Dr Rajiv Desai
An Educational Blog
ALCOHOL (beverage based on ethanol)
______
ALCOHOL (beverage based on ethanol):
______
President Obama loves Irish beer and celebrates the St.Patrick’s Day only with it!
________
Prologue:
Abraham Lincoln said: “It has long been recognized that the problems with alcohol relate not to the use of a bad thing, but to the abuse of a good thing.” We find alcohol throughout our daily lives. Alcoholic beverages have been consumed by humans since prehistoric times for a variety of hygienic, dietary, medicinal, religious, and recreational reasons. We associate the consumption of alcohol with the most pleasurable aspects of our culture. Parties and sports, picnics and vacations, summer and winter are all influenced by the attraction of alcoholic beverages. World Cup 2014: festival of football or alcohol? Whichever country hoists aloft the World Cup trophy, the real winner will be the alcohol industry according to BMJ report. I had written article on ‘Alcohol’ on February 6, 2009 and published on ourbollywood.com; the entire webpage was subsequently blocked by Indian media in December 2009. So I created my website www.drrajivdesaimd.com and re-published ‘Alcohol’ on it in January 2010. That article stated that alcohol is evil for human consumption, it destroys family and there is no safe limit for alcohol consumption. After going through various studies on the subject in detail, I felt the need to review the subject. I was teetotaler till I joined medical college. During medical studies, I used to drink once in 6 months under peer pressure. Later on since 1988 till 1999, I used to drink thrice a week of about 2-3 drinks per day. During those times, my health was poor with abnormal ECG, high LDL and high triglycerides levels. Since 2000, I practiced abstinence from alcohol and my health improved with ECG becoming normal and better lipid levels. Even though my alcohol consumption was moderate between 1988 till 1999, my health deteriorated while most studies worldwide suggest otherwise. Does alcohol help or harm? What is the safe limit of alcohol consumption? Are we biologically primed to drink alcohol? Is it moderate drinking or moderate life-style of moderate drinker that reduces cardiovascular mortality? Are most studies on alcohol flawed? I attempt to answer these questions. Alcohol is the most widely consumed drug worldwide. Alcohol is consumed by 80 % of people at some time in their lives. For many, drinking is as much a part of daily life as having dinner. Alcohol is a complex health and social issue. There is little doubt that considerable harm is done through its abuse – even the alcohol industry accepts this – but in moderation drinking alcohol is an acceptable convention utilized by over 2 billion people world-wide. Alcohol has been found outside the Solar System. Astronomers found alcohol as much as that in 400 trillion trillion beer bottles in G34.3, an interstellar cloud some 10,000 light-years from earth. Here on earth, I discuss the most prevalent and the most abused drink of all time, alcohol.
_________
Abbreviation and synonyms:
BAL = blood alcohol level (usually in milligrams of alcohol per 100 ml blood)
BAC = blood alcohol concentration/content (usually in grams of alcohol per 100 ml blood expressed as percentage)
For example: 80 BAL = 0.08 % BAC = 80 mg/100 ml blood = 0.08 gm/100 ml of blood
Conversion unit: one millimole of ethanol per liter of blood is equal to 4.61 milligrams of ethanol per 100 milliliters of blood.
ADH = alcohol dehydrogenase (remember, ADH also stands for anti-diuretic hormone i.e. vasopressin)
ALDH = aldehyde dehydrogenase
DSM-IV = The Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition
NADH = Reduced Nicotinamide adenine dinucleotide
Alcohol = ethanol= ethyl alcohol = C2H5OH (unless specified otherwise)
__________
Quotes on alcohol:
“Reality is an illusion created by a lack of alcohol.”
~ N.F. Simpson
“All is fair in love and beer.”
~ Kurt Paradis
“A drunk man’s words are a sober man’s thoughts.”
~ Steve Fergosi
“Beer is proof that God loves us and wants us to be happy.”
~ Benjamin Franklin
“Here’s to alcohol, the cause of, and solution to, all life’s problems.”
~ The Simpsons
“When I read about the evils of drinking, I gave up reading.”
~ Henry Youngman
“Alcohol may be man’s worst enemy, but the Bible says love your enemy.”
~ Frank Sinatra
_______
Key facts about alcohol updated till 2014:
•Worldwide, 3.3 million people die every year due to harmful use of alcohol, this represent 5.9 % of all deaths.
•The harmful use of alcohol is a causal factor in more than 200 disease and injury conditions.
•Overall 5.1 % of the global burden of disease and injury is attributable to alcohol, as measured in disability- adjusted life years (DALYs).
•Alcohol consumption causes death and disability relatively early in life. In the age group 20 – 39 years approximately 25 % of the total deaths are alcohol-attributable.
•There is a causal relationship between harmful use of alcohol and a range of mental and behavioural disorders, other noncommunicable conditions as well as injuries. The latest causal relationships that have been established between harmful drinking and incidence of infectious diseases include tuberculosis as well as HIV/AIDS.
•Beyond health consequences, the harmful use of alcohol brings significant social and economic losses to individuals and society at large.
____________
Introduction:
Commonest type of alcohol is ethyl alcohol, also known as ethanol. This has been consumed by human beings for its intoxicating and mind-altering effects. The term ‘alcohol’, unless specified otherwise, refers to ethanol or ethyl alcohol. Alcohol (or more precisely ethanol) is a colourless, tasteless, flammable liquid, formed during the fermentation of sugar by yeasts. In medicine, it is used as a tincture and antiseptic but its greatest use is in drinks. It is quickly absorbed into the bloodstream from the stomach & intestines. After absorption, it acts as a depressant on the central nervous system. This may have the beneficial effect of reducing feelings of fatigue but it also reduces judgment, self-control, and concentration. Reactions are slowed by alcohol and muscular coordination is impaired. . At high doses, the respiratory system slows down drastically and can cause a coma or death. It is particularly dangerous to mix alcohol with other depressants, such as GHB, Rohypnol, Ketamine, tranquilizers or sleeping pills. Combining depressants multiplies the effects of both drugs and can lead to memory loss, coma or death. Alcohol also acts as a diuretic, stimulating the kidneys to eliminate more urine which can result in dehydration. Alcoholic beverage is one of the most multipurpose drugs known to mankind, with multiple direct effects on neurochemical systems (Strohle et al., 2012). Alcohol is consumed by a large majority of people in the Western world because of naturally produced and easy to manufacturing, and reinforcement effects, and is likely to contribute to more morbidity, mortality, and public health costs than all of the illegal drugs (Ryden et al., 2012). It is usually consumed in diluted concentrations of absolute (i.e. 100 per cent) ethyl alcohol. Ethyl alcohol is also used as a reagent in some industrial applications. For such use, ethyl alcohol is combined with small quantities of methanol, with the mixture being called “denatured ethanol” to prevent theft for human consumption.
_
Alcohol is a product that has provided a variety of functions for people throughout all history. From the earliest times to the present, alcohol has played an important role in religion and worship. Historically, alcoholic beverages have served as sources of needed nutrients and have been widely used for their medicinal, antiseptic, and analgesic properties. The use of alcoholic beverages existed at least as early as 10,000 BC. The Greeks, Romans, and Babylonian are first culture which used alcohol for religious festivals, pleasure, as a source of nutrition and part of medicinal practices. Nowadays alcoholic beverages are incorporated into most cultures, and have a central role in daily life (Hanson, 1995). Whiskey, champagne, distilled spirits, gin and beer are the most alcoholic beverages that have been used throughout the world (Beyeler, 2011).
_
_
Alcohol (beverage ethanol) distributes throughout the body, affecting almost all systems and altering nearly every neurochemical process in the brain. This drug is likely to exacerbate most medical conditions, affect almost any medication metabolized in the liver, and temporarily mimic many medical (e.g., diabetes) and psychiatric (e.g., depression) conditions. Because 80% of people in Western countries have consumed alcohol, and two-thirds have been drunk in the prior year, the lifetime risk for serious, repetitive alcohol problems is almost 20% for men and 10% for women, regardless of a person’s education or income. While low doses of alcohol have some healthful benefits, the intake of more than three standard drinks per day on a regular basis enhances the risk for cancer and vascular disease, and alcohol use disorders decrease the life span by about 10 years. Alcohol is legal, which means it is available to the majority of adults who wish to purchase it at any number of outlets. Alcohol is widely advertised and marketed to consumers, and alcohol manufacturers are major sponsors of everything from national sporting, social and cultural events to individuals, local sports clubs and pub competitions.
_
Alcohol, when drunk responsibly, can produce a sense of relaxation, wellbeing and even euphoria in individuals, which enhances their enjoyment of whatever activity they are participating in. This is because alcohol is a central nervous system depressant and directly affects those parts of the brain which regulate emotion, memory, co-ordination and planning. It is rapidly absorbed into the blood stream and affects almost all of the body’s cells and systems. Consequently, for the majority of people who drink alcohol responsibly, it can act as a disinhibiting agent. This may allow them to ‘let their hair down’, feel more socially adept and reduce the anxiety they may feel in social situations. This is why alcohol is known as a ‘social lubricant’! It’s fast acting and loosens a person up so their interaction with their environment and other people seems to occur more smoothly and with a greater degree of pleasure. However, too much alcohol can cause concern. Some people drink in an attempt to self-medicate personal problems or perceived deficiencies in their lives, and use alcohol to ‘numb the pain’ and avoid thinking about their situation. Domestic violence, abuse, family problems, divorce, bullying, low self-esteem, health issues, unemployment, financial stress – alcohol can be seen as an escape for a while. For other people, the reasons for alcohol dependence are less obvious and may be associated not with negative personal triggers, but with our drinking culture. Their dependence often develops when the positive effects of alcohol – such as a sense of relaxation, more confidence – become more prominent and the person comes to see alcohol as an essential component of their enjoyment of activities such as attending sporting events, getting together with friends, even relaxing after a hard day’s work. Regardless of the reasons behind their drinking, as a person drinks more, they develop a tolerance to the effects of alcohol, and have to drink greater quantities of alcohol more frequently to achieve the same positive effects they used to receive from drinking. After a while, drinking alcohol may start to feature more prominently in the person’s life as an activity in its own right, supplanting time usually spent with family, friends and associates; and adversely affecting their ability to perform their job or engage in study or leisure activities.
_
Alcohol is socially acceptable because it has been around since biblical times and people have been using it in most cultures throughout history. Its use throughout history has prompted it to not only be thought of as ‘ok’ but also as being acceptable in society. Its use by monarchs and leaders globally would make it seem acceptable because the public’s views on them as role models would make these people think that consuming alcohol is fine. Because alcohol takes around 20-30 years for the long term effects to show up and when consumed in small amounts contains only miniscule risks, it is often thought to be harmless and not dangerous. This perception of alcohol being harmless would make people drink alcohol in both small and large amounts without worrying about the risks they are taking. Alcohol can also be a force for good as it brings people together and forms social bonds. Its use at social events and occasions help build friendships and improve socializing skills. It can also make people happier and can be an emotional stabilizer.
__________
Etymology:
The word alcohol appears in English as a term for a very fine powder in the 16th century. It was borrowed from French, which took it from medical Latin. Ultimately the word is from the Arabic كحل (al-kuḥl, “kohl, a powder used as eyeliner”). Al- is the Arabic definitive article, equivalent to the in English; alcohol was originally used for the very fine powder produced by the sublimation of the natural mineral stibnite to form antimony sulfide Sb2S3 (hence the essence or “spirit” of the substance), which was used as an antiseptic, eyeliner, and cosmetic. Bartholomew Traheron, in his 1543 translation of John of Vigo, introduces the word as a term used by “barbarous” (Moorish) authors for “fine powder.” Vigo wrote: the barbarous auctours use alcohol, or (as I fynde it sometymes wryten) alcofoll, for moost fine poudre. The 1657 Lexicon Chymicum by William Johnson glosses the word as antimonium sive stibium. By extension, the word came to refer to any fluid obtained by distillation, including “alcohol of wine,” the distilled essence of wine. Libavius in Alchymia (1594) refers to vini alcohol vel vinum alcalisatum. Johnson (1657) glosses alcohol vini as quando omnis superfluitas vini a vino separatur, ita ut accensum ardeat donec totum consumatur, nihilque fæcum aut phlegmatis in fundo remaneat. The word’s meaning became restricted to “spirit of wine” (the chemical known today as ethanol) in the 18th century and was extended to the class of substances so-called as “alcohols” in modern chemistry after 1850. The first alcohol (today known as ethyl alcohol) was discovered by the tenth-century Persian alchemist al-Razi. The current Arabic name for alcohol (ethanol) is الغول al-ġawl – where gawl in Arabic means spirit or ghost. The word’s meaning became restricted to “spirit of wine” (ethanol) in the 18th century, and was again extended to the family of substances so called in modern chemistry from 1850. The term ethanol was invented 1838, modeled on the German word äthyl (Liebig), which is in turn based on Greek aither ether and hyle “stuff.” Whisky is a short form of usquebaugh where uisce means water and bethad means of life. Whisky means water of life.
________
History of alcohol:
Fermented beverages of pre- and proto-historic China:
Chemical analyses of ancient organics absorbed into pottery jars from the early Neolithic village of Jiahu in Henan province in China have revealed that a mixed fermented beverage of rice, honey, and fruit (hawthorn fruit and/or grape) was being produced as early as the seventh millennium before Christ (B.C.). This prehistoric drink paved the way for unique cereal beverages of the proto-historic second millennium B.C., remarkably preserved as liquids inside sealed bronze vessels of the Shang and Western Zhou Dynasties. These findings provide direct evidence for fermented beverages in ancient Chinese culture, which were of considerable social, religious, and medical significance, and help elucidate their earliest descriptions in the Shang Dynasty oracle inscriptions. Chemical analysis of traces absorbed and preserved of ancient pottery jars from the neolithic village of Jiahu in the Henan province of northern China revealed residue left behind by the alcoholic beverages they had once contained. According to a study published in the Proceedings of the National Academy of Sciences, chemical analysis of the residue confirmed that a fermented drink made of grape and hawthorn fruit wine, honey mead and rice beer was being produced in 7000–5600 BC (McGovern et al., 2005; McGovern 2009).The results of this analysis were published in December 2004. This is approximately the time when barley beer and grape wine were beginning to be made in the Middle East.
_
Purposeful production of alcoholic beverages is common in many cultures and often reflects their cultural and religious peculiarities as much as their geographical and sociological conditions. Discovery of late Stone Age jugs suggest that intentionally fermented beverages existed at least as early as the Neolithic period (cir. 10,000 BC). Alcohol, as an intentional beverage, has been supposed to have been created, in the form of beer, during the late Stone Age due to the discovery of beer jugs; this was during the Neolithic period around 10,000 B.C. (Hanson, 1995). Egyptians appear to have introduced wine in 4,000 B.C. (Hanson, 1995). Some specialists have ventured to say that beer may have been a staple before bread thus one is able to draw the conclusion that it served as a necessity before a luxury possibly ensuring the survival of early man (Hanson, 1995). The earliest alcoholic beverages were derived from berries or honey (Hanson, 1995). Alcohol was used medicinally in places such as Sumer at approximately 2,000 B.C. (Hanson, 1995). By no coincidence alcohol found its way into early religions and became rather important in various ceremonies and forms of worship. Christians tend to use wine when taking the Lord’s Supper for it signifies their savior’s blood; Ancient Greeks had the wine god Dionysus; Egyptians had Osiris. Beer and wine were everyday products to these peoples and actually aided them with survival especially in areas where clean water was hard to find. These early alcoholic beverages were used globally from Europe throughout Asia. Not surprisingly the beverage has faced much controversy even during these early times. In China, laws with respect to the creation of wine were put into effect and withdrawn forty-one instances from 1,100 B.C. to A.D. 1,400 (Hanson, 1995). Excessive drinking has always been a sort of problem even in these cultures. Greeks rarely drank heavily except during festival times: binge drinking (Hanson, 1995). The Romans had serious issues with the beverage and one might be able to go as far as saying that it had a part in their downfall (alcoholism). Alcohol has always taken on this controversy but has for some reason or another stayed around. The viticulture we see and know today originated from monks during the middle ages (Hanson, 1995). With a stable environment they were able to perfect brewing and winemaking techniques which are still used today. One of the advances in brewing made by monks was the invention of distillation (Hanson, 1995). Called aqua vitae, this distilled alcohol was meant to be used medicinally (Hanson, 1995). Aqua vitae later took on the identity brandy, derived from brandewijn which means burnt wine; thus the invention of the first hard liquor (Hanson 1995). Soon to follow were Ireland’s whiskey in the sixteenth century and France’s champagne and gin in the seventeenth century (Hanson, 1995). In the year 2000 the United States was the leading producer of beer closely followed by China (beer: leading beer-producing countries, 2000).
_
Aboriginal alcohol consumption in Australia:
Alcoholic drinks before European invasion:
Aboriginal people knew of and used mild alcoholic drinks before the arrival of the white people. Their use, however, was strictly controlled. They produced alcohol from a variety of plants. Interestingly, Aboriginal words for ‘alcohol’ were often derived from words meaning ‘dangerous’, ‘bad’ or ‘poisonous’, but also ‘sweet’ or ‘delicious’ (central Australia) and ‘salty’, ‘bitter’ or ‘sour’. Use of these kinds of alcohol from natural sources was very limited for another reason: The absence of suitable containers, and climatically varying access to these resources, ensured that there was no large-scale production or consumption of alcohol. Traditionally, Aboriginal people used plant medicines, healing hands and spirit to recover from and heal trauma, grief, sadness, pain and sorrow. Today, alcohol has replaced these remedies.
Alcohol consumption after European invasion:
Aboriginal alcohol use changed significantly after white people invaded Australia. Within weeks of the arrival of the first fleet the first pubs opened, and this would shape the way Australian society developed over the next few decades. Many Aboriginal labourers were paid in alcohol or tobacco (if their wages were not stolen). In the early 1800s a favourite spectator sport of white people in Sydney was to ply Aboriginal men with alcohol and encourage them to fight each other, often to the death. White settlers also gave alcohol to Aboriginal people as payment for sex. Alcohol-induced prostitution had a harmful effect on child rearing and accelerated the birth rate of mixed descent children, usually rejected by their European fathers. Interestingly, Aboriginal people were initially denied alcohol consumption because it was feared that “natives were more adversely affected than others” when consuming alcohol.
_______
Alcohol-Timeline:
6000-4000 BCE
Viticulture, the selective cultivation of grape vines for making wine, is believed to originate in the mountains between the Black and Caspian seas (modern Armenia). The oldest archaeological evidence of wine is residue found inside of jars from Hajji Firuz Tepe in northern Iran.
3000-2000 BCE
Beer making flourishes in Sumerian/Mesopotamian civilization (modern day Iraq) with recipes for over twenty varieties of beer recorded on clay tablets.
3000-2000 BCE
Wine production and trade become an important part of Mediterranean commerce and culture. Ships carry large quantities between cities.
2200 BCE
Cuneiform tablet recommends beer as a tonic for lactating women.
3000-1000 BCE
Beer is unrefined and usually drunk through straw because it had large quantities of grain and mash in it.
1800 BCE
Beer is produced in quantity in northern Syria.
1500 BCE
Wine is produced commercially in the Levant and Aegean.
900-800 BCE
Extensive, large scale vineyards laid out in Assyria (modern Iraq) produced over 10,000 skins of wine for the new capitol at Nimrud by Assurbanipal II.
800 BCE
Distillation of barley and rice beer is practiced in India.
425 BCE
Earliest known wine press from France is evidence of winemaking having begun in the region.
50 BCE
Dionysius of Halicarnassus writes the Gauls (French) have no knowledge of wine but used a foul-smelling liquour made of barley rotted in water (beer).
500 AD
Wine making reaches Tang China along the Silk Road.
768 AD
First specific reference to the use of hops in beer from the Abbey St. Denis in France by King Pepin le Bref.
1100 AD
Alcohol distillation is documented by the medical school at Salerno, Italy. The product of the distillation is named ‘spirits’ in reference to it being the extracted spirit of the wine.
Middle Ages
Distillation of grain alcohol in Europe follows the earlier distillation of wine.
1516 AD
German Beer Purity Law (“Rheinheitsgebot”) makes it illegal to make beer with anything but barley, hops, and pure water.
Early 1500’s
Benedictine, a cognac-based alcohol with added herbs, is developed at the monastery in Fecamp, Normandy.
1525-1550
In England excessive use of distilled spirits first becomes apparent.
1524-1556
Viticulture spread through Peru, Chile and Argentina.
1500’s
The term ‘alcohol’ is now used specifically to refer to distilled spirits rather than its previous general meaning of any product of the process of vaporizing and condensing.
1550 – 1575
Thomas Nash describes widespread inebriety in Elizabethan England; drunkenness is mentioned for the first time as a crime, and preventive statutes multiply.
17th Century
Use of hashish, alcohol, and opium spreads among the population of occupied Constantinople
1600 – 1625
During the reign of James I, numerous writers describe widespread drunkenness from beer and wine among all classes. Alcohol use is tied to every endeavor and phase of life, a condition that continues well into the eighteenth century.
1606
British Parliament passes “The Act to Repress the Odious and Loathsome Sin of Drunkenness”.
17th century America
Massachusetts laws attempt to control widespread drunkenness, particularly from home-brews, and to supervise taverns. At the same time each town is ordered to establish a man to sell wines and “strong water” so that the public will not suffer from lack of proper accommodations (1637); inns are required to provide beer for entertainment (1649).
1643
Britain imposes an excise tax on distilled spirits. Along with a tax of alcohol came the development of the moonshine trade.
1650 – 1675
New England colonies attempt to establish a precise definition of drunkenness that includes the time spent drinking, amount, and behavior. Massachusetts laws against home-brews are reaffirmed (1654); a law forbidding the payment of wages in the form of alcohol results in a labor strike (1672).
1650 – 1675
Gin is developed in Holland (c. 1650) by distilling grain with the juniper berry. Gin can be produced cheaply and plentifully, and the gin industry grows rapidly in England after it is introduced by British soldiers fighting in the Low Countries.
1675 – 1700
New laws encourage the distillation and sale of spirits for revenues and support of the landed aristocracy (1690). The production of distilled liquors, mostly gin, increases dramatically; so do use, particularly among the poor. Excessive consumption of beer and wine is still prevalent among the middle and upper classes.
Late 1600’s
Western France develops a reputation as the producer of fine quality cognac.
1700
Scotland and Ireland develop reputations for their quality whiskies.
1770s
Viticulture brought to Alta California. Within a century, it became one of the great wine-producing regions of the world.
1791
The Act of 1791 (popularly called the “Whiskey Tax”) enacted a tax on both publicly and privately distilled whiskey.
1814-1817
A new alcohol tax is temporarily imposed in the United States to help pay for the War of 1812.
Early 19th Century
Development of the continuous still makes the process of alcohol distillation cheaper and easier to control.
1860
Legal alcohol distilleries were operating in the United States producing 88 million gallons of liquor per year.
1906
Pure Food and Drug Act is passed, regulating the labeling of products containing Alcohol, Opiates, Cocaine, and Cannabis, among others. The law went into effect Jan 1, 1907
Dec 1917
The 18th Amendment to the Constitution (prohibition amendment) is adopted by the required majority of both houses of Congress.
Jan 16, 1920
The 18th Amendment (prohibition amendment) takes effect, prohibiting the manufacture, sale, transportation, import, and export of intoxicating liquors for beverage purposes.
1920-1933
The illicit alcohol trade booms in the United States.
Dec 5, 1933
The prohibition of alcohol is repealed in the U.S. with the passage of the 21st Amendment, effective immediately.
Oct 14, 1978
US President Jimmy Carter signs bill legalizing home brewing of beer for the first time since Prohibition.
Dec 6, 2008
Entheogenesis Australis Symposium
_____
Historically problems commonly associated with industrialization and rapid urbanization were also attributed to alcohol. Thus, problems such as urban crime, poverty and high infant mortality rates were blamed on alcohol, although “it is likely that gross overcrowding and unemployment had much to do with these problems” (Soumia, 1990, p. 21). Over time, more and more personal, social and religious/moral problems would be blamed on alcohol. And not only would it be enough to prevent drunkenness; any consumption of alcohol would come to be seen as unacceptable. Groups that began by promoting temperance – the moderate use of alcohol – would ultimately become abolitionist and press for the complete and total prohibition of the production and distribution of beverage alcohol. Unfortunately, this would not eliminate social problems but would compound the situation by creating additional problems.
_________
Alcohol and culture:
_
Culture of alcohol:
Drinking culture refers to the customs and practices associated with the consumption of alcoholic beverages. Although alcoholic beverages and social attitudes toward drinking vary around the world, nearly every civilization has independently discovered the processes of brewing beer, fermenting wine, and distilling spirits. Alcohol and its effects have been present in societies throughout history. Drinking is documented in the Hebrew and Christian Bibles, in the Qur’an, in art history, in Greek and Roman literature as old as Homer, and in Confucius’s Analects.
_
_
Ethnic and Cultural influences on Drinking Patterns:
Alcohol consumption is governed, in large part, by the social rules, norms, customs, and traditions acquired through an individual’s cultural and ethnic contextual experiences, including immediate family, extended kin, peers, “teachings,” and “preaching.” Ignoring these influences can lead to misguided judgments about the appropriateness and inappropriateness of alcohol consumption and concomitant behaviors (Heath, 2000). For example, there is a danger that many Native Americans will develop a belief in the stereotype of the “drunken Indian” and that this inaccurate stereotype may lead an individual to conclude that drinking to excess is normative within the group (May & Smith, 1988). This conclusion was based on a set of observations of Navajo Indians. The concept has parallels in studies of individuals’ tendency to overestimate the amount of alcohol use/abuse that occurs within their communities or in the population, and the possibility that these misperceptions “normalize” their behavior (Perkins & Wechsler, 1996). Many interventions are based on assumptions that do not recognize the importance of these norms, practices, and influences on alcohol consumption and abuse. Such a lack of cultural relativity may result in a misinterpretation of intervention outcomes (Heath, 2000). For these reasons, Adrian (2002) cautions researchers to be alert to implicit assumptions about relationships between ethnicity and addiction, particularly in reference to differences in prevalence rates, associated problems, and use-related attitudes.
_
Cultural Norms and Values:
Ethnic and cultural group norms, values, and expectations concerning alcohol vary markedly, as do cultural strengths and resiliency factors (Amodeo & Jones, 1997; Oetting, et al., 1998). Members of different ethnic and cultural groups show preferences for different types of alcoholic beverages, which may, in turn, affect access and relative alcohol content/ exposure (Graves & Kaskutas, 2002; Heath, 2000). Individuals who drink in social groups and in situations where there are linked activities, adjust their consumption rates and rhythms to others in the group and/or to the linked activities rather than follow an individually-determined pattern of consumption (Heath, 2000). Some cultures abhor any alcohol use. For example, among non-drinking adolescents, religion often plays a central role in life. Muslim and non-Western immigrant teenagers are very likely to be abstainers-at least among Norway’s adolescents (Pedersen & Kolstad, 2000). Unfortunately, this does not guarantee an absence of alcohol-related problems, and when alcohol is a problem, these cultural norms may lead to hiding, minimizing, denial, or exclusion (Abudabbeh & Hamid, 2001; Straussner, 2001b). In cultures that accept some alcohol consumption, norms govern what types are consumed. There are also norms concerning how much is consumed, and what are acceptable forms of intoxicated behavior. “Some cultures reinforce abstinence as a norm; others approve of drinking only as part of religious ceremonies. Drinking, especially if it occurs in a group setting, may symbolize solidarity…” (Amodeo & Jones, 1997). Thus, any specific type of substance use could be differentially viewed as normative, deviant to some degree, or quite deviant behavior, depending on the cultural context (Oetting et al., 1998). Culture has a powerful influence on alcohol-related behaviors, as well as on belief systems about alcohol among users and among members of the users’ support systems (Amodeo & Jones, 1997). Furthermore, socialization theory explains how specific drinking customs and rituals are transmitted across generations and from one individual to another within a family, ethnic, or cultural group (Oetting et al., 1998). The degree to which cultural norms influence an individual’s drinking behavior is determined, in part, by the extent of that person’s identification with the group, the degree of consistency in the group’s norms, and the presence of confounding or complementary forces, such as gender and age norms (Oetting et al., 1998). Drinking and other drug use behavior are also associated with the perception of risk associated with consumption, and the risk perception may differ among ethnic and cultural groups. White individuals in a general population survey are the least likely to perceive risks for alcohol use (compared to Black and Hispanic respondents), and have the highest prevalence of past month use (Ma & Shive, 2000).
_
How Culture influences the way people drink:
Sociologists, anthropologists, historians, and psychologists, in their study of different cultures and historical eras, have noted how malleable people’s drinking habits are:
“When one sees a film like Moonstruck, the benign and universal nature of drinking in New York Italian culture is palpable on the screen. If one can’t detect the difference between drinking in this setting, or at Jewish or Chinese weddings, or in Greek taverns, and that in Irish working-class bars, or in Portuguese bars in the worn-out industrial towns of New England, or in run-down shacks where Indians and Eskimos gather to get drunk, or in Southern bars where men down shots and beers–and furthermore, if one can’t connect these different drinking settings, styles, and cultures with the repeatedly measured differences in alcoholism rates among these same groups, then I can only think one is blind to the realities of alcoholism.”
Peele, S., Diseasing of America, Lexington Books, Lexington, MA, 1989, pp. 72-73.
_
“Sociocultural variants are at least as important as physiological and psychological variants when we are trying to understand the interrelations of alcohol and human behavior. Ways of drinking and of thinking about drinking are learned by individuals within the context in which they learn ways of doing other things and of thinking about them–that is, whatever else drinking may be, it is an aspect of culture about which patterns of belief and behavior are modeled by a combination of example, exhortation, rewards, punishments, and the many other means, both formal and informal, that societies use for communicating norms, attitudes, and values.”
Heath, D.B., “Sociocultural Variants in Alcoholism,” pp. 426-440 in Pattison, E.M., and Kaufman, E., eds., Encyclopedic Handbook of Alcoholism, Gardner Press, New York, 1982, p. 438.
_
“Individual drinkers tend to model and modify each others’ drinking and, hence there is a strong interdependence between the drinking habits of individuals who interact…. Potentially, each individual is linked, directly or indirectly, to all members of his or her culture….”
Skøg, O., “Implications of the Distribution Theory for Drinking and Alcoholism,” pp. 576-597 in Pittman, D.J., and White, H.R., eds., Society, Culture, and Drinking Patterns Reexamined, Rutgers Center of Alcohol Studies, New Brunswick, NJ, 1991, p. 577.
_
“Over the course of socialization, people learn about drunkenness what their society `knows’ about drunkenness; and, accepting and acting upon the understandings thus imparted to them, they become the living confirmation of their society’s teachings.”
MacAndrew, C., and Edgerton, R.B., Drunken Comportment: A Social Explanation, Aldine, Chicago, 1969, p. 88.
__
Enormous differences can be observed as to how different ethnic and cultural groups handle alcohol:
“…In those cultures where drinking is integrated into religious rites and social customs, where the place and manner of consumption are regulated by tradition and where, moreover, self-control, sociability, and `knowing how to hold one’s liquor’ are matters of manly pride, alcoholism problems are at a minimum, provided no other variables are overriding. On the other hand, in those cultures where alcohol has been but recently introduced and has not become a part of pre-existing institutions, where no prescribed patterns of behavior exist when `under the influence,’ where alcohol has been used by a dominant group to exploit a subject group, and where controls are new, legal, and prohibitionist, superseding traditional social regulation of an activity which previously has been accepted practice, one finds deviant, unacceptable and asocial behavior, as well as chronic disabling alcoholism. In cultures where ambivalent attitudes toward drinking prevail, the incidence of alcoholism is also high.”
Blum, R.H., and Blum, E.M., “A Cultural Case Study,” pp. 188-227 in Blum, R.H., et al., Drugs I: Society and Drugs, Jossey-Bass, San Francisco, 1969, pp. 226-227.
_
“Different societies not only have different sets of beliefs and rules about drinking, but they also show very different outcomes when people do drink…. A population that drinks daily may have a high rate of cirrhosis and other medical problems but few accidents, fights, homicides, or other violent alcohol-associated traumas; a population with predominantly binge drinking usually shows the opposite complex of drinking problems…. A group that views drinking as a ritually significant act is not likely to develop many alcohol-related problems of any sort, whereas another group, which sees it primarily as a way to escape from stress or to demonstrate one’s strength, is at high risk of developing problems with drinking.”
Heath, D.B., “Sociocultural Variants in Alcoholism,” pp. 426-440 in Pattison, E.M., and Kaufman, E., eds., Encyclopedic Handbook of Alcoholism, Gardner Press, New York, 1982, pp. 429-430.
_
“One striking feature of drinking…is that it is essentially a social act. The solitary drinker, so dominant an image in relation to alcohol in the United States, is virtually unknown in other countries. The same is true among tribal and peasant societies everywhere.”
Heath, D.B., “An Anthropological View of Alcohol and Culture in International Perspective,” pp. 328-347 in Heath, D.B., ed., International Handbook on Alcohol and Culture, Greenwood Press, Westport, CT, 1995, p. 334.
_
Throughout history, wine and other alcoholic beverages have been a source of pleasure and aesthetic appreciation in many cultures:
“In most of the cultures…the primary image is a positive one. Usually drinking is viewed as an important adjunct to sociability. Almost as often, it is seen as a relatively inexpensive and effective relaxant, or as an important accompaniment to food…. Its use in religions is ancient, and reflects social approval rather than scorn…. Most people in the United States, Canada, and Sweden, when asked what emotions they associate with drinking, responded favorably, emphasizing personal satisfactions of relaxation, social values of sociability, an antidote to fatigue, and other positive features….”
Heath, D.B., “Some Generalizations about Alcohol and Culture,” pp. 348-361 in Heath, D.B., ed., International Handbook on Alcohol and Culture, Greenwood Press, Westport, CT, 1995, p. 350-351.
_
“[In colonial America] Parents gave it [alcohol] to children for many of the minor ills of childhood, and its wholesomeness for those in health, it appeared, was only surpassed by its healing properties in case of disease. No other element seemed capable of satisfying so many human needs. It contributed to the success of any festive occasion and inspirited those in sorrow and distress. It gave courage to the soldier, endurance to the traveler, foresight to the statesman, and inspiration to the preacher. It sustained the sailor and the plowman, the trader and the trapper. By it were lighted the fires of revelry and of devotion. Few doubted that it was a great boon to mankind.”
Levine, H.G., “The Good Creature of God and the Demon Rum,” pp. 111-161 in National Institute on Alcohol Abuse and Alcoholism, Research Monograph No. 12: Alcohol and Disinhibition: Nature and Meaning of the Link, NIAAA, Rockville, MD, 1983, p. 115.
_
“British attitudes are generally favorable to drinking in itself while disapproving of heavy or problematic drinking. The drinking scene in the UK has undergone marked changes during recent decades. Public bars are now far more congenial and attractive to drinkers of both genders…. The British generally enjoy drinking, and recent legislation has attempted to increase the social integration of alcohol use and to discourage alcohol-related problems, but not drinking in itself.”
Plant, M.A., “The United Kingdom,” pp. 289-299 in Heath, D.B., ed., International Handbook on Alcohol and Culture, Greenwood Press, Westport, CT, 1995, p. 298.
_
“…we want to assure moderate drinkers that the age-old bromides they learned from their grandmothers (like putting Amaretto on a teething baby’s gums) or their grandfathers (who told them a glass of wine completes a good meal) or their fathers (a beer on a hot day with friends is one of the great pleasures in life) are still sound and are worth passing on.”
Peele, S., Brodsky, A., and Arnold, M., The Truth About Addiction and Recovery, Simon & Schuster, New York, 1991, p. 339.
_
Young people in many cultures are introduced to drinking early in life, as a normal part of daily living:
Whereas educational programs in the U.S. typically emphasize that children must never taste alcohol, the reverse is true in societies that maintain the best moderate drinking practices. “The idea of a minimum age before [which] children should be `protected’ from alcohol is alien in China and France; where it is a matter of law, the mid or late teens are favored…. Children learn to drink early in Zambia by taking small quantities when they are sent to buy beer; children in France, Italy, and Spain are routinely given wine as part of a meal or celebration.”
Heath, D.B., “An Anthropological View of Alcohol and Culture in International Perspective,” pp. 328-347 in Heath, D.B., ed., International Handbook on Alcohol and Culture, Greenwood Press, Westport, CT, 1995, p. 339.
_
“A book on practical child-raising, known in [a French] village since the early twenties, [states that when a child has reached the age of two]: `One can also give at mealtime a half-glass of water lightly reddened with wine, or some beer or cider very diluted with water.’ In general, the recent literature is more cautious. It suggests, as a more suitable time for introducing children to alcoholic beverages, four years of age rather than two. Generally, though, wine is first offered when the child is two or more, can hold his own glass quite safely in his hand, and can join the family at table.”
Anderson, B.G., “How French Children Learn to Drink,” pp. 429-432 in Marshall, M., ed., Beliefs, Behaviors, & Alcoholic Beverages: A Cross-Cultural Survey, University of Michigan Press, Ann Arbor, MI, 1979, pp. 431-432.
_
“Eighteen…remains the minimum age for purchase in the United Kingdom. However, it is not illegal for those aged five and above to drink outside licensed premises.”
Plant, M.A., “The United Kingdom,” pp. 289-299 in Heath, D.B., ed., International Handbook on Alcohol and Culture, Greenwood Press, Westport, CT, 1995, p. 292.
_
“[In Spain] The undifferentiated beverage and food shops flourish not only in the community, but also in high schools and technical schools, which have students generally between the ages of 14 and 18. Such educational centers usually have a cantina (a bar or saloon) which closely duplicates the products sold in bars of the outside community; snacks, lunches, coffee, tea, sodas, beer, wine, and brandies are available…. Beer is generally available to students in all educational centers. However, a policy may be mandated that beer be the only alcoholic beverage available to students under 18 years of age, or that no alcohol be sold before noon, or that there be a two-drink limit for each person. These regulations may or may not be enforced, however. Observations in high school cafeterias reveal that the majority of students consume coffee or soft drinks and fewer than 20% take beer either separately or with lunch.”
Rooney, J.F., “Patterns of Alcohol Use in Spanish Society,” pp. 381-397 in Pittman, D.J., and White, H.R., eds., Society, Culture, and Drinking Patterns Reexamined, Rutgers Center of Alcohol Studies, New Brunswick, NJ, 1991, p. 382.
_
“Although the minimum legal age for purchasing alcohol in Spain is 16 years, no one is concerned with formalities of the law…. Spaniards sharply distinguish legality from morality. The penal code originates from the central government, whereas the code of moral behavior comes from the norms of the people. Consequently, there is a large part of the penal code to which the citizenry is morally indifferent…. My own observations reveal that youngsters of 10 and 12 years are able to buy liter bottles of beer in grocery and convenience stores if they choose.”
Rooney, “Patterns of Alcohol Use in Spanish Society,” p. 393.
_
“In sum, Spain along with other Southern European countries allows its youth early access to alcoholic beverages without the concomitant problems of rowdy behavior, vandalism, and drunk driving that Americans typically associate with youth drinking.”
Pittman, D.J., “Cross Cultural Aspects of Drinking, Alcohol Abuse, and Alcoholism,” pp. 1-5 in Waterhouse, A.L., and Rantz, J.M., eds., Wine in Context: Nutrition, Physiology, Policy (Proceedings of the Symposium on Wine & Health 1996), American Society for Enology and Viticulture, Davis, CA, 1996, p. 4.
_
_
Free drinks:
Various cultures and traditions feature the social practice of providing free alcoholic drinks for others. For example, during a wedding reception, or a bar mitzvah, free drinks are often served to guests, a practice that is known as “an open bar.” Free drinks may also be offered to increase attendance at a social or business function. They are commonly offered to casino patrons to entice them to continue gambling.
_
Symbolic functions:
• In all societies, alcoholic beverages are used as powerful and versatile symbolic tools, to construct and manipulate the social world. Cross-cultural research reveals four main symbolic uses of alcoholic beverages:
1. As labels defining the nature of social situations or events
2. As indicators of social status
3. As statements of affiliation
4. As gender differentiators.
• There is convincing historical and contemporary evidence to show that the adoption of ‘foreign’ drinks often involves the adoption of the drinking patterns, attitudes and behaviours of the alien culture. This has nothing to do with any intrinsic properties of the beverages themselves – beer, for example, may be associated with disorderly behaviour in some cultures or sub-cultures and with benign sociability in others.
• In Europe, the influence of some ‘ambivalent’, northern, beer-drinking cultures on ‘integrated’, southern, wine-drinking cultures is increasing, and is associated with potentially detrimental changes in attitudes and behaviour (e.g. the adoption of British ‘lager-lout’ behavior among young males in Spain).
• Historical evidence suggests that attempts to curb the anti-social excesses associated with an ‘alien’ beverage through Draconian restrictions on alcohol per se may result in the association of such behavior with the formerly ‘benign’ native beverage, and an overall increase in alcohol-related problems.
• Some societies appear less susceptible to the cultural influence of alien beverages than others. Although the current ‘convergence’ of drinking patterns also involves increasing consumption of wine in formerly beer- or spirits-dominated cultures, this has so far not been accompanied by an adoption of the more harmonious behavior and attitudes associated with wine-drinking cultures. (This may in part reflect the generally higher social status of those adopting wine-drinking.)
_
Drinking-places:
• Drinking is, in all cultures, essentially a social activity, and most societies have specific, designated environments for communal drinking.
• Cross-cultural differences in the physical nature of public drinking-places reflect different attitudes towards alcohol. Positive, integrated, non-Temperance cultures tend to favour more ‘open’ drinking environments, while negative, ambivalent, Temperance cultures are associated with ‘closed’, insular designs.
• Research also reveals significant cross-cultural similarities or ‘constants’:
1. In all cultures, the drinking-place is a special environment, a separate social world with its own customs and values
2. Drinking-places tend to be socially integrative, egalitarian environments
3. The primary function of drinking-places is the facilitation of social bonding.
_
Transitional rituals:
• In all societies, alcohol plays a central role in transitional rituals – both major life-cycle events and minor, everyday transitions.
• In terms of everyday transitions, cultures (such as the US and UK) in which alcohol is only used to mark the transition from work to play – where drinking is associated with recreation and irresponsibility, and regarded as antithetical to working – tend to have higher levels of alcohol-related problems.
• Cultures in which drinking is an integral part of the normal working day, and alcohol may be used to mark the transition to work (e.g. France, Spain, Peru), tend to have lower levels of alcohol-related problems.
• Shifts away from traditional pre-work or lunchtime drinking in these cultures could be a cause for concern, as these changes can indicate a trend towards drinking patterns and attitudes associated with higher levels of alcohol-related problems.
_
Festive rituals:
• Alcohol is universally associated with celebration, and drinking is, in all cultures, an essential element of festivity.
• In societies with an ambivalent, morally charged relationship with alcohol (such as the UK, US, Scandinavia, Australia), ‘celebration’ is used as an excuse for drinking. In societies in which alcohol is a morally neutral element of normal life (such as Italy, Spain and France), alcohol is strongly associated with celebration, but celebration is not invoked as a justification for every drinking occasion.
• In cultures with a tradition of casual, everyday drinking in addition to celebratory drinking, any shifts towards the more episodic celebratory drinking of ‘ambivalent’ cultures should be viewed with concern, as these patterns are associated with higher levels of alcohol-related problems.
_
Moderate-Drinking Cultures:
1. Alcohol consumption is accepted and is governed by social custom, so that people learn constructive norms for drinking behavior.
2. The existence of good and bad styles of drinking, and the differences between them, are explicitly taught.
3. Alcohol is not seen as obviating personal control; skills for consuming alcohol responsibly are taught, and drunken misbehavior is disapproved and sanctioned.
Immoderate-Drinking Cultures:
1. Drinking is not governed by agreed-upon social standards, so that drinkers are on their own or must rely on the peer group for norms.
2. Drinking is disapproved and abstinence encouraged, leaving those who do drink without a model of social drinking to imitate; they thus have a proclivity to drink excessively.
3. Alcohol is seen as overpowering the individual’s capacity for self-management, so that drinking is in itself an excuse for excess.
__________
Alcohol and religion:
Some religious beliefs prohibit the use of alcohol, whereas others advocate drinking in moderation. For example:
• Some Christian denominations choose never to drink alcohol (Salvation Army, Methodists) where as other Christians enjoy drinking alcohol and accept it as part of God’s good creation and advocate drinking in moderation. Some use wine in Holy Communion.
• In Islam, the use of alcohol is ‘haraam’ or forbidden as it causes people to lose control over their minds and bodies.
• In Sikhism, drinking alcohol clouds the mind and damages the body, which contradicts fundamental Sikh principles.
• Judaism does not ban the use of intoxicating substances. Wine has a prominent symbolic function with the Jewish tradition; again use is one of moderation. “But there are certain occasions when Jews are permitted (indeed commanded) to drink at a level which is likely to lead to intoxication. In the Pesach or Passover celebrations, for example, Jews are commanded to drink…. and on the festival of Purim, over-drinking is jocularly encouraged” (Velleman 2002).
• Hinduism accepts moderate use of alcohol, and some Hindus abstain from alcohol use. Ugrasena the King of Mathura, on the advice of Krishna imposed ban on liquor consumption in the kingdom. That showed that the people were abusing liquor and were failing in their day to day tasks. Soma-rasa which as per description appears to have been high quality single malt has mention of praises in Rigvedas. In Hinduism, wines as medicine are documented in the ancient Indian healing system of Ayurveda. Arishthas and Asavas are fermented juices, and herbs. Ayurveda, the oldest, documented system of medicine does not recommend wine for everyone. Wine is a potent healer for specific health conditions, on the other hand drinking wine without getting a pulse diagnosis done by an Ayurvedic doctor, may work the other way around. For instance, wine is recommended in specified quantity for Kapha body types.
–Buddhists typically avoid consuming alcohol (surāmerayamajja, referring to types of intoxicating fermented beverages), as it violates the 5th of the Five Precepts, the basic Buddhist code of ethics and can disrupt mindfulness and impeded one’s progress in the Noble Eightfold Path. Buddhism, the Thai state religion, teaches that use of intoxicants should be avoided. Nonetheless, many Thai people drink alcohol, and a proportion are alcohol-dependent or hazardous or harmful drinkers.
_
Alcohol and Islam:
The all Knowing God states in the Quran: “They ask you (O Muhammad, peace be upon him) about wine and gambling. Say, in them is great sin and some benefit for people, but their sin is greater than their benefit”. More than 1400 years ago, this patrician verse had been revealed to the prophet Mohammad and undoubtedly mankind at that time had been unaware about alcohol disadvantages. According to Islam, god introduced wine as a harmful substance and expressed its disadvantages is more than benefits more than 1400 years ago in holy Quran. So that usage of wine is great sin in Islam. Until two centuries ago, harmful complications of alcohol usage were not known but holy Quran revealed it 1400 years ago.
_
Alcohol and Christianity:
With the dawn of Christianity and its gradual displacement of the previously dominant religions, the drinking attitudes and behaviors of Europe began to be influenced by the New Testament (Babor, 1986, p. 11). The earliest biblical writings after the death of Jesus (cir. A.D. 30) contain few references to alcohol. This may have reflected the fact that drunkenness was largely an upper-status vice with which Jesus had little contact (Raymond, 1927). Austin (1985) has pointed out that Jesus used wine (Matthew 15:11; Luke 7:33-35) and approved of its moderate consumption (Matthew 15:11). On the other hand, he severely attacked drunkenness (Luke 21:34,12:42; Matthew 24:45-51). However, late in the second century, several heretical sects rejected alcohol and called for abstinence. By the late fourth and early fifth centuries, the Church responded by asserting that wine was an inherently good gift of God to be used and enjoyed. While individuals may choose not to drink, to despise wine was heresy. The Church advocated its moderate use but rejected excessive or abusive use as a sin. Those individuals who could not drink in moderation were urged to abstain (Austin, 1985, pp. 44 and 47-48). It is clear that both the Old and New Testaments are clear and consistent in their condemnation of drunkenness. However, some Christians today argue that whenever “wine” was used by Jesus or praised as a gift of God, it was really grape juice; only when it caused drunkenness was it wine. Thus, they interpret the Bible as asserting that grape juice is good and that drinking it is acceptable to God but that wine is bad and that drinking it is unacceptable. This reasoning appears to be incorrect for at least two reasons. First, neither the Hebrew nor Biblical Greek word for wine can be translated or interpreted as referring to grape juice. Secondly, grape juice would quickly ferment into wine in the warm climate of the Mediterranean region without refrigeration or modern methods of preservation (Royce, 1986, pp. 55-56; Raymond, 1927, pp. 18-22; Hewitt, 1980, pp. 11-12). The spread of Christianity and of viticulture in Western Europe occurred simultaneously (Lausanne, 1969, p. 367; Sournia, 1990, p. 12). Interestingly, St. Martin of Tours (316-397) was actively engaged in both spreading the Gospel and planting vineyards (Patrick, 1952, pp. 26-27).
_
Alcoholic beverages appear in the Bible, both in usage and in poetic expression. The Bible is ambivalent toward alcohol, considering it both a blessing from God that brings merriment and a potential danger that can be unwisely and sinfully abused. Christian views on alcohol come from what the Bible says about it, along with Jewish and Christian traditions. The biblical languages have several words for alcoholic beverages, and though prohibitionists and some abstentionists dissent, there is a broad consensus that the words did ordinarily refer to intoxicating drinks. The commonness and centrality of wine in daily life in biblical times is apparent from its many positive and negative metaphorical uses throughout the Bible. Positively, wine is used as a symbol of abundance and physical blessing, for example. Negatively, wine is personified as a mocker and beer a brawler, and drinking a cup of strong wine to the dregs and getting drunk are sometimes presented as a symbol of God’s judgment and wrath. The Bible also speaks of wine in general terms as a bringer and concomitant of joy, particularly in the context of nourishment and feasting. Wine was commonly drunk at meals, and the Old Testament prescribed it for use in sacrificial rituals and festal celebrations. The Gospels record that Jesus’s first miracle was making copious amounts of wine at the wedding feast at Cana, and when he instituted the ritual of the Eucharist at the Last Supper during a Passover celebration, he says that the wine is a “New Covenant in [his] blood,” though Christians have differed on the implications of this statement. Alcohol was also used for medicinal purposes in biblical times, and it appears in that context in several passages—as an oral anesthetic, a topical cleanser and soother, and a digestive aid.
_
Christian views on alcohol are varied. Throughout the first 1,800 years of church history, Christians consumed alcoholic beverages as a common part of everyday life and used “the fruit of the vine” in their central rite—the Eucharist or Last Supper. They held that both the Bible and Christian tradition taught that alcohol is a gift from God that makes life more joyous, but that over-indulgence leading to drunkenness is sinful or at least a vice. In the mid-19th century, some Protestant Christians moved from this historic position of allowing moderate use of alcohol (sometimes called moderationism) to either deciding that not imbibing was wisest in the present circumstances (abstentionism) or prohibiting all ordinary consumption of alcohol because it was believed to be a sin (prohibitionism). Today, all three of these positions exist in Christianity, but the historic position remains the most common worldwide, due to the adherence by the largest bodies of Christians including Anglicanism, Catholicism, and Orthodoxy. A majority of Evangelical leaders worldwide (52%) reject alcohol as incompatible with being a good Evangelical, ranging from 83% of Evangelical leaders within India/Nepal to still 42% of Evangelical leaders within nominally “Christian” countries. Today, the views on alcohol in Christianity can be divided into moderationism, abstentionism, and prohibitionism. Abstentionists and prohibitionists are sometimes lumped together as “teetotalers” and share some similar arguments for their positions, but the distinction between them is that the latter abstain from alcohol as a matter of law (that is, they believe God requires abstinence in all ordinary circumstances), while the former abstain as a matter of prudence (that is, they believe total abstinence is the wisest and most loving way to live in the present circumstances). Some groups of Christians fall entirely or virtually entirely into one of these categories, while others are divided between them. Evangelicals in Asia, Africa, and also in Muslim-majority countries are decidedly against drinking. 83% of Evangelical leaders in the region of India and Nepal say consuming alcohol is incompatible with being a good Evangelical. Roman Catholics in Kerala, India have also launched a major anti-drinking campaign, with a ban on drinking by church workers, alcohol consumption being a sin which must be confessed, also calling for prohibition of alcohol by the state.
_
Research has been conducted by social scientists and epidemiologists to see if potential links exist between religiosity and alcoholism. Cahalan and Room (1972) study of 2,746 adults found that more abstainers than infrequent, moderate, or heavy drinkers participated in church activities.
___________
Alcohol and military:
The Cavalier poet Richard Lovelace testifies to the connection between military life and alcohol.
Let others glory follow
In their false riches wallow
And in their grief be merry,
Leave me but love and sherry.
_
In peacetime alcohol helped blur the boredom of barracks life. British soldiers often drank themselves into insensibility in the ‘wet canteen’. As the 19th century went on reformers helped institute libraries and day rooms where tea and lemonade presented less risk, and the Army Temperance Society encouraged total abstinence. Officers and men on lonely garrison duty were especially vulnerable. The future Union general, Grant, fell victim to drink in the Pacific Northwest, while in the Caucasus Lermontov’s character Capt Maxim Maximich, drawn from life, warned: ‘I’ve gone a whole year without seeing a soul, and if you once take to drinking vodka, you’re done.’ Drink also played its part in the bonding process. Anglo-Saxon warriors boasted over their drinking-horns about the deeds they would perform in battle; Capt Stuart Mawson noted ‘a subtle parade of manhood, an unconscious swagger in the manner of drinking’ the night before his battalion dropped on Arnhem in 1944, and Samuel Janney recalled how a night’s drinking with his new platoon in Vietnam ‘definitely initiated me’. But alcohol has played a more spectacular part on the battlefield. British soldiers campaigning in the Low Countries in the 16th century were so impressed by the effects of a nip of genever as to coin the expression ‘Dutch courage’. British civil war armies were well aware of it. In 1643 the parliamentarian governor of Gloucester was reported to give raiding parties ‘as much wine and strong waters as they desired’, and at Preston in 1648 Capt John Hodgson’s men had martial zeal revived by ‘a pint of strong waters among several of us’. The two French divisions which attacked the Pratzen plateau at Austerlitz in 1805 had received a triple ration of brandy—nearly half a pint—per man: small wonder that they were reported to ‘burst with eagerness and enthusiasm’. Drinking helped calm pre-battle nerves. While the forlorn hope waited to assault Badajoz in 1812, Maj O’Hare of the 95th Regiment confided to Capt Jones of the 52nd that he felt depressed. ‘Tut, tut man!’ replied Jones. ‘I have the same sort of feeling, but keep it down with a drop of the cratur’, and passed his calabash. As they endured filthy weather the night before Waterloo, the British drank what they could. A footguards officer reported that with plenty of gin he was ‘wet and comfortable’, while the formidable prize-fighter Cpl John Shaw of the Life Guards rather overdid things and was killed the following day, fighting drunk, after hewing down several Frenchmen. Jack Vahey, regimental butcher of the 17th Lancers, spent the night before Balaclava in 1854 under guard because of over-indulging in commissariat rum, but the next morning he took part in the Charge of the Light Brigade in his bloody overalls, wielding an axe. The British army issued rum in both world wars. Brig Gen James Jack argued that it was ‘in no sense a battle dope’. It helped men endure the misery of the trenches: an officer told the 1922 War Office shell shock Committee that he did not think the war could have been won without it. Col W. N. Nicholson agreed that rum made life more bearable, but thought that it also blunted the impact of battle and aided recovery from its shock. ‘It is an urgent devil to the Highlander before action, ’ he wrote, ‘[and] a solace to the East Anglian countryman after the fight.’ Rudolf Binding guessed that 50, 000 Germans were the worse for captured drink during the offensive of March 1918, and Stephen Westmann complained that the attack was delayed ‘not for lack of German fighting spirit, but on account of the abundance of Scottish drinking spirit’. There was a similar pattern in WW II. John Horsfall, an officer in an Irish regiment, acknowledges that ‘We simply kept going on rum. Eventually it became unthinkable to go into action without it.’ Maj Martin Lindsay of the Gordon Highlanders saw some of his comrades get ‘well rummed-up’ and leave for an attack ‘in a state bordering on hilarity’. A German infantryman said that ‘There’s as much vodka, schnapps and Terek liquor on the [Eastern] front as there are Paks [anti-tank guns] … Vodka purges the brain and expands the strength.’ Alcohol was often home-made. Aqua-Velva aftershave could be mixed with orange juice to make a Tom Collins, and in both Italy and the Pacific copper piping from crashed aircraft was used by American soldiers to make stills for ‘raisin jack’ or ‘swipe’. Alcohol has played its part in promoting fighting spirit, but it is far from risk-free. It can inhibit clear thought. The royalist Capt ‘Wicked Will’ Hodgkins launched a successful raid on the parliamentarians but ‘was so loaded with drink that he fell off by the way’, and a parliamentarian gunner in the Lostwithiel campaign of 1644 was too drunk to reload his piece. It may provoke fighting frenzy, but is incompatible with the use of the sophisticated equipment: it was for this reason that the Royal Navy discontinued its rum ration. Lastly, exultation is followed by drop-off, and the combination of exhaustion and hangover is an unenviable one. Yet alcohol is not without merits. Lt Col Alan Hanbury-Sparrow, an infantry officer on the western front, admitted: ‘Certainly strong drink saved you. For the whole of your moral forces were exhausted. Sleep alone could restore them, and sleep, thanks to this blessed alcohol, you got.’ Cdr Rick Jolly, a medical officer in the Falklands war, noted that ‘the traditional use of alcohol’ helped stressed men sleep. There seems no sign that armed forces’ thirst for alcohol has disappeared. If there was little of it in the Gulf war it was because of a rigid Saudi Arabian policy of prohibition, while in the (former) Yugoslavia there have been many painful confrontations between tender constitutions and local slivovitz.
_
British armed forces suffer record levels of alcohol abuse in 2013:
Record levels of alcohol abuse in Britain’s armed forces have led to more than 1,600 service personnel – the equivalent of several infantry battalions – requiring medical treatment in the past year. New figures obtained from the Ministry of Defense (MoD) under Freedom of Information laws show that the number of service personnel falling victim to alcohol abuse is at its highest since incidents first began to be collected centrally by the Defense Medical Information Capability Program in 2007. Heart problems, alcohol poisoning, liver disease and alcoholic psychosis are among the conditions which the system records. And the numbers needing medical help for drink-related problems soared by 28 per cent between 2012 and 2013. It is a marked escalation on previous years, with 2011 and 2012 seeing year on year rises of 5 per cent and 4 per cent respectively.
____________
Alcohol and animals: Do animals like alcohol?
Vervet monkeys are one species that researchers hoped could help answer this question. Sometimes called green monkeys, they are native to Africa, but a handful of isolated groups wound up scattered across islands in the Caribbean. In the 18th and 19th Centuries, slavers often took the monkeys as pets, and when their ships landed in the new world, the monkeys easily escaped or were intentionally released. There, free of most of their predators, the small primates adapted quite well to tropical island life. For 300 years, the animals lived in an environment dominated by sugar cane plantations. And when the sugar cane was burned, or occasionally fermented before harvest, it became a treat for the monkeys. As they became accustomed to the ethanol in the fermented cane juice, the monkeys may have developed both a taste and tolerance for alcohol. Local stories are told of catching wild monkeys by supplying them with a mixture of rum and molasses in hollowed out coconut shells. The drunk primates could then be captured without hassle. Descendants of those introduced monkeys have since been studied so that we can understand more about their boozy behavior. One study found that nearly one in five monkeys preferred a cocktail of alcohol mixed with sugar water over a sip of sugar water alone. Intriguingly, younger individuals were more likely to drink than older individuals, and most of the drinking was done by teenagers of both sexes. The researchers, led by Jorge Juarez of Universidad Nacional Autonoma de Mexico, suspect that older monkeys shun alcohol because of the stresses of monkey politics. “It is [possible] that adults drink less because they have to be more alert and perceptive of the social dynamics of the group.” In other words, at some point the monkeys leave their days of heavy drinking and hangovers behind and start acting like adults.
_
The figure below shows drunken monkey:
_
A search of the scientific literature supported the notion that elephants could at least become drunk. A 1984 study showed that they were happy to drink up a 7% alcohol solution, and several drank enough to alter their behaviour. While they didn’t “act drunk”, in human terms, they decreased the time spent feeding, drinking, bathing, and exploring, and became more lethargic. Several displayed behaviours that indicated they were uncomfortable, or perhaps slightly ill. But just because elephants can become intoxicated doesn’t mean that they do it in the wild routinely enough to inspire all the marula tree legends. A 3,000kg (6,600lb) elephant would have to drink between 10 and 27 liters of a 7% alcohol solution in a relatively short amount of time to experience any overt behavioural changes. Even if marula fruit contained 3% ethanol (a generous estimate) an elephant eating only marula fruits at a normal pace would barely consume half the alcohol necessary in a single day to become drunk. If it wanted to get drunk, given the constraints of its anatomy and physiology, an elephant would have to eat marula fruit at 400% its normal feeding rate while also eschewing all additional water intake. “On our analysis,” the researchers conclude, “this seems extremely unlikely.”
_________
Chemistry of alcohol:
Alcohol is any of a class of organic compounds characterized by one or more hydroxyl (−OH) groups attached to a carbon atom of an alkyl group (hydrocarbon chain). Alcohols may be considered as organic derivatives of water (H2O) in which one of the hydrogen atoms has been replaced by an alkyl group, typically represented by R in organic structures. For example, in ethanol (or ethyl alcohol) the alkyl group is the ethyl group, −CH2CH3. An important class of alcohols is the simple acyclic alcohols; the general formula for which is is CnH2n+1OH. Of these ethanol (C2H5OH) is the alcohol found in alcoholic beverages; in common speech the word alcohol refers to ethanol. Other alcohols are usually described with a clarifying adjective, as in isopropyl alcohol (propanol) or wood alcohol (methyl alcohol, or methanol). In everyday life “alcohol” without qualification usually refers to ethanol, or a beverage based on ethanol.
_
_
Alcohol, any of a class of organic compounds with the general formula R-OH, where R represents an alkyl group made up of carbon and hydrogen in various proportions and -OH represents one or more hydroxyl groups. In common usage the term alcohol usually refers to ethanol. The class of alcohols also includes methanol; the amyl, butyl, and propyl alcohols; the glycols; and glycerol. An alcohol is generally classified by the number of hydroxyl groups in its molecule. An alcohol that has one hydroxyl group is called monohydric; monohydric alcohols include methanol, ethanol, and isopropanol. Glycols have two hydroxyl groups in their molecules and so are dihydric. Glycerol, with three hydroxyl groups, is trihydric. The monohydric alcohols are further classified as as primary (RCH2OH), secondary (R2CHOH), or tertiary (R3COH) according to the number of carbon atoms bonded to the carbon atom to which the hydroxyl group is bonded. Alcohols can also be characterized by the molecular configuration of the hydrocarbon portion (aliphatic, cyclic, heterocyclic, or unsaturated). Oxidation of primary alcohols produces aldehydes (RCHO) and carboxylic acids (RCO2H); oxidation of secondary alcohols yields ketones (RCOR′). Dehydration of alcohols produces alkenes and ethers (ROR). Reaction of alcohols with carboxylic acids results in the formation of esters (ROCOR′), a reaction of great industrial importance. The hydroxyl group of an alcohol is readily replaced by halogens or pseudohalogens.
_
Ethanol also called ethyl alcohol, pure alcohol, beverage alcohol, or drinking alcohol, is a volatile, flammable, colorless liquid with the structural formula CH3CH2OH, often abbreviated as C2H5OH or C2H6O. Ethanol is a psychoactive drug and is one of the oldest recreational drugs still used by humans. Ethanol can cause alcohol intoxication when consumed. Best known as the type of alcohol found in alcoholic beverages, it is also used in thermometers, as a solvent, and as a fuel. In common usage, it is often referred to simply as alcohol or spirits. The anesthetic ether is also made from ethanol. Alcohols are among the most common organic compounds. They are used as sweeteners and in making perfumes, are valuable intermediates in the synthesis of other compounds, and are among the most abundantly produced organic chemicals in industry. Perhaps the two best-known alcohols are ethanol and methanol (or methyl alcohol). Methanol is used as solvent, as a raw material for the manufacture of formaldehyde and special resins, in special fuels, in antifreeze, and for cleaning metals.
_
Nomenclature:
As with other types of organic compounds, alcohols are named by both formal and common systems. The most generally applicable system is that adopted at a meeting of the International Union of Pure and Applied Chemistry (IUPAC) in Paris in 1957. In the IUPAC system, the name of the alkane chain loses the terminal “e” and adds “ol”, e.g., “methanol” and “ethanol”. When necessary, the position of the hydroxyl group is indicated by a number between the alkane name and the “ol”: propan-1-ol for CH3CH2CH2OH, propan-2-ol for CH3CH(OH)CH3. Sometimes, the position number is written before the IUPAC name: 1-propanol and 2-propanol. If a higher priority group is present (such as an aldehyde, ketone, or carboxylic acid), then it is necessary to use the prefix “hydroxy”, for example: 1-hydroxy-2-propanone (CH3COCH2OH). The IUPAC nomenclature is used in scientific publications and where precise identification of the substance is important. In other less formal contexts, an alcohol is often called with the name of the corresponding alkyl group followed by the word “alcohol”, e.g., methyl alcohol, ethyl alcohol. Propyl alcohol may be n-propyl alcohol or isopropyl alcohol, depending on whether the hydroxyl group is bonded to the 1st or 2nd carbon on the propane chain. Alcohols are classified into 0°, primary (1°), secondary (2°); also italic abbreviated sec- or just s-, and tertiary (3°); also italic abbreviated tert- or just t-, based upon the number of carbon atoms connected to the carbon atom that bears the hydroxyl (OH) functional group. The primary alcohols have general formulas RCH2OH; secondary ones are RR’CHOH; and tertiary ones are RR’R”COH, where R, R’, and R” stand for alkyl groups. Methanol (C H3O H or CH4O) is a 0° alcohol. Some sources include methanol as a primary alcohol, including the 1911 edition of the Encyclopedia Britannica, but this interpretation is less common in modern texts.
_
Common names:
| Chemical Formula | IUPAC Name | Common Name |
| CH3OH | Methanol | Wood alcohol |
| C2H5OH | Ethanol | Alcohol |
| C3H7OH | Isopropyl alcohol | Rubbing alcohol |
| C4H9OH | Butyl alcohol | Butanol |
| C5H11OH | Pentanol | Amyl alcohol |
| C16H33OH | Hexadecan-1-ol | Cetyl alcohol |
_
Structure of Alcohols:
The structure of an alcohol resembles that of water as seen in the figure below. Water and alcohols have similar properties because water molecules contain hydroxyl groups that can form hydrogen bonds with other water molecules and with alcohol molecules, and likewise alcohol molecules can form hydrogen bonds with other alcohol molecules as well as with water. Many of the properties and reactions characteristic of alcohols are due to the electron charge distribution in the C-O-H portion of the molecule. With both alcohol and water, the bond angles reflect the effect of electron repulsion and increasing steric bulk of the substituents on the central oxygen. The oxygen atom of the strongly polarized O−H bond of an alcohol pulls electron density away from the hydrogen atom. The electronegativity of oxygen contributes to the unsymmetrical distribution of charge, creating a partial positive charge on the hydrogen and a partial negative charge on the oxygen. This uneven distribution of electron density in the O-H bond creates a dipole. This polarized hydrogen, which bears a partial positive charge, can form a hydrogen bond with a pair of nonbonding electrons on another oxygen atom. Hydrogen bonds, with strength of about 5 kilocalories (21 kilojoules) per mole, are much weaker than normal covalent bonds, with bond energies of about 70 to 110 kilocalories per mole. (The amount of energy per mole that is required to break a given bond is called its bond energy.)
_
_
Physical and chemical properties:
Most of the common alcohols are colourless liquids at room temperature. Methyl alcohol, ethyl alcohol, and isopropyl alcohol are free-flowing liquids with fruity odours. The higher alcohols—those containing 4 to 10 carbon atoms—are somewhat viscous, or oily, and they have heavier fruity odours. Some of the highly branched alcohols and many alcohols containing more than 12 carbon atoms are solids at room temperature. Ethanol has a slightly sweeter (or more fruit-like) odor than the other alcohols. In general, the hydroxyl group makes the alcohol molecule polar. Those groups can form hydrogen bonds to one another and to other compounds (except in certain large molecules where the hydroxyl is protected by steric hindrance of adjacent groups). This hydrogen bonding means that alcohols can be used as protic solvents. Two opposing solubility trends in alcohols are: the tendency of the polar OH to promote solubility in water, and the tendency of the carbon chain to resist it. Thus, methanol, ethanol, and propanol are miscible in water because the hydroxyl group wins out over the short carbon chain. Butanol, with a four-carbon chain, is moderately soluble because of a balance between the two trends. Alcohols of five or more carbons (pentanol and higher) are effectively insoluble in water because of the hydrocarbon chain’s dominance. All simple alcohols are miscible in organic solvents. Because of hydrogen bonding, alcohols tend to have higher boiling points than comparable hydrocarbons and ethers. The boiling point of the alcohol ethanol is 78.29 °C, compared to 69 °C for the hydrocarbon hexane (a common constituent of gasoline), and 34.6 °C for diethyl ether. Alcohols, like water, can show either acidic or basic properties at the -OH group. With a pKa of around 16-19, they are, in general, slightly weaker acids than water, but they are still able to react with strong bases such as sodium hydride or reactive metals such as sodium. The salts that result are called alkoxides, with the general formula RO- M+. Meanwhile, the oxygen atom has lone pairs of nonbonded electrons that render it weakly basic in the presence of strong acids such as sulfuric acid. Alcohols can also undergo oxidation to give aldehydes, ketones, or carboxylic acids, or they can be dehydrated to alkenes. They can react to form ester compounds, and they can (if activated first) undergo nucleophilic substitution reactions. The lone pair of electrons on the oxygen of the hydroxyl group also makes alcohols nucleophiles. As one moves from primary to secondary to tertiary alcohols with the same backbone, the hydrogen bond strength, the boiling point, and the acidity typically decrease.
___
Grades of ethanol:
Ethanol is available in a range of purities that result from its production or, in the case of denatured alcohol, are introduced intentionally.
Denatured alcohol:
Pure ethanol and alcoholic beverages are heavily taxed as psychoactive drugs, but ethanol has many uses that do not involve consumption by humans. To relieve the tax burden on these uses, most jurisdictions waive the tax when an agent has been added to the ethanol to render it unfit to drink. These include bittering agents such as denatonium benzoate and toxins such as methanol, naphtha, and pyridine. Products of this kind are called denatured alcohol.
Absolute alcohol:
Absolute or anhydrous alcohol refers to ethanol with a low water content. There are various grades with maximum water contents ranging from 1% to a few parts per million (ppm) levels. Absolute alcohol is not intended for human consumption. If azeotropic distillation is used to remove water, it will contain trace amounts of the material separation agent (e.g. benzene). Absolute ethanol is used as a solvent for laboratory and industrial applications, where water will react with other chemicals, and as fuel alcohol. Spectroscopic ethanol is an absolute ethanol with a low absorbance in ultraviolet and visible light, fit for use as a solvent in ultraviolet-visible spectroscopy. Pure ethanol is classed as 200 proof in the U.S., equivalent to 175 degrees proof in the UK system.
Rectified spirit:
Rectified spirit, also called “neutral grain spirit,” is alcohol which has been purified by means of “rectification” (i.e., repeated distillation). The term “neutral” refers to the spirit’s lacking the flavor that would have been present if the mash ingredients had been distilled to a lower level of alcoholic purity. Rectified spirit also lacks any flavoring added to it after distillation (as is done, for example, with gin). Other kinds of spirits, such as whiskey, are distilled to a lower alcohol percentage in order to preserve the flavor of the mash. Rectified spirit is a clear, colorless, flammable liquid that may contain as much as 95% ABV. It is often used for medicinal purposes. It may be a grain spirit or it may be made from other plants. It is used in mixed drinks, liqueurs, and tinctures, but also as a household solvent.
_______
Alcohol quantification: Measurement of Alcohol Strength:
There are several methods of measuring the alcohol contents of various beverages.
_
Specific gravity is the ratio of the density of a sample to the density of water. The ratio depends on the temperature and pressure of both the sample and water. Specific Gravity of ethanol is 0.79 –It is approximately 0.8, that means 1 ml of absolute alcohol weigh 0.8 grams. In other words, 1 gram of absolute alcohol is 1.25 ml of absolute alcohol.
_
Chemically alcohols are compounds with the general formula CnH (2n+1) OH. The alcohol in alcoholic beverages is ethyl alcohol (ethanol, C2H5OH); pure ethyl alcohol is also known as absolute alcohol. The energy yield of alcohol is 7 kcal (29 kJ)/gram. The strength of alcoholic beverages is most often shown as the percentage of alcohol by volume (sometimes shown as % v/v or % ABV). This is not the same as the percentage of alcohol by weight (% w/v) since alcohol is less dense than water: 5% v/v alcohol = 3.96% by weight (w/v); 10% v/v = 7.93% w/v and 40% v/v = 31.7% w/v.
_
ABV – Alcohol by Volume – It simply represents the amount of volume consumed by ethanol compared to the entire volume of the drink. It is expressed as a percentage. 40 % ABV means 40ml of absolute alcohol in 100 ml of beverage (40 % v/v).
_
Proof – This term is used among the strongest spirits. To compute liquor’s proof you simply multiply the ABV by 2. The theoretic highest possible strength of any drink is therefore 200-proof. In reality though the maximum for distilled spirits is 191-proof because not all of the water can be distilled from ethanol. 40 % ABV whisky (40 % v/v) is 80-proof.
_
ABW – Alcohol by Weight – This is similar to ABV but instead of the volume consumed by the ethanol its mass is used instead. 30 % ABW whisky means 30 gm of absolute alcohol in 100 ml of beverage. Beer brewers often used this measurement in states that require limits on strength of beer sold in food markets (for example 3.2 beer in Oklahoma). This is preferred over ABV in these cases because the ABW is roughly 80% of the ABV. Beer that is 4% alcohol by volume can be sold and still meet the 3.2 ABW limit.
__
Standard drink:
A standard drink is a notional drink that contains a specified amount of pure alcohol (ethanol). The standard drink is used in many countries to quantify alcohol intake. It is usually expressed as a certain measure of beer, wine, or spirits. One standard drink always contains the same amount of alcohol regardless of the container size or the type of alcoholic beverage, but does not necessarily correspond to the typical serving size in the country in which it is served. The standard drink varies significantly from country to country. For example, it is 10 grams (12.7 ml) of alcohol in Australia and New Zealand; in Japan it is 25 ml (19.75 grams). In the United Kingdom the term “standard drink” is not officially defined; instead a unit of alcohol is defined as 10 ml. The number of units in a typical serving is printed on bottles; the advent of smart phones has led to the creation of apps which report the number of units contained in an alcoholic drink. The system is intended to inform people how much alcohol they drink, not to determine serving sizes. Typical servings deliver 1–3 units. In the United States the standard drink contains 0.6 US fluid ounces (18 ml) of alcohol which corresponds to 14 gm absolute alcohol. This is approximately the amount of alcohol in a 12-US-fluid-ounce (350 ml) glass of 5% ABV beer, a 5-US-fluid-ounce (150 ml) glass of 12% ABV wine, or a 1.5-US-fluid-ounce (44 ml) glass of a 40% ABV (80 proof) spirit.
_
The figure below denotes one standard drink in the U.S.containing 18 ml or 14 gm of absolute alcohol:
_
_
A peg is an informal unit of measurement of alcoholic spirits. Peg measures for use in preparing alcoholic drinks can hold anywhere from 1 to 2 fluid ounces (30-60 ml). In some jurisdictions the “peg” is a standardized measure.1 peg is 30ml, 1 large peg is 60ml and 1 extra large peg is 90ml.
One peg =1unit=30ml of 40% whiskey/rum/gin/vodka = 12 ml alcohol = 10 gm alcohol
_
Alcohol equivalence:
Alcohol equivalence is a system of standard drink sizes of various alcoholic beverages. The amount of alcohol (i.e., ethanol) that is contained in a standard drink varies widely by country. In New Zealand one standard drink, as defined by the Alcohol Advisory Council, contains 10 grams of ethyl alcohol which is approximately 12.7 ml. This is approximately “a 330ml can of beer or a 100ml glass of table wine or a 30ml glass of straight spirits”. In the UK, one standard drink or “unit” of alcohol is defined as 10ml or 8g of pure alcohol. This equals one 25ml single measure of spirits,(ABV 40%), or a third of a pint of beer (ABV 5-6%), or half a standard (175ml) glass of red wine (ABV 12%). These beverages also have additional components known as congeners that affect the drink’s taste and might contribute to adverse effects on the body. Congeners include methanol, butanol, acetaldehyde, histamine, tannins, iron, and lead. (Vide infra)
_
Standard drinks as defined by various countries:
The amount of alcohol is stated in the table below in both grams and milliliters.
| Country | Mass (g) | Volume (ml) |
| Australia | 10 | 12.67 |
| Austria | 6 | 7.62 |
| Canada | 13.6 | 17.2 |
| Denmar | 12 | 15.2 |
| Finland | 12 | 15.2 |
| France | 12 | 15.2 |
| Hungary | 17 | 21.5 |
| Iceland | 8 | 10 |
| Ireland | 10 | 12.7 |
| Italy | 10 | 12.7 |
| Japan | 19.75 | 25 |
| Netherlands | 9.9 | 12.5 |
| New Zealand | 10 | 12.7 |
| Poland | 10 | 12.7 |
| Portugal | 14 | 17.7 |
| Spain | 10 | 12.7 |
| UK (unit) | 7.9 | 10 |
| USA | 14 | 17.7 |
| India | 10 | 12.7 |
___
___
I have made a chart of standard drink in various countries:
| DifferentCountries | Absolute Alcohol by weight | Absolute Alcohol by volume | Beer 5% ABV (v/v) | Wine 10% ABV (v/v) | Liquor 40 % ABV (v/v) |
| USA | 14 gm | 18ml | 360 ml | 180 ml | 45 ml |
| UK | 8 gm | 10 ml | 200 ml | 100 ml | 25 ml |
| New Zealand | 10 gm | 12.8 ml | 256 ml | 128 ml | 32 ml |
_
Importance of alcohol equivalence:
The health benefits associated with drinking in moderation are also similar for beer, wine and spirits. The primary factor associated with health and longevity appears to be the alcohol itself. Knowing about this alcohol equivalence can help us drink sensibly and in moderation. In the words of the American Dietetic Association, “Knowing the facts of beverage alcohol equivalence is a crucial aspect of responsible drinking.” For example, people won’t be fooled by the myth that drinking “hard liquor” leads more quickly to intoxication than other alcoholic beverages. Understanding alcohol equivalence prevents us from being fooled into thinking that “just having a few of beers” before driving is safer than having a few glasses of dinner wine or a few shots of whiskey or Martinis. Being aware of alcohol equivalence can help us avoid driving while impaired or intoxicated. That can prevent us from having trouble with the law, but much more important, it can prevent injuries and save lives. Knowing about alcohol equivalence also helps us understand that there is no drink of moderation, only behaviors of moderation. In a poll of physicians, 95% said it is important that people understand the alcohol equivalence of standard drinks and 98% believe it important for doctors to communicate this and other information about alcohol consumption. The research was conducted by the American Medical Women’s Association, the oldest and largest multi-specialty association of women physicians in the world. Dr. Raymond Scaletter, former Chairman (i.e., head or president) of the American Medical Association says “Incorporating standard drink information into routine examinations will help to reinforce moderation in those who drink and to identify problems associated with alcohol abuse.” The medical leader says that it’s important for doctors to “reinforce moderate and responsible drinking.
____
Shape of glass:
The shape of a glass can have a significant effect on how much one pours. A Cornell University study of students and bartenders’ pouring showed both groups pour more into short, wide glasses than into tall, slender glasses. Aiming to pour one shot of alcohol (1.5 ounces or 44.3 ml), students on average poured 45.5 ml & 59.6 ml (30% more) respectively into the tall and short glasses. The bartenders scored similarly, on average pouring 20.5% more into the short glasses. More experienced bartenders were more accurate, pouring 10.3% less alcohol than less experienced bartenders. Practice reduced the tendency of both groups to over pour for tall, slender glasses but not for short, wide glasses. These misperceptions are attributed to two perceptual biases: (1) Estimating that tall, slender glasses have more volume than shorter, wider glasses; and (2) Over focusing on the height of the liquid and disregarding the width. To avoid overpouring, use tall, narrow glasses or ones on which the alcohol level is pre-marked. To avoid underestimating the amount of alcohol consumed, studies using self reports of standard drinks should ask about the shape of the glass.
____________
Alcohol production:
Ethyl alcohol is derived from two main processes, hydration of ethylene and fermentation of sugars. Hydration of ethylene is the primary method for the industrial production of ethyl alcohol, while fermentation is the primary method for production of beverage alcohol.
_
Beverage alcohol production through fermentation:
Alcoholic fermentation, also referred to as ethanol fermentation, is a biological process in which sugars such as glucose, fructose, and sucrose are converted into cellular energy and thereby produce ethanol and carbon dioxide as metabolic waste products. Because yeasts perform this conversion in the absence of oxygen, alcoholic fermentation is considered an anaerobic process. Alcoholic fermentation occurs in the production of alcoholic beverages and ethanol fuel, and in the rising of bread dough. Primary process is fermentation using glucose produced from sugar from the hydrolysis of starch, in the presence of yeast and temperature of less than 37 °C to produce ethanol. For instance, such a process might proceed by the conversion of sucrose by the enzyme invertase into glucose and fructose, then the conversion of glucose by the enzyme zymase into ethanol (and carbon dioxide). Ethyl alcohol is actually a by-product of yeast metabolism. Yeast is a fungus that feeds on carbohydrates. Yeasts are present ubiquitously. For example, the white waxy surface of a grape is almost entirely composed of yeast. When, for example, the skin of a berry is broken, the yeast acts quickly and releases an enzyme that, under anaerobic conditions, converts the sugar (sucrose, C12H22O11) in the berry into carbon dioxide (CO2) and alcohol (C2H5OH). This process is known as fermentation (if the mixture is not protected from air, alcohol turns into acetic acid, producing vinegar). When cereal grains and potatoes are used, each requires a sprouting pretreatment (malting) to hydrolyze starch, during which diastase enzymes are produced that break down starches to simple sugars that the yeast, which lacks these enzymes, can anaerobically convert to alcohol. This process makes the sugar available for the fermentation process. The yeast then continues to feed on the sugar until it literally dies of acute alcohol intoxication. Because yeast expires when the alcohol concentration reaches 12 to 15 percent, natural fermentation stops at this point. In beer, which is made of barley, rice, corn, and other cereals, the fermentation process is artificially halted somewhere between 3 and 6 percent alcohol. Table wine contains between 10 and 14 percent alcohol, the limit of yeast’s alcohol tolerance. This amount is insufficient for complete preservation, and thus a mild pasteurization is applied. All beverage alcohol and much of that used in industry is formed through fermentation of a variety of products including grain such as corn, potato mashes, fruit juices, and beet and cane sugar molasses. (In earlier years, until about 1947, the largest proportion of the production of industrial alcohol was from fermentation, but the hydration of ethylene now provides the greatest source of industrial alcohol). Fermentation can be defined as an enzymatically anaerobic controlled transformation of an organic compound. With respect to alcohol, we are referring to the conversion of sugars to ethanol by microscopic yeasts in the absence of oxygen.
_
Fermentation does not require oxygen. If oxygen is present, some species of yeast (e.g., Kluyveromyces lactis or Kluyveromyces lipolytica) will oxidize pyruvate completely to carbon dioxide and water. This process is called cellular respiration. But these species of yeast will produce ethanol only in an anaerobic environment (not cellular respiration). However, many yeasts such as the commonly used baker’s yeast Saccharomyces cerevisiae, or fission yeast Schizosaccharomyces pombe, prefer fermentation to respiration. These yeasts will produce ethanol even under aerobic conditions, if they are provided with the right kind of nutrition. All organisms will generate energy in the most efficient manner possible. In the case of yeasts, the key condition is not the presence of oxygen – all yeast are either aerobic or facultative anaerobes. When oxygen is present, many yeasts will still use fermentation to generate energy if there is sufficient sugar present. With high concentrations of sugar, it is more efficient for them to use fermentation. Fermentation is biochemically faster than aerobic respiration and cells can use their entire cytoplasm as a location for fermentation while aerobic respiration can only be complete in the mitochondria. When sugar levels are low, they must gain the maximum energy per sugar and so fermentation decreases and aerobic respiration increases. The mechanism for this metabolic change is not known but it is consistently seem with many species.
_
Sucrose is a dimer of glucose and fructose molecules. In the first step of alcoholic fermentation, the enzyme invertase cleaves the glycosidic linkage between the glucose and fructose molecules.
C12H22O11 + H2O + invertase → 2 C6H12O6
_
The figure below uses a symbolic notation familiar in biochemistry. It shows the stepwise transformation of glucose to ethanol through intermediates, pyruvate and acetaldehyde.
_
_
_
The initial fermentation mixture contains approximately 3 to 5% ethanol such as in beer and up to 12 to 15% ethanol as in wine and sherry. Higher concentrations of ethanol cannot be achieved by fermentation, because the yeast becomes inactivated. In this case distillation is required to generate higher alcohol concentrations. Dry wines result when nearly all the available sugar is fermented. Sweet wines still have unfermented sugar. Pure alcohol also is added to fortify wines such as port and sherry. This addition boosts their percentage of alcohol to 18 or 20 percent (such wines do not require further pasteurization). “Still wines” are bottled after complete fermentation takes place. Sparkling wines are bottled before fermentation is complete so that the formed CO2 is retained. “White” wines are made only from the juice of the grapes; “reds” contain both the juice and pigments from skins. Two other alcohols that are relatively widely used (though not as much as methanol and ethanol) are propanol and butanol. Like ethanol, they are produced by fermentation processes. (However, the fermenting agent is the bacterium Clostridium acetobutylicum, which feeds on cellulose, not sugars like the Saccharomyces yeast that produces ethanol.)
_
Distillation: Distilled beverage and hard liquor:
The Chinese were distilling a beverage from rice by 800 BC. The Romans apparently produced a distilled beverage, although no references are found in writings before AD100. Archaeological evidence indicates that actual distillation of beverages began in the Jin (1115 – 1234) and Southern Song (1127-1279) dynasties. The earliest evidence of the distillation of alcohol (in Europe) comes from the School of Salerno in southern Italy in the 12th century. Distillation, which was also discovered about 800 C.E.in Arabia, is the man-made process designed to take over where the vulnerable yeast fungus leaves off. Distillation is a process that uses differences in boiling points to separate compounds. In the case of alcohol and particularly ethanol, knowledge that the boiling point of pure water is 100C, while that of ethanol is 78.3C allows the separation of the ethanol from the water by adjusting the distillation temperature to a point higher than that for ethanol, but lower than that for water. Thus, the concentration of ethanol can be enhanced by removing it as a distillate from the ethanol-water solution. A distilled beverage, spirit, or liquor is an alcoholic beverage produced by distilling (i.e., concentrating by distillation) ethanol produced by means of fermenting grain, fruit, or vegetables. Unsweetened, distilled, alcoholic beverages that have an alcohol content of at least 20% ABV are called spirits. For the most common distilled beverages, such as whisky and vodka, the alcohol content is around 40%. The term hard liquor is used in North America to distinguish distilled beverages from undistilled ones (implicitly weaker). Vodka, gin, baijiu, tequila, whiskey, brandy, and soju are examples of distilled beverages. Distilling concentrates the alcohol and eliminates some of the congeners. The distillation procedure also allows for the concentration of components of the beverage which provide some distinctive flavor. The distilled, or hard liquors, including brandy, gin, whiskey, scotch, bourbon, rum, and vodka, contain between 40 and 75 percent pure alcohol. This does not include beverages such as beer, wine, and cider, as they are fermented but not distilled having relatively low alcohol content, typically less than 10%.
_
Brewing:
Brewing is the production of beer through steeping a starch source (commonly cereal grains) in water and then fermenting with yeast. It is done in a brewery by a brewer, and the brewing industry is part of most western economies. Brewing has taken place since around the 6th millennium BC, and archaeological evidence suggests that this technique was used in most emerging civilizations including ancient Egypt and Mesopotamia. The basic ingredients of beer are water; a starch source, such as malted barley, which is able to be fermented (converted into alcohol); a brewer’s yeast to induce fermentation; and a flavouring, such as hops. A secondary starch source (an adjunct) may be used, such as maize (corn), rice or sugar. Less widely used starch sources include millet, sorghum and cassava root in Africa, potato in Brazil, and agave in Mexico, among others. The amount of each starch source in a beer recipe is collectively called the grain bill. There are several steps in the brewing process, which include malting, milling, mashing, lautering, boiling, fermenting, conditioning, filtering, and packaging. There are three main fermentation methods, warm, cool and wild or spontaneous. Fermentation may take place in open or closed vessels. There may be a secondary fermentation that can take place in the brewery, in the cask, or in the bottle. Brewing specifically includes the process of steeping, such as in making tea, sake, and soy sauce. Technically, wine, cider and mead are not brewed but rather vinified, as there is no steeping process involving solids. Brewing at home is subject to regulation and prohibition in many countries. Restrictions on homebrewing were lifted in the UK in 1963, Australia followed suit in 1972, and the USA in 1978, though individual states were allowed to pass their own laws limiting production.
_
Chemical routes for industrial alcohol:
In the Ziegler process, linear alcohols are produced from ethylene and triethylaluminium followed by oxidation and hydrolysis. The process generates a range of alcohols that are separated by distillation. Low molecular weight alcohols of industrial importance are produced by the addition of water to alkenes. Ethanol, isopropanol, 2-butanol, and tert-butanol are produced by this general method. Methanol was formerly obtained by the distillation of wood and called “wood alcohol.” It is now a cheap commodity, produced by the reaction of carbon monoxide and hydrogen under high pressure.
__________
Congeners:
Congeners are biologically active chemicals (chemicals which exert an effect on the body or brain) and are often contained in alcoholic beverages, in addition to ethanol, the key biologically active ingredient of alcohol. Congeners are produced in the process of fermentation or ageing, when organic chemicals (chemicals from plants) in the beverage break down. They may also be added during the production process to contribute to the taste, smell and appearance of the beverage. These substances include small amounts of chemicals such as occasionally desired other alcohols, like propanol and 3-methyl-1-butanol, but also compounds that are never desired like, acetone, acetaldehyde, esters, glycols, and ethyl acetate. Congeners are responsible for most of the taste, color and aroma of distilled alcoholic beverages, and contribute to the taste of non-distilled drinks. It has been suggested that these substances contribute to the symptoms of a hangover. The problem with congenerics is that there are so many different types of them that not much research has been carried out to test what their exact effect is on intoxication and hangovers. However, what we do know is that for the most part our body does not like them.
_
Congeners are primarily contained in darker liquors, brandy, tequila, whiskey and wine. Methanol is a congener contained in alcoholic beverages which is thought to contribute to hangover symptoms. When metabolised, methanol breaks down into formaldehyde and formic acid. The elimination of methanol from the body coincides with the onset of a hangover. People who metabolize methanol faster than others will feel greater physical symptoms of a hangover. Whiskey, red wine, brandy and other dark spirits contain the greatest volume of methanol, and have been suggested to cause worse hangovers, although this is yet to be confirmed. Ethyl carbamate is a congener formed in fermented foods and alcoholic beverages during the fermentation process or during storage. Public concerns regarding ethyl carbamate are related to its potential to cause cancer in human.
__
The figure below shows congener profile of malt whisky vs. blended whisky:
Any consumer complaints on ‘brand swapping’ or dilution are sent to the public analyst who determines the alcoholic strength of the sample by densitometry, and, for whisky, will use gas chromatography to separate and measure the concentrations of congeners. Congeners are formed during fermentation and maturation of whisky. The various alcohol fractions and the congener ‘fingerprint’ are compared with those for the authentic whisky sample.
__________
Alcoholic beverages:
Alcoholic beverages are a drink typically containing 1–50% ethanol by volume, have been produced and consumed by humans since pre-historic times. Alcoholic beverages are divided into three classes: beers, wines, and spirits (distilled beverages). They are legally consumed in most countries around the world. More than 100 countries have laws regulating their production, sale, and consumption. Alcoholic beverages have been produced and consumed by humans since the Neolithic Era, from hunter-gatherer peoples to nation-states. Other alcohols such as 2-methyl-2-butanol and γ-hydroxybutyric acid are also consumed by humans for their psychoactive effects.
