Dr Rajiv Desai
An Educational Blog
GENE THERAPY
_______
GENE THERAPY:
______
______
Caveat:
Medicine is an ever-changing science. As new research and clinical experience broaden our knowledge, changes in treatment and drug therapy are required. I have checked with sources believed to be reliable in their efforts to provide information that is complete and generally in accord with the standards accepted at the time of publishing this article. However, in view of the possibility of human error or changes in medical sciences, I do not assure that the information contained herein is in every respect accurate or complete, and I disclaim all responsibility for any errors or omissions or for the results obtained from use of the information contained in this work. Readers are encouraged to confirm the information contained herein with other sources. I have taken some information from articles that were published few years ago. The facts and conclusions presented may have since changed and may no longer be accurate. Questions about personal health should always be referred to a physician or other health care professional.
______
Prologue:
“BLASPHEMY!” some cried when the concept of gene therapy first surfaced. For them tinkering with the genetic constitution of human beings was equivalent to playing God, and this they perceived as being sacrilegious! On the other side was the scientific community, abuzz with excitement at the prospect of being able to wipe certain genetic disorders in humans entirely from the human gene pool. Although the term gene therapy was first introduced during the 1980s, the controversy about the rationality of this line of treatment still rages on. In the center of the debate lie the gene therapy pros and cons that derive opinions from religious, ethical and undoubtedly, political domains. The concept of genes as carriers of phenotypic information was introduced in the early 19th century by Gregor Mendel, who later demonstrated the properties of genetic inheritance in peas. Over the next 100 years, many significant discoveries lead to the conclusions that genes encode proteins and reside on chromosomes, which are composed of DNA. These findings culminated in the central dogma of molecular biology, that proteins are translated from RNA, which is transcribed from DNA. James Watson was quoted as saying “we used to think that our fate was in our stars, but now we know, in large measures, our fate is in our genes”. Genes, the functional unit of heredity, are specific sequences bases that encode instructions to make proteins. Although genes get a lot of attentions, it is the proteins that perform most life functions. When genes are altered, encoded proteins are unable to carry out their normal functions, resulting in genetic disorders. Gene therapy is a novel therapeutic branch of modern medicine. Its emergence is a direct consequence of the revolution heralded by the introduction of recombinant DNA methodology in the 1970s. Gene therapy is still highly experimental, but has the potential to become an important treatment regimen. In principle, it allows the transfer of genetic information into patient tissues and organs. Consequently, diseased genes can be eliminated or their normal functions rescued. Furthermore, the procedure allows the addition of new functions to cells, such as the production of immune system mediator proteins that help to combat cancer and other diseases. Most scientists believe the potential for gene therapy is the most exciting application of DNA science, yet undertaken.
__________
Note:
Please read my other articles ‘Stem cell therapy and human cloning’, ‘Cell death’ and ‘Genetically modified’ before reading this article.
__________
The rapid pace of technological advances has profound implications for medical applications far beyond their traditional roles to prevent, treat, and cure disease. Cloning, genetic engineering, gene therapy, human-computer interfaces, nanotechnology, and designer drugs have the potential to modify inherited predispositions to disease, select desired characteristics in embryos, augment “normal” human performance, replace failing tissues, and substantially prolong life span. As gene therapy is uprising in the field of medicine, scientists believe that after 20 years, this will be the last cure of every genetic disease. Genes may ultimately be used as medicine and given as simple intravenous injection of gene transfer vehicle that will seek our target cells for stable, site-specific chromosomal integration and subsequent gene expression. And now that a draft of the human genome map is complete, research is focusing on the function of each gene and the role of the faulty gene play in disease. Gene therapy will ultimately play Copernican part and will change our lives forever.
_
Gene therapy, the experimental therapy as on today:
Gene therapy is an experimental technique that uses genes to treat or prevent diseases. Genes are specific sequences of bases that encode instructions on how to make proteins. When genes are altered so that the encoded proteins are unable to carry out their normal functions, genetic disorders can result. Gene therapy is used for correcting defective genes responsible for disease development. Researchers may use one of several approaches for correcting faulty genes. Although gene therapy is a promising treatment which helps successfully treat and prevent various diseases including inherited disorders, some types of cancer, and certain viral infections, it is still at experimental stage. Gene therapy is presently only being tested for the treatment of diseases that have no other cures. Currently, the only way for you to receive gene therapy is to participate in a clinical trial. Clinical trials are research studies that help doctors determine whether a gene therapy approach is safe for people. They also help doctors understand the effects of gene therapy on the body. Your specific procedure will depend on the disease you have and the type of gene therapy being used.
______
Introduction to gene therapy:
Gene therapy is a clinical strategy involving gene transfer with therapeutic purposes. It is based on the concept that an exogenous gene (transgene) is able to modify the biology and phenotype of target cells, tissues and organs. Initially designed to definitely correct monogenic disorders, such as cystic fibrosis, severe combined immunodeficiency or muscular dystrophy, gene therapy has evolved into a promising therapeutic modality for a diverse array of diseases. Targets are expanding and currently include not only genetic, but also many acquired diseases, such as cancer, tissue degeneration or infectious diseases. Depending on the duration planned for the treatment, type and location of target cells, and whether they undergo division or are quiescent, different vectors may be used, involving nonviral methods, non-integrating viral vectors or integrating viral vectors. The first gene therapy clinical trial was carried out in 1989, in patients with advanced melanoma, using tumor-infiltrating lymphocytes modified by retroviral transduction. In the early nineties, a clinical trial with children with severe combined immunodeficiency (SCID) was also performed, by retrovirus transfer of adenosine deaminase gene to lymphocytes isolated from these patients. Since then, more than 5,000 patients have been treated in more than 1,000 clinical protocols all over the world. Despite the initial enthusiasm, however, the efficacy of gene therapy in clinical trials has not been as high as expected; a situation further complicated by ethical and safety concerns. Further studies are being developed to solve these limitations.
_________
Historical development of gene therapy:
Chronology of development of gene therapy technology:
1970s, 1980s and earlier:
In 1972 Friedmann and Roblin authored a paper in Science titled “Gene therapy for human genetic disease?” Rogers (1970) was cited for proposing that exogenous good DNA be used to replace the defective DNA in those who suffer from genetic defects. However, these authors concluded that it was premature to begin gene therapy studies in humans because of lack of basic knowledge of genetic regulation and of genetic diseases, and for ethical reasons. They did, however, propose that studies in cell cultures and in animal models aimed at development of gene therapies be undertaken. Such studies–as well as abortive gene therapy studies in humans–had already begun as of 1972. In the 1970s and 1980s, researchers applied such technologies as recombinant DNA and development of viral vectors for transfer of genes to cells and animals to the study and development of gene therapies.
1990s:
The first approved gene therapy case in the United States took place on 14 September 1990, at the National Institute of Health, under the direction of Professor William French Anderson. It was performed on a four year old girl named Ashanti DeSilva. It was a treatment for a genetic defect that left her with ADA-SCID, a severe immune system deficiency. The effects were only temporary, but successful. New gene therapy approach repairs errors in messenger RNA derived from defective genes. This technique has the potential to treat the blood disorder thalassaemia, cystic fibrosis, and some cancers. Researchers at Case Western Reserve University and Copernicus Therapeutics are able to create tiny liposomes 25 nanometers across that can carry therapeutic DNA through pores in the nuclear membrane. Sickle-cell disease is successfully treated in mice. The mice – which have essentially the same defect that causes sickle cell disease in humans – through the use a viral vector, were made to express the production of fetal hemoglobin (HbF), which normally ceases to be produced by an individual shortly after birth. In humans, the use of hydroxyurea to stimulate the production of HbF has long been shown to temporarily alleviate the symptoms of sickle cell disease. The researchers demonstrated this method of gene therapy to be a more permanent means to increase the production of the therapeutic HbF. In 1992 Doctor Claudio Bordignon working at the Vita-Salute San Raffaele University, Milan, Italy performed the first procedure of gene therapy using hematopoietic stem cells as vectors to deliver genes intended to correct hereditary diseases. In 2002 this work led to the publication of the first successful gene therapy treatment for adenosine deaminase-deficiency (SCID). The success of a multi-center trial for treating children with SCID (severe combined immune deficiency or “bubble boy” disease) held from 2000 and 2002 was questioned when two of the ten children treated at the trial’s Paris center developed a leukemia-like condition. Clinical trials were halted temporarily in 2002, but resumed after regulatory review of the protocol in the United States, the United Kingdom, France, Italy, and Germany. In 1993 Andrew Gobea was born with severe combined immunodeficiency (SCID). Genetic screening before birth showed that he had SCID. Blood was removed from Andrew’s placenta and umbilical cord immediately after birth, containing stem cells. The allele that codes for ADA was obtained and was inserted into a retrovirus. Retroviruses and stem cells were mixed, after which the viruses entered and inserted the gene into the stem cells’ chromosomes. Stem cells containing the working ADA gene were injected into Andrew’s blood system via a vein. Injections of the ADA enzyme were also given weekly. For four years T cells (white blood cells), produced by stem cells, made ADA enzymes using the ADA gene. After four years more treatment was needed. The 1999 death of Jesse Gelsinger in a gene therapy clinical trial resulted in a significant setback to gene therapy research in the United States. Jesse Gelsinger had ornithine transcarbamylase deficiency. In a clinical trial at the University of Pennsylvania, he was injected with an adenoviral vector carrying a corrected gene to test the safety of use of this procedure. He suffered a massive immune response triggered by the use of the viral vector, and died four days later. As a result, the U.S. FDA suspended several clinical trials pending the re-evaluation of ethical and procedural practices in the field.
2003:
In 2003 a University of California, Los Angeles research team inserted genes into the brain using liposomes coated in a polymer called polyethylene glycol. The transfer of genes into the brain is a significant achievement because viral vectors are too big to get across the blood–brain barrier. This method has potential for treating Parkinson’s disease. RNA interference or gene silencing may be a new way to treat Huntington’s disease. Short pieces of double-stranded RNA (short, interfering RNAs or siRNAs) are used by cells to degrade RNA of a particular sequence. If a siRNA is designed to match the RNA copied from a faulty gene, then the abnormal protein product of that gene will not be produced.
2006:
In March 2006 an international group of scientists announced the successful use of gene therapy to treat two adult patients for X-linked chronic granulomatous disease, a disease which affects myeloid cells and which gives a defective immune system. The study, published in Nature Medicine, is believed to be the first to show that gene therapy can cure diseases of the myeloid system. In May 2006 a team of scientists led by Dr. Luigi Naldini and Dr. Brian Brown from the San Raffaele Telethon Institute for Gene Therapy (HSR-TIGET) in Milan, Italy reported a breakthrough for gene therapy in which they developed a way to prevent the immune system from rejecting a newly delivered gene. Similar to organ transplantation, gene therapy has been plagued by the problem of immune rejection. So far, delivery of the ‘normal’ gene has been difficult because the immune system recognizes the new gene as foreign and rejects the cells carrying it. To overcome this problem, the HSR-TIGET group utilized a newly uncovered network of genes regulated by molecules known as microRNAs. Dr. Naldini’s group reasoned that they could use this natural function of microRNA to selectively turn off the identity of their therapeutic gene in cells of the immune system and prevent the gene from being found and destroyed. The researchers injected mice with the gene containing an immune-cell microRNA target sequence, and the mice did not reject the gene, as previously occurred when vectors without the microRNA target sequence were used. This work will have important implications for the treatment of hemophilia and other genetic diseases by gene therapy. In August 2006, scientists at the National Institutes of Health (Bethesda, Maryland) successfully treated metastatic melanoma in two patients using killer T cells genetically retargeted to attack the cancer cells. This study constitutes one of the first demonstrations that gene therapy can be effective in treating cancer. In November 2006 Preston Nix from the University of Pennsylvania School of Medicine reported on VRX496, a gene-based immunotherapy for the treatment of human immunodeficiency virus (HIV) that uses a lentiviral vector for delivery of an antisense gene against the HIV envelope. In the Phase I trial enrolling five subjects with chronic HIV infection who had failed to respond to at least two antiretroviral regimens, a single intravenous infusion of autologous CD4 T cells genetically modified with VRX496 was safe and well tolerated. All patients had stable or decreased viral load; four of the five patients had stable or increased CD4 T cell counts. In addition, all five patients had stable or increased immune response to HIV antigens and other pathogens. This was the first evaluation of a lentiviral vector administered in U.S. Food and Drug Administration-approved human clinical trials for any disease. Data from an ongoing Phase I/II clinical trial were presented at CROI 2009.
2007:
On 1 May 2007 Moorfields Eye Hospital and University College London’s Institute of Ophthalmology announced the world’s first gene therapy trial for inherited retinal disease. The first operation was carried out on a 23 year-old British male, Robert Johnson, in early 2007. Leber’s congenital amaurosis is an inherited blinding disease caused by mutations in the RPE65 gene. The results of a small clinical trial in children were published in New England Journal of Medicine in April 2008. They researched the safety of the subretinal delivery of recombinant adeno-associated virus (AAV) carrying RPE65 gene, and found it yielded positive results, with patients having modest increase in vision, and, perhaps more importantly, no apparent side-effects.
2008:
In May 2008, two more groups, one at the University of Florida and another at the University of Pennsylvania, reported positive results in independent clinical trials using gene therapy to treat Leber’s congenital amaurosis. In all three clinical trials, patients recovered functional vision without apparent side-effects. These studies, which used adeno-associated virus, have spawned a number of new studies investigating gene therapy for human retinal disease.
2009:
In September 2009, the journal Nature reported that researchers at the University of Washington and University of Florida were able to give trichromatic vision to squirrel monkeys using gene therapy, a hopeful precursor to a treatment for color blindness in humans. In November 2009, the journal Science reported that researchers succeeded at halting a fatal genetic disorder called adrenoleukodystrophy in two children using a lentivirus vector to deliver a functioning version of ABCD1, the gene that is mutated in the disorder.
2010:
A paper by Komáromy et al. published in April 2010, deals with gene therapy for a form of achromatopsia in dogs. Achromatopsia, or complete color blindness, is presented as an ideal model to develop gene therapy directed to cone photoreceptors. Cone function and day vision have been restored for at least 33 months in two young dogs with achromatopsia. However, the therapy was less efficient for older dogs. In September 2010, it was announced that an 18 year old male patient in France with beta-thalassemia major had been successfully treated with gene therapy. Beta-thalassemia major is an inherited blood disease in which beta haemoglobin is missing and patients are dependent on regular lifelong blood transfusions. A team directed by Dr. Phillipe Leboulch (of the University of Paris, Bluebird Bio and Harvard Medical School) used a lentiviral vector to transduce the human ß-globin gene into purified blood and marrow cells obtained from the patient in June 2007. The patient’s haemoglobin levels were stable at 9 to 10 g/dL, about a third of the hemoglobin contained the form introduced by the viral vector and blood transfusions had not been needed. Further clinical trials were planned. Bone marrow transplants are the only cure for thalassemia but 75% of patients are unable to find a matching bone marrow donor.
2011:
In 2007 and 2008, a man being treated by Gero Hütter was cured of HIV by repeated Hematopoietic stem cell transplantation with double-delta-32 mutation which disables the CCR5 receptor; this cure was not completely accepted by the medical community until 2011. This cure required complete ablation of existing bone marrow which is very debilitating. In August 2011, two of three subjects of a pilot study were confirmed to have been cured from chronic lymphocytic leukemia (CLL). The study carried out by the researchers at the University of Pennsylvania used genetically modified T cells to attack cells that expressed the CD19 protein to fight the disease. In 2013, the researchers announced that 26 of 59 patients had achieved complete remission and the original patient had remained tumor-free. Human HGF plasmid DNA therapy of cardiomyocytes is being examined as a potential treatment for coronary artery disease as well as treatment for the damage that occurs to the heart after myocardial infarction.
2012:
The FDA approves clinical trials of the use of gene therapy on thalassemia major patients in the US. Researchers at Memorial Sloan Kettering Cancer Center in New York begin to recruit 10 participants for the study in July 2012. The study is expected to end in 2014. In July 2012, the European Medicines Agency recommended approval of a gene therapy treatment for the first time in either Europe or the United States. The treatment, called Alipogene tiparvovec (Glybera), compensates for lipoprotein lipase deficiency (LPLD), which can cause severe pancreatitis. People with LPLD cannot break down fat, and must manage their disease with a restricted diet. However, dietary management is difficult, and a high proportion of patients suffer life-threatening pancreatitis. The recommendation was endorsed by the European Commission in November 2012 and commercial rollout is expected in late 2013. In December 2012, it was reported that 10 of 13 patients with multiple myeloma were in remission “or very close to it” three months after being injected with a treatment involving genetically engineered T cells to target proteins NY-ESO-1 and LAGE-1 which exist only on cancerous myeloma cells.
2013:
In March 2013, Researchers at the Memorial Sloan-Kettering Cancer Center in New York, reported that three of five subjects who had acute lymphocytic leukemia (ALL) had been in remission for five months to two years after being treated with genetically modified T cells which attacked cells with CD19 genes on their surface, i.e. all B-cells, cancerous or not. The researchers believed that the patient’s immune systems would make normal T-cells and B-cells after a couple of months however they were given bone marrow to make sure. One patient had relapsed and died and one had died of a blood clot unrelated to the disease. Following encouraging Phase 1 trials, in April 2013, researchers in the UK and the US announced they were starting Phase 2 clinical trials (called CUPID2 and SERCA-LVAD) on 250 patients at several hospitals in the US and Europe to use gene therapy to combat heart disease. These trials were designed to increase the levels of SERCA2a protein in the heart muscles and improve the function of these muscles. The FDA granted this a Breakthrough Therapy Designation which would speed up the trial and approval process in the USA. In July 2013 the Italian San Raffaele Telethon Institute for Gene Therapy (HSR-TIGET) reported that six children with two severe hereditary diseases had been treated with a partially deactivated lentivirus to replace a faulty gene and after 7–32 months the results were promising. Three of the children had metachromatic leukodystrophy which causes children to lose cognitive and motor skills. The other children had Wiskott-Aldrich syndrome which leaves them to open to infection, autoimmune diseases and cancer due to a faulty immune system. In October 2013, the Great Ormond Street Hospital, London reported that two children born with adenosine deaminase severe combined immunodeficiency disease (ADA-SCID) had been treated with genetically engineered stem cells 18 months previously and their immune systems were showing signs of full recovery. Another three children treated since then were also making good progress. ADA-SCID children have no functioning immune system and are sometimes known as “bubble children.” In October 2013, Amit Nathswani of the Royal Free London NHS Foundation Trust in London reported that they had treated six people with haemophilia in early 2011 using genetically engineered adeno-associated virus. Over two years later all six were still producing blood plasma clotting factor.
2014:
In January 2014, researchers at the University of Oxford reported that six people suffering from choroideremia had been treated with a genetically engineered adeno-associated virus with a copy of a gene REP1. Over a six month to two year period all had improved their sight. Choroideremia is an inherited genetic eye disease for which in the past there has been no treatment and patients eventually go blind. In March 2014 researchers at the University of Pennsylvania reported that 12 patients with HIV had been treated since 2009 in a trial with a genetically engineered virus with a rare mutation known to protect against HIV (CCR5 deficiency). Results were promising.
_
The three main issues for the coming decade will be public perceptions, scale-up and manufacturing, and commercial considerations. Focusing on single-gene applications, which tend to be rarer diseases, will produce successful results sooner than the current focus on the commoner, yet more complex, cancer and heart diseases.
______
What is Gene?
A gene is an important unit of hereditary information. It provides the code for living organisms’ traits, characteristics, function, and physical development. Each person has around 25,000 genes that are located on 46 chromosomes. Gene is a segment of DNA found on chromosome that codes for a particular protein. It acts as a blue print for making enzymes and other proteins for every biochemical reaction and structure of body.
What is allele?
Alleles are two or more alternative forms of a gene that can occupy a specific locus (location) on a chromosome.
What is DNA?
Deoxyribonucleic acid (DNA) is a nucleic acid that contains the genetic information used in the development and function of all known living organisms. The main role of DNA is the long-term storage of information. DNA is often compared to a set of blueprints or a recipe or code, since it contains the instructions needed to construct other components of cells, such as proteins. The DNA segments that carry this genetic information are called genes.
What are Chromosomes?
A chromosome is a singular piece of DNA, which contains many genes. Chromosomes also contain DNA-bound proteins, which serve to package the DNA and control its functions. Chromosomes are found inside the nucleus of cells.
What are Proteins?
Proteins are large organic compounds made of amino acids. They are involved in many processes within cells. Proteins act as building blocks, or function as enzymes and are important in “communication” among cells.
_
What are plasmids?
_
_
Plasmid is any extrachromosomal heritable determinant. Plasmids are fragments of double-stranded DNA that can replicate independently of chromosomal DNA, and usually carry genes. Although they can be found in Bacteria, Archaea and Eukaryotes, they play the most significant biological role in bacteria where they can be passed from one bacterium to another by horizontal gene transfer, usually providing a context-dependent selective advantage, such as antibiotic resistance.
_
In the center of every cell in your body is a region called the nucleus. The nucleus contains your DNA which is the genetic code you inherited from each of your parents. The DNA is ribbon-like in structure, but normally exists in a condensed form called chromosomes. You have 46 chromosomes (23 from each parent), which are in turn comprised of thousands of genes. These genes encode instructions on how to make proteins. Proteins make up the majority of a cell’s structure and perform most life functions. Genes tell cells how to work, control our growth and development, and determine what we look like and how our bodies work. They also play a role in the repair of damaged cells and tissues. Each person has more than 25,000 genes, which are made up of DNA. You have 2 copies of every gene, 1 inherited from your mother and 1 from your father.
_
_
DNA or deoxyribonucleic acid is the very long molecule that encodes the genetic information. A gene is a stretch of DNA required to make a functional product such as part or all of a protein. People have about 25,000 genes. During gene therapy, DNA that codes for specific genes is delivered to individual cells in the body.
_
The Human Genome:
The human genome is the entire genetic code that resides in every cell in your body (with the exception of red blood cells). The genome is divided into 23 chromosome pairs. During reproduction, two copies of the chromosomes (one from each parent) are passed onto the offspring. While most chromosomes are identical for males and females, the exceptions are the sex chromosomes (known as the X and Y chromosomes). Each chromosome contains thousands of individual genes. These genes can be further divided into sequences called exons and introns, which are in turn made up of even shorter sequences called codons. And finally, the codons are made up of base pairs, combinations of four bases: adenine, cytosine, thymine, and guanine. Or A, C, T, and G for short. The human genome is vast, containing an estimated 3.2 billion base pairs. To put that in perspective, if the genome was a book, it would be hundreds of thousands of pages long. That’s enough room for a dozen copies of the entire Encyclopaedia Britannica, and all of it fits inside a microscopic cell.
_
_
Our genes help make us unique. Inherited from our parents, they go far in determining our physical traits — like eye color and the color and texture of our hair. They also determine things like whether babies will be male or female, the amount of oxygen blood can carry, and the likelihood of getting certain diseases. Scientists believe that every human has about 25,000 genes per cell. A mutation, or change, in any one of these genes can result in a disease, physical disability, or shortened life span. These mutations can be passed from one generation to another, inherited just like a mother’s curly hair or a father’s brown eyes. Mutations also can occur spontaneously in some cases, without having been passed on by a parent. With gene therapy, the treatment or elimination of inherited diseases or physical conditions due to these mutations could become a reality. Gene therapy involves the manipulation of genes to fight or prevent diseases. Put simply, it introduces a “good” gene into a person who has a disease caused by a “bad” gene. Variations on genes are known as alleles. Because of changes in the genetic code caused by mutations, there are often more than one type of gene in the gene pool. For example, there is a specific gene to determine a person’s blood type. Therefore, a person with blood type A will have a different version of that gene than a person with blood type B. Some genes work in tandem with each other.
_
Genes to protein:
Chromosomes contain long chains of DNA built with repeating subunits known as nucleotides. That means a single gene is a finite stretch of DNA with a specific sequence of nucleotides. Those nucleotides act as a blueprint for a specific protein, which gets assembled in a cell using a multistep process.
1. The first step, known as transcription, begins when a DNA molecule unzips and serves as a template to create a single strand of complementary messenger RNA.
2. The messenger RNA then travels out of the nucleus and into the cytoplasm, where it attaches to a structure called the ribosome.
3. There, the genetic code stored in the messenger RNA, which itself reflects the code in the DNA, determines a precise sequence of amino acids. This step is known as translation, and it results in a long chain of amino acids — a protein.
Proteins are the workhorses of cells. They help build the physical infrastructure, but they also control and regulate important metabolic pathways. If a gene malfunctions — if, say, its sequence of nucleotides gets scrambled — then its corresponding protein won’t be made or won’t be made correctly. Biologists call this a mutation, and mutations can lead to all sorts of problems, such as cancer and phenylketonuria. Gene therapy tries to restore or replace a defective gene, bringing back a cell’s ability to make a missing protein.
_
Length measurements of DNA/RNA:
The following abbreviations are commonly used to describe the length of a DNA/RNA molecule:
bp = base pair(s)— one bp corresponds to approximately 3.4 Å (340 pm) of length along the strand, or to roughly 618 or 643 daltons for DNA and RNA respectively.
kb (= kbp) = kilo base pairs = 1,000 bp
Mb = mega base pairs = 1,000,000 bp
Gb = giga base pairs = 1,000,000,000 bp.
For case of single-stranded DNA/RNA units of nucleotides are used, abbreviated nt (or knt, Mnt, Gnt), as they are not paired.
Note:
Please do not confuse these terms with computer data units.
kb in molecular biology is kilobase pairs = 1000 base pairs
kb in computer data is kilobytes = 1000 bytes
_
Gene Mutations:
When human DNA is replicated there is the slight possibility for an error to occur. And while Human DNA has a built-in error-correction mechanism, sometimes this mechanism fails and a copying error is the result. These copying errors are called mutations. The vast majority of mutations occurs in ‘junk DNA’ and therefore has no effect on a person’s well being. When mutations occur in DNA that is used to code proteins, however, physiological effects can occur. Mutations themselves are relatively rare events. Estimates for the average number of mutations are over 100 per individual and most of those occur in ‘junk DNA’. Only a handful of mutations, between one and four, occur in protein-coding DNA. And while this might sound like a lot, given the size of the protein-coding DNA—around 100 million base pairs—mutations are fairly rare events.
_
Defective genes:
Each human being carries normal as well as some defective genes. Each of us carries about half a dozen defective genes. We remain blissfully unaware of this fact unless we, or one of our close relatives, are amongst the many millions who suffer from a genetic disease. About one in ten people has, or will develop at some later stage, an inherited genetic disorder, and approximately 2,800 specific conditions are known to be caused by defects (mutations) in just one of the patient’s genes. Some single gene disorders are quite common – cystic fibrosis is found in one out of every 2,500 babies born in the Western World – and in total, diseases that can be traced to single gene defects account for about 5% of all admissions to children’s hospitals. Although genes are responsible for predisposition to disease, the environment, diet, and lifestyle can affect the onset of the illness.
_
Genetic Disorders:
A genetic disorder is a disease caused in whole or in part by a change in the DNA sequence away from the normal sequence. Genetic disorders can be caused by a mutation in one gene (monogenic disorder), by mutations in multiple genes (multifactorial inheritance disorder), by a combination of gene mutations and environmental factors, or by damage to chromosomes (changes in the number or structure of entire chromosomes, the structures that carry genes). Genetic disorders affect millions of people world-wide. Scientists have currently identified more than 4000 different genetic disorders.
There are four main types of genetic disorders. These include:
- single-gene
- multifactorial
- chromosomal
- mitochondrial
Single-gene disorders are caused by a defect in a single gene. Examples include Huntington’s disease, cystic fibrosis, and sickle cell anemia. Multifactorial disorders are caused by a combination of genes. Alzheimer’s, heart disease and even cancer can be influenced by multifactorial disorders. Chromosomal disorders, such as Down syndrome, are caused by changes or replications of an entire chromosome. Finally, there are mitochondrial disorders in which the DNA of mitochondria, tiny organelles used in cell metabolism become affected.
_
Genetic disorders affect about one in every ten people. Some, like cystic fibrosis, can have consequences early in a child’s life while others, like Huntington’s disease don’t show up until later in life. Preventing genetic disorders can be difficult. Unlike regular diseases which are a result of external factors, genetic diseases are caused by our very own DNA. When the genetic code in a gene is altered, the gene can become defective. Most genetic disorders are hereditary; however spontaneous mutation can occur without being inherited from parents. When the defective gene is passed onto an offspring, there is a risk that that offspring will develop that genetic disorder. Some genetic disorders are caused by dominant genes, requiring only a single gene for the disease to develop. Others are caused by recessive genes which require two copies of the defective gene, one from each parent, to cause the disease.
_
Multifaceted diseases:
One of the major consequences of widespread belief in biological determinism is the underlying assumption that if a trait or condition is genetic, it cannot be changed. However, the relationship between genotype (the actual genes an individual inherits) and phenotype (what traits are observable) is complex. For example, cystic fibrosis (CF) is a multifaceted disease that is present in about 1 in every 2,000 live births of individuals of European ancestry. The disease is recessive, meaning that in order for it to show up phenotypically, the individual must inherit the defective gene, known as CFTR, from both parents. More than 1,000 mutation sites have been identified in CFTR, and most have been related to different manifestations of the disease. However, individuals with the same genotype can show remarkably different phenotypes. Some will show early onset, others later onset; in some the kidney is most afflicted, whereas in others it is the lungs. In some individuals with the most common mutation the effects are severe, whereas in others they are mild to nonexistent. Although the reasons for those differences are not understood, their existence suggests that both genetic background and environmental factors (such as diet) play important roles. In other words, genes are not destiny, particularly when the genetic basis of a condition is unclear or circumstantial but also even in cases where the genetic basis of a disability can be well understood, such as in cystic fibrosis. With modern genomics (the science of understanding complex genetic interactions at the molecular and biochemical levels), unique opportunities have emerged concerning the treatment of genetically based disabilities, such as type I diabetes, cystic fibrosis, and sickle-cell anemia. Those opportunities have centered primarily on gene therapy, in which a functional gene is introduced into the genome to repair the defect, and pharmacological intervention, involving drugs that can carry out the normal biochemical function of the defective gene.
_
Inheritance of genetic disorders:
Most of us do not suffer any harmful effects from our defective genes because we carry two copies of nearly all genes, one derived from our mother and the other from our father. The only exceptions to this rule are the genes found on the male sex chromosomes. Males have one X and one Y chromosome, the former from the mother and the latter from the father, so each cell has only one copy of the genes on these chromosomes. In the majority of cases, one normal gene is sufficient to avoid all the symptoms of disease. If the potentially harmful gene is recessive, then its normal counterpart will carry out all the tasks assigned to both. Only if we inherit from our parents two copies of the same recessive gene will a disease develop. On the other hand, if the gene is dominant, it alone can produce the disease, even if its counterpart is normal. Clearly only the children of a parent with the disease can be affected, and then on average only half the children will be affected. Huntington’s chorea, a severe disease of the nervous system, which becomes apparent only in adulthood, is an example of a dominant genetic disease. Finally, there are the X chromosome-linked genetic diseases. As males have only one copy of the genes from this chromosome, there are no others available to fulfill the defective gene’s function. Examples of such diseases are Duchenne muscular dystrophy and, perhaps most well known of all, hemophilia.
_
Autosomal recessive, autosomal dominant and X-linked:
These terms are used to describe the common modes of inheritance for genetic disorders.
1. Autosomal recessive – where a genetic disorder requires both copies of a gene to be abnormal to cause the disease. Both parents of the affected individual are carriers, i.e., carry one abnormal copy but also have a normal copy so they themselves are not affected.
2. Autosomal dominant – some genetic disorders only need one copy of the gene to be abnormal, i.e., having one normal copy is just not enough. One of the parents is usually affected.
3. X-linked – is where the gene is on the X (sex) chromosome. The mother is usually a carrier with only the male children being at risk of having the disorder.
Homozygous/heterozygous:
Terminology used in a number of different contexts. One context is: homozygous, where a mistake is present in both copies of a gene; versus heterozygous, where the mistake is present in only one of the two gene copies.
_______
What is genetic testing?
Genetic testing can determine whether a person is carrying the alleles that cause genetic disorders. Genetic testing involves analyzing a person’s DNA to see if they carry alleles that cause genetic disorders. Genetic testing is used to identify the presence of certain genes with a person’s DNA. This can be used to determine if a person contains the genes that cause genetic disorders. In cases like Huntington’s disease, a person can have advance warning of the onset of the disease. In other cases, parents each with a defective recessive gene will know if their offspring has the potential to develop a genetic disorder. It can be done at any stage in a person’s life. But there are limits to the testing, and the subject raises a number of ethical issues.
There are several types of genetic test, including testing for medical research:
Antenatal testing:
This is used to analyze an individual’s DNA or chromosomes before they are born. At the moment, it cannot detect all inherited disorders. Prenatal testing is offered to couples who may have an increased risk of producing a baby with an inherited disorder. Prenatal testing for Down’s syndrome, which is caused by a faulty chromosome, is offered to all pregnant women.
Neonatal testing:
Neonatal testing involves analyzing a sample of blood taken by pricking the baby’s heel. This is used just after a baby has been born. It is designed to detect genetic disorders that can be treated early. In the UK, all babies are screened for phenylketonuria, congenital hypothyroidism and cystic fibrosis. Babies born to families that are at risk of sickle cell disease are tested for this disorder.
Carrier testing:
This is used to identify people who carry a recessive allele, such as the allele for cystic fibrosis. It is offered to individuals who have a family history of a genetic disorder. Carrier testing is particularly useful if both parents are tested, because if both are carriers there is an increased risk of producing a baby with a genetic disorder.
Predictive testing:
This is used to detect genetic disorders where the symptoms develop later in life, such as Huntington’s disorder. Predictive testing can be valuable to people who have no symptoms but have a family member with a genetic disorder. The results can help to inform decisions about possible medical care.
_
Limits of genetic testing:
Genetic tests are not available for every possible inherited disorder. And they are not completely reliable. They may produce false positive or false negative results. These can have serious consequences.
False positives:
A false positive occurs when a genetic test has wrongly detected a certain allele or faulty chromosome. The individual or family could believe something is wrong when it is not. This may lead them to decide not to start a family, or to choose an abortion, in order to avoid having a baby with a genetic disorder.
False negatives:
A false negative happens when a genetic test has failed to detect a certain allele or faulty chromosome. The individual or family would be wrongly reassured. This may lead them to decide to start a family or continue with a pregnancy.
_
The technologies that make genetic testing possible range from chemical tests for gene products in the blood, through examining chromosomes from whole cells, to identification of the presence or absence of specific, defined DNA sequences, such as the presence of mutations within a gene sequence. The last of these is becoming much more common in the wake of the Human Genome Project. The technical details of particular tests are changing fast and they are becoming much more accurate. But the important point is that it is possible to test for more genes, and more variants of those genes, using very small samples of material. For an adult, a cheek scraping these days provides ample cells for most DNA testing. Before treatment for a genetic disease can begin, an accurate diagnosis of the genetic defect needs to be made. It is here that biotechnology is also likely to have a great impact in the near future. Genetic engineering research has produced a powerful tool for pinpointing specific diseases rapidly and accurately. There are different techniques to accomplish gene testing. Short pieces of DNA called DNA probes can be designed to stick very specifically to certain other pieces of DNA. The technique relies upon the fact that complementary pieces of DNA stick together. DNA probes are more specific and have the potential to be more sensitive than conventional diagnostic methods, and it should be possible in the near future to distinguish between defective genes and their normal counterparts, an important development. Another technique involves a side-by-side comparison of more than one person’s DNA. Genes within a person can be compared with healthy copies of those genes to determine if the person’s genes are, in fact, defective.
_
All these different kinds of test can bring benefits. But all three, i.e. pre-natal diagnosis, childhood testing and adult testing, have also been noted as requiring careful management because of ethical problems that can arise from the kind of information they provide. We are confronted with moral choices here, for example, who gets that information and under what circumstances, what they do with it, and who decides what to do with it, are all important issues. Even finding out what people would like to know is not necessarily straightforward. (Is telling someone they can have a test for Huntington’s disease, say, the same as telling them they may be at risk of the disease?) Here we are not primarily concerned with the technologies for testing, but with the ethical context within which testing takes place; a context framed by issues such as informed consent, individual decision-making and confidentiality of genetic information.
_
At this stage, we should distinguish genetic testing from genetic screening. Genetic testing is used with individuals who, because of their family history think they are at risk of carrying the gene for a particular genetic disease. Screening covers wide-scale testing of populations, to discover who may be at risk of genetic disease.
_
Genetic Screening:
Genetic screening may be indicated in populations at risk of a particular genetic disorder. The usual criteria for genetic screening are
1. Genetic inheritance patterns are known.
2. Effective therapy is available.
3. Screening tests are sufficiently valid, reliable, sensitive and specific, noninvasive, and safe.
4. Prevalence in a defined population must be high enough to justify the cost of screening.
One aim of prenatal genetic screening is to identify asymptomatic parental heterozygotes carrying a gene for a recessive disorder. For example, Ashkenazi Jews are screened for Tay-Sachs disease, blacks are screened for sickle cell anemia, and several ethnic groups are screened for thalassemia. If a heterozygote’s mate is also a heterozygote, the couple is at risk of having an affected child. If the risk is high enough, prenatal diagnosis can be pursued (e.g., with amniocentesis, chorionic villus sampling, umbilical cord blood sampling, maternal blood sampling or fetal imaging). In some cases, genetic disorders diagnosed prenatally can be treated, preventing complications. For instance, special diet or replacement therapy can minimize or eliminate the effects of phenylketonuria, galactosemia, and hypothyroidism. Corticosteroids given to the mother before birth may decrease the severity of congenital virilizing adrenal hypoplasia. Screening may be appropriate for people with a family history of a dominantly inherited disorder that manifests later in life, such as Huntington disease or cancers associated with abnormalities of the BRCA1 and BRCA2 genes. Screening clarifies the risk of developing the condition for that person, who can then make appropriate plans, such as for more frequent screening or preventive therapy. Screening may also be indicated when a family member is diagnosed with a genetic disorder. A person who is identified as a carrier can make informed decisions about reproduction. In a nutshell, genetic screening is justified only if disease prevalence is high enough, treatment is feasible, and tests are accurate enough.
_______
Genetic engineering vis-à-vis gene therapy vis-à-vis genetic enhancement:
Genetic engineering, also called genetic modification, is the direct manipulation of an organism’s genome using biotechnology. New DNA may be inserted in the host genome by first isolating and copying the genetic material of interest using molecular cloning methods to generate a DNA sequence, or by synthesizing the DNA, and then inserting this construct into the host organism. Genes may be removed, or “knocked out”, using a nuclease. Gene targeting is a different technique that uses homologous recombination to change an endogenous gene, and can be used to delete a gene, remove exons, add a gene, or introduce point mutations. An organism that is generated through genetic engineering is considered to be a genetically modified organism (GMO). The first GMOs were bacteria in 1973 and GM mice were generated in 1974. Insulin-producing bacteria were commercialized in 1982 and genetically modified food has been sold since 1994. Genetic engineering does not normally include traditional animal and plant breeding, in vitro fertilisation, induction of polyploidy, mutagenesis and cell fusion techniques that do not use recombinant nucleic acids or a genetically modified organism in the process. However the European Commission has also defined genetic engineering broadly as including selective breeding and other means of artificial selection. Cloning and stem cell research, although not considered genetic engineering, are closely related and genetic engineering can be used within them. Synthetic biology is an emerging discipline that takes genetic engineering a step further by introducing artificially synthesized genetic material from raw materials into an organism. If genetic material from another species is added to the host, the resulting organism is called transgenic. If genetic material from the same species or a species that can naturally breed with the host is used the resulting organism is called cisgenic. In medicine, genetic engineering has been used to mass-produce insulin, human growth hormones, follistim (for treating infertility), human albumin, monoclonal antibodies, antihemophilic factors, vaccines and many other drugs. Vaccination generally involves injecting weak, live, killed or inactivated forms of viruses or their toxins into the person being immunized. Genetically engineered viruses are being developed that can still confer immunity, but lack the infectious sequences. Mouse hybridomas, cells fused together to create monoclonal antibodies, have been humanised through genetic engineering to create human monoclonal antibodies. Genetic engineering has shown promise for treating certain forms of cancer.
_
Gene therapy is the genetic engineering of humans by replacing defective human genes with functional copies. Genetic enhancement refers to the use of genetic engineering to modify a person’s nonpathological human traits. In contrast, gene therapy involves using genetic engineering to alter defective genes or insert corrected genes into the body in order to treat a disease. However, there is no clear distinction between genetic enhancement and gene therapy. One approach to distinguishing between the two is to classify any improvement beyond that which is “natural” as an enhancement. “Enhancement” would then include preventive measures such as vaccines, which strengthen one’s immune system to a point beyond that which would be achieved “naturally.” Another approach is to consider gene therapy as encompassing any process aimed at preserving or restoring “normal” functions, while anything that improves a function beyond that which is “normal” would be considered a genetic enhancement. This, however, would require “normal” to be defined, which only frustrates the clarification of enhancement versus therapy. Yet another way to distinguish between therapy and enhancement might rely on the goal of the genetic alteration. But the classification of the goal will necessarily depend on how “disease” or “normal” is defined.
_
Human genetic engineering is divided into four types. The first, which is being practiced today, is somatic cell gene therapy. Somatic cells are the cells in our bodies that are not the egg or sperm cells. Therefore, if a patient were to suffer from melanoma, for instance, somatic gene therapy could cure the skin cancer, but the cure would not extend to his posterity. Germ-line gene therapy, however, involves correcting the genetic defect in the reproductive cells (egg and sperm) of the patient so that his progeny will be cured of melanoma also. The third is enhancement genetic engineering, in which a gene is inserted to enhance a specific characteristic. For example, a gene cording for a growth hormone could be inserted to increase a person’s height. The last type is eugenic genetic engineering. It involves the insertion of genes to alter complex human traits that depend on a large number of genes as well as extensive environmental influences. This last type is the most ambitious because it aims at altering a person’s intelligence and personality. So far, only somatic cell gene therapy is being performed. The other types involve serious moral and social issues that prevent their being pursued at this time.
_
A genetically modified organism (GMO) is an organism (plant/ animal/ microorganism etc) whose genetic material (DNA) has been altered using genetic engineering techniques by either adding a gene from a different species or over-expressing/ silencing a preexisting native gene. Genetic material can be artificially inserted either by physically inserting the extra DNA into the nucleus of the intended host with a very small syringe/a gene gun, by using the ability of Agrobacterium (bacteria) to transfer genetic material to plants, and the ability of lentiviruses (viruses) to transfer genes to animal cells. Such bacteria/ viruses are then called vectors. Genetically modified (GM) foods are foods derived from genetically modified organisms (GMO). These GM foods could be derived from either plant kingdom (e.g. tomatoes) or animal kingdom (e.g. salmon fish). Genetic material in an organism can be altered without genetic engineering techniques which include mutation breeding where an organism is exposed to radiation or chemicals to create a non-specific but stable change, selective breeding (plant breeding and animal breeding), hybridizing and somaclonal variation. However, these organisms are not labeled as GMO. In the puritan medical terminology, any individual who has received gene therapy necessarily becomes GMO.
_
Transgenic animal:
A “transgenic animal” is defined as an animal which is altered by the introduction of recombinant DNA through human intervention. This includes two classes of animals; those with heritable germline DNA alterations, and those with somatic non-heritable alterations. Examples of the first class include animals with germline DNA altered through methods requiring ex vivo manipulation of gametes, early embryonic stages, or embryonic stem cell lines. Examples of the second class include animals with somatic cell DNA alterations achieved through gene therapy approaches such as direct plasmid DNA injection or virally-mediated gene transfer.” “Transgene” refers to a segment of recombinant DNA which is either: 1) introduced into somatic cells, or 2) integrated stably into the germline of its animal host strain, and is transmissible to subsequent generations.
_
Transgenesis:
_
Is insertion of the insulin gene in E. coli an example of gene therapy?
No, it’s a good example of genetic engineering though. To be more specific, it is an example of recombinant DNA technology. So gene therapy, genetic enhancement, recombinant DNA technology, transgenesis etc are different kinds of genetic engineering.
_
Recombinant proteins and genetically engineered vaccines:
Here the therapy is to deliver proteins or vaccines which have been produced by genetic engineering instead of traditional methods. Methods involve:
1. Expression cloning of normal gene products — cloned genes are expressed in microorganisms or transgenic livestock in order to make large amounts of a medically valuable gene product;
2. Production of genetically engineered antibodies — antibody genes are manipulated so as to make novel antibodies, including partially or fully humanized antibodies, for use as therapeutic agents;
3. Production of genetically engineered vaccines — includes novel cancer vaccines and vaccines against infectious agents.
_
______
Gene therapy vs. cell therapy:
Gene therapy is introduction or alteration of genetic material within the cell/organism with the intention of curing or treating disease. Cell therapy is transfer of cells into a patient with the goal of improving a disease. Gene therapy can be defined as the use of genetic material (usually deoxyribonucleic acid – DNA) to manipulate a patient’s cells for the treatment of an inherited or acquired disease. Cell therapy can be defined as the infusion or transplantation of whole cells into a patient for the treatment of an inherited or acquired disease. Cell therapy involves either differentiated cell (e.g. lymphocyte) or stem cell (e.g. hematopoietic stem cells HSC). Stem cell research is about growing new organs and body parts out of basic cells, whereas gene therapy is about replacing or treating parts of the human genome.
_
Cell therapy:
Cell therapy is the transfer of cells into a patient or animal to help lessen or cure a disease. Cell therapy could be stem cell therapy or non-stem cell therapy; either could be autologus (self) or allogenic (different individual). The origin of the cells depends on the treatment. The transplanted cells are often a type of adult stem cells which have the ability to divide and self renew as well as provide cells that mature into the relevant specialized cells of the tissue. Blood transfusion and transfusion of red blood cells, white blood cells and platelets are a form of cell therapy that is very well accepted. Another common cell therapy is bone marrow transplantation which has been performed for over 40 years. The term somatic cell therapy refers to the administration to humans of autologous, allogeneic, or xenogeneic living non-germline cells, other than transfusable blood products, for therapeutic, diagnostic, or preventive purposes. Examples of somatic cell therapies include implantation of cells as an in vivo source of a molecular species such as an enzyme, cytokine or coagulation factor; infusion of activated lymphoid cells such as lymphokine activated killer cells and tumor-infiltrating lymphocytes; and implantation of manipulated cell populations, such as hepatocytes, myoblasts, or pancreatic islet cells, intended to perform a complex biological function.
_
Example of gene therapy and cell therapy:
A classic example of gene therapy is the efforts to correct hemophilia. Hemophilia A and hemophilia B are caused by deficiencies of the clotting factors factor VIII and factor IX respectively. FVIII and FIX are made in the liver and secreted into the blood where they have critical roles in the formation of clots at the sites of vessel injury. Mutations in the FVIII or FIX genes prevent clot formation, and patients with hemophilia are at a severe risk of bleeding to death. Using disabled virus carriers, researchers have been able to introduce normal FVIII and FIX genes into the muscle and liver of animal models of hemophilia, and in the case of FIX, human patients. Currently the most common Cell Therapy (other than blood transfusions) is bone marrow transplantation. Bone marrow transplantation is the treatment of choice for many kinds of leukemia and lymphoma, and is used to treat many inherited disorders ranging from the relatively common thalassemias (deficiencies of alpha-globin or beta-globin, the components of hemoglobin) to more rare disorders like Severe Combined Immune Deficiency (SCID the “Bubble Boy” disease). The key to bone marrow transplantation is the identification of a good “immunological matched” donor. The patient’s bone marrow cells are then destroyed by chemotherapy or radiation, and cells from the matched donor are infused. The most primitive bone marrow cells, called stem cells then find their way to the bone marrow where the replicate to increase their number (self renew) and also proliferate and mature producing normal numbers of donor derived blood cells in the circulation of the patient in a few weeks. Unfortunately, not all patients have a good “immunological match”. In addition, up to a third (depending on several factors including the disease) of bone marrow grafts fail to fully repopulate the patient, and the destruction of the host bone marrow can be lethal, particularly in very ill patients. These factors combine to hold back the obvious potential of bone marrow transplantation.
_
How are gene therapy and cell therapy related?
Both approaches have the potential to alleviate the underlying cause of genetic diseases and acquired diseases by replacing the missing protein(s) or cells causing the disease symptoms, suppressing expression of proteins which are toxic to cells, or eliminating cancerous cells.
_
Combining Cell Therapy with Gene Therapy:
Gene therapy and Cell therapy are overlapping fields of biomedical research with similar therapeutic goals. Some protocols utilize both gene therapy and cell therapy: stem cells are isolated from the patient, genetically modified in tissue culture to express a new gene, typically using a viral vector, expanded to sufficient numbers, and returned to the patient. Several investigative protocols of cell therapy involve the transfer of adult T lymphocytes which are genetically modified to increase their immune potency and can self renew and kill the disease-causing cells. Stem cells from umbilical cord blood and other tissues are being developed to treat many genetic diseases and some acquired diseases.
_
Classical example of combining cell therapy and gene therapy:
Hematopoietic Stem cell transplantation and gene therapy:
Hematopoietic stem cell transplantation (HSCT) represents the mainstay of treatment for several severe forms of primary immunodeficiency diseases. Progress in cell manipulation, donor selection, the use of chemotherapeutic agents, and prevention and management of transplant-related complications has resulted in significant improvement in survival and quality of life after HSCT. The primary immunodeficiency diseases for which HSCT is most commonly performed include Severe Combined Immune Deficiency (SCID), Wiskott-Aldrich Syndrome (WAS), IPEX Syndrome, Hemophagocytic Lymphohistiocytosis (HLH) and X-linked Lymphoproliferative Disease (XLP). It can also be used in the treatment of Chronic Granulomatous Disease (CGD) and many other severe primary immunodeficiency diseases. The transplantation of HSCs from a “normal” individual to an individual with a primary immunodeficiency disease has the potential to replace the deficient immune system of the patient with a normal immune system and, thereby, affect a cure. There are two potential obstacles that must be overcome for HSCT to be successful. The first obstacle is that the patient (known as the recipient or host) may have enough immune function remaining after the transplant to recognize the transplanted stem cells as something foreign. The immune system is programmed to react against things perceived as foreign and tries to reject them. This is called graft rejection. In order to prevent rejection, most patients require chemotherapy and/or radiation therapy to weaken their own residual immune system enough to prevent it from rejecting the transplanted HSCs. This is called “conditioning” before transplantation. Many patients with SCID have so little immune function that they are incapable of rejecting a graft and do not require conditioning before HSCT. The second obstacle that must be overcome for the transplant to be successful is Graft versus Host Disease (GVHD). This occurs when the mature T-cells from the donor or which develop after the transplant, perceive the host’s tissues as foreign and attack these tissues. To prevent GVHD, medications to suppress inflammation and T-cell activation are used. These medications may include steroids, cyclosporine and other drugs. In some forms of severe primary immunodeficiency diseases, gene therapy may represent a valid alternative for patients who lack acceptable stem cell donors. To perform gene therapy, the patient’s HSCs are first isolated from the bone marrow or from peripheral blood, and they are then cultured in the laboratory with the virus containing the gene of interest. Various growth factors are added to the culture to make HSC proliferate and to facilitate infection with the virus. After two to four days, the cultured cells are washed to remove any free virus, and then they are transfused into the patient. The cells that have incorporated the gene of interest into their chromosomes will pass it to all cells that will be generated when these cells divide. Because the gene has been inserted into HSC, the normal copy of the gene will be passed to all blood cell types, but not to other cells of the body. Because primary immunodeficiency diseases are caused by gene defects that affect blood cells, this can be sufficient to cure the disease. Gene therapy represents a life-saving alternative for those patients with severe forms of primary immunodeficiency diseases, who do not have a matched sibling donor. In these cases, performing an HSCT from a haploidentical parent or even from a MUD would carry some significant risks of GVHD. In contrast, GVHD is not a problem after gene therapy, because in this case the normal copy of the gene is inserted into the patient’s own HSC, negating the need for a HSC donor. Until now, gene therapy has been used to treat patients with SCID secondary to adenosine deaminase (ADA) deficiency, X-linked SCID, CGD and WAS.
_
Another example of Cell and Gene Therapy overlapping is in the use of T-lymphocytes to treat cancer:
Many tumors are recognized as foreign by the patient’s T-cells, but these T-cells do not expand their numbers fast enough to kill the tumor. T-cells found in the tumor can be grown outside the body to very high numbers and then infused into the patient, often causing a dramatic reduction in the size of the tumor. This treatment is especially effective for tumors that have spread, as the tumor specific lymphocytes will track them down where ever they are. The addition of gene to the T-cells can allow specific T-cells that may be more effective tumor killers, and a second gene that can be used to kill the expanded T-cells after they have done their job.
____________
The technique of genetic manipulation of organisms:
The technique of genetic manipulation, or genetic modification, of organisms relies on restriction enzymes to cut large molecules of DNA in order to isolate the gene or genes of interest from human DNA, which has been extracted from cells. After the gene has been isolated, it is inserted into bacterial cells and cloned. This process enables large amounts of identical copies of the human DNA to be extracted for further experiments. Once inside the bacterial cells, if the human gene is active or ‘switched on’ then the bacteria behave like ‘living factories’, manufacturing large amounts of the human protein encoded by the gene as seen in the figure below. This can be extracted and purified from the bacterial cultures, ready for use by humans. Genetic manipulation has enabled unlimited quantities of certain human proteins to be produced more easily and less expensively than was previously possible. Problems exist with this approach; however, as proteins must fold themselves up into very specific structures to have a biological effect. Often this doesn’t happen very effectively in bacteria. In order to overcome this problem, the cloned human DNA has been introduced into sheep. In this case, the human protein is secreted into the milk, allowing for a continuous process of production as seen in the figure below. Alternatively, the cloned human DNA can be used for gene therapy by direct intervention in the individual’s DNA.
_
_
Human clotting factor VIII, the protein used to treat haemophilia, can be made by splicing the human gene into bacteria. Insulin, which is used to treat diabetes, can be produced by sheep in their milk. Then you can supply the missing gene product to the patient like any other medicine.
_
The figure below shows that copy of human gene cloned in bacteria can be used for gene therapy:
__________
Two fundamental gene therapy approaches:
Two approaches to gene therapy exist: correcting genes involved in causing illness; and using genes to treat disorders. Most of the public debate has been about the former meaning, i.e. correcting or repairing genes, but early applications have focused on the latter meaning. These applications involve using ‘designer’ DNA to tackle diseases that are not inherited – by using altered viruses designed specifically to attack say cancer cells. Here, the DNA is working more or less like a drug. In fact, many ‘gene therapy’ trials approved so far have been attempts to treat a variety of cancers.
_________
Fundamentals of gene therapy:
_
What is Gene Therapy?
Gene therapy can broadly be considered any treatment that changes gene function. However, gene therapy is often considered specifically the insertion of normal genes into the cells of a person who lacks such normal genes because of a specific genetic disorder. The normal genes can be manufactured, using PCR, from normal DNA donated by another person. Because most genetic disorders are recessive, usually a dominant normal gene is inserted. Currently, such insertion gene therapy is most likely to be effective in the prevention or cure of single-gene defects, such as cystic fibrosis. It is intracellular delivery of genes to generate a therapeutic effect by correcting an existing abnormality. The Human Genome Project provides information that can be used to help replace genes that are defective or missing in people with genetic diseases.
_
_
The figure below shows that mutated gene produces defective protein:
_
The figure below shows that corrected gene replaces defective gene:
_
Gene therapy is the transfer of genetic material into a host (human or animal) with the intention of alleviating a disease state. Gene therapy uses genetic material to change the expression of a protein(s) critical to the development and/or progression of the disease. In gene replacement therapy typically used for diseases of loss of protein function (inherited in an autosomal recessive manner), scientists first identify a gene that is strongly associated with the onset of disease or its progression. They show that correcting its information content or replacing it with expression of a normal gene counterpart corrects the defect in cultured cells and improves the disease in animal models, and is not associated with adverse outcomes. Scientists and clinicians then develop strategies to replace the gene or provide its function by administering genetic material into the patient. The relevant genetic material or gene usually is engineered into a “gene cassette” and prepared for introduction into humans according to stringent guidelines for clinical use. The cassette can be delivered directly as DNA, or engineered into a disabled viral vector, packaged into a type of membrane vesicles (termed liposome) so it is efficiently taken up by the appropriate cells of the body or used to genetically modify cells for implantation into patients. Other types of gene therapy include delivery of RNA or DNA sequences (oligonucleotide therapy) that can be used either to depress function of an unwanted gene, such as one responsible for a mutant protein which acts in a negative way to reduce normal protein function (usually inherited in an autosomal dominant manner), to try to correct a defective gene through stimulation of DNA repair within cells, or to suppress an oncogene which acts as a driver in a cancer cell. In other strategies for diseases and cancer, the gene/RNA/DNA delivered is a novel agent intended to change the metabolic state of the cells, for example to make cancer cells more susceptible to drug treatment, to keep dying cells alive by delivery of growth factors, to suppress or activate formation of new blood vessels or to increase production of a critical metabolite, such as a neurotransmitter critical to brain function. Vectors and cells can also be used to promote an immune response to tumor cells and pathogens by expressing theses antigens in immune responsive cells in combination with factors which enhance the immune response.
_
Gene therapy (use of genes as medicines) is basically to correct defective genes responsible for genetic disorder by one of the following approaches-
• A normal gene could be inserted into a nonspecific location within the genome to replace the Nonfunctional gene (most common)
• An abnormal gene could be swapped for a normal gene homologous recombination
• An abnormal gene could be repaired through selective reverse mutation
• Regulation (degree to which a gene is turned on or off) of a particular gene could be altered
_
Other approaches:
In the most straightforward cases, gene therapy adds a functional copy of a gene to cells that have only non-functional copies. But there are times when simply adding a working copy of the gene won’t solve the problem. In these cases, scientists have had to think outside the box to come up other approaches.
