterial blood in ml (dissolved oxygen plus oxygen bound to hemoglobin)
ABG = Arterial blood gases
EtCO2 = End-tidal carbon dioxide
SpHb = Hemoglobin estimated by non-invasive pulse co-oximeter
Oxyhemoglobin = Hemoglobin with attached oxygen
Deoxyhemoglobin = Hemoglobin without attached oxygen = Reduced hemoglobin
Functioning Haemoglobin = Hemoglobin which is capable of carrying oxygen. Functioning hemoglobin includes oxygenated hemoglobin (O2Hb) and deoxygenated hemoglobin (Hb).
Non-functioning Hemoglobin = Hemoglobin which is not capable of carrying oxygen. Non-functioning hemoglobin includes carboxyhemoglobin (COHb) and methemoglobin (MetHb).
Pulse oximetry = Technique of measuring oxygen saturation of hemoglobin by shining red and infrared light through a peripheral site, such as a finger, toe, or nose.
Pulse oximeter = device that can detect a pulsatile signal in an extremity such as the finger or toe and can calculate the amount of oxygenated haemoglobin and the pulse rate.
Capnograph = monitor that detects the amount of carbon dioxide in each breath.
Hypoventilation = Breathing at a rate and/or depth that is less than normal.
______
Note:
There is a confusing terminology in pulse oximetry. Everybody uses the term ‘oxygen saturation’ but it is not oxygen that is saturated with hemoglobin but hemoglobin is saturated with oxygen. 70 % oxygen saturation means 70 % of hemoglobin is saturated with oxygen (oxyhemoglobin) and remaining 30 % hemoglobin is without oxygen (deoxyhemoglobin). Hence the term ‘oxygen saturation of hemoglobin’ is more appropriate.
_____
Oxygen content in blood:
_
Oxygen:
The fundamental purpose of the cardiorespiratory system is to deliver O2 and nutrients to cells and to remove CO2 and other metabolic products from them. Proper maintenance of this function depends not only on intact cardiovascular and respiratory systems but also on an adequate number of red blood cells and hemoglobin and a supply of inspired gas containing adequate O2. Body cells need oxygen to perform aerobic respiration. Respiration is one of the key ways a cell gains useful energy. The energy released in respiration is used to synthesize the adenosine triphosphate (ATP) to be stored. The energy stored in ATP can then be used to drive processes requiring energy, including biosynthesis, locomotion, or transportation of molecules across cell membranes. Decreased O2 availability to cells results in an inhibition of oxidative phosphorylation and increased anaerobic glycolysis. This switch from aerobic to anaerobic metabolism, the Pasteur effect, maintains some, albeit reduced ATP production. In severe hypoxia, when ATP production is inadequate to meet the energy requirements of ionic and osmotic equilibrium, cell membrane depolarization leads to uncontrolled Ca2+ influx and activation of Ca2+-dependent phospholipases and proteases. These events, in turn, cause cell swelling and, ultimately cell death. Human beings depend on oxygen for life. All organs require oxygen for metabolism but the brain and heart are particularly sensitive to a lack of oxygen. Shortage of oxygen in the body is called hypoxia. A serious shortage of oxygen for a few minutes is fatal.
_
Survival time before cellular damage occurs after total loss of oxygen delivery (anoxia):
_
Oxygen transport from air to tissues:
Oxygen in the atmosphere is brought into the lungs by breathing, and into the blood via lung capillaries. Then it is transported throughout the body by the blood. Each lung contains nearly 300 million alveoli which are surrounded by blood capillaries. Since alveolar walls and capillary walls are very thin, oxygen passing into the alveoli immediately transfers into the blood capillaries. (Usually in adults, the transfer would take about 0.25 seconds while resting.) A large proportion of the oxygen diffusing into the blood binds to hemoglobin in the red blood cells, while a part of the oxygen dissolves in the blood plasma. Blood enriched with oxygen (arterial blood) flows through pulmonary veins, then into the left atrium and left ventricle, and finally circulates throughout the body’s organs and their cells. The amount of oxygen transported around the body is determined mainly by the degree to which hemoglobin binds to oxygen (lung factor), hemoglobin concentration (anaemic factor), and cardiac output (cardiac factor). Oxygen saturation is an indicator of oxygen transport in the body, and indicates if sufficient oxygen is being supplied to the body.
_
Oxygen transport:
Oxygen is inhaled into the lungs, and carbon (carbon dioxide) is exhaled from the lungs to the air. This process is called ventilation. Inhaled air flows into the upper airway, then into the peripheral airways, and is finally distributed into the lungs. This process is called distribution. The lungs consist of tissues called alveoli. Oxygen is absorbed from the alveoli, then into the lung capillaries via alveolar membranes, while carbon dioxide moves from the lung capillaries to the alveoli. This process is called diffusion.
_
Oxygen is carried around the body attached to an iron-containing protein called haemoglobin (Hb) contained in red blood cells. After oxygen is breathed into the lungs, it combines with the haemoglobin in red blood cells as they pass through the pulmonary capillaries. The heart pumps blood continuously around the body to deliver oxygen to the tissues.
There are five important things that must happen in order to deliver enough oxygen to the tissues:
• Oxygen must be breathed in (or inspired) from the air into the lungs.
• Oxygen must pass from the air spaces in the lung (called the alveoli) to the blood. This is called alveolar gas exchange.
• The blood must contain enough haemoglobin to carry sufficient oxygen to the tissues.
• The heart must be able to pump enough blood to the tissues to meet the patient’s oxygen requirements.
• The volume of blood in the circulation must be adequate to ensure oxygenated blood is distributed to all the tissues.
_
Function of Hemoglobin:
To support oxygen transport, hemoglobin must bind O2 efficiently at the partial pressure of oxygen (PO2) of the alveolus, retain it, and release it to tissues at the PO2 of tissue capillary beds. Oxygen acquisition and delivery over a relatively narrow range of oxygen tensions depend on a property inherent in the tetrameric arrangement of heme and globin subunits within the hemoglobin molecule called cooperativity or heme-heme interaction. At low oxygen tensions, the hemoglobin tetramer is fully deoxygenated. Oxygen binding begins slowly as O2 tension rises. However, as soon as some oxygen has been bound by the tetramer, an abrupt increase occurs in the oxygen binding. Thus, hemoglobin molecules that have bound some oxygen develop a higher oxygen affinity, greatly accelerating their ability to combine with more oxygen.
_
Bound and dissolved oxygen:
Binding sites for oxygen are the heme groups, the Fe++-porphyrin portions of the hemoglobin molecule. There are four heme sites, and hence four oxygen binding sites per hemoglobin molecule. Heme sites occupied by oxygen molecules are said to be “saturated” with oxygen. The percentage of all the available heme binding sites saturated with oxygen is the hemoglobin oxygen saturation (in arterial blood, the SaO2).
_
Since each hemoglobin molecule can bind to 4 molecules of oxygen, it may bind with 1 to 4 molecules of oxygen. However, hemoglobin is stable only when bound to 4 molecules of oxygen or when not bound to any oxygen. It is very unstable when bound to 1 to 3 molecules of oxygen. Therefore, as shown in the above figure, hemoglobin exists in the body in the form of deoxygenated hemoglobin (Hb) with no oxygen bound, or as oxygenated hemoglobin (O2Hb) with 4 molecules of oxygen. When all Hemoglobin molecules are bound with 4 molecules of oxygen, we call oxygen saturation 100 %. When 50 % hemoglobin molecules are bound with 4 molecules of oxygen, we call oxygen saturation 50 %. This oxygen saturation in percentage is measured by pulse oximetry.
_
Hypoxia and hypoxaemia:
_
_
Hypoxia is a condition in which the body or a region of the body is deprived of adequate oxygen supply. Hypoxia may be classified as either generalized, affecting the whole body, or local, affecting a region of the body. Although hypoxia is often a pathological condition, variations in arterial oxygen concentrations can be part of the normal physiology, for example, during hypoventilation training or strenuous physical exercise. Hypoxia in which there is complete deprivation of oxygen supply is referred to as “anoxia”. Hypoxia means low oxygen supply and/or utilization by organ or tissue. Hypoxemia means low oxygen content of arterial blood. Hypoxaemia invariably leads to hypoxia but hypoxia can occur even without hypoxaemia. Ischemia, meaning insufficient blood flow to a tissue, can also result in hypoxia. This is called ‘ischemic hypoxia’. This can include an embolic event, a heart attack that decreases overall blood flow, or trauma to a tissue that results in damage. An example of insufficient blood flow causing local hypoxia is gangrene that occurs in diabetes. Diseases such as peripheral vascular disease can also result in local hypoxia. Hypoxemic hypoxia (hypoxic hypoxia) refers specifically to hypoxic states where the oxygen content of arterial blood is insufficient due to poor oxygenation. This can be caused by alterations in respiratory drive, such as in respiratory alkalosis, physiological or pathological shunting of blood, diseases interfering in lung function resulting in a ventilation-perfusion mismatch, such as a pulmonary embolus, or alterations in the partial pressure of oxygen in the environment or lung alveoli, such as may occur at altitude or when diving. Hemoglobin plays a substantial role in carrying oxygen throughout the body, and when it is deficient, anemia can result, causing ‘anaemic hypoxia’. A chronic hypoxic state can result from a poorly compensated anaemia. Histotoxic hypoxia results when the quantity of oxygen reaching the cells is normal, but the cells are unable to use the oxygen effectively, due to disabled oxidative phosphorylation enzymes. This may occur in cyanide poisoning. An another instance of hypoxemic hypoxia would be when carbon monoxide is present in the blood, as hemoglobin has a higher affinity to carbon monoxide than oxygen. Not only does the carbon monoxide prevent the oxygen from reaching the cells, it is also a metabolic poison, compromising the cell’s ability to transport oxygen resulting in Histotoxic hypoxia. Pulse oximetry can measure hypoxemic hypoxia due to poor oxygenation by measuring oxygen saturation of hemoglobin but cannot measure anemic, circulatory, ischaemic or histotoxic hypoxia.
_
If the O2 consumption of tissues is elevated without a corresponding increase in perfusion, tissue hypoxia ensues and the PO2 in venous blood declines. Ordinarily, the clinical picture of patients with hypoxia due to an elevated metabolic rate, as in fever or thyrotoxicosis, is quite different from that in other types of hypoxia: the skin is warm and flushed owing to increased cutaneous blood flow that dissipates the excessive heat produced, and cyanosis is usually absent.
________
Carbon dioxide:
Carbon dioxide is produced by cell metabolism in the mitochondria. The amount produced depends on the rate of metabolism and the relative amounts of carbohydrate, fat and protein metabolized. The respiratory quotient (RQ) is the ratio of CO2 produced to O2 consumed while food is being metabolized. RQ = CO2 eliminated/O2 consumed. The amount is about 200ml/min when at rest and eating a mixed diet; this utilises 80% of the oxygen consumed, giving a respiratory quotient of 0.8 A carbohydrate diet gives a RQ of 1 and a fat diet 0.7.
_
Carbon dioxide transport in the blood:
There are 3 ways in which carbon dioxide is transported in the blood:
1. Dissolved CO2:
Carbon dioxide is 20 times more soluble than oxygen. About 5 % of carbon dioxide is transported unchanged, simply dissolved in the plasma. Arterial blood contains about 2.5 ml per 100 ml of dissolved carbon dioxide and venous blood 3 ml per 100 ml. A cardiac output of 5 liter per minute will carry 150 ml of dissolved carbon dioxide to the lung, of which 25 ml will be exhaled. Because of this high solubility and diffusing capacity, carbon dioxide partial pressure of alveolar and pulmonary end-capillary blood are virtually the same. Even a large shunt of 50% will only cause an end-pulmonary capillary/ arterial carbon dioxide gradient of about 0.4 kPa.
2. Bound to hemoglobin and plasma proteins:
Carbon dioxide combines reversibly with haemoglobin to form carbaminohaemoglobin. Carbon dioxide does not bind to iron, as oxygen does, but to amino groups on the polypeptide chains of haemoglobin. Carbon dioxide also binds to amino groups on the polypeptide chains of plasma proteins. About 10 % of carbon dioxide is transported bound to haemoglobin and plasma proteins
3. Bicarbonate ions (HCO3-):
The majority of carbon dioxide is transported in this way. Carbon dioxide enters red blood cells in the tissue capillaries where it combines with water to form carbonic acid (H2CO3). This reaction is catalysed by the enzyme carbonic anhydrase, which is found in the red blood cells. Carbonic acid then dissociates to form bicarbonate ions (HCO3-) and hydrogen ions (H+). This reaction also occurs outside the red blood cells, in the plasma, but is much slower due to the lack of carbonic anhydrase, so approximately 75% of carbon dioxide is transport in the red blood cell and 25% in the plasma. The hydrogen ions, formed from the dissociated carbonic acid, combine with the haemoglobin in the red blood cell.
_
After releasing oxygen to the tissues, some of the Hb—which is now deoxygenated Hb—may pick up some of the carbon dioxide (CO2) formed as a by-product of cellular aerobic metabolism to form carbaminohemoglobin. Approximately 5%-10% of CO2 is transported as carbaminohemoglobin; the majority of CO2 (85% – 90%) is transported as bicarbonate. CO2 is transported to the lungs where it is released into the alveoli and eliminated in the process of ventilation.
________
Measurement of oxygen:
Oxygen can be measured in three forms:
1. Partial pressure of oxygen (PO2)/partial pressure of arterial oxygen (PaO2)
2. Oxygen saturation in arterial blood (SaO2) / Calculated estimate of oxygen saturation (SpO2) by pulse oximetry
3. Oxygen content in arterial blood (CaO2)
___
Concept of partial pressure:
According to Dalton’s Law, the total pressure of a mixture of gases is the sum of the pressures of the individual gases. In dry air, at an atmospheric pressure of 760 mm Hg, 78% of the total pressure is due to nitrogen molecules and 21% is due to oxygen. So atmospheric pressure of air is sum total of partial pressure of nitrogen and oxygen. Thus the PO2 that we breathe in is 160mm (760 X 0.21). After adjusting for dead airway space, elevation, patient temperature, and water vapor, the range of a normal PaO2 should be between 90-106 mm of Hg.
_
The figure below shows fall in PO2 from 160 mm Hg in atmosphere to 100 mm Hg in alveoli and oxygenation of blood:
_
PaO2 is partial pressure of oxygen in arterial blood. The arterial PO2 is frequently described as the PaO2 to denote that this is an arterial sample, as opposed to a venous or capillary PO2. PaO2, the partial pressure of oxygen in the plasma phase of arterial blood, is registered by an electrode that senses randomly-moving, dissolved oxygen molecules. The amount of dissolved oxygen in the plasma phase — and hence the PaO2 — is determined by alveolar PO2 and lung architecture only, and is unrelated to anything about hemoglobin. (With one exception: when there is both anemia and a sizable right to left shunt of blood through the lungs. In this situation a sufficient amount of blood with low venous O2 content can enter the arterial circulation and lead to a reduced PaO2. However, with a normal amount of shunting, anemia and hemoglobin variables do not affect PaO2.) Since PaO2 reflects only free oxygen molecules dissolved in plasma and not those bound to hemoglobin, PaO2 cannot tell us “how much” oxygen is in the blood; for that you need to know how much oxygen is also bound to hemoglobin, information given by the SaO2 and hemoglobin content. By administering supplemental oxygen or placing a patient in a hyperbaric chamber, PaO2 can be increased considerably resulting in increase of amount of oxygen that is dissolved in the arterial blood. The higher the partial pressure of oxygen, the more oxygen will be dissolved in blood. The normal partial pressure of oxygen in a human arterial blood is about 80-100 mm of mercury, and it refers only to the free oxygen within the blood, meaning the type that isn’t bound to hemoglobin.
_
One of the main functions of blood is to receive oxygen from the lungs and transport it into the body’s tissues. At the same time, blood receives carbon dioxide from the tissues, and brings it back to the lungs. The amount of gas dissolved in a liquid (blood, in this case) is proportional to the pressure (partial pressure) of the gas. In addition, each gas has a different solubility. There are two mechanisms by which oxygen could be coalesced with blood. The first is when oxygen is dissolved in plasma due to the partial pressure difference of oxygen that is present in the surrounding atmosphere and the blood in the lungs. Partial pressure is the pressure exerted by a single component of a mixture of gases, commonly expressed in mm Hg; for a gas dissolved in a liquid, the partial pressure is that of a gas that would be in equilibrium with the dissolved gas. This causes oxygen to dissolve in the plasma of the blood, for each 1mmHg partial pressure of oxygen 0.003ml dissolves in the plasma. Only about 0.3 ml of gaseous oxygen dissolves in 100 ml blood per mmHg (pressure). This amount is only 1/20 of carbon dioxide solubility. This suggests that a human could not get sufficient oxygen if solubility were the only way to get oxygen in the blood. For this reason, hemoglobin (Hb) has an important role as a carrier of oxygen. This is the second mechanism when oxygen binds with hemoglobin that is found in the red blood cells and forms oxyhemoglobin, which thereafter could be transported to all over the body, where the oxygen could be taken up, relieving the hemoglobin back to its original state. Here for every 1gm of hemoglobin, 1.34 ml of oxygen is carried. Since 100 ml of blood contain about 15 g of hemoglobin, the hemoglobin contained in 100 ml of blood can bind to 20.1 ml of oxygen. The dissolved fraction is available to tissues first and then, the fraction bound to hemoglobin. So as tissues metabolize oxygen or if oxygen becomes difficult to pick up through the lungs, the dissolved oxygen and the oxygen bound to hemoglobin will eventually become depleted. The dissolved oxygen can be measured by arterial blood gas analysis but this is not yet a practical field application. This fraction is not measured by pulse oximeter. The presence of available oxygen in form of oxyhaemoglobin in the blood could be simplified or rather related to what we call the oxygen saturation that is calculated by the pulse oximeter. The standard range for oxygen saturation is from 95-100% although a value up to 90% is accepted.
_
The PO2 of RBCs is the same as the PO2 of the plasma, yet the oxygen content of the plasma is minute, compared to the oxygen content of RBCs because RBCs contains hemoglobin that binds a lot of oxygen while the plasma contains only minute amounts of dissolved oxygen.
_
Correlation of partial pressure of oxygen and oxygen saturation of hemoglobin:
Oxygen molecules that pass through the thin alveolar-capillary membrane enter the plasma phase as dissolved (free) molecules; most of these molecules quickly enter the red blood cell and bind with hemoglobin. There is a dynamic equilibrium between the freely dissolved and the hemoglobin-bound oxygen molecules. However, the more dissolved molecules there are (i.e., the greater the PaO2) the more will bind to available hemoglobin; thus SaO2 always depends, to a large degree, on the concentration of dissolved oxygen molecules (i.e., on the PaO2). Because there is a virtually unlimited supply of oxygen molecules in the atmosphere, the dissolved O2 molecules that leave the plasma to bind with hemoglobin are quickly replaced by others; once bound, oxygen no longer exerts a gas pressure. Thus hemoglobin is like an efficient sponge that soaks up oxygen so more can enter the blood. Hemoglobin continues to soak up oxygen molecules until it becomes saturated with the maximum amount it can hold – an amount that is largely determined by the PaO2. Of course this whole process is near instantaneous and dynamic; at any given moment a given O2 molecule could be bound or dissolved. However, depending on the PaO2 and other factors, a certain percentage of all O2 molecules will be dissolved (about 1.5%) and a certain percentage will be bound (about 98.5%). PaO2 measures the oxygen that has passed through the lungs and into the blood. SaO2 measures the oxygen that has saturated the Hemoglobin in red blood cells after oxygen has passed into the blood from the lungs. In summary, PaO2 is determined by alveolar PO2 and the state of the alveolar-capillary interface, not by the amount of hemoglobin available to soak them up. PaO2, in turn, determines the oxygen saturation of hemoglobin (along with other factors that affect the position of the O2-dissociation curve, discussed below). The SaO2, plus the concentration of hemoglobin (15 gm/dl), determine the total amount of oxygen in the blood or CaO2 (vide infra). If the air is thin (at Mount Everest-low atmospheric pressure) or the lungs cannot take in oxygen appropriately due to any number of diseases, then obviously little oxygen gets into the lungs, into circulation, or both, thereby decreasing arterial partial pressure of oxygen. After oxygen has entered and dissolved within the blood, then, and only then, can oxygen bind to the hemoglobin in our blood. It is SaO2 that measures oxygen saturation of hemoglobin, and it should be clear that it depends on the partial pressure of arterial oxygen. If PaO2 drops, there’s less dissolved oxygen, and therefore less saturation of hemoglobin with oxygen. But oxygen saturation is tricky! If all of a sudden someone loses a lot of hemoglobin, as long as PaO2 remains the same, so will oxygen saturation. That’s because oxygen saturation measures the percentage of oxygen-binding sites occupied by oxygen on any and all remaining hemoglobin, not the total amount of oxygen bound to hemoglobin! Therefore both oxygen saturation and the partial pressure of oxygen in arterial blood are independent of the amount of hemoglobin in the blood. It is important to understand the difference between the PaO2, the oxygen saturation (SaO2), the oxygen content and the oxygen delivery rate.
_
The PaO2 and the SaO2 are related to each other by the oxygen hemoglobin dissociation curve discussed vide infra. This curve plots the oxygen saturation (in %) on the vertical axis and PaO2 on the horizontal axis. The oxygen saturation % steadily increases as the PO2 increases up to about a PO2 of 100 mmHg at which point the oxygen saturation is 99% to 100% (i.e., all the hemoglobin oxygen binding sites contain oxygen). If the patient breathes supplemental oxygen, the inspired PO2 increases to 200 mmHg, 400 mmHg or higher depending on how much oxygen is inhaled. Thus, a patient breathing supplemental oxygen may have a PaO2 as high as 400 mmHg, but his oxygen saturation is still 100%, since it can’t get any higher than this. The higher PaO2 will increase dissolved oxygen in plasma but oxygen carried by hemoglobin will remain same.
_
Oxygen saturation:
Red blood cells contain hemoglobin. One molecule of hemoglobin can carry up to four molecules of oxygen after which it is described as “saturated” with oxygen. If all the binding sites on the haemoglobin molecule are carrying oxygen, the haemoglobin is said to have a saturation of 100%. Oxygen is carried in the blood attached to haemoglobin molecules. Oxygen saturation is a measure of how much oxygen the blood is carrying as a percentage of the maximum it could carry. One haemoglobin molecule can carry a maximum of four molecules of oxygen. One hundred haemoglobin molecules could together carry a maximum of 400 (100 X 4) oxygen molecules, if these 100 haemoglobin molecules were carrying 380 oxygen molecules they would be carrying (380 / 400) X 100 = 95% of the maximum number of oxygen molecules that could carry and so together would be 95% saturated. Most of the haemoglobin in blood combines with oxygen as it passes through the lungs. A healthy individual with normal lungs, breathing air at sea level, will have an arterial oxygen saturation of 95% – 100% (PaO2 80 to 100mm). If the level is below 90 percent, it is considered low resulting in hypoxemia. Blood oxygen levels below 80 percent may compromise organ function, such as the brain and heart, and should be promptly addressed. Continued low oxygen levels may lead to respiratory or cardiac arrest. Oxygen therapy may be used to assist in raising blood oxygen levels. Oxygenation occurs when oxygen molecules (O2) enter the tissues of the body. For example, blood is oxygenated in the lungs, where oxygen molecules travel from the air and into the blood. Oxygenation is commonly used to refer to medical oxygen saturation. Extremes of altitude will affect these numbers. Venous blood that is collected from the tissues contains less oxygen and normally has a saturation of around 75% (PaO2 40mm). Arterial blood looks bright red whilst venous blood looks dark red. The difference in colour is due to the difference in haemoglobin saturation.
_
Oxygen saturation formula:
Oxygen saturation is a measurement of the percentage of oxygen binding sites that contain oxygen. If all the oxygen binding sites contain oxygen, then the oxygen saturation is 100%. Oxygen saturation is defined as the ratio of oxy-hemoglobin to the total concentration of hemoglobin present in the blood (i.e. Oxy-hemoglobin + reduced hemoglobin). When arterial oxy-hemoglobin saturation is measured by an arterial blood gas it is called SaO2. When arterial oxy-hemoglobin saturation is measured non-invasively by a finger pulse oximeter or handheld pulse oximeter, it is called SpO2. Note that SaO2/SpO2 alone doesn’t reveal how much oxygen is in the blood; for that we also need to know the hemoglobin content.
_
However in practice there will always be some haemoglobin that is dysfunctional or combined with something other than oxygen and so is not available to carry oxygen.
_
Functional oximetry vs. fractional oximetry:
It is important to understand the principle of the pulse oximeter so that a clinician has an understanding of what is actually being measured by the pulse oximeter and what its limitations are. An understanding of fractional oximetry (SaO2) versus functional oximetry (SpO2) is necessary. Oximeters can measure either functional or fractional oxygen saturations. Functional saturation is the ratio of oxygenated haemoglobin to all haemoglobin capable of carrying oxygen; fractional saturation is the ratio of oxygenated haemoglobin to all haemoglobin (including that which does not carry oxygen). Fractional saturation is approximately 2% lower than functional saturation. SpO2 represents an estimate of functional arterial hemoglobin saturation, which refers only to the arterial hemoglobin that is capable of transporting oxygen (functional hemoglobin = oxyhemoglobin/ [oxyhemoglobin + deoxyhemoglobin]). Functional saturation differs from fractional hemoglobin saturation (Fractional hemoglobin = oxyhemoglobin/ total hemoglobin), which can be measured by most blood gas analyzers with co-oximetry. The total hemoglobin denominator in the calculation of fractional hemoglobin might include abnormal or variant hemoglobin molecules with limited oxygen-carrying properties. Therefore, the terms “functional” and “fractional” hemoglobin saturation are not interchangeable. In situations such as dyshemoglobinemias, pulse-oximetry readings do not adequately reflect the oxygen-carrying properties of arterial blood.
_
SaO2 is defined as the oxyhemoglobin (O2Hb) divided by the total hemoglobin (including all hemoglobin species) in a sample and can be written as:
SaO2 = O2Hb / [O2Hb + Hb + MetHb + COHb]
Where O2Hb is oxyhemoglobin, Hb is deoxyhemoglobin, Met Hb is methemoglobin, and COHb is carboxyhemoglobin.
You multiply above fraction by 100 to get SaO2 in percentage. These values are determined by analysis of arterial blood sample using co-oximetry.
SpO2 is defined as the oxyhemoglobin divided by all the functional hemoglobin in a sample and can be written as:
SpO2 = O2Hb/ [O2Hb + Hb] It is determined by pulse oximetry.
_
The three most important measures of oxygen in blood are:
1. SaO2. It’s a percentage that shows how saturated your arterial blood (hemoglobin) is with oxygen. It’s obtained from an ABG with co-oximeter, so it’s very accurate. Normal is 95-98%, although 90% or better is usually considered acceptable. It determines fractional oxygen saturation.
2. PaO2. It’s the partial pressure of arterial oxygen. It’s obtained from an ABG, and is an accurate measure of dissolved oxygen in arterial blood. A normal range is 80-100 mm Hg, although 60 or better is usually considered acceptable.
3. SpO2. It’s similar to SaO2, although it’s estimated by pulse oximetry. A normal value is 95-98%, although 90% or better is usually considered acceptable. It determines functional oxygen saturation.
_
Some important considerations:
1. CaO2 is arterial oxygen content. Unlike either PaO2 or SaO2, the value of CaO2 directly reflects the total number of oxygen molecules in arterial blood, both bound and unbound to hemoglobin. CaO2 depends on the hemoglobin content, SaO2, and the amount of dissolved oxygen. Units for CaO2 are ml oxygen/100 ml blood (see below).
2. PaO2 is a sensitive and non-specific indicator of the lungs’ ability to exchange gases with the atmosphere. In patients breathing ambient or “room” air (FIO2 = 0.21), a decreased PaO2 indicates impairment in the gas exchange properties of the lungs, usually signifying V-Q imbalance. PaO2 is a very sensitive indicator of gas exchange impairment; it can be reduced from virtually any parenchymal lung problem, including asthma, chronic obstructive pulmonary disease, and atelectasis that doesn’t show up on a chest x-ray.
3. FIO2 is the same at all altitudes. The percentage of individual gases in air (oxygen, nitrogen, etc.) doesn’t change with altitude, but the atmospheric (or barometric) pressure does. FIO2, the fraction of inspired oxygen in the air, is thus 21% (or 0.21) throughout the breathable atmosphere. PaO2 declines with altitude because the inspired oxygen pressure declines with altitude (inspired oxygen pressure is fraction of oxygen times the atmospheric pressure). Average barometric pressure at sea level is 760 mm Hg; it has been measured at 253 mm Hg on the top of Mt. Everest (8,848 metres above sea level). As one ascends rapidly to 3000 m (10,000 ft), the reduction of the O2 content of inspired air (FiO2) leads to a decrease in alveolar PO2 to approximately 60 mmHg, and a condition termed high-altitude illness develops. At higher altitudes, arterial saturation declines rapidly and symptoms become more serious; and at 5000 m, unacclimated individuals usually cease to be able to function normally owing to the changes in CNS functions.
4. Normal PaO2 decreases with age. A patient over age 70 may have a normal PaO2 around 70-80 mm Hg, at sea level. A useful rule of thumb is normal PaO2 at sea level (in mm Hg) = 100 minus the number of years over age 40.
5. The body does not store oxygen. If a patient needs supplemental oxygen it should be for a specific physiologic need, e.g., hypoxemia during sleep or exercise, or even continuously (24 hours a day) as in some patients with severe, chronic lung disease.
6. Supplemental O2 is an FIO2 > 21%. Supplemental oxygen means an FIO2 greater than the 21% oxygen in room (ambient) air. When you give supplemental oxygen you are raising the patient’s inhaled FIO2 to something over 21%; the highest FIO2 possible is 100%. To give more oxygen requires a hyperbaric chamber.
7. High FIO2 doesn’t affect COPD hypoxic drive. The reason a high FIO2 may raise PaCO2 in a patient with COPD is not because the extra oxygen cuts off the hypoxic drive. Modest rise in PaCO2 occurs mainly because the extra oxygen alters V/Q relationships within the lungs, creating more physiologic dead space.
8. A given liter flow rate of nasal O2 does not equal any specific FIO2. The often-quoted rule that 2 l/min = an FIO2 of 24%, 3 l/min = 28%, etc., is an illusion, based on nothing experimental or scientific. The actual FIO2 with nasal oxygen depends on the patient’s breathing rate and tidal volume, i.e., the amount of room air inhaled through the mouth and nose that mixes with the supplemental oxygen.
9. Face masks cannot deliver 100% oxygen unless there is a tight seal. So-called non-rebreather face masks can deliver an FIO2 up to around 80%. It is a mistake to label a patient with any loose-fitting face mask as receiving an “FIO2 of 100%.” So100% oxygen can only be delivered with a ventilator or tight-fitting face mask.
________
Oxygen content of arterial blood (CaO2):
Tissues need a requisite amount of O2 molecules for metabolism. Neither the PaO2 nor the SaO2 provide information on the number of oxygen molecules, i.e., of how much oxygen is in the blood. (Note that neither PaO2 nor SaO2 have units that denote any quantity.) Of the three values used for assessing blood oxygen levels, how much is provided only by the oxygen content, CaO2 (ml O2/dl). This is because CaO2 is the only value that incorporates the hemoglobin content.
Oxygen content can be measured directly or calculated by the oxygen content equation:
Oxygen content of blood = bound oxygen + dissolved oxygen
Bound oxygen = Hb in blood x 1.34 mlO2/ gm Hb x SaO2 in fraction (100% = 1)
Dissolved oxygen = PaO2 x 0.003mlO2/mmHg
In other words
CaO2 = [Hb (gm/dl) x 1.34 ml O2/gm Hb x SaO2 fraction] + [PaO2 x (0.003 ml O2/mm Hg/dl)]
This calculation gives O2 in ml per 100 ml of blood. If the haemoglobin level is halved, the oxygen content of arterial blood will be halved.
_
The oxygen carrying capacity of one gram of hemoglobin is 1.34 ml. With a hemoglobin content of 15 grams/dl blood and a normal hemoglobin oxygen saturation (SaO2) of 98%, arterial blood has a hemoglobin-bound oxygen content of 15 x .98 x 1.34 = 19.7 ml O2/dl blood. An additional small quantity of O2 is carried dissolved in plasma: 0.003 ml O2/dl plasma/mm Hg PaO2, or 0.3 ml O2/dl plasma when PaO2 is 100 mm Hg. Since normal CaO2 is 16-22 ml O2/dl blood, the amount contributed by dissolved (unbound) oxygen is very small, only about 1.4% to 1.9% of the total. Given normal pulmonary gas exchange (i.e., a normal respiratory system), factors that lower oxygen content – such as anemia, carbon monoxide poisoning, methemoglobinemia, shifts of the oxygen dissociation curve – do not affect PaO2. PaO2 is a measurement of pressure exerted by uncombined oxygen molecules dissolved in plasma; once oxygen molecules chemically bind to hemoglobin they no longer exert any pressure. PaO2 affects oxygen content by determining, along with other factors such as pH and temperature, the oxygen saturation of hemoglobin (SaO2). The familiar O2-dissociation curve can be plotted as SaO2 vs. PaO2 and as PaO2 vs. oxygen content. For the latter plot the hemoglobin concentration must be stipulated. When hemoglobin content is adequate, patients can have a reduced PaO2 (defect in gas transfer) and still have sufficient oxygen content for the tissues (e.g., hemoglobin 15 grams%, PaO2 55 mm Hg, SaO2 88%, CaO2 17.8 ml O2/dl blood). Conversely, patients can have a normal PaO2 and be profoundly hypoxemic by virtue of a reduced CaO2. This paradox – normal PaO2 and hypoxemia – generally occurs one of two ways: 1) anemia, or 2) altered affinity of hemoglobin for binding oxygen. A common misconception is that anemia affects PaO2 and/or SaO2; if the respiratory system is normal, anemia affects neither value. (In the presence of a right to left intrapulmonary shunt anemia can lower PaO2 by lowering the mixed venous oxygen content; when mixed venous blood shunted past the lungs mixes with oxygenated blood leaving the pulmonary capillaries, lowering the resulting PaO2) Obviously, however, the lower the hemoglobin content the lower the oxygen content. It is not unusual to see priority placed on improving a chronically hypoxemic patient’s low PaO2 when a blood transfusion would be far more beneficial. Anemia can also confound the clinical suspicion of hypoxemia since anemic patients do not generally manifest cyanosis even when PaO2 is very low. Cyanosis requires a minimum quantity of de-oxygenated hemoglobin to be manifest – approximately 5 grams% in the capillaries. A patient whose hemoglobin content is 15 grams% would not generate this much reduced hemoglobin in the capillaries until the SaO2 reached 78% (PaO2 44 mm Hg); when hemoglobin is 9 grams% the threshold SaO2 for cyanosis is lowered to 65% (PaO2 34 mm Hg). Altered hemoglobin affinity may occur from shifts of the oxygen dissociation curve (e.g., acidosis, hyperthermia), from alteration of the oxidation state of iron in the hemoglobin (methemoglobinemia), or from carbon monoxide poisoning. Carbon monoxide by itself does not affect PaO2 but only SaO2 and O2 content. To know the oxygen content one needs to know the hemoglobin content and the SaO2; both should be measured as part of each arterial blood gas test. A calculated SaO2 may be way off the mark and can be clinically misleading. This is true even without excess CO in the blood.
_
How much oxygen in blood:
In a patient who is in good health:
• Each gram of haemoglobin combines with 1.34 ml of oxygen. Therefore, in blood with a normal haemoglobin concentration of 15g/dl, 100 ml of blood carries approximately 20 ml of oxygen combined with haemoglobin. In addition, a small quantity of oxygen is dissolved in the blood.
• The heart normally pumps approximately 5000 ml of blood per minute to the tissues in an average sized adult. This delivers about 1000 ml of oxygen to the tissues per minute.
• The cells in the tissues extract oxygen from the blood for metabolism, normally around 250ml of oxygen per minute. This means that if there is no oxygen being exchanged in the lung, there is only enough oxygen stored in the blood for around 3 minutes (only 75% of the oxygen carried by the haemoglobin is available to the tissues).
• Anaemic patients have lower levels of haemoglobin and are therefore unable to carry as much oxygen in the blood. At a haemoglobin concentration of less than 6g/dl, delivery of oxygen to the tissues may become too low to meet the metabolic demands. Patients who suffer major blood loss during surgery and become acutely anaemic should be given 100% oxygen to breathe. This will increase the amount of dissolved oxygen in the blood and will improve tissue oxygen delivery by a small amount. Blood transfusion may be life-saving.
_
The oxygen content is determined by the oxygen saturation percentage and the hemoglobin concentration. A patient with hemoglobin of 14 has twice as much oxygen per ml of blood compared to a patient with a hemoglobin of 7, assuming that they both have 100% oxygen saturations. Similarly, the visual presence of cyanosis is dependent upon the concentration of desaturated (blue) hemoglobin. Thus, a patient with hemoglobin of 7 at 80% saturation has a deoxygenated hemoglobin concentration of 1.4. This patient will visually appear to be just as blue (though paler) as a patient with a hemoglobin of 14 at 90% saturation, since this latter person also has a deoxygenated hemoglobin concentration of 1.4. Additionally, a patient with hemoglobin of 14 at 80% saturation will look more cyanotic than a patient with a hemoglobin of 7 at 80% saturation. In this comparison, the more cyanotic patient is doing better with a higher oxygen content and oxygen delivery.
_
The hematocrit is the percentage of the blood that contains RBCs. The hematocrit is directly proportional to the hemoglobin concentration. The hematocrit (in percent) is roughly three times the hemoglobin concentration (in gm per dl). Chronically hypoxic patients can survive by raising their hematocrit as a compensation maneuver. Chronic hypoxia stimulates erythropoietin which stimulates RBC production raising the hematocrit. Thus, a patient with a hemoglobin of 12 (hematocrit 36) and an oxygen saturation of 100%, has the same oxygen content as a patient with an oxygen saturation of 80% and a hemoglobin of 15 (hematocrit 45). The former patient looks pink, while the latter patient looks blue.
_
Oxygen delivery:
The last factor is the oxygen delivery rate. This is determined by the oxygen content and the cardiac output. Conceptually, imagine a patient with a weak heart and only half the cardiac output of a normal patient with signs of congestive heart failure. If pulmonary edema were not present, and such a patient had an oxygen saturation of 100%, their hemoglobin would have to be twice as high as another patient with a normal cardiac output to achieve the same oxygen delivery rate. This might be better understood by measuring a patient’s venous blood gas. In room air, a normal arterial O2 saturation would be 100 %, and the venous O2 saturation would be about 75%. However, if a patient had a very low cardiac output, the arterial O2 saturation might still be 100%, but the venous O2 saturation might be 50%. This occurs because the cardiac output is so low, that much more oxygen is extracted from the RBCs as they pass through the capillaries. Mixed venous oxygen saturation (SvO2) is the percentage of oxygen bound to hemoglobin in blood returning to the right side of the heart. This reflects the amount of oxygen “left over” after the tissues remove what they need. It is used to help us to recognize when a patient’s body is extracting more oxygen than normally. An increase in extraction is the body’s way to meet tissue oxygen needs when the amount of oxygen reaching the tissues is less than needed.
________
Oxygen Haemoglobin dissociation curve:
The oxygen–hemoglobin dissociation curve plots the proportion of hemoglobin in its saturated form on the vertical axis against the prevailing oxygen tension on the horizontal axis. The oxyhemoglobin dissociation curve is an important tool for understanding how our blood carries and releases oxygen. Specifically, the oxyhemoglobin dissociation curve relates oxygen saturation (SaO2) and partial pressure of oxygen in the blood (PaO2), and is determined by what is called “Hemoglobin affinity for oxygen”; that is, how readily hemoglobin acquires and releases oxygen molecules into the fluid that surrounds it. The amount of oxygen dissolved in the blood is proportional to the partial pressure of oxygen. The amount of oxygen bound to hemoglobin will increase as the partial pressure of oxygen increases. But the amount of oxygen bound to hemoglobin does not increase in proportion to the partial pressure of oxygen. The increase may be indicated by an S-shaped curve as shown in the figure below. This is called the oxygen dissociation curve. The oxygen dissociation curve is called the “standard oxygen dissociation curve” in which the body temperature is 37°C, pH 7.4. The curve may shift to the right or left, depending on patient conditions. If the body temperature decreases and pH increases, the curve will shift to the left. If the temperature increases and pH decreases, the curve will shift to the right.
_
__
At high partial pressures of oxygen, haemoglobin binds to oxygen to form oxyhaemoglobin. When the blood is fully saturated, all the red blood cells are in the form of oxyhaemoglobin. As the red blood cells travel to tissues deprived of oxygen the partial pressure of oxygen will decrease. Consequently, the oxyhaemoglobin releases the oxygen to form haemoglobin. The sigmoid shape of the oxygen dissociation curve is a result of the co-operative binding of oxygen to the four polypeptide chains. Co-operative binding is the characteristic of a haemoglobin to have a greater ability to bind oxygen after a subunit has bound oxygen. Thus, haemoglobin is most attracted to oxygen when three of the four polypeptide chains are bound to oxygen.
_
The hemoglobin tetramer can bind up to four molecules of oxygen in the iron-containing sites of the heme molecules. As oxygen is bound, 2,3-BPG and CO2 are expelled. Salt bridges are broken, and each of the globin molecules changes its conformation to facilitate oxygen binding. Oxygen release to the tissues is the reverse process, salt bridges being formed and 2,3-BPG and CO2 bound. Deoxyhemoglobin does not bind oxygen efficiently until the cell returns to conditions of higher pH, the most important modulator of O2 affinity (Bohr effect). When a tissue is more active, the amount of carbon dioxide produced will be increased (PCO2 is higher). Carbon dioxide reacts with water as shown in the following equation:
CO2+ H2O <—-> H+ + HCO–3
What this means is that as the amount of carbon dioxide increases, more H+ are formed and the pH will decrease. Thus, a lower pH in the blood is suggestive of an increased carbon dioxide concentration which in turn is suggestive of a more active tissue that requires more oxygen. According to Bohr, the lower pH will cause Hb to deliver more oxygen! The high content of carbon dioxide in venous capillary blood reduces the affinity of haemoglobin for oxygen leading to release of oxygen to the tissues. The oxygen dissociation curve shifts to the right (Bohr effect).
_
The partial pressure of oxygen dissolved in the plasma is measured as the PaO2. The oxygen dissociation curve shows the relation between SaO2 and PaO2. An SaO2 greater than 95% correlates to the normal range of PaO2, which is 80 to 100 mm Hg. A PaO2 of 60 mm Hg or less correlates to a SaO2 of less than 90% per the dissociation curve. Changes in temperature and pH cause a shift in this relation. As pH increases (alkalosis) or temperature decreases (hypothermia), the shift is to the left as hemoglobin binds more tightly with oxygen delaying its release to tissues. Acidosis (low pH) and fever shift the curve to the right, as the hemoglobin molecule loosens its affinity for oxygen, making it easier for oxygen to be released to the tissues.
_
| mm Hg | O2 saturation | |
| 27 | 50 % | This is the partial pressure of O2 with 50% saturation. |
| 40 | 75 % | This is the partial pressure of O2 in venous blood (PvO2). |
| 60 | 90 % | Sats < 90% are entering the steep part of the curve. |
| 100 | 98 % | This is the partial pressure of O2 in arterial blood (PaO2). |
_
When oxygen saturation is measured in arterial blood (SpO2/SaO2):
97% saturation = 97 PaO2 (normal)
90% saturation = 60 PaO2 (danger)
80% saturation = 45 PaO2 (severe hypoxia)
___________
___________
Clinical signs of hypoxemia:
Signs and symptoms of hypoxemia:
a. restlessness
b. altered or deteriorating mental status
c. increased pulse rate
d. increased or decreased respiratory rate
e. cyanosis (late sign)
_
What is obvious breathing?
Normal breathing at rest is simply not obvious; one has to look very closely for chest movement to appreciate breathing. If a patient’s breathing is obvious on initial contact (for example, when you first see the patient on walking into the room) it is abnormal. Six signs that may make someone’s breathing obvious to the observer – all abnormal – are:
• flaring of nostrils with breathing
• tachypnea (generally, to be obvious, respiratory rate is > 24 breaths/min)
• noisy breathing (wheezing, stridor, moaning, etc.)
• use of accessory breathing muscles (neck muscles, intercostal muscles, etc.)
• pursed lip breathing (often seen in severe COPD)
• Cheyne-Stokes breathing (alternating periods of apnea with tachypnea; apnea periods may last up to 30 seconds)
_
Fallibility of clinical signs of hypoxia:
Many studies have examined the use of simple clinical signs in assessing cardiopulmonary status in infants and children. In general these studies have shown that cardiorespiratory disease is frequently present when these signs are manifest, but of equal importance, the studies indicate the many children who have significant cardiorespiratory disease have none of these signs. Data from physiologic studies indicate that mild to moderate hypoxia produces at most a modest and temporary increase in ventilation. Transient hyperventilation is rapidly followed by a return to normal ventilatory levels. This biphasic response is a result of the way ventilation is controlled by the brainstem. Moderate hypoxia initially stimulates peripheral receptors to increase ventilation; however, the increase in ventilation produces a decrease in the PaCO2, an even more potent modulator of ventilation. In response to the decrease in the PaCO2, and because of a direct central depressive effect of hypoxia, the brainstem down-regulates the respiratory drive and returns ventilation back to baseline levels. Thus, most healthy individuals exposed to moderate hypoxia will not have a significant increase in their ventilation. Decreasing arterial oxygen pressure to less than 40 to 50 mm Hg produces a sustained increase in ventilation as the respiratory stimulation produced by hypoxia exceeds the inhibition generated by decreasing carbon dioxide levels. It is important to note, however, that most of the initial increase in ventilation is accomplished by augmenting tidal volume and peak flows while keeping respiratory rate constant. An increased respiratory rate occurs as a late response to severe hypoxemia. These physiologic findings suggest that in the clinical setting, respiratory rate should not be a sensitive indicator of arterial oxygen levels and cardiorespiratory status. One study confirms this concept. Only 48% of the children with SpO2 values of less than 90% had respiratory rate elevations above the 80th percentile for their age, and less than one third had rates in the upper 5th percentile for their age. The majority of the moderately hypoxic children in this study had respiratory rates that were indistinguishable from those of other children in the study. The fact that hypoxia may not be accompanied by an increased ventilatory drive may explain many of this study findings. In particular, this study demonstrates that after receiving triage pulse oximetry values, physicians were significantly more likely to change the treatment of children with SpO2 values of less than 95% compared with those having saturation values of 95% or greater. This is likely because of the difficulty physicians have in detecting cardiopulmonary and gas exchange abnormalities in patients who did not have evidence of respiratory distress. Without some sign of respiratory compromise, clinicians may often underestimate cardiorespiratory and gas exchange difficulties. Patients with pulmonary diseases such as viral respiratory tract infections, pneumonia, asthma, and bronchitis were most likely to have abnormal pulse oximetry values and were also most likely to have their medical treatment changed. This suggests that there were two reasons that pulse oximetry altered medical treatment: physicians either failed to appreciate subtle cardiopulmonary problems, or they did not recognize the severity of the illnesses they had diagnosed. Routine pulse oximetry measurements often alerted physicians to these problems by revealing SpO2 difficulties.
_
Respiratory rate vs. SpO2:
Respiratory rate measurements are notoriously sensitive to measurement techniques and are often assessed inaccurately. Even if the respiratory rate is accurately measured, it is found that respiratory rates correlated poorly with SpO2 levels and that clinicians often changed their medical treatment after receiving pulse oximetry measurements. This confirms the findings of many investigators and demonstrates the inadequacy of the respiratory rate alone in screening for significant cardiopulmonary disease and gas exchange abnormalities.
_
Hypoxemia is an important and potentially avoidable cause of morbidity and mortality in many hospital settings, including the intensive care unit (ICU), emergency department, procedure suite, and operating room. Rapid, accurate detection of hypoxemia is critical to prevent serious complications; however, oxygenation is difficult to assess on the basis of physical examination alone. The human eye is poor at detecting hypoxaemia. The traditional sign is cyanosis, which is defined as a concentration of more than 5 g/100 ml of reduced haemoglobin in capillary blood and depends on arterial oxygenation, skin perfusion, and haemoglobin content. The presence of central cyanosis, a blue coloration of the tongue and mucous membranes, is thought to be a more reliable indicator of hypoxaemia as these tissues are less likely to be poorly perfused. This definition translates to an oxyhaemoglobin saturation of about 75% with normal perfusion, which is clinically important hypoxaemia. The ability to detect cyanosis depends on the experience and eyesight of the observer, the colour balance of the ambient lighting, and the skin pigmentation of the subject. Places where hypoxaemia may be expected (operating theatres, accident departments, endoscopy suites) should have lighting with blue coloration (“northern daylight”) to facilitate detection. Several studies-the earliest was by Comroe and Bothelo in 1947 have shown that even under ideal conditions skilled observers cannot detect hypoxaemia until the oxyhaemoglobin saturation is under 80%. The pulse oximeter thus extends our clinical senses rather than replacing them. Because desaturation is detected earlier by pulse oximetry than by clinical observation, the use of pulse oximetry is recommended for any patient at risk for hypoxemia. Blood gas analysis was for many years the only available method of detecting hypoxemia in critically ill patients, but this technique is painful, has potential complications, and does not provide immediate or continuous data. Pulse oximetry allows noninvasive measurement of arterial hemoglobin saturation, without the risks associated with arterial puncture. Over the past 30 years, pulse oximetry has become the standard for continuous and/or noninvasive assessment of arterial oxygen saturation. Arterial oxygen saturation determination with pulse oximetry is now in such ubiquitous use that it has been called the “fifth vital sign”. Hypoxemia can be present before recognizable signs of respiratory distress-tachycardia, tachypnea, cyanosis, agitation, and lethargy-appear. But it wasn’t until the early 1980s that technology allowed for the easy and noninvasive measurement of arterial oxygen saturation. Initially used during surgery to prevent accidental death by oxygen desaturation, pulse oximeters are now found in nearly all settings, from EDs and ICUs to general units, and even in home care. The results of bedside pulse oximetry are at the heart of a wide range of clinical practice guidelines for patient care from the neonatal diagnosis of congenital heart disease to the management of chronic obstructive pulmonary disease and emergency oxygen therapy. Despite the widespread use of pulse oximetry in clinical monitoring, many practitioners are unaware of the potential limitations of this technology.