_
Ethanol is the principal psychoactive constituent in alcoholic beverages. With depressant effects on the central nervous system, it has a complex mode of action and affects multiple systems in the brain, most notably increasing the activity of GABA receptors. Through positive allosteric modulation, it enhances the activity of naturally produced GABA. Other psychoactives such as benzodiazepines, barbiturates exert their effects by binding to the same receptor complex, thus have similar CNS depressant effects. Alcoholic beverages vary considerably in ethanol content and in foodstuffs they are produced from. Most alcoholic beverages can be broadly classified as fermented beverages, beverages made by the action of yeast on sugary foodstuffs, or distilled beverages, beverages whose preparation involves concentrating the ethanol in fermented beverages by distillation. The ethanol content of a beverage is usually measured in terms of the volume fraction of ethanol in the beverage, expressed either as a percentage or in alcoholic proof units. Fermented beverages can be broadly classified by the foodstuff they are fermented from. Beers are made from cereal grains or other starchy materials, wines and ciders from fruit juices, and meads from honey. Cultures around the world have made fermented beverages from numerous other foodstuffs, and local and national classifications for various fermented beverages abound. Distilled beverages are made by distilling fermented beverages. Broad categories of distilled beverages include whiskeys, distilled from fermented cereal grains; brandies, distilled from fermented fruit juices; and rum, distilled from fermented molasses or sugarcane juice. Vodka and similar neutral grain spirits can be distilled from any fermented material (grain and potatoes are most common); these spirits are so thoroughly distilled that no tastes from the particular starting material remain. Numerous other spirits and liqueurs are prepared by infusing flavors from fruits, herbs, and spices into distilled spirits. A traditional example is gin, which is created by infusing juniper berries into a neutral grain alcohol. The ethanol content in alcoholic beverages can be increased by means other than distillation. Applejack is traditionally made by freeze distillation, by which water is frozen out of fermented apple cider, leaving a more ethanol-rich liquid behind. Ice beer (also known by the German term Eisbier or Eisbock) is also freeze-distilled, with beer as the base beverage. Fortified wines are prepared by adding brandy or some other distilled spirit to partially fermented wine. This kills the yeast and conserves a portion of the sugar in grape juice; such beverages are not only more ethanol-rich but are often sweeter than other wines. Fortified wine is wine, such as port or sherry, to which a distilled beverage (usually brandy) has been added. Fortified wine is distinguished from spirits made from wine in that spirits are produced by means of distillation, while fortified wine is simply wine that has had a spirit added to it. Alcoholic beverages are used in cooking for their flavors and because alcohol dissolves hydrophobic flavor compounds. Just as industrial ethanol is used as feedstock for the production of industrial acetic acid, alcoholic beverages are made into vinegar. Wine and cider vinegar are both named for their respective source alcohols, whereas malt vinegar is derived from beer.
_
Pure ethanol (200proof) cannot be obtained via conventional distillation of a water-ethanol mixture because a constant boiling mixture forms consisting of 95% ethanol-5% water (190 proof). Such a mixture is referred to as an azeotrope (azeotropic = a liquid mixture that is characterized by a constant concentration and constant minimum or maximum boiling point which is lower or higher than any of the components). Further concentration of the ethanol can be achieved by shifting the azeotropic point via vacuum distillation or addition of another substance to the mixture. Often times the compound added is highly toxic such as benzene, therefore absolute alcohol must never be consumed. The amount of ethyl alcohol in any one beverage varies. Thus, there are differences in the amount of alcohol between beer, wine, champagne and distilled spirits. The amount of alcohol is given as a percentage and also in “proof”. The proof of an alcohol beverage is equal to twice the percentage of ethyl alcohol contained therein. Thus, 100 proof ethanol is 50% and 50 proof ethanol is 25%, etc. Percentage means alcohol by volume (ABV) i.e. v/v
_
Types of Alcoholic Beverages:
1. Undistilled or fermented Alcoholic Beverages
2. Distilled Alcoholic Beverages
Both of the categories have a wide range of alcoholic beverages. These alcohol types have originated in different parts of the globe at different point of time.
1. Fermented Alcoholic Beverages:
The different fermented and undistilled alcoholic beverages include Beer, Chicha, Cider, Icarinne Liquor, Palm Wine, Sake, Tapache, Tiswin and Wine
2. Distilled Alcoholic Beverages:
Distilled alcoholic beverages a.k.a. liquor are nothing but concentrating the alcoholic content by distillation. It include
•Arrack – This distilled Alcohol is mainly produced in South Asia and South East Asia. This is produced by mixing fermented sap of coconut flower with sugarcane.
•Awamori – This distilled Alcoholic beverage is a Japanese production and made in Okinawa in Japan. This is actually made by fermenting rice and then distilling the fermented rice.
•Baijiu – This Chinese Alcoholic drink is also called as white liquor and its Alcoholic content is around 40% to 60%. This drink is produced by distilling Sorghum
•Gin – This is a type of distilled spirit that is made from Juniper Berries. There are different types of gin like Damson Gin and Sloe Gin. Damson gin is hugely popular in Britain.
•Mezcal – This distilled Alcoholic beverage had its origins in Mexico. It is prepared from a type of Agave plant like Maguey.
•Palinka – This is a type of fruit Brandy manufactured in Hungary. This fruit spirit is distilled from a mixture of different fruits including apple, apricot and plum. The Alcohol content varies widely between 40 % and 85%.
•Rum – Though consumed in different parts of the globe, rum is extremely popular in Caribbean region and Latin America. This is made by fermenting sugar cane juice or by fermenting molasses, one of the byproducts of sugarcane.
•Vodka – Vodka is a distilled spirit made by distilling fermented grain like wheat or corn. It has an alcoholic content of 40%.
•Whisky – This distilled alcoholic beverage is made by fermenting a combination of different grains including barley, malted barley, Rye, Corn and Wheat. The fermented whisky is then allowed to age in wooden casks.
◦Bourborn Whiskey – This is usually referred to as American Whiskey and is made from Corn.
◦Scotch Whisky – This type of Whisky is made by distilling fermented malt barley and had its origin in Scotland
•Brandy – This distilled beverage is made by distilling wine. It has an alcoholic content that ranges between 30% and 60%
•Horilka – This beverage had its origins in Ukraine and is made by distilling fermented grains
•Cognac – This distilled alcoholic beverage is a type of brandy and is famous in France.
•Tequila – This is a distilled beverage that is prepared from Blue Agave plant. It is named after a city in Mexico
•Guaro – Guaro is made by distilling fermented sugar cane juice and is hugely popular in Central and South American Countries
_
_
Alcohol content in various beverages:
On the basis of the information in the table below, you can see that drinking equivalent amounts of beer, wine or distilled spirits will provide greatly varying amounts of alcohol to the drinker.
_
| Alcoholic Beverage | Source | Alcohol Content(%ABV) | Absolute AlcoholGrams/100 ml | Proof % |
| Beer (standard) | Cereals | 3-4 | 2.3-3.1 | 4-8 |
| Beer (Strong) | Cereals | 8-11 | 6.2-8.6 | 16-22 |
| Wine | Grapes(and other fruits) | 5-13 | 3.9-10.1 | 10-26 |
| Fortified Wine | Grapes(and other fruits) | 14-20 | 10.9-15.9 | 28-40 |
| Distilled Spirits | Fruits, cereals, sugarcane | 40 | 31.2 | 80 |
| Arrack | Coconut flowers, sugarcane, grain | 33 | 25.7 | 66 |
_
Brief description of alcoholic beverages:
1. Wines are made from a variety of fruits, such as grapes, peaches, plums or apricots. The most common wines are produced from grapes. The soil in which the grapes are grown and the weather conditions in the growing season determine the quality and taste of the grapes which in turn affects the taste and quality of wines. When ripe, the grapes are crushed and fermented in large vats to produce wine.
2. Beer is also made by the process of fermentation. A liquid mix, called wort, is prepared by combining yeast and malted cereal, such as corn, rye, wheat or barely. Fermentation of this liquid mix produces alcohol and carbon dioxide. The process of fermentation is stopped before it is completed to limit the alcohol content. The alcohol so produced is called beer. It contains 4 to 8 per cent of alcohol.
3. Whisky is a type of distilled alcoholic beverage made from fermented grain mash. Different grains are used for different varieties, including barley, malted barley, rye, malted rye, wheat, buckwheat and corn. Whisky is typically aged in wooden casks, made generally of charred white oak. Whisky is a strictly regulated spirit worldwide with many classes and types. Whisky is made by distilling the fermented juice of cereal grains such as corn, rye or barley. Scotch whisky was originally made in Scotland. The word “Scotch” has become almost synonymous with whisky of good quality. Scotch whiskies are generally distilled twice, although some are distilled a third time and others even up to twenty times. Scotch Whisky Regulations require anything bearing the label “Scotch” to be distilled in Scotland and matured for a minimum of three years in oak casks, among other, more specific criteria. An age statement on the bottle, in the form of a number, must reflect the age of the youngest Scotch whisky used to produce that product. A whisky with an age statement is known as guaranteed age whisky. Scotch whisky without an age statement may, by law, be as young as three years old. Whiskies do not mature in the bottle, only in the cask, so the “age” of a whisky is only the time between distillation and bottling. This reflects how much the cask has interacted with the whisky, changing its chemical makeup and taste. Whiskies that have been bottled for many years may have a rarity value, but are not “older” and not necessarily “better” than a more recent whisky that matured in wood for a similar time. After a decade or two, additional aging in a barrel does not necessarily improve a whisky.
4. Rum is a distilled alcoholic beverage made from sugarcane byproducts, such as molasses, or directly from sugarcane juice, by a process of fermentation and distillation. The distillate, a clear liquid, is then usually aged in oak barrels. Caramel is sometimes used for colouring. Brandy is distilled from fermented fruit juices.
5. Brandy is usually aged in oak casks. The colour of brandy comes either from the casks or from caramel that is added. Brandy (from brandywine, derived from Dutch brandewijn, “burnt wine”) is a spirit produced by distilling wine. Brandy generally contains 35–60% alcohol by volume (70–120 US proof) and is typically taken as an after-dinner drink. Some brandies are aged in wooden casks, some are coloured with caramel colouring to imitate the effect of aging, and some brandies are produced using a combination of both aging and colouring. Brandy is also produced from fermented fruits other than grapes, but these products are typically named eaux-de-vie, especially in France. In some countries, fruit flavouring or some other flavouring may be added to a spirit that is called “brandy”.
6. Gin is a distilled beverage. It is a combination of alcohol, water and various flavours. Gin does not improve with age, so it is not stored in wooden casks. Gin is a spirit which derives its predominant flavour from juniper berries (Juniperus communis).
7. Liqueurs are made by adding sugar and flavouring such as fruits, herbs or flowers to brandy or to a combination of alcohol and water. Most liqueurs contain 20-65 per cent alcohol. They are usually consumed in small quantities after dinner.
8. Vodka is a distilled beverage composed primarily of water and ethanol, sometimes with traces of impurities and flavorings. Traditionally, vodka is made by the distillation of fermented grains or potatoes, though some modern brands use other substances, such as fruits or sugar.
9. Feni (sometimes spelt fenny or fenim) is a spirit produced exclusively in Goa, India. There are two types of Feni; cashew feni and coconut feni, depending on the original ingredient. The small batch distillation of feni has a fundamental effect on its final character; still retaining some of the delicate aromatics, congeners and flavour elements of the juice from which it was produced. As a thumb rule, the aroma is indicative of a carefully crafted feni.
_________
Mixed drink:
A mixed drink is a beverage in which two or more ingredients are mixed. Some mixed drinks contain liquor; others are non-alcoholic. Some popular types of mixed drinks are:
•Cobbler, a beverage made with wine or sherry, citrus juice, and sugar
•Cocktail, narrowly a mixture of liquor, sugar, water, and bitters; more broadly any sort of alcoholic mixed drink
•Cooler, a tall drink made with liquor, a carbonated beverage, and a fruit garnish
•Crusta, a liquor and citrus drink served in a glass rimmed with sugar
•Cup, a mixture of wine and other ingredients, typically fruit juice and a carbonated beverage, similar to a Wine cooler
•Fix, a mixture of liquor, citrus, and sugar
•Fizz, a fix with a carbonated beverage added
•Flip, an alcoholic mixed drink incorporating beaten egg, especially one made with liquor or wine, sugar, and egg, topped with powdered nutmeg and served hot or cold. Also used to describe a sailor’s drink made from beer mixed with rum or brandy, sweetened and served hot
•Highball
•Julep, a sweet drink of liquor and aromatics, specifically mint
•Punch
•Pousse-café, various liqueurs arranged in colored layers
•Sour
•Sling, originally American, a drink composed of spirit and water, sweetened and flavoured
_
Cocktails contain one or more types of liqueur, juice, fruit, sauce, honey, milk or cream, spices, or other flavorings. Cocktails may vary in their ingredients from bartender to bartender, and from region to region. Two creations may have the same name but taste very different because of differences in how the drinks are prepared.
_
The figure below shows that beer is the most consumed alcoholic beverage in the world:
_
Flavoring:
Alcohol is a moderately good solvent for many fatty substances and essential oils. This attribute facilitates the use of flavoring and coloring compounds in alcoholic beverages, especially distilled beverages. Flavors may be naturally present in the beverage’s raw material. Beer and wine may be flavored before fermentation. Spirits may be flavored before, during, or after distillation. Sometimes flavor is obtained by allowing the beverage to stand for months or years in oak barrels, usually American or French oak. A few brands of spirits have fruit or herbs inserted into the bottle at the time of bottling.
__________
Surrogate alcohol:
Surrogate alcohol is a term for any substance containing ethanol that is consumed but is not meant for consumption. Most people turn to these as a last resort either out of desperation or being unable to afford consumable alcoholic beverages.
Dangers to health:
Most surrogate alcohols have very high alcoholic levels, some as high as 95%, and thus can lead to alcohol poisoning, along with other symptoms of alcohol abuse such as vertigo, impaired coordination, balance and judgment, nausea, vomiting, blurred vision, and even long-term effects such as heart failure and stroke. Besides alcohol, there are many other toxic substances in surrogate alcohol such as hydrogen peroxide, antiseptics, ketones, as well as alcohols other than ethanol (drinking alcohol) such as isopropanol and methanol. Consumption of these can lead to internal hemorrhaging and scarring, ulcers, headaches, CNS depression, blindness, coma, and death.
Russia:
Consumption of surrogate alcohol is a common problem in Russia, contributing to the high rate of alcohol-related deaths in the country. During the Soviet regime, alcoholic beverages were often among the only consumer goods affordable for the general public, leading to rampant alcoholism which is still present in modern Russia. In 1985, Gorbachev instituted alcohol reform, attempting to fight widespread alcoholism by increasing prices and reducing availability. These changes, however, led to the formation of a black market for alcohol, including surrogates. The dissolution of the Soviet Union caused a further spike in alcohol prices, leading more people to cheaper surrogate alcohol.
_
In an ongoing study of 25- to 54-year-old Russian men living in an industrial city, researchers have discovered that a significant proportion consume “surrogate” alcohols, otherwise known as products containing alcohol that are not legally sold for consumption. Researchers have now analyzed the contents of these surrogate alcohol products, finding either high alcohol content or toxic contaminants. Results are published in the issue of Alcoholism: Clinical & Experimental Research.
•Heavy alcohol consumption is a major contributing factor to the very high death rate among Russians.
•Ongoing research shows that many Russians drink “surrogate” alcohols, such as “samogon” or moonshine, medicinal compounds, and other spirits such as aftershave products.
•New analyses indicate that these products have either very high concentrations of alcohol, or toxic contaminants.
“During the past decade we have been investigating reasons for the very high death rate among Russians,” said Martin McKee, professor of European public health at the London School of Hygiene and Tropical Medicine. “We have been looking in detail at men in Izhevsk, a city in central Russia. While we confirmed what we already knew, that a lot of vodka is drunk in Russia, we also found that a surprisingly large number of people, seven percent, were drinking substances containing alcohol but not meant to be drunk. For the current study, researchers analyzed the surrogate products being consumed, dividing them into three broad groups: “samogon” (home-produced spirits, also known as “moonshine” in North America); medicinal compounds, essentially tinctures containing herbal remedies; and other spirits (mainly aftershave products and cleaning fluids). Commercially produced vodkas were used for content comparison. The results indicate that a significant proportion of Russian men are drinking products that have either very high concentrations of ethanol, or contaminants known to be toxic.
___
Higher alcohols in alcoholic beverages and surrogate alcohol products:
Higher alcohols occur naturally in alcoholic beverages as by-products of alcoholic fermentation. Recently, concerns have been raised about the levels of higher alcohols in surrogate alcohol (i.e., illicit or home-produced alcoholic beverages) that might lead to an increased incidence of liver diseases in regions where there is a high consumption of such beverages. In contrast, higher alcohols are generally regarded as important flavour compounds, so that European legislation even demands minimum contents in certain spirits. In a study authors reviewed the scientific literature on the toxicity of higher alcohol, estimated tolerable concentrations in alcoholic beverages and concluded that scientific data are lacking so far to consider higher alcohols as a likely cause for the adverse effects of surrogate alcohol.
_
Poisonous Alcohols:
The difference between wood alcohol–also known as methyl alcohol or methanol–and ethanol is that wood alcohol has one less carbon and two less hydrogen atoms. The chemical formula for ethanol is C2H6O whereas the formula for methanol is CH4O. Alcohol dehydrogenase converts methanol into formaldehyde (CH2O) and aldehyde dehydrogenase turns this formaldehyde into a formic acid radical (CH2O-). Both formaldehyde and formic acid are highly poisonous and quickly dead to blindness and death. Another highly poisonous alcohol is ethylene glycol (C2H6O2) which is used in antifreeze. A metabolite of ethylene glycol is the highly poisonous oxalic acid. Rubbing alcohol (C3H8O)–also known as isopropyl alcohol–is more poisonous than ethanol but not as poisonous as methanol. Some chronic alcoholics turn to drinking rubbing alcohol when ethanol is unavailable–and some even come to prefer it.
_
Powdered alcohol (Palcohol) may be coming to a liquor store near you:
Putting a can of beer in a brown paper bag is about to look like child’s play. A new product that’s somehow been approved by US regulators makes booze as discreet as a packet of sugar. It’s called Palcohol, and it transforms a shot of vodka or rum into a pocketable pouch of powder. Tear it open, add some water, mix, and you’ve got hard liquor. Considering the age group that Palcohol is going to appeal to, however, the sweet, pre-mixed powders are probably going to be far more popular. To start off, the company plans to make margarita, mojito, cosmopolitan, and lemon drop flavors.
Palcohol will be made in two different formulations, a Beverage Formulation (ingestible) and an Industrial Formulation (non-ingestible). Beverage Formulation has several applications:
1. Outdoor Activity Applications: Palcohol is a boon to outdoors enthusiasts such as campers, hikers and others who wanted to enjoy adult beverages responsibly without having the undue burden of carrying heavy bottles of liquid.
2. Travel Applications: Similarly, adult travelers journeying to destinations far from home could conveniently and lawfully carry their favorite cocktail in powder format.
3. Hospitality Applications: Because powdered alcohol is so light, airlines can reduce the weight on an airplane by serving powdered vs. liquid alcohol and save millions on fuel costs.
Industrial Formulation (non-ingestible): The industrial formulation, different from the consumer formulation, has many possible positive uses in industry. Examples include: medical Applications, manufacturing Applications and energy Applications.
_________
Do different kinds of alcohol get you different kinds of drunk?
Alcohol is Alcohol – which is to say that the alcohol in wine is the same as the alcohol in beer is the same as the alcohol in liquor. That alcohol is ethyl alcohol, aka ethanol, and it’ll get you drunk. The fact that liquor tends to contain higher concentrations of ethanol than wine, and wine higher concentrations than beer, means that the same volume of different alcoholic beverages will get you more/less drunk, ergo the “standard drink” rule, as defined by the National Institutes of Health in the United States, a “standard” drink is any drink that contains about 0.6 fluid ounces or 14 grams of “pure” alcohol. The standard drink model suggests that when it comes to behavioral effects, the only difference between a can of beer and a shot of whiskey is the mode of delivery. Any perceived difference between the drunk you feel from the liquor and the drunk you feel from beer has to do with the rate at which you consumed the ethanol, not the beverage via which you consumed it. But what about hard alcohols that are comparable in ethanol concentration, and therefore equally efficient at getting you drunk? According to the Alcohol is Alcohol argument, 80-proof tequila should have the same effect on you as 80-proof vodka, rum, gin or whiskey. Yet we all know someone who insists that tequila makes them wild, that whiskey makes them angry, or that gin makes them sad. Why is that? One possible explanation: mixers. Lots of people shoot tequila straight, whereas rum is commonly taken in tandem with something else – cola, for example. Another explanation: congeners. Congeners are byproducts of the fermentation and distillation process, and include chemicals like acetone, acetaldehyde, and esters – not to mention forms of alcohol other than ethanol. Different alcoholic beverages contain different types and quantities of congeners, so even though 80-proof vodka, rum and gin all contain the same amount of ethanol; their congener content can vary considerably. This variation contributes mainly to tan alcohol’s colors and flavors, but may or may not also have an effect on the “flavor” of drunkenness it imparts. People also tend to drink strongly flavored drinks more slowly than tasteless drinks. So most people will get more alcohol into their system per hour when drinking vodka than they will when drinking whisky. Carbonation speeds the absorption of alcohol into the bloodstream. People drinking carbonated drinks will become intoxicated more quickly and achieve higher BACs than people dinking the same amount of alcohol per hour in the form of non-carbonated drinks. The most common explanation for the differential effects of booze is that it’s all in your head, and that your experience with a given alcohol is dictated largely by the social situations in which you choose to consume it: A lot of this is folk memories and cultural hangovers. A lot of it depends on what mood you were in when you started drinking and the social context. The idea that gin makes you unhappy probably comes from its nickname “mother’s ruin” – the idea that it makes women depressed, which is a cultural idea. But fundamentally, alcohol is alcohol whichever way you slice it. The psychosocial explanation for alcohol’s differential behavioral outcomes closely resembles the results of studies on alcohol expectancy effects, which examine not only the way people behave when they’ve ingested alcohol, but how they behave when they think they’ve ingested alcohol. Consider for example that even when test subjects are given a standardized dose of ethanol, and attain the same blood alcohol level as other study participants, their reactions tend to vary dramatically. Some act utterly sloshed, while others barely bat an eye. According to a 2006 review paper on alcohol expectancy effects, there’s evidence that this variability may stem from differences among test subjects in the how they expect to be affected by the alcohol they’re consuming: Studies of alcohol effects on motor and cognitive functioning have shown the individual differences in responses to alcohol are related to the specific types of effects that drinkers expect. In general, those who expect the least impairment are least impaired and those who expect the most impairment are most impaired under the drug. Moreover, this same relationship is observed in response to placebo. [Vide infra] In the end, our expectations can have tremendous sway over the perceived effects of an alcoholic beverage (or non-alcoholic, for that matter). In this light, the question of whether mixers or congeners affect our experiences with different alcohols seems almost inconsequential.
___________
Different types of drinking behaviors:
Teetotaler:
A person who completely abstains from alcoholic beverages may be called a teetotaler, a description which has surprisingly little to do with the non-alcoholic beverage known as tea. The word actually comes from a relatively obscure grammatical practice known as reduplication. By duplicating the first letter, the speaker gives additional emphasis to the entire word. Before it was applied to fervent non-imbibers, the term “T-total” was already in common use as a synonym for complete or absolute. A teetotaler, therefore, would be a person who has completely or absolutely sworn off the consumption of alcohol. It is believed the word became popular during British temperance meetings held in the 1830s. A teetotaler may never have taken a single sip of alcohol in his or her entire life, as opposed to a reformed alcoholic or social imbiber. Teetotalers are about 10% of population. He or she may cite religious or social convictions as the basis for his or her abstinence, or else he or she may have witnessed the effects of alcohol on relatives at an early age. A child of an active alcoholic may choose to never touch alcohol in order to break the cycle or to discourage their own children from picking up the destructive habit.
_
Social drinker – drinks some form of alcoholic beverage occasionally or regularly in moderation, i.e. within sensible limits.
Excessive drinking includes heavy drinking, binge drinking, and any drinking by pregnant women or people younger than drinking age limit.
Heavy drinker – drinks regularly and heavily (Men >5 units/day, Women >3 units/day).
Binge drinker – drinks irregularly and heavily. Most people who binge drink are not alcoholics or alcohol dependent.
Both heavy and binge drinking patterns will cause problems if prolonged.
Alcohol abuser (“problem drinker”) – drinking causes physical, psychological and social problems; continues to drink in spite of developing difficulties and criteria for alcohol dependence are not met. [Vide infra]
Dependent or addicted drinker (“alcoholic”) – has subjective awareness of compulsion to drink; exhibits prominent drink-seeking behaviour; becomes tolerant to alcohol; obvious physical, psychological and social problems; liable to withdrawal symptoms following cessation or reduction in alcohol intake; uses alcohol to avoid or relieve symptoms of withdrawal. [Vide infra]
_
Drinking culture:
Drinking culture refers to the customs and practices associated with the consumption of alcoholic beverages. Although alcoholic beverages and social attitudes toward drinking vary around the world, nearly every civilization has independently discovered the processes of brewing beer, fermenting wine, and distilling spirits. The many different cultural reasons why people around the world drink alcohol will be explained below.
1. Social drinking:
“Social drinking” refers to casual drinking in a social setting without intent to get drunk. Good news is often celebrated by a group of people having a few drinks. For example, drinks may be served to “wet the baby’s head” in the celebration of a birth. Buying someone a drink is a gesture of goodwill. It may be an expression of gratitude, or it may mark the resolution of a dispute.
_
2. Drinking Etiquette:
For the purposes of buying rounds of drinks in English public houses, William Greaves, a retired London journalist, devised a set of etiquette guidelines. When an individual arrives at a pub, common practice invites the newcomer to unilaterally offer a drink to a companion, with the unspoken understanding that when the drink has been nearly consumed, his/her companion will reciprocate. Trust and fair play are the root of the rules, though there are occasions (such as a requirement of one of the drinkers to need to carry out more important jobs, if any can be conceived of) where the rules can be broken. When taking alcohol to a BYOB (bring your own booze/beer) party, it is proper to leave any of your alcohol there that has not been consumed. It shows appreciation to the host and shows responsibility on your part. It is rude to take any alcohol back with you.
3. Free Drinks:
Various cultures and traditions feature the social practice of providing free alcoholic drinks for others. For example, during a wedding reception, or a bar mitzvah, free drinks are often served to guests, a practice that is known as “an open bar.” Free drinks may also be offered to increase attendance at a social or business function. They are commonly offered to casino patrons to entice them to continue gambling.
4. Session Drinking:
Session drinking is a chiefly British term that refers to drinking a large quantity of beer during a “session” (i.e. a specific period of time) without becoming intoxicated. A session is generally a social occasion. A “session beer”, such as a session bitter, is a beer that has moderate or relative low alcohol content. In the United States, a recent session beer definition has been proposed by beer writer Lew Bryson. His Session Beer Project blog includes a definition of 4.5% ABV or less for session beer. Followers of this definition include Notch Brewing, a session only beer brand. The Brewer Association has adopted a new category within their Great American Beer Fest competition which states a “session beer” is from 4.0%-5.1%
5. Binge Drinking:
Binge drinking is sometimes defined as drinking alcohol solely for the purpose of intoxication. It is quite common for binge drinking to occur in a social situation, which creates some overlap between social drinking and binge drinking. The National Institute on Alcohol Abuse and Alcoholism [NIAAA] defines binge drinking as a pattern of drinking alcohol that brings blood alcohol concentration [BAC] to 0.08 grams percent or above. For the typical adult, this pattern corresponds to consuming five or more drinks [men], or four or more drinks [women], in about 2 hours; on any day in previous six months. Alcohol abuse is associated with a variety of negative health and safety outcomes. This is true no matter the individual’s or the ethnic group’s perceived ability to “handle alcohol”. Persons who believe themselves immune to the effects of alcohol may often be the most at risk for health concerns and the most dangerous of all operating a vehicle.
_
The concept of a “binge” has been somewhat elastic over the years, implying consumption of alcohol far beyond that which is socially acceptable. In earlier decades, “going on a binge” meant drinking over the course of several days until one was no longer able to continue drinking. This usage is known to have entered the English language as early as 1854; it derives from an English dialectal word meaning to “soak” or to “fill a boat with water”. Understanding drinking in young people should be understood through a “developmental” framework. This would be referred to as a “whole system” approach to underage drinking as it takes into account a particular adolescent’s unique risk and protective factors—from genetics and personality characteristics to social and environmental factors. It is widely observed that in areas of Europe where children and adolescents routinely experience alcohol early and with parental approval, binge drinking tends to be less prevalent. Typically, a distinction is drawn between northern and southern Europe, with the northerners being the binge drinkers. The highest levels of both binge-drinking and drunkenness are found in the Nordic countries, UK, Ireland, Slovenia and Latvia. This contrasts with the low levels found in France, Italy, Lithuania, Poland and Romania – for example, binge-drinking more than twice in the last month was reported by 31% of boys and 33% of girls in Ireland, but in comparison 12%-13% of boys and 5%-7% of girls in France and Hungary. As early as the eighth century, Saint Boniface was writing to Cuthbert, Archbishop of Canterbury, to report how “In your diocese, the vice of drunkenness is too frequent. This is an evil peculiar to pagans and to our race. Neither the Franks nor the Gauls nor the Lombards nor the Romans nor the Greeks commit it”. It is probable, however, that “the vice of drunkenness” was present in all European nations. The 16th-century Frenchman Rabelais wrote comedic and absurd satires illustrating his countrymen’s drinking habits. And Saint Augustin used the example of a drunkard in Rome to illustrate certain spiritual principles. Binge drinking is common in Scandinavian countries, even in Norway and Sweden despite their history of high prices of and restricted access to alcohol in recent decades. For example, the Norwegian cultural phenomenon known as Russ provides high school seniors with a socially accepted venue for binge drinking. For younger people, from about 14–15 years and until leaving adolescence, binge drinking may be the main form of drinking. In Sweden people tend to drink huge amounts every weekend and especially during holidays. Denmark, which has the most lax access to alcohol in Scandinavia, unsurprisingly also has the highest alcohol consumption among teenagers, not only the highest in Scandinavia but also in the world. Still, the alcohol consumption among teenagers in Denmark is lower than the alcohol consumption of adults in Denmark, which is only average worldwide.
_
•Binge drinking by adults is a strong predictor of binge drinking by high school and college students living in the same state.
•There are approximately 1.5 billion episodes of binge drinking among persons aged 18 years or older in the United States annually, most of which involve adults age 26 years and older.
•More than half of all active duty military personnel report binge drinking in the past month, and young adult service members exposed to combat are at significantly greater risk of binge drinking than older service members.
•More than 90% of adult binge drinkers are not alcohol dependent.
_
Why is binge drinking hazardous?
Drinking significant volumes of alcohol in a single session is primarily dangerous because it leads to a greatly increased risk of injury. This may be an accident, such as simply falling over under the influence of drink, being involved as a pedestrian in a traffic accident or getting injured as the result of a fight. However, there is growing evidence that drinking large numbers of alcohol units over a relatively short period is likely to be far worse for your general health than spreading the same alcohol over a whole week, even though consumption is the same. Alcohol is a poison, and it may be that having high concentrations of it in the body over relatively short periods is worse for you that having lesser levels of it in your system more often. Repeated instances of binge drinking have been linked to strokes, kidney damage, memory loss and an increased breast cancer risk in women.
_
Does binge drinking make you an alcoholic?
Not necessarily. There is a big difference between someone who binges on occasion and someone who is dependent on alcohol. The difference is how you view alcohol. The danger of alcohol dependency should be considered if the very idea of going without a drink fills you with a sense of dread. While binge drinking may be a habit for many young people, the vast majority of those people could go a couple of days without a drink if necessary.
_
Alcohol consumption in humans is the third leading preventable cause of death in the United States (McGinnis & Foege, 1993). A common abuse pattern called binge drinking contributes to a substantial portion of alcohol-related deaths (Chikritzhs, Jonas, Stockwell, Heale, & Dietze, 2001). This type of drinking also is associated with alcohol poisoning, unintentional injuries, suicide, hypertension, pancreatitis, sexually transmitted diseases, and meningitis, among other disorders. As binge drinking is relatively common, it underlies many negative social costs, including interpersonal violence, drunk driving, and lost economic productivity, as reported by the National Institute on Alcohol Abuse and Alcoholism (NIAAA, 2000). These statistics have attracted increased attention from a variety of perspectives. The term “binge” originated as a clinical description of alcoholics and was defined by periods of heavy drinking followed by abstinence (Tomsovic, 1974). The word is distinct from the expression “binge drinking” that, since its conception, has engendered a wide array of definitional elements.
_
Cognitive Effects:
Binge-drinking studies that measure cognitive function have found frontal lobe and working memory deficits, although an empirical definition of binging has not been used consistently. Heavy social drinkers, defined to include those who engaged in binge-drinking episodes, demonstrated delayed auditory and verbal memory deficits that were related to task difficulty. These deficits were not found for the light social drinkers. The findings implied that “frequent intake of large amounts of alcohol in any one sitting (i.e., ‘binge’ drinking) may place individuals at an increased risk for suffering alcohol-related cognitive impairment” (Nichols & Martin, 1997)
_
Binge drinking is associated with many health problems, including—
•Unintentional injuries (e.g., car crashes, falls, burns, drowning)
•Intentional injuries (e.g., firearm injuries, sexual assault, domestic violence)
•Alcohol poisoning
•Sexually transmitted diseases
•Unintended pregnancy
•Children born with Fetal Alcohol Spectrum Disorders
•High blood pressure, stroke, and other cardiovascular diseases
•Liver disease
•Neurological damage
•Sexual dysfunction, and
•Poor control of diabetes.
_
Binge drinking costs everyone:
•Drinking too much, including binge drinking, cost the United States $223.5 billion in 2006, or $1.90 a drink, from losses in productivity, health care, crime, and other expenses.
•Binge drinking cost federal, state, and local governments about 62 cents per drink in 2006, while federal and state income from taxes on alcohol totaled only about 12 cents per drink.
_
Evidence-based interventions to prevent binge drinking and related harms include:
•Increasing alcoholic beverage costs and excise taxes.
•Limiting the number of retail alcohol outlets that sell alcoholic beverages in a given area.
•Holding alcohol retailers responsible for the harms caused by their underage or intoxicated patrons (dram shop liability).
•Restricting access to alcohol by maintaining limits on the days and hours of alcohol retail sales.
•Consistent enforcement of laws against underage drinking and alcohol-impaired driving.
•Maintaining government controls on alcohol sales (avoiding privatization).
•Screening and counseling for alcohol misuse.
_
6. Speed Drinking:
Speed drinking or competitive drinking is the drinking of a small or moderate quantity of beer in the shortest period of time, without an intention of getting heavily intoxicated. Unlike binge drinking, its focus is on competition or the establishment of a record. Speed drinkers typically drink a light beer, such as lager, and they allow it to warm and lose its carbonation in order to shorten the drinking time. The Guinness World Records (1990 edition, p. 464) listed several records for speed drinking. Among these were:
a) Peter G. Dowdeswell (born July 29, 1940) of Earls Barton, Northamptonshire, England, drank 2 liters in 6 seconds on February 7, 1975.
b) Steven Petrosino (born November, 1951) of New Cumberland, Pennsylvania, drank 1 liter in 1.3 seconds on June 22, 1977, at the Gingerbread Man Pub in Carlisle, Pennsylvania.
Neither of these records had been defeated when Guinness World Records banned all alcohol-related records from their book in 1991. Former Australian Prime Minister Bob Hawke held a record for the fastest consumption of “a yard” of beer. He drank 2.5 pints (1.4 liters) in 12 seconds.
________
The Fine Line between Social Drinking and Alcoholism:
If alcoholism is in your family, it will be easier for a social drink to become alcoholism due to genetics. Many people think that if you start drinking at any early age, it will lead to addiction, but alcoholism can happen at any age. If people want to find out if they have crossed that line, there are some simple questions they should ask themselves.
Have you ever felt guilty about your drinking and felt that you should cut down?
Have people criticized you about your drinking and you were annoyed with them for saying something?
Have you ever tried to self-medicate a hangover with “the hair of the dog” or needed a quick eye-opener in the morning? A big test would be to go to a party and not drink. If you cannot socialize with people without drinking, it could become a problem. Remember the saying “birds of a feather flock together”. If your friends insist you drink, it may be time to pick some new friends.
When you cross the Line:
Too many innocent people have been hurt or killed by someone under the influence of alcohol. When a drunken driver kills an innocent person, it is sad for everyone involved. The driver did not set out to kill someone when the party started. The driver could be your 18-year-old son or daughter during spring break. Before the accident, they had a bright future, he was a straight student, never took drugs, never had problems with the law, but for some reason had to get behind the wheel of a car under the influence. Bad decision! The worst decision this individual had ever made killed an innocent person, maybe another teenager, or a mother, or a successful entrepreneur or a grandpa. This affects everyone, including the driver’s family. When the driver comes out of their fog and realizes he or she killed someone, can you imagine what goes through their minds, other than wanting to do it over again? It is heartbreaking for all involved. It does not even have to go to that level to become a social problem. “Falls, fires, drownings, and suicides are also frequently associated with alcohol.” (Effects on Society, 2009) The fact that alcoholism is in any social class or structure, not settling with an income level or stereotype, is a scary thought. It could affect any one of us.
_
Harmful drinking behaviors:
| Type of Drinking Behaviour | Description |
| Hazardous drinkers | Those who drink over the sensible drinking limits, either regularly or through less frequent sessions of heavy binge drinking, but have so far avoided significant alcohol-related problems. |
| Harmful drinkers | Harmful drinkers are usually drinking at levels above those recommended for sensible drinking, typically at higher levels than most hazardous drinkers. Unlike hazardous drinkers, harmful drinkers show clear evidence of some alcohol-related harm. |
| Dependant Drinkers | Those who are likely to have increased tolerance of alcohol, suffer withdrawal symptoms, and have lost some degree of control over their drinking. In severe cases, they may have withdrawal fits and may drink to escape from or avoid these symptoms. |
_
Problem Drinking and Risky Drinking:
_
As it is commonly used, “problem drinking” often is synonymous with “alcoholism.” Among professionals, however, increasingly it is used to describe nondependent drinking that results in adverse consequences for the drinker. In contrast to the dependent drinker, the problem drinker’s alcohol problems do not stem from compulsive alcohol seeking, but often are the direct result of intoxication. Problem drinking represents a broader category than alcohol abuse disorder. The problem drinker may or may not have a problem severe enough to meet criteria for alcohol abuse disorder. While problem drinkers are currently experiencing adverse consequences as a result of drinking, risky drinkers consume alcohol in a pattern that puts them at risk for these adverse consequences.
_
Risky drinking includes:
1. High-volume drinking: 14 or more standard drinks per week on average for males, and 7 or more standard drinks for females.
2. High-quantity consumption: Consumption on any given day of 5 or more standard drinks for males, and 4 or more standard drinks for females.
3. Any consumption within certain contexts: Even when small quantities of alcohol are ingested, drinking is risky if it occurs within contexts that pose a particular danger, for example, during pregnancy, when certain health conditions are present, when certain medications are taken, etc.
_
How do physicians define “light,” “moderate,” and “heavy” drinking?
Although widely used, terms associated with consumption of alcohol–such as “light,” “moderate,” and “heavy”–are unstandardized. Physicians conveying health messages using these terms therefore may impart confusing information to their patients or to other physicians. As an initial attempt to assess if informal standardization exists for these terms, a study surveyed physicians for their definitions of such terms. Physicians operationally defined “light” drinking as 1.2 drinks/day, “moderate” drinking as 2.2 drinks/day, and “heavy” drinking as 3.5 drinks/day. Abusive drinking was defined as 5.4 drinks/day. One American drink equals 14 gm alcohol. There was considerable agreement for these operational definitions, indicating there is indeed an informal consensus among physicians as to what they mean by these terms. Gender and age did not influence these definitions, but self-reported drinking on the part of physicians was a factor. It must be brought to notice that different authors and different researchers and different governments have defined moderate drinking differently as seen in the table below.
_
_
_
Heavy drinking:
The National Institute on Alcohol Abuse and Alcoholism (NIAAA) definition is often used. For men, it’s having more than four drinks in a single day or more than 14 in a week, and for women, it’s having more than three drinks in a single day or more than seven in a week. The CDC defines heavy drinking for a man as exceeding 2 standard drinks per day for a man and one per day for a woman. The problem with these definitions is that they are purely black-and-white in nature and little better than the 19th century Temperance Movements attempt to classify everyone as either a teetotaler or a drunkard. The reality is that there is a world of difference between a person who drinks three beers on a Friday night and the person who is physically dependent on alcohol and drinks three fifths of whiskey per day.
_
Maximum quantity recommended:
Different countries recommend different maximum quantities. For most countries, the maximum quantity for men is 140 g–210 g per week. For women, the range is 84 g–140 g per week. Most countries recommend total abstinence whilst pregnant or breastfeeding.
_
From low risk to high risk drinking:
Low risk drinking according to the NIAAA, for men, is no more than four drinks in one day and no more than 14 drinks in a week. For women, it’s no more than three drinks in any day and no more than seven drinks in any week. Those figures may seem to be different than recommendations made by the U.S. Department of Health and Human Services, which call for no more than one drink per day for women and no more than two drinks per day for men. It’s important that both the daily and the weekly limits be considered. It’s when people begin to exceed those levels of consumption that their level of risk rises. When you start to consume more than those amounts per day or per week, your chances for developing alcohol dependence increases dramatically. According to NIAAA data, one in four people who exceed the low risk levels of alcohol consumption suffer from alcoholism or alcohol abuse. Just what does “at risk” mean in terms of actual likelihood for developing alcohol dependence? In a recent large scale prospective study of more than 40,000 people, researchers found that “people who were at risk drinkers daily or nearly daily had about seven times the risk of developing alcohol dependence compared with low risk drinkers. In terms of relative risk, that’s a pretty huge difference. In terms of absolute risk, however, heavier drinkers have less than a 20% chance of developing alcohol dependence—still an alarmingly high figure. That means out of 100 heavy drinkers about 20 would become alcoholic and out of 100 low risk drinkers, about 3 would become alcoholic. Most people who have high cholesterol don’t have heart attacks, and most people who smoke don’t get lung cancer, but that doesn’t mean they’re not at risk. People don’t understand risks that way.
As discussed earlier, standard drink is different for different countries.
I define low risk drinking as less than 40 gms of alcohol per any day and less than 140 gms of alcohol per week for men; and less than 30 gms of alcohol per any day and less than 70 gms of alcohol per week for non-pregnant women. Anything above is high risk drinking with health, social and legal consequences and high chance of getting alcohol dependence.
_
Under-reporting alcohol:
Drinkers underestimate their alcohol consumption by 40%, British study finds:
When researchers compared people’s self-reported alcohol intake to actual alcohol sales figures, they found a lot of drinks unaccounted for — and there’s no way a few dangerous drinkers are making up the difference, researchers said. Mostly, it’s people who claim to have had ‘just a few’ who are underreporting their habits. The study found that 19% more men than previously thought were regularly exceeding their recommend daily limit – and 26% more women. Total consumption across the week was also higher than officially thought – with 15% more men, and 11% more women drinking above the weekly guidelines. An analysis from the Centre for Public Health, published by Alcohol Concern, shows that drink surveys used to measure the public’s alcohol consumption grossly underestimate how much people really drink. The difference between survey data and actual sales data reveals that 225 million liters of alcohol per year go unaccounted for. This is equivalent to 430 million units of alcohol per week, or 44 million bottles of wine.
_
Canadians grossly underestimate their alcohol consumption:
A study results showed that people reported only about one third of their consumption when the amounts were compared to how much alcohol was actually sold every year — 8.2 liters of pure alcohol per person aged 15 and over.
__
Track your drinking by self-assessment tools:
Are you drinking within recommended limits? Use the drinking self-assessment tool to find out if you’re drinking too much. It’ll help you to assess the effects of your drinking and, if you are drinking too much, suggest ways of cutting down.
Unit calculators:
Use the alcohol unit calculator to find out how many units there are in a single drink or in a number of drinks.
iPhone tracker:
If you have an iPhone or iPod touch you can download the drinks tracker from the iTunes app store for free. The app allows you to calculate units in your drinks, track your drinking over months and get personalised feedback.
Desktop tracker:
The desktop tracker lets you calculate units, keep a drinks diary on your desktop and provides personalised feedback on your drinking.
Drinks diary:
Keeping a drinks diary for a week can be a real eye-opener to people who don’t realise how much they’re drinking. Download the drinks diary leaflet to work out your alcohol intake over a week.
____
Tips on cutting down:
If you regularly drink more than the recommended limits, try these simple tips to help you cut down. “Regularly” means drinking every day or most days of the week.
Make a plan:
Before you start drinking, set a limit on how much you’re going to drink.
Set a budget:
Only take a fixed amount of money to spend on alcohol.
Let them know:
If you let your friends and family know you’re cutting down and that it’s important to you, you could get support from them.
Take it a day at a time:
Cut back a little each day. That way, every day you do is a success.
Make it a smaller one:
You can still enjoy a drink but go for smaller sizes. Try bottled beer instead of pints, or a small glass of wine instead of a large one.
Have a lower-strength drink:
Cut down the alcohol by swapping strong beers or wines for ones with a lower strength (ABV in %). You’ll find this information on the bottle.
Stay hydrated:
Drink a pint of water before you start drinking, and don’t use alcohol to quench your thirst. Have a soft drink instead.
Take a break:
Have the odd day each week when you don’t have an alcoholic drink.
__________
The continuum of alcohol problems:
Alcohol problems can range in severity from mild, negative consequences in a single life situation to severe alcohol dependence with significant medical, employment, and interpersonal consequences. As shown in figure below, alcohol use and its associated problems can be viewed on a continuum — ranging from no alcohol problems following modest consumption, to severe problems often associated with heavy consumption.
__________
Alcohol statistics:
Worldwide alcohol consumption:
1. Worldwide consumption in 2010 was equal to 6.2 liters of pure alcohol consumed per person aged 15 years or older, which translates into 13.5 grams of pure alcohol per day.
2. A quarter of this consumption (24.8%) was unrecorded, i.e., homemade alcohol, illegally produced or sold outside normal government controls. Of total recorded alcohol consumed worldwide, 50.1% was consumed in the form of spirits.
3. Worldwide 61.7% of the population aged 15 years or older (15+) had not drunk alcohol in the past 12 months. In all WHO regions, females are more often lifetime abstainers than males. There is a considerable variation in prevalence of abstention across WHO regions.
_
_
_
_
Global status report on alcohol and health 2014:
The report stated that 38.3% of the global population consumed alcohol meaning those who do drink consume on average 17 liters of pure alcohol annually. Additionally, 16 percent of people in the world who use alcohol could be categorized as binge drinkers. On an average, an individual over 15 years of age consumed 6.2 liters of alcohol annually. Americans consumed 8.5 to 9.9 liters of alcohol per annum while the Canadians consumed a whopping 12.5 liters per annum. The report also states that in 2012, about 3.3 million deaths, or 5.9% of all global deaths, were attributable to alcohol consumption. Alcohol consumption cannot only lead to dependence but also increases the risk of developing more than 200 diseases. Alcohol consumption also contributes to about 10 percent of the disease burden due to tuberculosis, epilepsy, hemorrhagic stroke and hypertensive heart disease in the world, the report added.
The report also states:
1. Worldwide about 16.0% of drinkers aged 15 years or older engage in heavy episodic drinking.
2. In general, the greater the economic wealth of a country, the more alcohol is consumed and the smaller the number of abstainers. As a rule, high-income countries have the highest alcohol per capita consumption (APC) and the highest prevalence of heavy episodic drinking among drinkers.
3. In 2012, 139 million DALYs (disability-adjusted life years), or 5.1% of the global burden of disease and injury, were attributable to alcohol consumption.
4. There is also wide geographical variation in the proportion of alcohol-attributable deaths and DALYs, with the highest alcohol-attributable fractions reported in the WHO European Region.
_
Alcohol kills 3.3 million people worldwide each year, more than AIDS, tuberculosis and violence combined and alcohol causes one in 20 deaths globally every year. This actually translates into one death every 10 seconds. Drinking is linked to more than 200 health conditions, including liver cirrhosis and some cancers. Alcohol abuse also makes people more susceptible to infectious diseases like tuberculosis, HIV and pneumonia, the report found. Most deaths attributed to alcohol, around a third, are caused by associated cardiovascular diseases and diabetes. Alcohol-related accidents, such as car crashes, were the second-highest killer, accounting for around 17.1 per cent of all alcohol-related deaths.
_
_
Alcohol consumption is a necessary cause of nearly 80,000 deaths per year in the Americas, study finds:
A new study published in the scientific journal Addiction by the Pan American Health Organization, a branch of the World Health Organization, has measured the number and pattern of deaths caused by alcohol consumption in 16 North and Latin American countries. The study reveals that between 2007 and 2009, alcohol was a ‘necessary’ cause of death (i.e., death would not have occurred in the absence of alcohol consumption) in an average of 79,456 cases per year. Liver disease was the main culprit in most countries.
_
Statement of the Problem in the U.S.:
The cost of alcohol-related harm to society is enormous, both in human and economic terms:
• At least 85,000 Americans die each year from alcohol-related causes, making alcohol-related problems the third-leading cause of death in the United States (Mokdad, et al., 2004).
• Drinking and driving is a significant cause of injuries and fatalities in the United States. Alcohol was involved in 40 percent of traffic crash fatalities and in 7 percent of all crashes in 2003, resulting in 17,013 fatalities and injuring an estimated 275,000 people (NHTSA, 2004).
• Almost one in four victims of violent crime report that the perpetrator had been drinking prior to committing the violence. Alcohol was involved in 32 to 50 percent of homicides (Spunt, et al., 1995; Goldstein, et al., 1992; Greenfeld, 1998).
• Thirty-nine percent of accidental deaths (including drowning, poisonings, falls, and fires) and 29 percent of suicides in the United States are linked to the consumption of alcohol (Smith, et al., 1999).
• The total monetary cost of alcohol-attributable consequences (including health care costs, productivity losses, and alcohol-related crime costs) in 1998 was estimated to be $185 billion (USDHHS, 2000).
•Almost three times as many men (9.8 million) as women (3.9 million) are problem drinkers, and prevalence is highest for both sexes in the 18 to 29 age group.
•Studies of suicide victims in the general population show that about 20% are alcoholic.
_
Alcohol and race:
The figure below shows that Asians have lowest rate of alcohol dependence in the U.S.
_
The first recognition and reports of dangerous consequences of heavy consumption in alcoholics were noted in India, Greece, and Rome. In the United Kingdom, heavy drinking is blamed for about 33,000 deaths a year. A study in Sweden found that 29% to 44% of “unnatural” deaths (those not caused by illness) were related to alcohol. The causes of death included murder, suicide, falls, traffic accidents, asphyxia, and intoxication. A global study found that 3.6% of all cancer cases worldwide are caused by alcohol drinking, resulting in 3.5% of all global cancer deaths. A study in the United Kingdom found that alcohol causes about 6% of cancer deaths in the UK (9,000 deaths per year).
___________
Physiology of alcohol: absorption, distribution, metabolism and elimination in human body:
Absorption:
Absorption of ethyl alcohol into the blood can occur through the skin and via the lungs, though the major route of taking ethyl alcohol into the body is by drinking alcoholic beverages. Drinking is the primary means by which ethyl alcohol is taken into the human body. Ethyl alcohol taken in via ingestion passes from the mouth down the esophagus and into the stomach and on into the small intestine. At each point along the way ethyl alcohol can be absorbed into the blood stream. Alcohol is absorbed from mucous membranes of the mouth and esophagus (in small amounts), from the stomach and large bowel (in modest amounts), and from the proximal portion of the small intestine (the major site). The majority of the ethyl alcohol is absorbed from the stomach (approx. 20%) and the small intestine (approx. 80%). The rate of absorption is increased by rapid gastric emptying (as can be induced by carbonated beverages); by the absence of proteins, fats, or carbohydrates (which interfere with absorption); and by dilution to a modest percentage of ethanol (maximum at 20% by volume). No digestion required. Ethanol is such a small, simple molecule just two carbon atoms, six hydrogens, and one oxygen that it pours directly out of the stomach and small intestine into the bloodstream. The peak blood alcohol concentrations are achieved in fasting people within 0.5 to 2.0 hours, (average 0.75 – 1.35 hours depending upon dose and time of last meal) while non-fasting people exhibit peak alcohol concentrations within 1.0, and in extreme cases up to as much as 4.0 hours (average 1.06 – 2.12 hours). Between 2% (at low blood alcohol concentrations) and 10% (at high blood alcohol concentrations) of ethanol is excreted directly through the lungs, urine, or sweat, but the greater part is metabolized to acetaldehyde, primarily in the liver. The most important pathway occurs in the cell cytosol where alcohol dehydrogenase (ADH) produces acetaldehyde, which is then rapidly destroyed by aldehyde dehydrogenase (ALDH) in the cytosol and mitochondria. Alcohol dehydrogenase (ADH) is found in many tissues, including the gastric mucosa while acetaldehyde dehydrogenase (ALDH) is found predominantly in liver mitochondria. All ethyl alcohol which is broken down in the human body is first converted to acetaldehyde, and then this acetaldehyde is converted into acetic acid radicals–also known as acetyl radicals. This acetic acid radical combines with Coenzyme A to form acetyl-CoA. The acetyl-CoA then enters the Krebs cycle, which is the basic powerhouse of the human body. Inside the Krebs cycle this acetyl radical is eventually broken down into carbon dioxide, water and energy. A second pathway in the microsomes of the smooth endoplasmic reticulum (the microsomal ethanol-oxidizing system, or MEOS) is responsible for 10% of ethanol oxidation at high blood alcohol concentrations.
_
The oxidation of alcohol occurs in the following steps:
1. Ethanol —> Acetaldehyde
2. Acetaldehyde —> Acetate
3. Acetate —-> Carbon Dioxide + Water
_
Gastric emptying seems to be the most important determinant of the rate of absorption of ethyl alcohol taken in orally. In general the faster the gastric emptying, the more rapid absorption. Therefore, factors, which influence gastric emptying, influence absorption. One of the most important factors is the presence of food. Food delays gastric emptying and therefore delays absorption of ethyl alcohol. Interestingly, the type of food, whether fat, carbohydrate, or protein, does not seem to be a factor in the absorption of ethyl alcohol. Physiological factors such as strenuous physical exercise also delay gastric emptying, thus decrease ethyl alcohol absorption. Additional factors such as drugs (e.g. nicotine, marijuana, and ginseng), that modify physiological factors regulating gastric emptying also modify ethyl alcohol absorption in a predicted manner. The ethyl alcohol concentration of the beverage appears to be an important factor in absorption from the gastrointestinal tract. If just Fick’s Law were in effect then it would be expected that the higher the concentration of ethyl alcohol consumed the move rapid the absorption, however it appears that higher concentrations of alcohol may actually delay absorption. Though the precise reason for this finding is not known, it can be speculated that higher concentrations of ethyl alcohol may diminish the movement of the alcohol from the stomach through the pylorus (opening from stomach to small intestine) and into the small intestine. Absorption is most rapid when the alcohol concentration in the stomach is 10%-20% (fortified wine, beer & ‘chaser’). Higher concentrations of alcohol (neat spirit) irritate the gastric mucosa, causing increased secretion of mucus and delay in gastric emptying and absorption. Absorption rapid from carbonated drinks (champagne). If alcohol is taken slowly it can be eliminated as fast as it is being absorbed; blood alcohol concentration (BAC) will not rise any further.
_
Remember, Alcohol takes a while to be absorbed:
For those without a lot of experience drinking, it’s important to know that alcohol takes a while to be absorbed into the bloodstream after drinking. Practically, this means that if you drink too fast, by the time you first notice effects, the alcohol which has yet to be absorbed could be enough to make you sick.
_
Distribution of alcohol:
Ethyl alcohol (ethanol, CH3CH2OH) is a low molecular weight aliphatic (open chain) compound, which is completely miscible with water. This characteristic is due to its hydroxyl (-OH) group, which forms intermolecular hydrogen bonds to water. Thus, the hydroxyl group is referred to as being hydrophilic (water-attracting), whereas the ethyl (C2H5-) group is referred to as being hydrophobic (water-repelling). Because of the complete miscibility with water, ethyl alcohol is readily distributed throughout the body in the aqueous blood stream after consumption. Also and because of this water solubility, it is readily crosses important biological membranes, such as the blood brain barrier, to affect a large number of organs and biological processes in the body. The passage of ethyl alcohol across biological membranes occurs by a process of simple passive diffusion along concentration gradients, in accordance with Fick’s law. Since ethyl alcohol mixes freely with water it would be expected that even within the blood, alcohol distribution would parallel the distribution of water in the blood. This has been studied by several research groups (e. g. Hodgson and Shajani, 1985; Winek and Carfagna, 1987; Jones et al, 1990, 1992). Since plasma and serum have approximately the same water content (92%), whereas whole blood has about 80% water, it would be expected that the ratio of ethyl alcohol content in the plasma or serum to alcohol content in whole blood would be equal to the ratio of water in plasma to the water in whole blood. This is what was found, in that the ratio was approximately 1.12 for both (92%/80% = 1.15). Since water diffuses easily across cell membranes through aqueous channels, including vascular endothelium it is expected that ethyl alcohol would do the same. Further it is expected that the ethyl alcohol concentration in the tissues would rapidly reach equilibrium with the ethyl alcohol in the blood. This is certainly been found to be the case. The alcohol from the blood enters and dissolves in the water inside each tissue of the body (except fat tissue, as alcohol cannot dissolve in fat). Once inside the tissues, alcohol exerts its effects on the body. The observed effects depend directly on the blood alcohol concentration (BAC), which is related to the amount of alcohol consumed. The BAC can rise significantly within 20 minutes after having a drink.
_
Eventually, all the alcohol that was consumed will reach the bloodstream. Absorption is generally complete in one to three hours. Most of the alcohol in the body (about 91 per cent) is broken down by the liver. A small amount also leaves the body in urine, sweat and the breath. Since the liver can only break down about 10 ml an hour, sobering up takes time. If you consume more than this, your system becomes saturated, and the additional alcohol will accumulate in the blood and body tissues until it can be metabolized. This is why having a lot of shots or playing drinking games can result in high blood alcohol concentrations that last for several hours. Cold showers, exercise, black coffee, fresh air or vomiting will not speed up the process.
___
Metabolism of alcohol:
_
_
Ethanol cannot be excreted and must be metabolized, primarily by the liver. More than 90% of the ethyl alcohol that enters the body is completely oxidized to acetic acid. This process occurs primarily in the liver. The remainder of the alcohol is not metabolized and is excreted either in the sweat, urine, or given off in one’s breath. The latter provides the basis of the breathalyzer test used in law enforcement and is the reason one can smell alcohol on the breath of someone who has been drinking recently. There are several routes of metabolism of ethyl alcohol in the body. The major pathways involve the liver and in particular the oxidation of ethyl alcohol by alcohol dehydrogenase (ADH). Playing a role, particularly at higher alcohol concentrations is the oxidation of alcohol by the microsomal (small spherical vesicles) – cytochrome P450 system (MEOS) system. In addition to these routes, there is catalase-dependent oxidation of ethyl alcohol and oxidation of it by the stomach when it is first ingested. These latter two routes of metabolism are minor in comparison to the ADH and MEOS systems. As mentioned above perhaps the major route of metabolism of ethyl alcohol is its oxidation in the liver catalyzed by the cytosolic enzyme alcohol dehydrogenase (ADH). It catalyzes the following reaction:
CH3CH2OH + NAD+ -> CH3CHO + NADH + H+.
This reaction produces acetaldehyde, a highly toxic substance.
The second step, catalyzed by aldehyde dehydrogenase, takes place in mitochondria where acetaldehyde is converted into acetic acid (acetate) generating another NADH.
Acetaldehyde + NAD –> Acetic Acid + NADH
Final step of alcohol metabolism is conversion of acetate into acetyl-CoA
The two molecules joined by acetyl-CoA synthetase are acetate and coenzyme A (CoA). The complete reaction with all the substrates and products included is:
ATP + Acetate + CoA –>AMP + Pyrophosphate + Acetyl-CoA
Once acetyl-CoA is formed it can be used in the TCA cycle in aerobic respiration to produce energy and electron carriers. This is an alternate method to starting the cycle, as the more common way is producing acetyl-CoA from pyruvate through the pyruvate dehydrogenase complex. Acetyl Co-A can also be used in fatty acid & amino acid synthesis in a non-drinker as seen in the figure below:
_
The figure below denotes metabolic fate of acetyl-CoA in a non-drinker:
_
However, excess NADH in alcoholics modifies entire metabolism of carbohydrate, fat and protein. Note that ethanol consumption leads to an accumulation of NADH. This high concentration of NADH inhibits gluconeogenesis by preventing the oxidation of lactate to pyruvate. In fact, the high concentration of NADH will cause the reverse reaction to predominate, and lactate will accumulate. The consequences may be hypoglycemia and lactic acidosis. The NADH glut also inhibits fatty acid oxidation. The metabolic purpose of fatty acid oxidation is to generate NADH for ATP generation by oxidative phosphorylation, but an alcohol consumer’s NADH needs are met by ethanol metabolism. In fact, the excess NADH signals that conditions are right for fatty acid synthesis. Hence, triacylglycerols accumulate in the liver, leading to a condition known as “fatty liver.” Liver mitochondria can convert acetate into acetyl CoA in a reaction requiring ATP. The enzyme is the thiokinase that normally activates short-chain fatty acids. However, further processing of the acetyl CoA by the citric acid cycle is blocked, because NADH inhibits two important regulatory enzymes— isocitrate dehydrogenase and α-ketoglutarate dehydrogenase. The NADH may be used directly in the electron transport chain to synthesize ATP as a source of energy. The accumulation of acetyl CoA has several consequences. First, ketone bodies will form and be released into the blood, exacerbating the acidic condition already resulting from the high lactate concentration. The processing of the acetate in the liver becomes inefficient, leading to a buildup of acetaldehyde. This very reactive compound forms covalent bonds with many important functional groups in proteins, impairing protein function. If ethanol is consistently consumed at high levels, the acetaldehyde can significantly damage the liver, eventually leading to cell death.
_
The metabolic pathway for the disposal of excess NADH in alcoholics and the consequent blocking of other normal metabolic pathways is shown in the figure below:
_
The second pathway for ethanol metabolism is called the ethanol inducible microsomal ethanol-oxidizing system (MEOS). This cytochrome P450-dependent pathway generates acetaldehyde and subsequently acetate while oxidizing biosynthetic reducing power, NADPH, to NADP+. Because it uses oxygen, this pathway generates free radicals that damage tissues. Moreover, because the system consumes NADPH, the antioxidant glutathione cannot be regenerated, exacerbating the oxidative stress. The reaction catalyzed by MEOS is:
CH3CH2OH + NADPH + O2 -> CH3CHO + NADP+ + H2O.
Though of minor significance in comparison to ADH metabolism of ethanol, the MEOS system seems to play an increasingly important role at higher concentrations of ethanol. It is not surprising that there are variations in the P450E1 enzyme which lead to differences in the rate of ethanol metabolism. This may have implications for tissue damage from ethanol, particular in the liver. MEOS means microsomal ethanol oxidizing system.
_
Note:
Nicotinamide adenine dinucleotide, abbreviated NAD+, is a coenzyme found in all living cells. The compound is a dinucleotide, since it consists of two nucleotides joined through their phosphate groups. One nucleotide contains an adenine base and the other nicotinamide. In metabolism, NAD+ is involved in redox reactions, carrying electrons from one reaction to another. The coenzyme is, therefore, found in two forms in cells: NAD+ is an oxidizing agent – it accepts electrons from other molecules and becomes reduced. This reaction forms NADH, which can then be used as a reducing agent to donate electrons. These electron transfer reactions are the main function of NAD+. However, it is also used in other cellular processes, the most notable one being a substrate of enzymes that add or remove chemical groups from proteins, in posttranslational modifications.
_
Catalase:
Catalase is found in tiny organs inside of cells called peroxisomes. Catalase is found all over the human body. When catalase turns alcohol into acetaldehyde the hydrogen which is released is bound to hydrogen peroxide molecules which then become water. Although catalase is active everywhere in the body, catalase is of particular interest to researchers because it metabolizes alcohol in the brain. The acetaldehyde released into the brain by the metabolism of alcohol by catalase has the potential to combine with neurotransmitters to form new compounds known as THIQs (tetrahydroisoquinolines, also sometimes called TIQs). Some researchers believe that THIQs are the cause of alcohol addiction and that the presence of THIQs distinguishes addicted drinkers from social drinkers. Other researches strongly dispute the validity of the THIQ hypothesis of alcohol addiction. The actual role of THIQs remains controversial and a topic for further research.
__
The effects of ethanol on carbohydrate metabolism are complex. When given to individuals whose glycogen stores have been depleted by fasting, ethanol can lead to severe hypoglycemia primarily by reducing hepatic glucose production through inhibition of gluconeogenesis. The effects of ethanol in fed individuals are less well understood. In numerous studies, using many different experimental protocols, ethanol pretreatment has been associated with diminished, improved, or unchanged glucose tolerance. Moreover, several patients have been reported in whom ethanol abuse led to overt diabetes mellitus which disappeared with abstinence from alcohol. Ethanol is a preferred fuel preventing fat, and to lesser degrees, carb and protein, from being oxidized.
_
Alcohol may hinder the protein synthesis process:
Research indicates that alcohol affects protein nutrition by causing impaired digestion of proteins to amino acids, impaired processing of amino acids by the small intestine and liver, impaired synthesis of proteins from amino acids, and impaired protein secretion by the liver. A ground-breaking study conducted in 1991 and published in the journal “Alcohol and Alcoholism” found that chronic intake of alcohol suppressed protein synthesis and caused myopathy in many cases. Myopathy is a condition in which muscle fibers do not function properly, resulting in muscle weakness or loss of movement. This study focused on long-term use of alcohol, but short-term usage also inhibits protein synthesis from occurring at its full potential. A major part of protein synthesis involves several hormones involved in the muscle-building process, namely testosterone and human growth hormone. Alcohol affects the release of both of these hormones. Alcohol consumption decreases secretion of HGH by up to 70 percent. Alcohol consumption also causes your liver to release substances that virtually cancel out the effects of testosterone in your body. The result is an environment not suitable for muscle growth.
_
Rate of metabolism:
Blood alcohol concentration (BAC) depends on the amount of alcohol consumed and the rate at which the user’s body metabolizes alcohol. Because the body metabolizes alcohol at a fairly constant rate (somewhat more quickly at higher and lower alcohol concentrations), ingesting alcohol at a rate higher than the rate of elimination results in a cumulative effect and an increasing blood alcohol concentration. On average, it takes about one hour for the body to metabolise (break down) one UK unit of alcohol, 10 ml. In a healthy person, the rate of clearance of alcohol from the blood by liver is 15 mg alcohol per 100 ml blood per hour (the equivalent of one UK unit per hour). However, the range is from 10-40 mg per 100 ml per hour. However, this can vary with body weight, sex, age, personal metabolic rate, recent food intake, the type and strength of the alcohol, and medications taken. Healthy people metabolize alcohol at a fairly consistent rate. The rate of elimination tends to be higher when the blood alcohol concentration in the body is very high. Also chronic alcoholics may (depending on liver health) metabolize alcohol at a significantly higher rate than the average. Finally, the body’s ability to metabolize alcohol quickly tends to diminish with age. Alcohol may be metabolised more slowly if liver function is impaired. Currently, the only known substance that can increase the rate of metabolism of alcohol is fructose. The effect can vary significantly from person to person, but a 100g dose of fructose has been shown to increase alcohol metabolism by an average of 80%. Fructose also increases false positives of high BAC ratio readings in anyone with proteinuria and hematuria, due to kidney-liver metabolism.
__
After Your First Two Drinks:
After your first drink, your body starts to get rid of the alcohol quickly using the alcohol dehydrogenase (ADH) pathway. In this pathway, ADH converts the alcohol into acetaldehyde, which gets further broken down to acetate. These by-products (acetaldehyde and acetate) are considered to be highly reactive and can increase oxidation throughout the body, but especially in the liver. Because your body sees these by-products as dangerous, it wants to use them as fuel. This means your body will significantly blunt fat-burning close to 75% after just one and a half drinks. And it will stop using carbs for energy. Therefore, although very little alcohol will be stored as fat (less than 5%), the fat and carbs you are eating have an increased risk of being stored as fat. Your liver can process these toxins through the increased use of certain vitamins, such as the water soluble vitamins B1, B3, B6, folate and C, while also possibly depleting some of the fat-soluble vitamins, A, E and K1. Over-time these decreases in vitamins can play a secondary role in loss of motivation, energy, and well-being. After your first couple of drinks, your brain also starts to increase its usage of GABA. GABA is an inhibitory neurotransmitter in the brain and is a large reason why alcohol is known as a “depressant.” Over time, the GABA receptors get used to the effects of alcohol, which is a reason why people may need more and more alcohol to feel the effects from alcohol consumption. GABA is also the neurotransmitter, principally responsible for allowing you to stay asleep. Therefore when your brain uses more of it before you go to sleep, you have less while you’re actually sleeping, causing a disruption in restful sleep. Alcohol also affects the higher processing areas of the brain, the cerebral cortex, while leaving the lower areas of the brain somewhat unaffected. This leaves you more emotional than you would normally be. If you’ve ever experienced “drunk logic” while doing or saying things you would never think to do sober, then you’ve experienced the inhibitory effects of having your cerebral cortex taken out of the equation. While your body has started to use the alcohol as energy, your body releases anti-diuretic hormone (ADH) to help your body rid itself of the alcohol. This basically means that your urine volume increases significantly (about 100 ml per 10 grams of alcohol). If you’ve ever “broken the seal,” you know that the more you continue to drink, the more frequently you use the restroom. Since your kidneys are working over-time, your body releases an increase in certain minerals and electrolytes especially calcium, magnesium, copper, selenium and manganese. All of these play important roles not only in blood volume, but in bone health, blood pressure and the anti-oxidant pathways. In addition to everything above, a small increase in cortisol typically occurs with moderate drinking while testosterone levels will drop about 6.8% in men (not so much in women). Aromatase will also increase. Aromatase is an enzyme that helps to convert testosterone to estrogen and is obviously not something that is welcomed by many guys.
After Six to Eight Plus Drinks:
If you’re drinking a moderate amount of alcohol, those things listed above are the main effects, at least short-term. If you drink heavily and drink often, another system called the Microsomal Ethanol-Oxidizing System (MEOS) system kicks in at the point when the ADH pathway becomes overwhelmed. This system is interesting because it causes your body to generally burn off more energy as useless heat and probably saves your life from too high of a blood alcohol level. It is primarily controlled by a special enzyme that plays an important role in utilizing certain medications and the metabolism of fatty acids. This increased rate of medication breakdown can decrease their effectiveness, while the incomplete breakdown of fatty acids can cause an increase in oxidation. This increase in oxidation becomes exacerbated as the body’s main anti-oxidant (glutathione) is also impaired, decreasing your ability to fight the oxidation. As your drinking levels continue to increase, testosterone levels drop from 6.8% with 4 drinks to 23% with 8 drink. This drop, combined with a slowdown in protein synthesis, can cause havoc when trying to recover from a workout. In addition to that, fluid loss will generally become more significant, causing dehydration that might affect you for days afterwards. Finally, with heavy drinking, the breakdown of alcohol can occur for up to 48 hours after your last drink. This means less glucose is reaching your brain and working muscles, making you both more tired and quicker to fatigue if you do exercise.
_
Acetate may be used as fuel by brain in alcoholics: A study:
A new study from Yale University suggests that heavy drinking may actually accelerate the body’s ability to turn alcohol into energy-boosting acetate, especially in the brain. When people consume drinks such as beer or wine, their liver breaks down the compounds and turn them into acetate, which is then distributed throughout the body, into the bloodstream and to the brain. In order to interpret metabolic changes in the brain, researchers tested subjects’ blood-alcohol levels first and then administered the same levels of acetate for two hours. During that time, their reactions were scanned with a magnetic resonance spectroscopy machine (MRS) to determine the presence of natural N-acetylaspartate (NAA), C-labelled glutamate, glutamine and acetate. In the initial tests, the heavy drinkers had higher levels of acidic compounds in their blood prior to infusion, compared to the light drinkers. By the study’s end, they found that heavy drinkers had ingested twice as much acetate into their bloodstreams than light drinkers (which is a testament to their body’s ability to do so). These findings are monumental since it was always believed the body could only use sugar as a form of energy, but researchers showed that acetate is also used as fuel by brain. Scientists have long suspected that heavy drinkers ingest and burn more acetate, but now it is proven. The findings may also explain why tolerance levels are higher among heavy drinkers and why it so difficult for them to abstain from alcohol. Quitting drinking, as well as removing an addictive substance, would also be removing an energy source the brain can come to rely on. “Caloric reward” in turn, may encourage a heavy drinker’s continued alcohol abuse over time.
___
Gene expression and ethanol metabolism:
Ethanol to acetaldehyde in human adults:
In human adults, ethanol is oxidized to acetaldehyde mainly via the hepatic enzyme alcohol dehydrogenase IB (class I), beta polypeptide (ADH1B). The gene coding for this enzyme is on chromosome 4, locus 4q21-q23. The enzyme encoded by this gene is a member of the alcohol dehydrogenase family. Members of this enzyme family metabolize a wide variety of substrates, including ethanol, retinol, other aliphatic alcohols, hydroxysteroids, and lipid peroxidation products. This encoded protein, consisting of several homo- and heterodimers of alpha, beta, and gamma subunits, exhibits high activity for ethanol oxidation and plays a major role in ethanol catabolism. Three genes encoding alpha, beta and gamma subunits are tandemly organized in a genomic segment as a gene cluster.
Ethanol to acetaldehyde in human fetuses:
In human embryos and fetuses, ethanol is not metabolized via this mechanism as ADH enzymes are not yet expressed to any significant quantity in human fetal liver (the induction ADH only starts after birth, and requires years to reach adult levels). Accordingly, the fetal liver cannot metabolize ethanol or other low molecular weight xenobiotiocs. In fetuses, ethanol is instead metabolized at much slower rates by different enzymes from the cytochrome P-450 superfamily (CYP), in particular by CYP2E1. The low fetal rate of ethanol clearance is responsible for the important observation that the fetal compartment retains high levels of ethanol long after ethanol has been cleared from the maternal circulation by the adult ADH activity in the maternal liver. CYP2E1 expression and activity have been detected in various human fetal tissues after the onset of organogenesis (ca 50 days of gestation). Exposure to ethanol is known to promote further induction of this enzyme in fetal and adult tissues. CYP2E1 is a major contributor to the so called Microsomal Ethanol Oxidation Pathway (MEOS) and its activity in fetal tissues is thought to contribute significantly to the toxicity of maternal ethanol consumption. In presence of ethanol and oxygen, CYP2E1 is known to release superoxide radicals and induce the oxidation of polyunsaturated fatty acids to toxic aldehyde products like 4-hydroxynonenal (HNE).
Acetaldehyde to acetic acid:
Acetaldehyde is a highly unstable compound and quickly forms free radical structures which are highly toxic if not quenched by antioxidants such as ascorbic acid (Vitamin C) and Vitamin B1 (thiamine). These free radicals can result in damage to embryonic neural crest cells and can lead to severe birth defects. Prolonged exposure of the kidney and liver to these compounds in chronic alcoholics can lead to severe damage. The literature also suggests that these toxins may have a hand in causing some of the ill effects associated with hang-overs. The enzyme associated with the chemical transformation from acetaldehyde to acetic acid is aldehyde dehydrogenase 2 family (ALDH2). The gene encoding for this enzyme is found on chromosome 12, locus q24.2. This protein belongs to the aldehyde dehydrogenase family of proteins. Aldehyde dehydrogenase is the second enzyme of the major oxidative pathway of alcohol metabolism. Two major liver isoforms of aldehyde dehydrogenase, cytosolic and mitochondrial, can be distinguished by their electrophoretic mobilities, kinetic properties, and subcellular localizations. Most Caucasians have two major isozymes, while approximately 50% of East Asians have the cytosolic isozyme but not the mitochondrial isozyme. A remarkably higher frequency of acute alcohol intoxication among East Asians than among Caucasians could be related to the absence of a catalytically active form of the mitochondrial isozyme. The increased exposure to acetaldehyde in individuals with the catalytically inactive form may also confer greater susceptibility to many types of cancer.
Acetic acid to acetyl-CoA:
Two enzymes are associated with the conversion of acetic acid to acetyl-CoA the first is ACSS2 or acetyl CoA synthase-1; which is expressed by gene located on chromosome 20 locus q11.22. This gene encodes a nuclear-cytosolic enzyme that catalyzes the activation of acetate for use in lipid synthesis and protein acetylation reactions. The second enzyme is ACSS1 (acetyl CoA synthase-2) which is localized to mitochondria and is used for energy generation via the tricarboxylic acid cycle. The proteins act as monomers and produce acetyl-CoA from acetate in a reaction that requires ATP. Expression of ACSS2 is regulated by sterol regulatory element-binding proteins, transcription factors that activate genes required for the synthesis of cholesterol and unsaturated fatty acids. Two transcript variants encoding different isoforms have been found for this gene.
_
Genetic differences:
Alcohols flush reaction:
Alcohol flush reaction (also known as Asian flush syndrome, Asian flush, Asian glow, among others) is a condition in which an individual’s face or body experiences flushes or blotches as a result of an accumulation of acetaldehyde, a metabolic byproduct of the catabolic metabolism of alcohol. When alcohol is consumed, it is first metabolized into acetaldehyde, a chemical similar to formaldehyde, which causes DNA damage and has other cancer-promoting effects. ALDH2 is the main enzyme responsible for breaking down acetaldehyde into acetate, a non-toxic metabolite in the body. East Asians have two main variants of the ALDH2 gene — one that produces an enzyme with normal activity, and another that results in an inactive enzyme. When individuals with the inactive variant drink alcohol, acetaldehyde accumulates in the body, resulting in facial flushing, nausea, and rapid heartbeat. For people with two copies of the inactive variant, these symptoms are so severe that they can drink very little alcohol. However, individuals with only one copy of the inactive variant can become tolerant to the unpleasant effects of acetaldehyde, which puts them at risk for alcohol-related esophageal cancer. Roughly 50 percent of Japanese and other east Asians and some American Indians (but practically no Europeans or Africans) have a mutated gene that impairs ALDH2 activity. In these people, even a modest dose of alcohol, imbibed or endogenous, leads to acetaldehyde buildup and unpleasant symptoms: facial flushing, palpitations, dizziness, nausea, headache, and confusion. As acetaldehyde builds up, some is converted back to ethanol, retarding BAC decline. Eventually various enzymes slowly clear the acetaldehyde and the symptoms dissipate. The symptoms of flush syndrome are exactly the same as the symptoms caused in people who take the anti-drinking medication disulfiram which causes a build-up of acetaldehyde within the body. As many as 50% of people of Japanese descent are estimated to show flush syndrome. Flush syndrome is more severe in some individuals than others. This syndrome has been associated with an increased risk of esophageal cancer in those who drink. A series of epidemiologic studies by Akira Yokoyama and his colleagues in Japan have shown that individuals with one copy of the inactive variant are about 6-10 times more likely to develop esophageal cancer than are individuals with the fully active ALDH2 enzyme who drink comparable amounts of alcohol. Notably, these studies showed that individuals with the inactive variant who drink the equivalent of 33 or more U.S. standard drinks per week have a 89-fold increased risk of esophageal cancer compared to non-drinkers. It has also been associated with lower than average rates of alcoholism, possibly due to its association with adverse effects after drinking alcohol. It is estimated that individuals with severe flush syndrome do not develop alcohol problems because they find drinking alcohol to be extremely unpleasant. For measuring the level of flush reaction to alcohol, the most accurate method is to determine the level of acetaldehyde in the blood stream. This can be measured through both a breathalyzer test or a blood test. Additionally, measuring the amount of alcohol metabolizing enzymes alcohol dehydrogenases and aldehyde dehydrogenase through genetic testing can predict the amount of reaction that one would have. More crude measurements can be made though measuring the amount of redness in the face of an individual after consuming alcohol. Computer and phone applications can be used to standardize this measurement. Alcohol flush reaction is best known as a condition that is experienced by people of Asian descent. According to the analysis by HapMap project, the rs671 allele of the ALDH2 (gene) responsible for the flush reaction is rare among Europeans and Africans, and it is very rare among Mexican-Americans. 30% to 50% of people of Chinese and Japanese ancestry have at least one ALDH2 allele. The rs671 form of ALDH2, which accounts for most incidents of alcohol flush reaction worldwide, is native to East Asia and most common in southeastern China. It most likely originated among Han Chinese in central China, and it appears to have been positively selected in the past. Another analysis correlates the rise and spread of rice cultivation in Southern China with the spread of the allele. The reasons for this positive selection aren’t known, but it’s been hypothesized that elevated concentrations of acetaldehyde may have conferred protection against certain parasitic infections, such as Entamoeba histolytica. Since the mutation is a genetic issue, there is no cure for the flush reaction. Prevention would include not drinking alcohol. Treatment is the H2-antagonist class of medicine inhibits the ADH enzyme (the conversion from ethanol to acetaldehyde) both in the GI tract and in the liver, the conversion happens at a much slower pace, reducing the effects acetaldehyde has on the drinker.
_
Acetaldehyde Toxicity
Since acetaldehyde is approximately 30 times more toxic than alcohol, acetaldehyde is a major cause of alcohol-associated side effects. If acetaldehyde is not efficiently converted into acetic acid (the second step in the metabolism of alcohol), severe toxicity can result. This is a common problem among certain people of Asian extraction (notably Innuit and American Indians) who have a genetic weakness in the acetaldehyde dehydrogenase enzyme. Even in people who do not have this genetic trait, acetaldehyde dehydrogenase is often unable to fully keep up with the production of acetaldehyde during alcohol intoxication.
_
Flushing while drinking (acetaldehyde exposure) puts individuals at a higher risk of:
Gastric and esophageal cancer:
Studies demonstrate that upper digestive tract cancer risk is greatly increased in people that experience facial blushing. Moderate drinkers that flush are still at over twice the risk of esophageal cancer as heavy drinkers that do not flush. One study shows that 35% of the patients flushed, but accounted for 69% of the esophageal cancer cases. This is due to increased acetaldehyde exposure. The “Asian Flush” cancer correlation has been very well researched around the globe.
Liver cirrhosis and failure:
Studies show that there is a 60% higher risk of alcoholic cirrhosis in moderate drinkers that have facial flushing when compared to those that do not.
Alzheimer’s disease:
Individuals that flush demonstrate a higher chance of getting the degenerative brain disease Alzheimer’s. Studies show that 48% of Alzheimer’s patients flushed whereas only 37% flushed in the control group without Alzheimer’s.
_
Cross-Linking:
One of the most significant mechanisms of alcohol toxicity is the powerful cross-linking activity of acetaldehyde. Cross-linking is a process by which “molecular bridges” are formed between “reactive sites” on different molecules. These cross-links “tie up” the affected molecules and interfere with their normal function. In some circumstances, molecular function can be completely blocked by cross-linking. The primary detoxification mechanism for scavenging unmetabolized acetaldehyde is sulfur-containing antioxidants. The two most important are cysteine, a conditionally essential amino acid, and glutathione, a cysteine-containing tripeptide (a three-amino-acid polymer). Cysteine and glutathione are active against acetaldehyde (and formaldehyde) because they contain a reduced (unoxidized) form of sulfur called a sulfhydryl group, which contains a sulfur atom bonded to a hydrogen atom (abbreviated SH). Sulfhydryl groups interact with aldehydes to render them incapable of forming cross links. This “mops up” or scavenges any stray acetaldehyde that is not properly metabolized into acetate (acetic acid). Although this is a powerful aldehyde detoxification mechanism, it is easily overwhelmed by the relatively large amounts of alcohol that are typically consumed with alcoholic beverages as compared to the amounts of alcohol and acetaldehyde that are produced through normal metabolism. Fortunately, sulfhydryl antioxidants can easily be fortified through dietary supplementation.
_
In one experiment with rodents [Sprince et al., 1974], a LD-90 dose of acetaldehyde (the dose that would normally kill 90% of the animals) was completely blocked by pretreatment of the animals with cysteine and vitamins B-1 and C. In other words, none of the cysteine-treated animals succumbed to the lethal dose of acetaldehyde! N-Acetylcysteine (NAC) protected almost as well as cysteine. In another rodent experiment [Busnel & Lehman, 1980], alcohol’s ability to inhibit swimming after the alcohol had been completely metabolized was blocked by vitamin C. What this and the previous study suggest is that the pharmacologic and toxic effects of alcohol are different. The pharmacological effect (i.e., intoxication or drunkenness) is not inhibited by vitamin C or cysteine, but the toxic effect (e.g., the hangover, nervous irritability, swimming difficulty) is inhibited.
_
Dosage Suggestions:
Typical doses of cysteine that are sufficient to block a major portion of the toxic effect of alcohol/acetaldehyde are about 200 mg per ounce of alcohol consumed. However, the rapid assimilation and metabolism of alcohol requires both prior and concurrent dosing of cysteine to maintain protection. Furthermore, a multifold excess of vitamin C is required to keep the cysteine in its reduced state and “on the job” against acetaldehyde. You can use capsules (because they dissolve fast) containing 200 mg cysteine plus 600 mg of vitamin C (with or without extra B-1). Take one before you start drinking, one with each additional drink and one when you are finished. It works remarkably well.
_
Additional Nutrients:
There are several other nutrients which may synergize with cysteine and vitamin C. Glutathione, the predominant sulfhydryl antioxidant in the human body, should be considered. Although it is probably quite effective, it is many times more expensive than cysteine and it is not as concentrated; it contains only 10% sulfur compared to 26% sulfur in cysteine. Much larger doses of glutathione must be taken to get the same sulfhydryl concentration, and a significant but unknown amount of glutathione is broken down in the stomach into its component amino acids (glutamate, cysteine and glycine). So while glutathione is a great idea, it’s an expensive great idea. Thiamine (vitamin B-1) and lipoic (thioctic) acid are key sulfur-containing nutrients that may be depleted by alcohol and/or may help with acetaldehyde detoxification. Thiamine was tested by Sprince and colleagues [1974] and found to offer protective benefit to acetaldehyde toxicity when combined with C and cysteine. Whether this is due to a direct interaction between acetaldehyde and the thiamine-bound sulfur or an enhancement of cellular energy production by the active thiamine cofactor (thiamine pyrophosphate) is not known. Alcoholics are known to be thiamine depleted, but whether this depletion is caused by diminished intestinal absorption of thiamine by alcohol or by destruction of thiamine by acetaldehyde is not known. Even under normal circumstances, intestinal absorption of thiamine is not very efficient. In its reduced form, lipoic acid is a powerful sulfhydryl antioxidant. Due to lipoic acid’s twin sulfhydryl groups, it should scavenge aldehydes even more effectively that either cysteine or glutathione. However, supplemental lipoic acid is commercially available only in its oxidized form which contains no sulfhydryl sulfur. It is converted into the reduced form within the mitochondria after absorption from the bloodstream into the cell. So while lipoic acid may be a good cellular protector, it is not as efficient at scavenging acetaldehyde from the bloodstream as cysteine and glutathione. Lipoic acid is also fairly expensive. Within the cells of the liver, however, lipoic acid and acetaldehyde may be readily interacting. The liver metabolizes the largest percentage of ingested alcohol and acetaldehyde levels may be quite high in liver cells. Acetaldehyde may bind to reduced lipoamide (the active lipoic acid factor) to render it inactive. Due to this potential problem, it may be a good idea not to take one’s regular dose of lipoic acid near when one drinks alcohol but rather several hours before and after.
_
Addiction Mechanisms:
The toxicity of acetaldehyde is mitigated to a significant extent by alcohol itself. This provides a strong incentive for people who start drinking alcohol to keep drinking alcohol. When they stop drinking, the toxic effects of acetaldehyde increase as the alcohol is rapidly cleared from the body. This mechanism reinforces “binge” drinking.
_____
Why Alcohol has a Steady State Metabolism rather than a Half Life:
When a drug like diazepam is broken down by the human body the resultant metabolites are harmless. It is for this reason that drugs like diazepam are broken down as quickly as the body can process them–and hence they have a half life. The half life of diazepam is 35 hours on the average. This means that if you take a 10 mg dose of diazepam, then 35 hours later half of it will have been metabolized and only 5 mg will remain. In another 35 hours half of this will be metabolized and only 2.5 mg will remain and so on. When we plot the metabolism of diazepam on a graph we get an exponential curve–in other words–drugs which have a half life have an exponential rate of decay. Chemists refer to this as a First Order Reaction. Alcohol, on the other hand, shows a steady state metabolism not an exponential metabolism. The body of the average human metabolizes around 10 ml of alcohol per hour regardless. When we plot the metabolism of alcohol on a graph we get a straight line–in other words the rate of decay of alcohol is linear. Chemists refer to this as a Zero Order Reaction. The reason why alcohol has a steady state metabolism rather than a half-life metabolism is because the primary decay product of alcohol metabolism–acetaldehyde–is poisonous. The body must eliminate the acetaldehyde produced by the breakdown of alcohol before any more alcohol can be processed in order to avoid acetaldehyde poisoning. This slows down the rate of alcohol metabolism to a Zero Order Reaction rather than a First Order Reaction. Figure below graphically illustrates the difference between steady state metabolism and half life metabolism.
_
_
Alcohol is a central nervous system depressant and it is the central nervous system which is the bodily system that is most severely affected by alcohol (vide infra). The degree to which the central nervous system function is impaired is directly proportional to the concentration of alcohol in the blood. When ingested, alcohol passes from the stomach into the small intestine, where it is rapidly absorbed into the blood and distributed throughout the body. Because it is distributed so quickly and thoroughly the alcohol can affect the central nervous system even in small concentrations. In low concentrations, alcohol reduces inhibitions. As blood alcohol concentration increases, a person’s response to stimuli decreases markedly, speech becomes slurred, and he or she becomes unsteady and has trouble walking. With very high concentrations – greater than 0.35 grams/100 milliliters of blood (equivalent to 0.35 grams/210 liters of breath) – a person can become comatose and die. The American Medical Association has defined the blood alcohol concentration level of impairment for all people to be 0.04 grams/100 milliliters of blood (equivalent to .04 grams/210 liters of breath).
_________
Factors affecting alcohol metabolism and thereby alcohol effects:
Body Weight and Body Type:
Tissues rich in water (muscle) take up more alcohol from the blood than those rich in fat. The amount of water available for alcohol to distribute into depends on body weight and build. A large body weight offers a larger volume for alcohol to be distributed into. (Concentration of alcohol in the blood = Amount of alcohol consumed / Volume of water in the body) In general, the less you weigh the more you will be affected by a given amount of alcohol. As detailed above, alcohol has a high affinity for water. Basically one’s blood alcohol concentration is a function of the total amount of alcohol in one’s system divided by total body water. So for two individuals with similar body compositions and different weights, the larger individual will achieve lower alcohol concentrations than the smaller one if ingesting the same amount of alcohol.
However, for people of the same weight, a well muscled individual will be less affected than someone with a higher percentage of fat since fatty tissue does not contain very much water and will not absorb very much alcohol. A lean person has a greater muscle bulk which provides a larger volume of distribution for the alcohol than an obese counterpart of similar weight. This is because adipose tissue (fat) has a poor blood supply and alcohol is water-soluble and not fat-soluble. So a lean, muscular person will be less affected by drink than someone with more body fat: Water-rich muscle tissues absorb alcohol effectively, preventing it from reaching the brain.
_
Food
Having food in your stomach can have a big influence on the absorption of alcohol. The food will dilute the alcohol and slow the emptying of the stomach into the small intestine, where alcohol is very rapidly absorbed. Peak BAC could be as much as 3 times higher in someone with an empty stomach than in someone who has eaten a meal before drinking. Eating regular meals and having snacks while drinking will keep you from getting too drunk too quickly. The type of food ingested (carbohydrate, fat, protein) has not been shown to have a measurable influence on this affect but the larger the meal and closer in time between eating and drinking, the greater the diminution of peak alcohol concentration. Studies have shown reductions in peak alcohol concentration (as opposed to those of a fasting individual under otherwise similar circumstances) of 9% to 23%.
_
Medication:
If you are taking any medication, it could increase the effects of alcohol. You should always consult your physician or the medical information that accompanies the medication when drinking alcohol in conjunction with any medication.
_
East Asians and American Indians: See alcohol flush reaction vide supra:
_
Older Males: As men age they tend to produce less alcohol dehydrogenase. Older men are likely to become more intoxicated on smaller amounts of alcohol than younger men. Alcohol dehydrogenase in women is apparently not affected by age.
_
Menopausal Women: Apparently hormone changes which occur at menopause can cause menopausal women to become more intoxicated on smaller doses of alcohol.