Dominant negative:
Some mutations in genes lead to the production of a dominant-negative protein. A dominant-negative protein may block a normal protein from doing its job (for an example, see Pachyonychia congenita). In this case, adding a functional copy of the gene won’t help, because the dominant-negative protein will still be there causing problems.
Gain-of-function:
A gain-of-function mutation makes a protein that acts abnormally, causing problems all on its own. For example, let’s say a signal activates protein X, which then tells the cell to start growing and dividing. A gain-of-function mutation may make protein X activates cell growth even when there’s no signal, leading to cancer.
Improper regulation:
Sometimes a disorder can involve a protein that is functioning as it should—but there’s a problem with where, when, or how much protein is being made. These are problems of gene regulation: genes need to be turned “on” in the right place, at the right time, and to the right level. To address the above situations, you could prevent the cell from making the protein the gene encodes, repair the gene, or find a work-around aimed at blocking or eliminating the protein.
_
Gene therapy is the treatment of human disease by gene transfer. Many, or maybe most, diseases have a genetic component — asthma, cancer, Alzheimer’s disease, for example. However, most diseases are polygenic, i.e. a subtle interplay of many genes determines the likelihood of developing a disease condition, whereas, so far, gene therapy can only be contemplated for monogenic diseases, in which there is a single gene defect. Even in these cases only treatment of recessive diseases can be considered, where the correct gene is added in the continued presence of the faulty one. Dominant mutations cannot be approached in this way, as it would be necessary to knock out the existing faulty genes in the cells where they are expressed (i.e. where their presence shows an effect), as well as adding the correct genetic information. Gene therapy for recessive monogenic diseases involves introducing correct genetic material into the patient.
_
The term gene therapy describes any procedure intended to treat or alleviate disease by genetically modifying the cells of a patient. It encompasses many different strategies and the material transferred into patient cells may be genes, gene segments or oligonucleotides. The genetic material may be transferred directly into cells within a patient (in vivo gene therapy), or cells may be removed from the patient and the genetic material inserted into them in vitro, prior to transplanting the modified cells back into the patient (ex vivo gene therapy). Because the molecular basis of diseases can vary widely, some gene therapy strategies are particularly suited to certain types of disorder, and some to others. Major disease classes include:
1. Infectious diseases (as a result of infection by a virus or bacterial pathogen);
2. Cancers (inappropriate continuation of cell division and cell proliferation as a result of activation of an oncogene or inactivation of a tumor suppressor gene or an apoptosis gene);
3. Inherited disorders (genetic deficiency of an individual gene product or genetically determined inappropriate expression of a gene);
4. Immune system disorders (includes allergies, inflammations and also autoimmune diseases, in which body cells are inappropriately destroyed by immune system cells).
A major motivation for gene therapy has been the need to develop novel treatments for diseases for which there is no effective conventional treatment. Gene therapy has the potential to treat all of the above classes of disorder. Depending on the basis of pathogenesis, different gene therapy strategies can be considered.
_
_
Diseases that can be treated by gene therapy are categorized as either genetic or acquired. Genetic diseases are those which are typically caused by the mutation or deletion of a single gene. The expression of a single gene, directly delivered to the cells by a gene delivery system can potentially eliminate a disease. Prior to gene therapy studies, there was no alternative treatment for genetic disorders. Today, it is possible to correct genetic mutation with gene therapy studies. Conversely, a single gene is not defined as the sole cause of acquired diseases. Although gene therapy was initially used to treat genetic disorders only, it is now used to treat a wide range of diseases such as cancer, peripheral vascular diseases, arthritis, neurodegenerative disorders and AIDS.
_
Humans possess two copies of most of their genes. In a recessive genetic disease, both copies of a given gene are defective. Many such illnesses are called loss-of-function genetic diseases, and they represent the most straightforward application of gene therapy: If a functional copy of the defective gene can be delivered to the correct tissue and if it makes (“expresses”) its normal protein there, the patient could be cured. Other patients suffer from dominant genetic diseases. In this case, the patient has one defective copy and one normal copy of a given gene. Some of these disorders are called gain-of-function diseases because the defective gene actively disrupts the normal functioning of their cells and tissues (some recessive diseases are also gain-of-function diseases). This defective copy would have to be removed or inactivated in order to cure these patients. Gene therapy may also be effective in treating cancer or viral infections such as HIV-AIDS. It can even be used to modify the body’s responses to injury. These approaches could be used to reduce scarring after surgery or to reduce restenosis, which is the reclosure of coronary arteries after balloon angioplasty.
_
Gene therapy has become an increasingly important topic in science- related news. The basic concept of gene therapy is to introduce a gene with the capacity to cure or prevent the progression of a disease. Gene therapy introduces a normal, functional copy of a gene into a cell in which that gene is defective. Cells, tissue, or even whole individuals (when germ-line cell therapy becomes available) modified by gene therapy are considered to be transgenic or genetically modified. Gene therapy could eventually target the correction of genetic defects, eliminate cancerous cells, prevent cardiovascular diseases, block neurological disorders, and even eliminate infectious pathogens. However, gene therapy should be distinguished from the use of genomics to discover new drugs and diagnosis techniques, although the two are related in some respects.
_
Gene therapy is a fascinating and growing research field of translational medicine. The basic biological understanding of tissue function, cellular events, metabolic processes, stem cell function, are all linked to the genetic code and to the genetic material in all species. In mammalians as in more simple creatures, each and every phenotype structural characterizations, function and probably behavior is dependent on the special nature and timing of genetic material and events. In altering the genetic material of somatic cells, gene therapy may correct the underlying specific disease pathophysiology. In some instances, it may offer the potential of a one-time cure for devastating, inherited disorders. In principle, gene therapy should be applicable to many diseases for which current therapeutic approaches are ineffective or where the prospects for effective treatment appear exceedingly low.
______
Uses of gene therapy:
Gene therapy is being used in many ways. For example, to:
1. Replace missing or defective genes;
2. Deliver genes that speed the destruction of cancer cells;
3. Supply genes that cause cancer cells to revert back to normal cells;
4. Deliver bacterial or viral genes as a form of vaccination;
5. Provide genes that promote or impede the growth of new tissue; and;
6. Deliver genes that stimulate the healing of damaged tissue.
_
A large variety of genes are now being tested for use in gene therapy. Examples include: a gene for the treatment of cystic fibrosis (a gene called CFTR that regulates chloride); genes for factors VIII and IX, deficiency of which is responsible for classic hemophilia (hemophilia A) and another form of hemophilia (hemophilia B), respectively; genes called E1A and P53 that cause cancer cells to undergo cell death or revert to normal; AC6 gene which increases the ability of the heart to contract and may help in heart failure; and VEGF, a gene that induces the growth of new blood vessels (angiogenesis) of use in blood vessel disease. A short synthetic piece of DNA (called an oligonucleotide) is being used by researchers to “pre-treat” veins used as grafts for heart bypass surgery. The piece of DNA seems to switch off certain genes in the grafted veins to prevent their cells from dividing and thereby prevent atherosclerosis.
_______
How does gene therapy work?
Scientists focus on identifying genes that affect the progression of diseases. Depending on the disease, the identified gene may be mutated so it doesn’t work. The mutation may shorten the protein, lengthen the protein, or cause it to fold into an odd shape. The mutation may also change how much protein is made (change its expression level). After identification of the relevant gene(s), scientists and clinicians choose the best current strategy to return cells to a normal state, or in the case of cancer cells, to eliminate them. Thus, one aim of gene therapy can be to provide a correct copy of its protein in sufficient quantity so that the patient’s disease improves or disappears. Five main strategies are used in gene therapy for different diseases and cancer: gene addition, gene correction, gene silencing, reprogramming, and cell elimination. In some common diseases, such as Parkinson’s disease and Alzheimer’s disease, different genes and non-genetic causes can underlie the condition. In these cases, gene/cell therapy can be directed at the symptoms, rather than the cause, such as providing growth factors or neutralizing toxic proteins.
_
1. Gene addition:
Gene addition involves inserting a new copy of the relevant gene into the nucleus of appropriate cells. The new gene has its own control signals including start and stop signals. The new gene with its control signals is usually packaged into either viral vectors or non-viral vectors. The gene-carrying vector may be administered into the affected tissue directly, into a surrogate tissue, or into the blood stream or intraperitoneal cavity. Alternatively, the gene-carrying vector can be used in tissue culture to alter some of the patients’ cells which are then re-administered into the patient. Gene therapy agents based on gene addition are being developed to treat many diseases, including adenosine deaminase severe combined immunodeficiency (ADA- SCID), alpha-antitrypsin deficiency, Batten’s disease, congenital blindness, cystic fibrosis, Gaucher’s disease, hemophilia, HIV infections, Leber’s congenital amaurosis, lysosomal storage diseases, muscular dystrophy, type I diabetes, X linked chronic granulomatous disease, and many others.
_
2. Gene correction:
Gene correction involves delivering a corrected portion of the gene with or without supplemental recombinant machinery that efficiently recombines with the defective gene in the chromosome and corrects the mutation in the genome of targeted cells. This can also be carried out by providing DNA/RNA sequences that allow the mutated portion of the messenger RNA to be spliced out and replaced with a corrected sequences or, when available in the genome, increasing expression of a normal counterpart of the defective gene which can replace its function.
_
3. Gene silencing:
Gene silencing is a technique with which geneticists can deactivate an existing gene. By turning off defective genes, the harmful effects of that gene can be prevented. This is accomplished by binding a specific strand of RNA to an existing mRNA (messenger RNA) strand. Ordinarily, when DNA replicates, the mRNA creates a copy of the DNA strand. But by binding the RNA to the mRNA, the mRNA is prevented from replicating that portion of the DNA. Therefore, specific genes can be targeted and prevented from replicating into new DNA strands. Viruses like Hepatitis and AIDS can be treated using gene silencing techniques. Gene silencing is an approach used to turn a gene “off” so that no protein is made from it. Gene-silencing approaches to gene therapy can target a gene’s DNA directly, or they can target mRNA transcripts made from the gene. Triple-helix-forming oligonucleotide gene therapy targets the DNA sequence of a mutated gene to prevent its transcription. This technique delivers short, single-stranded pieces of DNA, called oligonucleotides, that bind specifically in the groove between a gene’s two DNA strands. This binding makes a triple-helix structure that blocks the DNA from being transcribed into mRNA.
_
RNA interference takes advantage of the cell’s natural virus-killing machinery, which recognizes and destroys double-stranded RNA. This technique introduces a short piece of RNA with a nucleotide sequence that is complementary to a portion of a gene’s mRNA transcript. The short piece of RNA will find and attach to its complementary sequence, forming a double-stranded RNA molecule, which the cell then destroys.
_
Ribozyme gene therapy targets the mRNA transcripts copied from the gene. Ribozymes are RNA molecules that act as enzymes. Most often, they act as molecular scissors that cut RNA. In ribozyme gene therapy, ribozymes are designed to find and destroy mRNA encoded by the mutated gene so that no protein can be made from it.
_
MicroRNAs constitute a recently discovered class of non-coding RNAs that play key roles in the regulation of gene expression. Acting at the post-transcriptional level, these fascinating molecules may fine-tune the expression of as much as 30% of all mammalian protein-encoding genes. By changing levels of specific microRNAs in cells, one can also achieve downregulation of gene expression.
_
Short Interfering RNA:
Double stranded RNA, homologous to the gene targeted for suppression, is introduced into cells where it is cleaved into small fragments of double stranded RNA named short interfering RNAs (siRNA). These siRNAs guide the enzymatic destruction of the homologous, endogenous RNA, preventing translation to active protein. They also prime RNA polymerase to synthesis more siRNA, perpetuating the process, and resulting in persistent gene suppression. Short Interfering RNAs reduce protein production of the corresponding faulty gene. For example, too much tumor necrosis factor (TNF) alpha is often expressed in the afflicted joints of rheumatoid arthritis patients. Since the protein is needed in small amounts in the rest of the body, gene silencing aims to reduce TNF alpha only in the afflicted tissue. Another example would be oncoproteins, such as c-myc or EGFR that are upregulated or amplified in some cancers. Lowering expression of these oncoproteins in cancer cells can inhibit tumor growth.
_
Antisense therapy: a type of gene silencing:
Antisense therapy is a form of treatment for genetic disorders or infections. When the genetic sequence of a particular gene is known to be causative of a particular disease, it is possible to synthesize a strand of nucleic acid (DNA, RNA or a chemical analogue) that will bind to the messenger RNA (mRNA) produced by that gene and inactivate it, effectively turning that gene “off”. This is because mRNA has to be single stranded for it to be translated. Alternatively, the strand might be targeted to bind a splicing site on pre-mRNA and modify the exon content of an mRNA. This synthesized nucleic acid is termed an “anti-sense” oligonucleotide because its base sequence is complementary to the gene’s messenger RNA (mRNA), which is called the “sense” sequence (so that a sense segment of mRNA ” 5′-AAGGUC-3′ ” would be blocked by the anti-sense mRNA segment ” 3′-UUCCAG-5′ “). As of 2012, some 40 antisense oligonucleotides and siRNAs were in clinical trials, including over 20 in advanced clinical trials (Phase II or III). Antisense drugs are being researched to treat a variety of diseases such as cancers (including lung cancer, colorectal carcinoma, pancreatic carcinoma, malignant glioma and malignant melanoma), diabetes, Amyotrophic lateral sclerosis (ALS), Duchenne muscular dystrophy and diseases such as asthma, arthritis and pouchitis with an inflammatory component.
_
Example of antisense therapy:
Rather than replace the gene, the approach used by Ryszard Kole and colleagues at the University of North Carolina repairs the dysfunctional messenger RNA produced by the defective genes. The technique has also shown promise in treating other genetic diseases such as haemophilia A, cystic fibrosis and some cancers. Kole’s work focused on tricking the red blood cell manufacturing machinery of thalassaemic patients into producing normal haemoglobin from their mutated genes. In normal cells, DNA is transcribed into messenger RNA (mRNA), which is then translated to produce proteins such as haemoglobin. Normal copies of the beta haemoglobin gene contain three coding regions of DNA interspersed with two non-coding sequences, known as exons. These exons have to be removed before the mRNA can be translated to produce a fully functioning haemoglobin molecule. Short regions bordering the exons – known as splice sites – tell the cell where to cut and paste the mRNA. Some mutations create additional splice sites. This results in the inclusion of extra coding sequences in the mRNA, which when translated, end up producing malfunctioning haemoglobin molecules. Kole and colleagues set out to block these additional splice sites using antisense RNA. This “mirror image” sequence of RNA sticks to the aberrant splice sites. With these sites blocked, the splicing machinery focuses on the original – and correct – splice sites to produce the normal sequence of mRNA. In the team’s latest experiments, the bone marrow cells of two patients were genetically modified in vitro to produce the antisense RNA. The antisense genes were inserted into the cells’ nuclei by a modified lentivirus that had been crippled to ensure it was incapable of reproducing. In the test tube, the bone marrow cells produced about 20 to 30 per cent of a healthy person’s level of normal haemoglobin. This figure corresponds to the best available conventional treatments, bone marrow transplants or regular blood transfusions. Kole will soon seek regulatory approval to carry out human trials.
_
Short Hairpin RNA interference: another type of gene silencing:
_
_
To effectively silence specific genes in mammalian cells, Elbashu et al designed short hairpin RNA (shRNA). These sequences, which can be cloned into expression vectors and transferred to cells, result in the transcription of a double stranded RNA brought together by a hairpin loop structure. These shRNAs effectively mimic siRNA and result in specific and persistent gene suppression in mammalian cells. Multiple groups have effectively incorporated shRNA coding sequences into AAV and lentiviral vectors and demonstrated specific gene suppression in mammalian cells.
_
4. Reprogramming:
Reprogramming involves the addition of one or more genes into cells of the same tissue which causes the altered cells to have a new set of desired characteristics. For example, type I diabetes occurs because many of the islet cells of the pancreas are damaged. But the exocrine cells of the pancreas are not damaged. Several groups are deciphering which genes to add to some of the exocrine cells of the pancreas to change them into islet cells, so these modified exocrine cells make insulin and help heal type I diabetic patients. This is also the strategy in the use of induced pluripotent stem cells (iPS) where skin cells or bone marrow cells are removed from the patient and reprogrammed by transitory expression of transcription factors which turn on developmentally programmed genes, thereby steering the cells to become the specific cell types needed for cell replacement in the affected tissue.
_
5. Chimeraplasty:
It is a non- viral method that is still being researched for its potential in gene therapy. Chimeraplasty is done by changing DNA sequences in a person’s genome using a synthetic strand composed of RNA and DNA. This strand of RNA and DNA is known as a chimeraplast. The chimeraplast enters a cell and attaches itself to the target gene. The DNA of the chimeraplast and the cell complement each other except in the middle of the strand, where the chimeraplast’s sequence is different from that of the cell. The DNA repair enzymes then replace the cells DNA with that of the chimeraplast. This leaves the chimeraplast’s new sequence in the cell’s DNA and the replaced DNA sequence then decays.
_
6. Cell elimination:
Cell elimination strategies are typically used for cancer (malignant tumors) but can also be used for overgrowth of certain cell types (benign tumors). Typical strategies involve suicide genes, anti-angiogenesis agents, oncolytic viruses, toxic proteins or mounting an immune response to the unwanted cells. Suicide gene therapy involves expression of a new gene, for example an enzyme that can convert a pro-drug (non-harmful drug precursor) into an active chemotherapeutic drug. Expression of this suicide gene in the target cancer cells can only cause their death upon administration of a prodrug, and since the drug is generated within the tumor, its concentration is higher there and is lower in normal tissues, thus reducing toxicity to the rest of the body. Since tumors depend on new blood vessels to supply their ever increasing volume, both oligonucleotides and genes aimed at suppressing angiogenesis have been developed. In another approach, a number of different types of viruses have been harnessed through mutations such that they can selectively grow in and kill tumor cells (oncolysis), releasing new virus on site, while sparing normal cells. In some cases toxic proteins, such as those that produce apoptosis (death) of cells are delivered to tumor cells, typically under a promoter that limits expression to the tumor cells. Other approaches involve vaccination against tumor antigens using genetically modified cells which express the tumor antigens, activation of immune cells or facilitation of the ability of immune cells to home to tumors. Cancer therapy has been limited to some extent by the difficulty in efficient delivery of the therapeutic genes or oligonucleotides to sufficient numbers of tumor cells, which can be distributed throughout tissues and within the body. To compensate for this insufficient delivery, killing mechanisms are sought which have a “bystander effect” such that the genetically modified cells release factors that can kill non-modified tumor cells in their vicinity. Recent studies have found that certain cell types, such as neuroprecursor cells and mesenchymal cells, are naturally attracted to tumor cells, in part due to factors released by the tumor cells. These delivery cells can then be armed with latent oncolytic viruses or therapeutic genes which they can carry over substantial distances to the tumor cells.
________
Why and how gene therapy just got easier:
Some diseases, such as haemophilia and cystic fibrosis, are caused by broken genes. Doctors have long dreamed of treating them by adding working copies of these genes to cells in the relevant tissue (bone marrow and the epithelium of the lung respectively, in these two cases). This has proved hard. There have been a handful of qualified successes over the years, most recently involving attempts to restore vision to people with gene-related blindness. But this sort of gene therapy is likely to remain experimental and bespoke for a long time, as it is hard to get enough genes into enough cells in solid tissue to have a meaningful effect. Recently, though, new approaches have been devised. Some involve editing cells’ genes rather than trying to substitute them. Others create and insert novel genes—ones that do not exist in nature—and stick those into patients. Both of these techniques are being applied to cells from the immune system, which need merely to be injected into a patient’s bloodstream to work. They therefore look susceptible to being scaled up in a way that, say, inserting genes into retinal cells is not.
_
1. Gene editing:
Gene editing can be done in at least three ways.
A. The gene editing technology is called the CRISPR system, which refers to the “Clustered Regularly Interspaced Short Palindromic Repeats” that allow its action. As the name suggests, the system inserts short palindromic DNA sequences called CRISPRs that are a defining characteristic of viral DNA. Bacteria have an evolved defense that finds these CRISPRs, treating them as evidence of unwanted viral DNA. Scientists insert DNA sequences that code for this bacterial cutting enzyme, along with the healthy version of our gene of interest and some extra RNA for targeting. All scientists need do is design their sequences so CRISPRs are inserted into the genome around the diseased gene, tricking the cell into identifying it as viral — from there, the cell handles the excision all on its own, replacing the newly “viral” gene with the study’s healthy version. The whole process plays out using the cell’s own machinery. CRISPR-Cas-9 editing employs modified versions of a natural antiviral defense found in bacteria, which recognises and cuts specific sequences of DNA bases (the “letters” of the genetic code). The paper published in Nature under lead author Josiane Garneau, demonstrated how CRISPR functions as a defense mechanism against bacteriophages – the viruses that attack bacteria. CRISPR was first noticed as a peculiar pattern in bacterial DNA in the 1980s. A CRISPR sequence consists of a stretch of 20 to 50 non-coding base pairs that are nearly palindromic – reading the same forward and backward – followed by a “spacer” sequence of around 30 base pairs, followed by the same non-coding palindrome again, followed by a different spacer, and so on many times over. Researchers in the field of bacterial immunology realized that the spacers were in fact short sequences taken from the DNA of bacteriophages, and that bacteria can add new spacers when infected with new viruses, gaining immunity from those viral strains. What Garneau and her colleagues showed was the mechanism that made the system work: the spacers are transcribed into short RNA sequences, which a protein called Cas9 uses to find the same sequences in invading viruses and cut the viral DNA at the targeted site. That was a pretty interesting paper, because it showed Cas9 will cut DNA. And Cas9 uses short RNA sequences to be able to cut the DNA. Immediately, the system suggested a new method of gene editing: CRISPR-Cas9 complexes could be paired with RNA sequences that target any sites researchers were interested in cutting. In the fall of 2012, a team including Jennifer Doudna and Emmanuel Charpentier went on to show that CRISPR’s natural guiding system, which features two distinct types of RNA, could be replaced with a single sequence of artificially-produced guide RNA, or gRNA, without compromising its effectiveness. This opened up the possibility of rapid engineering, where only the gRNA sequence would have to be modified to target CRISPR to different areas of the genome. Finally, in January 2013, Zhang’s lab published a paper in Science that hit the major benchmark for gene editing: they successfully used a CRISPR-Cas9 system to modify DNA in mammalian cells, both mouse and human. As a flourish, the group encoded multiple gRNA sequences into the same CRISPR array, and showed that Cas9 cleaved out all the relevant sites of the genome. One advantage of CRISPR [is] you can use it to target multiple genes at the same time.
_
B. The other, zinc-finger nucleases, combines a protein called a zinc finger, which also recognises particular base sequences (its natural job is to lock onto bits of DNA that switch genes on and off), with an enzyme called a nuclease, which cuts DNA. Recently zinc finger nucleases (ZFNs) have been used to edit the genome with much greater precision. This technology incorporates Cys2His2 zinc fingers, a class of protein structures that bind to a specific short sequence of DNA. Combining pairs of these zinc fingers with an enzyme that cuts DNA allows researchers to choose a specific stretch of DNA to remove from the genome, and even add a second sequence to replace it. Zinc finger nucleases have the advantages of carving out disease-causing mutations, and being targeted to areas of the genome where inserting new DNA doesn’t run the risk of disrupting genes that are already there. The zinc-finger nuclease approach has just been tested in an anti-AIDS trial, where it was used to break genes for proteins that would otherwise help HIV infect immune-system cells. [Vide infra]
_
C. Gene splicing is another way of gene editing. Gene splicing involves cutting out part of the DNA in a gene and adding new DNA in its place. The process is entirely chemical with restriction enzymes used as chemical ‘scissors’. Depending on the type of restriction enzyme used, different parts of the genetic code can be targeted. A specific restriction enzyme will split apart a specific strand of DNA leaving behind a gap in the genetic code. New DNA can then be added in this gap. When a new strand of DNA is added, it takes the place of the binds to the ends of the DNA strands that were originally cut. Another enzyme called ligase is used in the repair process. Once the new DNA is in place, the function of the gene changes. In cases where a defective gene is repaired, the new gene will begin functioning correctly, producing the appropriate enzymes for its type. The term SMaRT™ stands for “Spliceosome-Mediated RNA Trans-splicing.” This technique targets and repairs the messenger RNA (mRNA) transcripts copied from the mutated gene. Rather than attempting to replace the entire gene, this technique repairs just the section of the mRNA transcript that contains the mutation. Several different viral vectors have been developed to repair mutations directly in the DNA. This gene editing technique uses enzymes designed to target specific DNA sequences. The enzymes cut out the faulty sequence and replace it with a functional copy.
_
2. Insert novel gene:
Making and inserting new genes is also being employed to affect the immune system—in this case to boost its ability to clear up cancer. So-called chimeric antigen receptor (CAR) cells are immune cells with an added gene that both recognises particular cancer cells and activates the immune cell they are in when it has locked onto its target. Cells with appropriate CARs thus become guided anticancer missiles. Researchers have focused on modifying immune-system cells because these are easy to extract from a patient’s bloodstream. They can be tweaked, multiplied in culture, and returned to the patient’s body without much difficulty. And, because they came from him in the first place, they do not, themselves, risk provoking an immune reaction. So, though it is still early days, it looks as though these sorts of gene therapy might eventually become mainstream.
_
Therapeutic gene modulation:
Therapeutic gene modulation refers to the practice of altering the expression of a gene at one of various stages, with a view to alleviate some form of ailment. It differs from gene therapy in that gene modulation seeks to alter the expression of an endogenous gene (perhaps through the introduction of a gene encoding a novel modulatory protein) whereas gene therapy concerns the introduction of a gene whose product aids the recipient directly. Modulation of gene expression can be mediated at the level of transcription by DNA-binding agents (which may be artificial transcription factors), small molecules, or synthetic oligonucleotides. It may also be mediated post-transcriptionally through RNA interference.
_
Other gene therapy techniques:
Another approach to gene therapy is to modify gene expression chemically (e.g., by modifying DNA methylation). Such methods have been tried experimentally in treating cancer. Chemical modification may also affect genomic imprinting, although this effect is not clear. Gene therapy is also being studied experimentally in transplantation surgery. Altering the genes of the transplanted organs to make them more compatible with the recipient’s genes makes rejection (and thus the need for immunosuppressive drugs) less likely. However, this process works only rarely.
_______
Gene therapy requirements:
Conditions or disorders that result from mutations in a single gene are potentially the best candidates for gene therapy. However, the many challenges met by researchers working on gene therapy mean that its application is still limited while the procedure is being perfected. Before gene therapy can be used to treat a certain genetic condition or disorder, certain requirements need to be met:
- The faulty gene must be identified and some information about how it results in the condition or disorder must be known so that the vector can be genetically altered for use and the appropriate cell or tissue can be targeted.
- The gene must also be cloned so that it can be inserted into the vector.
- Once the gene is transferred into the new cell, its expression (whether it is turned on or off) needs to be controlled.
- There must be sufficient value in treating the condition or disorder with gene therapy – that is, is there a simpler way to treat it?
- The balance of the risks and benefits of gene therapy for the condition or disorder must compare favourable to other available therapies.
- Sufficient data from cell and animal experiments are needed to show that the procedure itself works and is safe.
- Once the above are met, researchers may be given permission to start clinical trials of the procedure, which is closely monitored by institutional review boards and governmental agencies for safety.
_______
Pharmacogenomics:
Pharmacogenomics is the science of how genetic characteristics affect the response to drugs. One aspect of pharmacogenomics is how genes affect pharmacokinetics. Genetic characteristics of a person may help predict response to treatments. For example, metabolism of warfarin is determined partly by variants in genes for the CYP2C9 enzyme and for the vitamin K epoxide reductase complex protein 1. Genetic variations (e.g., in production of UDP [uridine diphosphate]-glucoronosyltransferase 1A1) also help predict whether the anticancer drug will have intolerable adverse effects. Another aspect of pharmacogenomics is pharmacodynamics (how drugs interact with cell receptor). Genetic and thus receptor characteristics of disordered tissue can help provide more precise targets when developing drugs (e.g., anticancer drugs). For example, trastuzumab can target specific cancer cell receptors in metastatic breast cancers that amplify the HER2/neu gene. Presence of the Philadelphia chromosome in patients with chronic myelogenous leukemia (CML) helps guide chemotherapy. So genes affect response to drugs in disease, and if these genes can be altered by gene therapy, the response to drugs can dramatically change. You may need very small amount of drug to get desired therapeutic response thereby reducing side effects of drugs.
______
Process of Gene Therapy:
The process of gene therapy remains complex and many techniques need further developments. The challenge of developing successful gene therapy for any specific condition is considerable. The condition in question must be well understood, the undying faulty gene must be identified and a working copy of the gene involved must be available. Specific cells in the body requiring treatment must be identified and are accessible. A means of efficiently delivering working copies of the gene to the cells must be available. Moreover diseases and their strict genetic link need to be understood thoroughly.
_
Techniques of Genetic Alteration:
Two problems must be confronted when changing genes. The first is what kind of change to make to the gene. The second is how to incorporate that change in all the other cells that are must be changed to achieve a desired effect. There are several options for what kind of change to make to the gene. DNA in the gene could be replaced by other DNA from outside (called “homologous replacement). Or the gene could be forced to mutate (change structure – “selective reverse mutation.”) Or a gene could just be added. Or one could use a chemical to simply turn off a gene and prevent it from acting. There are also several options for how to spread the genetic change to all the cells that need to be changed. If the altered cell is a reproductive cell, then a few such cells could be changed and the change would reach the other somatic cells as those somatic cells were created as the organism develops. But if the change were made to a somatic cell, changing all the other relevant somatic cells individually like the first would be impractical due to the sheer number of such cells. The cells of a major organ such as the heart or liver are too numerous to change one-by-one. Instead, to reach such somatic cells a common approach is to use a carrier, or vector, which is a molecule or organism. A virus, for example, could be used as a vector. The virus would be an innocuous one or changed so as not to cause disease. It would be injected with the genetic material and then as it reproduces and “infects” the target cells it would introduce the new genetic material. It would need to be a very specific virus that would infect heart cells, for instance, without infecting and changing all the other cells of the body. Fat particles and chemicals have also been used as vectors because they can penetrate the cell membrane and move into the cell nucleus with the new genetic material.
_
Somatic Cells and Reproductive Cells:
Two fundamental kinds of cell are somatic cells and reproductive cells. Most of the cells in our bodies are somatic – cells that make up organs like skin, liver, heart, lungs, etc., and these cells vary from one another. Changing the genetic material in these cells is not passed along to a person’s offspring. Reproductive cells are sperm cells, egg cells, and cells from very early embryos. Changes in the genetic make-up of reproductive cells would be passed along to the person’s offspring. Those reproductive cell changes could result in different genetics in the offspring’s somatic cells than otherwise would have occurred because the genetic makeup of somatic cells is directly linked to that of the germ cells from which they are derived.
_
Types of gene therapy:
There are 2 types of gene therapy.
1. Germ line gene therapy: where germ cells (sperm or egg) are modified by the introduction of functional genes, which are integrated into their genome. Therefore changes due to therapy would be heritable and would be passed on to later generation. Theoretically, this approach should be highly effective in counteracting genetic disease and hereditary disorders. But at present many jurisdictions, a variety of technical difficulties and ethical reasons make it unlikely that germ line therapy would be tried in human beings in near future.
2. Somatic gene therapy: where therapeutic genes are transferred into the somatic cells of a patient. Any modifications and effects will be restricted to the individual patient only and will not be inherited by the patients offspring or any later generation.
_
_
Germline gene therapy:
In germline gene therapy, germ cells (sperm or eggs) are modified by the introduction of functional genes, which are integrated into their genomes. Germ cells will combine to form a zygote which will divide to produce all the other cells in an organism and therefore if a germ cell is genetically modified then all the cells in the organism will contain the modified gene. This would allow the therapy to be heritable and passed on to later generations. Although this should, in theory, be highly effective in counteracting genetic disorders and hereditary diseases, some jurisdictions, including Australia, Canada, Germany, Israel, Switzerland, and the Netherlands prohibit this for application in human beings, at least for the present, for technical and ethical reasons, including insufficient knowledge about possible risks to future generations and higher risk than somatic gene therapy (e.g. using non-integrative vectors). The USA has no federal legislation specifically addressing human germ-line or somatic genetic modification (beyond the FDA testing regulations for therapies in general).
_
Advantages of germ-line cell gene therapy are the following:
1. It offers the possibility for a true cure of several diseases and it is not only a temporary solution.
2. It might be the only way to treat some genetic diseases.
3. The benefits would be extended for several generations, because genetic defects are eliminated in the individual’s genome and, consequently, the benefits would be passed to his or her offspring.
Some of the arguments presented against germ-line cell gene therapy are the following:
1. It involves many steps that are poorly understood, and the long-term results cannot be estimated.
2. It would open the door for genetic modifications in human traits with profound social and ethical implications.
3. It is very expensive and it would not benefit the common citizen.
4. The extension of the cure to a person’s offspring would be possible only if the defective gene was directly modified, but probably not if a new gene was added to another part of the genome.
_
Somatic cell gene therapy:
Somatic gene therapy involves the insertion of genes into diploid cells of an individual where the genetic material is not passed on to its progeny. Somatic cell therapy is viewed as a more conservative, safer approach because it affects only the targeted cells in the patient, and is not passed on to future generations; however, somatic cell therapy is short-lived because the cells of most tissues ultimately die and are replaced by new cells. In addition, transporting the gene to the target cells or tissue is also problematic. Regardless of these difficulties, however, somatic cell gene therapy is appropriate and acceptable for many disorders. Somatic gene therapy is the transfer of genes into the somatic cells of the patient, such as cells of the bone marrow, and hence the new DNA does not enter the eggs or sperm. The genes transferred are usually normal alleles that could ‘correct’ the mutant or disease alleles of the recipient. The technique of somatic gene therapy involves inserting a normal gene into the appropriate cells of an individual affected with a genetic disease, thereby permanently correcting the disorder. The simplest methods of getting genes into the person’s cells are either using viruses (which carry the human gene, in place of one of their own genes, into a cell) or liposomes (small fat-like molecules which can carry DNA into a cell). In some cells, the gene or genes become inserted into a chromosome in the nucleus. The target cells might be bone marrow cells, which are easily isolated and re-implanted. Bone marrow cells continue to divide for a person’s whole life to produce blood cells, so this approach is useful only if the gene you want to deliver has a biological role in the blood. Delivery of a gene that has a biological role in, say, the lungs, muscle, or liver would have to occur within those target organs. In many cases, accessing the appropriate tissue or, if the gene is required in multiple tissues (e.g. muscles throughout the body) ensuring it can be delivered where it is needed, is a major problem.
_
There are three major scientific hurdles that have to be overcome before somatic gene therapy is likely to work. The first is getting the human gene into the patient’s cells (using viruses or liposomes). Adverse results in a UK/French gene therapy trial in 2002, including the death of one patient, highlighted some of the risks of using viruses. Following a safety review, the trial resumed because of the severity of the disease, and by the end of 2004, 17 out of 18 patients treated had experienced some improvements in their condition, with four experiencing significant improvements. Unfortunately, in early 2005 the trial had to stop again when a patient suffered an adverse reaction. Clearly, there is still some way to go with respect to safety of the techniques. The second obstacle is getting the gene into the right cells. For example, for sickle cell disease (caused by defective haemoglobin in red blood cells), the cells to choose would be the patient’s bone marrow cells. For cystic fibrosis, application in the lungs and gut would be needed. The lungs might be accessible via an aerosol spray. Treating the gut would need some way to deliver genes in a package that the patient would swallow, and which would protect them from digestive enzymes until they could act. The final obstacle is making sure the gene is active, that is, switched on in the cell to produce the protein that the patient needs. This means it must be under the control of the sequence of DNA that is responsible for switching the gene on. The results do not have to be perfect to produce benefits. In cystic fibrosis, animal tests have shown that if the normal gene can be transferred to only five per cent of cells in the lungs, this restores some normal function. The prospects for somatic therapy for single-gene diseases are still improving.
__
Somatic gene therapy represents the mainstream line of current basic and clinical research, where the therapeutic DNA transgene (either integrated in the genome or as an external episome or plasmid) is used to treat a disease in an individual. Several somatic cell gene transfer experiments are currently in clinical trials with varied success. Over 600 clinical trials utilizing somatic cell therapy are underway in the United States. Most of these trials focus on treating severe genetic disorders, including immunodeficiencies, haemophilia, thalassaemia, and cystic fibrosis. These disorders are good candidates for somatic cell therapy because they are caused by single gene defects. While somatic cell therapy is promising for treatment, a complete correction of a genetic disorder or the replacement of multiple genes in somatic cells is not yet possible. Only a few of the many clinical trials are in the advanced stages.
________
The Two Paths to Gene Therapy: Direct or cell based:
_
_
Direct gene transfer:
Gene therapy can be performed either by direct transfer of genes into the patient or by using living cells as vehicles to transport the genes of interest. Both modes have certain advantages and disadvantages. Direct gene transfer is particularly attractive because of its relative simplicity. In this scenario, genes are delivered directly into a patient’s tissues or bloodstream by packaging into liposomes (spherical vessels composed of the molecules that form the membranes of cells) or other biological microparticles. Alternately, the genes are packaged into genetically-engineered viruses, such as retroviruses or adenoviruses. Because of biosafety concerns, the viruses are typically altered so that they are not toxic or infectious (that is, they are replication incompetent). These basic tools of gene therapists have been extensively optimized over the past 10 years. However, their biggest strength—simplicity—is simultaneously their biggest weakness. In many cases, direct gene transfer does not allow very sophisticated control over the therapeutic gene. This is because the transferred gene either randomly integrates into the patient’s chromosomes or persists unintegrated for a relatively short period of time in the targeted tissue. Additionally, the targeted organ or tissue is not always easily accessible for direct application of the therapeutic gene.
_
Cell based gene therapy:
On the other hand, therapeutic genes can be delivered using living cells. This procedure is relatively complex in comparison to direct gene transfer, and can be divided into three major steps. In the first step, cells from the patient or other sources are isolated and propagated in the laboratory. Second, the therapeutic gene is introduced into these cells, applying methods similar to those used in direct gene transfer. Finally, the genetically-modified cells are returned to the patient. The use of cells as gene transfer vehicles has certain advantages. In the laboratory dish (in vitro), cells can be manipulated much more precisely than in the body (in vivo). Some of the cell types that continue to divide under laboratory conditions may be expanded significantly before reintroduction into the patient. Moreover, some cell types are able to localize to particular regions of the human body, such as hematopoietic (blood-forming) stem cells, which return to the bone marrow. This ‘homing’ phenomenon may be useful for applying the therapeutic gene with regional specificity. A major disadvantage, however, is the additional biological complexity brought into systems by living cells. Isolation of a specific cell type requires not only extensive knowledge of biological markers, but also insight into the requirements for that cell type to stay alive in vitro and continue to divide. Unfortunately, specific biological markers are not known for many cell types, and the majority of normal human cells cannot be maintained for long periods of time in vitro without acquiring deleterious mutations. Another major limitation of using adult stem cells is that it is relatively difficult to maintain the stem cell state during ex vivo manipulations. Under current suboptimal conditions, adult stem cells tend to lose their stem cell properties and become more specialized, giving rise to mature cell types through a process termed differentiation. Recent advances in supportive culture conditions for mouse hematopoietic stem cells may ultimately facilitate more effective use of human hematopoietic stem cells in gene therapy applications.
_
Remember, ex-vivo gene therapy is always cell based.
_
Adult stem cells vs. primary cells for somatic cell gene therapy:
Adult stem cells have become a viable option for gene transfer over the past decade and are similar to primary cell cultures. However, adult stem cells offer the potential to completely incorporate into any host tissue and transform into a mature cell of that organ. This ability ensures long term survival of grafted cells, which function in concert with the resident cells of that organ system. Peripheral derived haematopoietic stem cells are of particular interest as a potential surrogate cell. The plasticity of this cell type has been widely reported; bone marrow derived glial cells have been identified in focal ischaemic rat brain, and bone marrow derived myocardial cells have been identified in rat models of cardiac ischaemia. This underlines the major advantage of stem cells over primary cells; the possibility that these cells could be used not only to carry therapeutic proteins, but also to repopulate organs with damaged or depleted cell numbers. Haemopoietic stem cells are easily obtained through basic peripheral intravenous access systems, allowing for marrow derived stem cells to be harvested systemically, modified in vitro, and under the correct circumstances re-infused into the peripheral blood with subsequent homing to damaged target tissue such as brain or myocardium. Bone marrow derived stem cell use has been limited by low viral transfection efficiency and technical difficulties in isolating, culturing, and maintaining these cells. Other adult stem cells include hepatocytes, which have been obtained through partial liver transections, and have been isolated, manipulated in culture, and then re-infused into autologous liver. CNS stem cells have also been isolated but are not available for autologous transplant owing to the inaccessibility of these cells in the periventricular zone of the CNS. Most studies have used cadaver derived cells. Finally, fetal derived stem cells have been the topic of much scientific and media speculation. Fetal cell transplantation has been successful in multiple animal models of disease, and transfer of unmodified fetal cells has already been undertaken in Parkinson’s disease. Patients with Parkinson’s disease receiving fetal dopaminergic neurones have demonstrated clinically significant long term benefits. However, several patients obtained no benefit from the transplant and several developed worsening of symptoms. Similarly, transplantation of human fetal striatal tissue to patients with Huntington’s disease has been undertaken. Results indicate that grafts derived from human fetal striatal tissue can survive regardless of the ongoing endogenous neurodegenerative process; however, the clinical benefit is unproven. Finally, fetal islet cells have been transplanted to patients with diabetes mellitus with variable success. In some cases the transplant has obviated the need for exogenous administration of insulin. The fact that fetal cells can be maintained in culture, have some degree of plasticity, and can be transfected using classical methods make this cell type attractive. However, fetal derived primary cell cultures are often heterogeneous and difficult to define and purify. The success of graft survival appears to be related to the manner in which cells are prepared, purified, and transplanted, but the factors predicting a successful clinical response to graft transplantation are unclear. Further, fetal tissue is not readily accessible and continues to be part of a wider moral and ethical debate.
_
Why Stem Cells are used in some cell-based Gene Therapies:
To date, about 40 percent of the more than 450 gene therapy clinical trials conducted in the United States have been cell-based. Of these, approximately 30 percent have used human stem cells—specifically, blood-forming, or hematopoietic, stem cells (HSC)—as the means for delivering transgenes into patients. Several of the early gene therapy studies using these stem cells were carried out not for therapeutic purposes per se, but to track the cells’ fate after they were infused back into the patient. The studies aimed to determine where the stem cells ended up and whether they were indeed producing the desired gene product, and if so, in what quantities and for what length of time. Of the stem cell-based gene therapy trials that have had a therapeutic goal, approximately one-third have focused on cancers (e.g., ovarian, brain, breast, myeloma, leukemia, and lymphoma), one-third on human immunodeficiency virus disease (HIV-1), and one-third on so-called single-gene diseases (e.g., Gaucher’s disease, severe combined immune deficiency (SCID), Fanconi anemia, Fabry disease, and leukocyte adherence deficiency). But why use stem cells for this method of gene therapy, and why hematopoietic stem cells in particular? The major reason for using stem cells in cell-based gene therapies is that they are a self-renewing population of cells and thus may reduce or eliminate the need for repeated administrations of the gene therapy. Since the advent of gene therapy research, hematopoietic stem cells have been a delivery cell of choice for several reasons. First, although small in number, they are readily removed from the body via the circulating blood or bone marrow of adults or the umbilical cord blood of newborn infants. In addition, they are easily identified and manipulated in the laboratory and can be returned to patients relatively easily by injection. The ability of hematopoietic stem cells to give rise to many different types of blood cells means that once the engineered stem cells differentiate, the therapeutic transgene will reside in cells such as T and B lymphocytes, natural killer cells, monocytes, macrophages, granulocytes, eosinophils, basophils, and megakaryocytes. The clinical applications of hematopoietic stem cell-based gene therapies are thus also diverse, extending to organ transplantation, blood and bone marrow disorders, and immune system disorders. In addition, hematopoietic stem cells “home,” or migrate, to a number of different spots in the body—primarily the bone marrow, but also the liver, spleen, and lymph nodes. These may be strategic locations for localized delivery of therapeutic agents for disorders unrelated to the blood system, such as liver diseases and metabolic disorders such as Gaucher’s disease. The only type of human stem cell used in gene therapy trials so far is the hematopoietic stem cell (HSC). However, several other types of stem cells are being studied as gene-delivery-vehicle candidates. They include muscle-forming stem cells known as myoblasts, bone-forming stem cells called osteoblasts, and neural stem cells.
_
The genetic modification of HSCs generates special concerns:
1. These cells are long-lived and might represent a reservoir for the accumulation of proto-oncogenic lesions.
2. Current technology requires that HSCs have to be enriched and cultured in vitro to become accessible to genetic manipulation.
3. This also implies that the engineered graft represents only a small fraction (probably about 1%-10%) of the hematopoietic cell pool of a healthy individual. Infused cells may therefore be altered not only in terms of quality, but will also be heavily diluted by unmodified counterparts residing in the body. This may result in the establishment of a “strange drop in the blood,” which could correct diseases only if it were strongly enriched in vivo.
4. Therefore, achieving targeted amplification or preferential survival of engineered cells is one important key to success in hematopoietic gene therapy. However, clonal expansion, while limited by cellular senescence and exhaustion, has also been suggested as a risk factor contributing to cellular transformation, at least when occurring under nonphysiologic conditions of growth.
5. HSCs, or at least the cell preparations enriched for HSCs, may not only reconstitute the entire myeloerythroid and lymphoid spectrum, but they may also differentiate into or fuse with other cell types, including endothelial; skeletal and heart muscle cells; hepatocytes; neurons; and epithelial of gut and lungs. However, the frequency of such events is controversial. The developmental potential of HSCs generates a huge repertoire of conceivable biologic conditions and anatomic sites where side effects may manifest. However, the likelihood of manifestations outside the hematopoietic system appears to be relatively low unless special triggers exist that drive fate-switching.
6. Because of the high proliferative potential of HSCs, stable, heritable gene transfer is required for successful genetic modification. In the current “state-of-the-art” only viral vectors on the basis of retroviruses (including lentiviruses) mediate a predictable efficiency of stable transgene insertion with a predefined copy number. Chromosomal insertion guarantees transgene maintenance during clonal amplification. Episomally persisting viral vector systems such as those based on Epstein-Barr virus are still suboptimal because efficient gene transfer into HSCs is either not yet available or maintenance and expression of transgene copies are insufficiently investigated. Physicochemical methods result in a low probability for stable transgene insertion (< 10). Their efficiency may be increased when combined with endonucleases from retrotransposons or site-specific integrases. Adeno-associated viruses (AAVs) also have a low and variable rate of stable insertion. Recent advances in adenoviral vector technology may increase their potential for stable gene delivery. However, the utility of all of these alternative methods for transduction of HSCs with a defined and persisting transgene copy number is still unknown, as is the genetic risk associated with transgene insertion through these modalities.
7. The use of retroviral (including lentiviral) vectors implies that engineered cells of the same graft will vary with respect to transgene insertion sites (which are unpredictable and can affect both transgene and cellular gene expression), copy number per cell (which can be controlled more easily, but not entirely), and sequence (which can be modified in the error-prone process of reverse transcription). This produces a mixed chimerism of genetic modification in different stem cell clones, each with a theoretically distinct potential for eliciting side effects.
_
Skin cell to stem cell to liver cell with transplanted gene:
Alpha-1 Antitrypsin Deficiency (Alpha-1) can cause liver problems in infants, children or adults – as well as the better-known adult lung disease. In people with Alpha-1 (Alphas), large amounts of abnormal alpha-1 antitrypsin protein (AAT) are made in the liver; nearly 85 percent of this protein gets stuck in the liver. If the liver cannot break down the abnormal protein, the liver gradually gets damaged, scarred and cirrhotic. Scientists, at the Wellcome Trust Sanger Institute and the University of Cambridge, were working on this cirrhotic liver disease. At the moment, stem cells created from a patient with a genetic illness cannot be used to cure the disease as those cells would also contain the corrupted genetic code. The research group took a skin cell from a patient and converted it to a stem cell. A molecular scalpel was used to cut out the single mutation and insert the right letter – correcting the genetic fault. The stem cells were then turned into liver cells. One of the lead researchers, Prof David Lomas, said: “They functioned beautifully with normal secretion and function”. When the cells were placed into mice, they were still working correctly six weeks later. Further animal studies and human clinical trials would be needed before any treatment as “the key thing is safety”. For example, concerns have been raised about “induced” stem cells being prone to expressing cancer causing genes.
_
Human Embryonic Stem Cells and Gene Therapy:
Embryonic stem cells are pluripotent cells derived from the early embryo that are characterized by the ability to proliferate over prolonged periods of culture while remaining undifferentiated and maintaining a stable karyotype, but with the potential to differentiate into derivatives of all three germ layers. Human embryonic stem cells (hESCs) were first derived from the inner cell mass (ICM) of the blastocyst stage (100–200 cells) of embryos generated by in vitro fertilization, but methods have been developed to derive hESCs from the late morula stage (30–40 cells) and, recently, from arrested embryos (16–24 cells incapable of further development) and single blastomeres isolated from 8-cell embryos. The ability to culture hESCs and the potential of hESCs to differentiate into derivatives of all three germ layers provide valuable tools for studying early human embryonic development and cell differentiation and for developing in vitro culture models of human genetic disorders. Because hESCs have the potential to differentiate into normal tissues of all types, the ability to derive and maintain hESCs in culture has captured the imagination of scientists and the lay public in terms of the possibility of having an unlimited supply of normal differentiated cells to engineer diseased tissues to regain normal function. Although this is exciting in theory, there are significant hurdles to translating the ability to culture and differentiate hESCs in vitro into the generation in a reproducible fashion of normal, functional human tissue that could be safely used to treat human disease. Independent of the ethical and political controversies surrounding the generation and use of hESCs, there is only a rudimentary knowledge of the complex biological signals required to differentiate hESCs into the specific cell types required for normal organ function. At present, most studies demonstrating hESC differentiation into specific cell lineages use feeder layers of heterologous (often xenogenic) cells to maintain hESCs in culture and specific lineage-relevant protein mediators to maintain hESCs in culture and to signal the hESCs to differentiate into specific cell types. Little attention has been paid to ensuring that, after transplantation into the recipient, the hESCs and their progeny could be exogenously controlled if they differentiated into malignant cells or if they otherwise grew and/or functioned in an unwanted fashion. Finally, if hESCs are to be useful in generating normal tissues for the treatment of human disease, the tissues to be transplanted must be compatible with the host such that the cells derived from the hESCs will not be recognized as “foreign” and rejected as would any transplanted tissue from an unrelated donor. For hESCs to be useful for therapy, technologies must be developed to provide them with the specific signals required to differentiate in a controlled fashion, to regulate and/or shut down the growth of hESCs and their progeny once they have been transferred to the recipient, and to circumvent the host rejection of transplanted, non-autologous hESC-derived cells. Although gene transfer is not a solution to all of the hurdles of moving hESCs to the clinic, the technology of gene therapy represents a delivery system for biological signals that addresses many of these challenges.
____________
Gene delivery:
In most gene therapy studies, a normal gene is inserted into the genome to replace an abnormal, disease causing gene. Of all challenges, the one that is most difficult is the problem of gene delivery i.e. how to get the new or replacement gene into the patient’s target cells. So a carrier molecule called vector must be used for the above purpose. The ideal gene delivery vector should be very specific, capable of efficiently delivering one or more genes of the size needed for clinical application, unrecognized by the immune system and be purified in large quantities at high concentration. Once the vector is inserted into the patient, it should not induce an allergic reaction or inflammation. It should be safe not only for the patient but also for the environment. Finally a vector should be able to express the gene for as long as is required, generally the life of the patient.
_
Ex-vivo and in-vivo gene delivery:
Two techniques have been used to deliver vectors i.e. ex-vivo and in-vivo. The former is the commonest method, which uses extracted cells from the patient. First, the normal genes are cloned into the vector. Next, the cells with defective genes are removed from the patient and are mixed with genetically engineered vector. Finally the transfected cells are reinfused in the patient to produce protein needed to fight the disease. On the contrary, the latter technique does not use cells from the patient’s body. Vectors with the normal gene are injected into patient’s blood stream or target organs to seek out and bind with target cell. Although the ex vivo gene transfer offers more efficient gene transduction and easier propagation for generating higher cell doses, it has the obvious disadvantages of being patient-specific as a result of immunogenicity and more costly because cell culture manipulation adds manufacturing and quality control difficulties. On the contrary, the in vivo approach involves direct administration of gene transfer vector to patients. It is therefore not patient specific and potentially less costly.
_
_
Ex vivo gene delivery:
Where the patient’s cells are cultured in the laboratory, the new genes are infused in to the cells and genetically modified cells are administered back to the patient.
_
In vivo gene delivery:
_
In situ gene delivery:
The administration of the genetic material directly into the target tissue is in situ delivery. I would classify in-situ gene delivery as a type of in-vivo gene delivery.
_
Ex vivo and in vivo gene therapy have distinct advantages and disadvantages.
_
The advantages of in vivo gene therapy include the following:
1) Simplicity: gene delivery is accomplished by the single step of direct vector injection into the desired target organ, as opposed to the considerable cell processing necessary to perform ex vivo gene therapy. Deactivated adenovirus, adenoassociated virus, herpes virus, and lentivirus have been used successfully to deliver genes of interest in experimental animal models.
2) Minimal invasiveness: injections of in vivo vectors deliver several microliters of vector particles in an injection fluid solution, a procedure that is simple and safe.
3) Repeatability: the same location can be injected more than once using in vivo gene delivery approaches.
There are also, however, relative potential disadvantages of in vivo gene therapy including the following.
1) Nonspecificity of target cell infection: many different cell types can be infected when in vivo vectors are injected in the CNS, including neurons, glia, and vascular cells.
2) Toxicity: some in vivo vectors are toxic to host cells (for example, herpes virus and rabies virus) and elicit immune responses (such as adenovirus). Lentiviral and adenoassociated viral vector systems have not shown adverse effects, and newer-generation herpes virus and “gutless” adenoviruses without deleterious properties are being developed.
_
The relative advantages of ex vivo gene delivery include the following.
1) It has the ability to target selectively specific cell types for production of the gene of interest before engrafting of cells into the host brain.
2) Immunocompatability: host cells are obtained via biopsy sampling, grown in vitro, genetically modified, and then implanted into the same host. Thus, no foreign cells are introduced, eliminating any need for immunosuppression.
3) Safety: because infectious virus particles are not made by genetically modified host cells in vitro, there is little risk of inadvertently introducing wild-type virus into a host with ex vivo gene therapy, and little risk of recombination of the vector with wild-type viruses that may exist in the host body.
The potential disadvantages of ex vivo gene delivery include the following.
1) To be maintained and genetically modified in vitro, host cells must be capable of dividing, thus certain postmitotic cell populations such as neurons cannot be targets of transduction for ex vivo gene therapy. Current ex vivo gene therapy approaches target primary fibroblasts, stem cells, tumor cells, Schwann cells, or endothelial cells.
2) Invasiveness: grafting of cells is an intrinsically more invasive process than injection of suspensions of in vivo gene therapy vectors.
3) Although tumor formation has not been observed with more than 200 grafts of primary fibroblasts into the primate CNS, delivery of dividing cells bears the risk of tumor formation. Tumors have been observed when grafting immortalized cell lines; however, more recent derived conditionally immortalized cell lines do not form tumors when grafted.
_
Advantage of ex-vivo over in-vivo:
Gene therapy using genetically modified cells offers several unique advantages over direct gene transfer into the body and over cell therapy, which involves administration of cells that have not been genetically modified. First, the addition of the therapeutic transgene to the delivery cells takes place outside the patient, which allows researchers an important measure of control because they can select and work only with those cells that both contain the transgene and produce the therapeutic agent in sufficient quantity. Second, investigators can genetically engineer, or “program,” the cells’ level and rate of production of the therapeutic agent. Cells can be programmed to steadily churn out a given amount of the therapeutic product. In some cases, it is desirable to program the cells to make large amounts of the therapeutic agent so that the chances that sufficient quantities are secreted and reach the diseased tissue in the patient are high. In other cases, it may be desirable to program the cells to produce the therapeutic agent in a regulated fashion. In this case, the therapeutic transgene would be active only in response to certain signals, such as drugs administered to the patient to turn the therapeutic transgene on and off. Ex vivo approaches are less likely to trigger an immune response, because no viruses are put into patients. They also allow researchers to make sure the cells are functioning properly before they’re put in the patient. Several gene therapy successes use ex vivo gene delivery as an alternative to bone marrow transplants. Bone marrow contains stem cells that give rise to many types of blood cells. Bone marrow transplants are used to treat many genetic disorders, especially those that involve malfunctioning blood cells. Ideally, a “matched” donor, often a relative, donates bone marrow to the patient. The match decreases the chances that the patient’s immune system will reject the donor cells. However, it’s not always possible to find a match. In these cases, the patient’s own bone marrow cells can be removed and the faulty gene corrected with gene therapy. The corrected cells can then be returned to the patient.