__
The difficulty that physicians have in detecting hypoxemia was recently exemplified in a study of over 14000 patients being evaluated at the UCLA Emergency Department. Patients were monitored by oximetry but recordings were given to physicians only after they completed their initial assessment. Changes in diagnostic testing and treatment were most likely at an O2 saturation of 89%, and changes were actually less common at lower saturations, probably because the physicians were able to detect evidence of hypoxemia without requiring a pulse oximeter. With the proliferation of pulse oximeters in different locations of the hospital throughout the 1980s, several investigators demonstrated that episodic hypoxemia is much more common than previously suspected with an incidence ranging from 20–82%. The significance of episodic desaturation on patient outcome is largely unknown. In patients admitted to a general medical service, Bowton et al. found that O2 saturation <90% of at least 5 min duration occurred in 26% of the patients. On follow-up over the next 4–7 months, those patients experiencing hypoxemia during the first 24 h of hospitalization had more than a threefold higher mortality than patients who did not desaturate. Although episodic desaturation may simply be a marker of increased risk rather than the direct cause of decreased survival, an increased mortality rate was still observed in patients with episodic hypoxemia when the investigators corrected for severity of illness. Whether or not the early detection and treatment of episodic hypoxemia can affect patient outcome remains unknown.
_________
Methods for measuring oxygen saturation level:
Pulse Oximeter:
A pulse oximeter is a device intended for the non-invasive measurement of arterial blood oxygen saturation and pulse rate. Typically it uses two LEDs (light-emitting diodes) generating red and infrared lights through a translucent part of the body. Bone, tissue, pigmentation, and venous vessels normally absorb a constant amount of light over time. Oxy-hemoglobin and its deoxygenated form have significantly different absorption pattern. The arteriolar bed normally pulsates and absorbs variable amounts of light during systole and diastole, as blood volume increases and decreases. The ratio of light absorbed at systole and diastole is translated into an oxygen saturation measurement. Pulse oximeter is discussed in detail later on in the article. Pulse oximetry will not measure the oxygen saturation correctly for other hemoglobins such as methemoglobin or carboxyhemoglobin. However, for sickle hemoglobin or fetal hemoglobin, the measurement is nearly as accurate as for hemoglobin A.
_
Co-oximeter:
Pulse oximeters estimate oxygen saturation by comparing the absorbance of light at two wavelengths. Infrared light is absorbed by oxyhemoglobin, whereas red light is absorbed by deoxyhemoglobin. The absorbance characteristics of methemoglobin are similar to those of oxyhemoglobin, falsely elevating pulse-oximeter readings. Co-oximeters measure light absorbance at four or more discrete wavelengths, providing accurate measurement of oxygen saturation, methemoglobin, and carboxyhemoglobin. Co-oximeter is a device that measures the oxygen carrying state of hemoglobin in a blood specimen. Co-oximetry is useful in defining the causes for hypoxemia, hypoxia, or oxygen deficiency at the tissue level. The test is done with a device that measures absorption at several wavelengths to distinguish oxyhemoglobin from carboxyhemoglobin and determine the oxyhemoglobin saturation: the percentage of oxygenated hemoglobin compared to the total amount of hemoglobin, including carboxyhemoglobin (COHb), methemoglobin (metHb), oxyhemoglobin (O2Hb), and reduced hemoglobin (Hb). When a patient presents with carbon monoxide poisoning (CO), the Co-oximeter will detect the levels of each hemoglobin and will report the oxyhemoglobin saturation as markedly reduced. Traditionally, this measurement is made from arterial blood processed in a blood gas analyzer with a Co-oximeter. More recently, pulse Co-oximeters have made it possible to estimate carboxyhemoglobin with non-invasive technology similar to a pulse oximeter [vide infra]. In contrast, the use of a standard pulse oximeter is not effective in the diagnosis of CO poisoning as patients suffering from carbon monoxide poisoning may have a normal oxygen saturation reading on a pulse oximeter.
_
_
Oxygen saturation is measured by co-oximetry but this requires a blood sample. Co-oximetry is capable of determining the true oxygen saturation for methemoglobin and carboxyhemoglobin. If the true oxygen saturation is known, then the PO2 can be estimated or calculated using the oxygen hemoglobin dissociation curve assuming that the patient is circulating hemoglobin A (which is not always the case).
_
Arterial blood gas (ABG) analysis:
This is a blood test using samples extracted from an artery. The test determines the pH of the blood, the partial pressure of carbon dioxide and oxygen, and the bicarbonate level. Many blood gas analyzers will also report concentrations of lactate, hemoglobin, several electrolytes, oxy-hemoglobin, carboxyhemoglobin and methemoglobin. The arterial blood gas analysis determines gas exchange levels in the blood related to lung function.
_
_
An arterial blood gas (ABG) measures three components: pH, PCO2, PO2. All the other numbers on a blood gas are calculated. The bicarbonate (HCO3) value is calculated based on the measured pH and the measured PCO2, using the Henderson-Hasselbalch equation. The base excess (BE) is calculated using a similar equation. The oxygen saturation is calculated based on the assumption that normal adult hemoglobin (HbA) is the dominant hemoglobin in the sample (using the oxygen hemoglobin dissociation curve). How do venous and capillary blood gasses differ from an arterial blood gas? Looking at the three blood gas measurements: 1) The venous bicarb and the arterial bicarb are roughly the same. 2) The venous PCO2 is slightly higher than the arterial PCO2 because additional CO2 is picked up from the tissues, but the difference between the two is rather small. 3) The venous PO2 is substantially lower than the arterial PO2. Since only the PCO2 and the bicarb contribute to the pH, the venous pH and the arterial pH are roughly the same. A venous or a capillary blood gas very closely approximates the arterial pH, PCO2 and bicarb (or BE), under ideal conditions with well perfused tissues, but they do not approximate the arterial PO2. All that can be said about a venous PO2 is that it is lower than the arterial PO2. All that can be said about a capillary PO2 is that it lies somewhere between the venous PO2 and the arterial PO2. Fortunately, pulse oximetry accurately reflects the arterial PO2. Therefore, a venous blood gas or capillary blood gas done in conjunction with a pulse oximeter measurement, should accurately reflect the arterial blood gas as long as the capillary source is well perfused. Often, no blood gas is needed at all. The bicarb value can be obtained by ordering a standard set of electrolytes, the PO2 can be accurately estimated using a pulse oximeter, and the PCO2 can be clinically estimated using auscultation by listening for the degree of air exchange or by capnography.
_
The means used to determine oxygen saturation vary. Oxygen saturation is a percentage value indicating the amount of hemoglobin that is saturated with oxygen.
There are three different ways to determine oxygen saturation.
They are the fractional oxygen saturation, the function oxygen saturation, and the calculated oxygen saturation measurements.
1. The first method of determining oxygen saturation is by measuring the O2Hb and comparing it to all the hemoglobin measured. This method is common for fractional oxygen saturation measurements (FO2Hb) from co-oximetry. The equation for which is: FO2Hb = [O2Hb /tHb] x 100
2. The second method of determining oxygen saturation is by measuring the O2Hb and comparing it to O2Hb + deoxyHb. This is referred to as functional hemoglobin saturation and can be determined by using co-oximetry as well as pulse oximetry. This allows clinicians to assess how much of the hemoglobin capable of carrying oxygen is actually saturated with oxygen molecules. The equation for this measurement is: SaO2= 100 X O2Hb / [O2Hb + deoxyHb].
3. The third method of determining oxygen saturations is by calculating the oxygen saturation (ScO2) using an equation or algorithm using a measured PO2, pH, PCO2, and a calculated/ default hemoglobin. The challenge with the calculated oxygen saturation is that clinicians must often assume normal hemoglobin values in their critically ill patients that receive a blood gas and that there are no other inhibitors such as MetHb or COHb.
_
When comparing the above three different means of obtaining the oxygen saturation measurement, only O2Hb and SaO2 measured by co-oximeter provides direct measurement information to assess the oxygenation of hemoglobin. The use of ScO2 (calculated oxygen saturation) restricts’ the clinician’s ability to make a true determination of a patient’s oxygenation status by only assessing the oxygenation of the blood plasma and often assuming normal or default hemoglobin values in a patient. Therefore, in order to make an accurate assessment of a patient’s oxygenation statues, the PO2 measurement is needed in conjunction with the O2Hb measurement from a co-oximeter. Understanding the intent of an ABG is to measure both the acid-base balance and the oxygenation of a patient is fairly simple. However it is important for clinicians to understand the need to measure both the PO2 and O2Hb (by co-oximetry) in order to perform an accurate patient assessment of oxygenation. Once clinicians understand the need for co-oximetry with all ABG tests, the accuracy of a patient’s oxygenation will be assured.
_
________
________
Other technologies that measure blood oxygen saturation:
Near-infrared spectroscopy (NIRS):
Near-infrared spectroscopy (NIRS) is a non-invasive technique for measuring blood oxygen saturation that may be more accurate and sensitive than pulse oximetry, especially in areas of prime interest such as cerebral tissue. NIRS is based on the light absorption characteristics of oxygenated and deoxygenated hemoglobin and provides a continuous measure of regional O2 saturation in a tissue field containing both venous and arterial blood. NIRS employs two photo-detectors adjacent to a single light source to measure light reflected by perfused tissue. The depth at which reflected light penetrates tissue is a function of the source-sensor distance that measures a shallow signal and a deep signal and subtracts commonalities without interference from the skin, skull, or subcutaneous tissue. The NIRS technique reduces placement constraints and affords greater subject mobility than finger-mounted pulse oximeters. The central position of NIRS sensors allows measurement of cerebral oxygenation, which is highly sensitive to acute changes in air oxygen content. NIRS readings are independent of arterial pulse and in-house research has confirmed that NIRS is faster in reaching oxygen saturation benchmarks compared to a finger pulse oximeter. Although promising, research identified some drawbacks when using the NIRS (INVOS 5100C) sensor to detect varying levels of hypoxia exposure. Approximately 10% of subjects had baseline readings near or below the manufacturer recommended cut off (50%) for reliable readings. For subjects with low baselines, a large bias tended to exist between NIRS (normalized) and finger oximeter readings during minimum saturation plateaus, calling into question NIRS accuracy. The end result could be unacceptably high rates of false alarms for these individuals. Also, sensitivity to the placement of the sensors caused a fairly high degree of variation in daily baseline readings within individuals, such that baseline would likely need to be established prior to every flight. The baseline process takes approximately 10 minutes to complete which may be difficult to obtain during pre-flight procedures. Furthermore, similar to pulse oximetry NIRS is sensitive to G-induced drops in SPO2 which may make it difficult to determine whether a desaturation event is the product of stagnant or hypoxic hypoxia.
_
NIRS tissue oxygenation compared to pulse oximetry in critically ill patients: 2007 study:
Tissue oxygen monitoring based on the principle of Near Infrared Spectroscopy (NIRS) is a more sensitive non-invasive measure of oxygenation compared to conventional pulse oximetry. In septic patients undergoing vasopressor therapy, continuous measurement of blood oxygenation by pulse oximetry becomes erroneous and unreliable. Tissue oxygen saturation measurement is a superior way to continuously monitor the patient’s clinical status and guide therapeutic decisions.
_
Cerebral oximeter:
Cerebral oximetry is a non-invasive optical technology that measures cerebral cortex blood hemoglobin-oxygen saturation. Cerebral oximetry estimates the oxygenation of regional tissue by transcutaneous measurement of cerebral cortex using NIRS.
_
Occlusion spectroscopy technology:
OrSense’s NBM200 is based on the company’s proprietary SpectOLight technology, which uses an optical measurement platform combined with a ring-shaped sensor that is fitted on the subject’s finger. A gentle pressure is applied by the sensor, temporarily occluding the blood flow in the finger. New blood dynamics are created, generating a unique, strong optical transmission signal, with a high signal-to-noise ratio which is wholly blood specific. During the occlusion, optical elements in the sensor perform a sensitive measurement of the light transmitted through the finger. This method, called Occlusion Spectroscopy, provides a quick, accurate and painless measurement of the subject’s blood constituents. The NBM 200MP system utilizes OrSense’s proprietary SpectOLightTM occlusion spectroscopy technology, a novel and improved method for measuring hemoglobin oxygen saturation. The system offers non-invasive, continuous and accurate measurement of oxygen saturation in states of hypovolemia, hypothermia and vasoconstriction, as well as during regular perfusion. In addition to oxygen saturation, the system provides Hemoglobin (Hb) values. The NBM 200MP’s superior performance was validated by multi-center trials in the United States and Europe.
_______
_______
Vital signs:
Vital signs (often shortened to just vitals) are used to measure the body’s basic functions. These measurements are taken to help assess the general physical health of a person, give clues to possible diseases, and show progress toward recovery. The normal ranges for a person’s vital signs vary with age, weight, gender, and overall health. There are four primary vital signs: body temperature, blood pressure, pulse (heart rate), and breathing rate (respiratory rate). However, depending on the clinical setting these may include other measurements called the “fifth vital sign” or “sixth vital sign”. The fifth vital sign, pulse oximetry, routinely is used in every emergency department (ED) throughout the world. It is used to determine the baseline oxygenation of a patient in respiratory distress, to assess a patient’s response to therapeutic decisions, and to monitor a child during a conscious sedation or resuscitation. It is important to understand how the device functions and the limitations of this routinely used technology. Understanding that pulse oximetry measures functional saturation will help the clinician understand the limitations of this technology in the setting of a carbon monoxide exposure. It is also very important clinically to understand the limits of pulse oximetry in the setting of high venous pressures (congestive heart failure) or anemia. Certain clinical factors, such as sickle cell anemia, do not affect pulse oximetry, and the results provide meaningful information. As with every diagnostic test that a clinician performs, the information obtained is useful only if it can be interpreted accurately and applied appropriately to the individual patient.
_
Pulse oximetry as a fifth paediatric vital sign: 1997 study:
The study included 2127 consecutive children presenting to triage at a university emergency department. Of 305 children having triage pulse oximetry values less than 95%, physicians ordered second oximetry for 49, additional chest radiography for 16, complete blood counts for 7, arterial blood gas measurements for 4, spirometry for 2, and ventilation-perfusion scans for 2. Physicians ordered 39 new therapies for 33 patients, including antibiotics for 15, supplemental oxygen for 11, and beta-agonists for 8. Five patients initially scheduled for hospital discharge were subsequently admitted. Physicians changed or added diagnoses in 25 patients. Using pulse oximetry as a routine fifth vital sign resulted in important changes in the treatment of a small proportion of paediatric patients.
_
Pulse oximetry as a fifth vital sign in emergency geriatric assessment: a1998 study:
The study included 1,963 consecutive adults aged > or = 65 years presenting to triage at a university ED. 397 (20.2%) geriatric patients had triage pulse oximetry values <95%. Physicians ordered repeat oximetry for 51 patients, additional chest radiography for 23, CBC for 16, ABGs for 15, spirometry for 5, and ventilation-perfusion scans for none. Physicians ordered 49 new therapies for 44 patients, including antibiotics for 14, supplemental O2 for 29, and beta-agonists for 6. Nine patients initially scheduled for ED release were subsequently admitted to the hospital. Physicians changed or added diagnoses for 27 patients. Using pulse oximetry as a routine fifth vital sign resulted in important changes in the diagnoses and treatments of a small proportion of emergency geriatric patients.
_____
_____
History of pulse oximetry:
Modern day pulse oximetry had its beginnings in avionics research. In the early days of high altitude flight, it was important to study the effects of cabin pressure on the oxygenation of blood in the circulatory system of pilots. In 1935, Karl Matthes, a German scientist, introduced the first ear oxygen saturation meter using 2 photo sensors and lights initially in the red and green wavelengths, subsequently changed to light in the red and infrared wavelengths. Several years later, a US scientist, Glenn Millikan, produced a lightweight portable ear oxygen meter for use in pilots. It was Millikan who coined the term oximeter to describe his device. The oximeter was first commercialized in the 1960s by Hewlett Packard (Palo Alto, California) who sold a $10,000 device for use in pulmonary and sleep laboratories. It was not until the early 1970s that 2 Japanese bioengineers, Takuo Aoyagi and Michio Kishi discovered that the transmission of the red and infrared frequencies of light through an earlobe showed variations corresponding with the pulsatile flow of arterial blood perfusing the tissue. They established that by measuring the pulsatile component of light transmission through living tissues they could eliminate the variable absorption of light by bone, skin, and venous circulation. They also discovered that the transmission of light in the red and infrared wavelengths could be used to calculate oxygen saturation in the arterial circulation of tissue being analyzed. The first pulse oximeters were manufactured in Japan in the late 1970s by Nihon Kohden and Minolta, but their clinical utility was unknown at the time. Following studies indicating that these devices could have widespread medical applications, pulse oximeters were commercialized in the United States in 1981 by Biox/Ohmeda (Ohmeda Medical; Boulder, Colorado) and by Nellcor (Covidien; Mansfield, Massachusetts) in 1983. The devices began to be used clinically, mostly by anaesthesiologists to monitor patients undergoing sedation and anesthesia. Over the next several years, accumulated data indicated that pulse oximeters could prevent 2000 to 10,000 anesthesia deaths each year from undetected hypoxemia. In 1986, the American Society of Anesthesiologists recommended that these devices be used to monitor patients undergoing anesthesia. Over the next decade, pulse oximetry spread from the operating room to the emergency department, and then came to be used routinely in medical offices. Prior to the introduction of pulse oximetry, a patient’s oxygenation could only be determined by arterial blood gas, a single-point measurement that takes several minutes for sample collection and processing by a laboratory. In the absence of oxygenation, damage to the brain starts within 5 minutes with brain death ensuing within another 10–15 minutes. The worldwide market for pulse oximetry is over a billion dollars. With the introduction of pulse oximetry, a non-invasive, continuous measure of patient’s oxygenation was possible, revolutionizing the practice of anesthesia and greatly improving patient safety. By 1987, the standard of care for the administration of a general anesthetic in the U.S. included pulse oximetry. From the operating room, the use of pulse oximetry rapidly spread throughout the hospital, first to the recovery room, and then into the various intensive care units. Pulse oximetry was of particular value in the neonatal unit where the patients do not thrive with inadequate oxygenation, but too much oxygen and fluctuations in oxygen concentration can lead to vision impairment or blindness from retinopathy of prematurity (ROP). Furthermore, obtaining an arterial blood gas from a neonatal patient is painful to the patient and a major cause of neonatal anemia. In 1995, Masimo introduced Signal Extraction Technology (SET) that could measure accurately during patient motion and low perfusion by separating the arterial signal from the venous and other signals. In 2011, an expert workgroup recommended newborn screening with pulse oximetry to increase the detection of critical congenital heart disease (CCHD). In 2011, the US Secretary of Health and Human Services added pulse oximetry to the recommended uniform screening panel. Before the evidence for screening using signal extraction technology, less than 1% of newborns in the United States were screened. Today, the Newborn Foundation has documented near universal screening in the United States and international screening is rapidly expanding.
_________
_________
Principles of pulse oximetry:
Pulse oximetry uses light to work out oxygen saturation. Light is emitted from light sources which goes across the pulse oximeter probe and reaches the light detector. If a finger is placed in between the light source and the light detector, the light will now have to pass through the finger to reach the detector. Part of the light will be absorbed by the finger and the part not absorbed reaches the light detector. The amount of light that is absorbed by the finger depends on many physical properties and these properties are used by the pulse oximeter to calculate the oxygen saturation. Under normal physiological conditions arterial blood is 97% saturated, while venous blood is 75% saturated. The difference in absorption spectra of O2Hb and deoxyHb is used for the measurement of arterial oxygen saturation because the wavelength range between 600 nm and 1000nm is also the range for which there is least attenuation of light by body tissues (tissue and pigmentation absorb blue, green and yellow light and water absorbs the longer infra-red wavelength).
_
The principle of pulse oximetry is based on two technologies: infrared spectroscopy and pulse plethysmography.
1. Infrared spectroscopy detects the absorption of light by various tissues at two different wavelengths, namely the visual red and the infrared spectrum.
2. Pulse plethysmography describes the change in light absorption due to the pulsatile variation in volume of arteries and the transformation into a pulse waveform.
_
_
The theory behind spectroscopy is described by the Beer-Lambert law, which states that the absorption of light by a tissue is proportional to the concentration of the tissue and the path length through that tissue. Therefore, the tissue to which the probe is applied has to be sufficiently thin and translucent. The diodes in the probe emit energy alternately at 660nm (visible red light spectrum) and 940nm (infrared light spectrum). The absorption of light at these wavelengths by Hb differs, depending on the degree of its oxygenation: reduced Hb absorbs more red light compared to oxyHb, which absorbs more infrared light. The photodetector measures the amount of light absorbed at each wavelength, from which the amount of oxyHb and deoxyHb is calculated by a microprocessor and displayed on the monitor.
_
_
Modern pulse oximetry was born with the realization that pulsatile changes in light transmission through living tissues are due to alteration of the arterial blood volume in the tissue. Measurement of the pulsatile component would eliminate the variable absorption of light by bone, tissue, skin, pigment, etc from analysis. The most important premise of pulse oximetry therefore, is that the only pulsatile absorbance between the light source and the photo detector is that of arterial blood. Two wavelengths of light are used; 660 nanometers (red) and 940 nanometres (near infrared). At 660nm, reduced hemoglobin absorbs about ten times as much light as oxyhemoglobin. At the infrared wavelength, (940nm), the absorption coefficient of oxyhemoglobin is greater than that of reduced hemoglobin. The pulse oximeter directly senses the absorption of red and infra-red light, and the ratio of pulsatile to nonpulsatile light at the red and infrared wavelengths are translated through complex signal processing to a function of the arterial oxygen saturation. A microprocessor integrates the data, and through an elaborate calibration algorithm based on human volunteer data, the oxygen saturation can be estimated.
_
Physics of pulse oximetry:
Pulse oximetry depends on spectral analysis for measurement of oxygen saturation; i.e. the detection and quantification of components in solution by their unique light absorption characteristics. The pulse oximeter combines the two technologies of spectrophotometry (which measures haemoglobin oxygen saturation) and optical plethysmography (which measures pulsatile changes in arterial blood volume at the sensor site). Detection of oxygen saturation of hemoglobin by spectrophotometry is based on Beer-Lambert law. This is a combination of two laws describing absorption of monochromatic light by a transparent substance through which it passes:
Beer’s law: the intensity of transmitted light decreases exponentially as the concentration of the substance increases. August Beer, German Physicist (1825-1863)
Lambert’s law: the intensity of transmitted light decreases exponentially as the distance travelled through the substance increases. Johann Lambert, German Physicist (1728-1777).
_
Oxyhemoglobin absorbs more light in the infrared spectrum (850 to 1000 nm) whereas deoxyemoglobin absorbs more light in the red spectrum (600 to 750 nm). The pulse oximeter has two light emitting diodes (LED) of different wavelengths, one red and the other infrared. Typically the red LED has a wavelength of 660 nm and the infrared a wavelength of 940 nm. The LEDs are pulsed on and off hundreds of times per second and a photodetector collects the red and infrared light that passes through the tissue the pulse oximeter is placed on. A ratio of red to infrared light absorption is developed and applied to an internal algorithm in the pulse oximeters software. A number is then displayed on the readout. Newer pulse oximeters can compensate for extraneous light and the rapid sampling rate allows for detection of pulsatile blood flow which is assumed to be arterial. In clinical practice, a pulse oximeter is a non-invasive estimate of SpO2. This in turn can be used to estimate a patient PaO2 using the oxyhemoglobin dissociation curve.
_
The light absorbed by non-pulsatile tissues is constant (DC). The non-constant absorption (AC) is the result of pulsatile blood pulsations. The photo detector generates a voltage proportional to the transmitted light. The AC component of the wave accounts for between 1-5% of the total signal. The high frequency of the diodes allows the absorption to be calculated many times per second. This reduces movement effects on the signal. The microprocessor analyses both the DC and AC components at 660 nm and 940 nm. The absorption of oxyhaemoglobin and deoxyhaemoglobin at these two wavelengths is very different. Hence, these two wavelengths provide good sensitivity.
_
The figure above shows a schematic representation of the layers of human tissues that absorb light energy at the measuring site and the components of light absorption (constant—DC and variable—AC) by distinct tissue characteristics. The pulse oximeter is able to differentiate between the absorption of light in the pulsatile (AC – alternating current) and the non-pulsatile (DC – direct current) flow under the probe. The AC component is derived from arterial blood pulsation, whereas the DC component is derived from all other static tissues, where the majority of total absorption occurs. The photodetector records the light transmitted through both pulsatile and non-pulsatile tissues. The AC component, the signal of interest, represents only up to two per cent of the total absorption (Magee, 2005). This explains how even small interferences, such as movement or vasoconstriction, may have a considerable impact on its accuracy. The difference in light absorption depends on variation in the amount of blood flowing underneath the probe, the erythrocyte concentration, local blood velocity and the distance between the light source and the detector.
_
Isobestic point:
This is the point at which two substances absorb a certain wavelength of light to the same extent. In oximetry, the isobestic points of oxyhaemoglobin and deoxyhaemoglobin occur at 590 nm and 805 nm. These points may be used as reference points where light absorption is independent of the degree of saturation. Some earlier oximeters corrected for haemoglobin concentration using the wavelength at the isobestic points. Thus comparison of absorbencies at different wavelengths allows estimation of the relative concentrations of O2Hb and deoxyHb (i.e. saturation). Modern pulse oximeters may use two or more wavelengths, not necessarily including an isobestic point.
_
Currently available pulse oximeters are equipped with 2 light-emitting diodes (LEDs), 1 emitting at the red spectrum and the other at the infrared spectrum, most commonly at wavelengths of 660 and 940 nm, respectively. Emission of these 2 wavelengths alternates at frequencies of 0.6 to 1.0 kHz, and the nonabsorbed energy is detected by a semiconductor. A microprocessor subtracts the absorption by constant absorbers, thus rendering the final signal, which is displayed electronically as a plethysmographic wave form. The SpO2 is calculated from the conversion of the ratio of absorption ratios by using dedicated calibration algorithms stored in the microprocessor of the device. These algorithms are derived through SaO2 measurements in healthy volunteers breathing mixtures of decreased oxygen concentrations and are usually unique for each manufacturer.
_
The pulse oximeter readings lag behind the patient’s condition because there is a response delay as a result of signal averaging in the monitor. The length of signal averaging can be set on some machines for 4, 8, or 16 seconds, with most oximeters having a common default setting of 8 seconds. This means there is an interval after the actual arterial blood oxygen saturation starts to fall before it is detected by oximetry because the signal is averaged over several seconds. The PaO2 could potentially decrease to a critical level before the decreased SpO2 is displayed by the oximeter. The clinician needs to be aware of this time delay between a potentially hypoxic event such as a respiratory obstruction and the pulse oximeter registering a low oxygen saturation.
_
Calibration Adjustment:
Earlier I discussed how the pulse oximeter uses Beer’s and Lambert’s Law (absorbance depends on concentration and path length) as part of its factors that it uses to compute oxygen saturation. Unfortunately, there is a problem. In physics, the Beer and Lambert law have very strict criteria to be accurate. For an example, the light that goes through the sample should go straight through. However, in real life, this does not happen. Blood is not a neat red liquid. Instead, it is full of various irregular objects such as red cells etc. This makes the light scatter, instead of going in a straight line. Therefore Beer and Lamberts Law cannot be applied strictly. Because Beer and Lamberts law cannot be applied strictly, there would be errors if they were used to directly calculate oxygen saturation. A solution to this is to use a “calibration graph” to correct for errors. A test pulse oximeter is first calibrated using human volunteers. The test pulse oximeter is attached to the volunteer and then the volunteer is asked to breathe lower and lower oxygen concentrations. At intervals, arterial blood samples are taken. As the volunteers’ blood desaturates, direct measurements made on the arterial blood are compared simultaneously with the readings shown by the test pulse oximeter. In this way, the errors due to the inability of applying Beers and Lamberts law strictly are noted and a correction calibration graph is made. However, in order to not harm the volunteers, the oxygen saturation is not allowed to drop below about 75 – 80 %. A copy of this correction calibration graph is available inside the pulse oximeters in clinical use. When doing its calculations, the computer refers to the calibration graph and corrects the final reading displayed. As mentioned before, the volunteer studies described before do not allow the saturation to go below about 75 – 80 %. For saturations below this, the calibration curve is mathematically estimated .Therefore; pulse oximeters are typically less accurate below saturations of about 75 – 80 %.
_
The pulse oximeter uses empirical calibration curves developed from studies of healthy volunteers to calculate SpO2. Pulse oximeters use two light emitting diodes (LEDs) of specific and differing wavelength (typically 660 and 940 nm) to measure the combined absorption by a mixture of oxyhaemoglobin and deoxyhaemoglobin of red and infrared light measured using a photodiode. The photodiode measures the variation in the intensity of light falling upon it, and converts this into an electrical voltage. The ratio of the absorption at these two wavelengths is called the R value, and is compared with R values that are calibrated against direct measurements of arterial oxyhaemoglobin saturation (SaO2) and arterial partial pressure of oxygen (PaO2) for an individual model of pulse oximeter, using a volunteer population sample. Volunteers breathe controlled hypoxic gas mixtures to create a range of SaO2 values between 70% and 100% against which the SPO2 of an individual pulse oximeter sensor may be calibrated. Pulse oximeters cannot determine the concentrations of oxyhemoglobin or deoxyhemoglobin; they provide an estimate of SaO2 rather than a direct measurement. For each of the two wavelengths of light used in pulse oximeters, a ratio of the relative absorbance of oxyhemoglobin and deoxyhemoglobin is calculated. This ratio is empirically related to SaO2, as measured in experimental studies in human volunteers. Since it is unethical to induce a degree of oxygen saturation below 70% in volunteers, pulse oximeter readings of approximately 70% represent the lowest limit of accurate output. It is recommended that readings lower than approximately 70% should be regarded as inaccurate since they represent extrapolation of the empirical data. Thus, pulse oximeters do not measure SaO2 but provide estimates. The accuracy of commercially available oximeters differs widely, probably due to the algorithm differences in signal processing.
_
The pulse amplitudes (Vpp) of the red and infrared (IR) signals are measured and converted to Vrms, in order to produce a ratio value: Ratio = (Red_AC_Vrms/Red_DC) / (IR_AC_Vrms/IR_DC). The SpO2 can be determined using the ratio value and a look-up table that is made up of empirical formulas. The pulse rate can be calculated based on the pulse oximeter’s Analog-to-Digital Converter (ADC) sample number and sampling rate. A look-up table is an important part of a pulse oximeter. Look-up tables are specific to a particular oximeter design and are usually based on calibration curves derived from, among other things, a high number of measurements from subjects with various SpO2 levels. Figure below shows an example of a calibration curve.
_
The performance of each device is strictly related to the reliability and complexity of the algorithms used in signal processing and to the speed and quality of the microprocessor. There are numerous studies of the accuracy and precision of pulse oximeters in various adult and paediatric populations. Most manufacturers claim mean differences (bias) of ≤2% with SDs (precision) of ≤4%. It should be noted, however, that these results have been reported in subjects with SaO2 levels that exceed 80%; the performance of pulse oximeters deteriorates remarkably when SaO2 decreases to <80%. 95% confidence limit for Pulse Oximetry is +/- 4% at SpO2 >70% (the error is higher at SpO2 <70%). Correlation coefficients between pulse oximetry and direct blood oxygen saturation measurements are excellent, ranging from 0.77–0.99 when oxygen saturation is >70%.
_____
Accounting for ambient (room) light:
The pulse oximeter probe has a red LED and one infrared LED. On the other side, is a light detector. However, you will note that, though there are only two LEDs, the light detector is exposed to three sources of light. In addition to the red and infrared LED light sources, there is also light in the room (ambient light) that the pulse oximeter is working in. Some of this room light can also reach the detector. The pulse oximeter has to work with these three sources of light. It wants the red and infrared light to calculate oxygen saturation. On the other hand, the room light is unwanted “noise”, and needs to be taken account of. In reality, both LEDs are never lit together. Instead, the pulse oximeter rapidly switches the LED’s on and off in a particular sequence. First, the pulse oximeter activates the red LED light. The red light goes through the finger and reaches the detector. Stray room light also reaches the detector. The detector therefore records red light and room light that falls on it. Next, the pulse oximeter switches off the red LED light and switches on the infrared LED light. The infrared light goes through the finger and reaches the detector. Stray room light also reaches the detector. The detector therefore records infrared light and room light that falls on it. Finally the pulse oximeter switches off both the red and infrared LED lights. Now the only light that falls on the detector is the room light. The pulse oximeter now records the room light level. Because the pulse oximeter now knows the level of room light, it is able to subtract it from the readings to get the actual red and infrared light levels.
________
Pulse plethysmography:
Plethysmographic trace (Pleth):
Pulse oximeters often show the pulsatile change in absorbance in a graphical form. This is called the “plethysmographic trace ” or more conveniently, as “pleth”. The pleth is an extremely important graph to see. It tells you how good the pulsatile signal is. If the quality of the pulsatile signal is poor, then the calculation of the oxygen saturation may be wrong. The pulse oximeter uses very complicated calculations to work out oxygen saturation. A poor pleth tracing can easily fool the computer into wrongly calculating the oxygen saturation. As human beings, we like to believe what is good, so when we see a nice saturation like 99 %, we tend to believe it, when actually the patient’s actual saturation may be much lower. So always look at pleth first, before looking at oxygen saturation. The pleth is affected by factors that affect the peripheral blood flow. For an example, low blood pressure or peripheral cold temperature can reduce it. Sophisticated uses of the pleth are being developed. For example, it may be used to guide fluid therapy. Most pulse oximeters display oxygen saturation, heart rate and a plethysmographic trace. The most important function of the plethysmogram is to provide information regarding whether the pulse oximeter is working correctly. Readings displayed are only accurate and, therefore, reliable if this trace resembles an arterial pressure waveform and if the pulse rate displayed equals the actual patient’s pulse rate. The plethysmogram is also useful as an indicator of cardiac rhythm, as arrhythmias may result in changes in its regularity. Changes in cardiac output may be assessed by a change in amplitude of the trace and the area under the curve.
_
When properly attached, the ideal plethysmograph waveform shows a dicrotic notch as shown in the figure below:
_
Pulse oximetry signals:
_
A number of physiologic variables affect SpO2 reading:
1. Arterial blood flow to the vascular bed
2. Temperature of the digit or the area where the oximetry sensor is located
3. Patient’s oxygenation ability
4. Percentage of inspired oxygen
5. Ventilation-perfusion mismatch
6. Amount of ambient light seen by the sensor
7. Venous return at the probe location
________
_______
Procedure of pulse oximetry:
_
_
Pulse oximetry is a simple non-invasive method of monitoring the percentage of haemoglobin (Hb) which is saturated with oxygen. The pulse oximeter consists of a probe attached to the patient’s finger or ear lobe which is linked to a computerised unit. The unit displays the percentage of Hb saturated with oxygen together with an audible signal for each pulse beat, a calculated heart rate and in some models, a graphical display of the blood flow past the probe. Audible alarms which can be programmed by the user are provided. An oximeter detects hypoxia before the patient becomes clinically cyanosed. A pulse oximeter is a medical device that indirectly monitors the oxygen saturation of a patient’s blood (as opposed to measuring oxygen saturation directly through a blood sample) and changes in blood volume in the skin, producing a photoplethysmogram. The pulse oximeter may be incorporated into a multiparameter patient monitor. Most monitors also display the pulse rate. Portable, battery-operated pulse oximeters are also available for transport or home blood-oxygen monitoring. Continuous monitoring of arterial blood gases requires either repeated arterial punctures or an indwelling arterial catheter, and so may be difficult in many circumstances. Instead, the oxygen saturation fraction of hemoglobin can be measured continuously using pulse oximetry. However, since oxygen content varies relatively little with PaO2 at saturations above 90%, it is difficult to know the precise PaO2 using this device. In addition, PaCO2 is needed to fully assess the mechanism of hypoxemia, a value that is not revealed by pulse oximetry.
_
The body’s need for oxygen is certain. Its availability at a tissue level is sometimes in doubt. Blood gas measurements provide critical information regarding oxygenation, ventilation, and acid-base status. However, these measurements only provide a snapshot of the patient’s condition taken at the time that the blood sample was drawn. It is well known that oxygenation can change very quickly. In the absence of continuous oxygenation monitoring, these changes may go undetected until it is too late. Pulse oximeters measure blood oxygen saturation noninvasively and continuously. Pulse oximeters are used widely in emergency departments, anaesthesiology, and critical care. However, data on the role of pulse oximeters in general practice is limited. A recent survey of GPs revealed a minority (9%) reported they used a pulse oximeter to measure pulse rate, or to assess respiratory status (20%). In clinical examination, a traditional sign of hypoxia is central cyanosis. However, studies have shown clinicians have difficulty in reliably detecting hypoxaemia until the saturation is <80%.
_
Pulse oximeters may be used in a variety of situations but are of particular value for monitoring oxygenation and pulse rates throughout anaesthesia. They are also widely used during the recovery phase. The oxygen saturation should always be above 95%. In patients with long standing respiratory disease or those with cyanotic congenital heart disease readings may be lower and reflect the severity of the underlying disease. In intensive care oximeters are used extensively during mechanical ventilation and frequently detect problems with oxygenation before they are noticed clinically. They are used as a guide for weaning from ventilation and also to help assess whether a patient’s oxygen therapy is adequate. In some hospitals oximeters are used on the wards and in casualty departments. When patients are sedated for procedures such as endoscopy, oximetry has been shown to increase safety by alerting the staff to unexpected hypoxia.
_
Pulse oximetry provides a simple, non-invasive approximation of arterial oxygenation in a wide variety of clinical settings including emergency and critical-care medicine, hospital-based and ambulatory care, perioperative monitoring, inpatient and outpatient settings, and for specific diagnostic applications. Pulse oximetry is of utility in perinatal, paediatric, adult and geriatric populations but may require use of age-specific sensors in these groups. It plays a role in the monitoring and treatment of respiratory dysfunction by detecting hypoxaemia and is effective in guiding oxygen therapy in both adult and paediatric populations. Pulse oximetry does not provide information about the adequacy of ventilation or about precise arterial oxygenation, particularly when arterial oxygen levels are very high or very low. Arterial blood gas analysis is the gold standard in these settings. Pulse oximetry may be inaccurate as a marker of oxygenation in the presence of dyshaemoglobinaemias such as carbon monoxide poisoning or methaemoglobinaemia where arterial oxygen saturation values will be overestimated. Technical considerations such as sensor position, signal averaging time and data sampling rates may influence clinical interpretation of pulse oximetry readings.
_
Pulse oximeters are in common use because they are:
1. non invasive
2. cheap to buy and use
3. can be very compact
4. detects hypoxaemia earlier than you using your eyes to see cyanosis.
_
What does a pulse oximeter measure?
•The oxygen saturation of haemoglobin in arterial blood – which is a measure of the average amount of oxygen bound to each haemoglobin molecule. The percentage saturation is given as a digital readout.
•The pulse rate – in beats per minute, averaged over 5 to 20 seconds.
_
A pulse oximeter gives no information on any of these other variables:
•The oxygen content of the blood
•The amount of oxygen dissolved in the blood
•The respiratory rate or tidal volume i.e. ventilation
_
Oximeters give no information about the level of CO2 and therefore have limitations in the assessment of patients developing respiratory failure due to CO2 retention. On rare occasions oximeters may develop faults and like all monitoring the reading should always be interpreted in association with the patient’s clinical condition. Never ignore a reading which suggests the patient is becoming hypoxic. There is no doubt that pulse oximetry is the greatest advance in patient monitoring for many years and it is hoped that their use will eventually become routine during anaesthesia and surgery worldwide.
_
Normal values of pulse oximetry:
In a healthy person, oxygen saturation levels in arterial blood vary between 95 and 100 percent, according to the World Health Organization. A reading below 95 percent in a healthy person with normal lung function indicates low oxygen levels in the blood, a condition medically termed hypoxemia and requires medical investigation. People always want to know what their oxygen saturation “should be”. A fit, healthy young person will probably have an oxygen saturation of 95 – 99%. This will vary with age, degree of fitness, current altitude, oxygen therapy etc. Normal oxygen saturation for aged 70 and above when awake at rest and at sea level is greater than 94%. In healthy infants and children, mean SpO2 values at sea level have been reported to be 97% to 99% and they might be lower in neonates and young infants (range: 93%-100%). Pulse oximeters can either be used to take a ‘one-off’ reading from someone or can be left on for period of time. A single one-off reading often isn’t much use, trends over a period of time give more information. It is important to remember that pulse oximetry is one way of monitoring breathing. It is also necessary, as a minimum, to record respiratory rate and if pulse oximetry is used the amount of oxygen they are receiving must be recorded. As with all clinical assessments the ‘whole picture’ must be looked at.
_
Acceptable normal ranges for patients without pulmonary pathology are from 95 to 99 percent. Usually, levels of SpO2 range from 96 to 99% in healthy individuals. However, when patients have pulmonary or cardiovascular chronic diseases at the same time as a common cold or pneumonia, the level of SpO2 may drop rapidly. SpO2 lower than 90% is denotes acute respiratory failure. When SpO2 drops by 3 to 4% from its usual level, even if it is not less than 90%, an acute disease may be suspected. In some patients, usual levels of SpO2 may be below 90%. Most other individuals will have fluctuations of 3 to 4%. Depending on individual pulmonary or cardiovascular conditions, the level of SpO2 may be relatively higher at rest, even though the level drops considerably during exercise or sleep. As with “normal” body temperature, the level of SpO2 varies from person to person. Since pulse oximeters may produce errors, there is no “correct” or “incorrect” result. Therefore, it is best to record the individual’s level of SpO2 over a long period, and determine their typical range at rest and at various levels of activity so that abnormal decreases can be detected.
_
In the book “Manual of Elderly Home Care by Individual Illnesses,” published by Kinpodo Inc., two key insights into SPO2 rates are provided:
1. The ideal range of oxygen saturation is 96 to 98%. However, since some patients may have lower levels, the person’s normal levels should be determined.
2. If the level is lower than normal, first measure another finger. If the level is 3 to 5% lower than the usual stable level, or lower than 90%, consult your personal physician.
_
It is important to remember that pulse oximeters measure and calculate the oxygen saturation of the hemoglobin in arterial blood, not the actual oxygen content of the blood; therefore, they do not provide a measure of actual tissue oxygenation or how well the patient is ventilated. Be cautious interpreting readings when there has been a sudden change in SpO2. One example would be a sudden decrease from 97% SpO2 to 85% SpO2; this is physiologically impossible. Evaluate this information in conjunction with the patient’s clinical condition and limitations of pulse oximetry. Oxygen saturation values below 70% obtained by pulse oximetry are unreliable. Any time hypoxia is suspected, but not confirmed with pulse oximetry, ABGs should be performed. Even when the pulse oximeter reads the SpO2 as normal, the patient could have undetected carbon dioxide retention. Therefore, it is important not to rely on the information from pulse oximeters alone in the assessment and diagnosis of hypoxemia.
_
What are low oxygen levels?
Generally, hypoxemia is defined as a SpO2 level less than 95%, with severe hypoxemia being an SpO2 level less than 90% and a PaO2 level less than 70 mmHg. Oxygen saturation levels less than 90 percent should be considered a medical emergency, WHO advises.
_
Pulse Oximetry: What do the Numbers mean?
| SpO2, % | PaO2, mm Hg | Oxygenation Status |
| 95–100 | 80–100 | Normal |
| 91–94 | 60–80 | Mild hypoxemia |
| 86–90 | 50–60 | Moderate hypoxemia |
| Less than 85 | Less than 50 | Severe hypoxemia |
_
Circadian Variability of Pulse Oximetry:
Living organisms frequently present changes at the biochemical, cell and/or functional level during the 24h cycle, and the presence of this biological clock is an important advantage for adapting to an environment. The cardiovascular system and the respiratory tract present this type of circadian variation. Nevertheless, one of the possible consequences, which is the circadian modification of SpO2, has not been fully explored. Peripheral oxygen saturation (SpO2) measured by pulse oximetry is widely used in clinical practice, but its fluctuations over the course of the 24h of a day have not been explored at length. In a study done in children who were hospitalized due to non-cardiopulmonary diseases, it was found that SpO2 had a circadian variation. In another study, authors have evaluated whether this phenomenon is also present in clinically healthy children. The results corroborate the fact that there is a circadian variation in SpO2 and that it reaches maximal values in mid-afternoon and minimal values in the early hours of the morning.
_
High altitude:
In Denver where the altitude is virtually exactly 5,280 feet, the normal range of pulse oximetry is 94-97% and very acceptable. If you live along or near any of our coastlines (sea level) your “normals” are higher because you are almost literally at sea level. Perhaps a range of 95%-99% would be your normal range. The reason for the difference is due to two values. The first is the percentage of oxygen in the air we all breathe. This one is easy. The percentage of oxygen in “room air” is 21%. Pulmonologists and respiratory therapists know this as the FIO2 or Fraction of Inspired Oxygen. The second value we need to know is the barometric pressure. Barometric pressure (Pb) can be measured in several different ways. In pulmonary medicine the millimetre (mm) of mercury (Hg) is used as reference. At sea level the Pb is normally reported as 760 mmHg. For reference, in Denver, the Pb is normally around 620 mmHg. Since the FIO2 stays exactly the same at 21% up to an altitude of 60 miles, we simply have to multiply the Pb by the FIO2 to see the how much oxygen is available for us to breath at any altitude. This is reported as the PIO2 or the Pressure of Inspired Oxygen. So 760 x 0.21= about 160mmHg is partial pressure of inspired oxygen at sea level, and but in Denver 620 x 0.21= about 130mmHg. That 30 mmHg difference in partial pressure of inspired oxygen can mean a great deal physiologically to patients who require supplemental oxygen. A patient doing well on 2 L/min in Denver, may not need oxygen at all if they travel to Miami which is at sea level. Healthy individuals at sea level usually exhibit oxygen saturation values between 96% and 99%, and should be above 94%. At 5,280 feet altitude (one mile high) oxygen saturation should be above 92%.
_
Normal SpO2 values in paediatrics:
Normal paediatric SpO2 values have not yet been established. Pulse-oximetry readings vary with age and altitude. The substantial variation of normal SpO2 values among studies can be attributed to differences in sample size, instruments used, health of participants, probe positioning, and measurement protocols. Thus, in healthy infants and children, mean SpO2 values at sea level have been reported to be 97% to 99% (−2 SDs, 95%–96%), and they might be lower in neonates and young infants (range: 93%–100%). At moderate altitudes SpO2 values are somewhat lower (mean: 97%–98%; −2 SDs, 93%–96%) and decrease further at high altitudes (>3000 m; mean: 86%–91%; −2 SDs, 74%–82%). Authors of a recent systematic review concluded that supplemental oxygen should be administered to children who reside at altitudes of >3000 m if the SpO2 is <85%. Most children also exhibit a progressive fluctuation in SpO2 during a 24-hour cycle. Maximal values occur in the late afternoon, whereas minimal values appear in the first morning hours. This pattern is evident regardless of whether children are asleep or awake. Basal SpO2 values reported by polysomnography or home monitoring range from 95% to 100%, but normal saturation nadirs can be as low as 84% to 86%. However, although SPO2 values in the range of 90% to 93% are not uncommon during sleep, they might be associated with poorer academic performance.
_
Sleep SpO2 in adults:
Typically normal oxygen saturations are within 94-97% while sleeping. Patients with sleep breathing disorders, like sleep apnea may experience dips in this saturation. However, it is standard to try and keep saturation above 89%
_
Temporary Hypoxemia during Exercise:
When you do any type of strenuous exercise, you will notice that your breath is quickened, your pulse becomes faster, and your lungs expand. All of these are physiological responses that your body makes to meet the much higher demand for oxygen from the muscles, and to prevent you from feeling hypoxic. When you work out, muscles utilize more oxygen and need to draw more oxygen from the blood, creating an oxygen debt which puts you into a temporary state of hypoxemia. Your body will then self-adjust its respiratory and circulatory systems so that it can maximize the oxygen intake and transport abilities to make up for the low blood oxygen saturation. It is normal for your oxygen saturation to drop slightly during exercise, because your muscles are extracting more oxygen to handle the extra activity. However significant drop of SpO2 during routine exercise suggest cardio-pulmonary illness.