_
People with Liver Damage: People with liver damage produce less alcohol dehydrogenase than do those with healthy livers and thus can become more intoxicated on smaller doses of alcohol. This phenomenon is referred to as Reverse Tolerance.
_
Frequent Heavy Drinkers: Frequent heavy drinkers produce more alcohol dehydrogenase than other people and thus become less intoxicated on larger quantities of alcohol. These people can metabolize up to 30 ml of alcohol per hour whereas the average person metabolizes only around 10 ml per hour.
_
Diet Soda: Diet soda interacts with alcohol too, so people who drink mixed drinks made with diet soda will become intoxicated more quickly and achieve higher BACS than people drinking identical drinks made with regular soda. Researchers in Adelaide, Australia found that the stomach emptied into the small intestine in 21.1 minutes for the people who drank mixed drinks made with diet soda. When people drank drinks made with regular soda, the stomach emptied in 36.3 minutes (P <.01). Peak blood alcohol concentration was 0.053 g% for the diet drinks and 0.034 g% with the regular drinks.
_____
Gender difference: Why are men and women different?
Alcoholism:
Males had higher rates than females for all measures of drinking in the past month: any alcohol use (57.5% vs. 45%), binge drinking (30.8% vs. 15.1%), and heavy alcohol use (10.5% vs. 3.3%), and males were twice as likely as females to have met the criteria for alcohol dependence or abuse in the past year (10.5% vs. 5.1%).
_
Because of several physiological reasons, a woman will feel the effects of alcohol more than a man, even if they are the same size. There is also increasing evidence that women are more susceptible to alcohol’s damaging effects than are men. Below are explanations of why men and women process alcohol differently.
1. Women on average have a smaller body mass than men. They also have a higher proportion of body fat. As a result of these two factors women have a lesser volume of water in the body (or lean body mass) into which the alcohol can distribute. Because of these two factors, women usually achieve a higher BAC than men do after drinking the same amount of alcohol.
2. Women have lower levels of two enzymes—alcohol dehydrogenase and aldehyde dehydrogenase—that metabolize (break down) alcohol in the stomach and liver. As a result, women absorb more alcohol into their bloodstreams than men.
3. Premenstrual hormonal changes cause intoxication to set in faster during the days right before a woman gets her period. Birth control pills or other medication with estrogen will slow down the rate at which alcohol is eliminated from the body.
4. Women are more susceptible to long-term alcohol-induced damage. Women who are heavy drinkers are at greater risk of liver disease, damage to the pancreas and high blood pressure than male heavy drinkers. Proportionately more alcoholic women die from cirrhosis than do alcoholic men.
_
Are women more vulnerable to alcohol’s effects on the brain?
Women are more vulnerable than men to many of the medical consequences of alcohol use. For example, alcoholic women develop cirrhosis, alcohol–induced damage of the heart muscle (i.e., cardiomyopathy), and nerve damage (i.e., peripheral neuropathy) after fewer years of heavy drinking than do alcoholic men. Studies comparing men and women’s sensitivity to alcohol–induced brain damage, however, have not been as conclusive. Using imaging with computerized tomography, two studies compared brain shrinkage, a common indicator of brain damage, in alcoholic men and women and reported that male and female alcoholics both showed significantly greater brain shrinkage than control subjects. Studies also showed that both men and women have similar learning and memory problems as a result of heavy drinking. The difference is that alcoholic women reported that they had been drinking excessively for only about half as long as the alcoholic men in these studies. This indicates that women’s brains, like their other organs, are more vulnerable to alcohol–induced damage than men’s. Yet other studies have not shown such definitive findings. In fact, two reports appearing side by side in the American Journal of Psychiatry contradicted each other on the question of gender–related vulnerability to brain shrinkage in alcoholism. Clearly, more research is needed on this topic, especially because alcoholic women have received less research attention than alcoholic men despite good evidence that women may be particularly vulnerable to alcohol’s effects on many key organ systems.
___________
Energy from alcohol: alcohol and nutrition:
Ethanol supplies cells with energy and replaces other foods at the level of basic fuel. Ethanol is metabolized to carbon dioxide and water with 2 – 5% being lost through the urine and through respiration. The rate of oxidation is about 75 mg per kilogram of body weight per hour. About half of a group of middle class alcoholics obtained 20 to 39 percent of their dietary calories from alcohol while about one third of the individuals obtained between 40 and 59 percent. The calories provided by alcohol may be calculated by means of the following formula:
0.8 x proof x ounces = kilocalories.
The calorie contribution from the ethanol in wine or beer can be calculated by multiplying the percent alcohol by volume by two, and using this figure as the proof of the beverage. Ethanol in its disguise as a fuel can be considered a non-essential nutrient.
_
One gram of absolute alcohol generates 7 Kcal (7 food Calories) from metabolism in body:
Calories from alcohol are ’empty calories’, they have no nutritional value. Most alcoholic drinks contain traces of vitamins and minerals, but not usually in amounts that make any significant contribution to our diet. Alcohol has lots of calories (about 7 per gram), but your muscles are unfortunately not able to use these calories for fuel. Alcohol calories are not converted to glycogen, a form of stored carbohydrates, and are consequently not a good source of energy for your body during exercise. Drinking alcohol also reduces the amount of fat your body burns for energy. While we can store nutrients, protein, carbohydrates, and fat in our bodies, we can’t store alcohol. So our systems want to get rid of it, and doing so takes priority. All of the other processes that should be taking place (including absorbing nutrients and burning fat) are interrupted.
_
| Calories in Alcohol | |
| Drink | Calories (kcal) |
| A standard glass (175ml) of 12% wine | 126 |
| A pint of 5% strength beer | 170 |
| A glass (50ml) of (17%) cream liqueur |
118 |
| A standard bottle (330ml) of 5% alcopop |
237 |
| A double measure (50ml) of 17.5% fortified wine |
65 |
_
On a given day, one-third of men and 18% of women consume calories from alcoholic beverages. Although 67% of men and 82% of women do not consume any alcoholic beverages on a given day, almost 20% of men and 6% of women consume more than 300 calories from alcoholic beverages, which is equivalent to 2 or more 12-ounce (oz) beers, more than 2½ glasses of wine (12.5 oz), or more than 4.5 oz of spirits . On a given day, consumers of alcoholic beverages obtain approximately 16% of their total caloric intake from alcoholic beverages.
_
_
Alcohol as Food energy:
Alcoholic beverages are a source of food energy. The USDA uses a figure of 6.93 kcal per gram of alcohol (5.47 kcal per ml) for calculating food energy. In addition to alcohol, many alcoholic beverages contain carbohydrates. For example, beer usually contains 10–15 g of carbohydrates (40–60 kcal) per 12 US fluid ounces (350 ml). However, aside from the direct effect of its caloric content, alcohol is known to potentiate the insulin response of the human body to glucose, which, in essence, “instructs” the body to convert consumed carbohydrates into fat and to suppress carbohydrate and fat oxidation. Ethanol interferes with carbohydrate energy metabolism. Liver and muscle glycogen are depleted. As cellular toxin, ethanol is catabolic and promotes structural tissue loss. The catabolic effect causes a greater loss of weight than caloric input can replace in the form of fat stores. Typically, fat distribution shifts to the belly and trunk, leaving the extremities skinny and weak.
_
Nutritional value of alcohol:
While alcohol supplies calories (7 Kcal per gram), these are devoid of nutrients such as minerals, proteins, and vitamins. Alcohol use inhibits absorption of important nutrients such as thiamin, vitamin B12, folic acid, and zinc. In addition, alcohol can decreases their storage in the liver with modest effects on folate, pyridoxine (B6), thiamine (B1), nicotinic acid (niacin, B3), and vitamin A.
________
Low calorie alcoholic drinks:
Alcoholic drinks are high in calories particularly common beverages such as beer and cocktails. However, by cutting back on the amount you drink, it can significantly help to reduce your calorie intake. It can be useful to know that many alcoholic brands now have low alcohol alternatives containing less calories. Some light wines have under 80 calories in a 175ml glass compared to 159 calories in the same measure of 13% ABV wine. Another way to drink less calories is to opt for a low calorie mixer such as a diet coke or soda. Drinking water or low calorie soft drinks between alcoholic drinks is not only a good way to reduce your calorie intake but also helps to reduce the amount of units you are drinking.
_
Sensation of warmth:
In cold climates, potent alcoholic beverages such as vodka are popularly seen as a way to “warm up” the body, possibly because alcohol is a quickly absorbed source of food energy and because it dilates peripheral blood vessels (cardiovascular dilation). This is a misconception because the “warmth” is actually caused by a transfer of heat from the body’s core to its extremities, where it is quickly lost to the environment. However, the perception alone may be welcomed when only comfort, rather than hypothermia, is a concern.
_
Aperitifs and digestifs:
An aperitif is any alcoholic beverage usually served before a meal to stimulate the appetite while a digestif is any alcoholic beverage served after a meal, in theory to aid digestion. Fortified wine, liqueur, and dry champagne are common aperitifs. Because apéritifs are served before dining, the emphasis is usually on dry rather than sweet.
_
Alcohol and energy drinks:
Alcohol is a depressant which means it slows down the brain’s functions and can act as a sedative when drink a lot and you might slur your words, have slower reflexes and feel sleepy. The caffeine in energy drinks, on the other hand, is a stimulant, which produces the chemical adrenalin in the body, making you feel more alert. If you mix the two, you will feel the stimulant effects of the caffeine more strongly, masking the interference caused by alcohol to reaction time, memory and other processes in the brain. This makes mixing alcoholic drinks with energy drinks a very risky thing to do, and a worrying trend. They may make you feel like you can stay out all night but mixing alcohol mixed with energy drinks can be a dangerous combination. Energy drinks can mask the effects of alcohol, and make you ‘Wide awake drunk’, so you may underestimate your feeling and end up drinking more alcohol than you normally would. Mixing alcohol and energy drinks can mean you consume more sugar, calories and caffeine than drinking alcohol by itself. You could also experience increased physical and psychological side effects from drinking this combination. Since 2006, sales of energy drinks have increased by around 12% year on year in the UK. At the same time, mixing spirits and liqueurs with them has become increasingly popular. It is common to see bars, pubs and clubs promoting these drink combinations, and you can buy energy drinks and bottles of alcohol separately in supermarkets and off-licences to mix at home. But recent research has found that mixing energy drinks with alcohol could be more risky than drinking alcohol on its own, or with a more traditional mixer. You
•can drink more alcohol, become wide awake drunk and are more likely to take risks
•are likely to experience increased physical and psychological side effects, such as heart palpitations, problems sleeping, feeling tense or agitated
•can consume large amounts of caffeine, which in this quantity, can cause anxiety and panic attacks
•can consume a lot of calories and sugar, that can make you put on weight, adding to the risk of developing type 2 diabetes which you face when you drink alcohol on its own
•increase your chances of developing short and long-term health problems.
_
Alcohol concentration and carbonation of drinks: The effect on blood alcohol levels: A study:
Alcohol absorption and elimination vary considerably amongst individuals, and are subject to influences from a variety of factors. The effects of alcohol concentration and beverage mixer type on the rate of alcohol absorption, in a controlled environment were studied. 21 subjects (12 male, 9 female) consumed a solution containing alcohol, on three separate occasions. The three solutions were, A: Neat vodka (37.5 vol%), B: Vodka mixed with still water (18.75 vol%), C: Vodka mixed with carbonated water (18.75 vol%). The volume of alcohol each subject consumed was determined by Widmark’s equation. The alcohol was drunk in a 5 min period following an overnight fast and breath alcohol concentrations were measured over a 4 h period using a breathalyzer. 20/21 subjects absorbed the dilute alcohol at a faster rate than the concentrated alcohol. The difference between the absorption rates was found to be significant (p < 0.001). The use of a carbonated mixer had varying effects on the alcohol absorption rate. 14/21 subjects absorbed the alcohol with the carbonated mixer at a faster rate, with 7 subjects showing either no change or a decrease in rate. The mean absorption rate for solution C was 4.39 ± 0.45 (mg/100 ml/min), and the difference between this absorption rate and that with the still mixer (1.08 + 0.36) was significant (p = 0.006).
___________
Does gut produce alcohol?
Fermentation occurs when enzymes, typically produced by yeast, convert sugar molecules in grapes or grains into ethanol. That process can also happen in your digestive system through microbes, spiking every 100 ml of blood with 6 to 9 mg of alcohol in 24 hours which is far lower than body’s elimination rate resulting in zero blood alcohol content. Several of the benign bacteria in the intestine use fermentation as a form of anaerobic metabolism. This metabolic reaction produces ethanol as a waste product, just like aerobic respiration produces carbon dioxide and water. Thus, human bodies contain some quantity of alcohol endogenously produced by these bacteria and yeast. In rare cases, this can be sufficient to cause “auto-brewery syndrome” in which intoxicating quantities of alcohol are produced. Japanese doctors have observed patients with auto-brewery syndrome in which high levels of candida yeast in the intestines churn out so much alcohol that they can cause drunkenness. Auto-brewery syndrome has never been convincingly reported outside Japan. Why? Because 50 % Japanese have mutant aldehyde dehydrogenase giving alcohol flush reaction.
_
_
Review of Literature:
Gut Fermentation Syndrome is described as a syndrome whereby patients become intoxicated without ingesting alcohol. In addition to the term Auto-Brewery, this syndrome has also been called Drunkenness Disease and Endogenous Ethanol Fermentation. The underlying mechanism is thought to be an overgrowth of yeast in the gut whereby the yeast ferments carbohydrates into ethanol. The earliest cases of this phenomenon were de- scribed in Japan. Iwata detailed 12 cases prior to 1972. In 1976, Kaji and others described the case of a 24- year-old female who became intoxicated after consuming carbohydrates which fermented in the gastrointestinal tract. In this situation the causative organisms were determined by cultures to be Candida albicans and Candida krusei. This patient restricted her intake of carbohydrates in the diet and received a course of an antifungal agent whereby all symptoms of her intoxication subsided. Two cases of particular note were identified in children. Dahshan and Donovan described the case of a 13-year-old girl with short gut syndrome who became intoxicated after ingesting carbohydrates. She had been placed in a rehabilitation facility with no access to alcohol. Aspirates from her small intestines grew Candida glabrata and Saccharomyces cerevisiae. After treatment with fluconazole, the symptoms resolved. The other case was a 3-year-old girl with short bowel syndrome who became intoxicated after ingesting a carbohydrate-rich fruit drink. Cultures from the gastric fluids demonstrated Candida kefyr and Saccharomyces cerevisiae. Again a course of fluconazole eliminated the symptoms.
________________
Effects of alcohol on human body:
Alcohol affects each of us differently – depending on a range of factors including:
•weight;
•amount of muscle or fat;
•gender;
•age;
•other medicines and drugs in the system;
•other chemicals in drinks;
•how fast you are drinking;
•the amount of food in the stomach;
•drinking history;
• tolerance to alcohol;
• physical health; and
•mental health and emotional state.
_
Relatively low doses of alcohol (one or two drinks per day) have potential beneficial effects of increasing high-density lipoprotein cholesterol and decreasing aggregation of platelets, with a resulting decrease in risk for occlusive coronary disease and embolic strokes. Red wine has additional potential health-promoting qualities at relatively low doses due to flavinols and related substances, which may work by inhibiting platelet activation. Modest drinking might also decrease the risk for vascular dementia and, possibly, Alzheimer’s disease. However, any potential healthful effects disappear with the regular consumption of three or more drinks per day, and knowledge about the deleterious effects of alcohol can both help the physician to identify patients with alcohol abuse and dependence, and to supply them with information that might help motivate a change in behavior.
__
Consequences of Alcohol Use:
Drinking consequences represent a domain independent of dependence symptoms and should be measured separately. While many screening instruments and diagnostic clinical interviews contain interview questions designed to identify negative consequences, having your clients complete a self-administered questionnaire will provide a detailed picture of negative consequences across a variety of life domains, and in the case of marital or family assessment, from different family member perspectives. A thorough assessment of consequences also can be useful when evaluating treatment effects, since these measures have been shown to be sensitive to changes in drinking-related problems over time. Communicating these assessment results often is useful in helping the drinker appreciate the connection between drinking and negative consequences across life domains.
The Drinker Inventory of Consequences (DrInC) is a 50-item checklist of potentially adverse drinking consequences that provides summary scores in five areas:
- Interpersonal
- Physical
- Social
- Impulsive
- Intrapersonal
_
Short-term effects of alcohol can take on many forms. The drug alcohol, to be specific ethanol, is a central nervous system depressant with a range of side-effects. Cell membranes are highly permeable to alcohol, so once alcohol is in the bloodstream it can diffuse into nearly every biological tissue of the body. The concentration of alcohol in blood is usually measured in terms of the blood alcohol content. The amount and circumstances of consumption play a large part in determining the extent of intoxication; for example, eating a heavy meal before alcohol consumption causes alcohol to absorb more slowly. Hydration also plays a role, especially in determining the extent of hangovers. After excessive drinking, unconsciousness can occur and extreme levels of consumption can lead to alcohol poisoning and death (a concentration in the blood stream of 0.40% will kill half of those affected). Alcohol may also cause death by asphyxiation from vomit. Alcohol is an addictive drug that can greatly exacerbate sleep problems. During abstinence, residual disruptions in sleep regularity and sleep patterns are the greatest predictors of relapse.
_
Alcohol is among the most widely used and abused drugs in the world, yet our understanding of the mechanisms by which it regulates brain function and behavior is rudimentary. Some of the difficulties in understanding ethanol’s mechanism of action derive from the fact that, unlike other abused drugs (such nicotine, cocaine, and heroin), ethanol appears to have a broad spectrum of molecular targets in the nervous system. Ethanol readily crosses the blood-brain barrier and intercalates into cell membranes, changing membrane fluidity. It has been argued that ethanol’s effects in the nervous system are caused primarily by non-specific alterations in membrane properties (Wood et al., 1991). However, increasing evidence implicates certain proteins—mostly membrane proteins—as direct targets of ethanol in the nervous system (Peoples et al., 1996). How ethanol acts on these proteins and how these effects relate to ethanol-induced behaviors and the complex process of alcohol addiction is poorly understood. When ingesting low doses of ethanol, most humans exhibit responses such as disinhibition and euphoria. Higher doses cause incoordination and confusion, and in extreme cases, coma and death. The degree of response to ethanol is at least in part due to genetic predispositions. For example, young men with a family history of alcoholism are less sensitive to the motor, perceptual, and biochemical changes induced by intoxicating levels of ethanol than those from families without alcoholism (Schuckit and Gold, 1988; Schuckit et al., 1996). In addition, when reexamined a decade later, a significantly higher proportion of subjects with reduced ethanol sensitivity had developed alcoholism (Schuckit, 1994; Schuckit and Smith, 1996). These studies show that the initial level of response to ethanol is influenced genetically and may be a good predictor of risk for alcoholism. Recently, several chromosomal regions that harbor genes that may relate to this low responsiveness to ethanol have been identified (Wilhelmsen et al., 2003). A causal relationship between ethanol sensitivity and risk for alcoholism has however not been demonstrated and the biological bases for this correlation remain unknown. Yet, these studies imply that an understanding of fairly simple behaviors induced by acute ethanol exposure may help gain insights into the more complex process of alcohol addiction.
_
If you regularly drink alcohol in excess, it is likely to cause problems. Some of the known short and long term effects of alcohol misuse include:
Short-term effects
•Alcohol poisoning, coma and death
•Blackouts
•Blurred vision
•Drowning
•Fires
•Flushed appearance
•Headache
•Injuries associated with falls, accidents, violence and intentional self-harm
•Intense moods (aggression, elation, depression)
•Lack of co-ordination
•Loss of inhibitions and a false sense of confidence
•Motor vehicle, bicycle and pedestrian accidents
•Nausea and vomiting
•Reduced concentration
•Slower reflexes
•Slurred speech
_
Long-term effects
•Alcohol dependency
•Alcohol related brain injury
•Cancers (including cancer of the mouth, pharynx, larynx, oesophagus, bowel (in men) and breast (in women)
•Cirrhosis and liver failure
•Concentration and long-term memory problems
•Heart and cerebrovascular diseases including hypertension and stroke
•Poor nutrition
•Problems with the nerves of the arms and legs
•Sexual and reproductive problems (impotence, fertility)
•Skin problems
•Stomach complaints and problems
•Family and relationship problems
•Poor work performance
•Legal and financial difficulties
_
The effects of alcohol on memory
Performing your best involves learning plays or strategies for an event. Alcohol impairs the functioning of the hippocampus, a part of your brain that is vital to the foundation of memories. If you can’t form new memories, you can’t learn and store information. Creating memories is a complex process that takes a long time, and many memories are established even when you’re not thinking about them. In fact, the majority of memory foundation happens when you sleep. Alcohol disrupts the sequence of duration of your sleep cycle (even if you drink up to six hours before you go to sleep!), which reduces your brain’s ability to process information.
_
Why does alcohol make you urinate more?
Alcohol is a diuretic. It acts on the kidneys to make you pee out much more than you take in which is why you need to go to the toilet so often when you drink. In fact for every 1g of alcohol drunk, urine excretion increases by 10ml. Alcohol reduces the production of a hormone called vasopressin (ADH), which tells your kidneys to reabsorb water rather than flush it out through the bladder. So the popular notion that you urinate more as you drink more fluid during alcohol session is wrong. You urinate more due to reduced ADH and in fact it may cause dehydration.
_
How alcohol affects your skin:
Alcohol’s effect on your skin is similar to its effect on the rest of your body: it steals the good (hydration) and leaves the bad (dryness, bloating, redness). When you drink alcohol, it hinders the production of vasopressin — an anti-diuretic hormone. This causes your kidneys to work extra hard to remove excess water from your system, sending water to your bladder instead of your organs. Don’t forget that your skin is the largest organ in the body — and drinking a lot of alcohol leaves it dehydrated. When skin is dry, it is much more likely to wrinkle and make you look older than you are. Alcohol also robs your body of Vitamin A which is essential for cell renewal and turnover, so your skin could take on a dull gray appearance. Staying hydrated will obviously have opposing effects: smoothing out wrinkles, leaving your skin looking bright, young and fresh. Drinking water is the only way to combat the drying effects of alcohol, hydrating from within. Alcohol can also affect preexisting conditions like rosacea, causing it to worsen or flare up more often. Alcohol increases your blood flow, often causing blood vessels in your face to dilate (sometimes permanently) and often burst, leaving behind broken capillaries and red spots that are difficult to get rid of. What’s worse, drinking too much doesn’t only affect the appearance of your skin, it will dehydrate your hair, making it more prone to breaking and split ends.
_
Alcohol Disrupts the Molecular Circadian Clock:
The changes observed in the behavioral and biological systems also are observed on the molecular level as a disrupted molecular circadian clock, an effect that is evident both in vitro and in vivo. Exposure of intestinal epithelial cells to alcohol increases the levels of circadian clock proteins CLOCK and PER2. Likewise, alcohol-fed mice have disrupted expression of Per1–Per3 in the hypothalamus, human alcoholics demonstrate markedly lower expression of Clock, BMAL1, Per1, Per2, Cry1, and Cry2 in peripheral blood mononuclear cells compared with nonalcoholics, and in humans alcohol consumption is inversely correlated to BMAL1 expression in peripheral blood cells. The alcohol-induced changes seem to have long-lasting effects on the circadian clock, particularly when the exposure occurs early in life, which may be the consequence of epigenetic modifications. For example, neonatal alcohol exposure in rats disrupts normal circadian-clock expression levels and expression patterns over a 24-hour period. These examples illustrate the ability of alcohol to have profound and long-lasting effects on clock-gene expression in multiple organs and tissues. The mechanisms by which alcohol disrupts circadian rhythmicity are likely a consequence of alcohol metabolism and alcohol-induced changes in intestinal barrier integrity. SIRT1, which regulates the molecular circadian clock, is highly sensitive to the cellular NAD+/NADH ratio. Therefore, a perturbation in the availability of NAD+ (as a consequence of alcohol metabolism) would be one mechanism by which alcohol could disrupt the molecular circadian clock and resulting circadian rhythms. Another mechanism by which alcohol can exert a negative influence on circadian rhythmicity is by promoting intestinal hyperpermeability. Alcohol disrupts intestinal barrier integrity in vitro, in rodents , and humans. Intestinal hyperpermeability allows luminal bacterial contents such as endotoxin to translocate through the intestinal epithelium into the systemic circulation. Endotoxin can disrupt circadian rhythms. LPS administered to rodents impairs the expression of Per in the heart, liver, SCN, and hypothalamus and suppresses clock gene expression in human peripheral blood leukocytes . Thus, intestinal-derived LPS may be one mechanism by which alcohol disrupts circadian rhythmicity. Most studies of alcohol’s effects on human circadian rhythms have been conducted in chronic alcoholics undergoing alcohol abstinence and associated withdrawal. Several studies of abstinent alcoholics during acute and/or longer term alcohol withdrawal have reported abnormalities in the amplitude, timing, and/or patterning of circadian rhythms. A better understanding of the mechanisms by which circadian disruption affects health outcomes such as cancer, inflammation, metabolic disease, and alcohol-induced pathology is critical. This information may lead to the development of chronotherapeutic approaches to prevent and/or treat a wide variety of conditions that are promoted or exacerbated by circadian- rhythm disruption and may lead to better risk stratification for individuals who are at risk for developing chronic conditions.
_________
Alcohols, sports and exercise:
What impact does alcohol have on your fitness regime?
Unfortunately, toasting your gym session with post-exercise drinks at home or down the pub can undo all the good work you’ve just put in. There’s 180 calories in the average pint of lager and 159 calories in a 175ml glass of 13% ABV white wine, so you could end up topping up the weight you thought you’d lost through your fitness regime in no time at all. For instance, if you’ve just run for half an hour it will only take two pints to put back on the calories you’ve just burned off through exercise. The way alcohol is absorbed by the body can also reduce the amount of fat you’re able to burn by exercising. Because your body isn’t designed to store alcohol, it tries to expel it as quickly as possible. This gets in the way of other processes, including absorbing nutrients and burning fat. So as well as slowing down the burning of calories, alcohol gets in the way of the nutritional benefits of the healthy meals you eat.
_
Running on empty:
Fitness experts agree that to get the most from cardiovascular exercise such as running or swimming, you have to put in the physical effort. But while your hangover may make a less hectic workout feel welcome, it’s harder to build up the head of steam you need to stay in shape when you have a headache, and nausea is beginning to kick in. The night before’s alcohol leaves your body dehydrated, even before your session starts.
Body benefits:
If you feel like the balance between alcohol and exercise is veering too much towards the former, then it’s a good idea to consider cutting down. You can still enjoy a drink and maintain a healthy lifestyle; the key is sticking to the government’s daily unit guidelines. Re-assessing your relationship with alcohol doesn’t just do wonders for the effectiveness of your workout; it can also boost your general health too. In fact, if you’re looking to reduce your stress levels, lose weight and look your best, then reducing your intake will help. Best of all, cutting down delivers more than just short-term results. Drinking within the guidelines means you’re actively protecting your general health and reducing your risk of developing heart disease, having cancer and getting problems with your liver in the future as well.
_
Alcohol and sports:
Alcohol can lessen hand tremor and improve performance in ‘aiming’ sports such as archery, fencing, and shooting, but because of its potentially harmful effects, its use is restricted by some sports federations. Alcohol and its after-effects decrease aerobic fitness. Tests of rugby players showed that those suffering from a hangover 16 hours after drinking alcohol performed on average almost 12 per cent worse than when they had no hangover. Alcohol is no great friend to the athlete, nor is it to those on a weight-loss diet. Each gram of pure alcohol provides 7 Kcal of energy. In addition, alcoholic beverages often contain sugar and other nutrients, increasing their calorific value. A single measure of spirits contains about 50 Calories, and one pint of lager contains about 170 Calories. Drinking too much alcohol can lead to obesity because some is converted to fat. It is generally accepted that heavy drinking is not compatible with serious sport participation. Alcohol (ethanol) is on the World Anti-Doping Agency’s 2005 Prohibited List. It is considered prohibited when in-competition blood levels exceed the doping violation threshold of the relevant sports Federation. The following lists the doping threshold for each Federation aeronautic, FAI (0.20 g l−1); archery, FITA (0.10 g l−1); automobile, FIA (0.10 g l−1); billiards, WCBS (0.20 g l−1); boules, CMSB (0.20 g l−1); karate, WKF (0.10 g l−1); modern pentathlon, UIPM (0.10 g l−1) for disciplines involving shooting; motorcycling, FIM (0.00 g l−1); skiing, FLS (0.10 g l−1). Alcohol is classified in the Prohibited List as a ‘specified substance’. Specified substances are so generally available that it is easy for an athlete to unintentionally violate anti-doping rules. Doping violations involving a specified substance, such as a alcohol, may result in a reduced sanction if the athlete can establish that its use was not intended to enhance sport performance. Use of alcohol is banned at some sports venues (such as Scottish soccer grounds) because of its association with crowd violence.
_
Alcohol and your heart rate:
Most worryingly, drinking can increase the potential for unusual heart rhythms. This is a risk which significantly increases during exercise up to two days after heavy alcohol consumption.
_
How does Alcohol affect Your Athletic Performance?
Athletes should be especially careful about indulging because they run the risk of jeopardizing their athletic performance when they drink. Muscle health is the key to successful athletic performance, and science shows that alcohol can rob you of your hard work in the weight room. Here’s why:
• Alcohol use impairs muscle growth – Not only does working out under the influence increase your likelihood of injury, but it can also impede muscle growth. Long-term alcohol use diminishes protein synthesis, resulting in a decrease in muscle growth. Even short-term alcohol use can affect your muscles.
•Alcohol dehydrates your body – If you want to optimize your athletic performance, then you want your recovery from sore muscles to be as fast as possible. Alcohol has been shown to slow muscle recovery because it is a powerful diuretic that can cause dehydration and electrolyte imbalances. When dehydrated, an athlete is at a greater risk for cramps, muscle pulls, and muscle strains.
• Alcohol prevents muscle recovery – Getting enough rest is essential to building bigger and stronger muscles. However, because drinking alcohol negatively affects your sleep patterns, your body is robbed of a chemical called human growth hormone, or HGH, when you drink. HGH plays an integral role in building and repairing muscles, but alcohol can decrease the secretion of HGH by as much as 70 percent. Additionally, when alcohol is consumed in amounts typical with binge drinkers, it can reduce serum testosterone levels. Testosterone is essential for the development and recovery of your muscles. Decreases in testosterone are associated with decreases in lean muscle mass and muscle recovery, which can impair performance.
• Alcohol affects your energy metabolism- After alcohol is absorbed through your stomach and small intestine and moves into your cells, it can disrupt the water balance in your body. An imbalance of water in your muscle cells can hamper their ability to produce adenosine triphosphate (ATP), which provides the fuel that is necessary to help your muscles contract. A reduction in your body’s ATP can result in a lack of energy and loss of endurance. Also, when you are metabolising or breaking down alcohol the liver cannot produce as much glucose, which means you have low levels of blood sugar. Exercise requires high levels of sugar to give you energy. If your liver is not producing enough glucose, your performance will be adversely affected. If your body is forced to run from your supplies of fat rather than blood sugar, you will be slower and have less energy and won’t be able to exercise as intensely. As a result, your coordination, dexterity, concentration and reactions could be adversely affected too.
•Speeding the recovery of sore muscles and injuries is essential to the gains from a workout. On occasion, when a student is injured or sore and doesn’t work out, they may see this as an opportunity to use alcohol. The use of alcohol causes dehydration and slows your body’s ability to heal itself.
_
Brain damage caused by drinking Alcohol could be reversed by Aerobic Exercise:
Remarkably, a large body of new research has revealed that aerobic exercise not only builds muscle, it builds brain tissue. Aerobic exercise stimulates the birth of new neurons in specific parts of the brain where neurons can still divide in adults, including the hippocampus, which is involved in learning. Exercise protects against cognitive decline in aging and neurological diseases, including Alzheimer’s, and it strengthens the integrity of white matter tracts to the extent that the beneficial changes can be seen on an MRI. These recent discoveries motivated researchers Hollis Karoly and colleagues at the University of Colorado to ask whether aerobic exercise could prevent the damaging effects of heavy alcohol consumption on white matter in the human brain. Identifying any new treatment that could reverse brain damage caused by alcohol consumption would have profound health benefits for tens of thousands of individuals who consume alcohol. According to this new study, there is an effective treatment that requires no medication and has no negative side effects — aerobic exercise. To answer this intriguing hypothesis, the researchers compared the level of alcohol consumption in a population of men and women between the ages of 21-55 with the integrity of their white matter. This was accomplished by using an MRI brain imaging method that is highly sensitive to white matter integrity, called diffusion tensor imaging (DTI). Three conclusions were supported by the data, two of them confirming what was already shown in the literature, and the new finding reported here.
(1) White matter tracts in the brain are strongly affected by alcohol consumption. This was seen throughout the brain, but it was especially pronounced in some fiber tracts known to be necessary for higher level thinking and memory and other functions impaired in those who abuse alcohol. For example, the external capsule (EC) and superior longitudinal fasciculus (SLF) were especially sensitive to damage caused by drinking alcohol. When white matter integrity is graphed against the total number of alcoholic drinks consumed in 60 days (or other measures of alcohol consumption), white matter integrity drops in direct proportion to the amount of alcohol consumed.
(2) Conversely, white matter integrity increased in people who reported doing aerobic exercise in the last three months, and greater improvements were seen in those who did more than the average amount of exercise.
Both of these effects confirm and extend the result of other studies. The third result was that in people who exercised, the loss of white matter integrity caused by alcohol consumption was prevented or reduced, depending on how much exercise was done and which particular white matter tract in the brain is examined. For example, in people who reported doing a moderate amount of aerobic exercise in the last three months (that is, the average amount of aerobic exercise among all participants), the integrity of the EC white matter tract was maintained even for the heaviest drinkers. Even better results in preserving white matter integrity were seen in subjects reporting an above average level of aerobic exercise. The steep, straight-line drop in white matter integrity plotted against the amount of alcohol consumption, leveled out completely in those participating in high levels of aerobic exercise; that is, no deleterious effects of alcohol consumption at any level of consumption could be seen in the white matter tracts of these people. Again, the magnitude of the effects differed somewhat in different white matter tracts, but in general the beneficial effects of exercise were evident throughout many white matter tracts in the brain. The study also sorted the data according to self-reporting of cannabis use and tobacco smoking, because both of these have been implicated in white matter damage. Even accounting for these other effects on white matter structure, the beneficial effects of aerobic exercise on white matter integrity were still seen. The researchers conclude that the most damaging effects of alcohol consumption on white matter integrity are seen in those people who do not exercise regularly, “alcohol consumption did not appear to be associated with white matter damage among individuals who exercised regularly.” The design of this experiment can only provide correlative data. The associations revealed here must be tested in further experiments to show that there is a causal link between exercise and protection against white matter damage caused by drinking alcohol, and to uncover the biological mechanisms for the protection. However, these findings revealing the protective effects of aerobic exercise on preventing white matter brain damage in drinkers are compelling and valuable, regardless of whatever biological link to explain this correlation may be found in the future.
________
Alcohol and pain:
In everyday life, many people continue to deal with pain by self-medicating with alcohol. Due to its ability to depress the central nervous system (CNS), it slows down the brain and nervous system, and delivers a certain amount of pain relief. It also has muscle relaxant and sedating properties. Unfortunately, there is a tendency for alcohol to be abused (alcohol abuse and alcoholism), and the use of alcohol for pain relief can easily cause problems. It is not uncommon for the amount of alcohol used to become excessive. If combined with the wrong medications, alcohol can have an additional lowering (depressant) effect on the nervous system, leading to disastrous consequences. With prolonged use and excess consumption, the body begins to build up a tolerance to the effects of alcohol. It takes more alcohol to produce the same results. Increased amounts of alcohol over time can cause many health problems, affecting all organ systems in the body. This includes problems such as impaired brain function and memory, to peptic ulcers and liver cirrhosis. In addition, because alcohol is a major depressant, it will exacerbate any underlying depression and is also dangerously habit-forming (addictive). Alcohol may provide temporary relief of pain, but may worsen the problems that pain sufferers may face. In older population, many people suffer from pain and a large number of people drink alcohol excessively. There have been some studies performed, to examine the relationship between pain and alcohol problems amongst older adults. 401 adults living within the community were studied over a three year period. At the beginning of the study, more of the problem drinkers (people who drank too much alcohol) than non-problem drinkers reported having moderate to very severe pain (43% versus 30%). A greater proportion of problem drinkers used alcohol to treat their pain (38% versus 14%).
Results from the study show that the level use of alcohol to manage pain predicted:
•an increase amount of chronic health problems and injuries in men
•more drinking problems in women after three years.
In conclusion, whilst alcohol is used to self medicate and manage pain, there are many problems with its use. Large doses may seem to help temporarily, but more effective, safe and long term pain killers should be used to provide relief from pain.
__________
Alcohol and sleep:
Sleep is a necessary activity for all people. Lack of sleep can lead to severe disorders including increased risk for mood disorders, impaired breathing, and heart disease. Since the average adult appears to need about 7.5 to 8 hours of sleep per night it is important that people be aware that ethanol can induce sleep problems and sleep disorders. Normal sleep is characterized as having four different NREM stages plus an additional type of sleep called REM or rapid eye movement sleep. The four stages are generally characterized by having different types of electrical activity as measured by an electroencephalogram (EEG). Stages 1 and 2 have more rapid electrical activity, yet still slower than that seen during waking. Slow wave sleep (SWS) is most characteristic of stages 3 and 4 which are the stages of deep sleep. REM sleep, however, is characterized by having more rapid brain waves somewhat similar to those seen while one is awake. Dreaming occurs during REM, so it is interesting that the brain wave pattern during REM looks somewhat like that during wakefulness. After first going to sleep, one progresses from stage one to stage four sleep. During the night one cycles though the different stages from one to four and return to one. REM sleep occurs during most of the cycles. As the night progresses, the deeper sleep stages become less frequent, but REM sleep tends to increase in frequency. Interestingly, studies have shown that obtaining REM sleep is important since deprivation of REM will lead to an increased amount of REM during later sleeping opportunities.
The effect of ethanol on sleep can take several forms. These include:
1. Altering the time to fall asleep
2. Disrupting the sequence of sleep
3. Altering the total time of sleep
4. Diminishing the duration of particular types or stages of sleep.
Though it is true that drinking before bedtime may cause one to fall asleep sooner, it disrupts the second half of sleep. The person may have fitful sleep by awakening from dreams and having trouble returning to sleep. This sleep disruption may manifest the next day in fatigue and sleepiness. Persons who drink too much or elderly people and women who achieve higher blood alcohol concentrations my have increased problems. It is interesting that even if ethanol is drunk earlier in the day and has cleared the system, it still has the potential to disrupt sleep later in the night. This would suggest that ethanol acts on brain systems, which are still disrupted at a later, time. Neurotransmitters (NTs) serotonin and norepinephrine are important in the regulation of sleep. Serotonin seems primarily associated with sleep onset and with regulation of SWS, while norepinephrine seems to regulate REM and arousal. Since it known that ethanol affects both serotonin and norepinephrine, possible mechanisms for the effects of ethanol on sleep are via ethanol’s action on these NTs.
_
How alcohol affects your sleep patterns:
Alcohol interferes with the normal sleep process. When you drink a lot of alcohol close to bedtime, you can go straight into deep sleep, missing out on the usual first stage of sleep. Deep sleep is when the body restores itself, and alcohol can interfere with this. As the alcohol starts to wear off, your body can come out of deep sleep and back into REM sleep, which is much easier to wake from. That’s why you often wake up after just a few hours sleep when you’ve been drinking. In the course of a night you usually have six to seven cycles of REM sleep, which leaves you feeling refreshed. However, if you’ve been drinking you’ll typically have only one to two, meaning you can wake feeling exhausted. If you drink a lot, you may have to get up in the night to go to the toilet. And it’s not just the liquid you’ve drunk that you’ll be getting rid of. Alcohol is a diuretic, which means it encourages the body to lose extra fluid though sweat too, making you dehydrated. Drinking can also make you snore loudly. It relaxes the muscles in your body, which means the tissue in your throat, mouth and nose can stop air flowing smoothly, and is more likely to vibrate. Alcohol relaxes muscles in the pharynx, which can cause snoring and exacerbate sleep apnea; symptoms of the latter occur in 75% of alcoholic men older than age 60 years. Patients may also experience prominent and sometimes disturbing dreams. All of these sleep problems are more pronounced in alcoholics, and their persistence may contribute to relapse. So, all in all alcohol can equal a fitful night’s sleep.
_
How sleep is affected by alcohol, causing impaired memory:
For most students, studying and preparation for tests is essential to academic performance. When alcohol is in your system your brain’s ability to learn and store information is inhibited due to compromising the hippocampus, vital to the formation of new memories. Memories are solidified during sleep. Alcohol interferes with your sleep cycle by disrupting the sequence and duration of normal sleep, thus reducing your brain’s ability to retain information.
•The REM stage of sleep is compromised after a night of drinking, which is vital to memory.
•Even though someone who has been drinking might look as if they are crashed out, they will not be getting the deep sleep that is needed to recharge their batteries.
•The sleep deprivation suppresses normal hormonal levels decreasing oxygen availability and consumption, thus decreasing endurance.
_
People are still likely to feel tired after sleeping following a night of drinking as they will have missed out on quality sleep.
•Consuming five or more alcoholic beverages in one night can affect brain and body activities for up to three days.
•Two consecutive nights of drinking five or more alcoholic beverages can affect brain and body activities for up to five days.
•Attention span is shorter for periods up to forty-eight hours after drinking.
•Even small amounts of alcohol BAC of .03 can persist for a substantial period of time after the acute effects of alcohol impairment disappear.
____________
Alcohol and weight:
There are 7 calories in each gram of alcohol. This is compared to fat, which has 9 calories per gram and 4 calories in carbohydrates and protein. This makes alcohol pretty high in calories, and since it doesn’t provide much nutritional benefit, the calories that it provides are considered empty calories. When you drink alcohol, it’s broken down into acetate (basically vinegar), which the body will burn before any other calorie you’ve consumed or stored, including fat or even sugar. So if you drink and consume more calories than you need, you’re more likely to store fat & sugar from food because your body is getting all its energy from the acetate in the beer you sucked down. Further, studies show that alcohol temporarily inhibits “lipid oxidation”— in other words, when alcohol is in your system, it’s harder for your body to burn fat that’s already there. Alcohol can’t be stored in the body, so when you drink alcohol, your body will use the alcohol as fuel before other energy sources. All these lead to accumulation of fat in the liver and body.
What does the evidence suggest?
A study, published in the American Journal of Clinical Nutrition, looked at whether regular alcohol consumption can cause weight gain and increase the risk of obesity. The subjects included 7608 men between the ages of 40 and 59 years old. The study looked at the changes in body weight and alcohol intake of the men 5 years later to see if there was any change. The study found that the stable and heavy drinkers gained the most weight and had the highest BMI’s. The conclusion of the study was that people who consume more than 30g of alcohol per day are more likely to gain weight and become obese. Another article, also published in the American Journal of Clinical Nutrition, reviewed the findings from the first National Health and Nutrition Examination survey. It discussed the relationship between alcohol consumption, calorie intake and body weight. It stated that drinkers had higher calorie intake than nondrinkers, but mostly because they consume more calories from alcohol. However, the drinkers did not have higher obesity rates than the nondrinkers. It also stated that as drinkers calories from alcohol increased, their non-alcohol calories decreased. Finally, a third article, also from the American Journal of Clinical Nutrition, looked at whether drinking frequency is correlated with development of abdominal obesity. The subjects included 43, 543 men and women. Baseline information was gathered in the beginning of the study, and follow up was a few years later to see if there was any change in their waist circumference. The participants also reported their drinking frequency, total alcohol intake and total calorie intake. It was concluded that regular consumption of alcohol is not necessarily involved in the development of abdominal obesity.
So, does alcohol cause weight gain?
Based on the evidence from these 3 studies, alcohol can cause weight gain if you drink large quantities of it. The study stated greater than or equal to 30g/day. A standard drink (12 oz 4% alcohol beer, 1 oz of hard liquor, or about 4oz 12% alcohol wine) will provide about 10 grams of alcohol. Drinking alcohol does not always contribute to abdominal obesity. So, when you see someone with a “beer belly” it may not be from drinking alcohol, and may just be from consuming an excess amount of calories. So, basically alcohol can cause you to gain weight if it means you are consuming a greater amount of calories than you would if you weren’t drinking alcohol. It is also not recommended to drink alcohol instead of eating food because, as stated above, alcohol is considered empty calories. Although alcohol may not directly cause weight gain, it is no secret that when you drink alcohol, it may alter your judgment depending on how much you drink. You probably have ordered a pizza late at night after a night at the bar. And, maybe you even ate the whole thing. Drinking alcohol can make you crave other foods, or possibly even binge eat at night. Think of all of the extra calories you are eating on top of all of the calories you just drank. Also, depending on how much you drink, you may be hung over the next day. Often, being hung over may cause you to crave greasy, unhealthy food the next day, which could throw off your whole healthy eating regimen.
_
How Alcohol can pack on the Pounds:
1. Added Calories:
One of the obvious side effects of alcohol is that it adds calories to your diet. While many of us have a handle on the calories we eat, we often don’t know how many calories are in our drinks. While alcohol doesn’t contain fat, it does contain 7 calories per gram. That’s more than protein and carbs, both of which contain 4 calories per gram.
2. Increased Appetite:
Some studies suggest that alcohol can actually stimulate the appetite, at least in the short term. This is especially true when you’re at a party or some other social event where tempting foods are everywhere you turn. It’s hard enough to avoid fatty or sugary foods when you’re sober, but add alcohol and an increased appetite and it may become impossible.
3. License to Indulge:
Not only does alcohol add calories, it makes it harder to stick to a healthy diet. It takes high dose willpower to turn down high calorie foods. After a few drinks, that healthy diet you’ve been following so diligently suddenly doesn’t seem all that important anymore.
4. The Day After:
A night of drinking, even if it’s just one too many, not only leaves you vulnerable to temptation, it may leave you too tired or hungover to exercise the next day. When you’re hungover, you’re dehydrated, clumsy and nauseous – all things that preclude a workout.
_
Alcohol may not gain weight:
Alcohol contains calories, but drinking alcohol doesn’t lead to weight gain, according to other researchers, and some studies report a small reduction in weight for women who drink. The reason that alcohol doesn’t necessarily increase weight is unclear, but research suggests that alcohol energy is not efficiently used. Alcohol also appears to increase metabolic rate significantly, thus causing more calories to be burned rather than stored in the body as fat. Other research has found that the consumption of sugar decreases as the consumption of alcohol increases. Whatever the reasons, the consumption of alcohol is not associated with weight gain and is sometimes associated with weight loss in women. The medical evidence of this is based on a large number of studies of thousands of people around the world. Some of these studies are very large; one involved nearly 80,000 and another included 140,000 subjects.
_
Effects of alcohol intake on resting energy expenditure in young women social drinkers
This investigation evaluated the effects of alcohol consumption, controlled for the energy in alcohol and chronic effects of smoking, on resting energy expenditure (REE) in college-aged social drinkers. Sixteen women who both smoked and drank alcohol were administered, on 4 separate days in a counterbalanced order,1) cigarettes alone, 2) alcohol alone, 3) alcohol plus cigarettes, or 4) cigarettes with an energetic control. Each session consisted of a 25-min REE baseline, treatment in a randomly assigned order, and a 105-min assessment of REE. Analyses indicated that alcohol significantly (P<0.05) increased REE for up to 95 min after ingestion [increases of 29.6- 68.4 kJ (124-287 kcal)/24 h], increases that could not be accounted for by the energy content of the drink alone. Smoking and alcohol together also raised REE above baseline but not more than alcohol alone. It was concluded that alcohol intake raises REE, potentially explaining why alcohol interferes with energy utilization.
_
The relation between alcohol consumption and body weight remains an enigma for nutritionists. This is an important problem, because the average alcohol intake in adults is ≈10% of the total daily energy intake in several developed countries. The role of alcohol energy in body weight control has been studied by using 3 different approaches: epidemiology (alcohol intake and body weight), psychophysiologic investigations (alcohol and appetite regulation), and metabolic studies (effects of alcohol intake on energy expenditure and substrate oxidation). Epidemiologic evidence does not show a clear relation between daily alcohol energy intake and body weight. However, most studies report that people do not compensate for the alcohol energy by decreasing nonalcohol food energy intake. Except in alcoholics, alcohol energy is usually added to total food energy intake. Therefore, moderate alcohol drinkers tend to consume more energy than nondrinkers. Westerterp-Plantenga and Verwegen present an elegant study in 52 men and women on the effects on energy intake of an alcohol preload (1 MJ) ingested 30 min before lunch, in comparison with an isoenergetic carbohydrate, fat, or protein drink. The alcohol preload was followed by a greater energy intake at lunch than the other isoenergetic drinks. After the alcohol preload, there was no compensation for energy intake over the whole day. The alcohol preload also induced a higher eating rate and a longer meal duration at lunch than the other preloads. This study illustrates the short-term stimulatory effect of alcohol on appetite and food intake; alcohol did not induce any satiating effect. Whereas the alcohol preload significantly increased energy intake at lunch, the total energy intake for the day was not significantly altered in comparison with the other isoenergetic preloads. It was only when no preload was given (or an isovolumetric water preload) that the subjects consumed less energy than with the isoenergetic preloads. Other studies confirm that alcohol intake induces no or minimal dietary compensation. Therefore, both psychophysiologic studies on food intake regulation and epidemiologic investigations consistently show that in most individuals, the energy of alcohol is added to the energy of carbohydrate, fat, and protein of the daily diet. The paradox of increased alcohol-induced energy intake with no clear correlation between alcohol intake and body weight has led to the curious concept that alcohol energy has a low biological value. This hypothesis has not been confirmed by recent metabolic investigations on the effect of alcohol intake on energy expenditure and substrates oxidation in humans. Several studies carried out by using whole-body indirect calorimeters clearly showed that ethanol energy is used efficiently by the body and that alcohol energy does count! Ethanol-induced thermogenesis has been studied by several groups of investigators; a mean value of ≈15% for ethanol-induced thermogenesis has been obtained. After ethanol ingestion, the stimulation of energy expenditure induced by ethanol metabolism represents 15% of the ethanol energy; thus, 85% of ethanol energy is available as metabolizable energy for other metabolic processes. Ethanol-induced thermogenesis is smaller than protein-induced thermogenesis (≈25%) and larger than carbohydrate-induced thermogenesis (≈8%) and lipid-induced thermogenesis (≈3%). There is another way by which alcohol intake may alter body weight regulation. Ethanol is not stored in the body, but it is oxidized in preference over other fuels. The addition of ethanol to a diet reduces lipid oxidation measured over 24 h whereas oxidation of carbohydrate and protein are much less inhibited. Other studies confirm that alcohol ingestion reduces fat oxidation and favors a positive fat balance. In summary, metabolic studies show that ethanol energy is used with an efficiency comparable with that of a carbohydrate + protein meal and that it reduces fat oxidation. There is no reason to claim that ethanol energy does not play a role in energy balance regulation.
_
How can we resolve the above-mentioned paradox? Is it really true that alcohol intake is associated with increased energy intake in daily life? Have we sufficiently taken into account the influence of confounding factors such as underreporting of energy intake in obese subjects and the frequent association between smoking and alcohol intake? Clearly, the complex relation between alcohol intake and body weight regulation needs to be studied further by using a combined approach of epidemiology, psychophysiology, and metabolic investigations. Ideally, the effect of alcohol on energy intake and expenditure should be studied over several weeks or months. Your body has a set number of calories needed to maintain your weight. This need is based on your height, weight, age, gender, and activity level. When you consume more calories than your body needs, you will gain weight. Alcohol can lead to weight gain from the calories it provides and by causing you to eat more calories after consuming the alcohol. Research has shown a 20% increase in calories consumed at a meal when alcohol was consumed before the meal. There was a total caloric increase of 33% when the calories from the alcohol were added. Along with the increase in weight you can have an increased risk to your health because of where you gain the weight. A study of over 3,000 people showed that consuming elevated amounts of alcohol is associated with abdominal obesity in men. Many people joke about this being a “beer belly.” Unfortunately, a “beer belly” puts you at an increased risk for type 2 diabetes, elevated blood lipids, hypertension, and cardiovascular disease. Studies have shown that in the short term, alcohol stimulates food intake and can also increase feelings of hunger. Having your judgment impaired and stimulating your appetite is a recipe for failure if you are trying to follow a weight-loss plan.
_
Drinking a glass of wine may not cause weight gain:
The evidence is impressive. Researchers kept tabs on nearly 20,000 normal-weight women for 13 years. Over time, the women who drank a glass or two of red wine a day were 30 percent less likely to be overweight than the nondrinkers (they tracked women who drank liquor and beer too, but the link was strongest for red wine). That’s not surprising, since wine has other benefits. It’s rich in antioxidants that reduce cholesterol and blood pressure. One reason wine may contribute to a healthy weight is that digesting booze triggers your body to torch calories. Women make smaller amounts of the enzyme that metabolizes alcohol than men do, so to digest a drink, they have to keep producing it, which requires the body to burn energy. That means you’re likely to see more of a benefit than your guy since his body doesn’t have to work as hard to digest a glass of the grape. Alcohol also may burn calories due to a process called thermogenesis. Alcohol raises your body temperature (one reason some people get red cheeks when drinking), causing the body to burn calories to create heat. The study also showed that women who drank moderately ate less. While researchers can’t say why, it’s possible that they were more likely to slow down and savor their food and drink. If you combine all these factors, drinking wine could lead to taking in fewer calories while your body is burning energy, meaning you’re less likely to gain weight. Awesome, but you don’t want to replace food with wine—you’ll miss out on key nutrients. And keep in mind that wine has calories: about 125 for 5 ounces. That’s why drinking isn’t a weight-loss strategy on its own. Overdoing it is linked to health risks you don’t want to take, like breast cancer. But having a glass of wine along with a healthy diet and exercise, seems to be a marker for a healthier lifestyle.
_
Alcohol beverage drinking, diet and body mass index in across-sectional survey: The Finnish Foundation for Alcohol Studies:
The study was carried out to determine the associations of alcohol beverage drinking with macronutrients, antioxidants, and body mass index. Despite the similar total daily energy intakes, daily energy expenditure, and physical activity index, male drinkers were leaner than abstainers. In women, the proportion of underreporters of energy intake increased with increasing alcohol consumption, and the association between alcohol and body mass index was similar to that in men after the exclusion of underreporters. The study found that alcohol consumers were leaner than abstainers, and wine drinkers in particular had more antioxidants in their diet.
_
– A six-year study by the University of Denmark observed 43,500 people, and found that those who drank infrequently ended up gaining weight while daily drinkers had the least amount of weight gain.
– An eight-year study of 49,3000 women by the University College Medical School in London found that women who drank less two glasses of wine a day were 24% less likely to gain weight.
– A ten-year study of 7,230 people by the U.S. National Center for Disease Control found that alcohol consumption did not increase the risk of obesity.
But just because these new studies show alcohol can help you lose weight doesn’t mean you should be expecting your doctor to suggest a daily two wine drink minimum to help shed the pounds. The science isn’t quite conclusive and fails to address other variables such as personal fitness, economic class and education. So does alcohol make you fat? New evidence points to a reassuringly confident “probably not.” Just keep in mind, everyone’s body reacts to certain diets differently, and the choices you make for your health are best when decided by you.
______________
______________
The billion dollar question: Why drink alcohol?
_
Alcohol consumption has been part of human history since antiquity. There are not only numerous biblical examples and ancient myths which refer to alcohol but local oral history and archeological findings suggests that consumption has been part of African culture, rituals, tradition and custom since “time immemorial”. But the fact of enduring alcohol consumption and the passing down of this habit through generations does not adequately explain why alcohol is consumed. Moreover patterns of alcohol use have changed significantly over time and evidence suggests that the quantity used now is far greater than in earlier times. The WHO estimates that around 2 billion people worldwide consume alcohol (WHO 2004) and there is clearly no single reason why they do or why different people drink to different extents. It is apparent though that drinking is influenced by factors such as genetics, social environment, culture, age, gender, accessibility, exposure and personality. Cultural & religious factors influencing alcohol use is already discussed vide supra.
_
Aerobic vs. Anaerobic Glycolysis:
During aerobic glycolysis, NADH produced by oxidation of glyceraldehyde-3-phosphate, is oxidized by the mitochondrial electron transport chain, with the electrons transferred ultimately to oxygen. This oxidation of NADH, yields additional energy, with about 3 moles of ATP synthesized from ADP per mole of NADH oxidized. Since 2 moles of NADH are produced per mole of glucose entering the pathway, aerobic glycolysis yields considerably more ATP than anaerobic glycolysis. In anaerobic glycolysis, electrons from NADH do not enter the electron transport chain. Anaerobic glycolysis pathways include lactate fermentation and ethanol fermentation. Metabolism of glucose to either lactate or ethanol represents a nonoxidative process, as you can see by comparing the empirical formulas for glucose (C6H12O6) and lactate (C3H6O3). Clearly, there is no change in the overall oxidation state of the carbons, because the numbers of hydrogens and oxygens bound per carbon atom are identical for glucose and lactate. The same is true for ethanol plus CO2, when one counts the atoms in both. However, some individual carbon atoms of lactate and ethanol plus CO2 undergo oxidation, and some become reduced. When the oxygen supply runs short in heavy or prolonged exercise, muscles obtain most of their energy from an anaerobic (without oxygen) glycolysis. Yeast cells obtain energy under anaerobic conditions using a very similar process called alcoholic fermentation. Alcoholic fermentation is identical to anaerobic glycolysis except for the final step as seen in the figure below.
_
_
In alcoholic fermentation, pyruvic acid is broken down into ethanol and carbon dioxide. Both alcoholic fermentation and anaerobic glycolysis in muscles are anaerobic fermentation processes that begin with the sugar glucose. Glycolysis requires 11 enzymes which degrade glucose to lactic acid. Alcoholic fermentation follows the same enzymatic pathway for the first 10 steps. The last enzyme of glycolysis, lactate dehydrogenase, is replaced by two enzymes in alcoholic fermentation. These two enzymes, pyruvate decarboxylase and alcoholic dehydrogenase, convert pyruvic acid into carbon dioxide and ethanol in alcoholic fermentation. The most commonly accepted evolutionary scenario states that organisms first arose in an atmosphere lacking oxygen. Anaerobic fermentation is supposed to have evolved first and is considered the most ancient pathway for obtaining energy.
_
Evolutionary biology of alcohol consumption:
Drunken monkey hypothesis:
_
Dudley (2000) suggested that human ancestors developed a genetically based attraction to ethanol because they could use its odor plume to locate fruiting trees and because of health benefits from its consumption. If so, ethanol should be common in wild fruits and frugivores should prefer fruits with higher ethanol content. A literature review reveals that ethanol is indeed common in wild fruits but that it typically occurs in very low concentrations. Furthermore, frugivores strongly prefer ripe over rotting fruits, even though the latter may contain more ethanol. These results cast doubt on Dudley’s hypothesis and raise the question of how humans became exposed to sufficiently high concentrations of ethanol to allow its excessive consumption. Because fermentation is an ancient and widespread practice, it is suggested that humans “discovered” ethanol while using fermentation as a food preservation technique. They may have been predisposed to consume ethanol from previous and beneficial exposure to much lower doses and later on became addicted to it at high concentrations.
_
Alcohol may be part of our nature, in the sense that alcohol liking and seeking may have been under positive selection during our evolutionary history, which may make alcohol distinctive from other drugs of abuse:
Alcohol is part of our nature: Natural selection for low-level alcohol consumption:
From an evolutionary perspective, humans are well adapted to an ethanol-containing diet, which has regularly been provided by ripe fruits, typically below 1% ethanol, sometimes even above 3.5%. Humans have evolved the necessary enzymatic functions that provide metabolic tolerance to low amounts of ethanol, thereby preventing intoxication. Metabolic utilization of ethanol is facilitated by alcohol dehydrogenases (ADHs), one of the oldest and largest classes of enzymes. The existence of a rapidly evolving ADH system appears to guarantee adaptability to changing internal and external environments. Some variants of ADH and acetaldehyde dehydrogenase cause accumulation of toxic acetaldehyde upon alcohol intake and thereby provide strong protection against alcohol abuse. The allelic ADH variants differ between different human populations due to unknown selection pressures. Natural selection for low chronic exposure to environmental stressors often results in a nutrient–toxin continuum, whereby low concentrations are beneficial and higher concentrations harmful. For alcohol this has been shown in Drosophila species, where longevity is increased at very low concentrations of ethanol, but decreases rapidly with exposure to higher concentration. Another example is provided by alko alcohol (AA) and alko non-alcohol (ANA) rats, which are selectively bred and maintained such that AA rats voluntarily consume more than 5 g alcohol per kilogram of body weight per day (g/kg/day), whereas ANA rats consume less than 0.5 g/kg/day alcohol. AA rats live longer than the alcohol-avoiding ANA animals, and further in line with findings from Drosophila, segregated alleles between AA and ANA rats are strongly clustering on metabolic genes. It should be noted that natural selection of behavioural responses towards alcohol is not restricted to metabolism. It may have acted via various mechanism including olfactory responses, feeding stimuli, reward processes, and by affecting emotional states. Taken together, alcohol preference appears to be an evolutionary inherited trait that came under positive selection in periods of mostly scarce resources. No similar pressure worked on genes protecting against harmful effects caused by higher amounts of alcohol because exposure to such concentrations only became available in the last 2800 years, a period too short to induce adequate evolutionary counter responses. In this sense, modern alcoholism has been called an ‘evolutionary hangover’, which sets this disorder apart from other substance addictions such as nicotine or other naturally occurring psychotropes.
_
Biology, evolution and ethanol:
Throughout human history, alcoholic beverages have treated pain, thwarted infections and unleashed a cascade of pleasure in the brain that lubricates the social fabric of life, according to Patrick McGovern, an archaeochemist at the University of Pennsylvania Museum of Archaeology and Anthropology. For the past several decades, McGovern’s research has focused on finding archaeological and chemical evidence for fermented beverages in the ancient world. The details are chronicled in his recently published book, “Uncorking the Past: The Quest for Wine, Beer, and Other Alcoholic Beverages.” He argues that the mind-altering effects of alcohol and the mysterious process of fermentation may explain why these drinks dominated entire economies, religions and societies. He’s found evidence of fermented beverages everywhere he’s looked, which fits his hypothesis that alcohol “had a lot to do with making us what we are in biological and cultural terms.” The average human digestive system produces approximately 3g of ethanol per day merely through fermentation of its contents. Catabolic degradation of ethanol is thus essential to life, not only of humans, but of almost all living organisms. In fact, certain amino acid sequences in the enzymes used to oxidize ethanol are conserved all the way back to single cell bacteria. Such a functionality is needed because all organisms actually produce alcohol in small amounts by several pathways, primarily along the fatty acid synthesis, glycerolipid metabolism, and bile acid biosynthesis pathways. If the body had no mechanism for catabolizing the alcohols, they would build up in the body and become toxic. This could be an evolutionary rationale for alcohol catabolism also by sulfotransferase. “As far back as we can look, humans have had a love affair with fermented beverages,” said Patrick McGovern, an archaeological chemist at the University of Pennsylvania. “And it’s not just humans. From fruit flies to elephants, if you give them a source of alcohol and sugar, they love it.” Humans may have an added reason to be drawn to alcohol. Throughout antiquity, available water was likely to be polluted with cholera and other dangerous microbes, and the tavern may well have been the safest watering hole in town. Not only is alcohol a mild antiseptic, but the process of brewing alcoholic beverages often requires that the liquid be boiled or subjected to similarly sterilizing treatments. “It’s possible that people who drank fermented beverages tended to live longer and reproduce more” than did their teetotaling peers, Dr. McGovern said, “which may partly explain why people have a proclivity to drink alcohol.” Dr. McGovern and other archaeologists have unearthed extensive evidence of the antiquity and ubiquity of alcoholic beverages. One of the oldest known recipes, inscribed on a Sumerian clay tablet that dates back nearly 4,000 years, is for beer. Chemical traces inside 9,000-year-old pottery from northern China indicate that the citizens of Jiahu made a wine from rice, grapes, hawthorn and honey, a varietal recently brought back to life by the intrepid palates at Dogfish Head brewery in Delaware. Dr. McGovern of Cornell University and colleagues reported evidence in The Proceedings of the National Academy of Sciences that the earliest known chocolate drink, made from the cacao plant in Honduras 1,400 years ago, was probably a fermented beverage, with an alcohol content similar to beer, a discovery that brings to mind the classic Onion T-shirt: “I’m like a chocoholic but for booze.” Researchers caution, however, that if we humans are congenitally inclined to drink, we are designed to do so only in moderation. We are not, in other words, Syrian hamsters, the popular pet rodents that also are a favorite of alcohol researchers. Syrian hamsters are the Andy Capp of the animal kingdom. “They’ll drink alcohol whenever offered the option,” said Howard B. Moss, associate director for clinical and translational research at the National Institute on Alcohol Abuse and Alcoholism in Bethesda, Md. “You give them a bottle of water and a bottle of alcohol, they’ll always choose the alcohol over the water.” Researchers have traced this avidity to the hamster’s natural habits. The animals gather fruit all summer and save it for later by burying it underground, where the fruit ferments. “That’s how the hamsters find their cache of last summer’s goodies when it’s the middle of winter,” Dr. Moss said. “They’ve developed a preference for the taste and smell of fruit that’s turned.” They’ve also developed the necessary equipment to metabolize high doses of alcohol. “A hamster’s liver is five times the size of a human liver in comparison to the other abdominal organs,” Dr. Moss said. “It’s all liver in there.” Behind the hamster dance is the ancient chemical legerdemain of fermentation, which by its most general definition means extracting energy from sugar without using oxygen. There are many ways to do this: our muscle cells ferment when operating anaerobically, say, while lifting weights. The fermentation that yields ethanol, the type of alcohol we drink, is the work of yeast cells, which will latch onto any suitable sugar source and start feasting. As they break down the sugary chains, the yeast enzymes generate two key byproducts: carbon dioxide, which can be used to puff up bread dough, and ethanol. Alcohol, then, is nothing more than fungal scat. Ah, but how that scat can sing. An alcohol molecule consists of a knob of hydrogen and oxygen linked to a carbon-based stalk, and that telltale knob, that hydroxyl group, allows the molecule to mix easily with water. The hydroxyl group makes alcohol go to any cell in the body that has water which means alcohol goes to every tissue in the body. The brain is particularly well lubricated, and alcohol happily mingles therein, to noteworthy, crazy-quilt effect. It stimulates the secretion of dopamine, the neurochemical associated with the brain’s reward system. It stifles the brain’s excitatory circuits and excites the brain’s dampening circuits. It alters the membranes of neurons and the trafficking of important ions like calcium and sodium across neuronal borders. It stimulates like cocaine and it depresses like diazepam. It makes the shy voluble, the graceful clumsy and the operator of a motorized vehicle very dangerous.
_
Why do Humans have a way to break down Alcohol?
Practically every animal from the fruit fly to the elephant has a way to break down ethyl alcohol because ethyl alcohol is found everywhere in nature. Every time you eat a piece of fresh fruit, drink a glass of fresh orange juice, or have a slice of freshly baked bread then chances are that you are getting trace amounts of alcohol along with it. It is not uncommon to see intoxicated birds which have eaten fermented fruit. Monkeys are known to seek out fermented fruit for the intoxicating effect and Indian elephants have been known to break into breweries or wineries to drink up what is stored there. Not only are we constantly ingesting alcohol along with the food we eat, our own bodies produce alcohol as a part of the digestive process. Our digestive tracts contain millions of micro-organisms which are necessary for us to properly digest our food. Among these micro-organisms are yeasts which produce alcohol from sugars within our own bodies. With alcohol so omnipresent in nature it is necessary that animals have a way to break alcohol down, otherwise it would just accumulate in the body and no animal could function properly because the animals would always be constantly intoxicated. Other alcohols such as methyl alcohol (wood alcohol) and isopropyl alcohol (rubbing alcohol) do not normally occur in nature. This is why we do not have a mechanism to break them down and why they are poisonous.
_
Alcohol Response and Consumption in Adolescent Rhesus Macaques: Life History and Genetic Influences:
The use of alcohol by adolescents is a growing problem and has become an important research topic in the etiology of the alcohol use disorders. A key component of this research has been the development of animal models of adolescent alcohol consumption and alcohol response. Due to their extended period of adolescence, rhesus macaques are especially well-suited for modeling alcohol-related phenotypes that contribute to the adolescent propensity for alcohol consumption. In this review, authors discuss studies from their laboratory that have investigated both the initial response to acute alcohol administration and the consumption of alcohol in voluntary self-administration paradigms in adolescent rhesus macaques. These studies confirm that adolescence is a time of dynamic change both behaviorally and physiologically, and that alcohol response and alcohol consumption are influenced by life history variables such as age, sex, and adverse early experience in the form of peer-rearing. Furthermore, genetic variants that alter functioning of the serotonin, endogenous opioid, and corticotropin releasing hormone systems are shown to influence both physiological and behavioral outcomes, in some cases interacting with early experience to indicate gene by environment interactions. These findings highlight several of the pathways involved in alcohol response and consumption, namely reward, behavioral dyscontrol, and vulnerability to stress, and demonstrate a role for these pathways during the early stages of alcohol exposure in adolescence.
_
Intoxicated honey bee:
Researchers gave honey bees various levels of ethanol, the intoxicating agent in liquor, and monitored the ensuing behavioral effects of the drink – specifically how much time the bees spent flying, walking, standing still, grooming and flat on their backs, so drunk they couldn’t stand up. The researchers also measured the level of ethanol in the bees’ hemolymph – the circulatory fluid of insects that’s akin to blood. Not surprisingly, increasing ethanol consumption meant bees spent less time flying, walking and grooming, and more time upside down. The appearance of inebriation occurred sooner for bees that were given a larger dose of ethanol. Also, blood ethanol levels increased with time and the amount of ethanol consumed. This study is preliminary – the researchers simply wanted to see what effects ethanol had on honey bee behavior. In the future, however, they hope to use honey bees as a model for learning more about how chronic alcohol use affects humans, particularly at the molecular level. “The honey bee nervous system is similar to that of vertebrates,” said Geraldine Wright, a study co-author and a postdoctoral researcher in entomology at Ohio State. Mustard concurred. “On the molecular level, the brains of honey bees and humans work the same. Knowing how chronic alcohol use affects genes and proteins in the honey bee brain may help us eventually understand how alcoholism affects memory and behavior in humans, as well as the molecular basis of addiction.” The researchers presented their work in San Diego at the annual Society for Neuroscience conference. Honey bees were secured into a small harness made from a piece of drinking straw. The researchers then fed bees solutions of sucrose and ethanol, with several ethanol concentrations ranging from 10 to 100 percent. The 10 percent solution was equivalent to drinking wine, Wright said, while the 100 percent solution, which contained no sucrose, was equivalent to drinking 200-proof grain alcohol. A group of control bees was given sucrose only. The scientists fed the bees and then observed them for 40 minutes, tracking the insects’ behaviors – how much time each bee spent walking, standing still, grooming, flying and upside down on its back. Blood ethanol concentrations increased with time and with the amount of ethanol each bee had consumed. Behavioral differences between the bees depended on the amount of ethanol ingested. The bees that had consumed the highest concentrations of ethanol – 50, 75 and 100 percent – spent a majority of the observation period on their backs, unable to stand. This effect happened early on, within the first 10 minutes of the observation period. They also spent almost no time grooming or flying. “These bees had lost postural control,” Mustard said. “They couldn’t coordinate their legs well enough to flip themselves back over again.” Except for the control bees, bees that had consumed the least amount of ethanol – 10 percent – spent the least amount of time upside down. Even then, it took about 20 minutes for ethanol’s effect to set in and cause this behavior. The researchers hope to learn how alcohol consumption affects social behavior as well as gain a better understanding of the basic mechanisms that drive alcohol addiction and tolerance. “Honey bees are very social animals, which makes them a great model for studying the effects of alcohol in a social context,” Wright said. “Many people get aggressive when they drink too much,” she continued. “We want to learn if ethanol consumption makes the normally calm, friendly honey bee more aggressive. We may be able to examine how ethanol affects the neural basis of aggression in this insect, and in turn learn how it affects humans.” Mustard and Wright conducted this research with Ohio State colleagues Brian Smith, a professor of entomology, and Ian Maze, an undergraduate student studying microbiology.
_
Drunken honey bee:
_
Molecular Genetic Analysis of Ethanol Intoxication in Drosophila melanogaster (fruit fly):
Recently, the fruit fly Drosophila melanogaster has been introduced as a model system to study the molecular bases of a variety of ethanol-induced behaviors. It became immediately apparent that the behavioral changes elicited by acute ethanol exposure are remarkably similar in flies and mammals. Flies show signs of acute intoxication, which range from locomotor stimulation at low doses to complete sedation at higher doses and they develop tolerance upon intermittent ethanol exposure. Genetic screens for mutants with altered responsiveness to ethanol have been carried out and a few of the disrupted genes have been identified. This analysis, while still in its early stages, has already revealed some surprising molecular parallels with mammals. In its natural environment, rich in fermenting plant materials, the fruit fly Drosophila melanogaster encounters relatively high levels of ethanol. Fruit flies are well equipped to deal with the toxic effects of ethanol; they use it as an energy source and as a precursor for lipid biosynthesis. The effects of ethanol and its metabolites on Drosophila have been studied for decades, as a model for adaptive evolution. More recently, Drosophila has been introduced as a model to study the molecular bases of ethanol-related behaviors. While these fields of study have different primary goals, the information gained can be nicely complementary. For example, a definition of the genes (by mutagenesis) that regulate various ethanol-induced behaviors in the laboratory may provide candidate genes for evolutionary biologists and population geneticists. Conversely, knowledge of the role of ethanol in the fly’s ecology has important implications for the design of mutagenesis-driven approaches that aim to understand behavior. It has been postulated that the evolutionary origins of alcohol consumption in humans may be related to primate frugivory, which led to consumption of substantial amounts of ethanol (Dudley, 2000). Humans and Drosophila melanogaster share a common history of ethanol exposure.
_________
Alcohol and genes:
Genetic predisposition to alcoholism:
A number of socio-economic, cultural, biobehavioral factors and ethnic/gender differences are among the strongest determinants of drinking patterns in a society. Both epidemiological and clinical studies have implicated the excessive use of alcohol in the risk of developing a variety of organ, neuronal and metabolic disorders. Alcohol abuse related metabolic derangements affect almost all body organs and their functions. Race and gender differences in drinking patterns may play an important role in the development of medical conditions associated with alcohol abuse. The incidence of alcoholism in a community is influenced by per capita alcohol consumption and covariates with the relative price and availability of alcoholic drinks. The majority of the family, twin and adoption studies suggest that alcoholism is familial, a significant proportion of which can be attributed to genetic factors. The question is how much of the variance is explained by genetic factors and to what degree is this genetically mediated disorder moderated by personal characteristics. Among the most salient personal characteristics moderating, the genetic vulnerability may be factors such as age, ethnicity, and presence of psychiatric co morbidity. Cultural factors and familial environmental factors are most likely predictors as well.
_
Twin, family, and adoption studies have firmly established that genetics plays an important role in determining an individual’s preferences for alcohol and his or her likelihood for developing alcoholism. Alcoholism doesn’t follow the simple rules of inheritance set out by Gregor Mendel. Instead, it is influenced by several genes that interact with each other and with environmental factors. Perhaps the single greatest influence on the scope and direction of alcohol research has been the finding that a portion of the vulnerability to alcoholism is genetic. This finding, more than any other, helped to establish the biological basis of alcoholism. Today we know that approximately 50 to 60 percent of the risk for developing alcoholism is genetic. Genes direct the synthesis of proteins, and it is the proteins that drive and regulate critical chemical reactions throughout the human body. Genetics, therefore, affects virtually every facet of alcohol research, from neuroscience to Fetal Alcohol Syndrome.
_
Family History:
Research studies have found that children of alcoholics are four times more likely than the general population to develop alcohol problems. However, many people with a family history of alcoholism do not become alcoholics. Additional factors that increase the risk of developing alcoholism include having an alcoholic parent who is depressed or has other psychological problems, growing up in a family where both parents abuse alcohol or other drugs, having a parent with severe alcohol abuse problems and living in a family where conflicts lead to aggression and violence.
_
Findings from Twin/Family Studies:
The classic twin study design compares the resemblances for a trait of interest between monozygotic (MZ, identical) twins and dizygotic (DZ, fraternal) twins, in order to determine the extent of genetic influence, or heritability, of the trait. Heritability can be calculated because MZ twins are genetically identical, whereas DZ twins share only half their genes. The method relies on the “equal-environment assumption,” that is, that the similarity between the environments of both individuals in a pair of MZ twins is the same as the similarity between the environments of members of pairs of DZ twins. While earlier twin studies have been severely criticized for not testing this assumption sufficiently, researchers have taken care more recently to collect data on the twins’ environments, thereby allowing correction of results for any deviation from this assumption. While twin studies do not identify specific genes influencing a trait, they do provide important information on the trait’s genetic architecture (more general properties of its inheritance pattern, such as whether genes act independently of one another, or in concert, to influence a trait), which aspects of the trait are most heritable, whether the same genes are influencing the trait in both genders, and whether multiple traits share any common genetic influences. When data on twins are augmented by data on their family members, the study is termed a twin/family study and can provide more precise information about whether parents transmit a behavioral trait to their offspring genetically or via some aspect of the familial environment (cultural transmission). When detailed data about the environment are collected, twin and twin/family studies can provide information about how environmental factors interact with genetic predisposition to produce a disease.
_
While earlier twin studies have firmly established substantial heritability of alcoholism in men (on the order of 50 percent), they have generally failed to detect heritability in women. This failure may be due, in part, to the lower rate of alcoholism among women than men, thereby necessitating larger sample sizes to achieve statistically significant results. Since the first studies to report a substantial heritability of alcoholism in women (Kendler et al. 1992), others have reported analysis of a sample of volunteer adult Australian twins consisting of 1,328 MZ pairs and 1,357 DZ pairs (distributed among all possible combinations of genders) (Heath et al. 1997). Of these subjects, about 25 percent of the men and about 6 percent of the women met DSM-IIIR criteria for alcohol dependence. (DSM-IIIR refers to the Diagnostic and Statistical Manual of Mental Disorders, Third Edition, Revised, a standard classification system for mental disorders [American Psychiatric Association 1987].) Analysis of the concordances for alcoholism among the various classes of twins suggested that about two-thirds of the risk of becoming alcoholic was genetically mediated in both men and women, with the remainder of the risk determined by environmental factors not shared by the two members of a given twin pair. The data provided no evidence for a difference in the degree of heritability in men and women, nor any evidence for genetic factors operating in one gender but not the other. This last conclusion was particularly aided by analyses of data from opposite-sex twin pairs, a type of analysis not previously reported. Using the same subject sample, these researchers have more recently demonstrated that childhood conduct disorder is significantly associated with risk for adult alcohol dependence in both men and women, with genetic factors accounting for most of the association in both genders (Slutske et al. 1998). These findings further emphasize the similarities in factors leading to alcoholism in men and women and suggest either that there are common genetic risk factors for conduct disorder and alcoholism in both genders, or that conduct disorder is itself a genetic risk factor for alcoholism. Since the subject sample for these studies came from the general population and because most of the alcoholics contained therein were relatively mildly affected, it is possible that the conclusions of these studies might not apply to very severely affected alcoholics, such as those identified from treatment centers.
_
Since individuals who eventually become alcoholic typically begin experimenting with alcohol use during adolescence and then proceed through stages of increasingly heavy use until they become addicted, investigators have long been interested in factors influencing initiation of alcohol use during adolescence. The notion that adolescents learn to use alcohol by modeling the alcohol use of their parents is an old one. Investigators tested this notion in a sample of 1,396 Dutch families, each consisting of a pair of adolescent twins and their parents (Koopmans and Boomsma 1996). The twins’ alcohol use resembled that of their parents to some extent. For 17-year-olds, this resemblance could best be explained by genetic similarity of children to their parents, rather than by children modeling their parents’ drinking behavior. For 15- to 16-year-olds, while the resemblance of the children’s drinking to that of their parents was explained principally by some aspect of the familial environment, the parents’ drinking behavior itself accounted for, at best, only a small part of this resemblance. It appears from this study that children’s drinking behavior is influenced primarily by genetic factors and by environmental factors other than their parents’ alcohol use. This conclusion is consistent with findings from previous studies demonstrating strong peer influences on adolescent alcohol use.
_
Many, but not all, alcoholics suffer from medical complications of alcoholism, such as liver cirrhosis, pancreatitis, cardiomyopathy, or psychosis due to brain damage. The inconsistency with which medical complications occur in alcoholism has led to the plausible hypothesis that susceptibility to these complications is influenced by genetic factors independent of those influencing susceptibility to alcoholism itself. Researchers tested this hypothesis using 5,933 male MZ twin pairs and 7,554 male DZ twin pairs from the U.S. World War II Era Veteran Twin Registry (Reed et al. 1996). From this sample, 1,239 subjects had a diagnosis of alcoholism according to ICD-9 criteria (one of the two major classification systems used in International Classification of Disease, Ninth Revision, to diagnose mental disorders, including alcoholism [World Health Organization 1977]), 392 subjects had liver cirrhosis, and 242 subjects had alcoholic psychosis. Of the alcoholic subjects, 818 had neither cirrhosis nor psychosis, and 421 had either or both of these complications. From the MZ and DZ concordance rates for the three diseases, the investigators calculated heritabilities of 0.59 for alcoholism (in general agreement with results of other studies), 0.47 for liver cirrhosis, and 0.61 for alcoholic psychosis. For each trait, the remainder of the variance in susceptibility was due to environmental factors not shared by members of a twin pair. Using an analytic method that allowed for simultaneous analysis of all three diseases, the investigators calculated that 85 percent of the overall genetic risk was shared for alcoholism, cirrhosis, and psychosis. The small amount of genetic risk not accounted for by these shared factors was due to separate genetic factors for cirrhosis and psychosis, respectively. Although the role of these disorder-specific genetic factors was small, it was significant; removing these factors from the mathematical model resulted in a significantly worse fit to the data. The conclusion about the largely shared genetic susceptibility to all three diseases differs from that of an earlier analysis of part of these data (Hrubec and Omenn 1981), largely as a result of the more sophisticated analytic methods employed. Why is so much of the genetic part of the risk for cirrhosis and alcoholic psychosis due to factors influencing the risk for alcoholism itself? Overall genetic risk for cirrhosis or psychosis refers to those genetic factors influencing the transformation of a normal (nonalcoholic) person into an alcoholic with cirrhosis or psychosis, respectively. The physiologic pathways leading to these medical complications pass obligatorily through alcohol addiction itself, presumably because such addiction is a precondition for the sustained high levels of consumption necessary to bring about the medical complications. There are multiple pathways leading to alcoholism, each with multiple steps. It seems likely that human populations contain a large amount of variation in the genes influencing many of these steps, leading collectively to a large genetic risk. If the physiologic pathways leading to cirrhosis and psychosis, given that an individual is already consuming large amounts of alcohol, are relatively simple with relatively few steps, then there will be relatively few opportunities for genetic variation to influence those steps. Alternatively, regardless of the number of steps in this part of the pathway, human populations might contain relatively little variation in the genes influencing these steps. Either of these situations would result in cirrhosis-specific and psychosis-specific genetic factors accounting for only a small part of the overall genetic risk for these complications.
_
There is also some evidence that genes influence how alcohol affects the cardiovascular system. An enzyme called alcohol dehydrogenase helps metabolize alcohol. One variant of this enzyme, called alcohol dehydrogenase type 1C (ADH1C), comes in two “flavors.” One quickly breaks down alcohol, the other does it more slowly. Moderate drinkers who have two copies of the gene for the slow-acting enzyme are at much lower risk for cardiovascular disease than moderate drinkers who have two genes for the fast-acting enzyme. Those with one gene for the slow-acting enzyme and one for the faster enzyme fall in between. It’s possible that the fast-acting enzyme breaks down alcohol before it can have a beneficial effect on HDL and clotting factors. Interestingly, these differences in the ADH1C gene do not influence the risk of heart disease among people who don’t drink alcohol. This adds strong indirect evidence that alcohol itself reduces heart disease risk.
_
Approximately 60% of the risk for alcohol use disorders is attributed to genes, as indicated by the fourfold higher risk for alcohol abuse and dependence in children of alcoholics (even if these children were adopted early in life and raised by nonalcoholics) and a higher risk in identical twins as compared to fraternal twins of alcoholics. The genetic variations appear to operate primarily through intermediate characteristics that subsequently relate to the environment in altering the risk for heavy drinking and alcohol problems. These include genes relating to a high risk for all substance use disorders that operate through impulsivity, schizophrenia, and bipolar disorder. Another characteristic, an intense flushing response when drinking, decreases the risk for only alcohol use disorders through gene variations for several alcohol-metabolizing enzymes, especially aldehyde dehydrogenase (a mutation only seen in Asians), and to a lesser extent, variations in alcohol dehydrogenase.
_
Science Daily reports that in the study, published in the the journal Genetics, the research team measured the time it takes for flies to stagger due to alcohol intake while simultaneously identifying changes in the expression of all their genes. They used statistical methods to identify genes that work together to help the flies adapt to alcohol exposure. In looking at corresponding human genes, a counterpart gene called ME1 was associated with alcohol consumption in humans, as people with certain variations of the gene showed a tendency to drink stronger alcoholic beverages. Dr. Robert Anholt, William Neal Reynolds Professor of Biology and Genetics at North Carolina State and the senior author of the study, says the research has possible clinical implications. “Our findings point to metabolic pathways associated with proclivity for alcohol consumption that may ultimately be implicated in excessive drinking,” he said. “Translational studies like this one, in which discoveries from model organisms can be applied to insights in human biology, can help us understand the balance between nature and nurture, why we behave the way we do, and—for better or worse—what makes us tick.”
_
An additional genetically influenced characteristic, a low sensitivity to alcohol, affects the risk for heavy drinking and may operate, in part, through variations in genes relating to potassium channels, GABA, nicotinic, and serotonin systems. Alcoholism is more common in those people who are less sensitive to the motor, perceptual, and biochemical changes induced by alcohol due to genetic makeup. A low response per drink is observed early in the drinking career and before alcohol use disorders have developed. All follow-up studies have demonstrated that this need for higher doses of alcohol to achieve desired effects predicts future heavy drinking, alcohol problems, and alcohol use disorders. The impact of a low response to alcohol on adverse drinking outcomes is mediated, at least in part, by a range of environmental influences, including the selection of heavier-drinking friends, the development of more positive expectations of the effects of high doses of alcohol, and suboptimal ways of coping with stress.
_______
Other influences on alcohol use:
According to the Drug and Alcohol Services South Australia:
•71 % of people drink alcohol for socialising
•21 % of people drink alcohol because they like the taste
•12 % of people drink alcohol to feel at ease
•6 % of people drink alcohol to get intoxicated
•6 % of people drink alcohol because of peer pressure
•2 %of people drink alcohol to get drunk
•0 % of people drink alcohol to forget problems
_
The main reason people start drinking is very simple….curiosity! People are curious why alcohol is so celebrated by some and feared by others. We want to know what it feels like to consume alcohol. We want to know why the commercials on television promote people having fun, dancing and socializing. We want to know how it feels to be “tipsy”. Another reason is stress. We live in a world full of problems and when the weight of these problems fall on our shoulders, alcohol eases some of that pain. When a person is on medication, it just intensifies that feeling and becomes even a bigger problem. Loneliness and isolation make people drink. Elderly people with limited mobility and with little family and few or no friends find themselves turning to alcohol for comfort. Peer pressure among teens and young adults causes them to turn to alcohol. Some people go to taverns regularly to be part of something because of loneliness. Social gatherings that we all go to, like weddings, funerals, holidays, birthdays, anniversaries, office parties to name a few. People drink for various reasons. It provides them with a sense of confidence and they can let go of some of the daily pressure. For a short time, you feel euphoric, relaxed, and happy. If people could leave it at that, we would not have alcoholism and it would not be a social problem. (Effects on Society, 2009)
_
Common reasons why alcohol is consumed:
• Alcohol as a social lubricant:
Alcohol assists people to relax, converse more easily and mix socially. It disinhibits defenses and facilitates “good company”.
• Use of alcohol in ritual:
Alcohol has a “mystique” not shared by non-alcoholic beverages and its use in traditional rituals (locally and internationally) appears to add to the aura of special occasions.
• Social sharing:
Sharing an alcoholic drink with other people promotes a bonding and a connectedness amongst consumers often not gained through sharing non-alcoholic beverages.
• Drinking alcohol is accepted – and even expected – behavior:
There is very little public criticism of people who drink alcohol – even to states of drunkenness. On the contrary, in a number of cultures and situations it is expected that one drinks – even to states of drunkenness. Obvious examples would be to see in the New Year or “the coming of age” of a young person. Drinking in many situations is simply the “status quo”, i.e. that’s the way things are.
• Taste and quality:
Though an acquired taste, consumers of alcohol enjoy the taste of alcohol. Some people develop sophisticated palates for alcohol and sincerely appreciate good quality. Even traditionally made alcohol products vary in quality and demand is mediated by this. What one drinks and how one drinks it is very often an indication of culture and class.
• Alcohol as a reducer of stress:
Alcohol is often used to reduce the tension of an event – impending or actual.
Research suggests that drinking can reduce stress in certain people and under certain circumstances. Differences include a family history of alcoholism, personality traits, self-consciousness, cognitive functioning and gender (Sayette, 1999).
• Drinking as a means of dulling “the pain of poverty” or other hardships of life:
For many people life is simply intolerable. They live in abysmal poverty or in life circumstances which produce unbearable emotional pain. Alcohol dulls that pain for as long as they are drinking. (The fact that this leads into a cycle of ongoing poverty or pain does not influence this pattern).
• Consumption as “macho” behavior:
(Mainly) men consume large amounts of alcohol as an indication of their strength and manliness. Behaviours such as drinking more than anyone else or more quickly than anyone else are often regarded as admirable masculine qualities. With changing gender roles some women also “prove” themselves with binge drinking patterns.
• Consumption in youth:
As children are usually prohibited from drinking alcohol, youth (again mainly males) often see drinking alcohol as a state of adult behaviour to be aspired to.
• Enjoyment of a state of intoxication:
Many people simply enjoy the feeling of intoxication (from fairly mild to “motherless”).
• Maintaining a state of inebriation:
The state of inebriation is not maintained unless additional alcohol is consumed. This may lead to more consumption and to states of drunkenness not necessarily intended when starting to drink.
• Lack of information:
Many people are ignorant of the facts regarding the impacts and effects of alcohol and drink without knowing the dangers. “Counter advertising” and education around alcohol in schools are limited.
_
Pressure to consume alcohol:
• Responding to peer pressure:
Many people, especially youth, may be, or feel, pressurized to drink alcohol as this is regarded as the social norm or the norm of a particular age or social/cultural grouping. The pressure to conform, especially amongst youth, is a well-documented psychological phenomenon. People may be (or fear they may be) excluded from or ostracized by the group if they do not partake in alcohol.
• Pressure from advertising/following role-models:
While the alcohol industry claims that alcohol advertising is aimed solely at brand switching and that it is not aimed at promoting additional consumption – especially drinking amongst youth – evidence suggests that advertising does indeed increase consumption (Snyder 2006). The association of role models depicted in adverts such as sportspeople, attractive people, strong people, “outdoor” people, people who enjoy life, people with “superior” tastes etc, etc encourage drinking behaviour in the belief that emulating this behaviour makes one more like these “models”.
_
Alcohol as part of social control:
Since the arrival of European settlers in South Africa, alcohol was used as a form of social and economic control. At different periods it was used in barter for cattle, in exchange for labour (including the “dop” system), the education of slaves and played a pivotal role in “managing” labour in certain sectors of the economy such as mining and agriculture (Parry and Bennetts 1998). The history of alcohol in South Africa is an integral part of the history of apartheid and segregation. During apartheid who was allowed to buy liquor, when, what types and where were all determined by race and used to control the movements, social habits and freedoms of black people. In townships, municipal beer halls were established by local authorities to help finance township development and control the behaviour of black people. In response, many people turned to illegal liquor related activities – both brewing traditional African beer and setting up illegal outlets (shebeens) where liquor was sold. Importantly the growth of illegal shebeens in the second part of the 20th century served not only as a way to increase access to alcohol, as a means for social mixing and as employment for the owners and employees but also as a form of resistance to apartheid policies. Moreover during the 1976 uprisings in Soweto and other townships, beerhalls were specifically targeted as they had come to symbolize white domination and control.