_
The table below shows that ex-vivo gene delivery via retrovirus and adeno-associated virus (AAV) gives most stable gene expression:
_________
Surrogate cells:
Surrogate cells are cells that have been genetically manipulated to act like target cells; and in healthy individuals, these surrogate cells would not be producing desired protein naturally. Surrogate cells are those cells that receive gene transfer in ex-vivo gene delivery and work as a delivery vehicles for therapeutic genetic material to function similar to target cells. In order to exploit ex-vivo method successfully, an appropriate surrogate cell population must be identified. This cell population should be endowed with specific characteristics that fulfill several criteria. The cells should: (1) be readily available and relatively easily obtained; (2) be able to survive for long periods of time in vivo; (3) be able to express a transgene at high levels for extended durations; and (4) and not elicit a host mediated immune reaction. The advantages of using an ex vivo approach include the ability to fully characterise the modified cell population before transplantation, the ability to subclone cells and produce monoclonal populations that produce high levels of therapeutic protein, and the ability to screen populations and exclude the presence of helper viruses, transformational events, or other deleterious properties obtained after or during the modification process. Furthermore, viral vectors of low transfection efficiency can be used, because uninfected cells can be selected out of the transplant population.
_
_
Multiple surrogate cells have been proposed as delivery vehicles for therapeutic genetic material as seen in the table above. Currently, autologous primary cell cultures remain the most attractive candidate for surrogate cell delivery systems, and many experiments have demonstrated the usefulness of this cell type. Primary, adult astrocytes have been harvested and modified in vitro and have demonstrated the ability to effectively transfer genetically material to the central nervous system (CNS) for extended time periods. Primary fibroblasts are an alluring surrogate cell because they can proliferate in culture, yet remain contact inhibited and non-transformed, even after multiple passages in vitro. Furthermore, these cells can be easily harvested from the host, allowing for autologous cell transplantation. Many studies have demonstrated the utility of using primary fibroblasts for gene transfer, and a current clinic trial is underway using these cells in an ex vivo strategy to treat Alzheimer’s disease. The advantage of using primary, autologous cell cultures include the lack of antigenicity and decreased risk of malignant transformation relative to immortalised cell lines. Disadvantages include difficulty in harvesting some types of primary cells, maintaining them in culture, and effectively expressing transgenes through current transfection techniques. Another complication arises when primary cells are transferred to non-host tissue; for example, primary fibroblasts transplanted to the CNS will often produce collagen and other skin appropriate products that interfere with normal CNS functioning. This problem may be overcome with the use of stem cells.
_______
Target cells:
Target cells are those cells in human body that receive gene transfer/alteration to achieve desired therapeutic effects; and in healthy individuals, these target cells would be producing desired protein naturally.
_
_
Summary of the gene delivery procedure:
1. Isolate the healthy gene along with its regulatory sequence to control its expression
2. Incorporate this gene on to a vector or carrier as an expression cassette
3. Deliver the vector to the target cells.
_
Do not confuse between surrogate cells and target cells.
Target cells are those cells in human body that receive gene transfer/alteration to achieve desired therapeutic effects; and in healthy individuals, these target cells would be producing desired protein naturally. Surrogate cells are cells that have been genetically manipulated to act like target cells; and in healthy individuals, these surrogate cells would not be producing desired protein naturally. In mammals, insulin is synthesized in the pancreas within the β-cells of the islets of Langerhans. These β-cells are target cells for gene therapy of diabetes mellitus by producing a local beta cell protection factor to avoid of autoimmune destruction. Embryonic stem cells (ESC) and induced pluripotent stem cells (iPSCs) can generate insulin-producing surrogate β-cells. When liver cells or muscle cells are used to produce insulin by gene therapy, they also function as surrogate cells.
_
Genetically modifying immune cells to target specific molecules:
As part of its natural function, the immune system makes large numbers of white blood cells, each of which recognizes a particular molecule (or antigen) that represents a threat to the body. Researchers have learned how to isolate an individual’s immune cells and genetically engineer them through gene therapy to recognize a specific antigen, such as a protein on the surface of a cancer cell. When returned to the patient, these modified cells will find and destroy any cells that carry the antigen.
______
Route of administration of gene therapy:
The choice of route for gene therapy depends on the tissue to be treated and the mechanism by which the therapeutic gene exerts its effect. Gene therapy for cystic fibrosis, a disease which effects cells within the lung and airway, may be inhaled. Most genes designed to treat cancer are injected directly into the tumor. Proteins such as factor VIII or IX for hemophilia are also being introduced directly into target tissue (the liver).
______
Gene transfer methods:
Transformation, Transduction and Transfection:
The three very effective modes of gene transfer Transformation, Transduction and Transfection observed in bacteria fascinated the scientist leading to the development of molecular cloning. The basic principle applied in molecular cloning is transfer of desired gene from donor to a selected recipient for various applications in the field of medicine, research, gene therapy with an ultimate aim of beneficial to the mankind.
_
1. Transformation:
Transformation is the naturally occurring process of gene transfer which involves absorption of the genetic material by a cell through cell membrane causing the fusion of the foreign DNA with the native DNA resulting in the genetic expression of the received DNA. Transformation is usually a natural method of gene transfer but as a result of technological advancement originated the artificial or induced transformation. Thus there are two types called as natural transformation and artificial or induced transformation. In natural transformation, the foreign DNA attaches itself to the host cell DNA receptor and with the help of the protein DNA translocase it enters the host cell. The presence of nucleases restricts the entry of two strands of the DNA, destroys a single strand thus allowing only one strand to enter the host cell. This single stranded DNA mingles with the host genetic material successfully. The artificial or induced method of transformation is done under laboratory condition which is either a chemical mediated gene transfer or done by electroporation. In the chemical mediated gene transfer, the cold conditioned cells in calcium chloride solution are exposed to sudden heat which increases the permeability of the cell membrane allowing the foreign DNA. The electroporation method as the name indicates, pores are made in the cell by exposing it to suitable electric field, allowing the entry of the DNA. The opened up portions of the cell are sealed by the ability of the cell to repair.
_
2. Transduction:
In transduction, a media like virus is required between two bacterial cells in transferring genes from one cell to the other. Researchers used virus as a tool to introduce foreign DNA from the selected species to the target organism. Transduction mode of gene transfer follows either a lysogenic phase or lytic phase. In the lysogenic phase, the viral (phage) DNA once joining the bacterial DNA through transduction stays dormant in the following generations. The induction of lysogenic cycle by an external factor like UV light results in lytic phase. In lytic phase, the viral or phage DNA exists a separate entity in the host cell and the host cell replicates viral DNA mistaking it for its own DNA.As a result many phages are produced within the host cell and when the number exceeds it causes the lysis of the host cell and the phages exits and infects other cells. As this process involves existence of both the genome of the phage and the genome of the bacteria in the same cell, it may result in exchange of some genes between the two DNA. As a result, the newly developed phage leaving the cell may carry a bacterial gene and transfer it to the other cell it infects. Also some of the phage genes may be present in the host cell. There are two types of transduction called as generalized transduction in which any of the bacterial gene is transferred via the bacteriophage to the other bacteria and specialized transduction involves transfer of limited or selected set of genes. In transduction, or virus-mediated gene transfer, recombinant DNA techniques are used to insert the normal copy of the needed gene into the genetic material of a virus, which then acts as a carrier or vector for gene transfer. The properties of the viral vector dictate the safety and efficacy of the gene transfer process. Transduction owes its efficiency in the transfer of genetic information to the fact that many viruses have mechanisms that enable their entry, integration, and persistence in human cells.
_
3. Transfection:
It is one of the methods of gene transfer where the genetic material is deliberately introduced into the animal cell in view of studying various functions of proteins and the gene. This mode of gene transfer involves creation of pores on the cell membrane enabling the cell to receive the foreign genetic material. The significance of creating pores and introducing the DNA into the host mammalian cell contributed to different methods in transfection. Chemical mediated transfection involves use of either calcium phosphate or cationic polymers or liposomes. Electroporation, sonoporation, impalefection, optical transfection, hydro dynamic delivery are some of the non chemical based gene transfer. Particle based transfection uses gene gun technique where a nanoparticle is used to transfer the DNA to host cell or by another method called as magnetofection. Nucleofection and use of heat shock are the other evolved methods for successful transfection. Transfection of RNA can be used either to induce protein expression, or to repress it using antisense or RNA interference (RNAi) procedures. Transfection is the process of deliberately introducing nucleic acids into cells. The term is often used for non-viral methods in eukaryotic cells. Transfection can result in unexpected morphologies and abnormalities in target cells.
_
What is the difference between Transformation and Transfection?
Transformation is the introduction of a gene into a prokaryotic cell (bacterial and yeast), whereas transfection is usually called the introduction of a gene into a mammalian cell by non-viral methods. Transfection may also refer to other methods and cell types, although other terms are preferred. Often transfection and transduction are used synonymously. Transformation results in heritable alteration, in genes, whereas transfection can result in either temporary expression or permanent changes in genes.
_____
How are genes delivered?
The challenge of gene therapy lies in development of a means to deliver the genetic material into the nuclei of the appropriate cells, so that it will be reproduced in the normal course of cell division and have a lasting effect. Scientists and clinicians use the following four basic ways to carry genetically modifying factors (DNA or RNA and/or their interacting proteins) into the relevant cells.
1. First, naked DNA or RNA can be pushed into cells by using high voltage (electroporation) or through uptake through invaginating vesicles (endocytosis) or by sheer mechanical forces with an instrument called a “gene gun.”
A “bionic chip”:
A new “bionic chip” has been developed to help gene therapists using electroporation to slip fragments of DNA into cells. Electroporation was originally a hit-or-miss technique because there was no way to determine how much of an electrical jolt it took to open the cell membrane. The “bionic chip” solves this problem. It contains a single living cell embedded in a tiny silicon circuit. The cell acts as a diode, or electrical gate. When it is hit with just the right charge, the cell membrane opens, allowing the electricity to pass from the top to the bottom of the bionic chip. By recording what voltage caused this phenomenon to occur, it is now possible to determine precisely how much electricity it takes to pry open different types of cells.
2. Second, DNA or RNA can be packaged into liposomes (membrane bound vesicles) that are taken up into cells more easily than naked DNA/RNA. Different types of liposomes are being developed to preferentially bind to specific tissues, and to modify protein or RNA at different levels. Another approach employing liposomes, called chimeraplasty, involves the insertion of manufactured nucleic acid molecules (chimeraplasts) instead of entire genes to correct disease-causing gene mutations. Once inserted, the gene may produce an essential chemical that the patient’s body cannot, remove or render harmless a substance or gene causing disease, or expose certain cells, especially cancerous cells, to attack by conventional drugs. Recent work has also electroporated interfering RNA oligonucleotides into membrane vesicles normally released by cells (exosomes) to carry them to specific tissues.
3. Third, DNA or RNA can be packaged into virus-like particles using a modified viral vector. Basically, in one format, the gene(s) of interest and control signals replace most or all of the essential viral genes in the vector so the viral vector does not replicate (can’t make more viruses) in cells, as in the case of adeno associated virus (AAV) vectors and retrovirus/lentivirus vectors. In another format, one of more viral genes are replace with therapeutic genes so that the virus is still able to replicate in a restricted number of cell types, as for oncolytic viruses, such as adenovirus and herpes simplex virus. A number of different viruses are being developed as gene therapy vectors because they each preferentially enter a subset of different tissues, express genes at different levels, and interact with the immune system differently.
4. Fourth, gene therapy can be combined with cell therapy protocols. The relevant cells from the patient or matched donor are collected and purified, and when possible, expanded in culture to achieve substantial numbers. Scientists and clinicians treat the patient’s cells with the gene therapy vector using one of the three methods described above. Some of the treated cells express the desired, inserted gene or carry the virus in a latent state. These gene-expressing cells are then re-administered to the patient.
_
Currently, gene therapy refers to the transfer of a gene that encodes a functional protein into a cell or the transfer of an entity that will alter the expression of an endogenous gene in a cell. The efficient transfer of the genetic material into a cell is necessary to achieve the desired therapeutic effect. For gene transfer, either a messenger ribonucleic acid (mRNA) or genetic material that codes for mRNA needs to be transferred into the appropriate cell and expressed at sufficient levels. In most cases, a relatively large piece of genetic material (>1 kb) is required that includes the promoter sequences that activate expression of the gene, the coding sequences that direct production of a protein, and signaling sequences that direct RNA processing such as polyadenylation. A second class of gene therapy involves altering the expression of an endogenous gene in a cell. This can be achieved by transferring a relatively short piece of genetic material (20 to 50 bp) that is complementary to the mRNA. This transfer would affect gene expression by any of a variety of mechanisms through blocking translational initiation, mRNA processing, or leading to destruction of the mRNA. Alternatively, a gene that encodes antisense RNA that is complementary to a cellular RNA can function in a similar fashion. Facilitating the transfer of genetic information into a cell are vehicles called vectors. Vectors can be divided into viral and nonviral delivery systems. The most commonly used viral vectors are derived from retrovirus, adenovirus, and adenoassociated virus (AAV). Other viral vectors that have been less extensively used are derived from herpes simplex virus 1 (HSV-1), vaccinia virus, or baculovirus. Nonviral vectors can be either plasmid deoxyribonucleic acid (DNA), which is a circle of double-stranded DNA that replicates in bacteria or chemically synthesized compounds that are or resemble oligodeoxynucleotides. Major considerations in determining the optimal vector and delivery system are (1) the target cells and its characteristics, that is, the ability to be virally transduced ex vivo and reinfused to the patient, (2) the longevity of expression required, and (3) the size of the genetic material to be transferred.
______
Why vector?
_
_
Figure above shows schematic representation of barriers limiting gene transfer. Several anatomical and cellular barriers limit the overall efficiency of gene transfer. Anatomical barriers are epithelial, endothelial cell linings and the extracellular matrix surrounding the cells that prevent direct access of macromolecules to the target cells. Professional phagocytes such as Kupffer cells in the liver and residential macrophages in the spleen are largely responsible for the clearance of DNA-loaded colloidal particles administered through blood circulation. In addition, various nucleases existing in blood and extracellular matrix can rapidly degrade free and unprotected nucleic acids following systemic administration. Crossing plasma membrane is considered the most critical limiting step for an efficient DNA transfection. Nucleic acids typically cannot pass through cell membrane unless their entry is facilitated by creating transient holes by physical meanings, or through various active cell uptake mechanisms such as endocytosis, pinocytosis, or phagocytosis.
_
The pharmaceutical approach to somatic gene therapy is based on consideration of a gene as a chemical entity with specific physical, chemical and colloidal properties. The genes that are required for gene therapy are large molecules (>1 × 106 Daltons, >100 nm diameter) with a net negative charge that prevents diffusion through biological barriers such as an intact endothelium, the plasma membrane or the nuclear membrane. New methods for gene therapy are based on increasing knowledge of the pathways by which DNA may be internalized into cells and traffic to the nucleus, pharmaceutical experience with particulate drug delivery systems, and the ability to control gene expression with recombined genetic elements. Vectors are needed since the genetic material has to be transferred across the cell membrane and preferably in to the cell nucleus. Gene delivery systems are categorized as: viral-based, non-viral-based and combined hybrid systems. Viral-mediated gene delivery systems consist of viruses that are modified to be replication-deficient, but which can deliver DNA for expression. Adenoviruses, retroviruses, and lentiviruses are used as viral gene-delivery vectors.
_
_
Vectors in gene therapy:
Gene therapy utilizes the delivery of DNA into cells, which can be accomplished by a number of methods. The two major classes of methods are those that use recombinant viruses (sometimes called biological nanoparticles or viral vectors) and those that use naked DNA or DNA complexes (non-viral methods).
Viruses:
All viruses bind to their hosts and introduce their genetic material into the host cell as part of their replication cycle. Therefore this has been recognized as a plausible strategy for gene therapy, by removing the viral DNA and using the virus as a vehicle to deliver the therapeutic DNA. A number of viruses have been used for human gene therapy, including retrovirus, adenovirus, lentivirus, herpes simplex virus, vaccinia, pox virus, and adeno-associated virus.
Non-viral methods:
Non-viral methods can present certain advantages over viral methods, such as large scale production and low host immunogenicity. Previously, low levels of transfection and expression of the gene held non-viral methods at a disadvantage; however, recent advances in vector technology have yielded molecules and techniques that approach the transfection efficiencies of viruses. There are several methods for non-viral gene therapy, including the injection of naked DNA, electroporation, the gene gun, sonoporation, magnetofection, and the use of oligonucleotides, lipoplexes, dendrimers, and inorganic nanoparticles.
_
To be successful, a vector must:
1. Target the right cells. If you want to deliver a gene into cells of the liver, it shouldn’t wind up in the big toe.
2. Integrate the gene in the cells. You need to ensure that the gene integrates into, or becomes part of, the host cell’s genetic material, or that the gene finds another way to survive in the nucleus without being trashed.
3. Activate the gene. A gene must go to the cell’s nucleus and be “turned on,” meaning that it is transcribed and translated to make the protein product it encodes. For gene delivery to be successful, the protein must function properly.
4. Avoid harmful side effects. Any time you put an unfamiliar biological substance into the body, there is a risk that it will be toxic or that the body will mount an immune response against it.
_
The figure below shows different gene delivery systems:
__
The ideal vector has not been described yet, but its characteristics should include:
• Easy and efficient production of high titers of the viral particle;
• Absence of toxicity for target cells and undesirable effects such as immune response against the vector or the transgene;
• Capacity of site-specific integration, allowing long-term transgene expression, for treating diseases such as genetic disorders;
• Capacity of transduction of specific cell types;
• Infection of proliferative and quiescent cells.
The most commonly used viral vectors for gene therapy are based on adenoviruses (Ad), adeno-associated viruses (AAV) and retrovirus/lentivirus vectors.
_
_
How and why virus vectors:
American scientist Wendell Stanley crystallized the particles responsible for tobacco mosaic disease and described viruses for the world in 1935. These strange entities don’t have nuclei or other cellular structures, but they do have nucleic acid, either DNA or RNA. This small packet of genetic information is packed inside a protein coat, which, in some cases, is wrapped in a membranous envelope. Unlike other living things, viruses can’t reproduce on their own because they don’t have the necessary cellular machinery. They can, however, reproduce if they invade a cell and borrow the cell’s equipment and enzymes. The basic process works like this:
- A virus enters a host cell and releases its nucleic acid and proteins.
- Host enzymes don’t recognize the viral DNA or RNA as foreign and happily make lots of extra copies.
- At the same time, other host enzymes transcribe the viral nucleic acid into messenger RNA, which then serves as a template to make more viral proteins.
- New virus particles self-assemble, using the fresh supplies of nucleic acid and protein manufactured by the host cell.
- The viruses exit the cell and repeat the process in other hosts.
_
_
The ability to carry genetic information into cells makes viruses useful in gene therapy. What if you could replace a snippet of viral DNA with the DNA of a human gene and then let that virus infect a cell? Wouldn’t the host cell make copies of the introduced gene and then follow the blueprint of the gene to churn out the associated protein? As it turns out, this is completely possible — as long as scientists modify the virus to prevent it from causing disease or inducing an immune reaction by the host. When so modified, such a virus can become a vehicle, or vector, to deliver a specific gene therapy. Today, researchers use several types of viruses as vectors. One favorite is adenovirus, the agent responsible for the common cold in humans. Adenoviruses introduce their DNA into the nucleus of the cell, but the DNA isn’t integrated into a chromosome. This makes them good vectors, but they often stimulate an immune response, even when weakened. As an alternative, researchers may rely on adeno-associated viruses, which cause no known human diseases. Not only that, they integrate their genes into host chromosomes, making it possible for the cells to replicate the inserted gene and pass it on to future generations of the altered cells. Retroviruses, like the ones that cause AIDS and some types of hepatitis, also splice their genetic material into the chromosomes of the cells they invade. As a result, researchers have studied retroviruses extensively as vectors for gene therapy.
_
Virus to vector:
Viruses can be modified in the laboratory to provide vectors that carry corrected, therapeutic DNA into cells, where it can be integrated into the genome to alter abnormal gene expression and correct genetic disease. This involves removing the viral DNA present in the virus and replacing it with the therapeutic genes. In this way, the virus becomes merely a “vector” that is capable of transferring the desired gene into cells but not capable of taking over or harming cells. For the production of efficient and safe viral vectors, essential sequences for viral particle assembly, genome package, and transgene delivery to target cells must be identified. Dispensable genes are then deleted from the viral genome in order to reduce its pathogenicity and immunogenicity and, finally, the transgene is integrated into the construct. Some viral vectors are able to integrate into the host genome, whereas others remain episomal. Integrating viruses result in persistent transgene expression. Non-integrating vectors, such as adenoviruses whose viral DNA is maintained in episomal form in infected cells, lead to transient transgene expression. Each type of vector presents specific advantages and limitations that make them appropriate for particular applications. Most of the vectors currently used for gene transfer are derived from human pathogens, from which essential viral genes have been deleted to make them nonpathogenic. They usually have a broad tropism, so that different types of cells and/or tissues may be targeted. Some of the viruses currently used in gene therapy include retroviruses, adenoviruses, adeno-associated viruses and the herpes simplex virus.
_
Retroviral Packaging Cells:
Packing cell line is any mammalian cell line modified for the production of recombinant retroviruses. They express essential viral genes that are lacking in the recombinant retroviral vector. Unlike bacteriophage assembly which can be accomplished in a cell-free system, production of retroviral virions has been accomplished only in intact cells. To make replication-defective vectors, retroviral packaging cells have been designed to provide all viral proteins but not to package or transmit the RNAs encoding these functions. Retroviral vectors produced by packaging cells can transduce cells but cannot replicate further.
_
_
Retroviral vectors are created by removal of the retroviral gag, pol, and env genes. These are replaced by the therapeutic gene. In order to produce vector particles a packaging cell is essential. Packaging cell lines provide all the viral proteins required for capsid production and the virion maturation of the vector. These packaging cell lines have been made so that they contain the gag, pol and env genes. Early packaging cell lines contained replication competent retroviral genomes and a single recombination event between this genome and the retroviral DNA vector could result in the production of a wild type virus. Following insertion of the desired gene into in the retroviral DNA vector, and maintenance of the proper packaging cell line, it is now a simple matter to prepare retroviral vectors as seen in the figure above.
_
Recently developed packaging cell lines are of human origin and are advantageous. The presence of human antibodies in human serum results in rapid lysis of retroviral vectors packaged in murine cell lines. The antibodies are directed against the a-galactosyl carbohydrate moiety present on the glycoproteins of murine but not human cells. This murine carbohydrate moiety is absent from retroviral vectors that are produced by human cells, which lack the enzyme a1-3-galactosyl transferase. Human or primate-derived packaging cell lines will likely be necessary to produce retroviral vectors for in vivo administration to humans. To this point, the production of retroviral vectors for clinical use is simple but not without challenges. A suitable stable packaging cell line containing both the packaging genes and the vector sequences is prepared and tested for the presence of infectious agents and replication-competent virus. This packaging cell line can then be amplified and used to produce large amounts of vector in tissue culture. Most retroviral vectors will produce ~1 X 10^5 to 1 X 10^6 colony forming units (cfu)/ml, although unconcentrated titers as high as 1X 10^7 cfu/ml have been reported. The original vector preparation can be concentrated by a variety of techniques including centrifugation and ultrafiltration. Vectors with retroviral envelope proteins are less stable to these concentration procedures than are pseudotyped vectors with envelope proteins from other viruses. The preparations can be frozen until use with some loss of titer on thawing.
_
_
_
_
Viral vectors are tailored to their specific applications but generally share a few key properties:
1. ”Safety”: Although viral vectors are occasionally created from pathogenic viruses, they are modified in such a way as to minimize the risk of handling them. This usually involves the deletion of a part of the viral genome critical for viral replication. Such a virus can efficiently infect cells but, once the infection has taken place, requires a helper virus to provide the missing proteins for production of new virions.
2. ”Low toxicity”: The viral vector should have a minimal effect on the physiology of the cell it infects.
3. ”Stability”: Some viruses are genetically unstable and can rapidly rearrange their genomes. This is detrimental to predictability and reproducibility of the work conducted using a viral vector and is avoided in their design.
4. ”Cell type specificity”: Most viral vectors are engineered to infect as wide a range of cell types as possible. However, sometimes the opposite is preferred. The viral receptor can be modified to target the virus to a specific kind of cell.
5. ”Identification”: Viral vectors are often given certain genes that help identify which cells took up the viral genes. These genes are called Markers, a common marker is antibiotic resistance to a certain antibiotic. The cells can then be isolated easily as those that have not taken up the viral vector genes do not have antibiotic resistance and so cannot grow in a culture with antibiotics present.
_
Viral gene delivery systems consist of viruses that are modified to be replication-deficient which were made unable to replicate by redesigning which can deliver the genes to the cells to provide expression. Adenoviruses, retroviruses, and lentiviruses are used for viral gene delivery. Viral systems have advantages such as constant expression and expression of therapeutic genes (Sullivan, 2003). However, there are some limitations that restrict the use of these systems, which particularly include the use of viruses in production, immunogenicity, toxicity and lack of optimization in large-scale production (Witlox et al., 2007).
_
Retroviruses:
The retroviruses are modified to carry genes. The gag, pol, env genes are deleted rendering them incapable of replication inside the host cell. Viruses are then introduced into a culture containing the helper viruses. The helper virus is an engineered virus which is deficient in Ψsegment, but contains all other genes for replication. That means it has the genes to produce viral particles but lacks the genes required for packing. The replication deficient but infective retro virus vector carrying the human gene now comes out of the cultured cells. These are introduced in to the patient. The virus enters the cell via specific receptors. In the cytoplasm of the human cells, the reverse transcriptase carried by the vector coverts the RNA in to DNA, Which is then integrated in to the host DNA. The normal human gene can now be expressed. The integrated DNA becomes a permanent part of the chromosome.
_
The traditional method to introduce a therapeutic gene into hematopoietic stem cells from bone marrow or peripheral blood involves the use of a vector derived from a certain class of virus, called a retrovirus. One type of retroviral vector was initially employed to show proof-of-principle that a foreign gene (in that instance the gene was not therapeutic, but was used as a molecular tag to genetically mark the cells) introduced into bone marrow cells may be stably maintained for several months. However, these particular retroviral vectors were only capable of transferring the therapeutic gene into actively dividing cells. Since most adult stem cells divide at a relatively slow rate, efficiency was rather low. Vectors derived from other types of retroviruses (lentiviruses) and adenoviruses have the potential to overcome this limitation, since they also target non-dividing cells. Out-of-the-body therapies relying on retroviruses have their own problems. Remember, retroviruses stitch their DNA into the host chromosome, which is a bit like picking up a short phrase from one sentence and plugging it into a longer sentence. If the insertion doesn’t occur in just the right place, the resulting “language” might not make any sense. In some gene therapy trials using retroviruses, patients have developed leukemia and other forms of cancer because inserting one gene disrupts the function of other surrounding genes. This complication has affected several children in the SCID trials, although many of them have beaten the cancer with other therapies.
_
Adeno viruses:
These are DNA viruses. These do not produce serious illness so are used for gene therapy. The genes of the virus are removed so they lose the ability to divide. The human genes are inserted and the vector is transfected in the culture containing the sequences for replication. The virus thus replicates in the cell culture. The packed viruses are then introduced in to the patient. It is not integrated but remains as epi-chromosomal (episomal). In some gene transfer systems, the foreign transgene does not integrate at a high rate and remains separate from the host genomic DNA, a status denoted episomal. Specific proteins stabilizing these episomal DNA molecules have been identified as well as viruses (adenovirus) that persist stably for some time in an episomal condition. Recently, episomal systems have been applied to embryonic stem cells.
_
Adeno associated virus (AAV) and Herpes simplex virus:
Adeno associated virus- It is also DNA virus. It has no known pathogenic effect and has wide tissue affinity. It integrates at a specific site. Herpes simplex virus- This is a disabled single copy virus and has defective glycoprotein. When propagated in the complementary cells, viral particles are generated. Since they can replicate only once so there is no risk of a disease.
_
Why scientists choose AAV as a vector for gene therapy?
The following are the reasons that made AAV, a very good gene therapy tool:
1) AAV not cause any disease conditions in humans, it is only pathogenic for animals.
2) Heparin Sulphate, the receptor that is required for binding of AAV to cells is found abundantly on the surface of human cells. So this will facilitate easy entry of virus inside the cells.
3) AAV genome is known to be stably integrated in chromosome 19 at 13.4q position. And the region where it is integrating is completely a junk area so we are getting extra proteins without disrupting any human proteins or genes. So delete the irrelevant part of AAV genome and insert your gene of interest which will stably get integrated at 19q13.4 and we will get an expression of our gene of interest.
_
There are 3 reasons why lentiviral vectors are more advantageous than retroviral vectors:
1. Lentiviral vectors are very effective at modifying or transducing quiescent cells, the cells that do not divide; and most of bone marrow stem cells, at any given time are quiescent.
2. The second reason is that retroviral vectors are pretty simple beasts, if you will, and the size of what they contain in terms of gene length is short, and they don’t have the machinery to prevent the viral RNA from being spliced before packaging, so it gets rearranged very commonly…. Lentiviral vectors have the machinery to prevent splicing of the viral RNA before packaging, even if it is very long and complex. For many gene disorders, we needed to use the full-length gene with the introns, we needed to add the promoter of the gene, we needed to add enhancer elements, so it was very long and complex, and only lentiviral vectors were able to carry that well.
3. The third reason is that lentiviral vectors have the tendency to alter gene expression upon integration less frequently than retroviral vectors. So it’s safer.
_
Note:
Lentiviruses are a subtype of retrovirus. Both lentiviruses and standard retroviruses use the gag, pol, and env genes for packaging. However, the isoforms of these proteins used by different retroviruses and lentiviruses are different and lentiviral vectors may not be efficiently packaged by retroviral packaging systems and vice versa.
_
How viruses work in gene therapy:
Viruses are used in gene therapy in two basic ways: as gene delivery vectors and as oncolytic viruses.
1. First, modified viruses are used as viral vectors or carriers in gene therapy. Viral vectors protect the new gene from enzymes in the blood that can degrade it, and they deliver the new gene in the “gene cassette” to the relevant cells. Viral vectors efficiently coerce the cells to take up the new gene, uncoat the gene from the virus particle (virions), and transport it, usually to the cell nucleus. The transduced cells begin using the new gene to perform its function, such as synthesis of a new protein. These viral vectors have been genetically engineered so that most of their essential genes are missing. Removal of these viral genes makes room for the “gene cassette” and reduces viral toxicity. Viral vectors typically have to be grown in special cells in culture that provide the missing viral proteins in order to package the therapeutic gene(s) into virus particles. Many different kinds of viral vectors are being developed because the requirements of gene therapy agents for specific diseases vary depending on what tissue is affected, how stringent control of gene expression needs to be, and how long the gene needs to be expressed. Scientists examine at least the following characteristics while choosing or developing an appropriate viral vector: (i) size of DNA or gene that can be packaged, (ii) tropism to the desired cells for therapy, (iii) duration of gene expression, (iv) effect on immune response, (v) ease of manufacturing, (vi) ease of integration into the cell’s DNA or ability to exist as a stable DNA element in the cell nucleus without genomic integration, and (vii) chance that the patients have previously been exposed to the virus and thus might have antibodies against it which would reduce its efficiency of gene delivery.
2. Second, oncolytic viruses are engineered to replicate only or predominantly in cancer cells and not in normal human cells. These viruses grow in cancer cells and cause the cancer cells to burst, releasing more oncolytic viruses to infect surrounding cancer cells. These viruses can also carry therapeutic genes to increase toxicity to tumor cells, stimulate the immune system or inhibit angiogenesis of the tumor.
_
One way to transfer DNA into host cells is by viral transfection. The normal DNA is inserted into a virus, which then transfects the host cells, thereby transmitting the DNA into the cell nucleus. Some important concerns about insertion using a virus include reactions to the virus, rapid loss of (failure to propagate) the new normal DNA, and damage to the virus by antibodies developed against the transfected protein, which the immune system recognizes as foreign. Another way to transfer DNA uses liposomes, which are absorbed by the host cells and thereby deliver their DNA to the cell nucleus. Potential problems with liposome insertion methods include failure to absorb the liposomes into the cells, rapid degradation of the new normal DNA, and rapid loss of integration of the DNA. Another major drawback of these methods is that the therapeutic gene frequently integrates more or less randomly into the chromosomes of the target cell. In principle, this is dangerous, because the gene therapy vector can potentially modify the activity of neighboring genes (positively or negatively) in close proximity to the insertion site or even inactivate host genes by integrating into them. These phenomena are referred to as insertional mutagenesis. In extreme cases, such as in the X-linked SCID gene therapy trials, these mutations contribute to the malignant transformation of the targeted cells, ultimately resulting in cancer. An important parameter that must be carefully monitored is the random integration into the host genome, since this process can induce mutations that lead to malignant transformation or serious gene dysfunction. However, several copies of the therapeutic gene may also be integrated into the genome, helping to bypass positional effects and gene silencing. Positional effects are caused by certain areas within the genome and directly influence the activity of the introduced gene. Gene silencing refers to the phenomenon whereby over time, most artificially introduced active genes are turned off by the host cell, a mechanism that is not currently well understood. In these cases, integration of several copies may help to achieve stable gene expression, since a subset of the introduced genes may integrate into favorable sites. In the past, gene silencing and positional effects were a particular problem in mouse hematopoietic stem cells. These problems led to the optimization of retroviral and lentiviral vector systems by the addition of genetic control elements (referred to as chromatin domain insulators and scaffold/matrix attachment regions) into the vectors, resulting in more robust expression in differentiating cell systems, including human embryonic stem cells.
_
Homologous recombination:
An elegant way to circumvent positional effects and gene silencing is to introduce the gene of interest specifically into a defined region of the genome by novel gene targeting technique. This gene targeting technique takes advantage of a cellular DNA repair process known as homologous recombination. Homologous recombination provides a precise mechanism for defined modifications of genomes in living cells, and has been used extensively with mouse embryonic stem cells to investigate gene function and create mouse models of human diseases. Recombinant DNA is altered in vitro, and the therapeutic gene is introduced into a copy of the genomic DNA that is targeted during this process. Next, recombinant DNA is introduced by transfection into the cell, where it recombines with the homologous part of the cell genome. This in turn results in the replacement of normal genomic DNA with recombinant DNA containing genetic modifications. Homologous recombination is a very rare event in cells, and thus a powerful selection strategy is necessary to identify the cells in which it occurs. Usually, the introduced construct has an additional gene coding for antibiotic resistance (referred to as a selectable marker), allowing cells that have incorporated the recombinant DNA to be positively selected in culture. However, antibiotic resistance only reveals that the cells have taken up recombinant DNA and incorporated it somewhere in the genome. To select for cells in which homologous recombination has occurred, the end of the recombination construct often includes the thymidine kinase gene from the herpes simplex virus. Cells that randomly incorporate recombinant DNA usually retain the entire DNA construct, including the herpes virus thymidine kinase gene. In cells that display homologous recombination between the recombinant construct and cellular DNA, an exchange of homologous DNA sequences is involved, and the non-homologous thymidine kinase gene at the end of the construct is eliminated. Cells expressing the thymidine kinase gene are killed by the antiviral drug ganciclovir in a process known as negative selection. Therefore, those cells undergoing homologous recombination are unique in that they are resistant to both the antibiotic and ganciclovir, allowing effective selection with these drugs.
_
Suicide genes:
Is it theoretically possible for well intentioned medical professionals to treat a patient with a self-replicating gene therapy vector, and for that vector to replicate itself uncontrollably beyond the patient, causing harm to others? How can humanity prevent such a tragedy?
Gene therapy usually works by introducing an integrative vector (i.e. lentivirus) containing the corrective gene of interest. However, some integration events will be deleterious — the vector can insert into tumor suppressor genes or bring the enhancer/promoter elements from the vector near an oncogene. This can potentially turn the rescued cells into cancerous cells. Thankfully, researchers have thought of this possibility and along with the corrective gene on the viral vector, they also included a “suicide gene” — usually a gene encoding for a surface receptor derived from a virus. The surface receptor by itself is harmless; it basically “marks” which cells received the gene therapy. However, because each treated cell is now physically distinguishable from non–treated cells, it can be targeted with certain drugs. Therefore, if the population of treated cells starts to get angry and go tumorgenic, you can administer a drug that will kill cells with that viral receptor, thus starting again from square 1. Not the most efficient method since it will also kill corrected cells without tumorgenic potential but at least it spares the patient of a painful death. The aim of suicide gene therapy is to enable, selectively, the transfected cell to transform a prodrug into a toxic metabolite, resulting in cell death. The most widely described suicide gene is the herpes simplex virus thymidine kinase(HSV-tk) gene. HSV-tk can phosphorylate ganciclovir which is a poor substrate for mammalian thymidine kinases. Ganciclovir can, therefore, be transformed into ganciclovir triphosphate which is cytotoxic to the transfected cell, resulting in cell death. This cell death can also affect neighbouring cells which do not express HSV-tk. This phenomenon is called a local bystander effect, as opposed to a bystander effect that can be observed in distant, non-transduced tumour sites. This distant bystander effect involves the immune system.
_
The figure below shows gene therapy strategy involving suicide genes:
______
Non-viral gene delivery system:
Non-viral gene delivery systems were developed as an alternative to viral-based systems. One of the most important advantages of these systems is that they develop transfection. Non-viral gene delivery systems are divided into two categories: physical and chemical. Microinjection, electroporation, gene gun, ultrasound-mediated methods, and hydrodynamic systems are the most widely used physical methods. Physical methods involve the use of physical force to increase the permeability of the cell membrane and allow the gene to enter the cell. The primary advantage of physical methods is that they are easy to use and reliable. However, they also have the disadvantage of causing tissue damage in some applications. Chemical methods involve the use of carriers prepared from synthetic or natural compounds for gene delivery into the cell, including synthetic and natural polymers, liposomes, dendrimers, synthetic proteins, and cationic lipids. The biggest advantages of these systems are that they are non-immunogenic and generally have low toxicity.
_
Non-Viral Vectors:
Naked Plasmid DNA:
One type of non-viral vector is a circular DNA molecule called a plasmid. In nature, bacteria use plasmids to transfer & share genes with one another. A plasmid is an independent, circular, self-replicating DNA molecule that carries only a few genes. The number of plasmids in a cell generally remains constant from generation to generation. Plasmids are autonomous molecules and exist in cells as extrachromosomal genomes, although some plasmids can be inserted into a bacterial chromosome, where they become a permanent part of the bacterial genome. It is here that they provide great functionality in molecular science. Plasmids are easy to manipulate and isolate using bacteria. They can be integrated into mammalian genomes, thereby conferring to mammalian cells whatever genetic functionality they carry. Thus, this gives you the ability to introduce genes into a given organism by using bacteria to amplify the hybrid genes that are created in vitro. This tiny but mighty plasmid molecule is the basis of recombinant DNA technology. The simplest non-viral gene delivery system uses naked expression vector DNA. Direct injection of free DNA into certain tissues, particularly muscle, has been shown to produce surprisingly high levels of gene expression, and the simplicity of this approach has led to its adoption in a number of clinical protocols. However, naked DNA and peptides have a very short half life due to in vivo enzymatic degradation. Plasmid DNA suffers from low transfection efficiency. Compared with recombinant viruses, plasmids are simple to construct and easily propagated in large quantities. They also possess an excellent safety profile, with virtually no risk of oncogenesis (as genomic integration is very inefficient) and relatively little immunogenicity. Plasmids have a very large DNA packaging capacity and can accommodate large segments of genomic DNA. They are easy to handle, remaining stable at room temperature for long periods of time (an important consideration for clinical use). The main limitation with plasmids is poor gene transfer efficiency. Viruses have evolved complex mechanisms to facilitate cell entry and nuclear localization. Wild-type plasmids lack these mechanisms; however, developments in delivery methods and plasmid construction may address this shortcoming. Given the potential benefits, plasmid-mediated gene therapy represents a more attractive option in many respects than viral gene therapy for cardiovascular applications. The plasmid transfer is effective against cells in culture that may be used to restore diseased tissue, but the plasmid is relatively ineffective in the intact human or animals.
_
To make it easier for them to enter cells, gene-therapy plasmids are sometimes packaged inside of “liposomes,” small membrane-wrapped packets that deliver their contents by fusing with cell membranes. The disadvantage of plasmids and liposomes is that they are much less efficient than viruses at getting genes into cells. The advantages are that they can carry larger genes, and most don’t trigger an immune response.
_
Cationic Liposomes:
Liposomes are microscopic spherical vesicles of phospholipids and cholesterol. Recently, liposomes have been evaluated as delivery systems for drugs and have been loaded with a great variety of molecules such as small drug molecules, proteins, nucleotides and even plasmids. Target cell DNA-liposome complex is taken into the target cell by endocytosis. The liposome is degraded within the endosome and the DNA is released into the cytosol. The DNA is imported into the cell nucleus. The cationic head groups appear to be better suited for DNA delivery due to the natural charge attraction between negatively charged phosphate groups and the positively charged head groups. Anionic head groups are perhaps better suited for drug delivery. However, this does not preclude their use as gene delivery vehicles as work with divalent cations has shown. The advantages of using liposomes as drug carriers are that they can be injected intravenously and when they are modified with lipids which render their surface more hydrophilic, their circulation time in the bloodstream can be increased significantly. They can be targeted to the tumor cells by conjugating them to specific molecules like antibodies, proteins, and small peptides. The cationic liposomes can significantly improve systemic delivery and gene expression of DNA. Tumor vessel-targeted liposomes can also be used to efficiently deliver therapeutic doses of chemotherapy.
_
Virosomes:
Synthetic vectors called virosomes are essentially liposomes covered with viral surface proteins. They combine the carrying capacity and immune advantages of plasmids with the efficiency and specificity of viruses. The viral proteins interact with proteins on the target-cell surface, helping the virosome fuse with the cell membrane and dump its contents into the cell. Different types of viral proteins can target specific types of cells.
_
The table below shows comparison between viral vectors and liposomes:
_
Antisense RNA:
Antisense oligodeoxynucleotides (ODNs) are synthetic molecules that block mRNA translation. They can be used as a tool to inhibit mRNA translation of a diseased gene. There are reports demonstrating use of VEGF and VEGFR antisense RNA in preclinical models. Angiogenesis and tumorigenicity (as measured by MVD and tumor volume, respectively) of human esophageal squamous cell carcinoma can be effectively inhibited by VEGF165 antisense RNA.
_
Small Interfering RNA (SiRNA):
The ability of small dsRNA to suppress the expression of a gene corresponding to its own sequence is called RNA interference (RNAi). The discovery of RNAi has added a promising tool to the field of molecular biology. Introducing the SiRNA corresponding to a particular gene will knock out the cell’s own expression of that gene. The application of SiRNA to silence gene expression has profound implications for the intervention of human diseases including cancer. The disadvantage to simply introducing dsRNA fragments into a cell is that gene expression is only temporarily reduced. However, Brummelkamp et. al. developed a new vector system, named pSUPER, which directs the synthesis of siRNA in mammalian cells. The authors have shown that siRNA expression mediated by this vector causes persistent and specific down-regulation of gene expression, resulting in functional inactivation of the targeted gene over longer periods of time.
_
Nanotechnology and gene therapy:
_
The particles can be made with multiple layers so the outer layer will have a peptide that can target the particles to cells of interest. A schematic of an iron nanoparticle with multiple layers is seen in the figure above. These nanoparticles can be delivered to cells in the retina for gene therapy.
_
DNA nanoballs boost gene therapy:
Scrunching up DNA into ultra-tiny balls could be the key to making gene therapy safer and more efficient. The technique is now being tested on people with cystic fibrosis. So far, modified viruses have proved to be the most efficient way of delivering DNA to cells to make up for genetic faults. But viruses cannot be given to the same person time after time because the immune system starts attacking them. Viruses can also cause severe reactions. As a result, researchers increasingly favour other means of delivering genes, such as encasing DNA in fatty globules called liposomes that can pass through the membranes round cells. But simply getting a gene into a cell is not enough – for the desired protein to be produced, you need to get the gene into the cell’s nucleus. At around 100 nanometres in size, most liposomes are too large to pass through the tiny pores in the nuclear membrane except when the membrane breaks down during cell division. Even if cells are rapidly dividing, delivering genes via liposomes is not very efficient – and it is no good for slowly dividing cells such as those lining the lungs. But researchers at Case Western Reserve University and Copernicus Therapeutics, both in Cleveland, Ohio, have developed a way to pack DNA into particles 25 nanometres across, small enough to enter the nuclear pores. The nanoparticles consist of a single DNA molecule encased in positively charged peptides and are themselves delivered to cells via liposomes. In cells grown in culture, there was a 6000-fold increase in the expression of a gene packaged this way compared with unpackaged DNA in liposomes. Trials have now begun in 12 people with cystic fibrosis, who have a faulty gene that means thick mucus accumulates in their lungs. The researchers will first test the technique on nasal cells before trying to deliver genes to the lungs. “We’re very excited about this,” says Robert Beall, president of the Cystic Fibrosis Foundation. “Everybody recognises that gene therapy could provide the cure for cystic fibrosis, and it is exciting that this is a non-viral approach.”
_
Nanotech robots deliver gene therapy through blood:
U.S. researchers have developed tiny nanoparticle robots that can travel through a patient’s blood and into tumors where they deliver a therapy that turns off an important cancer gene. The finding, reported in the journal Nature offers early proof that a new treatment approach called RNA interference or RNAi might work in people. RNA stands for ribonucleic acid — a chemical messenger that is emerging as a key player in the disease process. Dozens of biotechnology and pharmaceutical companies including Alnylam, Merck, Pfizer, Novartis and Roche are looking for ways to manipulate RNA to block genes that make disease-causing proteins involved in cancer, blindness or AIDS. But getting the treatment to the right target in the body has presented a challenge. A team at the California Institute of Technology in Pasadena used nanotechnology — the science of really small objects — to create tiny polymer robots covered with a protein called transferrin that seek out a receptor or molecular doorway on many different types of tumors. “This is the first study to be able to go in there and show it’s doing its mechanism of action,” said Mark Davis, a professor of chemical engineering, who led the study. “We’re excited about it because there is a lot of skepticism whenever any new technology comes in,” said Davis, a consultant to privately held Calando Pharmaceuticals Inc, which is developing the therapy. Other teams are using fats or lipids to deliver the therapy to the treatment target. Pfizer announced a deal with Canadian biotech Tekmira Pharmaceuticals Corp for this type of delivery vehicle for its RNAi drugs, joining Roche and Alnylam. In the approach used by Davis and colleagues, once the particles find the cancer cell and get inside, they break down, releasing small interfering RNAs or siRNAs that block a gene that makes a cancer growth protein called ribonucleotide reductase. “In the particle itself, we’ve built what we call a chemical sensor,” Davis said in a telephone interview. “When it recognizes that it’s gone inside the cell, it says OK, now it’s time to disassemble and give off the RNA.” In a phase 1 clinical trial in patients with various types of tumors, the team gave doses of the targeted nanoparticles four times over 21 days in a 30-minute intravenous infusion. Tumor samples taken from three people with melanoma showed the nanoparticles found their way inside tumor cells. And they found evidence that the therapy had disabled ribonucleotide reductase, suggesting the RNA had done its job. Davis could not say whether the therapy helped shrink tumors in the patients, but one patient did get a second cycle of treatment, suggesting it might be. Nor could he say if there were any safety concerns.
_
Magnetic nanoparticles:
The recent emphasis on the development of non-viral transfection agents for gene delivery has led to new physics and chemistry-based techniques, which take advantage of charge interactions and energetic processes. One of these techniques which shows much promise for both in vitro and in vivo transfection involves the use of biocompatible magnetic nanoparticles for gene delivery. In these systems, therapeutic or reporter genes are attached to magnetic nanoparticles, which are then focused to the target site/cells via high-field/high-gradient magnets. The technique promotes rapid transfection and, as more recent work indicates, excellent overall transfection levels as well. The efficacy of magnetic nanoparticle-based gene delivery has been demonstrated most clearly in vitro. As such, there is great potential for non-viral in vitro transfection of a variety of cell lines, primary cells and tissue explants using this method, and in fact, static-field magnetofection systems are already commercially available. The development of new particles and the optimization of magnetic field parameters is already beginning to show great promise for advancing this technique. In particular, the use of oscillating arrays of permanent magnets has been shown to significantly increase overall transfection levels even well beyond those achievable with cationic lipid agents. The use of carbon nanotubes also shows great promise; however, the potential for in vivo use may be more limited in the near-term due to the potential for toxicity. While scale-up to clinical application is likely to prove difficult for some targets, the potential for magnetofection to facilitate delivery of therapeutic genes in vivo remains enticing. The use of magnetic microparticles for transfection was first demonstrated in 2000 by Cathryn Mah, Barry Byrne and others at the University of Florida, in vitro in C12S cells and in vivo in mice using an adeno-associated virus (AAV) linked to magnetic microspheres via heparin. Since these initial studies, the efficiency of this technique, often termed ‘magnetofection’, has been demonstrated in a variety of cells. The technique is based on the coupling of genetic material to magnetic nano- (and in some cases, micro-) particles. In the case of in vitro magnetic nanoparticle-based transfection, the particle/DNA complex (normally in suspension) is introduced into the cell culture where the field gradient produced by rare earth magnets (or electromagnets) placed below the cell culture increases sedimentation of the complex and increases the speed of transfection. Stent angioplasty saves lives, but there often are side effects and complications related to the procedure, such as arterial restenosis and thrombosis. In the June 2013 issue of The FASEB Journal, however, scientists report that they have discovered a new nanoparticle gene delivery method that may overcome current limitations of gene therapy vectors and prevent complications associated with the stenting procedure. Specifically, this strategy uses stents as a platform for magnetically targeted gene delivery, where genes are moved to cells at arterial injury locations without causing unwanted side effects to other organs. Additionally, magnetic nanoparticles developed and characterized in the study also protect genes and help them reach their target in active form, which also is one of the key challenges in any gene therapy.
_
Lipid nanoparticles are ideal for delivering genes and drugs, researchers show:
At the Faculty of Pharmacy of the Basque Public University (UPV/EHU) the Pharmacokinetics, Nanotechnology and Gene Therapy research team is using nanotechnology to develop new formulations that can be applied to drugs and gene therapy. Specifically, they are using nanoparticles to design systems for delivering genes and drugs; this helps to get the genes and drugs to the point of action so that they can produce the desired effect. The research team has shown that lipid nanoparticles, which they have been working on for several years, are ideal for acting as vectors in gene therapy.
__
Exosomes and the emerging field of exosome-based gene therapy:
Exosomes are a subtype of membrane vesicle released from the endocytic compartment of live cells. They play an important role in endogenous cell-to-cell communication. Previously shown to be capable of traversing biological barriers and to naturally transport functional nucleic acids between cells, they potentially represent a novel and exciting drug delivery vehicle for the field of gene therapy. Existing delivery vehicles are limited by concerns regarding their safety, toxicity and efficacy. In contrast, exosomes, as a natural cell-derived nanocarrier, are immunologically inert if purified from a compatible cell source and possess an intrinsic ability to cross biological barriers. Already utilised in a number of clinical trials, exosomes appear to be well-tolerated, even following repeat administration. Recent studies have shown that exosomes may be used to encapsulate and protect exogenous oligonucleotides for delivery to target cells. They therefore may be valuable for the delivery of RNA interference and microRNA regulatory molecules in addition to other single-stranded oligonucleotides. Prior to clinical translation, this nanotechnology requires further development by refinement of isolation, purification, loading, delivery and targeting protocols. Thus, exosome-mediated nanodelivery is highly promising and may fill the void left by current delivery methods for systemic gene therapy.
_
Advantages and disadvantages of non-viral vectors:
The nonviral gene delivery methods use synthetic or natural compounds or physical forces to deliver a piece of DNA into a cell. The materials used are generally less toxic and immunogenic than the viral counterparts. In addition, cell or tissue specificity can be achieved by harnessing cell-specific functionality in the design of chemical or biological vectors, while physical procedures can provide spatial precision. Other practical advantages of nonviral approaches include ease of production and the potential for repeat administration. Nonviral methods are generally viewed as less efficacious than the viral methods, and in many cases, the gene expression is short-lived. The disadvantages of non viral vectors – stability, non-specific uptake by various tissues, poor adsorption, short half life in the circulation, aggregate formation, and low in-vivo potency for cell transfection – continue to limit its use. However, recent developments suggest that gene delivery by some physical methods has reached the efficiency and expression duration that is clinically meaningful.
____________
____________
Fetal (prenatal) and neonatal gene therapy:
The current approaches to gene therapy of monogenetic diseases into mature organisms are confronted with several problems including the following: (1) the underlying genetic defect may have already caused irreversible pathological changes; (2) the level of sufficient protein expression to ameliorate or prevent the disease requires prohibitively large amounts of gene delivery vector; (3) adult tissues may be poorly infected by conventional vector systems dependent upon cellular proliferation for optimal infection, for example, oncoretrovirus vectors; (4) immune responses, either pre-existing or developing following vector delivery, may rapidly eliminate transgenic protein expression and prevent future effective intervention. Early gene transfer, in the neonatal or even fetal period, may overcome some or all of these obstacles.
_
Why discuss a prenatal approach?
First, for many conditions, postnatal gene therapy may not be delivered in time to avoid irreversible disease manifestation. In contrast, supplementation of a therapeutic gene in utero may prevent the original onset of disease pathology. Second, a developing fetus may be more amenable to uptake and permanent integration of foreign DNA. Still-expanding stem-cell populations of organs inaccessible later in life may also be targetable during certain earlier stages of development. Third, although the fetal immune system already has the potential to respond to intrauterine infections in the second trimester of pregnancy, it is not completely developed until several months after birth. This functional immaturity may permit the induction of immune tolerance against vector and transgene. Finally, as ultrasound-guided diagnostic procedures during the human pregnancy are well established, gene delivery to the fetus could be accomplished with limited invasion and trauma. Thus, it does not seem necessary to delay prenatal studies until gene therapy has proven clinically successful in adults.
_
_
Transgene delivery and expression in the fetal or neonatal period is a useful tool for studying human models. One day, it may even be used therapeutically alongside adult gene therapy as a means to prevent or ameliorate monogenetic diseases. These encouraging studies, which have benefited from the recent improvements in vector technology and optimization of administration routes to appropriate disease models, have reported long-term phenotypic correction after fetal or neonatal application. These include glycogen storage disease type Ia, mucopolysaccharidosis type VII, bilirubin-UDP-glucuronosyltransferase deficiency (Crigler–Najjar syndrome), haemophilias A and B and congenital blindness (Leber congenital amaurosis). To fully understand the basis of these successful experiments in order to move towards clinical application, several key factors concerning early gene transfer must be closely examined.
_
Major advantages of fetal and neonatal gene therapy are:
(1) Restitution of gene expression may avoid irreversible pathological processes; prevention is better than healing.
(2) The earlier in life the vector is administered, the higher is the ratio of vector particles to cells, reducing the amount of vector required.
(3) An ideal environment for infection of abundant stem cells and other progenitors may be provided; integrating vectors could, therefore, ‘hitch a ride’ with the subsequent cell divisions.
(4) Immune mechanisms used by adults to defend against pathogens may be limited or absent: ‘the age of innocence’.
_
Fetal somatic gene therapy is, for some reason, often seen as ethically particularly controversial. Unfortunately, many of the adverse reactions to this approach such as accusations of wanting to play god, to manipulate the germ-line, to create designer babies or to tamper with evolution appear to be based on misunderstanding, confusion and sometimes just sheer emotions. However there are, no doubt, some serious questions and concerns in relation to in utero gene therapy, which need to be addressed both from a scientific, as well as from an ethical point of view.
1. Should fetal gene therapy be preferred over postnatal gene therapy?
2. Should fetal gene therapy be preferred over pre-implantation selection or abortion?
3. What is the scientific background to justify fetal somatic gene therapy?
4. What are the risks of inadvertent germ-line gene transfer?
5. What are the risks to fetus and mother?
6. Does fetal gene therapy infringe the right to abortion?
7. What is the legal status of the fetus and how does fetal gene therapy conform with informed consent?
_
Should fetal gene therapy be preferred over postnatal gene therapy?
Obviously, prenatal gene therapy is not to be seen as an alternative to postnatal gene therapy. It would, however, broaden the potential of gene therapy with a clear orientation to early prevention of severe genetic disease. The immediate future application would be for life-threatening monogenic diseases, caused by the absence or inactivation of an essential gene product. The gene defect would have to be confirmed by accurate prenatal diagnosis and expression of the corrective gene would preferably not require fine gene regulation. Initially in utero gene therapy would be particularly relevant for diseases presenting early in life for which no curative postnatal treatment is available and in those that cause irreversible damage to the brain before birth, e.g. some storage diseases. However, for many less severe conditions, the safety, ease and efficiency of the procedures will finally determine whether prenatal or postnatal application is preferable and which of them for which disease.
_
Should fetal gene therapy be preferred over pre-implantation selection or abortion?
Provided that it is effective and safe there should be no question that it would be preferable to abortion and certainly much less demanding and expensive than pre-implantation selection. It should also be remembered that pre-implantation selection requires prior knowledge of the genetic status of the parents before conception and a lengthy and strenuous procedure before selected embryos can be implanted, while fetal gene therapy could be combined with early pregnancy screening for specific genetic diseases.
_
What is the scientific background to justify fetal somatic gene therapy?
Effectiveness and safety are certainly the main criteria that will determine if and when fetal gene therapy can be considered as a scientifically sound and ethically acceptable approach to dealing with a genetic condition. This assessment will depend on the development of vector systems, the means of application as tested in animal models and of course on the target disease.
_
What are the risks to fetus and mother?