_
How to improve your Oxygen Levels:
To improve your oxygen level if you are feeling winded, adopt a pursed-lip breathing technique. Breath in through your nose, allowing your inhalation to slow a bit, giving your body the chance to exchange oxygen and carbon dioxide in your blood. Make sure to take a long, deep, full breath as you inhale, and then exhale fully to get rid of the carbon dioxide. Purse your lips as you exhale to allow a controlled amount of air to leave your body at time.
__________
_________
Types of pulse oximetry:
Pulse oximetry is classified in two ways:
1. Transmissive vs. reflective oximetry
2. Continuous vs. intermittent oximetry
______
Transmissive vs. reflective oximetry:
_
_
Currently, the two basic types of pulse oximeter probes are transmission probes and reflectance probes.
Transmission probes:
With transmission probes, the light emitter and sensor are placed opposite each other on pulsatile tissue such as a digit or ear. The lights used to measure tissue oxygenation are typically placed across from a detector surrounding approximately 5-10 mm of tissue that contains pulsatile blood flow, such as a fingertip or ear lobe. In general, the transmission method can only be used on limited areas of the body, such as fingers, earlobes, etc. Furthermore, in some instances when the transmission method is used, physiological conditions such as stress and temperature can affect the accuracy of pulse oximetry readings.
Reflectance probes:
With reflectance probes, the light emitter and sensor are placed side by side on a flat body surface. The detector lies adjacent to the light source on a flat surface such as the forehead. This information can be used noninvasively to help evaluate the hemodynamic status of a patient and to detect hypoxemia in various clinical settings. Vasodilation and pooling of venous blood in the head due to compromised venous return to the heart, as occurs with congenital cyanotic heart disease patients, or in patients in the Trendelenburg position, can cause a combination of arterial and venous pulsations in the forehead region and lead to spurious SpO2 (Saturation of peripheral oxygen) results.
_
It is interesting to note that the ratios of the `AC/DC’ ratios at 660 nm and 940 nm (at which many commercial devices operate) are very similar (approximately 0.5) in both reflection and transmission modes. This means that using the same pulse oximeter with either reflection or transmission probes will produce reliable results.
___
Continuous vs. intermittent monitoring:
Continuous pulse oximetry monitoring is recommended for patients who:
•have a critical or an unstable airway
•are receiving conscious sedation during diagnostic procedures
•have a condition or history that suggests a risk of significant desaturation
•have known lung dysfunction
•have obstructive sleep apnoea or morbid obesity
•are in acute pain and receiving analgesics at dosages likely to cause respiratory depression
•have cardiopulmonary disorders severe enough to result in at least one documented desaturation episode treated with supplemental oxygen
•are at risk for desaturation at the time of discharge or transfer from an intensive or post-anesthesia care unit
•are undergoing haemodialysis.
Pulse oximetry should to used intermittently when the patient:
1. is on supplemental oxygen,
2. has a tracheostomy and is on long term mechanical ventilation with chronic stable respiratory failure with frequency of measurement dependent on the clinical conditions of a patient.
_
Sleep vs. waking SpO2 levels:
With intermittent vital-sign and SpO2 monitoring, a true pulse oximetry reading may never be obtained. A caregiver who approaches a sleeping patient to obtain vital signs may awaken the patient, causing immediate vital-sign changes. Many patients have normal SpO2 levels when awake but decreased levels during sleep. Roughly one-third to one-half of adverse events requiring critical interventions in hospitals are related to altered respiratory function. Thus, high-risk patients should undergo frequent if not continuous pulse oximetry monitoring—especially those with sleep-disordered breathing, as in sleep apnea. When transferred to med-surg floors, patients with sleep apnea, those receiving opioids, and those recently transferred from post-anesthesia care units or intensive care units (ICUs) where continuous SPO2 monitoring is used are at high risk for needing ICU readmission because of the switch from continuous to intermittent vital-sign and SpO2 monitoring. Patients with sleep-disordered breathing are more prone to arrhythmias, myocardial infarctions, and stroke. The nursing staff needs to be able to monitor them more closely to prevent serious adverse events.
___
How to use and choose pulse oximeter:
_
Ignorance about pulse oximetry:
Several studies show that there’s a knowledge deficit about pulse oximetry among medical and nursing staff. In one study, researchers administered a 17-question survey on pulse oximetry to 442 nurses, physicians, and respiratory therapists; the respondents’ mean score was just 66%. Another study of 50 nursing and medical staff found “an alarming deficit” in their understanding of pulse oximetry.
_
Do clinicians know how to use pulse oximetry? A literature review and clinical implications: a 2006 study.
Pulse oximetry has become one of the most commonly used tools in the clinical environment for assessing patients’ oxygenation status. It is employed almost continuously in critical care areas and frequently in the general ward environment. Although it is a much better tool for determining hypoxia than the human eye, its use is limited if clinicians do not understand relevant physiological principles, such as the oxyhaemoglobin dissociation curve and the inherent limitations of the device. Furthermore, the risk for compromised patient safety is significant if clinicians fail to recognise the potential for false or erroneous readings. This paper explores the research which has examined clinicians’ comprehension of pulse oximetry. Fourteen studies examining clinicians’ knowledge of pulse oximetry were reviewed. These studies revealed significant knowledge deficits about pulse oximetry amongst nurses, doctors and allied health professionals, all of whom used this technology frequently. Alarmingly, those lacking an adequate understanding of pulse oximetry included senior, experienced clinicians. Educators and clinicians alike must ensure that a safe level of knowledge for the use of pulse oximetry is maintained in order to ensure that patient outcomes are not compromised.
_
Types of pulse oximeters:
Today’s market offers a wide range of Pulse Oximeters available from many well renowned companies. If we are to look for the available models in circulation, it could be broken down into two large categories; one would be fingertip type and the other the handheld model. The handheld pulse oximeter has become a vital instrument in the care of infants, children and adults with cardiopulmonary diseases. It is an accurate, simple and non-invasive method of measuring arterial oxygen saturation. The handheld pulse oximeter provides an easy and accurate way to monitor the blood oxygen saturation and pulse rate. The size, simplicity and convenience of this pulse oximeter are favorite features among many professionals. The handheld pulse oximeter makes use of a probe, which is placed in the person’s finger or earlobe and the reading appears on an easy-to-read liquid crystal display (LCD). The hand-held pulse oximeter is designed for monitoring neonatal through adult patients in almost any setting, from hospital to home, although it is more appropriate in a clinical setting than in the home. It is ideal for spot checks or continuous monitoring. The fingertip model is a small, cost effective pulse oximeter accurately measures blood oxygen saturation levels and heartbeat pulse rates on adult patients. It’s a very compact and self-contained unit to which you need to simply slip the finger. Seconds afterward, it will display your data on high quality easy-to-read liquid crystal display (LCD). The fingertip pulse oximeter is very simple to use and since there is no special learning needed to use it without any setting up, calibration or adaptive devices, it is ideal for use in the hospital or clinical environment, during an emergency or patient transport, or for in-home use as well. The portability of the fingertip pulse oximeter makes it a very popular choice for home use, sports personals, aviators and for medical professionals who are always on the move, it brings a whole new cost effective solution for spot-checking and short term monitoring. A new addition to the fingertip model would be the Paediatric Finger pulse oximeter designed especially for children weighing 5-40kg used for spot-check of oxygen saturation and pulse rate.
_
What to look for in a Spot-Check Oximeter?
Finger pulse oximeters are ideal for spot checks and are portable, battery operated and user friendly. However, other factors should be considered, such as confidence in the reliability of the oximeter long-term as well as the belief in the accuracy of the device in challenging patients. A lot of oximeters are on the market, and any oximeter may work well on a certain patient, but it is the challenging patient population like those with chronic conditions who require the most accurate data to aid in better and faster decision making. Patients with chronic diseases usually suffer from low blood flow (e.g. perfusion), which can impact accuracy. It is important to ask the manufacturer for proven accuracy claims backed by evidence such as published clinical papers. Good pulse oximeters will have specific labelling for challenging conditions.
Here are some factors to consider:
Ideal Features and Functions for Spot-Check Oximeters:
Feature
• Small and portable
• Lightweight
• Easy to use: automatic on/off, simple battery changes, easy-to-read results
• Flexible fit—all finger sizes from adult to paediatric
Function
• Reliable—meets ±2% accuracy with proven clinical data
• Works with a variety of blood pressures and perfusion levels
• Accurate to 70% saturation
• Accurate with some motion
• Durable—able to withstand drops and some moisture
_
Oximeters are also classified as per technological features:
1. Best value
2. Oximeter with pleth-graph
3. Oximeter with pleth graph and alarm
4. Oximeter with continuous recording and memory (sleep study, exercise)
5. Pulse oximeter with Bluetooth support
6. Patient with very low blood perfusion
The best value category gives you well-built units with basic functions (pulse rate and blood oxygen saturation level). Any one from this category will serve you well unless you want more features or have special needs. Two most common features for oximeters are pleth graph and alarm. The pleth graph gives an indication of the change in volume of blood flow as the heart beats. The alarm gives an audio or visual signal when either the oxygen or pulse rate exceeds the normal range. Pleth graph is very useful to older patients. The plethysmograph can tell something about the condition of the patient’s heart, such as missing or irregular heartbeats, low blood flow… There are oximeters available if the patient has very poor blood circulation and more tolerant of motion.
________
________
Pulse Oximeter Usage:
The pulse oximeter consists of a peripheral probe, together with a microprocessor unit, which displays a waveform, the calculated oxygen saturation percentage, and the averaged pulse rate. Alarms are available which sound when a low SpO2 level is detected, or when the pulse rate is either tachycardic or bradycardic. The probe of the device must be positioned in such manner that the emitter and the detector are exactly opposite to each other with 5 to 10 mm of tissue between them. Typical measuring sites include the finger, the toe, the pinna, and the lobe of the ear, whereas for neonates and infants measurements are commonly obtained from the palm or the sole by using specially designed probes. Less commonly used sites are the cheek and the tongue. The probe must be placed on a pulsing vascular bed. A sharp waveform with a clear dicrotic notch indicates a good signal. The machine then reads and averages the values that the waveform receives from the vascular bed, which are read over 5 to 20 seconds, depending on the machine’s internal setting. Averaging the signal reduces erroneous readings and distinguishes artifact from true signal. A pulse rate and percentage of oxygen saturation are interpreted from these averaged values.
_
Correct use of the pulse oximeter includes proper placement of the probe. The emitter and detectors must be opposite each other, and light must not reach the detector other than through the tissue. Care must be used to ensure that the digit is fully inserted into the probe. Older products used a sensor cable that attached to a base pulse oximeter. Modern designs digitize the signals within a single enclosure, negating the need for a base unit in many cases. A modern design will also optionally feature a standardized wireless interface like low-power Bluetooth to send data to a capture or display device like a tablet or smartphone.
_
Proper probe position:
_
Improper probe position:
_
The finger should be the first choice of site used for measurement. A nondisposable clip-type probe is adequate for most purposes, especially when a single or spot reading is being taken. Self-adhesive probes are more useful for long-term monitoring or when motion artifact is expected. Toes may be used instead of fingers, but poor signal because of decreased perfusion is more likely. The lobe or pinna of the ear can be used with a clip-type probe. Care must be taken when using the ear so that pressure from the clip does not impair perfusion. Forehead or nasal sensors may also be used but, depending on clinical area of use, may not be as readily available as finger probes.
_
What is the best location for the pulse oximeter probe?
Choose a site with the best pulsatile vascular bed: the finger, toe, ear lobe, and bridge of the nose have been used. In infants, flexible probes work through the palm, foot, penis, or arm. The cheek or wing of the nostril have also been used. However, overall performance of finger probes is generally found to be better than performance of probes at other sites. Nose and forehead probes perform poorly when SpO2 is low. Manufacturers generally recommend use of the foot for infants.
_
When placing probes on fingers or toes, remove nail polish, especially blue, black, green, brown/ red, or synthetic nails; or place the probe sideways on the finger. Synthetic nails and some colors of nail polish may result in errors of 3% to 6%. In addition, SpO2 values may be lower in dependent extremities than in nondependent sites. Blood flow to the extremity where the sensor is placed should not be impeded in any way. The sensor should be placed on the extremity opposite arterial lines and noninvasive blood pressure monitoring devices so that pulsatile flow is not interrupted.
_
Approach Considerations:
There are several approaches to pulse oximetry.
Digit approach:
This is the preferred method. The transmission probe is placed on the end of a digit, usually the finger, with the emitter on one side and the sensor on the opposite side (see image below). The digit should be resting comfortably and out of excessive light. The probe is then connected to the monitoring unit. Excessive debris should be removed prior to probe attachment, as well as any nail polish or artificial nails.
_
Ear approach:
A transmission probe is placed on the end of an ear lobe with the emitter on one side and the sensor on the opposite side (see image below). The probe is then connected to the monitoring unit.
_
Palm/foot approach in neonates:
In neonates, in whom the digit or ear may be too small, a transmission probe may be placed over the palm or foot. The probe is then connected to the monitoring unit.
_
Forehead approach:
A reflectance probe should be placed low across the forehead right above the eyebrows and away from a major vessel (see image below). The patient should be resting in an inclined position. A headband around the probe and across the forehead should also be placed. The probe is then connected to the monitoring unit.
__
Pulse oximeter probes. A comparison between finger, nose, ear and forehead probes under conditions of poor perfusion: a 1991 study:
The performances of 10 pulse oximeters using finger probes were compared with the same pulse oximeters using alternative probes (eight finger probes, two nose probes and a forehead probe) in poorly perfused patients. All readings were then compared with directly measured arterial blood oxygen saturations. The mean difference (bias, ‘accuracy’), standard deviation (precision) and ‘drop out’ rate for each pulse oximeter combination was determined. An overall ranking of performance of each pulse oximeter was calculated using five criteria (accuracy, precision, number of readings within 3% of standard, percentage of readings given within 3% of standard, expected overread limit in 95% of cases). Nose and forehead probes performed poorly. Some ear probes performed well compared to some finger probes, but the overall performance of probes in other sites compared to finger probes was worse, (p = 0.05). Two of eight ear probes and no nose or forehead probes would be expected to be within 4% of the reference value in 95% of readings. The use of finger probes rather than probes in other sites is recommended in the patient with poor peripheral perfusion.
__
Pulse oximetry has gained wide clinical acceptance in many areas. Small portable systems are available for use virtually anywhere. Almost every patient that has oxygen or mechanical ventilation requirements would benefit from clinical monitoring of their oxygen status by pulse oximetry. This may be in the form of continuous monitoring or by intermittent testing. The oxygen saturation as calculated by pulse oximetry has a 95% confidence rate of ±4%, so oximetry is considered to be reliable at readings that range between 70% and 100% SpO2. This means that, although pulse oximetry is not a replacement for blood gas testing, it can be used as a screening tool when poor oxygen saturation is suspected.
_
Performing pulse oximetry:
1. Turn the machine on and allow for self-tests
2. Apply probe to patient’s finger or any other digit as recommended by the device manufacturer
3. Allow machine to register saturation level
4. Record time and initial saturation percent on room air if possible on/with the patient care report (PCR)
5. Verify pulse rate on machine with actual pulse of the patient
6. Monitor critical patients continuously until arrival at the hospital. If recording a one-time reading, monitor patients for a few minutes as oxygen saturation can vary
7. Document percent of oxygen saturation every time vital signs are recorded and in response to therapy to correct hypoxemia
8. In general, normal saturation is 95-99%. Below 95%, suspect a respiratory compromise.
9. Use the pulse oximetry as an added tool for patient evaluation. Treat the patient, not the data provided by the device.
10. The pulse oximeter reading should never be used to withhold oxygen from a patient in respiratory distress or when it is the standard of care to apply oxygen despite good pulse oximetry readings, such as chest pain
11. Factors which may reduce the reliability of the pulse oximetry reading include:
• Poor peripheral circulation (low blood volume, hypotension, vasoconstriction, hypothermia)
• Excessive pulse oximeter sensor motion
• Fingernail polish (may be removed with acetone pad)
• Carbon monoxide bound to hemoglobin
• Irregular heart rhythms (atrial fibrillation, SVT, etc.)
12. To improve quality of signal, hold finger dependent and motionless (motion may alter results) and cover finger sensor to occlude ambient light.
13. Assess site of oximetry monitoring for perfusion on a regular basis, because pressure ulcer may occur from prolonged application of probe.
14. Document inspired oxygen or supplemental oxygen and type of oxygen delivery device.
_
Nursing considerations and care:
Choose sensor appropriate for the client’s size and location to be used (finger, toe, and ear). Inappropriate size or device may cause inaccurate results or pain. Remove any finger nail polish or artificial nails on the fingers to be used if possible. The sensor may be unable to provide an accurate reading through nailpolish or acrylic nails. Using alcohol ensures that the site and the sensor are clean and dry. Place the adhesive sensors and finger clip. Appropriate location ensures accurate sensor for adults on the client’s index, reading. middle or ring finger. Adhesive sensor also can be placed on client’s toe. A small earlobe clip is available for use on small adults, children’s, and infants. If necessary place newborn adhesive. Decreased circulation could skew result, check the client proximal oxygen saturation readings, pulse and capillary refill. Check the sensor’s markings and if sensor’s are not aligned, make sure the light emitting diode sensor and photo detector are correctly aligned, they should be opposite each other. The continuous pulse oximeter gives audible and visual alarms. Setting the alarm ensures notification to the nurse if the client values are out of the desired range, indicating the possible problem that requires intervention. Move an adhesive sensor every 4 hours and a clip type sensor at least every 2 hours. Watch for signs of tissue breakdown or irritation from adhesives or clips. Moving the sensor helps to prevent tissue irritation and necrosis. Clean the sensor with alcohol wipes when it is removed. The American Association of Critical-Care Nurses (AACN) recommends assessing the prospective site for signs such as cyanosis, decreased peripheral pulse, and decreased temperature, as these can indicate diminished blood flow and lead to inaccurate SpO2readings. The AACN further recommends reevaluating the sensor site periodically. When using disposable sensors, assess the site every two to four hours and replace the sensor every 24 hours. When using a reusable sensor, the site should be checked every two hours and changed every four hours. With reusable sensors, the manufacturer’s recommendations regarding cleaning agents should also be followed.
Special reminder:
• Documentation includes each oximeter reading and location of the sensor.
• If the client is not receive oxygen, the reading is documented “on room air”
• Document if the client is receiving supplemental oxygen and if so, how much (e.g. O2 at 3 l/m)
• Report any downward changes in oxygen saturation of 3% to 5%.
Remember: Values obtained by pulse oximetry are unreliable in the presence of vasoconstricting medications, IV dyes, shock, cardiac arrest, severe anemia, and dyshemoglobins (e.g., carboxyhemoglobin, methemoglobin).
_
Sensor size:
Sensors are sized according to the patient’s weight; different manufacturers specify somewhat different ranges. It’s important to use the correct size to avoid skin complications and ensure accurate readings. Even when the correct size is used, skin breakdown at the placement site, caused by pressure from the sensor, has been reported.
_
Adult sensor/probe:
_
Neonate sensor/probe:
_
Check that the right type of sensor is being used. The sensor site should be chosen based on which location has the best pulsatile vascular bed. Generally the finger is chosen first; however, forehead sensors are particularly useful in patients with poor peripheral circulation. Forehead sensors are also a good alternative in patients under general anesthesia whose extremities aren’t readily accessible. To exclude motion artifact caused by shivering, patients should be kept warm. A study of trauma patients during prehospital transport found that those actively warmed with resistive heating blankets had significantly fewer oximeter alarms than those given wool blankets. The researchers attributed this to improved peripheral circulation in the actively warmed group. To avoid potential interference from ambient light, the sensor can be covered with the patient’s linens. Nail polish or artificial nails should be removed.
___
Some Pointers for Nurses:
Here are some important things to keep in mind when using a pulse oximeter:
• Ensure that continuous monitoring is used only on patients whose condition requires it, such as patients with a compromised airway. If your patient has an inappropriate order on the chart, alert the prescriber and ask that it be updated.
• Be aware of situations for which pulse oximetry is contraindicated, such as during CPR.
• Know causes of erroneous readings, such as movement or carbon monoxide poisoning.
• Choose the correct sensor size for the patient.
• Check the skin under the sensor and rotate the sensor site periodically.
• Explain the equipment and the reasons that alarms might sound to patients and family members, to reduce their anxiety.
• 100% oxygen should be administered to all patients despite a good SpO2 if they have respiratory distress
• Make sure that all dirt and nail polish or any obstructive covering is removed to prevent the unit from giving a false reading
• Attempt to obtain a room air reading and a reading with supplemental oxygen
• Do not read while BP being taken as it may give false readings
• Although the pulse oximeter displays the heart rate, the unit should not be used in place of the cardiac monitor and a physical assessment of the heart rate
• Many patients with COPD have chronic low oxygen readings and may lose their respiratory drive if administered prolonged high oxygen therapy; routinely assess pulse oximetry as well as respiratory drive when administering oxygen to these patients; do not withhold oxygen from any patient that requires it.
• The room air pulse oximetry reading is not required if the patient has been placed on supplemental oxygen prior to EMS arrival
_
_
Treatment guidelines:
| SpO2 Reading | Interpretation | Action |
| 100% to 95% | Ideal Range | No supplemental oxygen is needed |
| 95% to 90% | Mild to Moderate Hypoxemia | Check airway, start oxygen therapy via nasal cannula at 4-6 l/m |
| 90% to 85% | Severe Hypoxemia | Check airway, start aggressive oxygen therapy, high flow oxygen via nonrebreather mask at 15 l/m. Consider bag valve mask ventilation with 100% oxygen if the patient does not have adequate ventilations. |
| 85% to less | Respiratory Failure | Assist ventilations with 100% oxygen and bag valve mask; consider CPAP or intubation |
1. All patients who require vital signs to be taken should have oxygen saturation measured and recorded as part of the vital signs
2. Measure oxygen saturation before applying oxygen and repeat the measurement after oxygen has been applied, do not delay oxygen administration in patients experiencing severe respiratory distress
_
How do I clean/sterilize the probe after use on one baby and before being used on another?
Cleanse the probe with alcohol; let it dry before using on another baby.
_
Improving an oximeter signal:
Warm and rub skin
Apply a topical vasodilator – e.g., glyceryl trinitrate (GTN) cream
Try an alternative probe site
Try a different probe
Try a different machine
_
Using Pulse Oximeter with Cold Hands:
Pulse oximeter usually runs slow, if at all, in a cold environment. Cold hands and fingers mean that the blood flow and circulation to your hand is reduced and may cause problem for the oximeter to detect a good pulse signal. When this happens, a pulse oximeter may take several minutes to return a reading and sometimes the reading may be inaccurate. Under this situation, try to warm up the patient’s hands prior to taking a measurement. One good way is to massage patient’s hands by rubbing them gently against each other. Doing some hand exercise would also increase blood circulation.
_
Challenges of pulse oximetry:
One drawback of continuous pulse oximetry monitoring may be the cost of integrating it into a central monitoring system. Others include false alarms, staff complacency with alarms, and patient-related issues, such as limited ambulation, failure to keep sensors on, or failure of sensors to read properly. Many of these problems can be addressed when implementing a monitoring program.
_
False alarms:
Patient movement and low perfusion can increase false alarms and cause erroneous measurements. Also, if the oximetry sensor is placed on the same side as an automatic inflatable blood pressure cuff, a false alarm may sound when the cuff inflates. Frequent false alarms can cause “alarm fatigue” in caregivers. Hearing the same alarm go off or hearing frequent alarms on specific patient leads can desensitize nurses to alarms and cause them to miss significant true alarms. Also, use of the monitor may lead them to focus more on the monitor than the patient. In addition, false alarms may require staff interventions that interfere with patients’ sleep, and can cause anxiety in patients and families. Bedside equipment alarms can be frightening to patients and families, especially if they aren’t attended to promptly. Quality assurance studies conducted by member hospitals of the Child Health Corporation of America’s Pulse Oximetry Forum indicate that in paediatric populations, the false alarms that occur during continuous pulse oximetry cause needless anxiety for patients and families. Nurses should explain why pulse oximetry is being used, how it works, and what the readings indicate in language the patient and family can comprehend. The factors that can lead to false alarms should also be explained, as should the importance of frequent site assessment and rotation. Finally, nurses can remind prescribers to change the order from continuous monitoring to intermittent, as appropriate. Newer pulse oximetry technologies (sometimes called “smart” technologies) are designed to decrease false alarms, increase the reliability of true alarms, and alert clinicians to patterns or trends that give early warning of respiratory decompensation. Consider, for example, a patient with sleep apnea: If the patient stops breathing for several seconds, the SpO2 value may remain in the normal range or rise above the alarm limit range; or it may be slightly below the alarm range and then return to normal. In this case, the alarm may not sound because the time limit wasn’t violated; if the alarm does sound, the nurse might consider it a false alarm because it occurred only momentarily. With newer technology, the repeated pattern of lower SPO2 value and alarm violation alerts the staff to review the patterns and assess the patient further. Also, some newer oximetry systems have visual graphs that show the length and degree of desaturations, which are more telling than a single number or trend.
_______
Home use:
Technology can be slow and initially expensive, so the use of pulse oximeters at home is just getting started. But if we have a need for a pulse oximeter, they are now easy to obtain and reasonably priced. If you are buying one on your own, you need to look at the specifications and what it will measure. If you have a heart condition and you know your oxygen saturation is usually 85%, you don’t want to get a pulse oximeter that only measures 90 to 100% accurately. A good home pulse oximeter should measure 70% and above with good accuracy. Having a monitor at home can be important for many people. If saturations vary within the normal range, that is typical and okay. But if, for example saturations are in the range of 94% and your child takes a brisk walk and returns short of breath with saturation readings at 86%, then we need a doctor to assess those numbers and decide if an action or treatment is necessary or if there is a problem that needs addressed medically. We can only track this over time if we have a home pulse oximeter. In summary, using a pulse oximeter at home is a quick, easy, inexpensive way to track oxygen saturation.
_
For patients on long-term oxygen therapy, pulse oximetry arterial oxygen saturation (SpO2) measurements are unnecessary except to assess changes in clinical status, or to facilitate changes in the oxygen prescription. Home pulse oximetry is also indicated when there is a need to monitor the adequacy of SpO2 or the need to quantitate the response of SpO2 to a therapeutic intervention.
Consider a pulse oximeter for home use for the following indications:
A. To determine appropriate home oxygen liter flow for ambulation, exercise, or sleep;
B. To monitor individuals on a ventilator at home;
C. When a change in the individual’s physical condition requires an adjustment in the liter flow of their home oxygen needs;
D. When weaning the individual from home oxygen;
E. For interstage monitoring of children undergoing the Norwood procedure for hypoplastic left heart syndrome.
_
Experimental and investigational indications of pulse oximetry at home include:
A. Asthma management
B. Diagnosing nocturnal hypoventilation associated with neuromuscular disorders
C. Evaluating and teaching continuous positive airway pressure (CPAP)
D. When used alone as a screening/testing technique for suspected obstructive sleep apnea.
__
Pulse Oximetry Tips for Home Use:
Once you purchase a home pulse oximeter, take it with you to your doctor’s office for further operating instructions. With your doctor’s approval, you can work together to learn how to adjust your oxygen flow based on your fluctuating oxygen saturation levels.
Additionally, keep in mind the following tips before you start to use a pulse oximeter at home:
•Monitor and keep a log of your oxygen saturation levels at various times during the day and during specific activities. Share them with your doctor so she can get a better understanding as to how rest and activity affect your oxygen saturation levels.
•Work carefully with your doctor to develop a target oxygen saturation level. Under the instruction of your doctor, adjust your oxygen flow rate to maintain your target oxygen saturation level.
•Never titrate oxygen without specific instruction from your health care provider.
•Never rely on a pulse oximeter to determine how you should be feeling. If your oxygen saturation level is normal but you are severely short of breath and/or are experiencing other troubling symptoms, seek emergency medical attention and notify your health care provider as soon as possible.
•A sudden drop in oxygen saturation can be a sign of trouble. Call your doctor as soon as possible if your normal oxygen flow rate fails to maintain your target oxygen saturation level.
• You can use your oximeter at rest or during activities, such as walking or other exercise. However, your oximeter should not be submerged in water.
• Do not smoke! Smoking reduces the amount of oxygen reaching your tissues—while the oximeter will falsely suggest that oxygen level is satisfactory.
• A sudden drop in your oxygen level—for example during a severe cold or the flu—can be a sign of trouble. Call your doctor if your normal oxygen setting is no longer maintaining your saturation and you feel sick. Also, call your supplier if you feel your oxygen system is not working.
• A high resting pulse rate of greater than 100 or a low pulse of less than 40 (check with your doctor to determine your individual pulse ranges) are also reasons to call your doctor.
_
How to buy a Home Pulse Oximeter:
Common features:
1. FDA Certified: Pulse oximeter is a class II device and FDA registration is required before selling in US. Although almost all oximeters for sale on the market are now certified, this was not the case a few years ago. You can verify the certification by going to the FDA Medical Device Data Base and enter the manufacturer name in the search field to find out for sure.
2. Accuracy and reliability: The primary purpose of a pulse oximeter is to measure your oxygen saturation (SpO2) and pulse rate. So the key selection criterion is to find one that produce accurate results within its operating range consistently and reliability. Pulse oximeters generally use similar mechanisms for reading data and differ in how they are manufactured. If you need an accurate reading, you should validate your pulse oximeter by comparing it with others, such as those in your doctor’s office or medical clinics. Most oximeters can take a reading within a few seconds and have an accuracy of ±3%. The accuracy is often affected by motion. If your hand trembles, find a model that is more tolerant to hand movements or hold your hand still while taking readings.
3. Ease of use: Fingertip pulse oximeters operate by inserting your finger into the sensor and then pressing one button. They are easy to operate. Make sure the display is large enough for you to read. Some can display the data in different ways making them easier to read.
4. Sensor size: Make sure you can insert your finger comfortably in the sensor. This is normally not an issue for clip-on type. For children and persons with small hands, consider a paediatric pulse oximeter.
5. Other features: There are other features, non-essential, but will assist you in using the oximeter:
•Memory: Save previous readings and timestamps; generate various statistics.
•Computer interface: Save readings to a computer for further analysis by you or your doctor.
•Software program: Analyze the data.
_________
Pulse oximetry increasing usage:
According to a report by Frost & Sullivan entitled U.S. Pulse Oximetry Monitoring Equipment Market, US sales of oximeters were worth $201 million in 2006. According to a report by iData Research the U.S. pulse oximetry monitoring market for equipment and sensors was over 700 million USD in 2011. In 2008, more than half of the major internationally exporting medical equipment manufacturers in China were producers of pulse oximeters. In June 2009, video game company Nintendo announced an upcoming peripheral for the Wii console, dubbed the “Vitality Sensor”, which consists of a pulse oximeter. This marks the onset of the use of this device for non-medical, entertainment purposes.
_
An estimation of the pulse oximetry gap:
No study has ever quantified the extent to which pulse oximetry devices are available to operating room personnel in low and middle-income countries. Even basic information such as the number of operating rooms and the types of monitoring devices is lacking. Anecdotal evidence suggests the presence of an enormous and pervasive “pulse oximetry gap,” defined as the number of pulse oximeters needed to achieve 100% penetrance in a given setting. To estimate this “gap,” other data sources must be examined. We must first estimate the total number of operating rooms in resource-constrained settings. This will give us a sense of the “operating room market.” Once this market is estimated, the gap in pulse oximeter availability can be evaluated. Given the universal use of pulse oximetry in high-income countries, the gap is assumed to be present predominantly in low and middle-income countries.
_
Pulse oximetry market:
The table above shows that pulse oximetry penetrance is low in low income countries.
_
As demonstrated by the population-based estimate in table above, which exceeds 1 million pulse oximetry devices, the hospital bed and operative volume approaches probably both underestimate the true pulse oximetry market. They do not take into account labor rooms, post anaesthesia recovery rooms, emergency rooms, intensive care units, and other areas where pulse oximetry clearly has a place in clinical evaluation and monitoring. They also do not account for the future market as surgical services increase in the developing world. There is a vast distance between what is currently provided and what is actually needed in terms of surgical services in much of the developing world. As countries address the shortfall of surgical services, the need for and use of pulse oximetry for safe anaesthesia monitoring will need to increase in parallel.
_______
_______
Functions, uses and indications of pulse oximetry:
The basic rationale behind pulse oximetry is that hypoxaemia may be detected early and treatment can begin before serious or irreversible adverse effects occur. A pulse oximeter is a device intended for the non-invasive measurement of arterial blood oxygen saturation (SpO2) and pulse rate. Oximeters are widely used in hospitals, medical clinics, operating rooms, and homes. Both oxygen saturation level and pulse rate are vital signs of a patient. Oximeters are inexpensive and can report an accurate reading within seconds. Speed is important especially in an emergency situation. Pulse oximeter is used medically by patients with asthma, emphysema, chronic obstructive pulmonary disease (COPD), and other respiratory conditions. Patients with serious respiratory problems should have their SpO2 levels check regularly and especially if they are not feeling well. For many patients, doctors often recommend exercise to improve their physical state. However exercise can result in increasing shortness of breath, patients should monitor their oxygen saturation with pulse oximeters while exercising so they can adjust the pace as the oxygen saturation decreases. Patients with serious cardiac condition would often experience low SpO2 levels. Pulse oximeters would help them to monitor their conditions and use supplementary oxygen when required. Pleth graph produced by a pulse oximeter shows the change in blood volume during a heart pulse is often a good indication of certain heart conditions. Pilots, mountain climbers and people in high altitudes also use pulse oximeters to help guard against hypoxia. Proper breathing techniques, such as pursed lip breathing, can increase your oxygen saturation level. Lots of patients with low oxygen saturations are able to increase their saturations all the way up to 93% with good breathing techniques. Practice and pulse oximeter will help patients to achieve this level of efficiency. Pulse oximeter can also help athletes in high altitude training. The reduction in oxygen level can increase red blood cells in athletes and help to increase his/her endurance.
_
Functions of pulse oximeter:
Do remembering that the Pulse Oximeter measures a very important parameter of our body, that is important in ensuring our survival, the pulse oximeter take not only a prominent role for diagnosis in the medical field but also a great beneficial role for sports personals and pilots. With the development of the microprocessor and better sensor, the Pulse Oximeter has stepped into a whole new dimension and gained great acceptance in its clinical application may it be in the hospital institution or at home. If we are to break down the uses of a Pulse Oximeter from a clinical point of use, it could be stated that the any patient with unstable oxygenation has significant benefits from this device, this includes patients at the intensive care unit, at operations, recovery, and hospital ward setting. The general assessment of a patient’s need for oxygen is the most essential part in maintaining life as life cannot continue in the absence of oxygen. Therefore the pulse oximeter plays an important role as a general condition assessment device just like one that checks blood pressure, sugar levels and temperature. The pulse oximeter aids in other patient condition evaluation such as blood flow assessment, cardiopulmonary arrest, asthma and seizures. Because of its simplicity, versatility and speed, pulse oximeters are of critical importance in emergency medicine and more of a necessity for patients with respiratory and cardiac problems, for diagnosis of some sleep disorders such as apnea and hypopnea. It has definitely become a gold standard of use in ambulances, patients under anesthesia, neonates in the intensive care, newborn nurseries and delivery suites; the pulse oximeter serves an important role in transport internally within the hospitals and externally in the ambulance and Air transport. The function and role of the pulse oximeter could not be forgotten from a general diagnostic value as it is very useful in the initial staging of diagnosis as in PFT lab, exercise lab and the sleep lab. Finally it has a great use as an all-purpose assistant and aids in sub-acute care centers and home care patients being an indicator when supplement oxygen should be administered to the patients. The use of the Pulse Oximeter is not constrained to the medical institution, the non-medical oximeters are rather sporty versions of the pulse oximeter designed specifically for high altitude performance sports and the aviator market. Often coming as fingertip pulse oximeters, they are designed to provide correct blood Oximetry and pulse rate measurement while in motion. At higher altitude, it should be noted that blood oxygen saturation decreases because of reduced amount of oxygen in the air; this makes the finger pulse oximeter a very versatile piece of instrument allowing you to accurately assess how well you are adapting to high altitude, by measuring your saturated blood oxygen content and heart rate. Portable, battery operated pulse oximeters are very useful for pilots operating in a non-pressurized aircraft above 10,000 feet where supplemental oxygen is required. Prior to the oximeter’s invention, many complicated blood tests needed to be performed. Portable pulse oximeters are also useful for mountain climbers and athletes whose oxygen levels may decrease at high altitudes or with exercise.
_
Uses of pulse oximetry:
The use of pulse oximetry for patient assessment and monitoring is well established in critical care, anesthesiology, and emergency departments. In recent years, the availability of small, user-friendly, portable and affordable pulse oximeters, including those worn on the finger-tip has opened up the potential for use of this technique in an expanded variety of clinical settings, including primary care. In most countries, oximeters are only sold to patients under the guidance of a licensed healthcare professional, and use by patients should be supervised by their physicians or other qualified health care provider. Incorrect or inappropriate use of oximeters will not provide useful information, and they should be used as part of a broader clinical assessment and not in isolation. Examples of the use of pulse oximetry to monitor a patient’s clinical status include apnea monitoring, evaluation of periodic breathing (in infants), during transport (in the hospital or prehospital setting), and in critical care areas (e.g., the intensive care units and the ED). Pulse oximetry is used during airway procedures (e.g., intubations) and during lumbar punctures and other invasive procedures, (e.g., central lines), especially in infants. Pulse oximetry is used for monitoring patients on mechanical ventilation. In patients with an endotracheal (ET) tube, pulse oximetry may be a clue to a misplaced or blocked ET tube. The most beneficial use of a pulse oximeter in an anesthetized or ICU patient is as an early warning device for hypoxemia. During anesthesia, this most commonly happens during induction and recovery. It can also indicate the continued need for oxygen supplementation. A study determined that pulse oximetry provided the first warning of an incident in 27% of situations. Additionally, the number of unanticipated intensive care unit admissions decreased after the introduction of pulse oximetry. Other applications for use of pulse oximetry include controlling oxygen supplementation, monitoring circulation, determining systolic blood pressure, and monitoring vascular volume.
_
Pulse oximeters are now used routinely in critical care, anaesthesiology, and A&E departments, and are often found in ambulances. They are an increasingly common part of a GP’s kit. Pulse oximetry’s role in primary care may include:
• Diagnosing and managing a severe exacerbation of chronic obstructive pulmonary disease (COPD) in the community.
• Grading the severity of an asthma attack. Where oxygen saturations are less than 92% in air, consider the attack potentially life-threatening.
• Assessing severity and oxygen requirements for patients with community-acquired pneumonia.
• Assessing severity and determining management in infants with bronchiolitis.
_
Clinical uses of pulse oximetry:
_
Indications for pulse oximetry are categorized into three groups:
1) A baseline indicator or monitor of a patient’s oxygenation status,
2) Evaluation of response to therapy, and
3) Monitoring during procedures.
Pulse oximetry is indicated in patients with cardiopulmonary disease; unstable or critically ill patients; and patients with or the potential for apnea, hypoxia, respiratory distress/failure, or shock. Pulse oximetry has been used in the diagnosis of numerous cardiopulmonary diseases and to evaluate the response to treatment in various cardiopulmonary disorders ranging from asthma, chronic obstructive pulmonary disease, bronchiolitis, and reactive airway disease, to pneumonia, airway obstruction, heart failure, and cyanotic congenital heart disease.
_
Indications for pulse oximetry include the following:
• Patients with suspected hypoxemia
• All cases of respiratory distress
• For the treatment of primary respiratory or cardiac disease
• All cases of altered or depressed level of consciousness
• Drug overdoses
• Any patient requiring intubation or BVM support
• Major trauma
• Smoke Inhalation (may not be accurate due to CO)
• Any patient on home oxygen, home ventilator, or BiPAP
_____
Where pulse oximeter is used:
Initially, pulse oximeters gained wide acceptance in hospital operation and anaesthesia rooms. Equipment used for patients in acute condition includes stationary pulse oximeters and bioinstrumentation systems which can simultaneously monitor other important vital signs, for example when using an electrocardiogram. During post-operational recovery or in subacute phases, telemetric, hand-held monitoring units are fixed to the bedside in addition to the stationary pulse oximeter. This equipment is used to warn of sudden deterioration of a patient’s condition. Meanwhile, small portable pulse oximeters are frequently used both in hospitals and for outpatient care.
The following section describes where small, portable pulse oximeters are used.
1. Hospitals:
Small, portable pulse oximeters are used in hospitals, especially by nurses in respiratory and cardiovascular wards. The main purpose is to monitor the vital signs of hospitalized patients. SpO2 is the fifth most important vital sign monitored, after pulse rate, body temperature, blood pressure, and respiration. It is monitored in the morning, afternoon and evening in order to check patient conditions.
2. Outpatient:
The pulse oximeter is used mainly in respiratory departments. Some physicians use the pulse oximeter to monitor SpO2 of patients who are suspected of having respiratory diseases in order to learn their normal values. They then use the values as reference data if the patient’s condition deteriorates.
3. Respiratory function tests and rehabilitation in hospitals:
The pulse oximeter is used for examination and assessment of respiratory function tests and walking tests. These tests may be conducted by laboratory technicians or physical therapists. The device is also used by physical therapists for risk management during patient rehabilitation to confirm a decrease in SpO2 and an increase in pulse rate as needed.
4. Clinics (Clinical internists):
Hypoxemia involves the respiratory, cardiovascular, and nervous systems. The pulse oximeter is used in the field of respiratory internal medicine and general internal medicine, and can determine the necessity of sending patients to specialist hospitals. It can also make differential diagnoses and analyze the severity of a condition. At the same time, the portable pulse oximeter is an essential device for home-visit medical service.
5. Home visit nursing:
Most patients receiving home visit nursing service are elderly. Generally they have some respiratory or cardiovascular system difficulties even if respiratory disease is not the main cause of their problems. SpO2 measurement has been widely used by home visit nurses as a method to quickly assess their patients’ respiratory and cardiovascular conditions.
6. Eldercare facilities:
Pulse oximeter use in eldercare facilities has not yet reached the level of usage by home visit nurses. However, it is expected that the devices will become more widely accepted for vital sign monitoring of patients in hospitals and daycare facilities, especially during those times (often during the Night) when their condition may deteriorate.
7. Other situations:
When the air pressure drops, the partial pressure of oxygen in the air decreases resulting in a decrease in oxygen saturation. The pulse oximeter is used to prevent accidents that might occur during flight and high altitude climbing. Patients receiving HOT (home oxygen therapy) who travel by air or participate in mountain climbing events are often equipped with small, portable pulse oximeters, as are many airliners and organzations involved in high attitude sports and hypoxic training.
_
Common Areas for Use of Pulse Oximetry:
1 During anesthesia and postanesthesia care, including both general and conscious sedation
2 Intensive care units
3 Neonatal care units, including delivery, nursery, and neonatal intensive care unit
4 Hospital medical units
5 Transportation within the hospital and during ambulance or air ambulance transportation
6 Diagnostic testing, such as pulmonary function testing, exercise testing, and during sleep studies
7 Subacute care centers, such as nursing homes and rehabilitation centers
8 Home care patients
_________
_________
Pulse oximetry, oxygen and anaesthesia:
Pre-oxygenation:
Breathing 100% oxygen prior to induction of anaesthesia (preoxygenation) increases the oxygen stores in the lungs. If a patient stops breathing and is not ventilated, the amount of oxygen in the lungs will rapidly diminish. If the patient has been given 100% oxygen to breathe for several minutes prior to induction of anaesthesia, the increased oxygen reservoir will supply much needed oxygen, adding potentially life-saving minutes. There are many situations where this may be important. One example is in the pregnant mother where the enlarged uterus reduces lung volume and the metabolic demands are increased by the foetus. Another example is in young children who have small lung volumes and high metabolic demands. They can use up oxygen very quickly and can sometimes be resistant to efforts to preoxygenate them.
_
During anaesthesia, patients’ airways may become obstructed, their breathing may become depressed, their circulation may be affected by blood loss or an abnormal heart rhythm or the anaesthetic equipment may develop a problem such as an accidental disconnection or obstruction of the breathing circuit. These factors can result in a reduction of oxygen delivery to the tissues which, if not managed correctly, could lead to injury or death. The earlier the anaesthesia provider detects a problem, the sooner it can be treated so that no harm comes to the patient. During anaesthesia the oxygen saturation should always be 95 – 100%. If the oxygen saturation is 94% or lower, the patient is hypoxic and needs to be treated quickly. A saturation of less than 90% is a clinical emergency.
_
It has been difficult to identify a specific reason for the decline in anaesthesia mortality over the past three decades. Improvements in monitoring, ventilator safety, and provider training all occurred during this time. Yet, most would agree that the implementation of monitoring standards was critical. These standards transformed pulse oximetry from a technology that was rarely used into an essential device in nearly every operating room in the developed world. They allowed anaesthesia providers to continuously monitor oxygenation and detect hypoxemia earlier. Anaesthesiologists no longer had to wait for clinical signs, such as cyanosis, to respond to a hypoxic patient. Consequently, technical mishaps such as circuit disconnection, airway dislodgement or obstruction, or inadequate oxygen administration were identified sooner and providers could respond before adverse events occurred. Surprisingly, the relatively rapid inclusion of pulse oximetry into the anaesthesia armamentarium occurred without level one (randomized) evidence. In fact, most of the early data were observational. One of the most influential studies, published by Cooper and colleagues in 1984, involved 139 anaesthesia provider interviews. Over 500 “incidents” and 70 “critical incidents” were discussed with investigators. From these interviews, the authors determined that the leading cause of mortality was the failure to deliver adequate amounts of oxygen. Pulse oximetry would have made a difference in many of these incidents. Since Cooper’s study, there have been at least seven randomized controlled trials on pulse oximetry. One had inadequate postoperative data, which limited its usefulness for this discussion. Of the remaining six, the study published by Moller and colleagues in 1993 was by far the largest and most informative. In this study, over 20,000 adults undergoing general or regional anaesthesia were randomized to either pulse oximetry or no pulse oximetry during surgery and in the postoperative recovery unit. The primary outcome measures were hypoxemia detection and perioperative and postoperative complications. The authors clearly state in the discussion that the study was not powered to detect differences in mortality. Nearly 2 million patients would have been needed to include mortality as an outcome. Several critical pieces of information were obtained from this trial. Of utmost importance, the rate of hypoxemia detection increased nearly 20 fold in the pulse oximetry group (p<0.0001). Endobronchial intubation and hypoventilation were also detected more frequently. Patients with pulse oximeters experienced 50% fewer myocardial ischemic events than those without pulse oximeters (p=0.03). Cardiac arrest was also less frequent with pulse oximetry, although this difference was not statistically significant (4 arrests among 9,578 patients with pulse oximetry; 11 arrests among 9,772 patients without; 1 sided p value=0.06). Clearly, pulse oximetry benefited patients. It allowed identification of inappropriate airway management by revealing hypoxemia, and it decreased the frequency of both myocardial ischemia (presumably by ensuring adequate oxygenation of the myocardium) and cardiac arrest. As expected, mortality rates were unchanged (3 deaths in oximetry group and 4 in the control) as were postoperative morbidity rates, which included respiratory, cardiovascular, neurologic and infectious complications. Of the remaining 5 randomized trials which included nearly 1,500 patients, pulse oximetry consistently allowed early detection of hypoxemia by anaesthesia providers. None showed a mortality benefit. Although a randomized trial of two million patients addressing the effect of pulse oximetry on mortality would be powerful, this study will likely never be done; pulse oximetry is the standard of care today, and most would consider further attempts at randomization to be unethical. A 2014 Cochrane analysis of these trials concluded that the value of pulse oximetry “is questionable in relation to improved outcomes, effectiveness, and efficiency”; most anaesthesia experts around the world would disagree. Several retrospective reviews also strongly support the efficacy of pulse oximetry. One analysis of 2,000 anaesthesia-related adverse events showed a reduction in cardiac arrests when pulse oximetry was used. Another review of 4,000 “incidents” in Australia and New Zealand revealed no cases of hypoxic brain injury from inappropriate ventilation after the introduction of pulse oximetry and capnography. Oximetry alone would have detected 82% of the relevant incidents and 60% prior to organ damage. Capnography alone would have detected 55% and 43%, respectively.
_
In summary, pulse oximetry has been the standard of care in the developed world for nearly two decades. Though randomized data suggesting a mortality benefit are lacking, both expert consensus and a large volume of published data indicate that pulse oximetry is beneficial for patients. Anaesthesia providers in all settings have demonstrated a strong commitment to pulse oximetry since its inclusion into anaesthesia care. There are exceedingly few drawbacks to pulse oximetry once providers are appropriately trained. In resource limited settings, universal pulse oximetry could substantially improve the safety of anaesthesia. Today, if given the choice of one monitor, most anaesthesiologists would quickly choose the pulse oximeter over the electrocardiogram (ECG) or noninvasive blood pressure devices. However, pulse oximetry cannot reveal different types of cardiac arrhythmia and ST segment changes revealed by ECG monitor.
_______
Pulse oximetry vis-à-vis emergency and critical care:
First I will discuss role of pulse oximetry in emergency department (Emergency room [ER], accident and emergency [AE], emergency department [ED], casualty) and then I will discuss pulse oximetry in critical care (ICU).