______________
Blood alcohol concentration/content (BAC):
BAC is also called blood ethanol concentration, or blood alcohol level (BAL). There are several different units in use around the world for defining blood alcohol concentration. Each is defined as either a mass of alcohol per volume of blood or a mass of alcohol per mass of blood (never a volume per volume). 1 milliliter of blood is approximately equivalent to 1.06 grams of blood. Because of this, units by volume are similar but not identical to units by mass. In the U.S. the concentration unit 1% w/v (percent mass/volume, equivalent to 10g/l or 1 g per 100 ml) is in use. For instance, in North America a BAC of 0.1 means that there is 0.1 gm of alcohol in 100 ml of blood. It would mean BAL of 100 mg of alcohol in 100 ml blood in India. So BAC 0.1 means BAL 100. Blood levels of ethanol are expressed as milligrams or grams of ethanol per deciliter (e.g., 100 mg/dL = 0.1 gm/dL), with values of 0.02 gm/dL resulting from the ingestion of one typical drink. Deciliter (dL) means 100 ml. This is not to be confused with the amount of alcohol measured on the breath, as with a breathalyzer.
_
Legal statutes define driving while intoxicated in terms of whole-blood alcohol (ethanol) concentrations. Blood samples obtained in drunk driving cases are generally — but not always — analyzed as whole blood (sometimes called “legal blood”). If the sample is withdrawn for medical purposes, however, the test will probably be done with serum (often referred to as “medical blood”). Serum is the clear yellowish fluid obtained when blood is allowed to clot. Separating whole blood into its solid and liquid components by centrifuging the sample results in formation of plasma. The only difference between plasma and serum is that clotting factors are depleted in serum. Since plasma and serum have approximately the same water content (92%), whereas whole blood has about 80%; the ratio of ethyl alcohol content in the plasma or serum to alcohol content in whole blood would be equal to the ratio of water in plasma to the water in whole blood. That is 92%/80% = 1.15
Remember, plasma glucose is 15 % higher than whole blood glucose because of same logic. For diagnosis of diabetes, we estimate plasma glucose and not whole blood glucose. However, for legal drink limit for driving, we estimate blood alcohol content and not plasma/serum alcohol content.
_
To calculate estimated peak blood alcohol concentration (EBAC), a variation of the Widmark formula is used. The formula is:
where 0.806 is a constant for body water in the blood (mean 80.6%), SD is the number of standard drinks containing 10 grams of ethanol, 1.2 is a factor to convert the amount in grams to Swedish standards set by The Swedish National Institute of Public Health, BW is a body water constant (0.58 for men and 0.49 for women), Wt is body weight (kilogram), MR is the metabolism constant (0.017) and DP is the drinking period in hours. Regarding metabolism (MR) in the formula; Females demonstrated a higher average rate of elimination (mean, 0.017; range, 0.014-0.021 g/210 L) than males (mean, 0.015; range, 0.013-0.017 g/210 L). Female subjects on average had a higher percentage of body fat (mean, 26.0; range, 16.7-36.8%) than males (mean, 18.0; range, 10.2-25.3%). Additionally, men are, on average, heavier than women but it is not strictly accurate to say that the water content of a person alone is responsible for the dissolution of alcohol within the body, because alcohol does dissolve in fatty tissue as well. When it does, a certain amount of alcohol is temporarily taken out of the blood and briefly stored in the fat. For this reason, most calculations of alcohol to body mass simply use the weight of the individual, and not specifically his water content. Finally, it is speculated that the bubbles in sparkling wine may speed up alcohol intoxication by helping the alcohol to reach the bloodstream faster. A study conducted at the University of Surrey in the United Kingdom gave subjects equal amounts of flat and sparkling Champagne which contained the same levels of alcohol. After 5 minutes following consumption, the group that had the sparkling wine had 54 milligrams of alcohol in their blood while the group that had the same sparkling wine, only flat, had 39 milligrams.
_
Instead of BAC formula, you can use charts to determine BAC level:
_
_
_
My view:
One unit of alcohol = one standard drink = one drink = one peg = one shot.
Different countries have different amount of alcohol in one drink from 6 gm in Austria to 20 gm in Japan. This is unscientific, irrational and counter-productive as far as studies on harm vs. benefit by alcohol are considered. I therefore propose international alcohol unit equivalent to 10 grams of absolute alcohol.
One international unit (IU) = one international drink = 10 grams of absolute alcohol in any beverage.
I urge all nations to change their alcohol measurement in various beverages to international units (IU).
For example, a 750 ml beer bottle containing alcohol 5 % v/v contains 30 grams of absolute alcohol i.e. 3 IU—so that beer bottle label should mention that it contains 3 international unit of alcohol.
_
The average rate of alcohol metabolism is 100 milligrams of alcohol per kilogram of bodyweight per hour.
A 80 kg human eliminates approximately 10 ml alcohol equivalent to 8 gm alcohol per hour.
If he drinks 1 IU in one hour, his body will accumulate 10 – 8 = 2 gm of alcohol in body.
This 80 kg man has about 48 liters of water (60 % of weight). Alcohol is completely dissolved in body water after absorption and equally distributed in all tissues like water and crosses all biological membranes. Ethanol enters cells presumably by free diffusion, like water does, through the cell membrane. This can occur because the ethanol molecules, even though they are polar, are small enough. So accumulated 2 gm alcohol in 48 liters water will make it 41.6 mg/liter or 4.16mg/100 ml of (plasma) water. Since blood is 80 % water, BAL would be 4.16 x 0.8 = 3.33 mg per 100 ml blood. In other words, if 80 kg man drinks 1IU in one hour, his BAC will be 0.0033.
__________
My formula for BAC/BAL is as follows:
_
Negative value in above formula means alcohol elimination rate is faster than consumption rate; no alcohol in blood. Since every human has different alcohol elimination rate, it is impossible to exactly calculate BAL/BAC from any formula anyway.
_
Since BAC falls by 0.015 every hour (15 mg/hr) after drinking session is over, you can easily calculate how many hours it will take for blood to become alcohol free. If BAC is 0.06 then it will take 4 hours after drinking session to become zero BAC.
___
Effects of blood alcohol levels in the absence of tolerance:
| BAC in grams per 100 ml blood | Behavior | Impairment |
| 0.010–0.029 |
|
|
| 0.030–0.059 |
|
|
| 0.06–0.09 |
|
|
| 0.10–0.19 |
|
|
| 0.20–0.29 |
|
|
| 0.30–0.39 |
|
|
| 0.40–0.50 |
|
|
| >0.50 |
|
_
Legal BAC limit for driving:
The acute effects of a drug depend on the dose, the rate of increase in plasma, the concomitant presence of other drugs, and the past experience with the agent. “Legal intoxication” with alcohol in the U.S. requires a blood alcohol concentration of 0.08 g/dL, while levels of 0.04 or even lower are cited in other countries. However, behavioral, psychomotor, and cognitive changes are seen at levels as low as 0.02–0.03 g/dL (i.e., after one to two drinks). Deep but disturbed sleep can be seen at twice the legal intoxication level, and death can occur with levels between 0.30 and 0.40 g/dL. Beverage alcohol is probably responsible for more overdose deaths than any other drug. India has BAC 0.03 as legal BAC limit above which you cannot drive a vehicle. Most countries around the world have legal BAC limits. BAC levels are affected by how much alcohol has been drunk, the speed of drinking and over what period of time. An individual’s weight, gender, health, and food intake also affect the absorption and metabolism of alcohol, making an estimation of how much it is safe to drink before driving is risky.
_
Why breathalyzer:
Alcohol intoxication is legally defined by the blood alcohol concentration (BAC) level. However, taking a blood sample in the field for later analysis in the laboratory is not practical or efficient for detaining drivers suspected of driving while impaired (DWI) or driving under the influence (DUI). Urine tests for alcohol proved to be just as impractical in the field as blood sampling. What was needed was a way to measure something related to BAC without invading a suspect’s body. In the 1940s, breath alcohol testing devices were first developed for use by police. In 1954, Dr. Robert Borkenstein of the Indiana State Police invented the Breathalyzer, one type of breath alcohol testing device used by law enforcement agencies today.
_
Alcohol that a person drinks shows up in the breath because it gets absorbed from the mouth, throat, stomach and intestines into the bloodstream. Alcohol is not digested upon absorption, nor chemically changed in the bloodstream. As the blood goes through the lungs, some of the alcohol moves across the membranes of the lung’s air sacs (alveoli) into the air, because alcohol will evaporate from a solution — that is, it is volatile. The concentration of the alcohol in the alveolar air is related to the concentration of the alcohol in the blood. As the alcohol in the alveolar air is exhaled, it can be detected by the breath alcohol testing device. Instead of having to draw a driver’s blood to test his alcohol level, an officer can test the driver’s breath on the spot and instantly know if there is a reason to arrest the driver. Because the alcohol concentration in the breath is related to that in the blood, you can figure the BAC by measuring alcohol on the breath. The ratio of breath alcohol to blood alcohol is 2,100:1. This means that 2,100 milliliters (ml) of alveolar air will contain the same amount of alcohol as 1 ml of blood. Therefore, a breathalyzer measurement of 0.10 mg/L of breath alcohol converts to 0.021 g/210L of breath alcohol, or 0.021 g/100 ml of blood alcohol (0.021 BAC in the United States) or 21 mg/100 ml of BAL in India. For many years, the legal standard for drunkenness across the United States was 0.10, but many states have now adopted the 0.08 standard. The federal government has pushed states to lower the legal limit. The American Medical Association says that a person can become impaired when the blood alcohol level hits 0.05. If a person’s BAC measures 0.08, it means that there are 0.08 grams of alcohol per 100 ml of blood.
_
There are three major types of breath alcohol testing devices, and they’re based on different principles:
•Breathalyzer – Uses a chemical reaction involving alcohol that produces a color change
•Intoxilyzer – Detects alcohol by infrared (IR) spectroscopy
•Alcosensor III or IV – Detects a chemical reaction of alcohol in a fuel cell
_
_
A breathalyzer is a device for estimating blood alcohol content (BAC) from a breath sample. Breath analyzers do not directly measure blood alcohol content or concentration, which requires the analysis of a blood sample. Instead, they estimate BAC indirectly by measuring the amount of alcohol in one’s breath. Breathalyzer is the brand name for the instrument developed by inventor Robert Frank Borkenstein. It was registered as a trademark on May 13, 1958, and is active as of 2014 but the word has become a generic trademark.
_
When the user exhales into a breath-analyzer (breathalyzer), any ethanol present in their breath is oxidized to acetic acid at the anode:
CH3CH2OH + H2O = CH3CO2H + 4H+ + 4e–
At the cathode, atmospheric oxygen is reduced:
O2 + 4H+ + 4e– = 2H2O
The overall reaction is the oxidation of ethanol to acetic acid and water.
CH3CH2OH + O2 = CH3COOH + H2O
The electrical current produced by this reaction is measured by a microprocessor, and displayed as an approximation of overall blood alcohol content (BAC).
_
Common sources of error in breathalyzer:
Calibration:
Many handheld breath analyzers sold to consumers use a silicon oxide sensor (also called a semiconductor sensor) to determine the blood alcohol concentration. These sensors are far more prone to contamination and interference from substances other than breath alcohol. The sensors require recalibration or replacement every six months. Higher end personal breath analyzers and professional-use breath alcohol testers use platinum fuel cell sensors. These too require recalibration but at less frequent intervals than semiconductor devices, usually once a year.
Non-specific analysis:
One major problem with older breath analyzers is non-specificity: the machines identify not only the ethyl alcohol (or ethanol) found in alcoholic beverages but also other substances similar in molecular structure or reactivity.
Interfering compounds:
Some natural and volatile interfering compounds do exist, however. For example, the National Highway Traffic Safety Administration (NHTSA) has found that dieters and diabetics may have acetone levels hundreds or even thousands of times higher than those in others. Acetone is one of the many substances that can be falsely identified as ethyl alcohol by some breath machines. However, fuel cell based systems are non-responsive to substances like acetone. Substances in the environment can also lead to false BAC readings. For example, methyl tert-butyl ether (MTBE), a common gasoline additive, has been alleged anecdotally to cause false positives in persons exposed to it. Tests have shown this to be true for older machines; however, newer machines detect this interference and compensate for it. Any number of other products found in the environment or workplace can also cause erroneous BAC results. These include compounds found in lacquer, paint remover, celluloid, gasoline, and cleaning fluids, especially ethers, alcohols, and other volatile compounds.
Homeostatic variables:
Breath analyzers assume that the subject being tested has a 2100-to-1 partition ratio in converting alcohol measured in the breath to estimates of alcohol in the blood. However, this assumed partition ratio varies from 1300:1 to 3100:1 or wider among individuals and within a given individual over time. Assuming a true (and US legal) blood-alcohol concentration of 0.07%, for example, a person with a partition ratio of 1500:1 would have a breath test reading of .10%—over the legal limit.
Mouth alcohol:
One of the most common causes of falsely high breath analyzer readings is the existence of mouth alcohol. In analyzing a subject’s breath sample, the breath analyzer’s internal computer is making the assumption that the alcohol in the breath sample came from alveolar air—that is, air exhaled from deep within the lungs. However, alcohol may have come from the mouth, throat or stomach for a number of reasons. To help guard against mouth-alcohol contamination, certified breath-test operators are trained to observe a test subject carefully for at least 15–20 minutes before administering the test. The problem with mouth alcohol being analyzed by the breath analyzer is that it was not absorbed through the stomach and intestines and passed through the blood to the lungs. In other words, the machine’s computer is mistakenly applying the partition ratio and multiplying the result. Consequently, a very tiny amount of alcohol from the mouth, throat or stomach can have a significant impact on the breath-alcohol reading.
Testing during absorptive phase:
Absorption of alcohol continues for anywhere from 20 minutes (on an empty stomach) to two-and-one-half hours (on a full stomach) after the last consumption. Peak absorption generally occurs within an hour. During the initial absorptive phase, the distribution of alcohol throughout the body is not uniform. Uniformity of distribution, called equilibrium, occurs just as absorption completes. In other words, some parts of the body will have a higher blood alcohol content (BAC) than others. One aspect of the non-uniformity before absorption is complete is that the BAC in arterial blood will be higher than in venous blood. Other false positive of high BAC and also blood reading are related to patients with proteinuria and hematuria, due to kidney metabolization and failure. The metabolization rate of related patients with kidney damage is abnormal in relation to percent in alcohol in the breath. However, since potassium dichromate is a strong oxidizer, numerous alcohol groups can be oxidized by kidney and blood filtration, producing false positives. During the initial absorption phase, arterial blood alcohol concentrations are higher than venous. After absorption, venous blood is higher. This is especially true with bolus dosing. With additional doses of alcohol, the body can reach a sustained equilibrium when absorption and elimination are proportional, calculating a general absorption rate of 0.02/drink and a general elimination rate of 0.015/hour. (One drink is equal to 1.5 ounces of liquor, 12 ounces of beer, or 5 ounces of wine.) Breath alcohol is a representation of the equilibrium of alcohol concentration as the blood gases (alcohol) pass from the (arterial) blood into the lungs to be expired in the breath. Arterial blood distributes oxygen throughout the body. Breath alcohol concentrations are generally lower than blood alcohol concentrations, because a true representation of blood alcohol concentration is only possible if the lungs were able to completely deflate. Vitreous (eye) fluid provides the most accurate account of blood alcohol concentration.
_
Products that interfere with testing by breathalyzer:
On the other hand, products such as mouthwash or breath spray can “fool” breath machines by significantly raising test results. Listerine mouthwash, for example, contains 27% alcohol. The breath machine is calibrated with the assumption that the alcohol is coming from alcohol in the blood diffusing into the lung rather than directly from the mouth, so it applies a partition ratio of 2100:1 in computing blood alcohol concentration—resulting in a false high test reading. To counter this, officers are not supposed to administer a preliminary breath test for 15 minutes after the subject eats, vomits, or put anything in their mouth. In addition, most instruments require that the individual be tested twice at least two minutes apart. Mouthwash or other mouth alcohol will have somewhat dissipated after two minutes and cause the second reading to disagree with the first, requiring a retest. This was clearly illustrated in a study conducted with Listerine mouthwash on a breath machine and reported in an article entitled “Field Sobriety Testing: Intoxilyzers and Listerine Antiseptic” published in the July 1985 issue of The Police Chief. Seven individuals were tested at a police station, with readings of 0.00%. Each then rinsed his mouth with 20 milliliters of Listerine mouthwash for 30 seconds in accordance with directions on the label. All seven were then tested on the machine at intervals of one, three, five and ten minutes. The results indicated an average reading of 0.43 blood-alcohol concentration, indicating a level that, if accurate, approaches lethal proportions. After three minutes, the average level was still 0.020, despite the absence of any alcohol in the system. Even after five minutes, the average level was 0.011. In another study, a scientist tested the effects of Binaca breath spray on an Intoxilyzer 5000. He performed 23 tests with subjects who sprayed their throats and obtained readings as high as 0.81—far beyond lethal levels. The scientist also noted that the effects of the spray did not fall below detectable levels until after 18 minutes.
_
Base rate fallacy of breathalyzer:
One example is sufficient.
A group of policemen have breathalyzers displaying false drunkenness in 5% of the cases tested. However, the breathalyzers never fail to detect a truly drunk person. 1/1000 of drivers are driving drunk. Suppose the policemen then stops a driver at random, and force them to take a breathalyzer test. It indicates that he or she is drunk. We assume you don’t know anything else about him or her. How high is the probability he or she really is drunk?
Many would answer as high as 0.95, but the correct probability is about 0.02 according to Bayes’ theorem.
_
Drink driving limits worldwide:
Below is a list of countries and jurisdictions worldwide and the corresponding maximum legal permissible BAC limit for each country / jurisdiction. The BAC (blood alcohol content) limit defines the maximum legal amount of alcohol that is permitted to be in the blood for people to legally drive in each country and jurisdiction. BAC limits can also be referred to as ‘drink driving limits’, ‘drunk driving limits’ or ‘drink drive limits’. It is a criminal offence to drive with a blood alcohol content that is above the legal limit and the punishments and penalties for doing so can be severe! The legal BAC limit listed for each country is based on the maximum legal prescribed limit allowed for the average driver. Lower legal limits may be set in certain countries for inexperienced drivers, young drivers or professional drivers.
_
International Blood Alcohol Limits:
| BAC | Countries |
| Religion | The five listed countries currently believed to have a zero blood-alcohol limit primarily or specifically for reasons of religion are: Bahrain, Mali, Pakistan, Saudi Arabia, & UAE |
| Zero | Armenia, Azerbaijan, Czech Republic, Hungary, Jordan, Kyrgyzstan, Romania, Slovak Republic, (Uzbekistan) (10 countries) |
| 0.01% | Albania |
| 0.02% | Estonia, Norway, Poland, (Sudan), Sweden |
| 0.03% | China, Georgia, India, Japan, Moldova, Turkmenistan |
| 0.04% | Belarus, Lithuania |
| 0.05% | Argentina, Australia, Austria, Belgium, Bosnia Herzegovina, Bulgaria, Costa Rica, Croatia, Cyprus, Denmark, Finland, France, Germany, Greece, Iceland, Israel, Italy, Latvia, Macedonia, Monaco, Namibia, Netherlands, Portugal, Russia, Serbia, Slovenia, South Africa, South Korea, Spain, Switzerland, Taiwan, Thailand, Turkey, Yugoslavia |
| 0.06% | Peru |
| 0.08% | Belize, Brazil, Canada, Chile, Ecuador, Fiji, Ghana, Ireland, Jamaica, Luxembourg, Malaysia, Malta, Mauritius, New Zealand, Puerto Rico, Singapore, Tanzania, Uganda, United Kingdom, USA, Zimbabwe |
| 0.15% | Swaziland |
__________
How Alcohol can affect Safe Driving Skills:
Judgment: The ability to make sound and responsible decisions.
• Alcohol affects your mental functions first, and judgment is the first to go, which means reason and caution are quickly reduced.
• Can be affected as low as 0.02% BAC.
Concentration: The ability to shift attention from one point of action to another.
• Alcohol impairs a driver’s ability to concentrate on the multiple tasks involved in driving, such as vehicle speed, position of the vehicle, other traffic on the road, tuning the radio, and participating in conversation with passengers.
• Leaves the driver concentrating on a singular action.
Comprehension: The ability to understand situations, signs, and signals.
• Alcohol impairs the driver’s ability to “interpret” situations, signs, and/or signals which a driver must understand and/or respond to quickly to be safe on the road.
• Leaves the driver easily confused and not able to respond to emergency situations or to comprehend the meaning of simple signals (i.e.: running through a stop sign).
Coordination: The ability to coordinate motor skills.
• Impairs ability to coordinate motor skills, beginning with the fine motor skills (putting key in ignition) up to gross motor skills (walking to the car).
• Loss of coordination severely affects reaction time and ability to react.
Vision and hearing acuity: The ability to see and hear clearly.
• Reduces visual acuity up to 32%.
• Reduces peripheral vision resulting in tunnel vision.
• Impairs ability to judge distance and depth perception (position of car).
• Dilates pupil, slows down reactions of pupil resulting in problems with on-coming headlights (glare) and “blind” driving.
• Reduces the ear’s ability to hear, muffling sounds, and interfering with the ability to determine the direction of sounds.
Reaction time: Ability to see and understand a situation, then take an action.
• Severely reduced due to impairment of comprehension and coordination in particular.
• Slows down reaction time by 15-25%, resulting in crashes and accidents which could have been avoided if no alcohol was in the system.
_
Alcohol and night vision:
Alcohol consumption markedly impairs night-vision because it increases the perception of halos (luminous circles) and other visual night-time disturbances, a new study shows. This is because ethanol from alcoholic drinks passes into the tear and disturbs the outermost layer of the tear-film – the lipid layer – facilitating the evaporation of the aqueous part of the tear. In an eye with a deteriorated tear-film, the quality of the image that forms in the retina also deteriorates. Moreover, this deterioration of vision is significantly greater in subjects with breath alcohol content in excess of 0.25mg/liter – the legal limit for driving recommended by the World Health Organisation (WHO).
_
How much alcohol can I drink before driving?
The safest option is not to drink any alcohol at all if you plan to drive. Even a small amount of alcohol can affect your ability to drive, and there is no way to tell whether you are within the legal limit. If you are taking medication, one drink could put you into the “DUI” category. For some people, it often takes very little alcohol to become legally drunk and certain physical characteristics such as weight, gender and body fat percentage can all be factors in the equation. Eating can also affect your outcome – you are more likely to fail a blood alcohol test if you do not eat. So, practically, if you’re wondering how many drinks you can have before driving, the best answer is ‘None.’
_
Alcohol and reaction time:
A study was conducted to demonstrate effects of alcohol and practice on choice reaction time:
_
Effect of alcohol on reaction time:
Alcohol is water-soluble and is readily absorbed in the blood. More blood is supplied to the brain that to other organs, with the result that alcohol impairs your brain function within minutes. At a blood alcohol content (BAC) of 0.08 gm/100ml, the reaction time of the average driver doubles from 1.5 s to 3.0 s. Muscle coordination also diminishes and a driver is more likely to respond incorrectly to stimuli. A 1997 New England Journal of Medicine cited a study that found that talking on a cell phone quadruples a driver’s risk of collision, roughly the same as being drunk. Studies have shown that BAC levels as low as 0.04 gm/100 ml can affect reaction times. Simple reaction times (where the subject attempts to detect a stimulus and respond as quickly as possible) appear to be less affected by lower BACs than do complex reaction times (where the subject must discriminate between stimuli and respond appropriately.) If your BAC is 0.08 gm/100 ml, you are 4 times more likely to crash than if you are sober. At a BAC of 0.12 gm/100 ml, your chances are 15 times more likely and at a BAC of 0.16 gm/100 ml, your chances of crashing are 30 times more than if you are sober. According to an article in the 1/14/01 issue of Parade Magazine, “Three out of four teens say that they speed when they drive, and about half don’t wear seat belts. Plus, 40% say they’ve ridden with a teen driver who was intoxicated or impaired.”
_
Alcohol impairs the cognitive component of reaction time to an omitted stimulus:
Research from a recent study indicates that cognitive performance is impaired by an acute dose of alcohol at blood alcohol concentrations (BACs) that do not affect motor performance. That study measured reaction time (RT) to the omission of a recurring stimulus and used behavioral criteria to fractionate premotor (cognitive) and motor components of RT when stimuli occurred at slow, 2-second intervals (0.5 Hz). The present experiment tested the generality of the evidence when stimuli occurred at slow or fast, 0.143-second intervals (7 Hz). Using muscle potential to fractionate RT, authors tested the reproducibility of the findings obtained by a behavioral fractionation procedure. Thirty male social drinkers were randomly assigned to two groups (n = 15 each) that received 0.8 g/kg alcohol or a placebo (0 g/kg). All participants performed a drug-free baseline test and a test during rising BACs. A test presented fast and slow frequency auditory stimuli in counterbalanced order within groups. Tests using both fast and slow frequency stimuli showed that alcohol slowed premotor RT and had no detectable effect on motor RT. Fractionated RT based on muscle potential reproduced the findings based on behavioral fractionation. The generality of the deleterious effects of alcohol on premotor RT was demonstrated by manipulating the frequency of the recurring stimuli. The consistent results obtained with the omitted stimulus paradigm provide a basis for new alcohol research that incorporates electrophysiological measures of the brain potential that are associated with the omission of a stimulus.
_
Alcohol, reaction time and memory: A meta-analysis:
Moderate doses of alcohol impair performance on a variety of information processing tasks. Two separate meta-analyses were conducted on the results of (1) reaction time studies, and (2) recognition memory studies, representing 25 and 16 different task conditions, respectively. In both cases, performance with alcohol (either 0.8 or 1.0 ml/kg body weight) was plotted as a function of performance with no alcohol. For reaction time, a linear fit accounted for 99.7 per cent of the variance. The same function applied not only to the mean but to the distribution of reaction times from the 5th to the 95th percentiles. For recognition memory, a linear fit accounted for 96.2 per cent of the variance in accuracy (expressed as the logarithm of proportion correct). Thus alcohol appears to have a general linear effect on information processing, rather than specific effects on a subset of stages. It is concluded that the results are consistent with a reduced processing resources hypothesis for the impairment with alcohol.
_
Alcohol and accidents:
The association between alcohol use and accidental injury or death has been acknowledged for a long time. Alcohol is thought to contribute to 50 000 deaths per year and up to 500 000 hospital admissions annually in the UK. Thus, up to 40% of all hospitalisation relates directly or indirectly to alcohol. As blood alcohol concentration (BAC) rises, so does the risk of accidents. It’s affected by all sorts of factors, including how much alcohol you drink, how fast you drink it, your body size, how much you’ve eaten, your gender and even your emotional health. Adverse effects on vision have been found at blood alcohol concentrations of 30mg%, and the psychomotor skills required for driving have been found to show impairment from 40mg% (in the UK the legal blood alcohol limit for drivers is 80mg%). Raised risk of accident can also remain some time after drinking, as skills and faculties do not necessarily return to normal immediately even once all alcohol has left the body. Alcohol’s ability to increase the risk of danger extends beyond the home. According to Alcoholics Anonymous, a quarter of accidents at work are drink-related.
_
Alcohol and Accidents: Can one drink kill?
The article, by sociologists David Phillips and Kimberly Brewer, appears in the issue of the journal Addiction. The authors find that any amount of alcohol consumed by drivers increases the severity of injuries in automobile accidents. On the basis of this finding, they argue that the legal limits of blood alcohol concentration for drivers should be lowered below the current level: “The severity of life-threatening motor vehicle accidents increases significantly at blood alcohol concentrations far lower than the current US limit of 0.08%.” Their data comes from the Fatality Analysis Reporting System (FARS), a data set which has the advantages of including all fatal auto accidents in the US and measuring blood alcohol concentration (BAC) in increments of only 0.01%.
_
_
The graph above shows that the relative seriousness of injuries drops when BAC rises to 0.03% and it remains stable at 0.04%, before rising at 0.05% to about the same level of severity found at 0.02%. Following the authors’ policy inferences from their findings, one might advise drivers to avoid that first drink, but if they are already up to 0.02% BAC, they should take another drink to bring them up to 0.03% or 0.04% BAC, since that would reduce their likelihood of serious injury. Of course, no one would seriously make this suggestion. But this shows the danger of prescribing policy based on a data analysis that is confined to the last two data points at one end of the tail of a statistical curve. Nonetheless, it is clear that even one drink can cause accident and death.
_
Traffic accidents: drunk vs. sober drivers:
It is clear that drinking drivers who crash are similar in many ways to sober drivers who crash. Both groups are disproportionately young, male, single, suffer from alcohol or drug problems, and are characterized by aggression, hostility or other “undesirable” attitudes and personality traits. Drunk drivers don’t become model drivers when sober. Even when completely sober, those who sometimes drive drunk, are at high risk of being involved in traffic accidents. But there’s every reason to believe that alcohol frequently contributes to crashes. One technique that demonstrates this is called responsibility analysis. By examining multiple-vehicle crash reports without knowledge of drivers’ blood alcohol concentrations (BACs), researchers estimate the degree to which each driver was responsible for his or her crash. In a sample of injured drivers in Monroe County, NY, it was estimated that 34-43% of sober drivers were responsible compared to 74-90% of intoxicated drivers (BAC of 0.10 or higher). A large study of 1,882 fatally injured drivers in several states concluded that 68% of sober drivers and 94% of intoxicated drivers (0.10 BAC or higher) were responsible for their crashes. The responsibility rates were higher in this study, which included single vehicle crashes, largely because drivers in single vehicle crashes are almost always deemed responsible. Nevertheless, the pattern is the same: responsibility for accidents increases with intoxication. How many drunk drivers would have had accidents if they were sober? Again, no one knows. But one expert, James Hedlund, has identified three broad types of drinking drivers, for whom the answer probably differs:
1. “Normal” drivers who are social drinkers. Such drivers may miscalculate the effects of alcohol on their performance. Dr. Hedlund asserts that alcohol increases their crash risk and their crash rates would decrease substantially if they did not drive after drinking,
2. “High-risk” drivers. These are frequent drinkers, for whom alcohol abuse “may be just another manifestation of risk-taking behavior or may enable this behavior by removing what inhibitions they have.” Abstaining may not reduce their crash rates much, and
3. Alcoholics, for whom alcohol abuse is an integral part of life Abstaining would require a complete lifestyle change. If they abstained, their crash rates should drop significantly.
The three groups are affected differently by measures to limit drinking and driving. “Normal” drivers can be deterred by the legal consequences of arrest and sanction for impaired driving and also can be affected by education and prevention methods. Arguably, much of the reduction in alcohol-involved crashes may have come from changes in the behavior of this group. In contrast, alcoholics are unlikely to be affected by anything that does not deal directly with their alcoholism. Traffic safety can play an important role by screening DWI offenders for alcohol problems and assuring that they are referred to treatment as appropriate, but other traffic safety measures are unlikely to have much effect. “High-risk” drivers are perhaps the hardest group to affect. Deterrence, even arrest and punishment, may have little influence on their behavior. Some high-risk behavior is outgrown as drivers mature. However, since high-risk behavior is rooted so deeply in some drivers’ personalities, any change requires measures for broader than those available to traffic safety. Although it appears to be significant, the proportion of alcohol-involved traffic accidents that would have occurred even if the drivers had been sober remains unknown.
_
What proportion of all motor vehicle crashes is caused by alcohol?
It is impossible to say with certainty. Although alcohol is known to increase crash likelihood, its presence is neither necessary nor sufficient to cause a crash. Every crash in which a driver has a high BAC is not caused by alcohol. To learn the number of crashes caused by driving at various BACs, it would be necessary to find out how many trips that do not involve crashes are driven by people with positive BACs — something that is only measured periodically in roadside surveys or special studies of motorists not involved in crashes.
What proportion of motor vehicle crashes involves alcohol?
The most reliable information about alcohol involvement comes from fatal crashes. In 2002, 32 percent of fatally injured drivers had BACs of at least 0.08 percent. Although alcohol may not have been a causal factor in all of the crashes, this statistic is frequently used to measure the change over time in alcohol involvement in fatal crashes. In 2002, the National Highway Traffic Safety Administration (NHTSA) estimated that 35 percent of all traffic deaths occurred in crashes in which at least one driver or non-occupant had a BAC of 0.08 percent or more and that any alcohol was present in 41 percent of all fatal crashes in 2002.Such statistics are sometimes cited as proof that a third to half of all fatal crashes are caused by “drunk driving” and that none of the crashes that involve alcohol would occur if the alcohol were not present. But this is incorrect and misleading because alcohol is only one of several factors that contribute to crashes involving drinking drivers. Furthermore, some fatally injured people in alcohol-related crashes are pedestrians with positive BACs, and these fatalities still would occur even if every driver were sober. Alcohol involvement is much lower in crashes involving nonfatal injuries, and it is lower still in crashes that do not involve injuries at all. Ten percent (10%) of all people who receive injuries in traffic accidents do so in alcohol-related crashes, according to NHTSA estimates. It is estimated that 3.22% of these injury-producing crashes involve intoxicated drivers. Seven percent (7%) of all traffic accidents involve alcohol use, according to NHTSA estimates. It is estimated that 2.25% of all vehicular crashes involve intoxicated drivers. These statistics are all estimates based on incomplete information. Often they are estimates based on other estimates. However, 12.8% of all drivers involved in fatal accidents in the U.S. during 2001 are known to have been intoxicated according to the BAC laws (.10 or .08) of their state. This number is based on a systematic examination of the official records of each and every accident involving a fatality during that year in the US. It is based on factual evidence rather than on estimates or guesses. The higher numbers commonly reported in the press refers to accidents in which NHTSA believes that some alcohol has been consumed by someone associated with the accident. For example, if a person who was believed to have consumed any alcohol is stopped at a red light and is rear-ended by an inattentive completely sober driver, that accident is considered to be alcohol-related. Alcohol consumption, cell phone use, drowsy driving, aggressive driving, and drugged driving are all important but preventable causes of traffic accidents, injuries and deaths. There has been a dramatic and continuing drop in alcohol-related traffic crashes, but much more needs to be done to prevent drunk driving.
_
Alcohol effect lingers on brain:
In a study of airline pilots who had to perform routine tasks in a simulator under 3 alcohol test conditions, it was found that:
•before the ingestion of any alcohol, 10% of them could not perform all the operations correctly;
•after reaching a blood alcohol concentration of 100mg/dl, 89% could not perform all the operations correctly;
•and 14 hours later, after all the alcohol had left their systems, 68% still could not perform all the operations correctly.
_
Alcohol impairs the functioning of the brain for longer than previously thought, research suggests. In fact, even after people think the effects have worn off, it is actually still having a negative impact on certain functions. Scientists examined the effect of alcohol on complex, or executive, brain functions such as abstract reasoning, planning and the ability to monitor our own behaviour in response to external feedback. They found that performance in these areas was affected even after the concentration of alcohol in the blood had dipped to the point that people were no longer aware of its effect. In fact, the effect on these “higher order” brain functions appeared to be more pronounced as blood alcohol concentration began to decline from its peak. Executive brain functions are controlled by an area of the brain known as the frontal lobe. The frontal lobe is more than twice as large in humans as it is in our nearest primate relatives. Many scientists believe it is this area of the brain that defines us as a species because it provides us with the ability for complex thought. The researchers compared the performance of volunteers who were given a mix of alcohol and orange juice to drink with that of a control group who were given a non-alcoholic placebo. Lead researcher Professor Robert Pihl, of McGill University, Montreal, Canada, said the results had serious implications for activities such as driving. He said: “People who think they’ve waited their two hours before driving home may need to actually wait six hours; or else, maybe at the time when you least expect it, you’re the most vulnerable.” “The drinker in the process of re-attaining sobriety is likely to be more dangerous, for example, than the drinker who is still imbibing.” A spokeswoman for the charity Alcohol Concern told BBC News Online: “It is obviously a matter of concern that alcohol affects cognitive performance. “We need to be more aware of the effect of alcohol has on our functioning.” Action on Addiction welcomed the study. “These results confirm what many have long suspected”, said Lesley King-Lewis, its chief executive. “People cannot think clearly after drinking, even the next day.” “This has important economic implications. British office staffs have a culture of drinking after work. This research suggests that they cannot be effective the next day. “Binge-drinking can also have serious effects on mental health. The effects of alcohol on the brain are not yet fully understood and need to be investigated further. “This research is particularly concerning as more and more people are regularly drinking well over the recommended limits.” The research is published in the journal Alcoholism: Clinical & Experimental Research.
_________
Alcohol toxicity:
Primary alcohols (R-CH2-OH) can be oxidized either to aldehydes (R-CHO) (e.g. acetaldehyde) or to carboxylic acids (R-CO2H), while the oxidation of secondary alcohols (R1R2CH-OH) normally terminates at the ketone (R1R2C=O) stage. Tertiary alcohols (R1R2R3C-OH) are resistant to oxidation. Ethanol’s toxicity is largely caused by its primary metabolite, acetaldehyde and secondary metabolite acetic acid. All primary alcohols are broken down into aldehydes then to carboxylic acids whose toxicities are similar to acetaldehyde and acetic acid. Metabolite toxicity is reduced in rats fed N-acetylcysteine and thiamine. Tertiary alcohols cannot be metabolized into aldehydes and as a result they cause no hangover or toxicity through this mechanism. Some secondary and tertiary alcohols are less poisonous than ethanol because the liver is unable to metabolize them into toxic by-products. This makes them more suitable for recreational and medicinal use as the chronic harms are lower. Ethchlorvynol and tert-Amyl alcohol are good examples of tertiary alcohols which saw both medicinal and recreational use. Other alcohols are substantially more poisonous than ethanol, partly because they take much longer to be metabolized and partly because their metabolism produces substances that are even more toxic. Methanol (wood alcohol), for instance, is oxidized to formaldehyde and then to the poisonous formic acid in the liver by alcohol dehydrogenase and formaldehyde dehydrogenase enzymes, respectively; accumulation of formic acid can lead to blindness or death. Likewise, poisoning due to other alcohols such as ethylene glycol or diethylene glycol are due to their metabolites, which are also produced by alcohol dehydrogenase. Methanol itself, while poisonous (LD50 5628 mg/kg, oral, rat), has a much weaker sedative effect than ethanol. Isopropyl alcohol is oxidized to form acetone by alcohol dehydrogenase in the liver but has occasionally been abused by alcoholics, leading to a range of adverse health effects. An effective treatment to prevent toxicity after methanol or ethylene glycol ingestion is to administer ethanol. Alcohol dehydrogenase has a higher affinity for ethanol, thus preventing methanol from binding and acting as a substrate. Any remaining methanol will then have time to be excreted through the kidneys.
_
What is the difference between a blackout and passing out?
“Blackouts” (sometimes referred to as alcohol-related memory loss or “alcoholic amnesia”) occur when people have no memory of what happened while intoxicated. During a blackout, someone may appear fine to others; however, the next day s/he cannot remember parts of the night and what s/he did. The cause of blackouts is not well understood but may involve the interference of short-term memory storage, deep seizures, or in some cases, psychological depression. Blackouts shouldn’t be confused with “passing out,” which happens when people lose consciousness from drinking excessive amounts of alcohol. Losing consciousness means that the person has reached a very dangerous level of intoxication; they could aspirate on their vomit or slip into a coma. If someone has passed out, call EMS immediately (401.863-4111). S/he needs immediate medical attention.
_
Alcohol consumption and balance:
Alcohol can affect balance, by changing the viscosity of the endolymph within the otolithic membrane, the fluid inside the semicircular canals inside the ear. The endolymph surrounds the cupula which contains hair cells within the semicircular canals. When the head is tilted, the endolymph flows and moves the cupula. The hair cells then bend and send signals to the brain indicating the direction in which the head is tilted. By changing the viscosity of the endolymph to become less dense when alcohol enters the system, the hair cells can move more easily within the ear, which sends the signal to the brain and results in exaggerated and overcompensated movements of body. This can also result in vertigo, or “the spins.”
_
Acute alcoholic intoxication:
Alcohol intoxication (also known as drunkenness or inebriation) is a physiological state induced by the ingestion of ethyl alcohol (ethanol). Alcohol intoxication is the consequence of alcohol entering the bloodstream faster than it can be metabolized by the liver, which breaks down the ethanol into non-intoxicating byproducts. Some effects of alcohol intoxication (such as euphoria and lowered social inhibitions) are central to alcohol’s desirability as a beverage and its history as one of the world’s most widespread recreational drugs. Despite this widespread use and alcohol’s legality in most countries, many medical sources tend to describe any level of alcohol intoxication as a form of poisoning due to ethanol’s damaging effects on the body in large doses, and some religions consider alcohol intoxication to be a sin. Alcohol is a depressant, which means it slows the function of the central nervous system. Alcohol actually blocks some of the messages trying to get to the brain. This alters a person’s perceptions, emotions, movement, vision, and hearing. In very small amounts, alcohol can help a person feel more relaxed or less anxious. More alcohol causes greater changes in the brain, resulting in intoxication. Symptoms of alcohol intoxication include euphoria, flushed skin and decreased social inhibition at lower doses, with larger doses producing progressively severe impairments of balance, muscle coordination (ataxia), and decision-making ability (potentially leading to violent or erratic behavior) as well as nausea or vomiting from alcohol’s disruptive effect on the semicircular canals of the inner ear and chemical irritation of the gastric mucosa. People who have overused alcohol may stagger, lose their coordination, and slur their speech. They will probably be confused and disoriented. Depending on the person, intoxication can make someone very friendly and talkative or very aggressive and angry. Reaction times are slowed dramatically — which is why people are told not to drink and drive. People who are intoxicated may think they’re moving properly when they’re not. They may act totally out of character. When large amounts of alcohol are consumed in a short period of time, alcohol poisoning can result. Sufficiently high levels of blood-borne alcohol will cause coma and death from the depressive effects of alcohol upon the central nervous system. “Acute alcohol poisoning” is a related medical term used to indicate a dangerously high concentration of alcohol in the blood, high enough to induce coma, respiratory depression, or even death. It is considered a medical emergency. In the USA approximately 50,000 cases of alcohol poisoning are reported annually. About one patient dies each week in the USA from alcohol poisoning. Those at highest risk of suffering from alcohol poisoning are college students, chronic alcoholics, those taking medications that might clash with alcohol, and sometimes children who may drink because they wish to know what it is like. Acute ethanol ingestion may cause severe effects, including hypothermia, hypotension and reduced consciousness, especially in alcohol‐naive patients. Clinical effects might not become apparent until several hours after ingesting potentially toxic quantities of ethanol. Therefore, consideration should be given to monitoring the patient for at least 4 h after ingestion. Intensive supportive care is needed until ethanol concentrations fall to non‐toxic levels.
_
The median lethal dose of alcohol in test animals is a blood alcohol content of 0.45%. This is about six times the level of ordinary intoxication (0.08%), but vomiting or unconsciousness may occur much sooner in people who have a low tolerance for alcohol. The high tolerance of chronic heavy drinkers may allow some of them to remain conscious at levels above 0.40%, although serious health dangers are incurred at this level.
_
Diagnosis of acute alcoholic intoxication and poisoning:
Definitive diagnosis relies on a blood test for alcohol, usually performed as part of a toxicology screen. Law enforcement officers often use breathalyzer units and field sobriety tests as more convenient and rapid alternatives to blood tests. For determining whether someone is intoxicated by alcohol by some means other than a blood-alcohol test, it is necessary to rule out other conditions such as hypoglycemia, stroke, usage of other intoxicants, mental health issues, and so on. It is best if his/her behavior has been observed while the subject is sober to establish a baseline. Several well-known criteria can be used to establish a probable diagnosis. For a physician in the acute-treatment setting, acute alcohol intoxication can mimic other acute neurological disorders, or is frequently combined with other recreational drugs that complicate diagnosis and treatment.
_
Differential Diagnoses of acute alcoholic intoxication:
•Attention Deficit Hyperactivity Disorder
•Child Abuse & Neglect: Reactive Attachment Disorder
•Cognitive Deficits
•Conduct Disorder
•Dehydration
•Diabetic Ketoacidosis
•Gastroenteritis
•Head Trauma
•Hyperammonemia
•Hypoglycemia
•Hyponatremia
•Respiratory Distress Syndrome
•Respiratory Failure
•Toxicity, Carbon Monoxide
•Toxicity, Oral Hypoglycemic Agents
_
Know what not to do:
Acute alcohol poisoning can be extremely dangerous. Your best intentions could make it worse. There are so many myths around about how to deal with people who have drunk to excess, so it is a good idea to make sure you are aware of what NOT to do.
NEVER:
•Leave someone to sleep it off. The amount of alcohol in someone’s blood continues to rise even when they are not drinking. That is because alcohol in the digestive system carries on being absorbed into the bloodstream.
•Give them a coffee. Alcohol dehydrates the body. Coffee will make someone who is already dehydrated even more so. Severe dehydration can cause permanent brain damage.
•Make them vomit. Their gag reflex won’t be working properly which means they could choke on their vomit.
•Walk them around. Alcohol is a depressant which slows down your brain’s functions and affects your sense of balance. Walking them around might cause accidents.
•Put them under a cold shower. Alcohol lowers your body temperature, which could lead to hypothermia. A cold shower could make them colder than they already are.
•Let them drink any more alcohol. The amount of alcohol in their bloodstream could become dangerously high.
_
Five things to do if someone is showing signs of alcohol poisoning
1. Try to keep them awake and sitting up.
2. Give them some water, if they can drink it.
3. Lie them on their side in the recovery position if they have passed out, and check they are breathing properly.
4. Keep them warm.
5. Stay with them and monitor their symptoms.
_
Management:
The first priority in treating severe intoxication is to assess vital signs and manage respiratory depression, cardiac arrhythmia, or blood pressure instability, if present. The possibility of intoxication with other drugs should be considered by obtaining toxicology screens for opioids or other CNS depressants such as benzodiazepines. Aggressive behavior should be handled by offering reassurance but also by considering the possibility of a show of force with an intervention team. If the aggressive behavior continues, relatively low doses of a short-acting benzodiazepine such as lorazepam (e.g., 1–2 mg PO or IV) may be used and can be repeated as needed, but care must be taken not to destabilize vital signs or worsen confusion. An alternative approach is to use an antipsychotic medication (e.g., 0.5–5 mg of haloperidol PO or IM every 4–8 h as needed, or olanzapine 2.5–10 mg IM repeated at 2 and 6 h, if needed). Acute alcohol poisoning is a medical emergency due to the risk of death from respiratory depression and/or inhalation of vomit if emesis occurs while the patient is unconscious and unresponsive. Emergency treatment for acute alcohol poisoning strives to stabilize the patient and maintain a patent airway and respiration, while waiting for the alcohol to metabolize:
Also:
• Assess the airway. If necessary, secure the airway with an endotracheal (ET) tube if the patient is not maintaining good ventilation or if a significant risk of aspiration is observed. Provide respiratory support and mechanical ventilation if needed.
◦ Obtain intravenous (IV) access and replace any fluid deficit or use a maintenance fluid infusion. Use plasma expanders and vasopressors to treat hypotension, if present.
◦ Ensure that the patient maintains a normal body temperature.
•Treat hypoglycaemia (low blood sugar) with 50 ml of 50% dextrose solution and saline flush, as ethanol induced hypoglycaemia is unresponsive to glucagon.
• Administer the vitamin thiamine to prevent Wernicke-Korsakoff syndrome, which can cause a seizure (more usually a treatment for chronic alcoholism, but in the acute context usually co-administered to ensure maximal benefit).
• Apply haemodialysis if the blood concentration is dangerously high (>400 mg %), and especially if there is metabolic acidosis.
• Provide oxygen therapy as needed via nasal cannula or non-rebreather mask.
◦ Fructose infusion can increase the ethanol clearance by 25%. However, the use of fructose is not recommended because significant adverse effects may occur. For instance, fructose infusion can cause lactic acidosis, severe osmotic diuresis, and GI symptoms; therefore, it is not routinely used in the treatment of ethanol intoxication.
Additional medication may be indicated for treatment of nausea, tremor, and anxiety.
___________
Hangover:
Hangovers are the body’s reaction to poisoning and withdrawal from alcohol. Hangovers begin 8 to 12 hours after the last drink and symptoms include fatigue, depression, headache, thirst, nausea, and vomiting. The severity of symptoms varies according to the individual and the quantity of alcohol consumed. The exact cause of hangovers is not completely understood, but they are a well known problem with ingesting alcohol. Bad alcohol hangovers are considered to be worse than the day-after effects of nearly any other psychoactive.
Alcohol Hangover Symptoms are as follows:
- Headache
- Irritability, bad mood
- Thirst
- Nausea, vomiting, and/or dry-heaves
- Vertigo (dizziness that becomes worse with movement)
- Light and sound sensitivity (loud noises and bright lights cause pain/discomfort)
- Inability to think clearly
- Muscle fatigue and pain
- Sweating, tremors
Cause / Mechanism of Hangover:
There are a variety of factors that determine how bad a hangover is. The primary causes of hangover are believed to be dehydration and related electrolyte imbalance, blood sugar regulation disturbance, acute withdrawal, toxicity from alcohol metabolites, interaction with congeners (non-alcohol components of drinks), reduced sleep quality, and personal biological profile.
Dehydration and Electrolyte Imbalance: Alcohol is a diuretic, causing the body to urinate more than normal, leading to dehydration and electrolyte imbalances. Alcohol intake inhibits ‘anti-diuretic hormone’ (ADH, also known as vasopressin), which alters how urine is produced. Reduced ADH levels cause more urine to be produced and electrolytes (salts such as sodium, potassium, or magnesium) are expelled with the urine. Generally, dehydration and electrolyte imbalances just make everything else worse and even moderate loss of fluid can cause dizziness, lightheadedness, weakness, and difficulty thinking clearly.
Blood Sugar / Hypoglycemia: Alcohol ingestion can also cause changes to blood sugar levels, tending to cause hypoglycemia (low blood sugar) that can contribute to weakness, fatigue and bad mood.
Sleep Quality: It is common for people to drink heavily just before or during their normal sleep period. Drinking heavily worsens sleep quality, and reduced sleep quality contributes to hangover-related tiredness and generally worsens other symptoms.
Short-term tolerance and withdrawal: Perhaps the most surprising component of alcohol hangovers is that it is currently believed that alcohol causes short-term tolerance followed by acute withdrawal as blood levels fall. This short-term accustomation to the presence of alcohol may lead to withdrawal effects as the body re-calibrates as the alcohol is cleared from the system. This ‘acute withdrawal’ effect is the reason the “hair of the dog” hangover remedy works at all (drinking more alcohol in the morning to combat a bad hangover). The mechanism for the acute withdrawal symptoms is currently believed to be the short-term down regulation of GABA receptors and up-regulation of glutamate receptors as the body counterbalances the sedative effects of the alcohol. As alcohol levels in the bloodstream fall, it takes time for the GABA and glutamate systems to return to normal.
Alcohol Metabolites: Ethyl alcohol (drinking alcohol) is metabolized first by the enzyme alcohol dehydogenase into acetaldehyde, which is then metabolized into acetate by the enzyme aldehyde dehydrogenase. Although acetaldehyde is quickly metabolized by most people and its exact role in hangover is not well understood, acetaldehyde by itself is toxic at moderate doses, causing sweating, nausea, and vomiting.
Congeners: Congeners are also believed to play a large role in many hangovers. Congeners include tannins, flavorings, colorings, etc. Red wine, for instance, is known to cause mild histamine reactions in many people whereas white wine does not. The congeners are believed to contribute to hangovers from drinking darker alcoholic beverages such as red wine, whiskey, brandy, etc.
Long-term tolerance: Regular drinkers tend to have less symptoms from hangover than occasional binge drinkers. As with many other toxins, it is likely that those who are regular alcohol users have developed tolerance to and physical ability to manage the toxic effects. Occasional drinkers are more likely to get bad hangovers than regular ones.
Personal biological profiles: Everyone reacts differently to every substance, and alcohol is no exception. Family history, personal idiosyncrasies, and a variety of other poorly understood factors determine whether someone will get a hangover and/or how bad it is. There are many stories of people who get no hangover whatsoever even after extremely heavy binge drinking. It is also common for this ‘ability’ to change over time, and some people who formerly never got hangovers find themselves getting hangovers as bad as everyone else.
_
Biology of a Hangover: Congeners:
Different types of alcohol can result in different hangover symptoms. This is because some types of alcoholic drinks have a higher concentration of congeners, byproducts of fermentation in some alcohol. The greatest amounts of these toxins are found in red wine and dark liquors such as bourbon, brandy, whiskey and tequila. White wine and clear liquors such as rum, vodka and gin have fewer congeners and therefore cause less frequent and less severe hangovers. In one study, 33 percent of those who drank an amount of bourbon relative to their body weight reported severe hangover, compared to 3 percent of those who drank the same amount of vodka. Because different alcoholic drinks (beer, wine, liquor) have different congeners, combining the various impurities can result in particularly severe hangover symptoms. Additionally, the carbonation in beer actually speeds up the absorption of alcohol. As a result, following beer with liquor gives the body even less time than usual to process.
_
Biology of a Hangover: Glutamine Rebound:
After a night of alcohol consumption, a drinker won’t sleep as soundly as normal because the body is rebounding from alcohol’s depressive effect on the system. When someone is drinking, alcohol inhibits glutamine, one of the body’s natural stimulants. When the drinker stops drinking, the body tries to make up for lost time by producing more glutamine than it needs. The increase in glutamine levels stimulates the brain while the drinker is trying to sleep, keeping them from reaching the deepest, most healing levels of slumber. This is a large contributor to the fatigue felt with a hangover. Severe glutamine rebound during a hangover also may be responsible for tremors, anxiety, restlessness and increased blood pressure.
__
People have tried many different things to relieve the effects of “the morning after,” and there are a lot of myths about what to do to prevent or alleviate a hangover. The only way to prevent a hangover is to drink in moderation:
Here are some of the things that WON’T help a hangover:
•Drinking a little more alcohol the next day. This simply puts more alcohol in your body and prolongs the effects of the alcohol intoxication.
•Having caffeine while drinking will not counteract the intoxication of alcohol; you simply get a more alert drunk person. Excessive caffeine will continue to lower your blood sugar and dehydrate you even more than alcohol alone.
•It’s best not to take a pain reliever before going to bed. Give your body a chance to process the alcohol before taking any medication.
_
Here are some things that MIGHT help a hangover:
•When you wake up, it’s important to eat a healthy meal. Processing alcohol causes a drop in blood sugar and can contribute to headaches.
•Drink plenty of water and juice to get rehydrated.
Drink water to avoid Hangovers:
The best hangover remedy is to make sure to drink water while you’re drinking alcohol. Ideally this means interspersing an occasional glass of water while you’re drinking. But even if you can’t do this…drink a large glass of water before bed and set another next to your bed to drink from in the middle of the night. Despite the simplicity of this method, most people don’t do it.
•Take a pain reliever like acetaminophen when you wake up. Do not take a pain reliever before going to bed because it will tax your liver. Let your body process the alcohol while you are sleeping.
•Avoid excessive caffeine as it may contribute to dehydration. However, if you drink coffee every morning, have your first cup not more than a couple of hours after your regular time. Don’t force your body to go through caffeine withdrawal in addition to alcohol withdrawal.
•An over-the-counter antacid may relieve some of the symptoms of an upset stomach.
•Do not go too many hours without food as this will increase the effect of the low blood sugar caused by alcohol.
•Eat complex carbohydrates like crackers, bagels, bread, cereal or pasta.
_________________
Alcohol and brain:
Alcohol’s action on the brain produces of a number of behavioral effects. These effects are dependent upon the
1. amount of alcohol taken in,
2. the time period over which the alcohol is drunk,
3. whether other drugs are being taken at the same time,
4. the previous drinking history of the individual,
5. the physical state of the person doing the drinking,
6. the genetic background of the individual( i.e. ethnicity, gender),
7. the mood and psychological makeup of the individual and
8. the environment when alcohol is taken.
_
1. Amount of alcohol drunk: Generally small amounts of alcohol [Blood Alcohol Concentrations (BAC) = 0.03 – 0.12%] produce lowered inhibitions, feelings of relaxation, more self confidence, diminished judgment, reduced attention span, and slight incoordination. BAC’s of 0.09 to 0.25% induce more incoordination, slower reaction times, loss of balance, blurred vision, exaggerated motions, difficulty in remembering. Higher BACs to 0.3% result in confusion, dizziness, slurred speech, severe intoxication, alterations in mood including withdrawal, aggression, or increased affection, and diminished ability to feel pain. Even higher BACs, to 0.4%, can result in stupor, being incapacitated, having loss of feeling,, being difficult to arouse, and lapses in and out of consciousness. Finally, as the blood level approaches 0.50% the person may die due to a variety of physiological complications such as diminished reflexes, slower heart rate, lower respiration, and decreased body temperature.
2. Time over which the alcohol is drunk: Rapid intake of alcohol results in more alcohol in the stomach and small intestine. This produces a larger gradient of alcohol and greater absorption into the blood stream and thus distribution into the tissues including the brain. If alcohol is taken in more rapidly than it is metabolized, the BAC continues to rise.
3. Use of other drugs with alcohol: The utilization of other drugs at the same time that alcohol is being drunk can result in increased effects of the alcohol. This action can occur several ways including enhancing the absorption and distribution of alcohol, action on the same chemical systems in the brain as alcohol, and/or slowing the metabolism of ethanol through competition at the liver for metabolizing enzymes or even damage to the liver so it doesn’t work as well.
4. Previous drinking history: The previous drinking history is influential in determining the effects of current alcohol consumption. Often times, dependent upon the amount and timing of prior alcohol consumption, the person will develop a tolerance. Tolerance to alcohol can be loosely defined as needing more alcohol to produce the same effect. Therefore, a person who has developed tolerance will need more alcohol to produce some of the same effects. It should be noted that not all systems underlying behavior develop tolerance at the same rate. In addition to tolerance, it is probably that after heavy long-term drinking that damage has been done to the brain and to the liver. In these cases response to alcohol may be different than that originally seen and/or prolonged since the liver can’t metabolize the ethanol as rapidly.
5. Physical state: A person’s physical state can be an important determinant of their response to alcohol. As mentioned in number four above, if a person has an impaired liver, then the metabolism of ethanol will be impaired thus enhancing and/or prolonging the alcohol action. Further, the nutritional status of the person can be an important determinant of the action. Food in the stomach will compete with ethanol for absorption into the blood stream. It is well known that alcohol competes and influences the processing of nutrients in the body. To the extent that a well nourished body is able to respond to everyday demands of living, the extent of malnourishment may determine the extent and magnitude to which the body can respond to alcohol.
6. Genetic background: The genetic background of an individual is an important determinant in the response to alcohol. There are several important examples of this. A certain portion of the Asian population carries modifications of enzymes responsible for the metabolism of alcohol such that drinking causes these individuals to have facial flushing and become sick or nauseous. Women are generally more responsive than men to the same amount of alcohol because of differences in metabolism and differences in the amount of body water. Children of alcoholics are much more likely to become alcoholic, findings that are not a result of environment. Many strains of animals are more responsive to alcohol than are other strains and animals have been bred to prefer alcohol, sleep longer after ethanol administration, and to have more severe withdrawal from alcohol.
7. Mood and psychological makeup: Use of alcohol tends to potentiate the mood of the user. Thus, if one is sad, alcohol may make you sadder. If you are happy, alcohol may make you happier. The psychologically make-up of an individual becomes important since alcohol may diminish some controls, which keep the person functioning well under usual circumstances. Loss of those controls may lead to difficulties such as aggression and other unwanted behaviors.
8. Environment: The environment in which a person drinks is an important determinant of the effects of alcohol. For example drinking at a festive party will often cause the person to become more festive. A good example of this is the behavior of the thousands of people who attend Mardi Gras in New Orleans each year. This is essentially a huge party that goes on and on and people’s behavior and energy level is potentiated by the group. In contrast, it would be expected that drinking at sad occasions would result in more sadness.
_
Drinking is a learned behavior. Children begin to learn about alcohol and its effects long before they have had their first drinking experience. They continue to learn about it as a function of where and how they obtain their first drink, who introduces it, how much the environment allows or even encourages a progression of drinking, and their own subjective experience of the drug’s pharmacologic effects. Thus, alcohol involvement occurs over time and progresses—or not—according to an intricate process that involves the larger sociocultural system; the individual’s age, life stage, and social role within that system; the demands and opportunities of the individual’s more immediate social environment; and the unique pattern of neurobiological vulnerability and protection that his or her genetic endowment provides.
_
The order in which alcohol affects the various brain centers is as follows:
1. Cerebral cortex
2. Limbic system
3. Cerebellum
4. Hypothalamus and pituitary gland
5. Medulla (brain stem)
_
Cerebral Cortex:
The cerebral cortex is the highest portion of the brain. The cortex processes information from your senses, does your “thought” processing and consciousness (in combination with a structure called the basal ganglia), initiates most voluntary muscle movements and influences lower-order brain centers. In the cortex, alcohol does the following:
•Depresses the behavioral inhibitory centers – The person becomes more talkative, more self-confident and less socially inhibited.
•Slows down the processing of information from the senses – The person has trouble seeing, hearing, smelling, touching and tasting; also, the threshold for pain is raised.
•Inhibits thought processing – The person does not use good judgment or think clearly.
These effects get more pronounced as the BAC increases.
Limbic System:
The limbic system consists of areas of the brain called the hippocampus and septal area. The limbic system controls emotions and memory. As alcohol affects this system, the person is subject to exaggerated states of emotion (anger, aggressiveness, withdrawal) and memory loss.
Cerebellum:
The cerebellum coordinates the movement of muscles. The brain impulses that begin muscle movement originate in the motor centers of the cerebral cortex and travel through the medulla and spinal cord to the muscles. As the nerve signals pass through the medulla, they are influenced by nerve impulses from the cerebellum. The cerebellum controls fine movements. For example, you can normally touch your finger to your nose in one smooth motion with your eyes closed; if your cerebellum were not functioning, the motion would be extremely shaky or jerky. As alcohol affects the cerebellum, muscle movements become uncoordinated. In addition to coordinating voluntary muscle movements, the cerebellum also coordinates the fine muscle movements involved in maintaining your balance. So, as alcohol affects the cerebellum, a person loses his or her balance frequently. At this stage, this person might be described as “falling down drunk.”
Hypothalamus and Pituitary Gland:
The hypothalamus is an area of the brain that controls and influences many automatic functions of the brain through actions on the medulla, and coordinates many chemical or endocrine functions (secretions of sex, thyroid and growth hormones) through chemical and nerve impulse actions on the pituitary gland. Alcohol has two noticeable effects on the hypothalamus and pituitary gland, which influence sexual behavior and urinary excretion. Alcohol depresses the nerve centers in the hypothalamus that control sexual arousal and performance. As BAC increases, sexual behavior increases, but sexual performance declines. Alcohol inhibits the pituitary secretion of anti-diuretic hormone (ADH), which acts on the kidney to reabsorb water. Alcohol acts on the hypothalamus/pituitary to reduce the circulating levels of ADH. When ADH levels drop, the kidneys do not reabsorb as much water; consequently, the kidneys produce more urine.
Medulla:
The medulla, or brain stem, controls or influences all of the bodily functions that you do not have to think about, like breathing, heart rate, temperature and consciousness. As alcohol starts to influence upper centers in the medulla, such as the reticular formation, a person will start to feel sleepy and may eventually become unconscious as BAC increases. If the BAC gets high enough to influence the breathing, heart rate and temperature centers, a person will breathe slowly or stop breathing altogether, and both blood pressure and body temperature will fall. These conditions can be fatal.
_
The effect of alcohol on the nervous system is even more pronounced among alcohol-dependent individuals. Chronic high doses cause peripheral neuropathy in 10% of alcoholics: similar to diabetes, patients experience bilateral limb numbness, tingling, and paresthesias, all of which are more pronounced distally. Approximately 1% of alcoholics develop cerebellar degeneration or atrophy. This is a syndrome of progressive unsteady stance and gait often accompanied by mild nystagmus; neuroimaging studies reveal atrophy of the cerebellar vermis. Fortunately, very few alcoholics (perhaps as few as 1 in 500 for the full syndrome) develop Wernicke’s (ophthalmoparesis, ataxia, and encephalopathy) and Korsakoff’s (retrograde and anterograde amnesia) syndromes, although a higher proportion have one or more neuropathologic findings related to these syndromes. These occur as the result of low levels of thiamine, especially in predisposed individuals, e.g., those with transketolase deficiency. Alcoholics can manifest cognitive problems and temporary memory impairment lasting for weeks to months after drinking very heavily for days or weeks. Brain atrophy, evident as ventricular enlargement and widened cortical sulci on MRI and CT scans, occurs in 50% of chronic alcoholics; these changes are usually reversible if abstinence is maintained. There is no single alcoholic dementia syndrome; rather, this label is used to describe patients who have apparently irreversible cognitive changes (possibly from diverse causes) in the context of chronic alcoholism. Excessive alcohol intake is associated with impaired prospective memory. This impaired cognitive ability leads to increased failure to carry out an intended task at a later date, for example, forgetting to lock the door or to post a letter on time. The higher the volume of alcohol consumed and the longer consumed, the more severe the impairments. One of the organs most sensitive to the toxic effects of chronic alcohol consumption is the brain. In France approximately 20% of admissions to mental health facilities are related to alcohol-related cognitive impairment, most notably alcohol-related dementia. Chronic excessive alcohol intake is also associated with serious cognitive decline and a range of neuropsychiatric complications. The elderly are the most sensitive to the toxic effects of alcohol on the brain. There is some inconclusive evidence that small amounts of alcohol taken in earlier adult life are protective in later life against cognitive decline and dementia. Acetaldehyde is produced from ethanol metabolism by the liver. The acetaldehyde is further metabolized by the enzyme acetaldehyde dehydrogenase. A deficiency of this enzyme is not uncommon in individuals from Northeastern Asia as pointed out in a study from Japan. This study has suggested these individuals may be more susceptible to late-onset Alzheimer’s disease as individuals with this defect generally do not drink alcohol.
_
Cerebral atrophy seen in alcoholics from imaging studies:
_
_
_
Structural damage to the brain resulting from chronic alcohol abuse can be observed in different ways:
Results of autopsy show that patients with a history of chronic alcohol abuse have smaller, less massive, and more shrunken brains than nonalcoholic adults of the same age and gender.
•The findings of brain imaging techniques, such as CT scans consistently show an association between heavy drinking and physical brain damage, even in the absence of chronic liver disease or dementia.
•Brain shrinking is especially extensive in the cortex of the frontal lobe – the location of higher cognitive faculties.
•The vulnerability to this frontal lobe shrinkage increases with age. After 40 some of the changes may be irreversible.
•Repeated imaging of a group of alcoholics who continued drinking over a 5-year period showed progressive brain shrinkage that significantly exceeded normal age-related shrinkage. Moreover, the rate of shrinkage correlated with the amount of alcohol consumed.
The relationship between alcohol consumption and deterioration in brain structure and function is not simple. Measures such as average quantity consumed, or even total quantity consumed over a year, do not predict the ultimate extent of brain damage. The best predictor of alcohol related impairment is: maximum quantity consumed at one time, along with the frequency of drinking that quantity. In addition to the toxic effects of frequent high levels of alcohol intake, alcohol related diseases and head injuries (due to falls, fights, motor vehicle accidents, etc.) also contribute. Although changes in brain structure may be gradual, performance deficits appear abruptly. The individual often appears more capable than is actually the case, because existing verbal abilities are among the few faculties that are relatively unimpaired by chronic alcohol abuse.
_
The Pattern of Recovery:
Despite the grim realities described above, the situation is not hopeless: With abstinence there is functional and structural recovery! Predictably cognitive functions and motor coordination improve, at least partially, within 3 or 4 weeks of abstinence; cerebral atrophy reverses after the first few months of sobriety.
•Indications of structural pathology often disappear completely with long-term abstinence.
•Hyper-excitability of the central nervous system persists during the first several months of sobriety and then normalizes.
•Frontal lobe blood flow continues to increase with abstinence, returning to approximately normal levels within 4 years.
•In general, skills that requires novel, complex, and rapid information processing take longest to recover. New verbal learning is among the first to recover. Visual-spatial abilities, abstraction, problem solving, and short-term memory, are the slowest to recover. There may be persistent impairment in these domains, particularly among older alcoholics [over 40]. However, even this population may show considerable recovery with prolonged abstinence.
_
The whole-brain and whole-systems approaches afforded by in vivo magnetic resonance imaging to quantify brain structure and function have yielded two principles of alcohol’s effect on the brain: 1) Alcoholism affects selective brain systems, leaving others relatively intact; and 2) alcoholism modifies brain structure without necessarily killing neurons, thereby providing a basis for the “incomplete lesion” as the underlying neuropathology of alcoholism and potential for recovery. A unifying biological substrate of the alcoholism syndrome is identification of selective neural circuits commonly compromised in alcoholism. Target networks relevant to alcoholism’s loci of neuropathology and neuropsychological compromise involve frontocerebellar circuitry, frontolimbic circuitry, and frontostriatal circuitry.
_
Effects of Alcohol on the Nervous System:
As mentioned above, alcohol is a central nervous system depressant. It acts at many sites, including the reticular formation, spinal cord, cerebellum and cerebral cortex, and on many neurotransmitter systems. Alcohol is a very small molecule and is soluble water solutions. Because of these properties, alcohol gets into the bloodstream very easily and also crosses the blood brain barrier. Some of the neurochemical effects of alcohol are:
•Increased turnover of norepinephrine and dopamine
•Decreased transmission in acetylcholine systems
•Increased transmission in GABA systems
•Increased production of beta-endorphin in the hypothalamus
_
While alcohol has a wide range of pharmacological effects on the body, the brain is a primary target. However, the molecular mechanisms by which alcohol alters neuronal activity in the brain are poorly understood. Participants in a symposium at the June 2010 annual meeting of the Research Society on Alcoholism in San Antonio, Texas addressed recent findings concerning the interactions of alcohol with prototype brain proteins thought to underlie alcohol actions in the brain. “Alcohol is the most common drug in the world, has been used by diverse human communities longer than recorded history, yet our understanding of its effects on the brain is limited when compared to other drugs,” said Rebecca J. Howard, a postdoctoral fellow at The University of Texas at Austin Waggoner Center for Alcohol & Addiction Research and corresponding author for this study. Howard explained that neuroscientists have discovered how marijuana, cocaine, and heroin each bind to a special type of protein on the surface of brain cells, fitting like a key into a lock to change that protein’s normal function. Yet alcohol has special properties that make it difficult to characterize its lock-and-key binding in detail, for example, alcohol is much smaller than other drugs, and appears to interact with several different types of proteins. “The adverse effects of alcohol abuse are devastating on a personal level and on a societal level,” added Gregg Homanics, a professor of anesthesiology and pharmacology & chemical biology at the University of Pittsburgh. “Alcohol abuse costs our society more than the costs of all illegal drug abuse combined. For many years, most investigators thought that alcohol exerted nonspecific effects on the brain and simply perturbed neuronal function by dissolving in the membranes of nerve cells. However, our understanding of alcohol action has dramatically shifted in the last 10 to 15 years or so. There is now solid experimental evidence that alcohol binds in a very specific manner to key protein targets in the brain to cause the drug’s well known behavioral effects. Combining X-ray crystallography, structural modeling, and site-directed mutagenesis may be better suited to studying alcohol’s low-affinity interactions than traditional techniques such as radioligand binding or spectroscopy. Alcohol has a ‘low affinity’ for proteins, compared to how other drugs interact with their own protein targets. This is one reason it takes such a large quantity of alcohol to affect the brain: whereas users of cocaine or heroin may consume just a few milligrams at a time, a person drinking a shot of strong liquor consumes about 1,000 times that much alcohol (several grams). The low affinity of alcohol for its protein targets [also] makes it difficult to study by traditional methods that rely on detecting stable drug-protein complexes over a long period of time. Some common themes are beginning to emerge from a review of diverse proteins such as inwardly rectifying potassium, transient receptor potential, and neurotransmitter-gated ion channels, as well as protein kinase C epsilon. There is now overwhelming evidence that specific alcohol binding sites exist on a variety of brain protein targets. Alcohol exerts its effects via binding sites on target molecules just like all other drugs we know about. There is now solid evidence from several different putative alcohol targets using several different techniques that alcohol interacts with specific brain targets in a highly selective manner. This is particularly important for more senior clinicians and researchers that were trained years ago when the predominant theory of alcohol action was via nonspecific effects on the nervous system. Great progress is being made in understanding how alcohol exerts its effects on the brain at the molecular level. Understanding how alcohol affects brain proteins on a molecular level is essential if we are to effectively develop rational treatments to combat alcohol use disorders.
_
Acute and chronic alcohol consumption can have both subtle as well as dramatic effects on the brain and its functioning. The effects of alcohol on the brain can occur by both direct and indirect means. Thus, it is not really necessary that the alcohol actually reach the brain, though it does, for brain function to be modified. For example, damage to the brain can occur through alcohol-induced deficiencies in nutrition, liver disease, and through alterations the function of other bodily systems (e.g. immune, hormonal), which produce substances which end up in the blood and get transported to the brain. In the most extreme case, another person who has been drinking could become violent and injure you, e.g. automobile crashes.
_
Alcoholism affects brain through various mechanisms:
_
Alcohol abuse is associated with widespread and significant brain lesions. Alcohol related brain damage is not only due to the direct toxic effects of alcohol; alcohol withdrawal, nutritional deficiency, electrolyte disturbances, and liver damage are also believed to contribute to alcohol-related brain damage. The long-term effects of alcohol on brain chemistry is an important cause of chronic fatigue.
_
Short-term cognition deficits during early alcohol withdrawal are associated with elevated plasma homocysteine levels in patients with alcoholism:
Higher plasma homocysteine levels have been found in actively drinking alcoholics as well as in early abstinent patients. Furthermore, elevated homocysteine levels are associated with cognitive decline in dementia and in healthy elderly people. The aim of this prospective study was to investigate a possible association between homocysteine serum levels and clinically well known cognitive deficits during alcohol withdrawal. Authors examined 89 patients (67 men, 22 women) during early withdrawal treatment. Cognitive function was assessed using the c.I.-Test. Patients with cognitive deficits showed significantly higher homocysteine serum levels (Mann-Whitney-U, p = 0.004) than patients without cognitive deficits, while the difference in blood alcohol concentration was not significant. Using logistic regression analysis, cognitive deficits were best predicted by high homocysteine serum levels (Wald χ2 = 4.071, OR = 1.043, 95% CI 1.001–1.086, p<0.05), which was confirmed by Receiver Operating Curves (AUC = 0.68, 95% CI = 0.57–0.79, p = 0.004). The present results show first evidence of an association between elevated plasma homocysteine levels in alcoholics and cognition deficits in patients undergoing alcohol withdrawal.
___________
The Neuropharmacology of Ethyl Alcohol:
Alcohol has the ability to enhance the effects of the neurotransmitter GABA, which is an inhibitory neurotransmitter. Enhancing an inhibitor would have the effect of making things sluggish, which matches the behavior you see in a drunk person. Glutamine is an excitatory neurotransmitter that alcohol weakens. By making this excitatory neurotransmitter less effective, you also get sluggishness. Alcohol does this by interacting with the receptors on the receiving cells in these pathways. Alcohol affects various centers in the brain, both higher and lower order. The centers are not equally affected by the same BAC — the higher-order centers are more sensitive than the lower-order centers. As the BAC increases, more and more centers of the brain are affected.
_
Alcohol’s direct action on the brain is as a depressant. It generally decreases the activity of the nervous system. One could ask how it could be a depressant if after one or two drinks a person tends to talk more and become more active. The answer is that alcohol can cause disinhibition, i.e. inhibits cells and circuits in the brain which themselves are normally inhibitory. Nerve cells communicate with one another via electrical and chemical signals. In essence signals coming from outside the body like light, sound, smells, tastes, and pressure are converted (transduced) into chemical and electrical signals which pass from one part of the body to another and from one part of the brain to another. Once inside the brain electrical signals and chemical signals continue to be generated to allow communication between the brain parts and regions. Electrical signals generated in one neuron causes of the release of chemicals called neurotransmitters (NTs) from that neuron. These NTs in turn are then available to act at other neurons in close proximity to the first to either excite or inhibit that neuron’s activity. There are a substantial number of NTs in the brain. Four of the most important NTs with respect to alcohol are glutamate, gamma aminobutyric acid (GABA), dopamine (DA), and serotonin. Glutamate is the major excitatory NT in the brain. Ethyl alcohol acts to inhibit a subset (N- methy-D-aspartate, NMDA) of glutamate receptors, thus diminishing the excitatory actions of glutamate. GABA is the major inhibitory NT in the brain. Alcohol acts primarily at the GABAa receptor to facilitate its action, thus in essence creating enhanced inhibition. Changes in the number of both NMDA and GABA receptors and ability of these receptors to bind their NTs appear to be involved in the development of tolerance to and dependence on alcohol. The third important NT in alcohol action, Dopamine, is involved in reward processes and thus seems to be responsible for the rewarding aspects of alcohol consumption. Other things that people find rewarding such as food, sex, and other drugs of abuse also act to release DA in the brain. Serotonin also appears to play a role in reward processes and therefore seems to be important in alcohol use and abuse. In addition, serotonin is a prominent player in mood states, compulsive disorders, aggression, and effects of other drugs of abuse like methamphetamine and LSD.
_
Alcohol acutely decreases neuronal activity and has similar behavioral effects and cross-tolerance with other depressants, including benzodiazepines and barbiturates. In the brain, alcohol affects almost all neurotransmitter systems, with acute actions that are often the opposite of those seen following desistance after a period of heavy drinking. The most prominent actions relate to boosting gamma aminobutyric acid (GABA) activity, especially in GABAA receptors. Enhancement of this complex chloride channel system contributes to anticonvulsant, sleep-inducing, antianxiety, and muscle relaxation effects of all GABA-boosting drugs. Acutely administered alcohol produces a release of GABA, and continued use of this drug increases density of GABAA receptors, while alcohol withdrawal states are characterized by decreases in GABA-related activity. Equally important is the ability of acute alcohol to inhibit postsynaptic N-methyl-d-aspartate (NMDA) excitatory glutamate receptors, while chronic drinking and desistance are associated with an upregulation of these excitatory receptor subunits. The relationships between greater GABA and diminished NMDA receptor activity during acute intoxication and diminished GABA with enhanced NMDA actions during alcohol withdrawal explain much of intoxication and withdrawal phenomena.
_
A recent theory supported by several researchers, pins alcohol’s effect on voltage and ligand-gated ion channels that control neuronal activity. Two distinct ligand-gated channels have been identified, inhibitory ones (GABA receptors and strychnine-sensitive glycine receptors) and excitatory ones (N-methyl-D-aspartate (NMDA) and non-NMDA glutamate-activated channels and the 5HT3 subtype of serotonin receptors). The inhibitory aspect occurs due to a hyperpolarization of neurons, secondary to an influx of chloride ions. The neuron becomes less likely to achieve the threshold membrane potential. The excitatory receptor is dependent on the NMDA and non-NMDA glutamate receptors that control the influx of sodium and calcium, which bind to endogenous neurotransmitters (glutamate or aspartate) and depolarize the neuronal membrane. The NMDA receptor seems to have a high permeability to calcium, which acts as a catalyst to several intracellular events. Chronic exposure to alcohol seems to alter the NMDA receptors and this may play a role in the clinical symptoms of alcohol withdrawal. In vitro studies have demonstrated an increase in the binding sites for MK801 (dizocilpine) in neurons chronically exposed to alcohol. This rise may account for the acclimation process, in which greater concentrations of alcohol are needed to cause experimental and clinical symptoms of intoxication. NMDA can cause seizure activity. Mice that have been exposed to chronically elevated levels of alcohol reveal increased numbers of NMDA receptors and NMDA related seizure activity. The NMDA antagonist MK801 has been shown to decrease the severity of seizures in these mice during withdrawal. Through a complex process of cell membrane ion pumps and neurotransmitter stimulation, the multi-faceted effects of alcohol and alcohol withdrawal are becoming better understood.
_
Alcohol’s effects on GABA-A receptors seem tantalizing, but generally unlikely, due to either a far too high or too low potency, depending on the subunit makeup. Ethanol’s inhibition of NMDA receptors seems likely to be a contributor to its effects. The inhibition of AMPA and kainate receptors is too weak to mediate recreational effects, but it may be responsible for ethanol-induced coma. Ethanol’s potentiation of alpha7 nicotinic acetylcholine receptors seems a likely cause of some of its rewarding effects, but not a mediator of its general “depressant” character. Ethanol’s effects at voltage-gated sodium channels are far too weak to have any effect during recreational usage. BK channel activation might cause some of the effects of ethanol at high concentrations and GIRK channel potentiation could be responsible for its analgesic effects. Potentiation of glycine receptors might cause spinal inhibition and lead to some effects of ethanol, but not the classical cognitive effects. 5-HT3 receptor effects are too weak to mediate ethanol’s effects. Inhibition of voltage-gated calcium channels is another likely mediator of ethanol’s effects, as it would cause general inhibition of synaptic activity.
_
Alcohol, according to conventional wisdom, is a depressant. Yet, that doesn’t fully explain alcohol’s effects. People often drink to liven up a party, not mellow it out. A few drinks can spark energy, elation and excitement; it gives you a buzz. Alcohol may be more than simply a depressant. Classification of drugs can be explained by their chemical targets within the brain. Stimulants may influence dopamine or norepinephrine. Depressants target a chemical called GABA, the primary inhibitory neurotransmitter within the brain. As early research failed to show that alcohol targeted a specific receptor, scientists speculated that alcohol non-specifically altered cell membranes. A gatekeeper, the cell membrane’s job is to regulate what goes in and out of a cell. Alcohol might disrupt cell membranes throughout our body, making them leaky. At this point, our understanding of alcohol’s effects was a bit cloudy, as if rather than looking through a microscope, we were wearing beer goggles. More things could get into our cells, but we didn’t know what those things were or why it was happening. Our scientific explanation was as precise as our lay explanation. When we drink, our cells get messed up. Is this the best we could do? At the same time, behavioral researchers sought to understand the physiological and psychological effects of drinking. Drinking profoundly alters mood, arousal, behavior, and neuropsychological functioning. However, studies have found that the specific effects depend not just on how much someone drinks, but also on whether blood alcohol content (BAC) is rising or falling; while in the process of drinking, alcohol acts as a stimulant, but as drinking tapers off it begins to act more as a sedative. As BAC ascends, drinkers report increases in elation, excitement and extroversion, with simultaneous decreases in fatigue, restlessness, depression and tension. Conversely, a descending BAC corresponds to a decrease in vigor and an increase in fatigue, relaxation, confusion, and depression. A subsequent group of researchers found that drinking increases levels of norepinephrine, the neurotransmitter responsible for arousal, which would account for heightened excitement when someone begins drinking. Norepinephrine is the chemical target of many stimulants, suggesting that alcohol is more than merely a depressant. Elevated levels of norepinephrine increase impulsivity, which helps explain why we lose our inhibitions drinking. Drunken brains are primed to seek pleasure without considering the consequences; no wonder so many hook-ups happen after happy hour. Although increased norepinephrine offers some explanation of alcohol’s effects, it doesn’t tell us where in the brain changes are occurring. To see which regions of the brain were more or less active while drinking, researchers gave a group of subjects a PET scan after injecting them with harmless radioactive glucose, the brain’s preferred source of energy. Highly active regions consume more glucose, and those regions are brightly lit during the PET scan, whereas less active regions are dimmer. The regions of the brain with the greatest decrease in activity were the prefrontal cortex and the temporal cortex. Decreased activity in the prefrontal cortex, the region responsible for decision making and rational thought, further explains why alcohol causes us to act without thinking. The prefrontal cortex also plays a role in preventing aggressive behavior, so this might help explain the relationship between alcohol and violence. The temporal cortex houses the hippocampus, the brain region responsible for forming new memories. Reduced activity in the hippocampus might account for why people black out when drinking. Alcohol also decreases energy consumption in the cerebellum, a brain structure that coordinates motor activity. With a cerebellum running at half-speed, it would be hard to walk a straight line or operate heavy machinery. Despite gaining insight into which brain regions were less active, we still had no mechanism that could explain why alcohol was reducing these brain functions. Alcohol has been found to affect over 100 unique receptors in the brain. However, many systems in the brain are interrelated. It’s not clear if alcohol directly acts on all those receptors or if they’re a downstream result of its action elsewhere. The smoking gun would be to isolate a receptor and show that alcohol affects it. If alcohol is a depressant, it should facilitate GABA receptors. When GABA receptors were first isolated, they did respond to alcohol, but not until alcohol concentrations reached 330 mg/dL. The legal limit for driving is 80 mg/dL in the U.S. For the normal human, concentrations over 300mg/dL are enough to cause someone to pass out and vomit. How would that account for the buzz we feel after a few glasses of wine? Nonetheless, alcohol shared properties with classical depressants, like diazepam. Experiments in mice showed that when given diazepam regularly, not only did they develop a tolerance to it, but they also developed increased tolerance to alcohol. Called cross-tolerance, it indicates that both drugs act at the same receptor, the GABA receptor. Mounting evidence suggested that alcohol acted at GABA receptors, but research had still been unable to pin down a specific mechanism. Part of the problem stemmed from the fact that GABA receptors are varied. Each receptor is composed of five subunits, and there are multiple subunits to choose from. Is it possible that we just hadn’t tested the right one? Yes, it turned out. One of the less common types of GABA contains a delta subunit. In the past ten years, researchers began suspecting that the delta receptor might differ from other GABA receptors. When isolated, they found that it responded to low levels of alcohol, like the amount in a glass of wine. So researchers found the smoking gun. The delta receptor is concentrated in the prefrontal cortex, the hippocampus and the cerebellum, the same regions which had lowered activity in the PET scanner. Although GABA activity doesn’t entirely explain alcohol’s effects and we don’t know exactly what the delta receptor does, a big part of the mystery seems to have come unraveled. Because GABA is the primary inhibitory neuron in the brain, it can affect virtually every system. Alcohol is more than simply a depressant. The physical structure of the brain remains constant, but the addition of a tiny chemical drastically alters brain function and ultimately behavior. Understanding how alcohol affects our brain also offers insight into how our brains work in general.
_
Low-dose alcohol actions on α4β3δ GABA-A receptors are reversed by the behavioral alcohol antagonist Ro15-4513: A study:
Although it is now more than two decades since it was first reported that the imidazobenzodiazepine Ro15-4513 reverses behavioral alcohol effects, the molecular target(s) of Ro15-4513 and the mechanism of alcohol antagonism remain elusive. Here, authors show that Ro15-4513 blocks the alcohol enhancement on recombinant “extrasynaptic” α4/6β3δ GABAA receptors at doses that do not reduce the GABA-induced Cl− current. At low ethanol concentrations (≤30 mM), the Ro15-4513 antagonism is complete. However, at higher ethanol concentrations (≥100 mM), there is a Ro15-4513-insensitive ethanol enhancement that is abolished in receptors containing a point mutation in the second transmembrane region of the β3 subunit (β3N265M). Therefore, α4/6β3δ GABA receptors have two distinct alcohol modulation sites: (i) a low-dose ethanol site present in α4/6β3δ receptors that is antagonized by the behavioral alcohol antagonist Ro15-4513 and (ii) a site activated at high (anesthetic) alcohol doses, defined by mutations in membrane-spanning regions. Receptors composed of α4β3N265Mδ subunits that lack the high-dose alcohol site show a saturable ethanol dose-response curve with a half-maximal enhancement at 16 mM, close to the legal blood alcohol driving limit in most U.S. states (17.4 mM). Like in behavioral experiments, the alcohol antagonist effect of Ro15-4513 on recombinant α4β3δ receptors is blocked by flumazenil and β-carboline-ethyl ester (β-CCE). Author’s findings suggest that ethanol/Ro15-4513-sensitive GABAA receptors are important mediators of behavioral alcohol effects.
_
Chronic Intermittent Ethanol Treatment Selectively Alters N-Methyl-d-aspartate Receptor Subunit Surface Expression in Cultured Cortical Neurons: A study:
A chronic intermittent ethanol (CIE) exposure regimen consists of repeated episodes of ethanol intoxication and withdrawal. CIE treatment has been reported to result in a significant enhancement of N-methyl-d-aspartate (NMDA) receptor-mediated synaptic responses in vivo, and trafficking of NMDA receptors is emerging a key regulatory mechanism that underlies the channel function. Therefore, in the present study, authors examined the effects of CIE on NMDA receptor subunit surface expression. Cultured cortical neurons were exposed to 75 mM ethanol for 14 h followed by 10 h of withdrawal, repeated this cycle five times, and followed by 2 or 5 days of withdrawal. Surface-expressed NMDA receptor subunits and their endocytosis were measured by biotinylation and Western blots. CIE significantly increased NMDA receptor (NR) 1 and NR2B but not NR2A subunit surface expression after 5 days of treatment. However, CIE treatment did not reduce the NMDA receptor endocytosis. Quantification of immunocytochemistry confirmed CIE-induced increase in both the total number of NR1 and NR2B subunit clusters and their targeting to synaptic sites. It is noteworthy that this effect persisted even after ethanol withdrawal with a peak expression occurring between 0 and 2 days after withdrawal, and the expression on the plasma membrane was still at high levels after 5 days of withdrawal. In addition, this was accompanied by significant increases in postsynaptic density protein 95 clusters. Protein kinase A inhibitor completely reversed CIE-induced increase in NR1 and partially in NR2B surface level and a long-lasting effect. These changes may contribute to the development of ethanol-induced neurotoxicity and ethanol dependence.
_________
Alcohol myopia theory:
Why does alcohol cause disinhibited behaviour in some cases but not in others? An explanation is offered by alcohol myopia, which states that alcohol limits cognitive capacity such that intoxicated individuals tend to focus on cues in the environment that are most salient (Steele and Josephs, 1990). Alcohol myopia postulates that intoxicated individuals are unable to attend to all relevant cues simultaneously because of the limitation of cognitive capacity associated with alcohol intoxication. In other words, alcohol produces a myopic effect causing individuals to attend primarily to, and hence be more influenced by, salient environmental cues at the expense of less salient cues. Individuals who are not intoxicated, however, are not as easily influenced by salient cues because they are better able to attend to all the relevant information in the environment. Evidence to support alcohol myopia has been found in the domain of health-relevant behaviours, such as drinking and driving or engaging in unprotected sex. MacDonald et al. (1995) found that when asked about their attitudes towards drinking and driving, both sober and intoxicated individuals reported very negative attitudes. However, when the wording of the question included an impelling cue to drink and drive (e.g. having to drive only a short distance), intoxicated individuals reported less negative attitudes than sober individuals. This pattern is consistent with alcohol myopia because intoxicated participants were influenced by the impelling cue, but sober participants were not. Intentions towards engaging in unprotected sex have also been shown to be influenced by salient inhibiting cues such that intoxicated individuals actually reported more prudent intentions compared with sober controls (MacDonald et al., 2000). It is important to note that disinhibition theory cannot account for these findings; it cannot explain situations in which intoxicated individuals behave more prudently than sober individuals. If alcohol is a general disinhibitor, intoxicated individuals should always exhibit disinhibited behaviour.
___________
Neurobiology of alcohol tolerance and dependence (addiction):
Alcohol dependence is a complex psychological and neurobiological disorder. It is important to recognize that as an individual moves from initial alcohol use to the other end of the spectrum (dependence), parallel dynamic changes are occurring throughout the nervous system (i.e., these systems are constantly moving targets). These perturbations and disruptions result in neuroadaptations that contribute to overall dysregulations in normal daily behaviors (e.g., work, social interactions) as well as the development of alcohol dependence. Several key receptors mediate the response to acute and chronic alcohol intake.
_
Some individuals are more vulnerable than others to becoming addicted. This enhanced vulnerability can be ascribed to genetic (biochemically regulated vulnerability) as well as environmental factors (situational impact). It is also clear that people without an apparent enhanced vulnerability can be addicted to ethanol.
What is the current thinking about biochemical basis of addition? Two general processes contribute to alcohol addiction.
1. A modified reward process whereby drinking of alcohol provides an overall positive effect (euphoria or decrease in an unpleasant situation). This is coupled in those vulnerable individuals with a pattern of diminishing or ignoring the negative impacts of overconsumption – the hangovers, loss of memory, fights, violence and arrests. The less vulnerable individual equates heavy alcohol consumption as overall unpleasant as result of the negative effects outweighing the positive.
2. Neuroadaptation whereby the brain attempts to compensate for something (ethanol) which influences normal functioning.
_
Reward system involvement:
It should be recognized that in addition to the regions or parts of the brain and the billions of neurons in the brain, there are also various systems. Systems often involve numerous parts just like the fuel system in a car involves the fuel tank, the fuel pump, the tubing, the fuel injectors, etc. One important system mentioned above is the reward system, which plays an important role in the rewarding (reinforcing) properties ethyl alcohol and other drugs such as cocaine. A major part of the reward system starts deep within the brain in an area called the ventral tegmental area and projects to the nucleus accumbens and then on to upper parts of the brain such as the cerebral cortex. Types of rewarding (positive) experiences gained after drinking include the taste of the alcohol itself and the feelings (e.g. relaxation) gained after drinking ethanol. One can also gain a positive experience by avoiding negative situations such as those felt in anxiety provoking situations (public speaking, attending a party) or avoiding the effects of withdrawal from ethanol. The rewarding aspects of ethanol use involve the brain’s reward system. This system is comprised of brain structures and circuitry (e.g. ventral tegmental area, extended amygdala and the nucleus accumbens within) that appears to be important in the reinforcing (rewarding) properties of a variety of drugs.