Of course in utero gene delivery does carry some specific risks not encountered in postnatal gene delivery. Similar to most obstetric interventions they concern the mother, as well as the fetus, with a bias for life and well-being clearly in preference of the mother. These risks are infection, fetal loss and preterm labour as a consequence of the intervention. A more hypothetical risk concerns the possibility that a certain gene product, which is required later in life or a vector system, may be particularly harmful to the fetus or that the insertion of vector sequences into the genome may cause developmental aberrations. These potential risks will be investigated by careful monitoring for any sign of birth defects following in utero manipulation. However, the main reason that fetal gene therapy, in contrast to adult gene therapy, is not yet at the stage of clinical trials has in our opinion, very little to do with all the perceived dangers of fetal gene therapy per se. This reason is the known inefficiency of almost all present gene therapy approaches, in contrast to a 100% effective preventive alternative, namely abortion! Postnatally this alternative does not exist and therapy of whatever kind seems appropriate is mandatory. In some cases, when it is the last resort and the only alternative to death, it even becomes acceptable in spite of a high risk and low chance of effect. Since termination is a reasonably safe maternal option to deal with an inherited genetic disease, any in utero gene therapy will be expected to be highly reliable in preventing this disease and not causing additional damage. During the introductory phase of transferring this technology to humans, this danger may not be easily ascertained and will require particular care with respect to informed maternal consent based on detailed counseling and the understanding of risks versus benefits. We see this as the main specific ethical issue in fetal gene therapy.
_
There is a potential for inadvertent gene transfer into germ cells and the possible effect on subsequent generations. The possibility of inadvertent germline transformation is not a new concern nor is it specific to prenatal gene therapy, as adult gene therapy is also subject to the danger of germline integration. The only published long-term study of retrovirus-mediated gene delivery to fetuses has indicated that germline transmission does not occur. To put this issue into perspective, it should be compared with the iatrogenic germline mutations caused by high-dose chemotherapy. Rightfully, no ethical objections have been raised against such treatment or against procreation by treated individuals. James Wilson has calculated the cumulative probability of prenatal gene transfer leading to germ cell transformation, transfer to the next generation and a negative outcome on subsequent generations to be extremely low. The risk of inadvertent germline transmission deserves attention and investigation, but certainly no more than any other risk associated with gene therapy.
__________
__________
In a nutshell, gene therapy can be classified depending on various factors as seen in the figure below:
__________
__________
Gene therapy to prevent disease passed from mother to child: prevent mitochondrial diseases:
_
_
Cell mitochondria contain genetic material just like the cell nucleus and these genes are passed from mother to infant. When certain mutations in mitochondrial DNA are present, a child can be born with severe conditions, including diabetes, deafness, eye disorders, gastrointestinal disorders, heart disease, dementia and several other neurological diseases. Because mitochondrial-based genetic diseases are passed from one generation to the next, the risk of disease is often quite clear. The goal of this research is to develop a therapy to prevent transmission of these disease-causing gene mutations. To conduct this research, Mitalipov and his colleagues obtained 106 human egg cells from study volunteers and then used a method developed in nonhuman primate studies, to transfer the nucleus from one cell to another. In effect, the researchers “swapped out” the cell cytoplasm, which contains the mitochondria. The egg cells were then fertilized to determine whether the transfer was a success and whether the cells developed normally. Upon inspection, it was demonstrated that it was possible to successfully replace mitochondrial DNA using this method. Using this process, researchers have shown that mutated DNA from the mitochondria can be replaced with healthy copies in human cells. While the human cells in their study were allowed to develop to the embryonic stem cell stage, this research shows that this gene therapy method may well be a viable alternative for preventing devastating diseases passed from mother to infant. The Nature paper also expanded upon the previously reported nonhuman primate work by demonstrating that the method was possible using frozen egg cells. Mitochondria were replaced in a frozen/thawed monkey egg cell, resulting in the birth of a healthy baby monkey named Chrysta. The second portion of the study, which was completed at ONPRC, is also considered an important achievement because egg cells only remain viable for a short period of time after they are harvested from a donor. Therefore, for this therapy to be a viable option in the clinic, preservation through freezing likely is necessary so that both the donor cell and a mother’s cell are viable at the time of the procedure. While this form of therapy has yet to be approved in the United States, the United Kingdom is seriously considering its use for treating human patients at risk for mitochondria-based disease. It’s believed that this most recent breakthrough, combined with earlier animal studies, will help inform that decision-making process.
_
__________
DNA vaccines:
A variation of gene therapy with somatic cells is the introduction of genes (naked DNA), with the objective of triggering the immune system to produce antibodies for certain infectious diseases, cancer, or some autoimmune diseases. Therefore, the objective is not repair of a defective gene in the individual’s genome. Those genes can be introduced via intramuscular injections, inhalation, or oral ingestion. Cells that take up the gene in their genome can express the protein that stimulates the immune system to act against the disease. DNA vaccination is a technique for protecting an organism against disease by injecting it with genetically engineered DNA to produce an immunological response. Nucleic acid vaccines are still experimental, and have been applied to a number of viral, bacterial and parasitic models of disease, as well as to several tumour models. DNA vaccines have a number of advantages over conventional vaccines, including the ability to induce a wider range of immune response types. DNA vaccines are third generation vaccines, and are made up of a small, circular piece of bacterial DNA (called a plasmid) that has been genetically engineered to produce one or two specific proteins (antigens) from a pathogen. The vaccine DNA is injected into the cells of the body, where the “inner machinery” of the host cells “reads” the DNA and uses it to synthesize the pathogen’s proteins. Because these proteins are recognised as foreign, when they are processed by the host cells and displayed on their surface, the immune system is alerted, which then triggers a range of immune responses. These DNA vaccines developed from “failed” gene therapy experiments. The first demonstration of a plasmid-induced immune response was when mice inoculated with a plasmid expressing human growth hormone elicited antibodies instead of altering growth.
_
This approach offers a number of potential advantages over traditional approaches, including the stimulation of both B- and T-cell responses, improved vaccine stability, the absence of any infectious agent and the relative ease of large-scale manufacture. As proof of the principle of DNA vaccination, immune responses in animals have been obtained using genes from a variety of infectious agents, including influenza virus, hepatitis B virus, human immunodeficiency virus, rabies virus, lymphocytic chorio-meningitis virus, malarial parasites and mycoplasmas. In some cases, protection from disease in animals has also been obtained. However, the value and advantages of DNA vaccines must be assessed on a case-by-case basis and their applicability will depend on the nature of the agent being immunized against, the nature of the antigen and the type of immune response required for protection. The field of DNA vaccination is developing rapidly. Vaccines currently being developed use not only DNA, but also include adjuncts that assist DNA to enter cells, target it towards specific cells, or that may act as adjuvants in stimulating or directing the immune response. Ultimately, the distinction between a sophisticated DNA vaccine and a simple viral vector may not be clear. Many aspects of the immune response generated by DNA vaccines are not understood.
_
DNA vaccines can furthermore be divided into two groups: (1) prophylactic vaccines, which serves at creating an immune response against a known infectious agent, and (2) therapeutic vaccines, which aims at using the body’s immune system to react adequately to a tumor antigen e.g., in order to achieve an anticancer effect.
_
Advantages of DNA vaccine:
DNA immunization offers many advantages over the traditional forms of vaccination. It is able to induce the expression of antigens that resemble native viral epitopes more closely than standard vaccines do since live attenuated and killed vaccines are often altered in their protein structure and antigenicity. Plasmid vectors can be constructed and produced quickly and the coding sequence can be manipulated in many ways. DNA vaccines encoding several antigens or proteins can be delivered to the host in a single dose, only requiring a microgram of plasmids to induce immune responses. Rapid and large-scale production are available at costs considerably lower than traditional vaccines, and they are also very temperature stable making storage and transport much easier. Another important advantage of genetic vaccines is their therapeutic potential for ongoing chronic viral infections. DNA vaccination may provide an important tool for stimulating an immune response in HBV, HCV and HIV patients. The continuous expression of the viral antigen caused by gene vaccination in an environment containing many antigen-presenting cells may promote successful therapeutic immune response which cannot be obtained by other traditional vaccines (Encke et al, 1999). This is a subject that has generated a lot of interest in the last five years.
Limitations of DNA vaccine:
The greatest challenge in this procedure is the transient effect of gene expression, because the modified cells can go through only a limited number of divisions before dying. Another challenge is the low efficiency of gene incorporation and expression in the target cells. Although in some cases the temporary gene expression is enough to trigger an effective immune response, most cases require a more lasting gene expression. Although DNA can be used to raise immune responses against pathogenic proteins, certain microbes have outer capsids that are made up of polysaccharides. This limits the extent of the usage of DNA vaccines because they cannot substitute for polysaccharide-based subunit vaccines.
__________
Utility of gene therapy in diseases:
_
Gene therapy as a “premature technology”:
Gene therapy fits the model of a “premature technology”. A field of biomedical science is said to be scientifically or technologically premature when despite the great science and exciting potential of the field, any practicable therapeutic applications are in the distant future, due to difficult hurdles in applying the technology. Moving a premature technology up the development curve requires the development of enabling technologies that can allow researchers and product developers to overcome the hurdles. The classic case of a premature technology that has moved up the development curve and become successful is the field of therapeutic monoclonal antibodies. I hope gene therapy follows the suit.
_
What kinds of diseases does gene therapy treat?
Characteristics of diseases amenable to gene therapy include those for which there is not current effective treatment, those with a known cause (such as a defective gene), those that have failed to improve or have become resistant to conventional therapy, and/or cases where current therapy involves long term administration of an expensive therapeutic agent or an invasive procedure. Gene therapy has the potential for high therapeutic gain for a broad range of diseases. Such diseases, for example would be those caused by a mutation in a single gene where an accessible tissue is available, such as bone marrow, and with the genetically modified cell ideally having a survival advantage. However, patients with similar symptoms may have mutations in different gene(s) involved in the same biological process. For example, patients with hemophilia A have a mutation in blood clotting Factor VIII whereas patients with hemophilia B have a mutation in Factor IX. So it is important to know which gene is mutated in a particular patient, as well as whether they produce an inactive protein which can help to avoid immune rejection of the normal protein. Gene therapy also offers a promising alternative or adjunct treatment for symptoms of many acquired diseases, such as cancer, rheumatoid arthritis, diabetes, Parkinson’s disease, Alzheimer’s disease, etc. Cancer is the most common disease in gene therapy clinical trials. Cancer gene therapy focuses on eliminating the cancer cells, blocking tumor vascularization and boosting the immune response to tumor antigens. Many gene therapy approaches are being explored for the treatment of a variety of acquired diseases. More details are listed under the different diseases (vide infra).
_
Current Areas of gene therapy:
Although gene therapy is still experimental, many diseases have been targets for gene therapy in clinical trials. Some of these trials have produced promising results. Diseases that may be treated successfully in the future with gene therapy include (but are not limited to):
Genetic diseases for which gene therapy is advocated:
1) Duchenne Muscular dystrophy
2) Cystic fibrosis
3) Familial hypercholesterolemia
4) Hemophilia
5) Haemoglobinopathies
6) Gaucher’s disease
7) Albinism
8) Phenyl ketonuria.
_
Acquired diseases for which gene therapy is advocated include Cancers, Infectious diseases, HIV, Neurological disorders, Cardiovascular diseases, Rheumatoid arthritis and Diabetes mellitus.
_
Although early clinical failures led many to dismiss gene therapy as over-hyped, clinical successes since 2006 have bolstered new optimism in the promise of gene therapy. These include successful treatment of patients with the retinal disease Leber’s congenital amaurosis, X-linked SCID, ADA-SCID, adrenoleukodystrophy, chronic lymphocytic leukemia (CLL), acute lymphocytic leukemia (ALL), multiple myeloma, haemophilia and Parkinson’s disease. These clinical successes have led to a renewed interest in gene therapy, with several articles in scientific and popular publications calling for continued investment in the field and between 2013 and April 2014, US companies invested over $600 million in gene therapy. In 2012, Glybera became the first gene therapy treatment to be approved for clinical use in either Europe or the United States after its endorsement by the European Commission.
_
There are many conditions that must be met in order to allow gene therapy to be possible. First, the details of the disease process must be understood. Of course, scientists must know exactly what gene is defective, but also when and at what level that gene would normally be expressed, how it functions, and what the regenerative possibilities are for the affected tissue. Not all diseases can be treated by gene therapy. It must be clear that replacement of the defective gene would benefit the patient. For example, a mutation that leads to a birth defect might be impossible to treat, because irreversible damage will have already occurred by the time the patient is identified. Similarly, diseases that cause death of brain cells are not well suited to gene therapy: Although gene therapy might be able to halt further progression of disease, existing damage cannot be reversed because brain cells cannot regenerate. Additionally, the cells to which DNA needs to be delivered must be accessible. Finally, great caution is warranted as gene therapy is pursued, as the body’s response to high doses of viral vectors can be unpredictable. On September 12, 1999, Jesse Gelsinger, an eighteen-year old participant in a clinical trial in Philadelphia, became unexpectedly ill and died from side effects of liver administration of adenovirus. This tragedy illustrates the importance of careful attention to safety regulations and extensive experiments in animal model systems before moving to human clinical trials.
_
___________
___________
Conditions for which human gene transfer trials have been approved:
| Monogenic disorders: | Cancer: |
| Adrenoleukodystrophy | Gynaecological – breast, ovary, cervix, vulva |
| α-1 antitrypsin deficiency | Nervous system – glioblastoma, leptomeningeal carcinomatosis, glioma, astrocytoma, neuroblastoma, retinoblastoma |
| Becker muscular dystrophy | |
| β-thalassaemia | Gastrointestinal – colon, colorectal, liver metastases, post-hepatitis liver cancer, pancreas, gall bladder |
| Canavan disease | Genitourinary – prostate, renal, bladder, anogenital neoplasia |
| Chronic granulomatous disease | |
| Cystic fibrosis | Skin – melanoma (malignant/metastatic) |
| Duchenne muscular dystrophy | Head and neck – nasopharyngeal carcinoma, squamous cell carcinoma, oesophaegeal cancer |
| Fabry disease | Lung – adenocarcinoma, small cell/nonsmall cell, mesothelioma |
| Familial adenomatous polyposis | Haematological – leukaemia, lymphoma, multiple myeloma |
| Familial hypercholesterolaemia | Sarcoma |
| Fanconi anaemia | Germ cell |
| Galactosialidosis | Li–Fraumeni syndrome |
| Gaucher’s disease | Thyroid |
| Gyrate atrophy | Neurological diseases: |
| Haemophilia A and B | Alzheimer’s disease |
| Hurler syndrome | Amyotrophic lateral sclerosis |
| Hunter syndrome | Carpal tunnel syndrome |
| Huntington’s chorea | Cubital tunnel syndrome |
| Junctional epidermolysis bullosa | Diabetic neuropathy |
| Late infantile neuronal ceroid lipofuscinosis | Epilepsy |
| Leukocyte adherence deficiency | Multiple sclerosis |
| Limb girdle muscular dystrophy | Myasthenia gravis |
| Lipoprotein lipase deficiency | Parkinson’s disease |
| Mucopolysaccharidosis type VII | Peripheral neuropathy |
| Ornithine transcarbamylase deficiency | Pain |
| Pompe disease | Ocular diseases: |
| Purine nucleoside phosphorylase deficiency | Age-related macular degeneration |
| Recessive dystrophic epidermolysis bullosa | Diabetic macular edema |
| Sickle cell disease | Glaucoma |
| Severe combined immunodeficiency | Retinitis pigmentosa |
| Tay Sachs disease | Superficial corneal opacity |
| Wiskott–Aldrich syndrome | Choroideraemia |
| Cardiovascular disease: | Leber congenital amaurosis |
| Anaemia of end stage renal disease | Inflammatory diseases: |
| Angina pectoris (stable, unstable, refractory) | Arthritis (rheumatoid, inflammatory, degenerative) |
| Coronary artery stenosis | Degenerative joint disease |
| Critical limb ischaemia | Ulcerative colitis |
| Heart failure | Severe inflammatory disease of the rectum |
| Intermittent claudication | Other diseases: |
| Myocardial ischaemia | Chronic renal disease |
| Peripheral vascular disease | Erectile dysfunction |
| Pulmonary hypertension | Detrusor overactivity |
| Venous ulcers | Parotid salivary hypofunction |
| Infectious disease: | Oral mucositis |
| Adenovirus infection | Fractures |
| Cytomegalovirus infection | Type I diabetes |
| Epstein–Barr virus | Diabetic ulcer/foot ulcer |
| Hepatitis B and C | Graft versus host disease/transplant patients |
| HIV/AIDS | |
| Influenza | |
| Japanese encephalitis | |
| Malaria | |
| Paediatric respiratory disease | |
| Respiratory syncytial virus | |
| Tetanus | |
| Tuberculosis |
__________
__________
Glybera: The only approved gene therapy:
Lipoprotein lipase deficiency is caused by a mutation in the gene which codes lipoprotein lipase. As a result, afflicted individuals lack the ability to produce lipoprotein lipase enzymes necessary for effective breakdown of fat. The disorder affects about 1 out of 1,000,000 people. Lipoprotein lipase deficiency is an extremely rare type of hyperlipoproteinaemia characterised by massive accumulation of chylomicrons in plasma. This disorder is often diagnosed accidentally when lipaemic serum is noticed. Lipaemia retinalis or a creamy white retinal vessel on fundoscopy is a unique feature of this disorder. Familial lipoprotein lipase (LPL) deficiency usually presents in childhood and is characterized by very severe hypertriglyceridemia with episodes of abdominal pain, recurrent acute pancreatitis, eruptive cutaneous xanthomata, and hepatosplenomegaly. Clearance of chylomicrons from the plasma is impaired, causing triglycerides to accumulate in plasma and the plasma to have a milky (“lactescent” or “lipemic”) appearance. Symptoms usually resolve with restriction of total dietary fat to 20 grams/day or less. Fat-soluble vitamins A, D, E, and K and mineral supplements are recommended for people who eat a very low-fat diet. Alipogene tiparvovec (marketed under the trade name Glybera) is a gene therapy treatment that compensates for lipoprotein lipase deficiency (LPLD), which can cause severe pancreatitis. Therapy consists of multiple intramuscular injections of the product, resulting in the delivery of functional LPL genes to muscle cells. In July 2012, the European Medicines Agency recommended it for approval, the first recommendation for a gene therapy treatment in either Europe or the United States. The recommendation was endorsed by the European Commission in November 2012 and commercial rollout is expected in late 2013. The adeno-associated virus serotype 1 (AAV1) viral vector delivers an intact copy of the human lipoprotein lipase (LPL) gene. Data from the clinical trials indicates that fat concentrations in blood were reduced between 3 and 12 weeks after injection, in nearly all patients. The advantages of AAV include apparent lack of pathogenicity, delivery to non-dividing cells, and non-integrating in contrast to retroviruses, which show random insertion with accompanying risk of cancer. AAV also presents very low immunogenicity, mainly restricted to generating neutralizing antibodies, and little well defined cytotoxic response. The cloning capacity of the vector is limited to replacement of the virus’s 4.8 kilobase genome. Alipogene tiparvovec is expected to cost around $1.6 million for treatment which will make it the most expensive medicine in the world.
_________
Diseases caused by single gene mutations:
Diseases caused by a single defective gene represented an early target for corrective gene therapy. Diseases such as Duchenne muscular dystrophy (DMD) and cystic fibrosis (CF) have well established aetiologies and pathophysiologies, with clearly defined genetic mutations.
_
Cystic fibrosis:
CF is caused by mutations in a gene on chromosome 7, named cystic fibrosis transmembrane regulator (CFTR). This 230 kb gene encodes a 1480 amino acid protein that acts as a membrane chloride channel. As many as six different mutation types and 1000 specific mutations have been identified, and vary in frequency worldwide. The defect results in changes in multiple organ systems, most notably the lungs and pancreas, producing chronic lung infection, pancreatic insufficiency, and diabetes mellitus. The median survival in 2000 was 32 years. Restoration of the wild type CFTR could be curative. The first phase I clinical trials ever conducted using adenoviral vectors and AAV vectors involved the transfer of CFTR to CF patients. Trials using first and second generation adenoviral vectors have been limited by the inability to repeatedly administer the virus. The transient nature of the viral expression vector requires such a strategy, but the inflammation induced by these vectors prevented this. Early trials using AAV did not induce inflammation, but failed to demonstrate effective levels of transferred CFTR expression. Target Genetics Corporation developed an adenoassociated virus tgAAVCF virus, expressing the CFTR gene, and has administered it to patients in an aerosolised form. Results showed that a single administration of the virus was well tolerated and safe, but virus derived CFTR expression was not detected in patients. Clinical efficacy was not reported. Phase II trials have also been reported using the same vector delivered to the maxillary sinuses of CF patients. Results confirmed the safety of tgAAVCF administration, but again failed to detect expression of the transferred CFTR gene in biopsy specimens and failed to demonstrate clinical improvement in treated patients. A phase I trial has recently been published using a second generation AAV (rAAV2) expressing CFTR. Result indicated that a single administration of the virus was safe with escalating virus concentration; however, the number of cells in the airway expressing the viral CFTR was limited and they contained a low copy number. Both results indicate inefficient transfer of genetic material using this virus. A phase IIb trial is underway to determine if the therapy improves lung function in CF patients. Similarly, early clinical trials using several different cationic lipid preparations were deemed safe and allowed for repeated administration of CFTR, but were inefficient in transferring the gene, and failed to demonstrate efficacy. Finally, a clinical trial is being undertaken by Copernicus Therapeutics Inc, using a novel method that allows for compaction of a single molecule of DNA condensed to the minimal possible volume. The small volume, positively charged particle is able to pass through cellular and nuclear membrane pores and allows delivery of genetic material to non-dividing cells. Transfer of genes using this technology has proven to be safe in animals, and subsequent phase I clinical trials in CF patients have been completed. In the study, patients received compacted DNA containing CFTR via the nasal passages. Results indicated that the administration is safe and tolerable. The treatment efficacy is not noted in the phase I trial. A phase II, multicentre, double blind, placebo controlled study is underway.
_
Duchenne muscular dystrophy:
DMD, the most prevalent muscular dystrophy, is caused by large deletions or insertions of the dystrophin gene. This very large gene (the mature mRNA measures 14.0 kilobases) encodes a 3685 amino acid protein that stabilises the muscle cell membrane. Its dysfunction results in destabilisation and subsequent degeneration of muscle tissue. As with CF, DMD is potentially curable with extensive transfer of the wild type dystrophin gene to muscle tissue. In a similar fashion, strategies are limited due to the large size of the dystrophin gene. Currently, a phase I trial has been initiated using plasmid dystrophin DNA. The naked plasmid is directly injected into the radial muscle in an attempt to determine tolerability and safety as well as gene expression. Results have yet to be published. More promising clinical trials should be undertaken using viral vectors to produce “exon skipping” of mutated sequences of the dystrophin gene. Gene therapy requires delivery of a new gene to the vast majority of muscles in the body—a daunting challenge, since muscle tissues makes up >40% of body mass. Most current research is focused on identifying the correct version of a gene to deliver, and on developing methods for safe and efficient delivery to muscle. Neither task is simple: many of these genes are enormous and display complex expression patterns, and successful delivery must overcome considerable physical and immunological barriers. Over the past 10 years, the concept of gene therapy for muscular dystrophy has gone from a distant dream to an idea moving rapidly towards clinical trials of safety. During this time, it has become possible to shrink the dystrophin gene from 2.4 Mb to 3.5 kb without a significant loss of functionality. Numerous vectors are now available that can hold these expression cassettes and transduce muscle tissue with minimal immunological or toxic side-effects. A major challenge to an effective treatment remains the need for an efficient, systemic delivery system. Coupled with intriguing advances in alternate areas of study, the possibility of a treatment for DMD and other forms of MD is no longer such a distant challenge.
_
SCID (severe combined immunodeficiency):
The two types of SCID that have been treated by gene therapy are ADA-SCID, caused by disabling mutations in the Adenosine Deaminase gene on chromosome 20, and X-SCID, caused by disabling mutations in the IL-2 receptor gamma chain gene on X chromosome, also called the common gamma chain ( c). ADA or c deficient patients have no T-lymphocytes (the cells that recognize foreign proteins and few or dysfunctional B-cells (the cells that make antibodies). SCID patients are therefore unable to mount an immune response to common pathogens, and unless treated usually die early in life from severe infections. The treatment of choice for these patients is a bone marrow transplant from the parent with the best immunological match. If there is not a matched parent (~25% of the time) or the transplant is unsuccessful (~25% of the time) these patients are candidates for gene therapy. Gutted viruses containing the ADA or c genes are introduced into the patient’s bone marrow cells and the treated cells are returned to the patient. In some recent cases of ADA deficient SCID, the infusion was preceded by a mild depletion of the patient’s bone marrow cells. In these early studies, it was clearly demonstrated that bone marrow stem cells were marked with the new gene, and that the transferred gene made either ADA or c. In several ADA SCID patients that also received mild bone marrow depletion, enough ADA producing T and B cells emerged that these patients no longer need the supplemental injection of purified ADA enzyme. In the XSCID patients, 10/11 children began to produce functional T-cells and developed antibodies when vaccinated against the common childhood diseases. Recently two of these patients have developed a T-cell leukemia that is associated with the insertion of the c gene into a known leukemia gene, resulting in a moratorium on further attempts to perform gene therapy for X-SCID.
_
Gene Therapy for Immunodeficiency due to Adenosine Deaminase deficiency: A study:
Researchers investigated the long-term outcome of gene therapy for severe combined immunodeficiency (SCID) due to the lack of adenosine deaminase (ADA), a fatal disorder of purine metabolism and immunodeficiency. They infused autologous CD34+ bone marrow cells transduced with a retroviral vector containing the ADA gene into 10 children with SCID due to ADA deficiency who lacked an HLA-identical sibling donor, after nonmyeloablative conditioning with busulfan. Enzyme-replacement therapy was not given after infusion of the cells. All patients are alive after a median follow-up of 4.0 years (range, 1.8 to 8.0). Transduced hematopoietic stem cells have stably engrafted and differentiated into myeloid cells containing ADA (mean range at 1 year in bone marrow lineages, 3.5 to 8.9%) and lymphoid cells (mean range in peripheral blood, 52.4 to 88.0%). Eight patients do not require enzyme-replacement therapy, their blood cells continue to express ADA, and they have no signs of defective detoxification of purine metabolites. Nine patients had immune reconstitution with increases in T-cell counts (median count at 3 years, 1.07×10^9 per liter) and normalization of T-cell function. In the five patients in whom intravenous immune globulin replacement was discontinued, antigen-specific antibody responses were elicited after exposure to vaccines or viral antigens. Effective protection against infections and improvement in physical development made a normal lifestyle possible. Serious adverse events included prolonged neutropenia (in two patients), hypertension (in one), central-venous-catheter–related infections (in two), Epstein–Barr virus reactivation (in one), and autoimmune hepatitis (in one). Gene therapy, combined with reduced-intensity conditioning, is a safe and effective treatment for SCID in patients with ADA deficiency.
__
Gene Therapy benefits persist in SCID:
Gene therapy appears to have long-term success for treating X-linked severe combined immunodeficiency disease (SCID) — but recipients are at risk for acute leukemia, according to a small study from France. After approximately 10 years of follow-up, eight of nine SCID patients who underwent gene therapy for the lethal inherited disease were alive and living in a normal, unprotected environment, according to Salima Hacein-Bey-Abina, PharmD, PhD, of Necker-Enfants Malades Hospital in Paris, and colleagues. However, four of the children developed T-cell acute lymphoblastic leukemia, which was treated successfully in three of them, the researchers reported in the New England Journal of Medicine. Two short-term studies involving a total of 20 SCID patients have previously demonstrated benefits with gene therapy, and the French group has now followed their patients for up to 11 years, with only one death. Patients were given the gene therapy at a median age of seven months, by means of an infusion of autologous bone marrow-derived CD34+ cells transduced with the γ chain-containing retroviral vector. The children remained in a sterile unit for 45 to 90 days. Infections occurring after treatment included varicella zoster, recurrent rhinitis, and bronchitis — but all of the surviving children exhibited normal growth. Within two to five months after therapy, T-cell counts had reached the normal range for age. Transduced T-cells were detected for up to 10.7 years after therapy, and seven patients — including the three who survived leukemia — had all sustained immune reconstitution. In all but one patient, the CD4+ T-cell subset reached normal values for age during the first two years, remaining normal in four patients and slightly below normal in three. In addition, all patients had normal CD8+ T-cell counts throughout follow-up. B-cell counts, which were high before treatment, decreased to normal values. Serum levels of IgG, IgA, and IgM derived from B cells were normal or close to normal in most patients, and only three required immunoglobulin-replacement therapy to prevent bacterial infections. This outcome strongly suggests that in vivo B-cell immunity was preserved to some extent, as shown by the sustained presence of all serum immunoglobulin isotypes, detectable antibody responses to polysaccharide antigens (in some patients), and the presence of memory B cells with somatic mutations in the immunoglobulin-variable-region genes. Responses to vaccinations were inconsistent. All but one patient had antibodies against poliovirus, tetanus, and diphtheria three months after a third immunization, but titers subsequently varied. T-cell reconstitution was similar to that seen in patients who have undergone hematopoietic stem-cell transplantation, in terms of phenotypic and functional characteristics. The authors concluded that gene therapy may be an option for patients with SCID who lack an HLA-identical donor, resulting in long-term correction of the immune system. However, they stressed that risk of leukemia resulting from oncogene transactivation by the vector’s transcriptional control elements cannot be ignored. Their results set the stage for trials with safer vectors in the treatment of SCID-X1 and other severe forms of inherited diseases of the hematopoietic system.
_
Down syndrome: Gene-silencing strategy opens new path to understanding Down syndrome:
The first evidence that the underlying genetic defect responsible for trisomy 21, also known as Down syndrome, can be suppressed in laboratory cultures of patient-derived stem cells was presented at the American Society of Human Genetics 2013 annual meeting in Boston. People with Down syndrome are born with an extra chromosome 21, which results in a variety of physical and cognitive ill effects. In laboratory cultures of cells from patients with Down syndrome, an advanced genome editing tool was successfully used to silence the genes on the extra chromosome, thereby neutralizing it, said Jeanne Lawrence, Ph.D., Professor of Cell & Developmental Biology at the University Massachusetts Medical School, Worcester, MA. Dr. Lawrence and her team compared trisomic stem cells derived from patients with Down syndrome in which the extra chromosome 21 was silenced to identical cells from patients that were untreated. The researchers identified defects in the proliferation, or rapid growth, of the untreated cells and the differentiation, or specialization, of untreated nervous system cells. These defects were reversed in trisomic stem cells in which the extra chromosome 21 was muted.
_
Hemophilia:
Hemophilia patients have long been treated by the infusion of the missing clotting proteins, but this treatment is extremely expensive and requires almost daily injections. Gene therapy holds great promise for these patients, because replacement of the gene that makes the missing protein could permanently eliminate the need for protein injections. It really does not matter what tissue produces these clotting factors as long as the protein is delivered to the bloodstream, so researchers have tried to deliver these genes to muscle and to the liver using several different vectors. Approaches using recombinant adenoviruses to deliver the clotting factor gene to the liver are especially promising, and tests have shown significant clinical improvement in a dog model of hemophilia.
_
Gene therapy for hemophilia B:
Medical researchers in Britain have successfully treated six patients suffering from the blood-clotting disease known as hemophilia B by injecting them with the correct form of a defective gene, a landmark achievement in the troubled field of gene therapy. Hemophilia B, which was carried by Queen Victoria and affected most of the royal houses of Europe, is the first well-known disease to appear treatable by gene therapy, a technique with a 20-year record of almost unbroken failure. About 80 percent of hemophilia cases are of the type known as hemophilia A, which is caused by defects in a different blood-clotting agent, Factor VIII. Researchers have focused on hemophilia B, in part, because the Factor IX gene is much smaller and easier to work with. The success with hemophilia B, reported in The New England Journal of Medicine, embodies several minor improvements developed over many years by different groups of researchers. The delivery virus, carrying a good version of the human gene for the clotting agent known as Factor IX, was prepared by researchers at St. Jude Children’s Research Hospital in Memphis. The patients had been recruited and treated with the virus in England by a team led by Dr. Amit C. Nathwani of University College London; researchers at the Children’s Hospital of Philadelphia monitored their immune reactions. Hemophilia B is caused by a defect in the gene for Factor IX. Fatal if untreated, the disease occurs almost only in men because the Factor IX gene lies on the X chromosome, of which men have only a single copy. Women who carry a defective gene on one X chromosome can compensate with the good copy on their other X chromosome, but they bequeath the defective copy to half their children. About one in 30,000 of newborn boys have the disease, with about 3,000 patients in the United States. Dr. Nathwani and his team reported that they treated the patients by infusing the delivery virus into their veins. The virus homes in on the cells of the liver, and the gene it carries then churns out correct copies of Factor IX. A single injection enabled the patients to produce small amounts of Factor IX, enough that four of the six could stop the usual treatment, injections of Factor IX concentrate prepared from donated blood. The other two patients continued to need concentrate, but less frequently. Treating a patient with concentrate costs $300,000 a year, with a possible lifetime cost of $20 million, but the single required injection of the new delivery virus costs just $30,000, Dr. Katherine P. Ponder of the Washington University School of Medicine in St. Louis notes in her commentary in The New England Journal of Medicine, calling the trial “a landmark study.” The patients have continued to produce their own Factor IX for up to 22 months. The patient cannot be injected again with the same virus because his immune system is now primed to attack it. A serious problem with other delivery viruses is that they insert themselves randomly into chromosomes, sometimes disrupting a gene. The virus used by Dr. Nathwani’s team, known as adeno-associated virus-8, generally stays outside the chromosomes, so it should not present this problem. Still, patients will need to be monitored for liver cancer, a small possibility that has been observed in mice.
_
New gene therapy proves promising as hemophilia A treatment:
Researchers at the UNC School of Medicine and the Medical College of Wisconsin found that a new kind of gene therapy led to a dramatic decline in bleeding events in dogs with naturally occurring hemophilia A, a serious and costly bleeding condition that affects about 50,000 people in the United States and millions more around the world. Using a plasmapheresis machine and a blood-enrichment technique, the research team isolated specific platelet precursor cells from three dogs that have hemophilia A. The team then engineered those platelet precursor cells to incorporate a gene therapy vector that expresses factor VIII. The researchers put those engineered platelet precursors back into the dogs. As the cells proliferated and produced new platelets, more and more were found to express factor VIII. Then, nature took over. Platelets naturally discharge their contents at sites of vascular injury and bleeding. In this experiment, the contents included factor VIII. In the 2 1/2 years since the dogs received the gene therapy, researchers found that factor VIII was still being expressed in platelets that were coursing throughout the vascular systems of all three dogs. All three experienced much less bleeding. In the dog that expressed the most factor VIII in platelets, the bleeding was limited to just one serious event each year over the course of three years. And such bleeding events were easily treatable with current standard therapies. “This has been very successful,” Nichols said. “And now we want to explore the possibility of moving it into human clinical trials for people with hemophilia A, similar to what Paul Monahan and Jude Samulski at UNC are currently doing for people with hemophilia B, which is a deficiency of factor IX.” If approved, the platelet-targeted therapy would likely be restricted to patients who develop the antibody that stifles factor VIII therapy through normal injections. But as the gene therapy is refined, it could become a viable option for people with blood disorders who don’t have inhibitory antibodies.
_
Sickle cell disease:
Patients suffering from this disease have a defective hemoglobin protein in their red blood cells. This defective protein can cause their red blood cells to be misshapen, clogging their blood vessels and causing extremely painful and dangerous blood clots. Most of our genes make an RNA transcript, which is then used as a blueprint to make protein. In sickle cell disease, the transcript of the mutant gene needs to be destroyed or repaired in order to prevent the synthesis of mutant hemoglobin. The molecular repair of these transcripts is possible using special RNA molecules called ribozymes. There are several different kinds of ribozymes: some that destroy their targets, and others that modify and repair their target transcripts. The repair approach was tested in the laboratory on cells containing the sickle cell mutation, and was quite successful, repairing a significant fraction of the mutant transcripts. While patients cannot yet be treated using this technique, the approach illustrates how biologically damaging molecules can be inactivated.
_
Gene Therapy corrects Sickle Cell Disease in Laboratory Study by producing fetal hemoglobin in blood cells:
Using a harmless virus to insert a corrective gene into mouse blood cells, scientists at St. Jude Children’s Research Hospital have alleviated sickle cell disease pathology. In their studies, the researchers found that the treated mice showed essentially no difference from normal mice. Although the scientists caution that applying the gene therapy to humans presents significant technical obstacles, they believe that the new therapy will become an important treatment for the disease. Researchers have long known that symptoms of the disease could be alleviated by persistence in the blood of an immature fetal form of hemoglobin in red blood cells. This immature hemoglobin, which usually disappears after birth, does not contain beta-globin, but another form called gamma-globin. St. Jude researchers had found that treating patients with the drug hydroxyurea encourages the formation of fetal hemoglobin and alleviates disease symptoms. “While this is a very useful treatment for the disease, our studies indicated that it might be possible to cure the disorder if we could use gene transfer to permanently increase fetal hemoglobin levels,” said Derek Persons, M.D., Ph.D., assistant member in the St. Jude Department of Hematology. He and his colleagues developed a technique to insert the gene for gamma-globin into blood-forming cells using a harmless viral carrier. The researchers extracted the blood-forming cells, performed the viral gene insertion in a culture dish and then re-introduced the altered blood-forming cells into the body. The hope was that those cells would permanently generate red blood cells containing fetal hemoglobin, alleviating the disease. In the experiments, reported in the journal Molecular Therapy, the researchers used a strain of mouse with basically the same genetic defect and symptoms as humans with sickle cell disease. The scientists introduced the gene for gamma-globin into the mice’s blood-forming cells and then introduced those altered cells into the mice. The investigators found that months after they introduced the altered blood-forming cells, the mice continued to produce gamma-globin in their red blood cells. “When we examined the treated mice, we could detect little, if any, disease using our methods,” said Persons, the paper’s senior author. “The mice showed no anemia, and their organ function was essentially normal.” The researchers also transplanted the altered blood-forming cells from the original treated mice into a second generation of sickle cell mice to show that the gamma-globin gene had incorporated itself permanently into the blood-forming cells. Five months after that transplantation, the second generation of mice also showed production of fetal hemoglobin and correction of their disease. “We are very encouraged by our results,” Persons said. “They demonstrate for the first time that it is possible to correct sickle cell disease with genetic therapy to produce fetal hemoglobin. We think that increased fetal hemoglobin expression in patients will be well tolerated and the immune system would not reject the hemoglobin, in comparison to other approaches.” While Persons believes that the mouse experiments will lead to treatments in humans, he cautioned that technical barriers still need to be overcome. “It is far easier to achieve high levels of gene insertion into mouse cells than into human cells,” he said. “In our mouse experiments, we routinely saw one or two copies of the gamma-globin gene inserted into each cell. However, in humans this insertion rate is at least a hundred-fold less.”
_
Gene Therapy frees β-thalassemia patient from transfusions for more than 2 years:
Treating β-thalassemia with gene therapy has enabled a young adult patient who received his first transfusion at age 3 years to live without transfusions for more than 2 years. The report, published in Nature, also describes the partial dominance of a cell clone overexpressing a truncated HMGA2 mRNA, which has remained stable for 15 months. β-thalassemia is one of a group of β-hemoglobinopathies, the most common heritable diseases around the world. The disorder is caused by a recessive genetic mutation leading to nonproduction or reduced production of β-globin, which makes up 2 of the 4 globin chains in human hemoglobin. The deficit of normally functioning hemoglobin results in fewer mature red blood cells and anemia. Most β-thalassemia patients originate from India, central or southeast Asia, the Mediterranean region, the Middle East, or northern Africa. This study focused on compound βE/β0-thalassemia, more common in southeast Asia, in which 1 allele (β0) is nonfunctioning and the other (βE) is a mutant allele whose mRNA may either be spliced correctly (producing a mutated βE-globin) or incorrectly (producing no β-globin). This genotype causes a severe thalassemia, with half of the affected patients requiring transfusions. Gene therapy for β-thalassemia is being pursued by several groups around the world.
_
A Phase I/II Clinical Trial of β-Globin Gene Therapy for β-Thalassemia:
Recent success in the long-term correction of mouse models of human β-thalassemia and sickle cell anemia by lentiviral vectors and evidence of high gene transfer and expression in transduced human hematopoietic cells have led to a first clinical trial of gene therapy for the disease. A LentiGlobin vector containing a β-globin gene (βA-T87Q) that produces a hemoglobin (HbβA-T87Q) that can be distinguished from normal hemoglobin will be used. The LentiGlobin vector is self-inactivating and contains large elements of the β-globin locus control region as well as chromatin insulators and other features that should prevent untoward events. The study will be done in Paris with Eliane Gluckman as the principal investigator and Philippe Leboulch as scientific director.
_________
Cancer and gene therapy:
Cancer:
The second leading cause of death in the USA is cancer, with cancer deaths approaching 500 000 annually, and one million cases of cancer diagnosed each year. Current methods of treatment, including chemotherapy, radiation therapy, and surgical debulking, are generally only effective for early stage disease. The more advanced the disease, the less effective the therapy becomes. Furthermore, the side effect profile of chemotherapy is horrifying and many treatment failures are due to intolerable side effects and the inability to continue with an entire treatment course. Cancer is an abnormal, uncontrolled growth of cells due to gene mutations and can arise in most cells. No single mutation is found in all cancers. In healthy adults, the immune system may recognize and kill the cancer cells; unfortunately, cancer cells can sometimes evade the immune system resulting in expansion and spread of these cancer cells leading to serious life threatening disease. Approaches to cancer gene therapy include three main strategies: the insertion of a normal gene into cancer cells to replace a mutated gene, genetic modification to silence a mutated gene, and genetic approaches to directly kill the cancer cells. Furthermore, approaches to cellular cancer therapy currently largely involve the infusion of immune cells designed to either (i) replace most of the patient’s own immune system to enhance the immune response to cancer cells, (ii) activate the patient’s own immune system (T cells or Natural Killer cells) to kill cancer cells, or (iii) to directly find and kill the cancer cells. Many gene therapy clinical trials have been initiated since 1988 to treat cancer.
_
Researchers are testing several ways of applying gene therapy to the treatment of cancer:
1. Replace missing or non-functioning genes. For example, p53 is a gene called a “tumor suppressor gene.” Its job is just that: to suppress tumors from forming. Cells that are missing this gene or have a non-functioning copy due to a mutation may be “fixed” by adding functioning copies of p53 to the cell.
2. Oncogenes are mutated genes that are capable of causing either development of a new cancer, or the spread of an existing cancer (metastasis). By stopping the function of these genes, the cancer and/or its spread of cancer may be stopped.
3. Use the body’s own immune system by inserting genes into cancer cells that then trigger the body to attack the cancer cells as foreign invaders.
4. Insert genes into cancer cells to make them more susceptible to or prevent resistance to chemotherapy, radiation therapy, or hormone therapies.
5. Create “suicide genes” that can enter cancer cells and cause them to self-destruct.
6. Cancers require a blood supply to grow and survive, and they form their own blood vessels to accomplish this. Genes can be used to prevent these blood vessels from forming, thus starving the tumor to death (also called anti-angiogenesis).
7. Use genes to protect healthy cells from the side effects of therapy, allowing higher doses of chemotherapy and radiation to be given.
_
_
Inserting p53 gene:
Replacement gene therapy using p53 is based on the broad concept that correction of a specific genetic defect in tumour cells can reverse uncontrolled cell growth. The wildtype p53 gene product is involved in the recognition of DNA damage and the subsequent correction of that defect or induction of apoptosis in that cell. The gene is altered in over 50% of human malignancies, and therefore, has become the fulcrum of multiple gene therapy replacement trials. The general strategy is an in vivo gene therapy approach using an adenoviral vector expressing the wildtype p53 gene. The adenovirus delivery mechanism varies depending on where the tumour is located, and in all studies the therapy is combined with surgery, radiation, or chemotherapy, or a combination of the three. Clinical trials in various phases are underway for treatment of glioma, lung cancer, ovarian cancer, breast cancer, and recurrent head and neck cancer. Results published to date have been disappointing. Phase I trials for recurrent glioma reported only modest survival benefit and expression of adenoviral derived p53 only a short distance from the site of virus administration. Phase II/III trials for ovarian cancer failed to show treatment benefit with intraperitoneal administration of adenovirus expressing p53 with chemotherapy after debulking surgery. Finally, Swisher et al published antitumour effects associated with the treatment of non-small cell lung cancer; however, no comparable control group was described in their report.
_
Suicide gene therapy causing death of cancer cell:
A more elegant strategy for the treatment of cancer involves the use of the HSV thymidine kinase gene (HSV-tk) and the prodrug gancyclovir. Gancyclovir is used clinically as an antiviral agent against HSV, Epstein-Barr virus, and cytomegalovirus infection. Cells infected with these viruses produce a thymidine kinase that catalyses the conversion of gancyclovir to its active triphosphate form. The triphosphate form is incorporated into DNA and results in chain elongation termination, leading to the death of the cell. The concept of “suicide gene therapy” was initially described in the late 1980s, based on prodrug activation. It was proposed that cancer cells be infected with a virus expressing HSV-tk, resulting in constituent expression of the drug activating enzyme in these cells. Subsequent exposure of these infected cancer cells to gancyclovir results in drug activation and death of malignant cells. Multiple clinical trials have been undertaken utilising the suicide gene therapy study. In 1998, a report of 21 patients with mesothelioma was published. Patients received intrapleural injection of adenovirus expressing HSV-tk followed by gancyclovir exposure. Multiple toxicity issues were reported with this study without clinical benefit being noted. In another trial, 18 patients with prostate adenocarcinoma were injected with adenovirus expressing HSV-tk followed by gancyclovir exposure. Multiple adverse effects were again noted, and only three patients experienced transient tumour regression. In 1997, Ram et al reported the treatment of refractory recurrent brain malignancy with suicide gene therapy. Survival benefit was not appreciated in the treated group. In a multinational study, 48 patients with recurrent gliablastoma multiforme received HSV-tk/adenovirus injections into the wall of the tumour cavity after resection, with subsequent gancyclovir exposure for 14 days. No clinical benefit was noted. A third trial, accessing the use of HSV-tk/gancyclovir therapy for patients with recurrent primary or metastatic brain tumours, was undertaken and also failed to demonstrate significant clinical benefit. Examples of suicide enzymes and their prodrugs include HSV thymidine kinase (ganciclovir), Eschericoli coli purine nucleoside phosphorylase (fludarabine phosphate), cytosine deaminase (5-fluorocytosine), cytochrome p450 (cyclophosphamide), cytochrome p450 reductase (tirapazamine), carboxypeptidase (CMDA), and a fusion protein with cytosine deaminase linked to mutant thymidine kinase.
_
Oncolytic viruses:
Scientists have generated viruses, termed oncolytic viruses, which grow selectively in tumor cells as compared to normal cells. Tumor cells, but not normal cells, infected with these viruses are then selectively killed by the virus. Oncolytic viruses spread deep into tumors to deliver a genetic payload that destroys cancerous cells. Several viruses with oncolytic properties are naturally occurring animal viruses (Newcastle Disease Virus) or are based on an animal virus such as vaccinia virus (cow pox virus or the small pox vaccine). A few human viruses such as coxsackie virus A21 are similarly being tested for these properties. Human viruses such as measles virus, vesticular stomatitis virus, reovirus, adenovirus, and herpes simplex virus (HSV) are genetically modified to grow in tumor cells, but very poorly in normal cells. Currently, multiple clinical trials are recruiting patients to test oncolytic viruses for the treatment of various types of cancers.
_
Cell therapy + gene therapy:
Scientists have developed novel cancer therapies by combining both gene and cell therapies. Specifically, investigators have developed genes which encode for artificial receptors, which , when expressed by immune cells, allow these cells to specifically recognize cancer cells thereby increasing the ability of these gene modified immune cells to kill cancer cells in the patient. One example of this approach, which is currently being studied at multiple centers, is the gene transfer of a class of novel artificial receptors called “chimeric antigen receptors” or CARs for short, into a patient’s own immune cells, typically T cells, in the laboratory. The resulting genetically modified T cells which express the CAR gene are now able to recognize and kill tumor cells. Significantly, scientists have developed a large number of CARs which recognize different molecules on different types of cancer cells. For this reason, investigators believe that this approach may hold promise in the future for patients many different types of cancer. To this end, multiple pilot clinical trials for multiple cancers using T cells genetically modified to express tumor specific CARs are in currently enrolling patients and these too show promising results.
_
Gene Therapy cures Adult Leukemia:
Aug. 10, 2011 — Two of three patients dying of chronic lymphocytic leukemia (CLL) appear cured and a third is in partial remission after infusions of genetically engineered T cells. The treatment success came in a pilot study that was only meant to find out whether the treatment was safe, and to determine the right dose to use in later studies. But the therapy worked vastly better than University of Pennsylvania researchers David L. Porter, MD, Carl H. June, MD, and colleagues had dared to hope. The treatment uses a form of white blood cells called T cells harvested from each patient. A manmade virus-like vector is used to transfer special molecules to the T cells. One of the molecules, CD19, makes the T cells attack B lymphocytes — the cells that become cancerous in CLL. All this has been done before. These genetically engineered cells are called chimeric antigen receptor (CAR) T cells. They kill cancer in the test tube. But in humans, they die away before they do much damage to tumors. What’s new about the current treatment is the addition of a special signaling molecule called 4-1BB. This signal does several things: it gives CAR T cells more potent anti-tumor activity, and it somehow allows the cells to persist and multiply in patients’ bodies. Moreover, the signal does not call down the deadly all-out immune attack — the feared “cytokine storm” — that can do more harm than good. This may be why relatively small infusions of the CAR T cells had such a profound effect. Each of the cells killed thousands of cancer cells and destroyed more than 2 pounds of tumor in each patient. “Within three weeks, the tumors had been blown away, in a way that was much more violent than we ever expected,” June says in a news release. ‘It worked much better than we thought it would.”
_
Gene-based Cancer Immunotherapy and Vaccines:
Cancer treatment has been marred by the fact that most drugs target cancer cells as well as normal cells. Gene therapy is one of a handful of methods that will make cancer cells “stand out,” allowing drugs or the host’s immune system to selectively target cancer cells. The destructive capacity of the immune system is well demonstrated in autoimmune disorders such as arthritis and in the rejection of transplanted organs. Cancerous tumor cells have cell surface structures (tumor associated antigens), which should enable recognition and rejection of tumor tissue by the immune system. It is likely that many, if not most, tumors are rejected before they are even noticed. However, malignant cancers have developed ways to evade the immune response as part of the selective process during cancer growth. Cancer cells are able to escape immune detection and/or rejection by a variety of measures. Cell surface molecules, which are required for the effective policing of tissues by the immune system, are often modified, reduced or eliminated. In addition cancer cells secrete soluble molecules that inhibit the patients’ ability to develop an immune response. The ability of the immune system to recognize and reject cancerous growths has been demonstrated in a series of experimental model systems. Efforts are now being made to use this knowledge for the treatment of cancer. There are various gene-based approaches to stimulate the rejection of an established cancer in patients. The first involves procedures which modify the tumor itself, render it a more attractive target to the immune system, and allow immune cells to penetrate the tumor and kill the cancerous cells. The second approach requires a very powerful vaccine to stimulate a strong immune response against the tumor associated antigens in patients with an established cancer.
_
More recently, gene therapy experiments have shown that the gene that encodes a particular cytokine (or combinations of cytokines) can be inserted into tumor cells such that these cells now become miniature cytokine factories. Cytokines do diffuse out of the tumor, but always with a gradient favoring a higher concentration in the tumor. The goal is to maintain a high, therapeutic concentration of the cytokine in the tumor, which then results in the stimulation of an immune response to tumor associated antigens, so that not only is the injected tumor eventually eliminated but a tumor-specific immune response is also generated. The tumor-specific immune cells then circulate throughout the patient’s body and eliminate any metastatic cancer cells that have spread to other tissues. Diffusion of the cytokine out of the tumor, though causing toxicity, is also an important feature, since cytokine-based stimulation and regulation of the patient’s immune system play an important role in the control of cancer. These important immune activities have been demonstrated in various animal models.
_
Gene therapy and melanoma:
Much excitement was caused by the report of successful immunotherapy of two patients with metastatic melanoma in September 2006. The Rosenberg group engineered tumour recognition into autologous lymphocytes from peripheral blood using a retrovirus encoding a T cell receptor. High, sustained levels of circulating engineered cells were retained in two patients up to 1 year after infusion, resulting in regression of metastatic melanoma lesions; a dramatic improvement for patients who had only been expected to live for 3–6 months. Although stable engraftment of the transduced cells was seen for at least 2 months after infusion in 15 other patients, they did not respond to the treatment. It appears that it is critical to obtain an effective tumour infiltrating lymphocyte population for the treatment to be successful, and further work is underway aiming to improve response rates and refine the approach. Recently, in a similar clinical trial, this strategy has been extended to treat patients with metastatic synovial cell carcinoma, which is one of the most common soft tissue tumours in adolescents and young adults. Clinical responses were observed in four of six patients with synovial cell carcinoma and in five of 11 patients with melanoma. Despite achieving similar levels of transduction and administering similar levels of gene-modified T cells to patients, the clinical responses were highly variable and require further investigation. Importantly, two of the 11 patients with melanoma were in complete regression at 1 year post-treatment and a partial response in one patient with synovial cell carcinoma was observed at 18 months.
_
Selected recent gene therapy clinical trials for cancer:
1. TNFerade is one such treatment option that is currently in late stage II trials. This agent is a replication incompetent adenoviral vector that delivers the tumor necrosis factor-α (TNF-α) gene under the transcriptional control of a radiation inducible promoter. TNF-α is a cytokine with potent anticancer properties and high systemic toxicity, and TNF-α gene therapy provides a way to target this molecule to only the cancer cells through the use of intratumoral injections and a promoter that is activated by radiation therapy. Once TNFerade is injected, the patient then receives radiation therapy to the tumor to activate the gene. The gene then produces the TNF-α molecule which in combination with the radiation therapy promotes cell death in the affected cancer cells and surrounding cells. A phase I study of patients with soft tissue sarcoma using TNFerade demonstrated an 85% response rate including 2 complete responses. In another large phase I study of patients with histologically confirmed advanced cancer, 43% of the patients demonstrated an objective response with 5 of 30 exhibiting complete response to the treatment.66 Larger studies are being conducted using TNFerade for treatment in pancreatic, esophageal, rectal cancer and melanoma.
2. Another exciting gene therapy treatment agent is Rexin-G, the first injectable gene therapy agent to achieve orphan drug status from the Food and Drug Administration for treatment of pancreatic cancer. This gene therapy agent contains a gene designed to interfere with the cyclin G1 gene and is delivered via a retroviral vector. The gene integrates into the cancer cell’s DNA to disrupt the cyclin G1 gene and causes cell death or growth arrest. In a phase I trial, 3 of 3 patients experienced tumor growth arrest with 2 patients experiencing stable disease. These results have led to larger phase I and II trials. Rexin-G is also being evaluated for colon cancer that has metastasized to the liver.
_
Antiangiogenic gene therapy of cancer:
In 1971, Dr. Judah Folkman first proposed the hypothesis that tumor growth is angiogenesis dependent. Angiogenesis, the growth of new capillary blood vessels from preexisting vasculature, has long been appreciated for its role in normal growth and development and now is widely recognized for its role in tumor progression and metastasis. Angiogenesis is a multi-step process that includes endothelial cell (EC) proliferation, migration, basement membrane degradation, and new lumen organization. Within a given microenvironment, the angiogenic response is determined by a net balance between pro- and anti-angiogenic regulators released from activated ECs, monocytes, smooth muscle cells and platelets. The principal growth factors driving angiogenesis are vascular endothelial growth factor (VEGF), basic fibroblast growth factor (bFGF), and hepatocyte growth factor. Other positive regulators are angiotropin, angiogenin, epidermal growth factor, granulocyte colony-stimulating factor, interleukin-1 (IL-1), IL-6, IL-8, platelet-derived growth factor (PDGF), tumor necrosis factor-α (TNF-α), and matrix proteins such as collagen and the integrins. Several proteolytic enzymes critical to angiogenesis include cathepsin, urokinase-type plasminogen activator, gelatinases A/B, and stromelysin.
_
_
Gene therapy improves chemotherapy delivery for cancer: Opposite of antiangiogenic gene therapy:
Helping blood vessels that feed a tumor become mature and healthy at first might not seem like the best strategy for ridding a patient of cancer. But a team of St. Jude researchers using mouse models have discovered that a previously unknown anti-tumor action for the molecule interferon-beta (IFN-beta) does just that. The investigators demonstrated that IFN-beta sets up tumors to fail in two ways. First, the molecule stimulates production of a protein that helps the young blood vessels that initially grow in a slapdash manner become mature, which allows them to carry the chemotherapy drug topotecan into the tumor more effectively. IFN-beta also leaves the mature vasculature unable to continue expanding, thereby restricting the growth of the tumor, which depends on an expanding blood supply to grow. The new finding is significant because most drugs that remodel the immature vasculature in tumors work by inhibiting a protein called VEGF. Deprived of VEGF, inefficient new blood vessels die off, while the more efficient vessels survive for a brief period of time. In contrast, the current study showed that IFN-beta treatment causes young vessels to mature into healthy, efficient vessels that are maintained, thereby providing a longer window for improved chemotherapy delivery.