_
Pulse oximetry in emergency department (ED/ER/AE):
_
Effect of routine emergency department triage pulse oximetry screening on medical management: 1995 study:
The study included 14,059 consecutive patients presenting to triage at a university ED. Of 1,175 patients having triage pulse oximetry values less than 95%, physicians ordered repeat pulse oximetry on 159 (13.5%), additional chest radiography on 5.4%, CBC count on 3.1%, arterial blood gases on 2.9%, spirometry on 0.9%, and ventilation-perfusion scans on 0.3%. Physicians ordered 178 new therapies on 134 patients (11.4%), including supplemental oxygen for 6.5%, antibiotics for 3.9%, and beta-agonists for 1.8%. Thirty-five patients (3.0%) initially scheduled for hospital discharge were subsequently admitted. Physicians changed or added diagnoses in 77 patients (6.6%). Providing physicians with routine triage pulse oximetry measurements resulted in significant changes in medical treatment of these patients.
_
Effect of routine pulse oximetry measurements on ED triage classification: a 1998 study:
Pulse oximetry is commonly used to rapidly determine oxygen saturation and is incorporated in emergency triage as a screening for potential cardiopulmonary complications. This study examined the effect of routine pulse oximetry measurements on emergency department (ED) triage classification. Using a portable pulse oximeter, oxygen saturation of 1,235 adults presenting to a university-based, urban ED was obtained and each patient was assigned a classification of severity based on a standard 1-to-4 scale before and after the measurement. According to data obtained, a small but statistically significant group (2.8%) benefitted from the routine use of pulse oximetry in an emergency triage system and only 40% of these patients required admission or extended care. Although this group is small in number, the potential consequences of missing a hypoxic condition could be devastating for the individual patient. Since pulse oximetry is presently an inexpensive technology, it would seem to be a worthwhile screening tool for emergency triage.
_
The accuracy of pulse oximetry in the emergency department: a 2000 study:
The objective of this retrospective study was to identify factors affecting the accuracy of pulse oximetry in the ED. Over a 3-year period, 664 consecutive emergency department (ED) patients had simultaneous arterial blood gas (ABG) and pulse oximeter readings taken. Pulse oximeter saturations (SpO2) were compared with ABG CO-oximeter saturations (SaO2) for accuracy. Multiple variables including age, sex, hemoglobin, bicarbonate, pH, and carboxyhemoglobin (COHb) were analyzed to see if they affected SpO2 accuracy. ROC curves were used to determine the best pulse oximeter threshold for detecting hypoxia. Using multivariate analysis, COHb was the only statistically significant factor affecting the accuracy of pulse oximetry. In patients with COHb < 2%, SpO2 overestimated SaO2 by more than 4% in 8.4% of cases. In patients with COHb ≥ 2%, SpO2 overestimated SaO2 by more than 4% in 35% of cases. The best pulse oximetry threshold for detecting hypoxia is 92%. At this threshold, if COHb is <2%, pulse oximetry has a sensitivity of 0.92 and specificity of 0.90. If COHb is ≥2%, sensitivity is 0.74 and specificity is 0.84. For patients likely to have a COHb < 2, pulse oximetry is an effective screening tool for detecting hypoxia. However, more caution must be exercised when using pulse oximetry in patients likely to have a COHb ≥ 2%.
_
The accuracy of pulse oximetry in emergency department patients with severe sepsis and septic shock: a retrospective 2010 cohort study:
Sepsis results in characteristic microcirculatory derangements that could theoretically affect pulse oximeter accuracy. The cohort consisted of 88 subjects, with a mean age of 57 years (19 – 89). The mean difference (SpO2 – SaO2) was 2.75% and the standard deviation of the differences was 3.1%. Subgroup analysis demonstrated that hypoxemia (SaO2 < 90) significantly affected pulse oximeter accuracy. The mean difference was 4.9% in hypoxemic patients and 1.89% in non-hypoxemic patients (p < 0.004). In 50% (11/22) of cases in which SpO2 was in the 90-93% range the SaO2 was <90%. Though pulse oximeter accuracy was not affected by acidoisis, hyperlactatementa, anemia or vasoactive drugs, these factors worsened precision. Pulse oximetry overestimates ABG-determined SaO2 by a mean of 2.75% in emergency department patients with severe sepsis and septic shock. This overestimation is exacerbated by the presence of hypoxemia. When SaO2 needs to be determined with a high degree of accuracy arterial blood gases are recommended.
____
Pulse oximetry in critical care:
Pulse oximetry is a routine part of the monitoring and management of critically ill patients. Studies have proposed that specific pulse oximeter oxygen saturations (SpO2) be targeted to decrease the likelihood of hypoxemia, to titrate fractional inspired oxygen, and to wean mechanical ventilation. The accuracy of pulse oximetry to estimate arterial oxygen saturation (SaO2) in critically ill patients has yielded mixed results. Both the degree of inaccuracy, or bias, and its direction has been inconsistent. In addition, while certain studies of critically ill patients have demonstrated that hypoxemia, anemia, requirement for vasoactive drugs, and acidosis influence the accuracy of pulse oximetry, others have not. Data on the effects of other physiologic derangements, such as hyperlactatemia and bacteremia, are absent. Pulse oximeters utilize the pulsatile nature of arterial blood flow to distinguish it from venous flow and estimate oxygen saturation in arterial blood. Processes that increase venous blood flow or alter pulsatility can interfere with the ability of pulse oximeters to estimate arterial oxygen saturation. Hemodynamic derangements in septic patients, such as arteriovenous shunting, cutaneous arteriolar dilation and decreased vascular resistance can alter pulsatility and venous blood flow and therefore theoretically affect pulse oximeter accuracy. When reproduced in healthy volunteers, cutaneous vasodilation has been shown to interfere with the pulse oximetry signal and significantly decrease its accuracy. This has also been demonstrated in animal models of severe sepsis.
_
Because such recent oxygen therapies substitute the SpO2 for SaO2, the accuracy of pulse oximeters around 90% is crucial to avoid hypoxemia, but some studies suggest that SpO2 overestimates SaO2, especially in patients with critically illnesses. In a retrospective study including patients with septic shock, Wilson et al. reported that the mean bias (SpO2-SaO2) was positive and 2.75 +/- 3.1%. Wilson et al. also showed that among patients with 90%-93% SpO2 value, 50% of patients were with hypoxemia (SaO2< = 90%). Jubran et al. retrospectively evaluated patients in the ICU and found that the cut-off value of SpO2 to detect hypoxemia (SaO2< = 90%) should be 94%. These results alert the possibility that SpO2 overestimates SaO2 in the ICU, and a cut-off value of SPO2< = 90% may leave patients at risk for hypoxemia. Because each pulse oximeter follows different algorithms, it is necessary to define optimal SpO2 values to avoid hypoxemia by gathering SaO2 and SpO2 data prospectively from patients in the ICU. Of note, patients in the ICU have different backgrounds and frequently have hemodynamic instability and hypoxemia. Studies have shown that these factors influence the SpO2 values. Therefore, patients with poor oxygenation and without hemodynamic instability, hypercapnia and acidosis may be ideal candidates for defining optimal SpO2 values to avoid hypoxemia.
_
Accuracy of pulse oximetry in the intensive care unit: a 2001 study:
Pulse oximetry (SpO2) is a standard monitoring device in intensive care units (ICUs), currently used to guide therapeutic interventions. Few studies have evaluated the accuracy of SPO2 in critically ill patients. One hundred two consecutive patients admitted to the ICU in whom one or serial arterial blood gas analyses (ABGs) were performed and a reliable pulse oximeter signal was present. For each ABG, authors collected SaO2, SpO2, the type of pulse oximeter, the mode of ventilation and requirement for vasoactive drugs. Three hundred twenty-three data points were collected. The mean difference between SpO2 and SaO2 was -0.02% and standard deviation of the differences was 2.1%. From one sample to another, the fluctuations in SpO2 to arterial saturation difference indicated that SaO2 could not be reliably predicted from SPO2 after a single ABG. Subgroup analysis showed that the accuracy of SpO2 appeared to be influenced by the type of oximeter, the presence of hypoxemia and the requirement for vasoactive drugs. Finally, high SpO2 thresholds were necessary to detect significant hypoxemia with good sensitivity. Large SpO2 to SaO2 differences may occur in critically ill patients with poor reproducibility of SpO2. A SpO2 above 94% appears necessary to ensure a SaO2 of 90%.
_______
_______
Pulse oximetry in COPD, Asthma and other respiratory illnesses:
Chronic respiratory diseases such as COPD and asthma are among the most common health conditions seen in primary care practices, affecting more than 1 billion patients worldwide. Primary care clinicians are also often the first point of contact for patients suffering from acute respiratory infections such as influenza and pneumonia. These health care professionals need tools to help them evaluate, monitor, and decide when to refer patients with respiratory conditions. In patients with COPD, pulse oximetry is useful in stable patients with severe disease (FEV1 < 50% predicted), and in patients with worsening symptoms or other signs of an acute exacerbation, as a tool for patients to use at home to assist with their management under physician guidance. It is important to note that pulse oximetry complements, rather than competes with, spirometry in the assessment of COPD patients. Spirometry remains the gold standard for diagnosing and staging COPD, while pulse oximetry provides a method for rapid assessment especially of short-term respiratory compromise. In patients with asthma, pulse oximetry complements peak flow meters in assessing the severity of asthma attacks/exacerbations and response to a treatment.
_
Clinical Questions:
1. In patients with chronic obstructive pulmonary disease, is pulse oximetry effective in assessing the need for long-term oxygen therapy (LTOT), compared to arterial blood gas?
2. In patients with asthma, is oxygen saturation monitoring by pulse oximetry an objective measure of acute asthma severity compared to peak expiratory flow rate?
3. In patients with community-acquired pneumonia does pulse oximetry accurately stratify patients requiring hospital admission compared to signs and symptoms alone?
_
Answers to clinical questions:
1. In terms of COPD, studies suggest that pulse oximetry is not a reliable method alone for diagnosis. COPD is currently diagnosed based on clinical features along with spirometry, where a ratio of forced expiratory volume in 1 second (FEV1) to forced vital capacity (FVC) of less than 0.7 indicates airway obstruction. Oxygen saturations are not useful for diagnosis of COPD; saturations of <98% had sensitivity of 79%, but specificity of only 37%. However, pulse oximetry could have a valuable role in determining long-term oxygen therapy criteria in patients with COPD, and in indicating the need for referral to hospital in acute exacerbations.
2. The 2008 British Thoracic Society (BTS) guideline on the management of asthma and the Scottish Intercollegiate Guidelines Network recommend SpO2 monitoring by pulse oximetry as an objective measure of acute asthma severity, particularly in children, in both primary and secondary care. In children who require oxygen, pulse oximetry is recommended to determine the adequacy of oxygen therapy and the need for ABG analysis. According to these guidelines, a SpO2 <92% is considered life threatening and these patients require an ABG measurement. What is less clear is how useful SpO2 is compared to other measures of asthma severity in primary care, such as peak flow or clinical assessment.
3. Studies into the diagnosis of community acquired pneumonia (CAP) have indicated the identification of arterial hypoxaemia has direct treatment implications, including the delivery of supplemental oxygen and hospitalisation, for more intensive clinical observation. The routine use of pulse oximetry in patients suspected of having CAP would detect clinically unrecognised hypoxaemia, thereby identifying patients requiring hospitalisation. A 2004 update of the BTS guideline for the management of CAP in adults recommended pulse oximetry, with appropriate training, should become increasingly available to GPs responsible for the assessment of patients in the out-of-hours setting, for assessment of severity and oxygen requirement for patients with CAP and other acute respiratory illnesses. The extent to which SpO2 sats provide diagnostic information that complements clinical assessment of children by GPs is not known. NICE lists SpO2 <95% as an amber flag feature in assessing children with acute febrile illness. This guideline also recommends measuring heart rate in children with acute illness. Accurate measurement of heart rate in children is difficult using non-electronic methods; however, its added value as a vital sign in children is still unclear in primary care.
_
What is the normal range for pulse oximeter readings in a patient with COPD?
The patient with COPD probably lives with an O2 saturation of 88- 90(with the help of O2). His PaO2 is less than 80mm. He probably never reaches a normal O2 level. However, he has learned to live with these low values. He has adjusted to a life with less O2 and more CO2 on board. He eventually, over years, becomes exhausted and O2 sats will gradually drop in end-stage COPD. There is no set range specifically for COPD patients. However, if the patient has COPD with CO2 retention you generally want to keep SpO2 around 90-92% so you do not knock out there hypoxic drive.
_
Home overnight pulse oximetry (OPO) has been used to evaluate nocturnal desaturation in patients with chronic obstructive pulmonary diseases (COPD). However, Lewis et al (2003) found that nocturnal desaturation in patients with COPD exhibited marked night-to-night variability when measured by home OPO. A single home OPO recording may be insufficient for accurate assessment of nocturnal desaturation. Gay (2004) stated that for COPD patients who exhibit more profound daytime hypercapnia, polysomnography is preferred over nocturnal pulse oximetry to rule out other co-existing sleep-related breathing disorders such as OSA (overlap syndrome) and obesity hypoventilation syndrome. An interesting observation was the presence of a moderate to strong correlation between the severity of airflow obstruction (FEV1 % predicted) and SpO2 in the COPD patients who presented with an acute exacerbation or worsening of dyspnoea (r = 0.55 and r = 0.31, respectively), whereas no relevant correlation was observed in the patients with stable COPD (r = 0.19). These observations suggest that with regard to primary care COPD, pulse oximetry is mainly useful in patients with (very) severe airflow obstruction (FEV1 % predicted ≤50%) and worsening of symptoms. This coincides with previous observations from a Spanish study in stable COPD patients, which showed that the rate of tests with SPO2 ≤92% increases when the FEV1 % predicted value is <50%.
__
Current Clinical Uses of Pulse Oximetry in Primary Care COPD:
A. Stable disease:
• Establishing a baseline value in patients with stable disease.
• Monitoring of patients with exercise-related dyspnea.
• In patients with moderate to severe COPD, a screening tool to identify patients (i.e., those with SpO2 < 92%) who should be referred for comprehensive oxygen assessment.
• In patients with stable COPD or those recovering from an exacerbation at home, an SpO2 88% or less is a strong indication to initiate long-term oxygen therapy. However, ideally the decision to initiate oxygen therapy should be made based on arterial oxygen tension (PaO2 < 7.3 kPa / 55 mm Hg).
• Titrating oxygen flow setting in patients on long-term oxygen therapy, provided their disease is stable and they have good circulation. In general, the goal should be to maintain SpO2 > 90% during all activities.
• Evaluation of patients with severe disease (FEV1 < 50% predicted), cyanosis, or cor pulmonale for possible respiratory insufficiency/failure.
B. Exacerbations:
• Assessment of patients with acutely worsening symptoms, especially dyspnea, and determination of the severity of the exacerbation.
• Triage for arterial blood gas measurement, referral to emergency department, and/or determination of whether to initiate oxygen therapy or other treatment for exacerbation.
• Monitoring patients after the initiation of oxygen therapy. Measure SpO2 regularly—every 5 to 30 minutes, especially if the patient’s clinical condition deteriorates. For patients at risk of hypercapnic respiratory failure, aim to maintain SpO2 88-92%; for all other patients, aim for SpO2 94-98%.
• Evaluating patients for initiation of hospital-at-home/intermediate care, and monitoring them once they are enrolled in this form of care.
_
The benefits of long-term oxygen therapy (LTOT) in patients with chronic obstructive pulmonary disease (COPD) have been reported by a number of investigators. Since the 1980s, domiciliary oxygen therapy has been generally accepted as an important part of the routine treatment of COPD patients with chronic severe hypoxaemia. The main indication for LTOT is a low arterial oxygen tension (PaO2), usually lower than 55 mmHg (7.3 kPa). The prescribed oxygen flow should increase PaO2 to at least 65 mmHg (8.7 kPa). The blood gas tensions used to qualify the patients for treatment are measured at rest. The oxygen flow rate is also adjusted in resting conditions. In some cases, arterial oxygen saturation (SaO2) during treadmill/cycle ergometer exercise or during sleep is also assessed, but rather to confirm the subject’s eligibility for LTOT than to establish the adequate oxygen flow rate. After the prescription of LTOT, the patients are followed in out-patient clinics or at home, and blood gas measurements are periodically performed at rest. Thus, there is no information about SaO2 in those patients during their daily activities at home. It is possible that some activities may cause important drops in SaO2, despite adequate oxygenation while resting 24 h.
_
How accurate are pulse oximeters in patients with acute exacerbations of chronic obstructive airways disease? A 2001 study:
In conclusion, there is not sufficient agreement for oxygen saturation measured by pulse oximetry to replace analysis of an arterial blood gas sample in the clinical evaluation of oxygenation in emergency patients with COPD. However, oxygen saturation by pulse oximetry may be an effective screening test for systemic hypoxia, with the screening cut-off of 92% having sensitivity for the detection of systemic hypoxia of 100% with specificity of 86%.
_
Ambulatory pulse oximetry monitoring in Japanese COPD outpatients not receiving oxygen therapy: a 2014 study:
This study aims to analyse the frequency of desaturation in COPD outpatients, and investigate whether the desaturation profile predicts the risk of exacerbation. The 24-hour ambulatory oximetry monitoring provided precise data regarding the desaturation profiles of COPD outpatients. Both daytime and night-time desaturations were infrequent. The proportion of ambulatory SpO2 values below 90% was not a significant predictor of exacerbation.
______
Six-Minutes Walk test:
Doctors often use an assessment called the six-minute walk test for patients with heart and lung disease, such as congestive heart failure (CHF), chronic obstructive pulmonary disease (COPD) and asthma. The test provides information regarding a patient’s functional capacity and response to therapy for a wide range of chronic cardiopulmonary conditions.
_
Chronic obstructive pulmonary disease (COPD) is a leading cause of morbidity and disability worldwide, and is predicted to become the third highest cause of death by 2020. Desaturation profiles during a 6-minute walk test (6MWT) may predict prognosis primarily in patients with severe COPD with a percent predicted forced expiratory volume in one second (FEV1) of <50%. Time to desaturation during a 6MWT also predicts desaturation time in 24-hour ambulatory oximetry monitoring primarily in moderately hypoxaemic COPD patients with a resting partial pressure of arterial oxygen (PaO2) between 60 and 70 mmHg. However, it remains unknown whether desaturation profiles measured by ambulatory oximetry can predict prognosis in COPD patients. Transient desaturations have been observed in patients with moderate to severe chronic pulmonary disorders, even without significant resting hypoxemia. Point measurements of resting oxygen saturation by pulse oximetry (SpO2) and PaO2, the conventional parameters used to determine requirements of long-term oxygen therapy, are not sufficient for assessment of desaturation during activities of daily living. Field walking tests such as the 6MWT, which is the standard test used for assessment of functional exercise tolerance, do not always provide a good reflection of variations in oxygen saturation, because most activities of daily living are performed at submaximal levels of effort. 6MWT results did not predict the degree of desaturation during defecation in patients with chronic respiratory failure. Conventional assessment methods are therefore not satisfactory for obtaining a comprehensive understanding of oxygen saturation throughout the day.
_
Oxygen desaturation during a 6 min walk test is a sign of nocturnal hypoxemia: a 2011 study:
Patients with chronic obstructive pulmonary disease (COPD) may experience sleep disordered breathing with nocturnal desaturation. Results from the present study suggest that monitoring oxygen saturation changes during a 6MWT is useful in helping to identify COPD patients who may experience significant nocturnal desaturation.
_______
Asthma:
Clinical findings are usually insufficient to properly determine the severity of acute asthma. Significant changes in lung function may be present despite the lack of clinical manifestation, as first reported in the 1970’s and confirmed by subsequent studies. The severity of acute asthma is classified as mild, moderate, severe, and very severe based on clinical and functional criteria, the most widely used being pulse oximetry (SpO2) and peak expiratory flow (PEF). Few reports are available about possible correlations between these two methods in children and adolescents. Although the Global Initiative for Asthma (GINA) states that measurements of lung function and oximetry are critical for patient assessment, it is not clear whether both methods should be included in the evaluation of acute asthma, since no critical comparison of the two measurements has been done.
_
Use of pulse oximetry in the hospital management of acute asthma in childhood: a 1993 study:
A post-nebulizer saturation of less than 91 % had a sensitivity of 100% [95% confidence interval (CI), (54–1001 with a specificity of 98%] (95% CI, 92–100) and a positive predictive value of 86% for severe asthma necessitating intravenous treatment.
_
Pulse oximetry in the evaluation of the severity of acute asthma and/or wheezing in children: a 1999 study:
SpO2 levels correlated positively with FEV1 and FVC (25-75) values, and negatively with clinical scores and heart rate. The data revealed that a clinical score greater than 3 and an SpO2 < 94% were associated with increased severity of the asthma attack. In addition, SpO2 levels < or = 92% were associated with a 6.3-fold greater relative risk for requiring additional treatment. Authors concluded that determination of oxygen saturation by pulse oximetry is helpful in monitoring the severity of an acute exacerbation of asthma and/or wheezing, and has a prognostic value.
_
Correlations between pulse oximetry and peak expiratory flow in acute asthma: a 2007 study:
The present prospective observational study was carried out to determine if there is correlation between pulse oximetry and peak expiratory flow determination in 196 patients with acute asthma aged 4 to 15 years diagnosed according to the Global Initiative for Asthma criteria. The results showed that one measure cannot substitute the other (Pearson’s coefficient <0.7), probably because they evaluate different aspects in the airways, suggesting that peak expiratory flow should not be used alone in the assessment of acute asthma in children and adolescents.
_
Role of pulse oximetry during an asthma attack:
• Evaluation and assessment of severity, complementing peak flow meter data.
• Triage for arterial blood gas measurement, referral to emergency department, and/or determining when to initiate acute oxygen therapy.
• Monitoring patients after the initiation of oxygen therapy or response to other therapy
• Particularly important in children with severe acute wheezing.
• Follow-up of patients after a severe or complicated exacerbation.
_
A National Heart, Lung and Blood Institute/World Health Organization Global Asthma Initiative Report concluded that pulse oximetry was not an appropriate method of monitoring patients with asthma. The report explained that, during asthma exacerbations, the degree of hypoxemia may not accurately reflect the underlying degree of ventilation-perfusion (V-Q) mismatch.
_______
_______
Foetal and paediatric pulse oximetry:
_
Foetal Pulse Oximetry:
There is a new intervention in maternity care. And it may very well reduce some the need for some caesarean sections due to unreliable FHR tracings. It is the Fetal Pulse Oximetry. Introduced in the 1990s and approved by the FDA in 2000, this technology is based on the same principle as adult pulse oximetry, which has become common-place in hospitals world-wide. Fetal oximetry is a developing technique that uses reflectance oximetry, using LEDs of 735nm and 900nm. The fetal oxygen monitor has a single-use, disposable sterile sensor which is inserted through the birth canal once the membranes have ruptured, the cervix is < 2 cm, fetus is at -2 station or below, and gestational age is at least 36 weeks. The sensor rests against the fetal cheek, forehead or temple and is held in place by the uterus. The oxygen saturation is displayed on the monitor screen as a percentage. The normal oxygen saturation for a baby in the womb, receiving oxygenated blood from the placenta, is usually between 30 and 70 percent. Varney cautions that when the fetal oxygen saturation remains less than 30% or the signal is unobtainable for more than 10 minutes, the need for intervention is present. However, some conditions may alter readings including fetal scalp edema, caput succedaneum, dark/thick/curly hair, or vernix. There has been some interest in the use of fetal pulse oximetry in combination with routine cardiotocography (CTG) monitoring, although its use does not reduce the operative delivery rate. Contraindications to fetal oxygen monitoring include placenta previa, a FHR pattern that clearly indicates immediate delivery, other reasons for immediate delivery such as profuse vaginal bleeding, maternal HIV, active genital herpes or Hepatitis B infections.
_
Paediatric pulse oximetry:
Accuracy of pulse oximetry in neonates, infants and children:
Pulse oximetry equipment is largely calibrated using adult patients. Various studies represent a comprehensive attempt to gain information on the accuracy of pulse oximetry devices in infants and children across a large range of oxygen saturations, child ages, and skin colors. The gold standard with which the instruments were compared was arterial oxygenation readings obtained by arterial blood gas measurements.
_
Normal oxygen saturation values in paediatric patients: a 2005 study.
Although SpO2 of 95% and 96% are adequate (i.e., not requiring acute oxygen therapy), these values are associated with higher rates of respiratory and cardiovascular illnesses and thus should be considered potentially abnormal. SpO2 of 97% is on the border of normal. Normal SpO2 can occur with respiratory and cardiovascular illnesses, but SpO2 less than 97% is associated with a higher risk of respiratory and cardiovascular illnesses.
_
Validation of oxygen saturation monitoring in neonates: a 2007 study.
The mean difference of oxygen saturation as determined by pulse oximetry and oxyhemoglobin in arterial blood samples was 2.5%. The safety limits for pulse oximeters are higher and narrower in neonates than in adults, and clinical guidelines for neonates may require modification.
_
Pulse oximeter accuracy and precision affected by sensor location in cyanotic children: a 2008 study.
Children’s digits are often too small for proper attachment of oximeter sensors, necessitating sensor placement on the sole of the foot or palm of the hand. No study has determined what effect these sensor locations have on the accuracy and precision of this technology. The objective of this study was to assess the effect of sensor location on pulse oximeter accuracy (i.e., bias) and precision in critically ill children. Co-oximeter-measured arterial oxygen saturation (SaO2) was compared with simultaneously obtained pulse oximetry saturations (SpO2). A total of 98 measurements were obtained, 48 measurements in the upper extremities (finger and palm) and 50 measurements in the lower extremities (toe and sole). The median Sao2 was 92% (66% to 100%). There was a significant difference in bias (i.e., average SpO2 – Sao2) and precision (+/-1 sd) when the sole and toe were compared (sole, 2.9 +/- 3.9 vs. toe, 1.6 +/- 2.2, p = .02) but no significant difference in bias and precision between the palm and the finger (palm, 1.4 +/- 3.2 vs. finger, 1.2 +/- 2.3, p = .99). There was a significant difference in bias +/- precision when the Sao2 was <90% compared with when Sao2 was >or=90% in the sole (6.0 +/- 5.7 vs. 1.8 +/- 2.1, p = .002) and palm (4.5 +/- 4.5 vs. 0.7 +/- 2.4, p = .006) but no significant difference in the finger (1.8 +/- 3.8 vs. 1.1 +/- 1.8, p = .95) or toe (1.9 +/- 2.9 vs. 1.6 +/- 1.9, p = .65). The Philips M1020A pulse oximeter and Nellcor MAX-N sensors were less accurate and precise when used on the sole of the foot or palm of the hand of a child with an SaO2 <90%.
_
Pulse oximeter accuracy and precision at five different sensor locations in infants and children with cyanotic heart disease: a 2010 study:
Cyanotic heart disease patients pose a unique dilemma in terms of the reliability and precision of the pulse oximetry readings and the determination of the best location of the sensor, especially in infants. An understanding of the bias and precision of the pulse oximetry at various sensor sites would go a long way in the effective management of patients with cyanotic heart disease in the perioperative period. Authors strongly recommend that clinicians should verify the measurements by a co-oximeter and evaluate the pulse oximetry sensor used with the particular body site reliability indices to avoid any unacceptable over- or underestimation of the SaO2. This becomes even more relevant in hypoxemic patients with low SaO2 readings as the margin of safety is very small. Authors found that sole is the most accurate site of sensor location in cyanotic heart disease paediatric patients. Authors could also re-establish the finding that at low saturation states, pulse oximetry accuracy deteriorates and tends to overestimate the SaO2. In terms of reproducibility, the best sensor site could not be determined definitely and consistently in our study.
_
Accuracy of Pulse Oximetry in Children: a 2013 study:
The study objective was to measure the accuracy of pulse oximetry in the saturations from pulse oximetry (SpO2) range of 65% to 97%. This institutional review board–approved prospective, multicenter observational study in 5 PICUs included 225 mechanically ventilated children with an arterial catheter. With each arterial blood gas sample, SpO2 from pulse oximetry and arterial oxygen saturations from Co-oximetry (SaO2) were simultaneously obtained if the SpO2 was ≤97%. The lowest SPO2 obtained in the study was 65%. In the range of SpO2 65% to 97%, 1980 simultaneous values for SpO2 and SaO2 were obtained. The bias (SpO2 – SaO2) varied through the range of SpO2 values. The bias was greatest in the SpO2 range 81% to 85% (336 samples, median 6%, mean 6.6%, accuracy root mean squared 9.1%). SpO2 measurements were close to SaO2 in the SpO2 range 91% to 97% (901 samples, median 1%, mean 1.5%, accuracy root mean squared 4.2%). This study identified that the accuracy of pulse oximetry varies significantly as a function of the SpO2 range. Saturations measured by pulse oximetry on average overestimate SaO2 from Co-oximetry in the SpO2 range of 76% to 90%. Better pulse oximetry algorithms are needed for accurate assessment of children with saturations in the hypoxemic range.
______
Congenital heart disease (CHD):
Cardiovascular malformations are the commonest type of congenital malformation, but a sizeable proportion is not detected by routine neonatal examination. Cardiovascular malformations account for 6-10% of all infant deaths and 20-40% of deaths caused by congenital malformation. About 1-1.8 babies per 1000 live births have a duct dependent circulation, with a persistent ductus arteriosus being necessary for survival. These babies are at particular risk from the worldwide trend towards early discharge from maternity units, as the effects of ductal closure may not be apparent at an early discharge examination. Some 10-30% of babies who die from congenital heart disease do not have their condition diagnosed before autopsy. In Sweden over the past decade increasing proportions of babies with critical congenital heart disease have been leaving hospital with their condition undiagnosed. Screening infants with non-invasive measurement of oxygen saturation has been proposed as an aid for early detection of duct dependent circulation. Current routine screening for CHDs relies on a mid-trimester anomaly ultrasound scan in pregnant women, involving imaging of the heart chambers, and a postnatal clinical examination involving assessment of the cardiovascular system. Both of these have a relatively low detection rate and a number of babies are discharged from hospital before a CHD is diagnosed.
_
Routine neonatal examination fails to diagnose more than half of babies with heart disease; examination at 6 weeks misses one-third. Spending more time on physical examination is unrewarding as only milder cases of pulmonic stenosis and other relatively benign forms of CHD are diagnosed, which has little impact on the morbidity and mortality from undiagnosed CHD. Pulse oximetry can pick up lesions producing low oxygen saturation levels consequent to substantial abnormal mixing of systemic and pulmonary blood streams or critical obstructive duct-dependent lesions (mostly cyanotic CHD). Although it may fail to detect acyanotic CHD and critical CHD with non-critical obstruction or mixing, these lesions do not contribute to early mortality and morbidity. A recent systematic review of data from 229421 new born babies reported that pulse oximetry is having high specificity and acceptable sensitivity for detection of critical CHD. The false-positive rate for detection of critical congenital heart defects was particularly low when new born pulse oximetry was done after 24 h from birth than when it was done before 24 h. Although pulse oximetry is inexpensive and without side effects, it cannot detect CHD in every neonate with congenital heart disease, before they leave the hospital. Pulse oximetry is highly specific for detection of critical congenital heart defects with moderate sensitivity that meets criteria for universal screening. In a country with a huge population and poor prenatal diagnostic infrastructure, it is probably the best thing to do and should become a recommendation.
_
Critical Congenital Heart Disease (CCHD):
According to the Centers for Disease Control and Prevention (CDC), congenital heart defects account for 24% of infant deaths due to birth defects. In the United States, about 4,800 (or 11.6 per 10,000) babies born every year have CCHDs. Babies with a CCHD are at significant risk for death or disability if their CCHD is not diagnosed and treated soon after birth. Pulse oximetry, which is a test to determine the amount of oxygen in the blood, is the recommended screening method to detect CCHDs in newborns.
There are seven defects classified as CCHD:
• Hypoplastic left heart syndrome
• Pulmonary atresia (with intact septum)
• Tetralogy of Fallot
• Total anomalous pulmonary venous return
• Transposition of the great arteries
• Tricuspid atresia
• Truncus arteriosus
_
Gold standard:
Postnatal echocardiography is well established as the gold standard for diagnosing CHDs. However, it has to be remembered that, as studies of prevalence show, echocardiography may also contribute to an apparent rising incidence of CHDs mainly as a result of the detection of abnormalities which are of no functional or clinical significance. As a result, echocardiography is likely to have significant limitations as a screening tool, mainly because of the high false positive rate, but also as a result of cost and lack of availability of trained personnel to perform the examinations
_
Pulse oximetry:
The rationale for pulse oximetry screening is based on the fact that hypoxaemia is present, to some degree, in the majority of CHDs. This may result in obvious cyanosis; however, mild degrees of hypoxaemia cannot be detected by clinical observation, even by experienced clinicians. The difficulty is exacerbated in infants with pigmented skin.
_
A common feature of many forms of congenital heart disease is hypoxemia. Hypoxemia results from the mixing of systemic and venous circulations or parallel circulations as one might see in dextro-transposition of the great arteries. Hypoxemia may result in obvious cyanosis. However, generally, 4 to 5 g of deoxygenated hemoglobin is needed to produce visible central cyanosis, independent of hemoglobin concentration. For the typical newborn with a hemoglobin concentration of 20 g/dL, cyanosis will only be visible when arterial oxygen saturation is <80%; if the infant only has a hemoglobin concentration of 10 g/dL, the saturation must be <60% before cyanosis is apparent. Importantly, those children with mild hypoxemia, with arterial oxygen saturation of 80% to 95%, will not have visible cyanosis. Moreover, the identification of cyanosis is particularly problematic in black and Hispanic neonates because of skin pigmentation.
_
Pulse Oximetry Screening of Newborns:
In the fall of 2011, universal pulse oximetry screening of newborns was recommended by Secretary Kathleen Sebelius of the Department of Health and Human Services, the American Academy of Paediatrics, the American College of Cardiology and the American Heart Association. The objective is to prevent morbidity and mortality associated with unrecognized critical congenital heart disease. The guideline recommends screening of all newborns in the well-baby or intermediate-care nursery between 24 and 48 hours of age, or as close as possible to discharge if the newborn is discharged prior to 24 hours of age. False positives increase when screening is performed before 24 hours of age or when the newborn is asleep. Currently, CCHD is not detected in some newborns until after their hospital discharge, which results in significant morbidity and occasional mortality. Furthermore, routine pulse oximetry performed on asymptomatic newborns after 24 hours of life, but before hospital discharge, may detect CCHD. Routine pulse oximetry performed after 24 hours in hospitals that have on-site paediatric cardiovascular services incurs very low cost and risk of harm.
_
How should failed screens be handled?
Failed screens should be resolved prior to discharge by echocardiography; discussion with a pediatric cardiologist prior to obtaining an echocardiogram is strongly recommended.
_
What is the sensitivity of the screen?
An estimated 1/500 to 1/1,000 newborns will fail the screen; 20% to 25% of those that fail will have critical congenital heart disease. The screen has a sensitivity of 60% to 75% for critical congenital heart disease, and thus a normal screen does not rule out heart disease.
_
When should babies be screened?
Many normal newborns have oxygen saturations lower than 95 to 100 percent in the first hours of life as their bodies adjust to life outside the womb. By 24 hours of life this transition period should be done and oxygen saturations should be 95 percent or greater. Pulse oximetry screening should always be done after 24 hours to avoid falsely labelling a baby as failing the screening test. Some babies require supplemental oxygen after they are born. In this case, screening should be delayed until the baby no longer needs extra oxygen. If a baby is going home on supplemental oxygen, pulse oximetry screening for CCHD should be done prior to discharge.
_
Where should babies be screened?
A pulse oximetry probe will measure the oxygen saturation in the right hand and in either of the feet. Measuring in these two places gives a more accurate picture of the function of the heart. Right upper extremity probe attachment is pre-ductal location giving more accurate result.
_
How are babies screened?
“Two Sites, Three Strikes” is the easiest way to understand CCHD screening:
Two Sites- A pulse oximetry probe will measure the oxygen saturation in the right hand and the right or left foot. Measuring in these two places gives a more accurate picture of the function of the heart.
Three Strikes -A baby has three chances to pass pulse oximetry screening unless they are found to have very low oxygen saturation (less than 90 percent) in the hand or the foot at any point in the screening process.
_
How does a baby pass or fail the screen?
Pass- Pulse oximetry reading greater than 95 percent in either hand or foot and difference between hand and foot less than or equal to 3 percent is an immediate pass and no further testing is needed.
Fail- Pulse oximetry reading less than 90 percent anywhere anytime is an immediate fail and baby requires further evaluation. Learn more about a failed screening. Repeat if the pulse oximetry reading is between 90 and 94 percent in right hand and foot or if there is greater than 3 percent difference between two sites, the screen will be repeated one hour later. At the repeat screen the baby can pass, fail, or require one more repeat screen an hour later. After the third screen the baby must either pass or fail. Pulse oximetry between 90 and 94 percent in right hand and foot or greater than 3 percent difference between two sites on the third screen is considered a fail.
_
_
Accuracy of pulse oximetry in screening for congenital heart disease in asymptomatic newborns: a systematic review of 2007.
Eight studies were included with a total of 35960 newborns. Pulse oximetry was performed on asymptomatic newborns in all studies; three studies excluding newborns with an antenatal diagnosis of congenital heart disease. Either functional or fractional oxygen saturation was measured by pulse oximetry with oxygen saturation below 95% as the cut‐off level in most studies. On the basis of the eight studies, the summary estimates of sensitivity and specificity were 63% (95% CI 39% to 83%) and 99.8% (95% CI 99% to 100%), respectively, yielding a false positive rate of 0.2% (95% CI 0% to 1%). Pulse oximetry was found to be highly specific tool with very low false positive rates to detect congenital heart disease. Large, well‐conducted prospective studies are needed to assess its sensitivity with higher precision.
_
Impact of pulse oximetry screening on the detection of duct dependent congenital heart disease: a Swedish prospective screening study in 39821 newborns: a 2009 study.
Introducing pulse oximetry screening before discharge improved total detection rate of duct dependent circulation to 92%. Such screening seems cost neutral in the short term, but the probable prevention of neurological morbidity and reduced need for preoperative neonatal intensive care suggest that such screening will be cost effective long term.
_
Pulse oximetry as a screening test for congenital heart defects in newborn infants: a 2012 study.
Fifty-three of the 20,055 babies screened had a major CHD (24 critical and 29 serious), a prevalence of 2.6 per 1000 live births. Pulse oximetry had a sensitivity of 75.0% [95% confidence interval (CI) 53.3% to 90.2%] for critical cases and 49.1% (95% CI 35.1% to 63.2%) for all major CHDs. Pulse oximetry is a simple, safe, feasible test that is acceptable to parents and staff and adds value to existing screening. It is likely to identify cases of critical CHDs that would otherwise go undetected. It is also likely to be cost-effective given current acceptable thresholds. The detection of other pathologies, such as significant CHDs and respiratory and infective illnesses, is an additional advantage. Other pulse oximetry techniques, such as perfusion index, may enhance detection of aortic obstructive lesions.
_
Pulse oximetry with clinical assessment to screen for congenital heart disease in neonates in China: a prospective study of 2014:
Several pioneering studies have provided evidence for the introduction of universal pulse oximetry screening for critical congenital heart disease. However, whether the benefits of screening reported in studies from high-income countries would translate with similar success to low-income countries is unknown. Authors assessed the feasibility and reliability of pulse oximetry plus clinical assessment for detection of major congenital heart disease, especially critical congenital heart disease, in China. In the pilot study, 6785 consecutive newborn babies were screened; 46 of 49 (94%) cases of asymptomatic major congenital heart disease and eight of eight (100%) cases of asymptomatic critical disease were detected by pulse oximetry and clinical assessment. In the prospective multicentre study, we screened 122738 consecutive newborn babies (120707 asymptomatic and 2031 symptomatic), and detected congenital heart disease in 1071 (157 critical and 330 major). In asymptomatic newborn babies, the sensitivity of pulse oximetry plus clinical assessment was 93·2% (95% CI 87·9–96·2) for critical congenital heart disease and 90·2% (86·4–93·0) for major disease. The addition of pulse oximetry to clinical assessment improved sensitivity for detection of critical congenital heart disease from 77·4% (95% CI 70·0–83·4) to 93·2% (87·9–96·2). The false-positive rate for detection of critical disease was 2·7% (3298 of 120 392) for clinical assessment alone and 0·3% (394 of 120 561) for pulse oximetry alone. Pulse oximetry plus clinical assessment is feasible and reliable for the detection of major congenital heart disease in newborn babies in China. This simple and accurate combined method should be used in maternity hospitals to screen for congenital heart disease.
_
Use signal extraction technology for neonatal pulse oximetry:
The CCHD workgroup cited the results of two large, prospective studies of 59,876 subjects that exclusively used signal extraction technology to increase the identification of CCHD with minimal false positives. The CCHD workgroup recommended newborn screening be performed with motion tolerant pulse oximetry that has also been validated in low perfusion conditions. In 2014, a third large study of 122,738 newborns (discussed above) that also exclusively used signal extraction technology showed similar, positive results as the first two large studies.
_
Limitations to newborn pulse oximetry in detection of CCHD:
There are technical limitations to oximetry measurement in the newborn. As discussed earlier, the mean SpO2 in the newborn at >24 hours of age is 97% to 98%; however, when continuous pulse oximetry is used, multiple investigators have demonstrated periodic and/or sustained desaturation below 95% during sleep, feeding, and crying. Sustained rather than variable hypoxemia is consistent with the diagnosis of cyanotic congenital heart disease. Low oximetry readings in the setting of normal arterial oxygen saturation have been reported by multiple investigators. In fact, falsely low oximetry readings in the newborn population are known to be associated with low peripheral perfusion and motion artifact, probe placement site and partial probe detachment, and hyperbilirubinemia or dyshemoglobinemias. It is known that technical differences between the various types of oximeters in general use include measurement of functional or fractional oxygen saturation, preset signal-averaging times, and methods for the exclusion of motion artifact. There has been some research into the variability among various commercially available pulse oximeters; however, most of the variability occurs in the cyanotic range (<90%) or at the highest saturations (99% to 100%). The peak performance of the commercially available oximeters occurs in the range of 92% to 97%. Therefore, in the critical range for oximetry screening (94% to 97%), the variability of the most commonly used oximeters should be negligible. There has also been concern that pulse oximeters may not be as accurate in darkly pigmented adults and children. At low SpO2 levels (<70%), commercially available oximeters appear to overestimate arterial saturation by 3% in darkly pigmented subjects. However, when SpO2 is >90%, measurement bias related to skin pigmentation appears negligible (<0.2%). Lastly, the quality of oximetry measurements may be lower when performed in a screening setting.
________
Disease-Specific Applications of pulse oximetry in paediatric practice:
Respiratory Applications:
In paediatric practice, pulse oximetry must be readily available in any situation associated with hypoxemia. Oxygen saturation is a particularly sensitive indicator of disease severity in conditions associated with ventilation/perfusion (V/Q) mismatch, such as exacerbations of asthma or chronic lung disease of prematurity, acute bronchiolitis, and pneumonia. Conversely, SpO2 is not a reliable indicator of disease severity in proximal (laryngeal or tracheal) airway obstruction such as acute laryngotracheitis, foreign-body aspiration, and vocal cord dysfunction. The principle mechanism of hypoxemia in such cases is hypoventilation, which primarily leads to an increase in PaCO2. These patients might not present with particularly low SpO2 readings. Current guidelines state that oxygen saturation should be monitored by pulse oximetry during asthma exacerbations to assess severity of the disease and response to treatment. Mild asthma exacerbations are associated with SpO2 values of >95%, moderate exacerbations with values of 90% to 95%, and severe exacerbations with values of <90%. Although SpO2 values of <92% at presentation have been suggested to predict hospitalization or return to the hospital, more recent studies have not confirmed this finding. Instead, a 1-hour post-treatment SpO2 of <92% to 94% has been shown to be a better predictor of the need for hospitalization. To date, there is no consensus on the SpO2 thresholds that should be used to admit, treat, and discharge infants with acute bronchiolitis. The American Academy of Paediatrics guideline recommends administration of supplemental oxygen if SPO2 values fall to <90. Pulse oximetry is essential for prompt detection and management of pediatric pneumonia, because infants and children might not appear cyanotic despite significant hypoxemia. The British Thoracic Society guideline for the management of community-acquired pneumonia recommends that symptomatic infants and children with an SpO2 of ≤92% should be treated with oxygen and admitted to the hospital.
_
Cardiovascular Applications:
Pulse oximetry can be used for heart rate monitoring or might serve more specialized applications, such as the assessment of peripheral perfusion and hemodynamic status. The plethysmographic waveform has been shown to be useful in the estimation of blood pressure when manometry fails. It can also offer a semi-quantitative evaluation of “pulsus paradoxus” by identifying an exaggerated decrease of pulse-wave amplitude during inspiration.
_
Neonatal Resuscitation:
Assessment of skin color is not a reliable indicator of oxygenation status during the immediate postnatal period. Moreover, the optimal management of oxygenation during neonatal resuscitation is critical, because there is strong evidence that both hypoxia and hyperoxia can be harmful. The feasibility and reliability of pulse oximetry during neonatal resuscitation have been proven in several studies. Thus, SpO2 monitoring in the delivery room is currently recommended for neonates with persistent cyanosis, when assisted ventilation and supplementary oxygen administration are required, or when neonatal resuscitation is anticipated (high-risk deliveries). Under acceptable conditions of peripheral perfusion, SpO2 values can be reliably measured ∼2 minutes after birth. Use of new-generation devices and sensors of appropriate size, as well as probe attachment to a preductal location (i.e., right upper extremity), preferably before connecting the probe to the device, might result in more accurate and timely readings. However, health care professionals should be aware that, even in uncompromised neonates, an increase in SpO2 at levels of >90% might take >10 minutes to achieve. Therefore, pulse oximetry should be used in conjunction with, but not as a substitute for, clinical assessment during the transitional period after birth.
_
Neonatal Screening for Congenital Heart Disease—already discussed vide supra:
_
Prevention of Hyperoxia:
Although for ventilator-dependent patients pulse oximetry can assist in the titration of inspired oxygen concentration, it cannot reliably prevent hyperoxic events. SpO2 values of >92% do not accurately correlate with PaO2, as is clearly depicted by the shape of the Oxygen dissociation curve. At such high SpO2 values, small variations of SpO2 might relate to disproportionally wider variations of PaO2. Therefore, caution is required when interpreting pulse-oximetry readings in situations in which hyperoxia is to be avoided, especially in case of preterm and low birth weight neonates for whom excessive oxygen administration can be particularly harmful. Although a single best range has not been established yet, there is convincing evidence that SpO2 values between 85% and 93% are sufficient to maintain normoxemia and to decrease the incidence of retinopathy of prematurity in infants receiving supplemental oxygen. In extremely preterm neonates, however, lower SpO2 targets (i.e., 85%–89%) have been associated with an increased risk of mortality compared with higher SpO2 levels (i.e., 91%–95%). To limit oxygen toxicity in premature neonates, supplemental oxygen can be tapered to maintain an oxygen saturation of 90% – thus avoiding the damage to the lungs and retinas of neonates. Although pulse oximeters are calibrated for adult haemoglobin, HbA, the absorption spectra of HbA and HbF are almost identical over the range used in pulse oximetry, so the technique remains reliable in neonates.
_
Can we replace Arterial Blood Gas Analysis by Pulse Oximetry in Neonates with Respiratory Distress Syndrome: a 2015 study:
Neonates with respiratory distress syndrome (RDS) require arterial blood gas (ABG) analysis to decide on appropriate management. Authors conducted this study to investigate the validity of pulse oximetry instead of frequent ABG analysis in the evaluation of these patients. From a total of 193 blood samples obtained from 30 neonates <1500 grams with RDS, 7.2% were found to have one or more of the followings: acidosis, hypercapnia, or hypoxemia. Authors found that pulse oximetry in the detection of hyperoxemia had a good validity to appropriately manage patients without blood gas analysis. However, the validity of pulse oximetry was not good enough to detect acidosis, hypercapnia, and hypoxemia.
_________
_________
Other uses of pulse oximetry:
_
Blood volume and blood pressure estimation:
Photoplethysmography:
A photoplethysmogram (PPG) is an optically obtained plethysmogram, a volumetric measurement of an organ. A PPG is often obtained by using a pulse oximeter which illuminates the skin and measures changes in light absorption. A conventional pulse oximeter monitors the perfusion of blood to the dermis and subcutaneous tissue of the skin. With each cardiac cycle the heart pumps blood to the periphery. Even though this pressure pulse is somewhat damped by the time it reaches the skin, it is enough to distend the arteries and arterioles in the subcutaneous tissue. If the pulse oximeter is attached without compressing the skin, a pressure pulse can also be seen from the venous plexus, as a small secondary peak. The change in volume caused by the pressure pulse is detected by illuminating the skin with the light from a light-emitting diode (LED) and then measuring the amount of light either transmitted or reflected to a photodiode. Each cardiac cycle appears as a peak. Because blood flow to the skin can be modulated by multiple other physiological systems, the PPG can also be used to monitor breathing, hypovolemia, and other circulatory conditions. While pulse oximeters are a commonly used medical device, the PPG derived from them is rarely displayed, and is nominally only processed to determine heart rate. PPGs can be obtained from transmissive absorption (as at the fingertip) or reflection (as on the forehead). In outpatient settings, pulse oximeters are commonly worn on the finger. However, in cases of shock, hypothermia, etc. blood flow to the periphery can be reduced, resulting in a PPG without a discernible cardiac pulse. In this case, a PPG can be obtained from a pulse oximeter on the head, with the most common sites being the ear, nasal septum, and forehead. PPGs can also be obtained from the vagina and esophagus.