_
Circuitry for positive reinforcement and the mesolimbic dopamine system:
Investigations into the neurobiological substrates of reward and motivated behaviours (reward system) established that the positive reinforcing properties of most, if not all addictive drugs, originate within a brain circuit comprised of dopamine (DA)-containing neurons originating in the midbrain ventral tegmental area and their release of DA into the ventral striatum, particularly within the nucleus accumbens. An extensive review of such interactions, which formed the basis for the DA theory of addiction, and their pertinence for the treatment of alcohol addiction has been provided by Soderpalm and Ericson. Importantly, the role of DA for the actions of alcohol is less clear as for other drugs of abuse. Extensive lesions of the DA system in experimental animals failed to decrease, or even increased an established pattern of ethanol consumption. Such conflicting observations may result from DA-independent reinforcement implying multiple ways for activation of critical reinforcement circuitry that could be modulated by alcohol’s wide range of neurochemical effects. Nevertheless, human neuroimaging studies demonstrated DA release into the ventral striatum as well as activation of this structure after intravenous or oral administration of alcohol in healthy social drinkers. Interactions of the DA and opioid systems play an important role in mediating reward; their implications for alcohol and addiction have been reviewed in Spanagel and Heilig et al. Interestingly, genetic variation at the human mu-opioid receptor gene, i.e. an A-to-G substitution within the genetic code, determines the striatal DA release. Carriers of the G allele of this single nucleotide polymorphism are consistently associated with increased experience of euphorigenic effects of alcohol. A combined study in humans and transgenic animals established that the G allele confers much stronger striatal alcohol-evoked DA release compared to the A allele, although the underlying mechanism remains unknown. Importantly, while G allele carriers show no established elevation of risk for alcoholism, if addicted they seem to respond better to treatment with the mu-opioid receptor antagonist naltrexone. Understanding this and other genetic heterogeneity in the context of medication response in patient populations will slowly pave the road for an individualized pharmacogenomically driven therapeutic approach to alcoholism.
_
Hippocampus and Ventral Tegmental Area:
Researchers have hypothesized that alcohol’s effects on GABAergic neurotransmission involve alteration in the expression of GABA receptor subunits in specific regions of the brain that occur with chronic treatment or alcohol. A recent study suggests that these effects are found not only in the (cerebral) cortex but also in the hippocampus, a brain structure involved in the consolidation of new memories, and the ventral tegmental area (VTA) (Charlton et al. 1997). The VTA is the source of dopamine in the mesolimbic system, a region of the brain involved in the mediation of alcohol reinforcement. The cell bodies of this mesolimbic dopamine system originate in the VTA and send projections to the nucleus accumbens and basal forebrain, transmitting information to the dopamine receptors in these brain areas. Exposing laboratory animals to alcohol for 12 consecutive weeks decreased GABAA α 1 subunit activity in the VTA and hippocampus, suggesting potential changes in brain structures implicated in the rewarding and cognitive effects of alcohol, respectively. Researchers failed to detect a similar change in these regions after only 4 weeks of exposure to alcohol—a clue to the involvement of these areas specifically with chronic alcohol exposure.
_
Current research supports the idea that initial exposure to alcohol activates the reward pathway releasing DA in the Nucleus accumbens, which in turn sends messages to the cortex to be coded as experiences and perhaps as memories. Once coded, these experiences can influence, i.e. promote, subsequent behavior such further alcohol intake. Since these “memories” of drinking are linked to the environment in which the drinking took place, it is not surprising that the environmental cues can be important in guiding subsequent drinking behavior. As with all pleasurable activities, drinking alcohol acutely increases dopamine levels in the brain, especially in the ventral tegmentum and related brain regions, and this effect plays an important role in continued alcohol use, craving, and relapse. The changes in dopamine pathways are also linked to increases in “stress hormones,” including cortisol and adrenocorticotropic hormone (ACTH) during intoxication and decreases in these hormones during withdrawal. Such alterations are likely to contribute to both feelings of reward during intoxication and depression during falling blood alcohol concentrations. Also closely linked to alterations in dopamine (especially in the nucleus accumbens) are alcohol-induced changes in opioid receptors, with acute alcohol also causing release of beta endorphins. Additional important neurochemical changes include increases in synaptic levels of serotonin during acute intoxication, and subsequent upregulation of serotonin receptors. Acute increases in nicotinic acetylcholine systems also contribute to the impact of alcohol in the ventral tegmental region, which occur in concert with enhanced dopamine activity. In the same regions, alcohol impacts on cannabinol receptors, with resulting release of dopamine, GABA, and glutamate as well as subsequent effects on brain reward circuits.
_
Starting with dopamine; acute alcohol administration in intoxicating doses (20–40 mM) activates neurons in the ventral tegmental area both in vivo in anesthetized rats and in vitro using extracellular recording in brain slice preparations. Following dependence and during withdrawal from alcohol, there is a decrease in dopaminergic activity in the ventral tegmental area that has been linked to the dysphoria of acute and protracted withdrawal. The decrease in dopaminergic activity in the ventral tegmental area is consistent with microdialysis studies showing decreases in dopamine release in the nucleus accumbens during alcohol withdrawal. Reduced dopaminergic neurotransmission is prolonged, outlasting the physical signs of withdrawal.
_
Despite the generally held view that alcohol is an unspecific pharmacological agent, recent molecular pharmacology studies demonstrated that alcohol has only a few known primary targets. These are the NMDA, GABAA, glycine, 5-hydroxytryptamine 3 (serotonin) and nicotinic ACh receptors as well as L-type Ca2+ channels and G-protein-activated inwardly rectifying K+ channels. Following this first hit of alcohol on specific targets in the brain, a second wave of indirect effects on a variety of neurotransmitter/neuropeptide systems is initiated that leads subsequently to the typical acute behavioural effects of alcohol, ranging from disinhibition to sedation and even hypnosis, with increasing concentrations of alcohol. Finally, addictive behaviour towards alcohol as measured by alcohol-seeking and relapse behaviour is reviewed in the context of specific neurotransmitter/neuropeptide systems and their signaling pathways. The activity of the mesolimbic dopaminergic system plays a crucial role during the initiation phase of alcohol consumption. Following long-term, chronic alcohol consumption virtually all brain neurotransmission seems to be affected, making it difficult to define which of the systems contributes the most to the transition from controlled to compulsive alcohol use. However, compulsive alcohol drinking is characterized by a decrease in the function of the reward neurocircuitry and a recruitment of antireward/stress mechanisms comes into place, with a hypertrophic corticotropin-releasing factor system and a hyperfunctional glutamatergic system being the most important ones. Innate differences in the functioning of several brain systems, which define the reinforcing properties of alcohol, contribute to an individual response to this drug. In addition, very recent studies suggest that appetite-regulating peptides, such as leptin, ghrelin and orexin also play a relevant role in the regulation of the reinforcement system (Jerlhag et al., 2006a, 2007; Lawrence et al., 2006). It is suggested that in addition to the mesolimbic DA system, other brain systems, including the mesocortical and nigrostriatal pathways as well as their non-DAergic feedback loops and glutamatergic inputs might be involved in alcohol addiction. Furthermore, a persistent recruitment of antireward/stress mechanisms such as hypertrophic CRF1 receptor signaling might come into place as well.
_
Opioids:
Endogenous opioids are crucial for mediating alcohol-induced reward. The opioid receptor antagonist naltrexone reverses alcohol-induced DA release in the NAC in rats, and suppression of operant alcohol-reinforced behaviour by naltrexone is associated with attenuation of the alcohol-induced increase in dialysate DA levels in the NAC (Gonzales and Weiss, 1998). These findings not only show that alcohol reinforcement depends on the activity of endogenous opioid systems but also confirm that DA output in the NAC is associated with this reinforcement process (Herz, 1997). Furthermore, alcohol-preferring AA rats show lower opioidergic activity in areas involved in alcohol reinforcement (Nylander et al., 1994), and many other studies have also reported innate differences in opioid systems in other alcohol-preferring and -avoiding lines of animals, such as AA vs ANA, and P vs alcohol non-preferring rats, or C57BL/6 vs DBA/2 mice (Herz, 1997; Jamensky and Gianoulakis, 1997; McBride and Li, 1998). In line with the conclusion that endogenous opioid systems are crucial in mediating alcohol reward, naltrexone was shown to slow down the acquisition of alcohol drinking in mice (Phillips et al., 1997).
_
Opioid Antagonists for Pharmacological Treatment of Alcohol Dependence:
Alcohol dependence is a widespread psychiatric disorder. While relapse prevention therapy in alcoholism was exclusively dominated by social and psychological treatments for many years, in the last decades the benefits of pharmacological agents for the rehabilitation treatment in alcoholism have become increasingly evident. Naltrexone, an opiate receptor antagonist, blocks the pleasant and reinforcing effects of alcohol by preventing the stimulation of opioid receptors and the reduction of dopamine release in the ventral tegmental area (VTA). Clinical evidence about the effectiveness of the substance is not always consistent, but meta-analyses confirm naltrexones effect on the risk of heavy drinking. Evidence about the abstinence-maintaining effects of the substance comes from a relatively small database and needs further investigation. The evaluation of differential effects of naltrexone depending on biological or psychological profiles, which could further enhance the effectiveness of treatments for alcohol dependence, remains a challenge. Nalmefene, another opioid antagonist, as well as naltrexone depot, a sustained release formulation of naltrexone, are further promising strategies for the treatment of alcohol dependence.
_
Reinforcement and Reward in Chronic Drinking:
Because alcoholism centers on compulsive, often excessive, use of alcohol, the concept of reinforcement or motivation is a crucial part of this syndrome. A reinforcer is defined as any event that increases the probability of a response. This explanation also can be used to define reward; in fact, “reinforcement” and “reward” frequently are used interchangeably. However, reward often also connotes an additional emotional value, such as pleasure (White and Wolf 1991). Many sources of reinforcement, such as pleasure, mood elevation, and removal of negative emotional states, contribute to compulsive alcohol use during the course of alcoholism. The primary pharmacologic action of alcohol produces a direct effect through positive or negative reinforcement. Positive reinforcement refers to a pleasurable or otherwise positive event that increases the likelihood that additional alcohol will be sought. Alcohol itself can serve as a powerful positive reinforcing agent through its ability to induce pleasurable or mood-elevating feelings (so-called euphoric or euphorogenic effects). In contrast, negative reinforcement describes an adverse event or situation that also will lead the individual to obtain more alcohol. Examples of negative reinforcement include situations in which an individual or animal self-medicates in an attempt to overcome an existing aversive state (depression or anxiety) or to treat a drug-generated aversive state (alcohol-related withdrawal) (Wikler 1973). Both the positive and negative types of reinforcement encourage alcohol-seeking behavior and appear to contribute to chronic drinking, alcohol dependence, and a return or relapse to drinking among persons recovering from alcoholism. The secondary pharmacologic effects of alcohol also can have powerful motivating properties. Conditioned reinforcement—when an individual learns to associate the reinforcing effects of alcohol with a previously neutral event or stimulus—results in secondary positive reinforcing effects. In practical terms, a person entering a familiar bar or pub can experience positive feelings similar to those induced by consumption of alcohol. Secondary reinforcing effects can be negative or positive; someone can also learn to associate particular stimuli with unpleasant aspects of abstinence, such as withdrawal symptoms. However, alcohol may, under certain conditions, serve as a deterrent to the seeking or obtaining of more alcohol. Research shows that alcohol can be aversive at high doses and, in animals, can cause both place avoidance, in which animals avoid an environment where they have previously received alcohol, and taste avoidance, in which animals avoid a taste previously paired with alcohol ingestion (Cunningham et al. 1992). Alcohol-dependent individuals have what is known as elevated aversion thresholds; that is, they can consume higher levels of alcohol than non-dependent individuals before they stop drinking or avoid alcohol. This elevated aversion threshold may contribute to excessive drinking among dependent persons.
_____
Neuroadaptation:
The second process important in addiction has to do with the ability of the brain to adapt to influences, which affect its normal function. The ability is called neuroadaptation. For example, the drinking of one or two beers or one or two drinks (acute intake of ethanol) activates a variety of processes in the body and in particular impacts the functioning of the brain. In order to keep the brain functioning normally, the brain attempts to chemically counteract whatever ethanol is doing to disrupt its action. A simple illustration is the reaction of the body if someone starts pushing it. The natural reaction is to compensate by correcting the balance and attempting to counteract the pressure of the push until the push is gone and the body returns to normal. Interestingly, neuroadaptation also sometimes results in an increased response to the drug (sensitization). Whether there is a diminished response or an enhanced response depends upon a variety of factors including the amount of the compound taken in and the timing of the intake. The development of sensitization to drugs such as cocaine may be more likely with intermittent exposure than with continuous exposure.
Ethanol
1. facilitates the action of the major depressant neurotransmitter in the brain (GABA) and
2. inhibits the action of the major excitatory neurotransmitter in the brain (glutamate).
Ethanol acts at specific sites on a specific subset of GABA and glutamate receptors (protein molecules upon which the neurotransmitters act). By influencing the action of these receptors, ethanol “slows down” the functioning of the nervous system. Thus, ethanol is called a central nervous system (CNS) depressant. With neuroadaptation, the brain attempts to counteract this depressant effect by increasing the activity of the glutamate system and decreasing the activity of the GABA system. This in part can be accomplished by altering the number or function of the receptors. GABA and glutamate receptors are only two of a number of key players in the transmission of information from one cell to the next. Activation of receptors is the occasion for intracellular signaling, meaning that a series of events within the cell take place when a neurotransmitter binds to the receptor. Thus, neuroadaptation can also take place at other locations within the cascade of events that take place in the brain. Just as there is adaptation upon the presence of something new, there is neuroadaptation when the compound leaves the brain. Thus, through neuroadaptation the brain is able in many instances to up-regulate (increase) or down-regulate (decrease) its function to compensate for the presence or absence of ethanol. (It should be recognized that the body and the brain have an amazing ability to adapt and only in extreme situations or after damage, such as seen in alcoholism, do the regulatory processes fail).
_
If a person chooses to drink more regularly (chronic intake), the brain attempts to adapt to the increasing amounts of ethanol. Generally, neuroadaptation can take place up to a point. After chronic consumption and ongoing adaptation, it will now take more ethanol to produce the same effect as the first drink. When this is the case, tolerance has developed and substantial adaptation has taken place. If the person now chooses to quit drinking the body tries to return to its original state in doing so causes a number of withdrawal signs including tremors, seizures, nausea, and negative emotional states. Since further drinking will delay, diminish, or prevent withdrawal, the person often chooses to drink again. Even if the person stops drinking, the neuroadaptations that took place in the brain may persist for a period of time well beyond the time when ethanol is no longer present in the body. It has been speculated that these may be the source of the urges to drink again. For most people it is relatively easy to modulate ethanol intake. Depending upon the vulnerability of the individual, as drinking progresses regulation of drinking becomes more difficult. Simultaneously, the ability of the brain to adapt is diminished or lost. Systems become increasingly dysregulated, perhaps due to damage, so that in the brain communication and coordination diminishes or fails. This is particularly true after repeated withdrawals from ethanol, since the severity of withdrawal increases. Perhaps this is the reason for saying the drink appears to take on a life of its own.
“First the person takes a drink, then the drink takes a drink, then the drink takes the person”.
In general there appears to be a general loss of control. The individual has lost control over drinking and neuroadaptive mechanisms have been overwhelmed. Thus alcoholism can be characterized as a disease with takes over the body and brain.
____________
Tolerance, Abuse and Dependence:
Tolerance:
Tolerance is the diminution of the effectiveness of a drug after a period of prolonged or heavy use of that drug or a related drug (cross-tolerance). Studies have shown that chronic alcohol users can have twice the tolerance for alcohol as an average person. Repeated use of alcohol contributes to tolerance, a complex phenomenon involving at least three types of compensatory mechanisms.
(1) After 1–2 weeks of daily drinking, metabolic or pharmacokinetic tolerance can be seen, with up to 30% increase in the rate of hepatic ethanol metabolism. Because of the higher metabolic rate for alcohol lower peak blood alcohol concentrations are achieved by chronic alcohol users than the average drinker when the same amount of alcohol is ingested. This alteration disappears almost as rapidly as it develops.
(2) Cellular or pharmacodynamic tolerance develops through neurochemical changes that maintain relatively normal physiologic functioning despite the presence of alcohol. Subsequent decreases in blood levels contribute to symptoms of withdrawal.
(3) Individuals learn to adapt their behavior so that they can function better than expected under influence of the drug (learned or behavioral tolerance).
_
The figure below shows development of alcohol-related harm:
_
In talking about alcohol or drug use, distinctions must be made between:
1. use,
2. abuse, and
3. dependence.
Use = Taking of alcohol or drug
Abuse = Any harmful use of alcohol or drugs
Dependence = Addiction (alcoholism)
_
Alcohol abuse:
Alcohol abuse is defined as repetitive problems with alcohol in any one of four life areas—social, interpersonal, legal, and occupational—or repeated use in hazardous situations such as driving while intoxicated in an individual who is not alcohol dependent. Alcohol abuse is a pattern of drinking that result in harm to one’s health, interpersonal relationships, or ability to work. According to Gelder, Mayou & Geddes (2005) alcohol abuse is linked with suicide. They state the risk of suicide is high in older men who have a history of drinking, as well as those suffering from depression. Certain manifestations of alcohol abuse include failure to fulfill responsibilities at work, school, or home; drinking in dangerous situations, including the operation of a motor vehicle; legal concerns associated with alcohol use; and continued drinking despite problems that are caused or worsened by drinking. Alcohol abuse can lead to alcohol dependence. About 50% of those with alcohol abuse continue to have alcohol problems 2–5 years later, but only 10% of these patients—including adolescents—go on to develop alcohol dependence.
_
Alcohol abuse is defined as a pattern of drinking that result in one or more of the following situations within a 12-month period (DSM-IV):
•Failure to fulfill major work, school, or home responsibilities
•Drinking in situations that are physically dangerous, such as while driving a car or operating machinery
•Having recurring alcohol-related legal problems, such as being arrested for driving under the influence of alcohol or for physically hurting someone while drunk
•Continued drinking despite having ongoing relationship problems that are caused or worsened by the drinking.
_
Alcoholism:
To establish a more precise use of the term alcoholism, a 23-member multidisciplinary committee of the National Council on Alcoholism and Drug Dependence and the American Society of Addiction Medicine conducted a 2-year study of the definition of alcoholism in the light of current concepts. The goals of the committee were to create by consensus a revised definition that is (1) scientifically valid, (2) clinically useful, and (3) understandable by the general public. Therefore, the committee agreed to define alcoholism as a primary, chronic disease with genetic, psychosocial, and environmental factors influencing its development and manifestations. The disease is often progressive and fatal. It is characterized by impaired control over drinking, preoccupation with the drug alcohol, use of alcohol despite adverse consequences, and distortions in thinking, most notably denial. Each of these symptoms may be continuous or periodic.
_
Alcoholism is a broad term for problems with alcohol, and is generally used to mean compulsive and uncontrolled consumption of alcoholic beverages, usually to the detriment of the drinker’s health, personal relationships, and social standing. It is medically considered a disease, specifically an addictive illness. In psychiatry several other terms have been used, specifically “alcohol abuse”, “alcohol dependence,” and “alcohol use disorder” which have slightly different definitions. In 1979, an expert World Health Organization committee discouraged the use of “alcoholism” in medicine, preferring the category of “alcohol dependence syndrome”. In the 19th and early 20th centuries, alcohol dependence in general was called dipsomania, but that term now has a much more specific meaning. People suffering from alcoholism are often called “alcoholics”. Many other terms, some of them insulting or informal, have been used throughout history. The World Health Organization estimates that there are 140 million people with alcoholism worldwide. The American Medical Association considers alcoholism as a disease and supports a dual classification of alcoholism to include both physical and mental components. The biological mechanisms that cause alcoholism are not well understood. Social environment, stress, mental health, family history, age, ethnic group, and gender all influence the risk for the condition. Significant alcohol intake produces changes in the brain’s structure and chemistry, though some alterations occur with minimal use of alcohol over a short term period, such as tolerance and physical dependence. These changes maintain the person with alcoholism’s compulsive inability to stop drinking and result in alcohol withdrawal syndrome if the person stops. Alcohol misuse has the potential to damage almost every organ in the body, including the brain. The cumulative toxic effects of chronic alcohol abuse can cause both medical and psychiatric problems. Identifying alcoholism is difficult for the individual afflicted because of the social stigma associated with the disease that causes people with alcoholism to avoid diagnosis and treatment for fear of shame or social consequences. The evaluation responses to a group of standardized questioning are a common method for diagnosing alcoholism. These can be used to identify harmful drinking patterns, including alcoholism. In general, problem drinking is considered alcoholism when the person continues to drink despite experiencing social or health problems caused by drinking.
_
Alcoholism is influenced by genetic, psychological, social and environmental factors that have an impact on how it affects your body and behavior. The process of becoming addicted to alcohol occurs gradually, although some people have an abnormal response to alcohol from the time they start drinking. Over time, drinking too much may change the normal balance of chemicals and nerve tracks in your brain associated with the experience of pleasure, judgment and the ability to exercise control over your behavior. This may result in your craving alcohol to restore good feelings or remove negative ones. Individuals vary widely in their innate responses to alcohol; however, the neurobiological mechanisms underlying these differences are likely not the ones causal to addiction. Alcohol addiction is not defined by physical dependence, i.e. the emergence of withdrawal symptoms upon cessation of drinking, but rather by its chronic relapsing course, where relapse is triggered by powerful urges or cravings that cause the loss of behavioural control. The phenomenon of craving is at the focus of neurobiological theories of alcohol addiction.
_
The lifetime risk for alcohol dependence in most Western countries is about 10–15% for men and 5–8% for women. Rates are generally similar in the United States, Canada, Germany, Australia, and the United Kingdom; tend to be lower in most Mediterranean countries, such as Italy, Greece, and Israel; and may be higher in Ireland, France, and Scandinavia. Even higher lifetime prevalence has been reported for most native cultures, including American Indians, Eskimos, Maori groups, and aboriginal tribes of Australia. These differences reflect both cultural and genetic influences. In Western countries, the typical alcoholic is more often a blue- or white-collar worker or homemaker. The lifetime risk for alcoholism among physicians is similar to that of the general population. Alcoholism is appropriately considered a disease rather than a weakness of character or chosen pattern of bad behavior. Alcohol abuse and alcoholism cut across gender, race, and ethnicity. Nearly 14 million people in the United States are dependent on alcohol. More men than women are alcohol dependent or have alcohol problems. Alcohol problems are highest among young adults ages 18-29 and lowest among adults ages 65 and older. Also, people who start drinking at an early age have a greater chance of developing alcohol problems at some point in their lives.
_
Alcoholism signs and symptoms include those below. You may:
•Be unable to limit the amount of alcohol you drink
•Feel a strong need or compulsion to drink
•Develop tolerance to alcohol so that you need more to feel its effects
•Drink alone or hide your drinking
•Experience physical withdrawal symptoms — such as nausea, sweating and shaking — when you don’t drink
•Not remember conversations or commitments, sometimes referred to as a “black out”
•Make a ritual of having drinks at certain times and become annoyed when this ritual is disturbed or questioned
•Be irritable when your usual drinking time nears, especially if alcohol isn’t available
•Keep alcohol in unlikely places at home, at work or in your car
•Gulp drinks, order doubles or become drunk intentionally to feel good, or drink to feel “normal”
•Have legal problems or problems with relationships, employment or finances due to drinking
•Lose interest in activities and hobbies that used to bring you pleasure
If you binge drink or have other problems with alcohol, you may have many of the signs and symptoms above, although you may not feel as much of a compulsion to drink compared with someone who has alcoholism. Also, you may not have physical withdrawal symptoms when you don’t drink. But this pattern of drinking can still cause serious problems and lead to alcoholism. As with alcoholism, you may not be able to quit problem drinking without help.
_
Risk factors for alcoholism include:
•Steady drinking over time. Drinking too much on a regular basis for an extended period or binge drinking on a regular basis can produce a physical dependence on alcohol.
•Age. People who begin drinking at an early age are at a higher risk of problem drinking or physical dependence on alcohol.
•Family history. The risk of alcoholism is higher for people who have a parent or other close relatives who have problems with alcohol.
•Depression and other mental health problems. It’s common for people with a mental health disorder such as anxiety, depression or bipolar disorder to have problems with alcohol or other substances.
•Social and cultural factors. Having friends or a close partner who drinks regularly could increase your risk of alcoholism. The glamorous way that drinking is sometimes portrayed in the media also may send the message that it’s OK to drink too much.
•Mixing medication and alcohol. Some medications interact with alcohol, increasing its toxic effects. Drinking while taking these medications can either increase or decrease their effectiveness, or even make them dangerous.
_
Warning signs:
Alcohol is addictive. Some warning signs are:
•you do not feel right without a drink, or need a drink to start the day
•you get very shaky, sweaty, and anxious/tense a few hours after your last drink
•you can drink a lot without becoming drunk
•you need to drink more and more to get the same effect
•you try to stop, but find you can’t
•you carry on drinking even though you can see it is interfering with your work, family and relationships
•you get “memory blanks” where you can’t remember what happened for a period of hours or days.
_
How can you tell if someone has a drinking problem?
Signs of a drinking problem include behaviors like drinking for the purpose of getting drunk, drinking alone or keeping it secret, drinking to escape problems, hiding alcohol in odd places, getting irritated when you are unable to obtain alcohol to drink, and having problems at work, school, home, or legally as a result of your drinking. Other warning signs of alcohol use disorder include losing interest in activities you used to enjoy, having blackouts because of heavy drinking, and getting annoyed when loved ones say you may have a drinking problem. Behaviors that may indicate that a person is suffering from alcoholism include being able to drink more and more alcohol, trouble stopping once you start drinking, powerful urges to drink, and having withdrawal symptoms like nervousness, nausea, shaking, or having cold sweats when you don’t have a drink.
Can an alcoholic just cut back or stop drinking?
While some people with alcohol use disorder can cut back or stop drinking without help, most are only able to do so temporarily unless they get treatment. Individuals who consume alcohol in lower amounts and tend to cope with problems more directly are more likely to be successful in their efforts to cut back or stop drinking without the benefit of treatment.
_
According to the DSM-IV criteria for alcohol dependence, at least three out of seven of the following criteria must be manifest during a 12 month period:
•Tolerance
•Withdrawal symptoms or clinically defined Alcohol Withdrawal Syndrome
•Use in larger amounts or for longer periods than intended
•Persistent desire or unsuccessful efforts to cut down on alcohol use
•Time is spent obtaining alcohol or recovering from effects
•Social, occupational and recreational pursuits are given up or reduced because of alcohol use
•Use is continued despite knowledge of alcohol-related harm (physical or psychological)
Dependence predicts a course of recurrent problems with the use of alcohol and the consequent shortening of the life span by a decade.
_
In psychology and psychiatry, the DSM is the most common global standard, while in medicine, the standard is ICD. The terms they recommend are similar but not identical.
| Organization | Preferred term(s) | Definition |
| APA’s DSM-IV | “alcohol abuse” and “alcohol dependence” | Alcohol abuse = repeated use despite recurrent adverse consequences.Alcohol dependence = alcohol abuse combined with tolerance, withdrawal, and an uncontrollable drive to drink.The term “alcoholism” was split into “alcohol abuse” and “alcohol dependence” in 1980’s DSM-III, and in 1987’s DSM-III-R behavioral symptoms were moved from “abuse” to “dependence”. It has been suggested that DSM-V merge alcohol abuse and alcohol dependence into a single new entry, named “alcohol-use disorder”. |
| WHO’s ICD-10 | “alcohol harmful use” and “alcohol dependence syndrome” | Definitions are similar to that of the DSM-IV. The World Health Organisation uses the term “alcohol dependence syndrome” rather than alcoholism. The concept of “harmful use” (as opposed to “abuse”) was introduced in 1992’s ICD-10 to minimize underreporting of damage in the absence of dependence. The term “alcoholism” is removed from ICD. |
_
The Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) recognizes two alcohol use disorders: alcohol dependence and alcohol abuse.
1. Alcohol dependence is characterized by multiple symptoms, including tolerance, signs of withdrawal, diminished control over drinking, as well as cognitive, behavioral, and/or physiological symptoms that suggest the individual continues to drink despite experiencing significant alcohol-related problems.
2. Alcohol abuse, on the other hand, is a maladaptive pattern of drinking that leads to clinically significant impairment or distress. An individual diagnosed with alcohol abuse drinks despite alcohol-related physical, social, psychological, or occupational problems. Alcohol abuse does not necessarily entail a consistent pattern of heavy drinking, but is defined by the adverse consequences associated with the drinking pattern.
_
In May 2013, the American Psychiatric Association issued the 5th edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM–5). Although there is considerable overlap between DSM–5 and DSM–IV, the prior edition, there are several important differences:
Changes Disorder Terminology:
DSM–IV described two distinct disorders, alcohol abuse and alcohol dependence, with specific criteria for each.
DSM–5 integrates the two DSM–IV disorders, alcohol abuse and alcohol dependence, into a single disorder called alcohol use disorder (AUD) with mild, moderate, and severe sub-classifications.
Changes Diagnostic Thresholds:
Under DSM–IV, the diagnostic criteria for abuse and dependence were distinct: anyone meeting one or more of the “abuse” criteria (see items 1 through 4) within a 12-month period would receive the “abuse” diagnosis. Anyone with three or more of the “dependence” criteria (see items 5 through 11) during the same 12-month period would receive a “dependence” diagnosis.
Under DSM–5, anyone meeting any two of the 11 criteria during the same 12-month period would receive a diagnosis of AUD. The severity of an AUD—mild, moderate, or severe—is based on the number of criteria met.
_
DSM-5 could categorize 40% of College Students as Alcoholics:
_
Are you or have you ever been a college binge drinker? Welcome to alcoholism, a diagnosis your college self could qualify for under the changes proposed to the next edition of psychiatry’s diagnostic manual, the DSM-5. The DSM-5, short for the Diagnostic and Statistical Manual of Mental Disorders 5; will have just one diagnosis for addiction problems, though they will be characterized as either mild, moderate or severe. Currently, alcohol and other drug problems come in two flavors. The first, “substance abuse” is a short-term, self-limiting problem: it encompasses most heavy drinking in college. The second “substance dependence,” is what everyone else calls addiction or alcoholism and is typically chronic and marked by relapses. Fortunately, the new diagnosis will get rid of the confusing term “dependence” (physically needing a drug to function isn’t actually addiction) and the stigmatizing term “abuse.” Unfortunately, however, it will also tremendously elevate the number of people considered alcoholics. One Australian study suggested that using DSM-5 definitions will increase the number of people diagnosed with alcoholism by a stunning 60%. Proponents of the new system argue that it will allow substance problems that might develop into serious addictions to be nipped in the bud: “We can treat them earlier,” said Dr. Charles P. O’Brien, a professor of psychiatry at the University of Pennsylvania and the head of the group of researchers devising the manual’s new addiction standards. “And we can stop them from getting to the point where they’re going to need really expensive stuff like liver transplants.”
_
Alcohol abuse and dependence, now both included under the diagnosis of alcohol use disorder, is a disease that is characterized by the sufferer having a pattern of drinking excessively despite the negative effects of alcohol on the individual’s work, medical, legal, educational, and/or social life. It may involve a destructive pattern of alcohol use that includes a number of symptoms, including tolerance to or withdrawal from the substance, using more alcohol and/or for a longer time than planned, and trouble reducing its use. Alcohol abuse, on the less severe end of the alcohol use disorder spectrum, affects about 10% of women and 20% of men in the United States, most beginning by their mid teens.
_
Under the new criteria, people who often drink more than intended and crave alcohol may be considered mild addicts. Under the old criteria, more serious symptoms, like repeatedly missing work or school, being arrested or driving under the influence, were required before a person could receive a diagnosis as an alcohol abuser. Dr. George E. Woody, a professor of psychiatry at the University of Pennsylvania School of Medicine, said that by describing addiction as a spectrum, the manual would reflect more accurately the distinction between occasional drug users and full-blown addicts. Currently, only about 2 million of the nation’s more than 22 million addicts get treatment, partly because many of them lack health insurance. Dr. Keith Humphreys, a psychology professor at Stanford who specializes in health care policy and who served as a drug control policy adviser to the White House from 2009 to 2010, predicted that as many as 20 million people who were previously not recognized as having a substance abuse problem would probably be included under the new definition, with the biggest increase among people who are unhealthy users, rather than severe abusers, of drugs. “This represents the single biggest expansion in the quality and quantity of addiction treatment this country has seen in 40 years,” Dr. Humphreys said, adding that the new federal health care law may allow an additional 30 million people who abuse drugs or alcohol to gain insurance coverage and access to treatment. Some economists have said that the number could be much lower, though, because many insurers will avoid or limit coverage of addiction treatment.
_
What are the stages of alcohol use disorder?
Five stages of alcohol and drug use disorders have been identified. The first stage is described as having access to alcohol rather than use of alcohol. In that stage, minimizing the risk factors that make a person more vulnerable to using alcohol are an issue. The second stage of alcohol use ranges from experimentation or occasional use to regular weekly use of alcohol. This or any of the more severe stages of alcoholism may involve binge drinking. The third stage is characterized by individuals further increasing the frequency of alcohol use and/or using the substance on a regular basis. This stage may also include either buying or stealing to get alcohol. In the fourth stage of alcohol use, users have established regular alcohol consumption, have become preoccupied with getting intoxicated (“high”) and have developed problems in their social, educational, vocational, or family life as a result of using the substance. The final and most serious fifth stage of alcohol use is defined by the person only feeling normal when they are using alcohol. During this stage, risk-taking behaviors like stealing, engaging in physical fights, or driving while intoxicated increase, and they become most vulnerable to having suicidal thoughts.
_
My view:
Any amount/duration of alcohol consumption with any harm (harm could be physical health, social, psychological, legal, educational, work related and economic) to any individual including self-harm is alcohol use disorder.
_
I delineate alcohol use spectrum in the following diagram:
__________
Screening tools:
The Alcohol Use Disorders Identification Test (AUDIT) is considered the most accurate alcohol screening tool for identifying potential alcohol misuse, including dependence. It was developed by the World Health Organisation, designed initially for use in primary healthcare settings with supporting guidance. Its use has replaced older screening tools such as CAGE but there are many shorter alcohol screening tools, mostly derived from the AUDIT. The Severity of Alcohol Dependence Questionnaire (SAD-Q) is a more specific twenty item inventory for assessing the presence and severity of alcohol dependence. The diagnosis of alcohol abuse or dependence ultimately rests on the documentation of a pattern of repeated difficulties associated with alcohol use. Thus, in screening it is important to probe for marital or job problems, legal difficulties, histories of accidents, medical problems, evidence of tolerance, etc., and then attempt to tie in use of alcohol or another substance. Some standardized questionnaires can be helpful, including the 10-item Alcohol Use Disorders Identification Test (AUDIT) as seen in the table below, but these are only screening tools, and a face-to-face interview is still required for a meaningful diagnosis.
_
The alcohol use disorders identification test (AUDIT):
| Item | 5-Point Scale (Least to Most) |
| 1. How often do you have a drink containing alcohol? | Never (0) to 4+ per week (4) |
| 2. How many drinks containing alcohol do you have on a typical day? | 1 or 2 (0) to 10+ (4) |
| 3. How often do you have six or more drinks on one occasion? | Never (0) to daily or almost daily (4) |
| 4. How often during the last year have you found that you were not able to stop drinking once you had started? | Never (0) to daily or almost daily (4) |
| 5. How often during the last year have you failed to do what was normally expected from you because of drinking? | Never (0) to daily or almost daily (4) |
| 6. How often during the last year have you needed a first drink in the morning to get yourself going after a heavy drinking session? | Never (0) to daily or almost daily (4) |
| 7. How often during the last year have you had a feeling of guilt or remorse after drinking? | Never (0) to daily or almost daily (4) |
| 8. How often during the last year have you been unable to remember what happened the night before because you had been drinking? | Never (0) to daily or almost daily (4) |
| 9. Have you or someone else been injured as a result of your drinking? | No (0) to yes, during the last year (4) |
| 10. Has a relative, friend, doctor or other health worker been concerned about your drinking or suggested that you should cut down? | No (0) to yes, during the last year (4) |
The AUDIT is scored by simply summing the values associated with the endorsed response.
_
The Paddington alcohol test (PAT) was first published in the Journal of Accident and Emergency Medicine in 1996. It was designed to identify alcohol-related problems amongst those attending accident and emergency departments. It concords well with the Alcohol Use Disorders Identification Test (AUDIT) questionnaire but is administered in a fifth of the time. When 40–70% of the patients in an accident and emergency department (AED) are there because of alcohol-related issues, it is useful for the staff of the AED to determine which of them are hazardous drinkers so that they can treat the underlying cause and offer brief advice which may reduce the health impact of alcohol for that patient. In accident and emergency departments it is also important to triage incoming patients as quickly as possible, to reduce staff size and cost. In one study, it took an average of 73 seconds to administer the AUDIT questionnaire but only 20 seconds for the PAT.
_
Identification of the Alcoholic:
Even in affluent locales, 20% of patients have an alcohol use disorder. These men and women can be identified by asking questions about alcohol problems and noting laboratory test results that are likely to be abnormal in the context of regular consumption of six to eight or more drinks per day. The two blood tests with 60% sensitivity and specificity for heavy alcohol consumption are -glutamyl transferase (GGT) (>35 U) and carbohydrate-deficient transferrin (CDT) (>20 U/L or >2.6%); the combination of the two is likely to be more accurate than either alone. The values for these serologic markers are likely to return toward normal within several weeks of abstinence. Other useful blood tests include high-normal MCVs (91 m3) and serum uric acid (>416 mol/L, or 7 mg/dL).
____
What are the long-term physical and psychological effects of alcohol use disorder?
The long-term effects of alcohol use disorder can be devastating and even life-threatening. Chronic excessive alcohol consumption can negatively affect virtually every organ system. Specific examples of alcohol-use disorder effects on the body include everything from general effects like poor coordination, thiamine deficiency, and other forms of poor nutrition, cardiovascular effects like hypertension and irregular heartbeat, reproductive effects like impotence and irregular menses, as well as gastrointestinal problems like jaundice, cirrhosis of the liver, and pancreatitis. Alcohol-use disorder complications that involve the brain include, but are by no means limited to, strokes, confusion, and amnesia. Approximately 10%-15% of people with alcoholism tend to commit suicide. Intoxication is associated with suicide attempts using more lethal methods, and positive blood-alcohol levels are often found in people who complete suicide. Men who have lost their spouses within the year are at highest risk of suicide.
_
Natural History:
Although the age of the first drink (15 years) is similar in most alcoholics and nonalcoholics, a slightly earlier onset of regular drinking and drunkenness, especially in the context of conduct problems, is associated with a higher risk for later alcohol use disorders. By the early to midtwenties, most nonalcoholic men and women moderate their drinking (perhaps learning from more minor problems), whereas alcoholics are likely to escalate their patterns of drinking despite difficulties. The first major life problem from alcohol often appears in the late teens to early twenties, and a pattern of multiple alcohol difficulties by the midtwenties. Once established, the course of alcoholism is likely to be one of exacerbations and remissions, with little difficulty in temporarily stopping or controlling alcohol use when problems develop, but without help, desistance usually gives way to escalations in alcohol intake and subsequent problems. Following treatment, between half and two-thirds of alcoholics maintain abstinence for years, and often permanently. Even without formal treatment or self-help groups there is also at least a 20% chance of spontaneous remission with long-term abstinence. However, should the alcoholic continue to drink, the life span is shortened by 10 years on average, with the leading causes of death, heart disease, liver cirrhosis, cancer, accidents, and suicide.
_
Treatment of addiction of alcohol:
The approach to treating alcohol-related conditions is relatively straightforward: (1) recognize that at least 20% of all patients have alcohol abuse or dependence; (2) learn how to identify and treat acute alcohol-related conditions; (3) know how to help patients begin to address their alcohol problems; and (4) know enough about treating alcoholism to appropriately refer patients for additional help.
_
New oral drugs reduce alcohol consumption:
Four medications have clinical value in treating patients with alcohol-use disorders, according to a systematic review in JAMA. Researchers examined over 120 studies of medications used for alcohol-use disorders. Some 23,000 patients were enrolled, most after detoxification or a period of sobriety. Acamprosate (a glutamine antagonist and γ-aminobutyric acid agonist) and oral naltrexone (an opioid antagonist) were about equally effective in preventing resumption of any drinking (number needed to treat, 12–20). Naltrexone was also effective in reducing heavy drinking, but acamprosate was not. Disulfiram (an acetaldehyde dehydrogenase inhibitor) did not reduce alcohol consumption. Two off-label medications — nalmefene (an opioid antagonist) and topiramate (an anticonvulsant) — were associated with improvements in heavy drinking. There was insufficient evidence for other off-label drugs, including SSRIs, tricyclic antidepressants, atypical antipsychotics, and gabapentin. Primary care clinicians should realize that, because effective medications exist to supplement psychosocial interventions, they can engage patients more assertively in shared decision-making, take primary responsibility for managing mild-to-moderate alcohol-use disorder, and coordinate effective referrals for complex patients.
_
Ondansetron has been found to be effective in treating alcohol use disorder in people whose problem drinking began before they were 25 years old. Baclofen has been found to be a potentially effective treatment to decrease alcohol cravings and withdrawal symptoms. Some research indicates that psychiatric medications like lithium and sertraline may be useful in decreasing alcohol use in people who have another mental-health disorder in addition to alcohol use disorder.
_
Disulfiram:
Disulfiram (Antabuse) competitively inhibits the enzyme aldehyde dehydrogenase, so that even a single drink usually causes a toxic reaction due to acetaldehyde accumulation in the blood. Administration of the drug should not begin until 24 hours after the patient’s last drink. The physician must warn the patient about the drug or for as long as 2 weeks thereafter. Those who drink while taking disulfiram turn purple, become severely ill for 30 to 60 minutes (or longer) and often vomit. Patients on disulfiram may also have this same response to alcohol ingested in mouthwash, wine sauces or vinegars, or even to inhaled alcohol vapors from aftershave lotions. Disulfiram may also exacerbate psychotic symptoms in schizophrenic patients (but this is uncommon). Disulfiram can be of critical importance in helping the alcoholic to make the essential decision to stop drinking. There should be nothing surreptitious about the use of disulfiram (i.e., no slipping the drug into the coffee by the spouse). It should be discussed with the patient, with full disclosure of its side effects and dangers. The initial dosage (after a minimum of 24 hours’ abstention from alcohol) is 500 mg/d in a single dose in the morning. This can be decreased to a maintenance dose of 250 mg/d, continued indefinitely. Disulfiram frees the alcoholic from ruminating as to whether he should or should not have a drink and prevents the relapses that usually follow a sudden and impulsive first drink.
_
What is the prognosis of alcohol use disorder?
With treatment, about 70% of people with alcoholism are able to decrease the number of days they consume alcohol and improve their overall health status within six months. On the other hand, most individuals who have been treated for a moderate to severe alcohol-use disorder have relapsed at least once during the first year after treatment. Those individuals seem to drink less often and lower amounts after receiving treatment compared with before treatment.
_
Alcoholism in family system:
Alcoholism in family systems refers to the conditions in families that enable alcoholism, and the effects of alcoholic behavior by one or more family members on the rest of the family. Mental health professionals are increasingly considering alcoholism and addiction as diseases that flourish in and are enabled by family systems. Family members react to the alcoholic with particular behavioral patterns. They may enable the addiction to continue by shielding the addict from the negative consequences of his actions. Such behaviors are referred to as codependence. In this way, the alcoholic is said to suffer from the disease of addiction, whereas the family members suffer from the disease of codependence. Alcoholism is one of the leading causes of a dysfunctional family. As of 2001, there were an estimated 26.8 million children of alcoholics (COAs) in the United States, with as many as 11 million of them under the age of 18. Children of addicts have an increased suicide rate and on average have total health care costs 32 percent greater than children of nonalcoholic families. According to the American Psychiatric Association, physicians stated three criteria to diagnose this disease: (1) physiological problems, such as hand tremors and blackouts, (2) psychological problems, such as excessive desire to drink, and (3) behavioral problems that disrupt social interaction or work performance. Adults from alcoholic families experience higher levels of state and trait anxiety and lower levels of differentiation of self than adults raised in non-alcoholic families. Additionally, adult children of alcoholics have lower self-esteem, excessive feelings of responsibility, difficulties reaching out, higher incidence of depression, and increased likelihood of becoming alcoholics. Parental alcoholism may affect the fetus even before a child is born. In pregnant women, alcohol is carried to all of the mother’s organs and tissues, including the placenta, where it easily crosses through the membrane separating the maternal and fetal blood systems. When a pregnant woman drinks an alcoholic beverage, the concentration of alcohol in her unborn baby’s bloodstream is the same level as her own. A pregnant woman who consumes alcohol during her pregnancy may give birth to a baby with Fetal Alcohol Syndrome (FAS). FAS (fetal alcohol syndrome) is known to produce children with damage to the central nervous system, general growth and facial features. The prevalence of this class of disorder is thought to be between 2-5 per 1000. Alcoholism does not have uniform effects on all families. The levels of dysfunction and resiliency of the non-alcoholic adults are important factors in effects on children in the family. Children of untreated alcoholics score lower on measures of family cohesion, intellectual-cultural orientation, active-recreational orientation, and independence. They have higher levels of conflict within the family, and many experience other family members as distant and non-communicative. In families with untreated alcoholics, the cumulative effect of the family dysfunction may affect the children’s ability to grow in developmentally healthy ways.
____________
Alcohol withdrawal:
Alcohol withdrawal syndrome is a set of symptoms that can occur when an individual reduces or stops alcoholic consumption after long periods of use. Prolonged and excessive use of alcohol leads to tolerance and physical dependence. The withdrawal syndrome is largely a hyper-excitable response of the central nervous system to lack of alcohol. Symptoms typical of withdrawal include agitation, seizures, and delirium tremens. Sedative-hypnotics, such as alcohol, are well known for their propensity to induce physiological dependence. This dependence is due to alcohol-induced neuro-adaptation. Withdrawal is characterized by neuropsychiatric excitability and autonomic disturbances. Dependence on other sedative-hypnotics can increase the severity of the withdrawal syndrome.
_
Epidemiology
•Only about 50% of alcohol-dependent patients develop clinically relevant symptoms of withdrawal.
•Less than 1 in 20 people who are alcohol-dependent have a grand mal seizure during withdrawal (usually on day 2), or severe agitated confusion (delirium tremens).
_
These symptoms usually begin within 5–10 h of decreasing ethanol intake, peak on day 2 or 3, and improve by day 4 or 5, although mild levels of these problems may persist for 4–6 months as a protracted abstinence syndrome. The spectrum of alcohol withdrawal symptoms ranges from such minor symptoms as insomnia and tremulousness to severe complications such as withdrawal seizures and delirium tremens. Although the history and physical examination usually are sufficient to diagnose alcohol withdrawal syndrome, other conditions may present with similar symptoms.
_
_
Alcohol withdrawal seizures:
The topic of alcohol withdrawal syndrome (AWS), including delirium tremens and especially seizures, is reviewed. From mice and rat studies, it is known that both N-methyl-d-aspartate (NMDA) and γ-aminobutyric acid (GABA) receptors are involved in AWS. During alcohol intoxication chronic adaptations of NMDA and GABA receptors occur, and during alcohol withdrawal a hyperexcitable state develops. In studies on humans, during intoxication the NMDA receptors are activated and mediate tonic inhibition. In withdrawal, a rebound activation of these receptors occurs. Both GABA-A and GABA-B receptors, especially the α2 subunit of GABA-A receptors, are also likely involved. Homocysteine increases with active drinking, and in withdrawal, excitotoxicity likely is induced by a further increase in homocysteine, viewed as a risk factor for AWS and also as a screening tool. The dopamine transporter gene is also associated with AWS. Characteristics involves changes in the ECG, especially an increase in QT interval, and EEG changes, including abnormal quantified EEG, at times periodic lateralized epileptiform discharges, and especially seizures, usually occurring 6–48 h after the cessation of drinking.
_
__
Diagnostic Criteria for Alcohol Withdrawal:
| A. Cessation of (or reduction in) alcohol use that has been heavy and prolonged. | |
| B. Two (or more) of the following, developing within several hours to a few days after criterion A: | |
| 1. Autonomic hyperactivity (e.g., sweating or pulse rate greater than 100 beats per minute) | |
| 2. Increased hand tremor | |
| 3. Insomnia | |
| 4. Nausea or vomiting | |
| 5. Transient visual, tactile, or auditory hallucination s or illusions | |
| 6. Psychomotor agitation | |
| 7. Anxiety | |
| 8. Grand mal seizures | |
| C. The symptoms in criterion B cause clinically significant distress or impairment in social, occupational, or other important areas of functioning. | |
| D. The symptoms are not due to a general medical condition and are not better accounted for by another mental disorder. | |
_
Kindling:
Kindling is a phenomenon where repeated alcohol detoxifications lead to an increased severity of the withdrawal syndrome. For example, binge drinkers may initially experience no withdrawal symptoms, but with each period of alcohol use followed by cessation, their withdrawal symptoms intensify in severity and may eventually result in full blown delirium tremens with convulsive seizures. Alcoholics who experience seizures during detoxification are more likely to have had previous episodes of alcohol detoxification than patients who did not have seizures during withdrawal. In addition, patients with previous withdrawal syndromes are more likely to have more medically complicated alcohol withdrawal symptoms. Kindling can cause complications and may increase the risk of relapse, alcohol-related brain damage and cognitive deficits. Chronic alcohol misuse and kindling via multiple alcohol withdrawals may lead to permanent alterations in the GABA-A receptors. The mechanism behind kindling is sensitization of some neuronal systems and desensitization of other neuronal systems which leads to increasingly gross neurochemical imbalances. This in turn leads to more profound withdrawal symptoms including anxiety, convulsions and neurotoxicity.
_
_
Binge drinking is associated with increased impulsivity, impairments in spatial working memory and impaired emotional learning. These adverse effects are believed to be due to the neurotoxic effects of repeated withdrawal from alcohol on aberrant neuronal plasticity and cortical damage. Repeated periods of acute intoxication followed by acute detoxification have profound effects on the brain and are associated with an increased risk of seizures as well as cognitive deficits. The effects on the brain are similar to those seen in alcoholics who have been detoxified multiple times but not as severe as in alcoholics who have no history of prior detox. Thus the acute withdrawal syndrome appears to be the most important factor in causing damage or impairment to brain function. The brain regions most sensitive to harm from binge drinking are the amygdala and prefrontal cortex. People in adolescence who experience multiple withdrawals from binge drinking show impairments of long-term nonverbal memory. Alcoholics who have had two or more alcohol withdrawals show more frontal lobe cognitive dysfunction than alcoholics who have experienced one or no prior withdrawals. Kindling of neurons is the proposed cause of withdrawal related cognitive damage. Kindling from multiple withdrawals leads to accumulating neuroadaptational changes. Kindling may also be the reason for cognitive damage seen in binge drinkers.
_
Treatment:
The first step in treating withdrawal is to perform a thorough physical examination in all alcoholics who are considering stopping drinking, including a search for evidence of liver failure, gastrointestinal bleeding, cardiac arrhythmia, infection, and glucose or electrolyte imbalance. It is also important to offer adequate nutrition and oral multiple B vitamins, including 50–100 mg of thiamine daily for a week or more. The prophylactic administration of thiamine intravenously is recommended before starting any carbohydrate containing fluids or food. Alcoholics are often deficient in various nutrients which can cause severe complications during alcohol withdrawal such as the development of Wernicke syndrome. The vitamins of most importance in alcohol withdrawal are thiamine and folic acid. To help to prevent Wernicke syndrome alcoholics should be administered a multivitamin preparation with sufficient quantities of thiamine and folic acid. Vitamins should always be administered before any glucose is administered otherwise Wernicke syndrome can be precipitated. Because most alcoholics who enter withdrawal are either normally hydrated or mildly overhydrated, IV fluids should be avoided unless there is a relevant medical problem or significant recent bleeding, vomiting, or diarrhea.
_
The next step is to recognize that because withdrawal symptoms reflect the rapid removal of a CNS depressant, alcohol, the symptoms can be controlled by administering any depressant in doses that decrease the agitation and then gradually tapering the dose over 3–5 days. While most CNS depressants are effective, benzodiazepines have the highest margin of safety and lowest cost and are, therefore, the preferred class of drugs. Short-half-life benzodiazepines can be considered for patients with serious liver impairment or evidence of brain damage, but they must be given every 4 h to avoid abrupt blood-level fluctuations that may increase the risk for seizures. Therefore, most clinicians use drugs with longer half-lives (e.g., chlordiazepoxide), adjusting the dose if signs of withdrawal escalate, and withholding the drug if the patient is sleeping or has evidence of orthostatic hypotension. The average patient requires doses of 25–50 mg of chlordiazepoxide or 10 mg of diazepam given PO every 4–6 h on the first day, with doses then decreased to zero over the next 5 days. While alcohol withdrawal can be treated in a hospital, patients in good physical condition who demonstrate mild signs of withdrawal despite low blood alcohol concentrations and who have no prior history of DTs or withdrawal seizures can be considered for outpatient detoxification. These patients should return daily for evaluation of vital signs and can be hospitalized if signs and symptoms of withdrawal escalate.
_
The choice of agent is based on pharmacokinetics. Diazepam and chlordiazepoxide are long-acting agents that have been shown to be excellent in treating alcohol withdrawal symptoms. Because of the long half-life of these medications, withdrawal is smoother, and rebound withdrawal symptoms are less likely to occur. Lorazepam and oxazepam are intermediate-acting medications with excellent records of efficacy. Treatment with these agents may be preferable in patients who metabolize medications less effectively, particularly the elderly and those with liver failure. Lorazepam is the only benzodiazepine with predictable intramuscular absorption (if intramuscular administration is necessary). Rarely, it is necessary to use extremely high dosages of benzodiazepines to control the symptoms of alcohol withdrawal. Dosages of diazepam as high as 2,000 mg per day have been administered. Because clinicians often are reluctant to administer exceptionally high dosages, undertreatment of alcohol withdrawal is a common problem. One randomized controlled trial (RCT) affirmed previous findings that carbamazepine is an effective alternative to benzodiazepines in the treatment of alcohol withdrawal syndrome in patients with mild to moderate symptoms. Patients in the study received 800 mg of carbamazepine on the first day, with the dosage tapered to 200 mg by the fifth day. Carbamazepine also appears to decrease the craving for alcohol after withdrawal. It is not sedating and has little potential for abuse. Although carbamazepine is used extensively in Europe, its use in the United States has been limited by lack of sufficient evidence that it prevents seizures and delirium.
_
Most patients undergoing alcohol withdrawal can be treated safely and effectively as outpatients. Pharmacologic treatment involves the use of medications that are cross-tolerant with alcohol. Benzodiazepines, the agents of choice, may be administered on a fixed or symptom-triggered schedule. Carbamazepine is an appropriate alternative to a benzodiazepine in the outpatient treatment of patients with mild to moderate alcohol withdrawal symptoms. Medications such as haloperidol, beta blockers, clonidine, and phenytoin may be used as adjuncts to a benzodiazepine in the treatment of complications of withdrawal.
_
Treatment of the patient with DTs can be challenging, and the condition is likely to run a course of 3–5 days regardless of the therapy employed. The focus of care is to identify and correct medical problems and to control behavior and prevent injuries. Many clinicians recommend the use of high doses of a benzodiazepine (as much as 800 mg/d of chlordiazepoxide has been reported), a treatment that will decrease agitation and raise the seizure threshold but probably does little to improve the confusion. Other clinicians recommend the use of antipsychotic medications, such as haloperidol or olanzapine, although these drugs have not been directly evaluated for DTs. Antipsychotics are less likely to exacerbate confusion but may increase the risk of seizures; they have no place in the treatment of mild withdrawal symptoms.
_
Treatment of alcohol withdrawal should be followed by treatment for alcohol dependence. In 1992, approximately 13.8 million Americans (7.4 percent of the U.S. adult population) met the criteria for alcohol abuse or dependence. In 2000, 226,000 patients were discharged from short-stay hospitals (excluding Veteran’s Affairs and other federal hospitals) with one of the following diagnoses: alcohol withdrawal, alcohol withdrawal delirium, or alcohol withdrawal hallucinosis. It is estimated that only 10 to 20 percent of patients undergoing alcohol withdrawal are treated as inpatients, so it is possible that as many as 2 million Americans may experience symptoms of alcohol withdrawal conditions each year.
_
Anticonvulsants for alcohol withdrawal: A review:
Alcohol abuse and dependence represents a most serious health problem worldwide with major social, interpersonal and legal interpolations. Besides benzodiazepines, anticonvulsants are often used for the treatment of alcohol withdrawal symptoms. Anticonvulsants drugs are indicated for the treatment of alcohol withdrawal syndrome, alone or in combination with benzodiazepine treatments. In spite of the wide use, the exact role of the anticonvulsants for the treatment of alcohol withdrawal has not yet been adequately assessed. Fifty-six studies, with a total of 4076 participants, met the inclusion criteria. Comparing anticonvulsants with placebo, no statistically significant differences for the six outcomes considered. Comparing anticonvulsant versus other drug, 19 outcomes considered, results favour anticonvulsants only in the comparison carbamazepine versus benzodiazepine (oxazepam and lorazepam) for alcohol withdrawal symptoms (CIWA-Ar score): 3 studies, 262 participants, MD -1.04 (-1.89 to -0.20), none of the other comparisons reached statistical significance. Comparing different anticonvulsants no statistically significant differences in the two outcomes considered. Comparing anticonvulsants plus other drugs versus other drugs (3 outcomes considered), results from one study, 72 participants, favour paraldehyde plus chloral hydrate versus chlordiazepoxide, for the severe-life threatening side effects, RR 0.12 (0.03 to 0.44) Results of this review do not provide sufficient evidence in favour of anticonvulsants for the treatment of AWS. There are some suggestions that carbamazepine may actually be more effective in treating some aspects of alcohol withdrawal when compared to benzodiazepines, the current first-line regimen for alcohol withdrawal syndrome. Anticonvulsants seem to have limited side effects, although adverse effects are not rigorously reported in the analysed trials. This Cochrane review summarizes evidence from forty-eight randomized controlled trials evaluating the effectiveness and safety of anticonvulsants in the treatment of alcohol withdrawal symptoms. There are limited data comparing anticonvulsants versus placebo and no clear differences between anticonvulsants and other drugs in the rates of therapeutic success. Data on safety outcomes are sparse and fragmented. There is a need for larger, well-designed studies in this field.
__
Prognosis:
Failure to manage the alcohol withdrawal syndrome appropriately can lead to permanent brain damage or death. It has been proposed that brain damage due to alcohol withdrawal may be prevented by the administration of NMDA antagonists, calcium antagonists, and glucocorticoid antagonists. The NMDA antagonist acamprosate reduces excessive glutamate rebound thereby suppressing excitotoxicity and potential withdrawal related neurotoxicity.
____
Abstinence from alcohol:
_
_
Abstinence from alcohol:
In Great Britain, 15% of adults have never drank alcohol. Over 51.1 percent of the American population 18-years of age and over are drinkers (having at least 12 or more drinks in a year). Statistics on abstainers vary, from 22.5 percent of men, to 11.6 percent of women. Somewhere in between those numbers are the moderate drinkers, those who consume about four drinks a day. Authors take a look at some of the reasons why people choose to abstain, and highlight instances where it is advisable to go alcohol-free. Despite the widespread assumption that drinking alcohol is an integral part of growing up, a 2012 report into why young people abstain showed that choosing not to drink is commonplace. Indeed, figures show that around half of 16 to 24 year olds in England said they’d drank nothing the week before they were asked about their drinking habits. While the decision not to is central to many people’s identity, for others it is no big deal, just one of many of life’s choices. There are a number of reasons why people abstain. It might be because of religious or medical reasons or because they don’t like the taste or effects of alcohol. Others don’t like how drinking makes them feel and want to stay in control of what they say and do.
Abstinence, ethnicity and religion:
Globally, 45% of people have never consumed alcohol. In the UK, people from minority ethnic groups tend to have higher rates of abstinence as well as lower levels of frequent and heavy drinking compared with the British population as a whole. Those from South Asia, mostly Pakistan and Bangladesh, are the ethnic group most likely to report they have never drank alcohol. This includes people who were born in South Asia or people whose ancestors are from there. Religion is the most common reason people give for not drinking. Overall, in the UK, Muslims are the religious group most likely to not drink, while Christians and people who say they have no religion, are the least likely to abstain.
Avoiding alcohol dependency or addiction:
Another reason for abstinence is the fear of becoming dependent on alcohol. The NHS estimates that around 9% of men in the UK and 4% of UK women show signs of alcohol dependence. We also know that the tendency to develop alcohol dependency is 60% inherited. One of the main reasons that young native UK citizens do not drink is because they have had a bad home experience with alcohol, often with parents with alcohol dependency.
Medical ground:
The Department of Health recommends that pregnant women, or women trying for a baby, should avoid alcohol altogether. If they do choose to drink, to minimise risk to the baby, the Department of Health’s advice is to have no more than one to two units of alcohol once or twice a week. The National Institute for Health and Clinical Excellence (NICE) additionally advises that the risks of miscarriage in the first three months of pregnancy mean that it is particularly important for women not to drink alcohol at all during that period. People taking sedative drugs, like Diazepam, or antidepressants, such as fluoxetine should avoid alcohol altogether. Alcohol is a depressant which slows down aspects of brain activity. The effects of alcohol can make some drugs, taken for long-term conditions, less effective. Examples include people taking drugs for epilepsy or diabetes, or drugs like warfarin to thin the blood. Alcohol can affect the way these drugs are absorbed by the body or broken down in the liver. If you drink alcohol regularly, especially if you drink excessive amounts, your liver produces more enzymes so that it can get rid of the alcohol more quickly. Those same enzymes break down some medications so they no longer have the same effect. People with diabetes who are treated with insulin or some tablets, including suplhonylureas, are at risk of low blood sugar. Alcohol can increase the risk of severe hypoglycemia, which can cause brain damage and can even be fatal. Many medications, including some antihistamines and many painkillers, can cause drowsiness. Even a small amount of alcohol can increase this effect, putting you at risk of accidents. The anti-microbial metronidazole and tinidazole can lead to a build-up of acetaldehyde, one of the breakdown products of alcohol which causes nausea, vomiting, flushing of the skin, accelerated heart rate or shortness of breath. So you should always read the label of the antibiotics to check whether they can be mixed with alcohol. NHS advice is that people who choose to drink when taking antibiotics that are safe to mix with alcohol, should limit their intake in line with the government’s lower risk guidelines. If people have an abnormal reaction to drinking alcohol, it could mean that they are intolerant to it. Some people have a genetic mutation of the enzyme needed to break down alcohol; this can lead to flushes or nasal congestion if they drink alcohol because their bodies can’t break it down properly. In this case, the medical advice is to abstain from drinking alcohol. You might also be allergic to some of the ingredients in alcoholic drinks, for example wheat or yeast in beer. Much of the protein which causes allergy to wheat and yeast is eliminated in the brewing process but it is theoretically possible that people with these allergies might also be allergic to beer. If you do develop liver problems, then you must stop drinking altogether. If you have early stage liver damage, abstaining from alcohol can allow the organ to recover. And if you have end stage cirrhosis, cutting out alcohol is essential to prevent you from dying from liver failure which is when your liver stops working completely.
_
Many medical experts recommend taking regular days off from drinking to ensure you don’t become addicted to alcohol. Taking regular breaks from alcohol can help to break any habitual patterns of drinking you have unintentionally fallen into. Such as going straight to the fridge or wine rack to get a glass of wine or beer after coming home from work or after putting the kids to bed. It will also reduce the risk of you building up a tolerance to alcohol, which is when you find yourself having to drink more to get the same effect. This can mean you end up drinking to levels that are harmful to your short and long-term health.
_
Sobriety has marked and early, globally averaged and regionally specific morphological, metabolic as well as functional benefits for convalescent alcoholics. Whether this is due to glial or neuronal viability or both remains somewhat unclear but prolonged dependence might possibly limit rapid recovery from white matter brain injury. Elucidating the precise nature and cellular mechanisms of this recovery further may serve as a valuable model of brain regeneration and, in the future, become relevant for other disorders with toxic insults of white matter, in particular.
___________
Alcohol and mental health:
Psychiatric Comorbidity:
Most mental disorders occur much more often than expected by chance among people who are abusing alcohol or are alcohol dependent (Kessler et al. 1996). Of these individuals, those who are alcohol dependent are more likely than alcohol abusers to have mental disorders. In fact, alcohol dependence elevates the risk for all types of affective and anxiety disorders (Kessler et al. 1996). One recent study found that alcohol consumption is related to the lifetime prevalence of mental disorders (Ross et al. 1997). In this study, current at-risk drinkers, defined as individuals who had consumed at least 29 alcoholic drinks in the previous week, had approximately twice the risk of mental disorder as lifetime abstainers (Ross et al. 1997). The likelihood of having an antisocial personality disorder was very high for current at-risk drinkers compared with lifetime abstainers. In addition, current at-risk drinkers were two to three times as likely as lifetime abstainers to have mood disorders and between one-and-a-half and two times as likely to have anxiety disorders. Unlike in previous studies (Leifman et al. 1995; Lipton 1994; Vaillant 1995), Ross and colleagues found no protective effect for any kind of drinking pattern (Ross et al. 1997). As many as two-thirds of alcohol-dependent individuals meet the criteria for a psychiatric syndrome in the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) of the American Psychiatric Association. Half of these relate to a preexisting antisocial personality manifesting as impulsivity and disinhibition that contribute to both alcohol and drug dependence. The lifetime risk is 3% in males, and 80% of such individuals demonstrate alcohol and/or drug dependence. Another common comorbidity occurs with dependence on illicit substances. The remainder of alcoholics with psychiatric syndromes has preexisting conditions such as schizophrenia or manic-depressive disease and anxiety disorders such as panic disorder. The comorbidities of alcoholism with independent psychiatric disorders might represent an overlap in genetic vulnerabilities, impaired judgment in the use of alcohol from the independent psychiatric condition, or an attempt to use alcohol to alleviate some of the symptoms of the disorder or side effects of medications.
_
Many psychiatric syndromes can be seen temporarily during heavy drinking and subsequent withdrawal. These alcohol-induced conditions include an intense sadness lasting for days to weeks in the midst of heavy drinking seen in 40% of alcoholics, which tends to disappear over several weeks of abstinence (alcohol-induced mood disorder); temporary severe anxiety in 10–30% of alcoholics, often beginning during alcohol withdrawal, which can persist for a month or more after cessation of drinking (alcohol-induced anxiety disorder); and auditory hallucinations and/or paranoid delusions in a person who is alert and oriented, seen in 3–5% of alcoholics (alcohol-induced psychotic disorder).
_
Treatment of all forms of alcohol-induced psychopathology includes helping patients achieve abstinence and offering supportive care, as well as reassurance and “talk therapy” such as cognitive-behavioral approaches. However, with the exception of short-term antipsychotics or similar drugs for substance-induced psychoses, substance-induced psychiatric conditions only rarely require medications. Recovery is likely within several days to 4 weeks of abstinence. Conversely, because alcohol-induced conditions are temporary and do not indicate a need for long-term pharmacotherapy, a history of alcohol intake is an important part of the workup for any patient with one of these psychiatric symptoms.
_
Comorbid Depression and Alcohol Dependence:
Both major depression and alcohol dependence carry a significant risk for the development of the other. Severity in one disorder is associated with severity in the other. Moreover, alcohol dependence prolongs the course of depression, and persistent depression during abstinence from alcohol is a risk factor for relapse to heavy drinking. Thus, logic dictates that both disorders be identified and managed concurrently and aggressively. Integrated psychosocial outpatient treatment programs and the ability to treat alcohol and depression simultaneously have reinforced the need to revisit the traditional management of comorbid major depression and alcohol dependence more formally.
_
Studies are finding a strong link between serious alcohol use and depression. The question is, does regular alcohol consumption lead to depression, or are depressed people more likely to drink excessively? Research is split on the issue. It’s also possible that depression and alcohol abuse share common genetic or environmental risk factors that trigger both conditions.
Does Depression lead to Alcohol Abuse?
Nearly one-third of people with major depression also have an alcohol problem, according to one major study conducted by the National Institute on Alcohol Abuse and Alcoholism. In many cases, depression may be the first to occur. Research shows that children who are depressed are more prone to develop alcohol problems once they reach adolescence. Teens who’ve had an episode of major depression are twice as likely as those who aren’t depressed to start drinking alcohol. Depression may be a particularly significant trigger for alcohol use in women, who are more than twice as likely to start drinking heavily if they have a history of depression. Experts say that women are more likely than men to self-medicate with alcohol.
Does Alcohol Abuse lead to Depression?
A number of studies have shown that alcohol abuse increases the risk for depression. This connection may be because of the direct neurotoxic effects of heavy alcohol exposure to the brain. Researchers know that heavy alcohol consumption can lead to periods of depression. Alcohol abuse also can have serious repercussions on a person’s life, leading to financial and legal troubles, impaired thinking and judgment, as well as marital stress. If you’re struggling with money or grappling with a failed relationship, you’re more likely to feel depressed.
_
Are Genes or Lifestyle Factors responsible for the Link between Alcohol Use and Depression?
It’s not clear yet whether depression triggers alcohol abuse or vice versa, but it’s very likely that they share common triggers. Studies of twins have shown that the same factors that contribute to heavy drinking in families also contribute to the risk for major depression. Researchers have been searching for a common gene or genes that might lie behind both conditions. They have pinpointed at least one — a variant of the gene CHRM2 — that is involved in several important brain functions, including memory and attention. Variations in this gene might put people at risk for alcohol dependence and depression. A person’s home and social environment also can play a big role in determining whether they will develop both depression and a drinking problem. Children who have been abused or who were raised in poverty appear to be more likely to develop both conditions
_
Alcohol and suicide:
Substance abuse is the second most common risk factor for suicide after major depression and bipolar disorder. Both chronic substance misuse as well as acute intoxication is associated. When combined with personal grief, such as bereavement, the risk is further increased. Additionally substance misuse is associated with mental health disorders. Most people are under the influence of sedative-hypnotic drugs (such as alcohol or benzodiazepines) when they commit suicide with alcoholism present in between 15% and 61% of cases. Countries that have higher rates of alcohol use and a greater density of bars generally also have higher rates of suicide with this link being primarily related to distilled spirit use rather than total alcohol use. About 2.2–3.4% of those who have been treated for alcoholism at some point in their life die by suicide. Alcoholics who attempt suicide are usually male, older, and have tried to commit suicide in the past. The association of alcohol and drugs with suicidal thinking and behavior is both causal and conductive. The subjective state of hopelessness is key to the disposition to actual suicides. Alcohol and drugs are influential in providing a feeling of hopelessness by their toxic effects, by possible manipulating of neurotransmitters responsible for the mood and judgment and by disruption of interpersonal relationships and social supports. The identification of alcohol and drug use and dependence is critical to the proper assessment of suicide. According to studies, over fifty percent of all suicides are associated with alcohol and drug dependence and at least 25% of alcoholics and drug addicts commit suicide. Over 70% of adolescent suicides may be complicated by drug and alcohol use and dependence. Because alcoholism and drug addiction are leading risk factors for suicidal behavior and suicide, any alcoholic or drug addict should be assessed for suicide, especially if actively using alcohol or drugs.
_
Psychosocial Consequences of alcohol use:
Alcohol use plays a role in many social activities, from the “business lunch” to the parties to the special occasions, such as gift giving. The benefits to those who drink during social occasions are greatly influenced by culture, the setting in which drinking occurs, and people’s expectations about alcohol’s effects (Goldman et al. 1987; Heath 1987; Leigh 1989; Leigh and Stacy 1991). In the few studies available of people who reported receiving psychological benefits from alcohol use, the number of benefits reported correlated with how much alcohol they drank as well as with how often they drank heavily (Hauge and Irgens-Jensen 1990; Mäkelä and Mustonen 1988). Stress reduction, mood elevation, increased sociability, and relaxation are the most commonly reported psychosocial benefits of drinking alcohol (Baum-Baicker 1985; Hauge and Irgens-Jensen 1990; Leigh and Stacy 1991; Mäkelä and Mustonen 1988). Alleviating psychological stress may be the most significant of these potential benefits, since stress reduction is reported to contribute to a lowered risk of cardiovascular disease and other health problems (Klatsky 1996; Pohorecky 1990; Poikolainen 1994; Zeichner et al. 1983). However, studies have not measured the effectiveness of alcohol use relative to other means for reducing stress-related diseases. There is extensive evidence indicating that people who suffer psychological distress and rely on alcohol to relieve their stress are more likely to develop alcohol abuse and dependence (Castaneda and Cushman 1989; Kessler et al. 1996, 1997). Even moderate amounts of alcohol can be harmful to people with mood and anxiety disorders because their symptoms are likely to worsen, and they may experience adverse drug interactions if they are taking medication (Castaneda et al. 1996).
__________
Factors affecting alcohol consumption and alcohol related harm:
A variety of factors have been identified at the individual and the societal levels, which affect the magnitude and patterns of consumption and can increase the risk of alcohol use disorders and other alcohol-related problems in drinkers and others (Shi & Stevens, 2005; Babor et al., 2010). Environmental factors such as economic development, culture, availability of alcohol and the level and effectiveness of alcohol policies are relevant factors in explaining differences in vulnerability between societies, historical trends in alcohol consumption and alcohol-related harm (WHO, 2007; Babor et al., 2010; Nelson et al., 2013). For a given level or pattern of drinking, vulnerabilities within a society are likely to have many of the same differential effects as those for differences between societies. Many of these differences are mitigated, but not entirely removed, by the universal availability of health care within the society. Where there is unequal access to treatment or other resources, the health and social consequences of a given level or pattern of drinking are also likely to be more severe for those with less resources (Shi & Stevens, 2005; WHO, 2007; Blas & Kurup, 2010). Although there is no single risk factor that is dominant, the literature suggests that the more vulnerability a person has, the more likely the person is to develop alcohol problems (Schmidt et al., 2010). From a public health perspective, vulnerability denotes susceptibility to poor health or illness, which can be manifested through physical, mental and social outcomes, including alcohol-related problems. It has been shown that vulnerable individuals are often at greater risk of having more than one individual risk factor, e.g., unhealthy diet, lack of physical activity and tobacco use (Blas & Kurup, 2010).
Age:
Children, adolescents and elderly people are typically more vulnerable to alcohol-related harm from a given volume of alcohol than other age groups (Hilton, 1987; Midanik & Clark, 1995; Mäkelä & Mustonen, 2000). Also, early initiation of alcohol use (before 14 years of age) is a predictor of impaired health status because it is associated with increased risk for alcohol dependence and abuse at later ages (Grant & Dawson, 1997; Grant, 1998; DeWit et al., 2000; Kraus et al., 2000, Sartor et al., 2007), alcohol-related motor vehicle crashes (Hingson et al., 2001; Hingson, Edwards & Zha, 2009), and other unintentional injuries (Hingson et al., 2000; Cherpitel, 2013). At least part of the excess risk among young people is related to the fact that, typically, a greater proportion of the total alcohol consumed by young people is consumed during heavy drinking episodes (US Surgeon General, 2007). Also, young people appear to be less risk-averse and may engage in more reckless behaviour while drunk. Alcohol-related harm among elderly people is due to somewhat different factors than alcohol-related harm among young people. While alcohol consumption generally declines with age, older drinkers typically consume alcohol more frequently than other age groups. Also, as people grow older, their bodies are typically less able to handle the same levels and patterns of alcohol consumption as in previous life years, leading to a high burden from unintentional injuries, such as alcohol-related falls (Sorock et al., 2006; Grundstrom et al., 2012). The alcohol-related burden of disease among older age groups is an increasing public health concern because of the rapidly ageing population in many countries worldwide (WHO, 2012). Age-related vulnerability is the basis for age-specific monitoring of alcohol consumption and policy responses. Alcohol policies that are based on age-related vulnerability include partial or total advertising bans, restrictions on access to alcohol through minimum ages at which it is legal to purchase alcohol, and laws aimed to prevent any alcohol consumption by young people when driving vehicles.
Gender:
Harmful use of alcohol is the leading risk factor for death in males aged 15–59 years, yet there is evidence that women may be more vulnerable to alcohol-related harm from a given level of alcohol use or a particular drinking pattern. The vulnerability of females to alcohol-related harm is a major public health concern because alcohol use among women has been increasing steadily in line with economic development and changing gender roles (Grucza et al., 2008; Wilsnack, 2013) and because it can have severe health and social consequences for newborns (Abel & Sokol, 1987; Lupton et al., 2004; Popova et al., 2013). 7.6% of all male deaths in 2012 were attributable to alcohol, compared to 4.0% of female deaths. Men also have a far greater rate of total burden of disease expressed in disability-adjusted life years (DALYs) attributable to alcohol than women – 7.4% for men compared to 2.3% for women. The increased burden of disease among men is largely explained by the fact that compared to women, men are less often abstainers, drink more frequently and in larger quantities. When the number of health and social consequences is considered for a given level of alcohol use or drinking pattern, sex differences for social outcomes reduce significantly or even reverse. One explanation is the higher prevalence of injuries among men (Midanik & Clark, 1995; Bongers et al., 1998; Mäkelä & Mustonen, 2000; Hoeksema, 2004); however, for health outcomes such as cancers, gastrointestinal diseases or cardiovascular diseases, the same level of consumption leads to more pronounced outcomes for women (Rehmet al., 2010a). “Sex” refers to the biological and physiological characteristics and “gender” refers to the socially constructed roles, behaviours etc. The vulnerability of women may be explained by a wide range of factors (Wilsnack et al., 2013). For example, women typically have lower body weight, smaller liver capacity to metabolize alcohol, and a higher proportion of body fat, which together contribute to women achieving higher blood alcohol concentrations than men for the same amount of alcohol intake. Women are also affected by interpersonal violence and risky sexual behaviour as a result of the drinking problems and drinking behaviour of male partners (Morojele et al., 2006; Kalichman et al., 2007). Moreover, alcohol use has been shown to be a risk factor for breast cancer (Allen et al., 2009; Boyle & Boffetta, 2009; Seitz et al., 2012). Also many societies hold more negative attitudes towards women’s drinking alcohol than men’s drinking, and especially towards their harmful drinking (Otto, 1981; Gomber, 1988; Pretorius et al., 2009), which, depending on the cultural context, may increase women’s vulnerability to social harm. Finally, women who drink during pregnancy may increase the risk of fetal alcohol spectrum disorder (FASD), and other preventable health conditions in their newborns (Barr & Steissguth, 2001; Viljoen et al., 2005). This is part of the evidence supporting mandatory health warning labels on alcoholic beverage containers, including information for all pregnant women on the impact of alcohol on the fetus.
Familial risk factors:
A family history of alcohol use disorders is considered a major vulnerability factor for both genetic and environmental reasons (Merigankas et al., 1998; WHO, 2004a). Heritable or genetic risk factors account for a substantial proportion of the variation in alcohol dependence. Multiple genes influence alcohol use initiation, metabolism and reinforcing properties in different ways (Clark, 2006), contributing to the increased susceptibility to toxic, psychoactive and dependence-producing properties of alcohol in some vulnerable groups and individuals. Parental alcohol use disorders have been found to negatively affect the family situation during childhood. Parents with alcohol use disorders display particular patterns of alcohol consumption and thereby increase the likelihood that their children will develop drinking patterns associated with high risk of alcohol use disorders when they are introduced to alcohol. Heavy drinking by parents affects family functioning, the parent–child relationship and parenting practices, which in turn affects child development adversely (Latendresse et al., 2008). The mistreatment of children, including sexual abuse, physical abuse and neglect, may also lead to childhood psychopathology and later to problem drinking (Shin et al., 2009).
Socioeconomic status:
Surveys and mortality studies, particularly from the developed world, suggest that there are more drinkers, more drinking occasions and more drinkers with low-risk drinking patterns in higher socioeconomic groups, while abstainers are more common in the poorest social groups. However, people with lower socioeconomic status (SES) appear to be more vulnerable to tangible problems and consequences of alcohol consumption (Grittner et al., 2012). For example, manual workers seem more vulnerable to severe alcohol-related health outcomes, including mortality, than non-manual workers for a given pattern of drinking. Notably, this vulnerability is found to be handed down through the generations (Norström & Romelsjö, 1998; Mäkelä et al., 1999a, 2002; Hemström et al., 2002). One explanation for the potentially greater vulnerability among lower SES groups is that they are less able to avoid adverse consequences of their behaviour due to a lack of resources. For example, individuals with higher SES may be more able to choose safer environments in which to drink, purchase social or spatial buffering of their behaviour and have better access to high-quality health care services (potentially explaining SES-related differences in survival after hospitalization or treatment for alcohol problems). A second explanation could be that individuals in lower SES groups have a less extensive support network, i.e., fewer factors or persons to motivate them to address alcohol problems before severe consequences occur. A third, contested, explanation that has been proposed in the past is that of an “all or nothing” pattern of behaviour in lower SES groups, i.e., poor people drink less often, but when they drink, they drink a lot (Schmidt et al, 2010). The link between SES and alcohol-related harm is an area of growing public health concern, because market liberalization and increasing affluence have increased the availability of alcohol to lower SES groups in growing economies. Given that changes in affordability of alcohol have often increased drinking, particularly among lower SES groups (Mäkelä,1999b; McKee et al., 2000; Hradilova Selin, 2004), a rise in alcohol consumption is expected to increase the alcohol-attributable burden of disease in developing economies. The process of marginalization and stigmatization related to alcohol use disorders, and the drift in social status that may result, may also cause significant social burden.
Economic development:
The most important of the societal vulnerability factors related to alcohol consumption, as well as to alcohol-attributable disease burden, is economic development. The research on links between alcohol consumption, alcohol-related harm and economic development of a society, country or region largely mirrors data on associations between alcohol consumption and the SES of an individual. Greater economic wealth is broadly associated with higher levels of consumption and lower abstention rates. However, for a given level or pattern of drinking, the alcohol-attributable mortality and burden of disease and injury will generally be greater in societies with lower economic development than in more affluent societies. For chronic effects of heavy drinking such as liver cirrhosis, for instance, there will often be a worse outcome because of the existence of cofactors such as nutritional deficiencies or viral hepatitis (Room et al., 2002a). Also, services to mitigate the adverse health effects of drinking are likely to be less widely available. Drink–driving may also have a worse outcome because less affluent societies have less safe streets and vehicles.
Culture and context:
The degree of risk for harm due to use of alcohol varies with the drinker’s age, sex, familial factors and SES, as well as the drinker’s behaviour and alcohol exposure (volume, patterns and quality of alcohol consumed). However, it also varies with the physical and socioeconomic context in which a given drinking occasion and the ensuing hours take place. Moreover, the nature and extent of the harm that results from drinking can vary widely depending on the context. In some contexts, drinkers will be vulnerable to alcohol-related social harm, disease, injury or even death if any volume of alcohol is consumed. This is the case for instance if a person drinks before driving a car or piloting an airplane, when consuming alcohol can result in serious penalties and harm. Also, in many countries there can be serious social or legal consequences for drinking at all, due to laws and regulations or cultural and religious norms, which can increase the vulnerability of drinkers to alcohol-related social harm. Studies showing differences in consumption or alcohol-related harm between different ethnicities within countries have underlined the importance of further research on culture-related vulnerabilities (Neumark et al., 2003; Chartier et al., 2013).
Alcohol control and regulation:
Another critical factor in determining the level of vulnerability to harmful use of alcohol and alcohol-related harm across countries is the level and effectiveness of alcohol control and regulations in each country, and within countries, in each jurisdiction with the ability to set alcohol policies (Babor et al., 2010).
_
Factors affecting alcohol consumption and alcohol related harm can be summarized in the figure below:
_
According to the 2010 US Dietary Guidelines for Americans, some groups of people should not drink alcoholic beverages at all. These include:
• Children and teens
• People who cannot limit their drinking or who are recovering from alcoholism
• Women who are or may become pregnant
• People who plan to drive or operate machinery
• People who take part in other activities that require attention, skill, or coordination or in situations where impaired judgment could cause injury or death
• People taking prescription or over-the-counter medicines that interact with alcohol
• People with certain medical conditions (such as liver disease or pancreatitis)
________________
Alcohol and physical health:
Alcohol is a psychoactive substance with dependence-producing properties that has been widely used in many cultures for centuries. The harmful use of alcohol causes a large disease, social and economic burden in societies.
1. Environmental factors such as economic development, culture, availability of alcohol and the level and effectiveness of alcohol policies are relevant factors in explaining differences and historical trends in alcohol consumption and related harm.
2. Alcohol-related harm is determined by the volume of alcohol consumed, the pattern of drinking, and, on rare occasions, the quality of alcohol consumed.
3. The harmful use of alcohol is a component cause of more than 200 disease and injury conditions in individuals, most notably alcohol dependence, liver cirrhosis, cancers and injuries.
4. The latest causal relationships suggested by research are those between harmful use of alcohol and infectious diseases such as tuberculosis and HIV/AIDS.
5. A wide range of global, regional and national policies and actions are in place to reduce the harmful use of alcohol.
_
_
Alcohol Consumption and the Prevalence of the Metabolic Syndrome:
Inconsistent results have been reported between alcohol and the metabolic syndrome. Yoon et al. reported that 1–15 g of alcohol per day was associated with decreased prevalence of the metabolic syndrome, whereas Park et al. reported a decrease only in women. This difference may relate to the fact that Park et al. included in the “heavy” drinking category participants who had a history of “ever consuming five or more drinks almost daily” even if they were not currently drinking. Furthermore, participants were included if they fasted for ≥6 h, whereas the present that of Yoon et al. required ≥8 and 10–12 h, respectively. Numerous studies show serum HDL cholesterol concentrations increase in a dose-dependent response to alcohol consumption. Serum triglycerides are higher in heavy drinkers but can be lower in light to moderate drinkers. The relation with obesity, on the other hand, has not been reported in a consistent fashion. Nevertheless, some data demonstrate that moderate amounts of alcohol, especially wine, are associated with smaller waist circumference as compared with no alcohol consumption. Furthermore, several studies have demonstrated lower insulin concentrations and increased insulin sensitivity among drinkers. In contrast, only a few studies have shown a beneficial effect of alcohol consumption on blood pressure, whereas the majority of studies support that alcohol consumption results in elevated blood pressure. The strength of the association between alcohol consumption and the metabolic syndrome may depend heavily upon the prevalence of these individual criteria in a given population. Researchers found that the reduced prevalence of metabolic syndrome was stronger among drinkers of wine and beer than of liquor. In summary, mild to moderate alcohol consumption, especially of beer and wine, is associated with a lower prevalence of the metabolic syndrome and with a favorable influence on serum lipids, waist circumference, and fasting serum insulin. This observed association between alcohol consumption and the metabolic syndrome was particularly strong in white individuals. To examine the relationship between alcohol consumption and metabolic syndrome, a meta-analysis was conducted of seven studies with 22,000 participants. Metabolic syndrome is a dangerous cluster of risk factors that increase the risk for coronary artery disease, stroke, and type 2 diabetes. The analysis found that drinking alcohol in moderation significantly reduced the prevalence of metabolic syndrome. The positive effects existed among men who consumed up to a little over three drink per day and among women who consumed up to one and one-half drinks each day.
_
Gastrointestinal System:
Alcohol consumption can interfere with the function of all parts of the gastrointestinal tract. Acute alcohol ingestion induces changes in the motility of the esophagus and stomach that favor gastroesophageal reflux and, probably, the development of reflux esophagitis. Alcohol abuse may lead to damage of the gastric mucosa, including hemorrhagic lesions. Beverages with a low alcohol content stimulate gastric acid secretion, whereas beverages with a high alcohol content do not. In the small intestine, alcohol inhibits the absorption of numerous nutrients. The importance of these absorption disorders for the development of nutritional disturbances in alcoholics, however, is unclear. In alcoholics with other digestive disorders (e.g., advanced liver disease or impaired pancreatic function), impaired digestion is more significant. Acute alcohol consumption also damages the mucosa in the upper region of the small intestine and may even lead to the destruction of the tips of the villi. The findings of human and animal studies suggest that these mucosal defects favor the following sequence of events: Alcohol-induced mucosal damage in the small intestine increases the mucosa’s permeability, facilitating the transport of large molecules, such as bacterial endotoxin and/or other toxins, into the blood or lymph. This results in the release of potentially toxic cytokines by certain white blood cells and Kupffer cells. These cytokines, in turn, exert multiple injurious effects on membranes and the microcirculation. The result is possible cell damage and even cell death in the liver and other organs. Motility disorders, maldigestion, and malabsorption in alcoholics can result in digestive problems, such as anorexia, nausea, and abdominal pain. Alcohol abuse also promotes the development of cancers of the tongue, larynx, pharynx, and esophagus. Finally, the results of recent epidemiological studies indicate an association between alcohol consumption and the development of colorectal cancer. Esophageal dysfunction, barrett’s esophagus and traumatic rupture of the esophagus have been seen following heavy alcohol consumption. In stomach, heavy alcohol use can disrupt the gastric mucosal barrier and cause acute and chronic gastritis (Thrift et al., 2011). Chronic alcohol digestions result in malabsorption in the small intestine. The major symptom is frequent loose stools. The rectal fissures and pruritus ani that frequently are associated with heavy drinking probably are related to chronic diarrhea (Daniel et al., 1994). Alcohol beverage usage is the most common causes of both acute and chronic pancreatitis in the world (Masamune and Shimosegawa, 2012). Some studies have been showed that uses of medicinal plant with anti-inflammatory and antioxidant properties could prevent from induction and progression of acute pancreatitis in an animal model of pancreatitis (Abed et al., 2012; Minaiyan et al., 2012).
_
Pancreatitis:
In addition to causing stomach irritation (gastritis), drinking can inflame the pancreas. Chronic pancreatitis interferes with the digestive process, causing severe abdominal pain and persistent diarrhea –and it’s not fixable. Some cases of chronic pancreatitis are triggered by gallstones, but up to 60% stem from alcohol consumption.
_
Hematological and Immunological Systems:
Chronic alcohol consumption is associated with some anemia. Microcytic and Macrocytic anemia and increases in mean corpuscular volume may occur in the absence of vitamin deficiencies. Normochromic anemia also can occur because of chronic effects on hematopoiesis. In the presence of severe liver disease, morphological changes including the development of burr cells, schistocytes, and ringed sideroblasts (Fujioka, 1997). Ethanol causes an increase in red blood cell size [mean corpuscular volume (MCV)], which reflects its effects on stem cells. If heavy drinking is accompanied by folic acid deficiency, there can also be hypersegmented neutrophils, reticulocytopenia, and a hyperplastic bone marrow; if malnutrition is present, sideroblastic changes can be observed. Chronic heavy drinking can decrease production of white blood cells, decrease granulocyte mobility and adherence, and impair delayed-hypersensitivity responses to novel antigens (with a possible false-negativetuberculin skin test). Associated immune deficiencies can contribute to vulnerability toward infections, including hepatitis and HIV, and interfere with their treatment. Finally, many alcoholics have mild thrombocytopenia, which usually resolves within a week of abstinence unless there is hepatic cirrhosis or congestive splenomegaly.
____________
Cardiovascular Diseases: Alcohol and heart:
Any advice about the consumption of alcohol must take into account not only the complex relation between alcohol and cardiovascular disease but also the well-known association of heavy consumption of alcohol with a large number of health risks. One approach would be to recommend no consumption of alcohol. However, a large number of recent observational studies have consistently demonstrated a reduction in coronary heart disease (CHD) with moderate consumption of alcohol. Any prohibition of alcohol would then deny such persons a potentially sizable health benefit. More than 100 prospective studies show an inverse association between moderate drinking and risk of heart attack, ischemic (clot-caused) stroke, peripheral vascular disease, sudden cardiac death, and death from all cardiovascular causes. The effect is fairly consistent, corresponding to a 25 percent to 40 percent reduction in risk.