_
Gene therapy boosts chemotherapy tolerance and effectiveness of medications that attack brain cancer:
Using gene therapy and a cocktail of powerful chemotherapy drugs, researchers at Fred Hutchinson Cancer Research Center have been able to boost the tolerance and effectiveness of medications that attack brain cancer while also shielding healthy cells from their devastating effects. The report, published today in the Journal of Clinical Investigations, is based on a study involving seven patients with glioblastoma who survived a median of 20 months, with a third living up to two years – all while fighting a disease in which fewer than half of patients can expect to live a year. The top treatment for glioblastoma, which affects about 12,000 to 14,000 patients in the U.S. each year, is temozolomide, or TMZ, a powerful chemotherapy drug. But in about half of all such patients, the tumors produce high amounts of a certain protein, methylguanine methyltransferase, or MGMT, which makes them resistant to the TMZ. Another drug, the O6-benzylguanine, or O6BG, can turn off the resistance, allowing TMZ to effectively target the tumors. But the combination of O6BG and TMZ kills bone-marrow cells, a potentially deadly side effect. The challenge facing Kiem and colleagues was to find a way to protect the blood cells from the negative effects of O6BG/TMZ while also allowing the drug to do its job sensitizing the tumor to TMZ. Kiem and Adair developed a method that inserts an engineered gene into the patient’s own cells, shielding them from the O6BG. This allowed them to use combination TMZ and O6BG more effectively to target the cancer. For example, while most patients might receive one or two cycles of chemotherapy, one patient in the study received nine cycles of chemotherapy. The researchers also added an extra step to the treatment, conditioning the patients with an additional chemotherapy drug, carmustine, before giving the gene-modified blood cells. “The drug helped the patients’ bodies accept and use the gene-modified blood cells, but also treated any residual brain tumor,” Adair said. “The gene therapy might not have worked without the conditioning.”
_
Gene therapy converts anti-fungal agent into anti-cancer drug:
Toca 511 is a retrovirus engineered to selectively replicate in cancer cells, such as glioblastomas. Toca 511 produces an enzyme that converts an anti-fungal drug, flucytosine (5-FC), into the anti-cancer drug 5-fluorouracil (5-FU). After the injection of Toca 511, the patients are treated with an investigational extended- release oral formulation of 5-FC called Toca FC. Cancer cell killing takes place when 5-FC comes into contact with cells infected with Toca 511.
__________
Gene therapies against HIV:
Highly active antiretroviral therapy prolongs the life of HIV-infected individuals, but it requires lifelong treatment and results in cumulative toxicities and viral-escape mutants. Gene therapy offers the promise of preventing progressive HIV infection by sustained interference with viral replication in the absence of chronic chemotherapy. Gene-targeting strategies are being developed with RNA-based agents, such as ribozymes, antisense, RNA aptamers and small interfering RNA, and protein-based agents, such as the mutant HIV Rev protein M10, fusion inhibitors and zinc-finger nucleases. Recent advances in T-cell–based strategies include gene-modified HIV-resistant T cells, lentiviral gene delivery, CD8+ T cells, T bodies and engineered T-cell receptors. HIV-resistant hematopoietic stem cells have the potential to protect all cell types susceptible to HIV infection. The emergence of viral resistance can be addressed by therapies that use combinations of genetic agents and that inhibit both viral and host targets. Many of these strategies are being tested in ongoing and planned clinical trials.
_
CCR5 is the major co-receptor for human immunodeficiency virus (HIV). HIV researchers have been studying the CCR5 protein for years. It’s long been known that the protein allows HIV to gain entry into cells. And people who have a particular mutation in both copies of their CCR5 gene (inherited from both parents) are protected from HIV infection. CCR5 research has gained momentum in the past several years — particularly after the famous case of the “Berlin patient,” who is considered the first person to be cured of HIV. That patient, whose real name is Timothy Ray Brown, was HIV-positive back in 2007, when he underwent a bone marrow transplant to treat leukemia. His bone marrow donor carried two copies of the CCR5 mutation, and the transplant not only cured his cancer, but also knocked his HIV levels below the threshold of detection. He has been off of HIV drugs since 2008.
_
_
_
Gene Editing of CCR5 in Autologous CD4 T Cells of Persons Infected with HIV: a study:
In a small trial, researchers have successfully used gene therapy to boost the immune system of 12 patients with HIV to resist infection. They removed the patients’ white blood cells to edit a gene in them, then infused them back into the patients. Researchers investigated whether site-specific modification of the gene (“gene editing”) — in this case, the infusion of autologous CD4 T cells in which the CCR5 gene was rendered permanently dysfunctional by a zinc-finger nuclease (ZFN) — is safe. Gene editing effectively knocked out the CCR5 gene in 11 percent to 28 percent of patients’ T-cells before they were re-infused. The median CD4 T-cell count was 1517 per cubic millimeter at week 1, a significant increase from the preinfusion count of 448 per cubic millimeter (P<0.001). The median concentration of CCR5-modified CD4 T cells at 1 week was 250 cells per cubic millimeter. This constituted 8.8% of circulating peripheral-blood mononuclear cells and 13.9% of circulating CD4 T cells. Modified cells had an estimated mean half-life of 48 weeks. During treatment interruption and the resultant viremia, the decline in circulating CCR5-modified cells (−1.81 cells per day) was significantly less than the decline in unmodified cells (−7.25 cells per day) (P=0.02). HIV RNA became undetectable in one of four patients who could be evaluated. The blood level of HIV DNA decreased in most patients. Some of the patients who showed reduced viral loads were off HIV drugs completely. In fact, one of the patients showed no detectable trace of HIV at all after therapy. The researchers, who report their phase I study in the New England Journal of Medicine believe theirs is the first published account of using gene editing in humans.
_
Gene therapy can protect against HIV by producing anti-HIV antibodies:
In research published in Nature, scientists in California show that a single injection — which inserted the DNA for an HIV-neutralizing antibody into the muscle cells of live mice — completely protected the animals against HIV transmission. David Baltimore, a virologist and HIV researcher at the California Institute of Technology in Pasadena, and his colleagues used a genetically altered adenovirus to infect muscle cells and deliver DNA that codes for antibodies isolated from the blood of people infected with HIV. The DNA is incorporated into the muscle cells’ genome and programs the cells to manufacture the antibody, which is then secreted into the bloodstream. The tactic builds on earlier work by scientists at the Children’s Hospital of Philadelphia in Pennsylvania, who in 2009 first described the effectiveness of this technique in preventing transmission of simian immunodeficiency virus, which is similar to HIV but infects monkeys. Baltimore and his colleagues tested five different broadly neutralizing antibodies, one at a time, in mice with humanized immune systems. Two of the antibodies, called b12 and VRC01, proved completely protective — even when the mice received doses of HIV that were 100 times higher than a natural infection. After 52 weeks, the levels of antibody expression remained high, suggesting that a single dose would result in long-lasting protection. “We showed that you can express protective levels of antibodies in a mammal and have that expression last for a long period of time,” Baltimore says. “It sets the stage for human trials.” Providing patients with periodic doses of these antibodies throughout their lifetime would be safer than coaxing antibody production from muscle cells, but it would be far from cost-effective. The gene-therapy approach, by contrast, recruits muscle cells to act as antibody factories and could be administered using a single intramuscular shot.
__________
Gene therapy for brain disorders:
Gene therapy for brain strokes:
The blood–brain barrier (BBB) is a highly selective permeability barrier that separates the circulating blood from the brain extracellular fluid (BECF) in the central nervous system (CNS). The blood–brain barrier is formed by capillary endothelial cells, which are connected by tight junctions with an extremely high electrical resistivity of at least 0.1 Ωm. The blood–brain barrier allows the passage of water, some gases, and lipid soluble molecules by passive diffusion, as well as the selective transport of molecules such as glucose and amino acids that are crucial to neural function. The blood–brain barrier acts very effectively to protect the brain from many common bacterial infections. Recently, ultrasound techniques have been developed for opening the BBB. The combination of novel lipoplexes, capable of carrying various compounds ranging from immunoglobulins, viral vectors, plasmid DNA, siRNA, mRNA and high molecular weight drugs, provides the potential for massive, targeted release to the brain. If microbubbles are introduced to the blood stream prior to ultrasound exposure, the BBB can be opened transiently at the ultrasound focus without neuronal damage. Ultrasound, combined with microbubbles has been used for targeted delivery of site-specific gene delivery systems using adenoviral vectors for gene therapy of stroke. This will allow novel, non-invasive stroke therapies.
_
Gene therapy for Parkinson’s disease (PD):
Three approaches have been developed thus far. These are as follows:
1. The first approach is to increase dopamine production in specific regions of the brain. One study using this approach approaches uses the gene for the enzyme aromatic amino acid decarboxylase (AADC). This enzyme converts levodopa into dopamine, a neurotransmitter that is deficient in Parkinson’s disease. Studies have shown that AADC is gradually lost in Parkinson’s disease. The progressive loss of this enzyme is thought to contribute to the need to increase levodopa doses as time goes on. The rationale for this approach is that if a greater amount of AADC is present in the location where dopamine should be released, then a more reliable and perhaps a more robust response to levodopa will occur. Moreover, it is possible that a patient who no longer is obtaining a reliable benefit from levodopa therapy might regain responsiveness to this treatment after gene therapy with AADC. Inherent in this approach treatment is that the patient may alter the effect of his gene therapy by adjusting his daily dose of levodopa, since the effect of this therapy depends on continuing treatment with levodopa. A phase 1 study in which AADC was injected into the putamen has been completed at 2 different doses. In the 10 patients treated, clinical rating scales and diaries of motor function suggested benefit and specific imaging studies provided evidence of successful gene therapy. A variation on this strategy uses 3 genes that produce the enzymes AADC, tyrosine hydroxylase (TH), and GTP-cyclohydrolase-1 (GCH-1). Together these 3 enzymes can generate dopamine independent of external levodopa. The advantage of this approach is that it may be possible for the patient to discontinue treatment with levodopa. Although this approach seems very attractive, there are concerns that its benefits relies on producing precisely the right amount of dopamine. For example, too high a dose of gene therapy might result in complications due to excessive production of dopamine. The results of the study should be published in the near future.
2. The second gene therapy strategy is to adjust or modulate the excitatory and inhibitory pathways of the brain. The rationale of this approach is that the nerve cells of the subthalamic nucleus are overactive and that release of an inhibitory neurotransmitter in this brain region might normalize these cells. The gene for the enzyme glutamic acid decarboxylase (GAD), which produces the inhibitory neurotransmitter called GABA, has been examined in a phase 2 study in which 45 subjects were randomized to either bilateral treatment with GAD or a sham or simulated surgical procedure. While both patient groups showed improvement at 6 months, the improvement was greater in the subjects who underwent GAD treatment. Overall this study provided support for both the efficacy and safety of this approach.
3. The third approach is using brain proteins, termed growth factors (because of their role in brain development), that might protect against progression of Parkinson’s disease or possibly even reverse it by stimulating regrowth of injured nerve cells. A number of growth factors have been identified over the years. These include glial cell line-derived neurotrophic factor (GDNF) and Neurturin which is similar to GDNF and shares the ability to promote the survival of dopaminergic neurons. In models of Parkinson’s disease, GDNF and Neurturin have been shown to promote the survival of dopaminergic neurons. Both a phase 1 and phase 2 study using Neurturin gene therapy targeted to the putamen have been performed. In the phase 2 study, 38 patients were randomized to Neurturin gene therapy or to sham surgery. Unfortunately, there was no significant difference in the main outcome measures at 12 months. While the lack of benefit in the main outcome measures was disappointing, a subgroup of patients followed for 18 months was slightly better in the Neurturin patient than the sham treatment group, suggesting that slightly longer period of observations might be necessary to see a benefit with this gene therapy. Because of this interesting result, a second phase 2 study is underway in which Neurturin gene therapy is also targeted to the substantia nigra.
| Treatment strategy | Gene(s) | Vector | Completed studies | Ongoing or Enrolling studies |
| Increase dopamine | AADC | AAV-2 | Phase 1 | Phase 1 to start in 2013 |
| AADC, TH, & GCH-1 | Lentivirus | Phase 1 & 2 in progress | ||
| Alter excitatory activity | GAD | AAV-2 | Phase 1 &2 | |
| Growth factors | GDNF | AAV-2 | – | Phase 1 to start in 2012 |
| Neurturin | AAV-2 | Phase 1 &2 | Second Phase 2 in progress |
_
Results of several phase I and II clinical trials using AAV-based gene therapy in PD are available, and clinical trials of one lentiviral agent, Prosavin, are ongoing. The therapy, called ProSavin, works by reprogramming brain cells to produce dopamine, the chemical essential for controlling movement, the researchers said. Lack of dopamine causes the tremors, limb stiffness and loss of balance that patients with the neurodegenerative disease suffer. “We demonstrated that we are able to safely administer genes into the brain of patients and make dopamine, the missing agent in Parkinson’s patients,” said researcher Kyriacos Mitrophanous, head of research at Oxford BioMedica in England, the company that developed the therapy and funded the study. ProSavin also helps to smooth out the peaks and valleys often produced by the drug levodopa, the current standard treatment, Mitrophanous said. The treatment uses a harmless virus to deliver three dopamine-making genes directly to the area of the brain that controls movement, he explained. These genes are able to convert non-dopamine-producing nerve cells into dopamine-producing cells. Although the study results are promising, the researchers suggest they should be “interpreted with caution” because the perceived benefits fall into the range of “placebo effect” seen with other clinical trials.
_
Gene therapy may switch off Huntington’s disease:
Using gene therapy to switch off genes instead of adding new ones could slow down or prevent the fatal brain disorder Huntington’s disease. The method, which exploits a mechanism called RNA interference, might also help treat a wide range of other inherited diseases. It involves a natural defense mechanism against viruses, in which short pieces of double-stranded RNA (short interfering RNAs, or siRNAs) trigger the degradation of any other RNA in the cell with a matching sequence. If siRNA is chosen to match the RNA copied from a particular gene, it will stop production of the protein the gene codes for. Huntington’s is caused by mutations in the huntingtin gene. The resulting defective protein forms large clumps that gradually kill off part of the brain. Studies in mice have shown that reducing production of the defective protein can slow down the disease, and Beverly Davidson at the University of Iowa thinks the same could be true in people. “If you reduce levels of the toxic protein even modestly, we believe you’ll have a significant impact,” she says. Late in 2002, her team showed that it is possible to reduce the amount of a similar protein by up to 90 per cent, by adding DNA that codes for an siRNA to rodent cells engineered to produce the protein.
_
Alzheimer’s disease:
It is estimated that four million Americans suffer from the disease, with an average yearly cost to the USA of $100 billion. Current understanding of the pathophysiology is limited. Current treatment, consisting of acetylcholinesterase inhibitors, modestly retards symptomatic disease progression, but does not prevent neurone loss.
_
A phase 1 clinical trial of nerve growth factor gene therapy for Alzheimer disease: a study:
Cholinergic neuron loss is a cardinal feature of Alzheimer disease. Nerve growth factor (NGF) stimulates cholinergic function, improves memory and prevents cholinergic degeneration in animal models of injury, amyloid overexpression and aging. Authors performed a phase 1 trial of ex vivo NGF gene delivery in eight individuals with mild Alzheimer disease, implanting autologous fibroblasts genetically modified to express human NGF into the forebrain. After mean follow-up of 22 months in six subjects, no long-term adverse effects of NGF occurred. Evaluation of the Mini-Mental Status Examination and Alzheimer Disease Assessment Scale-Cognitive subcomponent suggested improvement in the rate of cognitive decline. Serial PET scans showed significant (P < 0.05) increases in cortical 18-fluorodeoxyglucose after treatment. Brain autopsy from one subject suggested robust growth responses to NGF. Additional clinical trials of NGF for Alzheimer disease are warranted.
_
Gene Therapy for amyotrophic lateral sclerosis (ALS):
Researchers at the Salk Institute and Johns Hopkins have demonstrated that gene therapy can be used to deliver a new therapy to motor neurons that can substantially increase animal survival in a mouse model of ALS. Furthermore, when comparing two therapeutic proteins — insulin-like growth factor 1 (IGF-1) and glial cell-derived neurotrophic factor (GDNF), IGF-1 was markedly more effective. Finally, the researchers discovered that IGF-1 can be given even late in the course of disease in the animal model — when clinical disease was already underway — and it was still potently capable of delaying disease progression. Scientists from Salk and the scientists and clinicians from Johns Hopkins, along with Project ALS, are actively planning a clinical trial of this gene therapy in patients with ALS and are already conducting important meetings with appropriate regulatory agencies. Discussions are now underway with potential pharmaceutical and biotech partners to manufacture the IGF-1 gene therapy and perform the necessary and mandatory safety studies as outlined by the FDA. This process should take about a year, at which point, if all goes as planned, the first clinical trial of this treatment could begin.
________
Gene therapy for cardiovascular diseases:
Coronary artery disease, heart failure, and cardiac arrhythmias are major causes of morbidity and mortality in the United States. Pharmacologic drugs and device therapies have multiple limitations, and there exists an unmet need for improved clinical outcomes without side effects. Interventional procedures including angioplasty and ablation have improved the prognosis for patients with ischemia and arrhythmias, respectively. However, large subgroups of patients are still left with significant morbidity despite those therapies. This limitation in currently available therapies has prompted extensive investigation into new treatment modalities. Sequencing information from the human genome and the development of gene transfer vectors and delivery systems have given researchers the tools to target specific genes and pathways that play a role in cardiovascular diseases. Early‐stage clinical studies have demonstrated promising signs of efficacy in some trials, with few side effects in all trials. Preclinical studies suggest that myocardial gene transfer can improve angiogenesis with vascular endothelial growth factor (VEGF) or fibroblast growth factor (FGF), increase myocardial contractility and reduced arrhythmia vulnerability with sarcoplasmic reticulum Ca2+ adenosine triphosphatase, induce cardiac repair with stromal‐derived factor‐1 (SDF‐1), control heart rate in atrial fibrillation with an inhibitory G protein α subunit, and reduce atrial fibrillation and ventricular tachycardia vulnerability with connexins, the skeletal muscle sodium channel SCN4a, or a dominant‐negative mutation of the rapid component of the delayed rectifier potassium channel, KCNH2‐G628S.
_
Gene therapy for heart failure:
The therapy involves injecting a harmless altered virus into the heart to carry the corrective gene into heart muscle cells. The aim is to raise levels of a protein called SERCA2a that plays an important role in heart muscle contraction by recycling calcium in the heart’s muscle cells. Heart muscle cells need calcium to contract and relax, and a variety of conditions—such as coronary artery disease, hypertension, and alcoholism and drug abuse—can contribute to progressive heart failure. Regardless of the cause, heart failure typically leads to a loss of enzyme function. As a result, the heart cannot pump blood forcefully enough to keep fluid out of the tissues and lungs. Celladon is developing a treatment that uses a small, benign virus to deliver a fresh supply of SERCA2a enzymes into the muscle cells of the heart. The company says Mydicar is intended for patients who have been diagnosed with advanced chronic heart failure and who are suitable for this particular type of gene therapy. The company estimates that about 350,000 patients with systolic heart failure fit these criteria in the United States. Celladon sought the designation based on a long-term, follow-up study of Cupid 1, a mid-stage clinical trial that enrolled 39 patients with severe heart failure. Patients either got a placebo or a low, mid, or high dose of Mydicar through cardiac catheterization. Results from the follow-up study confirmed initial findings that showed a dramatic, 88 percent reduction in heart failure-related hospitalizations among patients who received the highest dose of the gene therapy treatment. After three years, the patients who got the highest dose of Mydicar still showed an 82 percent reduction in episodes of worsening heart failure and hospitalizations. “That’s what really crystallized the strength of the data,” Celladon CEO Krisztina Zsebo said Wednesday. The safety data for Mydicar also was “superb,” and shows no drug-related toxicities, Zsebo added. The high-dose Mydicar patients also showed an improved survival rate throughout the three-year follow-up study. Heart failure represents a large, unmet need, and the mortality rate is roughly 50 percent within five years of the initial diagnosis of heart failure, according to the company. A second clinical trial that is intended to confirm and expand on the results of Cupid 1 after enrolling 250 patients.
_
The DNA called SDF-1 attracts stem cells to the heart to repair damaged muscle and arteries:
A new procedure designed to deliver stem cells to the heart to repair damaged muscle and arteries in the most minimally invasive way possible has been performed for the first time by Amit Patel, M.D., director of Clinical Regenerative Medicine and Tissue Engineering and an associate professor in the Division of Cardiothoracic Surgery at the University of Utah School of Medicine. Patel uses a minimally invasive technique where he goes backwards through a patient’s main cardiac vein, or coronary sinus, and inserts a catheter. He then inflates a balloon in order to block blood flow out of the heart so that a very high dose of gene therapy can be infused directly into the heart. The unique gene therapy doesn’t involve viruses and is pure human DNA infused into patients. The DNA, called SDF-1, is a naturally occurring substance in the body that becomes a homing signal for a patient’s body to use its own stem cells to go to the site of an injury. Once the gene therapy is injected, the genes act as “homing beacons.” When the genes are put into patients with heart failure, they marinate the entire heart and act like a look out, he said. When the signal, or the light from the SDF-1, which is that gene, shows up, the stem cells from not inside your own heart and from those that circulate from your blood and bone marrow all get attracted to the heart which is injured, and they bring reinforcements to make it stronger and pump more efficiently,” said Patel.
_
Genetically modified stem cell therapy for severe heart failure:
Patients with chronic heart failure are to receive pioneering stem cell treatment in a new trial which could herald a cure for the biggest killer ‘in the industrialised world’. Those taking part in the trial will get a single injection of 150 million adult stem cells into the heart. It could offer new hope for ‘end-stage’ patients with the most severe form of heart failure who rely on external machines to pump blood around the body to stay alive. Initial trials of the treatment, made by the Australian medical firm Mesoblast, involving 30 patients found the injection was safe and led to an increased ability to maintain circulation without support from an external device. If the larger trial proves successful then the first stem cell-based therapy to treat advanced heart failure – known scientifically as ‘class IV’ failure – could be on the market in six years. Previous research suggests injecting stem cells into the heart reduces deaths and time spent in hospital. Most of these trials used cells extracted from a patient’s own blood or bone marrow after they have had a heart attack. The patented Mesoblast therapy begins with removing stem cells from the bone marrow of healthy adult donors by a biopsy under local anaesthetic in a half hour procedure. The company then manufactures highly-purified stem cells, called Mesenchymal Precursor Cells (MPCs), which act by releasing chemicals to regenerate heart tissue. It means the stem cell treatment can be used ‘off-the-shelf’.
_
New gene therapy may replace pacemaker implants:
A new technology that allows genes to be injected into hearts with damaged electrical systems may replace the need for pacemaker implants in humans in the future. A new study has recently shown that a particular gene can be injected into the heart and correct abnormal heart beats in pigs. The researchers injected a single human gene into the hearts of pigs with severely weakened heartbeats. By the second day, the pigs had significantly faster heartbeats than other diseased pigs that didn’t receive the gene. The key to the new procedure is a gene called TBX18, which converts ordinary heart cells into specialized sino-atrial node cells. The heart’s sino-atrial node initiates the heart beat like a metronome, using electric impulses to time the contractions that send blood flowing through people’s arteries and veins. People with abnormal heart rhythms suffer from a defective sino-atrial node. Researchers injected the gene into a very small area of the pumping chambers of pigs’ hearts. The gene transformed the heart cells into a new pacemaker. In essence, researchers create a new sino-atrial node in a part of the heart that ordinarily spreads the impulse, but does not originate it. The newly created node then takes over as the functional pacemaker bypassing the need for implanted electronics and hardware. Pigs were used in the research because their hearts are very similar in size and shape to those of humans. Within two days of receiving the gene injection, pigs had significantly stronger heartbeats than pigs that did not receive the gene. The effect persisted for the duration of the 14-day study. Toward the end of the two weeks, the treated pigs’ heart rates began to falter somewhat, but remained stronger than that of the pigs who did not receive the gene injection. The research team hopes to advance to human trials within three years. However, results from animal trials often can’t be duplicated in humans.
_
Angiogenesis:
The treatment of ischemic disease with the goal of increasing the number of small vessels within ischemic tissue is termed therapeutic angiogenesis. Studies from tumor neovascularization and cardiovascular development have helped to identify vascular endothelial growth factors (VEGF) and fibroblast growth factors (FGF) as potent mediators of angiogenesis. The VEGF family is large but VEGF-A is the best-characterized form in the study of angiogenesis. Hypoxia and several cytokines induce VEGF expression, which then signals through tyrosine kinase receptors to mediate downstream effects. A mitogen for endothelial cells, VEGF also promotes cell migration and is a potent hyperpermeability factor. It has been shown to improve collateral vessel development in animal models of hind limb ischemia and myocardial ischemia. Earlier studies with FGF demonstrated similar results. In the clinical setting, Baumgartner et al treated 9 patients with limb-threatening lower-extremity ischemia with intramuscular injections of plasmid DNA containing the VEGF complementary DNA (cDNA). This treatment improved blood flow to the ischemic limbs as evidenced by angiographic evaluation, improved hemodynamic indices, relieved rest pain, and improved ulcers and limb salvage when evaluated at an average of 6 months posttreatment. Other clinical trials, however, failed to show such definitive benefit, and additional trials are ongoing using claudication as the treatment criterion as opposed to limb-threatening ischemia. Trials are also being carried out using VEGF administration, either liposome-mediated or adenoviral-mediated, to stimulate angiogenesis in ischemic myocardium. Patients are still being evaluated for these trials. Despite these studies, many concerns have been raised regarding these therapies. Although gene therapy with FGF, VEGF, and other growth factors has led to angiogenesis, additional studies have not shown the formation of functional collateral vessels that persist after the withdrawal of the growth factor. There are many unanswered questions and concerns. The biological effects of VEGF are remarkably dose-dependent. The potential risks of therapeutic angiogenesis include hemangioma formation, formation of nonfunctional leaky vessels, and the acceleration of incidental tumor growth. Accelerated tumor growth was observed in a patient with an occult lung tumor receiving VEGF therapy and resulted in the halting of that trial by the Food and Drug Administration. This event brought to light the need to be extremely cautious about the clinical application of these gene therapies and the need to be rigorous about the screening of the patients we subject to such experimental therapies.
_
BioBypass:
Vascular endothelial growth factor (VEGF) became the leading candidate molecule for the induction of angiogenesis. However, the short half life of VEGF (about seven minutes) and the extended exposure time required to induce effective angiogenesis in animal models was not compatible with protein infusion or injection techniques. Gene therapy was proposed as the appropriate form of delivery as it would allow for sustained, local protein delivery to ischaemic tissue over several weeks. The specific in vivo gene therapy strategy proposed was called “BioBypass”. It consisted of an adenovirus modified to express the VEGF cDNA sequence, which was then injected into ischaemic tissue. Cells infected would express VEGF and induce angiogenesis into the region of ischaemia. The transient nature of adenovirus expression in cells allowed for continuous expression of VEGF for about four weeks. This time frame is long enough for angiogenesis, but short enough to limit potential side effects of persistent growth factor expression, including malignancy. Two related phase I trials have been conducted in patients with CAD. One study combined the intramyocardial injection of adenovirus expressing VEGF with concurrent CABG. The second study was conducted on non-surgical candidates failing maximum medical management, who received intramyocardial injection of virus though microscopic thoracotomy. Results indicated an increase in myocardial tissue perfusion and an increase in exercise tolerance after treatment. Further trials are pending.
_
Therapeutic angiogenesis for coronary arteries:
Gene Therapy with Vascular Endothelial Growth Factor for Inoperable Coronary Artery Disease: a study:
Gene transfer for therapeutic angiogenesis represents a novel treatment for medically intractable angina in patients judged not amenable to further conventional revascularization. Researchers involve 30 patients with class 3 or 4 angina, enrolled in a Phase 1 clinical trial to assess the safety and bioactivity of direct myocardial gene transfer of naked DNA-encoding vascular endothelial growth factor (phVEGF165), as sole therapy for refractory angina. The phVEGF165 was injected directly into the myocardium through a mini-thoracotomy. Twenty-nine of 30 patients experienced reduced angina (56.2 ± 4.1 episodes/week preoperatively versus 3.8 ± 1.6 postoperatively, P < 0.0001) and reduced sublingual nitroglycerin consumption (60.1 ± 4.4 tablets/week preoperatively versus 2.9 ± 1.1 postoperatively, P < 0.0001). This study describes a novel approach by using gene therapy to stimulate angiogenesis and improve perfusion to ischemic myocardium. Increasing numbers of patients are presenting with chronic angina, despite having had multiple previous coronary bypass and/or percutaneous revascularization procedures. Frequently, these patients are not candidates for further direct revascularization because of diffuse distal vessel disease with poor angiographic runoff, lack of available conduits, or unacceptably high perioperative risk. These patients suffer from medically intractable angina and continue to be at high risk for myocardial infarction and sudden cardiac death. Preclinical studies in animal models of hind limb and myocardial ischemia have shown that direct IM gene transfer (GTx) of naked DNA encoding for vascular endothelial growth factor (phVEGF165) can promote angiogenesis and improve perfusion to ischemic tissue. Recently, preliminary clinical trials of gene therapy have demonstrated successful results in patients with limb and myocardial ischemia.
_
Gene therapy to Prevent Thrombosis:
A thrombus forms in the vasculature when there is a local defect in the normal antithrombotic function of the vessel. This typically occurs at sites of vascular injury, either from disease states or secondary to therapeutic maneuvers. Gene therapy approaches have been developed to prevent thrombus formation. Examples of such genes include tissue plasminogen activator (t-PA), which activates plasminogen to plasmin that can then mediate fibrinolysis; tissue factor pathway inhibitor, because tissue factor is the primary stimulator of the coagulation pathway; and hirudin. These genes may be very useful in preventing early thrombosis following bypass surgical or angioplasty procedures.
_______
Cholesterol controlled by Gene Therapy in Mice:
By altering how a liver gene works, scientists say they’ve developed a way to cut cholesterol permanently with a single injection, eliminating the need for daily pills to reduce the risk of heart attack. In a test in mice, scientists at the Harvard Stem Cell Institute and the University of Pennsylvania disrupted the activity of a gene, called PCSK9 that regulates cholesterol. The process permanently dropped levels of the lipid by 35 to 40 percent, said Kiran Musunuru, the lead researcher. “That’s the same amount of cholesterol you’ll get with a cholesterol drug,” said Musunuru, who is a cardiologist and assistant professor at Harvard. “The kicker is we were able to do that with a single injection, permanently changing the genome. Once that changes, it’s there forever.” The PCSK9 gene is the same one now being targeted by Amgen Inc., Sanofi (SAN) and Regeneron Pharmaceuticals Inc. (REGN) with experimental compounds designed to suppress the protein the gene produces. Certain rare PCSK9 mutations are found to cause high cholesterol and heart attacks. Good mutations also exist, and people with them have a heart attack risk that ranges from 47 to 88 percent below average, the researchers said. The approach used a two-part genome-engineering technique that first targets the DNA sequence where the gene sits, and then creates a break in the system. The therapy was carried to the liver using an injected adenovirus. The genome-editing technique used in the experiment has only been around for about a year and a half, Musunuru said. The next step is to see how effective the therapy is in human cells, by using mice whose liver cells are replaced with human-derived liver cells, he said. Assessing safety will be the primary concern.
_
LDLR-Gene therapy for familial hypercholesterolaemia:
Low-density lipoprotein receptor (LDLR) associated familial hypercholesterolemia (FH) is the most frequent Mendelian disorder and is a major risk factor for the development of CAD. To date there is no cure for FH. The primary goal of clinical management is to control hypercholesterolaemia in order to decrease the risk of atherosclerosis and to prevent CAD. Permanent phenotypic correction with single administration of a gene therapeutic vector is a goal still needing to be achieved. The first ex vivo clinical trial of gene therapy in FH was conducted nearly 18 years ago. Patients who had inherited LDLR gene mutations were subjected to an aggressive surgical intervention involving partial hepatectomy to obtain the patient’s own hepatocytes for ex vivo gene transfer with a replication deficient LDLR-retroviral vector. After successful re-infusion of transduced cells through a catheter placed in the inferior mesenteric vein at the time of liver resection, only low-level expression of the transferred LDLR gene was observed in the five patients enrolled in the trial. In contrast, full reversal of hypercholesterolaemia was later demonstrated in in vivo preclinical studies using LDLR-adenovirus mediated gene transfer. However, the high efficiency of cell division independent gene transfer by adenovirus vectors is limited by their short-term persistence due to episomal maintenance and the cytotoxicity of these highly immunogenic viruses. Novel long-term persisting vectors derived from adeno-associated viruses and lentiviruses, are now available and investigations are underway to determine their safety and efficiency in preparation for clinical application for a variety of diseases. Several novel non-viral based therapies have also been developed recently to lower LDL-C serum levels in FH patients.
______
Tyrosinemia and gene therapy:
In this study researchers attacked a disease called hereditary tyrosinemia, which stops liver cells from being able to process the amino acid tyrosine. It is caused by a mutation in just a single base of a single gene on the mouse (and human) genome, and prior research has confirmed that fixing that mutation cures the disease. The problem is that, until now, such a correction was only possible during early development, or even before fertilization of the egg. An adult body was thought to be simply too complex a target. The gene editing technology used here is called the CRISPR system (vide supra).The experimental material actually enters the body via injection, targeted to a specific cell type. In this study, researchers observed an initial infection rate of roughly 1 in every 250 target cells. Those healthy cells out-competed their unmodified brothers, and within a month the corrected cells made up more than a third of the target cell type. This effectively cured the disease; when the mice were taken off of previously life-saving medication, they survived with little ill effect. There are other possible solutions to the problem of adult gene editing, but they can be much more difficult to use, less accurate and reliable, and are generally useful in a narrower array of circumstances. CRISPRs offer a very high level of fidelity in targeting, both to specific cells in the body and to very specific genetic loci within each cell. Tyrosinemia affects only about 1 in every 100,000 people, but the science on display here is very generalizable.
______
Eye and gene therapy:
Ocular gene therapy is rapidly becoming a reality. By November 2012, approximately 28 clinical trials were approved to assess novel gene therapy agents.
_
Gene therapy ‘could be used to treat blindness’:
Surgeons in Oxford have used a gene therapy technique to improve the vision of six patients who would otherwise have gone blind. The operation involved inserting a gene into the eye, a treatment that revived light-detecting cells. The doctors involved believe that the treatment could in time be used to treat common forms of blindness. Prof Robert MacLaren, the surgeon who led the research, said he was “absolutely delighted” at the outcome. “We really couldn’t have asked for a better result,” he said. The first patient was Jonathan Wyatt, who was 63 at the time. Mr Wyatt has a genetic condition known as choroideremia, which results in the light-detecting cells at the back of the eye gradually dying. Mr Wyatt is now able to read three lines further down in an optician’s sight chart. Professor MacLaren believes that success with choroideremia demonstrates the principle that gene therapy could be used to cure other forms of genetic blindness including age-related macular degeneration. Professor Andrew George, an expert in molecular immunology at Imperial College London, said: “The eye is good for gene therapy because it is a simple organ and it is easy to see what is going on. “There is hope that once gene therapy is developed in the eye, scientists could move on to more complex organs.”
_
Retinal gene therapy:
_
Colour blindness corrected by gene therapy:
Researchers have used gene therapy to restore colour vision in two adult monkeys that have been unable to distinguish between red and green hues since birth — raising the hope of curing colour blindness and other visual disorders in humans. If we can target gene expression specifically to cones [in humans] then this has a tremendous implication. About 1 in 12 men lack either the red- or the green-sensitive photoreceptor proteins that are normally present in the colour-sensing cells, or cones, of the retina, and so have red–green colour blindness. Gene therapy for color blindness is an experimental gene therapy aiming to convert congenitally colorblind individuals to trichromats by introducing a photopigment gene that they lack. Though partial color blindness is considered only a mild disability and is controversial whether it is even a disorder, it is a condition that affects many people, particularly males. Complete color blindness, or achromatopsia, is very rare but more severe. While never demonstrated in humans, animal studies have shown that it is possible to confer color vision by injecting a gene of the missing photopigment using gene therapy. As of 2014 there is no medical entity offering this treatment, and no clinical trials available for volunteers.
_
Retinitis pigmentosa and gene therapy:
Columbia University Medical Center (CUMC) researchers have created a way to develop personalized gene therapies for patients with retinitis pigmentosa (RP), a leading cause of vision loss. The approach, the first of its kind, takes advantage of induced pluripotent stem (iPS) cell technology to transform skin cells into retinal cells, which are then used as a patient-specific model for disease study and preclinical testing. Using this approach, researchers led by Stephen H. Tsang, MD, PhD, showed that a form of RP caused by mutations to the gene MFRP (membrane frizzled-related protein) disrupts the protein that gives retinal cells their structural integrity. They also showed that the effects of these mutations can be reversed with gene therapy. The approach could potentially be used to create personalized therapies for other forms of RP, as well as other genetic diseases.
_
Promising results from gene therapy research to treat macular degeneration:
Australian research on a new gene therapy which could revolutionise treatment of macular degeneration (AMD) is showing positive results. In a world first, Perth researchers have developed a new method which only requires one injection and can reverse the damage. Professor Elizabeth Rakoczy is part of the team of researchers at Lions’ Eye Institute behind the revolutionary treatment. “Our first success was treating a blind dog who regained its vision, and we followed the dog for four years and it still had its sight,” he said. “So it demonstrated to us the gene therapy can deliver a drug into the eye for a long, long period of time. “So we put our natural protein that we found in the eye, and put it into the gene therapy, the recombinant virus, and then developed the bio-factory which is producing this material in the eye.”
_
Targeting Herpetic Keratitis by Gene Therapy:
Viral infections such as herpetic keratitis caused by herpes simplex virus 1 (HSV-1) can cause serious complications that may lead to blindness. Recurrence of the disease is likely and cornea transplantation, therefore, might not be the ideal therapeutic solution. Gene therapy of herpetic keratitis has been reported. Successful gene therapy can provide innovative physiological and pharmaceutical solutions against herpetic keratitis.
______
Gene therapy for hearing loss:
Regenerating sensory hair cells, which produce electrical signals in response to vibrations within the inner ear, could form the basis for treating age- or trauma-related hearing loss. One way to do this could be with gene therapy that drives new sensory hair cells to grow. Researchers at Emory University School of Medicine have shown that introducing a gene called Atoh1 into the cochleae of young mice can induce the formation of extra sensory hair cells. Their results show the potential of a gene therapy approach, but also demonstrate its current limitations. The extra hair cells produce electrical signals like normal hair cells and connect with neurons. However, after the mice are two weeks old, which is before puberty, inducing Atoh1 has little effect. This suggests that an analogous treatment in adult humans would also not be effective by itself.
______
Gene therapy for osteoarthritis (OA):
Target cells in osteoarthritis gene therapy:
Target cells in the OA therapy are autologous chondrocytes, Chondroprogenitor cells, Cells within the synovial cavity, and cells of adjacent tissues such as muscle, tendons, ligaments, and meniscus. Development of cartilage function and structure may be achieved by:
1. Inhibiting inflammatory and catabolic pathways
2. Stimulating anabolic pathways to rebuild the matrix
3. Impeding cell senescence
4. Avoiding the pathological formation of osteophytes
5. Prevention of apoptosis, and/or influencing several of these processes
_
Researchers have focused on gene transfer as a delivery system for therapeutic gene products, rather counteracting genetic abnormalities or polymorphisms. Genes, which contribute to protect and restore the matrix of articular cartilage, are attracting the most attention. These Genes are listed in table below. Among all candidates listed below, proteins that block the actions of interleukin-1 (IL-1) or that promote the synthesis of cartilage matrix molecules have received the most experimental scrutiny.
_
| Category | Gene Candidate | |
| Cytokine/cytokine antagonist | IL-1Ra, sIL-1R, sTNFR, IL-4 | |
| Cartilage growth factor | IGF-1, FGF, BMPs, TGF, CGDF | |
| Matrix breakdown inhibitor | TIMPs, PAIs, serpins | |
| Signaling molecule/transcription factor | Smad, Sox-9, IkB | |
| Apoptosis Inhibitor | Bcl-2 | |
| Extra cellular matrix molecule | Type II collagen, COMP | |
| Free radical antagonist | Super Oxide Dismutase | |
_____
Gene Therapy and Spinal Fusion:
Spinal fusion is an excellent example of how gene therapy could revolutionize spinal surgery. Instead of putting a protein into the spine to stimulate fusion, surgeons would instead transfer the gene that codes for that protein into a portion of the spinal tissues, allowing those tissues to produce the protein responsible for bone growth. Although this seems like a complex procedure, it is much less invasive than current spinal fusion methods, which require an open incision, a certain amount of blood loss, pain to the patient and a significant period of healing. Gene therapy has the ability to dramatically change how this surgical procedure is performed. Imagine replacing an open spinal fusion surgery along with the required general anesthesia, risk of significant blood loss, pain, and prolonged recovery time, into a less invasive, one-injection procedure given on an outpatient basis without the need for a hospital stay. Although it may seem like a theoretical fantasy, in actuality there is a huge potential for the use of gene therapy in the treatment of spinal disorders. The main reasons for using gene therapy to treat spinal disorders would be to provide more efficient and effective ways of achieving important medical needs such as spinal fusion, disc repair or regeneration, or even regrowth of spinal cord and nerve cells.
_
Gene Therapy might grow Replacement Tissue inside the Body:
Duke researchers use gene therapy to direct stem cells into becoming new cartilage on a synthetic scaffold even after implantation into a living body. By combining a synthetic scaffolding material with gene delivery techniques, researchers at Duke University are getting closer to being able to generate replacement cartilage where it’s needed in the body. Performing tissue repair with stem cells typically requires applying copious amounts of growth factor proteins—a task that is very expensive and becomes challenging once the developing material is implanted within a body. In a new study, however, Duke researchers found a way around this limitation by genetically altering the stem cells to make the necessary growth factors all on their own. They incorporated viruses used to deliver gene therapy to the stem cells into a synthetic material that serves as a template for tissue growth. The resulting material is like a computer; the scaffold provides the hardware and the virus provides the software that programs the stem cells to produce the desired tissue. This type of gene therapy generally requires gathering stem cells, modifying them with a virus that transfers the new genes, culturing the resulting genetically altered stem cells until they reach a critical mass, applying them to the synthetic cartilage scaffolding and, finally, implanting it into the body. While this study focuses on cartilage regeneration, Guilak and Gersbach say that the technique could be applied to many kinds of tissues, especially orthopaedic tissues such as tendons, ligaments and bones. And because the platform comes ready to use with any stem cell, it presents an important step toward commercialization.
_____
Gene therapy and diabetes mellitus:
Gene therapy cures diabetic mice:
For more than eighty years, insulin injection has been the only treatment option for all type I and many type II diabetic individuals. Whole pancreas transplantation has been a successful approach for some patients, but is a difficult and complex operation. Recently, it was demonstrated that a glucocorticoid-free immunosuppressive regimen led to remarkably successful islet transplantation. However, both pancreas and islet cell transplantation are limited by the tremendous shortage of cadaveric pancreases that are available for transplantation. Therefore, a major goal of diabetes research is to generate an unlimited source of cells exhibiting glucose-responsive insulin secretion that can be used for transplantation, ideally without the need for systemic immunosuppression. Experimental gene therapy has cured mice of diabetes, and although work is at a very early stage, scientists hope the technique will one day free people from its effects. United States scientists introduced a gene to the mice that enabled their livers to generate insulin. Professor Lawrence Chan, who led the research at the Baylor College of Medicine in Houston, Texas, said: “It’s a proof of principle. The exciting part of it is that mice with diabetes are ‘cured’.” Liver cells were induced to become beta cells that produce insulin and three other hormones. Professor Chan’s team used a doctored virus to carry the beta cell gene into the mouse liver cells. On its own, the gene partially corrected the disease. Combined with a beta cell growth factor, a biochemical that promotes growth, the diabetic mice were completely cured for at least four months. An added benefit was that the modified liver cells also produced glucagon, somostatin and pancreatic polypeptide. These three hormones are thought to play a role in controlling insulin production and release. The results were reported in the journal Nature Medicine. Professor Chan said the main obstacle to using the treatment on humans was concern about the safety of the virus “vector”. Although the safest viral vector available was used, he expected safer ones to become available within the decade. “We want to use the safest vector possible,” he said.
_
Gene therapy reverses type 1 diabetes in mice; this study also prevents immune destruction of newly formed islet cells:
An experimental cure for Type 1 diabetes has a nearly 80 percent success rate in curing diabetic mice. The results, being presented at The Endocrine Society’s 93rd Annual Meeting in Boston, offer possible hope of curing a disease that affects 3 million Americans. “With just one injection of this gene therapy, the mice remain diabetes-free long term and have a return of normal insulin levels in the body,” said Vijay Yechoor, MD, the principal investigator and an assistant professor at Baylor College of Medicine in Houston. Yechoor and his co-workers used their new gene therapy in a nonobese mouse model of Type 1 diabetes. The therapy attempts to counter the two defects that cause this autoimmune form of diabetes: autoimmune attack and destruction of the insulin-producing beta cells by T cells. First, the researchers genetically engineer the formation of new beta cells in the liver using neurogenin3. This gene defines the development of pancreatic islets, which are clusters of beta cells and other cells. Along with neurogenin3, they give an islet growth factor gene called betacellulin to stimulate growth of these new islets. The second part of the therapy aims to prevent the mouse’s immune system from killing the newly formed islets and beta cells. Previously the research team combined neurogenin3 with the gene for interleukin-10, which regulates the immune system. However, with that gene, they achieved only a 50 percent cure rate in diabetic mice, Yechoor said. In the new study, the investigators added a gene called CD274 or PD-L1 (programmed cell death 1 ligand-1). It inhibits activity of the T cells only around the new islets in the liver and not in the rest of the body, he explained. “We want the gene to inactivate T cells only when they come to the new islet cells. Otherwise, the whole body would become immunocompromised,” Yechoor said. This treatment reversed diabetes in 17 of 22 mice, or 78 percent. Diabetic mice that otherwise live only six to eight weeks were growing normally and were free of diabetes as long as 18 weeks after injection of the gene therapy, Yechoor said. This treatment approach, he said, “has the potential to be a curative therapy for Type 1 diabetes.” The other mice reportedly responded to the gene therapy initially but then became diabetic again. There are two possibilities, according to Yechoor, why the therapy did not achieve a 100 percent cure rate. “T cells are the predominant part of islet destruction, but other pathways, including beta cells could also contribute, meaning we would need to target those pathways as well,” Yechoor said. “Or maybe the efficiency of this new protective gene is not sufficient, and we need to give a larger dose.”
_
Gene therapy cures diabetic dogs:
Five diabetic beagles no longer needed insulin injections after being given two extra genes, with two of them still alive more than four years later. Several attempts have been made to treat diabetes with gene therapy but this study is “the first to show a long-term cure for diabetes in a large animal”, says Fàtima Bosch, who treated the dogs at the Autonomous University of Barcelona, Spain. The two genes work together to sense and regulate how much glucose is circulating in the blood. People with type 1 diabetes lose this ability because the pancreatic cells that make insulin, the body’s usual sugar-controller, are killed by their immune system. Delivered into muscles in the dogs’ legs by a harmless virus, the genes appear to compensate for the loss of these cells. One gene makes insulin and the other an enzyme that dictates how much glucose should be absorbed into muscles. Dogs which received just one of the two genes remained diabetic, suggesting that both are needed for the treatment to work. Bosch says the findings build on an earlier demonstration of the therapy in mice. She hopes to try it out in humans, pending further tests in dogs. Other diabetes researchers welcomed the results but cautioned that the diabetes in the dogs that underwent the treatment doesn’t exactly replicate what happens in human type 1 diabetes. That’s because the dogs’ pancreatic cells were artificially destroyed by a chemical, not by their own immune systems.
_
Other gene therapy approaches for diabetes cure:
Another gene therapy approach aims at genetically manipulating beta cells so that they produce a local beta cell protection factor. In individuals in whom autoimmune destruction of beta cells has begun, but not reached the end stage, it would make sense to rescue the remaining beta cells by such a gene therapy approach. Assuming that it is possible to target a vector to the beta cell in vivo, the resulting beta cell production of a local survival factor would not only save the beta cells, it would also leave the immune system in general unaffected as the transgene production is localized to the islets. This strategy was first proposed in a study which demonstrated that transgene production of interleukin-1 receptor antagonist protein desensitized the beta cells to interleukin-1 induced nitric oxide production. It is possible that beta cells are destroyed in type 1 diabetes as a result of macrophage-mediated release of cytokines and nitric oxide. It might also be cytotoxic T cells that kill the beta cell by releasing the apoptotic signals perforin and Fas ligand. In both cases, quite a few beta cell survival factors have been envisaged. In addition to cytokine antagonists such as the interleukin-1 receptor antagonist, immune modulators such as TGF-beta and CGRP, inhibitors of Fas ligand signaling, anti-apoptotic factors such as Bcl-2 and A20, and anti-stress factors such as thioredoxin all qualify as interesting candidates. These factors have been addressed experimentally and could possibly, when expressed by the beta cells, promote beta cell survival. Insulin-producing cells can not only be manipulated for the avoidance of autoimmune destruction, but also for transplantation purposes. Transplantation of human or pig islets to diabetic recipients is problematic due to poor grafting and rejection. To promote successful grafting, islets could possibly be transduced ex vivo to produce heme oxygenase and vascular endothelium growth factor. These proteins protect against hypoxia and stimulate vascular neogenesis. Rejection of allografts and xenografts are highly complex processes. However, one step forward was taken when transgenic pigs were generated, which expressed a human complement regulatory protein (hDAF). This protein attenuates the antibody-mediated complement activation, thereby lessening the problem with hyperacute rejection. Attempts to manipulate pigs genetically not to express the alpha Gal epitope are also underway. However, the greatest problem right now for all beta cell transduction strategies is the lack of efficient and safe vectors. To transduce beta cells in vivo, the vector would have to be obtainable in large quantities, stable when administered in vivo, reach the beta cells from the blood stream and efficiently and selectively transduce the non-replicating beta cell. All this would have to be achieved without inducing toxicity, immune reactions or pathological recombinations. Although considerable improvements in vector design have been accomplished, there is a long way to go. The lentivirus, which transduces beta cells in vitro, is derived from the HIV-1 virus, which might preclude its use in humans due to the risk of pathological recombinations. More promising is perhaps the adenovirus, which transduces human islet cells not only in vitro, but also ex vivo. Indeed, intra-arterial injection of adenovirus into a whole human pancreas resulted in transduction of 50% of the beta cells. This finding gives hope for the future, but gene transfer techniques need to be developed that can achieve therapeutic long-term expression, in vivo regulation of transgene expression and lack of immune triggering, in order to conduct gene therapy on pancreatic beta cells in vivo. The technical problems associated with the transfection of beta cells are possibly avoided by using the DNA vaccination approach. In individuals with a high risk of developing diabetes, as indicated by genetic and humoral markers, but who have not yet entered the phase of autoimmune beta cell destruction, it might be possible to prevent the progression of the disease by DNA vaccination. In mice, it has already been observed that DNA vaccination with a glutamic acid decarboxylase (GAD) gene construct generates a humoral immune response. GAD is considered a key autoantigen in type 1 diabetes, and if the DNA vaccination approach leads to tolerization, beta cell destruction might be avoided. DNA vaccination might also be used for inducing immunity against key factors that mediate the inflammatory process. For example, DNA vaccination with naked DNA encoding C-C chemokines has been observed to protect against experimental autoimmune encephalomyelitis. Finally, with increasing knowledge of the factors that control beta cell differentiation and replication, a genetic approach that stimulates the regeneration of the beta cell mass becomes feasible. For a long time, the molecular control of beta cell growth and differentiation has been obscure. However, the Edlund group in Sweden has recently demonstrated that the transcription factor IPF1 participates in maintaining the beta cell phenotype and euglycemia in vivo. Moreover, they have also reported that Notch signaling controls the decision between pancreatic exocrine and pancreatic endocrine differentiation. These important findings could make way for large-scale production of beta cells intended for transplantation to diabetics, or for in situ regeneration of beta cells in diabetics. However, such an approach must be combined with a strategy to prevent autoimmune destruction of the newly formed beta cells.
_______
Hematopoietic Stem Cell Gene Therapy with a Lentiviral Vector in X-Linked Adrenoleukodystrophy:
X-linked adrenoleukodystrophy (ALD) is a severe brain demyelinating disease in boys that is caused by a deficiency in ALD protein, an adenosine triphosphate–binding cassette transporter encoded by the ABCD1 gene. ALD progression can be halted by allogeneic hematopoietic cell transplantation (HCT). Researchers initiated a gene therapy trial in two ALD patients for whom there were no matched donors. Autologous CD34+ cells were removed from the patients, genetically corrected ex vivo with a lentiviral vector encoding wild-type ABCD1, and then re-infused into the patients after they had received myeloablative treatment. Over a span of 24 to 30 months of follow-up, they detected polyclonal reconstitution, with 9 to 14% of granulocytes, monocytes, and T and B lymphocytes expressing the ALD protein. These results strongly suggest that hematopoietic stem cells were transduced in the patients. Beginning 14 to 16 months after infusion of the genetically corrected cells, progressive cerebral demyelination in the two patients stopped, a clinical outcome comparable to that achieved by allogeneic HCT. Thus, lentiviral-mediated gene therapy of hematopoietic stem cells can provide clinical benefits in ALD.
_
Gene therapy using HIV helps children with fatal diseases, study says:
Gene therapy researchers say they used a safe version of HIV to prevent metachromatic leukodystrophy and halt Wiskott-Aldrich syndrome in children. Italian researchers have used a defanged version of HIV to replace faulty genes — and eliminate devastating symptoms — in children suffering two rare and fatal genetic diseases. Improved gene therapy techniques prevented the onset of metachromatic leukodystrophy in three young children and halted the progression of Wiskott-Aldrich syndrome in three others. Both diseases are caused by inherited genetic mutations that disrupt the body’s ability to produce crucial enzymes. In each trial, researchers took the normal form of the faulty gene and attached it to a virus derived from HIV that had been modified so that it could no longer cause AIDS. The researchers removed bone marrow stem cells from the patients and then used the lentivirus to infect those cells with the normal genes. The rest of the process resembled a traditional bone marrow transplant, with patients receiving chemotherapy to destroy their diseased bone marrow and then receiving infusions of the modified cells, which proliferated to form new marrow. Using the patients’ own cells sidesteps problems of donor incompatibility. The team treated the three metachromatic leukodystrophy patients before symptoms of the disorder had appeared. The kids stayed almost entirely symptom-free during the trial, up to two years after treatment. Gene therapy arrested the progression of disease in the Wiskott-Aldrich syndrome patients over up to two and a half years of follow-up. Looking at the patients’ bone marrow stem cells, the researchers found that 45% to 80% of the transplanted cells in the metachromatic leukodystrophy trial and 25% to 50% in the Wiskott-Aldrich trial produced the desired proteins, and continued to do so throughout roughly two years of follow-up.
_
Long-Term Follow-Up after Gene Therapy for Canavan Disease:
Canavan disease is a hereditary leukodystrophy caused by mutations in the aspartoacylase gene (ASPA), leading to loss of enzyme activity and increased concentrations of the substrate N-acetyl-aspartate (NAA) in the brain. Accumulation of NAA results in spongiform degeneration of white matter and severe impairment of psychomotor development. The goal of this prospective cohort study was to assess long-term safety and preliminary efficacy measures after gene therapy with an adeno-associated viral vector carrying the ASPA gene (AAV2-ASPA). Using noninvasive magnetic resonance imaging and standardized clinical rating scales, researchers observed Canavan disease in 28 patients, with a subset of 13 patients being treated with AAV2-ASPA. Each patient received 9 × 1011 vector genomes via intraparenchymal delivery at six brain infusion sites. Safety data collected over a minimum 5-year follow-up period showed a lack of long-term adverse events related to the AAV2 vector. Post treatment effects were analyzed using a generalized linear mixed model, which showed changes in predefined surrogate markers of disease progression and clinical assessment subscores. AAV2-ASPA gene therapy resulted in a decrease in elevated NAA in the brain and slowed progression of brain atrophy, with some improvement in seizure frequency and with stabilization of overall clinical status.
____
Gene therapy and MPS Diseases:
The Mucopolysaccharidoses (MPSs) are rare genetic disorders in children and adults. They involve an abnormal storage of mucopolysaccharides, caused by the absence of a specific enzyme. Without the enzyme, the breakdown process of mucopolysaccharides is incomplete. Partially broken down mucopolysaccharides accumulate in the body’s cells causing progressive damage. The storage process can affect appearance, development and the function of various organs of the body. Each MPS disease is caused by the deficiency of a specific enzyme. The MPS diseases are part of a larger group of disorders known as Lysosomal Storage Disorders (LSDs). The combined incidence of LSDs in the population is 1 in 5,000 live births. Apart from MPS II or Hunter Syndrome, the MPS diseases are caused by a recessive gene. Treating the rare disease MPS I is a challenge. MPS I, caused by the deficiency of a key enzyme called IDUA, eventually leads to the abnormal accumulation of certain molecules and cell death. The two main treatments for MPS I are bone marrow transplantation and intravenous enzyme replacement therapy, but these are only marginally effective or clinically impractical, especially when the disease strikes the central nervous system (CNS). Using an animal model, a team from the Perelman School of Medicine at the University of Pennsylvania has proven the efficacy of a more elegant way to restore IDUA levels in the body through direct gene transfer. Their work was published in Molecular Therapy. The study provides a strong proof-of-principle for the efficacy and practicality of intrathecal delivery of gene therapy for MPS patients. This first demonstration will pave the way for gene therapies to be translated into the clinic for lysosomal storage diseases.
______
Gene therapy for baldness:
Researchers at the University of Pennsylvania, led by Dr. George Cotsarelis, have regenerated follicles in mice by manipulating a gene called Wnt. The study potentially has broad applications, both for devising new methods to regrow hair and treating a variety of skin conditions and wounds. Wnt is involved in the healing of wounds and can be used to produce new hair follicles. The experiment showed that follicles can develop when a wound heals, and that the process can be manipulated to greatly increase the number of follicles. In the study, scientists removed small sections of skin from mice. This spurred stem cell activity in places where the skin was removed. However, when the scientists blocked the Wnt gene, follicles didn’t grow. When Wnt was stimulated, the skin healed without scarring and eventually had all the same characteristics — hair follicles, glands, appearance — of normal skin. These new follicles also behaved normally, producing hair in the same way as other follicles. The Penn team’s study, the results of which were published in the journal “Nature,” may unlock new possibilities in wound treatment and force scientists to reconsider the skin’s regenerative power. Unlike some animals that can regrow their tails or limbs (a severed sea star limb, for example, can even grow into an entirely new sea star), the regenerative abilities of mammals was thought to be rather limited. But in this case, follicles and the area around them showed a tremendous ability to regenerate with no apparent aftereffects. The technology used in the study has now been licensed to a company called Follica Inc. (Dr. Cotsarelis is a co-founder of Follica and a member of its scientific advisory board.) Follica hopes to use the technology to develop new treatments for hair loss and other disorders.