_
PPG tracing:
Premature Ventricular Contraction (PVC) can be seen in the PPG just as in the ECG and the Blood Pressure (BP).
_
Because the skin is so richly perfused, it is relatively easy to detect the pulsatile component of the cardiac cycle. The DC component of the signal is attributable to the bulk absorption of the skin tissue, while the AC component is directly attributable to variation in blood volume in the skin caused by the pressure pulse of the cardiac cycle. The height of AC component of the photoplethysmogram is proportional to the pulse pressure, the difference between the systolic and diastolic pressure in the arteries. Shamir, Eidelman, et al. studied the interaction between inspiration and removal of 10% of a patient’s blood volume for blood banking before surgery. They found that blood loss could be detected both from the photoplethysmogram from a pulse oximeter and an arterial catheter. Patients showed a decrease in the cardiac pulse amplitude caused by reduced cardiac preload during exhalation when the heart is being compressed.
_
Use of Pulse Oximetry as a Noninvasive Indicator of Intravascular Volume Status: a 2013 study.
The use of pulse oximetery as a noninvasive method to assess intravascular volume status is described. Pulse oximeters providing a continuous display of the pulse waveform offer a new method of estimating relative volume status during positive-pressure ventilation. Like intraarterial pressure tracings, the peaks of the pulse waveform demonstrate increased variation in response to positive-pressure ventilation when a patient becomes hypovolemic. Pulse oximeter waveform tracings were compared with central venous pressure and intraarterial pressure tracings in 12 patients undergoing major operative procedures. A significant correlation (r = 0.61) was seen between pulse waveform variation and systolic pressure variation, which has previously been shown to be a sensitive indicator of hypovolemia. When data from individual patients were analyzed separately, the correlation between pulse waveform variation and systolic pressure variation was as high as 0.88.
_
Blood pressure measurement by pulse oximetry:
Recently, another method of measuring blood pressure non-invasively, using the pulse oximeter, has been reported. This requires a manual blood pressure cuff to be placed on the same extremity as the pulse oximeter probe. The pressure is recorded at disappearance and/or reappearance of the oximeter waveform display during cuff inflation/deflation, which approximates to systolic blood pressure. This was first described in 1987 after it was noted intraoperatively that the loss of the audio and visual oximeter (Nellcor Pulse Oximeter Model N-100) display correlated with the systolic blood pressure obtained by Doppler when the Doppler and pulse oximeter probes were on the same extremity. Subsequent studies have verified the usefulness of this methodology and have expanded it to use the disappearance and/or reappearance of the real time plethysmographic waveform available on many pulse oximeters.
_
One easy way to palpate a blood pressure is to place the pulse oximeter probe on a digit in the extremity in which you’re taking a blood pressure. Wait for a steady waveform and decent saturation reading, then inflate your BP cuff. Watch the numbers as the waveform disappears, and when it reappears during deflation. Those numbers are roughly equivalent to the systolic blood pressure reading you’d obtain during conventional palpation of a blood pressure. It can be done with a manual sphygmanometer and a hand-held pulse oximeter, but it is most easily accomplished using your cardiac monitor with integrated pulse oximetry and NIBP functions. It’s not as accurate as direct auscultation, but it’s quick, and far better than simply noting the presence or absence of a distal pulse when circumstances or ambient noise keep you from obtaining anything else.
_
Use of pulse oximetry for blood pressure measurement after cardiac surgery: a 1998 study:
Blood pressure measurement using pulse oximeter waveform change was compared with an oscillometric measurement and the gold standard, intra-arterial measurement, in children after cardiac surgery. Forty six patients were enrolled and divided into groups according to weight. Simultaneous blood pressure measurements were obtained from the arterial catheter, the oscillometric device, and the pulse oximeter. Pulse oximeter measurements were obtained with a blood pressure cuff proximal to the oximeter probe. The blood pressure measurements from the pulse oximeter method correlated better with intra-arterial measurements than those from the oscillometric device (0.77-0.96 v 0.42-0.83). The absolute differences between the pulse oximeter and intra-arterial measurements were significantly smaller than between the oscillometric and intra-arterial measurements in children less than 15.0 kg. The pulse oximeter waveform change is an accurate and reliable way to measure blood pressure in children non-invasively, and is superior to the oscillometric method for small patients.
_________
_________
Sleep medicine:
Obstructive sleep apnoea (OSA) occurs because sleep causes the muscle tone to relax and at the level of the throat, the human airway is composed of collapsible walls of soft tissue which can obstruct breathing during sleep. One of the most common symptoms being loud snoring associated with sleepless nights and sleepiness during the day times. The definite investigation for suspected obstructive sleep apnoea is Polysomnography, which is a detailed overnight sleep study that includes recording of EEG that permit the identification of sleep at various stages. Because polysomnography is a time-consuming and expensive test, an overnight recording of arterial oxygen saturation by Oximetry can be used to confirm the diagnosis and obviate the need for a full polysomnography, although a negative result doesn’t eliminate the diagnosis but rather mandates that a patients’ needs to do a polysomnography.
_
Overnight pulse oximetry:
In the past 5 years, debate has centered on the effectiveness of overnight pulse oximetry as a screening tool to identify patients with sleep-disordered breathing from the larger group of patients with simple snoring and those with excessive daytime sleepiness from other causes. This controversial discussion has arisen from needs to reduce the cost for diagnostic procedures in sleep disorders while technologic advances have made pulse oximeters handier, cheaper, and more reliable. Pulse oximetry is a well-established tool routinely used in many settings of modern medicine to determine a patient’s arterial oxygen saturation and heart rate. The decreasing size of pulse oximeters over recent years has broadened their spectrum of use. For diagnosis and treatment of sleep-disordered breathing, overnight pulse oximetry helps determine the severity of disease and is used as an economical means to detect sleep apnea. Overnight pulse oximetry is a very useful tool for the diagnosis of sleep-disordered breathing. Authoritatively establishing a final diagnosis is very difficult without oximetry data. As a screening tool for the diagnosis of OSA, pulse oximetry is cost-effective and shows substantial accuracy. Sensitivity and specificity remain controversial, however, and deserve further clarification through controlled studies. Technical limitations, limited user knowledge, and the lack of consensus on interpretation of data all play a role in diminishing the value of pulse oximetry as a diagnostic tool.
_
A flow diagram to delineate the clinical use of overnight pulse oximetry as a screening tool for sleep-disordered breathing:
In clinical practice, the number of desaturations per hour, oxygen desaturation index (ODI), is used as an important diagnostic criterion. The ODI is the number of times per hour of sleep that the SpO2 level drops by 3 percent or more from baseline. The ODI >10 demonstrated a sensitivity of 93% and a specificity of 75% to detect moderate and severe Sleep-disordered breathing.
_
Diagnosis of obstructive sleep apnoea using pulse oximeter derived photoplethysmographic signals: a 2014 study:
Increasing awareness of the high prevalence of obstructive sleep apnea (OSA) and its impact on health in conjunction with high cost, inconvenience, and short supply of in-lab polysomnography (PSG) has led to the development of more convenient, affordable, and accessible diagnostic devices. Authors evaluated the reliability and accuracy of a single-channel (finger pulse-oximetry) photoplethysmography (PPG)-based device for detection of OSA (Morpheus Ox). PPG-derived data compare well with simultaneous in-lab PSG in the diagnosis of suspected OSA among patients with and without cardiopulmonary comorbidities. Use of a device such as the PPG is attractive for a number of reasons. First, it requires minimal set-up, hence making home testing extremely convenient and simple. Second, its unobtrusive nature potentially allows more normal sleep compared to traditional diagnostic modalities. Finally the device’s relative low cost can facilitate its more widespread use as well as its application for several nights’ sleep, thus potentially improving the detection rate of OSA. These advantages clearly need to be matched by proven diagnostic efficacy.
_
High resolution pulse oximetry (HRPO) has been developed for in-home sleep apnoea screening and testing in patients for whom it is impractical to perform polysomnography. It stores and records both pulse rate and SpO2 in 1 second intervals and has been shown in one study to help to detect sleep disordered breathing in surgical patients. Pulse oximetry alone is not an efficient method of screening or diagnosing patients with suspected obstructive sleep apnea (OSA). The sensitivity and negative predictive value of pulse oximetry is not adequate to rule out OSA in patients with mild to moderate symptoms. Therefore, a follow-up sleep study would be required to confirm or exclude the diagnosis of OSA, regardless of the results of pulse oximetry screening. Overnight pulse oximetry is also commonly used for the evaluation of potential hypoxemia in COPD.
________
________
Dentistry:
Pulse Oximetry: A new tool in Pulpal Vitality Testing:
The assessment of pulp vitality is a crucial diagnostic procedure in the practice of endodontics. Conventionally, the dentist has relied on tests that depend on the patient’s perceived response to a stimulus as well as the dentist’s interpretation of that response. These methods include thermal stimulation (as in the case of heat or cold application), electric stimulation, or direct dentin stimulation (test cavity). A major shortcoming with the present pulp testing methods is that they indirectly monitor pulp vitality by measuring neural response, not vascular circulation. Stimulation of nerve fibers is not the ideal method to determine vitality status. Thus, vascular supply, not innervation, is the most accurate determinant for assessing pulp vitality. As a result, teeth that have temporarily or permanently lost their sensory function (e.g., teeth damaged by trauma) will be nonresponsive to these tests. However, they may have intact vasculature. Moreover, the nervous tissue, being highly resistant to inflammation, may remain reactive long after the surrounding tissues have degenerated. Therefore, thermal and electrical tests may give false-positive responses if only the pulp vasculature is damaged. Further, all these tests have the potential to produce an unpleasant and occasionally painful sensation, and inaccurate results may be obtained. Recent attempts to develop a method for determination of pulpal circulation have involved the use of laser Doppler flowmetry, dual-wavelength spectrophotometry, and pulse oximetry. Pulse oximetry can be used in endodontics for differential diagnosis of vital pulps and necrotic ones. This test produces no noxious stimuli, therefore, apprehensive or distressed patients may accept it more readily than routine methods.
_
The critical requirement of using pulse oximeter in dentistry is as follows.
1. Sensor should conform to the size, shape, and anatomical contours of teeth.
2. Light-emitting diode sensor and the photoreceptor should be as parallel as possible to each other so that the photoreceptor sensor receives the light-emitted from LED.
3. The sensor holder should allow firm placement of the sensor onto the tooth to obtain accurate measurements
_
_
Evaluation of efficacy of a new custom-made Pulse Oximeter Dental Probe in comparison with the Electrical and Thermal Tests for assessing Pulp Vitality: a 2007 study:
The sensitivity of the pulse oximeter was found to be 1.00, as compared to 0.81 with the cold test and 0.71 with the electrical test. The specificity of the pulse oximeter was 0.95, as compared to 0.92 with the cold and electrical pulp tests. Thus, the custom made pulse oximeter dental probe is an effective, accurate, and objective method of evaluating pulp vitality. This in vivo study showed that the custom-built PODP is an effective, accurate, and objective method of determining the vitality of permanent teeth.
__________
Testicular torsion:
Potential use of Pulse Oximetry for the Diagnosis of Testicular Torsion: a 2014 study:
Scrotal Doppler ultrasonography (scrotal US) has been commonly used for evaluating patients with suspected testicular torsion (TT). However, scrotal US is not available in all medical facilities. Comparatively, pulse oximetry is easily available at all institutions; it is used for monitoring pulse oximeter saturation (SpO2) with an accuracy equivalent to that of conventional arterial oxygen saturation (SaO2) and is the standard for noninvasive SaO2 monitoring in most medical facilities. Authors evaluated the SpO2 and pulse rate (PR) values on the scrotums of patients undergoing exploration for TT to determine whether these values are feasible for monitoring testicular viability in TT. The results demonstrate that SpO2 values and PRs were undetectable in all of the torsed testes, in contrast to that in normal subjects. However, it may be difficult to diagnose epididymal torsion compared with TT using pulse oximetry, as the epididymis is relatively difficult to locate owing to its small size. This shortcoming may be overcome with subsequent improvements in oximetry techniques.
_
The Sensor Pad attached on the Scrotal Skin Surface:
________
Peripheral vascular disease:
Pulse oximetry as a potential screening tool for lower extremity arterial disease in asymptomatic patients with diabetes mellitus: a 2005 study.
Lower extremity arterial disease (LEAD) is common and underdiagnosed in patients with diabetes mellitus and is associated with higher total mortality. Authors compared the accuracy of pulse oximetry, the ankle-brachial index (ABI), and the combination of the two to diagnose LEAD in consecutive outpatients with type 2 diabetes who had no symptoms of LEAD, in a primary care setting. Pulse oximetry of the toes seems as accurate as ABI to screen for LEAD in patients with type 2 diabetes. Combination of the two tests increases sensitivity.
_
A prospective comparison of bilateral photoplethysmography versus the ankle-brachial pressure index for detecting and quantifying lower limb peripheral arterial disease: a 2008 study:
This study prospectively assessed the diagnostic accuracy of a novel bilateral photoplethysmography toe pulse measurement technique for the detection of significant lower limb peripheral arterial disease. Bilateral photoplethysmography toe pulse measurements were compared with the ankle-brachial pressure index (ABPI) gold standard reference. Pulse wave analysis techniques extracted timing, amplitude, and shape characteristics for the great toes and their right-to-left side differences. These characteristics were compared with previously obtained normative ranges, and the accuracy was assessed for all significant disease (ABPI <0.9) and higher-grade disease (ABPI <0.5). The degree that pulse shape fell beyond the normal range of normalized pulse shapes was at the threshold of substantial to almost perfect agreement compared with ABPI for significant disease detection (diagnostic accuracy, 91% [kappa = 0.80]; sensitivity, 93%; specificity, 89%), and with 90% accuracy (kappa = 0.65) for higher-grade disease detection. Pulse transit time differences between right and left toes also had substantial agreement with ABPI, with diagnostic accuracy of 86% for significant disease detection (pulse transit time to pulse foot [kappa = 0.71] and to pulse peak [kappa = 0.70]) and reached at least 90% for these for the higher-grade disease. With the shape and pulse transit time measurements, the negative-predictive values of the 5% disease population screening-prevalence level were at least 99% and had positive-predictive values of at least 98% for the 90% disease-prevalence level for vascular laboratory referrals. This simple-to-use technique could offer significant benefits for the diagnosis of peripheral arterial disease in settings such as primary care where noninvasive, accurate, and diagnostic techniques not requiring specialist training are desirable. Improved diagnosis and screening for peripheral arterial disease has the potential to allow identification and risk factor management for this high-risk group.
_
Diagnostic importance of pulse oximetry in the determination of the stage of chronic arterial insufficiency (CAI) of lower extremities: a 2010 study:
The aim of this work was to determine the diagnostic importance of pulse oximetry in the early detection of stage of lower extremities CAI based on peripheral arterial oxygen saturation of haemoglobin (SpO2). Using pulse oximetry, depending on the stage of lower extremities CAI, authors revealed a considerable difference in the stages of functional ischemia. In 3 patients with gangrenous foot and fingers, SpO2 was immeasurable and progressive decrease in SpO2 of arterial capillaries (p < 0.01 between stages). Due to the reliability and simplicity of pulse oximetry it can be a routinely used diagnostic device for patients with early determined stage of lower extremities CAI.
_________
Collateral blood flow:
Pulse oximetry compared with Doppler ultrasound for assessment of collateral blood flow to the hand: a 2007 study:
Ischaemic injury to the hand after arterial cannulation is a rare but well documented complication and routine testing of the adequacy of collateral circulation is widely advocated. The widespread availability of the pulse oximeter in the operating theatre, its applicability in circumstances where the patient is unable to cooperate, and its dependence on pulsatile blood flow suggest that this device could potentially be usefully applied to the assessment of collateral blood flow. The reliability of the pulse oximeter to detect the presence or absence of collateral circulation was prospectively compared to Doppler ultrasound in 109 hands from 64 adult patients. Nine hands demonstrated inadequate ulnar collateral flow, one hand demonstrated inadequate radial collateral flow and a persistent median artery was found in one hand. In all patients the results of pulse oximeter testing (probe placed on the thumb) correlated precisely with the results obtained with the Doppler device (probe located over the lateral aspect of the superficial palmar arch). These results demonstrate pulse oximetry to be a reliable method of assessing collateral blood flow to the hand before arterial cannulation.
_
You can also use your pulse oximeter to continuously evaluate distal circulation in an injured extremity. If you’ve splinted a fractured limb, or applied a pressure dressing to a laceration, make it a point to place your pulse oximeter probe on a digit in the injured extremity. As long as it gives you a numerical readout and a waveform, you can reasonably assume that distal circulation is adequate.
_________
Pulse oximetry as screening tool of aspiration:
Dysphagia is common after stroke, occurring in 25% to 42% of patients. About one third of patients with dysphagia aspirate food or fluid into their airways, and in 40% of them aspiration is silent (i.e., it does not trigger a cough or cause symptoms or signs of distress). Detection of silent aspiration is important because aspiration often leads to such serious complications as pulmonary infections, septicemia, dehydration, and malnutrition. There are no reliable clinical signs of silent aspiration, and aspirating patients frequently do not complain of swallowing difficulties. Furthermore, bedside assessment of dysphagic patients, unless coupled with an objective method such as videofluoroscopy or nasal endoscopy, often fails to detect silent aspiration. Although nasal endoscopy detects silent aspiration in nearly all patients, the procedure requires a certain degree of expertise and is time consuming and sometimes poorly tolerated by patients. Similarly, videofluoroscopy is not suitable for routine clinical use, especially when repeated assessments of severely ill patients are required. In recent years, pulse oximetry has been advocated as an alternative to nasal endoscopy and videofluoroscopy for the assessment of dysphagic patients. It has been suggested that aspiration of food or fluid into the airways causes reflex bronchoconstriction that leads to ventilation-perfusion mismatch and oxygen desaturation of arterial blood, which can be readily measured by pulse oximetry. Pulse oximetry is noninvasive, simple, and repeatable, and it does not involve exposure to radiation. However, the value of this method in the diagnosis of silent aspiration has yet to be fully examined. In 49 patients with stroke, Zaidi et al studied oxygen saturation after the swallowing of 10 mL of water. They then compared the pulse oximetry results with the findings of bedside assessment by an independent speech and language therapist. The authors found a close correlation between aspiration as diagnosed clinically by the therapist and the drop in arterial blood oxygen saturation measured by pulse oximetry. However, the authors did not perform the dysphagia assessment simultaneously with the pulse oximetry. This poses a problem with the interpretation of their data, as aspiration may occur intermittently. Furthermore, the subjective clinical evaluation of dysphagia is unreliable: 42% to 60% of patients aspirating food or fluid are not recognized. Four studies compared oxygen saturation levels with video fluoroscopy, three being simultaneous. Of these, two have suggested that pulse oximetry may be useful in diagnosing aspiration. The others have been more cautious, but there is sufficient support to warrant further research. In a recent study, Colodny compared pulse oximetry with ®bre-optic endoscopic evaluation in 104 subjects and found no relationship between SpO2 levels and aspiration. She did, however, conclude that pulse oximetry may be used as an adjunct to discriminate dysphagia from non-dysphagia.
_
Pulse oximetry does not reliably detect aspiration on videofluoroscopic swallowing (VFSS) study: a 2014 study:
Simultaneously monitoring the arterial oxygen saturation (SpO2) by pulse oximetry is done while patients were performing VFSS. A decrease in SpO2 exceeding 3% was considered as significant desaturation. Bolus or portion of bolus passing through the vocal cords and entering the subglottic space was defined as aspiration on VFSS. The results of pulse oximetry and VFSS were compared. No significant correlation existed between desaturation measured by pulse oximetry and aspiration on VFSS (χ2 test, P=0.87). The positive predictive rate of pulse oximetry in detecting aspiration on VFSS was 39.1%, and the negative predictive rate was 59.4%. Aspiration occurring on VFSS cannot be predicted based on decrease in SpO2 in pulse oximetry. The application of pulse oximetry to detect aspiration during regular meals requires further investigation.
________
________
Accuracy of pulse oximetry:
Numerous studies have addressed the accuracy of pulse oximeters, primarily over the range of 70% to 100% saturation. Excellent correlation has been found between pulse oximetry and the “gold standard” in vitro Co-oximetry measurements. These have been found to be accurate for SpO2 from 70% to 100% and within ± 2%. For SpO2 above 70%, approximately 68% of the data will fall within ±2% of the actual saturation, and 95% of the data will fall within ±4% of the actual saturation. For example, in a patient with a pulse oximeter reading of 92%, 95% of the time the true SaO2 value, as measured by arterial blood gases, would be between 88% and 96%. For saturations below 70%, manufacturers generally state that accuracy is “unspecified.” Pulse – rate monitoring with pulse oximetry ranges from 20 to 30, to 250 beats per minute, with manufacturers accuracy statements indicating a range from ±1 to 2 beats per minute for the scale stated. Once in use, there is little evidence that pulse oximeters are ever re-calibrated or have their accuracy assessed. A high reliance is placed upon the continuing reliability of the wavelength of the light emitted from the LEDs. Should the wavelength of the light emitted by one or both LEDs alter, the degree of absorption will alter and the R value will change. The mathematical algorithm contained within the pulse oximeter software for the estimation of SpO2 will then be fed incorrect information, and an inaccurate estimation of SpO2 will be displayed on the monitor. This may in turn lead to incorrect diagnosis and treatment of a patient. The common manufacturing literature claim for accuracy for pulse oximeters is ± 2–3% SpO2 over a declared range of 70–100%, and the International Standard for pulse oximeter manufacture ISO 80601-2-61-2011 requires an accuracy of ≤ 4% error in this range.
_
Pulse oximeter accuracy, along with clinical reliability are the two most important parameters to consider when choosing a technology for the critical task of monitoring the oxygenation of patients. To establish their accuracy claims for market clearance by the FDA, pulse oximetry manufacturers provide data from studies done in their laboratory on healthy volunteers. In order for accuracy claims made by a manufacturer to be clinically meaningful they must be validated by independent, clinical research. It is not until the technology is tested by independent investigators on patients in clinical settings or on volunteers during challenging physiological conditions where the SpO2 readings are compared against arterial blood analysis, that the “working accuracy” of the pulse oximetry technology is truly revealed. Pulse oximetry estimates arterial hemoglobin oxygen saturation (SaO2) from the ratio of the pulsatile to the total transmitted red light divided by the same ratio for infrared light transilluminating a finger, ear, or other tissue. The SaO2 estimated by pulse oximetry (SpO2) may not be independent of skin pigmentation and many other variables, such as haemoglobin concentration, nail polish, dirt, and jaundice. So numerous factors can influence the accuracy of pulse oximeters in the clinical environment. During the empirical calibration of pulse oximeter systems, great care is taken to only use volunteers with normal levels of carboxyhemoglobin (COHb) and methemoglobin (MetHb) because values above 2 to 3% COHb and 1 to 1.5% MetHb seen clinically, will affect the accuracy of the SpO2 measurements. Additionally, body temperature can cause as much as a 3% difference in the SpO2 measurements. Digits that are warm (> 30 °C) may read 96 to 97% SPO2 while cold digits (< 20 °C) may read 99 to 100% SpO2 in the subject at the same PaO2. This phenomenon is thought to be due to arterial to venous (A-V) shunting in the digits. A-V shunts may be open in warm hands causing “venous pulsations” which result in a lower SPO2 compared to cold hands with no A-V shunting. That is why the empirical calibration is always done on normothermic volunteers. There are conflicting studies regarding the effect on skin pigment and painted fingernails on the accuracy of pulse oximeters. Thus numerous factors can cause the pulse oximeter system to exceed its specified accuracy in actual patients. Because all manufacturers submit similar data from normal healthy volunteers to the FDA for market clearance, one can expect pulse oximeters from various manufacturers to perform similarly on healthy subjects or patients who are not physiologically compromised. However, factors such as motion and low perfusion in patients that are compromised can significantly affect the accuracy of SpO2 measurements. Thus, when evaluating the accuracy of a device it is important to review published clinical studies that test the performance of the device on compromised patients. A device that is marketed to have accuracy of + 2% in the 70% to 100% range may not achieve those results on a poorly perfused patient, or even worse, a poorly perfused, moving patient. Likewise, a device that has an accuracy claim of + 3% from 60% to 80% (for healthy adult volunteers) may not accurately display data on a cyanotic congenital heart disease infant whose SaO2 is chronically below 80%. For this reason, pulse oximeters need to be tested in all these clinical populations.
_
Bias and precision:
Bias is the mean difference between SaO2 and SpO2. Precision is defined as the standard deviation (SD) of the differences between SaO2 and SpO2. In the 1980s, pulse oximeter manufacturers stated their accuracy as 2% or 3% (+ 1 SD), where + 1 SD mathematically represents approximately two thirds of the population. Therefore, a device and sensor combination with a 3% (+ 1 SD) accuracy, would have results that were within + 3% (digits) 2/3 of the time. Thus if the actual SaO2 is 94%, a device with + 3% accuracy can be expected to read SpO2 values between 91% to 97% approximately 2/3 of the time. Recently, the FDA has required manufacturers to report their accuracy based on an accuracy specification metric referred to as ‘root mean square’ which reports accuracy as a function of both bias and precision. The root mean square is calculated by taking the square root of the sum of the square of the bias plus the square of the precision.
_
Pulse Oximetry accuracy as a reflection of Arterial PO2 is impacted by the Sigmoidal Shape of the Oxyhemoglobin Dissociation Curve. At high levels of Oxygenation, Pulse Oximetry is insensitive at detecting significant changes in PaO2: since these are being measured in the flat part of the oxyhemoglobin dissociation curve.
Example 1: the PaO2 could drop from 150 to 70 mmHg without an appreciable change in the SpO2, as this change occurs over the flat part of the oxyhemoglobin dissociation curve
Example 2: once hemoglobin is 100% saturated, no further increase in the PaO2 will be reflected in the SpO2 –this makes SpO2 poor at quantifying the degree of hyperoxemia.
_
An assessment of the accuracy of pulse oximeters: a 2012 study:
Peripheral pulse oximetry has become a core monitoring modality in most fields of medicine. Pulse oximeters are used ubiquitously in operating theatres, hospital wards, outpatient clinics and general practice surgeries. This study used a portable spectrometer (Lightman®, The Electrode Co. Ltd., Monmouthshire, UK) to measure the emission spectra of the two light emitting diodes within the pulse oximeter sensor and to determine the accuracy of 847 pulse oximeters currently in use in 29 NHS hospitals in the UK. The standard manufacturing claim of accuracy for pulse oximeters is ± 2–3% over the range of 70–100% SpO2. Eighty-nine sensors (10.5%) were found to have a functional error of their electrical circuitry that could cause inaccuracy of measurement. Of the remaining 758 sensors, 169 (22.3%) were found to have emission spectra different from the manufacturers’ specification that would cause an inaccuracy in saturation estimation of > 4% in the range of 70–100% saturation. This study has demonstrated that a significant proportion of pulse oximeter sensors may be inaccurate.
_________
_________
Limitations, errors and problems with pulse oximetry:
Oximetry is not a complete measure of respiratory sufficiency. A patient suffering from hypoventilation (poor gas exchange in the lungs) given 100% oxygen can have excellent blood oxygen levels while still suffering from respiratory acidosis due to excessive carbon dioxide. It is also not a complete measure of circulatory sufficiency. If there is insufficient blood flow or insufficient hemoglobin in the blood (anemia), tissues can suffer hypoxia despite high oxygen saturation in the blood that does arrive. Pulse oximetry measures solely hemoglobin saturation, not ventilation and is not a complete measure of respiratory sufficiency. It is not a substitute for blood gases checked in a laboratory, because it gives no indication of base deficit, carbon dioxide levels, blood pH, or bicarbonate (HCO3−) concentration. The metabolism of oxygen can be readily measured by monitoring expired CO2, but saturation figures give no information about blood oxygen content. Most of the oxygen in the blood is carried by hemoglobin; in severe anemia, the blood will carry less total oxygen, despite the hemoglobin being 100% saturated. Pulse oximeters do not require user calibration. Thus, it is important that users of the device are aware of the inherent limitations that may give false readings. The pulse oximeter will function properly only if it is able to detect a modulation in transmitted light. If perfusion is decreased and pulse amplitude is small, the signal will be decreased, and the device will be liable to error or be unable to obtain a reading. During cardiac arrest peripheral pulses may be so weak that the device cannot detect them, so monitoring SpO2 by pulse oximetry could be contraindicated. Pulse oximetry has been found to be reliable with systolic blood pressure readings greater than 80 mm Hg. Hypotensive systolic blood pressure readings less than 80 mm Hg cause inaccurate and unreliable pulse oximetry readings. Hypotension, low cardiac output, vasoconstriction, vasoactive drugs (dobutamine or dopamine), and hypothermia all reduce tissue blood flow. These low perfusion states produce a low signal-to-noise ratio and create a signal that can be altered by artifact. Lowered perfusion reduces the signal strength, and the oximeter may not be able to adequately differentiate between arterial pulsations and background noise. This causes inaccurate readings, because the sensor is unable to distinguish the true signal. Conversely, increased venous pulsation, such as occurs with tricuspid regurgitation may be misread by the pulse-oximeter as arterial blood, with a low resultant reading. Motion artifact can interfere with signal detection and interpretation of the signal by the device because of an unstable waveform. Improperly seated sensors, shivering, seizures, or parkinsonian tremors can cause movement, creating an inaccurate reading. Adjustment of the device to a longer signal averaging time may reduce the effects of motion artifact. The pulse oximeter may also be inaccurate in bradycardia and irregular cardiac rhythms, because the device is not able to average the signal waveform in the set amount of time. Edema or venous congestion of the limb can also interfere with readings because of decreased signal. Because pulse oximeters use two-wavelength spectrophotometry, readings are inaccurate in the presence of abnormal hemoglobin levels. Thus, carbon monoxide poisoning will result in an erroneous SpO2 reading as a result of carboxyhemoglobin. Smokers will often have artificially high readings after smoking a cigarette because cigarette smoke contains carbon monoxide. The presence of methemoglobin will also give an unreliable oximeter reading.
_
_
Safe versus unsafe limitations of pulse oximetry:
Pulse oximeters rarely cause any harm directly, though apparently some older models could cause burns and there are reports of the probes causing pressure ulcers. However if their limitations are not borne in mind, harm could be caused by someone having the wrong (or no) treatment. So it’s important to know what the limitations are. Safe limitations are circumstances in which a possible inaccuracy in the displayed SpO2 can be easily suspected; the observer is usually warned by the device (alarm) about the pitfall. Potentially unsafe limitations are those situations in which the inaccuracy is difficult to recognize; the displayed SpO2 is erroneous but the observer is not warned about the pitfall. One limitation is that pulse oximeters cannot operate reliably with a poor signal. This has been referred to as a ‘safe’ limitation, in that the pulse oximeter is not able to give an accurate reading but in some way indicates this fact. Obviously pulse oximeters need to be technically capable of indicating this and the person using it must be aware of this point. The other sort of limitation is more dangerous in that the pulse oximeter may appear to have a good signal and be displaying a saturation figure, but either the figure is inaccurate or gives a false sense of security.
_
| Limitations | Mechanism | Bias | Proposed Action |
| Safe limitations | |||
| Motion | Sensor movement | Lower SpO2 readings | Evaluate plethysmographic waveform |
| Increased noise caused by changes in nonpulsatile component of light absorption | False alarms | Stabilize sensor | |
| Change sensor position | |||
| Use new-generation pulse oximeters | |||
| Poor perfusion | Decreased signal caused by decreased pulsatile (arterial) component of light absorption | Lower SpO2 readings | Evaluate plethysmographic waveform |
| Check and correct skin temperature and peripheral perfusion | |||
| Place sensor more centrally | |||
| Use new-generation pulse oximeters | |||
| Skin pigmentation | Probably caused by calibration assumptions for dark skin pigmentation | Lower or less reliable SpO2 readings at lower SaO2 values | Use new-generation pulse oximeters |
| Nail polish and artificial nails | Decreased signal because of decreased light absorption with artificial nails or nail polish of black, blue, or green color | Lower SpO2 readings | Change sensor position |
| Irregular rhythms | Increased noise caused by tachyarrhythmias | Lower or less reliable SpO2 readings | Evaluate plethysmographic waveform |
| Use new-generation pulse oximeters | |||
| Electromagnetic interference | External electromagnetic energy interference caused by electrosurgical cauterization units, cellular phones, or MRI devices | Lower SpO2 readings | Evaluate plethysmographic waveform |
| False alarms | Avoid external electromagnetic energy sources | ||
| Heating of the sensor and thermal injury (MRI) | Use pulse oximeters with fiber-optic technology (MRI) | ||
| Potentially unsafe limitations | |||
| Calibration | Device-specific calibration algorithms derived by correlating light absorption ratios over a SaO2 spectrum of 80%–100% in healthy young adults | SpO2 readings of <80%–85% are less accurate especially at the extremes of the age spectrum | Use new-generation pulse oximeters |
| Lower SpO2 values calculated by mathematical equations | |||
| Time lag | Software-related delay between sudden changes in blood oxygenation and SpO2 readings | Delay in detecting clinically important desaturation, which may exceed 15–20 s | Use new-generation pulse oximeters |
| Do not use pulse oximetry as a substitute for cardiorespiratory monitoring in critically ill patients | |||
| Probe positioning | The emitted light energy is projected tangentially to the detector because of inappropriate sensor placement (“penumbra” or “optical shunting” effect) | Lower SpO2 readings | Place sensor with the emitter and the detector exactly opposite to each other |
| Use probes of appropriate size in neonates and infants | |||
| light interference | Intense external light energy (as in phototherapy) may interfere with the photodetector (“flooding” effect) | Lower SpO2 readings | Use new-generation pulse oximeters |
| Cover the sensor | |||
| Abnormal hemoglobin molecules | COHb presents red-light absorption similar to oxyhemoglobin | In carboxyhemoglobinemia pulse oximetry overestimates blood oxygenation | Check arterial SaO2 if abnormal hemoglobin molecules are suspected (i.e., carbon monoxide intoxication) |
| Methemoglobin absorbs equal amount of energy in the red and infrared spectra, which affects the ratio of absorption | In significant methemoglobinemia, SpO2 tends toward 85% | Suspect abnormal hemoglobin molecules if the SaO2–SpO2 difference exceeds 5% | |
| Use pulse co-oximetry | |||
| Pulsatile veins | Increased noise because of pulsations of venous blood (i.e., significant tricuspid regurgitation, hyperdynamic circulation states) | Lower or less reliable SpO2 readings | Use new-generation pulse oximeters |
| Intravenous dyes | Intravenous dyes such as methylene blue, indocyanine green, and indigo carmine interfere with light absorption | Lower SpO2 readings | Do not use pulse oximetry or interpret pulse-oximetry readings with caution |
| Check SaO2 |
New-generation pulse oximeters are less susceptible to these limitations because of more sophisticated calibration and signal-extraction algorithms. Pulse co-oximeters are capable of detecting abnormal hemoglobin molecules by using multiwavelength technology.
______
Limitations of pulse oximetry in detail:
Poor signal:
Pulse oximeters need a strong regular pulse in the finger (or ear etc.) that the probe is on. A common problem is that during cold weather people can have cold hands and feet, and have peripheral vasoconstriction. In this case a pulse oximeter may display a reading but it might not be accurate. Some pulse oximeters have a means of indicating how strong the signal is they are receiving and it is important to check this. A still weaker signal may mean the pulse oximeter is not able to work at all. An irregular signal can also cause problems for a pulse oximeter trying to determine oxygen saturation. This can be caused by an irregular heart beat or by the patient moving, shivering or fitting. Poor positioning of the probe can cause inaccurate readings due to various problems. This can be a particular problem with very small fingers and very large ones. Make sure the probe is well on the finger. If the probe is not properly attached, it may detect a variety of noise, resulting in inaccurate measurement.
_
Problem of movement:
When you think of problems associated with pulse oximeters it is important to remember that the signal that is analyzed is really tiny. As explained earlier, it is only about 2 % of the total light that is analyzed. Which such a small signal, it is easy to see how errors can occur. Pulse oximeters are very vulnerable to motion, such as a patient moving his hand especially in recovery room. As the finger moves, the light levels change dramatically. Such a poor signal makes it difficult for the pulse oximeter to calculate oxygen saturation. Motion artifact can be a significant limitation to pulse oximetry monitoring resulting in frequent false alarms and loss of data. The reason for this is that during motion and low peripheral perfusion, many pulse oximeters cannot distinguish between pulsating arterial blood and moving venous blood, leading to underestimation of oxygen saturation. Early studies of pulse oximetry performance during subject motion made clear the vulnerabilities of conventional pulse oximetry technologies to motion artifact.
_
Problem of optical shunting:
The pulse oximeter operates best when all the light passes through arterial blood. However, if the probe is of the wrong size or has not being applied properly, some of the light, instead of going through the artery, goes by the side of the artery (shunting). This reduces the strength of the pulsatile signal making the pulse oximeter prone to errors. It is therefore important to select the correct sized probe and to place the finger correctly in the chosen probe for best results.
_
Problem of too much ambient light:
As discussed before, in addition to the light from the LEDs, ambient (room) light also hits the detector. For good functioning of the pulse oximeter, the strength of the LED light falling on the detector should be good when compared with the strength of the ambient light falling on the detector. If the ambient light is too strong, the LED light signal gets “submerged” in the noise of the ambient light. This can lead to erroneous readings. Therefore, it is important to minimise the amount of ambient light falling on the detector. One can try and move away strong sources of room light. One can also try and cover the pulse oximeter probe and finger with a cloth etc. Light from heat lamps and phototherapy lights has been reported to skew the readings. The high intensity of light emitted from these sources masks the small changes in light transmission from the probe. The remedy is to shield the probe from the ambient light by black paper (e.g. carbon paper) or black polythene or aluminium foil.
_
The 2 wavelengths sensed by the oximeter probe (660 nm and 940 nm) can be generated (in various proportions) by several ambient light sources commonly used in clinical settings. For example, the spectrum of energy produced by both quartz-halogen and incandescent bulbs begins in the visible range, at 650 nm, and peaks around 1,000 nm. An infrared heat lamp, with spectral output beginning at approximately 700 nm, generates little energy in the visible (red) range. In contrast, bilirubin and fluorescent light sources emit more energy at shorter wavelengths and minimal energy in the infrared range. Bilirubin light peaks around 200–400 nm. Fluorescent light produces most of its energy in the visible range: 405–579 nm. Since pulse oximetry depends on accurate measurement of the 660–940 nm range and quartz-halogen, incandescent, infrared, fluorescent, and bilirubin bulbs produce wavelengths in that range, those light sources could, theoretically, affect pulse oximetry readings.
_
Does Ambient Light affect the accuracy of Pulse Oximetry? A 2003 study:
Forty-five faculty and students at a university, none of whom had pale skin, dark skin, or evidence of cardiopulmonary disease were included in study. Any nail polish was removed. Five light sources were individually tested: incandescent, quartz-halogen, infrared, fluorescent, and bilirubin light. A pulse oximetry probe was placed on the subject’s finger, and the finger and probe were placed sideways under each light source, on a predetermined mark. The greatest difference in pulse oximetry reading between any of the light sources was 0.5%. Repeated-measures analysis of variance yielded a p value of 0.204. Ambient light has no statistically significant effect on pulse oximetry readings. Even had the differences been statistically significant, the magnitude of the differences was small and thus clinically unimportant. Pulse oximeter readings are not significantly affected by 5 light sources commonly found in the clinical setting.
_
Problem of electromagnetic interference:
Electrical equipment such as surgical diathermy emit strong electric waves which may be picked up by the wires of the pulse oximeter. These waves make small currents form in the wires, confusing the pulse oximeter which assumes these currents come from the light detector. During diathermy use, one should be cautious about interpreting pulse oximeter readings. If electric appliances such as televisions, mobile telephones, or medical devices which produce high levels of electromagnetic waves are used near the pulse oximeter, the electromagnetic waves from these devices may interfere with accurate measurement. Radiofrequency emissions from MRI scanners (and electrocautery devices) may interfere with pulse oximetry. In addition, 2nd/3rd-degree burns beneath pulse oximeter probes have been reported in patients undergoing MRI scans due to generation of electrical skin currents beneath the looped pulse oximeter cables, which act as an antenna.
___
Problem of poor peripheral perfusion:
A good peripheral blood flow makes the arteries in fingers nicely pulsatile. As discussed before, it is the pulsatile change in absorbance that is used in the calculation of oxygen saturation. When the peripheral perfusion is poor (e.g. in hypotension), the arteries are much less pulsatile. The change in absorbance is therefore less and the pulse oximeter may then find the signal inadequate to correctly calculate oxygen saturation.
_
_
A reduction in peripheral pulsatile blood flow produced by peripheral vasoconstriction (hypovolaemia, severe hypotension, cold, cardiac failure, some cardiac arrhythmias) or peripheral vascular disease result in an inadequate signal for analysis. Venous congestion, particularly when caused by tricuspid regurgitation, may produce venous pulsations which may produce low readings with ear probes. Venous congestion of the limb may affect readings as can a badly positioned probe. When readings are lower than expected it is worth repositioning the probe. In general, however, if the waveform on the flow trace is good, then the reading will be accurate.
____
Problem of not detecting hyperoxia:
The problem is that the pulse oximeter cannot “see” the extra dissolved oxygen. When PaO2 is higher than 100 mm due to supplemental oxygen, the saturation still shows 100 %, instead of say 120 %. The 100 % saturation tells us that the patient is getting enough oxygen. However, it does not tell you that the patient is getting too much oxygen (hyperoxia). Oxygen, while necessary for life, can be harmful if given in excess. Therefore, other means (e.g. arterial blood gas) have to be used to detect hyperoxia.
______
Delay:
Pulse Oximetry measurements are signal averaged over several seconds. Therefore, the pulse oximeter may not detect a hypoxemic event until several seconds after it has occurred: this may be particularly important when the pulse oximeter is being used to monitor SpO2 during intubation.
____
Anemia:
In theory there is no reason anaemia should cause pulse oximeters to be inaccurate and experiments in dogs have shown accuracy reliable enough for “clinical purposes” as long as the packed cell volume was larger than 15%. Clinical experience has shown good performance with haemoglobin as low as 2.3 g/dl. However in severe anemia (with Hb <5 g/dL) with SaO2 <80%, SpO2 underestimates the SaO2: this may be due to increased signal/noise ratio from the surrounding tissue. A 1990 study of retrospective evaluation of simultaneous tests of oximeters of various manufacturers in volunteer subjects disclosed greater errors at low saturations in subjects with low hemoglobin (Hb) concentrations. The error due to anemia was zero at 97% SaO2 and became evident when SaO2 fell below 75%.
_____
Sickle cell disease:
It has been shown that pulse oximetry can detect low oxygen saturation accurately in sickle cell disease, however other researchers have suggested caution in interpreting pulse oximetry values in sickle cell disease.
_
Pulse Oximetry and factors associated with Hemoglobin Oxygen Desaturation in children with Sickle Cell Disease: a 1993 study:
Authors conclude that pulse oximetry may be useful to assess whether progressive pulmonary dysfunction begins at an early age in Hb SS patients, and to assess acutely ill patients for the presence of hypoxemia associated with acute chest syndrome.
_
Accuracy of Pulse Oximetry in Sickle Cell Disease: a 1999 study:
This study confirms in adults that pulse oximetry has acceptable accuracy for reliable clinical diagnosis of serious gas exchange abnormalities in sickle cell disease. Despite patients’ severe anemia, which has been shown to impair the accuracy of pulse oximetry, as long as strong and regular photoplethysmographic waves were present, authors found that pulse oximeters could be relied upon not to misdiagnose either hypoxemia or normoxemia in such patients. As in all other patients, additional tests for the severity of anemia, the adequacy of cardiac output, and sometimes the carboxyhemoglobin (and met-hemoglobin) levels are required for full evaluation of oxygen transport.
______
Carbon dioxide:
A pulse oximeter can cause a false sense of security by giving a good saturation figure when someone’s breathing is completely inadequate. This is especially true when a patient is getting supplementary oxygen. There are two main functions of breathing, one is getting oxygen out of the air and into the body, the other is getting carbon dioxide out of the body and into the air. It possible for someone to be getting enough oxygen into their body but not be getting rid of enough carbon dioxide. Oxygen saturation by itself does not tell the whole story about breathing – this is especially true if someone is being given oxygen. During acute hypoventilation, the PCO2 can rise significantly before desaturation occurs on the SpO2: this is especially true if the patient is receiving supplemental oxygen, in this case, the PCO2 can continue to rise while the SpO2 is artificially “supported” by the supplemental oxygen. As a minimum it is also necessary to record the respiratory rate, and if they are having oxygen, how much they are having. Pulse Oximetry does not measure PCO2 or pH and gives no information about ventilation.
______
Problem of coloured dyes and nail polish:
The dye, methylene blue, if in the patient’s circulation, will artificially lower the displayed oxygen saturation. When methylene blue is used in surgery to the parathyroids or to treat methaemoglobinaemia a shortlived reduction in saturation estimations is registered. Finger nail polish can affect the accuracy of saturation determination. Nail varnish may cause falsely low readings.
Nail varnish:
Some research has shown that dark nail varnish bias pulse oximeter readings, but not by a clinically significant amount. However there are limitations to this research such as a lack of trials at lower saturations, so in practice nail varnish should still be removed.
_
The effect of nail polish and acrylic nails on pulse oximetry reading using the Lifebox oximeter in Nigeria: a 2013 study:
Fifty non-smoking volunteers had their fingers numbered from right to left (little finger of right hand =1 and little finger of left hand =10). Alternate fingers were nails painted with clear, red, brown and black nail polish and the 5th finger had acrylic nail applied. The corresponding finger on the other hand acted as control. The oxygen saturation was determined using the Lifebox pulse oximeter. All fingers (100%) with clear nail polish, red nail polish and acrylic nails recorded a saturation value. Each of the mean saturation value for clear nail polish, red nail polish and acrylic nails was not significantly different from the control mean (p= 0.378, 0.427 and 0.921). Only 12% and 64% of nails polished black and brown respectively recorded a saturation value. The mean SpO2 for black and brown polish were significantly different from their control mean (p<0.001). Black and brown polish resulted in a significant decrease in SpO2 with the Lifebox oximeter. Dark coloured nail polish should be removed prior to SpO2 determination to ensure that accurate readings can be obtained.
_______
Skin pigmentation:
Previous research on pulse oximetry has found that skin pigmentation has no clinically significant effect. Recently however it has been found that pulse oximeters from three manufacturers overestimated oxygen saturation in individuals with darkly pigmented skin at saturations below 80%. The authors suggested that pulse oximeters should carry a warning about this. Above 80% the researchers concluded that the effect was probably of no clinical significance.
_________
__________
Bilirubin:
The literature concerning the effect of bilirubin on oximetry can appear confused. Two authors state that bilirubin can affect pulse oximetry readings, but neither give any evidence or references to support this. Moyle in the authoritative ‘Pulse Oximetry’ reviews the subject and concludes that pulse oximetry is accurate, but that co-oximetry – the usual ‘gold standard’ method of verifying pulse oximeter readings – is not. This last point is supported by two case studies, the authors of which feel “… in the presence of severe hyperbilirubinemia, pulse oximetry may be more accurate than co-oximetry”. Abrams et al looked at pulse oximetry in patients with liver disease. They found that pulse oximetry overestimated oxygen saturation as measured by a co-oximeter in both their subjects and their controls. Veyckmans et al carried out research on the influence of bilirubin on pulse oximetry and concluded “There was no demonstrable direct influence of high bilirubin plasma levels on SpO2 as measured by a Nellcor (r) pulse oximeter”.
_________
_________
_________
_________
Dyshemoglobinemia:
The dyshemoglobinemia are a constellation of disorders in which the hemoglobin is functionally altered and prevented from carrying oxygen. They include carboxyhemoglobin, methemoglobin and sulfhemoglobin. Since pulse oximetry only measures the percentage of bound hemoglobin, a falsely high or falsely low reading will occur when hemoglobin binds to something other than oxygen.
•Hemoglobin has a higher affinity to carbon monoxide than oxygen, and a high reading may occur despite the patient actually being hypoxemic. In cases of carbon monoxide poisoning, this inaccuracy may delay the recognition of hypoxia.
•Methemoglobinemia characteristically causes pulse oximetry readings in the mid-80s.
_
Carbon monoxide (CO):
Carbon monoxide is a colourless, odourless gas that is produced in most fires. Breathing in carbon monoxide will lead to it becoming attached to haemoglobin in preference to oxygen, so it is only necessary to breath in a small amount of carbon monoxide to have a large amount of haemoglobin taken up by it and therefore not available to carry oxygen. For instance if 25% of someone’s haemoglobin is taken up by carbon monoxide then only 75% is available to carry oxygen, and so their oxygen saturation could, at best, be only 75%. Pulse oximeters will display an oxygen saturation which is approximately equal to the percentage of haemoglobin combined with oxygen plus the percentage of haemoglobin combined with carbon monoxide. So if someone has 25% of their haemoglobin saturated with carbon monoxide and true oxygen saturation of 70% a pulse oximeter will display an oxygen saturation of about 95%. This is obviously extremely dangerous and for this reason pulse oximeters should not be used with people who may have inhaled smoke, i.e. anyone who has been involved with any sort of fire, unless you are certain that they do not have any significant level of carbon monoxide in their blood.