_
Coronary Heart Disease (CHD):
Several large prospective studies have reported a reduced risk of death from CHD across a wide range of alcohol consumption levels. These include studies among men in the United Kingdom (Doll et al. 1994), Germany (Keil et al. 1997), Japan (Kitamura et al. 1998), and among more than 85,000 U.S. women enrolled in the Nurses’ Health Study (Fuchs et al. 1995). In research studies, definitions of moderate drinking vary. However, in these studies, most, if not all, of the apparent protective effect against CHD was realized at low to moderate levels of alcohol consumption. (In the last study cited above, for example, “light to moderate” drinking ranging from one to three drinks per week to one to two drinks per day was associated with a reduced risk of death from cardiovascular diseases.) Similarly, a meta-analysis that pooled data from 19 cohort studies and 6 case-control studies found that although the risk of death from CHD was reduced at all levels of alcohol consumption, the maximum reduction in risk occurred at low levels (English et al. 1995). Other studies also have shown that drinking more is not associated with any additional reduction in risk (Maclure 1993). An analysis of data from a 9-year follow-up of 490,000 Americans in the Cancer Prevention Study II (Thun et al. 1997) showed that, compared with abstainers, both men and women who consumed alcohol had a 30 to 40 percent lower risk of death from all cardiovascular diseases, with little relationship to the amount consumed. The reduced risk of death from CHD was especially marked among people at particular risk for cardiovascular diseases. In addition to a reduced risk of heart disease death, several large studies have found a decreased incidence (number of new cases) of CHD in people consuming alcohol at low to moderate levels. For example, an analysis of data from the 1988 National Health Interview Survey indicated that both men and women had a reduced risk of heart disease at lower levels of drinking (the risk increased at drinking levels above five drinks per day for men and two drinks per day for women) (Hanna et al. 1997).
_
Some researchers have argued that wine confers special protection against CHD (Goldberg et al. 1995). Others have concluded that any benefit alcoholic beverages in protecting against CHD is derived mostly or wholly from alcohol itself rather than from components of particular beverages (Doll 1997; Rimm et al. 1996). Laboratory studies as well as studies in humans have produced mixed results concerning the effects of wines in reducing the concentration of lipids, or fats, in the blood (Chadwick and Goode 1998; Goldberg et al. 1995) or in raising the blood levels of antioxidants—compounds that counter the effect of destructive by-products of metabolism (Puddey and Croft 1997). A study of Chinese men found no additional reduction in overall mortality associated with drinking rice-fermented wine (Yuan et al. 1997).
_
More than a dozen prospective studies have demonstrated a consistent, strong, dose-response relation between increasing alcohol consumption and decreasing incidence of CHD. The data are similar in men and women in a number of different geographic and ethnic groups. Consumption of one or two drinks per day is associated with a reduction in risk of approximately 30% to 50%. Studies of coronary narrowings defined by cardiac catheterization or autopsy show a reduction in atherosclerosis in persons who consume moderate amounts of alcohol. In general, the inverse association is independent of potential confounders, such as diet and cigarette smoking. Concerns that the association could be an artifact due to cessation of alcohol consumption in persons who already have CHD have largely been disproved. No clinical trials have been performed to test the alcohol-CHD relation. However, the large numbers of observational studies support a true protective effect of moderate consumption of alcohol.
_
Mechanisms for Cardioprotective Effects of Moderate Consumption of Alcohol:
Recent analyses suggest that approximately 50% of the protective effect of alcohol is mediated through increased levels of HDL cholesterol. HDL removes cholesterol from the arterial wall and transports it back to the liver and probably has several other protective effects on the arterial system. A number of epidemiological studies and small clinical trials have demonstrated that moderate consumption of alcohol raises HDL cholesterol levels. When HDL cholesterol was added to computer models predictive of CHD, about half the benefit of alcohol in protecting against CHD could be attributed to its effect on HDL levels. A number of other mechanisms have been proposed to explain the other half of the protective effect of alcohol against CHD. One or two alcoholic drinks per day apparently do not affect other major risk factors, such as LDL cholesterol and blood pressure. Several studies have suggested that alcohol may affect blood clotting, either by causing the blood to clot less avidly through effects on coagulation factors and platelets or by enhancing the ability of the blood to break up clots when they form. These studies are supported by epidemiological data that suggest that acute alcohol consumption causes a short-term beneficial effect in protection against CHD in addition to long-term effects. Other studies have focused on the nonalcoholic components of alcoholic beverages, particularly in red wine and dark beer, which may have antioxidant properties. However, the epidemiological evidence favoring one type of beverage over another is inconsistent, possibly because of large differences in diet, smoking, and other risk behaviors among drinkers. Again, at least half of the inverse association between alcohol and CHD appears to be directly linked to alcohol through increased HDL cholesterol levels. The potential benefit of moderate drinking on lipids appears to be more important in patients with a higher risk profile, such as men with metabolic syndrome. Heavy alcohol consumption, on the other hand, will lead to loss of the beneficial effect with worsening of the metabolic syndrome and elevation in plasma homocysteine levels. Thus, drinking in moderation is beneficial to serum lipid levels and decreases risk of cardiovascular mortality, whereas excessive drinking exerts the opposite effect.
_
Alcohol and Markers of Inflammation:
Imhof et al studied a random cross-sectional sample of ≈8000 men and women representative of the general population of 3 European countries: Germany, Scotland, and France. The study population represented largely moderate consumers of a variety of alcoholic drinks including beer, wine, and spirits. Overall, the group representing moderate alcohol consumers exhibited lower levels of white blood cell counts and inflammatory markers including fibrinogen and C-reactive protein compared with nondrinkers and heavy drinkers, after adjustment for potential confounders. Maraldi et al followed 2487 subjects without known history of heart disease for 5.6 years. Patients classified as mild drinkers, defined by 1 to 7 drinks per week, had a significant reduction in all-cause mortality. This benefit was more marked among men with high baseline interleukin-6, a proinflammatory cytokine. Thus, mild alcohol consumption decreases inflammatory markers in the subjects, and this seems to be an important mechanism related to the beneficial effects of alcohol.
_
The moderate consumption of alcohol promotes good heart health in a number of ways, including the following:
- Alcohol improves blood lipid profile
- It increases HDL (“good”) cholesterol
- It decreases LDL (“bad”) cholesterol
- It improves cholesterol (both HDL and LDL) particle size
- Alcohol decreases thrombosis (blood clotting)
- It reduces platelet aggregation
- It reduces fibrinogen (a blood clotter)
- It increases fibrinolysis (the process by which clots dissolve)
- Alcohol acts in additional ways
- It reduces coronary artery spasm in response to stress
- It increases coronary blood flow
- It reduces blood insulin level
- It increases estrogen levels
_
Effect of alcohol consumption on biological markers associated with risk of coronary heart disease: systematic review and meta-analysis of interventional studies:
Of 63 eligible studies, 44 on 13 biomarkers were meta-analyzed in fixed or random effects models. Quality was assessed by sensitivity analysis of studies grouped by design. Analyses were stratified by type of beverage (wine, beer, spirits). Alcohol significantly increased levels of high density lipoprotein cholesterol (pooled mean difference 0.094 mmol/L, 95% confidence interval 0.064 to 0.123), apolipoprotein A1 (0.101 g/L, 0.073 to 0.129), and adiponectin (0.56 mg/L, 0.39 to 0.72). Alcohol showed a dose-response relation with high density lipoprotein cholesterol (test for trend P=0.013). Alcohol decreased fibrinogen levels (−0.20 g/L, −0.29 to −0.11) but did not affect triglyceride levels. Results were similar for crossover and before and after studies, and across beverage types. Favourable changes in several cardiovascular biomarkers (higher levels of high density lipoprotein cholesterol and adiponectin and lower levels of fibrinogen) provide indirect pathophysiological support for a protective effect of moderate alcohol use on coronary heart disease.
_
On one hand, alcohol reduces risk of CHD; on the other hand, it increases risk of cardiac arrhythmias and cardiomyopathy:
_
Holiday heart syndrome and sudden cardiac death:
Cardiac arrhythmias refer to an alteration in the rhythm of the heartbeat. Such alterations lead to fluctuations in the supply of blood to the body and brain, thus potentially affecting the function of these organs. Cardiac arrhythmias have been observed after both acute intake of large amounts of ethanol and after chronic alcohol consumption. For example, ethanol intake over a long weekend may result in electrophysiological anomalies referred to as “holiday heart syndrome”, whereas sudden cardiac death has been associated with alcoholism (Zakhari, 1997). A number of hypotheses have been advanced to explain the disturbances in cardiac rhythms. These include scaring of the heart muscle, alterations in the chemicals, which influence heart function such as electrolytes and catecholamines, and alterations in the amount of oxygen coming to the heart.
_
New UCSF Research examines Causal Link between Alcohol Consumption and Atrial Fibrillation:
The term “holiday heart syndrome” was coined in a 1978 study to describe patients with atrial fibrillation who experienced a common and potentially dangerous form of heart palpitation after excessive drinking, which can be common during the winter holiday season. The symptoms usually went away when the revelers stopped drinking. Now, research from UCSF builds on that finding, establishing a stronger causal link between alcohol consumption and serious palpitations in patients with atrial fibrillation, the UCSF researchers report that people with atrial fibrillation had almost a four and a half times greater chance of having an episode if they were consuming alcohol than if they were not.
_
Effect of ethanol on cardiac single sodium channel gating:
Alcohol in modest and higher doses has the potential to induce cardiac arrhythmias. The most famous alcohol-related arrhythmia is the holiday heart syndrome. Furthermore, there is a clear association between excessive alcohol consumption and the risk of sudden cardiac death. However, the acute effects of ethanol on arrhythmia induction are not well understood. The effect of ethanol on single cardiac sodium channels has not been studied yet. To elucidate the effect of ethanol on human cardiac sodium channels authors performed a patch clamp study in HEK-293 cells overexpressing the human cardiac sodium channel. They used HEK-293 cells overexpressing the human cardiac sodium channel (Na1.5). Single channel gating was investigated by the cell-attached patch clamp technique. Sodium channel currents were elicited by depolarizing pulses from −120 to −20 mV for a duration of 150ms. Single channel availability, open probability and peak average current were assessed baseline and after addition of ethanol in increasing concentrations 10.9mM (0.05 %), 21.7mM (1%), 43.5mM (2%) and 87.0mM (4%). They found a concentration-dependent reduction of open probability which was statistically significant at 2.00 % ethanol (66.5±14% of control). At higher concentrations (4.00 %) also availability decreased to 66.5±11.0% of control. This resulted in a significant decrease of peak average current at 2.00 % and at 4.00 % ethanol (61.8±7.4 and 53.0±8.2% of control). For the first time the present study demonstrates acute inhibitory effects of ethanol on single cardiac sodium channel gating and provides one potential mechanism for the well known clinical observation that ethanol triggers supraventricular and ventricular arrhythmias.
_
Alcoholic cardiomyopathy:
Long-term excess alcohol consumption is a leading cause of secondary, nonischemic dilated cardiomyopathy. However, recovery of cardiac function can occur if the disease is diagnosed early and further alcohol intake is reduced or halted. Alcoholic cardiomyopathy is a type of dilated cardiomyopathy. Due to the direct toxic effects of alcohol on heart muscle, the heart is unable to pump blood efficiently, leading to heart failure. It can affect other parts of the body if the heart failure is severe. It is most common in males between the ages of 35-50.
_
The alcohol heart debate:
The American Heart Association has reported that “More than a dozen prospective studies have demonstrated a consistent, strong, dose-response relation between increasing alcohol consumption and decreasing incidence of CHD (coronary heart disease). The data are similar in men and women in a number of different geographic and ethnic groups. Consumption of one or two drinks per day is associated with a reduction in risk of approximately 30% to 50%”. Heart disease is the largest cause of mortality in the United States and many other countries. Therefore, some physicians have suggested that patients be informed of the potential health benefits of drinking alcohol in moderation, especially if they abstain and alcohol is not contraindicated. Others, however, argue against the practice in fear that it might lead to heavy or abusive alcohol consumption. Heavy drinking is associated with a number of health and safety problems.
_
Debate over research methods:
Ex-drinkers versus never-drinkers:
A logical possibility is that some of the alcohol abstainers in research studies previously drank excessively and had undermined their health, thus explaining their high levels of risk. To test this hypothesis, some studies have excluded all but those who had avoided alcohol for their entire lives. The conclusion remained the same in some studies: moderate drinkers are less likely to suffer heart disease. On the other hand, an analysis by Dr. Kaye Fillmore and colleagues failed to find significant support. Analyzing 54 prospective studies, the authors found that those studies which were free of the potential error (including former drinkers in the abstaining group) did not demonstrate significant cardiac protection from alcohol, although they continued to exhibit a J-shaped relationship in which moderate drinkers were less likely (but not at a statistically significantly level of confidence) to suffer cardiac disease than lifelong abstainers. Dr. Arthur Klatsky noted that the flaw pointed out by Fillmore existed in one of his early studies of alcohol consumption, but that his later studies illustrating a protective effect of moderate alcohol consumption did not contain this flaw. To overcome the inherent weaknesses of all epidemiological studies, even when properly conducted, he calls for a randomized trial in which some subjects are assigned to abstain while others are assigned to drink alcohol in moderation and the health of all is monitored for a period of years. This question of confusion of abstainers with previously heavy drinkers in epidemiologic studies is overcome with studies showing dose response effects. That is, higher amounts of alcohol consumption seem associated with greater cardiovascular benefit.
Studies on possible confounding effects:
Some have suggested the cardioprotective effects of alcohol consumption could be explained by confounding variables. For example moderate drinkers might have more healthful lifestyles, higher economic status, better dietary habits, better healthcare, or higher educational levels, etc. However, when these and other factors are considered, the cardioprotective effects of alcohol are still evident.
Confirmation of Cardioprotection:
Multiple studies on moderate alcohol consumption have now reconfirmed earlier suspected cardioprotection findings. A 2006 study concluded, “Even in men already at low risk on the basis of body mass index, physical activity, smoking, and diet, moderate alcohol intake is associated with lower risk for MI [myocardial infarction]. Another study found that when men increased their alcohol intake from very low to moderate, they significantly reduced their risk of coronary heart disease. The study monitored the health of 18,455 males for a period of seven years.A multicenter randomized diet study published in 2013 included over 7000 persons at risk to develop cardiovascular disease, and found that a Mediterranean-diet, including an encouragement to daily wine consumption in habitual drinkers, led to decreased cardiovascular events by about 30%. The study was halted prematurely since the health benefits were so dramatic.
_
More than half a dozen very large long-term studies have linked moderate alcohol consumption to a reduced risk of suffering a heart attack and dying of coronary heart disease. While most of the studies involved men or mostly men, a recent report from the continuing Nurses’ Health Study of 89,000 middle-aged women at the Harvard School of Public Health found that women who typically consumed three to nine drinks a week were 40 percent less likely to develop heart disease than nondrinkers. A report from a 10-year study of nearly 130,000 men and women by researchers at the Kaiser Permanente Medical Center in Oakland, Calif., found that people who typically consumed one or two drinks a day were 30 percent less likely to die from coronary heart disease than people who abstained from alcohol. And then came the so-called French paradox: the apparent fact that despite a diet rich in animal fats, the French seem to be spared Americans’ epidemic rates of heart disease. The French penchant for wine, particularly red wine, was singled out as the likely protector against saturated fats and cholesterol. Researchers at Cornell University and the University of California at Davis quickly isolated from red wine substances called phenolic flavonoids, which they say act as antioxidants, preventing LDL cholesterol from clogging coronary arteries. Another Kaiser Permanente researcher, Dr. Arthur Klatsky, reported that white wine appeared to be equally beneficial, based on coronary rates among the 82,000 people in the study who drank various kinds of alcoholic beverages. In fact, Dr. Klatsky said in reviewing the various large studies, benefits to the heart have been seen not just from wine but also from beer and hard liquor. In addition, the Framingham Heart Study, among others, has linked alcohol consumption to an increase in the protective HDL cholesterol, which acts like arterial Drano, cleaning out accumulated fatty deposits. Alcohol also seems to have an anticlotting effect, accounting for a related benefit in moderate drinkers: a reduced risk of stroke.
_
The National Institute on Alcohol Abuse and Alcoholism found that moderate drinking is beneficial to heart health, resulting in a sharp decrease in heart disease risk (40%-60%). This is important because cardiovascular disease is the number one cause of death in the United States and heart disease kills about one million Americans each and every year. The Director of the National Institute on Alcohol Abuse and Alcoholism wrote that “Numerous well-designed studies have concluded that moderate drinking is associated with improved cardiovascular health,” and the Nutrition Committee of the American Heart Association reported that “The lowest mortality occurs in those who consume one or two drinks per day. A World Health Organization Technical Committee on Cardiovascular Disease asserted that the relationship between moderate alcohol consumption and reduced death from heart disease can no longer be doubted.
1. Researchers studied volunteers in seven European countries and found that people who have a daily drink of beer, wine or distilled spirits (whiskey, rum, tequila, etc.) have significantly better arterial elasticity, a strong indicator of heart health and cardiovascular health, than nondrinkers. Moderate drinkers also had significantly better pulse rates than those of abstainers from
2. A study of 1,795 subjects found that the risk of extensive coronary calcification was 50% lower in individuals who consumed one to two alcoholic drinks per day than in nondrinkers.
3. Research demonstrates that moderate alcohol consumption is associated with better endothelial function, which contributes to better heart health and lowers risk of atherosclerosis and cardiovascular disease.
4. A study of over 3,000 men and women found that those who never drank alcohol were at a greater risk of having high levels of CRP and IL-6 (excellent predictors of heart attack) than were those who consumed alcoholic beverages in moderation.
5. A National Institute on Alcohol Abuse and Alcoholism review of research studies from at least 20 countries around the world demonstrate a 20- to 40-percent lower coronary heart disease (CHD) incidence among drinkers compared to nondrinkers. It asserts that “The totality of evidence on moderate alcohol and CHD supports a judgment of a cause-effect relationship… there are cardioprotective benefits associated with responsible, moderate alcohol intake.
6. Harvard researchers have identified the moderate consumption of alcohol as a proven way to reduce coronary heart disease risk.
7. A study of 18,455 males from the Physicians Health Study revealed that those originally consuming one drink per week or less who increased their consumption up to six drinks per week had a 29% reduction in CVD risk compared to those who did not increase their consumption. Men originally consuming 1-6 drinks per week who increased their consumption moderately had an additional 15% decrease in CVD risk.
8. The Harvard Health Professionals Follow-Up Study of over 44,000 men found moderate alcohol consumption to be associated with a 37% reduction in coronary disease.
9. A British study of women found moderate consumption of alcohol to be associated with lower levels of cardiovascular risk factors.
10. A study of over 5,000 women with type 2 diabetes mellitus found that coronary heart disease rates “were significantly lower in women who reported moderate alcohol intake than in those who reported drinking no alcohol.” Women who drank more than 5 grams (about one-third glass) a day reduced their risk of CHD (fatal or nonfatal) by more than half.
11. In a study of nearly 88,000 men, researchers found that drinking reduced risk of coronary heart disease risk among both diabetics and non-diabetics. Weekly consumption of alcohol reduced CHD risk by one-third (33%) while daily consumption reduced the risk by over half (58%) among diabetics. For non-diabetics, weekly consumption reduced CHD risk by 18% while daily consumption reduced the risk by 39%.
12. Light to moderate consumption of alcohol appears to reduce the risk of coronary heart disease by as much as 80% among individuals with older-onset diabetes, according to a study published in the Journal of the American Medical Association.
13. The Honolulu Heart Study found a 49% reduction in coronary heart disease among men who drank alcohol in moderation.
14. Harvard researchers concluded about coronary heart disease that Consumption of one or two drinks of beer, wine, or liquor per day has corresponded to a reduction in risk of approximately 20-40%.
15. At a scientific conference, researchers from Korea, Italy, Germany, Poland, the Netherlands, and the United States reported finding striking reductions in death among moderate drinkers, with heart disease and total mortality rates about one half or less compared to non-drinkers.
16. After over 6,000 participants in the Framingham Heart Study were followed for a period of six to ten years, researchers found that “when consumed in moderation, alcohol appears to protect against congestive heart failure.
17. The American Heart Association, based on the research evidence, concludes that the Consumption of one or two drinks per day is associated with a [CHD] reduction in risk of approximately 30% to 50%.
18. After reviewing the research, Dr. David Whitten reported that the studies that have been done show pretty clearly that the chances of suffering cardiac death are dramatically reduced by drinking one or two drinks a day and asserted that we don’t have any drugs that are as good as alcohol.
19. Based on the medical evidence, noted investigator Dr. Curtis Ellison asserted that abstinence from alcohol is a major risk factor for coronary heart disease.
_
Association of alcohol consumption with selected cardiovascular disease outcomes: a systematic review and meta-analysis: BMJ-2011:
In this review of 84 studies of alcohol consumption and cardiovascular disease, alcohol consumption at 2.5–14.9 g/day (about ≤1 drink a day) was consistently associated with a 14–25% reduction in the risk of all outcomes assessed compared with abstaining from alcohol. Such a reduction in risk is potentially of clinical importance, but consumption of larger amounts of alcohol was associated with higher risks for stroke incidence and mortality. This review clarifies several discrepancies among prior reports. Corrao et al reported a J shaped relation between alcohol intake and coronary heart disease, whereas the review by Maclure described this relation as L shaped because he did not observe an increase in coronary heart disease risk associated with higher alcohol consumption. This updated meta-analysis supports the latter association for coronary heart disease, with a 25–35% risk reduction for light to moderate drinking that also is present with heavier drinking.
_
The Moderate Consumption of Alcohol increases the Survivability of Heart Attacks:
1. Drinking alcohol in moderation throughout the year before a heart attack or acute myocardial infarction (AMI) has been found to reduce the risk of dying afterward. Moderate drinkers had the lowest mortality rate, reducing their risk by 32%, compared to abstainers. The health benefits were virtually identical for beer, distilled spirits, and wine.
2. Men who consume two to four drinks of alcohol after a heart attack are less likely to experience a second heart attack than are abstainers, according to a study of 353 male heart attack survivors. Researchers found that men who consumed an average of two drinks of alcohol per day were 59% less likely than non-drinkers to have another heart attack. Those who drank an average of four drinks per day experienced a risk reduction of 52% compared to abstainers.
3. Research at the University of Missouri-Columbia found that drinking alcohol (beer, wine, or distilled spirits) in moderation reduced the damage to effected tissue following a heart attack.
4. A study for a five year period of over 85,000 men who had suffered previous heart attacks found that “moderate alcohol intake was associated with a significant decrease in total mortality” compared to nondrinkers.
_
Alcohol Abstainers who begin Drinking reduce their risk of Cardiovascular Disease:
During a ten year study of 7,697 non-drinkers, investigators found that 6% began consuming alcohol in moderation. After four years of follow-up, new moderate drinkers had a 38% lower chance of developing cardiovascular disease than did those who continued abstaining. Even after adjusting for physical activity, Body Mass Index (BMI), demographic and cardiac risk factors, this difference persisted.
_
A contrary study:
Impact of alcohol on coronary heart disease in Indian men:
Authors did not observe an inverse (protective) association between alcohol intake and the prevalence of CHD. In contrast, their study indicated an association in the reverse direction, suggesting possible harm of alcohol for coronary risk in Indian men. This relationship needs to be further examined in large, prospective study.
_
Alcohol and Cardiovascular Health: The Razor-Sharp Double-Edged Sword:
An extensive body of data shows concordant J-shaped associations between alcohol intake and a variety of adverse health outcomes, including coronary heart disease, diabetes, hypertension, congestive heart failure, stroke, dementia, Raynaud’s phenomenon, and all-cause mortality. Light to moderate alcohol consumption (up to 1 drink daily for women and 1 or 2 drinks daily for men) is associated with cardioprotective benefits, whereas increasingly excessive consumption results in proportional worsening of outcomes. Alcohol consumption confers cardiovascular protection predominately through improvements in insulin sensitivity and high-density lipoprotein cholesterol. The ethanol itself, rather than specific components of various alcoholic beverages, appears to be the major factor in conferring health benefits. Low-dose daily alcohol is associated with better health than less frequent consumption. Binge drinking, even among otherwise light drinkers, increases cardiovascular events and mortality. Alcohol should not be universally prescribed for health enhancement to nondrinking individuals owing to the lack of randomized outcome data and the potential for problem drinking.
_
If you drink alcohol, do so in moderation. This means an average of one to two drinks per day for men and one drink per day for women. (A drink is one 12 oz. beer, 4 oz. of wine, 1.5 oz. of 80-proof spirits, or 1 oz. of 100-proof spirits.) Drinking more alcohol increases such dangers as alcoholism, high blood pressure, obesity, stroke, breast cancer, suicide and accidents. Also, it’s not possible to predict in which people alcoholism will become a problem. Given these and other risks, the American Heart Association cautions people NOT to start drinking … if they do not already drink alcohol. Consult your doctor on the benefits and risks of consuming alcohol in moderation. Drinking too much alcohol can raise the levels of some fats in the blood (triglycerides). It can also lead to high blood pressure, heart failure and an increased calorie intake. (Consuming too many calories can lead to obesity and a higher risk of developing diabetes.) Excessive drinking and binge drinking can lead to stroke. Other serious problems include fetal alcohol syndrome, cardiomyopathy, cardiac arrhythmia and sudden cardiac death.
_
Over the past several decades, many studies have been published in science journals about how drinking alcohol may be associated with reduced mortality due to heart disease in some populations. Some researchers have suggested that the benefit may be due to wine, especially red wine. Others are examining the potential benefits of components in red wine such as flavonoids and other antioxidants in reducing heart disease risk. Some of these components may be found in other foods such as grapes or red grape juice. The linkage reported in many of these studies may be due to other lifestyle factors rather than alcohol. Such factors may include increased physical activity and a diet high in fruits and vegetables and lower in saturated fats No direct comparison trials have been done to determine the specific effect of wine or other alcohol on the risk of developing heart disease or stroke.
_
Research is being done to find out what the apparent benefits of drinking wine or alcohol in some populations may be due to, including the role of antioxidants, an increase in HDL (“good”) cholesterol or anti-clotting properties. Clinical trials of other antioxidants such as vitamin E have not shown any cardio-protective effect. Also, even if they were protective, antioxidants can be obtained from many fruits and vegetables, including red grape juice. The best-known effect of alcohol is a small increase in HDL cholesterol. However, regular physical activity is another effective way to raise HDL cholesterol, and niacin can be prescribed to raise it to a greater degree. Alcohol or some substances such as resveratrol found in alcoholic beverages may prevent platelets in the blood from sticking together. That may reduce clot formation and reduce the risk of heart attack or stroke. (Aspirin may help reduce blood clotting in a similar way.) How alcohol or wine affects cardiovascular risk merits further research, but right now the American Heart Association does not recommend drinking wine or any other form of alcohol to gain these potential benefits. The AHA does recommend that to reduce your risk you should talk to your doctor about lowering your cholesterol and lowering high blood pressure, controlling your weight, getting enough physical activity and following a healthy diet. There is no scientific proof that drinking wine or any other alcoholic beverage can replace these conventional measures.
_
Does Alcohol truly prevent coronary heart disease?
Although the evidence of a lower risk of coronary heart disease among moderate drinkers is substantial and consistent, controversy remains about whether the relationship is truly causal-that is, whether moderate alcohol consumption really prevents coronary heart disease. For example, some investigators have argued that abstainers are an inappropriate control population because at least some of these people may abstain because of illness or former alcohol abuse. Furthermore, other dietary, lifestyle, and developmental factors may differ between abstainers and drinkers. Both of these concerns warrant closer scrutiny. The first of these concerns, also called the “sick quitter” hypothesis, was proposed by Shaper and colleagues (1988) in the United Kingdom. It states that the pool of abstainers includes many former drinkers who quit drinking because of illness or because alcohol interacts with prescription drugs they are taking. Obviously, comparisons of healthy drinkers with abstainers who take prescription drugs or who have underlying illnesses that raise one’s risk for heart disease will produce a biased result in favor of the alcohol-consuming subjects. Similarly, alcoholic patients in recovery rarely return to moderate, or social, drinking. Thus, people who have alcoholism, whether still active or in remission, will tend toward the extremes of alcohol consumption (i.e., abstention or heavy drinking). People with active alcoholism, however, tend to be underrepresented in large, prospective studies of heart disease. As a result, comparison of drinkers (who underrepresent active alcohol abusers) to abstainers (who include recovering alcoholics) may produce misleading results if heavy alcohol consumption contributes to a higher risk of heart disease. A similar bias may occur if, in self-report surveys, people who consume alcohol in excess deliberately describe themselves as abstainers because of the social stigma attached to alcohol abuse. Other fundamental differences also exist between abstainers and drinkers. For example, abstainers tend to come from less welcoming childhood environments (The term “less welcoming” in this instance refers to the degree of parental warmth and cohesion in a child’s life as measured on a “Childhood Environmental Strengths Scale” administered by trained psychological interviewers.) and to report poorer health than do drinkers, even in early adulthood (Vaillant 1995). Moreover, many abstainers have chosen to forsake alcohol intake because of adverse experiences with alcoholic family members. Such differences, which might influence a person’s underlying risk of heart disease, are difficult to account for with standard epidemiological or statistical methods. Finally, the level of alcohol consumption is a marker for several lifestyle factors that strongly influence health (Fillmore et al. 1998). Moderate drinkers tend to be younger, leaner, more physical active, of higher socioeconomic status, and more likely to be married compared with people who abstain or drink rarely. All of these factors have been shown to influence one’s risk of coronary heart disease.
Approaches for Accounting for Potential Confounding Factors:
Researchers have sought to address these concerns in several ways. Some epidemiological studies have separated former drinkers from long-term abstainers to address the sick quitter hypothesis. For example, in an analysis of 87,526 women, the risk of coronary heart disease was only 10 percent higher among former drinkers than among long-term abstainers (Stampfer et al. 1988). Furthermore, the exclusion of former drinkers among the abstainers did not alter the 40 percent lower risk of coronary heart disease among women who drank 5.0–14.9 grams of alcohol (about 0.3–1 standard drinks) daily. Moreover, Rimm and colleagues (1991) found comparable risks of coronary heart disease among abstainers and light drinkers (i.e., people who consumed less than 5.0 grams of alcohol, or 0.3 standard drinks, daily) in their study of 51,529 healthy men, suggesting that abstainers are not an inappropriate reference group. Other studies have excluded participants who developed coronary heart disease or died during the first few years of follow up, as a means of excluding unidentified “sick” subjects, with similar results (Fuchs et al. 1995). Taken together these findings indicate that the presence of sick quitters or former alcoholics among the abstainers is not responsible for the apparent benefits of alcohol consumption on the risk of coronary heart disease. Researchers also have sought to separate the confounding influence of dietary, lifestyle, and socioeconomic factors from the role of alcohol consumption itself. In the separate prospective studies of men and women noted earlier (Rimm et al. 1991; Stampfer et al. 1988), researchers controlled for the participants’ body-mass index (a measure of obesity) and dietary intake of cholesterol, saturated fat, and polyunsaturated fat. These analyses confirmed that diet alone is unlikely to have caused the apparent effect of alcohol consumption on heart disease. Studies that have controlled for the participants’ social integration, social class, physical activity, or occupation have reported similar results (Murray et al. 1999). Another area of controversy remains the role of the type of beverage a drinker consumes preferentially. The French paradox-the observation that the rate of coronary heart disease in France is relatively low despite high rates of saturated fat intake and cigarette smoking-has led to the belief that red wine is particularly beneficial for health. This specific effect has been suggested to result from the antioxidant properties of some components of red wine rather than its alcohol content. However, observational studies have not consistently shown a difference in the risk of heart disease between wine drinkers and consumers of other alcoholic beverages (Rimm et al. 1996). In summary, all of this evidence implicates alcohol consumption rather than lifestyle factors (including those that correlate with the consumption of specific beverage types) as the primary factor in the lower rates of cardiovascular disease found among moderate drinkers.
_
The role of genetic factors in the association of alcohol and heart disease:
One unresolved question is whether the relationship of alcohol consumption to heart disease is consistent throughout the general population or differs among certain subgroups (e.g., men and women). For example, because men and women differ in how they metabolize alcohol and in their underlying risk of cardiovascular disease, they may also differ in how alcohol consumption relates to their risk of heart disease. Such variability is difficult to assess in randomized trials of alcohol consumption, which have been too small to allow subgroup comparisons. Observational studies, however, provide some intriguing answers to this question. For example, the studies of healthy men (Rimm et al. 1991) and women (Stampfer et al. 1988) mentioned previously suggest that moderate drinking is associated with lower risk of heart disease in both sexes, despite the differences in alcohol metabolism and risk of cardiovascular disease. These studies also demonstrate, however, that the level of alcohol consumption associated with the lowest risk of heart disease is lower among women than among men, consistent with public health recommendations that advise consumption of no more than two drinks per day for men and no more than one drink per day for nonpregnant women. Genetic factors may also modify the relationship between moderate drinking and coronary heart disease in interesting ways. For example, the initial breakdown of the alcohol contained in alcoholic beverages-chemically referred to as ethanol-is mediated by an enzyme called alcohol dehydrogenase (ADH). Three different versions of ADH exist-ADH1, ADH2, and ADH3. Of these, ADH3 has two common genetic variants, or alleles, that break down ethanol at different speeds (i.e., fast and slow). Each person carries two copies of the ADH3 gene, one inherited from the father and one inherited from the mother. Accordingly, a person can carry either two fast alleles, two slow alleles, or one fast and one slow allele of the ADH3 gene. A recent study of 396 men with myocardial infarction and 770 control men studied the relationship between these ADH3 alleles and the risk of heart disease (Hines et al. 2001). The study found that compared with men who carried two copies of the fast allele and drank less than once per week, men who carried two copies of the fast allele and drank daily had a 38 percent lower risk of myocardial infarction. In contrast, daily drinkers who had two copies of the slow allele had an 86 percent lower risk of myocardial infarction compared with men with two slow alleles who drank less than weekly. These results suggest that, within the range of moderate drinking, greater exposure time to alcohol (on the basis of more frequent drinking and slower metabolism), may lower one’s risk of myocardial infarction. The researchers also found that among daily drinkers, “good” HDL-C cholesterol increased with the number of slow ADH3 alleles-that is, daily drinkers with two slow ADH3 alleles had higher HDL-C levels than did daily drinkers with no slow ADH3 allele levels; men with one slow allele had intermediate HDL-C levels. This finding provides a plausible explanation for the gene-related variation in the relationship between alcohol consumption and risk of myocardial infarction described in the study. Danish investigators reported intriguing findings in a study of 3,383 men (Hein et al. 1993). The investigators compared the risk of cardiovascular mortality among men with different Lewis blood group types. Much like the common ABO blood group system, a person’s Lewis blood type can include just an “a” component (a+b-), just a “b” component (a-b+), both components (a+b+), or neither component (AB). People with the AB blood type seem to be at higher risk for diabetes and cardiovascular mortality than people with other Lewis blood types. In the study, men with Lewis blood group type AB who consumed 22 or more drinks per week had an 80 percent lower risk of coronary heart disease than did men who consumed 0–10 drinks per week. Among men with other Lewis blood group types, however, alcohol consumption was not appreciably related to the risk of heart disease. Taken together, these two studies suggest that genetic factors that influence potentially beneficial variables linked to alcohol use (e.g., HDL-C levels) or the baseline risk of heart disease (e.g., Lewis blood type groups) may modify the link between alcohol consumption and heart disease in important and informative ways.
_
Is it overestimation?
The much-publicized beneficial effects of light to moderate alcohol consumption may have been vastly overestimated.
Epidemiologists, cardiologists, public health experts and sociologists at a Novartis Foundation Symposium on Alcohol and Cardiovascular Disease expressed concern that the ‘J-shaped’ alcohol-consumption/coronary-heart disease- risk curve for the over 50s could be explained largely in terms of inappropriate questionnaires, misleading classifications and poor statistical analysis. The relation between alcohol and total mortality depends on the distribution of causes of death amongst the population studied and on the level and patterns of alcohol consumption within the population. The most consistent observation is that, in industrialized countries, non-drinkers (ex-drinkers and lifelong teetotalers) have higher rates of all-cause morbidity and mortality than light/ moderate drinkers. However, having seen little evidence that light-drinkers owe their good health to alcohol, researchers are beginning to wonder whether drinking habits are a reflection of other, more powerful, risk factors such as social class, education and general ill-health. Despite the overwhelming consensus that, beyond a certain age, alcohol consumption of 5-20g/day attenuates the risk of major coronary heart disease (CHD) events, the degree of protection has almost certainly been exaggerated by use of inappropriate control groups said Professor Gerry Shaper (Royal Free Hospital, London). Shaper’s work on the British Regional Heart Study (a longitudinal study of over 7000 men), whose detailed meta-analysis of six other large-scale surveys has revealed that the J-shape could result largely from two factors that make non-drinkers a seriously biased baseline group. First, there is a strong downward drift from heavy or moderate drinking towards non-drinking as people get older associated with declining health; secondly, nondrinkers (like heavy drinkers) are usually working class, of limited education and in poorer health than regular light drinkers who are the healthiest, wealthiest and fittest group of all. Taking all this into consideration Shaper concludes that the alcohol induced reductions in CHD we are talking about are in the region of 1-3 fewer heart attacks per 1000 person years. A minuscule benefit then, and at what cost? For individuals under 50 years of age 20 g of alcohol per day increases all-cause mortality by 15-20%; or, as Dr Peter Anderson of the World Health Organization put it, ‘to talk about alcohol as though it were some new prophylactic drug is ridiculous and dangerous. In a clinical trial it would fall at the first fence: it’s addictive, it impairs neurological function, and it increases the risk of violent death, suicide, hypertension, haemorrhagic stroke, cirrhosis, and many cancers and causes huge social problems. Already one-third of men, and one in ten women, in Europe drink more than 20 g per day. In the developed world alcohol is responsible for 3% of all deaths and for 7% of all potential life-years lost. Given that there is a vast panoply of very effective and under-used cardiovascular drugs and that the beneficial effects of alcohol are small and ill-understood, all those present at the Novartis Foundation meeting concurred that global recommendations such as ‘1-3 drinks per day are good for you’ are not only meaningless but also irresponsible. Michael Gaziano (Harvard Medical School), who works on alcohol’s impressive ability to raise high density lipoprotein and thus reduce CHD risk by reverse cholesterol transport, was nonetheless enthusiastic: ‘Even if the size of this effect is less than anticipated it could have real implications for society as a whole’. He conceded that, in terms of being able to make recommendations, researchers know about as much about alcohol as they did about cholesterol 40 years ago. What we need now, if we are to secure information relevant to healthcare, are more large-scale, tailor-made epidemiological studies with frequent cycles involving all age groups and using modem interviewing techniques. Considering that in some studies almost twice as much alcohol is sold as people admit to consuming, there is also a crying need for a non-invasive blood alcohol marker to winkle out the truth about how much is really drunk. Until then, the public health message should be that, whatever the effects of light drinking, heavy drinking is bad for you.
_
Alcohol and the Heart: need for large randomized controlled trial (RCT):
Although numerous studies have described a J-shaped or U-shaped curve to describe the relationship between alcohol intake versus total mortality and cardiovascular mortality, these studies have all been observational and epidemiological in nature. Most reviews warn of not prescribing alcohol for those who do not drink. However, a large, multicenter, prospective, randomized study in which 1 group of patients receives alcohol long term versus another has not been done because of ethical, behavioral, and logistic challenges. Is this really the correct approach? The observational data collected thus far appear consistent that light to moderate alcohol has a cardiovascular benefit even when corrected for confounding factors, and 0.5 to 1 drink per day appears protective. Perhaps the time has arrived for a long-term prospective, randomized trial in which 1 group of people abstain totally and a second group receives 1 glass of alcohol, perhaps in the form of red wine, per day (or perhaps every other day). The patients are then followed long term for total mortality, cardiovascular events (including cardiovascular death, nonfatal myocardial infarction, development of angina, congestive heart failure), cerebrovascular events, and noncardiovascular/noncerebrovascular disease. Obviously, inclusion and exclusion criteria will need to be strict and probably complex. Former alcohol abusers, those with liver disease, and those with esophagitis, gastrointestinal ulcers, or bleeding should not be included. The patient cohort must be very compliant; liver function tests would need to be performed, and clinical monitoring would need to be of the highest quality. Methods would be needed to ensure that the control group had not started drinking. On the other hand, perhaps such a trial should not be very restricted and have broad inclusion criteria so as to be applicable to the types of patients usually seen by physicians, including the very elderly, diabetics, and those patients on various medicines. Any randomized controlled study would need to be large, on the order of at least ≈7500 patients, and would need to be conducted over at least ≈4 years. However, in a prospective trial, if 1 glass of wine per day could reduce mortality by the same 17% to 18% suggested in a recent meta-analysis, these data would provide strong evidence that a glass of wine per day is a major and cost-effective therapeutic intervention. Until large, prospective, randomized trials are available, the preponderance of data suggests that drinking 1 to 2 drinks in men and 1 in women will benefit the cardiovascular system. However, this statement is tempered by the observation in a large study of an increase in breast cancer among women who drank.
_
Two scientific camps:
Only a decade ago most alcohol researchers believed low to moderate drinking could help protect us against heart disease, type 2 diabetes and some strokes. This was because of observational studies that followed people over time and showed those who reported drinking at low to moderate levels seemed to get less heart disease, strokes and diabetes than people who didn’t drink at all. In fact moderate drinkers seemed to die later from any cause. But the ability of these types of studies to prove that a reduced risk of disease is caused by a person’s level of drinking is really limited. Indeed since around 2005, an increasing number of studies are suggesting the effect observed in previous studies may not have been real, but rather the result of flawed research methods.These include:
1. misclassification errors where reformed heavy drinkers – many of whom have health issues from their old drinking habit – are lumped in together with those who have never drunk in a group classed as “non drinkers”, making it look like those who don’t drink are worse off than they really are; and
2. confounding errors that arise from the difficulty of taking into account how lifestyle factors other than a person’s drinking habits might explain an observed correlation between good or bad health outcomes. Moderate drinkers for instance “do a lot of things [in their lives] moderately,” which might explain a relatively lower risk of certain diseases.
There are increasingly two camps of the scientific community’s current view on the debate.
One camp believes low-level drinking can protect against heart disease, type 2 diabetes, ischaemic stroke – the 70 per cent of strokes caused by blocked blood vessels to the brain – and perhaps some other health conditions such as dementia.
The other camp is “open to questioning” this observed protective effect. They say that we need to be extremely cautious about the conclusions we draw about protective effects, especially when those arguments are being used to promote moderate drinking as being good for your health.
_
A reason to drink?
Based on the current wealth of evidence, it is tempting to recommend small daily doses of alcohol (for example, 1 drink per day) to everyone, including non-drinkers with or at high risk for CV disease and/or diabetes. It might seem reasonable to recommend a drink a day to people who have no personal or family history of prior substance abuse, no history of depression or bipolar disorder and who are non-smokers. However, because alcohol use is a double-edged sword, light to moderate drinking cannot be responsibly recommended without a few warnings — even to those with CV disease. As health protective as a glass or two of wine a day may be, there is also considerable data showing that light to moderate daily alcohol is a slippery slope that can lead some people to heavy drinking. Heavy alcohol use is the cause of much distress and morbidity both at the personal and societal levels, and for some, moderate use quickly escalates to abuse. Alcohol abuse, the third largest preventable cause of death, is responsible for killing more than 100,000 Americans annually. The current American Heart Association guidelines advise individuals not to start drinking if they do not already drink alcohol because it is difficult to predict in which people alcohol abuse might become a problem. In general, we are best guided by the words of Abraham Lincoln: “It has long been recognized that the problems with alcohol relate not to the use of a bad thing, but to the abuse of a good thing.”
_
So given there’s still a sizeable group of scientists who believe low-level drinking might make you less likely to get heart disease, strokes and diabetes – and make you live longer – than if you didn’t drink at all, should a non-drinker consider taking up the habit?
The answer is a resounding NO.
Not only is the evidence of health benefits controversial but “if you want to reduce your risk of heart disease, there are many other things you can do besides turn to alcohol. There’s also always the risk you might start drinking at a low-risk level but end up slipping into a range that causes greater harm. If you’re going to drink, drink moderately for your enjoyment and other reasons but don’t drink because someone’s told you it will be good for you.
_
And if you’re already a moderate drinker, is there is any reason to consider cutting down?
The genetics behind alcoholism is complex but you might want to keep a closer eye on your drinking if you have parents or siblings who had alcohol [dependence] problems. And you might be extra vigilant if you are very concerned about certain cancers. Indeed while your lifetime risk of harm from alcohol-related cancers – which include cancers of the breast, bowel and mouth – is less than one in 100 if you drink less than two standard drinks a day, there is no safe lower limit. When we’re talking about cancers caused by alcohol, the [increased] risk begins with the first drink. Even consuming less than two standard drinks a day is nonetheless estimated to cause around 1500 deaths in Australia every year – most of them cancers. People are notorious for underestimating what they drink. They tend to forget those days where they drank a bit more or a lot more.
_________
Alcohol and diabetes mellitus:
The hormone insulin, which is produced in the pancreas, is an important regulator of blood sugar levels. In people with diabetes, the pancreas does not produce sufficient insulin (type 1 diabetes) or the body does not respond appropriately to the insulin (type 2 diabetes). Alcohol consumption by diabetics can worsen blood sugar control in those patients. For example, long-term alcohol use in well-nourished diabetics can result in excessive blood sugar levels. Conversely, long-term alcohol ingestion in diabetics who are not adequately nourished can lead to dangerously low blood sugar levels. Heavy drinking, particularly in diabetics, also can cause the accumulation of ketones in the blood that may result in severe health consequences. Finally, alcohol consumption can worsen diabetes-related medical complications, such as disturbances in fat metabolism, nerve damage, and eye disease.
_
A heavy ethanol load in a fasting, healthy individual is likely to produce transient hypoglycemia within 6–36 h, secondary to the acute actions of ethanol on gluconeogenesis. Alcohol ketoacidosis, probably reflecting a decrease in fatty acid oxidation coupled with poor diet or recurrent vomiting, can be misdiagnosed as diabetic ketosis. With the former, patients show an increase in serum ketones along with a mild increase in glucose but a large anion gap, a mild to moderate increase in serum lactate, and a -hydroxybutyrate/lactate ratio of between 2:1 and 9:1 (with normal being 1:1).
_
Occasional episodes of alcohol consumption generally do not worsen blood sugar control in people with diabetes and may even have beneficial effects as alcohol increases insulin sensitivity. Regular consumption of even moderate amounts of alcohol (i.e., two to four drinks per day), however, clearly interferes with diabetic blood sugar control and increases the risk of impotence; peripheral neuropathy; and, possibly, retinopathy. At the same time, similar levels of alcohol consumption are associated with a decreased risk of heart attacks and death from cardiovascular disease. The latter findings, however, were obtained with populations that included diabetics as well as nondiabetics, thereby limiting researchers’ ability to apply those findings to diabetics. Accordingly, more studies are needed to determine whether the beneficial effects of daily moderate alcohol consumption outweigh the deleterious effects. Diabetics clearly should avoid heavy drinking (i.e., more than 10 to 12 drinks per day), because it can cause ketoacidosis and hypertriglyceridemia. Moreover, heavy drinking in a fasting state can cause hypoglycemia and ultimately increase diabetics’ risk of death from noncardiovascular causes.
_
Alcohol can make it more difficult to manage your diabetes and can cause the following risks and complications:
•Interference with insulin or diabetic medications:
•Hypoglycaemia
•Higher blood pressure
•Increased body weight by consuming extra calories
•Higher levels of triglycerides or blood fats in your blood stream
_
Effects of Alcohol on Diabetes:
Here are some other ways that alcohol can affect diabetes:
•While moderate amounts of alcohol can cause blood sugar to rise, excess alcohol can actually decrease your blood sugar level — sometimes causing it to drop into dangerous levels.
•Beer and sweet wine contain carbohydrates and may raise blood sugar.
•Alcohol stimulates your appetite, which can cause you to overeat and may affect your blood sugar control.
•Alcohol may also affect your judgment or willpower, causing you to make poor food choices.
•Alcohol can interfere with the positive effects of oral diabetes medicines or insulin.
•Alcohol may increase triglyceride levels.
•Alcohol may increase blood pressure.
•Alcohol can cause flushing, nausea, increased heart rate, and slurred speech. These may be confused with or mask the symptoms of low blood sugar.
_
Diabetes risk and alcohol:
1. Researchers examined the results of 15 different studies and found that moderate drinkers are less likely to have type 2 diabetes than are abstainers. Teetotalers and heavy drinkers have equally high risk of the disease. The 15 studies were conducted in the U.S., Japan, Finland, Korea, the Netherlands, Germany and the UK and followed a total of 369,862 men and women for an average of 12 years. Moderate drinkers (those who drank between about a half a drink to four drinks per day) were found to be 30% less likely to develop type 2 diabetes than abstainers or heavy drinkers. Whether drinkers consume beer, wine or distilled spirits makes little difference, but the pattern of consumption does. It’s much better to consume frequently (such as daily) rather than infrequently for maximum health benefits.
2. An analysis of 13 studies found that “The results of these studies are consistent with regard to moderate alcohol consumption, indicating a protective effect in the order of 30%.” There was no evidence that high consumption of alcohol increased risk of diabetes.
3. An analysis of 32 studies found that compared with no alcohol use, moderate consumption (one to 3 drinks/d) is associated with a 33% to 56% lower incidence of diabetes and a 34% to 55% lower incidence of diabetes-related coronary heart disease.
4. An analysis of 20 cohort studies found that, compared with lifetime abstainers, a U-shaped pattern exists between alcohol consumption and risk of type 2 diabetes. The researchers concluded that “Our analysis confirms previous research findings that moderate alcohol consumption is protective for type 2 diabetes in men and women.”
5. The American Diabetes Association reports that in people with diabetes, light-to-moderate amounts of alcohol are associated with a decreased risk of heart disease, probably because alcohol raises HDL cholesterol, the so-called ‘good cholesterol.
6. An analysis of pairs of twins with different drinking patterns found that those who consumed alcohol in moderation had half the risk of developing type 2 (adult-onset) diabetes compared to those who consumed less alcohol. The study involved nearly 23,000 Finnish twins.
7. A prospective study of 85,051 women found that the risk of diabetes decreased as the consumption of alcohol increased. Compared with non-drinkers, those who consumed one-third to one drink per day had a 20% reduction in risk and those who consumed over one drink per day had a 40% reduced risk of developing diabetes.
8. A study of almost 21,000 physicians for over 12 years has found that men who are light to moderate drinkers have a decreased risk of Type 2 (non-insulin dependent) diabetes mellitus.
9. A study of 8,663 men over a period of as long as 25 years found that the incidence of type 2 diabetes was significantly lower among moderate drinkers than among either abstainers or heavy drinkers. These findings persisted after adjusting for age, smoking, blood pressure, HDL cholesterol, waist circumference, parental diabetes, fasting plasma glucose, body mass index (BMI), serum triglyceride concentration, and cardiorespiratory fitness.
10. Pre-menstrual women who consume a daily drink of beer, wine or distilled spirits (whiskey, rum, tequila, etc.) have a much lower risk of developing type 2 diabetes than abstainers, according to a study that duplicates similar findings in men. The Harvard study involved about 110,000 women age 25 to 42 over a ten -year period. Dramatic reductions (about 60%) occurred among women who drank between 1/2 and two drinks daily compared with abstainers. The reduction of risk was lower for those who drank less.
11. Drinking alcohol (beer, wine, or distilled spirits) in moderation was associated with a lower risk of developing type 2 diabetes among women age 40-70 in a large study in the Netherlands that followed them for an average of over six years. The authors wrote that the “findings support the evidence of a decreased risk of type 2 diabetes with moderate alcohol consumption and expand this to a population of older women.
12. Research conducted at the University of Padova Medical School in Italy found that consuming alcohol directly improved the action of insulin in both healthy diabetics. Alcohol also improved fatty acid levels.
13. A study of 5,221 men in Britain that followed them for almost 17 years found that that the risk of developing diabetes was lowest for light and moderate drinkers.
____________
Alcohol and hypertension:
Effects of Alcohol on Blood Pressure:
The relationship between alcohol consumption and blood pressure is noteworthy because hypertension is a major risk factor for stroke as well as for CHD. A national consensus panel in Canada recently conducted an extensive review of the evidence concerning this relationship (Campbell et al. 1999), concluding that studies have consistently observed an association between heavy alcohol consumption and increased blood pressure in both men and women. Researchers analyzing data from middle-aged British men found an association between heavy drinking and an overall increased risk of stroke that was largely related to alcohol’s effect on blood pressure (Wannamethee and Shaper 1996). However, in many studies comparing lower levels of alcohol use with abstention, findings are mixed. Some studies have found low alcohol consumption to have no effect on blood pressure or to result in a small reduction, while in other studies blood pressure levels increased as alcohol consumption increased. Randomized controlled trials to determine the effect of reductions in alcohol consumption on blood pressure in people with both normal and high blood pressure have consistently found that reductions in alcohol consumption were associated with declining blood pressure levels, although not all of these reductions were statistically significant (Cushman et al. 1998). Drinking pattern—how often drinking occurs— may have as important an effect on blood pressure as how much a person drinks (Russell et al. 1991). In summary, heavy drinking appears to increase the risk of hypertension and, although the evidence is not entirely consistent, also may increase the risk of stroke. It remains uncertain whether lower levels of alcohol can help prevent ischemic stroke. In addition to examining how much alcohol is consumed, it may be important to consider drinking pattern in determining stroke risk.
_
1. The regular consumption of alcohol elevates blood pressure, with global estimates that the attributable risk for hypertensive disease from alcohol is 16%.
2. The increase in blood pressure is approximately 1 mmHg for each 10 g alcohol consumed and is largely reversible within 2-4 weeks of abstinence or a substantial reduction in alcohol intake.
3. This increase in blood pressure occurs irrespective of the type of alcoholic beverage. In particular, the postulated effects of vasodilator flavonoid components of red wine to lessen or reverse alcohol-related hypertension have not been borne out in intervention studies.
4. Heavy drinking, especially a binge pattern of drinking, is linked to a higher incidence of cerebral thrombosis, cerebral haemorrhage and coronary artery disease deaths, although a role for alcohol-related hypertension in the causal pathway is not well defined.
5. In contrast, the light to moderate intake of alcohol has been consistently linked to a reduced risk of atherosclerotic vascular disease end-points. Such a protective effect may also extend to hypertensive subjects.
6. However, the magnitude of any protective effect appears to have been exaggerated because of unmeasured confounders, especially diet, lifestyle and patterns of drinking. Furthermore, a decrease in overall mortality with drinking appears confined to older subjects and to populations with a high background cardiovascular risk profile.
7. Any putative cardiovascular benefits from drinking need to be carefully considered against the effects of alcohol to elevate blood pressure, together with many other adverse health consequences from drinking. Maximum cardiovascular benefit occurs at relatively low levels of consumption (i.e. one to two standard drinks a day in men (10-20 g alcohol) and up to one a day in women (10 g alcohol)). In hypertensive subjects, consumption beyond these levels would be unwise.
_
Several mechanisms have been proposed for the relationship between alcohol and elevated BP. An immediate effect of alcohol ingestion is vasodilation in some vascular beds. Sustained intake accompanied by high blood alcohol levels, however, results in short-term elevation of BP. In addition, BP levels usually correlate best with alcohol intake within the prior 24 hours, and fall within hours to days after cessation or reduction in intake. Therefore, it is likely that the effect of alcohol on BP is not mediated by long-term structural alterations, but by neural, hormonal, or other reversible physiologic changes. According to one hypothesis, the hypertensive effect of alcohol is from a chronic state of alcohol withdrawal in frequent, heavy drinkers, but there is much evidence in favor of a direct effect of alcohol on BP. Suggested mediators of a direct effect include: 1) stimulation of the sympathetic nervous system, endothelin, renin-angiotensin-aldosterone system, insulin (or insulin resistance), or cortisol; 2) inhibition of vascular relaxing substances, e.g., nitric oxide; 3) calcium or magnesium depletion; 4) increased intracellular calcium or other electrolytes in vascular smooth muscle, possibly mediated by changes in membrane electrolyte transport; and 5) increased acetaldehyde. There appears to be more evidence to support the role of the sympathetic nervous system or cellular transport and electrolytes, or both, than the other mechanisms suggested, but this remains an open question. Alcohol can disrupt the sympathetic nervous system, which, among other things, controls the constriction and dilation of blood vessels in response to stress, temperature, exertion, etc. Heavy drinking — and bingeing, in particular — can cause blood pressure to rise. Over time, this effect can become chronic. High blood pressure can lead to many other health problems, including kidney disease, heart disease, and stroke.
_
Numerous studies have suggested that excess alcohol intake causes an increase in blood pressure. Klatsky et studied 83,947 men and women as part of a Kaiser-Permanente Multiphasic Health Examination study and reported that men and women who drank ≥3 drinks per day had both higher systolic and diastolic blood pressure compared with nondrinkers. In addition, those who drank ≥3 drinks a day had a greater prevalence of blood pressure ≥160/95 mm Hg. They also showed that excess alcohol contributed to elevated blood pressure after controlling for other variables and that beginning within days of abstinence, alcohol-related hypertension regresses. In the International Study of Sodium, Potassium, and Blood Pressure (INTERSALT), alcohol consumption for 7 days before a standard blood pressure measurement was obtained in >4800 men and 4800 women. After correction for confounding variables, men who drank 300 to 499 mL alcohol per week had an increase of systolic/diastolic blood pressure 2.7/1.6 mm Hg greater than that of nondrinkers; those men who drank ≥500 mL alcohol per week had an increase of systolic/diastolic blood pressure of 4.6/3.0 mm Hg. Women who drank ≥300 mL per week had an increase in systolic/diastolic blood pressure of 3.9/3.1 mm Hg. Binge drinking was associated with higher blood pressure than regular constant drinking. The authors concluded that a significant association existed between heavy drinking (3 to ≥4 drinks per day) and blood pressure; furthermore, this relationship was observed in both sexes and in both younger and older individuals.
_
Stroke and Hypertension:
Cerebrovascular disease, in which arteries in the brain are blocked or narrowed, can lead to a sudden, severe disruption of blood supply to the brain, called a stroke. Ischemic stroke, which is by far the predominant type of stroke, results from a blockage of a blood vessel; hemorrhagic stroke is due to rupture of a blood vessel. Alcohol-related hypertension, or high blood pressure, may increase the risk of both forms of stroke. Yet, in people with normal blood pressure, the risk of ischemic stroke may be decreased due to the apparent ability of alcohol to lessen damage to blood vessels due to lipid deposits and to reduce blood clotting. Alcohol’s anticlotting effects, while perhaps decreasing the risk of ischemic stroke, may increase the risk of hemorrhagic stroke (Hillbom and Juvela 1996). These studies are coming closer to providing a clear picture of the relationship between alcohol and risk of stroke.
_
Alcohol and Stroke:
Findings for associations between alcohol and stroke have been variable in the literature. Although light to moderate drinking consistently reduces cardiovascular events, effects on stroke have not been as consistent. In a study of 38,156 male professionals, Mukumal et al showed that, compared with nondrinkers, light drinkers (0.1 to 9.9 g/d) had an adjusted relative risk of 0.99 (95% CI, 0.72 to 1.37) for ischemic stroke, moderate drinkers (10.0 to 29.9 g/d) had a relative risk of 1.26 (95% CI, 0.90 to 1.76), and heavier drinkers (≥30 g/d or ≥3 drinks per day) had a relative risk of 1.42 (95% CI, 0.97 to 2.09; P=0.01). Although red wine was inversely related to risk, other beverages were not. Patterns of drinking also affected outcome: Consuming moderate alcohol on 3 to 4 days per week was associated with the lowest relative risk of ischemic stroke (0.68; 95% CI, 0.44 to 1.05). Stampfer et al studied 87,526 female nurses over ≈4 years. Moderate alcohol intake was associated with a decrease in coronary heart disease. Five to 14 g of alcohol per day (≈3 to 9 drinks per week) was associated with a decreased relative risk of ischemic stroke (0.3; 95% CI, 0.1 to 0.7), and for ≥15 g per day the relative risk was 0.5 (95% CI, 0.2 to 1.1). However, 5 to 14 g of alcohol per day increased the relative risk of subarachnoid hemorrhage (3.7; 95% CI, 1.0 to 13.8). In a very large trial, Klatsky et al studied the association between alcohol use in 128,934 members of a health plan and hemorrhagic stroke. Only persons who drank ≥6 drinks per day had an increase in hemorrhagic stroke (relative risk=1.9; 95% CI, 1.0 to 3.5). Elkind et al also recently reported in a multiethnic population of both sexes that moderate drinking (≥1 drink in the past month to ≤2 per day) was associated with a reduced risk of ischemic stroke (0.67; 95% CI, 0.46 to 0.99) compared with patients who did not drink in the prior year. When the reference group was people who never drank, results were the same. In contrast, a 2007 study by Beulen reported that the relative risk of ischemic stroke for hypertensive patients consuming 10 to 29.9 g alcohol per day was 1.55 (95% CI, 0.90 to 2.68) versus abstainers.
_
Alcohol and Stroke: various studies:
1. A systematic review and meta-analysis of 26 research studies (cohort or case-control) found that consuming two drinks per day is associated with a reduced risk of ischemic stroke.
2. The American Stroke Association states that studies now show that drinking up to two alcoholic drinks per day can reduce your risk for stroke by about half.
3. A study of over 22,000 men found that light and moderate alcohol consumption significantly reduces the overall risk of stroke.
4. A study published in the Journal of the American Medical Association found that consuming one or two drinks a day can reduce the risk of stroke by about half. It also found the protective effects of alcohol to occur among white, African- American, and Hispanic populations and among both men and women. The investigators concluded that their findings support the National Stroke Association Stroke Prevention Guidelines regarding the beneficial effects of moderate alcohol consumption.
5. Research has found that HDL (“good” cholesterol) is protective against stroke and that drinking alcohol in moderation is one of the ways that HDL can be increased.
6. A study published in the American Heart Association’s journal found abstainers’ risk of stroke to be double that of moderate drinkers.
7. The American Heart Association also reports that moderate consumption of alcohol is associated with dramatically decreased risk of stroke among both men and women, regardless of age or ethnicity.
_
Abstainers have much higher Risk of Stroke than Drinkers:
1. A study published in the Journal of the American Medical Association found that consuming one or two drinks a day can reduce the risk of ischemic stroke by about half. Its findings support the National Stroke Association Stroke Prevention Guidelines regarding the beneficial effects of moderate alcohol consumption.
2. A study of 944 residents of a Spanish city found that consumption of up to two alcoholics per day reduced the risk of strokes by 42%.
_
In summary, ethanol consumption can be both beneficial and harmful. The precise outcome for any one individual is hard to predict, nevertheless as a general guide one can use the information in the table below.
Effects of moderate and heavy drinking:
| MODERATE DRINKING | HEAVY DRINKING |
| Reduction of plaque deposits in arteries (atherosclerosis) | Increased risk for heart muscle disease(cardiomyopathy) |
| Protection against blood clot formation (protects against heart attack and stroke) | Increased risk for disturbed heart rhythm (arrhythmia) |
| Promotion of blood clot dissolution (protects against heart attack and stroke) | Increased risk for high blood pressure |
| Increased risk for hemorrhagic stroke |
_______
Alcohol and liver disease:
An association between alcohol consumption and liver disease has been known for over 200 years (Smart and Mann, 1992). In fact, the most common cause of illness and death from liver disease is from long-term alcohol consumption (National Center on Health Statistics, 1994). Since the liver is the primary site of alcohol metabolism, it is not surprising that it is particularly susceptible to alcohol-related injury. The injury to the liver from long-term drinking apparently comes not only from ethanol, but also from the dangerous products generated upon the metabolism of ethanol. These include acetaldehyde and highly reactive molecules called free radicals. Since the liver is the largest organ in the body (approx. 3.3lbs) and one of the most important being involved in a number of important processes, it has considerable reserves and is able to regenerate itself. Therefore, limited damage to the liver can go undetected and the insult needs to be quite substantial in order for damage to occur. With respect to alcohol, this means drinking large quantities of alcohol over many years. It has been estimated (Mazey et al., 1988) that in men the dose needed would be 600 kilograms taken chronically. This is equivalent to 72 oz of beer, 1 liter of wine, or 5 or 6 standard drinks (1.5oz) daily for 20 years. For women, the amount needed would be one-fourth of this due to gender differences in the ability to “handle” alcohol.
There are three major categories of liver damage (French et al, 1993) from alcohol ingestion, which are usually thought of as a progression in severity; however this is not always the case. These are:
1. Fatty liver – Fatty liver means fat disposition in the liver. This can occur after as single drinking session and after chronic consumption. Fatty liver is reversible and may not lead to more serious liver problems.
2. Alcoholic hepatitis – This disorder is characterized by widespread inflammation and destruction of the liver. The liver may have scar tissue. The symptoms may include fever, jaundice and abdominal pain. The condition may be fatal, but may be reversible if one quits drinking. It occurs in 50% of heavy drinkers.
3. Alcoholic cirrhosis – This is the most advanced form of liver disease and is diagnosed in 15 to 30 % of heavy drinkers. Between 40 and 90 percent of the 26,000 annual deaths from cirrhosis are alcohol related. (Dufour et al, 1993). Cirrhosis is characterized by extensive scar tissue (fibrosis) that stiffens blood vessels and distorts the internal structure of the liver. Cirrhosis causes malfunction of other bodily organs such as the brain and kidneys.
_
The risk factors presently known are:
•Quantity of alcohol taken: Consumption of 60–80g per day (about 75–100 ml/day) for 20 years or more in men, or 20g/day (about 25 ml/day) for women significantly increases the risk of hepatitis and fibrosis by 7 to 47%.
•Pattern of drinking: Drinking outside of meal times increases up to 3 times the risk of alcoholic liver disease.
•Gender: Women are twice as susceptible to alcohol-related liver disease, and may develop alcoholic liver disease with shorter durations and doses of chronic consumption. The lesser amount of alcohol dehydrogenase secreted in the gut, higher proportion of body fat in women, and changes in fat absorption due to the menstrual cycle may explain this phenomenon.
•Hepatitis C infection: A concomitant hepatitis C infection significantly accelerates the process of liver injury.
•Genetic factors: Genetic factors predispose both to alcoholism and to alcoholic liver disease. Both monozygotic twins are more likely to be alcoholics and to develop liver cirrhosis than both dizygotic twins. Polymorphisms in the enzymes involved in the metabolism of alcohol, such as ADH, ALDH, CYP4502E1, mitochondrial dysfunction, and cytokine polymorphism may partly explain this genetic component. However, no specific polymorphisms have currently been firmly linked to alcoholic liver disease.
•Iron overload (Hemochromatosis)
•Diet: Malnutrition, particularly vitamin A, B complex, C and E deficiencies, can worsen alcohol-induced liver damage by preventing regeneration of hepatocytes. This is particularly a concern as alcoholics are usually malnourished because of a poor diet, anorexia, and encephalopathy.
_
How Alcohol disrupts normal Liver Functioning:
•The coenzyme NAD is reduced, which greatly reduces critical energy pathways in the body
•Our pH balance shifts towards acid, which creates an environment for disease, dehydration, inflammation, and pain
•Fatty acid synthesis is impaired, leading the accumulation of fat. Fat accumulation can be seen in the liver after a single night of drinking
•Vitamin D cannot properly be activated – leading to low vitamin D levels. Vitamin D is needed for proper immune functioning, prevents osteoporosis, and is essential to the brain and nervous system, muscles, cartilage, pancreas and reproductive organs.
•Slows the release of bile – leading to poor digestion, gallstone development and the backup of toxins
•Death of liver cells and the formation of fibrous scar tissue
•The impairment of nutrient processing, hormone conjugation, and energy production
•Suppression of the nervous system
•Lactic Acid build up and uric acid secretion – leading to a higher risk of kidney stones and inflammation of the joints
•Alters protein metabolism – weakening the immune system and resulting in protein deficiency, despite a healthy diet
_
80% of alcohol passes through the liver to be detoxified. Chronic consumption of alcohol results in the secretion of pro-inflammatory cytokines (TNF-alpha, Interleukin 6 [IL6] and Interleukin 8 [IL8]), oxidative stress, lipid peroxidation, and acetaldehyde toxicity. These factors cause inflammation, apoptosis and eventually fibrosis of liver cells. Why this occurs in only a few individuals is still unclear. Additionally, the liver has tremendous capacity to regenerate and even when 75% of hepatocytes are dead, it continues to function as normal.
____________
Alcohol and Cancer:
Alcohol has been linked to a number of cancers, including cancers of the head and neck (mouth, pharynx, larynx, and esophagus), digestive tract (stomach, colon, and rectum) and breast (World Cancer Research Fund/American Institute for Cancer Research [WCRF/AICR] 1997; Doll et al. 1993; International Agency for Research on Cancer [IARC] 1988). Research suggests that the risk of cancers of the upper digestive tract is associated with both the concentration of alcohol in beverages and the number of drinks consumed (Doll et al. 1993). Even users of mouthwash containing a high alcohol concentration are at increased risk for cancers of the oral cavity and pharynx (Doll et al. 1993; Kato and Nomura 1994). Alcohol acts synergistically with tobacco to dramatically increase the risk of cancers of the oral cavity, pharynx, larynx, and esophagus (Doll et al. 1993; Longnecker 1995), that is, above that for alcohol or tobacco use alone.
_
A causal association has been established between alcohol consumption and cancers of the oral cavity, pharynx, larynx, oesophagus, liver, colon, rectum, and, in women, breast; an association is suspected for cancers of the pancreas and lung. Evidence suggests that the effect of alcohol is modulated by polymorphisms in genes encoding enzymes for ethanol metabolism (e.g., alcohol dehydrogenases, aldehyde dehydrogenases, and cytochrome P450 2E1), folate metabolism, and DNA repair. The mechanisms by which alcohol consumption exerts its carcinogenic effect have not been defined fully, although plausible events include: a genotoxic effect of acetaldehyde, the main metabolite of ethanol; increased estrogen concentration, which is important for breast carcinogenesis; a role as solvent for tobacco carcinogens; production of reactive oxygen species and nitrogen species; and changes in folate metabolism. Alcohol consumption is increasing in many countries and is an important cause of cancer worldwide.
_
If we assume causality between alcohol consumption and cancer, about 10% of all cancer cases in men and 3% of all cancer cases in women are attributable to current and former alcohol consumption in the investigated European countries. For cancers that are causally related to alcohol consumption, the proportions were 32% in men and 5% in women, with a substantial part (40-98%) being attributable to current alcohol consumption above the recommended upper limit of two drinks a day in men and one drink a day in women
_
Breast Cancer:
Unfortunately, the adverse effects of alcohol on the breast occur at the same levels of drinking that protect the heart. In the Nurses’ Health Study, for example, women who typically consumed three to nine drinks a week were 30 percent more likely than nondrinkers to develop breast cancer. Other studies have indicated that one drink a day is associated with an increased breast cancer risk of from 18 to 40 percent. Dr. Matthew Longnecker of the University of California at Los Angeles analyzed 38 studies on alcohol and breast cancer. He concluded that one drink a day increased breast cancer risk by about 10 percent and two drinks increased it by 25 percent. Dr. Marsha E. Reichman at the National Cancer Institute showed that premenopausal women given the equivalent of two drinks a day had a shift in estrogen hormones that could be the mechanism behind the rise in breast cancer associated with alcohol. Breast tissue is acutely sensitive to estrogen, and certain types of estrogen are known to stimulate growth of breast cancer cells.
_
Alcohol itself is not a carcinogen but may act as a tumor promoter. However, it remains unclear why only a minority of heavy drinkers develop alcohol-related tumors and severe alcohol-related diseases, while the vast majority of alcoholics do not. Recently, host genetic factors that modulate the individual risk have been suggested, after it was shown from twin studies that the susceptibility for alcohol-related organ injury is genetically determined in a substantial proportion. Since the inherited differences in alcohol metabolism could provide an attractive explanation for the individual susceptibility, the functional genetic polymorphisms of alcohol-metabolizing enzymes have been proposed as possible candidates. Alcohol is predominantly metabolized by the action of alcohol dehydrogenase (ADH) and the inducible microsomal cytochrome P450 2E1 (CYP2E1). Regarding ADH, several distinct isoenzymes have been cloned and characterized, which can be categorized into 5 different classes. The classification has recently been revised and the former isoenzymes ADH2 and ADH3 are now referred to as ADH1B and ADH1C. Two polymorphisms have been identified for ADH1C (ADH1C-1 and ADH1C-2), which encode the γ1 and γ2 subunits. The γ1γ1-isoenzyme (kcat, 87 min−1) reveals an enzymatic activity that is 2.5-fold higher than that of the γ2γ2-isoenzyme (kcat, 35 min−1), and therefore produces more acetaldehyde. Thus, it has been hypothesized that individuals with homozygosity for the allele ADH1C-1 carry an increased risk for alcohol-induced organ damage, such as liver cirrhosis, than patients with heterozygosity or those homozygous for ADH1C-2. However, a large European cohort study involving 876 alcoholic patients could not detect such association. Nonetheless, a contribution of the functional ADH polymorphisms to the formation of alcohol-associated malignancies could be important. The established different kinetics of polymorphic ADH enzymes may modulate the development of cancers since the metabolic product of their enzymatic activity is acetaldehyde, a highly toxic compound that has been identified as a carcinogen in animal experiments because of its mutagenic and carcinogenic properties that lead to genomic alterations, increased cell regeneration and metaplasia. However, when data from 7 population-based studies with respect to the possible role of ADH1C in the development of upper aerodigestive tract cancers including a total of 1,325 cases and 1,760 controls were recently analyzed, it was concluded that the ADH1C-1 allele does not confer an increased risk for head and neck cancers. This meta-analysis reevaluated pooled retrospective data originating from various regions with ethnic differences and largely minor to moderate alcohol consumption with limited data regarding smoking and, in some instances, drinking habits. The role of ADH1C-1/1 genotype in the development of hepatocellular and esophageal cancer was not investigated at all. A study from Puerto Rico demonstrated, that ADH1C-1/1 increases alcohol-associated cancer risk mainly in patients with high alcohol intake, showing evidence that the catalytic differences of ADH1C-1/1 may play a major role in these patients.
_
Alcohol in Hepatocellular Cancer:
Alcoholic cirrhosis of liver is a predisposing factor for hepatocellular cancer. Alcohol may act as a cocarcinogen, and has strong synergistic effects with other carcinogens including hepatitis B and C, aflatoxin, vinyl chloride, obesity, and diabetes mellitus. Acetaldehyde, the main metabolite of alcohol, causes hepatocellular injury, and is an important factor in causing increased oxidant stress, which damages DNA. Alcohol affects nutrition and vitamin metabolism, causing abnormalities of DNA methylation. Abnormalities of DNA methylation, a key pathway of epigenetic gene control, lead to cancer. Other nutritional and metabolic effects, for example on vitamin A metabolism, also play a key role in hepatocarcinogenesis. Alcohol enhances the effects of environmental carcinogens directly and by contributing to nutritional deficiency and impairing immunological tumor surveillance.
_
Light drinking and cancer:
In a meta-analysis of 222 studies comprising 92,000 light drinkers and 60,000 nondrinkers with cancer, light drinking was associated with risk for oropharyngeal cancer, esophageal squamous cell carcinoma, and female breast cancer. From this meta-analysis, it was estimated that in 2004 worldwide, 5000 deaths from oropharyngeal cancer, 24,000 from esophageal squamous cell carcinoma, and 5000 from breast cancer were attributable to light drinking. Light drinking was not associated with cancer of the colon-rectum, liver, or larynx. However, a caveat is in order here. When alcohol use is self-reported, respondents might underestimate, or underreport, their actual alcohol intake. This can result in finding associations between cancer and light to moderate drinking, when in reality, alcohol intake is much higher.
_______
Alcohol and brain injury:
Brain injury can be caused by alcohol because it:
•Has a toxic effect on the central nervous system (CNS)
•Results in changes to metabolism, heart functioning and blood supply
•Interferes with the absorption of vitamin B1 (thiamine), which is an important brain nutrient
•May be associated with poor nutrition
•Can lead to falls and accidents that injure the brain.
_
Alcohol abuse may cause alcohol related brain impairment (ARBI). ‘Binge drinking’, drinking in excess of recommended levels in a single session or heavy drinking over a long time may lead to ARBI. Alcohol is one of the many causes of acquired brain injury. The problems caused by alcohol misuse are together called alcohol related brain impairment (ARBI). A person with ARBI might experience problems with memory, thinking-related abilities and physical coordination.
_
Disorders associated with ARBI:
ARBI is associated with changes in cognition (memory and thinking abilities), difficulties with balance and coordination, and a range of medical and neurological disorders. Some alcohol-related disorders include:
•Cerebellar atrophy – the cerebellum is the part of the brain responsible for muscle coordination. Damage results in difficulties with balance and walking, which is called ‘ataxia’.
•Frontal lobe dysfunction – the brain’s frontal lobes are involved in abstract thinking, planning, problem solving and emotion. Damage results in cognitive difficulties.
•Hepatic encephalopathy – many people with alcohol-related liver disease develop particular psychiatric symptoms, such as mood changes, confusion and hallucinations.
•Wernicke’s encephalopathy – a disorder caused by a severe deficiency of vitamin B1. Some of the symptoms include ataxia, confusion and problems with vision.
•Korsakoff’s amnesic syndrome – this includes a loss of short-term memory, an inability to acquire new information and ‘confabulation’ (the person fills in gaps in their memory with fabrications that they believe to be true).
_
Nerve damage:
Heavy drinking can cause a form of nerve damage known as alcoholic neuropathy, which can produce a painful pins-and-needles feeling or numbness in the extremities as well as muscle weakness, incontinence, constipation, erectile dysfunction, and other problems. Alcoholic neuropathy may arise because alcohol is toxic to nerve cells, or because nutritional deficiencies attributable to heavy drinking compromise nerve function.
_
Alcohol and dementia:
Among lifestyle-related factors, low to moderate alcohol drinking has been proposed as a protective factor against the development of age-related changes in cognitive function, predementia syndromes, and cognitive decline of degenerative (Alzheimer’s disease, AD) or vascular origin (vascular dementia, VaD) in several longitudinal studies, but contrasting findings also exist. Furthermore, many of these studies were limited by cross-sectional design, restriction by age or sex, or incomplete ascertainment. Different outcomes, beverages, drinking patterns, or follow-up periods, or possible interactions with other lifestyle-related (i.e., smoking) or genetic factors [i.e., apolipoprotein E (APOE) genotyping] may be sources of great variability. Light to moderate alcohol use may be associated with a reduced risk of unspecified incident dementia and AD, while for VaD, cognitive decline, and predementia syndromes, the current evidence is only suggestive of a protective effect. In conclusion, as intervention studies are not feasible in this area, the best evidence comes from an overview of epidemiological studies, suggesting that the protective effects are more likely with wine consumption and the absence of an APOE e4 allele. At present, there is no indication that light to moderate alcohol drinking would be harmful to cognition and dementia, and it is not possible to define a specific beneficial level of alcohol intake.
__
Alcohol and Alzheimer’s disease and Other Dementia: various studies:
1. A study in France found moderate drinkers to have a 75% lower risk for Alzheimer’s Disease and an 80% lower risk for senile dementia.
2. Research on 7,460 women age 65 and older found that those who consumed up to three drinks per day scored significantly better than non-drinkers on global cognitive function, including such things as concentration, memory, abstract reasoning, and language. The investigators adjusted or controlled for such factors as educational level and income that might affect the results, but the significant positive relationships remained.
3. Researchers in Australia studied 7,485 people age 20 to 64 years. They found that moderate drinkers performed better than abstainers on all measures of cognitive ability. Sex, race, education and extroversion-introversion failed to account for the findings.
4. Older people who drink in moderation generally suffer less mental decline than do abstainers, another study finds. Over one thousand persons age 65 and older were studied over a period of seven years. Overall, light and moderate drinkers experienced less mental decline than did non-drinkers.
5. Women who consume alcohol (beer, wine or distilled spirits) moderately on a daily basis are about 20% less likely than abstainers to experience poor memory and decreased thinking abilities, according to data from 12,480 women age 70 to 81 who participated in the long-term study.
6. A study of about 6,000 people age 65 and older found that moderate drinkers have a 54% lower chance of developing dementia than abstainers. The type of alcohol beverage consumed (wine, spirits, or beer) didn’t make a difference in the protective effects of drinking in moderation.
7. A study of 7,983 people aged 55 of age or older in The Netherlands over an average period of six years found that those who consumed one to three drinks of alcohol (beer, wine, or distilled spirits) per day had a significantly lower risk of dementia (including Alzheimer’s) than did abstainers.
8, A study of over 400 people at least 75 years old who were followed for a period of six years found that drinkers were only half as likely to develop dementia (including Alzheimer’s disease) as similarly-aged abstainers from alcohol. Abstainers were defined as people who consumed less than one drink of alcohol per week.
9. Moderate drinking among older women can benefit memory according to research funded by the National Institutes of Health. Moderate drinkers performed better on instrumental everyday tasks, had stronger memory self-efficacy and improved memory performance.” The performance memory tests include such topics as remembering a story, route, hidden objects, future intentions and connecting random numbers and letters. In all cases, the group who drank scored better than those who did not drink. Women who drank alcohol in moderation (defined as consuming up to two drinks of beer, wine or spirits per day) also performed better on attention, concentration, psychomotor skills, verbal-associative capacities and oral fluency.
10. A study of 1,018 men and women age 65-79 whose physical and mental health was monitored for an average of 23 years found that “drinking no alcohol, or too much, increases risk of cognitive impairment,” in the words of the editor of the British Medical Journal, which published the study.
11. A study of over 6,000 people in the U.K. found that those who consume as little as a single drink of alcoholic beverage per week have significantly greater cognitive functioning than teetotalers. Abstainers were twice as likely as occasional drinkers to receive the lowest cognitive functioning test scores. The beneficial mental effects of alcohol were found when a person drinks up to about 30 drinks per week, and increased with consumption. The researchers did not test the effects of higher levels of alcohol drinking. The research team suggests that alcohol (beer, wine, or liquor) improves mental functioning because it increases blood flow to the brain.
12. Moderate alcohol consumption protects older persons from the development of cognitive impairment, according to a study of 15,807 Italian men and women 65 years of age and older. Among the drinkers only 19% showed signs of mental impairment compared to 29% of the abstainers. The relationship continued even when other factors in cognitive impairment, such as age, education, and health problems were considered.
13. An 18-year study of Japanese-American men found “a positive association between moderate alcohol intake among middle-aged men and subsequent cognitive performance in later life.” Moderate drinkers scored significantly higher on the Cognitive Abilities Screening Instrument (CASI), which includes tests of attention, concentration, orientation, memory, and language. Both non-drinkers and heavy drinkers had the lowest CASI scores.
14. The moderate consumption of alcohol was associated with superior mental function among older women compared to abstainers in a study of 9,000 women aged 70 to 79 over a period of 15 years. The women’s mental function was assessed with seven different tests. After adjusting for other factors that might affect mental function, the researchers found that the women who drank in moderation performed significantly better on five of seven tests. They also performed significantly better on a global score that combined all seven tests. The researchers found that the effect of moderate alcohol consumption on cognitive functioning was the equivalent of being one to two years younger.
15. Drinking alcohol (beer, wine or liquor) in moderation is one of the strategies that can reduce the risk of cognitive decline and dementia in later life according to a review of research conducted by scholars from the School of Aging Studies at the University of South Florida and the University of Alabama at Birmingham. They systematically analyzed the existing research to identify how dementia can be reduced. Abstaining from alcohol and abusing alcohol are both risk factors for cognitive decline and dementia.
_
Alcohol, dementia and cognitive decline in the elderly: a systematic review:
Despite chronic alcohol abuse causing progressive neurodegenerative disease , several studies have suggested that alcohol consumption, within limits and/or of certain types, is associated with a decreased risk of dementia or cognitive decline. There are many mechanisms proposed in the literature to explain this. It has been suggested that the antioxidant properties of the flavenoids in wine may help prevent the oxidative damage implicated in dementia. Alcohol also increases levels of HDL cholesterol and fibrinolytic factors leading to lower platelet aggregation and possibly lower risk of stroke/ischemia . At least one study has found that light to moderate alcohol intake (one drink per week to four drinks per day) is associated with a lower prevalence of vascular brain findings on imaging and less atrophy of the hippocampus and amygdala in APOEe4 carriers as assessed by magnetic resonance imaging (MRI). The consumption of alcohol has also been associated with decreased cardiovascular risk via the mechanisms described above and possible enhancement of insulin sensitivity or reduction in inflammatory response. Given the link between vascular dementia (VaD), vascular function, and the increasing body of evidence suggesting that Alzheimer’s disease (AD) may be influenced by vascular factors, it may be concluded that this cardiovascular protection decreases incident dementia/cognitive decline. Counter to this are the effects of heavy alcohol consumption and alcoholism as detrimental to memory function. While most evidence is derived from studies of younger adults, the possible protective effects of alcohol may also apply to older adults, i.e. those at greatest risk from dementia. Lower levels of alcohol intake have proportionally greater effects in the elderly, due to their decreased lean body mass and lower percentage of body weight made up of water. Alcohol may also have negative impacts on other body systems in this age group and may be the cause of falls, with potentially more serious consequences than in younger people, although the evidence for this is not clear cut. An examination of all research published within the last 10 years suggests that, at least in epidemiological studies, low to moderate alcohol use is associated with a 38% reduced risk of unspecified incident dementia. For AD also, low to moderate alcohol was associated with a significantly reduced risk of 32%.
_
A contrary study:
Chronic effects of low to moderate alcohol consumption on structural and functional properties of the brain: beneficial or not?
Some studies suggest that the effects of low to moderate drinking (about 1–3 standard glasses of alcohol per day) on the brain and cognitive performance are positive. In this study this hypothesis is investigated. For this purpose studies on the effects of low to moderate drinking on brain structure (Magnetic Resonance Induction (MRI) studies) and on cognitive performance were analysed and discussed. In MRI studies, a linear negative effect of alcohol consumption on brain volume was found. Furthermore, a linear decrease in grey matter concurring with a linear increase in white matter volumes as a function of number of drinks was reported in males, but not in females. Only in elderly low to moderate drinkers (aged > 65 years) there appeared to be a U-shaped relationship between alcohol consumption and white matter integrity (grade) on the one hand and cognition on the other hand. The changes reported in brain shrinkage, grey matter and white matter volume, as a result of low to moderate alcohol consumption offer support for the contention that such drinking decreases brain health than for its beneficial effect. An exception might hold for elderly light and moderate drinkers where less white matter damage was found than in abstainers concurring with better cognitive performance. However, methodological problems impose limits on this conclusion.
_
Heavy drinking and Dementia:
As people age, their brains shrink, on average, at a rate of about 1.9% per decade. That’s considered normal. But heavy drinking speeds the shrinkage of certain key regions in the brain, resulting in memory loss and other symptoms of dementia. Heavy drinking can also lead to subtle but potentially debilitating deficits in the ability to plan, make judgments, solve problems, and perform other aspects of “executive function,” which are “the higher-order abilities that allow us to maximize our function as human beings. In addition to the “nonspecific” dementia that stems from brain atrophy, heavy drinking can cause nutritional deficiencies so severe that they trigger other forms of dementia.
_
Alcohol responsive tremor:
Essential tremors can be temporarily relieved in up to two-thirds of patients by drinking small amounts of alcohol. Ethanol is known to activate aminobutyric acid type A (GABA-A) and inhibit N-methyl-D-aspartate (NMDA) glutamate receptors, which are both implicated in essential tremor pathology and could underlie the ameliorative effects. Additionally, the effects of ethanol have been studied in different animal essential tremor models. Many patients with essential tremor (ET) report transient improvement of symptoms after drinking alcohol. However, the brief duration of action, subsequent rebound, and the risk of developing alcohol addiction make the use of alcohol as a treatment for ET inappropriate. Whether excessive alcohol consumption is a risk for or a consequence of ET has been a subject of some controversy.
_
A study of hereditary essential tremor:
Twenty index patients with hereditary essential tremor and their kindred were studied to define the phenotype of this condition. Ninety-three first degree and 38 more distant relatives were examined; 53 definite and 18 possible secondary cases were identified. The age of tremor onset was bimodally distributed with a median at 15 years. Segregation analysis indicated autosomal dominant inheritance and penetrance was virtually complete by the age of 65 years. There were no examples of the disease skipping a generation. Men and women were affected in equal proportions. About 50% of cases were alcohol responsive. In the majority of families alcohol responsiveness was either consistently present or did not occur, but in 20% of kindred definite heterogeneity of responsiveness was encountered within each family.
_
The effect of ethanol on alcohol-responsive essential tremor: A positron emission tomography study:
Authors used H215O positron emission tomography (PET) to investigate the effect of ethyl alcohol on regional cerebral blood flow in 6 patients with alcohol-responsive essential tremor and 6 age-matched control subjects. The patients were scanned while at rest and during involuntary postural tremor of the extended right arm. Normal control subjects were scanned at rest and during passive wrist oscillation of the right arm at tremor frequency. Regional cerebral blood flow associated with these conditions was measured before and after oral administration of 2 to 3 units of alcohol. The mean blood alcohol level was 35.3 ± 20.0 mg/dl in the patient group and caused marked suppression of tremor; it was 33.9 ± 12.9 mg/dl in the control group. Similar to previous PET studies on essential tremor patients, tremor compared with rest was associated with bilateral cerebellar activation including the cerebellar vermis. This pattern of activation differed from passive wrist oscillation where ipsilateral cerebellar activation was observed. Ethanol ingestion led to bilateral decreases of cerebellar blood flow in both tremor patients and normal subjects, and this was associated with suppression of tremor in the patients. Alcohol-associated increases of regional cerebral blood flow were observed in the inferior olivary nuclei in the patients but not in the control subjects. Authors conclude that alcohol-induced suppression of essential tremor is mediated via a reduction of cerebellar synaptic overactivity resulting in increased afferent input to the inferior olivary nuclei.
___________
Alcohol and Arthritis:
1. A recent study found that alcohol consumption is associated with a significantly reduced risk of developing arthritic conditions including Rheumatoid Arthritis (RA), Osteoarthritis (OA), reactive arthritis, psoriatic arthritis and spondylarthropathy.
2. A large study in Sweden found that the risk of developing arthritis decreased as the consumption of alcohol increased from light to moderate levels.
3. Data from two other research studies in Scandinavia show that drinking alcohol is associated with a reduction in the risk of rheumatoid arthritis. Two independent case-control studies of rheumatoid arthritis were used. The Swedish study used 1,204 cases and 871 controls and the Danish study used 444 cases and 533 controls. Among alcohol consumers, the quarter with the highest consumption levels had a decreased risk of rheumatoid arthritis of 40-50% compared to the half with the lowest alcohol consumption.
4. A study of 1,877 men and women found that drinking alcohol reduced both the risk and severity of rheumatoid arthritis. Non-drinkers were four times more likely to develop rheumatoid arthritis than people who drank alcohol on more than ten days a month. The risk of developing rheumatoid arthritis decreased according to the frequency of alcohol consumption.
5. Analysis of data from 1,666 patients in Finland indicates that alcohol consumption significantly reduces the risk of developing rheumatoid arthritis.
_
Ethanol prevents development of destructive arthritis: A study:
Environmental factors are thought to play a major role in the development of rheumatoid arthritis. Because the use of ethanol is widespread, authors assessed the role of ethanol intake on the propensity to develop chronic arthritis. Collagen type II-immunized mice were given water or water containing 10% (vol/vol) ethanol or its metabolite acetaldehyde. Their development of arthritis was assessed, as well as the impact of ethanol on leukocyte migration and activation of intracellular transcription factors. Mice exposed daily to this dose of ethanol did not display any liver toxicity, and the development of erosive arthritis was almost totally abrogated. In contrast, the antibody-mediated effector phase of collagen-induced arthritis was not influenced by ethanol exposure. Also, the major ethanol metabolite, acetaldehyde, prevented the development of arthritis. This antiinflammatory and antidestructive property of ethanol was mediated by (i) down-regulation of leukocyte migration and (ii) up-regulation of testosterone secretion, with the latter leading to decreased NF-κB activation. Authors conclude that low but persistent ethanol consumption delays the onset and halts the progression of collagen-induced arthritis by interaction with innate immune responsiveness.
____
Alcohol and bone mineral density:
1. Researchers examined the evidence from 33 studies and found that alcohol consumption increased neck bone density for each drink per day over the range of 0-3 drinks per day; reduced the risk for hip fracture with increasing quantities consumed; and was generally associated with reduced bone loss over time, compared with abstention from alcohol.
2. A study was conducted using identical female twins, in which one twin drank very little and the other twin drank moderately (one or two drinks each day). Twins were used because they are genetic clones. Because they have the same genes and grew up in the same environment, it’s easier to control for any other possible confounding factors. The study found that moderate drinkers had significantly denser bones than the control group of twins consisting of very light drinkers.