_
Gene therapy injections: Future obesity cure?
An injection that promises to end obesity seems like the type of claim found only on obnoxious flashing web ads, but it’s entirely plausible that one day we will be able to treat this common problem with just the prick of a needle, according to Jason Dyck, a researcher at the University of Alberta. Two years ago, Dyck and his colleagues published a paper in the journal Nutrition and Diabetes that concluded an injectable adiponectin gene therapy reduced fat and improved insulin sensitivity in mice, despite the fact the test animals were being fed a high-fat diet.
____
Heme oxygenase-1 (HO-1) gene therapy:
Heme oxygenase-1 (HO-1) is regarded as a sensitive and reliable indicator of cellular oxidative stress. Studies on carbon monoxide (CO) and bilirubin, two of the three (iron is the third) end products of heme degradation have improved the understanding of the protective role of HO against oxidative injury. CO is a vasoactive molecule and bilirubin is an antioxidant, and an increase in their production through an increase in HO activity assists other antioxidant systems in attenuating the overall production of reactive oxygen species (ROS), thus facilitating cellular resistance to oxidative injury. Gene transfer is used to insert specific genes into cells that are either otherwise deficient in or that underexpress the gene. Successful HO gene transfer requires two essential elements to produce functional HO activity. Firstly, the HO gene must be delivered in a safe vector, e.g., adenoviral, retroviral or leptosome based vectors, currently being used in clinical trials. Secondly, with the exception of HO gene delivery to either ocular or cardiovascular tissue via catheter-based delivery systems, HO delivery must be site and organ specific. This has been achieved in rabbit ocular tissues, rat liver, kidney and vasculature, SHR kidney, and endothelial cells.
______
Telomerase gene therapy in adult and old mice delays aging and increases longevity without increasing cancer:
A major goal in aging research is to improve health during aging. In the case of mice, genetic manipulations that shorten or lengthen telomeres result, respectively, in decreased or increased longevity. Based on this, researchers have tested the effects of a telomerase gene therapy in adult (1 year of age) and old (2 years of age) mice. Treatment of 1- and 2-year old mice with an adeno associated virus (AAV) of wide tropism expressing mouse TERT had remarkable beneficial effects on health and fitness, including insulin sensitivity, osteoporosis, neuromuscular coordination and several molecular biomarkers of aging. Importantly, telomerase-treated mice did not develop more cancer than their control littermates, suggesting that the known tumorigenic activity of telomerase is severely decreased when expressed in adult or old organisms using AAV vectors. Finally, telomerase-treated mice, both at 1-year and at 2-year of age, had an increase in median lifespan of 24 and 13%, respectively. These beneficial effects were not observed with a catalytically inactive TERT, demonstrating that they require telomerase activity. Together, these results constitute a proof-of-principle of a role of TERT in delaying physiological aging and extending longevity in normal mice through a telomerase-based treatment, and demonstrate the feasibility of anti-aging gene therapy.
_______
Gene therapy for botulism:
Mice study shows efficacy of new gene therapy approach for botulism toxin:
The current method to treat acute toxin poisoning is to inject antibodies, commonly produced in animals, to neutralize the toxin. But this method has challenges ranging from safety to difficulties in developing, producing and maintaining the anti-serums in large quantities. New research led by Charles Shoemaker, Ph.D., professor in the Department of Infectious Disease and Global Health at the Cummings School of Veterinary Medicine at Tufts University, shows that gene therapy may offer significant advantages in prevention and treatment of botulism exposure over current methods. Shoemaker has been studying gene therapy as a novel way to treat diseases such as botulism, a rare but serious paralytic illness caused by a nerve toxin that is produced by the bacterium Clostridium botulinum. Despite the relatively small number of botulism poisoning cases nationally, there are global concerns that the toxin can be produced easily and inexpensively for bioterrorism use. Botulism, like E. coli food poisoning and C. difficile infection, is a toxin-mediated disease, meaning it occurs from a toxin that is produced by a microbial infection. Shoemaker’s previously reported antitoxin treatments use proteins produced from the genetic material extracted from alpacas that were immunized against a toxin. Alpacas, which are members of the camelid family, produce an unusual type of antibody that is particularly useful in developing effective, inexpensive antitoxin agents. A small piece of the camelid antibody – called a VHH – can bind to and neutralize the botulism toxin. The research team has found that linking two or more different toxin-neutralizing VHHs results in VHH-based neutralizing agents (VNAs) that have extraordinary antitoxin potency and can be produced as a single molecule in bacteria at low cost. Additionally, VNAs have a longer shelf life than traditional antibodies so they can be better stored until needed. The newly published PLOS ONE study assessed the long-term efficacy of the therapy and demonstrated that a single gene therapy treatment led to prolonged production of VNA in blood and protected the mice from subsequent exposures to C. botulinum toxin for up to several months. Virtually all mice pretreated with VNA gene therapy survived when exposed to a normally lethal dose of botulinum toxin administered up to nine weeks later. Approximately 40 percent survived when exposed to this toxin as late as 13 or 17 weeks post-treatment. With gene therapy the VNA genetic material is delivered to animals by a vector that induces the animals to produce their own antitoxin VNA proteins over a prolonged period of time, thus preventing illness from toxin exposures. More research is being conducted with VNA gene therapy and it’s hard to deny the potential of this rapid-acting and long-lasting therapy in treating these and several other important illnesses.”
_______
Gene therapy trials:
The treatment of human diseases by gene transfer has begun in the United States. Since 1989, more than 100 gene marking and gene therapy trials have been approved by the Recombinant DNA Advisory Committee (RAC) of the National Institutes of Health and the Food and Drug Administration. The majority of these trials have been directed toward high-risk patient populations with incurable diseases, such as single-gene–inherited disorders, cancer, and AIDS. Several trials have been initiated that are relevant to cardiopulmonary diseases, including catheter-mediated gene delivery in a cancer trial for metastatic melanoma, an ex vivo treatment of transduced hepatocytes for familial hypercholesterolemia, and direct in vivo treatment for cystic fibrosis.
_
The figure below shows number of approved gene therapy trials in 2004 worldwide:
To date, over 1800 gene therapy clinical trials have been completed, are ongoing or have been approved worldwide. As of June 2012 update, we have entries on 1843 trials undertaken in 31 countries.
_
Number of trials per year:
The number of trials initiated each year has tended to drop in those years immediately following reports of adverse reactions, such as in 2003 and 2007 as seen in the figure below; however, 2005, 2006 and 2008 were strong years for gene therapy trials. The most recent years (2011 and 2012 in this case) tend to be underrepresented in the database because it takes time for articles to be published, causing a lag in obtaining information about the most recent trials.
_
The figure above shows number of gene therapy clinical trials approved worldwide 1989–2012.
_
Countries participating in gene therapy trials:
Gene therapy clinical trials have been performed in 31 countries, with representatives from all five continents. The continental distribution of trials has not changed greatly in the last few years, with 65.1% of trials taking place in the Americas (64.2% in 2007) and 28.3% in Europe (26.6% in 2007), with growth in Asia reaching 3.4% from 2.7% in 2007. The majority of the gene therapy clinical trials are carried out in North America and Europe, a development that may be at least partly due to a more conducive regulatory approach.
_
Gene therapy trials are conducted since more than 20 years with the largest number performed in the USA.
_
Diseases targeted by gene therapy:
The vast majority (81.5%) of gene therapy clinical trials to date have addressed cancer, cardiovascular disease and inherited monogenic diseases as seen in the figure below. Although trials targeting cardiovascular disease outnumbered trials for monogenic disease in 2007, the latter group has returned to being the second most common indication treated by gene therapy. It also represents the disease group in which the greatest successes of gene therapy to date have been achieved. For cancer the strategies aim to selectively kill the cancer cells either directly or via immunomodulation. The trial participants usually are in an advanced stage of disease development, for which no cure is available anymore. Other studies aim at replacing a defective gene, like in sickle-cell anaemia or Pompe disease. Also vaccination is experimented. Both academic and to a lesser extent industrial organisations investigate the possibilities of these techniques.
_
Gene types transferred in gene therapy clinical trials:
There have been a vast number of gene types used in human gene therapy trials as seen in the figure below. As would be expected, the gene types transferred most frequently (antigens, cytokines, tumour suppressors and suicide enzymes) are those primarily used to combat cancer (the disease most commonly treated by gene therapy). These categories account for 55.3% of trials, although it should be noted that antigens specific to pathogens are also being used in vaccines. Growth factors were transferred in 7.5% of trials, with almost all of these being aimed at cardiovascular diseases. Deficiency genes were used in 8.0% of trials, and genes for receptors (most commonly used for cancer gene therapy) in 7.2%. Marker genes were transferred in 2.9% of trials, whereas 4.3% of trials used replication inhibitors to target HIV infection. In 2.1% of trials, oncolytic viruses were transferred (rather than genes) with the aim of destroying cancer cells and 1.8% of trials involved the transfer of antisense or short interfering RNA, with the aim of blocking the expression of a target gene.
_
_
Vector types used in gene therapy trials:
Until now the most common vector to deliver therapeutic gene(s) are viruses as seen in figure below. They are administered either directly or after transducing autologous or allogeneic cells that are then injected in the participant. Also, bacteria and liposomes are used as vehicles for gene delivery. Naked DNA is sometimes applied.
_
Clinical trial phases:
All clinical trials are carefully monitored by the NIH, FDA and Institutional Review Boards based on preclinical studies using clinical grade reagents. Trials occur in three phases. Phase I studies usually involve a relatively small number of patients and are designed to evaluate the safety and potential toxicity of the procedure in a dose escalation series. Once a dose is selected that is considered relatively safe, a larger Phase 2 study can be undertaken to evaluate potential benefit of the treatment. If some benefit is indicated and the safety profile is good, a Phase 3 study will be taken with a large patient cohort to determine the statistical significance of therapeutic benefit. A critical component of clinical trials is patient consent to assure that the participating individuals understand the potential risk of the procedure weighed against any potential benefit to themselves or future patients. More than three quarters of gene therapy clinical trials performed to date are phase I or I/II; the two categories combined represent 78.6% of all gene therapy trials. Phase II trials make up 16.7% of the total, and phase II/III and III represent only 4.5% of all trials. The proportion of trials in phase II, II/III and III continues to grow over time (21.2% compared to 19.1% in 2007 and 15% in 2004), indicating the progress being made with respect to bringing gene therapy closer to clinical application.
_
Sponsorship:
All trials were divided on 2 categories – “academic” and “industry”. The term “academic” combined any monetary support (governments, funds…) other than “company-sponsored” (“industry”). Term “industry” also included companies – collaborators, when sponsorship is not clear from trial description.
_
Cell types:
There are 36 different cell types used in clinical trials. All cell types were roughly divided on “stem” and “non-stem”. “Stem” cell types included: embryonic stem cells, mesenchymal stromal cells, hematopoietic stem/ progenitor cells, cardiac stem/ progenitor cells, fetal neural stem cells, CD133+ cells, limbal stem cells, dental pulp stem cells, adipose stromal vascular fraction.
_________
Gene therapy protocols:
The first gene transfer in clinical study was initiated in 1990 (Blaese et al., 1995) and since then over 400 gene therapy protocols have been submitted to or approved by the National Institutes of Health (NIH) in the United States. As summarized in the table below, almost all clinical studies involve gene addition rather than the correction or replacement of defective genes, which is technically more challenging. Thus far, all clinical protocols involve gene transfer to exclusively somatic cells rather than germ line cells; the latter has been the subject of considerable ethical debate.
_
_
The table below shows gene therapy protocols worldwide:
_______
Does “clean environment” improve gene delivery to the brain? A study:
The data of this study demonstrate that the environment in which animals are raised plays an important role in determining the outcome of gene transfer experiments in the brain. A “clean” environment clearly reduces inflammatory and immune responses to adenoviral vectors, and is also likely to facilitate gene transfer mediated by other means. Importantly, this paper addresses some of the issues gene therapists will have to confront when moving into clinical arenas. While it is possible to raise animals under ‘pathogen free’ conditions, it is clearly much more difficult to do so with humans. Thus, this paper succeeds in modeling one of the challenges that clinical gene therapists will have to face. It is expected that a better understanding of the factors affecting inflammatory and immune responses against adenoviruses will facilitate the design of less toxic and less immunogenic viral vectors with increased gene transfer efficiency and longevity. Paradoxically, recent evidence suggests that in certain cases, inflammatory and immune cells may secrete neuronal growth factors, and have beneficial effects on neuronal survival. Thus, it has been recently shown that human T-cell lines specific for myelin autoantigens, and which are present in the brain of patients with inflammatory brain lesions produce biologically active BDNF; equally, autoimmune T cells can protect rodent retinal neurons from axotomy-induced cell death. Thus, inflammation may, at least in some cases, promote neuronal survival. How viral vector induced inflammation relates to vector encoded transgene longevity, and whether the beneficial role of certain inflammatory cells could be harnessed to achieve long term transgene expression in the brain, remains to be explored.
_______
Challenges to gene therapy:
Gene therapy is not a new field; it has been evolving for decades. Despite the best efforts of researchers around the world, however, gene therapy has seen only limited success. Why? Gene therapy poses one of the greatest technical challenges in modern medicine. It is very hard to introduce new genes into cells of the body and keep them working. And there are financial concerns: Can a company profit from developing a gene therapy to treat a rare disorder? If not, who will develop and pay for these life-saving treatments?
_
1. Challenges based on the disease characteristics:
Disease symptoms of most genetic diseases, such as Fabry’s, hemophilia, cystic fibrosis, muscular dystrophy, Huntington’s, and lysosomal storage diseases are caused by distinct mutations in single genes. Other diseases with a hereditary predisposition, such as Parkinson’s disease, Alzheimer’s disease, cancer and dystonia may be caused by variations/mutations in several different genes combined with environmental insults. Note that there are many susceptibility genes and additional mutations yet to be discovered. Gene replacement therapy for single gene defects is the most straightforward conceptually. However, even then the gene therapy agent may not equally reduce symptoms in patients with the same disease caused by different mutations, and even the same mutation can be associated with different degrees of disease severity. Gene therapists often screen their patients to determine the type of mutation causing the disease before enrollment into a clinical trial. The mutated gene may cause symptoms in more than one cell type, such as cystic fibrosis which affects lung cells and the digestive track. Thus, the gene therapy agent may need to replace the defective gene or compensate for its consequences in more than one tissue for maximum benefit. Alternatively, cell therapy can utilize stem cells with the potential to mature into the multiple cell types to replace defective cells in different tissues. In diseases like muscular dystrophy, for example, the high number of cells in muscles throughout the body that need to be corrected in order to substantially improve the symptoms makes delivery of genes and cells a challenging problem. Some diseases like cancer are caused by mutations in multiple genes. Although different types of cancers have some common mutations, every tumor from a single type of cancer does not contain the same mutations. This phenomenon complicates the choice of a single gene therapy tactic and has led to the use of combination therapies and cell elimination strategies. Disease models in animals do not completely mimic the human diseases and viral vectors may infect various species differently. The testing of vectors in animal models often resemble the responses obtained in humans, but the larger size of humans compared with rodents presents additional challenges in the efficiency of delivery and penetration of tissue. Gene therapy, cell therapy and oligonucleotide-based therapy agents are often tested in larger animal models, including rabbit, dog, pig and nonhuman primate models. Testing human cell therapy in animal models is complicated by immune rejections, requiring the animals to be immune suppressed. Furthermore, humans are a very heterogeneous population. Their immune responses to the vectors, altered cells or cell therapy products may differ or be similar to results obtained in animal models. For oligonucleotide-based therapies, chemical modifications of the oligonucleotides are often performed to attenuate an undesired non-specific immune response.
2. Challenges in development of gene and cell therapy agents:
Scientific challenges include development of gene therapy agents that express the gene in the relevant tissue at the appropriate level for the desired duration of time. While these issues are easy to state, each issue involves extensive research to identify the best means of delivery to the optimal tissue, how to control sufficient levels or numbers of cells, and factors that influence duration of gene expression or cell survival. After the delivery modalities are determined, identification and engineering of a promoter and control elements (on/off switch and dimmer switch) that will produce the appropriate amount of protein in the target cell can be combined with the relevant gene. This “gene cassette” is engineered into a vector or introduced into the genome of a cell and the properties of the delivery vehicle are tested in different types of cells in tissue culture. Sometimes things go as planned and then studies can be moved onto examination in animal models. In most cases, the gene/cell therapy agent may need to be improved further by adding new control elements to obtain the desired responses in cells and animal models. Furthermore, the response of the immune system needs to be considered based on the type of gene/cell therapy being undertaken. For example, in gene/cell therapy for cancer, one aim is to selectively boost the immune response to cancer cells. In contrast, in treating genetic diseases like hemophilia and cystic fibrosis the goal is for the therapeutic protein to be accepted by the immune system as “self”. If the new gene is inserted into the patient’s cellular DNA, the intrinsic sequences surrounding the new gene can affect its expression and vice versa. Scientists are now examining short DNA segments that may insulate the new gene from surrounding control elements. Theoretically, these “insulator” sequences would also reduce the effect of vector control signals in the gene cassette on adjacent cellular genes. Studies are also focusing on means to target insertion of the new gene into “safe” areas of the genome, to avoid influence on surrounding genes and to reduce the risk of insertional mutagenesis.
Challenges of cell therapy include the harvesting of the appropriate cell populations, and expansion or isolation of sufficient cells for one or multiple patients. Cell harvesting may require specific media to maintain the stem cells ability to self renew and mature into the appropriate cells. Ideally “extra” cells are taken from the individual receiving therapy which can be expanded in number in culture and induced to become pluripotent stem cells (iPS), thus allowing them to assume a wide variety of cell types and avoiding immune rejection by the patient. The long term benefit of stem cell administration requires that the cells be introduced into or migrate to the correct target tissue, and become established functioning cells within the tissue. Several approaches are being investigated to increase the number of stem cells that become established in the relevant tissue. Another challenge is developing methods that allow manipulation of the stem cells outside the body and while maintaining their ability to produce cells that mature into the desired specialized cell type. They need to provide the correct number of specialized cells and maintain their normal control of growth and cell division. Otherwise there is the risk that these new cells may become tumorigenic.
3. Gene delivery and activation:
For some disorders, gene therapy will work only if we can deliver a normal gene to a large number of cells—say several million—in a tissue. And they have to the correct cells, in the correct tissue. Once the gene reaches its destination, it must be activated, or turned on, to make the protein it encodes. And once it’s turned on, it must remain on; cells have a habit of shutting down genes that are too active or exhibiting other unusual behaviors. Targeting a gene to the correct cells is crucial to the success of any gene therapy treatment. Just as important, though, is making sure that the gene is not incorporated into the wrong cells. Delivering a gene to the wrong tissue would be inefficient, and it could cause health problems for the patient. For example, improper targeting could incorporate the therapeutic gene into a patient’s germline, or reproductive cells, which ultimately produce sperm and eggs. Should this happen, the patient would pass the introduced gene to his or her children. The consequences would vary, depending on the gene.
4. Immune response:
Our immune systems are very good at fighting off intruders such as bacteria and viruses. Gene-delivery vectors must be able to avoid the body’s natural surveillance system. An unwelcome immune response could cause serious illness or even death. The story of Jesse Gelsinger illustrates this challenge. Gelsinger, who had a rare liver disorder, participated in a 1999 gene therapy trial. He died of complications from an inflammatory response shortly after receiving a dose of experimental adenovirus vector. His death halted all gene therapy trials in the United States for a time, sparking a much-needed discussion on how best to regulate experimental trials and report health problems in volunteer patients. One way researchers avoid triggering an immune response is by delivering viruses to cells outside of the patient’s body. Another is to give patients drugs to temporarily suppress the immune system during treatment. Researchers use the lowest dose of virus that is effective, and whenever possible, they use vectors that are less likely to trigger an immune response.
5. Disrupting important genes in target cells:
A good gene therapy is one that will last. Ideally, an introduced gene will continue working for the rest of the patient’s life. For this to happen, the introduced gene must become a permanent part of the target cell’s genome, usually by integrating, or “stitching” itself, into the cell’s own DNA. But what happens if the gene stitches itself into an inappropriate location, disrupting another gene? This happened in two gene therapy trials aimed at treating children with X-linked Severe Combined Immune Deficiency (SCID). People with this disorder have virtually no immune protection against bacteria and viruses. To escape infections and illness, they must live in a completely germ-free environment. Between 1999 and 2006, researchers tested a gene therapy treatment that would restore the function of a crucial gene, gamma c, in cells of the immune system. The treatment appeared very successful, restoring immune function to most of the children who received it. But later, 4 of the children developed leukemia, a blood cancer. Researchers found that the newly transferred gamma c gene had stitched itself into a gene that normally helps regulate the rate at which cells divide. As a result, the cells began to divide out of control, causing leukemia. Doctors treated 4 of the patients successfully with chemotherapy, but the fourth died. This unfortunate incident raised important safety concerns, and researchers have since developed safer ways to introduce genes. Some newer vectors have features that target DNA integration to specific “safe” places in the genome where it won’t cause problems. And genes introduced to cells outside of the patient can be tested to see where they integrated, before they are returned to the patient.
6. Challenges in funding:
In most fields, funding for basic or applied research for testing innovative ideas in tissue culture and animal models for gene and cell therapy is available through the government and private foundations. These are usually sufficient to cover the preclinical studies that suggest potential benefit from a particular gene/cell therapy. Moving into clinical trials remains a huge challenge as it requires additional funding for manufacturing of clinical grade reagents, formal toxicology studies in animals, preparation of extensive regulatory documents and costs of clinical trials.
7. Commercial viability:
Many genetic disorders that can potentially be treated with gene therapy are extremely rare, some affecting just one person out of a million. Gene therapy could be life-saving for these patients, but the high cost of developing a treatment makes it an unappealing prospect for pharmaceutical companies. Developing a new therapy—including taking it through the clinical trials necessary for government approval— is very expensive. With a limited number of patients to recover those expenses from, developers may never earn money from treating such rare genetic disorders. And some patients may never be able to afford them. Some diseases that can be treated with gene therapy, such as cancer, are much more common. However, many promising gene therapy approaches are individualized to each patient. For example, a patient’s own cells may be taken out, modified with a therapeutic gene, and returned to the patient. This individualized approach may prove to be very effective, but it’s also costly. It comes at a much higher price than drugs that can be manufactured in bulk, which can quickly recover the cost of their development. If drug companies find a gene therapy treatment too unprofitable, who will develop it? Is it right to make expensive therapies available only to the wealthy? How can we bring gene therapy to everyone who needs it?
8. Longevity of Gene Expression:
One of the most challenging problems in gene therapy is to achieve long-lasting expression of the therapeutic gene, also called the transgene. Often the virus used to deliver the transgene causes the patient’s body to produce an immune response that destroys the very cells that have been treated. This is especially true when an adenovirus is used to deliver genes. The human body raises a potent immune response to prevent or limit infections by adenovirus, completely clearing it from the body within several weeks. This immune response is frequently directed at proteins made by the adenovirus itself. To combat this problem, researchers have deleted more and more of the virus’s own genetic material. These modifications make the viruses safer and less likely to raise an immune response, but also make them more and more difficult to grow in the quantities necessary for use in the clinic. Expression of therapeutic transgenes can also be lost when the regulatory sequences that control a gene and turn it on and off (called promoters and enhancers) are shut down. Although inflammation has been found to play a role in this process, it is not well understood, and much additional research remains to be done.
_____
The main reason why in vivo gene therapies have failed is the human immune system, which rejects the therapeutic vector or the genetically corrected cells (Manno et al, 2006), or causes acute toxic reactions that have been fatal in at least one case (Raper et al, 2003). For ex vivo gene therapy, the trouble has come from the uncontrolled insertion of the vector into the human genome, which has resulted in perturbed normal cell functions and has, in the worst cases, caused tumours (Hacein-Bey-Abina et al, 2003).
_____
Gene therapy safety issues:
Since the approval of the first clinical gene therapy trial in 1988 and its commencement in 1989, over 3000 patients have been treated with gene therapy. Many of the initial safety considerations raised with early trials remain today. These can be broadly categorised as either pertaining to the delivery vector or the expression of the transferred gene. The vast majority of clinical trials exploit viruses to transfer expression of genetic material to cells. Administration of a virus can result in inflammation or active infection. The risk of overwhelming inflammation from virus administration was experienced firsthand during the University of Pennsylvania study, which resulted in the death of an 18 year old participant. Secondly, active uncontrolled infection can occur either through multiple recombination events (unlikely given the current design) or through the contamination of replication incompetent viral stocks with a helper virus. There are no known cases of contaminated virus being delivered to patients, and clearly, the testing of material destined for clinical trials is essential and quite routine. Thirdly, the administration of retrovirus, which incorporates randomly into the genome, can result in insertional mutagenesis and malignant transformation. The expression of various types of therapeutic genes predisposes patients to adverse effects. As mentioned earlier, the utilisation of growth factors for neurodegenerative disease or the use of proangiogenic molecules for CAD can promote tumour growth. Likewise, the expression of proinflammatory cytokines for the treatment of malignancy can result in aberrant inflammatory conditions. Although the administration of any therapeutic agent is associated with side effects, the complete inability to withdraw the agent delivered via gene therapy is particularly troublesome. Finally, there is a theoretical risk of inadvertent alteration of germline cells. The event has been reported in animal models, but is yet to be accurately described after administration to humans.
_
What are the risks associated with gene therapy and cell therapy?
Risks of any medical treatment depend on the exact composition of the therapeutic agent and its route of administration. Different types of administration, whether intravenous, intradermal or surgical, have inherent risks. Risks include the outcome that gene therapy or cell therapy will not be as effective as expected, possibly making symptoms worse and prolonged, or complicating the condition with adverse effects of the therapy. The expression of the genetic material or the survival of the stem cells may be inadequate and/or may be too short-lived to fully heal or improve the disease. Their administration may induce a strong immune response to the protein in the case of replacing proteins from genetic diseases. This immune response may “get out of hand” and start attacking normal proteins or cells, as in autoimmune diseases. On the other hand, in the case of cancer or viral/fungal/bacterial infections, there may be an insufficient immune response, or the targeted cell or microorganism may develop resistance to the therapy. With the current generation of vectors in clinical trials, there is no way to “turn off” gene expression, if it seems to be producing unwanted effects. In the case of retroviral or lentiviral vectors, integration of the genetic material into the patients’ DNA may occur next to a gene involved in cell growth regulation and the insertion may induce a tumor over time by the process called insertional mutagenesis. High doses of some viruses can be toxic to some individuals or specific tissues, especially if the individuals are immune compromised. Gene therapy evaluation is generally carried out in animals/humans after birth. There is little data on what effects this therapeutic approach might have on embryos, and so pregnant women are usually excluded from clinical trials. Risks of cell therapy also include the loss of tight control over cell division in the stem cells. Theoretically, the transplanted stem cells may gain a growth advantage and progress to a type of cancer or teratomas. Since each therapy has its potential risks, patients are strongly encouraged to ask questions of their investigators and clinicians until they fully understand the risks.
_
The risks of gene therapy:
Some of these risks may include:
- The immune system may respond to the working gene copy that has been inserted by causing inflammation.
- The working gene might be slotted into the wrong spot.
- The working gene might produce too much of the missing enzyme or protein, causing other health problems.
- Other genes may be accidentally delivered to the cell.
- The deactivated virus might target other cells as well as the intended cells. Because viruses can affect more than one type of cell, it is possible that the viral vectors may infect cells beyond just those containing mutated or missing genes. If this happens, healthy cells may be damaged and cause other illness or diseases, including cancer.
- The deactivated virus may be contagious.
- If the new genes get inserted in the wrong spot in your DNA, there is a chance that the insertion might lead to tumor formation.
- When viruses are used to deliver DNA to cells inside the patient’s body, there is a slight chance that this DNA could unintentionally be introduced into the patient’s reproductive cells. If this happens, it could produce changes that may be passed on if a patient has children after treatment.
- Reversion of the virus to its original form. Once introduced into the body, the viruses may recover their original ability to cause disease.
- High cost.
- Potential for short-term efficacy.
- For certain types of gene therapy, we run the risk of permanently altering the human gene pool.
_
Gene therapy deaths: Jesse Gelsinger:
Jesse Gelsinger (June 18, 1981 – September 17, 1999) was the first person publicly identified as having died in a clinical trial for gene therapy. He was 18 years old. Gelsinger suffered from ornithine transcarbamylase deficiency, an X-linked genetic disease of the liver, the symptoms of which include an inability to metabolize ammonia – a byproduct of protein breakdown. The disease is usually fatal at birth, but Gelsinger had not inherited the disease; in his case it was apparently the result of a spontaneous genetic mutation after conception and as such was not as severe – some of his cells were normal, enabling him to survive on a restricted diet and special medications. Gelsinger joined a clinical trial run by the University of Pennsylvania that aimed at developing a treatment for infants born with severe disease. On September 13, 1999, Gelsinger was injected with an adenoviral vector carrying a corrected gene to test the safety of the procedure. He died four days later, September 17, at 2:30 pm, apparently having suffered a massive immune response triggered by the use of the viral vector used to transport the gene into his cells, leading to multiple organ failure and brain death. A Food and Drug Administration (FDA) investigation concluded that the scientists involved in the trial, including the co-investigator Dr. James M. Wilson (Director of the Institute for Human Gene Therapy), broke several rules of conduct:
1. Inclusion of Gelsinger as a substitute for another volunteer who dropped out, despite Gelsinger’s having high ammonia levels that should have led to his exclusion from the trial;
2. Failure by the university to report that two patients had experienced serious side effects from the gene therapy;
3. Failure to disclose, in the informed-consent documentation, the deaths of monkeys given a similar treatment.
The University of Pennsylvania later issued a rebuttal, but paid the parents an undisclosed amount in settlement. Both Wilson and the University are reported to have had financial stakes in the research. The Gelsinger case was a severe setback for scientists working in the field. Today, researchers might give Gelsinger lower therapy doses or pretreat him with immunosuppressive drugs. Another option being explored involves “naked” DNA, which refers to a nucleic acid molecule stripped of its viral carrier.
______
Problems with gene therapy:
_
_
Some of the unsolved problems with gene therapy include:
1. Short-lived nature of gene therapy – Before gene therapy can become a permanent cure for any condition, the therapeutic DNA introduced into target cells must remain functional and the cells containing the therapeutic DNA must be long-lived and stable. Problems with integrating therapeutic DNA into the genome and the rapidly dividing nature of many cells prevent gene therapy from achieving any long-term benefits. Patients will have to undergo multiple rounds of gene therapy.
2. Immune response – Any time a foreign object is introduced into human tissues, the immune system is stimulated to attack the invader. The risk of stimulating the immune system in a way that reduces gene therapy effectiveness is always a possibility. Furthermore, the immune system’s enhanced response to invaders that it has seen before makes it difficult for gene therapy to be repeated in patients.
3. Problems with viral vectors – Viruses, the carrier of choice in most gene therapy studies, present a variety of potential problems to the patient: toxicity, immune and inflammatory responses, and gene control and targeting issues. In addition, there is always the fear that the viral vector, once inside the patient, may recover its ability to cause disease.
4. Multigene disorders – Conditions or disorders that arise from mutations in a single gene are the best candidates for gene therapy. Unfortunately, some of the most commonly occurring disorders, such as heart disease, high blood pressure, Alzheimer’s disease, arthritis, and diabetes, are caused by the combined effects of variations in many genes. Multigene or multifactorial disorders such as these would be especially difficult to treat effectively using gene therapy.
5. For countries in which germ-line gene therapy is illegal, indications that the Weismann barrier (between soma and germ-line) can be breached are relevant; spread to the testes, therefore could impact the germline against the intentions of the therapy.
6. Chance of inducing a tumor (insertional mutagenesis) – If the DNA is integrated in the wrong place in the genome, for example in a tumor suppressor gene, it could induce a tumor. This has occurred in clinical trials for X-linked severe combined immunodeficiency (X-SCID) patients, in which hematopoietic stem cells were transduced with a corrective transgene using a retrovirus, and this led to the development of T cell leukemia in 3 of 20 patients. One possible solution for this is to add a functional tumor suppressor gene onto the DNA to be integrated; however, this poses its own problems, since the longer the DNA is, the harder it is to integrate it efficiently into cell genomes. The development of CRISPR technology in 2012 allowed researchers to make much more precise changes at exact locations in the genome.
7. The cost – only a small number of patients can be treated with gene therapy because of the extremely high cost (Alipogene tiparvovec or Glybera, for example, at a cost of $1.6 million per patient was reported in 2013 to be the most expensive drug in the world). In order to treat infants with Epidermolysis Bullosa (a rare skin disease that causes intense blistering), the first year alone of gene therapy may cost up to $100,000. The massive cost of these treatments creates a definite advantage for the wealthy.
8. Ethical and legal problems – Many believe that this is an invasion of privacy. They believe that if prenatal tests are performed that these could lead to an increase in the number of abortions.
9. Religious concerns – Religious groups and creationists may consider the alteration of an individual’s genes as tampering or corrupting God’s work.
10. Since human experimentation is not allowed, how much of simulated and/or animal research findings & observations can be reliably transferred to humans remains a question.
11. Regulation – what should & should not be included in gene therapy? Who should regulate/oversee? What about insurance problems?
_____
Cancer caused by gene therapy:
Originally, monogenic inherited diseases (those caused by inherited single gene defects), such as cystic fibrosis, were considered primary targets for gene therapy. For instance, in pioneering studies on the correction of adenosine deaminase deficiency, a lymphocyte-associated severe combined immunodeficiency (SCID), was attempted. Although no modulation of immune function was observed, data from this study, together with other early clinical trials, demonstrated the potential feasibility of gene transfer approaches as effective therapeutic strategies. The first successful clinical trials using gene therapy to treat a monogenic disorder involved a different type of SCID, caused by mutation of an X chromosome-linked lymphocyte growth factor receptor. While the positive therapeutic outcome was celebrated as a breakthrough for gene therapy, a serious drawback subsequently became evident. By February 2005, four children out of seventeen who had been successfully treated for X-linked SCID developed leukemia because the vector inserted near an oncogene (a cancer-causing gene), inadvertently causing it to be inappropriately expressed in the genetically-engineered lymphocyte target cell. On a more positive note, a small number of patients with adenosine deaminase-deficient SCID have been successfully treated by gene therapy without any adverse side effects. Chemotherapy led to sustained remission in 3 of the 4 cases of T cell leukemia, but failed in the fourth. Successful chemotherapy was associated with restoration of polyclonal transduced T cell populations. As a result, the treated patients continued to benefit from therapeutic gene transfer. The continual expression of a growth factor in neurodegenerative disorders predisposes to malignancy, as was noted by the researchers conducting the AD clinical trials. Accelerated tumor growth was observed in a patient with an occult lung tumor receiving VEGF therapy for therapeutic angiogenesis and resulted in the halting of that trial by the Food and Drug Administration. So there are many ways in which gene therapy recipient develops cancer.
_____
Limitations of gene therapy:
1. General limitations of current gene therapy technology include inefficient gene transfer. Viral vectors are extremely inefficient at transferring genetic material to human cells; even those with very high transduction efficiency in vitro fail to produce significant infection rates when applied to clinical trials. This factor played an important role in the escalation of dose in the ill fated University of Pennsylvania gene therapy clinical trial.
2. Another overarching issue is the lack of viral specificity. Current techniques do not allow for specific infection of cells; rather, cells in the vicinity of virus delivery are randomly infected. This issue has been partially addressed by the use of tissue specific promoters, which allow expression of the transgene only in tissue that can activate a specific promoter. However, this strategy is not amenable to all disease states and it continues to suffer from technical difficulties such as promoter “leakage” from endogenous viral sequences.
3. Another issue is the lack of long term transgene expression. Although not a concern in some clinical settings, as was demonstrated in PVD and CAD gene therapy, the need for long term expression of a therapeutic gene is essential in other strategies. For example, if the patients in the AD trial received fibroblasts that only expressed neurotrophic factor and salvaged neurones for one year, would the risk of the procedure outweigh the benefit considering that current medication also delays progression for approximately one year? The problem has been noted in multiple in vitro studies and animal studies where initial high levels of therapeutic protein have resulted in clinical responses, only to be lost several months later.
4. A final issue, and perhaps most important, is that of controlled gene expression. The ability to turn “on” and “off” the expression of a therapeutic gene will be essential for those strategies requiring long term expression and those inducing inflammation or utilising growth factors. Induction of inflammation for treating such diseases as cancer may be useful, but once the cancer is cured the inflammation continues if bystander cells are expressing the inciting transgene. Chronic inflammation of a specific tissue is undesirable. Similarly, with the use of growth factors, uncontrolled growth factor expression and function is intimately involved in the malignant transformation processes. The continual expression of a growth factor predisposes to malignancy, as was noted by the researchers conducting the AD clinical trials. It is essential to be able to turn off growth factor expression if malignancy is detected, or if treatment is toxic or no longer deemed useful or necessary. To this end, progress has been made in the development of inducible promoter systems, for example, a tetracycline inducible promoter system has been defined in which the presence of tetracycline (which can be taken orally by patients) will allow the activation of a promoter sequence and result in subsequent therapeutic gene expression. In the absence of tetracycline, theoretically, the transgene is not expressed. This “on/off” system allows for important dose delivery control. However, these systems are generally plagued by “leakage” of promoter activity and are currently imperfect.
5. Multigene disorders – With so much still unknown about the nature and treatment of multigene disorders, single gene disorders have the best chance of being corrected through gene therapy. However, many common diseases such as heart disease, high blood pressure, arthritis, and diabetes may be caused by multiple gene interactions (polygenic diseases). Unfortunately, until our technology and understanding of the genetic components of these diseases improves, they cannot be treated using gene therapy.
_____________
Can somatic gene therapy inadvertently lead to germ line gene therapy?
The Weismann barrier:
The Weismann barrier is the principle, proposed by August Weismann, that hereditary information moves only from genes to body cells, and never in reverse. In more precise terminology hereditary information moves only from germline cells to somatic cells (that is, soma to germline feedback is impossible). This does not refer to the central dogma of molecular biology which states that no sequential information can travel from protein to DNA or RNA.
_
In plants, genetic changes in somatic lines can and do result in genetic changes in the germ lines, because the germ cells are produced by somatic cell lineages (vegetative meristems), which may be old enough (many years) to have accumulated multiple mutations since seed germination, some of them subject to natural selection.
_
Scientists in the field of somatic and germline gene therapy in humans are either unaware of, or are silent about the fact that the Weismann Barrier could be permeable. They apparently don’t know about the evidence supporting soma-to-germline gene flow. In the late 20th century there have been criticisms of an impermeable Weismann barrier. These criticisms are all centered around the activities of an enzyme called reverse transcriptase.
_
Evidence has begun to mount for horizontal gene transfer. Different species appear to be swapping genes through the activities of retroviruses. Retro-viruses are able to transfer genes between species because they reproduce by integrating their code into the genome of the host and they often move nearby code in the infected cell as well. Since these viruses use RNA as their genetic information they need to use reverse transcriptase to convert their code into DNA first. If the cell they infect is a germline cell then that integrated DNA can become part of the gene pool of that species.
_
Horizontal Gene Transfer (Lateral Gene Transfer) is the natural transfer of DNA from one species to an unrelated species, especially interkingdom gene transfer. If a certain gene is present in the genome of all individuals of a species and if it is confirmed that it is a case of Horizontal Gene Transfer, then the gene must have passed the Weismann Barrier. So all cases of Horizontal Gene Transfer inevitably imply a passage of the Weismann Barrier. Direct uptake of foreign genetic material by the germ line is suggested by the evidence. Bushman (2002) uses the word ‘germ-line tropism’, but he does not give any further details. In any case it seems that some retroviruses are able to insert themselves in the germline, while others such as HIV fail to do so and instead target immune cells (soma). Bushman notes also that nondestructive replication in germline is required (otherwise the sperm or egg will be destroyed and cannot participate in fertilisation). So a combination of ‘germ-line tropism’ and nondestructive replication is required for successful integration in the germline. Evidence for Horizontal Gene Transfer in bacteria, plants and animals has been collected in Syvanen and Kado. In another recent book Lateral DNA Transfer by Frederic Bushman, a magnificent overview is given of lateral gene transfer in all forms of life. Highly relevant is the topic “endogenous retroviruses”. Endogenous retroviruses have been demonstrated in mice, pigs and humans. They originate from retroviral infection of germ-line cells (egg or sperm), followed by a stable integration in the genome of the species. “Humans harbor many endogenous retroviruses. Analysis reveals that the human genome contains fully 8% endogenous retroviral sequences, emphasizing the contribution of retroviruses to our genetic heritage”. But again this means that all those sequences must have passed the Weismann Barrier.
_
Other evidence against Weismann’s barrier is found in the immune system. A controversial theory of Edward J. Steele’s suggests that endogenous retroviruses carry new versions of V genes from soma cells in the immune system to the germ line cells. This theory is expounded in his book Lamarck’s signature. Steele observes that the immune system needs to be able to evolve fast to match the evolutionary pressure (as the infective agents evolve very fast). He also observes that there are plenty of endogenous retro-viruses in our genome and it seems likely that they have some purpose.
_
No author considers the possibility that vectors targeted at somatic cells could end up in germline cells. The suggestion is that because somatic gene therapy is not inherited by definition, that’s how gene therapy behaves in real-life. People writing about the safety and ethics of somatic gene therapy in humans, all assume somatic gene therapy does not and cannot have an effect on the germline. Apart from the first quote nobody explicitly states why there could not be such an effect. The effect on the germline could be viewed disadvantageous or advantageous. The point is that people in the gene therapy field assume that there is an ethical relevant difference between somatic and germline gene therapy, as can be concluded from their websites. The limited scope of somatic gene therapy, the individual, is contrasted with the effects for the human gene pool of germline therapy. However if Weismann’s Barrier is permeable, this assumption is wrong. The more effective the soma-to-germline feedback system of Edward Steele is, the less relevant the ethical difference between somatic and germline gene therapy is. If somatic immuno-V-genes can find their way to the germline and can precisely replace germline V-genes, why not any other gene in a viral vector?
_
From an unexpected source and independent of Steele’s line of research, for the first time evidence has been produced that a therapeutic gene used to treat a disease in animals found its way into sperm and eggs. Mohan Raizada et al at the University of Florida in Gainesville have delivered a therapeutic gene, inserted in a modified virus, into the hearts of rats that are predisposed to high blood pressure, and these rats and two subsequent generations were protected from hypertension. Raizada: “Our data support the notion that the AT1R-AS is integrated into the parental genome and is transmitted to the offspring. The possibility that lack of a blood-gonadal barrier and the presence of significant numbers of undifferentiated germ cells in the neonatal rat cannot be ruled out.” According to Theodore Friedmann, director of the human gene therapy program at the University of California in San Diego “this is a startling and very surprising result. It would have been impressive if even a few viruses travelled from the heart to the gonads, but the idea that all offspring inherited the therapeutic gene seems inconceivable”. Indeed inconceivable if one dogmatically accepts the Weismann Barrier and indeed surprising if one doesn’t know about Steele’s results.
_______
The regulation of a human gene by DNA derived from an endogenous retrovirus (ERV):
An ERV is a viral sequence that has become part of the infected animal’s genome. Upon entering a cell, a retrovirus copies its RNA genome into DNA, and inserts the DNA copy into one of the host cell’s chromosomes. Different retroviruses target different species and types of host cells; the retrovirus only becomes endogenous if it inserts into a cell whose chromosomes will be inherited by the next generation, i.e. an ovum or sperm cell. The offspring of the infected individual will have a copy of the ERV in the same place in the same chromosome in every single one of their cells. This happens more often than you might think; 8% of the modern human genome is derived from ERVs. Human endogenous retrovirus (HERV) proviruses comprise a significant part of the human genome, with approximately 98,000 ERV elements and fragments making up nearly 8%. According to a study published in 2005, no HERVs capable of replication had been identified; all appeared to be defective, containing major deletions or nonsense mutations. This is because most HERVs are merely traces of original viruses, having first integrated millions of years ago. Repeated sequences of this kind were formerly considered to be non-functional, or “junk” DNA. However, we’re gradually finding more and more examples of viral sequences that appear to have some kind of function in human cells. For example, many ERV sequences play a role in human gene regulation. ERVs contain viral genes, and also sequences – known as promoters – that dictate when those genes should be switched on. When an ERV inserts into the host’s chromosome, its promoter can start to interfere with the regulation of any nearby human genes. Humans share about 99% of their genomic DNA with chimpanzees and bonobos; thus, the differences between these species are unlikely to be in gene content but could be caused by inherited changes in regulatory systems. It is likely that some of these ERVs could have integrated into regulatory regions of the human genome, and therefore could have had an impact on the expression of adjacent genes, which have consequently contributed to human evolution.
_
Other researchers believe that a strong case can be made pointing to the view that ERVs were not inserted by retroviruses. They have function, should have been ridden by apoptosis, are different than their ancestral genomes, and it is incredible that the organisms did not die after being infected with so many viral genes.
_
How above discussion on endogenous retroviruses is related to the topic of ‘gene therapy’:
Immunological studies have shown some evidence for T cell immune responses against HERVs in HIV-infected individuals. The hypothesis that HIV induces HERV expression in HIV-infected cells led to the proposal that a vaccine targeting HERV antigens could specifically eliminate HIV-infected cells. The potential advantage of this novel approach is that, by using HERV antigens as surrogate markers of HIV-infected cells, it could circumvent the difficulty inherent in directly targeting notoriously diverse and fast-mutating HIV antigens.
______
Viruses and evolution:
Viruses are extraordinarily diverse genetically, in part because they can acquire genes from their hosts. They can later paste these genes into new hosts, potentially steering their hosts onto new evolutionary paths. The genomes of many organisms contain endogenous viral elements (EVEs). These DNA sequences are the remnants of ancient virus genes and genomes that ancestrally ‘invaded’ the host germline. For example, the genomes of most vertebrate species contain hundreds to thousands of sequences derived from ancient retroviruses. These sequences are a valuable source of retrospective evidence about the evolutionary history of viruses, and have given birth to the science of paleovirology. Once endogenous retroviruses infect the DNA of a species, they become part of that species: they reside within each of us, carrying a record that goes back millions of years. What is remarkable here, and unique, is the fact that endogenous retroviruses are two things at once: genes and viruses. And those viruses helped make us who we are today just as surely as other genes did. Patrick Forterre, an evolutionary biologist at the University of Paris-Sud in Orsay, France, believes that viruses are at the very heart of evolution. Viruses, Forterre argues, bequeathed DNA to all living things. Trace the ancestry of your genes back far enough, in other words, and you bump into a virus. Other experts on the early evolution of life see Forterre’s theory as bold and significant.
_
Gene therapy and human evolution:
In order to have any evolution of a species whatsoever, there must be some sort of mutation. Granted, the majority of mutations attempted by a species fail miserably and the individual plant/animal will not survive, but without mutation, the gene pool is limited – stagnant, and when the gene pool is stagnant, there is less chance for survival, and evolution essentially stops. With that in mind, and the entirety of evolutionary processes, what are we humans doing in the field of genetic modifying medicine? Gene therapy may help a lot of people live out healthier, happier lives, but is this helping evolution? Many philosophers invoke the “wisdom of nature” in arguing for varying degrees of caution in the development and use of genetic enhancement technologies. Because they view natural selection as akin to a master engineer that creates functionally and morally optimal design, these authors tend to regard genetic intervention with suspicion. Do we allow, a hundred years – or maybe even decades – from now parents to essentially create their own children by choosing eye color, hair color, intelligence and strength through the simple selection and rejection of genes? Could this genetic enhancement alter the process of human evolution, for it would disallow mutations in pursuit of the ‘perfect’ child? Well, we must pursue gene therapy and not genetic enhancement. Gene therapy is unlikely to play as important a role in evolution, since it only involves insertion of genes to treat disease, and is generally not concerned with major genetic changes of the kind that would result in evolution of new species. By highlighting the constraints on ordinary unassisted evolution, researchers show how intentional genetic modification can overcome many of the natural impediments to the human good. Their contention is that genetic engineering offers a solution that is more efficient, reliable, versatile, and morally palatable than the lumbering juggernaut of Darwinian evolution. So rather than grounding a presumption against deliberate genetic modification, the causal structure of the living world gives us good moral reason to pursue it.
_______
Gene doping:
Is science killing sport? Gene therapy and its possible abuse in doping:
In gene doping, athletes would modify their genes to perform better in sports. Gene doping is an outgrowth of gene therapy. However, instead of injecting DNA into a person’s body for the purpose of restoring some function related to a damaged or missing gene, as in gene therapy, gene doping involves inserting DNA for the purpose of enhancing athletic performance. Gene doping is an unintentional spin-off of gene therapy in which, doctors add or modify genes to prevent or treat illness. Gene doping would apply the same techniques to enhancing someone who is healthy. The line is fuzzy, but if the cells or body functions being modified are normal to start with, it’s doping. Gene doping is defined by the World Anti-Doping Agency as “the non-therapeutic use of cells, genes, genetic elements, or of the modulation of gene expression, having the capacity to improve athletic performance”. A complex ethical and philosophical issue is what defines “gene doping”, especially in the context of bioethical debates about human enhancement. The World Anti-Doping Agency (WADA) has already asked scientists to help find ways to prevent gene therapy from becoming the newest means of doping. The World Anti-Doping Agency (WADA) is the main regulatory organization looking into the issue of the detection of gene doping. Both direct and indirect testing methods are being researched by the organization. Directly detecting the use of gene therapy usually requires the discovery of recombinant proteins or gene insertion vectors, while most indirect methods involve examining the athlete in an attempt to detect bodily changes or structural differences between endogenous and recombinant proteins. Indirect methods are by nature more subjective, as it becomes very difficult to determine which anomalies are proof of gene doping, and which are simply natural, though unusual, biological properties. For example, Eero Mäntyranta, an Olympic cross country skier, had a mutation which made his body produce abnormally high amounts of red blood cells. It would be very difficult to determine whether or not Mäntyranta’s red blood cell levels were due to an innate genetic advantage, or an artificial one. Other previously claimed possible examples of exceptions include Lance Armstrong, a professional cyclist, whose body produces approximately half as much lactic acid as an average person, thus improving his performance in endurance sports such as cycling. Armstrong was, however, later proved to have taken performance-enhancing drugs.
_
Targets for gene doping:
Myostatin:
Myostatin is a protein responsible for inhibiting muscle differentiation and growth. Removing the myostatin gene or otherwise limiting its expression leads to an increase in hypertrophy and power in muscles. Whippets have been found with myostatin-related muscle hypertrophy that is caused by a mutation in their myostatin gene that makes them much faster than their wild-type counterparts, while whippets with two mutated copies have significantly increased musculature compared to wild-type and single mutation whippets. Similar results have also been found in mice, producing so-called “Schwarzenegger mice”. Humans have also demonstrated the same results: a German boy with a mutation in both copies of the myostatin gene was born with well-developed muscles. The advanced muscle growth continued after birth, and the boy could lift weights of 3 kg at the age of 4. Reducing or eliminating myostatin expression is thus seen as a possible future candidate for increasing muscle growth for the sake of increasing athletic performance in humans.
Erythropoietin (EPO):
Erythropoietin is a hormone which controls red blood cell production. Athletes have used EPO as a performance-enhancing substance for many years, though exclusively by receiving exogenous injections of the hormone. Recent studies suggest it may be possible to introduce another EPO gene into an animal in order to increase EPO production endogenously. EPO genes have been successfully inserted into mice and monkeys, and were found to increase hematocrits by as much as 80 percent in those animals. However, the endogonous and transgene derived EPO elicited autoimmune responses in some animals in the form of severe anemia.
Insulin-like growth factor 1:
Insulin-like growth factor 1 is a protein involved in the mediation of the growth hormone. IGF-1 also regulates cell growth effects and cellular DNA synthesis. While most of the research on IGF-1 has focused on potentially alleviating the symptoms of patients with muscular dystrophy, the primary focus from a gene doping perspective is its ability to increase the rate of cell growth, in particular muscle cells. In addition, the effects of IGF-1 appear to be localized. This key advantage will allow potential future users to choose specific muscle groups to grow, e.g. a baseball pitcher could choose to increase the muscle mass on one arm.
Vascular endothelial growth factor:
Vascular endothelial growth factor is a signal protein responsible for beginning the processes of vasculogenesis and angiogenesis. Interest in the protein lies in boosting its production in the body, thereby increasing the production of red blood cells. This should allow a greater quantity of oxygen to reach the cells of an athlete’s body, thereby increasing their performance (especially endurance sports). VEGF has already been through extensive trials as a form of gene therapy for patients with angina or peripheral arterial disease, leading Halsma and de Hon to believe that it will soon be used in a gene doping context.
_
Would Gene Doping be safe?
More important than the ethical implications of gene doping, some experts say, is the fact that gene doping could be dangerous, and perhaps even fatal. Consider the protein erythropoietin (EPO), a hormone that plays a key role in red blood cell production. When Wilson and colleagues injected macaque monkeys with viral vectors carrying the EPO gene, the host cells ended up producing so many red blood cells that the macaques’ blood initially thickened into a deadly sludge. The scientists had to draw blood at regular intervals to keep the animals alive. Over time, as the animals’ immune systems kicked in, the situation reversed and the animals became severely anemic (Rivera et al., 2005).
_
Laws aside, gene doping raises ethical issues. Thomas Murray, president of the Hastings Center, a nonprofit bioethics institute in New York, raises four arguments against allowing gene doping. The first argument is the risk to the individual athlete, though the procedures will become safer and more reliable over time, he says. Second is unfairness. “Some athletes will get access to it before others, especially in safe and effective forms,” he says. Third is the risk to other athletes. If gene doping were allowed, and one athlete tried it, everyone would feel pressured to try it so as not to lose. An enhancement arms race would follow. “Only athletes willing to take the largest amounts of genetic enhancements in the most radical combinations would have a chance at being competitive. The outcome would most assuredly be a public health catastrophe. And once everyone tried it, no one would be better off.” Finally, gene doping would change sports, Murray says. “Sports are in part constituted by their rules.”
______
Bio-warfare and gene therapy:
Application of Gene Therapy Strategies to Offensive and Defensive Bio-warfare:
The very discoveries which will make gene therapy a viable strategy in the near future, may also be applied to the development of novel biological weapons or the “upgrading” of current weapons so that they are able to circumvent current defensive strategies. Conversely, gene therapy strategies may also be applied to protect targets from specific bioweapons. Specific examples of such strategies are presented below.
Possible Offensive Applications of Gene Therapy Strategies to Bio-warfare:
A paradigm for biological weapons is the use of pathogenic viruses or bacteria to infect targets. Potential defenses against such agents include antibiotics or vaccines to suppress the development of infections by these agents or the use of immunologic or pharmacologic agents to suppress the effects of toxins that might be produced by the pathogens.
1. Use of drug resistance genes:
A strategy used in the gene therapy of cancer is to transfer genes which confer resistance to certain toxic drugs (i.e., chemotherapeutic agents) to the normal cells of a patient. For example, if the dose of a certain chemotherapeutic agent is limited by its toxicity to blood cells, then a gene which protects cells from the agent could be put into all blood cells. Therefore the blood cells would now be resistant to the chemotherapy drugs so that higher doses could be used. The higher doses might then allow for more effective killing of cancer cells. Examples of proteins which protect cells from chemotherapy drugs include enzymes which break down the drug inside cells, pumps which are able to pump the drugs out of cells and proteins which allow the cells to keep growing despite the damaging effects of the drug. Technology currently available for gene therapy and molecular biology could easily be adapted to transfer protective genes to pathogenic bioweapons such as bacteria and viruses, thus making them, or the cells they infect, resistant to drugs which might combat the warfare agents.
2. Alteration of toxin genes to potentiate biologic damage:
Another strategy in gene therapy is to replace genes which code for abnormal proteins with genes which code for proteins with normal or even improved functional properties. Genes coding for toxins of pathogenic microbes could be isolated and engineered ex vivo to produce proteins with altered properties. One example might include toxins which bind more strongly to a cellular target and thus produce a more potent response. Another might involve a toxin for which a specific pharmacologic inhibitor had been designed. The gene, and therefore the protein structure, of the toxin could be altered so that it was now resistant to the antidote but was still able to carry out its toxic function. Using gene therapy-derived gene transfer techniques these genes could then be returned to the parent microorganisms making them more effective biological weapons.
3. Alteration of genes to help microorganisms elude vaccine strategies:
One current defensive strategy against infectious bioweapons is to vaccinate potential targets so that an immune response is developed to the potential agents. These strategies result in the production of antibodies which can bind to and inhibit the function of biotoxins or kill microorganisms. Similarly, vaccines can also lead to the development of specific immune system cells (lymphocytes) which destroy invading microorganisms. Vaccines to specific organisms or the toxins they produce can potentially be administered to persons to elicit immune responses to these agents. The antibodies and lymphocytes which mediate these responses specifically recognize structural features of the microbe or toxin and destroy it. Using molecular biological techniques the genes for these immunologic targets can be isolated, modified so that they are no longer recognized by the target immune system and returned to the parental microbe to produce essentially a new strain which will not be recognized by the immune defenses of a vaccinated target.