_
Carboxyhemoglobin does not carry oxygen. It is really a hemoglobin molecule with all oxygen carrying sites occupied by CO. The CO has such a high affinity for hemoglobin, that oxygen cannot displace it. CO has about 240 times the affinity of O2 for Hemoglobin and binds to same sites. Consider carboxyhemoglobin totally useless in oxygen transport. The presence of COHb also shifts the O2 dissociation curve to the left, thus interfering with the unloading of O2. This is an additional feature of the toxicity of CO. CO poisoning results from CO exposure, most commonly exposure to fuel combustion (fuel burning heaters, stoves, automobile exhaust, etc.), so it most commonly occurs during cold periods where people are in closed quarters to conserve the heat originating from fuel combustion. Symptoms include headache, nausea, vomiting and weakness. The patient is classically described as cherry red, but in reality, they appear to be pink, which lowers the clinician’s suspicion for hypoxia. Thus, these symptoms are commonly attributed to viral flu-like illnesses. If a patient has a carboxyhemoglobin level of 25%, and their hemoglobin is 12, this means that they effectively have a hemoglobin of only 9 (since 25% of their hemoglobin is useless). If the carboxyhemoglobin level is 25%, then the maximum oxygen saturation that can be attained is 75%. However, the pulse oximeter will read 100% because light absorption characteristic of carboxyhemoglobin is similar to oxyhemoglobin. Thus, pulse oximetry measurements are fooled by CO poisoning. The arterial blood gas is not usually helpful either. Since the ABG measures oxygen gas tension (PaO2) and not oxygen content or true oxygen saturation, the oxygen gas tension (PaO2) will be normal. The only abnormality on an ABG may be metabolic acidosis, which is a consequence of inadequate oxygen delivery to the peripheral tissues, resulting an anaerobic metabolism and lactic acid production. If CO poisoning is suspected, one must order a CO level or a test called co-oximetry. Co-oximetry is done routinely in some blood gas analyzers, but most do not, so this must be specifically ordered. Co-oximetry is capable of measuring the true oxygen saturation percentage and the percentage of nonfunctional hemoglobins such as carboxyhemoglobin and methemoglobin. The treatment for CO poisoning is 100 % oxygen, but if the CO level is very high, or if the victim is pregnant, hyperbaric oxygen is indicated to more effectively displace the CO from the hemoglobin. Hyperbaric oxygen therapy is used to increase the amount of oxygen dissolved in the plasma, by increasing the ambient pressure.
_
CO is synthesized naturally in the body and serves a range of physiological functions including vasodilation, angiogenesis, vascular remodeling, protection against tissue damage and modulation of the inflammatory response. Approximately 85% of the CO is produced by heme oxygenase (HO), which catalyses heme to CO, iron and biliverdin. Biliverdin is further broken down into bilirubin. The major site of heme catabolism, and thus CO production, is the liver. The normal blood COHb saturation in non-smokers is approximately 1%, the mean saturation in smokers of approximately 20 cigarettes per day lies around 5.5%. The majority of CO is removed from the body via expiration.
_
Common CO Poisoning Sources:
Faulty furnaces, heaters
Auto exhaust
Gas generators
Charcoal grills used indoor
Tobacco smoke
Fires
Small gas engines or equipment
Gas appliances
Gas heaters in enclosed area
_
Carbon Monoxide and SpCO% Measurement:
0 – 5%
Considered normal in non-smokers. When > 3% with symptoms, consider high flow oxygen and evaluate environment for CO sources. Consider measuring others in same room/office/vehicle as patient. In absence of symptoms, no further medical evaluation of SpCO needed.
5 – 10%
Considered normal in smokers, abnormal in non-smokers. If symptoms are present, consider high flow oxygen and inquire if others are ill. Alert Fire Department.
10 – 15%
Abnormal in any patient. Assess for symptoms, consider high flow oxygen. Evaluate environment for CO sources.
> 15%
Significantly abnormal in any patient. Administer high flow oxygen, assess for symptoms, consider transport. Evaluate environment for CO sources.
> 30%
Consider transport to hyperbaric facility (some experts recommend hyperbaric referral for any patient > 25% or with altered mental status or pregnant).
_
Confirmation of the pulse oximetry gap in carbon monoxide poisoning: a 1997 study.
Study was conducted to demonstrate the degree to which pulse oximetry overestimates actual oxyhemoglobin (O2Hb) saturation in patients with carbon monoxide (CO) poisoning. There is a linear decline in O2Hb saturation as COHb saturation increases. This decline is not detected by pulse oximetry, which therefore overestimates O2Hb saturation in patients with increased COHb levels. The pulse oximetry gap increases with higher levels of COHb and approximates the COHb level. In patients with possible CO poisoning, pulse oximetry must be considered unreliable and interpreted with caution until the COHb level has been measured.
_
Pulse oximetry correction for smokers: a 1996 study.
Pulse oximetry oxygen saturation (SpO2) does not distinguish carboxyhemoglobin (COHb) from oxyhemoglobin (O2Hb), giving a false impression of the apparent degree of oxyhemoglobin saturation in smokers who have elevated levels of COHb. This pilot study suggests that smoking exposure history correlates with COHb levels and that correction for smoking exposure improves the accuracy of pulse oximetry.
_
Current pulse oximeters overestimate arterial oxygenation in patients with elevated COHb. The amount of overestimation is approximately equal to the amount of COHb present. Accurate measurement of arterial oxygen saturation in patients with elevated COHb can only be performed via analysis of arterial blood with a laboratory co-oximeter or newly designed non-invasive pulse co-oximeter.
______
Methaemoglobin:
Methaemoglobin is formed by oxidation of the iron moiety of haemoglobin, which changes from the normal, ferrous state (Fe++) to a ferric state (Fe+++). Methaemoglobinaemia is a clinical condition in which more than 1% of haemoglobin is oxidised to methaemoglobin. It manifests as cyanosis when levels of methaemoglobin are more than 10% (1.5 g/dl).Ferric haem is incapable of binding oxygen and causes an allosteric change in the remaining haem moieties of the molecule, which impairs the release of oxygen and shifts the oxyhemoglobin-dissociation curve to the left. Methaemoglobin is an abnormal type of haemoglobin that does not bind oxygen well. Normally 1-2% of people’s haemoglobin is methaemoglobin, a higher percentage than this can be genetic or caused by exposure to various chemicals and depending on the level can cause health problems.
_
_
Methemoglobin is brown in color. Patients with methemoglobinemia are classically “ashen gray” in color. Their pulse oximetry value will read low, so this condition does not fool the pulse oximeter as it does in CO poisoning. Another clue is that when supplemental oxygen is given to the patient, the pulse oximetry reading does not change. It will still be low. When an arterial blood gas is drawn, the blood appears to be a chocolate brown color which is quite eye opening. The cause is usually idiopathic, but the ingestion of nitrites is one of the known causes. The condition is usually self-limited and resolves gradually with IV fluid hydration. IV methylene blue can be given for severe cases. Oxygen supplementation is somewhat helpful and PRBC transfusion can be used to increase the oxygen carrying capacity in severe cases.
_
A typical ABG in CO poisoning or methemoglobinemia patients is pH 7.26, PCO2 34, PO2 100, bicarb 15, BE -11, if the patient is breathing room air. If the patient is breathing supplemental oxygen, then the ABG will be pH 7.26, PCO2 34, PO2 400, bicarb 15, BE -11 (i.e., just the PO2 goes up), although this does not change the oxygen saturation much. Although the blood gas machine will calculate that the oxygen saturation is 100%, remember that the ABG machine did not measure this, but rather it calculates this based on the assumption that the sample contains normal hemoglobin (which is not the case if the patient has CO poisoning or methemoglobinemia). The paradox is that the ABG slip will indicate that the oxygen saturation is 100%, while the co-oximetry report will indicate that the oxygen saturation is very low (e.g., 70%). In summary, CO poisoning has a low true oxygen saturation, red color, 100% oxygen saturation on pulse oximetry (which is false), and normal PO2 on ABG. Methemoglobinemia has a low true oxygen saturation, brown color, low oxygen saturation on pulse oximetry, and normal PO2 on ABG. Clinicians need to be aware of the effect that MetHb has on pulse oximetry. As a general rule of thumb, large quantities of MetHb (> 10%) may result in a SpO2 reading of approximately 85%. Low amounts of MetHb (< 10%) will reduce a high SpO2 by approximately half the MetHb%.
_
Why methaemoglobinaemia causes trouble with pulse oximetry:
The extinction coefficient of methemoglobin at 660 nm is similar to that at 940 nm, resulting in a red-to-infrared ratio of 1:1. The corresponding SpO2 value for this ratio is approximately 85 percent. Hence, as the methemoglobin level increases, the SPO2 will tend toward this value. When methemoglobin levels are in excess of 30 percent, the SpO2 will plateau at 85 percent and will be relatively unaffected by the oxygenation status.
_
Finally, it should be noted that pulse oximeters are not reliable in the presence of dyshemoglobins – hemoglobins that cannot bind oxygen. The two major dyshemoglobins encountered in clinical practice are carboxyhemoglobin (COHb) and methemoglobin (MetHb). Oximeters do not differentiate hemoglobin bound to carbon monoxide from hemoglobin bound to oxygen; the machines report the sum of both values as oxyhemoglobin. In contrast to blood co-oximeters, which utilize four wavelengths of light to separate out oxyhemoglobin from reduced hemoglobin, methemoglobin and carboxyhemoglobin, pulse oximeters utilize only two wavelengths of light. As a result, pulse oximeters measure COHb and part of any MetHb along with oxyhemoglobin, and combine the three into a single reading, the SpO2. (MetHb absorbs both wavelengths of light emitted by pulse oximeters, so that SpO2 is not affected as much by MetHb as for a comparable level of COHb).Thus a patient with 80% oxyhemoglobin and 15% carboxyhemoglobin would show a pulse oximetry oxygen saturation (SpO2) of 95%, a value too high by 15%. For this reason pulse oximeters should be used cautiously (if at all) when there may be an elevated carbon monoxide level, for example in patients assessed in an emergency department. Note that excess carboxyhemoglobin is present in all cigarette and cigar smokers. A resting SpO2 should be interpreted cautiously in any outpatient who has smoked within 24 hours. The half-life of CO breathing ambient air is about 6 hours, so 24 hours after smoking cessation the CO level should be normal, i.e., less than 2.3%. If there is concern about the true SaO2, it should be measured on an arterial blood sample in co-oximeter; alternatively, the percent COHb can be measured on a venous sample, and the value subtracted from the SpO2. The spectrophotometric technique used by pulse oximeters also makes their oxygen saturation reading less reliable in the presence of excess methemoglobin (metHb). MetHb reduces the SpO2 linearly until a level of about 85%, at which point further increases in metHb do not cause further lowering of SpO2. A finding of unexpectedly low SPO2 (e.g., 91% in a patient with normal cardiorespiratory system who is receiving nasal oxygen) should make one think of excess methb; in such cases an arterial blood sample should be obtained for direct measurement of SaO2 and PaO2.
_
Sulphaemoglobin contains an additional sulphur molecule compared to haemoglobin. It has no respiratory function, doesn’t alter the life-span of the red-cell and remains unchanged in the cells. Symptoms include a blueish or greenish discoloration of the blood, skin, and mucous membranes, even though a blood count test may not show any abnormalities in the blood. This discoloration is called cyanosis, and is caused by greater than 5 grams per cent of deoxyhemaglobinemia, or 1.5 grams per cent of methemaglobinemia, or 0.5 grams per cent of sulphemaglobinemia, all serious medical abnormalities. Increases are associated with antimony compounds, acetanalide and phenacetin medication (compounds related to paracetamol), sulphonamide therapy, nitro-glycerine poisoning and ingestion of bromide, nitrate (often in impure ground water), sulphur, sulphides and thiosulphate. These substances may cause damage to the red-cell enzymes or there may be an association with the formation of hydrogen sulphide in the bowel. The condition generally resolves itself with erythrocyte (red blood cell) turnover, although blood transfusions can be necessary in extreme cases.
__
Oxygen concentration in blood can be measured as functional saturation or fractional saturation. Commercial pulse oximeters display functional saturation which takes into account two species of hemoglobin, oxyhemoglobin (O2Hb) and deoxyhemoglobin, also called reduced hemoglobin (Hb). Simply put, functional saturation is the amount of oxygenated blood compared to deoxygenated blood. A laboratory Co-oximeter, which utilizes four or more wavelengths of light instead of two, is capable of measuring both functional saturation and fractional saturation, a more specific and accurate measurement of blood oxygenation. Fractional saturation takes into account all common species of hemoglobin: O2Hb, deoxyHb, methemoglobin (MetHb) and carboxyhemoglobin (COHb). In most clinical situations, when it can be assumed that MetHb and COHb levels are normal, functional saturation is adequate for determining a patient’s respiratory status and pulse oximetry can be used to monitor the patient. However when MetHb or COHb levels of the patient are outside the normal ranges they can interfere with the accurate reading of oxygenated hemoglobin by pulse oximetry. In these cases, Co-oximetry is needed to monitor the patient’s true respiratory status. The most widely accepted method for determining the accuracy of pulse oximetry readings is a direct comparison with functional arterial saturation readings (SaO2) from a laboratory Co-oximeter. This comparison has routinely been reported in the literature in the terms of bias and precision.
_______
Case-1
A 54-year-old man came to the emergency room (ER) complaining of headaches and shortness of breath. On room air his PaO2 was 89 mm Hg, PaCO2 38 mm Hg, pH 7.43; hematocrit was 44%. SaO2 was not directly measured but instead calculated at 98% for this PaO2, based on a standard oxygen dissociation curve. After some improvement he was scheduled for a brain CT scan two days later, and discharged from the ER. He was brought back to the ER the next evening, unconscious. Ambulance attendants alerted the ER physician to a possible faulty heater in the patient’s house. This time carbon monoxide and SaO2 were measured along with routine arterial blood gases. The results: PaO2 79 mm Hg, PaCO2 31 mm Hg, pH 7.36, SaO2 53%, carboxyhemoglobin 46%. This patient’s true SaO2 would have been much lower than 98% had it been measured on the first ER visit instead of just calculated. The physician missed hypoxemia as a cause of headache and dyspnea because of the ‘normal’ calculated SaO2. Carbon monoxide by itself does not affect PaO2 but only SaO2 and O2 content. (Slight reduction in PaO2 on the patient’s second visit was attributed to some basilar atelectasis and resulting V-Q imbalance). Confusion about interpretation of oxygen saturation in the presence of excess CO is not unusual and even finds its way into peer-review literature. To know the oxygen content one needs to know the hemoglobin content and the SaO2; both should be measured as part of each arterial blood gas test. As shown above, a calculated SaO2 may be way off the mark and can be clinically misleading. This is true even without excess CO in the blood. One study of over 10000 arterial samples found wide variation in measured SaO2 for a given PaO2; for example, in the PaO2 range of 56-64 mm Hg the measured SaO2 ranged from 69.7 percent to 99.4 percent.
_
Case-2
_
Oxygen saturation (SO2) can be measured by three approaches that are often used interchangeably, although the measured systems are quite different. Pulse oximetry is a noninvasive, spectrophotometric method to determine arterial oxygen saturation. Co-oximetry is a more complex and reliable method that measures the concentration of hemoglobin derivatives in the blood from which various quantities such as hemoglobin derivative fractions, total hemoglobin, and saturation are calculated. Blood gas instruments calculate the estimated O2 saturation from empirical equations using pH and PO2 values. In most patients, the results from these methods will be virtually identical, but in cases of increased dyshemoglobin fractions, including methemoglobinemia, it is crucial that the distinctions and limitations of these methods be understood.
_________
Diabetes mellitus:
Pulse Oximetry may be affected by other Abnormal Hemoglobin:
Glycosylated Hemoglobin A1c levels >7% in type 2 diabetics with poor glucose control have been shown to result in overestimation of oxygen saturation as assessed by pulse oximetry.
Pulse oximetry not reliable for diabetic patients? A 2012 study.
According to the results of a recent clinical study, pulse oximetry may not be suitable for assessment of blood oxygenation among type 2 diabetic patients with poor glycemic control and consequent increased HbA1c. The study population comprised 261 type 2 diabetes patients who were critically ill and required oxygen therapy and/or mechanical ventilation. Their care included continuous monitoring of oxygen saturation using a pulse oximeter. Fasting blood was sampled from each study patient for glucose and HbA1c. Arterial blood was sampled for blood gas analysis, including measurement of SaO2. As arterial blood was sampled, the patient’s SpO2 reading from pulse oximeter was recorded. For the purposes of this study poor glycemic control was defined as HbA1c > 7.0 %; by this definition 114 of the 261 patients (44 %) had poor glycemic control. There was essentially no difference between SpO2 and SaO2 among those with adequate glycemic control: mean SpO2 95.1 % ± 2.8 and mean SaO2 95.3 % ± 2.8. However, there was a significant difference (bias) between the two parameters among those with poor glycemic control: mean SpO2 98.0 % ± 2.6 and mean SaO2 96.2 % ± 2.9. The magnitude of the bias was demonstrated to correlate with HbA1c, so that the higher the HbA1c the greater is the difference between SPO2 and SaO2. The authors were able to conclude that among patients with poorly controlled type 2 diabetes, pulse oximetry overestimates arterial oxygen saturation. It may be more appropriate to use arterial blood gas analysis, rather than pulse oximetry, to monitor treatment of hypoxemia in these patients.
________
________
Meta-analysis of arterial oxygen saturation monitoring by pulse oximetry in adults: 1998:
There were a total of 169 oximeter trials on 41 oximeter models from 25 different manufacturers. Studies were conducted in various settings with a variety of subjects, with most being healthy adult volunteers. Pulse oximeters were found to be accurate within 2% (± 1 SD) or 5% (± 2 SD) of in vitro oximetry in the range of 70% to 100% SaO2. In comparing ear and finger probes, readings from finger probes were more accurate. Pulse oximeters may fail to record accurately the true SaO2 during severe or rapid desaturation, hypotension, hypothermia, dyshemoglobinemia, and low perfusion states.
_______
_______
Falsely high or falsely low SpO2 reading:
_
No effect on SpO2:
Fetal haemoglobin (HbF), Bilirubin (absorption peaks are 460, 560 and 600 nm), dark skin.
_
Cyanide poisoning gives a high reading, because it reduces oxygen extraction from arterial blood. In this case, the reading is not false, as arterial blood oxygen is indeed high in early cyanide poisoning.
________
________
Response to errors in pulse oximetry:
_________
_________
Synopsis of pulse oximetry limitations:
_________
_________
Patients who need Oxygen regardless of Oxygen Saturation Measurement:
1 Patients in cardiac or respiratory arrest
2 Patients with chest pain suspected to be of cardiac origin
3 Patients with multisystem trauma
4 Patients who are apnoeic or who require assisted ventilation
5 Patients with suspected or confirmed carbon monoxide poisoning or smoke inhalation
6 Neonatal patients in distress
7 Patients with suspected sickle cell crisis
8 Hypotensive patients (SBP < 80 mm Hg)
9 Near drowning patients
______
______
Pulse oximetry vs. ABG:
Pulse oximeters give non-invasive estimation of the arterial haemoglobin oxygen saturation. The gold standard for measurement of oxygen saturation remains arterial blood gas (ABG) analysis with co-oximetry. However, this is invasive, painful, time consuming, costly, provides only intermittent information on patient status, and is impractical in most primary care settings.
_
Speed:
•Pulse oximetry measures a patient’s arterial saturation of oxygen (SpO2) in seconds; measurements obtained from arterial blood gases (ABG) can take several minutes to acquire and are usually drawn by a respiratory therapist, transported to the blood gas lab, measured and finally reported back to the doctor. The information from an ABG analysis provides for more information than just the oxygen level and is essential in emergencies, but oximetry is equally important to ensure the patient does not suffer the effects of hypoxia unnecessarily.
Accurate and Easy to Use:
•While not as precise as an ABG measurement, pulse oximeters are accurate with most patients, especially in emergency situations where seconds matter; however, it should not be used indiscriminately for some chronic conditions, such as chronic obstructive pulmonary disease (COPD), in which a patient may have chronically low oxygen levels and raising them too high can be dangerous. Little to no training is needed to perform pulse oximetry. Most oximeters have only one button and as long as the probe is placed properly, virtually anyone can use it. In their infancy, oximeters were the size of old cassette recorders and just as cumbersome. The newest generation of oximeters is streamlined, rugged and even easier to use. Furthermore, they are now available for home use.
Non-Invasive and Reliable:
•ABG measurements, though exact, require blood drawn from an artery, which can lead to complications ranging from hematoma to laceration of the artery. Pulse oximetry is performed on a fingertip and measures through the nail bed. As long as the oximeter is used properly and is calibrated regularly, it is easy to use and usually reliable. Good peripheral circulation in the patient’s extremities is critical to obtaining accurate readings and most oximeters on the market incorporate a perfusion gauge, usually in LED bar lights, that shows the strength of the patient’s peripheral circulation. When a strong pulse is not present in the hands or feet, readings can be made with a special adhesive probe placed on the patient’s earlobe or even the bridge of the nose.
_
Contraindication to ABG:
1. Bleeding diathesis
2. AV fistula
3. Severe peripheral vascular disease, absence of an arterial pulse
4. Infection over site
Obviously pulse oximetry or pulse co-oximetry or pulse oximetry with capnography are only alternatives when ABG is contraindicated.
_
Why ABG instead of SpO2:
1. Pulse oximetry does not assess ventilation (PCO2) or acid base status.
2. Pulse oximetry becomes unreliable when saturations fall below 70-80%.
3. Technical sources of error (ambient or fluorescent light, hypoperfusion, nail polish, skin pigmentation)
4. Pulse oximetry cannot interpret methemoglobin or carboxyhemoglobin.
__
The patient’s pulse oximetry reading is SpO2 98% on air. PaO2 23mm and SaO2 38 % on ABG.
What are the possible explanations for the discrepancy between the pulse oximetry reading and the oxygen saturation on the arterial blood gas?
Possible explanations for ‘pseudo-hypoxaemia’ include:
1. Equipment failure
— faulty pulse oximeter
— faulty blood gas analyser
2. Blood sample used was actually venous in ABG
3. Blood sample taken from a site affected by localised hypoxemia, e.g. ischaemic limb
4. Excessive oxygen consumption following blood sample collection (e.g. massive leukocytosis or thrombocytosis)
_
Arterial puncture or pulse oximetry?
Arterial puncture is the general accepted standard method for monitoring oxygen therapy in critically ill patients, but this technique is painful for the patient, has the potential of complications, and does not provide immediate continuous data. Pulse oximetry is a non-invasive method used to measure arterial oxygen saturation with a clinically acceptable accuracy of +/- 2%. Despite some limitations, pulse oximetry is considered to be reliable in most cases in detecting hypoxaemia and monitoring oxygen therapy in stationary units. The pulse oximeter can reduce the number of arterial punctures, personnel’s time consumption, and limit oxygen abuse. Furthermore the new transportable and hand-held pulse oximeters offer new possibilities for continuous 24 hour monitoring of oxygen saturation also out of hospitals. The pulse oximeter can optimize monitoring patients’ oxygen saturation in the stationary units, however, arterial puncture will remain the most reliable method in the assessment of hypoxaemia and hypercapnia, especially in acute situations.
__
A comparison of Arterial Oxygen Saturation measured both by Pulse Oximeter and Arterial Blood Gas Analyzer in Hypoxemic and Non-hypoxemic Pulmonary Diseases: a 2006 study:
The purpose of this study was to determine the correlation between SpO2 and arterial O2 saturation measured with blood gas analyzer (SaO2) in hypoxemic and non-hypoxemic patients. Hypoxemia was considered as SpO2<90%. In pulmonary diseases with SpO2 ≥ 80%, pulse oximetry has high accuracy in estimating SaO2 and may be used instead of arterial blood gases (ABG). In patients with SpO2 < 80%, however, the exact estimation of SaO2 and the evaluation of oxygenation by pulse oximeter is not a good substitution for ABG analyzer.
_
Pulse oximetry versus arterial blood gas specimens in long-term oxygen therapy (LTOT):
Portable pulse oximeters are now widely available for the assessment of arterial oxygenation, and the U.S. Medicare program considers saturation readings to be acceptable substitutes for arterial PO2 in selecting patients for long-term oxygen therapy (LTOT). Current oximeters are reasonably accurate (plus or minus 2 or 3 percent of the co-oximetry value), but the clinician should be aware of several potential problems. Readings may be inaccurate in the presence of hemodynamic instability, carboxyhemoglobinemia, or dark skin pigmentation, and also during exercise. Indicated saturation may substantially overestimate arterial PO2 if the patient is alkalemic. Pulse oximetry cannot detect hypercapnia or acidosis. For these and other reasons, pulse oximetry should not be used in initial selection of patients for LTOT, as a substitute for arterial blood gas analysis in the evaluation of patients with undiagnosed respiratory disease, during formal cardiopulmonary exercise testing, or in the presence of an acute exacerbation. Pulse oximetry is an important addition to the clinician’s armamentarium, however, for titrating oxygen dose in stable patients, in assessing patients for desaturation during exercise, for sleep studies, and for in-home monitoring.
________
________
Pros and cons of pulse oximetry:
_
The advantages of the pulse oximeter could be listed as follows:
• Affordable Price: almost all pulse oximeter are at quite an affordable price in the market.
• Fast: Provides real-time, absolute measurement of oxygen levels without the use of empirical tables.
• Versatile: it can be used virtually anywhere – hospital or home – to determine oxygen levels.
• Accurate: the pulse oximeter provides a relatively accurate measure which could be taken into account for a proper diagnosis
• Extended use: The patient mobility makes this technology suitable for long-term patient monitoring.
• Noninvasive sampling: The accuracy of this technology allows doctors, clinics and hospitals to replace traditional invasive sampling procedures, such as arterial puncture or an indwelling arterial catheter, for obtaining absolute oxygen measurement.
• Ease of use: Does not require preliminary calibration.
_
Advantages:
A pulse oximeter is useful in any setting where a patient’s oxygenation is unstable, including intensive care, operating, recovery, emergency and hospital ward settings, pilots in unpressurized aircraft, for assessment of any patient’s oxygenation, and determining the effectiveness of or need for supplemental oxygen. Assessing a patient’s need for oxygen is the most essential element to life; no human life thrives in the absence of oxygen (cellular or gross). Because of their simplicity and speed, pulse oximeters are of critical importance in emergency medicine and are also very useful for patients with respiratory or cardiac problems, especially COPD, or for diagnosis of some sleep disorders such as apnea and hypopnea. Portable battery-operated pulse oximeters are useful for pilots operating in a non-pressurized aircraft above 10,000 feet (12,500 feet in the US) where supplemental oxygen is required. Prior to the oximeter’s invention, many complicated blood tests needed to be performed. Portable pulse oximeters are also useful for mountain climbers and athletes whose oxygen levels may decrease at high altitudes or with exercise. Some portable pulse oximeters employ software that charts a patient’s blood oxygen and pulse, serving as a reminder to check blood oxygen levels.
_
Pulse oximetry’s advantages over arterial blood gases measurements are obvious: noninvasive, less pain and risk than arterial puncture, less expensive, more real-time or point-of-care testing method (immediately available vs time for obtaining/ transporting/ running/reporting a blood gas), and a continuous monitor (rather than an isolated points in time). The advantages of pulse oximetry include use as a continuous noninvasive marker or warning signal for adverse patient events that can result in hypoxia/arterial desaturation. By detecting those events early, treatment can be initiated sooner with the goal of improving patient outcomes. Because clinical detection of cyanosis is unreliable, use of pulse oximetry should allow earlier detection of hypoxemia. Reports from the recovery room and the operating room do indicate a faster detection of hypoxic episodes, a lower incidence and shorter duration of arterial desaturation, and fewer adverse events in the recovery room in cases where pulse oximetry is used. However, several studies of pulse oximetry in anesthesia/post anesthesia care and in general care units failed to show a difference in patient outcome with its use. The consensus and expert opinion are that pulse oximetry can and should be used, and there are many clinical indications for its use.
_
Pulse oximetry is easy to use and requires no special training. It can be applied easily and quickly and is inexpensive. It is small, lightweight, and portable; therefore, it can be used in almost any area and requires little space. It can be stand-alone equipment or incorporated into a bedside monitoring unit. It can be used in any age or type of patient from newborns to geriatric patients, in the ED, intensive care units, inpatient floors, operating suite, recovery room, and in prehospital care. It has become the fifth vital sign and is a standard of care during procedures requiring general anesthesia and during procedural sedation and analgesia.
_
The cons of using Pulse Oximetry:
Like any medical device, pulse oximeters have their downside. Patients are cautioned to use common sense when using a pulse oximeter at home and not to rely, solely, on an oxygen saturation reading as an indicator that something is medically wrong. Moreover, before purchasing a home pulse oximeter, you should understand that they:
•may provide a false reading; for example, a COPD patient can be severely short of breath, but their oxygen saturation reading may be near normal.
•may be ineffective in the presence of certain conditions, including cardiac or respiratory arrest, cardiac arrhythmias, shock, carbon monoxide poisoning, conditions that cause poor circulation or poor perfusion to the tissues, arteriovenous fistulas, cold extremities, edema, black, green or blue nail polish, tremors, shivering, rigor or muscle twitching.
•may lag behind a patient’s condition; for example, the blood oxygen level (PaO2) could potentially decrease to a critical level before the decreased SpO2 (oxygen saturation reading) is displayed on the monitor.
_
Warnings of using pulse oximeter:
• One of the greatest draw back would be although a pulse oximeter is used to monitor oxygenation; it cannot determine the metabolism of oxygen, or the amount of oxygen being used by a patient. For this purpose, it is necessary to also measure carbon dioxide (CO2) levels.
• The pulse oximeter also fails to function properly when there is a reduction of peripheral blood flow as in peripheral vasoconstriction, severe hypotension, cold, cardiac failure, some cardiac arrhythmia and peripheral vascular diseases. This is due to inadequate signal for analysis.
• Venous congestion due to tricuspid regurgitation and various systemic abnormal pulsations can produce low reading.
• Bright overhead lights in surgical rooms and shivering can cause an error in the reading.
• Another huge problem would be the inability to distinguish between different forms of hemoglobin as in methemoglobin and carboxyhemoglobin where low saturations of hemoglobin with oxygen due to the presence of these other forms can bring about a false high saturation value.
_
Pitfalls of SpO2:
_
Pulse oximetry is noninvasive and considered safe, although rare reports of pressure necrosis and burns due to defective probes have been reported. Pulse oximetry probes can be a source of nosocomial infection if they become contaminated with pathogenic bacteria. However, there are many methods to avoid this possibility. Disposable probes can be resterilized, and protective sheaths can be placed on the probe to allow for multiple uses. Pulse oximetry has a low failure rate. In one operating room study, the failure rate was less than 5% with a trend toward failure occurring in elderly and sicker patients and during longer surgical procedures. Accidental disconnection or probe misplacement are probably the most common causes of pulse oximetry failure.
_
Contraindications to pulse oximetry:
Pulse oximetry monitoring should not be used
1. during CPR
2. when patient is hypovolemic
3. for assessing adequacy of ventilator support
4. for detecting worsening of lung function in patients on high concentration of oxygen
These conditions all require blood gas analysis and other laboratory tests for diagnosis and monitoring.
_
A pulse oximeter should never be used during a cardiac arrest situation because of the extreme limitations of blood flow during cardiopulmonary resuscitation and the pharmacological action of vasoactive agents administered during the resuscitation effort.
_______
Look at the Whole Clinical Picture:
There are other pitfalls of oximetry as well. Caregivers must always verify results by looking at the whole clinical picture. A patient’s skin pallor, presence of cyanosis and other factors can belie or substantiate a pulse oximeter reading. Also, since cyanosis of nail beds can be due to poor circulation, the oral mucosa should be checked for color and/or presence of cyanosis. In certain instances, such as the smoke inhalation, an arterial blood gas with co-oximetry may be needed. This will give actual SaO2 and carboxyhemoglobin levels. Even accurate oximeter readings must be used as part of the total assessment. For example, a patient with acute change in his level of consciousness. His pulse oximeter reading may be over 90 percent, and yet, to dismiss a possible respiratory reason for the change in consciousness may be in error, since an increase in carbon dioxide in the blood can cause this change and will not necessarily be picked up by oximetry. Patients with chronic obstructive pulmonary disease can have a reasonable saturation and yet be retaining carbon dioxide, resulting in an acute change consciousness. The use of a pulse oximeter to detect hypoventilation is impaired with the use of supplemental oxygen, as it is only when patients breathe room air that abnormalities in respiratory function can be detected reliably with its use. Therefore, the routine administration of supplemental oxygen may be unwarranted if the patient is able to maintain adequate oxygenation in room air, since it can result in hypoventilation going undetected. Pulse oximetry is an excellent tool as long as care is taken to not depend entirely on this technology in the absence of correlating clinical information.
_______
_______
Oxygenation vs. Ventilation:
Ventilation, which can be spontaneous (as in breathing) or artificial (as in mechanical ventilation) is the movement of air in and out lungs. Both PaO2 and PaCO2 are affected by ventilation. During hypoventilation at room air, PaCO2 will rise and PaO2 will be reduced as less air brings less oxygen and takes away less carbon dioxide. Perfusion is amount of blood flowing in lung capillaries for gas exchange. The blood will exchange oxygen and carbon dioxide at alveolar-capillary membrane with alveolar air. If perfusion is reduced for example due to massive pulmonary embolism, less blood will be available to alveolar air, less blood will be oxygenated and PaO2 and SaO2 will fall. However, PaCO2 will not rise because of high solubility and high diffusing capacity of carbon dioxide compared to oxygen. So CO2 will be exhaled in sufficient quantity despite poor perfusion as long as ventilation is good. In fact hypoxemia induced hyperventilation would wash away CO2 and PaCO2 may be lower (hypocapnia). Additionally, every minute we inhale net 250 ml O2 and exhale net 25 ml CO2 as majority of CO2 produced is converted into H2CO3 to be used in acid-base balance. So this 25 ml CO2 with high diffusing capacity can be removed easily. In other words, oxygenation requires good perfusion and good ventilation while carbon dioxide removal needs good ventilation alone. In other words, carbon dioxide level can be used to judge adequacy of ventilation.
_
Oxygenation refers to the amount of oxygen in a medium. In blood it may be taken to be synonymous with saturation, which describes the degree to which the oxygen-carrying capacity of haemoglobin is utilised, normally 98-100%. PaO2 is affected by supplemental oxygen. If you give supplemental oxygen to a patient, you will see PaO2 rise but PaCO2 unaffected. So PaO2/SpO2 measures oxygenation. A complete respiratory assessment of at-risk patients must include assessment of both oxygenation and CO2 removal i.e. ventilation. Oxygenation—how well oxygen is moving across the alveolar-capillary membrane and into the blood to be carried to tissue—can be determined by analyzing a patient’s partial oxygen pressure (PaO2) and SpO2 (or SaO2). Ventilation (how well a patient can exhale carbon dioxide produced by metabolic activities) can be determined by analyzing a patient’s partial carbon dioxide pressure (PaCO2), and the partial pressure of carbon dioxide in exhaled gas—the end-tidal CO2 (EtCO2). Pulse oximetry estimates oxygenation. Capnography estimates ventilation.
_
What pulse oximetry can’t tell you?
Pulse oximetry is a useful tool for assessing oxygen saturation (oxygenation), but it doesn’t provide a complete picture of your patient’s respiratory status. Understanding what pulse oximetry can and can’t do will help you to use this technology wisely. Pulse oximetry is a noninvasive method of monitoring a patient’s pulse rate and arterial oxygen saturation. A pulse oximeter uses a light-emitting diode (LED) and a photodetector to estimate the percentage of total hemoglobin that’s saturated (filled) with oxygen molecules, based on the amounts of red and infrared light that pass through the vascular bed. Arterial oxygen saturation is represented by the symbol SpO2 when measured by pulse oximetry or SaO2 when measured by co-oximetry. For a healthy patient, an SpO2 of 95% – 100% is generally considered normal. Pulse oximetry is now a part of routine perioperative monitoring, and is widely used to monitor patients in many different settings, including the ED, OR, ICU, PACU, and med/surg units. However, because it doesn’t provide any information about a patient’s ventilation, relying on pulse oximetry alone could compromise patient safety, particularly in patients who are receiving supplemental oxygen or who are at risk of respiratory depression. Yet, a recent study found that only 35% of nurses (and 39% of physicians) in a major medical center knew that pulse oximetry monitored oxygen saturation only and did not reflect changes in ventilation. The study also found that an educational program significantly improved clinicians’ knowledge of pulse oximetry. Pulse oximetry is a valuable tool, but it’s only one part of a complete assessment of a patient’s respiratory status. To be most effective, it must be used properly, and in conjunction with other methods of respiratory monitoring. By understanding the uses and limitations of pulse oximetry, you’ll be able to better assess and care for your patients. Pulse oximetry can tell you about saturation only; to assess other measures of oxygenation and ventilation, you need to consider ABG analysis and capnography (which will be discussed below). In some cases, acceptable pulse oximetry readings (“good sats”) have falsely reassured clinicians despite serious deterioration in a patient’s respiratory status as shown by dangerously high levels of PaCO2. I would emphasize that measurements of carbon dioxide (CO2) and acid–base balance are also critical in the care of patients with respiratory disorders or unbalanced pH and that these disorders cannot be evaluated with the use of pulse oximetry. In particular, a normal pulse oximetry measurement does not exclude important abnormalities in the partial pressure of arterial carbon dioxide (PaCO2) or pH. Therefore, serious elevations in the PaCO2, which are indicative of ventilatory dysfunction, can be present when the results of pulse oximetry are normal. Pulse oximetry is an excellent oxygenation monitor, but it does not alert the clinician to changes in ventilation in a timely manner, particularly when supplemental oxygen is used. Anesthesiologists are well aware of this limitation of pulse oximetry and recommend the use of capnography to monitor ventilation during procedural sedation.
_
Taking a more comprehensive approach to respiratory monitoring is especially important for patients at increased risk of respiratory depression, which can be precipitated by:
• altered level of consciousness due to sedation, medications such as opioids, or other conditions;
• decreased blood flow to the brain’s respiratory centers as the result of increased intracranial pressure, shock, or other factors;
• fatigue associated with the increased work of breathing;
• cardiac or pulmonary diseases that affect oxygenation.
At-risk patients may need not only pulse oximetry but also ABG analysis or capnography. ABG analysis provides a more complete picture of a patient’s respiratory status, including PaO2, PaCO2, arterial pH, and acid-base balance, but it requires a sample of arterial blood and takes time to receive the results.
_
Alveolar hypoventilation is the main form of respiratory failure postoperatively and results from combinations of central respiratory depression, muscular weakness, and upper airways obstruction. As arterial carbon dioxide tension rises so does alveolar carbon dioxide tension (PCO2) because CO2 diffuses rapidly across alveolar capillary membrane; concurrently alveolar PO2 falls, leading to arterial hypoxaemia. If the patient is breathing room air then the saturation will fall early and is a reasonably sensitive indicator of hypoventilation. The situation is different if the patient is receiving supplemental oxygen. The alveolar PO2 will now be much higher and consequently higher PaO2 will raise SpO2.The failure to detect hypoventilation in such a patient is not a failure of pulse oximetry as such but an example of a false sense of security generated by a single physiological variable being within safe limits. The same caveat applies to the use of pulse oximetry to detect hypoventilation under anaesthesia, when patients routinely receive high fractional inspired oxygen concentrations. Although pulse oximetry may be “the most significant technological advance ever made in the monitoring of the well-being and safety of patients during anaesthesia, recovery and critical care,”‘ it must be understood that a normal reading of saturation in the presence of an increased inspired oxygen concentration gives no information about the adequacy of ventilation. Falls in saturation under these circumstances will occur late and are non-diagnostic. Under no circumstances should the pulse oximeter be relied on as the sole monitor to detect such events as oesophageal intubation, cardiac arrest, breathing system disconnections, or failure of the oxygen supply.
_
Although the physiologic consequences of moderate hypoventilation have not been clearly elucidated, profound hypoventilation with the development of carbon dioxide narcosis can cause coma, respiratory arrest, and circulatory failure. Various studies have reported the difficulty in detecting hypoventilation in patients undergoing sedation for GI, dental, and other endoscopic procedures. Moreover, several reports have discussed the failure to diagnose severe hypoventilation in the perioperative period.
_
Historically, an SpO2 90% has been used to define “arterial hypoxemia.” Accordingly, clinicians often will administer supplemental oxygen out of habit to ensure “adequate” oxygenation and to avoid reaching the 90% threshold. But is this clinical practice warranted? Currently, there is no consensus in the literature regarding recommendations on the prophylactic administration of supplemental oxygen to all postoperative patients, and some communications have stressed the dangers of masking severe hypoventilation with supplemental oxygen. It is suggested that the decision to administer supplemental oxygen not be based on routine, but should entail consideration of the risk of masking undetected hypoventilation. One must determine whether lower SpO2 indicate hypoventilation, or mismatching of ventilation and perfusion. Then, appropriate treatment may be administered. Sedation may cause profound respiratory depression and hypoventilation. Thus, accurate monitoring of ventilatory status of sedated patients is desirable. Methods to detect hypoventilation in the spontaneously breathing patients receiving respiratory depressant drugs are limited. Pulse oximetry primarily has been used to assess oxygenation, but not ventilation. A decline in SpO2 during room-air breathing appears to be a reliable indicator of ventilator abnormalities, whether occurring at a global or regional level; the presence of such abnormalities will go undetected in the presence of supplemental oxygen. Without the need for capnography and arterial blood gas analysis, pulse oximetry is a useful tool to assess ventilation in the absence of supplemental inspired oxygen.
_
Supplemental Oxygen impairs detection of Hypoventilation by Pulse Oximetry: a 2004 study:
Study objective: This two-part study was designed to determine the effect of supplemental oxygen on the detection of hypoventilation, evidenced by a decline in oxygen saturation (SPO2) with pulse oximetry.
Design: Phase 1 was a prospective, patient-controlled, clinical trial. Phase 2 was a prospective, randomized, clinical trial.
Setting: Phase 1 took place in the operating room. Phase 2 took place in the postanesthesia care unit (PACU).
Patients: In phase 1, 45 patients underwent abdominal, gynecologic, urologic, and lowerextremity vascular operations. In phase 2, 288 patients were recovering from anesthesia.
Interventions: In phase 1, modelling of deliberate hypoventilation entailed decreasing by 50% the minute ventilation of patients receiving general anaesthesia. Patients breathing a fraction of inspired oxygen (FIO2) of 0.21 (n 25) underwent hypoventilation for up to 5 min. Patients with an FIO2 of 0.25 (n 10) or 0.30 (n 10) underwent hypoventilation for 10 min. In phase 2, spontaneously breathing patients were randomized to breathe room air (n 155) or to receive supplemental oxygen (n 133) on arrival in the PACU.
Measurements and results: In phase 1, end-tidal carbon dioxide and SPO2 were measured during deliberate hypoventilation. A decrease in SpO2 occurred only in patients who breathed room air. No decline occurred in patients with FIO2 levels of 0.25 and 0.30. In phase 2, SpO2 was recorded every min for up to 40 min in the PACU. Arterial desaturation (SpO2 < 90%) was fourfold higher in patients who breathed room air than in patients who breathed supplemental oxygen (9.0% vs 2.3%, p 0.02).
Conclusion: Hypoventilation can be detected reliably by pulse oximetry only when patients breathe room air. In patients with spontaneous ventilation, supplemental oxygen often masked the ability to detect abnormalities in respiratory function in the PACU. Without the need for capnography and arterial blood gas analysis, pulse oximetry is a useful tool to assess ventilator abnormalities, but only in the absence of supplemental inspired oxygen.
_
The efficacy of lung function is evaluated primarily by arterial blood gas analysis. If PaO2 and PaCO2 are within normal limits, then lung function is normal. Many medical decisions, such as whether or not to administer supplementary oxygen in the hospital, prescribe home oxygen therapy, initiate noninvasive ventilation, or initiate mechanical ventilation or wean the patient from it, etc., are based on the interpretation of arterial blood gas values. Some of these decisions, which must be taken more and more often in recent years, have important personal, social, and economic repercussions. Technical innovations have made the equipment used for analyzing gases simpler and easier to handle. It is in this context oxyhemoglobin assessment through pulse oximetry (SpO2) and with the continuous, indirect estimation of PaCO2 by way of end-tidal carbon dioxide pressure (EtCO2) using capnography are discussed.
_______
_______
Capnography vis-à-vis pulse oximetry:
_
Capnography:
Capnography is the monitoring of the concentration or partial pressure of carbon dioxide (CO2) in the respiratory gases. Its main development has been as a monitoring tool for use during anaesthesia and intensive care. Capnography is a form of noninvasive monitoring of the end-tidal carbon dioxide (EtCO2) levels in the patient’s breath. By tracking the carbon dioxide in a patient’s exhaled breath, capnography enables paramedics to objectively evaluate a patient’s ventilatory status (and indirectly circulatory and metabolic status), as the medics utilize their clinical judgement to assess and treat their patients. It is usually presented as a graph of expiratory CO2 (measured in millimeters of mercury, “mmHg”) plotted against time, or, less commonly, but more usefully, expired volume. The plot may also show the inspired CO2, which is of interest when rebreathing systems are being used. The capnogram is a direct monitor of the inhaled and exhaled concentration or partial pressure of CO2, and an indirect monitor of the CO2 partial pressure in the arterial blood. In healthy individuals, the difference between arterial blood and expired gas CO2 partial pressures is very small. In the presence of most forms of lung disease, and some forms of congenital heart disease (the cyanotic lesions) the difference between arterial blood and expired gas increases and can exceed 1 kPa. Capnographs usually work on the principle that CO2 absorbs infrared radiation. A beam of infrared light is passed across the gas sample to fall on a sensor. The presence of CO2 in the gas leads to a reduction in the amount of light falling on the sensor, which changes the voltage in a circuit. The analysis is rapid and accurate. Capnography refers to a unit that displays both a numeric EtCO2 value and a CO2 waveform (capnogram). Capnography provides a graphic representation (a capnogram) of the level of exhaled carbon dioxide (CO2). The capnogram gives you breath-to-breath information about the CO2 that’s being exhaled from the lungs.
Capnography – the measurement of carbon dioxide (CO2) in exhaled breath.
Capnometer – the numeric measurement of CO2.
Capnogram – the wave form.
Capnograph – a device that measures CO2 in breath
End Tidal CO2 (EtCO2) – the level of (partial pressure of) carbon dioxide released at end of expiration.
_
Capnogram:
A typical capnogram is shown in the figure below. During inspiration the CO2 tension should be neligible unless there is rebreathing. Dead space gas is exhaled first, it contains no CO2, and is followed by alveolar gas and a rapid rise in CO2 which reaches a clear plateau in normal lungs and is termed the end-tidal CO2 tension. However, if there is significant inhomogeneity of ventilation within the lungs no clear plateau is discernible and an accurate end-tidal CO2 cannot be measured. This occurs in obstructive airway disease and asthma. If tidal volumes are very small there is inadequate distinction between dead space and alveolar gas resulting in an indistinct expiratory plateau and the end-tidal CO2 tension is inaccurate.
_
_
End-tidal CO2 (EtCO2) is the quantitative value of exhaled carbon dioxide measured from a sample source of gas obtained at the point of end-tidal exhalation. Normal values of EtCO2 are 35-45 mmHg (4.5% – 6 %), and in normal lungs, the EtCO2 approximates the arterial CO2 concentration in the blood with a value that is usually lower by 2 to 5 mmHg. Use of capnography is not limited to intubated patients; nasal cannulas and face masks can be modified to detect EtCO2. Capnography devices are now easy to use and available for patients without artificial airways; exhaled CO2 is collected from a nasal cannula-like device. Most effective way to evaluate ventilation in an alert but sedated patient is by sidestream capnography. The use of oxygen cannulas modified with an I.V. catheter that do not provide total separation on insufflated oxygen and aspirated CO2 will not produce a reliable baseline for CO2 monitoring that will be consistent with the PaCO2. Monitors are available for bedside use in med/surg, as part of portable monitor-defibrillators for transport, and as cartridges that can be added to the wall-mounted component of central monitoring systems in critical care areas.
_
There is a simple reason capnography monitoring is increasingly becoming the standard of care during outpatient surgery procedures: it provides an immediate alarm for life-threatening breathing problems during moderate or deep sedation. Capnography monitors track end-tidal carbon dioxide (EtCO2), the concentration of carbon dioxide in exhaled air. Capnography waveforms immediately detect changes in CO2 levels that could signal respiratory distress or failure. Pulse oximeters, which had been the standard of care in outpatient surgery, take much longer to register respiratory distress. This is because oxygen levels in blood can remain normal for several minutes after a patient stops breathing.
The benefits of capnography are being recognized by professional organizations in a wide range of fields, including:
•American Association of Oral and Maxillofacial Surgeons: AAOMS Office Anesthesia Evaluations began requiring capnography in 2014 for moderate sedation, deep sedation and general anesthesia.