3. The National Osteoporosis Risk Assessment followed over 200,000 postmenopausal women in the U.S. with no previous diagnosis of osteoporosis who were seen at doctors’ offices, with no previous diagnosis of osteoporosis. As a result of screening, the study found that 39.6% had osteopenia or low bone density and 7% had osteoporosis. The study found that drinking alcohol reduced the chances of developing osteoporosis.
4. Analyses using data from 13,512 persons ages 20 or older found that bone density was higher in men and postmenopausal women compared with those who do not drink.
5. A population-based cohort study of 5,865 adults aged 65 years and older from four U.S. communities found that moderate drinking was associated with a significant decrease in risk of hip fracture. Compared with long-term abstainers, moderate drinkers of beer, wine or spirits had a 22% lower chance of developing osteoporosis. Alcohol consumption was also associated with bone mineral density of the total hip and femoral neck in a stepwise manner, with approximately 5% higher bone density among consumers of 14 or more drinks per week than among abstainers.
_
However, effects of repeated heavy drinking on the skeletal system include changes in calcium metabolism, lower bone density, and decreased growth in the epiphyses, leading to an increased risk for fractures and osteonecrosis of the femoral head.
______
Alcohol and Infections:
Excessive alcohol consumption depresses the immune system and increases the propensity to severe infections, including pneumonia, tuberculosis, bacterial peritonitis, HIV/AIDS and other sexually transmitted diseases . People who drink heavily also are more likely to engage in risky sex. Heavy drinking is associated with a three-fold increase in the risk of contracting a sexually transmitted disease. Research has found moderate drinkers to be more resistant than abstainers to five strains of the common cold virus. Those who consumed two to three drinks daily had an 85% greater resistance. Those drinking one to two drinks daily had a 65% lower risk and those who drank less than daily had a 30% lower risk than abstainers.
_
Gout:
A painful condition, gout is caused by the formation of uric acid crystals in the joints. Although some cases are largely hereditary, alcohol and other dietary factors seem to play a role. Alcohol also seems to aggravate existing cases of gout.
_
Alcohol and Kidney:
Ethyl alcohol can induce urine flow within 20 minutes. As a result of these fluid losses the concentrations of electrolytes in the blood can changed and can be dramatic, particularly in cases of extreme loss of water. Ethyl alcohol appears to affect a hormone called anti-diuretic hormone, which induces the kidney to conserve fluids. This effectively concentrates the urine. Ethyl alcohol decreases the ability of the body to concentrate urine, thus promotes water loss rather than allowing the water to be absorbed back into the body. As a result of this electrolyte levels in the blood also rise due to less water being taken back in.
_
As with most organs in the body there are a number of regulatory processes which allow the kidney to function normally and optimally, ethyl alcohol can disturb these controls. The precise effects depend upon the amount of alcohol taken and the time over which it is consumed. Alcohol has been shown to change the structure and function of the kidney and impair their ability to regulate the volume and composition of fluid and electrolytes in the body. Gross and microscopic changes in the kidney include alterations in the structure of the glomerulus, swelling or enlargement (nephromegaly) of the kidney, and increased number of cells with fat, protein, and water. These effects alter the ability of the kidneys to function normally. The rate of blood flow through the kidneys is an important determinant of the amount of filtration of the blood and absorption of substances from the blood that can take place. Various effects of alcohol have been reported including both increased and reduced blood flow. These effects seem to be related to whether or not the person also had liver disease and in animal models which species of animal was used. Alcohol’s effect on electrolyte balance has major implications for the satisfactory functioning of the cells of the body. As a prime example, the cells of the brain and particularly neurons are highly dependent upon proper amounts of sodium, potassium, chloride, and calcium being available. Disruption in the proper flow and availability of these electrolytes alters the ability of the neurons to function which leads to modifications in behavior and the ability of the brain to regulate other bodily processes.
_
Effect of Ethyl Alcohol on Electrolytes:
| Problem | Major Cause(s) |
| Low sodium level (hyponatremia) | Massive intake of solute-free fluid (beer) |
| Low potassium level (hypokalemia) | Dietary deficiency, gastric losses, leaky membranes, shifts from extracellular to intracellular |
| Low phosphorus level (hypophosphatemia) | Dietary deficiency, malabsorption, increased cellular uptake |
| Low magnesium level (hypomagnesemia) | Dietary deficiency, malabsorption, phosphorus deficiency |
_
Proper acid-base balance (i.e. hydrogen ion concentration) is crucial to the proper functioning of most of the body’s metabolic reactions. The kidneys play an important role in regulating this acidity, thus the rate at which metabolic processes proceed. Examples of alcohol-related acid-base disturbances include low levels of phosphate, which may result from hyperventilation during withdrawal from alcohol and cases of alkalosis (loss of acid) which may be a result of severe vomiting after binge drinking.
_
Prospective Study of Beverage Use and the Risk of Kidney Stones:
Patients with kidney stones are routinely advised to increase their fluid intake to decrease the risk of stone recurrence. However, there has been no detailed examination to determine whether the effect on recurrence varies by the type of beverage consumed. The authors conducted a prospective study of the relation between the intake of 21 different beverages and the risk of symptomatic kidney stones in a cohort of 45,289 men, 40-75 years of age, who had no history of kidney stones. Beverage use and other dietary information was measured by means of a semiquantitative food frequency questionnaire in 1986. During 6 years of follow-up (242,100 person-years), 753 incident cases of kidney stones were documented. After adjusting simultaneously for age, dietary intake of calcium, animal protein and potassium, thiazide use, geographic region, profession, and total fluid intake, consumption of specific beverages significantly added to the prediction of kidney stone risk (p < 0.001). After mutually adjusting for the intake of other beverages, the risk of stone formation decreased by the following amount for each 240-ml (8-oz) serving consumed daily: caffeinated coffee, 10% (95% confidence interval 4-15%); decaffeinated coffee, 10% (3-16%); tea, 14% (5-22%); beer, 21% (12- 30%); and wine, 39% (10-58%). For each 240-ml serving consumed daily, the risk of stone formation increased by 35% (4-75%) for apple juice and 37% (1-85%) for grapefruit juice. The authors conclude that beverage type may have an effect on stone formation that involves more than additional fluid intake alone.
_
Alcohol and gall stone disease:
A total of 80,898 women in the U.S. were followed for 20 years, with alcohol consumption being measured every two to four years. The resulting finding was that alcohol consumption decreased the risk of developing gallstone disease. As consumption increased, the risk decreased. Compared with women who did not drink, those who drank an average of up to one drink per day experienced a 14% decrease in risk whereas those who drank an average of four or more drinks per day had a 38% reduced risk of developing gallstone disease. In addition, as frequency of consumption increased risk decreased dramatically. Beer, wine and spirits all reduced risk.
_
Other diseases:
Between one-half and two-thirds of alcoholics have skeletal muscle weakness caused by acute alcoholic myopathy, a condition that improves but which might not fully remit with abstinence. Hormonal changes include an increase in cortisol levels, which can remain elevated during heavy drinking; inhibition of vasopressin secretion at rising blood alcohol concentrations and enhanced secretion at falling blood alcohol concentrations (with the final result that most alcoholics are likely to be slightly overhydrated); a modest and reversible decrease in serum thyroxine (T4); and a more marked decrease in serum triiodothyronine (T3). Hormone irregularities should be reevaluated as they may disappear after a month of abstinence. In a study of 18,339 observations, researchers found that drinking alcohol in moderation significantly reduces the risk of intermittent claudication. IC is associated with a two- to four-fold increased risk of death from cardiovascular disease. Harvard researchers found moderate drinkers to be almost 1/3 less likely to suffer Peripheral Artery Disease (a significant cause of death among the elderly) than those consuming less than one drink per week. An analysis of 19 published studies that included over 120,000 men found that drinking two or more drinks a day was associated with a 35% reduction in risk of developing benign prostate enlargement.
_
Alcohol and Malnutrition:
Alcoholism is a major cause of malnutrition. The reasons are threefold. First, alcohol interferes with central mechanisms that regulate food intake and causes food intake decreases. Second, alcohol is rich in energy (7.1 kcal/g), and like pure sugar most alcoholic beverages are relatively empty of nutrients. Increasing amounts of alcohol ingested lead to the consumption of decreasing amounts of other foods, making the nutrient content of the diet inadequate, even if total energy intake is sufficient. Thus chronic alcohol abuse causes primary malnutrition by displacing other dietary nutrients. Third, gastrointestinal and liver complications associated with alcoholism also interfere with digestion, absorption, metabolism, and activation of nutrients, and thereby cause secondary malnutrition. It is important to note that although ethanol is rich in energy, its chronic consumption does not produce the expected gain in body weight. This may be attributed, in part, to damaged mitochondria and the resulting poor coupling of oxidation of fat metabolically utilizable with energy production. The microsomal pathways that oxidize ethanol may be partially responsible. These pathways produce heat rather than adenosine triphosphate (ATP) and thereby fail to couple ethanol oxidation to useful energy-rich intermediates such as ATP. Thus, perhaps because of these energy considerations, alcoholics with higher total caloric intake do not experience expected weight gain despite physical activity levels similar to those of the non-alcohol-consuming overweight population.
_____________
In a nutshell, effect of alcohol on physical health is summarized in the figure below:
_____________
Alcohol and mortality:
Moderate alcohol consumption and health benefits:
Alcohol has been used medicinally throughout recorded history; its medicinal properties are mentioned 191 times in the Old and New Testaments. As early as the turn of the century there was evidence that moderate consumption of alcohol was associated with a decrease in the risk of heart attack. And the evidence of health benefits of moderate consumption has continued to grow over time. Reviews of research evidence report a strong, consistent relationship between moderate alcohol consumption and reduction in cardiovascular disease in general and coronary artery disease in particular. On the basis of its extensive review of research, the National Institute on Alcohol Abuse and Alcoholism (NIAAA) reported that moderate drinkers have the greatest longevity. It also found that moderate drinking is beneficial to heart health, resulting in a sharp decrease in heart disease risk (40%-60%). This is important because cardiovascular disease is the number one cause of death in the United States, and heart disease kills about one million Americans each and every year. The health benefits of moderate alcohol consumption have long been known. One of the earliest scientific studies on the subject was published in the Journal of the American Medical Association in 1904. The Director of the National Institute on Alcohol Abuse and Alcoholism wrote that “Numerous well-designed studies have concluded that moderate drinking is associated with improved cardiovascular health,” and the Nutrition Committee of the American Heart Association reported that “The lowest mortality occurs in those who consume one or two drinks per day.” A World Health Organization Technical Committee on Cardiovascular Disease asserted that the relationship between moderate alcohol consumption and reduced death from heart disease could no longer be doubted. But the benefits are not limited, important as they are, to reductions in heart disease.
_
The figure below shows all cause mortality is lower in moderate drinker than abstainer or heavy drinker:
_
Moderate drinkers tend to enjoy better health than do either abstainers or heavy drinkers.
1. A nation-wide survey in the U.S. revealed that daily moderate drinkers experienced significantly less acute hospitalization.
2. A nine year study of indicators of good health found moderate alcohol consumption to be associated with the most favorable health scores.
3. A study that examined nearly 10,000 men and women at age 23 and again at age 33 found that the moderate drinkers experience lower levels of poor general health, long-term illness, and psychological distress when compared to abstainers and heavy drinkers.
4. A study of nearly 20,000 Spaniards found that moderate consumption of any alcohol — beer, wine, or spirits — was linked to better overall health, compared to abstinence from alcohol.
5. A nation-wide Canadian study found that moderate drinkers who consumed alcohol daily had 15% less disability than the general population.
6. A Dutch study found that moderate drinkers under stress were less likely to be absent from work than were either abstainers or heavy drinkers. The investigators concluded that abstinence is at least as unhealthy as excessive drinking.
7. A study of 3,803 individuals age 18 to 101 found that lifelong teetotalers as well as former drinkers are consistently less healthy than light to moderate drinkers (those who consume up to 60 drinks per month). The health superiority of light and moderate drinkers extends to both physical and mental health.
_
Moderate Drinking vs. Lifestyle:
Why drink to reduce the risk of heart disease? Wouldn’t eating a good diet, exercising, and losing weight do the same thing? No, it wouldn’t. The moderate consumption of alcohol appears to be more effective than most other lifestyle changes that are used to lower the risk of heart and other diseases. For example, the average person would need to follow a very strict low-fat diet, exercise vigorously on a regular basis, eliminate salt from the diet, lose a substantial amount of weight, and probably begin medication in order to lower cholesterol by 30 points or blood pressure by 20 points. But medical research suggests that alcohol can have a greater impact on heart disease than even these hard-won reductions in cholesterol levels or blood pressure. Only cessation of smoking is more effective. Additionally, other medical research suggests that adding alcohol to a healthful diet is more effective than just following the diet alone.
1. The lowest risk of fatal heart disease occurred among those who both drank moderately and exercised. They had a 50% reduced risk compared to non-drinkers who didn’t exercise. (Moderate drinking was defined as consuming an average of up to two drinks per day for both men and women. This is twice as high as the US federal recommendation for women.)
2. A higher risk was found among (a) those who abstained from alcohol but exercised and (b) those who drank in moderation but didn’t exercise. In both cases the risk of heart disease dropped about 30% compared to abstaining non-exercisers.
3. The highest risk was found among those who neither drank nor exercised. Their risk of dying from heart disease was twice as high as those who drank moderately and exercised.
Moderate drinking and exercise are cumulative in their positive effects on the cardiovascular system. Doing one is better than nothing, but doing both is the best choice of all and dramatically reduces the risk death from heart attack. The same is also found for all-cause mortality.
_
Relation between Alcohol Consumption and Total Mortality:
A large number of observational studies have consistently demonstrated a J-shaped relation between alcohol consumption and total mortality. This relation appears to hold in men and women who are middle aged or older. The lowest mortality occurs in those who consume one or two drinks per day. In teetotalers or occasional drinkers, the rates are higher than in those consuming one or two drinks per day. In persons who consume three or more drinks per day, total mortality climbs rapidly with increasing numbers of drinks per day. A number of studies have dissected the J-shaped curve into specific diseases. It is clear that a stepwise decline in CHD death occurs with increasing drinks per day. Because CHD accounts for one third or more of total deaths, those with no alcohol consumption have higher total mortality than those drinking one to two drinks per day. On the other hand, mortality due to a large number of other diseases increases with an increasing number of drinks consumed per day. Diseases related to heavy consumption of alcohol and alcoholism include stroke, alcoholic cardiomyopathy, several kinds of cancer, cirrhosis, and pancreatitis, as well as accidents, suicide, and homicide. It should be noted that heavy consumption of alcohol is a major cause of hypertension, so that the diseases related to hypertension, such as stroke, are generally related to alcohol consumption. Heavy consumption of alcohol also appears to affect heart muscle and possibly arterial tissues directly. Alcoholic cardiomyopathy is a common diagnosis in long-term alcoholics. While the relative and absolute risks of these diseases are negligible at one or two drinks per day, the mortality rates rise sharply. The J-shaped distribution for total mortality is then the sum of the protective effect on CHD mortality and the detrimental effect of high levels of consumption on these other causes of death.
_
J shaped curve depicting alcohol and mortality relationship:
_
Numerous mechanisms have been proposed to explain the benefit that light-to-moderate alcohol intake has on the heart, including an increase of high-density lipoprotein cholesterol, reduction in plasma viscosity and fibrinogen concentration, increase in fibrinolysis, decrease in platelet aggregation, improvement in endothelial function, reduction of inflammation, and promotion of antioxidant effects. Controversy exists on whether alcohol has a direct cardioprotective effect on ischemic myocardium.
_
Why J shaped curve:
J shaped curve shows greater alcohol consumption ceases to be beneficial at a certain point, and instead starts to take its toll on your health. The same diseases that were prevented by alcohol at low doses are caused by alcohol at high doses. High doses of alcohol lead to the induction of the P450 hepatic microsomal ethanol-oxidizing system resulting in a considerably higher clearance rate of ethanol from the bloodstream for an extended period of time. Small amounts alcohol is not sufficient to induce P450. P450 is a class, or family, of liver enzymes whose main functions include catalyzing the metabolism of drugs and the oxidation of organic substances. In simplistic terms, higher alcohol consumption sends this system into high gear, and starts clearing ethanol from your system. However, this pathway generates free radicals that damage tissues and because the system consumes NADPH, the antioxidant glutathione cannot be regenerated, exacerbating the oxidative stress. These free radicals and reduced anti-oxidants cause alcohol-related diseases. Also, a simplified explanation for how you become a habitual drinker (which also tends to lead to drinking increasing amounts of alcohol) is that the more you drink, the more efficient this ethanol-clearing system becomes, and you begin to be able to drink more before you notice the effects of the alcohol. This is a compelling explanation of the dose region of adverse effects of the J-shaped curve with high ethanol consumption, which shows increased risk of the same diseases which were prevented by low dose, could be the mechanism by which humans get habituated to ethanol. In other words, high doses of alcohol harm body and also makes you habitual drinker with increase tolerance to alcohol resulting in dependence. High doses of alcohol is not only responsible for various alcohol related diseases but also responsible for habituation to alcohol by induction of the P450 hepatic microsomal ethanol-oxidizing system.
_
An excellent and very recent updated meta-analysis of 34 prospective studies was published by Di Castelnuovo and associates to show the relationship between alcohol dosing and total mortality. The 34 studies in men and women included information on >1 million subjects and >94 500 deaths. The authors described a J-shaped relationship between alcohol intake and mortality in which after an initial reduction in mortality, as alcohol intake was increased, the curve reached a plateau and then demonstrated an increase in mortality at higher doses of alcohol. In the Di Castelnuovo updated meta-analysis, the lowest mortality was observed at 6 g of alcohol per day (approximately half a drink per day; relative risk=0.81; 95% confidence interval [CI], 0.80 to 0.83), but lower mortality compared with zero alcohol consumption was observed with up to ≈4 drinks per day. Differences in response by sex existed, in that whereas up to 4 drinks per day in men was protective, only up to 2 drinks per day in women was protective. Doses of alcohol of >4 drinks per day in men and >2 in women were associated with an increase in mortality. Maximum protection was 17% in men and 18% in women. The basic shape of the curves persisted after adjustment for confounding variables. The authors concluded that low levels of alcohol intake were “inversely associated with total mortality in both men and women.” The authors speculated on why this inverse association disappears at a lower dose in women than in men. Possibilities included an increased risk of cancer in women. In addition, for equal amounts of alcohol consumption, women are exposed to a higher blood level of alcohol compared with men, perhaps because of differences in the way alcohol is metabolized between women and men (women have lower gastric alcohol dehydrogenase activity). Additionally, the benefits of alcohol on total mortality in women may be blunted by the fact that premenopausal women have a low incidence of coronary artery disease mortality.
_
Overall Mortality: J shaped curve to linear curve:
The overall impact of alcohol consumption on mortality can be assessed in two ways (Rehm and Bondy 1998): (1) by conducting meta-analyses using epidemiologic studies that examine all factors contributing to mortality, or (2) by combining risk for various alcohol-caused diseases with a weighted prevalence or incidence of each respective disease.
The meta-analysis approach to assessing overall mortality was used by researchers to examine the results of 16 studies, 10 of which were conducted in the United States (English et al. 1995). In this overview, researchers found the relationship between alcohol intake and mortality for both men and women to be J-shaped curves: the lowest observed risk for overall mortality was associated with an average of 10 grams of alcohol (less than one drink) per day for men and less for women. An average intake of 20 grams (between one and two drinks) per day for women was associated with a significantly increased risk of death compared with abstainers. The risk for women continued to rise with increased consumption and was 50 percent higher among those consuming an average of 40 grams of alcohol (between three and four drinks) per day than among abstainers. Men who averaged 30 grams of alcohol (two drinks) per day had the same mortality as abstainers, whereas a significant increase in mortality was found for those consuming at least 40 grams of alcohol per day. The effect found in this evaluation—that, in industrialized countries, low to moderate drinking is associated with reduced overall mortality— holds true in more recent research in which epidemiologists adjusted statistically for the “unhealthy abstainer” effect. Including former drinkers in abstainer groups also can influence, and confound, the shape of the curve used to describe the relationship between alcohol intake and mortality (Fillmore et al. 1998a,b; Leino et al. 1998). The proposed J-shaped relationship between alcohol intake and mortality does not apply in all cases, however. For example, because most of the physiologic benefit of moderate drinking is confined to ischemic cardiovascular conditions, such as CHD, in areas of the world where there is little mortality from cardiovascular diseases, alcohol provides little or no reduction in overall mortality. Rather, the relationship between intake and all-cause mortality assumes more of a direct, linear shape (Murray and Lopez 1996c), with increasing consumption associated with higher overall mortality. The same holds true for people under age 45, who have little ischemic cardiovascular mortality (Andréasson et al. 1988, 1991; Rehm and Sempos 1995a). Alcohol consumption is believed to have mixed effects on health:
• Risk of various cancers, hypertension, liver disease, and accidents and violence all increase with increasing alcohol consumption
• Risk of ischaemic heart disease is lower in moderate drinkers than nondrinkers
In people with substantial risk of dying from ischaemic heart disease (compared with these other causes), overall mortality is therefore lower among moderate drinkers than among non-drinkers – the so-called “J-shaped curve”. However, drinking patterns and disease incidence rates vary with age and sex. In young people, ischaemic heart disease is rare while accidents and violence are relatively common, so the left arm of the J may disappear altogether as seen in the figure below.
_
Do drinkers live longer than non-drinkers?
A recent study shows that people who have never taken a drink in their lives will die prematurely, while those who drink in moderation will live longer. It does seem strange, but there may be a good explanation for this startling information. According to Time magazine, Alcoholics Anonymous has an explanation. Those who take part in studies as abstainers are actually former hard-core drunks who have already incurred a number of alcohol-related health problems. But surprisingly, a paper published in the journal, Alcoholism: Clinical and Experimental Research, detailed a study conducted by psychologist Charles Holahan and a team of scientists at the University of Texas at Austin, that showed people who drank in moderation lived longer that non-drinkers. The tightly controlled study followed 1,824 people, ages 55 to 65 and lasted twenty years. It also took into consideration a number of variables, including socioeconomic status, physical activity, number of friends, as well as several other factors. The study was divided into three groups, abstainers, moderate drinkers and heavy drinkers. Abstainers were identified as people who never drank, or those who had drank in the past, but stopped drinking. Heavy drinkers were defined as those who drank 4 or more drinks daily. Moderate drinkers consumed one to three drinks a day. After 20 years, the study revealed that moderate drinkers had the lowest mortality rate, while heavy drinkers actually lived longer than non-drinkers, who had the highest mortality rate. In percentages, 69 percent of non-drinkers died prematurely, compared to 41 percent of moderate drinkers. Heavy drinkers came out much better than the abstainers, with a 60 percent mortality rate. Among the teetotalers, only 31 percent survived to the end of the 20th year. Among the heavy drinkers, 40 percent, and the moderate drinkers, 59 percent. While the researchers don’t have an explanation for their findings, an article from Time magazine offers a couple of theories. Firstly, non-drinkers tend to be in a lower socioeconomic class because drinking can be costly, especially in social settings such as at pubs and bars. There is a known connection between being poor and a lower life expectancy. Secondly, if moderate drinking involves red wine, that might account for a slightly longer life because of the associated heart health benefits of resveratrol. And while Alcoholics Anonymous offers one explanation, mainly that many teetotalers used to be alcoholics who have incurred past health problems, the Time article points out that the researchers accounted for this variable in their study. Teetotalers, regardless of whether they used to be alcoholics, still had a lower life expectancy than moderate and heavy drinkers.
_
Nondrinkers may have higher mortality risk than light drinkers, but reasons for abstaining make a big difference:
As a class, people who don’t drink at all have a higher mortality risk than light drinkers. But nondrinkers are a diverse bunch, and the reasons people have for abstaining affects their individual mortality risk, in some cases lowering it on par with the risk for light drinkers, according to a University of Colorado study. “Among nondrinkers, people have all sorts of background reasons for why they don’t drink,” said sociology Professor Richard Rogers, director of CU-Boulder’s Population Program in the Institute of Behavioral Science. “We wanted to tease that out because it’s not really informative to just assume that nondrinkers are a unified group.” For the new study, published in issue of the journal Population Research and Policy Review, Rogers and his colleagues relied on data collected in 1988 by the National Health Interview Survey about the drinking habits of more than 41,000 people from across the United States. The researchers also had access to information about which respondents died between taking the survey and 2006. During the survey, nondrinkers were asked to provide their reasons for not drinking. Possible answers ranged from “don’t socialize very much” to “not to become alcoholic” to “religious or moral reasons.” The research team divided nondrinkers into three general categories: “abstainers,” or people who have never had more than 12 drinks in their lives; “infrequent drinkers,” or people who have fewer than 12 drinks a year; and “former drinkers.” Each category was further divided using a statistical technique that grouped people together who gave similar clusters of reasons for not drinking. The team then calculated the mortality risk for each subgroup compared with the mortality risk for light drinkers, and they found that the risks varied markedly. Abstainers who chose not to drink for a cluster of reasons that included religious or moral motivations, being brought up not to drink, responsibilities to their family, as well as not liking the taste, had similar mortality risks over the follow-up period to light drinkers. “So this idea that nondrinkers always have higher mortality than light drinkers isn’t true,” Rogers said. “You can find some groups of nondrinkers who have similar mortality risks to light drinkers.” The scientists also found that infrequent drinkers generally had a slightly higher mortality risk than light drinkers. Former drinkers, however, had the highest mortality risk of all nondrinkers. Former drinkers whose cluster of reasons for not drinking now included being an alcoholic and problems with drinking, for example, had a 38 percent higher mortality risk than light drinkers over the follow-up period. By comparison, people who drink between one and two drinks per day, on average, have a 9 percent higher mortality rate than light drinkers, while people who drink between two and three drinks per day have a 49 percent higher mortality. People who consume more than three drinks per day had a 58 percent higher mortality risk over the follow-up period compared with light drinkers. Despite confirming that some subgroups of nondrinkers have a higher mortality rate than light drinkers, it doesn’t necessarily follow that those people’s mortality rates would fall if they began drinking, Rogers said. For example, people who were problem drinkers in the past might increase their mortality risk further by starting to drink again. Also, people who don’t drink at all, as a group, have lower socioeconomic characteristics than light drinkers, which could be one of the underlying causes for the mortality differences, Rogers said. In that case, starting to drink without changing a person’s socioeconomic status also would not likely lower mortality rates. “I think the idea that drinking could be somewhat beneficial seems like it’s overstated,” Rogers said. “There may be other factors that lower mortality for light drinkers. It’s not just the act of drinking.”
_
_
A Sobering Look at Alcohol: 10-Year study finds High Death Rate:
A study of thousands of alcoholics found their death rate, from a host of different causes, was significantly higher than that of the population. A number of studies in the past few years have suggested health benefits from drinking small or moderate amounts of alcohol. This can encourage people to look at alcohol almost as if it’s medicine. A recent study of alcohol use in Italy paints a much more sobering picture. Following over 2,000 alcoholics in Tuscany for an average of 10 years, the study found they had a much higher death rate from a host of different causes, including cancer, than the general population. Death rates from infections, diabetes, diseases of the immunological, nervous, cardiovascular, respiratory, and digestive systems, and violent causes all were elevated, as were death rates from many types of cancer. And while women in the study fared better than men, they still fared worse than the rest of the population. It’s hardly news that alcoholism is bad for the health. But few studies have examined these effects in such detail and in such a large population. The study’s take home message about alcohol: less is better. This message isn’t just for alcoholics, it’s for anyone who drinks. And it’s especially important with holiday season approaching, when people tend to drink more than usual. The study shows in great detail that extreme drinking leads to extreme health problems. And studies of more moderate drinking don’t contradict its findings. Alcohol is estimated to be responsible for four percent of all deaths and five percent of all diseases worldwide. People who’ve heard that one drink a day might be good for the heart should also remember that just a bit more is known to increase the risk of 60 diseases and 14 cancers. Two studies published in 2009 offer some very specific findings on the effect of more moderate drinking on health. The Zutphen Study looked at the effects of alcohol consumption on over 1,000 men in a small town in the Netherlands for 40 years. It found that men who drank sparingly had a longer life expectancy than those who didn’t drink at all. Wine worked best; men who drank an average of 0.7 ounces of wine daily lived about 2.5 years longer than those who drank beer or liquor and five years longer than non-drinkers. Taking this study to heart and trying to drink 0.7 ounces of wine daily, the first step would be finding a glass small enough to allow you to do so. In contrast, the aptly named Million Women Study looked at the effect of drinking on cancer in over one million women in the U.K. It found that any alcohol consumption at all increased their cancer risk over the next seven years. The more alcohol they drank, the higher their cancer risk. On average, the women in the study had a single drink per day. It’s not that studies showing health benefits from small amounts of alcohol are wrong; it’s just that that’s not how most people do drink. And the way many people drink damages their health. The Italian study, while it looks at extreme drinking, is a reminder of this.
_
True alcohol related mortality is the difference between deaths prevented and death caused by alcohol:
A report of the United States Centers for Disease Control estimated that medium and high consumption of alcohol led to 75,754 deaths in the U.S. in 2001. Low consumption of alcohol had some beneficial effects, so a net 59,180 deaths were attributed to alcohol. The effects of low-to-moderate alcohol consumption on mortality are age-dependent. Low-to-moderate alcohol use increases the risk of death for individuals aged 16-34 (due to increased risk of cancers, accidents, liver disease, and other factors), but decreases the risk of death for individuals ages 55+ (due to decreased risk of ischemic heart disease).
_
Alcohol causes more deaths than prevented.
_________
Alcohol and pregnancy:
Consequences of drinking alcohol in pregnancy:
The repeated ingestion of high doses of ethanol by women can result in amenorrhea, a decrease in ovarian size, absence of corpora lutea with associated infertility, and an increased risk of spontaneous abortion. Alcohol is a teratogen which may affect the development of a fetus. Alcohol passes freely through the placenta and reaches concentrations in the fetus that are as high as those in the mother. The fetus has limited ability to metabolise alcohol. Alcohol and acetaldehyde can damage developing fetal cells. Alcohol can also impair placental/fetal blood flow, leading to hypoxia. Miscarriage and stillbirth are among the consequences of alcohol exposure in pregnancy. In the child, alcohol exposure in pregnancy can result in prematurity, brain damage, birth defects, growth restriction, developmental delay and cognitive, social, emotional and behavioural deficits. As the child grows, the social and behavioural problems associated with alcohol exposure in pregnancy may become more apparent. Intellectual and behavioural characteristics in individuals exposed to alcohol in pregnancy include low IQ, inattention, impulsivity, aggression and problems with social interaction.
_
Evidence of risk:
The amount of alcohol that is safe for the fetus has not been determined. Damage to the fetus is more likely to occur with high amounts of alcohol and, of particular risk, is a pattern of drinking in which high amounts of alcohol are consumed on any one occasion. There is controversy about the consequences of low to moderate alcohol consumption in pregnancy. Some studies, though not all, show links between lower amounts of alcohol and low birth weight, miscarriage, stillbirth, birth defects, developmental and neurobehavioural problems. Research on the relationship between alcohol consumption during pregnancy and child outcomes is complicated by multiple prenatal, postnatal and childhood factors and the difficulty of obtaining accurate information on the level of alcohol exposure. The relationship between alcohol consumption and risk is one of dose response, not one in which there is a threshold of consumption over which damage to the fetus occurs. Not all children exposed to alcohol during pregnancy will be affected or affected to the same degree, and a broad range of effects is possible. The level of harm is related to the amount of alcohol consumed, the frequency of the consumption and the timing of the exposure. The effects of alcohol use in pregnancy on the fetus are also influenced by a number of other factors such as the general health and nutritional status of the mother, genetic factors, socio-economic status, other drug use, psychological wellbeing and combinations of these factors. The level of risk to the fetus is hard to predict.
_
Amount and frequency of consumption and timing of exposure:
The amount of alcohol consumed, and the frequency and timing of consumption all play a part in the manifestation and variation of adverse effects on the fetus. All types of alcoholic beverages can be harmful during pregnancy, and the risk to the fetus is proportional to the amount of alcohol consumed. Frequent heavy drinking poses the highest risk for detrimental effects on the fetus and damage is more likely to occur with high blood alcohol levels. Five or more standard drinks per occasion is associated with increased risk for the fetus. There is no safe time to drink alcohol during pregnancy. Alcohol exposure can have consequences for the development of the fetus throughout pregnancy and variation in effects can be due to the stage of development of the fetus at the time of exposure. There is no known level of alcohol consumption in pregnancy below which no damage to a fetus will occur. Women should therefore be advised that, no alcohol in pregnancy is the safest choice.
_
Fetal Alcohol Spectrum Disorder (FASD):
Fetal Alcohol Spectrum Disorder (FASD) is a general term that was introduced in 2004 describing the range of effects that can occur in an individual who was exposed to alcohol during pregnancy. The effects include physical, mental, behavioural and learning disabilities with possible life-long implications. In the United States, the estimated rate of FASD is 1in 100 live births. FASD is not a diagnostic term. It represents a spectrum of disorders and includes the diagnostic terms of Fetal Alcohol Syndrome (FAS), Alcohol Related Birth Defects (ARBD) and Alcohol Related Neurodevelopmental Disorder (ARND).
Children with diagnoses included under the general term of FASD often have:
• brain damage
• birth defects
• poor growth
• developmental delay
• difficulty hearing
• difficulty sleeping
• problems with vision
• high levels of activity
• difficulty remembering
• a short attention span
• language and speech deficits
• low IQ
• problems with abstract thinking
• poor judgment
• social and behavioural problems
• difficulty forming and maintaining relationships.
_
The epidemiological methods used to study the prevalence and characteristics of FAS, ARBD, and ARND have progressed substantially since the initial studies in the mid-1970s. Useful findings about the prevalence, patterns, and characteristics of risk factors for FAS have improved substantially, leading to the development of a general profile of those mothers who are most likely to have a child with prenatal alcohol dam-age. The overall prevalence of FAS in the United States was estimated by the Institute of Medicine to be between 0.5 and 3.0 per 1,000 births. Based on the review which has the advantage of more recent studies, authors believe that FAS prevalence in the general population of the U. S. can now be estimated to be between 0.5 and 2 per 1,000 births, and the prevalence of FAS and ARBD combined is likely to be at least 10 per 1,000, or 1 percent of all births. This rate is too high for any population to accept.
_
Fetal alcohol syndrome (FAS):
Fetal alcohol syndrome (FAS) is a pattern of mental and physical defects that can develop in a fetus in association with high levels of alcohol consumption during pregnancy. Alcohol crosses the placental barrier and can stunt fetal growth or weight, create distinctive facial stigmata, damage neurons and brain structures, which can result in mental retardation and other psychological or behavioral problems, and also cause other physical damage. The main effect of FAS is permanent central nervous system damage, especially to the brain. Developing brain cells and structures can be malformed or have development interrupted by prenatal alcohol exposure; this can create an array of primary cognitive and functional disabilities (including poor memory, attention deficits, impulsive behavior, and poor cause-effect reasoning) as well as secondary disabilities (for example, predispositions to mental health problems and drug addiction). Alcohol exposure presents a risk of fetal brain damage at any point during a pregnancy, since brain development is ongoing throughout pregnancy. FAS should not be confused with Fetal Alcohol Spectrum Disorders (FASD), a condition which describes a continuum of permanent birth defects caused by maternal consumption of alcohol during pregnancy, which includes FAS, as well as other disorders, and which affects about 1% of live births in the US (i.e., about 10 cases per 1000 live births). The lifetime medical and social costs of FAS are estimated to be as high as US$800,000 per child born with the disorder. Surveys found that in the United States, 10–15% of pregnant women report having recently drunk alcohol, and up to 30% drink alcohol at some point during pregnancy. The current recommendation of the Surgeon General of the United States, the British Department of Health and the Australian Government National Health and Medical Research Council is to drink no alcohol at all during pregnancy.
_
The figure below shows facial characteristics that are associated with fetal alcohol exposure:
_
_
Heavy drinking during pregnancy results in the rapid placental transfer of both ethanol and acetaldehyde, which may have serious consequences for fetal development. One severe result is the fetal alcohol syndrome (FAS), seen in 5% of children born to heavy-drinking mothers, which can include any of the following: facial changes with epicanthal eye folds; poorly formed ear concha; small teeth with faulty enamel; cardiac atrial or ventricular septal defects; an aberrant palmar crease and limitation in joint movement; and microcephaly with mental retardation. The amount of ethanol required and the time of vulnerability during pregnancy have not been defined, making it advisable for pregnant women to abstain completely.
_
_
Drinking ethanol while pregnant is the same as feeding ethanol to the baby. Since ethanol freely mixes with the body water through diffusion, it is rapidly distributed into the blood. Since the mothers blood circulation is connected to that of the fetus, the alcohol is rapidly transported to the fetus to be distributed in the cells and tissues of the infant and into the fluid surrounding the fetus. Once distributed, alcohol has the opportunity to directly influence the growth and development of the child. Alterations by ethanol in the function of growth factors and other chemical mediators known to be important in guiding the development of the fetus have in fact been amply demonstrated. Ethanol can also influence fetal development indirectly by exerting effects on the mother, which in turn influence the fetus. These indirect effects can include altering the nutritional status of the mother so that the fetus gets less nutrition; altering the function of the placenta, so that fewer nutrients and/or oxygen gets to the fetus; producing metabolites of ethanol such as acetaldehyde, which is known to be toxic; and compounding the effects of other drugs (therapeutic and nontherapeutic) that mother might be taking. Each of these possibilities has been the focus of extensive investigation in both animal and human studies (10th Special Report to the U.S. Congress on Alcohol and Health, 2000). The degree of damage incurred by the fetus is influenced by several factors, including the period of gestation when alcohol exposure occurs, how much the mother drinks during pregnancy, the pattern and timing of her drinking, and the genetic makeup of both mother and child. Because of these factors and others, it is not possible to know what level of drinking is safe for each individual, and so abstinence is recommended to all women who are pregnant, nursing, or who may become pregnant. Recent studies have shown several risk factors for delivering alcohol-affected children. These include alcohol consumption during pregnancy (and specifically, binge drinking, maternal age > 25, low socioeconomic status, unemployment, living in a culture that is tolerant of heavy drinking, social transience, and being separated, divorced or never married (May, 1995).
_
_
The manifestations of Prenatal Exposure to Alcohol fall on a continuum from severely affected (including death) to near normalcy. The most severely affected show:
- 1. particular craniofacial patterns
- 2. pre-and/or postnatal growth deficiencies
- 3. central nervous system dysfunctions
- 4. psychiatric disturbances; and
- 5. impairments in psychosocial skills.
_
_
MRI of brain of children affected with FAS:
_
A novel suppressive effect of alcohol dehydrogenase 5 in neuronal differentiation:
Alcohol dehydrogenase 5 (ADH5) is a widely conserved enzyme for alcohol and aldehyde metabolism in mammals. Despite dynamic expression throughout neurogenesis, its role in neuronal development remains unknown. Here authors present the first evidence that ADH5 is a negative regulator of neuronal differentiation. Gene expression analyses identify a constant reduction of ADH5 levels throughout neuronal development. Overexpression of ADH5 reduces both development and adult neuronal differentiation of mouse neurons. This effect depends on the catalytic activity of ADH5 and involves ADH5 mediated denitrosation of histone deacetylase 2 (HDAC2). The results indicate that ADH5 counteracts neuronal differentiation of human neural stem cells, and that this effect can be reversed by pharmacological inhibition of ADH5. Based on these observations, authors propose that ADH5 is a novel suppressor of neuronal differentiation and maturation. Inhibition of ADH5 may improve adult neurogenesis in a physiological or pathological setting.
_
Important corollary is that neurobiological pathology of fetal alcohol syndrome is due to increased activity of ADH 5 in fetal brain due to exposure of fetal brain to alcohol resulting in retarding neuronal development & differentiation.
_
Alcohol and lactation:
Risky or daily intake of alcohol is not recommended for any breastfeeding mother due to issues relating to the care of the infant and the risk of conditions that make up FASD for a subsequent pregnancy. Alcohol consumed by the mother passes into her bloodstream and her breast milk. Alcohol levels in the breast milk are similar to the blood alcohol levels of the mother at the time of feeding. The effect on the infant can be sedation, irritability and weak sucking. Alcohol consumption can also lead to decreased milk supply and milk odour. The Australian Guidelines to Reduce Health Risks from Drinking Alcohol state that for women who are pregnant, are planning a pregnancy or are breastfeeding, “not drinking is the safest option”. Excessive consumption of alcohol can affect milk flow in breastfeeding mothers.
Adverse effects on infants who are breastfeeding can include:
• impaired motor development
• decrease in milk intake
• changes in sleep patterns
• risk of hypoglycaemia.
____________
Alcohol co-addictions:
_
The figure above shows that alcohol is the substance of youth in the America. However, many people who consume alcohol also consume tobacco and marijuana. So let me briefly overview co-addictions.
_
Alcohol and tobacco co-use:
Alcohol and tobacco are among the top causes of preventable deaths in the United States. Moreover, these substances often are used together: Studies have found that people who smoke are much more likely to drink, and people who drink are much more likely to smoke. Dependence on alcohol and tobacco also is correlated: People who are dependent on alcohol are three times more likely than those in the general population to be smokers, and people who are dependent on tobacco are four times more likely than the general population to be dependent on alcohol. Cigarette smoking slows gastric emptying and as a consequence delays alcohol absorption resulting in person drinking more alcohol to get the same pleasure and relaxation.
_
The link between alcohol and tobacco has important implications for those in the alcohol treatment field. Many alcoholics smoke, putting them at high risk for tobacco-related complications including multiple cancers, lung disease, and heart disease (i.e., cardiovascular disease). In fact, statistics suggest that more alcoholics die of tobacco-related illness than die of alcohol-related problems. Also, questions remain as to the best way to treat these co-occurring addictions; some programs target alcoholism first and then address tobacco addiction, whereas others emphasize abstinence from drinking and smoking simultaneously. Effective treatment hinges on a better understanding of how these substances—and their addictions—interact. Understanding just how alcohol and tobacco interact is challenging. Because co-use is so common, and because both substances work on similar mechanisms in the brain, it’s proving difficult to tease apart individual and combined effects of these drugs.
_
How prevalent are alcohol tobacco co-use?
_
_
The National Institute on Alcohol Abuse and Alcoholism’s (NIAAA’s) 2001–2002 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), which is one of the largest comorbidity studies ever conducted, included extensive questions about alcohol and tobacco use and related disorders. NESARC data confirmed the widespread use of alcohol with tobacco: Approximately 46 million adults used both alcohol and tobacco in the past year, and approximately 6.2 million adults reported both an AUD and dependence on nicotine. Alcohol and tobacco use varied according to gender, age, and ethnicity, with men having higher rates of co-use than women. Younger people tended to have a higher prevalence of AUDs, nicotine dependence, and co-use. Although Whites were more likely to drink alcohol, American Indians/Alaskan Natives were most likely to smoke, or to smoke and drink concurrently. Asians/Native Hawaiians/Pacific Islanders were least likely to smoke or drink, or smoke and drink concurrently. Comorbid mood or anxiety disorders are another risk factor for both alcoholism and nicotine dependence. NESARC data show that alcohol abuse is strongly correlated with a co-occurring mood or anxiety disorder. The presence of comorbid mental illness also raises risk for tobacco addiction. In another study, Williams and Ziedonis found that 50 to 90 percent of people with mental illness or addiction were dependent on nicotine.
_
Health risks associated with alcohol and tobacco co-use:
Alcohol and tobacco use may lead to major health risks when used alone and together. In addition to contributing to traumatic death and injury (e.g., through car crashes), alcohol is associated with chronic liver disease, cancers, cardiovascular disease, acute alcohol poisoning (i.e., alcohol toxicity), and fetal alcohol syndrome. Smoking is associated with lung disease, cancers, and cardiovascular disease. Additionally, a growing body of evidence suggests that these substances might be especially dangerous when they are used together; when combined, alcohol and tobacco dramatically increase the risk of certain cancers.
_
Biological and Genetic factors in alcohol tobacco co-use:
Why do tobacco and alcohol use co-occur so frequently? Clearly environmental factors contribute to the problem. Both drugs are legally available and easily obtained. Over the past two decades, however, it also has become clear that biological factors are at least partly responsible. Although tobacco and nicotine have very different effects and mechanisms of action, Funk and colleagues speculate that they might act on common mechanisms in the brain, creating complex interactions. These possible mechanisms are difficult to study because alcohol and nicotine can affect people differently depending on the amount of the drugs consumed and because numerous factors, including gender and age, influence the interaction between nicotine and alcohol. Still, a common mechanism might explain many of the interactions between tobacco and alcohol, as well as a possible genetic link between alcoholism and tobacco dependence.
Mutual craving:
Studies show that consuming tobacco and alcohol together can augment the pleasure users experience from either drug alone. For example, in a study by Barrett and colleagues, subjects were given either nicotine- containing or nicotine-free cigarettes and asked to perform progressively more difficult tasks in order to earn alcoholic beverages. The subjects who smoked nicotine-containing cigarettes worked harder and drank more alcohol than those smoking nicotine-free cigarettes. Conversely, Rose and colleagues showed that drinking alcohol enhances the pleasure reported from smoking cigarettes. This research is supported by animal studies, which show that nicotine-treated animals consumed more alcohol than did control animals.
A common brain system:
Evidence increasingly suggests that both alcohol and tobacco may act on the mesolimbic dopamine system, a part of the brain that is involved in reward, emotion, memory, and cognition. Brain cells (i.e., neurons) that release dopamine—a key brain chemical involved in addiction—have small docking molecules (i.e., receptors) to which nicotine binds. Evidence suggests that the interaction between alcohol and tobacco may take place at these nicotinic receptors. When nicotinic receptors are blocked, people not only tend to consume less nicotine but also less alcohol. This common mechanism of action may explain some of the interactions between alcohol and tobacco, including why alcohol and tobacco can cause users to crave the other drug and the phenomenon of cross-tolerance.
Neurotransmitter link between tobacco and alcohol:
Researchers have discovered “striking” new biochemical evidence explaining why so many alcoholics are also heavy smokers. Their report in the journal Neuroscience Letters says both alcohol and nicotine target the same cell sites in the nervous system, which may explain an underlying mechanism involved in both addictions. According to Toshio Narahashi, professor of pharmacology at Northwestern University Medical School in Chicago, nicotine stimulates and then deadens or desensitizes the nicotinic acetylcholine receptor site on nerve cells in the brain. “The acetylcholine receptor of the nicotine addict may be slightly desensitized, meaning that higher doses of alcohol are required to stimulate it,” Narahashi said. He and his colleagues point to research showing that about 10% of the U.S. population are heavy smokers, but among alcoholics, 70% to 90% are heavy smokers. The Chicago researchers say both nicotine and alcohol affect the same receptors at minute concentrations. Narahashi says the potent action of alcohol on acetylcholine receptors suggest that both substances interact at this site on nerve cells. “Our findings may also shed new light on the molecular mechanism of alcohol,” he said.
Tolerance and cross-tolerance:
A decrease in a person’s sensitivity to a drug’s effects often is referred to as tolerance. This phenomenon occurs when a person must consume more of a substance in order to achieve the same rewarding effect. In the case of alcohol and tobacco, this puts him or her at greater risk for developing dependence. Cross-tolerance—that is, when tolerance to one drug confers tolerance to another—also has been documented in people who smoke and drink.
Genetic factors:
Recent studies suggest that common genetic factors may make people vulnerable to both alcohol and tobacco addiction. Clearly, both alcohol and nicotine dependence runs in families. Identical twins (who share 100 percent of their DNA) are twice as likely as fraternal twins (who, like all siblings, share 50 percent of their DNA) to be nicotine and alcohol dependent if the other twin is dependent. And recently, the Collaborative Study on the Genetics of Alcoholism—the first study to examine the human genetic makeup (or genome) for regions that involve both alcohol dependence and smoking—has identified genes and regions of genes that may be involved in both AUDs and nicotine dependence. Davis and De Fiebre suggest that some overlap may exist between genes that code for sensitivity to alcohol and those that influence sensitivity to nicotine. People may be more or less sensitive to alcohol and tobacco’s effects because of natural genetic variations in the number and type of nicotinic receptors that they possess.
_
Twin studies on alcohol tobacco co-use:
While many observers have noted that alcoholics smoke very heavily, the reasons for this dual substance use have been poorly understood. Recent twin studies are shedding considerable light on the reasons for this phenomenon. In one such study, researchers analyzed tobacco and alcohol use versus nonuse in a sample of 2,612 adolescent and young adult Dutch twin pairs (Koopmans et al. 1997). At all ages tested (12 through 25 years), regular alcohol use was highly correlated with regular tobacco use. For 12- to 16-year-olds, shared environmental factors were the principal influence on both alcohol and tobacco use. The same environmental factors (peer pressure very likely prominent among them) influenced both smoking and drinking. For 17- to 25-year-old men, both alcohol and tobacco use were highly genetically determined, with shared environmental influences playing a significant but lesser role. For 17- to 25-yearold women, alcohol use was highly genetically determined, and tobacco use was influenced by both genetic and shared environmental factors. The same genetic factors influenced both alcohol and tobacco use, both in young adult men and women. These findings suggest that while initial exposure to alcohol and nicotine is environmentally influenced, persistence in using these substances is under strong shared genetic influence. Other investigators analyzed alcohol and tobacco use in 173 adult male MZ twin pairs and 183 adult male DZ twin pairs from the U.S. World War II Era Veteran Twin Registry (Swan et al. 1996). In this sample, both alcohol and tobacco consumption were approximately equally influenced by genetic and shared environmental factors. Correlations between alcohol and tobacco use were largely explained by a common genetic factor influencing use of both substances. There were also specific genetic factors influencing the use of either substance individually. Environmental factors influencing alcohol use were apparently different from those influencing tobacco use. These observations applied to the average range of alcohol and tobacco use, not heavy use. The same investigators analyzed heavy alcohol use (more than 67 drinks per month) and heavy tobacco use (more than 30 cigarettes per day) in a sample of 749 MZ twin pairs and 1,267 DZ twin pairs from the same registry (Swan et al. 1997). The threshold for heavy substance use was set at the top 20 percent of the range of quantity consumed, excluding nonusers from the distribution. This study demonstrated a common genetic influence on both heavy alcohol use and heavy tobacco use as well as genetic influences specific to the heavy use of each substance individually. The physiologic mechanism of the shared genetic influence on alcohol and tobacco consumption is currently a matter of speculation, as illustrated by the following two hypotheses: Individuals with high reactivity to stress may use both substances for stress relief. Alternatively, use of either substance may induce physiologic tolerance to the other, leading to a need to consume greater amounts of the latter substance in order to experience a subjective effect. Independent twin studies have identified a shared genetic influence between alcoholism and depression (Kendler et al. 1993a), as well as between smoking and depression (Kendler et al. 1993b). The shared genetic influence on smoking and drinking could thus be related to their respective connections to depression. One study analyzed the relationship between tobacco use and perceived intoxication after consumption of a controlled dose of alcohol in a small sample of Australian twins (194 pairs) (Madden et al. 1997). This exploratory study suggested a complex genetic relationship in women between use of and responses to alcohol and tobacco. There appear to be at least two independent genetic factors involved, one influencing both alcohol and tobacco use, and another influencing smoking and feelings of intoxication after alcohol use but not alcohol use itself. The investigators found that subjects who smoked felt less intoxicated than those who did not. Further laboratory studies are needed to elucidate the biochemical and pharmacologic basis of this finding. The negative genetic correlation between smoking and sensitivity to alcohol, combined with Schuckit’s observations that reduced sensitivity to alcohol predicts greater risk of alcoholism (Schuckit 1998), suggests that smoking may increase risk of alcoholism by reducing smokers’ sensitivity to alcohol. The results of twin studies on smoking and drinking thus suggest that efforts toward prevention and treatment of alcohol abuse may benefit from inclusion of efforts to abate tobacco use.
_
Alcohol and cocaine:
A common but particularly dangerous partnership, alcohol and cocaine together increase the risk of heart attacks and fits and even sudden death. The two drugs interact to produce a highly toxic substance in your liver called cocaethylene. It can increase the depressive effects of alcohol, making your reaction to the cocaine stronger. You are also more likely to be aggressive with cocaethylene in your system. Cocaethylene takes longer to get out of your system than either the alcohol or the cocaine, subjecting your heart and liver to a longer period of stress. Mixing alcohol and cocaine can be fatal up to 12 hours after you have taken it.
_
Alcohol and marijuana (cannabis):
If you use cannabis and alcohol together, the results are both physical and psychological and can be unpredictable. Having alcohol in your blood can potentially cause your body to absorb the active ingredient tetrahydrocannabinol (THC) faster. This can lead to the cannabis having a much stronger effect than it would normally have. Physically, you can experience dizziness, nausea and vomiting. Psychological effects include panic, anxiety or paranoia. Skunk, a term for stronger types of cannabis, can pose even greater risks, because it may contain three times as much THC. There is a serious long-term risk to your health too. Cannabis is usually smoked with tobacco, which can cause cancer. Tobacco and alcohol work together to damage the cells of the body, multiplying the damage. Alcohol makes it easier for the mouth and throat to absorb the cancer-causing chemicals in tobacco.
__
_
Alcohol and ecstasy (MDMA):
It is possible that alcohol will deaden the high you feel from ecstasy while the drugs are in your system. But the next day, when you come down, you will feel much worse if you have been drinking alcohol. A severe hangover is one of the milder side-effects of combining these drugs though together they can be deadly. Ecstasy dehydrates you. So does alcohol. You risk overheating and becoming dangerously dehydrated when you combine the two. Alcohol is involved in most ecstasy related deaths, many of which are from heatstroke after people have danced for long periods of time in hot clubs without replacing the fluids they have lost by drinking water. As alcohol is a diuretic, which means it makes you go to urinate more, it is even harder to keep enough fluid in your body when you drink it while on ecstasy.
_
Alcohol and amphetamines (speed):
The effects of amphetamines are very much like an adrenalin rush. When you take it, your breathing, blood pressure and heart rate speed up. Like ecstasy, speed can also increase your body temperature and cause dehydration which is heightened when you add alcohol. As speed already puts pressure on your heart, if you add alcohol, that pressure can be fatal. Alcohol can intensify your emotions and make you lose your inhibitions. So can speed. Combine the two and you may end up behaving in a way you seriously regret. Under the influence of speed you may feel more confident or energised, but you can easily become agitated, paranoid or aggressive, particularly when you put alcohol in the mix. Mixing the two means you can drink dangerous amounts without realizing.
_
Alcohol and heroin:
Alcohol with heroin is one of the most dangerous combinations of drugs. The National Treatment Agency for Substance Misuse says that even small amounts of alcohol seem to lower the amount of heroin needed to fatally overdose. Around three quarters of people who die from heroin overdoses have drunk alcohol.
_
Alcohol and legal high:
Previously known as legal high, drugs such as Mephedrone actually became illegal in 2010 when they were classified as class B drugs. A powerful stimulant, Mephedrone is part of the cathinone family, a group of drugs that are closely related to the amphetamines. They are derived from the plant khat, commonly used as a stimulant in East Africa and have similar effects to ecstasy and speed. These drugs can over stimulate circulation, damaging the heart, speed up the nervous system and cause fits. They can also make you anxious and paranoid. As with any drug that gives a high, combine them with alcohol and you are at risk of everything from nausea and vomiting to coma and death.
____________
Alcohol and medicines:
Harmful Interactions: Mixing Alcohol with Medicines:
Mixing alcohol and a medication puts you at risk for dangerous reactions. Protect yourself by avoiding alcohol if you are taking a medication and don’t know its effect. To learn more about a medicine and whether it will interact with alcohol, talk to your pharmacist or health care provider. You’ve probably seen this warning on medicines you’ve taken. The danger is real. Mixing alcohol with certain medications can cause nausea and vomiting; headaches; drowsiness; fainting; loss of coordination; and can put you at risk for internal bleeding, heart problems, and difficulties in breathing. Alcohol also can decrease the effectiveness of a medication or make it totally ineffective. Many of these medications can be purchased “over-the-counter” without a prescription, including herbal remedies and others you may never have suspected of reacting with alcohol. Many types of medication can make you sleepy. Taking these medicines while drinking can make you even more drowsy, dizzy, and lightheaded. You may have trouble concentrating or performing mechanical skills. Mixing alcohol with certain medicines makes it dangerous for you to drive. Combining alcohol with some medicines can lead to falls and serious injuries, especially among older people. Some medications, including many popular painkillers and cough, cold, and allergy remedies, contain more than one ingredient that can react with alcohol. Read the label on your medication bottle to find out exactly what ingredients it contains. Certain medicines contain up to 10 percent alcohol. Cough syrup and laxatives have some of the highest alcohol concentrations. Women and older people are at higher risk for harmful alcohol medication reactions. Alcohol and medicines can interact harmfully even if they are not taken at the same time.
_
| Symptoms/ Disorders |
Common medications and selected brand names |
Some possible reactions with alcohol |
| Angina (chest pain), coronary heart disease | isosorbide, nitroglycerine | Rapid heartbeat, sudden changes in blood pressure |
| Anxiety/insomnia | Alprazolam, clonazepam, diazepam, lorazepam | Drowsiness, dizziness; increased risk for overdose |
| Blood clots | warfarin | Occasional drinking may lead to internal bleeding; heavier drinking may have the opposite effect, resulting in possible blood clots, strokes, or heart attacks |
| Colds, coughs, flu, allergies | Diphenhydramine, chlorpheniramine, codeine | Drowsiness, dizziness; increased risk for overdose |
| Depression | Amitriptyline, clomipramine, desipramine, nefazodone, trazodone | Drowsiness, dizziness; increased risk for overdose |
| Diabetes | Glyburide, metformin, tolbutamide | Rapid heartbeat, sudden changes in blood pressure; convulsions, coma, death |
| Heartburn, indigestion, sour stomach | Cimetidine, nizatidine, ranitidine, metoclopramide | Rapid heartbeat, sudden changes in blood pressure (metoclopramide); increased alcohol effect |
| Infections | Griseofulvin, metronidazole, nitrofurantoin, sulfamethoxazole, isoniazid, cycloserine | Rapid heartbeat, sudden changes in blood pressure; liver damage (isoniazid) |
| Muscle pain | Carisoprodol, cyclobenzaprine | Drowsiness, dizziness; increased risk of seizures; increased risk for overdose |
| Nausea, motion sickness | Meclizine, hydroxyzine, promethazine) | Drowsiness, dizziness; increased risk for overdose |
| Pain such as that from headache, fever, muscle ache, arthritis; inflammation& | NSAIDs like aspirin, ibuprofen etc | Stomach upset, bleeding and ulcers; liver damage (acetaminophen); rapid heartbeat |
| Seizures | Clonazepam, Phenobarbital, phenytoin | Drowsiness, dizziness; increased risk of seizures |
| Herbal preparations (Chamomile, Valerian, Lavender) | Increased drowsiness |
_
Alcohol must not be used during the following medications’ administration:
– Anticoagulants
– Medication for diabetes
– Beta blockers
– Antihistamines
– Antibiotics
– Antidepressants
– Pain relievers
– Sleeping pills
_______________
Alcohol Use and Sexual Behavior:
In the past two decades, over 600 studies have investigated the association between using alcohol and having sex (Cooper, 2006). The majority of studies have found a positive association (Cooper, 2002, 2006; Leigh & Stall, 1993), although most have used purely cross-sectional, between-subjects, and correlational designs (Cooper, 2006; Cooper & Orcutt, 2000; Leigh & Stall, 1993). Emerging adults commonly consume alcohol before having sex (Cooper, Peirce, & Huselid, 1994): estimates range from ¼ to more than ½ of people at the most recent sexual occasion (Desiderato & Crawford, 1995; MacNair-Semands & Simono, 1996). Hingson et al. (2005) estimated that 8% of U.S. college students aged 18 to 24 (474,000 people) have unprotected sexual intercourse resulting from alcohol use annually. In addition, students tend to overestimate the number of drinks they can consume without experiencing negative consequences such as unwanted sex (Mallett, Lee, Neighbors, Larimer, & Turrisi, 2006). However, a more complete picture of the associations between alcohol use and sexual behaviors within-persons and across occasions is required to understand whether a link between alcohol and sex is prevalent and whether it is perceived as rewarding (i.e., experienced positive sex consequences) or not (i.e., negative sex consequences). The perceived consequences of sex after drinking have particular relevance for the potential reinforcement of alcohol-sex expectancies and the perpetuation of both alcohol use and sexual behaviors. Alcohol use may lead to sex directly through disinhibition (Kaly, Heesacker, & Frost, 2002; MacDonald, MacDonald, Zanna, & Fong, 2000; Steele & Josephs, 1990). Alcohol myopia theory, for example, states that the acute disinhibitory effects of alcohol reduce ability to process complex information (such as long-term goals), thus allowing immediate and salient goals (such as sexual arousal) to influence behavior more strongly (Cooper, 2002; Dermen & Cooper, 2000; Steele & Josephs, 1990). Conversely, the desire to engage in sexual behavior may lead to heavier drinking because of the belief that alcohol favorably influences sexuality (Abbey et al., 1999; Goldman & Roehrich, 1991). Based on alcohol expectancy theory (Cooper, 2002; Dermen & Cooper, 2000), one of the reasons some college students use alcohol is their expectation that alcohol facilitates sexual drive and sexual affect (Abbey et al., 1999) and decreases sexual inhibitions (Kotchick, Shaffer, Forehand, & Miller, 2001). An analysis of interviews with sexually active women, for example, revealed that about half had used alcohol or drugs instrumentally to make sex more likely to occur (Taylor, Fulop, & Green, 1999). Alcohol consumption has a number of effects on sexual behavior. The effects of alcohol are balanced between its suppressive effects on sexual physiology, which will decrease sexual activity, and its suppression of psychological inhibitions, which will increase the desire for sex.
_
Alcohol and sex in men:
Men’s sexual behaviors can be affected dramatically by alcohol. Both chronic and acute alcohol consumption have been shown in most but not all studies to inhibit testosterone production in the testes. This is believed to be caused by the metabolism of alcohol reducing the NAD+/NADH ratio both in the liver and the testes; since the synthesis of testosterone requires NAD+, this tends to reduce testosterone production. As testosterone is critical for libido and physical arousal, alcohol tends to have deleterious effects on male sexual performance. Studies have been conducted that indicate increasing levels of alcohol intoxication produce a significant degradation in male masturbatory effectiveness (MME). This degradation was measured by measuring blood alcohol concentration (BAC) and ejaculation latency. Alcohol intoxication can decrease sexual arousal, decrease pleasure ability and intensity of orgasm, and increase difficulty in attaining orgasm. Long term excessive intake of alcohol can lead to damage to the central nervous system and the peripheral nervous system resulting in loss of sexual desire and impotence in men. This can result due to a reduction of testosterone from ethanol-induced testicular atrophy, resulting in increased feminisation of males and is a clinical feature of alcohol abusing males who have cirrhosis of the liver.
_
Alcohol abuse is the leading cause of impotence and other disturbances in sexual dysfunction. Episodic erectile failure in alcoholic men is fairly routine, found to be significantly higher in men consuming more than three standard units of alcohol (12 g ethanol) daily and in subjects smoking more than 10 cigarettes/day. Van Thiel and Lester reported that 61% of patients dependent on alcohol reported sexual dysfunction, the most common being erectile dysfunction followed by reduced sexual desire. Erectile dysfunction and reduced sexual desire were frequently seen to be coexisting. Vijayasenan found that of 97 male inpatients admitted for the treatment of alcoholism, 71% suffered from sexual dysfunction for a period of more than 12 months prior to admission to a hospital. The disturbances noted were diminished sexual desire (58%), ejaculatory incompetence (22%), erectile impotence (16%) and premature ejaculation (4%). Virtually all aspects of the human sexual response are affected by alcohol especially sexual desire and erection.
_
Alcohol and sex in women:
In many women, alcohol increases sexual arousal and desire, although it does lower the physiological signs of arousal. Women have a different response to alcohol intoxication. Studies have shown that acute alcohol consumption tends to cause increased levels of testosterone and estradiol. Since testosterone controls in part the strength of libido in women, this tends to cause an increased interest in sex. Also, because women have a higher percentage of body fat and less water in their bodies, alcohol can have a quicker, more severe impact. Women’s bodies take longer to process alcohol; more precisely, a woman’s body often takes one-third longer to eliminate the substance. Sexual behavior in women under the influence of alcohol is also different from men. Studies have shown that increased BAC is associated with longer orgasmic latencies and decreased intensity of orgasm. Some women report a greater sexual arousal with increased alcohol consumption as well as increased sensations of pleasure during orgasm. Because ejaculatory response is visual and can more easily be measured in males, orgasmic response must be measured more intimately. In studies of the female orgasm under the influence of alcohol, orgasmic latencies were measured using a vaginal photo-plethysmograph, which essentially measures vaginal blood volume. Psychologically, alcohol has also played a role in sexual behavior. It has been reported that women who were intoxicated believed they were more sexually aroused than before consumption of alcohol. This psychological effect contrasts with the physiological effects measured, but refers back to the loss of inhibitions because of alcohol. Often, alcohol can influence the capacity for a woman to feel more relaxed and in turn, be more sexual. Alcohol may be considered by some women to be a sexual “disinhibitor”.
_
Sexual risk-taking:
Alcohol intoxication is associated with an increased risk that people will become involved in risky sexual behaviours, such as unprotected sex. It is unclear whether the two are linked or the personality types of people who often drink large amounts of alcohol are more tolerant of risk-taking. Alcohol is linked to a large proportion of unwanted outcomes associated with sex such as date rape, unwanted pregnancy and sexually transmitted diseases. Studies show that almost 50 percent of unplanned sexual encounters involve alcohol, and 60 percent of STDs are transmitted when alcohol is involved. Young adults who use alcohol are seven times more likely to have unprotected sex.
_
Causal links between binge drinking patterns, unsafe sex and HIV in South Africa: it’s time to intervene:
South Africa has a massive burden of HIV and alcohol disease, and these pandemics are inextricably linked. Much evidence indicates that alcohol independently influences decisions around sex, and undermines skills for condom negotiation and correct use. Thus, not surprisingly, people with problem drinking in Africa have twofold higher risk for HIV than non-drinkers. Also, sexual violence incidents often coincide with heavy alcohol use, both among perpetrators and victims. Implementation of effective interventions could alleviate much alcohol-attributable disease, including unsafe sex, sexual violence, unintended pregnancy and, likely, HIV transmission.
_
Alcoholic beverages as a source of estrogens:
Alcoholic beverages contain not only alcohol but also numerous other substances (i.e., congeners) that may contribute to the beverages’ physiological effects. Plants used to produce alcoholic beverages contain estrogen-like substances (i.e., phytoestrogens). Observations that men with alcoholic cirrhosis often show testicular failure and symptoms of feminization have suggested that alcoholic beverages may contain biologically active phytoestrogens as congeners. Biochemical analyses have identified several phytoestrogens in the congeners of bourbon, beer, and wine. Studies using subjects who produced no estrogen themselves (i.e., rats whose ovaries had been removed and postmenopausal women) demonstrated that phytoestrogens in alcoholic beverage congeners exerted estrogen-like effects in both animals and humans. Those effects were observed even at moderate drinking levels. In men, high levels of estrogen can lead to testicular failure and the development of feminine traits including development of male breasts, called gynecomastia. In women, increased levels of estrogen due to excessive alcohol intake have been related to an increased risk of breast cancer.
_
Female fertility and alcohol:
Alcohol doesn’t cause problems only after you are pregnant. It can make women less fertile too. There is a link between drinking and fertility, although exactly how alcohol makes women less fertile isn’t understood clearly. Many studies have shown that even drinking lightly can have an effect. These include a Danish study that showed drinking between one and five drinks a week can reduce a women’s chances of conceiving, and 10 drinks or more decreases the likelihood of conception even further. A 2009 study done at Harvard University of couples undergoing IVF showed that women who drank more than six units per week were 18% less likely to conceive, while men were 14% less likely.
Male fertility and alcohol:
Excessive alcohol lowers testosterone levels and sperm quality and quantity in men. It can also reduce libido, and cause impotence. If a man drinks heavily it can really reduce a couple’s chances of conceiving. However, if you reduce what you drink, these effects can be quickly reversed. Drinking in adolescence can affect normal sexual development and reproductive onset. At any age, modest ethanol doses (e.g., blood alcohol concentrations of 0.06 gm/dL) can increase sexual drive but also decrease erectile capacity in men. Even in the absence of liver impairment, a significant minority of chronic alcoholic men show irreversible testicular atrophy with shrinkage of the seminiferous tubules, decreases in ejaculate volume, and a lower sperm count.
____________
Alcohol and family, relationship and children:
When someone experiences alcohol problems, the negative effects of drinking exert a toll, not only on the drinker, but also on their partner and other family members. Recent data suggest that approximately one child in every four (28.6%) in the United States is exposed to alcohol abuse or dependence in the family. One of the clearest demonstrations of how alcohol use negatively impacts the family is the widely documented association between alcohol use and interpersonal violence.
Family problems that are likely to co-occur with alcohol problems include:
Violence
Marital conflict
Infidelity
Jealousy
Economic insecurity
Divorce
Fetal alcohol effect
Drinking problems may negatively alter marital and family functioning, but there also is evidence that they can increase as a consequence of marital and family problems. Thus, drinking and family functioning are strongly and reciprocally linked. Not surprisingly, alcohol problems are common in couples that present for marital therapy, and marital problems are common in drinkers who present for alcohol treatment.
_
Children of alcoholic:
Growing up in a family where one or both of the parents are alcoholic can prove to be so painful and emotionally traumatic that many years later the adult child will still be suffering from the scars. Frequently, as children they had to become “superchildren,” responsible for running the family, feeding their parents, while constantly living in fear of their parents. In addition, they often feel guilty over their inability to save their parents. Consequently, these children have a very poor self-image and, as adults, often find it impossible to have satisfactory relationships. They have grown to mistrust all people and are frequently very accepting of unacceptable behavior on the part of others. These psychological scars, combined with the strong possibility that the genetic traits for alcoholism may be inherited, result in a very high percentage of alcoholism—25 percent— among children of alcoholics. Even if the child does not become an adult alcoholic, other psychological problems may result, such as obsessive-compulsive disorders and the unrealistic need to be “perfect.” By constantly searching for the approval of others, and by placing the needs of others before their own, adult children of alcoholics may grow so accustomed to living with a dysfunctional person that as an adult they may seek codependent relationships.
_
Alcoholism and Alcohol Effects on Relationships:
People that drink heavily often assume that any problem with alcohol is a problem with their own behaviors. If the individual is not an abusive drunk, for instance, they assume that their bodies are the only thing they are punishing, not their families. But the truth about heavy drinking is that just because the individual may not be a dangerous drunk does not mean they are not severely negatively impacting their relationships. Alcohol effects on relationships go much deeper, and the alcoholic can cause rifts between themselves and others.
1. The first issue, of course, is money. Alcohol is expensive. Spending a great deal of money each day on alcoholic beverages is serious problem that can put a great deal of strain on your wallet. Unless you are independently wealthy, you are likely to suffer financial consequences of constant drinking.
2. Alcohol causes people to become less sensitive to the feelings of others. Alcohol makes it difficult for people to distinguish between the other person’s emotions, and thus they may make incorrect judgments that negatively impact their relationship with the other person.
3. Time is an issue as well. Drinking is not a “one and done” type of activity. It takes hours out of your day – hours that you could be spending with a partner. Instead, that lack of time can cause you to drift apart emotionally.
4. There is evidence that non-alcoholic partners of individuals with alcohol dependence start to become addicted to taking care of their alcoholic partner, causing them additional grief and unfairly putting them in a situation they will have difficulty breaking free from.
5. Alcoholism causes a change in the individual’s personality over time. If you have a relationship with someone, and you start to show signs of changing, there is always a chance that your partner will not like the new you.
Alcoholism may be terrible for your body and cause poor decision making, but even if you are able to keep that part of your life in check, negative alcohol effects on relationships can still occur.
___________
Social effects of alcohol:
People around the globe consume alcohol in various forms and within various cultural settings. But although alcohol is used the world over, it is also commonly misused or abused. Whenever and wherever it occurs, the abuse of alcohol has deleterious effects on the abuser, those close to him/her and to the wider society.
Alcohol Abuse hurts the Family:
Although most people abuse alcohol because it makes them feel better about themselves, the truth is that over-use of alcohol tends to negatively impact the abuser’s personality. Increased irritability, poor judgment and reasoning are just a couple of ways that alcohol damages the human personality and relationships by extension. One study suggested that abuse of alcohol is behind as much as 40 percent of instances of serious domestic violence. Alcoholism is attributable to verbal and physical abuse of the spouse and the children and carries a great responsibility for the breakup of marriages. Children living in the home with an alcoholic have lower grades, higher rates of depression and frequently feel socially isolated.
The common presence of Psychological Harm which accompanies Alcoholism:
When alcohol is abused over a period of time, the risk of psychological damage to the drinker increases. Study after study points to the link between alcohol abuse and psychological disorders such as anxiety disorder and depression. People may initially over-drink in order to overcome their low feelings of depression, but in fact, the more they drink, the more depressed they become. Alcohol does not counteract depression, instead it exacerbates the problem. This connection probably explains why 15-70 percent of those who misuse alcohol are also sufferers of depression. Other people use alcohol as a tool to help them relax and deal with stressful social situations. Maybe they use alcohol in order to feel better in tense family settings or to help them overcome social phobias when they need to attend social functions related to work or dating. As with depression, the number of people who are alcoholic and who live with social phobias is remarkably high. Sadly, people who abuse alcohol, often behave in ways that cause others to withdraw from them society. Pretty soon, only others who abuse alcohol are within the social circle.
Alcohol Abuse hurts Society at Large:
The damaging effects of alcohol abuse are not limited to the person and those living closest to them. Alcohol abuse is linked to many social ills which affect people otherwise unconnected to the drinker. There is a clear connection between alcohol abuse and higher rates of workplace absenteeism. Abuse of alcohol is also linked to higher rates of violent crime in neighborhoods. Because alcohol impairs good judgment, it is often connected to risky sexual activity. Finally, alcohol is involved in a majority of automobile accidents. Alcohol is damaging to everyone intimately or remotely connected to the one who abuses it.
_
Alcohol harms to other individuals:
_
Psychological and Social Impacts of Alcohol:
Let’s face it. People like to drink alcohol for its positive effects. If you’re anxious, a drink can help you relax. Bored? You can enjoy a gourmet experience. Hurting? You’ll go numb. Shy? You’ll be less inhibited. Lonely? Other drinkers are your instant friends — and “social” binge drinking often starts in high school or college. This habit often continues into early adulthood and is hard to break, because many people have known no other ways to gather socially. Also, your job or identity can link you to alcohol. This is a common issue for restaurant staff, or in any job that requires selling, networking or travel. Other situations can trigger the urge to drink excessively, such as holidays or anniversary dates of important personal events, or longing for a lost love. People familiar with computer programming know that you get junk data unless you process both zeros and ones. Similarly, frequent alcohol and drug use to feel better filters out negative experiences but robs us of needed perceptions. Consider what it would be like to turn off the pain receptors in your feet. You wouldn’t notice much difference at first, until you step on a sharp object without knowing it and make the injury much worse. We need access to unpleasant feelings to alert ourselves to situations that need correction. Although alcohol in moderation doesn’t create problems for some people, for many, moderate or binge drinking has unwanted psychosocial effects, even after alcohol has left their system:
•Irrational thinking, including such cognitive distortions as black and white thinking and emotional reasoning
•Defensiveness, such as denial; blaming; escape and avoidance of uncomfortable situations; isolation and withdrawal
•Aggression, including intense and violent temper; unwanted sexual advances; physical fights, sexual abuse or assaults
•Lack of integrity, such as broken promises; underfunctioning that leads to codependency; driving under the influence (DUI) — a serious danger to self and others; infidelity; refusing to take responsibility; and facilitating other addictions, like pathological gambling
•Mood problems, including depression, anxiety, anger and irritability, low self-esteem, increased risk of suicide and homicide
•Family problems, such as arguing, bickering, stonewalling, withdrawal, and generally poor communication; neglectful, emotionally abusive, codependent or stagnant relationships; infidelity or not coming home; poor sexual performance; financial distress
•Career difficulties, including failure to advance, conflicts at work, job loss
•Worsening of other mental health issues, such as anxiety, phobias, panic attacks, depression, bipolar disorder, mood swings, attention deficit/hyperactivity disorder (ADHD), paranoia, personality disorders, schizophrenia, poor anger management
_________
Alcohol, gender and culture:
Alcoholic beverages have been a part of social life for millennia, yet societies have always found it difficult to understand or restrain their use. To better understand alcohol consumption and its consequences, we need to better understand social and cultural influences on the differences between men and women and therefore more studies & research need to be done on this aspect of alcohol. That theme deserves careful and detailed attention for several reasons.
1. First, compared with women throughout the world, men are more likely to drink, consume more alcohol, and cause more problems by doing so. This gender gap is one of the few universal gender differences in human social behavior. It is evident in all areas of the world, in drinking versus abstinence, in heavy drinking and intoxication and in alcohol use disorders. The gender gap has varied but persisted for a long time, at least in European history and in the traditions of many pre-industrial societies elsewhere. Research has suggested several possible reasons why universal gender differences in drinking behavior might arise. For example, if women have lower rates of gastric metabolism of alcohol than men or smaller volumes of body water in which alcohol is distributed, women may need to consume less alcohol than men to derive the same effects. Or, women may be more likely than men to experience unpleasant acute effects from alcohol (such as hangover symptoms), or may not enjoy risky and poorly controlled behavioral effects of alcohol as much as men, characteristics which might inhibit women’s drinking. However, despite the universality of gender differences in drinking behavior, the size of gender differences has not varied greatly in different societies, historical eras, and drinking patterns; and the universality nor the variability of those gender differences has yet been adequately explained.
2. A second important reason to study how gender and alcohol interact is that some of the gender differences in drinking, and much of the variation in such gender differences, are cultural. Societies have long used alcohol consumption and its effects as important ways to differentiate, symbolize, and regulate gender roles. Differences in normative drinking patterns help reveal to what extent societies differentiate gender roles, for example, by making drinking behavior a demonstration of masculinity or by forbidding women to drink as a symbol of subservience or to prevent sexual autonomy. Better understanding of how men’s and women’s drinking patterns differ is thus an important key to answering broader questions of how and why societies try to get women and men to behave differently. In recent decades there has been increased concern about drinking behavior as an aspect of gender roles, because in some societies gender differences in drinking behavior have grown smaller. A common hypothesis about such convergence in drinking patterns is that increased opportunities for women to perform traditionally male roles (particularly in the workforce) have also enabled and encouraged women to increase their drinking, with more adverse consequence. Consistent with this hypothesis, where convergence has occurred, it has usually been most evident among adolescents or young adults. However, convergence has not always occurred where it might be expected; it may occur for some aspects of drinking behavior but not others; it may sometimes occur because men are drinking less instead of women drinking more; and it is not always related to women’s nontraditional roles. If social influences on women’s and men’s drinking are likely to be historically and culturally complex, better cross-cultural research on gender and drinking over longer periods of time may be essential to avoid oversimplified conclusions about effects of changes in women’s and men’s roles.
3. A third important reason to study how gender affects alcohol use is that false assumptions about male or female drinking may adversely affect how societies identify and try to control alcohol-related problems. If heavy drinking is associated with displays of masculinity or male camaraderie, this may encourage male drinkers to deny or minimize problems resulting from their drinking, or to regard drunken behavior as normal or permissible, even when it leads to violence. On the other hand, assumptions that women do not drink heavily may lead to women’s drinking problems being underestimated or overlooked (for example, by physicians). However, when women’s alcohol abuse or dependence becomes conspicuous, it has often provoked social outrage and the use of punishment or coercion to try to stop such behavior, most recently by taking custody of children or by forcing alcohol abusing women to be hospitalized or incarcerated if pregnant. Better understanding of gender stereotypes about both men’s and women’s drinking is essential to reduce the negative effects such stereotypes may have on treatment and prevention of alcohol-related problems.
______
Alcohol does make you hunt for pretty faces: Beer Google hypothesis:
‘Beer Goggle’ is real. People become more attracted to the opposite sex after a few drinks and even a small amount of alcohol can shift your attention to gorgeous ladies. According to researchers from University of Bristol, attractiveness ratings were higher for participants in the alcohol group compared to the placebo group. To prove their point, they asked volunteers to look at photos of men, women and landscapes before and after drinking. They conducted lab tests to gauge whether drink changed people’s perceptions of what is attractive. The results confirmed the ‘Beer Goggle’ hypothesis, suggesting that the effect is less to do with the level of attractiveness and more to do with a lack of restraint and decision-making skills. Now the team is extending the research into pubs. “If alcohol does change perceptions of attractiveness then that could be a factor in the kind of risky behaviour you see when people are drunk, such as unprotected sex,” study author Olivia Maynard from University of Bristol says.
________
Children and teenage drinking:
_
The figure below shows various sources from where a college student gets alcohol:
_
Children drinking alcohol:
In England, children aged 11 to 17 years drink around 20 million units of alcohol every week. That is the equivalent of 9 million pints of beer or 2 million bottles of wine. Children and their parents and carers are advised that an alcohol-free childhood is the healthiest and best option. However, if children drink alcohol, it should not be until at least the age of 15 years. Beginning to drink before age 14 is associated with increased health risks, including alcohol-related injuries, involvement in violence, and suicidal thoughts and attempts. Drinking at an early age is also associated with having more sexual partners, STD, pregnancy, using drugs, employment problems, and risky driving behaviors. Significant changes in brain structure accompanying heavy drinking in young people with alcohol use disorders can affect brain functions related to motivation, reasoning and other processes. Heavy drinking during adolescence may also affect normal brain functioning during adulthood. Young people who drink heavily may experience adverse effects on liver, bone, growth and endocrine development. If young people aged 15 to 17 years consume alcohol, it should always be with the guidance of a parent or carer or in a supervised environment. Harsh parenting, family conflict and a permissive approach to alcohol by parents are associated with risky drinking in adolescence. Alcohol consumption by young people, including heavy and regular drinking, increases as the amount of spending money young people have available to them increases.
_
_
Risks Associated with Alcohol Misuse in Children and Young People:
The evidence suggests that there are a number of risk factors associated with alcohol misuse by children and young people. These include:
• a genetic predisposition (generational transmission)
• physical and sexual abuse in childhood, which may lead to later drinking behaviour
• early exposure to drinking alcohol, which may increase the risk of problematic drinking in adolescence
• behavioural patterns of alcohol consumption of parents, grandparents and siblings
• family history of alcohol problems
• early behaviour problems in children, which may place them at especially high risk of alcohol problems, particularly if there is a family history of alcohol problems
• antisocial behaviour and inter-personal problems in pre-adolescent children, which may be predictive of substance use disorders
• children and young people who are sensation-seeking or have impulsive personality types may drink in large quantities
• heavy and binge drinking by young people can be a mechanism for coping with stress or anxiety
• there may be gender differences between mothers and fathers in terms of their influence on the behaviour of sons and daughters
• involvement in drinking games can lead to very high levels of alcohol consumption
• mechanisms to protect children and young people, such as excessive criticism of their drinking behaviour, may not be protective but harmful.
• young people should be advised and supported to rely less on alcohol to facilitate social integration with their peers and to develop other more constructive peer group relationships.
_
Protective Factors that Inhibit Alcohol Misuse in Children and Young People:
Protective factors are very important as they can ameliorate risk factors. Our examination of the evidence about protective factors has shown that:
• the location of a young person’s first drink may be important to future alcohol misuse, children who first use alcohol in a home environment and learn about its effects from parents are less likely to misuse alcohol than those who begin drinking outside the home and experiment with peers
• delaying the time of a young person’s first drink may reduce the risk of harmful drinking.
• having adults who retain good relationships with a young person, characterised by appropriate levels of support and control, is likely to be protective
• controlled alcohol use is not in itself predictive of negative outcomes
• religious affiliation, especially attendance at religious services, may have a protective effect against alcohol consumption
• Key factors that seem to buffer the adverse effects of alcohol consumption in children and young people include informed and supportive parental guidance about alcohol and a delay in the age of initiation into drinking.
_
Adverse Consequences of Drinking Alcohol for Children and Young People:
There are potentially adverse consequences for children and young people who misuse alcohol. The evidence suggests that:
• adolescents who misuse alcohol are more likely to suffer from side effects including appetite changes, weight loss, eczema, headaches and sleep disturbance
• the most common impacts of alcohol intoxication are vomiting and coma
• young people are not immune to the chronic diseases and conditions associated with excess alcohol consumption in adults, and deaths from liver disease are now occurring at younger ages
• adolescents and young people who drink and drive, or allow themselves to be carried by a drunk driver, are more likely to be involved in a car accident
• adolescents and young people who drink alcohol are more likely to sustain an injury, often as a result of an assault
• alcohol abuse in adolescence, during a developmentally sensitive period, poses a particular danger to the emerging brain faculties of executive functioning and long term memory
• adolescents are likely to be more vulnerable than adults to both subtle brain damage and long lasting cognitive deficits following alcohol exposure
• alcohol may increase feelings of depression
• stress / anxiety based drinking is associated with long-term and more severe negative outcomes
• there is a relationship between adolescent alcohol use and mental health problems, so it is important that all young people with alcohol problems should have a mental health assessment
• alcohol consumption during an evening may affect a child’s performance at school on the following day, since it takes time to metabolize alcohol and this process varies depending on the dose of alcohol that was consumed and differing metabolic capacity
• the evidence shows that there are associations between alcohol consumption and subsequent behaviour with peers and friends. Indeed, excessive alcohol use can be detrimental to a young person being able to maintain friendships, particularly if the consumption levels are higher than among the peer group generally.
Moreover, there is evidence that
• young people of college age who use alcohol are more likely than their abstaining peers to use cannabis
• alcohol consumption can have a detrimental effect on young people’s short term educational performance
• students are more likely to miss classes because of drinking
• alcohol consumption by young people, particularly students, is more likely to make them vulnerable to being the victims of crime
• alcohol may make some young people more likely to display aggressive behaviour, although it is likely that other factors such as their personality and family life will play a role
In relation to sexual health and behaviour, the evidence confirms that alcohol consumption is associated with:
• not using a condom during a young person’s first sexual encounter
• an increased likelihood of having sex and at a younger age
• unprotected sex
• teenage pregnancy
• the likelihood of contracting sexually transmitted diseases
_
The figure below shows differences in brains of 15 year old non-drinker vs. drinker through brain imaging study:
_
Are there any Positive Consequences of Children and Young People drinking Alcohol?
While the negative consequences of alcohol misuse are considerable and must be taken seriously, there is evidence of some positive impacts associated with young people being able to drink sensibly. For example, the evidence shows that:
• some young people may benefit by having increased confidence when communicating with members of the opposite sex
• alcohol use at certain levels (undefined) can increase young peoples’ feelings of sociability
• drinking alcohol as a means of celebrating and on special occasions may also be positive for young people.
_
Every year in the U.S., roughly 5,000 people under the age of 21 die from an alcohol-related incident including car crashes, homicides, suicides, alcohol poisoning and other related injuries. 70% of 18-year-olds admit to drinking an alcoholic beverage at least once, while 80% of college-aged students report consuming alcohol. 2/3 of the high school-age students who drink do so to the point of intoxication.
_
Can parents teach responsible drinking to children by be giving them a taste for booze?
Many parents believe small quantities of alcohol teach responsible drinking: But a study, led by psychologist Dr Aric Sigman, says parents must delay giving alcohol in childhood because it can do long-lasting neurological damage. Parents who give their children small amounts of alcohol in the belief they are instilling a sensible attitude to drinking may unwittingly be giving them a taste for booze, a psychologist has warned. Aric Sigman said adults needed to realise that alcohol was more damaging to the young brain and body. Studies showed the earlier a child was introduced to drink, the greater their odds of becoming an alcoholic, he added. In a report to an EU think-tank on childhood and adolescence, Dr Sigman said it was ‘imperative’ that parents delayed the age at which they introduce their children to alcohol. He said that ‘even in small amounts’, alcohol may have long-lasting effects on the young brain, which continues developing long after the body matures. Under current rules in U.K., it is illegal for under-18s to buy alcohol or for someone to buy it for them, with the exception that 16 and 17-year-olds can drink beer, wine or cider with a meal out with an adult. Dr Sigman, a fellow of the Royal Society of Medicine, said parents were wrong if they believe that by giving their children small amounts of alcohol at home, they were teaching them to drink responsibly. In fact, research suggests that early exposure to alcohol primes the brain to enjoy it more. Dr Sigman’s review of medical literature also raised concerns that girls who drink may be raising their odds of infertility and breast cancer in later life. He said that in an ideal world, no one would touch alcohol before the age of 25. However, he acknowledged that 16 was a more realistic age for parents to first allow their children to drink at home. For instance, a US government-funded study found that that those who had their first drink before the age of 18 ran a ‘far greater’ risk of becoming dependent on alcohol as adults. And the World Health Organisation has stated: ‘The longer the onset of consumption is delayed, the less likely it is that alcohol-related problems and alcohol dependence will emerge in adult life.’ Official advice in Britain is similar – but few parents realise, says Dr Sigman. Others may fear that stopping youngsters from drinking at home risks will simply increase alcohol’s appeal. He also uses his report to call for the legal drinking age, at which youngsters can buy alcohol in pubs and shops, to be harmonised at 18 across Europe. The Chief Medical Officer advises that an alcohol free childhood is the safest option and that those under 15 year olds, ideally, should not drink at all.
_
In general, the risk of youth experiencing these problems is greater for those who binge drink than for those who do not binge drink. Youth who start drinking before age 15 years are five times more likely to develop alcohol dependence or abuse later in life than those who begin drinking at or after age 21 years.
______
Legal Drinking Age:
The legal drinking age is the age at which a person can consume or purchase alcoholic food or alcoholic beverages. These laws cover a wide range of issues and behaviours, addressing when and where alcohol can be consumed. The minimum age alcohol can be legally consumed can be different from the age when it can be purchased. These laws vary among different countries and many laws have exemptions or special circumstances. Most laws apply only to drinking alcohol in public places, with alcohol consumption in the home being mostly unregulated. Some countries also have different age limits for different types of alcoholic drinks. For example, the legal drinking age in the UK and Australia is 18, whereas the law in the USA is 21. The United Kingdom is the only country that has a minimum legal age for drinking alcohol in a home. In some countries, it is not illegal for minors to drink alcohol but the alcohol can be seized without compensation. In some cases, it is illegal to sell or give alcohol to minors. Some countries such as Cambodia don’t have a set limit and on the other side of the coin, alcohol consumption is illegal in places like Afghanistan and Saudi Arabia.
_
Calls for legal drinking age to be raised to 21 years:
Pressure is mounting for various governments to raise the legal drinking age to 21 to protect the health of young people whose brains are still vulnerable to the toxicity of alcohol at 18. Raising the age limit would protect young people from the brain damage that can be caused by too much alcohol and the harms associated with being drunk, such as car accidents and violence. There was increasing evidence that the accessibility of alcohol from the age of 18 was causing great harm to young people.Advertisement In the US, a review of 17 studies in various states that raised the legal drinking age found the average number of young people involved in road accidents decreased 16 per cent. Furthermore, research in some Canadian provinces showed that a higher minimum legal purchasing age reduced the number of young people being hospitalised due to alcohol use disorder, alcohol poisoning, suicidal behaviour and traffic crash injuries. The evidence strongly suggests that raising the minimum purchasing age for alcohol would reduce youth alcohol-related harm.
_
_
Contrary study:
A 2009 study by Harvard Professor Jeffrey Miron concluded that “any life-saving effect in those states that first raised the drinking age was only temporary, occurring largely in the first year or two after switching to the minimum legal drinking age of 21.” Some studies have found no relation between the drinking age and other alcohol-related harms like suicide, homicide, or vandalism.
_
Why 21 years?
More than 25,000 lives have been saved in the U.S. thanks to the 21 Minimum Legal Drinking Age. This law continues to prevent tragedies—decreasing crashes by an estimated 16 percent and keeping young people safer from many risks. Sometimes, without knowing all the facts, people assert that youth shouldn’t have to wait until they’re 21 to drink. Many activities have ages of initiation. A person must wait until age 16 to start driving, age 18 to marry without parental consent, age 35 to become president, and so on in the U.S. The age limit for alcohol is based on research which shows that young people react differently to alcohol. Teens get drunk twice as fast as adults, but have more trouble knowing when to stop. Teens naturally overdo it and binge more often than adults. Enforcing the legal drinking age of 21 reduces traffic crashes, protects young people’s maturing brains, and keeps young people safer overall.
Can’t parents teach their teens how to drink alcohol responsibly by giving them small amounts—under supervision—before they reach 21?
As matter of fact, there is evidence to contrary. When teens feel they have their parents’ approval to drink, they do it more and more often when they are not with their parents. When parents have concrete, enforced rules about alcohol, young people binge drink less.
Would lowering the legal drinking age make alcohol less of a big deal, and less attractive to teens?