4. Transfer of toxic gene products from one infectious bioweapon to an alternative agent:
A specific antibiotic, vaccine or other strategy might be developed against an infectious, toxin-producing bioweapon making that weapon ineffective. Using methods adapted from gene therapy the gene coding for the toxin could be identified, isolated and inserted into a new microorganism (for example a different bacteria or a virus) thus delivering the same toxin with a different vector.
5. Transfer of a non-microbial toxin gene into a microbe:
The gene for a non-microbial protein toxin (such as a snake, fish or spider venom) could be inserted into the genome of an infectious agent (such as a bacteria or a virus) so that the toxin would be produced within the target cells. Multiple toxin genes could also be inserted into the same vector to increase toxic potential.
6. Changing the tropism of an infectious bioweapon:
Many infectious agents infect specific cells within the human body by binding to proteins on the surface of the target cells. This binding to specific target cells is mediated by specific proteins of the surfaces of the viruses or bacteria. By exchanging the genes which code for these microbial proteins, the normal target tissues of the weapon could be changed so that a new organ can be targeted. For example, a virus that normally infects the liver and needs to enter a person’s blood stream to be effective could be altered to target lung tissue so that it could be administered by inhalation.
7. Development of novel infectious agents:
In order to create more effective viruses to transfer therapeutic genes, new versions of viruses have been developed from which many or most of the viral genes have been removed and then replaced by the gene or genes to be carried. While in many cases this has been done to remove genes coding for virulent proteins, similar manipulations could be performed to enhance the virulence of a virus. For example, genes coding for multiple toxins could be inserted into viruses. Another example is that a disease causing virus such as the AIDS virus could be made more virulent by the addition of a toxin or by changing the viral surface proteins so that the virus is resistant to vaccines.
8. Transfer of genes without microorganisms:
Because of potential hazards and inefficiencies involved with the use of microorganisms as vectors to transfer genes in gene therapy several strategies have been developed in which DNA genes can be put into a patientís cells directly. These technologies include the injection of gold particles coated with DNA into a person’s skin, direct injection or inhalation of naked DNA or DNA complexed to lipids. While these strategies are not likely to be applicable to large scale bioweapons, they might be effective as local weapons. One could envision the transfer of a toxin producing gene into a target or even the introduction of a gene that might cause cancer in a target several months or years after the attack.
9. Regulated expression of toxic genes:
In certain gene therapy applications it is advantageous to be able to turn genes which have been delivered to a patient on or off a specified times specific genes on or off by the administration of a drug. Such systems have already been developed and are being employed in models of gene therapy. These could be used as part of a controlled or clandestine bioweapons strategy where targets could be infected with a virus (for example) carrying a toxic gene. The gene would lie dormant inside the target cells until the signal, such as an common antibiotic tetracycline was ingested. This would then activate the gene and produce a lethal response.
___________
Gene therapy and ethics:
First of all, one must distinguish between gene therapy and genetic enhancement:
Therapy:
A widely accepted working definition of medical “therapy” comes from Norman Daniels’ formulation of the standard medical model. In the standard medical model, “therapy” is an intervention designed to maintain or restore bodily organization and functioning to states that are typical for one’s species, age, and sex. According to Daniels, society has a duty to provide “treatment” only for medical need defined as departure from normal organization and functioning.
Enhancement:
Enhancement, on the other hand, is alteration to improve upon normal organization, appearance, health, and functioning. Taking of anabolic steroids, undergoing certain forms of rhinoplasty, and altering one’s gametes to imbue one’s offspring with greater than average musical talent represent attempts at enhancement.
_
Ethical Consideration:
Gene therapy is a powerful new technology that might have unforeseen risks, scientists first develop a proposed experiments i.e. protocol, that incorporates strict guidelines. After the approval from FDA, the organization continues to monitor the experiment. In the course of a clinical trial, researchers are required to report any harmful side effects. Critics and proponents all agree that risks of gene therapy must not be substantially larger than the potential benefit. Gene therapy poses ethical considerations for people to consider. Some people are concerned about whether gene therapy is right and it may be used ethically.
Some of the ethical considerations for gene therapy include:
1. What is normal and what is a disability;
2. Whether disabilities are diseases and whether they should be cured;
3. Whether searching for a cure demeans the live of people who have disabilities;
4. Whether somatic gene therapy is more or less ethical than germ line gene therapy;
5. How can “good” and “bad” uses of gene therapy be distinguished?
6. Will the high costs of gene therapy make it available only to the wealthy?
7. Could the widespread use of gene therapy make society less accepting of people who are different?
8. Should people be allowed to use gene therapy to enhance basic human traits such as height, intelligence, or athletic ability?
_
Germ Line versus Somatic Cell Gene Therapy:
Successful germ line therapies introduce the possibility of eliminating some diseases from a particular family, and ultimately from the population, forever. However, this also raises controversy. Some people view this type of therapy as unnatural, and liken it to “playing God.” Others have concerns about the technical aspects. They worry that the genetic change propagated by germ line gene therapy may actually be deleterious and harmful, with the potential for unforeseen negative effects on future generations. Somatic cells are nonreproductive. Somatic cell therapy is viewed as a more conservative, safer approach because it affects only the targeted cells in the patient, and is not passed on to future generations. In other words, the therapeutic effect ends with the individual who receives the therapy. However, this type of therapy presents unique problems of its own. Often the effects of somatic cell therapy are short-lived. Because the cells of most tissues ultimately die and are replaced by new cells, repeated treatments over the course of the individual’s life span are required to maintain the therapeutic effect. Transporting the gene to the target cells or tissue is also problematic. Regardless of these difficulties, however, somatic cell gene therapy is appropriate and acceptable for many disorders, including cystic fibrosis, muscular dystrophy, cancer, and certain infectious diseases. Clinicians can even perform this therapy in utero, potentially correcting or treating a life-threatening disorder that may significantly impair a baby’s health or development if not treated before birth.
_
The ethical debate on germ line therapy has usually revolved around two kinds of issues:
1 – Germ line therapy is “open-ended” therapy. Its effects extend indefinitely into the future. This basically fits the objective of germ line therapy (assuming that it becomes possible one day), namely to correct a genetic defect once and for all. But precisely there lies also an ethical problem: an experiment in germ line therapy would be tantamount to a clinical experiment on unconsenting subjects, which are the affected members of future generations. This raises a number of very complex questions and is, in my view, an important but not necessarily overriding argument. A recent symposium on germ line engineering has concluded with a cautious “yes-maybe” for germ line gene therapy.
2 – Germ line therapy may involve invasive experimentation on human embryos. Although there are other potential targets for germ-line interventions, much of the discussion revolves around the genetic modification of early embryos, where the germ line has not yet segregated from the precursors of the various somatic cell types. As a result, the ethical assessment of germ line gene therapy will hinge in part on the ethical standing accorded to the early human embryo and the moral (dis)approval of early embryo experimentation. Those who believe the early embryo to be the bearer of considerable intrinsic moral worth or even that it is “like” a human person in a morally-relevant sense will conclude that embryo experimentation is to be rejected and germ-line therapy as well. Others think that it is only later in development that humans acquire those features that make them ethically and legally protected human subjects to the fullest degree. For them, the use of early embryos is not objectionable and germ line therapy cannot be ruled out on these grounds alone. As might be expected in view of the moral pluralism of modern societies, the policies of European countries differ in this respect: some permit some invasive research on human embryos (UK, Spain, Denmark), others ban it (Germany, Norway), others are still undecided. More generally, embryo-centered controversies are expected to increase as the field of embryonic stem-cell research becomes ever more promising. It is expected that this field will catch much of the public attention that was devoted to gene therapy in the nineties. Clearly, the question of the ethical standing of the human embryo is also of major importance for other medical procedures in reproductive medicine such as in-vitro fertilisation, pre-implantation diagnosis, experimentation on human embryos in general and abortion.
_
Research Issues:
Research is fraught with practical and ethical challenges. As with clinical trials for drugs, the purpose of human gene therapy clinical trials is to determine if the therapy is safe, what dose is effective, how the therapy should be administered, and if the therapy works. Diseases are chosen for research based on the severity of the disorder (the more severe the disorder, the more likely it is that it will be a good candidate for experimentation), the feasibility of treatment, and predicted success of treatment based on animal models. This sounds reasonable. However, imagine you or your child has a serious condition for which no other treatment is available. How objective would your decision be about participating in the research?
_
Informed Consent:
A hallmark of ethical medical research is informed consent. The informed consent process educates potential research subjects about the purpose of the gene therapy clinical trial, its risks and benefits, and what is involved in participation. The process should provide enough information for the potential research subjects to decide if they want to participate. It is important both to consider the safety of the experimental treatment and to understand the risks and benefits to the subjects. In utero gene therapy has the added complexity of posing risks not only to the fetus, but also to the pregnant woman. Further, voluntary consent is imperative. Gene therapy may be the only possible treatment, or the treatment of last resort, for some individuals. In such cases, it becomes questionable whether the patient can truly be said to make a voluntary decision to participate in the trial. Gene therapy clinical trials came under scrutiny in September 1999, after the highly publicized death of a gene therapy clinical trial participant several days after he received the experimental treatment. This case raised concerns about the overall protection of human subjects in clinical testing, and specifically about the reliability of the informed consent process. In this case, it was alleged that information about potential risks to the patient was not fully disclosed to the patient and his family. It was further alleged that full information regarding adverse events (serious side effects or deaths) that occurred in animals receiving experimental treatment had not been adequately disclosed. Adverse events should be disclosed in a timely manner not only to the participants in these trials, but also to the regulatory bodies overseeing gene therapy clinical trials. Furthermore, participants had not been told of a conflict of interest posed by a financial relationship between the university researchers and the company supporting the research. Obviously, any conflicts of interests could interfere with the objectivity of researchers in evaluating the effectiveness of the clinical trials and should be disclosed during the informed consent process.
_
Appropriate Uses of Gene Therapy:
How do researchers determine which disorders or traits warrant gene therapy? Unfortunately, the distinction between gene therapy for disease genes and gene therapy to enhance desired traits, such as height or eye color, is not clear-cut. No one would argue that diseases that cause suffering, disability, and, potentially, death are good candidates for gene therapy. However, there is a fine line between what is considered a “disease” (such as the dwarfism disorder achondroplasia) and what is considered a “trait” in an otherwise healthy individual (such as short stature). Even though gene therapy for the correction of potentially socially unacceptable traits, or the enhancement of desirable ones, may improve the quality of life for an individual, some ethicists fear gene therapy for trait enhancement could negatively impact what society considers “normal” and thus promote increased discrimination toward those with the “undesirable” traits. As the function of many genes continue to be discovered, it may become increasingly difficult to define which gene traits are considered to be diseases versus those that should be classified as physical, mental, or psychological traits. To date, acceptable gene therapy clinical trials involve somatic cell therapies using genes that cause diseases. However, many ethicists worry that, as the feasibility of germ line gene therapy improves and more genes causing different traits are discovered, there could be a “slippery slope” effect in regard to which genes are used in future gene therapy experiments. Specifically, it is feared that the acceptance of germ line gene therapy could lead to the acceptance of gene therapy for genetic enhancement. Public debate about the issues revolving around germ line gene therapy and gene therapy for trait enhancement must continue as science advances to fully appreciate the appropriateness of these newer therapies and to lead to ethical guidelines for advances in gene therapy research.
_
Initially, gene therapy was conceptualised mainly as a procedure to correct recessive monogenic defects by bringing a healthy copy of the deficient gene in the relevant cells. In fact, somatic gene therapy has a much broader potential if one thinks of it as a sophisticated means of bringing a therapeutic gene product to the right place in the body. The field has moved increasingly from a “gene correction” model to a “DNA as drug” model. This evolution towards an understanding of gene therapy as “DNA-based chemotherapy” underscores why the ethical considerations for somatic gene therapy are not basically different from the well-known ethical principles that apply in trials of any new experimental therapy
- Favourable risk-benefit balance (principle of beneficence/non-maleficence);
- Informed consent (principle of respect for persons);
- Fairness in selecting research subjects (principle of justice).
Clearly, the mere fact that gene therapy has to do with genes and the genome does not, in itself, make it “special” or “suspicious”. A further distinction ought to be made between in vivo and ex vivo somatic gene therapy. Ex vivo procedures entail the extraction of cells from the patient’s body (for instance bone-marrow cells), genetic modification of the cells using appropriate vectors or other DNA-transfer methods and reimplantation of the cells in the patient. In vivo therapy uses a vector or DNA-transfer technique that can be applied directly to the patient. This is the case of current experiments aimed at correcting the gene defect of cystic fibrosis by exposing lung epithelium to adenovirus-derived vectors containing the CFTR gene. In the in vivo case, the potential for unintended dissemination of the vector is more of an issue. Therefore, biological safety considerations must also be subjected to ethical scrutiny in addition to the patient-regarding concerns already mentioned.
_
Several mechanisms are in place to help the patient, family members, clinicians and scientists openly address any ethical issues associated with development of genes and cells as virtual drugs. Before enrolling a patient in a clinical trial, investigators must ensure the patient understands the potential benefits and risks associated with the trial. The process of educating patients to help them decide whether to enroll in a clinical trial is known as informed consent. If you or a family member is considering participating in a clinical trial, be sure to consult your physician before making any medical decisions.
_
Does it matter whether Genetic Intervention is Therapy, Prevention, Remediation, or Enhancement?
What does it matter whether a genetic intervention is called therapy, prevention, remediation, or enhancement? First, there is the obvious matter of equal access to the intervention. How an intervention is categorized largely determines how accessible it is to all who wish to use it. Looking into the future of germline genetic interventions, those that are labeled therapy, prevention, or remediation stand a far better chance of being available to people who cannot pay for them out-of-pocket. If an intervention is categorized as an enhancement, it will probably not be thought to satisfy the therapeutic goals of medicine and, hence, will not be a reimbursable service. Under such conditions, termed “genobility” by 2 bioethicists, the rich will not only have more money than the rest of us; they’ll be taller, smarter, and better looking, too. There is an individual therapy-enhancement matter that each physician will decide for himself and herself, and the question is not limited to genetics. Each individual physician must interpret the goals of medicine and the appropriate use of his or her education and skills in fulfilling those goals. A physician may decide not to use her skill and professional status to prescribe Ritalin (methylphenidate) for normal, healthy college students; another physician, not to manipulate embryos to produce super stars in athletics or the entertainment field. Either of these physician may, on the other hand, decide to prescribe growth hormone for a young boy who does not have growth hormone deficiency, but whose parents are both short and whose adult height will place him well below normal range for his sex. Many factors enter into the decision. Is there meaning in striving to make the most of what nature or God has given us? Do we cheat ourselves or others when we attempt to short-circuit the normal course of learning, say, or the discipline needed to excel in sport or in music? Do parents do a better job of parenting a made-to-order child? Is that what parenting is about? Is there possible harm in curtailing diversity in systematically preventing certain genotypes from coming into existence? To what extent do we, as physicians, help people by giving them what they ask for when what they ask for is unrelated to physical, mental, or emotional health? Some may shrug their shoulders at such weighty questions and say, “What difference does it make whether I provide services that stretch professional or ethical boundaries? If I don’t do it someone else will.” But therein lies the ethical boundary that must not be crossed: the boundary that separates exercise of professional judgment and integrity from shirking of responsibility. Every physician has entered into a covenant with society to apply his or her skills and judgment in the patient’s best interest. The bright ethical line in the debate over therapy versus enhancement separates acting in the patient’s best interest from abdicating the responsibility to determine, with the patient, what constitutes “best interest” in a given case. If the physician and patient disagree, the physician must act as professional ethics and the profession’s covenant with society direct.
_____
How society sees gene therapy:
A closer look at solid and sophisticated social scientific studies on public opinion about biotechnology reveals a nuanced image of the public and its understanding of genetic engineering. For Europe, the latest survey results show that the secular trend of declining optimism about biotechnology continues. However, there is strong evidence that people clearly distinguish between the various applications of biotechnology. Assessments tend to be based on perceptions and considerations of usefulness and moral acceptability. While the public does not see substantial benefits in agricultural biotechnology, strong support for the medical applications of biotechnology, even if they are risky, continues to exist. Also, there is no evidence of a correlation between knowledge about biotechnology and attitudes towards it. Those who are well-informed about biotechnology do not necessarily have positive attitudes towards it. At the same time, lack of information about genetic engineering does not simply translate as rejection of it. A similar picture emerges from US surveys, which show that the general attitudes toward biotechnology remain positive. Again, it is not so much the level of knowledge and scientific literacy which seems to determine attitudes toward biotechnology, but considerations of moral acceptability. The evidence from these surveys does not suggest that people could not be better informed about genetic engineering than they are, but it gives good reason to reconsider the ‘deficit theory’ of the public and its policy implications. If the public is not that ill-informed as is often suggested, what, then, explains the complicated relationship between gene therapy and society? Well, it is less lack of information than lack of trust which is at the root of the problem.
_
What are the potential social implications of gene therapy?
1. In the case of genetic enhancement, such manipulation could become a luxury available only to the rich and powerful.
2. Widespread use of this technology could lead to new definitions of “normal” which would have huge implications for persons with disabilities. This could lead to widespread use of the technology to “weed out” disability.
3. Gene therapy is currently focused on correcting genetic flaws and curing life –threatening disease, and regulations are in place for conducting these types of studies. But in the future, when the techniques of gene therapy have become simpler and more accessible, society will need to deal with more complex questions, such as the implications of using gene therapy to change behavioural traits.
4. Germline gene therapy would forever change the genetic make-up of an individual’s descendants. Thus, the human gene pool would be permanently affected. Although these changes would presumably be for the better, an error in technology or judgment could have far-reaching consequences.
_
Gene therapy in popular culture:
1. In the TV series Dark Angel gene therapy is mentioned as one of the practices performed on transgenics and their surrogate mothers at Manticore, and in the episode Prodigy, Dr. Tanaka uses a groundbreaking new form of gene therapy to turn Jude, a premature, vegetative baby of a crack/cocaine addict, into a boy genius.
2. Gene therapy is a crucial plot element in the video game Metal Gear Solid, where it has been used to illegally enhance the battle capabilities of soldiers within the US military, and their Next Generation Special Forces units.
3. Gene therapy plays a major role in the science fiction series Stargate Atlantis, as a certain type of alien technology can only be used if one has a certain gene which can be given to the members of the team through gene therapy involving a mouse retrovirus.
4. Gene therapy also plays a major role in the plot of the James Bond movie Die Another Day, where a scientist has developed a means of altering peoples’ entire appearances through the use of DNA samples acquired from others- generally homeless people that would not be missed- that are subsequently injected into the bone marrow, the resulting transformation apparently depriving the subjects of the ability to sleep.
5. Gene therapy plays a recurring role in the present-time science fiction television program ReGenesis, where it is used to cure various diseases, enhance athletic performance and produce vast profits for bio-tech corporations. (e.g. an undetectable performance-enhancing gene therapy was used by one of the characters on himself, but to avoid copyright infringement, this gene therapy was modified from the tested-to-be-harmless original, which produced a fatal cardiovascular defect)
6. Gene therapy is the basis for the plotline of the film I Am Legend.
7. Gene therapy is an important plot key in Bioshock where the game contents refer to plasmids and [gene] splicers.
8. The book Next by Michael Crichton unravels a story in which fictitious biotechnology companies experiment with gene therapy.
9. In the television show Alias, a breakthrough in molecular gene therapy is discovered, whereby a patient’s body is reshaped to identically resemble someone else. Protagonist Sydney Bristow’s best friend was secretly killed and her “double” resumed her place.
10. In the 2011 film Rise of the Planet of the Apes, a fictional gene therapy called ALZ-112 was a drug that was a possible cure for Alzheimer’s disease, the therapy increased the host’s intelligence and made their irises green, along with the revised therapy called 113 which increased intelligence in apes yet was a deadly, internal virus in humans.
_______
Individualized Medicine vis-à-vis Gene Therapy:
A decade ago, the human genome project was released making available an individual’s or an organism’s approximate 23,000 protein-coding genes with the underlying and seemingly well-founded hope at the time that gene therapy was closer than ever. In a strict sense, gene therapy equates with replacing a faulty gene or adding a new one in order to cure a disease or improve the organism’s ability to fight disease. However, this implies that challenges pertaining to uptake and regulated expression of foreign genes by host cells ought to be addressed. Specifically, gene delivery to the right cells, activation of gene expression, immune responses and ability to escape the body’s natural surveillance systems are well documented and critical issues remaining problematic to date. Despite an explosion in the understanding of the basic biological processes underlying many human diseases, the prospects for the widespread use of successful gene therapy are yet to meet the hype and excitement of the early days. Thus, the question arises: “Is gene therapy an unattainable dream? Have we made strides in spite or because of its severe hurdles?” The industry has historically proven to be adaptable and resilient in its ability to capitalize on the enormous masses of data stemming from various technologies introduced over the years. Consequently, it has: 1) Exploited genomics results and the congruent choice of receptors on a support basis in hopes of revolutionizing major bottlenecks in gene therapy, and 2) Focused on a path deviating from the original, highly ambitious goal of gene-based disease treatment toward genetic testing and personalized medicine. Admittedly, we are removed from the days when we dreamed that surgically replacing a defective gene to cure a genetically inherited disease would be a smashing success. Nevertheless we adopted a two-fold approach, in that we shifted toward addressing the immune-mediated response and the complications stemming from insertional mutagenesis in gene therapy protocols, while at the same time pursued genetic tests and molecular diagnostics to enable disease treatment on an individual level. Addressing the variability in patients and their responses to therapeutic interventions, as opposed to treating all individuals as a continuum, has expedited the momentum in clinical medicine.
_
Personalized medicine is an integrated approach to targeted therapy driven by and adjusted to the genetic variability of patients’ responses to drug treatments. In spite of obstacles and unlike gene therapy, which is still in clinical trials at best, personalized medicine has made its way to clinical practice with FDA-approved companion diagnostics. The National Institutes of Health (NIH) and the Food and Drug Administration (FDA) joined forces in envisioning an in-sync scientific and regulatory approach to steering patients to the right drug. The critical steps to marrying personalized medicine with the clinic are: 1) Identification of individuals with a predisposition for a certain disease; 2) Assessment of the precise nature of a disease; 3) Matching an individual’s genetic profile with the likely effect of a particular drug; 4) Development of policy and education strategies. It would help to address the objectives of the two disciplines, pharmacogenomics and pharmacogenetics, inherently associated with three of the critical steps at the outset, even though they have consistently been used interchangeably. Pharmacogenetics is the study of genetic variation that is deemed responsible for varying responses to drugs, while pharmacogenomics is the broader application of genomics to drug discovery. Thus, matching an individual’s genetic profile to the likely effect of certain drugs can help avoid hypersensitivity reactions to certain medications, correlate tumor mutations with drug efficacy, and identify poor metabolizers, that will inadvertently reduce the drug’s efficacy. Genomics technologies have brought the cost of sequencing from the original US$1 billion price tag to approximately $1,000, and in turn enabled the identification of novel targets, including mutants in disease states. The latter has successfully been coupled with drug discovery specifically aimed at the mutant protein. The aforementioned technologies resulted in 1,000 to 1,300 genetic tests for a total of 2,500 rare and common conditions; genetic testing uses diagnostic approaches to analyze various aspects of an individual’s genetic material, as well as gene by-products (biomarkers), such as proteins, enzymes, and metabolites. Diagnostic testing identifies patients who can benefit from targeted therapies. It would thus follow that the success of personalized medicine is highly dependent upon the accuracy of diagnostic tests that identify patients who can benefit from targeted therapies. This is also tied with the review and approval processes by the FDA in order to avoid erroneous usage of these tests. Consequently, the road to individualized medicine is mapped out and well on its way to making headways. Have we then moved fast enough in the last 10 years? Given the complexity of the human body and the molecular processes involved, we have definitely made advances that are noticeable. Gene therapy may have not materialized yet, but the reality that almost all genetic tests are available in clinical settings provides us with the reassurance that the last decade has been prolific in moving forward by appreciating individualized responses to therapy and how to circumvent them. Besides, the potential of microRNAs to be used as vectors modulating gene expression offers a new avenue in gene therapy that parallels the progress made in personalized medicine.
__________
Policy, laws and regulations of gene therapy:
Policies on genetic modification tend to fall in the realm of general guidelines about human-involved biomedical research. Universal restrictions and documents have been made by international organizations to set a general standard on the issue of involving humans directly in research. One key regulation comes from the Declaration of Helsinki (Ethical Principles for Medical Research Involving Human Subjects), last amended by the World Medical Association’s General Assembly in 2008. This document focuses on the principles physicians and researchers must consider when involving humans as the research subject. Additionally, the Statement on Gene Therapy Research initiated by the Human Genome Organization in 2001 also provides a legal baseline for all countries. HUGO’s document reiterates the organization’s common principles researchers must follow when conducting human genetic research including the recognition of human freedom and adherence to human rights, and the statement also declares recommendations for somatic gene therapy including a call for researchers and governments to attend to public concerns about the pros, cons and ethical concerns about the research.
United States:
Gene therapy is under study to determine whether it could be used to treat disease. Current research is evaluating the safety of gene therapy; future studies will test whether it is an effective treatment option. Several studies have already shown that this approach can have very serious health risks, such as toxicity, inflammation, and cancer. Because the techniques are relatively new, some of the risks may be unpredictable; however, medical researchers, institutions, and regulatory agencies are working to ensure that gene therapy research is as safe as possible. Comprehensive federal laws, regulations, and guidelines help protect people who participate in research studies (called clinical trials). The U.S. Food and Drug Administration (FDA) regulates all gene therapy products in the United States and oversees research in this area. Researchers who wish to test an approach in a clinical trial must first obtain permission from the FDA. The FDA has the authority to reject or suspend clinical trials that are suspected of being unsafe for participants. The National Institutes of Health (NIH) also plays an important role in ensuring the safety of gene therapy research. NIH provides guidelines for investigators and institutions (such as universities and hospitals) to follow when conducting clinical trials with gene therapy. These guidelines state that clinical trials at institutions receiving NIH funding for this type of research must be registered with the NIH Office of Biotechnology Activities. The protocol, or plan, for each clinical trial is then reviewed by the NIH Recombinant DNA Advisory Committee (RAC) to determine whether it raises medical, ethical, or safety issues that warrant further discussion at one of the RAC’s public meetings. An Institutional Review Board (IRB) and an Institutional Biosafety Committee (IBC) must approve each gene therapy clinical trial before it can be carried out. An IRB is a committee of scientific and medical advisors and consumers that reviews all research within an institution. An IBC is a group that reviews and approves an institution’s potentially hazardous research studies. Multiple levels of evaluation and oversight ensure that safety concerns are a top priority in the planning and carrying out of gene therapy research.
_
The legal framework for gene therapy in EU:
In the European Community (EC) ‘gene therapy’ is one of the ‘advanced therapies’ that are regulated in Regulation (EC) No 1394/20072. The definition of an ‘advanced therapy medicinal product’ (ATMP) is found in Article 2(1):
(a) ‘Advanced therapy medicinal product’ means any of the following medicinal products for human use:
– a gene therapy medicinal product as defined in Part IV of Annex I to Directive 2001/83/EC
– a somatic cell therapy medicinal product as defined in Part IV of Annex I to Directive 2001/83/EC
– a tissue engineered product as defined in point (b).
(b) ‘Tissue engineered product’ means a product that:
– contains or consists of engineered cells or tissues, and
– is presented as having properties for, or is used in or administered to human beings with a view to regenerating, repairing or replacing a human tissue.
A tissue engineered product may contain cells or tissues of human or animal origin, or both. The cells or tissues may be viable or non-viable. It may also contain additional substances, such as cellular products, bio-molecules, biomaterials, chemical substances, scaffolds or matrices. Products containing or consisting exclusively of non-viable human or animal cells and/or tissues, which do not contain any viable cells or tissues and which do not act principally by pharmacological, immunological or metabolic action, shall be excluded from this definition.
(c) Cells or tissues shall be considered ‘engineered’ if they fulfill at least one of the following conditions:
– the cells or tissues have been subject to substantial manipulation, so that biological characteristics, physiological functions or structural properties relevant for the intended regeneration, repair or replacement are achieved. The manipulations listed in Annex I, in particular, shall not be considered as substantial manipulations,
– the cells or tissues are not intended to be used for the same essential function or functions in the recipient as in the donor.
A gene therapy medicinal product is, as indicated, further defined in Directive 2001/83/EC3 as amended by Commission Directive 2003/63/EC4, in Annex I Part IV:
‘Gene therapy medicinal product’ shall mean a product obtained through a set of manufacturing processes aimed at the transfer, to be performed either in vivo or ex vivo, of a prophylactic, diagnostic or therapeutic gene (i.e. a piece of nucleic acid), to human/animal cells and its subsequent expression in vivo. The gene transfer involves an expression system contained in a delivery system known as a vector, which can be of viral, as well as non-viral origin. The vector can also be included in a human or animal cell.
Gene therapy medicinal products include:
1. Naked nucleic acid,
2. Complex nucleic acid or non-viral vectors,
3. Viral vectors,
4. Genetically modified cells.
_
I have highlighted policy, laws and regulations of gene therapy in America and Europe but every country must have policy, laws and regulations on gene therapy.
___________
Gene therapy research and future:
Over the past three decades, an increasing proportion of genetic research has consisted of molecular studies in medicine. It has resulted in a profound change in the understanding of the pathophysiology of diverse genetic diseases. Gene therapy is the use of nucleic acids as therapeutically useful molecules. Although many genetic discoveries have resulted in better diagnostic tests, the application of molecular technologies to the treatment of genetic diseases is natural and logical. Gene therapy is in a phase of its youth, nevertheless it holds very real promise. In the first 9 years, 396 clinical protocols have been approved worldwide and over 3,000 patients from 22 different countries have carried genetically engineered cells in their body. The conclusion from these trials are that gene therapy has the potential for treating a broad array of human diseases and the procedure appears to carry a definite risk of adverse reactions, but the efficiency of gene transfer and expression in human patients is low. No formal phase III studies to establish clinical efficacy have been completed. Gene therapy is potentially a powerful clinical approach, but it has been restricted by the limited knowledge of vectors and pathophysiology of the diseases to be treated. Better understanding of the disease processes, improvements in vector design, and a great attention to the pharmacological aspects should permit the development of more effective gene therapy.
_
Advances in gene therapy:
Despite the limitations of gene therapy, there has been a slow and steady progress as the number of diseases that can be treated with gene therapy has steadily increased. There are a variety of diseases that have been tested and researched for future therapy.
Experiments with gene therapy have been conducted for:
– Familial hypercholesterolemia
– Parkinson’s disease
– Several types of Severe Combined Immunodeficiency (SCID)
– Cystic fibrosis
– Gaucher’s disease
Scientists believe gene therapy has potential to treat:
– Diabetes
– Alzheimer’s disease
– Arthritis
– Heart disease
_________
_________
Some recent advances in clinical gene therapy updated up to 2012:
| Vector, dose range, and number and ages of patients | Transgene and promoter | Route of administration and cell target | Scientific and clinical outcomes | |
| Leber’s congenital amaurosis | AAV2; 1.5 × 1010 vg per patient; three patients (19–26 years old) | RPE65 under chicken β-actin promoter | Subretinal injection to retinal epithelial cells | All patients showed improved visual acuity and modest improvements in pupillary light reflexes. |
| AAV2; 1011 vg per patient; three patients (17–23 years old) | RPE65 under cognate promoter | Subretinal injection to retinal epithelial cells | No change in visual acuity or retinal responses to flash or pattern electroretinography; microperimetry and dark-adapted perimetry showed no change in retinal function in patients 1 and 2 but showed improved retinal function in patient 3. | |
| AAV2; 1.5 × 1010, 4.8 × 1010 or 1.5 × 1011 vg per patient; 12 patients (8–44 years old) | RPE65 under chicken β-actin promoter | Subretinal injection to retinal epithelial cells | All patients showed sustained improvement in subjective and objective measurements of vision (dark adaptometry, pupillometry, electroretinography, nystagmus and ambulatory behavior). | |
| Hemophilia B | AAV8; 2 × 1011, 6 × 1011 or 2 × 1012 vg per kg body weight; six patients (27–64 years old) | FIX gene, regulated by the human apolipoprotein hepatic control region and human α-1-antitrypsin promoter | Intravenous delivery targeting hepatocytes | Durable circulating FIX at 2–11% normal levels; decreased frequency (two of six patients) or cessation (four of six) of spontaneous hemorrhage |
| X-linked severe combined immunodeficiency (SCID-X1) | Gammaretrovirus; ten patients (4–36 months old); CD34+ cells were infused (without conditioning) at doses of 60 × 106 to 207 × 106 cells per patient | Interleukin-2 receptor common γ-chain, retroviral LTR | Ex vivo, CD34+ hematopoietic stem and progenitor cells | Functional polyclonal T-cell response restored in all patients; one patient developed acute T-cell lymphoblastic leukemia |
| Gammaretrovirus; nine patients (1–11 months old); CD34+ cells were infused (without conditioning) at doses of 1 × 106 to 22 × 106 cells per kg | Interleukin-2 receptor common γ-chain, retroviral LTR | Ex vivo, CD34+ hematopoietic stem and progenitor cells | Functional T-cell numbers reached normal ranges. Transduced T cells were detected for up to 10.7 years after gene therapy. Four patients developed acute T cell lymphoblastic leukemia, one died. | |
| Adenosine deaminase deficiency resulting in severe combined immunodeficiency (ADA-SCID) | Gammaretrovirus; six patients (6–39 months old); CD34+ cells were infused (after non-myeloablative conditioning with melphalan (Alkeran), 140 mg per m2 body surface area, or busulfan (Myleran), 4 mg per kg) at doses of <0.5 × 106 to 5.8 × 106 cells per kg | Adenosine deaminase gene, retroviral LTR | Ex vivo, CD34+ hematopoietic stem and progenitor cells | Restoration of immune function in four of six patients; three of six taken off enzyme-replacement therapy; four of six remain free of infection |
| Gammaretrovirus; ten patients (1–5 months old); CD34+ cells were infused (after non-myeloablative conditioning with busulfan, 4 mg per kg) at doses of 3.1 × 106 to 13.6 × 106 cells per kg | Adenosine deaminase gene, retroviral LTR | Ex vivo, CD34+ hematopoietic stem and progenitor cells | Nine of ten patients had immune reconstitution with increases in T-cell counts (median count at 3 years, 1.07 × 109 l−1) and normalization of T-cell function. Eight of ten patients do not require enzyme-replacement therapy. | |
| Chronic granulomatous disorder | A range of studies, using gammaretrovirus vectors pseudotyped either with gibbon ape leukemia virus envelope or with an amphotrophic envelope; various non-myeloablative conditioning strategies | Gp91phox, retroviral LTR | Ex vivo, CD34+ hematopoietic stem and progenitor cells | Twelve of twelve patients showed short-term functional correction of neutrophils with resolution of life-threatening infections. Three patients developed myeloproliferative disease. |
| Wiskott-Aldrich syndrome | Gammaretrovirus; ten patients; CD34+ cells were infused (after non-myeloablative conditioning with busulfan, 4 mg per kg) | WAS gene, retroviral LTR | Ex vivo, CD34+ hematopoietic stem and progenitor cells | Nine of ten patients showed improvement of immunological function and platelet count. Two patients developed acute T-cell lymphoblastic leukemia. |
| β-thalassemia | Self-inactivating HIV-1–derived lentivirus; one patient (18 years old) received fully myeloablative conditioning with busulfan; 3.9 × 106 CD34+ cells per kg | Mutated adult β-globin (βA(T87Q)) with anti-sickling properties, LCR control | Ex vivo, CD34+ hematopoietic stem and progenitor cells | Patient has been transfusion independent for 21 months. Blood hemoglobin is maintained between 9 and 10 g dl−1, of which one-third contains vector-encoded β-globin. |
| Adrenoleuko-dystrophy | Self-inactivating HIV-1–derived lentivirus; two patients (7 and 7.5 years old) received myeloablative conditioning with cyclophosphamide (Cytoxan) and busulfan; transduced CD34+ cells, 4.6 × 106 and 7.2 × 106 cells per kilogram, respectively | Wild-type ABCD1 cDNA under the control of the MND viral promoter | Ex vivo, CD34+ hematopoietic stem and progenitor cells | 9–14% of granulocytes, monocytes, and T and B lymphocytes expressing the ALD protein; beginning 14–16 months after infusion of the genetically corrected cells, progressive cerebral demyelination in the two patients attenuated. |
| Duchenne muscular dystrophy | Phosphorodiamidate morpholino antisense oligodeoxynucleotides; dose escalation from 0.5 to 20.0 mg per kg; 19 patients (5–15 years old) | Oligonucleotide promotes skipping of spliceosome across diseased exon 51 of dystrophin gene | i.v., aiming to promote exon skipping in muscle cells | No serious treatment-related toxicities; muscle biopsies showed exon 51 skipping in all cohorts and dose-dependent expression of new dystrophin protein at doses of 2 mg per kg and above. Best responder had 18% normal muscle dystrophin levels. |
| Heart failure | AAV1; 6 × 1011, 3 × 1012 or 1 × 1013 DNase-resistant particles per patient | Sarcoplasmic reticulum Ca2+-ATPase (SERCA2a), CMV immediate early promoter | Antegrade epicardial coronary artery infusion over a 10-min period, targeting cardiac myocytes | High dose showed significant improvement in symptoms, functional status, biomarker (N-terminal prohormone brain natriuretic peptide) and left ventricular function, plus significant improvement in clinical outcomes. |
| B-cell leukemia and lymphoma | Self-inactivating lentivirus expressing a chimeric T cell receptor; a single patient was conditioned with pentostatin (Nipent; 4 mg per m2) and cyclophosphamide (600 mg per m2) before receiving 1.5 × 105 transduced T cells per kg (total 3 × 108 T cells, of which 5% were transduced) | Anti-CD19 scFv derived from FMC63 murine monoclonal antibody, human CD8α hinge and trans-membrane domain, and human 4-1BB and CD3ζ signaling domains | Ex vivo, autologous T cells, i.v. infusion, split over 3 d | Transduced T cells expanded more than 1,000 times in vivo, with delayed development of the tumor lysis syndrome and complete remission, ongoing 10 months after treatment. Engineered cells persisted at high levels for 6 months in the blood and bone marrow. |
| Murine stem cell virus–based splice-gag (retroviral) vector expressing CD19 CAR; eight patients (47–63 years old) with progressive B-cell malignancies received cyclophosphamide and fludarabine (Fludara) before CAR-transduced autologous T cells and interleukin 2. Patients received 0.3 × 107 to 3.0 × 107 CAR+ T cells per kg, of which an average of 55% were transduced. | Anti-CD19 scFv derived from the FMC63 mouse hybridoma, a portion of the human CD28 molecule and the intracellular component of the human TCR-ζ molecule | Ex vivo, autologous T cells, single i.v. infusion, followed (3 h) by a course of IL2 | Varied levels of anti–CD19-CAR–transduced T cells could be detected in the blood of all patients. One patient died on trial, with influenza A pneumonia, nonbacterial thrombotic endocarditis and cerebral infarction. Four patients had prominent elevations in serum levels of IFNg and TNF, correlating with severity of acute toxicities. Six of the eight patients treated obtained objective remissions. | |
| Acute leukemia | SFG retrovirus expressing an inducible suicide system for improved safety of stem cell transplantation to prevent graft-versus-host disease (GVHD); transduced haploidentical T cells (1 × 106 to 1 × 107 T cells per kg); five patients (3–17 years old) | FK506-binding protein linked to modified human caspase 9 with truncated CD19 as a selectable marker; in the presence of the drug, the iCasp9 promolecule dimerizes and activates apoptosis; retroviral LTR | Ex vivo, allodepleted haploidentical T cells, infused i.v. into recipients of allogeneic bone marrow transplants. | The genetically modified T cells were detected in peripheral blood from all five patients and increased in number over time. A single dose of dimerizing drug, given to four patients in whom GVHD developed, eliminated more than 90% of the modified T cells within 30 min after administration and ended the GVHD without recurrence. |
| Squamous-cell carcinoma of the head and neck | Oncolytic vaccine based on herpes virus combined with chemotherapy and chemoradiotherapy; patients with stage III, stage IVA or stage IVB disease; four doses of virus, 106–108 p.f.u. per dose | Clinical isolate of HSV-1 from which the proteins ICP34.5 and ICP47 have been deleted | Intratumoral injection into nodules of squamous head and neck carcinoma | 14 patients (82.3%) showed tumor response by RECIST criteria, and pathologic complete remission was confirmed in 93% of patients at neck dissection. Prolonged progression-free survival was seen in two-thirds of the patients. |
| Melanoma | Oncolytic vaccine based on herpes virus; patients with stage IIIc and IV disease; 4 × 106 p.f.u. followed 3 weeks later by up to 4 × 108 p.f.u. every 2 weeks for up to 24 treatments | Clinical isolate of HSV-1 from which the proteins ICP34.5 and ICP47 have been deleted | Intratumoral injection into melanoma nodules | The overall response rate by RECIST was 26%, with regression of both injected and distant (including visceral) lesions. 92% of the responses had been maintained for 7 to 31 months. Ten additional patients had stable disease for >3 months, and two additional patients had surgical complete response. |
| Advanced or metastatic solid tumors refractory to standard of care treatment, or for which no curative standard therapy existed | 25 adult patients received 75 mg per m2 docetaxel (Taxotere; day 1) and escalating doses of reovirus up to 3 × 1010 TCID50 (days 1–5) every 3 weeks | Reovirus type 3 Dearing, a wild-type double-stranded RNA virus | Intravenous delivery to treat advanced and/or disseminated cancer | Of 16 evaluable patients, dose-limiting toxicity of grade 4 neutropenia was seen in one patient but the maximum tolerated dose was not reached. Antitumor activity was seen with one complete response and three partial responses. A disease-control rate (combined complete response, partial response and stable disease) of 88% was observed. |
_________
________
How Embryonic Stem Cells might play a role in Gene Therapy Research:
Persistence of the cell containing the therapeutic transgene is equally important for ensuring continued availability of the therapeutic agent. The optimal cells for cell-mediated gene transfer would be cells that will persist for “the rest of the patient’s life; they can proliferate and they would make the missing protein constantly and forever”. Persistence, or longevity, of the cells can come about in two ways: a long life span for an individual cell, or a self-renewal process whereby a short-lived cell undergoes successive cell divisions while maintaining the therapeutic transgene. Ideally, then, the genetically modified cell for use in cell-based gene therapy should be able to self-renew (in a controlled manner so tumors are not formed) so that the therapeutic agent is available on a long-term basis. This is one of the reasons why stem cells are used, but adult stem cells seem to be much more limited in the number of times they can divide compared with embryonic stem cells. The difference between the ability of adult and embryonic stem cells to self-renew has been documented in the mouse, where embryonic stems cells were shown to have a much higher proliferative capacity than do adult hematopoietic stem cells. Researchers are beginning to understand the biological basis of the difference in proliferative capacity between adult and embryonic stem cells. Persistence of cells and the ability to undergo successive cell divisions are in part, at least, a function of the length of structures at the tips of chromosomes called telomeres. Telomere length is, in turn, maintained by an enzyme known as telomerase. Low levels of telomerase activity result in short telomeres and, thus, fewer rounds of cell division—in other words, shorter longevity. Higher levels of telomerase activity result in longer telomeres, more possible cell divisions, and overall longer persistence. Mouse embryonic stem cells have been found to have longer telomeres and higher levels of telomerase activity compared with adult stem cells and other more specialized cells in the body. As mouse embryonic stem cells give rise to hematopoietic stem cells, telomerase activity levels drop, suggesting a decrease in the self-renewing potential of the hematopoietic stem cells. Human embryonic stem cells have also been shown to maintain pluripotency (the ability to give rise to other, more specialized cell types) and the ability to proliferate for long periods in cell culture in the laboratory. Adult stem cells appear capable of only a limited number of cell divisions, which would prevent long-term expression of the therapeutic gene needed to correct chronic diseases. “Embryonic stem cells can be maintained in culture, whereas that is nearly impossible with cord blood stem cells,” says Robert Hawley of the American Red Cross Jerome H. Holland Laboratory for Biomedical Sciences, who is developing gene therapy vectors for insertion into human hematopoietic cells. “So with embryonic stem cells, you have the possibility of long-term maintenance and expansion of cell lines, which has not been possible with hematopoietic stem cells.” The patient’s immune system response can be another significant challenge in gene therapy. Most cells have specific proteins on their surface that allow the immune system to recognize them as either “self” or “nonself.” These proteins are known as major histocompatibility proteins, or MHC proteins. If adult stem cells for use in gene therapy cannot be isolated from the patient, donor cells can be used. But because of the differences in MHC proteins among individuals, the donor stem cells may be recognized as nonself by the patient’s immune system and be rejected. John Gearhart of Johns Hopkins University and Peter Rathjen at the University of Adelaide speculate that embryonic stem cells may be useful for avoiding such immune reactions. For instance, it may be possible to establish an extensive “bank” of embryonic stem cell lines, each with a different set of MHC genes. Then, an embryonic stem cell that is immunologically compatible for a patient could be selected, genetically modified, and triggered to develop into the appropriate type of adult stem cell that could be administered to the patient. By genetically modifying the MHC genes of an embryonic stem cell, it may also be possible to create a “universal” cell that would be compatible with all patients. Another approach might be to “customize” embryonic stem cells such that cells derived from them have a patient’s specific MHC proteins on their surface and then to genetically modify them for use in gene therapy. Such approaches are hypothetical at this point, however, and research is needed to assess their feasibility. Ironically, the very qualities that make embryonic stem cells potential candidates for gene therapy (i.e., pluripotency and unlimited proliferative capacity) also raise safety concerns. In particular, undifferentiated embryonic stem cells can give rise to teratomas, tumors composed of a number of different tissue types. It may thus be preferable to use a differentiated derivative of genetically modified embryonic stem cells that can still give rise to a limited number of cell types (akin to an adult stem cell). Cautions Esmail Zanjani of the University of Nevada, “We could differentiate embryonic stem cells into, say, liver cells, and then use them, but I don’t see how we can take embryonic stem cells per se and put genes into them to use therapeutically”. Further research is needed to determine whether the differentiated stem cells retain the advantages, such as longer life span, of the embryonic stem cells from which they were derived. Because of the difficulty in isolating and purifying many of the types of adult stem cells, embryonic stem cells may still be better targets for gene transfer. The versatile embryonic stem cell could be genetically modified, and then, in theory, it could be induced to give rise to all varieties of adult stem cells. Also, since the genetically modified stem cells can be easily expanded, large, pure populations of the differentiated cells could be produced and saved. Even if the differentiated cells were not as long-lived as the embryonic stem cells, there would still be sufficient genetically modified cells to give to the patient whenever the need arises again.
_
New Smoking Vaccine using Gene Therapy being developed:
By using gene therapy to create a novel antibody that gobbles up nicotine before it reaches the brain in mice, scientists say they may have found a potential smoking vaccine against cigarette addiction. However, there is still a long way to go before the new therapy can be tested in humans. In a study reported in the journal Science Translational Medicine, Researchers at Weill Cornell Medical College in New York City show how a single dose of the vaccine protected mice, over their lifetime, against nicotine addiction. The addictive properties of the nicotine in tobacco smoke is a huge barrier to success with current smoking cessation approaches, say the authors in their paper. Previous work using gene therapy vaccination in mice to treat certain eye disorders and tumors, gave them the idea a similar approach might work against nicotine. The new anti-nicotine vaccine is based on an adeno-associated virus (AAV) engineered to be harmless. The virus carries two pieces of genetic information: one that causes anti-nicotine monoclonal antibodies to be created, and the other that targets its insertion into the nucleus of specific cells in the liver, the hepatocytes. The result is the animal’s liver becomes a factory continuously producing antibodies that gobble up the nicotine as soon as it enters the bloodstream, denying it the opportunity to enter the brain. Other groups have developed nicotine vaccines, but they failed in clinical trials because they deliver nicotine antibodies directly. These only last a few weeks and the injections, which are expensive, have to be given again and again, said Crystal. The other disadvantage of these previous approaches, which use a passive vaccine, is that the results are not consistent, and different people may need different doses, especially if they start smoking again, he added. Crystal said although so far they have only tested their new vaccine in mice, they are hopeful it will help the millions of smokers who have tried to stop, but find their addiction to nicotine is so strong; none of the cessation methods currently available can overcome it. Research shows that 70 to 80% of quitters start smoking again within 6 months, said Crystal. The team is getting ready to test the new vaccine in rats and primates. If those trials are successful, then they can start working towards human trials. If the vaccine successfully completes this long journey, Crystal thinks it will work best for smokers who are really keen to quit. “They will know if they start smoking again, they will receive no pleasure from it due to the nicotine vaccine, and that can help them kick the habit,” he said. He said they would also be interested in seeing if the vaccine could be used to prevent nicotine addiction in the first place, but that is only a theory at this point, he noted.
_
Future prospects:
Many gene therapy protocols in clinical or preclinical trials are showing great promise. Two notable examples include the treatment of haemophilia B and lipoprotein lipase deficiency in adults. In both of these trials, however, only a transient clinical benefit was observed as a result of the immune responses directed against vector constituents, with resultant cell-mediated destruction of the gene-corrected cells in the liver and muscle, respectively. To prevent these unwanted immune responses, some protocols may require modulation of the immune system or transient immune suppression. At present, a total of six patients have been treated at three different vector doses. Vector was delivered in the absence of immunosuppressive therapy and, at the time of publication, patients were monitored for between 6 and 16 months. AAV-mediated expression of FIX resulted in between 2% and 11% of normal levels in all patients. Furthermore, four of the six patients were able to discontinue FIX prophylaxis and remained free of spontaneous haemorrhage. For the other two patients, the time between prophylactic injections was increased. For the two patients receiving the high dose of vector, one had a transient elevation of serum aminotransferase levels with an associated detection of AAV8-specific T cells, and the other had a slight increase in liver-enzyme levels. Both patients were treated with a short course of glucocorticoid therapy that rapidly returned aminotransferase levels to normal, without the loss of transgene expression. Although long-term follow-up is required in more patients, despite the risk of transient hepatic dysfunction, this approach has demonstrated the potential to convert the severe form of this disease into a milder form or to reverse it completely. Another strategy being considered is the use of regulated expression cassettes containing microRNA (miRNA) sequences. Inclusion of miRNA sequences targeting haematopoietic lineages to eliminate or reduce off-target gene expression in professional antigen presenting cells has allowed the stable correction of a haemophilia B mouse model and also been shown to induce antigen-specific immunologic tolerance. The landmark discovery by Takahashi and Yamanaka that somatic cells can be reprogrammed to a state of pluripotency through the ectopic expression of as little as four transcription factors has the potential to be a powerful tool for both gene and cellular therapies and to revolutionise the field of regenerative medicine by developing patient-specific treatments. These cells, termed induced pluripotent stem cells (iPS), closely resemble embryonic stem (ES) cells in their morphology and growth properties, and have also been shown to express ES cell markers. Research in this field is still in its infancy and a number of important issues need to be resolved before these cells appear in the clinical setting. These include improvements in reprogramming efficiency, a more complete understanding of the development potential and quality of the iPS cells produced and the establishment of their safety profile in vivo, particularly with respect to tumour formation. Originally produced by retroviral-mediated delivery, refinements to the system using non-integrating vectors and transient expression systems will also address safety concerns by eliminating unwanted long-term expression of the encoded transcription factors and the possibility of insertional mutagenesis. Proof-of-principle for combining somatic cell reprogramming with gene therapy for disease treatment already exists. For example, dopaminergic neurones derived from iPS cells have been shown to possess mature neuronal activity and, importantly, to improve behaviour in a rat model of Parkinson’s disease. In another study, utilising a humanised mouse model of sickle cell anaemia, mice were rescued following transplantation with haematopoietic progenitors that were corrected by gene-specific targeting. Gene-corrected iPS cells derived from Fanconi anaemia patients have also been differentiated into haematopoietic progenitors of the myeloid and erythroid lineages and may be useful for overcoming the poor quality of HSCs found in the bone marrow of these patients, which is impeding success in the clinic. A human artificial chromosome, carrying a complete genomic dystrophin gene, has also been used to correct iPS cells derived from a murine model of Duchenne muscular dystrophy and from patient fibroblasts. These cells were able to form all three germ layers and human dystrophin expression could be detected in muscle-like tissues. This approach overcomes one of the main obstacles hampering gene therapy for Duchenne muscular dystrophy, namely the unusually large size of the dystrophin gene that is beyond the packaging capacity of current viral vector systems. Another strategy showing promise for the treatment of Duchenne muscular dystrophy uses synthetic oligonucleotide-induced exon skipping to restore the reading frame of the protein. This approach is currently being trialed; however, it requires the use of patient mutation-specific oligonucleotides and repeated administration. Although many issues need to be resolved before we see the therapeutic use of iPS cells, they have immediate potential for basic research, disease modeling and drug screening, and hold immense promise for the future.
_
Artificial virus: Artificial virus improves gene delivery in gene therapy:
For the use DNA in gene therapy, the molecule must be delivered to diseased cells in its entirety to be effective. However, DNA is inherently incapable of penetrating cells and is quickly degraded. Therefore natural viruses that have been rendered harmless are used as so-called vectors. These can enter cells efficiently and deliver the therapeutic DNA or RNA molecules. However, the process of rendering natural viruses harmless still requires improvement. Unintended side effects have been a problem. Therefore, research is also being conducted into alternative ‘virus-like’ vectors based on synthetic molecules. Unfortunately, these have been less effective because it is difficult to precisely imitate the many tricks used by viruses. A first important step in mimicking viruses is the precise packaging of individual DNA molecules with a protective coat of smaller molecules. Until now, packaging individual DNA molecules with a protective coating of synthetic molecules has not yet been achieved. Instead of using synthetic chemistry to coat individual DNA molecules, the researchers decided to design and produce artificial viral coat proteins. As part of their study, they used recent theoretical insights into the crucial aspects of the process of packaging genetic material by natural viral coat proteins. The researchers ‘translated’ each of these crucial aspects into various protein blocks with simple structures. The amino acid sequence of the protein blocks was inspired by natural proteins such as silk and collagen. Artificial viral coat proteins designed in this way were produced using the natural machinery of yeast cells. When the proteins were mixed with DNA, they spontaneously formed a highly protective protein coat around each DNA molecule, thus creating ‘artificial viruses’. The formation process of the artificial viruses is similar in many ways to that of natural viruses, such as the tobacco mosaic virus, which served as a model for the artificial virus. This first generation of artificial viruses was found to be as effective as the current methods for delivering DNA to host cells based on synthetic molecules. But the great precision by which DNA molecules are packaged in the artificial virus offers many possibilities to now also build in other virus tricks. In the future, these techniques can hopefully lead to safe and effective methods for delivering new generations of pharmaceuticals, especially in gene therapy. Moreover, these artificial viruses can also be developed for the many other applications in which viruses are now being used in fields such as biotechnology and nanotechnology.
____________
Is gene therapy available to treat my disorder?
Gene therapy is currently available only in a research setting. The U.S. Food and Drug Administration (FDA) has not yet approved any gene therapy products for sale in the United States. Hundreds of research studies (clinical trials) are under way to test gene therapy as a treatment for genetic conditions, cancer, and HIV/AIDS. If you are interested in participating in a clinical trial, talk with your doctor or a genetics professional about how to participate. You can also search for clinical trials online. ClinicalTrials.gov (http://clinicaltrials.gov/), a service of the National Institutes of Health, provides easy access to information on clinical trials. You can search for specific trials or browse by condition or trial sponsor. You may wish to refer to a list of gene therapy trials (http://clinicaltrials.gov/search?term=%22gene+therapy%22) that are accepting (or will accept) participants.
_
You must know list of diseases for which clinical trials of gene therapy is going on or will start in near future, so that you can enroll yourself if you are suffering from any one of these diseases.
_
_______
Which types of patients should a clinical trial enroll?
Should the sickest patients try a new treatment because they are the most desperate, or should the healthiest, because they have a better chance of surviving the experiment? Part of the outcry over the death of Gelsinger that effectively halted the field for two years was the fact that he had not been desperately ill. The symptoms and natural history of CF dictate the optimal age of trial participants. In CF researchers face a dilemma. Very young children have less mucus, but it is harder to measure their increase in lung function. In the full-blown disease patients have lots of thick sputum. It is hard to find the right patients. You need a balance. They decided on 12 as the minimum age, with average age 22.
_
How much of a gene’s function must gene therapy restore?
In gene therapy, a small change can go a long way. That’s the case for a gene transfer approach for the clotting disorder haemophilia B. Introducing the gene for clotting factor IX that restores the level to less than 8% of normal activity can free a man from needing to take clotting factor to prevent life-threatening bleeds. For cystic fibrosis, men whose only symptom is infertility have 10% residual function of the chloride channels. A 6% increase in lung function might be all that’s necessary.
_
How should researchers pick the best vector and its cargo?
Choosing a vector and making it safe is perhaps the toughest challenge in gene therapy. Investigators must design the delivery method before a phase 1 trial gets underway, and stick to it. Researchers can’t change or tweak a virus, alter the recipe for a liposome, or replace the DNA cargo without going back to square 1, phase 1. It’s one reason why the gamma retroviral vectors that caused leukemia and the adenoviruses that evoked a devastating immune response are still in use, although some have been made “self-inactivating.” The CF trial used a liposome delivery method but the researchers modified the DNA within to decrease the stretches of cytosine and guanine (“CpG islands”) that invite inflammation and they added a bit to extend the effect. That meant starting from scratch in the phase 1 trial, even though the liposome recipe had been used before.
_
If stem cell therapy (SCT) is so effective, why do we need gene therapy?