•Institute for Safe Medication Practices: The ISMP recommends patient-controlled analgesia procedures follow the Anesthesia Patient Safety Foundation’s guidelines on using capnography to detect unrecognized hypoventilation and carbon dioxide retention.
•American Heart Association: In 2010, the AHA began recommending the use of capnography to verify endotracheal tube placement in during triage for patients with acute coronary syndromes.
•Society of Interventional Radiology: In response to the American Society of Anesthesiologists capnography standards, the SIR recommends that interventional radiologists familiarize themselves with how capnography works and its benefits over pulse oximetry.
•Anesthesia Patient Safety Foundation: The APSF Winter 2012 Newsletter includes a four-part case study on capnography monitoring reform at St. Joseph’s/Candler Health System in Savanna, Ga.
•American Association for Accreditation of Ambulatory Surgery Facilities: The ASAASF updated its 2014 standards to include mandatory, continual end-tidal carbon dioxide monitoring to confirm correct endotracheal tube placement.
•Journal of Emergency Medical Services: A 2014 article touts the importance of prehospital airway management through the use of capnography and other monitoring techniques.
•Canadian Anesthesiologists’ Society: The CAS 2012 Guidelines were expanded to require capnography monitoring during conscious sedation and when patient airways have not been instrumented.
•Oregon Board of Dentistry: Oregon state laws were updated in 2014 to include capnography monitoring for patients under moderate sedation, deep sedation and general anesthesia. To receive permits in the above listed kinds of sedation, practices must have both capnography and pulse oximetry on site available for immediate use.
______
Capnography versus Pulse Oximetry:
Capnographs and pulse oximeters present different views of the same cardiopulmonary processes. Oximeters measure saturated hemoglobin in peripheral blood and provide additional information about the adequacy of lung perfusion and oxygen delivery to the tissues. However, pulse oximetry is a late indicator of O2 supply, and is less sensitive than capnography. Healthy patients can maintain SaO2 > 90% for minutes even with inadequate ventilation. It does not afford a complete picture of ventilatory status. Capnography provides an immediate picture of patient condition. Pulse oximetry is delayed. Hold your breath. Capnography will show immediate apnea, while pulse oximetry will show a high saturation for few minutes. While capnography is a direct measurement of ventilation in the lungs, it also indirectly measures metabolism and circulation. For example, an increased metabolism will increase the production of carbon dioxide increasing the EtCO2. A decrease in cardiac output will lower the delivery of carbon dioxide to the lungs decreasing the EtCO2. Accurate pulse oximetry measurement is dependent upon adequate peripheral perfusion and may be unreliable in patients who have compromised peripheral circulation. Capnography continuously and nearly instantaneously measures pulmonary ventilation and is able to rapidly detect small changes in cardio-respiratory function before oximeter readings change. Many sources recommend monitoring both SpO2 and EtCO2 on intubated and non-intubated patients.
_
Which is better, pulse oximetry or waveform capnography?
The best choice depends on what we are trying to do.
If the patient is receiving paralytics during an intubation attempt, does waveform capnography matter?
No, but the pulse oximetry is important in determining how long it is safe to continue to attempt to intubate before ventilating the patient again (whether with a BVM or a crichothyrotomy). With use of preoxygenation and passive apneic oxygenation, patients may tolerate apnea for extended periods without desaturation. Apneic oxygenation dramatically changes the way we approach airway management.
Does it matter if the patient is not breathing, if the patient’s oxygen saturation is in the high 90s?
Yes, because ventilation is the removal of CO2. If the patient is already acidotic, even a brief period of apnea may kill the patient.
Does it matter if the cardiac arrest patient is receiving ventilation?
No. Chest compressions appear to provide adequate ventilation without any use of the usual means of ventilation.
Does pulse oximetry have a place in the assessment of endotracheal tube placement?
Yes, but waveform capnography is almost always the best means of tube confirmation.
_
Ideally, when monitoring ventilation and oxygenation in the prehospital environment, capnography should be combined with pulse oximetry. With capnography, providers are able detect respiratory insufficiency early and are able to institute early interventions, thereby preventing arterial oxygen desaturation. However, as with any monitoring technology, the best “monitor” is the provider. Pulse oximeters and capnometers do not treat patients. Integrating the information from your monitors and clinical assessment to make sound clinical decisions is the key to successful airway management. As evidenced by the astute assessment and action of a paramedic, knowing the difference between ventilation and oxygenation is a critical concept that must be understood.
_
Capnography (carbon dioxide detection) is a modality that is recommended by most anaesthesia societies, including the ASA and WFSA. It allows detection of esophageal intubation and hypoventilation nearly 100% of the time and is the monitoring modality of choice for this purpose. Yet, in resource limited settings, the benefits of capnography are less compelling than those of pulse oximetry. As Webb and colleagues have reported, pulse oximetry detects adverse events more frequently. This is presumably because pulse oximetry detects hypoxemia, which is the most common cause of death as Cooper showed nearly 20 years ago. Furthermore, increased alveolar carbon dioxide concentrations from any cause (notably hypoventilation) can be detected early with pulse oximetry if the inspired oxygen concentration is maintained at or close to that in ambient air. By contrast, early hypoxia is not readily detected with capnography. Additionally, the cost and maintenance of oximetry are generally lower than capnography. For these reasons, pulse oximetry is the preferred monitoring modality in resource-limited settings.
_
Accuracy and reliability of pulse oximetry at different arterial carbon dioxide pressure levels: a 2008 study:
The present study aimed to assess whether arterial carbon dioxide pressure (PaCO2) has an impact on agreement between oxygen saturation measured with pulse oximetry (SpO2) or arterial blood gas co-oximetry (SaO2). Arterial carbon dioxide pressure status can contribute to impaired agreement between arterial oxygen saturation and arterial oxygen saturation measured with pulse oximetry, particularly in patients with hypercapnia. The main finding emerging from the present study is that PaCO2 levels can affect the accuracy and reliability of SpO2 measurements. Agreement between SaO2 and SpO2 decreases as PaCO2 increases, regardless of the grade of associated hypoxaemia. Moreover, in a large series of determinations, the present study also confirmed that SpO2 correlates poorly with SO2 when PaO2 is low, particularly when it is 54 mmHg (7.20 kPa).
_______
Capnography with pulse oximetry (combination):
Over the past two decades, technologies have developed to allow for rapid and continuous determination of many physiologic parameters in anesthetized and critical care patients. Two of the most important modalities are pulse oximetry and capnometry. With their use, a clinician is better equipped to ensure adequate oxygen delivery at the cellular and microcellular level and ensure a proper pH for optimal physiologic cellular function in patients. This has led to a dramatic improvement in patient safety, care and outcomes. In a study of closed claims of anesthetic-related malpractice cases, it was determined that a combination of pulse oximetry and capnography could have prevented 93% of avoidable mishaps.
_
Capnography with pulse oximetry:
The Capnostream is a portable bedside monitor that continuously monitors a patient’s:
• End tidal carbon dioxide (EtCO2) – level of carbon dioxide in exhaled breath.
• Respiratory rate (RR).
• Fractional inspired carbon dioxide (FiCO2) – level of carbon dioxide present during inhalation.
• Oxygen saturation (SpO2).
• Pulse rate (PR).
The Capnostream combined capnograph/pulse oximeter monitor is intended to provide professionally trained health care providers the continuous, non-invasive measurement and monitoring of carbon dioxide concentration of the expired and inspired breath and respiration rate, and for the continuous non-invasive monitoring of functional oxygen saturation of arterial hemoglobin (SpO2 and pulse rate). It is intended for use with neonatal, pediatric and adult patients in hospitals, hospital type facilities, intra hospital moves and home environments.
_
Capnostream:
_
Nonin 9847 Hand Held Pulse Oximeter with CO2 Detector, Alarms & Memory:
The Nonin 9847 combines proven pulse oximetry technology with reliable CO2 detection, making it an ideal monitor for patient transport and emergency use. The Nonin 9847 Pulse Oximeter/CO2 Detector provides “first breath” activation by eliminating any warm-up time – simply turn on the power and start taking measurements. Nonin’s patented semi-quantitative CO2 technology, combined with mainstream sampling, eliminates the need for calibration, thus reducing operating expenses.
_
A single-blind study of combined pulse oximetry and capnography in children: a 1991 study.
This single-blind study examined four levels of monitoring in 402 pediatric cases. Patients were randomly assigned to one of four groups: 1) oximeter and capnograph; 2) only oximeter; 3) only capnograph; or 4) neither oximeter nor capnograph data available to the anesthesia team. An anesthesiologist, not involved in patient care, observed all cases and continuously recorded hemoglobin oxygen saturation (SpO2), ECG, expired CO2, and the oximeter plethysmographic output. Mean age, weight, ASA physical status, airway management (mask or endotracheal tube), and anesthetic technique were similar in each group. Two-hundred sixty problems were documented in 153 patients. Fifty-nine events in 43 patients resulted in “major” desaturation (SpO2 less than or equal to 85% for greater than or equal to 30 s). Fifteen “major” capnograph events (esophageal intubation, disconnection, accidental extubation, or obstructed endotracheal tube) were observed in 11 patients; 8 of these also developed varying degrees of desaturation. One-hundred thirty “minor” desaturation events (SpO2 less than or equal to 95% for greater than 60 s) and 79 “minor” capnograph events (hypercarbaria or hypocarbia) were observed. A number of problems fulfilled criteria in multiple categories. Infants less than or equal to 6 months of age had the highest incidence of major desaturation events (18 of 65 [27%]) compared to toddlers 7-24 months of age or children greater than 24 months of age (P less than 0.001). Blinding the oximeter data increased the number of patients (12 vs. 31) experiencing major desaturation events (P = 0.003); blinding the capnograph data altered neither the frequency of desaturation events nor the incidence of major capnograph events.
_
Pulse Oximetry and Capnography in Lung Function Laboratories: a 2004 study.
Objective was to compare values reflecting oxyhemoglobin saturation obtained by pulse oximetry (SpO2) and values for end-tidal carbon dioxide pressure (EtCO2) obtained by capnography with direct measures of gas saturation values and pressures (PaO2 and PaCO2) in arterial blood gas samples. Both measurement devices (pulse oximeter and capnograph) are appropriate for use in a lung function laboratory. The difference between EtCO2 and the PaCO2 should be kept in mind. The findings of the present study indicate that oxyhemoglobin saturation estimated as SpO2 by pulse oximetry adequately reflects arterial blood oxyhemoglobin saturation. EtCO2 obtained by capnography enabled estimation of alveolar ventilation, with a bias in the same direction–since it indirectly reflects PaCO2. However, these two devices for automatic measurement have certain limitations and appropriate applications, which interpreters should be aware of and take into proper consideration.
_
Application of capnography and SpO2 measurement in the evaluation of respiratory failure in patients with chronic obstructive pulmonary disease: a 2010 study.
In patients with COPD (especially those with also type II respiratory failure), the modified monitoring method of PCO2 and maintenance of SpO2 above 90% can precisely estimate PaCO2 and PaO2. This method is feasible for clinical noninvasive and dynamic evaluation of respiratory failure in COPD patients, especially in primary care facilities where arterial blood gases analysis is not available.
_______
_______
Common causes of hypoxemia:
| Hypoxemia | SpO2 by pulse oximetry | EtCO2 by capnography | Can supplemental O2 raise SpO2? |
| Hypoventilation | Low | High | Yes |
| Low inspired O2 (e.g. high altitude) | Low | Low due to hypoxemia induced hyperventilation | Yes |
| R to L shunt | Low | Normal | No but with small shunt yes |
| V/P mismatch | Low | Normal | Yes |
| Diffusion defect | Low | Normal | Yes |
Three points emerge from above table:
1. Only hypoventilation causes hypoxemia with hypercapnia. All other causes of hypoxemia have no hypercapnia.
2. Supplemental oxygen raises SpO2 in almost all cases of hypoxemia.
3. Capnography is useful essentially in hypoventilation but of no use in all other causes of hypoxemia.
_________
_________
Transcutaneous Carbon dioxide and Oxygen monitoring:
Transcutaneous measurements of oxygen and carbon dioxide are based on the principle that a heating element in the electrode elevates the temperature of the underlying tissues. This increases the capillary blood flow and the partial pressure of oxygen and carbon dioxide, and makes the skin permeable to gas diffusion. It must be remembered that the electrode is measuring the gas tensions of the underlying tissue and not the arterial gas tension. When haemodynamic conditions are stable, the transcutaneous measurements correlate well with arterial values but are not identical. The actual level of transcutaneous oxygen reflects the relationship between the increase in partial pressure in the capillary blood due to heating, the level of skin blood flow and the metabolic oxygen consumption of the skin. In spite of these physiological factors, when blood flow is normal, transcutaneous oxygen values can reliably reflect arterial values. In the case of PtcCO2, the elevated temperature at which the transcutaneous electrode operates in order to increase skin permeability will also raise skin metabolism and lead to an increase in CO2 production. The measured values will, therefore, be significantly higher than arterial values at 37 C. The transcutaneous values can be temperature corrected, thus enabling a readout of values comparable to those at the normal body temperature. These will deviate by a small metabolic contribution from the carbon dioxide production in the epidermis. Transcutaneous monitoring of carbon dioxide tension (PCO2) has been shown to be more reliable than the transcutaneous measurement of oxygen due to the greater diffusion capacity of carbon dioxide through the skin. The more recent development in transcutaneous technology has been the introduction of a solid-state combined PtcO2/PtcCO2 electrode with the glass section of the PtcCO2 electrode being strengthened by incorporation of ceramic material, making it much more robust and less liable to damage.
_
_
Site selection:
The absolute value of PtcO2 is affected by skin thickness and capillary density. It is therefore important to place the electrode at a site of high capillary density and minimal thickness for optimal transcutaneous measurements. This presents no problem in the newborn, in whom these conditions are usually fulfilled. In adults, there is greater variation from site to site and the suggested locations for optimal transcutaneous measurements are the forearm, chest or abdomen.
_
Combination of pulse oximetry with transcutaneous CO2 sensor:
The TOSCA monitor (Linde Medical Sensors AG, Basel, Switzerland) combines pulse oximetry (SpO2) and transcutaneous PCO2 (PtcCO2) monitoring in a single ear sensor:
Monitoring carbon dioxide tension and arterial oxygen saturation by a single earlobe sensor in patients with critical illness or sleep apnea: a 2005 study:
The purpose of the study was to evaluate a novel, combined sensor for transcutaneous monitoring of arterial oxygen saturation and carbon dioxide tension. The new monitoring technique was compared to established reference methods. Continuous measurements were performed over several hours by the novel heated (temperature, 42 degrees C) earlobe sensor (TOSCA; Linde Medical Sensors; Basel, Switzerland), incorporating electrochemical and optical elements for carbon dioxide measurement (PtcCO2) and pulse oximetry (SPO2), respectively. The data were compared to the results of repeated arterial blood gas analyses in critically ill patients and to simultaneous nocturnal pulse oximetry performed with different devices with earlobe or finger sensors in sleep apnea patients. In critically ill patients, the mean difference and limits of agreement (bias +/- 2 SDs) of transcutaneous PtcCO2 vs arterial PaCO2 were 3 +/- 7 mm Hg; the corresponding values for changes in PtcCO2 vs PaCO2 were 1 +/- 6 mm Hg. The bias +/- 2 SDs for pulse oximetric SpO2 vs arterial oxygen saturation (SaO2) were 1 +/- 4%. In sleep apnea patients, the combined earlobe sensor identified more transient oxygen desaturations, and the rate of change in oxygen saturation during events was greater compared to those with other tested pulse oximeters, indicating a faster response. Due to its ability to accurately assess both ventilation and oxygenation by a single transcutaneous sensor, the described noninvasive monitoring technique is a valuable tool for respiratory monitoring with potential applications in critical care and sleep medicine.
_________
_________
Integrated Pulmonary Index:
Integrated Pulmonary Index (IPI) is a patient pulmonary index which uses information from capnography and pulse oximetry to provide a single value that describes the patient’s respiratory status. IPI may be used by clinicians to quickly assess the patient’s respiratory status to determine the need for additional clinical assessment or intervention. The IPI incorporates four patient parameters (end-tidal CO2 and respiratory rate measured by capnography, as well as pulse rate and blood oxygenation SpO2 as measured by pulse oximetry) into a single index value. The IPI value on the patient monitor indicates the patient ventilatory status, where a score of 10 is normal, indicating optimal pulmonary status, and a score of 1 or 2 requires immediate intervention. The IPI algorithm was developed based on data from a group of medical experts (anaesthesiologists, nurses, respiratory therapists, and physiologists) who evaluated cases with varying parameter values and assigned an IPI value to a predefined patient status. A mathematical model was built using patient normal ranges for these parameters and the ratings given to various combinations of the parameters by these professionals. Fuzzy logic, a mathematical method which mimics human logical thinking, was used to develop the IPI model. Clinical validation studies indicate that the IPI value produced by the IPI algorithm accurately reflects the patient’s ventilatory status. In studies on both adult and pediatric patients, in which experts’ ratings of ventilatory status were collected along with IPI data, the IPI scores were found to be highly correlated with the experts’ annotated ratings. IPI can promote early awareness to changes in a patient’s ventilatory status. The caregiver can view the IPI trend, which indicates changes in IPI over time. A quick view of the IPI trend can show that if the IPI has changed over the previous minutes or hours, to help the clinician ascertain if the patient’s overall ventilatory status is worsening, remaining steady, or improving. This information can help determine the next steps in patient care. Thus, IPI can simplify the monitoring of patients in clinical environments. The caregiver can quickly and easily assess a patient’s ventilatory status by following one number, the IPI, before checking the four parameters that make up this number. The four parameters continue to be displayed on the monitor screen. A significant change in the IPI is a “red flag” indicator, indicating that the clinician should review other monitored data and assess the patient. In the clinical environment, a quick check of the IPI value and IPI trend is a first indicator of pulmonary status of the patient and may be used to determine if further patient assessment is warranted. IPI can increase patient safety, by indicating the presence of slow-developing patient respiratory issues not easily identified with individual instantaneous data to the caregiver in real time. This enables timely decisions and interventions to reduce patient risk, improve outcomes and increase patient safety. Since normal values for the physiological parameters are different for different age categories, the IPI algorithm differs for different age groups (three paediatric age groups and adult). IPI is not available for neonatal and infant patients (up to the age of 1 year).
______
______
Innovations in the conventional two wavelength (660 and 940nm) pulse oximeter:
_
Since first generation devices, technical advances which have been made to improve pulse oximetry include:
● Calibration resistors and chips embedded into the sensor to compensate for LED differences
● The use of ECG synchronization techniques to anticipate arterial pulses by simultaneously recording the electrocardiograph.
● Various motion sensing improvements to help with reducing artifact and low pulsatile flow situations. An example of a new development can be found at Masimo SET (vide infra)
● Specialty sensors for high altitude climbers, resuscitation situations and cyanotic babies.
● Smart alarm systems for pulse oximeters.
● A reduction in size, cost and power use. Researchers at MIT have developed a ring sized pulse oximeter.
● Fingertip pulse oximeters with wireless connection via Bluetooth technology are made by NONIN
_
Wavelength selection for low-saturation pulse oximetry:
Conventional pulse oximeters are accurate at high oxygen saturation under a variety of physiological conditions but show worsening accuracy at lower saturation (below 70%). Numerical modelling suggests that sensors fabricated with 735 and 890 nm emitters should read more accurately at low saturation under a variety of conditions than sensors made with conventionally used 660 and 900 nm band emitters. Recent animal testing confirms this expectation. It is postulated that the most repeatable and stable accuracy of the pulse oximeter occurs when the fractional change in photon path lengths due to perturbations in the tissue (relative to the conditions present during system calibration) is equivalent at the two wavelengths. Additionally, the penetration depth (and/or breadth) of the probing light needs to be well matched at the two wavelengths in order to minimize the effects of tissue heterogeneity. At high saturation these conditions are optimally met with 660 and 900 nm band emitters, while at low saturation 735 and 890 nm provide better performance.
_
Advanced pulse oximetry:
Signal extraction technology (SET):
For many years, bioengineers realized that the movement of blood in the venous circulation in a tissue might introduce a significant degree of “noise” to the pulse oximetry readings, which may interfere with these devices displaying readings in situations of low perfusion or movement. Because of this noise, traditional pulse oximeters are subject to false alarms or inaccurate readings, often in critical situations. In 1995, Masimo (Irvine, California) introduced an advanced method of obtaining pulse oximetry readings, using what it calls signal extraction technology (SET). These devices include the traditional-appearing Pronto pulse oximeter as well as the touchscreen Pronto-7. Many studies have demonstrated the advantages of SET in a variety of clinical situations. For example, it has been shown that Masimo’s SET pulse oximeters in the neonatal intensive care unit can reduce the incidence of retinopathy of prematurity by helping to control oxygen exposure. The technology also reduces the number of false alarms in critical care situations because SET pulse oximeters can obtain accurate readings under circumstances of low perfusion or movement. Masimo’s SET pulse oximeters and sensors were exclusively used in the 2 studies that were the basis for the Critical Congenital Heart Disease (CCHD) workgroup decision to recommend newborn screening, and the devices were the first to receive US Food and Drug Administration (FDA) clearance with labelling for CCHD screening.
_
Twenty-four years ago, two young engineers asked themselves why pulse oximetry wouldn’t work during patient motion and low perfusion–and by doing so, set a new course that created a revolution in patient monitoring. Since its inception, pulse oximetry was plagued by unreliability when it was needed most–during patient motion and low perfusion. The industry had given up and considered the problem “unsolvable.” Clinicians were forced to live with the results–excessive false alarms, delayed notification due to long averaging times, inaccurate data, and an inability to obtain data on the most critical patients. Conventional pulse oximetry works under the assumption that by looking at only the pulse and normalizing the pulsating signal over the non-pulsating signal, oxygen saturation (SpO2) can be measured without calibration. Although this was a big step forward in the evolution of pulse oximetry, it has one major flaw–it assumes the only pulsating component is arterial blood. Unfortunately for conventional pulse oximetry, venous blood moves every time the patient moves or breathes. This causes conventional pulse oximeters to display false low or high SpO2 and pulse rates–resulting in false alarms as high as 90% in ICUs and recovery rooms. When Joe Kiani and Mohamed Diab looked at the same pulse oximetry signal differently than anyone had before, they created new possibilities. By employing advanced signal processing techniques–including parallel engines and adaptive filters–they believed they could find the true arterial signal that would allow accurate monitoring of arterial oxygen saturation and pulse rate, even during the most challenging conditions. Signal Extraction Technology assumes that both the arterial and venous blood can move and uses parallel signal processing engines to separate the arterial signal from sources of noise (including the venous signal) to measure SpO2 and pulse rate accurately, even during motion. Conventional pulse oximetry uses the standard red over infrared algorithm to provide SpO2, while SET uses that conventional algorithm but has added four other algorithms that all run in parallel. These algorithms allow the distinction between arterial and venous signal during motion and low perfusion by identifying and isolating the non-arterial and venous noise SpO2 from the true arterial SpO2 components in the signal. Because of its unmatched reliability during challenging conditions of motion and low perfusion, clinicians at thousands of hospitals around the world count on SET pulse oximeter every day to help them care for patients. And while many leading hospitals have already integrated SET pulse oximetry technology, more are converting every day. These hospitals and clinicians trust SET to help them deliver the most effective and efficient patient care possible. With fewer false alarms, clinicians can focus on the patients who need the most attention. With more trustworthy measurements, clinicians can more tightly control oxygenation levels. And with more timely detection of true events, clinicians can intervene earlier for better patient outcomes and improved patient safety.
_
Clinical Accuracy of SET pulse oximetry:
To date, more than 100 independent and objective studies have shown that SET outperforms all other pulse oximetry technologies, providing clinicians with unmatched sensitivity and specificity to make critical patient care decisions. Published papers have compared signal extraction technology to other pulse oximetry technologies and have demonstrated consistent favorable results for signal extraction technology. Signal extraction technology pulse oximetry performance has also been shown to translate into helping clinicians improve patient outcomes. In one study, retinopathy of prematurity (eye damage) was reduced by 58% in very low birth weight neonates at a center using signal extraction technology, while there was no decrease in retinopathy of prematurity at another center with the same clinicians using the same protocol but with non-signal extraction technology. Other studies have shown that signal extraction technology pulse oximetry results in fewer arterial blood gas measurements, faster oxygen weaning time, lower sensor utilization, and lower length of stay. The measure-through motion and low perfusion capabilities it has also allow it to be used in previously unmonitored areas such as the general floor, where false alarms have plagued conventional pulse oximetry. As evidence of this, a landmark study was published in 2010 showing clinicians using signal extraction technology pulse oximetry on the general floor were able to decrease rapid response team activations, ICU transfers, and ICU days.
_
With SET pulse oximetry, false alarms have been reduced by over 95%, while true alarm detection has increased to over 97%–even during conditions of motion and low perfusion.
_
_
_
Detection of SpO2 in patients with extremely low Cardiac Output or Cardiac Standstill:
Sensitivity of Pulse Oximeter system during extremely low local perfusion:
Attempts have been made to maximize sensitivity for detecting pulsation and SpO2 values in patients suffering from extremely low cardiac output and/or low local perfusion levels. Signal extraction technology can read perfusion levels at least 10 fold lower than conventional pulse oximeters. SET pulse oximeter provides valuable information (when other pulse oximeters cannot) in critical situations where very low perfusion can occur, such as ICU, Trauma, Cardio-Pulmonary Bypass and, resuscitation.
The level of SpO2 in a dying or dead patient:
This is somewhat variable and depends on the cause of death and the clinical treatment the patient is receiving at the time of death. However, it is quite possible for a dying or dead patient to have a high SpO2 value. This is the case when peripheral oxygen consumption is quite low, resulting in an increased mixed venous saturation. If extraction is very low and the patient is still receiving oxygen therapy, it is easily possible for the patient to have a high SpO2 value.
_
Additionally, the Pronto and Pronto-7 oximeters can be used to estimate the arterial hemoglobin content (called SpHb) when used with proprietary “rainbow” sensors that use 7 separate wavelengths of light to obtain their measurements. Current SpHb sensors are too large to be used with small children, but Masimo just recently developed a sensor for use in children weighing as little as 10 kg. This new sensor is presently being evaluated by the FDA. A consumer version of Masimo’s SET pulse oximeter sensor can be used with an application that runs on iOS or Android.
_
Masimo pulse oximeters produce a measurement called the perfusion index (PI) that has been shown to correlate with the well-being of premature babies in the first weeks of life. The PI is the ratio of the pulsatile blood flow to the nonpulsatile or static blood in peripheral tissue and it represents a noninvasive measure of peripheral perfusion. In 1995 Masimo introduced perfusion index, quantifying the amplitude of the peripheral plethysmograph waveform. Perfusion index has been shown to help clinicians predict illness severity and early adverse respiratory outcomes in neonates, predict low superior vena cava flow in very low birth weight infants, provide an early indicator of sympathectomy after epidural anesthesia, and improve detection of critical congenital heart disease in newborns.
_
In 2007, Masimo introduced the first measurement of the pleth variability index (PVI), which multiple clinical studies have shown provides a new method for automatic, noninvasive assessment of a patient’s ability to respond to fluid administration. Appropriate fluid levels are vital to reducing postoperative risks and improving patient outcomes: fluid volumes that are too low (under-hydration) or too high (over-hydration) have been shown to decrease wound healing and increase the risk of infection or cardiac complications. Recently, the National Health Service in the United Kingdom and the French Anesthesia and Critical Care Society listed PVI monitoring as part of their suggested strategies for intra-operative fluid management.
__________
Non-invasive pulse co-oximeter:
All pulse oximeters in common use measure tissue light transmission at two wavelengths (two colors) to estimate arterial hemoglobin saturation. With only two wavelengths, these pulse oximeters must “assume” the presence of only two light absorbers in the blood: oxyhemoglobin and reduced hemoglobin. If any other light absorbers are present in the blood, the pulse oximeter’s calibration may be invalid. Intravenous injection of dyes such as methylene blue can cause very low oxygen saturation (SpO2) readings—as low as 4% in one study. The common dyshemoglobins, methemoglobin and carboxyhemoglobin, have been shown to produce serious errors in SpO2 readings in animal studies. These errors have been confirmed in clinical case reports. No previous commercially produced pulse oximeter has successfully measured these dyshemoglobins, or even provided accurate SpO2 values in their presence. Given the life-threatening dangers of methemoglobin and carboxyhemoglobin toxicity, a pulse oximeter capable of measuring these dyshemoglobins would be an important addition to our monitoring armamentarium. Masimo has now developed such an instrument, the Rainbow-SET Rad-57 Pulse CO-Oximeter (Masimo Inc., Irvine, CA). The Rad-57 uses eight wavelengths of light instead of the usual two and is thereby able to measure more than two species of human hemoglobin. It is approved by the US Food and Drug Administration for the measurement of both carboxyhemoglobin and methemoglobin. In addition to the usual SpO2 value, the Rad-57 displays SpCO and SpMet, which are the pulse oximeter’s estimates of carboxyhemoglobin and methemoglobin percentage levels, respectively.
_
Measurement of Carboxyhemoglobin and Methemoglobin by Pulse Co-oximetry: a 2006 study:
A new eight-wavelength pulse oximeter is designed to measure methemoglobin and carboxyhemoglobin, in addition to the usual measurements of hemoglobin oxygen saturation and pulse rate. This study examines this device’s ability to measure dyshemoglobins in human volunteers in whom controlled levels of methemoglobin and carboxyhemoglobin are induced. The Rad-57 measured carboxyhemoglobin with an uncertainty of 2% within the range of 0–15%, and it measured methemoglobin with an uncertainty of 0.5% within the range of 0–12%. Masimo Rainbow-SET Rad-57 Pulse CO-Oximeter can detect and measure both methemoglobin and carboxyhemoglobin within the ranges covered by this experiment: 0–12% for methemoglobin and 0–15% for carboxyhemoglobin. This study did not investigate the accuracy of the Rad-57 for the measurement of SpO2. The Rad-57 currently uses the same two-wavelength SpO2 calculation algorithm used by previous Masimo SET pulse oximeters, and the accuracy will therefore be the same as those instruments. Because it calculates SpO2 using two wavelengths (as opposed to the eight wavelengths used to calculate SpMet and SpCO), the Rad-57 SPO2 readings will be subject to the usual errors induced by methemoglobin and carboxyhemoglobin, as discussed before.
_
With any new technology, questions arise and suspicions abound. Touger et al, in an Annals of Emergency Medicine paper published in October 2010, suggested the RAD-57 was not accurate. In his New York City (Jacobi Medical Center) study of CO poisoned patients, the RAD-57 had a sensitivity of only 48%, meaning that only 48% of actually CO poisoned patients were detected by the device. As expected, the manufacturer vigorously defended their device, suggesting that the Touger study was yet one negative appraisal of their technology amidst a plethora of more favorable evaluations. Many EMS systems, in apparent deference to skepticism, put the brakes in widespread use of RAD-57 technology. Even the Eagles, a cutting edge (and perhaps the premier annual) EMS scientific conference offered an analysis of Touger and its implications for EMS. In July 2011 came Roth et al, also in Annals of Emergency Medicine. In this (massively larger) study done at AKH, one of the biggest hospitals in Vienna, Austria, the RAD-57 had a sensitivity of 94%. The authors concluded that the RAD-57 most certainly could reliably screen large numbers of potentially CO poisoned patients. Roth evaluated 1,578 patients compared to 120 patients in the Touger study.
_
Total hemoglobin measurement by non-invasive pulse co-oximetry:
Hemoglobin can be measured on a variety of devices using different principles of operation. Non-invasive pulse Co-oximetry represents the latest development in hemoglobin measuring technology. Pulse Co-oximetry (Masimo Corp, Irvine, CA, USA) is commercially available technology that allows for the continuous non-invasive measurement of haemoglobin, referred to as SpHb. This technology uses a multiple wavelength, spectrophotometric sensor that may be an adhesive single use type for continuous monitoring or a reusable finger clip sensor for spot check assessments. Pulse Co-oximetry allows the non-invasive measurement of carboxyhaemoglobin, methaemoglobin, oxygen content, Pleth Variability Index, along with standard pulse oximetry parameters, oxygen saturation, pulse rate, and perfusion index. SpHb measurement with Pulse Co-oximetry is available in a number of devices designed for the continuous monitoring at the hospital bedside (Radical-7, Rad-87) or for spot check applications with hand held devices (Rad-57, Pronto).
_
Rad-87
_
Rad-87 Measurements:
•Total Hemoglobin (SpHb)
• Oxygen Content
•Carboxyhemoglobin (SpCO)
•Methemoglobin (SpMet)
•Plus: SET measurements of Oxygen Saturation (SpO2), Pulse Rate (PR), Perfusion Index (PI), and Pleth Variability Index (PVI)
_
Most of the studies published thus far on the performance of SpHb measurement with Pulse Co-oximetry assess the accuracy of continuous monitoring in surgical patients. Berkow and colleagues investigated the accuracy of SpHb compared to laboratory Co-oximetry measurement of 130 arterial blood samples from 29 complex spine surgery patients and found an absolute bias and standard deviation of 0.8 ± 0.6 g/dL. Causey et al. studied both surgical and intensive care patients and found a similar bias of 0.29 g/dL. In a study on 44 patients with acute haemorrhage during surgery, Lamhaut et al. compared SpHb and capillary haemoglobin measurement to laboratory determination. The authors obtained a total of 85 measurements, which showed a bias of only −0.02 g/dL (SD 1.39) and a precision of 1.11 g/dL (SD 0.83). However, in comparison to laboratory haemoglobin determination, the percentage of outliers was significantly higher with noninvasive than with capillary measurement. Conversely, when Frasca et al. examined the performance of SpHb in 62 ICU patients providing 471 samples, the bias was 0.0 ± 1.0 g/dL compared to the reference laboratory haematology analyser. However the bias and standard deviation of capillary measurement by HemoCue was 0.3 ± 1.3 g/dL when compared to the reference haematology analyser, significantly higher than SpHb. In general continuous SpHb monitoring accuracy has been found to be comparable to invasive point of care capillary measurement, with some studies showing it to be slightly higher and some studies showing it to be slightly lower when used in the operating room and intensive care unit. There have also been a few studies published in Emergency Room patients. Sjostrand et al. investigated the accuracy of SpHb using repetitive controls of venous blood samples from 30 patients in a tertiary care emergency room. A total of 242 comparative data pairs were obtained, resulting in a mean deviation of −0.47 g/dL (CI −0.39 to −0.09) for SpHb. After exclusion of 5 patients due to low signal quality, the deviation decreased to −0.24 g/dL (CI −0.39 to −0.09). Although the vast majority of published evaluations of SpHb with Pulse Co-oximetry have been accuracy studies, the true clinical benefit of the technology may be as a trend monitor to detect unexpected changes in haemoglobin, such as with occult bleeding, or to confirm expected changes in haemoglobin as they occur during and after transfusion of red blood cells . The rapid and noninvasive measurement of haemoglobin and the availability of continuous haemoglobin data have the potential to be enormously useful in clinical practice in a variety of situations, such as in trauma, gastrointestinal bleeding, in the perioperative setting, or for guiding blood management during invasive interventions. Because the technology is not intended to replace laboratory measurements, it is less important to receive a measurement that exactly mirrors a laboratory value, rather than to provide continuous information regarding the changes or stability of haemoglobin. For the spot check applications, the immediacy of data and noninvasive nature of the device make it ideal for prehospital triage decisions such as choosing the right hospital. At the hospital, this technology has the potential to assist emergency department staff in making triage priorities and in assigning staff and infrastructure. The ease of use of these devices allows for the universal screening of all presenting patients for anaemia which could indicate occult bleeding or other disease processes requiring intervention. More data from prospective studies is needed to confirm the reliability of this method to guide therapy during surgery or on-going bleeding. Additionally, prospective randomised trials would be desirable to investigate the potential of SpHb monitoring to reduce blood transfusions during surgery or in the intensive care unit. In conclusion, SpHb by Pulse CO-Oximeter is a promising new medical technology that has the potential to improve the process of care and patient outcomes in many different healthcare settings.
__
New Study presented at the 2015 Euroanaesthesia Congress evaluated the impact on Mortality and Morbidity with Masimo SpHb and PVI:
The study evaluated Masimo’s parameters of noninvasive, continuous haemoglobin, SpHb, and fluid responsiveness, PVI, with patients in hospital settings. Dr. Sebastien Ponsonnard and researchers at CHU Limoges, Department of Anaesthesiology & Intensive Care, in Limoges, France, evaluated the impact on mortality and morbidity in patients who underwent general anaesthesia at the hospital after the introduction of Masimo SpHb continuous haemoglobin measurement and response to fluid loading by PVI. Operating rooms and ICUs were equipped with Masimo Radical-7 Pulse CO-Oximeter® monitors. Over a six-month period (Feb. 6-Aug. 7, 2014), patients receiving general anaesthesia were monitored noninvasively. At one month, mortality decreased in 2014 (vs. 84/5123 = 1.64% vs. 121/5478 = 2.2%, P = 0.024). In-hospital mortality was not different between the two years. Death in cardiothoracic surgery was slightly lower (P = 0.07). Researchers concluded: “These results suggest that by using a non-invasive monitor, measuring SpHb and fluid loading responsiveness is possible on a large scale. The observed reduction of mortality agrees with multi-centric randomized studies using more invasive monitoring systems and supports the large use of such a device.”
__________
__________
New method developed for measuring oxygen saturation in capillary blood:
Like the pulse oximeter—the standard oxygen monitor used in the ICU and surgery— the new device determines oxygen levels by noninvasively reading the blood’s color. But unlike the pulse oximeter, this new monitor can zero in on the amount of oxygen reaching specific tissues. An added benefit is that it works even if the patient has no pulse. Brock-Utne, Benaron, Pieter van der Starre, MD, and 16 others produced a study in animals and humans and showed that the device reliably monitors oxygen levels, even in situations in which pulse oximetry fails. The study appeared in the June 2004 Anesthesiology. Among pulse oximetry’s blind spots is one that occurs during bypass surgery. Because the pulse oximeter relies on the pulsing of a patient’s blood vessels to assess the oxygen level, it’s of little use during such an operation, as this pulse ceases. Many studies from different institutions have shown that between 5 and 10 percent of cardiac bypass patients experience subtle declines in intellectual ability due to diminished oxygen supply to the brain. This new monitor uses shorter light waves, primarily blue and green, to measure the blood’s color. The use of shorter light waves allows the device to monitor only the smallest blood vessels, called capillaries, where oxygen is delivered to the tissues. In contrast, the pulse oximeter’s longer light waves offer information about arteries, which are the larger vessels that merely move the blood to the capillaries. The vascular surgeons believe the device could alert surgeons to a rare but deadly complication of a surgery to repair an aneurysm in the abdominal section of the aorta. In about 3 percent of those undergoing the procedure the colon becomes starved of oxygen. The problem is, there’s no way to detect the problem until days later, and 57 percent die before leaving the hospital. This device will reveal ischemia of the colon while the patient is still in the operating room, giving surgeons a chance to restore flow before damage occurs. The inventor, former Stanford associate professor David Benaron, MD, suggests that the device also shows promise for uses outside of surgery and critical care. Among these: tumor detection and drug development.
______
Researchers develop Wearable, Disposable Device for Pulse Oximetry:
_
_
Pulse oximetry is considered to be a noninvasive, painless, general indicator of oxygen delivery to the peripheral tissues (such as the finger, earlobe, or nose). For decades, pulse oximetry has been ubiquitous in the hospital. Now, because of recent advance, this field is poised for a paradigm shift away from simple monitoring devices to advanced products capable of connecting patients to electronic systems that continuously gather data and notify caregivers when values become critical. A group of bioengineering doctoral students at the University of California Berkeley (UC Berkeley) have invented an inexpensive Band-Aid-style oximeter that uses red and green light to non-invasively monitor pulse rate and oxygen level in blood. While this device could revolutionize pulse oximetry monitoring in healthcare settings, the technology might also be applied to measuring other useful biomarkers as one approach to eliminate invasive specimen collection. Conventional pulse oximeters use light-emitting diodes (LEDs) to send red and infrared light through the fingertip or earlobe to detect oxygen saturation. The student scientists explained that the device uses green (532 nm) and red (626 nm) organic light-emitting diodes (OLEDs) with an organic photodiode (OPD)—a semiconductor device that converts light into current—sensitive at specific OLED wavelengths. The sensor’s active layers are deposited from solution-processed materials via spin-coating and printing techniques. Using a solution-based processing system, the researchers deposited the green and red organic LEDs and the translucent light detectors onto a flexible piece of plastic. By detecting the pattern of fresh arterial blood flow the device can calculate a pulse. The organic oximeter sensor is interfaced with conventional electronics at 1 kHz. To determine accuracy, the device’s acquired pulse rate and oxygenation level were calibrated and compared with a commercially available oximeter. In a study comparing this prototype to conventional oximeters, the device measured pulse rate and oxygenation with errors of 1% and 2%, respectively, noted a December 10, 2014, Nature Communications paper.
_______
iPhone app work as pulse oximeter:
It is the only app that measures both the heart rate and blood oxygen saturation without an external device. It is integrated with Apple’s HealthKit. NOT FOR CLINICAL USE. Pulse Oximeter uses your iPhone’s camera to detect your pulse and oxygen levels from your fingertip. Whether you are training, doing simple exercise, or just monitoring stress levels, download the App today and use your camera’s flash to monitor your progress! Place the tip of your index finger on the iPhone’s camera, and in a couple of seconds your pulse and oxygen levels will be shown. Results are also recorded in a graph, just tilt iPhone to view Data Chart.
_
Samsung’s Galaxy S5 also has app work as pulse oximeter:
Samsung has updated their S Health app in the Galaxy Apps Store, adding some new features, while removing others for users in some countries. New features include weight management, sleeping time, and oxygen saturation measurement. Oxygen saturation, also known as SpO₂, uses the sensor on the back of your Samsung device. Just place your finger on the sensor and measurement will start automatically.
_
Wireless Pulse Oximeter shares data with Mobile Devices:
An innovative wireless fingertip pulse oximeter enables clinicians to track and trend measurements through smart mobile devices. The Bluetooth-enabled device allow clinicians to track and trend up to 12 hours of patient measurements on smart mobile devices, and to share that data via standard comma-separated-value (CSV) files, as well as transfer the data to the Apple Health app. Other pulse oximetry software applications allow you to display your pulse oximeter data in a histogram format and also send your pulse oximeter session data to an email address for storage on your personal computer, phone or tablet.
_
Wristwatch-style oximeter lets patients’ measure blood oxygen levels remotely:
A new wristwatch-style oximeter will allow COPD patients – and everyone else – to continue with their normal round of daily activities, without having to “take a break” in order to have their blood oxygen levels measured. This oximeter is a device that measures blood oxygen saturation levels – that patients can wear, with information about their current condition monitored by their Bluetooth-connected smartphones. If a critical blood oxygen threshold that can endanger a patient’s health is recorded, the app that communicates with the device can inform the caregiver of the situation, and appropriate action can be taken.
_
MoveSense app makes cell-phone an oxygen saturation monitor without using pulse oximetry:
The ability to accurately measure oxygen saturation without the use of a pulse oximeter is something that has never been achieved, until now. Researchers developed a smartphone app, MoveSense, which monitors cardiopulmonary patients by analyzing the way they walk, then predicts their oxygen saturation level — without the use of a pulse oximeter. Patients wore pulse oximeters (so readings could be compared to MoveSense data) and carried smartphones running MoveSense software, which continuously recorded saturation and motion. Continuous saturation defined categories corresponding to status levels, including transitions. This, by itself, was a new medical observation. Continuous motion was used to compute eight gait parameters from the sensor data. Their existing gait model was then trained with these data points and used to predict transitions in oxygen saturation. The researchers discovered oxygen saturation readings clustered patients into three pulmonary function categories: one with consistently high saturation, one with consistently low saturation, and a third where saturation varied and patients were clinically unstable. In addition, they discovered that analysis of the saturation, combined with the gait data, could predict saturation category with 100 percent accuracy. The model uses a voting scheme to account for patients walking faster and slower, as their hearts and lungs struggle to keep up with demand. The ability to predict the saturation category of the patient internally from motion of the patient externally is remarkable. This new capability will allow medical professionals to monitor patients’ vital signs, predict their clinical stability, and act quickly should their condition decline. Patients need only carry their personal phones during daily living, as testing has shown that periodic samples are sufficient and that even inexpensive smartphones are powerful enough to record these.
__________
__________
The moral of the story:
_
1. Pulse oximetry provides a simple, non-invasive approximation of oxygen saturation of hemoglobin in arterial blood and used in a wide variety of clinical settings either continuously or intermittently. A single one-off reading often isn’t of much use; trends over a period of time give more information. Always measure oxygen saturation before applying oxygen and repeat the measurement after oxygen has been applied.
_
2. Hemoglobin molecule has 4 binding site for oxygen molecule. However, hemoglobin is stable only when bound to 4 molecules of oxygen or when not bound to any oxygen. It is very unstable when bound to 1 to 3 molecules of oxygen. Therefore hemoglobin exists in the RBC in the form of deoxygenated hemoglobin with no oxygen bound, or as oxygenated hemoglobin with 4 molecules of oxygen. When all Hemoglobin molecules are bound with 4 molecules of oxygen, we call oxygen saturation 100 %. When 50 % hemoglobin molecules are bound with 4 molecules of oxygen, we call oxygen saturation 50 %. Oxygen saturation is a measure of how much oxygen the hemoglobin is carrying as a percentage of the maximum it could carry. This oxygen saturation in percentage is measured by pulse oximetry.
_
3. Pulse oximetry uses light to work out oxygen saturation. Two wavelengths of light are used; 660 nanometers (red) and 940 nanometres (near infrared). At 660nm, deoxyhemoglobin absorbs about ten times as much light as oxyhemoglobin. At the infrared wavelength (940nm), oxyhemoglobin absorbs more light than that of deoxyhemoglobin. The pulse oximeter directly senses the absorption of red and infrared light, and estimates arterial hemoglobin oxygen saturation from the ratio of the pulsatile to the non-pulsatile absorption of red light divided by the same ratio for infrared light transilluminating a finger, ear, or other tissue. A microprocessor integrates the data, and through an elaborate calibration algorithm based on human volunteer data, the oxygen saturation can be estimated. It is interesting to note that the ratios of the ‘AC/DC’ ratios at 660 nm and 940 nm are very similar in both reflection and transmission modes. This means that using the same pulse oximeter with either reflection or transmission probes will produce reliable results. Pulse oximeters cannot determine the concentrations of oxyhemoglobin or deoxyhemoglobin; they provide an estimate of arterial oxygen saturation of hemoglobin rather than a direct measurement. The pulsatile component represents only up to two per cent of the total light absorption by pulse oximetry. This explains how interferences such as movement or low perfusion may have a considerable impact on its accuracy. The pulse oximeter uses empirical calibration curves developed from studies of healthy volunteers to calculate SpO2. Since it is unethical to induce a degree of oxygen saturation below 70% in volunteers, pulse oximeter readings of approximately 70% represent the lowest limit of accurate output. So at low saturation states, pulse oximetry accuracy deteriorates and tends to overestimate the laboratory co-oximeter measured SaO2.
_
4. Functional saturation is the ratio of oxygenated haemoglobin to all haemoglobin capable of carrying oxygen; fractional saturation is the ratio of oxygenated haemoglobin to all haemoglobin including those which do not carry oxygen. SpO2 is estimating functional saturation by pulse oximetry while SaO2 is estimating fractional saturation by using arterial blood sample in ABG analyser with co-oximetry. Fractional saturation (SaO2) is approximately 2% lower than functional saturation (SpO2) in a healthy person. ABG analyser without co-oximeter also calculates oxygen saturation ScO2 which is different from SaO2 measured directly by co-oximeter. Calculated ScO2 misses dyshemoglobins while measured SaO2 takes into account dyshemoglobins. So we have three ways of measuring oxygen saturation of hemoglobin; estimation by pulse oximeter (SpO2), calculation by ABG analyser (ScO2) and direct measurement by laboratory co-oximeter (SaO2).
_
5. Pulse oximetry SpO2 has many limitations including inaccuracy below 70% saturation, poor perfusion, movement artifact, improper probe position, body temperature, skin pigmentation, henna, nail varnish, dyshemoglobinemia, ambient light, irregular heartbeats, electromagnetic interference, pulsatile veins, intravenous dyes, uncontrolled diabetes mellitus etc. A calculated ScO2 by ABG analyser may be way off the mark and can be clinically misleading. The most accurate way to measure oxygen saturation is direct measurement of an arterial sample in laboratory co-oximeter (SaO2); the only exception being foetal hemoglobin and jaundice.
_
6. It is important to understand the difference between the partial pressure of arterial oxygen PaO2, the oxygen saturation of arterial blood (SaO2), the oxygen content of arterial blood CaO2 and the oxygen delivery. Oxygen content depends on the hemoglobin level, SaO2, and the amount of dissolved oxygen. If the haemoglobin level is halved, the oxygen content of arterial blood will be halved even if PaO2 and SaO2 are normal. Oxygen delivery is determined by oxygen content and cardiac output. Mixed venous oxygen saturation (SvO2) is used to help us to recognize when a patient’s body is extracting more oxygen than normally. An increase in extraction (lower SvO2) is the body’s way to meet tissue oxygen needs when the oxygen delivery is reduced to tissues.