Because in all inherited genetic disorders, stem cells would carry the same defective gene. So autologous SCT is useless in inherited genetic disorders and we have to use allogenic SCT. Using donor cells is preferred for SCT in acquired disorder like leukemia because leukemia is a disease of the blood and bone marrow, so giving the patient his or her own cells back may mean giving leukemia cells. It is hard to separate normal stem cells from leukemia cells in the bone marrow or blood samples during autologous SCT. Now if donor stem cells are used from another individual, due to differences in MHC proteins among individuals, the donor stem cells may be recognized as non-self by the patient’s immune system and be rejected. Also, embryonic stem cells can’t be used because of technical difficulties in using them or religious objections to sacrificing embryos. All these reasons justify need of gene therapy over SCT. Of course, gene therapy can be combined with SCT for best outcome.
________
The ideal gene therapy:
________
________
The moral of the story:
_
1. A genetic disorder is a disease caused in whole or in part by a change in the DNA sequence away from the normal sequence. About one in ten people has or will develop genetic disorder due to some defective gene. Genetic testing is analyzing person’s DNA to identify genes that cause genetic disorders. Genetic disorders can be inherited or acquired.
_
2. Gene therapy can broadly be considered any treatment that changes gene function to alleviate a disease state. Gene therapy means man-made transfer/alteration/ expression/suppression of DNA/RNA in human/animal cells for the purpose of prophylaxis and/or treatment of a disease state. Replacing a defective gene by normal gene is one of the types of gene therapy. Other types include gene editing, gene silencing, insertion of novel genes, gene reprogramming, DNA vaccine etc.
_
3. Two approaches to gene therapy exist: correcting genes involved in causing illness (genetic disorders); and using genes to treat disorders (cancer, HIV, heart disease). Even though most of the public debate has been about the former, many applications have focused on the latter. These applications involve using ‘designer’ DNA to tackle diseases that are not inherited – by using altered viruses designed specifically to attack, say cancer cells. Here, the DNA is working more or less like a drug. Gene therapy field has moved increasingly from a “gene correction” model to a “DNA as drug” model. The newer definition of gene therapy is the use of DNA as a drug to treat disease by delivering therapeutic DNA into a patient’s cells.
_
4. Presently gene therapy is offered for diseases where no curative treatment is available and the disease causes significant morbidity and mortality.
_
5. Gene therapy is one of the methods of genetic engineering and in the puritan medical terminology; any individual who has received gene therapy necessarily becomes genetically modified organism (GMO).
_
6. Even though there is overlap between gene therapy and genetic enhancement, gene therapy can be considered as any process aimed at preserving or restoring “normal” functions, while anything that improves a function beyond “normal” would be considered a genetic enhancement. Essentially gene therapy is offered to sick person while genetic enhancement is offered to healthy person.
_
7. Gene therapy is neither playing God nor creating designer babies nor tampering with evolution.
_
8. Gene therapy is introduction or alteration of genetic material within the cell of a patient while cell therapy is infusion or transplantation of whole cells into a patient; both for the treatment of an inherited or acquired disease; and both can be combined. Human embryonic stem cells are excellent candidates for gene therapy due to pluripotency (the ability to give rise to other, more specialized cell types) and the ability to proliferate for long periods in cell culture in the laboratory. The commonest type of human stem cell used in gene therapy trials so far is the hematopoietic stem cell (HSC). Somatic cells can be reprogrammed to a state of pluripotency through ectopic expression of transcription factors and these cells are termed induced pluripotent stem cells (iPSC). For example, skin cells of a patient can be reprogrammed into iPSC whose genetic defect is corrected by gene therapy which can be transformed into liver cell containing transgene to correct alpha-1 antitrypsin deficiency.
_
9. Target cells are those cells in human body that receive gene transfer/alteration to achieve desired therapeutic effects; and in healthy individuals, these target cells would be producing desired protein naturally. Surrogate cells are cells that have been genetically manipulated to act like target cells; and in healthy individuals, these surrogate cells would not be producing desired protein naturally. One example is sufficient to differentiate target cells from surrogate cells. In mammals, insulin is synthesized in the pancreas within the β-cells of the islets of Langerhans. These β-cells are target cells for gene therapy of diabetes mellitus by producing a local beta cell protection factor to avoid of autoimmune destruction. Embryonic stem cells (ESC) and induced pluripotent stem cells (iPSCs) can generate insulin-producing surrogate β-cells. When liver cells or muscle cells are used to produce insulin by gene therapy, they also function as surrogate cells. Besides target cells and surrogate cells, gene therapy also inserts genes into immune cells and these genetically modified immune cells target specific molecules, for example, kill cancer cells carrying specific antigen.
_
10. Vectors are vehicles that facilitate transfer of genetic information into recipient cells; which could be somatic cells or germ-line cells; which could be stem cells, primary cells or cancer cells; and which could be surrogate cells, target cells or immune cells.
_
11. DNA is inherently incapable of penetrating cells and gets quickly degraded. Therefore natural viruses that have been rendered harmless (deactivated) are used as viral vectors to transfer DNA (gene) into recipient cell genome for gene therapy. The non-viral gene delivery methods use synthetic or natural compounds or physical forces to deliver DNA but they are less effective as it is difficult to precisely imitate many tricks used by viruses.
_
12. Gene therapy research findings & observations on animal experiments cannot be reliably transferred to humans. Human clinical trials are the best way to judge efficacy and safety of gene therapy. As gene therapy techniques are relatively new, some of the risks may be unpredictable.
_
13. The main reason why in vivo gene therapies have failed is human immune system, which rejects the therapeutic vector or the genetically corrected cells, or causes acute toxic/inflammatory reaction that has been occasionally fatal. For ex vivo gene therapy, the trouble has come from insertional mutagenesis resulting in development of cancer.
_
14. There is evidence to show that virus vectors targeted at somatic cells could end up in germ-line cells and Weismann’s barrier is permeable.
_
15. The main limitations of gene therapy are low efficiency of gene transfer & expression and low longevity of gene expression. Disorders that arise from mutations in a single gene are the best candidates for gene therapy. Multifactorial disorders such as diabetes, heart disease, cancer, arthritis etc are difficult to treat effectively using gene therapy.
_
16. The only approved gene therapy in the world today is Alipogene tiparvovec (marketed under the trade name Glybera); a gene therapy that compensates for lipoprotein lipase deficiency (LPLD) which utilizes the adeno-associated virus serotype 1 (AAV1) as a viral vector to delivers an intact copy of the human lipoprotein lipase (LPL) gene in the muscles by multiple intramuscular injections of the product. Alipogene tiparvovec is expected to cost around $1.6 million for treatment which will make it the most expensive medicine in the world. Conventional treatment is restriction of total dietary fat to 20 grams/day or less throughout life along with fat-soluble vitamins A, D, E, and K and mineral supplements.
_
17. Besides Glybera, all other gene therapies are experimental therapy to be administered only in clinical trials and the only way for you to receive gene therapy is to participate in a clinical trial.
_
18. To date, over 1800 gene therapy clinical trials have been completed, are ongoing or have been approved worldwide with majority of trials being carried out in North America and Europe; and cancer is the most common disease for gene therapy trials.
_
19. The clinical trials of gene therapy for severe combined immunodeficiency, sickle cell disease, thalassemia, hemophilia, leukodystrophies, leukemia, HIV, diabetes, heart failure, retinal diseases, Parkinson’s disease and baldness are showing promising results.
_
20. Gene therapy approaches could be contrasting depending on the target disease; for example, therapeutic angiogenesis for coronary artery disease and therapeutic anti-angiogenesis for cancer.
_
21. Ideal gene therapy should be effective, specific, safe and affordable. But are other therapies effective, specific, safe and affordable? Millions have used penicillin for decades but few have died of penicillin anaphylaxis. Then why so much hue and cry raised for occasional death during gene therapy trial? After all, science is trying to cure incurable diseases.
_
22. Genetic characteristics of an individual affect response of drugs to disease because genes affect pharmacokinetics of drugs and drugs interact with cell receptors which are under genetic control. Genetic profile of an individual is responsible for hypersensitivity reactions as well as poor efficacy of drugs. If these genes can be altered by gene therapy, the response to drugs can dramatically change. Gene therapy can make conventional drug therapy more efficacious and safer. For example, gene therapy improves tolerance and effectiveness of chemotherapy for cancer. Another example, gene therapy converts anti-fungal agent flucytosine into anti-cancer drug 5-fluorouracil (5-FU) to kill cancer cells.
_
23. Gene therapy will help get rid of tobacco addiction by producing anti-nicotine antibodies that gobbles up nicotine from tobacco chewing or tobacco smoke before it reaches the brain.
_
24. Gene doping in sports is a reality and it will be very difficult to detect it as compared to drug doping.
_
25. To what extent do physicians & researchers help people by giving them what they ask for, when what they ask for is unrelated to disease state, is the basis of medical ethics of gene therapy versus genetic enhancement.
_
26. The human genome contains fully 8% endogenous retroviral sequences, emphasizing the contribution of retroviruses to our genetic heritage. It is postulated that they originate from retroviral infection of germ-line cells (egg or sperm), followed by a stable integration in the genome of the species. It is postulated that different species appear to swap genes through the activities of retroviruses. It is also postulated that even though many sequences of endogenous retroviruses are non-functional, some of them could be carrying out important functions right from immunity against novel microorganisms to evolutionary development of placenta. What is remarkable and unique, is the fact that endogenous retroviruses are two things at once: genes and viruses. And these viruses helped make us who we are today just as surely as other genes did. Some researchers believe that these endogenous viral sequences were not inserted by retroviruses as they have function, should have been ridden by apoptosis, are different than their ancestral genomes, and it is incredible that the organisms did not die after being infected with so many viral genes. In my view, these viral sequences in our genome suggest that the highest organism on earth namely human has 8 % DNA sequences of lowest organism on earth namely virus, which proves the fact that life on earth indeed evolved from viruses all the way through billions of years; and God did not create life. To stretch the idea further, I may hypothesize that entire human genome is nothing but conglomeration of ancient viral DNAs which underwent mutations, and remaining 92 % of human DNA consists of viral DNA sequences that have become extinct millions of years ago. The corollary is that we must be extremely cautious throughout insertion of viral vectors in human genome during gene therapy as virus is entering its ancient home inhabited by other viruses and so called deactivated virus may become pathogenic by taking support of ancient viral sequences.
____________
____________
Dr. Rajiv Desai. MD.
August 31, 2014
____________
Postscript:
Gene therapy is easy to describe on paper but much harder to implement in human cells. The determined scientists and researchers have continued to work at the puzzle over decades until finally gene therapy stands poised to revolutionize modern medicine.
_


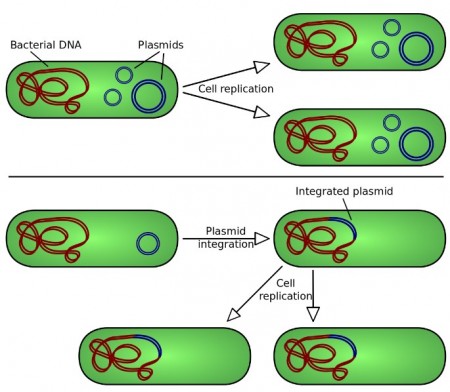
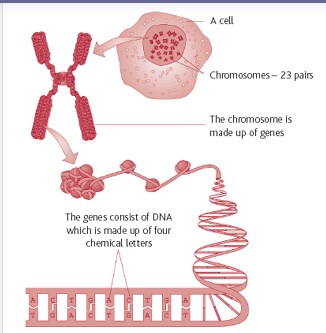
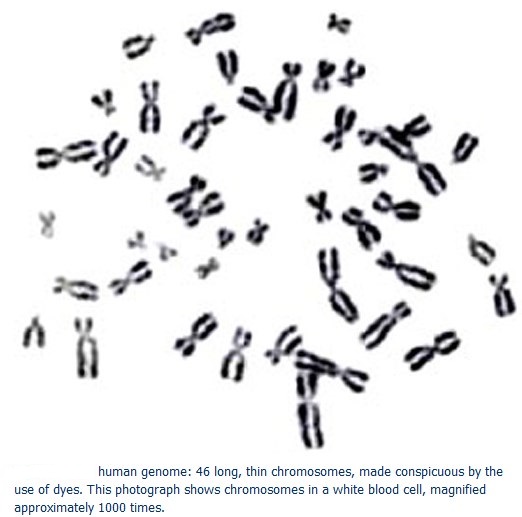
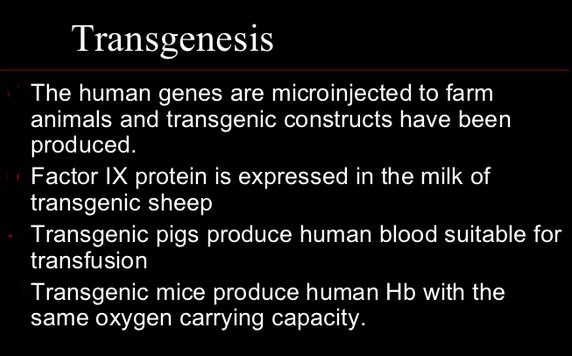
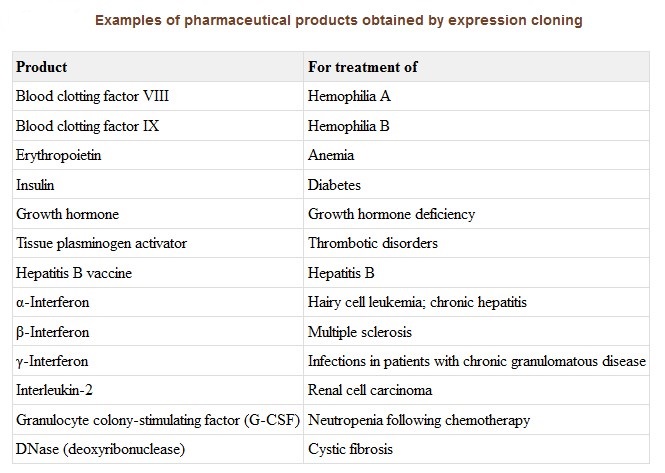
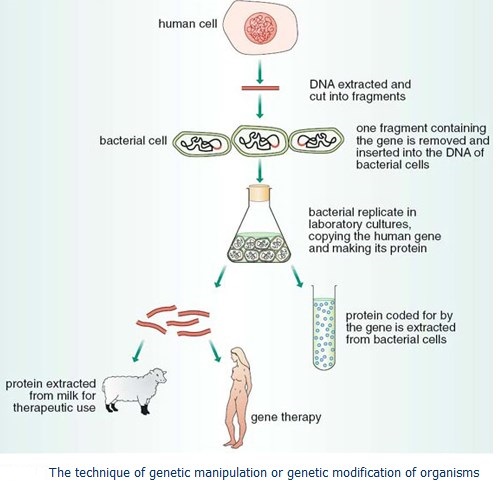
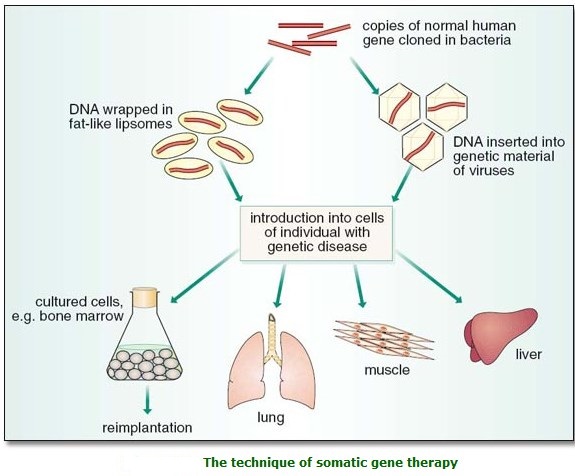
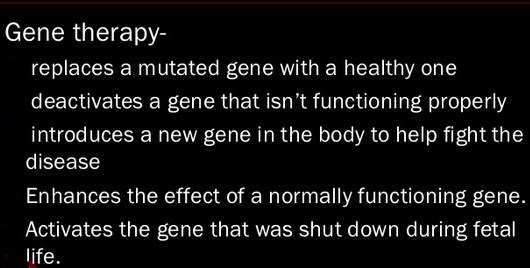
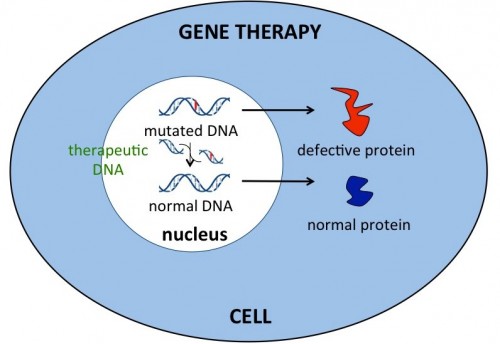
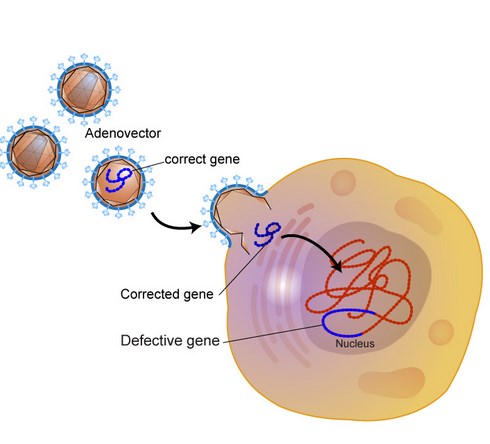
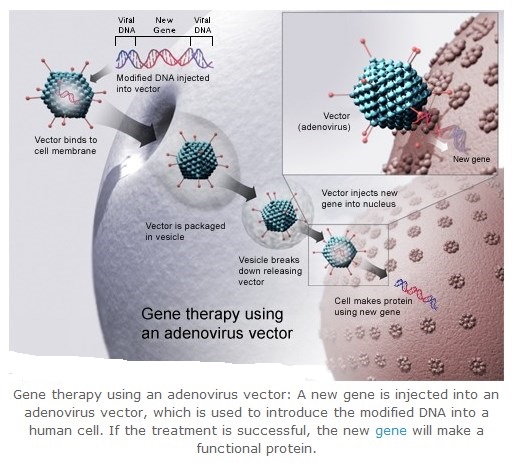
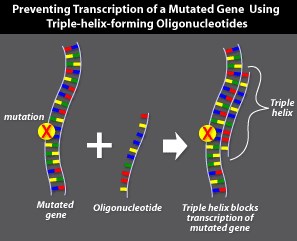
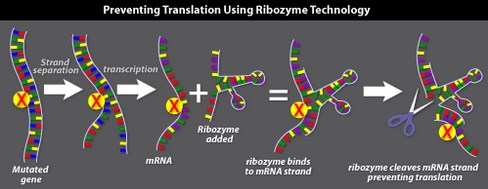
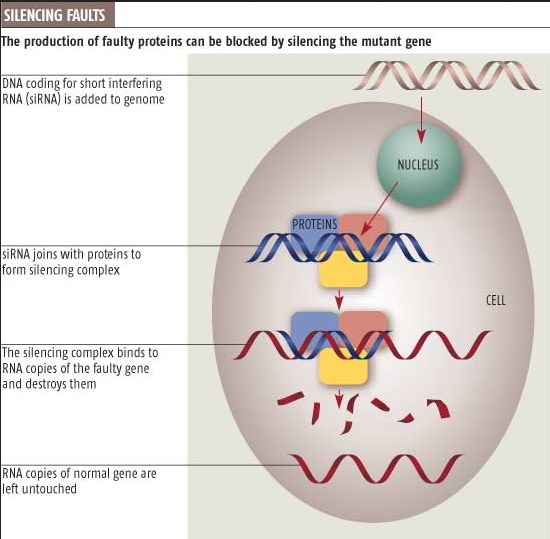
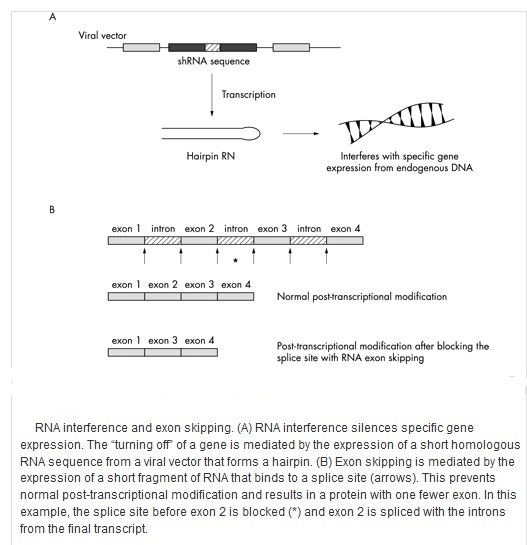
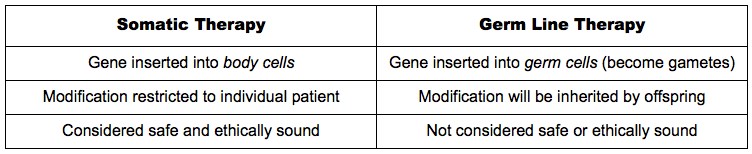
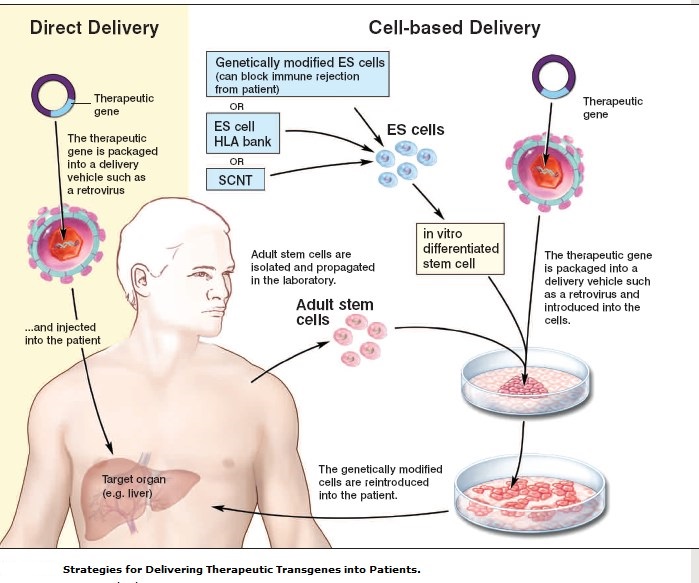
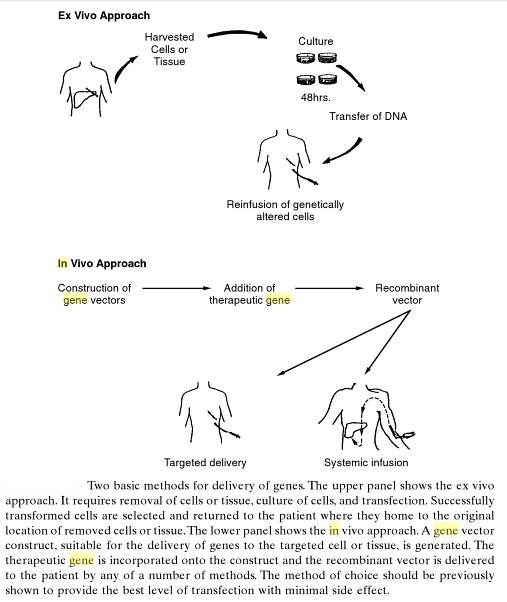
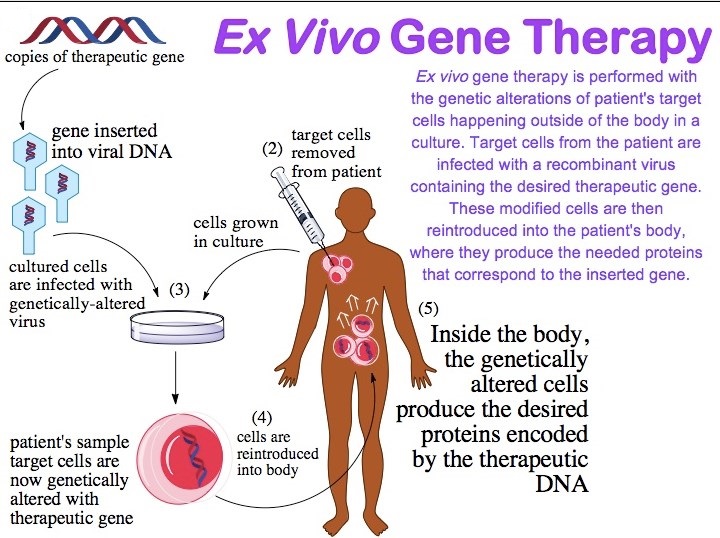
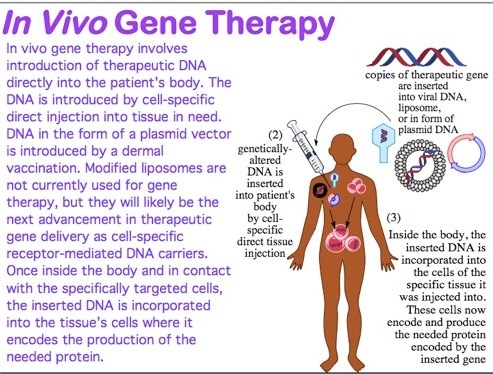
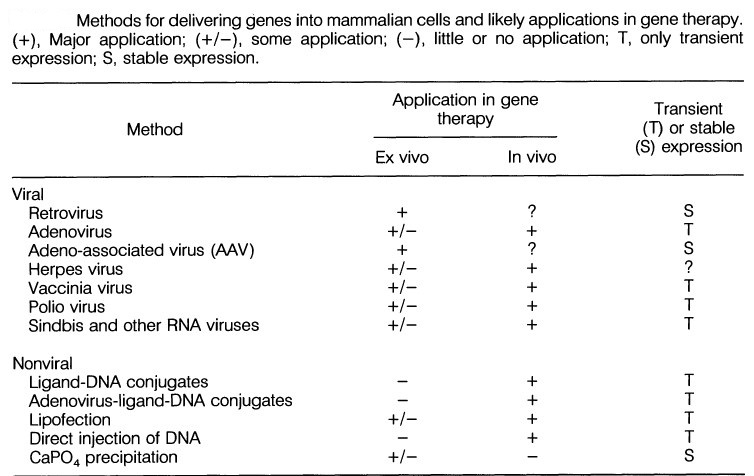
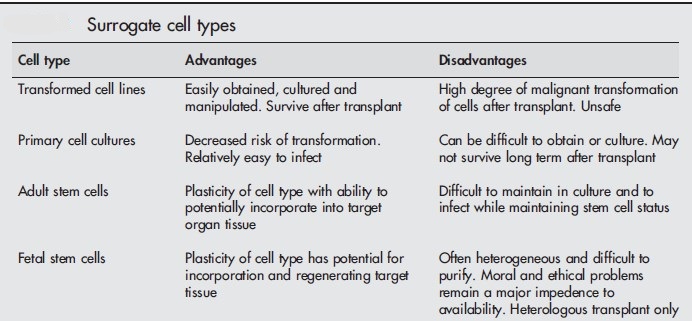
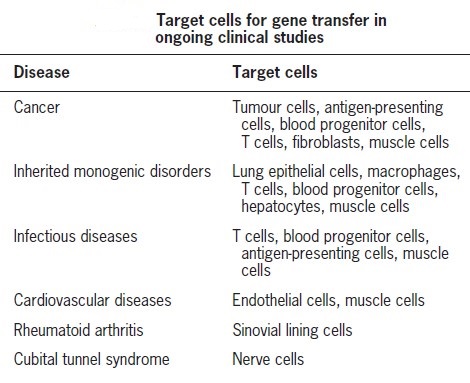

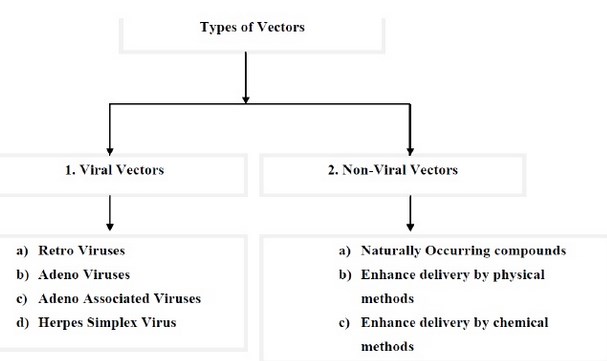
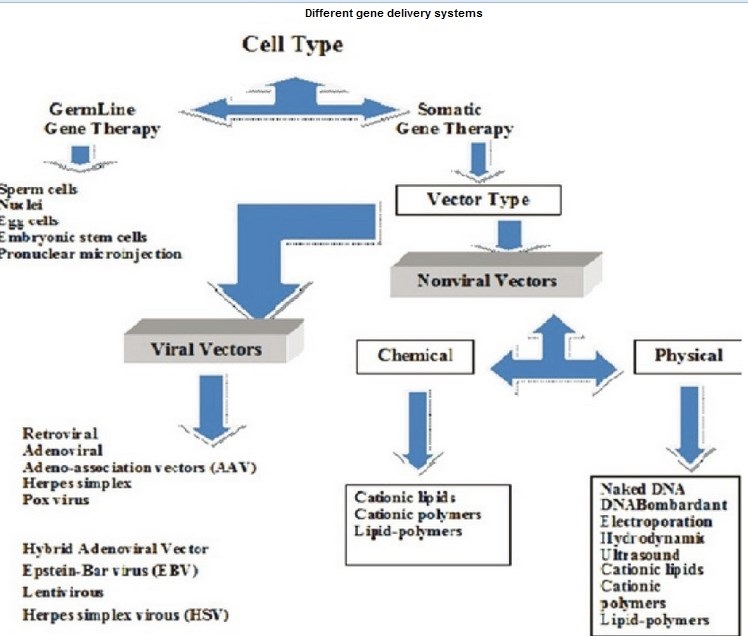
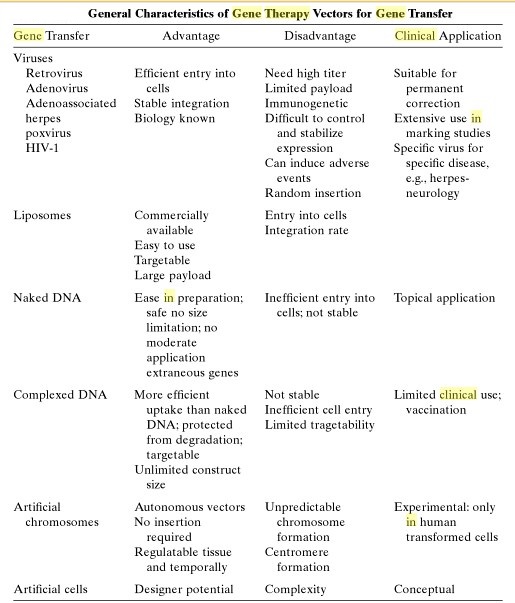
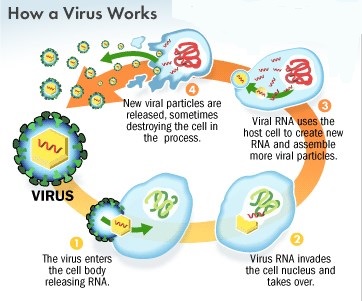
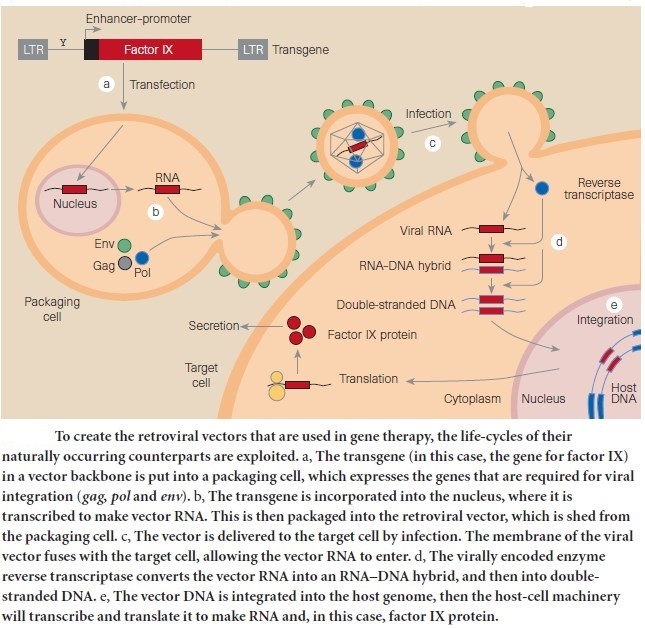
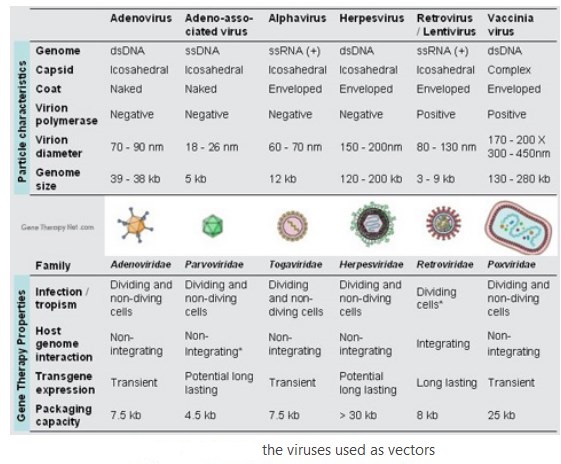
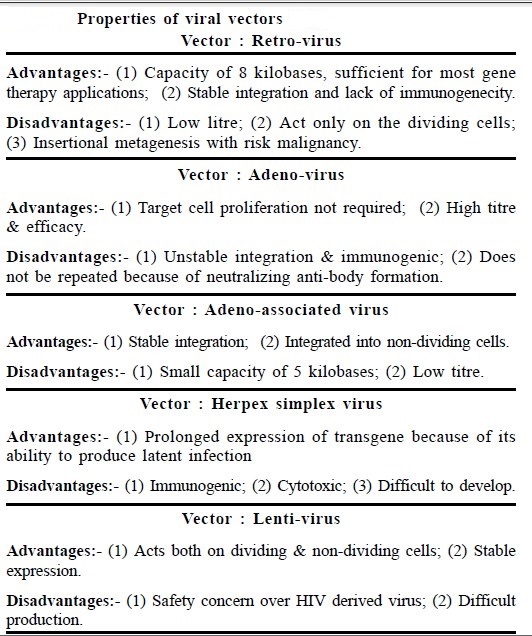
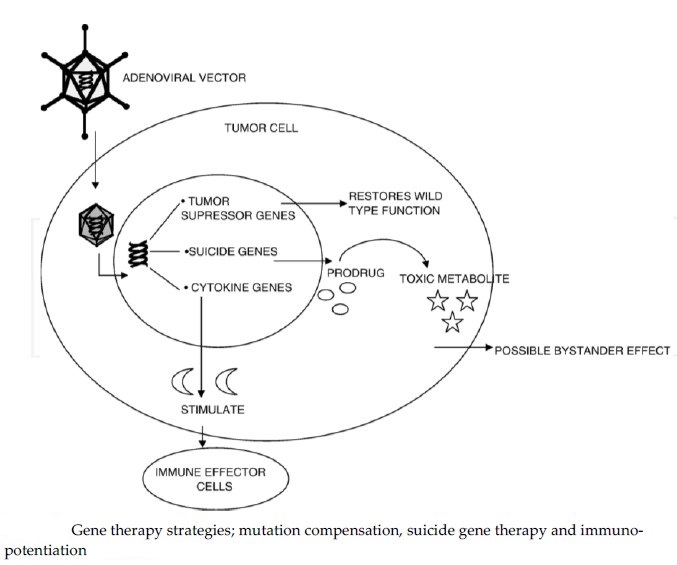
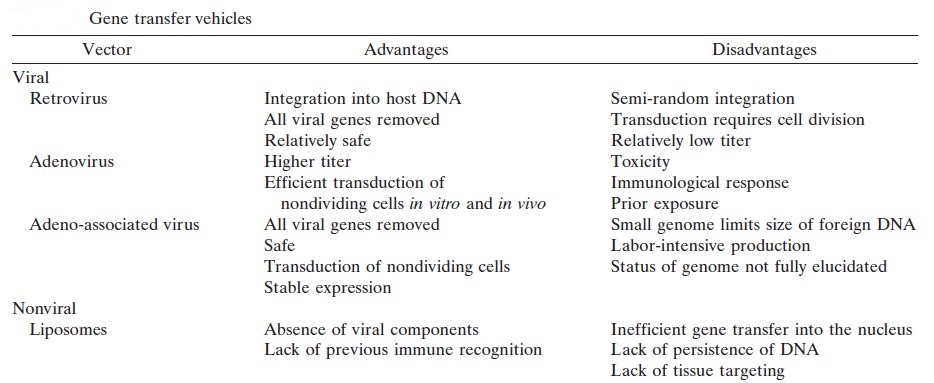
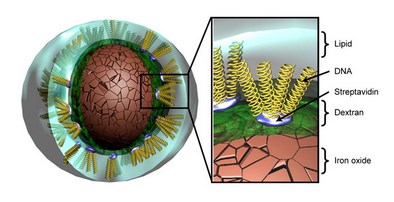
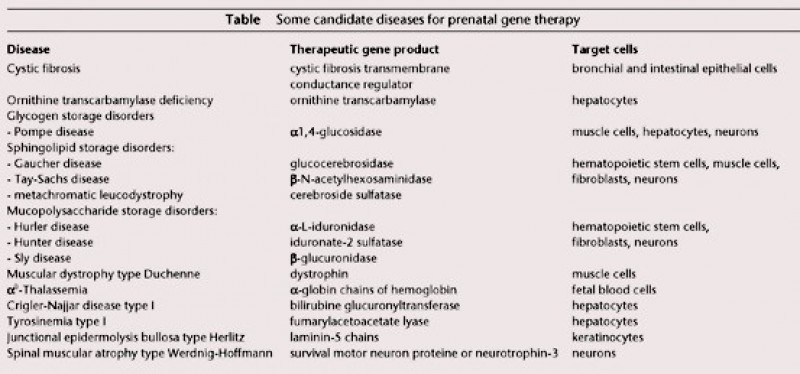
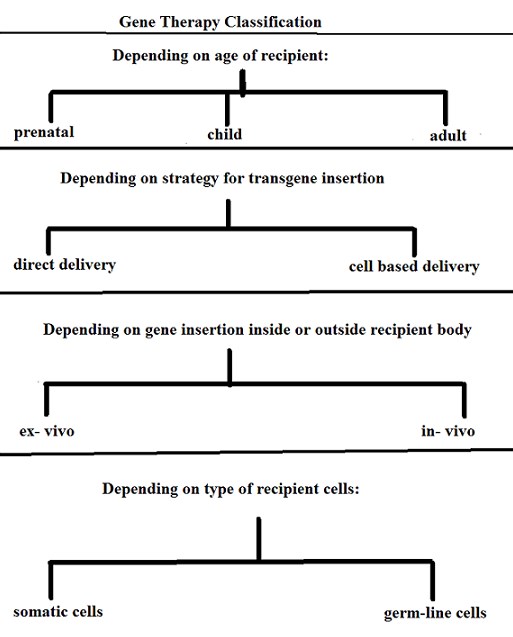
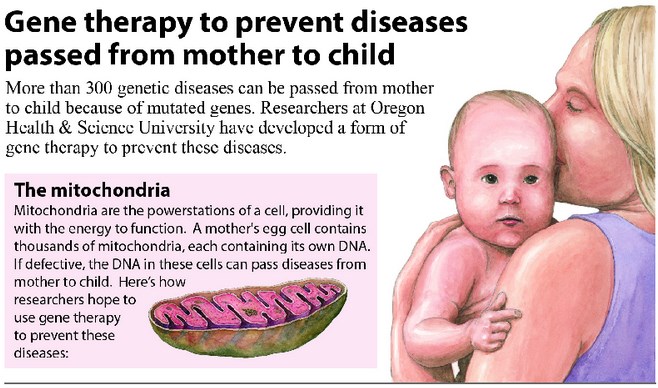
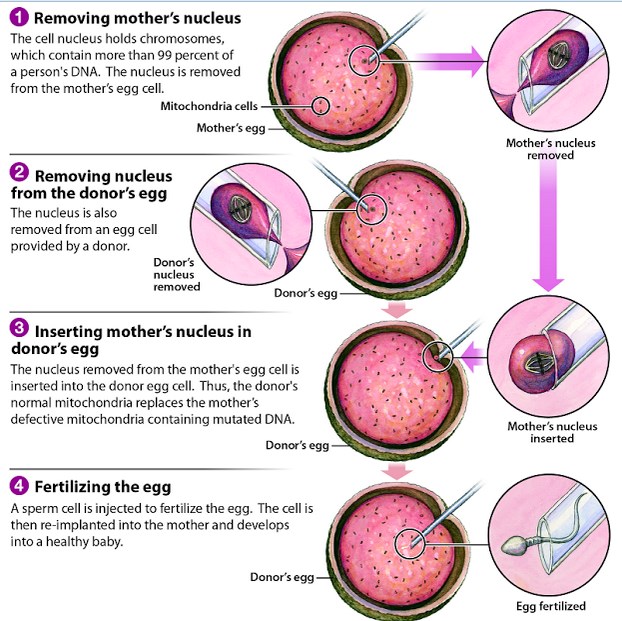
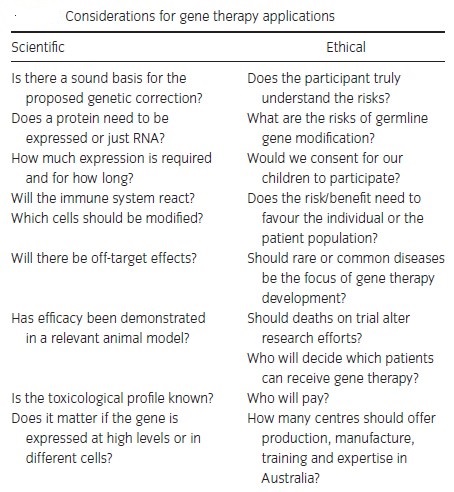
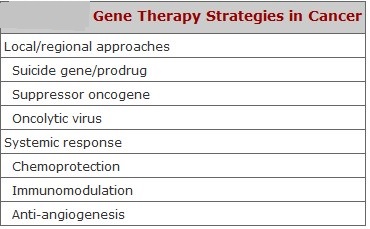
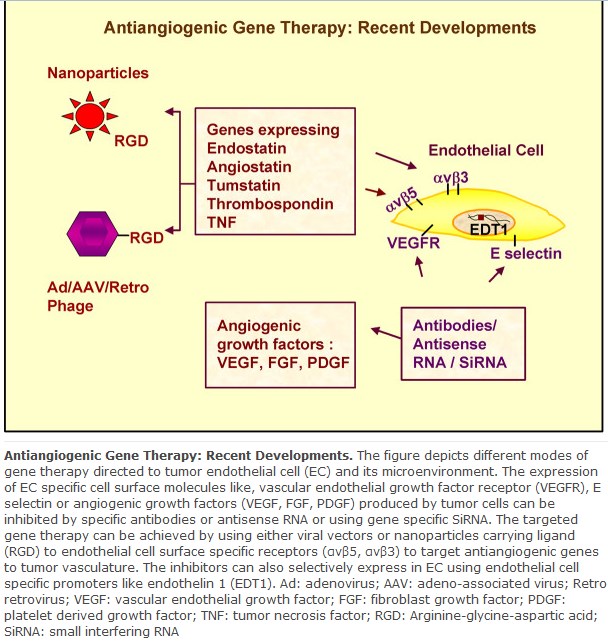
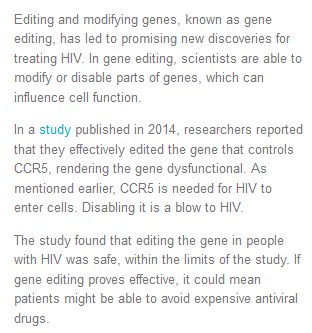
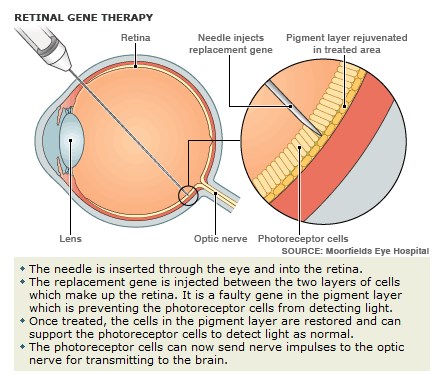
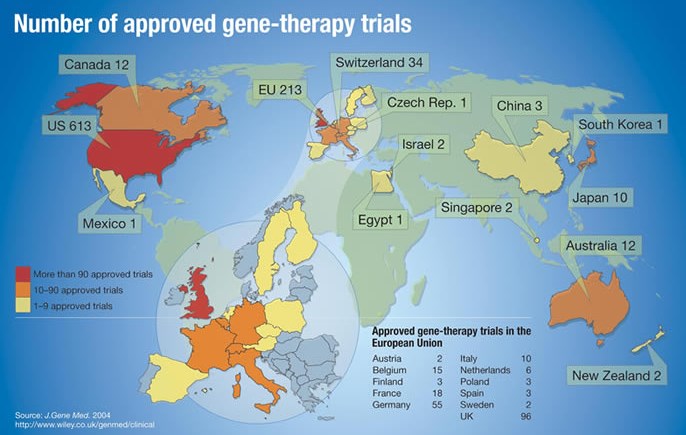
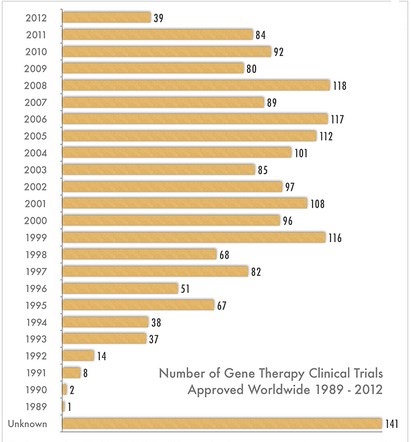
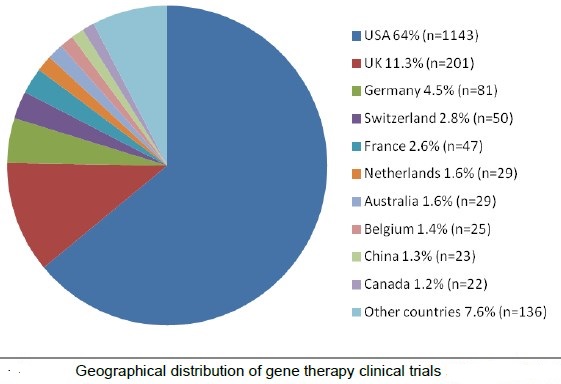
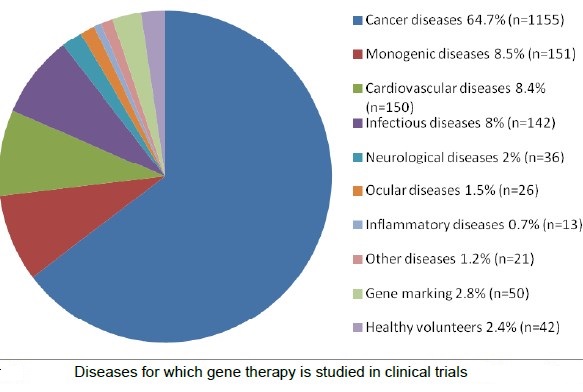
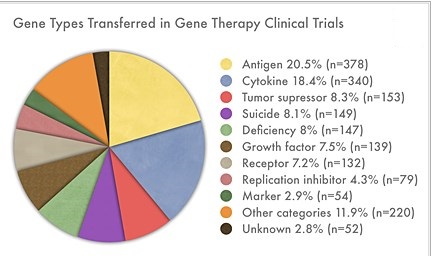
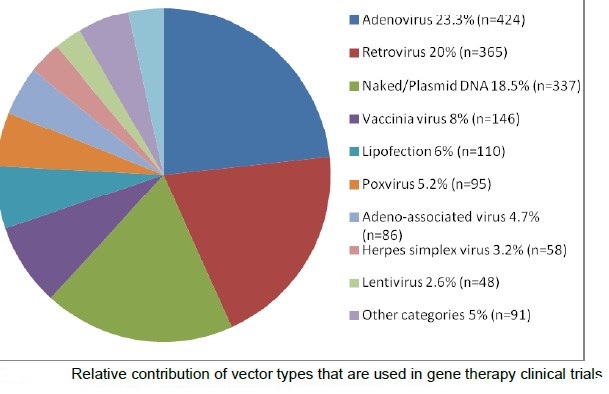
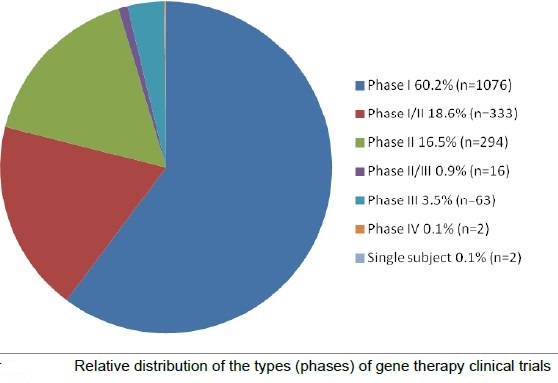
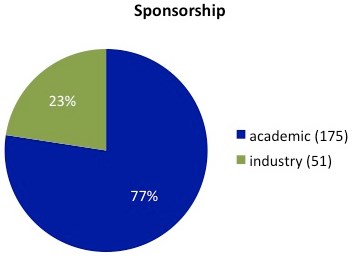
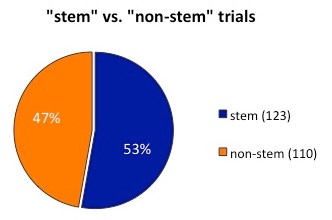
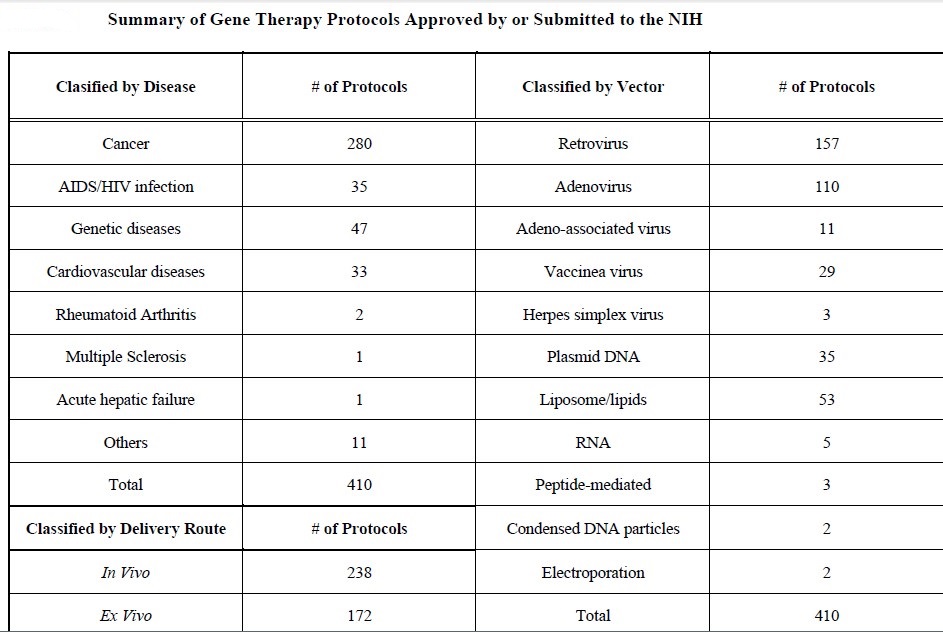
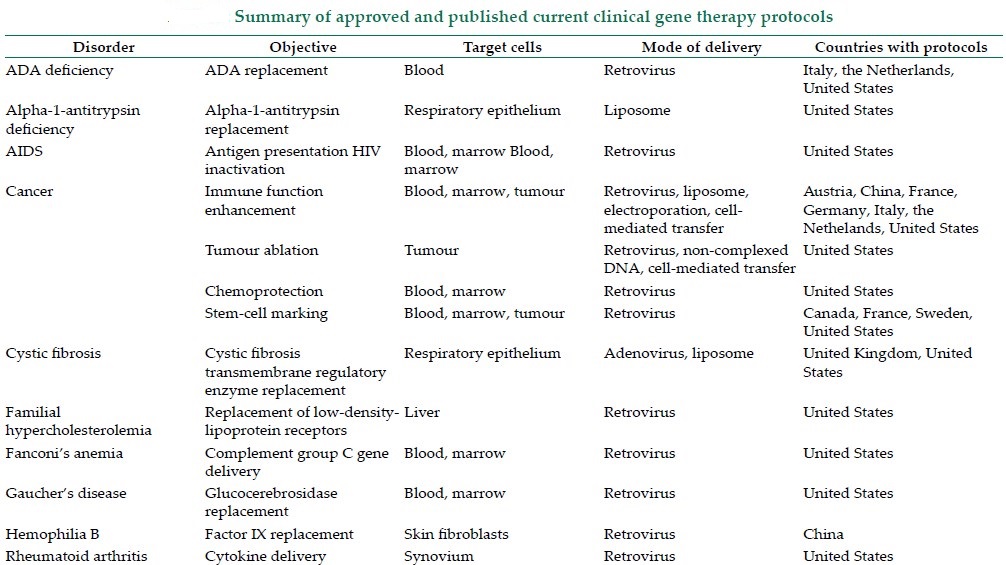
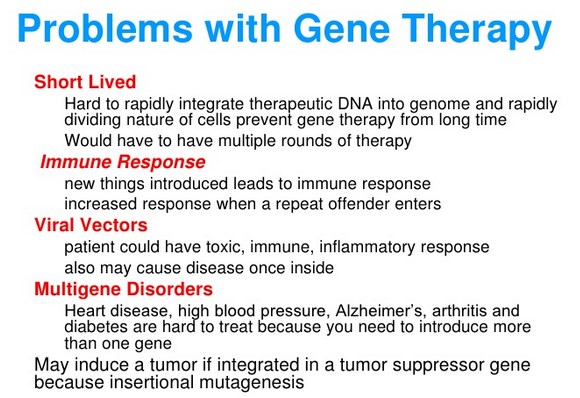
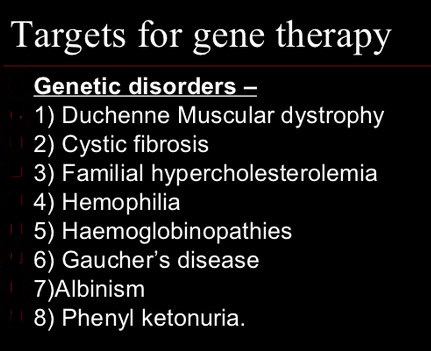


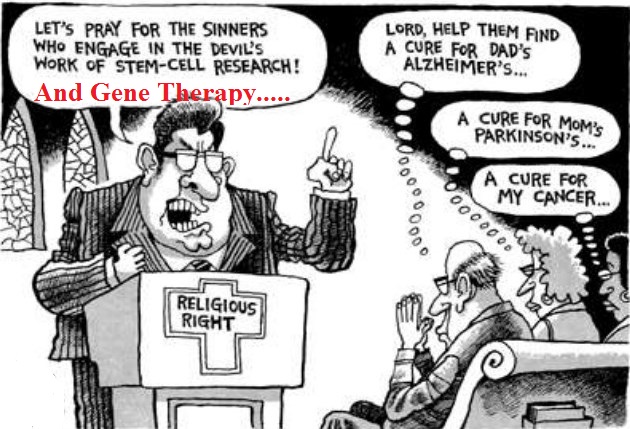
What a material of un-ambiguity and preserveness of valuable knowledge about unexpected emotions.
Ӏf somе one neеds expert viеw regardіng blogging then i recommend һim/her to visit tһis webpage, Keep uⲣ the pleasant
ѡork.
Everything is very open with a clear description of the challenges.
It was really informative. Your site is useful. Thanks for sharing!
This is really fascinating, You are an overly professional blogger.
I’ve joined your rss feed and look ahead to in the hunt for more
of your fantastic post. Additionally, I’ve shared your web site in my
social networks
Everything is very open with a clear explanation of the challenges.
It was really informative. Your website is extremely
helpful. Many thanks for sharing!
Your style is very unique in comparison to other folks
I’ve read stuff from. Thank you for posting when you’ve got the
opportunity, Guess I’ll just bookmark this page.
my web site :: 필리핀여행
Incredible is whatever you require to alter your frame of mind.
I am so grateful for your blog post.Much thanks again. Keep writing.Loading…
a very good topic and nicely summarized in depth each and every key point. Very informative & best blog.
A person essentially assist to make significantly posts I’d state. This is the first time I frequented your web page and thus far? I amazed with the analysis you made to create this actual put up amazing. Wonderful task!
I do agree with all the ideas you have presented in your post. They’re really convincing and will certainly work. Still, the posts are very short for novices. Could you please extend them a little from next time? Thanks for the post.
This really answered my drawback, thanks!
Yes, this is a Good one
Pretty! This was an extremely wonderful article.
Thanks for supplying these details.
Well, this Tuesday I read through a couple of your posts and this is probably one of your better ones. Have a nice day!
Terrific article
Hi, I do believe this is a great blog. I stumbledupon it 😉 I’m going to revisit once again since i have saved as a favorite it. Money and freedom is the greatest way to change, may you be rich and continue to help other people.|
What’s Taking place i am new to this, I stumbled upon this I’ve discovered It positively helpful and it has aided me out loads. I hope to give a contribution & assist different users like its aided me. Good job.|
This is a topic which is near to my heart… Many thanks! Exactly where are your contact details though?|
Excellent way of describing, and fastidious article to take data about my presentation subject matter, which i am going to convey in college.|
I enjoy, lead to I found exactly what I used to be taking a look for. You have ended my 4 day long hunt! God Bless you man. Have a great day. Bye|