_
7. Oxygen enters blood from lungs as dissolved oxygen (PaO2) and then binds with hemoglobin (SaO2). After oxygen has entered and dissolved within the blood, then and only then, oxygen can bind to the hemoglobin in the blood. Oxygen leaves blood to be utilized by tissues as dissolved oxygen first and then dissociates from hemoglobin. So dissolved oxygen is available to tissues first and then oxygen bound to hemoglobin. Pulse oximetry cannot measure dissolved oxygen (1.5%) but measure oxygen bound to hemoglobin (98.5%) as oxygen saturation. Supplemental oxygen therapy increases dissolved oxygen resulting in increased oxygen saturation; and even if oxygen saturation is 100% and cannot rise beyond it, oxygen therapy increases oxygen content and delivery by increasing dissolved oxygen in blood although the amount of dissolved oxygen is much lesser than bound oxygen.
_
8. Patients who suffer acute major blood loss and become acutely anaemic should be given 100% oxygen to breathe even if SpO2 is normal. This will increase the amount of dissolved oxygen in the blood and will improve tissue oxygen delivery by a small amount. Of course, blood transfusion may be life-saving. On the other hand, blood transfusion would be far more beneficial than supplemental oxygen in improving a chronically anemic & hypoxemic patient’s low SpO2.
_
9. Hypoxemia is an important and potentially avoidable cause of morbidity and mortality. Rapid and accurate detection of hypoxemia is critical to prevent serious complications and save life; however, oxygenation is difficult to assess on the basis of physical examination alone. Hypoxemia occurs much before clinical signs appear and clinical signs of hypoxemia are neither easily recognizable nor sensitive nor specific. Because desaturation is detected earlier by pulse oximetry than by clinical observation, the use of pulse oximetry is recommended for any patient at risk for hypoxemia. A study found that the rate of hypoxemia detection increased nearly 20 fold in the pulse oximetry group compared to group not using it. Supplemental oxygen raises SpO2 in almost all cases of hypoxemia due to poor oxygenation.
_
10. Pulse oximetry detects hypoxemic hypoxia due to poor oxygenation by measuring oxygen saturation of hemoglobin but cannot detect anemic, circulatory, ischaemic or histotoxic hypoxia. Pulse oximetry does not provide a measure of actual tissue oxygenation.
_
11. Using pulse oximetry as a routine fifth vital sign does result in important changes in the diagnoses and treatments of patients at variety of settings including neonatal & paediatric care, emergency & critical care, pre/intra/post-operative care, out-patients & in-patients care and invasive procedures.
_
12. A 2014 Cochrane review concluded that the value of pulse oximetry is questionable in relation to improved outcomes, effectiveness, and efficiency but most anaesthesia experts around the world would disagree. The accumulated data indicated that pulse oximeters could prevent 2000 to 10,000 anaesthesia deaths each year from undetected hypoxemia. There is no study that shows pulse oximetry saves life because a randomized trial of nearly 2 million patients would be needed to include mortality as an outcome.
_
13. Although the standard manufacturing claim of accuracy for pulse oximeters is ± 2–3% over the range of 70–100% SpO2, a significant proportion of pulse oximeter sensors may be inaccurate. Once in use, there is little evidence that pulse oximeters are ever re-calibrated or have their accuracy assessed.
_
14. Pulse oximeter is reliable if the displayed plethysmographic trace resembles an arterial pressure waveform and the pulse rate displayed equals the actual pulse rate of patient. If the SpO2 level is lower than normal, measure SpO2 in another finger of the patient. You may also cross-check pulse oximeter accuracy by using your own finger rather than the patient finger.
_
15. During motion and low perfusion, pulse oximeters using signal extraction technology (SET) have 97 % sensitivity and 95 % specificity for estimating oxygen saturation as compared to conventional pulse oximetry having 57 % sensitivity and 72 % specificity. Remember; patient movement, low perfusion and improper probe placement are common causes of false alarms in conventional pulse oximeters.
_
16. Studies suggest that pulse oximeter SpO2 overestimates laboratory Co-oximeter measured SaO2 in patients with critical illnesses.
_
17. Although pulse oximetry is not an appropriate method of monitoring patients with bronchial asthma, a post-nebulizer saturation of less than 91 % predicts severe asthma.
_
18. Pulse oximetry is a worthwhile screening tool for emergency triage.
_
19. Pulse oximetry is recommended as a screening method to detect Critical Congenital Heart Disease (CCHD) in new-borns to prevent morbidity and mortality associated with unrecognized CCHD. The new-born pulse oximetry must be done 24 hours after birth when the baby is neither asleep nor crying nor feeding. The screen has a sensitivity of 60% to 75% with conventional pulse oximetry and 93 % with signal extraction technology for critical congenital heart disease.
_
20. To limit oxygen toxicity and prevent hyperoxia in premature neonates, pulse oximetry is used so that supplemental oxygen can be tapered to maintain an oxygen saturation of 90%.
_
21. It is normal for your oxygen saturation to drop slightly during exercise, because your muscles are extracting more oxygen to handle the extra activity although your cardio-respiratory system is compensating for increased oxygen demand. However a significant drop of SpO2 during routine exercise suggests cardio-pulmonary illness.
_
22. Body temperature can cause as much as a 3% difference in the SpO2 measurements. Body temperature affects SpO2 differentially depending upon systemic or local temperature change. In cold weather, body tries to maintain core body temperature by peripheral vasoconstriction reducing peripheral perfusion and thereby giving spurious low SpO2. On the other hand, local hyperthermia (warm digits) gives low SpO2 and local hypothermia (cold digits) give normal SpO2 due to arterial to venous (A-V) shunting in the digits. A-V shunts may be open in warm hands causing “venous pulsations” which result in a lower SpO2 compared to cold hands with no A-V shunting.
_
23. There is significant knowledge deficit about pulse oximetry amongst paramedics, nurses and doctors who are using this technology frequently, resulting in failure to understand limitations of pulse oximetry, thus compromising patient safety.
_
24. Although pulse oximetry usage is increasing worldwide, its penetrance is low in low-income countries where it is most useful.
_
25. Besides detecting hypoxemia in various cardio-respiratory illnesses and at high altitude; pulse oximeter is also useful in controlling oxygen supplementation, monitoring circulation, determining systolic blood pressure, monitoring vascular volume, monitoring desaturation during exercise; and diagnosing peripheral vascular diseases, collateral circulation, distal circulation, sleep apnoea, aspiration, testicular torsion and pulp vitality in dentistry.
_
26. Falsely high SpO2 is more dangerous than falsely low SpO2 because it would give unwarranted complacency and prevent appropriate treatment. Significant hypoxia can be masked in carboxyhemoglobinemia, methmoglobinemia, cyanide poisoning and anemia (total hemoglobin < 10gm/dl) due to high SpO2 reading by conventional pulse oximeter. Additionally, high SpO2 level due to supplemental oxygen can mask hypoventilation and high PaCO2 level.
_
27. Supplemental oxygen must be given despite normal SpO2 (95 to 100%) in the following conditions:
A. Acute major blood loss
B. Ischaemic chest pain
C. Methmoglobinemia and carboxyhemoglobinemia including smoke inhalation and tobacco smoker.
D. Sickle cell crisis
E. Near drowning
F. Cyanide poisoning
G. Multi-system trauma
H. Restlessness
I. Respiratory distress
J. On assisted ventilation due to any cause
K. Apnoea
L. Cardiac arrest, although pulse oximetry should not be done while doing CPR
_
28. A pulse oximeter should never be used during a cardiac arrest situation because of the extreme limitations of blood flow during cardiopulmonary resuscitation and the pharmacological action of vasoactive agents administered during the resuscitation effort. On the other hand, it is quite possible for a dying or dead patient to have a high SpO2 value. This is the case when peripheral oxygen consumption is quite low, resulting in an increased mixed venous saturation. If extraction is very low and the patient is still receiving oxygen therapy, it is easily possible for the patient to have a high SpO2 value.
_
29. Pseudo-hypoxemia means normal SpO2 and low PaO2/SaO2 with ABG and co-oximetry. Pseudo-hypoxemia occurs due to faulty equipment, venous blood sample for ABG/co-oximetry, blood sample from ischaemic limb and excessive oxygen consumption following blood sample collection due to massive leucocytosis (leukemia) or thrombocytosis.
_
30. Non-invasive ‘pulse co-oximeter’ not only estimates signal extraction technology SpO2 but also estimates dyshemoglobins, total hemoglobin level (SpHb), oxygen content, pulse rate, Perfusion Index (PI), and Pleth Variability Index (PVI). The rapid and noninvasive measurement of haemoglobin (SpHb); and the availability of continuous haemoglobin data have the potential to be enormously useful in clinical practice in a variety of situations such as trauma, gastrointestinal bleeding and perioperative setting.
_
31. Oxygenation is how well oxygen is moving across the alveolar-capillary membrane and into the blood to be carried to tissue. Oxygenation is synonymous with oxygen saturation of hemoglobin. Ventilation, which can be spontaneous (as in breathing) or artificial (as in mechanical ventilation) is the movement of air in and out lungs. Pulse oximetry estimates oxygenation of arterial hemoglobin which is dependent on both alveolar ventilation and pulmonary perfusion. Capnography estimates carbon dioxide removal which is predominantly dependent on alveolar ventilation. During alveolar hypoventilation, as arterial carbon dioxide tension rises so does alveolar carbon dioxide tension (PCO2) because CO2 diffuses rapidly across alveolar capillary membrane; concurrently alveolar PO2 falls, leading to fall in arterial oxygen saturation. If the patient is breathing room air then the saturation will fall early and is a reasonably sensitive indicator of hypoventilation. The situation is different if the patient is receiving supplemental oxygen. The alveolar PO2 will now be much higher and consequently higher PaO2 will raise SpO2.The failure to detect hypoventilation in such a patient is not a failure of pulse oximetry as such but an example of a false sense of security generated by a single physiological variable being within safe limits. It must be understood that a normal reading of SpO2 in the presence of supplemental oxygen gives no information about CO2 removal i.e. the adequacy of ventilation. Oxygenation can be erroneously interpreted as ventilation if EtCO2 by capnography is not monitored. A recent study found that only 35% of nurses and 39% of physicians in a major medical center knew that pulse oximetry monitored oxygen saturation only and did not reflect changes in ventilation. All patients who are prone to hypoventilation and/or respiratory depression due to any cause must undergo capnography (EtCO2) along with pulse oximetry (SpO2) to determine both carbon dioxide removal (ventilation) and oxygen saturation (oxygenation).
_
32. Hypoventilation can be detected early with pulse oximetry by lower SpO2 if patient is breathing in ambient air. By contrast, poor oxygenation cannot be detected early with capnography by higher EtCO2. Only hypoventilation causes hypoxemia with hypercapnia. All other causes of hypoxemia have no hypercapnia. Capnography is useful essentially in hypoventilation but of no use in all other causes of hypoxemia. Additionally, the cost and maintenance of oximetry are generally lower than capnography. For these reasons, pulse oximetry is the preferred monitoring modality in resource-limited settings.
_
33. Integrated Pulmonary Index (IPI) is a patient pulmonary index which uses information from capnography and pulse oximetry to provide a single value that describes the patient’s respiratory status. The IPI incorporates four patient parameters (end-tidal CO2 and respiratory rate measured by capnography, as well as pulse rate and blood oxygenation SpO2 as measured by pulse oximetry) into a single index value. IPI score correlate very well with ventilator status of a patient. IPI can increase patient safety, by indicating the presence of slow-developing patient respiratory issues not easily identified with individual instantaneous data available to the caregiver in real time. This enables timely decisions and interventions to reduce patient risk, improve outcomes and increase patient safety.
_
34. A critical patient needs repeated arterial punctures for ABG monitoring; today it can be replaced by continuous non-invasive capnography, continuous non-invasive pulse oximetry (preferably pulse co-oximetry) and simple venous blood collection for bicarbonate, electrolytes, hemoglobin and pH. Studies have shown that bicarbonate and pH differ very little between arterial and venous blood.
________
________
Dr. Rajiv Desai. MD.
August 24, 2015
________
Postscript:
This article is written not for lay people to do pulse oximetry at home but for medical students, paramedics, nurses and doctors as there is a significant knowledge deficit about pulse oximetry amongst them.
_____


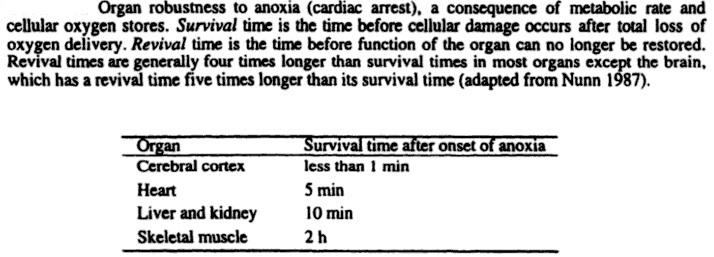
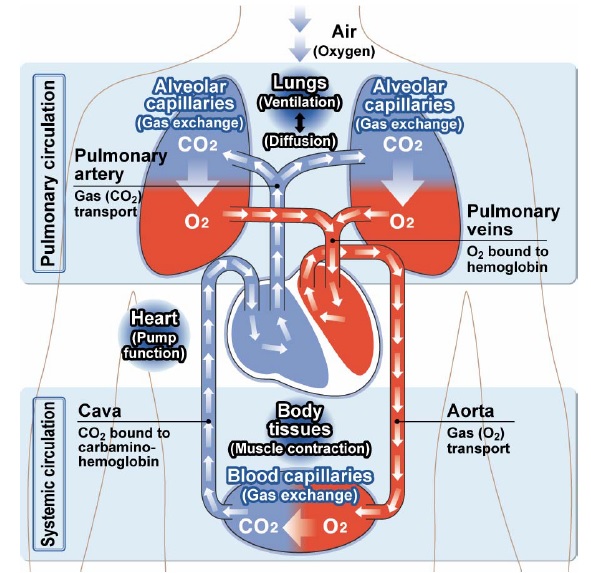
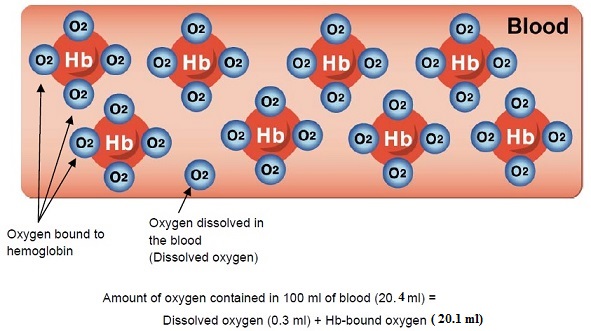
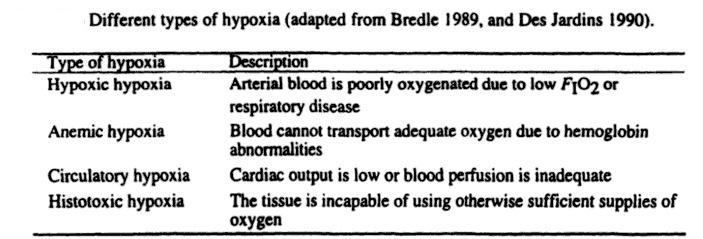
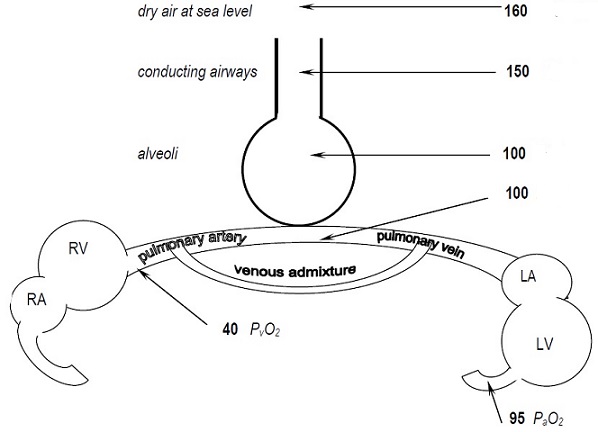
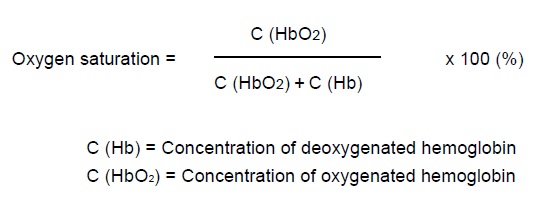
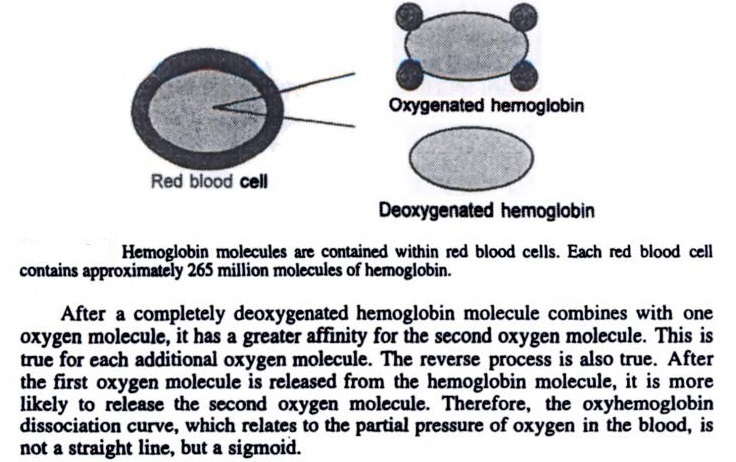
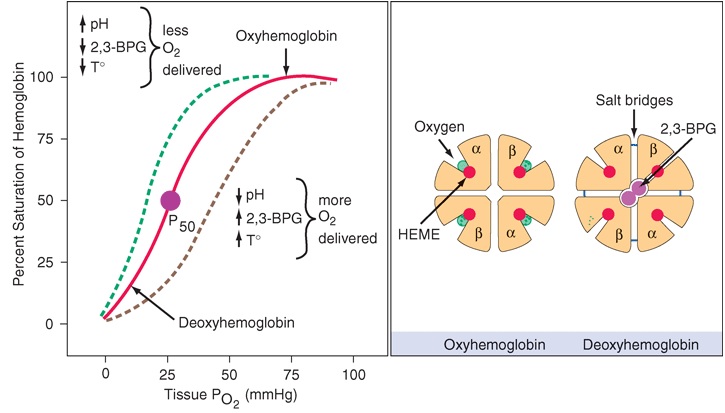
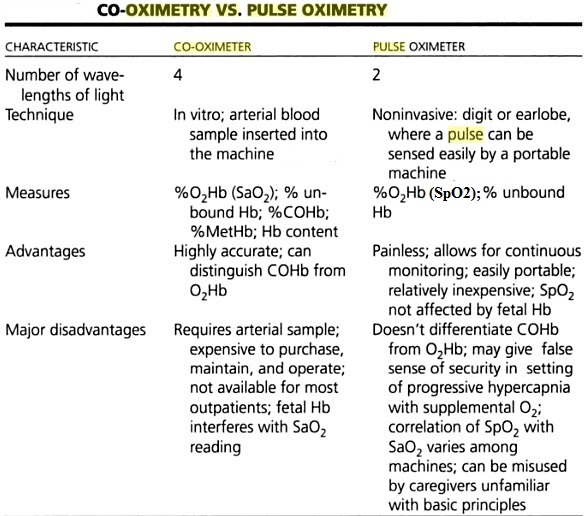
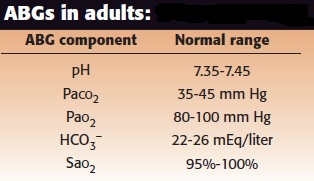
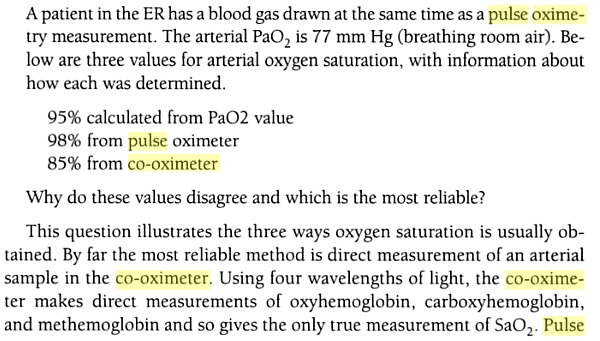
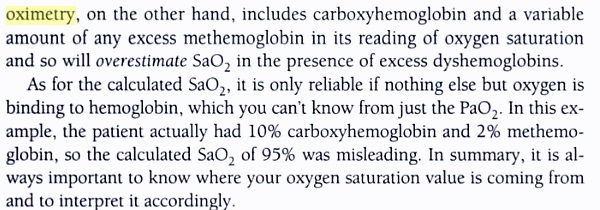
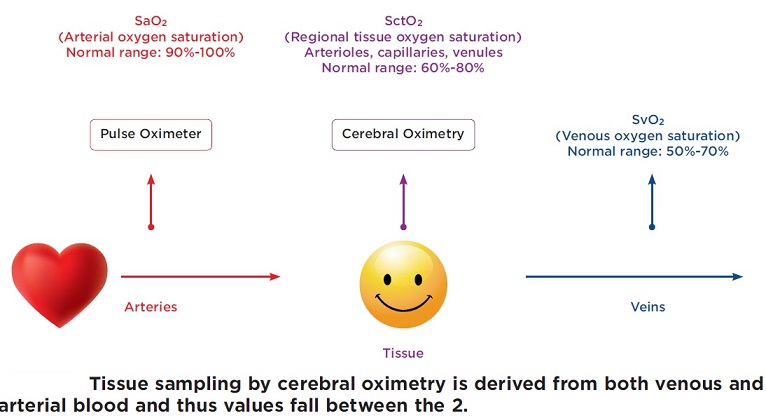
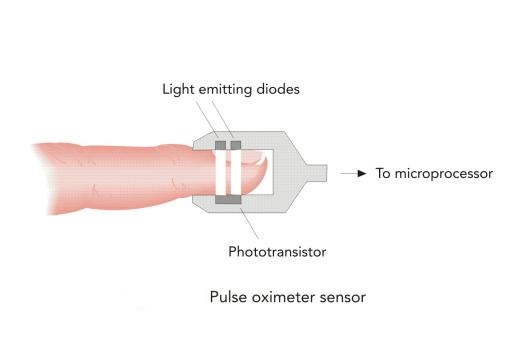
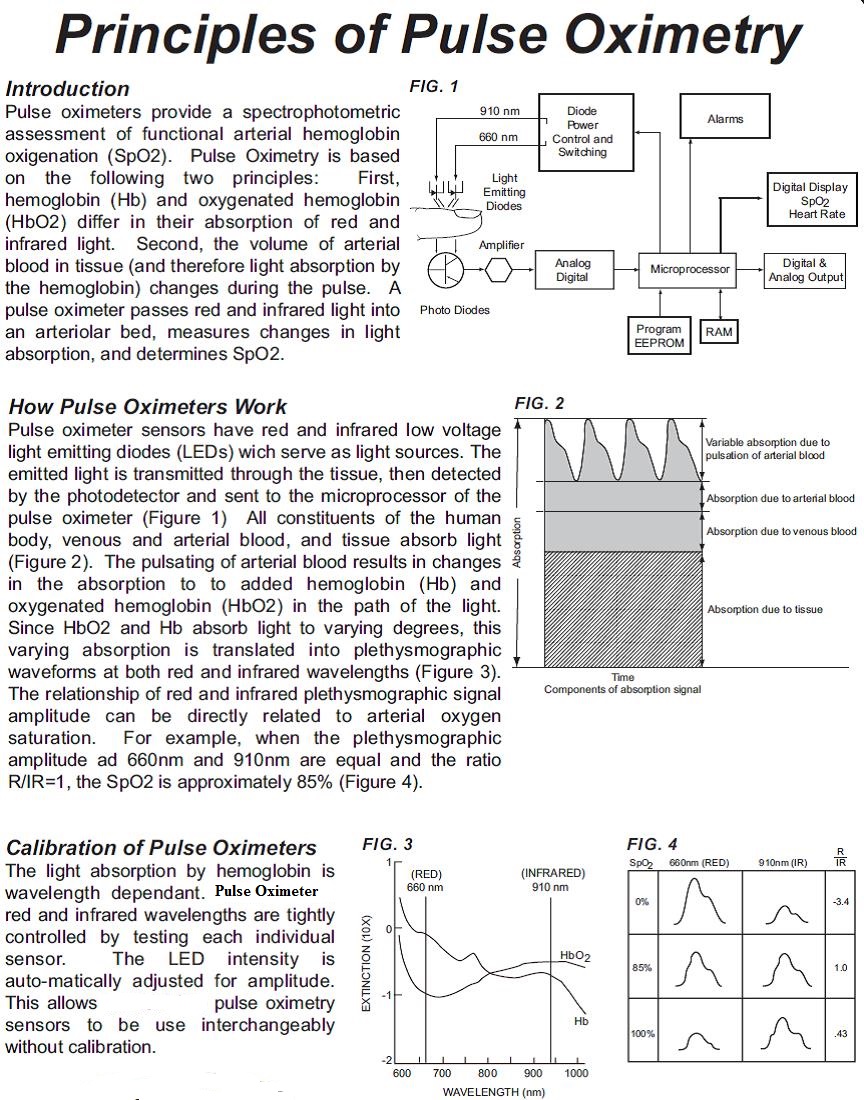
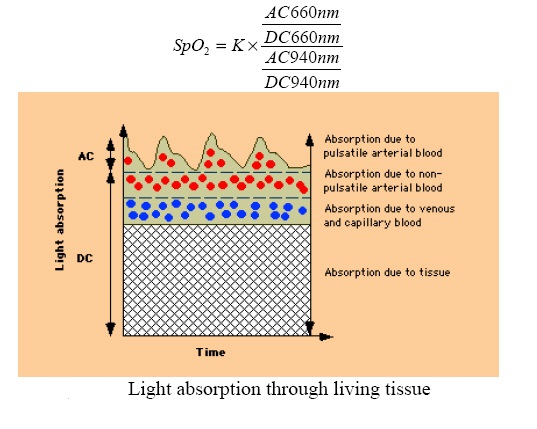
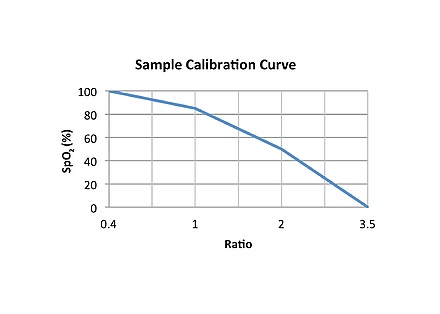
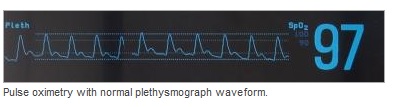
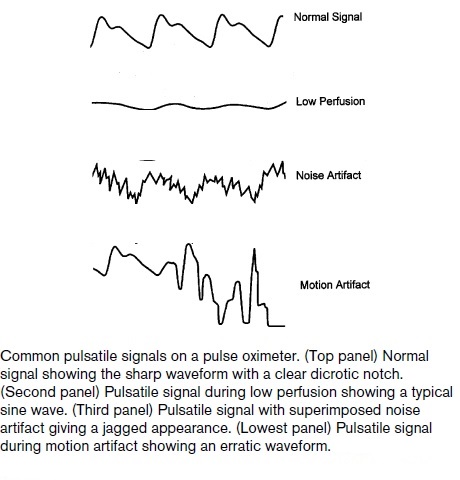
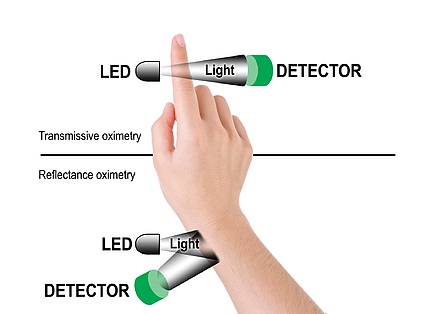
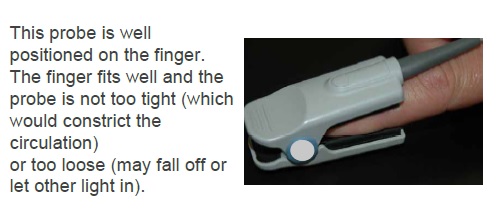
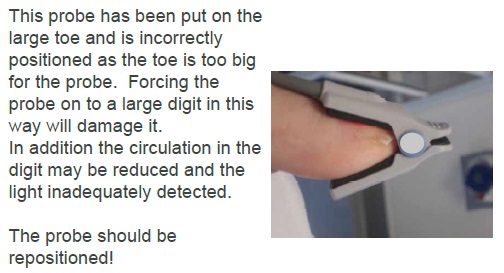
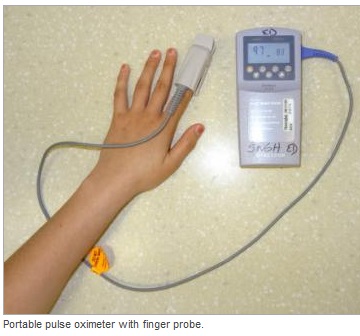
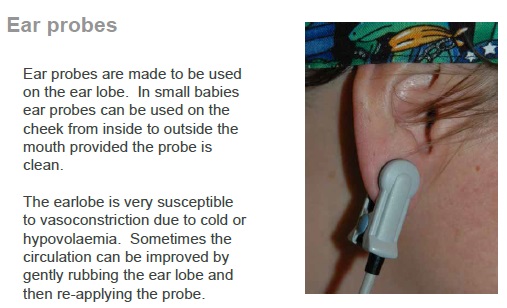


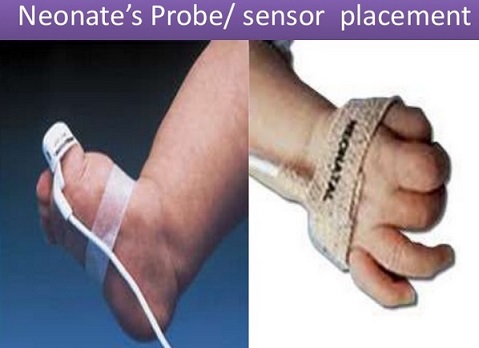
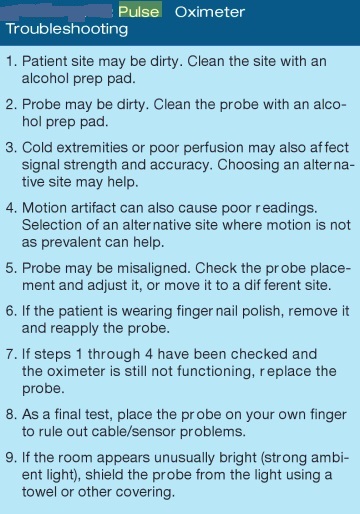
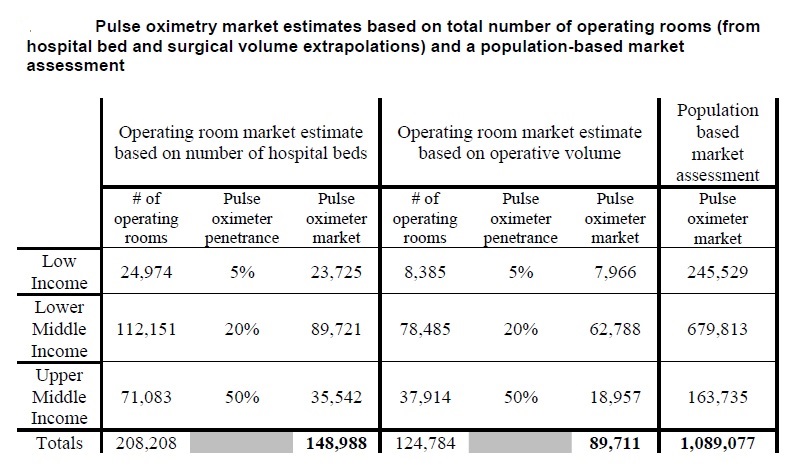
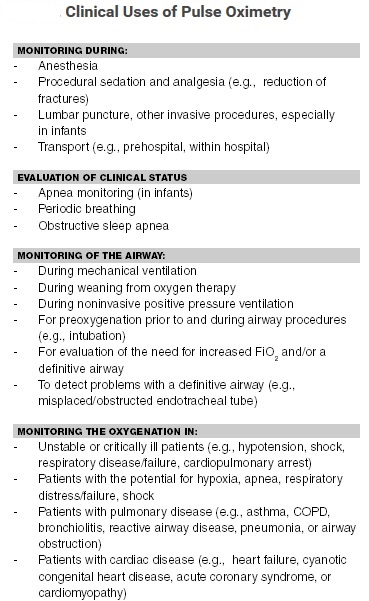
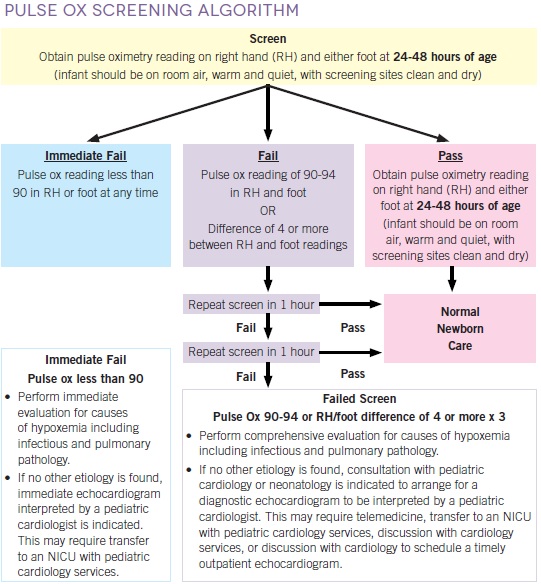
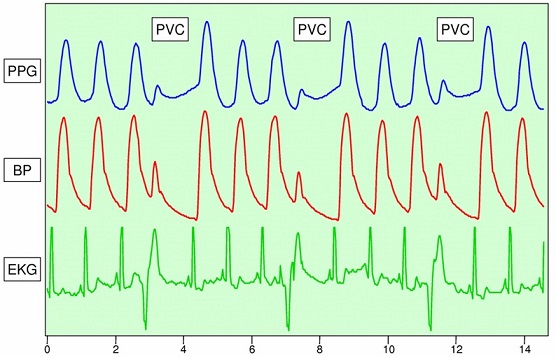
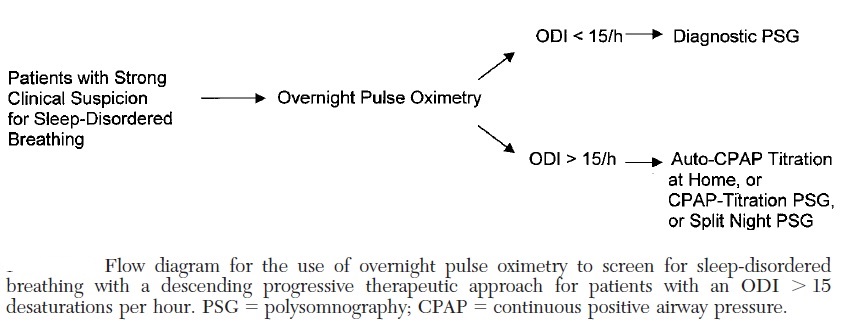
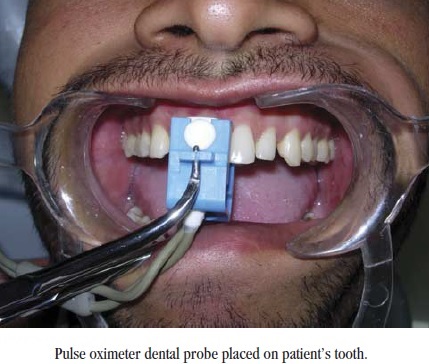
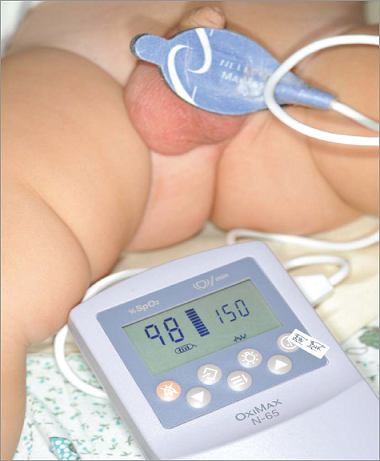
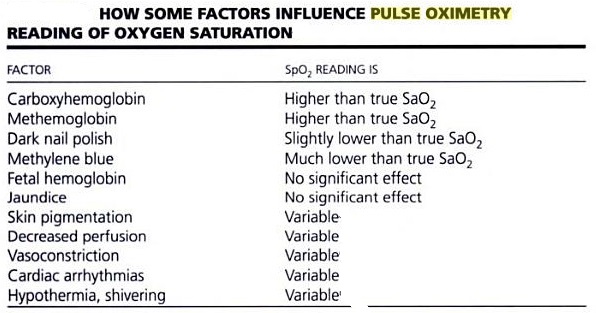
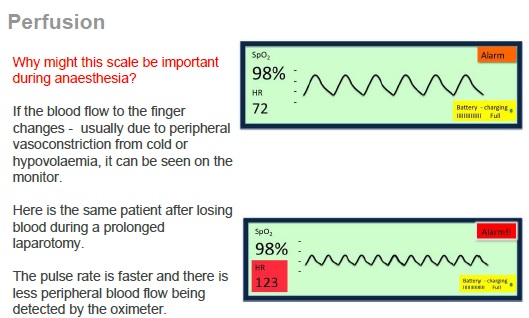
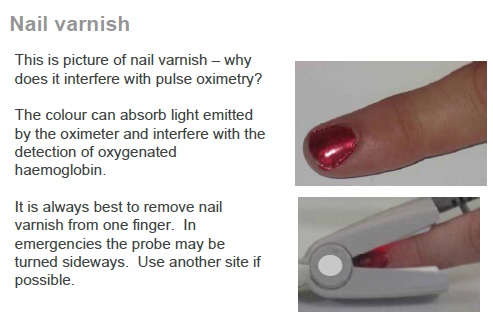
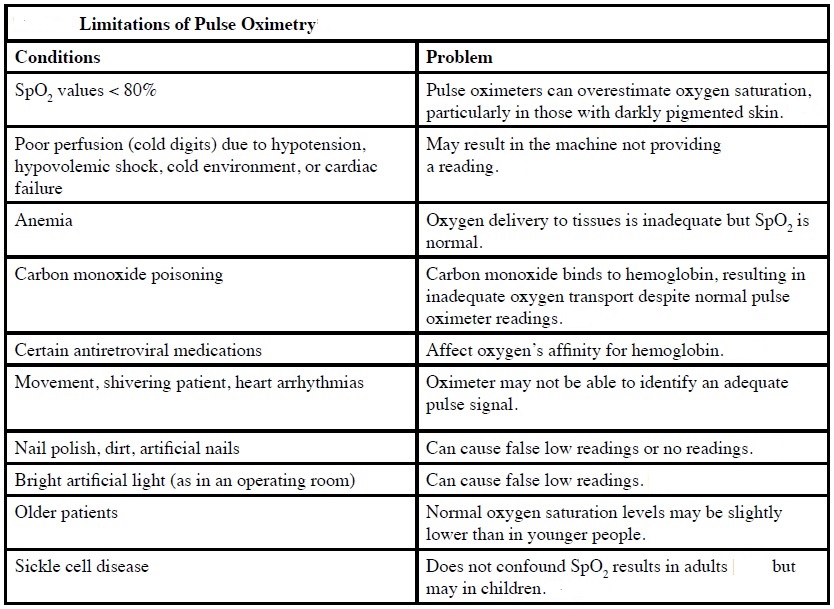
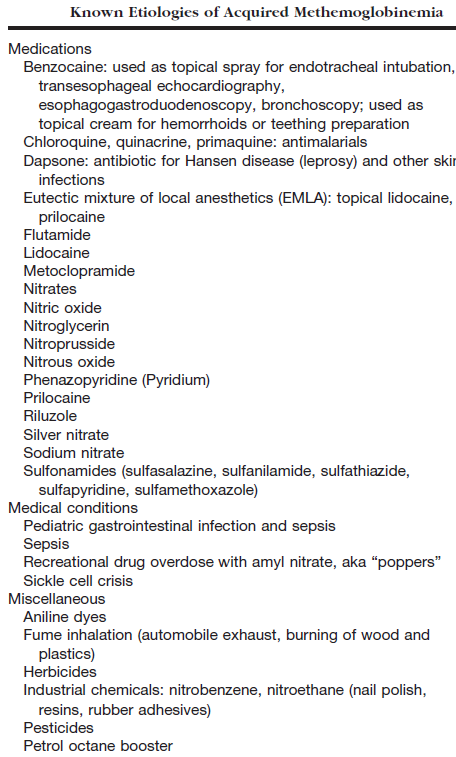
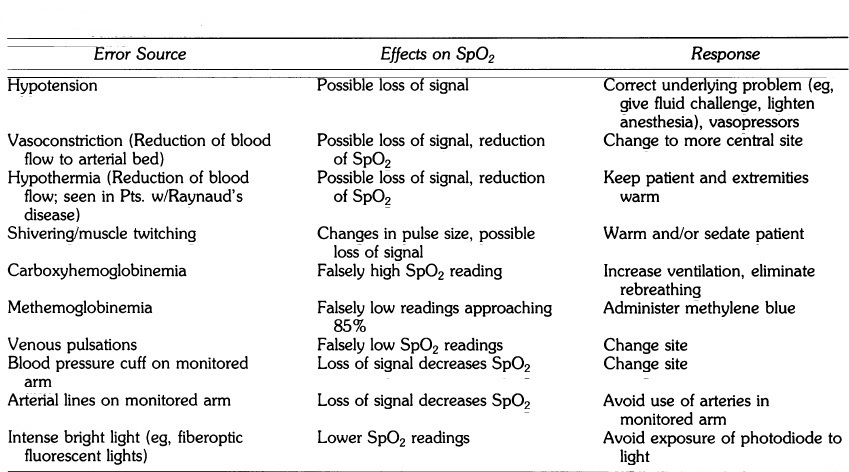
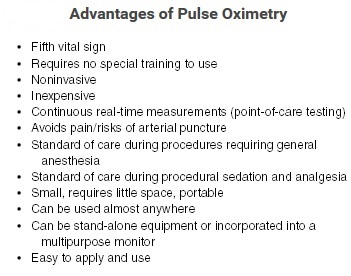
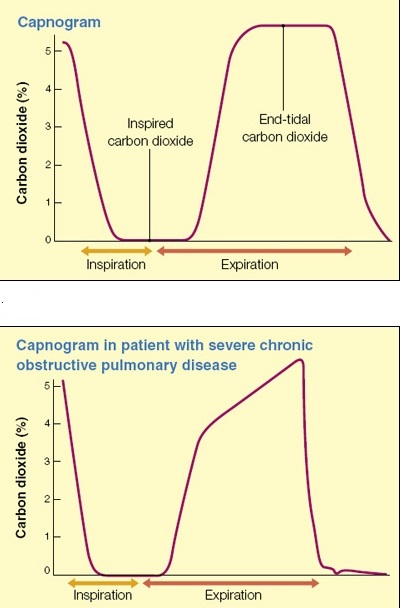
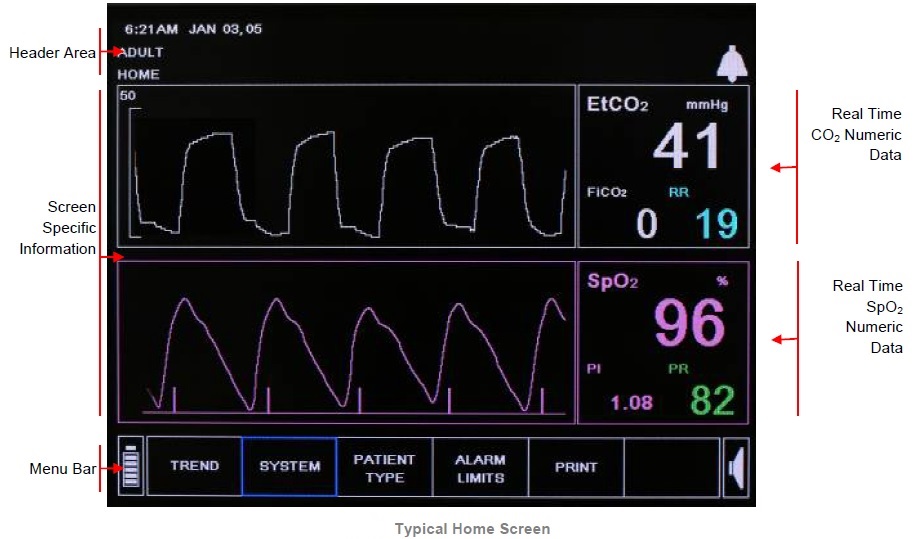
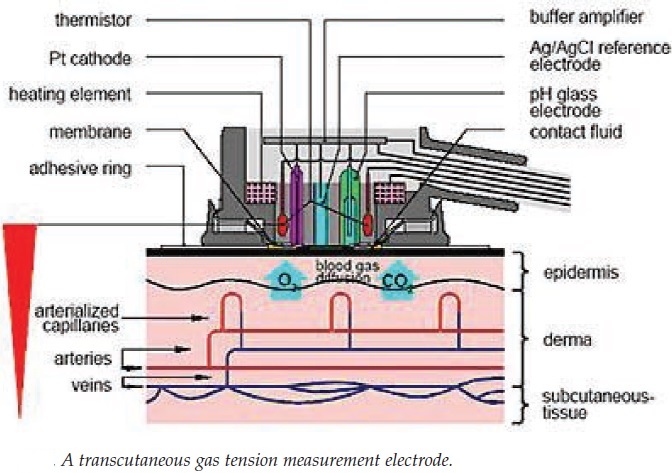
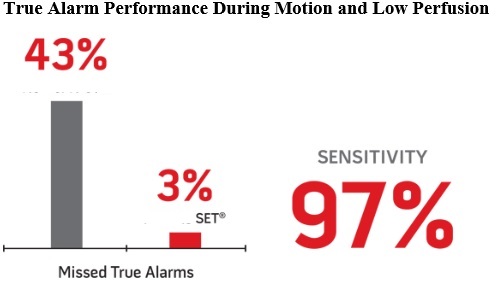
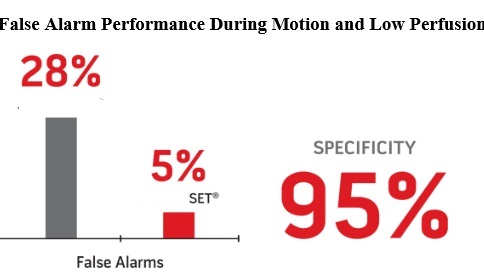


Thanks for another informative website. Where else could I get that type of info written in such an ideal way? I have a project that I’m just now working on, and I’ve been on the look out for such information.
Your determination is inspiring! You always have something favorable to claim.
Remarkable is the excellent efficiency tool that can help you obtain even more carried out in less time!
You have a terrific feeling of style and style! You are so comprehending as well as kind-hearted.
You provided readers with an comprehensive analysis of the subject that left no stone unturned.
Tremendous issues here. I’m very satisfied tosee your article. Thank you so much and I am having a look ahead to touch you.Will you please drop me a e-mail?
I am so grateful for your article.Really thank you! Fantastic.
wow, awesome blog post.Much thanks again. Will read on…
Nice post. I learn something new and challenging on sites I stumbleupon everyday. It’s always helpful to read through articles from other writers and use something from their sites.
נערות ליווי בתל אביב
I am so grateful for your article.Much thanks again. Really Cool.
whoah this blog is magnificent i really like reading your articles. Stay up the good paintings! You know, lots of persons are hunting round for this information, you could aid them greatly.
Awesome blog.Really thank you! Great.
Your common sense should be taken as the rule when it comes to this topic.
It’s not boring when you discuss it.. out every blog on this, yours stands out.
Very informative, educational and useful – thank you very much indeed
Hi there, You’ve done an excellent job. I’ll certainly digg it and personally recommend to my friends. I’m sure they will be benefited from this web site.|
Im thankful for the blog article.Thanks Again. Want more.
Its like you read my mind! You appear to know so much about this, like you wrote the book in it or something. I think that you could do with a few pics to drive the message home a little bit, but other than that, this is fantastic blog. An excellent read. I’ll definitely be back.|
This is one awesome article.Really looking forward to read more. Keep writing.
Im obliged for the article post.Really looking forward to read more. Much obliged.
I am so grateful for your article post.Much thanks again. Awesome.
Fine way of explaining, and pleasant post to take information concerning my presentation subject matter, which i am going to convey in college.|
Very good information. Lucky me I recently found your site by accident (stumbleupon). I’ve bookmarked it for later!|
I just want to mention I am just newbie to weblog and certainly loved this web-site. Probably I’m planning to bookmark your blog . You surely have awesome stories. Appreciate it for sharing your web page.
Greate pieces. Keep posting such kind of information on your page. Im really impressed by it.
Very neat blog article.Much thanks again.
Awesome post. Cool.
It’ѕ actually a nice and usеful pіece оf information. I’m happy that you shɑred this һelpful info with us.
Please stаy us informed lіke this. Thank you for sharing.
A round of applause for your blog.Really thank you! Great.
I cannot thank you enough for the article post.Much thanks again. Awesome.