History says no. When states had lower legal drinking ages in the U.S., the underage drinking problem was worse. For example, before the 21 minimum legal drinking age was implemented by all states, underage drunk drivers were involved in over twice as many fatal traffic crashes as today. European countries have worse problems than America does, as far as binge drinking and drinking to intoxication. Studies show that Europe has more underage drunkenness, injury, rape, and school problems due to alcohol. Since alcohol is more available there, it actually increases the proportion of kids who drink in Europe.
Is it a good idea to propose alcohol education course for teens that would entitle teens to drink before 21?
Research shows that education alone doesn’t prevent risky behaviors. For example, driver education by itself does not reduce youth car crashes. Beginning drivers need other restrictions in place to stay safe. In addition, there are clear health risks associated with underage drinking.
_
Do not mix up drinking age with voting age and marriage age:
Evidence from various studies suggests that legal drinking age of 21 years is reasonable. Legal drinking age need not correlate with marriage age and voting age. Young people react differently to alcohol; get drunk twice as fast as adults and have more trouble knowing when to stop and more likely to abuse alcohol (vide infra). The same logic cannot be applied to voting and marriage age. Biological logic need not correlate with legal logic. A 16 year old girl can give consent for sex to satisfy her biological need but legal age of marriage is 18 years and marriage is consider consummated only if she has sex with husband even though she could have had legal sex between 16 to 18 years without marriage. Biologically speaking 20 year old man’s brain cannot handle alcohol that well as an adult even though the same brain can vote rationally and can have sex with a 16 year girlfriend consensually.
_________________
Relationship between Youth and Adult Drinking:
Adolescence as a critical window for developing an alcohol use disorder: Current findings in neuroscience:
Alcohol consumption during adolescence greatly increases the likelihood that an alcohol use disorder will develop later in life. Elucidating how alcohol impacts the adolescent brain is paramount to understanding how alcohol use disorders arise. Adolescence, defined as ages 10-19 by the World Health Organization, represents the developmental transition to adulthood during which the brain is in a unique and dynamic state. This stage is marked by increased novelty seeking and risk-taking behavior as adolescents experiment with adult aspects of life, including the initiation of alcohol use. By twelfth grade, 73% of adolescents have experimented with alcohol while 30% have been drunk within the past month. Further, more than half of 12-17 year-olds who consume alcohol, binge drink (>5/4 drinks for males and females respectively). Unfortunately, alcohol use during adolescence increases the risk for developing an alcohol use disorder (AUD). Elucidating the neurobiology of this risk is considered critical to understanding how AUDs develop. To date, two overlapping hypotheses have emerged to explain why adolescence is a critical time for developing an AUD. First, the adolescent brain responds uniquely to alcohol, which may result in fewer physiological cues to self-regulate intake. Second, the adolescent brain exhibits an enhanced sensitivity to many alcohol effects, especially neurodegenerative effects of alcohol that dysregulate behavioral control systems and lead to addiction. Adolescent’s unique response to alcohol promotes excessive intake. Adolescents respond to the effects of alcohol distinctly from adults. Adolescents are less sensitive to negative effects of alcohol, including cues that influence self-regulation of intake, but are more sensitive to positive effects, which may serve to reinforce or promote excessive intake. The distinct response of adolescents has both pharmacodynamic and pharmacokinetic components such that age-related differences in alcohol (ethanol) absorption and metabolism must be considered when examining these differences. Specifically, it takes a larger dose of alcohol for an adolescent to achieve similar blood alcohol concentrations as an adult. However, well-controlled animal studies have shown that despite similar blood alcohol concentrations, adolescents demonstrate enhanced sensitivities or vulnerabilities to many aspects of alcohol use and abuse. Recent studies continue to show that corticolimbic systems, such as the PFC, mesolimbic reward system and hippocampus, are undergoing significant developmental transitions during adolescence that make them primary targets for alcohol-induced structural and functional changes. The adolescent’s decreased response to the negative aspects of alcohol consumption (motor impairment, sedation, anxiety, and social depression) coupled with increased or altered response to the positive and rewarding effects of alcohol may promote excessive intake. Repeated exposure to excessive intake and the adolescent’s enhanced susceptibility to alcohol-induced damage – whether through toxicity, teratogenicity, or other effects on plasticity – further dysregulates behavioral control of consumption. Thus, the adolescent’s unique response to alcohol combined with increased susceptibility to alcohol-induced neurodegeneration interacts to facilitate excessive alcohol consumption, the hallmark of an AUD. However, the mechanisms behind the adolescent’s unique response to and consequences of alcohol use/abuse are not well understood. Additional research is desperately needed to understand the responses and consequences of alcohol exposure on the dynamic and developing adolescent brain. Because AUDs commonly begin in adolescence and AUDs affect over 8% of the U.S. population, research is critical to public health in order to better prevent and reduce the prevalence of AUDs.
_
Age at onset of alcohol use and its association with DSM-IV alcohol abuse and dependence: results from the national longitudinal alcohol epidemiologic survey:
Data from 27,616 current and former drinkers interviewed in the 1992 National Longitudinal Alcohol Epidemiologic survey were used to examine the relationship between age at first use of alcohol and the prevalence of lifetime alcohol abuse and alcohol dependence, among all U.S. adults 18 years of age and over and within subgroups defined by sex and race. The rates of lifetime dependence declined from more than 40% among individuals who started drinking at ages 14 or younger to roughly 10% among those who started drinking at ages 20 and older. The rates of lifetime abuse declined from just over 11% among those who initiated use of alcohol at ages 16 or younger to approximately 4% among those whose onset of use was at ages 20 or older. After using multivariate logistic regression models to adjust for potential confounders, the odds of dependence decreased by 14% with each increasing year of age at onset of use, and the odds of abuse decreased by 8%.
_
Figure below shows Alcohol Dependence or Abuse in the past year among Adults Aged 21 or Older, by Age at First Use of Alcohol in the U.S. 2010:
The figure above shows that lower the age of first use of alcohol, higher is the probability of alcohol abuse and dependence.
_
Early drunkenness emerges as key risk factor for alcohol abuse:
It is not when you take your first drink but when you first get drunk that tends to determine a lifetime’s outcomes. European research into young drinkers has overturned the widely held view that the age youngsters first drink determines later problems with alcohol. The research may go some way to reassuring parents concerned because their kids have had their first taste of alcohol this Christmas. Many studies had reported that the younger a person when they first drink the higher the chances that person will develop drinking-related problems. But the studies had failed to show why young people drinking small amounts would lead to later problems. The new study looks at the link between early-age drinking and problem behaviours such as smoking, marijuana use, injuries, fights and low academic performance among tens of thousands of 15-year-olds. It concluded that early drunkenness rather than early-age drinking was a risk factor. The results are published in the March 2013 issue of Alcoholism: Clinical & Experimental Research. Emmanuel Kuntsche, a senior scientist at Addiction Switzerland, said the misunderstanding arose because early drinking had previously been defined in terms of toxicity exposure. “However, this thinking neglects two principal issues when it comes to alcohol use: one, consumption of small amounts of alcohol such as a sip are not toxic, and two, the majority of the population is not constantly exposed to toxic amounts of alcohol,” Dr Kuntsche said. Adolescents, in particular, had large variations in drinking from day to day – and long periods of abstinence. Dr Kuntsche and his colleagues analysed data dating back to 1983 from 44,801 15-year-old girls and boys who had drunk alcohol from 38 North American and European countries. “We found that early drunkenness was a risk factor for various adolescent problem behaviours at 15 years of age rather than an early age of first drink,” he said. To prevent harm, research should focus on what is behind early drunkenness rather than first drink age. “Negative life events, behavioural problems and parents’ alcoholism are possible underlying problems,” he said.
_
Teen drinking and antisocial behavior:
Though well-documented, the relationship between alcohol (mis)use and antisocial behaviour is not simple, different perspectives producing different predictions about the direction of causality. These can be formulated as three basic hypotheses, representing disinhibition, susceptibility, and reciprocal effects respectively, each of which can be applied in both the shorter and longer term.
1. The first (disinhibition hypothesis) implies that alcohol causes or facilitates antisocial behaviour in the shorter (more immediate) term, as a consequence of its acute effects on the brain, in particular its impact on pre-frontal functioning (Room and Collins, 1988; Bushman and Cooper, 1990; Graham et al., 1998). For example, a study of young adults concluded that violence among alcohol-dependent individuals occurred when, and possibly because, they were under the influence of alcohol (Arseneault et al., 2000). In the longer term, there is a potential additional impact of chronic alcohol (mis)use on antisocial behaviour through hippocampal damage (impairing memory, learning, and consequently, overall executive functioning) or other neurological impairment (Tapert et al., 2005; Howard, 2006). In addition, excessive alcohol use may be associated with impaired relationships with parents and peers, difficulties in education or work, conflict with law enforcement agencies and a deviant or antisocial friendship network (Brook et al., 1998).
2. Contrasting with perspectives that posit an effect of alcohol on antisocial behaviour, the second (susceptibility) hypothesis implies the reverse; people with susceptibility to, or on a trajectory for antisocial behaviour, use alcohol to a greater extent than those who are less susceptible. Thus, antisocial behaviour is the cause of alcohol (mis)use, in either the shorter or longer term. Substance use, including alcohol in adolescence, has been related to characteristics such as under control and aggression at (much) younger ages (Block et al., 1988; Windle, 1990; White et al., 1993; Brook et al., 1996), resulting from a general inability to regulate behaviour. This could arise from a variety of causes including common genetic factors (Clark et al., 2002; Cooper et al., 2003; Stallings et al., 2005) or social factors. Each of these explanations is consistent with the notion of higher order factors representing core psychopathological processes, in this case expressed in externalizing problems (Krueger et al., 1998). Alternatively (or additionally), antisocial behaviour may cause alcohol (mis)use through association with antisocial, alcohol-using peers (Barnow et al., 2002).
3. Finally, the third (reciprocal hypothesis) implies both that alcohol (mis)use causes antisocial behaviour and that antisocial behaviour causes alcohol (mis)use, thus establishing a feedback loop. In the shorter term, alcohol and antisocial behaviour may fuel each other, escalating aggression in particular social contexts (Graham et al., 1998, 2000). In the longer term, the consequences of alcohol (mis)use may interact with individual factors (impulsivity, sensation-seeking, aggressive personality), so increasing dysregulation and problems with judgement, leading to further, and worsening alcohol use and antisocial behaviour (Howard, 2006; Measelle et al., 2006).
Each of the above hypotheses relates to the relationship between alcohol (mis)use and antisocial behaviour in general. More specific alcohol-related trouble such as fights, arguments, or involvement with the police due to drinking may be a joint outcome of (tendencies towards) antisocial behaviour in addition to alcohol (mis)use. As such, the same three hypotheses are relevant to its prediction. Thus, the disinhibition hypothesis suggests that alcohol (mis)use is a better predictor of alcohol-related trouble, the susceptibility hypothesis that it is better predicted by antisocial behaviour, and the reciprocal hypothesis that both alcohol and antisocial behaviour predict alcohol-related trouble. In support of the latter, a recent study found that significant predictors of adolescent alcohol-related fighting included frequent and high volume drinking (suggesting disinhibition) and troubles in school such as relationship problems with teachers or peers, or attention difficulties (suggesting susceptibility) (Swahn and Donovan, 2005).
_
Despite the current assumption that alcohol is a major cause of antisocial behaviour, the majority of young people perceive relatively few, or minor problems in relation to their own alcohol consumption and feel such ‘minor difficulties’ are a relatively small price to pay for the enjoyment associated with drinking (Coleman and Cater, 2005). Objective evidence suggests that this is an unrealistic perception. As evidenced by alcohol-related disorder and accidents, the burden of short-term harm is borne particularly by young drinkers (Plant and Plant, 2006) and this is especially true of those with a predisposition to antisocial behaviour.
___________
Alcohol, crime and law:
_
_
Alcohol laws regulate the manufacture, sale, and consumption of alcoholic beverages. Such laws often seek to reduce the availability of these beverages for the purpose of reducing the health and social effects of their consumption. In particular, such laws specify the legal drinking age which usually varies between 16 and 25 years, sometimes depending on the type of drink. Some countries do not have a legal drinking or purchasing age, but most set the age at 18 years. This can also take the form of distribution only in licensed stores or in monopoly stores. Often, this is combined with some form of taxation. In some jurisdictions alcoholic beverages have been totally prohibited for reasons of religion (e.g., Islamic countries with certain interpretations of sharia law) or perceived public morals and health (e.g., Prohibition in the United States from 1920 to 1933).
_
Alcohol Consumption Laws:
Legal Drinking Age: discussed vide supra
Legal Drink Driving Limit: discussed vide supra
_
Please do not mix up legal drinking age with legal drink driving limit:
All states in the United States have adopted BAC 0.08% (80 mg/dL) as the legal limit for operating a motor vehicle for drivers aged 21 years or older. However, drivers younger than 21 are not allowed to operate a motor vehicle with any level of alcohol in their system. So when your age is below legal drinking age, you cannot consume any alcohol no matter whether you drive or not. In other words, if you are 20 years old in America and you are driving car with blood alcohol level well below legal drink driving limit, you have nonetheless violated a law.
_
Why is Alcohol Legal?
Alcohol is, without question, world’s deadliest recreational drug – and one of the most addictive. But it’s also the most legal and, in a country where criminal justice system regularly ruins thousands of lives over marijuana for less reason, that should give us pause. So why is alcohol legal, and what does this tell us about how our government makes drug policy decisions?
1. Because too many people drink:
This is, ultimately, the main reason alcohol is legal. Marijuana legalization advocates often point to a large-scale 2008 study that showed 42% of Americans had tried marijuana, but the same study shows that more than twice as many Americans – 91.6% – have had an alcoholic beverage. Realistically speaking, how can you outlaw something that more than 9 out of 10 Americans have already done?
2. Because the alcohol industry is too powerful:
Firearms are a $32 billion industry, and almost impossible to regulate. Tobacco is a $96 billion industry, so a cigarette ban is out of the question. But alcohol – a $400 billion industry with 3.9 million employees in the U.S. – dwarfs them both. That’s a lot of economic muscle.
3. Because alcohol is endorsed by the Christian tradition in the Western nations:
Prohibitionists have historically used religious arguments to ban alcohol, but they’ve had to fight the Bible to do it. Alcohol production was Jesus’ first miracle, according to the Gospel of John, and the ceremonial drinking of wine is central to the Eucharist – the oldest and most sacred Christian ceremony. Wine is a central symbol within the Christian tradition. That’s a lot of tradition to overcome.
4. Because alcohol has an ancient history:
Archaeological evidence suggests that the fermentation of alcoholic beverages is at least as old as civilization – dating all the way back to ancient China, Mesopotamia, and Egypt. There was never a time in recorded human history when alcohol wasn’t part of our experience, as a species.
5. Because alcohol is easy to produce:
As you might expect (given how long it has been around), alcohol is pretty easy to make. “Fermentation,” is a natural process – and banning the product of natural processes is always tricky.
6. Because the government has already tried, and failed, to ban it:
The Eighteenth Amendment to the U.S. Constitution was ratified in 1919, and would remain the law of the land for 14 years – but even in its first few years of enforcement, its failure was evident. As H.L. Mencken wrote in 1924: Five years of Prohibition have had, at least, this one benign effect: they have completely disposed of all the favorite arguments of the Prohibitionists. None of the great boons and usufructs that were to follow the passage of the Eighteenth Amendment has come to pass. There is not less drunkenness in the Republic, but more. There is not less crime, but more. There is not less insanity, but more. The cost of government is not smaller, but vastly greater. Respect for law has not increased, but diminished. The prohibition of alcohol was such a complete and humiliating failure to America that, in the 80 years since its repeal, no mainstream politician has advocated restoring it.
_
Should alcohol be banned?
Points for prohibition:
1. It is the obligation of the government to protect the citizens from the ill effects of harmful substances. Alcohol alters the mind of a person which can cause such individual to take actions which they would not take otherwise. It is not about loses inhibitions but extends to dangerous acts which can harm the person and others also. It is the responsibility of the government to protect its citizens including those who behave irresponsibly by consuming harmful substantial like alcohol. Such a ban would help these individuals in making significant contribution towards the society which they could not make if they consume alcohol in large quantities.
2. A ban on alcohol would protect third parties like family members. Alcohol is the cause of a large number of disputes and distress in the society. It causes psychological problems for the children whose parents consume alcohol. They number of children with at least one alcoholic parent is increasing throughout the world. These children should not be made to suffer if their parents have decided to indulge in alcoholism. Psychological studies have shown that a large number of children coming from alcohol abuse families face problems like loneliness, guilt, fear of abandonment, feeling of helplessness, low self esteem and chronic depression. In some cases the children even start feeling themselves responsible for the problems created by the alcoholic person. Apart from the psychological damage it also causes great physical harm. Alcohol has always been a factor for domestic violence and the incidents of domestic abuse are higher in households where there is alcohol abuse.
3. A ban on alcohol would result in healthier individuals. A ban on alcohol would also have a positive impact on the health of the individuals. Long lasting abuse of alcohol leads to several chronic diseases like pancreatitis, liver cirrhosis, high blood pressure and different types of cancers including mouth, liver, larynx, throat and esophagus. A ban on alcohol would decrease the rate of consumption as has been seen in case of the present drug laws. Therefore a ban on alcohol would decrease the cases of alcohol addiction and also reduce the financial burden caused by health problems among the alcoholics.
_
Benefits of an alcohol ban:
•less incidents of domestic violence, assaults, injuries, drunkenness and anti-social behaviour,
•“elders are being able to sleep at night”,
•families were buying food instead of alcohol,
•police callout rates and arrests dropped by about two thirds,
•there were fewer and less serious hospital admissions (the Queensland community of Woorabinda reported a drop from 11 to one hospital admission per quarter for assault when the community went dry, Norseman (WA) reported over 60% less admissions, Fitzroy Crossing (also WA) 48%), however, hospital admissions in nearby communities can increase;
•fewer suicides; in Fitzroy Crossing suicides before the ban were as high as one per month,
•some give up alcohol completely and move back to their homelands outside of towns,
•people go out and socialise as they go fishing and hunting,
•school attendance rises, in Fitzroy Crossing by more than 14%.
_
Points against prohibition:
1. Alcohol should be kept legal so that the rights of the citizens could be maximized. The government should allow the people to live freely as long as they don’t cause any harm to others. A government may wish to have a society which is obedient, productive and free from all flaws, such a society would be without alcohol, drugs or cigarettes. While such a society may have some benefits in short term, in long term it would only result in a large number of unsatisfied individuals. A lot of people consumable alcohol responsibly and do not cause any harm to others. A free society has a high number of happy individuals who contributes significantly in the development of society.
2. Ban on alcohol is impractical and can create a black market for alcohol. As compare to other drugs, alcohol can be produced easily, moreover it is deeply engraved in a lot of cultures. Therefore any ban on alcohol would be ineffective due to its cultural acceptance and the ease of production. While the legal implications of the consuming alcohol would scare some people if a ban on alcohol is imposed, a large number of people would be attracted towards consuming more alcohol as there would be strong demand which would be met by illegal supply.
3. Ban on alcohol is a quick fix treatment for the wider social problems. A ban on alcohol is like a quick fix treatment which ignores the real causes which make people drink excessively and make bad decisions under the influence of alcohol. For example drunk driving is a problem faced by many countries but with the help of strict laws, some governments have been able to reduce the number of accidents cause by drunk drivers. This is a battle which has to be fought by the governments for a long time and quick fix solutions will not work effectively.
4. A ban on alcohol would harm the economy. A ban on alcohol would not only infringe the civil liberties of the citizens, it would also cause great financial loss. A ban on alcohol would put thousands of persons out of work as the alcohol industry is an enormous industry of the world. Large amount of revenue is collected by the governments in the form of taxes and duties levied on alcoholic drinks. A ban on alcohol would take away a major source of revenue which used for public services.
_
Disadvantages of an alcohol ban:
•Health services have to deal with people having difficulties to detox.
•Drug use can increase, especially amphetamines.
•Student school attendance drops significantly.
•Violence and fighting increases.
•Alcohol addicts embark on grog sprints driving hundreds of kilometers to buy alcohol, increasing their risk of having an accident in the process.
•Non-drinkers do sly-grogging to supply drinkers with alcohol.
•Publicans oppose bans. Publicans can be the only source of alcohol for hundreds of kilometers, making “a killing” from selling alcohol. They earn thousands of dollars a week and have no interest in a ban.
•Families lose money because of fines they have to pay when a member violates the ban.
•Drinkers simply relocate, for example to the outskirts of town.
•Crime rates rise as people break into properties looking for alcohol.
•Drinkers set up drinking camps outside restricted zones where they binge drink.
_
Mafia and prohibition:
The American Mafia, an Italian-American organized-crime network with operations in cities across the United States, particularly New York and Chicago, rose to power through its success in the illicit liquor trade during the 1920s Prohibition era. After Prohibition, the Mafia moved into other criminal ventures, from drug trafficking to illegal gambling, while also infiltrating labor unions and legitimate businesses such as construction and New York’s garment industry. The Mafia’s violent crimes, secret rituals and notorious characters such as Al Capone and John Gotti have fascinated the public and become a part of popular culture.
_
My view on prohibition:
Historically and culturally majority of world population have been drinking alcoholic beverages for thousands of years. There is also a biological proclivity for low alcohol consumption by humans. Light responsible drinking has many health benefits. The prohibition of alcohol was a complete and humiliating failure to America in 1920s. Prohibition invariably leads to illicit liquor trade. The state loses large amount of revenue in the form of taxes and duties levied on alcoholic drinks which goes to liquor mafia. In India, Gujarat state has prohibition but alcohol is available all over Gujarat with police officers making money to allow production and sale of alcohol albeit illegally. I live in a town Daman bordering Gujarat and I see tourists coming to Daman from Gujarat only to drink unlimited legal alcohol, so called liquor tourists. In my view, prohibition always fails; better options are education and making liquor very expensive. I found that whenever alcohol is expensive, it is consumed less.
______
Effects on Society of Alcohol Use: Injuries and Violence:
Researchers have identified and classified a wide variety of adverse consequences for people who drink and their families, friends, co-workers, and others they encounter (Edwards et al. 1994; Harford et al. 1991; Hilton 1991). Alcohol-related problems include economic losses resulting from time off work owing to alcohol-related illness and injury, disruption of family and social relationships, emotional problems, impact on perceived health, violence and aggression, and legal problems. The risk of such consequences for the individual varies widely and depends on the situation. However, researchers have found a general trend toward an increased risk of adverse effects on society as the average alcohol intake among individuals increases (Mäkelä and Mustonen 1988; Mäkelä and Simpura 1985). The pattern of drinking also is important in determining the risk of alcohol-related problems. Variables such as the frequency of heavier drinking occasions (Midanik 1995; Midanik et al. 1996; Room et al. 1995) and the frequency of drinking to intoxication (Harford et al. 1991; Hilton 1991a; Knupfer 1984; Midanik 1995) help to predict potential problems related to alcohol, even after average volume of intake is controlled for.
Injuries:
Alcohol use is associated with increased risk of injury in a wide variety of circumstances, including automobile crashes, falls, and fires (Cherpitel 1992; Freedland et al. 1993; Hingson and Howland 1993; Hurst et al. 1994). The increased risk of injury stems primarily from reduced cognitive function, impaired physical coordination and performance, and increased risk-taking behavior (Koelega 1995). In addition, alcohol increases the likelihood of more serious injury and lowers the probability of survival because of its effects on the heart and circulatory system (Fuller 1995; Li et al. 1997). Culture and drinking environment also influence the relationship between alcohol and various types of injury (Cherpitel 1997).
Research shows that as people drink increasing quantities of alcohol, their risk of injury increases steadily and the risk begins to rise at relatively low levels of consumption (Cherpitel et al. 1995). An analysis of risk in relation to alcohol use in the hours leading up to an injury has suggested that the amount of alcohol consumed during the 6 hours prior to injury is related directly to the likelihood of injury occurrence (Vinson et al. 1995). The evidence showed a dose-response relationship between intake and injury risk—the more a person drank, the greater the risk—and found no level of drinking to be without risk. In contrast, two studies of injury among older adults reported a U-shaped relationship between alcohol use and occupational injury (Zwerling et al. 1996) and between alcohol use and traumatic deaths (Ross et al. 1990). In these studies, abstaining was associated with a higher risk of injury than were low to moderate levels of alcohol intake. However, abstinence among the elderly may be related to existing health or cognitive problems, which, in turn, are related to risk of injury (Zwerling et al. 1996). The pattern of drinking, such as binge drinking, clearly relates to the relative risk of injury, with risk increasing markedly as blood alcohol concentration rises (Hurst et al. 1994). Tolerance to the effects of alcohol may mediate the risk and severity of injury (Li et al. 1997), but the degree of protection is limited. Both frequent heavy drinking and frequent drunkenness are associated with injury, particularly that resulting from violence (Cherpitel 1996). Variation in the amount a person drinks on different occasions appears to have the strongest relationship with a high risk of injury; in contrast, consistently drinking small amounts of alcohol across occasions is associated with a lower risk of injury (Gruenewald et al. 1996a,b; Treno et al. 1996).
Violence:
Patterns of alcohol consumption also increase the risk of violence and the likelihood that aggressive behavior will escalate (Cherpitel 1994; Martin 1992; Martin and Bachman 1997; Norton and Morgan 1989; Zhang et al. 1997). Alcohol appears to interact with personality characteristics, such as impulsiveness and other factors related to a personal propensity for violence (Lang 1993; Zhang et al. 1997). Violence-related trauma also appears to be more closely linked to alcohol dependence symptoms than to other types of alcohol-related injury (Cherpitel 1997). Of the 11.1 million victims of violent crime each year, almost one in four, or 2.7 million, report that the offender had been drinking alcohol prior to committing the crime (Greenfeld 1998). Alcohol-related violence is the result of complex interactions between individual and environmental factors that either promote or inhibit violence. Findings from numerous studies implicate several variables—including personality factors, individual expectancies, situational elements, and sociocultural influences—that may interact with alcohol’s pharmacologic effects.
_
Does Alcohol consumption cause Crime?
Although there is a close relationship between alcohol and crime, the impact of alcohol as a cause of crime should be seen in the context of other causal factors. The use of alcohol alone, explains very little, whereas alcohol use in combination with an assortment of other variables can account for a substantial proportion of criminal behaviour. Clearly, there is much crime that is not committed under the influence of alcohol and many persons who drink, and even abuse alcohol, do not commit criminal offences. This fact alone casts doubt on the existence of a direct causal link. For example, Scutt (1980) states, with reference to domestic violence, that in almost one-third of cases (if not more) there is no prior consumption of alcohol. “Thus in many cases drink can in no way be said to ‘cause’ or be related to the violence – what then is the cause in these cases?”. Despite the complexities in establishing a causal relationship between alcohol and crime, some research suggests that alcohol consumption may promote or facilitate the planning or execution of a crime. On the other hand it can be argued that alcohol consumption may actually impede or inhibit the commission of some criminal offences. Although no research on this possibility has been noted, Collins (1981) claims the existence of a “malevolent assumption” that whenever drinking is associated with an unwelcome event it is considered to be the cause of that event.
_
Alcohol-related crime includes not only offences that are alcohol-specific such as drunk and disorderly or offences against the licensing laws but covers a continuum of offences which involve alcohol to a greater or lesser degree. Alcohol can be a disinhibitor, can be used as an excuse, or can result in crime because the individual has a drinking problem. Although alcohol can cause crime, usually it is no more than associated with offending. Drunkenness as a crime appears to cross all age boundaries but is associated mainly with the young, particularly young males where the offence involves aggression. The link between alcohol and aggression is not a simple one. Situational factors appear to play a strong role in alcohol-related aggressive acts which are in turn often influenced by the protagonist’s expectations of the outcome of a situation. A ccohol-related aggression often results in facial injury, with beer glasses used as weapons. Men, particularly young men, are the most likely victims. However, there is also a strong link between domestic violence where women are the victims, and alcohol. Men who drink heavily are more likely to physically abuse their partners. Consequently, women are more likely than men to be injured in the home, while men are more likely to sustain injury near licensed premises.
_
Alcohol and interpersonal violence:
_
Based on victim reports, alcohol use by the offender was a factor in:
•37% of rapes and sexual assaults
•15% of robberies
•27% of aggravated assaults, and
•25% of simple assaults
_
Researchers in Australia have also estimated that 47% of all those who commit violent crimes, and 43% of all victims of these crimes, were drunk prior to the event. Alcohol is responsible for 44% of fire injuries, 34% of falls and drownings, 30% of car accidents, 16% of child abuse instances, and 7% of industrial accidents.
_
_
Research on the Alcohol and Crime Connection:
Studies overwhelmingly indicate that there is a strong link between the consumption of alcohol and violent acts.
1. Almost one in four victims of violent crime report that the perpetrator had been drinking prior to committing the violence.
2. Over one-third of victims of rapes or sexual assaults report that the offender was drinking at the time of the act.
3. It is estimated that 32 to 50 percent of homicides are preceded by alcohol consumption by the perpetrator.
4. Between 31 percent and 36 percent of prisoners convicted of a violent crime against an intimate reported that they were drinking alcohol at the time of the offense. These figures rise to approximately 50 percent when reports from those who were consuming both alcohol and drugs at the time of the offense are considered.
5. Two-thirds of the victims of intimate violence reported that the offender was using alcohol at the time of the act.
6. Between 27 percent and 47 percent of all homicides and acts of purposeful injury are attributable to the use of alcohol
_
_
Alcohol expectations:
Alcohol expectations are beliefs and attitudes that people have about the effects they will experience when drinking alcoholic beverages. They are just largely beliefs about alcohol’s effects on a person’s behaviors, abilities, and emotions. Some people believe that if alcohol expectations can be changed, then alcohol abuse might be reduced. Men tend to become more aggressive in laboratory studies in which they are drinking only tonic water but believe that it contains alcohol. They also become less aggressive when they believe they are drinking only tonic water, but are actually drinking tonic water that contains alcohol. The phenomenon of alcohol expectations recognizes that intoxication has real physiological consequences that alter a drinker’s perception of space and time, reduce psychomotor skills, and disrupt equilibrium. The manner and degree to which alcohol expectations interact with the physiological short-term effects of alcohol, resulting in specific behaviors, is unclear. A single study found that if a society believes that intoxication leads to sexual behavior, rowdy behavior, or aggression, then people tend to act that way when intoxicated. But if a society believes that intoxication leads to relaxation and tranquil behavior, then it usually leads to those outcomes. Alcohol expectations vary within a society, so these outcomes are not certain. People tend to conform to social expectations, and some societies expect that drinking alcohol will cause disinhibition. However, in societies in which the people do not expect that alcohol will disinhibit, intoxication seldom leads to disinhibition and bad behavior. Alcohol expectations can operate in the absence of actual consumption of alcohol. Research in the United States over a period of decades has shown that men tend to become more sexually aroused when they think they have been drinking alcohol, — even when they have not been drinking it. Women report feeling more sexually aroused when they falsely believe the beverages they have been drinking contained alcohol (although one measure of their physiological arousal shows that they became less aroused).
_
Alcohol primes and aggression:
Alcohol-related terms can influence people in same way as actually drinking, study finds:
New psychology research shows that exposing people to alcohol-related words can influence aggressive behaviour in ways similar to actually consuming alcohol. Researchers found however that this aggressive behaviour occurred when people were subjected to provocation in a way that was not a clear-cut insult. Although it has been long known that drinking alcohol can increase aggression, a team of five psychologists, including Dr Eduardo Vasquez of the University of Kent and others from two US universities, demonstrated in two experiments that participants exhibited aggression following exposure to alcohol-related words – known as alcohol priming. This effect was demonstrated in situations when they were provoked in a way that was ambiguous or not obvious. These findings will have implications for understanding the way people behave in situations where alcohol is present, including bars sporting events and parties. The study – titled, Are You Insulting Me? Exposure to Alcohol Primes Increases Aggression Following Ambiguous Provocation – was conducted via two experiments involving US undergraduates. In the first, half of the students were exposed to alcohol primes – for example, the words ‘wine’, ‘beer’ and ‘whiskey’ – while the other half were exposed to non-alcohol primes – for example, ‘milk’, ‘water’ and ‘juice’ – prior to receiving feedback on an essay they had written. Participants demonstrated increased aggressive retaliation when provoked by the essay feedback, but only when the provocation could not be clearly interpreted as an insult. An unambiguous or clear provocation produced highly aggressive responses, regardless of whether a person was primed with alcohol or not. The second experiment showed that the effects of alcohol priming are fairly short-lived – the effect begins to diminish after seven minutes and is gone after about fifteen minutes following exposure to alcohol words. It also showed that alcohol priming influenced aggression by making the ambiguous provocation appear more hostile. Dr Vasquez, of Kent’s School of Psychology, said: ‘These results provide another strong demonstration that exposing someone to alcohol-related words alone can influence social behaviour in ways that are consistent with the effects of alcohol consumption. ‘Our research also examined the parameters within which alcohol priming is likely to affect aggression. These effects seem to occur primarily when the provocation is not clear-cut and obvious, and are thus more open to interpretation. Under alcohol priming, the interpretation becomes more negative, and people become more aggressive. ‘We’ve shown that people attending events where alcohol is typically present do not have to drink to experience, or be subject to, the aggression-enhancing effects of alcohol, a fact that would seem to suggest caution in all such environments.’
___
Alcohol and sexual assault:
• At least 50% of college students’ sexual assaults are associated with alcohol use
• In 81% of the alcohol related sexual assaults, both victim and the perpetrator had consumed alcohol
• When alcohol is involved, survivors are less likely to name the experience “rape”
_
Alcohol and rape: The connection:
Date rape and acquaintance rape are forms of sexual assault involving coercive sexual activities perpetrated by an acquaintance of the rape survivor. The perpetrator is almost always a man, and though both men and women can be raped, women are most often the targets of this violence. In many instances of rape, particularly acquaintance rape, alcohol is often involved as alcohol lowers inhibitions and impairs judgment.
1. A woman is more likely to place herself in a potentially dangerous situation (e.g., being alone with someone she does not know well) if she has been drinking. In addition, a potential victim would be less likely to recognize “early signs” of trouble and would be less effective in fleeing or resisting should either become necessary.
2. Alcohol also lowers inhibitions and reduces one’s “normal” checks on behavior. A perpetrator is less likely to notice and to respect subtle or direct messages to stop.
3. Drinking interferes with communication between partners. Discussing what you do and don’t want is difficult in an impaired state.
4. Assailants may consciously choose an impaired victim. It is easier to force sex on an impaired individual. As such, a potential victim may be encouraged to drink excessively or her drinks may be “spiked” in order to sexually exploit her.
5. Drinking/drunkenness is often used to justify behavior that would never be acceptable in a sober state. Ironically, a woman’s use of alcohol or drugs often implicates her in the eyes of others. She is viewed as responsible for the assault if she was drinking.
_
Research on Alcohol’s Effects on Aggressive and Sexual Behavior:
Research suggests that alcohol exerts its effects on aggressive behavior principally through its pharmacological effects on cognitive processing, whereas alcohol’s effects on sexual behavior occur through pharmacological processes as well as psychological expectancies. Crowe and George (1989) summarized the literature by arguing that expectancies reduce “inhibitory conflict, enabling alcohol-induced cognitive impairments to disinhibit behavior. As inebriation increases, therefore, inhibition is reduced both by expectancies and by increasing inability to process inhibitory cues.”
_
Alcohol’s Effects in Sexual Assault Situations:
Abbey and colleagues (1994, 1996) have developed a model to explain the role of alcohol in sexual assaults perpetrated by acquaintances. The model suggests that alcohol acts at two distinct points during the interaction between the perpetrator and the victim to increase the likelihood of sexual assault. The first point is during the early stages of the interaction, when the man is evaluating the likelihood that his companion wants to have sex with him. This evaluation is an ongoing process. During a date or other social interaction, many points occur at which a man evaluates the potential sexual meaning of a female companion’s verbal or non-verbal cues. Alcohol can contribute to the misperception of the woman’s cues in such a way that the man perceives her as being more encouraging than she really is because of alcohol’s effects on his cognitive functioning. The woman experiences the same cognitive deficits as the man does if the woman also consumes alcohol. Thus, if she feels that she has made it clear that she is not interested in sex at this point, alcohol consumption will make her less likely to process the man’s cues indicating that he has misread her intentions. This model is difficult to test directly, however, because researchers must rely on participants’ retrospective recall of sexual assault situations. Nevertheless, a study among college men found that increased alcohol consumption in social situations increased the participants’ misperceptions of women’s cues (Abbey et al. 1998). The extent of such misperceptions, in turn, was related to the frequency with which the men committed sexual assault. In a parallel study among college women, drinking in situations in which men misperceived the women’s sexual intentions increased the likelihood that the women became victims of a sexual assault (Abbey et al. 1996a). In addition, Testa and Livingston (1999) found that women who had been drinking prior to being sexually assaulted reported that their intoxication made them take risks that they normally would avoid. For example, the women felt comfortable accepting a ride home from a party with a man they did not know well or letting an intoxicated man into their apartment. The second point at which alcohol plays a role in sexual assault is when the man forces sex on a woman against the woman’s wishes. Alcohol is not necessary in this scenario, because some men feel entitled to force sex on women if they feel that they have been “led on” or teased (Abbey et al. 1994). The cognitive deficits associated with alcohol consumption, however, can enhance a man’s likelihood of behaving aggressively, because an intoxicated man may have more difficulty generating non-aggressive solutions to gaining sexual satisfaction. Thus, when a man is intoxicated, he can more easily focus on his immediate sexual gratification, sense of entitlement, and anger, rather than on his internalized sense of appropriate behavior, future regret, the victim’s suffering, or the possibility that he will be punished for his actions. Furthermore, in laboratory studies, intoxicated men tend to retaliate strongly when they feel threatened, and once they begin behaving aggressively, they can only be stopped with great difficulty (Taylor and Chermack 1993). Accordingly, if an intoxicated man feels that his female companion has implicitly agreed to sex, he may perceive any resistance as a threat and thus become aggressive in retaliation. The effect of his aggressive behavior is further exacerbated if the woman is intoxicated, because alcohol’s effects on motor skills may limit her ability to resist effectively (Koss and Dinero 1989). To support the aforementioned hypotheses, researchers must demonstrate that sexual assaults involving intoxicated perpetrators and/or intoxicated victims are more likely than other sexual assaults to include extreme levels of forced sex, more violent behavior, and more injuries to the victim. In fact, some studies indicate that completed rapes (as opposed to attempted rapes) are more common among intoxicated victims than among sober victims, suggesting that intoxicated women are less able than sober women to resist an assault effectively (Abbey et al. 1996b; Harrington and Leitenberg 1994). Surprisingly, recent studies focusing on alcohol consumption among men have not confirmed that drinking men are more likely to successfully commit rape, as opposed to attempt rape but fail in their efforts. Nonetheless, more serious victim injuries have been associated with alcohol consumption by the perpetrator (Martin and Bachman 1998; Ullman et al. 1999). These studies, however, suffer from serious methodological limitations with respect to measuring the perpetrators’ alcohol consumption. The investigators assessed only whether the perpetrators consumed any alcohol before the assault and did not determine how much alcohol the perpetrators consumed or how far in advance of the assaults the drinking occurred. Consequently, the studies did not provide conclusions as to how intoxicated the perpetrators were at the times of the assaults. For example, men who had consumed only one drink several hours before the assault may not have been intoxicated at all. Conversely, men who were extremely intoxicated may have experienced sexual and motor impairments that made sexual assault completion unlikely.
____________
Rehabilitation of alcoholic:
After completing alcoholic rehabilitation, 60% of alcoholics, especially middle-class patients, maintain abstinence for at least a year, and many achieve lifetime sobriety. The core of treatment uses cognitive-behavioral approaches to help patients recognize the need to change, while working with them to alter their behaviors to enhance compliance. A key step is to optimize motivation toward abstinence through education about alcoholism and instructions to family members to stop protecting the patient from problems caused by alcohol. After years of heavy drinking, patients also need counseling, vocational rehabilitation, and self-help groups such as Alcoholics Anonymous (AA) to help them learn how to deal with life’s stresses while sober. A third component, relapse prevention, helps the patient to identify situations in which a return to drinking is likely, formulate ways of managing these risks, and develop coping strategies that increase the chances of a return to abstinence if a slip occurs. While many patients can be treated as outpatients, more intense interventions work better, and some alcoholics do not respond to AA or outpatient groups. Whatever the setting, subsequent contact with outpatient treatment staff should be maintained for a minimum of 6 months and preferably a full year after abstinence. Counseling focuses on areas of improved functioning in the absence of alcohol (i.e., why it is a good idea to continue to abstain) and helping the patient to manage free time without alcohol, develop a nondrinking peer group, and handle stresses on the job.
_
The physician serves an important role in identifying the alcoholic, diagnosing and treating associated medical or psychiatric syndromes, overseeing detoxification, referring the patient to rehabilitation programs, providing counseling, and, if appropriate, selecting which (if any) medication might be needed. For insomnia, patients should be reassured that troubled sleep is normal after alcohol withdrawal and will improve over subsequent weeks. They should be taught the basic elements of “sleep hygiene” including maintaining consistent schedules for bedtime and awakening. Sleep medications have the danger of being misused and of rebound insomnia when stopped. Sedating antidepressants (e.g., trazodone) should not be used as they interfere with cognitive functioning the next morning and disturb the normal sleep architecture, but occasional use of over-the-counter sleeping medications (sedating antihistamines) can be considered. Anxiety can be addressed by helping the person to gain insight into the temporary nature of the symptoms and to develop strategies to achieve relaxation as well as by using forms of cognitive therapy.
_
Medications for Rehabilitation:
Several medications have modest benefits when used for the first 6 months of recovery. The opioid-antagonist, naltrexone, 50–150 mg/d orally, appears to shorten subsequent relapses, whether used in the oral form or as a once-per-month 380-mg injection, especially in individuals with the G allele of the AII8G polymorphism of the opioid receptor. By blocking opioid receptors, naltrexone may decrease activity in the dopamine-rich ventral tegmental reward system, and decrease the feeling of pleasure or reward if alcohol is imbibed. A second medication, acamprosate at 2 g/d divided into three oral doses, has similar modest effects; acamprosate inhibits NMDA receptors, decreasing mild symptoms of protracted withdrawal. Several trials of combined naltrexone and acamprosate using doses similar to those noted above have reported that the combination may be superior to either drug alone, although not all studies agree.
_
It is more difficult to establish the asset-to-liability ratio of a third drug, disulfiram, an ALDH inhibitor, used at doses of 250 mg/d. This drug produces vomiting and autonomic nervous system instability in the presence of alcohol as a result of rapidly rising blood levels of the first metabolite of alcohol, acetaldehyde. This reaction can be dangerous, especially for patients with heart disease, stroke, diabetes mellitus, or hypertension. The drug itself carries potential risks of depression, psychotic symptoms, peripheral neuropathy, and liver damage. Disulfiram is best given under supervision of another individual (such as a spouse), especially during discrete periods identified as representing high-risk drinking situations (such as the Christmas holiday). Other relevant drugs under investigation include the nicotinic receptor agonist varenicline, the serotonin antagonist ondansetron, the -adrenergic agonist prazosin, the GABA-B receptor agonist baclofen, the anticonvulsant topiramate, and cannabinol receptor antagonists. At present, there are insufficient data to determine the asset-to-liability ratio for these medications in treating alcoholism and, therefore, no data to offer solid support for their use in clinical settings.
_
Ways to reduce the burden from harmful use of alcohol:
The health, safety and socioeconomic problems attributable to alcohol can be effectively reduced and requires actions on the levels, patterns and contexts of alcohol consumption and the wider social determinants of health. Countries have a responsibility for formulating, implementing, monitoring and evaluating public policies to reduce the harmful use of alcohol. Substantial scientific knowledge exists for policy-makers on the effectiveness and cost–effectiveness of the following strategies:
•regulating the marketing of alcoholic beverages (in particular to younger people);
•regulating and restricting availability of alcohol;
•enacting appropriate drink-driving policies;
•reducing demand through taxation and pricing mechanisms;
•raising awareness of public health problems caused by harmful use of alcohol and ensuring support for effective alcohol policies;
•providing accessible and affordable treatment for people with alcohol-use disorders; and
•implementing screening and brief interventions programs for hazardous and harmful drinking in health services.
_
Self-regulation and discriminated aversive conditioning in the modification of alcoholics’ drinking behavior: A study:
Sixty alcoholics were treated with one of three treatment conditions: (1) aversion plus self-regulation which included blood alcohol concentration feedback training, discriminated aversive conditioning, training in self-regulation, education, and psychotherapy; (2) self-regulation which was identical to the aversion plus self-regulation condition, except that no shock was used; and (3) aversion which was identical to the aversion plus self-regulation group, except that no emphasis was given to the self-regulatory processes. Patients were evaluated in their homes at the end of treatment and at 6 and 12 months with additional information from a confederate of the patient. The group receiving both aversion training and self-regulation performed at the highest level throughout, with the self-regulation alone group responding better than the aversion group. This latter difference was not statistically significant. Relapse rates did not differ significantly. The study reflected the importance of individual responsibility and aversion therapy combined.
_
Alcoholics Anonymous (AA):
Alcoholics Anonymous is a fellowship of men and women who share their experience, strength and hope with each other that they may solve their common problem and help others to recover from alcoholism. The only requirement for membership is a desire to stop drinking. There are no dues or fees for AA membership; they are self-supporting through our own contributions. AA is not allied with any sect, denomination, politics, organization or institution; does not wish to engage in any controversy; neither endorses nor opposes any causes. Their primary purpose is to stay sober and help other alcoholics to achieve sobriety. Alcoholics Anonymous (AA) is an international mutual aid fellowship founded in 1935 by Bill Wilson and Dr. Bob Smith in Akron, Ohio. The Traditions recommend that members and groups remain anonymous in public media, altruistically help other alcoholics, avoiding affiliations with any other organization. The Traditions also recommend that those representing AA avoid dogma and coercive hierarchies. The scope of AA’s program is much broader than just abstinence from drinking alcohol. Its goal is to effect enough change in the alcoholic’s thinking “to bring about recovery from alcoholism” through a spiritual awakening. More informally than not, AA’s membership has helped popularize the disease concept of alcoholism, though AA officially has had no part in the development of such postulates which had appeared as early as the late eighteenth century. Though AA initially avoided the term “disease”, in 1973 conference-approved literature categorically stated that “we had the disease of alcoholism.” Regardless of official positions, from AA’s inception most members have believed alcoholism to be a disease. Internal AA surveys suggest that about 40% of the members sober for less than a year will remain another year. About 80% of those sober more than one year, but less than five years will remain sober and active in the fellowship another year. About 90% of the members sober five years or more will remain sober and active in the fellowship another year. Those who remained sober outside the fellowship could not be calculated using the survey results. AA is nonprofessional – it doesn’t have clinics, doctors, counselors or psychologists. All members are themselves recovering from alcoholism. There is no central authority controlling how AA groups operate. It is up to the members of each group to decide what they do. However, the AA program of recovery has proved to be so successful that almost every group follows it in very similar ways.
_
What AA does not do:
AA does not:
1. Furnish initial motivation for alcoholics to recover
2. Solicit members
3. Engage in or sponsor research
4. Keep attendance records or case histories
5. Join “councils” of social agencies
6. Follow up or try to control its members
7. Make medical or psychological diagnoses or prognoses
8. Provide drying-out or nursing services, hospitalisation, drugs, or any medical or psychiatric treatment
9. Offer religious services
10. Engage in education about alcohol
11. Provide housing, food, clothing, jobs, money or any other welfare or social services
12. Provide domestic or vocational counseling
13. Accept any money for its services, or any contributions from non-AA sources
14. Provide letters of reference to parole boards, lawyers, court officials, social agencies, employers, etc.
_
WHO response:
WHO aims is to reduce the health burden caused by the harmful use of alcohol and, thereby, to save lives, prevent injuries and diseases and improve the well-being of individuals, communities and society at large. WHO emphasizes the development, implementation and evaluation of cost-effective interventions for harmful use of alcohol as well as creating, compiling and disseminating scientific information on alcohol use and dependence, and related health and social consequences. In 2010, the World Health Assembly approved a resolution to endorse a global strategy to reduce the harmful use of alcohol. The resolution urged countries to strengthen national responses to public health problems caused by the harmful use of alcohol. The global strategy to reduce the harmful use of alcohol represents a collective commitment by WHO Member States to reduce the global burden of disease caused by harmful use of alcohol. The strategy includes evidence-based policies and interventions that can protect health and save lives if adopted, implemented and enforced. The strategy also contains a set of principles to guide the development and implementation of policies; it sets priority areas for global action, recommends target areas for national action and gives a strong mandate to WHO to strengthen action at all levels. The policy options and interventions available for national action can be grouped into 10 recommended target areas, which are mutually supportive and complementary. The 10 areas are:
•leadership, awareness and commitment
•health services’ response
•community action
•drink–driving policies and countermeasures
•availability of alcohol
•marketing of alcoholic beverages
•pricing policies
•reducing the negative consequences of drinking and alcohol intoxication
•reducing the public health impact of illicit alcohol and informally produced alcohol
•monitoring and surveillance.
The Global Information System on Alcohol and Health (GISAH) has been developed by WHO to dynamically present data on levels and patterns of alcohol consumption, alcohol-attributable health and social consequences and policy responses at all levels.
_________
Alcohol education:
Most people who consume beverage alcohol experience few problems as a result of their drinking. However, for some individuals, alcohol consumption is associated with harmful health and social consequences, largely as a result of their drinking patterns. Education around alcohol consumption is therefore an important tool in prevention and an essential component of health education in general. Structured approaches to alcohol education have been developed to help share specific information and change behavior. However, much of what we know about alcohol, how we view drinking, and whether we make the decision to drink are the result of an informal process that involves learning through personal experience and is largely shaped by culture. For policy and prevention, it is important to view alcohol education as one of several elements needed to reduce the risk for harm within a comprehensive approach to alcohol. While it may not offer all the solutions, alcohol education is an integral component of wide-ranging and balanced policies and prevention measures.
The aim of alcohol education is twofold:
1. to raise awareness and share knowledge and skills that will enable consumers to make healthy and informed choices about their drinking;
2. to help those who choose to drink avoid patterns that are associated with health and social harm to themselves and others.
Special efforts in alcohol education focus on individuals deemed at increased risk for harm. However, raising awareness among the general population and ensuring that those who choose to consume alcohol do so as safely as possible is another important outcome of education efforts (International Center for Alcohol Policies, 2004).
Alcohol education may be delivered in a range of formats, whose impact and effectiveness has been closely examined.
1. Mass media and information campaigns are widely used, although they are generally viewed as ineffective in changing behavior when implemented in isolation. However, there is evidence that such campaigns may be helpful in raising awareness about certain issues.
2. School-based education about alcohol is another popular approach, but there is also debate around its effectiveness in changing behavior, although some initiatives show more promise than others.
3. Targeted efforts that address particular groups of individuals are commonly used. These include programs for young people, problem drinkers, or other at-risk populations.
4. Specific interventions have been developed to deal with drinking patterns that may be especially problematic, such as “binge” drinking or drinking and driving.
5. Warning labels that address possible health outcomes, drinking and driving, or drinking during pregnancy may be found on containers of beverage alcohol in a number of countries. While labels may raise awareness among some individuals, when used by themselves, they have been largely ineffective in changing behavior.
6. Alcohol education may be integrated into general health education and provided through physicians, nurses, and other health or social workers.
7. Views, attitudes, and behaviors around drinking are largely the result of culture and environment. Parents, peers, and others who play an important role in the lives of young people, for example, can be operative in teaching youths about alcohol, and direct parental involvement is essential.
In general, there is evidence that targeted education measures with high specificity are likely to be more effective than broad-based approaches.
_
What Students need to be taught:
Alcohol abuse is becoming an increasing important topic among high school students. Although teachers try to teach them to not to ever start drinking and that it’s illegal to for a minor to consume alcohol, the reality is that they will be likely try it before they finish high school. A survey conducted by Chilton Shelby Mental Health Center showed that 79 of 187 students had at least tried alcohol and over half of the students said access to alcohol was easy because they got it from either friends or family members. When it’s easy to get alcohol while hanging out with friends at parties, then you will be more likely to drink because of peer pressure or plain curiosity. The best way to avoid alcohol abuse is to not start drinking. That is something that is taught in schools by showing them images and movies about what can happen to you when you drink. That can work for some students, but today it seems like the students will try it anyway regardless of the consequences. A better alternative might be to teach students more about alcoholic drinks and how to drink more responsibly. That means students will need to understand their limits to how much alcohol they can consume without becoming wasted. It would also be good to educate students on just how much alcohol is contained in certain drinks. Also, students should be taught about the dangers of driving under the influence of alcohol. This is done to an extent at schools, but the message is to always avoid drinking altogether. A better message to send students is that they shouldn’t try to drive when they’ve had too much to drink. Before the night starts, one person should be the designated driver. If everyone is going to drink, then you might want to instead decide to have a friend on call to come by and drive you home. We all know the best way not to abuse alcohol is not to start, but if you do drink, then you should at least know how to do it safely.
_
In a nutshell
1. Alcohol education should be an integral part of the school curriculum and should be tailored for different age groups and different learning needs
2. A ‘whole school’ approach should be adopted, covering everything from policy development and the school environment to staff training and parents and pupils should be involved in developing and supporting this
3. Where appropriate, children and young people who are thought to be drinking harmful amounts should be offered one-to-one advice or should be referred to an external service
4. Schools should work with a range of local partners to support alcohol education in schools, ensure school interventions are integrated with community activities and to find ways to consult with families about initiatives to reduce alcohol use.
___________
Strategies to Reduce the Personal and Public Costs of Alcohol:
Personal health behaviors:
•Monitor your alcohol intake (“know your number”). This is similar to knowing your blood pressure, cholesterol level, or calorie intake.
•Limit consumption to 20 g daily for men and 15 g daily for women.
•Less is more: Lower alcohol consumption leads to greater health and longevity.
•Take a day off. Not drinking for 1-2 days each week can help the liver recover from the effects of alcohol and reduce the risk for liver complications.
Government intervention:
•Apply a minimum pricing policy to alcohol to reduce consumption of cheap alcohol, especially by young people.
•Label the amount of alcohol in grams (like food labeling) to allow consumers to track the exact amount of alcohol they are consuming.
•Limit the times and places alcohol can be purchased to reduce impulse buying, and avoid contact with alcohol in shops and supermarkets.
•Provide treatment to benefit individuals and society; offer to all people with an alcohol dependence problem.
•Invest in research to develop new approaches to addiction.
•Develop alternatives to alcohol — investigate new drugs that mimic the milder effects of alcohol; simulate relaxation without the negative side effects of alcohol.
___________
Alcohol, economy and advertising:
Global Alcoholic Drinks Industry:
The global alcoholic drinks industry is expected to exceed $1 trillion in 2014, according to MarketLine. Market volume is predicted to reach almost 210 billion liters in 2014, a 10% increase in five years. Beer, cider and flavored alcoholic beverages represent the leading market segment with over half of the overall market value. The EU represents almost 57% of the world alcoholic drinks market. The industry is characterized by fragmentation with the three leading companies holding almost 40% of overall market volume. The market is lead by Anheuser-Busch InBev, which has over 20% of the overall market volume. Alcoholic beverages include beer, cider, ale, wine (including sparkling, barley, and rice wine) and spirits such as rum, whiskey, brandy and vodka. Almost 40% of the world’s alcoholic beverage consumption involves branded drinks that are usually large companies operating at an international level and investing heavily in marketing to promote image and encourage consumer loyalty.
_
The brewing industry (beer production) is a global business, consisting of several dominant multinational companies and many thousands of smaller producers known as microbreweries or regional breweries depending on size and region. More than 133 billion liters (35 billion gallons) are sold per year—producing total global revenues of $294.5 billion (£147.7 billion) as of 2006. SABMiller became the largest brewing company in the world when it acquired Royal Grolsch, brewer of Dutch premium beer brand Grolsch. InBev was the second-largest beer-producing company in the world and Anheuser-Busch held the third spot, but after the acquisition of Anheuser-Busch by InBev, the new Anheuser-Busch InBev company is currently the largest brewer in the world.
_
Economic impacts of alcohol:
The economic impacts of alcohol can usually be split into 2 categories; benefits and costs.
The economic benefits alcohol brings to society can be measured by the revenues generated in both the on and off-trade from the sales of alcoholic beverages locally, which in turn the Treasury receives a proportion of by taxation of company profits. They are also represented in the number of jobs created within any region where alcoholic beverages are produced and also indirectly for those who distribute alcohol as a commodity. These benefits may be more straightforward to calculate than some of the costs. There are uncertainties and disagreements about what should be included as a cost and how costs are to be measured. There are a number of different methodologies that can be employed in estimating economic costs, and these can have different implications for policy. In alcohol policy, costs are typically framed in terms of harm to the individual and the wider society. This allows policymakers to focus on the tangible factors that justify government intervention in order to be remedied, such as the costs to the health service of treating alcohol-related disease, and to the criminal justice system of dealing with alcohol related crime and disorder. However, the lack of a definitive set of ‘costs’ criteria means that there is no single figure representing the cost of alcohol consumption to the UK.
_
Alcohol – Economic costs and benefits in the EU:
Based on a review of existing studies, the total tangible cost of alcohol to EU society in 2003 was estimated to be €125bn, split between crime costs, health costs and lost productivity costs, equivalent to 1.3% GDP, which is roughly the same value as that found for tobacco. The intangible costs show the value people place on pain, suffering and lost life that occurs due to the criminal, social and health harms caused by alcohol. In 2003 these were estimated to be €270bn. The €125bn tangible cost of alcohol to EU society needs to be compared with the estimated value of the alcohol industry (€45bn), alcohol excise duties (€25bn), and alcohol’s contribution to the Union’s balance of trade (€9bn). Alcohol is also associated with a number of jobs, including over three-quarters of a million in drinks production (mainly wine). Further jobs are related to alcohol elsewhere in the supply chain, e.g. in pubs or shops. However, the size of the industry is not necessarily a good guide to the economic impact of alcohol policies – for example, trends in alcohol consumption show no crude correlation with trends in the number of jobs in associated areas such as hotels, restaurants, and bars, suggesting that the effect of changes in consumption may be relatively weak. A reduction in spending on alcohol would also be expected to free consumer funds to be spent on other areas, with the economic impact depending on the exact nature of the new expenditure.
In a nutshell, economic cost of alcohol to the state far exceeds tax revenue to state and jobs creation by alcohol manufacturers and supply chain.
_
Alcohol Abuse and its Effects on the Economy:
Drunk Driving Costs:
Drunk driving is a sensitive subject to many people because so many lives have been affected by this crime. The National Highway Traffic Safety Administration reports that alcohol-related motor vehicle crashes kill someone every 31 minutes and nonfatally injure someone every two minutes. During 2005, 16,885 people in the U.S. died in alcohol-related motor vehicle crashes, comprising 39% of all traffic-related deaths.
Medical and Social Costs:
Alcohol inflicts costs in many other ways as well. Alcohol abusers are medically at risk for liver damage, brain damage, and cancer, as well as causing Fetal Alcohol Syndrome in pregnant women. Alcohol is often a factor in homicides and suicides. Crimes caused by individuals influenced by alcohol put a strain on the criminal justice system, and inflict costs for police officers, legal fees, and property repair.
Workplace Costs:
Another large portion of the cost to the economy is the impact on employers by their alcohol-abusing employees. Health care costs have already skyrocketed, and because of the increased risk of medical problems with alcoholics, these individuals will incur higher health care costs. Absences are another issue for employers. Because of poor health, hangovers, or other alcohol related problems, alcohol abusers are more likely to miss work than many of their co-workers. Finally, loss of productivity is a strain businesses have to manage with employees that abuse alcohol. Even if an alcoholic is present at work and not drinking, their performance at work can often be compromised by hangovers, health complications, lack of focus, or psychiatric issues.
_
_
Ethanol boosts the price of your hamburger in the U.S.
Because nearly 40 percent of the nation’s corn crop is diverted to ethanol production for energy resources, the cost of beef is going up. Corn is used as feed for cows, and farmers are finding it harder to control prices. Checked the price of hamburger at the grocery store lately? Beef prices have been soaring, along with the cost of dairy, fruits and vegetables.
_
_
Alcohol sales thrive in bad economy.
Studies have shown that when the economy is down and at its low points the liquor sales go up in grocery stores but down in restaurants. Consumers are trying to save money by not going and spending lots of money at the restaurants and instead just going to the grocery store. Alcohol is withstanding the economic slowdown very well, compared to other categories that might be considered indulgent or not necessary to many consumers; alcoholic beverages are an affordable luxury.
_
Increased Prosperity brings added Alcohol Risks to Developing Countries:
Drinking will slow in the world’s leading economies and increase in developing nations over the next decade, posing risks for the global economy, a new report warns. The study’s findings support the link between a country’s economic wealth and how much its people drink. But drinking in a richer country also tends to be a safer proposition than in a poor one because such nations tend to have programs to deal with alcohol abuse as well as better health care and sounder infrastructure—such as safer roads—that mitigate risks. Public policies to contain possible damage from alcohol include drinking ages, bans on advertising, addiction treatment and measures against drunk driving.
_
The alcohol economy in India:
More than a fifth of alcohol produced in the world is consumed by Indians. State governments are becoming more and more dependent on alcohol revenue to pay their bills. The increasing consumption of alcohol will only fuel this dependence. With the exception of Gujarat, Nagaland, Mizoram and Manipur, where liquor is officially prohibited, alcohol revenue takes the second, third or fourth place in terms of contributions to a State’s coffers. Take, Tamil Nadu, for instance; in the last financial year, the Tamil Nadu State Marketing Corporation (Tasmac), the government-owned IMFL monopoly, alone paid a whopping Rs 21,800 crore into the government kitty. In Kerala, where 22 per cent of the total government revenue came from the bottle, the total excise and commercial tax revenue from alcohol (IMFL and toddy) was close to Rs 8,000 crore. However, alcohol taxation statistics are woefully inadequate and complex as revenue from liquor goes to many accounts in many departments, such as Excise and Commercial Taxes. Sales tax, Excise duty, import fee and education cess are some of the various forms of alcohol revenue. Indian Liquor Industry with estimated market value of INR 340 billion is growing at 12-15% over the last two years. The industry is estimated to have sold 115 million cases of IMFL last year. The sector is expected to maintain its CAGR of ~15% while the premium segment Wine and Vodka is expected to grow at a higher rate. With consolidation and foreign acquisitions gaining steam the sector is about to witness next phase with realization rising in line with that of their foreign counterparts. There are 325 distilleries in India, with an installed capacity of about 3.58 billion liters of liquor. However, production rate is about 40% of total licensed capacity as total requirement of liquor stands at 1.3 billion liters.
_
The Economics of Alcohol Abuse and Alcohol-Control Policies vis-à-vis India:
Economic research has contributed to the evaluation of alcohol policy through empirical analysis of the effects of alcohol-control measures on alcohol consumption and its consequences. It has also provided an accounting framework for defining and comparing costs and benefits of alcohol consumption and related policy interventions, including excise taxes. The most important finding from the economics literature is that consumers tend to drink less ethanol, and have fewer alcohol-related problems, when alcoholic beverage prices are increased or alcohol availability is restricted. That set of findings is relevant for policy purposes because alcohol abuse imposes large “external” costs on others. Important challenges remain, including developing a better understanding of the effects of drinking on labor-market productivity. Price levels, including excise taxes, are effective at controlling alcohol consumption. Raising excise taxes would be in the public interest. The production and sale of alcoholic beverages account for a small share of national product in the United States and in other advanced economies. However, the deleterious effects of alcohol consumption on health and safety constitute a substantial economic burden, reducing India’s overall standard of living. Chronic heavy drinking causes organ damage that result in disability and early death. Other possible consequences include cognitive impairment, addiction, reduced productivity, neglect of family responsibilities, and birth defects. The acute effects of alcohol abuse are still more costly: traumatic injury and property damage from accidents, criminal victimization, domestic violence, unwanted sexual encounters and venereal diseases, and hangover. In sum, alcohol is not just another commodity. Around the world, historically and currently, public concern about the consequences of excess alcohol consumption for individual health and community well-being has been incorporated in cultural norms, which are often reinforced by private rules and government regulation. The nature and extent of government involvement in the alcohol market has varied widely over time and place, reaching a logical extreme in the United States with Prohibition in the 1920s. In India, every state now has a wide array of alcohol-control measures in place, including a minimum age of purchase (twenty-one), excise taxes, a licensing system for retail outlets, and penalties for driving under alcohol’s influence. While alcohol control is not so contentious as when the temperance movement was in full flower, the relevant policies continue to be debated and are subject to change. To some extent, the debate over appropriate policy is concerned with factual issues. That is the arena in which economists have made their primary contribution. Economic research on the effects of alcohol-control measures on consumption and its consequences has helped to establish that such measures can be effective in reducing alcohol abuse and improving public health. But the debate is also concerned with values—of how best to balance the conflicts between individual liberty and community well-being. Economists have contributed to this discussion through application of cost-benefit analysis to the evaluation of alcohol-control measures and treatment. Economists’ normative framework is distinguished in part by its incorporation of the consumer-sovereignty principle, acknowledging the pleasures of drinking as well as the pains.
_
Alcohol pricing vs. consumption:
One thing that economists agree on is that if the price of a commodity is increased, the quantity purchased and consumed will decrease, other things being equal. But it is tempting to believe that alcoholic beverages—and especially the “active ingredient,” ethanol—may be an exception to this rule. For one thing, consumption of alcohol is limited in a variety of ways, not just price. Legal restrictions, cultural norms, and rules imposed by employers and other private organizations on where and when alcohol can be consumed are all relevant. Another limiting factor is widespread distaste for alcohol and the consequences of consumption. Price may be a secondary concern in this mix. Furthermore, alcohol represents a rather small part of the typical household budget, amounting to 2 percent of personal consumption expenditures, and employers pick up the tab for about 20 percent of alcohol sales. The most compelling argument that “alcohol is different” when it comes to the price effect may be that drinking is habit forming. Conventional wisdom (but not, it should be noted, economic theory) suggests that price will not matter much to those who have become addicted. In response to a general price increase for alcoholic beverages, alcoholics without much income could preserve their habit by seeking cheaper sources of ethanol: drinking off-premises rather than in bars, or buying fortified wine instead of table wine. However, and despite these plausible speculations, the evidence is clear that alcoholic beverages do obey the economists’ dictum after all: An increase in price results in reduced consumption, not only of the volume of beverage but also of ethanol.
_
The price level of alcoholic beverages influences per capita consumption levels of ethanol, as well as the incidence of alcohol abuse and its health-related consequences. Hence, excise taxes on alcoholic beverages are effective alcohol-control measures that can be used to promote public health. The minimum purchase age is also effective at reducing abuse. Other measures, including restrictions on alcohol advertising and dram-shop liability, appear promising.
_____
Alcohol advertising:
Alcohol advertising is the promotion of alcoholic beverages by alcohol producers through a variety of media. Along with tobacco advertising, it is one of the most highly-regulated forms of marketing. Some or all forms of alcohol advertising are banned in some countries. Scientific research, health agencies and universities have, over decades, been able to demonstrate a correlation between alcohol beverage advertising and alcohol consumption. Does alcohol advertising increase the overall level of alcohol consumption? Does it predispose children and adolescents to drinking? Although these and other related questions have been raised by public health advocates and echoed in public opinion surveys, the evidence from research to date is mixed and far from conclusive. In general, studies based on economic analyses suggest that advertising does not increase overall consumption, but instead may encourage people to switch beverage brands or types. At the same time, research based on survey data indicates that children who like alcohol advertisements intend to drink more frequently as adults. While these findings might offer some grounds for both reassurance and concern, the limitations of the research methods that have been used hinder the ability to draw firm conclusions about cause and effect in either case.
_
The figure above shows that alcohol advertising does not increase alcohol consumption. However many studies prove that advertising does increase alcohol consumption as reported in the following paragraphs.
_
Alcohol advertising with celebrity endorsers, humor, animation, and rock music has been shown to be especially appealing to adolescents (Atkin and Block 1983; Grube 1995). In addition, a study of adolescent boys confirmed that they were particularly attracted to alcohol advertisements depicting sports (Slater et al. 1996c, 1997). In one recent study, adolescents perceived that a significant number of alcohol advertisements portray people under 21 years of age (Slater et al. 1996b). Other research has indicated, however, that adolescents’ identification with the actors in the ads, or their desire to be like the actors, is relatively low (Austin and Meili 1994). Lifestyle- or image-oriented alcohol advertising has been shown to be more appealing to both adults and adolescents than is alcohol advertising that promotes only product quality (Covell et al. 1994).
_
How much alcohol advertising reaches youth:
•Alcohol advertisers spent $2 billion on alcohol advertising in measured media (television, radio, print, outdoor, major newspapers and Sunday supplements) in 2005.
•Working from alcohol company documents submitted to them, the Federal Trade Commission estimated in 1999 that the alcohol industry’s total expenditures to promote alcohol (including through sponsorship, Internet advertising, point-of-sale materials, product placement, brand-logoed items and other means) were three or more times its expenditures for measured media advertising. This would mean that the alcohol industry spent approximately $6 billion or more on advertising and promotion in 2005.
•Between 2001 and 2005, youth exposure to alcohol advertising on television in the U.S. increased by 41%. Much of this increase resulted from the rise in distilled spirits advertising on television from 1,973 ads in 2001 to 46,854 ads in 2005.
•Youth exposure to alcohol advertising in magazines decreased by 31% between 2001 and 2004. In 2004, more than half of youth exposure to alcohol advertising in magazines came from 22 brands, all of which exposed youth to their advertising more effectively than adults.
•In a sample of radio advertising for the 25 leading alcohol brands in the summer of 2004, more than two-thirds of youth exposure to alcohol advertising came from ads placed on youth-oriented programming, defined as programming with youth audiences larger than the population of youth ages 12 to 20 in the local market.
•From 2001 through 2003, youth in the United States were 96 times more likely per capita to see an ad promoting alcohol than an industry ad discouraging underage drinking. In fact, compared to underage youth, adults age 21 and over were nearly twice as likely per capita to see advertising discouraging underage drinking.
•A study of alcohol advertising in magazines from 1997 to 2001 found that the number of beer and distilled spirits ads tended to increase with a magazine’s youth readership. For every 1 million underage readers ages 12-19 in a magazine, researchers found 1.6 times more beer advertisements and 1.3 times more distilled spirits advertisements.
_
What teens and others think about alcohol advertising and youth:
•A USA Today survey found that teens say ads have a greater influence on their desire to drink in general than on their desire to buy a particular brand of alcohol.
•Eighty percent of general public respondents in a poll by the Bureau of Alcohol, Tobacco and Firearms believed “that alcohol advertising influences youth to drink alcoholic beverages.”
•Another poll, done for an alcohol-industry-funded organization called the Century Council, found that 73% of the public believes that “alcohol advertising is a major contributor to underage drinking.”
•The National Association of Broadcasters (NAB) recognizes the influence advertising can have on youth: “The impact of advertising on radio and television audiences, particularly kids, cannot be overstated. Clever jingles, flashy lights, fast talking, and quick pacing, all contribute to the message of commercials.”
_
According to 2001 College Alcohol Study (CAS), continuous alcohol promotions and advertisements including lowering prices on certain types of alcohol on a college campus have increased the percentage of alcohol consumption of that college community. Alcohol advertising on college campuses have also shown to increase binge drinking among students. However, it is concluded that the consistency of these special promotions and ads could also be useful in reducing binge drinking and other related drinking problems on campus. (Kuo, 2000, Wechsler 2000, Greenberg 2000, Lee 2000).
•Results from one study indicate that beer advertisements are a significant predictor of an adolescent’s knowledge, preference, and loyalty for beer brands, as well as current drinking behavior and intentions to drink (Gentile, 2001).
•Television advertising changes attitudes about drinking. Young people report more positive feelings about drinking and their own likelihood to drink after viewing alcohol ads (Austin, 1994; Grube, 1994).
•The alcohol industry spends $2 billion per year on all media advertising (Strasburger, 1999).
•The beer brewing industry itself spent more than $770 million on television ads and $15 million on radio ads in 2000 (Center for Science in the Public Interest, 2002).
Research clearly indicates that, in addition to parents and peers, alcohol advertising and marketing have a significant impact on youth decisions to drink. (The Center on Alcohol Marketing and Youth [CAMY]). “While many factors may influence an underage person’s drinking decisions, including among other things parents, peers and the media, there is reason to believe that advertising also plays a role.” (Federal Trade Commission, Self-Regulation in the Alcohol Industry, 1999) Parents and peers have a large impact on youth decisions to drink. However, research clearly indicates that alcohol advertising and marketing also have a significant effect by influencing youth and adult expectations and attitudes, and helping to create an environment that promotes underage drinking.
_
Evidence from long-term studies:
•A national study published in January 2006 concluded that greater exposure to alcohol advertising contributes to an increase in drinking among underage youth. Specifically, for each additional ad a young person saw (above the monthly youth average of 23), he or she drank 1% more. For each additional dollar per capita spent on alcohol advertising in a local market (above the national average of $6.80 per capita), young people drank 3% more.
•Another study found that, among a group of 2,250 middle-school students in Los Angeles, those who viewed more television programs containing alcohol commercials while in the seventh grade were more likely in the eighth grade to drink beer, wine/liquor, or to drink three or more drinks on at least one occasion during the month prior to the follow-up survey.
•Researchers followed 3,111 students in South Dakota from seventh to ninth grade, and found that exposure to in-store beer displays in grade 7 predicted onset of drinking by grade 9, and exposure to magazine advertising for alcohol and to beer concessions at sports or music events predicted frequency of drinking in grade 9.
•A study of 2,406 never-drinking New Hampshire middle school students found that ownership of alcohol-branded merchandise at baseline was significantly associated with increased likelihood of having initiated drinking (OR=1.5) at follow-up one to two years later, after adjusting for wide range of confounders.
•Researchers from Dartmouth Medical School followed more than 5,000 Vermont and New Hampshire students ages 10 to 14 from 13 to 26 months, and found that those with higher exposure to movie alcohol use at the initial assessment were more likely to have started drinking at time of follow-up. They also found depictions of alcohol use in 92% of 601 contemporary movies, including in 52% of G-rated films.
_
Evidence from studies of the effects of reductions in alcohol advertising:
•An econometric analysis using data from the National Longitudinal Survey of Youth 1997 estimated that a 28% reduction in alcohol advertising would reduce adolescent monthly alcohol participation from 25% to between 24% and 21%, and would reduce adolescent participation in binge drinking from 12% to between 11% and 8%.
•An effort to estimate the likely effects of several alcohol policies on youth drinking behavior in the U.S. population concluded that a complete ban on alcohol advertising would be the most effective, resulting in 7,609 fewer deaths from harmful drinking and a 16.4% drop in alcohol-related life-years lost.
•An analysis of the impact of evidence-based personal and environmental interventions on disability-adjusted life-years (DALYs) in 12 regions of the world found that in regions where heavy drinking is less prevalent, targeted strategies such as brief physician advice, roadside breath testing, and advertising bans would be most effective.
_
Evidence of how alcohol advertising attracts and influences young people:
•A study on the responses of young people to alcohol advertising found that underage youth are drawn to music, animal and people characters, story and humor in alcohol advertising. Ads that were liked by youth in the study were more likely to elicit responses from youth saying they wanted to purchase the brand and products advertised. The three most popular alcohol ads among youth in the study used animal characters as the leading actors.
•A review of the neuroscience, psychology and marketing literatures concluded that adolescents, because of how the human brain develops, may be particularly attracted to branded products such as alcohol that are associated with risky behavior and that provide, in their view, immediate gratification, thrills and/or social status.
•If young people like alcohol ads, they are more likely to have positive expectancies about alcohol use and to intend to drink or to drink.
•Exposure to alcohol advertising shapes attitudes and perceptions about alcohol use among both young people (defined in this study as ages 15-20) and young adults (ages 21 to 29). However, these attitudes and perceptions predict young people’s positive expectancies and intentions to drink, but not those of young adults.
_
Advertising and consumption of alcohol: A study:
The purpose of this paper is to empirically examine the relationship between alcohol advertising bans and alcohol consumption. Most prior studies have found no effect of advertising on total alcohol consumption. A simple economic model is provided which explains these prior results. The data set used in this study is a pooled time series of data from 20 countries over 26 years. The empirical model is a simultaneous equations system which treats both alcohol consumption and alcohol advertising bans as endogenous. The primary conclusions of this study are that alcohol advertising bans decrease alcohol consumption and that alcohol consumption has a positive effect on the legislation of advertising bans. The results indicate that an increase of one ban could reduce alcohol consumption by five to eight percent. The results suggest that recent exogenous decreases in alcohol consumption will decrease the probability of enactment of new bans and undermine the continuance of existing bans. Canada, Denmark, New Zealand and Finland have recently rescinded alcohol advertising bans. Alcohol consumption in these countries may increase or decrease at a slower rate than would have occurred had advertising bans remained in place.
_
Marketers in India evade Alcohol Ad Ban by promoting Surrogate Products:
It has never been easy for liquor companies to advertise in India, and so the country’s local brands have been taking the surrogate advertising route to make their names visible. Numerous brand extensions — CDs, mineral water, achievement awards, even an airline and a cricket team — flaunt the names of liquor brands and companies. The surrogate ads accounted for 5% of Indian ad spending, which totals about $4.5 billion.
__
Alcohol Advertising in Sports on TV:
• Alcohol producers spent $991 million on television advertising in 2002 – 60% of that was on sports programming
• Alcohol producers spent $596 million advertising on sports programming in 2002, an increase of more than 22% over 2001
• Beer marketers spent $58 million in 2002 for 6,251 ads in college sports programs
• In 2002, alcohol advertising represented 5.3% of all advertising dollars on college sports, compared to only 2.0% of all advertising on television
“We need to sever the tie between college sports and drinking. Completely, absolutely, and forever.”
Donna Shalala, Former Secretary U.S. Department of Health and Human Services:
_
The biggest factor of alcohol being socially acceptable would be the media:
The constant commercials and advertisements shown on TV by alcohol beverage companies have a major influence on society’s perception of alcohol. These commercials advertise these brands and encourage people to drink alcohol. Its images of people having a good time and feeling refreshed make people who watch these commercials think that it has these positive affects and yet no negative effects. Alcohol use by characters in various movies and TV Shows has also influenced drinking. Research has shown that after watching such movies, adolescents are more prone to drinking at a younger age. Media can also have a positive effect on the consumption of alcohol. Advertisements that discourage drink driving, alcoholism etc. has potential to reduce deaths and binge drinking rates. These advertisements designed by government agencies and alcohol help organisations could very much help the rate of alcohol and binge drinking in today’s society.
__
Alcohol and movies:
Alcohol use in movies can drive people to drink more:
Glamourised drinking in movies can encourage young adults to consume more alcohol, a new study has warned. The study of the effects of alcohol portrayals in movies has found that positive and negative portrayals of alcohol can contribute to viewers’ emotional involvement or “transportation” attitude towards, and evaluation of the movie. Drinking can be portrayed as being the cool thing to do in movies, but the consequences are rarely shown. “It is my understanding that alcohol portrayals are depicted in the majority of movies, 80 to 95 per cent, and that they are mostly framed or portrayed in a positive manner,” said Marloes Kleinjan, an assistant professor of developmental psychopathology at Radboud University Nijmegen. “Exposure to alcohol portrayals in the media – including movies, but also advertisements and digital media such as Facebook – can encourage drinking in young people. “Since movie characters can be regarded as role models by young people, the manner in which these characters portray alcohol use in a movie might have an impact on the beliefs and attitudes towards alcohol use by youngsters themselves,” said Kleinjan. The way and context in which alcohol is portrayed might play a role in the effects of movie alcohol portrayals “It is essential to test the extent to which alcohol portrayals affect engagement and transportation into a movie because emotional involvement in media content can be a significant requisite for being influenced by persuasive messages,” said Renske Koordeman, who wrote her dissertation on the topic while at Radboud University Nijmegen, Netherlands, and is the corresponding author for the study. Koordeman and her co-authors used a within-subjects design in which participants were exposed to eight different movie clips containing alcohol (positive or negative context), or no alcohol portrayals, in a controlled lab setting. A total of 159 college students (84 males, 75 females), 18 to 30 years of age, participated in the experiment. Transportation and attitude towards the movie were measured for each participant after each movie clip. “This study provides initial evidence that alcohol and the way in which alcohol is portrayed in movies contributes to how people evaluate and become transported in movies,” said Koordeman. “Participants were more transported into and had a more positive attitude towards movie clips with alcohol portrayals compared to the same movie clips with no alcohol portrayals. “In addition, participants were more transported into movie clips with negative alcohol portrayals compared to clips with positive alcohol portrayals. However, participants endorsed more positive attitudes towards clips with positive alcohol portrayals compared to clips with negative alcohol portrayals,” Koordeman said. Researchers agreed that the way and context in which alcohol is portrayed might play a role in the effects of movie alcohol portrayals. The study appears in the journal Alcoholism: Clinical & Experimental Research.
_____________
Alcohol as fuel:
Throughout history, alcohol has been used as a fuel. The first four aliphatic alcohols (methanol, ethanol, propanol, and butanol) are of interest as fuels because they can be synthesized chemically or biologically, and they have characteristics which allow them to be used in internal combustion engines. The general chemical formula for alcohol fuel is CnH2n+1OH. Most methanol is produced from natural gas, although it can be produced from biomass using very similar chemical processes. Ethanol is commonly produced from biological material through fermentation processes. However, ethanol that is derived from petroleum should not be considered safe for consumption as the mixture contains about 5% methanol and may cause blindness or death. Biobutanol has the advantage in combustion engines in that its energy density is closer to gasoline than the simpler alcohols (while still retaining over 25% higher octane rating); however, biobutanol is currently more difficult to produce than ethanol or methanol. When obtained from biological materials and/or biological processes, they are known as bioalcohols (e.g. “bioethanol”). There is no chemical difference between biologically produced and chemically produced alcohols. One advantage shared by the four major alcohol fuels is their high octane rating. This tends to increase their fuel efficiency and largely offsets the lower energy density of vehicular alcohol fuels (as compared to petrol/gasoline and diesel fuels), thus resulting in comparable “fuel economy” in terms of distance per volume metrics, such as kilometers per liter, or miles per gallon.
_
Why choose Alcohol Fuel?
One of the strongest arguments for ethanol fuel is that we can make it ourselves, with no dependence on foreign resources. In 1925, Henry Ford told a New York Times reporter that “There’s enough alcohol in one year’s yield of an acre of potatoes to drive the machinery necessary to cultivate the fields for a hundred years.” This self-made businessman recognized the value of the American farm, and more specifically, the importance of domestically sourced materials. He envisioned farms across the country providing the crops needed to make both fuel and food. Another reason ethanol is such an attractive fuel option is that it’s basically liquid energy. Ethanol is a clear liquid that packs a lot of energy into a usable, storable, and transportable form — only petroleum can compete with ethanol on an energy-per-volume basis. But ethanol has an added benefit in that it’s oxygenated, meaning it has oxygen in its molecular structure, which results in a cleaner burn. Compared to gasoline, ethanol emits about 20 percent less hydrocarbons and carbon monoxide.
_
Advantages of alcohol fuel:
1. Almost every country can become energy independent. Anywhere that has sunlight and land can produce alcohol from plants. Brazil, the fifth largest country in the world imports no oil, since half its cars run on alcohol fuel made from sugarcane, grown on 1% of its land.
2. We can reverse global warming. Since alcohol is made from plants, its production takes carbon dioxide out of the air, sequestering it, with the result that it reverses the greenhouse effect (while potentially vastly improving the soil). Recent studies show that in a permaculturally designed mixed-crop alcohol fuel production system, the amount of greenhouse gases removed from the atmosphere by plants—and then exuded by plant roots into the soil as sugar—can be 13 times what is emitted by processing the crops and burning the alcohol in our cars.
3. We can revitalize the economy instead of suffering through Peak Oil. Oil is running out, and what we replace it with will make a big difference in our environment and economy. Alcohol fuel production and use is clean and environmentally sustainable, and will revitalize families, farms, towns, cities, industries, as well as the environment. A national switch to alcohol fuel would provide many millions of new permanent jobs.
4. No new technological breakthroughs are needed. We can make alcohol fuel out of what we have, where we are. Alcohol fuel can efficiently be made out of many things, from waste products like stale donuts, grass clippings, food processing waste and even ocean kelp. Many crops produce many times more alcohol per acre than corn, using arid, marshy, or even marginal land in addition to farmland. Just our lawn clippings could replace a third of the autofuel we get from the Mideast.
5. Unlike hydrogen fuel cells, we can easily use alcohol fuel in the vehicles we already own. Unmodified cars can run on 50% alcohol, and converting to 100% alcohol or flexible fueling (both alcohol and gas) costs only a few hundred dollars. Most auto companies already sell new dual-fuel vehicles.
6. Alcohol is a superior fuel to gasoline! It’s 105 octane, burns much cooler with less vibration, is less flammable in case of accident, is 98% pollution-free, has lower evaporative emissions, and deposits no carbon in the engine or oil, resulting in a tripling of engine life. Specialized alcohol engines can get at least 22% better mileage than gasoline or diesel.
7. It’s not just for gasoline cars. We can also easily use alcohol fuel to power diesel engines, trains, aircraft, small utility engines, generators to make electricity, heaters for our homes—and it can even be used to cook our food.
8. Alcohol has a proud history. Gasoline is a refinery’s toxic waste; alcohol fuel is liquid sunshine. Henry Ford’s early cars were all flex-fuel. It wasn’t until gasoline magnate John D. Rockefeller funded Prohibition that alcohol fuel companies were driven out of business.
9. The byproducts of alcohol production are clean, instead of being oil refinery waste, and are worth more than the alcohol itself. In fact, they can make petrochemical fertilizers and herbicides obsolete. The alcohol production process concentrates and makes more digestible all protein and non-starch nutrients in the crop. It’s so nutritious that when used as animal feed, it produces more meat or milk than the corn it comes from. That’s right; fermentation of corn increases the food supply and lowers the cost of food.
10. Locally produced ethanol supercharges regional economies. Instead of fuel expenditures draining capital away to foreign bank accounts, each gallon of alcohol produces local income that gets recirculated many times. Every dollar of tax credit for alcohol generates up to $6 in new tax revenues from the increased local business.
11. Alcohol production brings many new small-scale business opportunities. There is huge potential for profitable local, integrated, small-scale businesses that produce alcohol and related byproducts, whereas when gas was cheap, alcohol plants had to be huge to make a profit.
12. Scale matters—most of the widely publicized potential problems with ethanol are a function of scale. Once production plants get beyond a certain size and are too far away from the crops that supply them, closing the ecological loop becomes problematic. Smaller-scale operations can more efficiently use a wide variety of crops than huge specialized one-crop plants, and diversification of crops would largely eliminate the problems of monoculture.
13. The byproducts of small-scale alcohol plants can be used in profitable, energy-efficient, and environmentally positive ways. For instance, spent mash (the liquid left over after distillation) contains all the nutrients the next fuel crop needs and can return it back to the soil if the fields are close to the operation. Big-scale plants, because they bring in crops from up to 45 miles away, can’t do this, so they have to evaporate all the water and sell the resulting byproduct as low-price animal feed, which accounts for half the energy used in the plant.
14. The level of interest in using alcohol as a motor fuel has followed cycles of fuel shortages and/or low feed-grain prices.
15. Alcohols burn more completely, thus increasing combustion efficiency.
16. Advantages of mixing alcohol with gasoline are that alcohol tends to increase the octane rating and reduce carbon monoxide emissions.
_
Run your car on Ethanol:
Car engines have to be modified to run on straight ethanol. The simplest engine modifications include advancing the ignition timing by several degrees, rejetting the carburetor’s main fuel circuit to increase jet diameter by 30 to 35 percent in area, and adjusting or enlarging the idle circuit to allow more fuel flow. Fuel-injected engines can have their injectors replaced for greater flow, or the fuel pressure increased. There are also aftermarket kits designed to trick the engine’s microprocessor control unit into holding the fuel pulse open longer or compensating for an artificially lean condition by enriching the air-fuel mixture. Engines can be further optimized for ethanol by preheating the fuel and air, varying the heat range of the spark plugs and boosting the compression ratio.
_
| Energy content of some fuels compared with ethanol: | |||
| Fuel type | MJ/L | MJ/kg | |
| Dry wood (20% moisture) | ~19.5 | ||
| Methanol | 17.9 | 19.9 | |
| Ethanol | 21.2 | 26.8 | |
| E85 (85% ethanol, 15% gasoline) |
25.2 | 33.2 | |
| Liquefied natural gas | 25.3 | ~55 | |
| Autogas (LPG) (60% propane + 40% butane) |
26.8 | 50. | |
| Aviation gasoline (high-octane gasoline, not jet fuel) |
33.5 | 46.8 | |
| Gasohol (90% gasoline + 10% ethanol) |
33.7 | 47.1 | |
| Regular gasoline/petrol | 34.8 | 44.4 | |
| Diesel | 38.6 | 45.4 | |
| Charcoal, extruded | 50 | 23 | |
_
Ethanol is a renewable, domestically produced alcohol fuel made from plant material, such as corn, sugar cane, or grasses. Using ethanol can reduce oil dependence and greenhouse gas emissions. The United States became the world’s largest producer of ethanol fuel in 2005. The U.S. produced 13.9 billion U.S. liquid gallons (52.6 billion liters) of ethanol fuel in 2011, an increase from 13.2 billion U.S. liquid gallons (49.2 billion liters) in 2010, and up from 1.63 billion gallons in 2000. Brazil and U.S. production accounted for 87.1% of global production in 2011. In the U.S, ethanol fuel is mainly used as an oxygenate in gasoline in the form of low-level blends up to 10 percent (E10), and to an increasing extent, as E15 fuel for flex-fuel vehicles. The vehicle owner’s manual may indicate the manufacturer’s maximum recommended ethanol content. Vehicles will typically go 3% to 4% fewer miles per gallon on E10 and 4% to 5% fewer on E15 than on 100% gasoline. More than 20% of Brazilian cars are able to use 100% ethanol as fuel, which includes ethanol-only engines and flex-fuel engines. Flex-fuel engines in Brazil are able to work with all ethanol, all gasoline or any mixture of both. Brazil supports this population of ethanol-burning automobiles with large national infrastructure that produces ethanol from domestically grown sugar cane. Sugar cane not only has a greater concentration of sucrose than corn (by about 30%), but is also much easier to extract. The bagasse generated by the process is not wasted, but is used in power plants to produce electricity.
____________________
Other uses of alcohol:
_
Alcohol as antiseptic:
Alcohols, most commonly ethanol (60–90%), 1-propanol (60–70%) and 2-propanol/isopropanol (70–80%) or mixtures of these alcohols, are commonly referred to as “surgical alcohol”, and are used to disinfect the skin before injections are given, often along with iodine (tincture of iodine) or some cationic surfactants (benzalkonium chloride 0.05–0.5%, chlorhexidine 0.2–4.0% or octenidine dihydrochloride 0.1–2.0%).
_
Rubbing alcohol, USP / Surgical spirit, B.P. is a liquid prepared and used primarily for topical application. It is prepared from a special denatured alcohol solution and contains approximately 70 percent by volume of pure, concentrated ethanol (ethyl alcohol) or isopropyl alcohol (isopropanol). Individual manufacturers can use their own “formulation standards” in which the ethanol content usually ranges from 70-99% v/v. In Ireland and the UK, the equivalent skin preparation is surgical spirit, which is always an ethyl alcohol-isopropyl alcohol mixture. It is colorless. The melting point is -89 °C. The boiling point is 82.5 °C. The term “rubbing alcohol” has become a general non-specific term for either isopropyl alcohol (isopropanol) or ethyl alcohol (ethanol) rubbing-alcohol products.
_
Although several alcohols have been shown to be effective antimicrobials, ethyl alcohol (ethanol, alcohol), isopropyl alcohol (isopropanol, propan-2-ol) and n-propanol (in particular in Europe) are the most widely used. Alcohols exhibit rapid broad-spectrum antimicrobial activity against vegetative bacteria (including mycobacteria), viruses, and fungi but are not sporicidal. They are, however, known to inhibit sporulation and spore germination, but this effect is reversible. Because of the lack of sporicidal activity, alcohols are not recommended for sterilization but are widely used for both hard-surface disinfection and skin antisepsis. Lower concentrations may also be used as preservatives and to potentiate the activity of other biocides. Many alcohol products include low levels of other biocides (in particular chlorhexidine), which remain on the skin following evaporation of the alcohol, or excipients (including emollients), which decrease the evaporation time of the alcohol and can significantly increase product efficacy. In general, isopropyl alcohol is considered slightly more efficacious against bacteria and ethyl alcohol is more potent against viruses; however, this is dependent on the concentrations of both the active agent and the test microorganism. For example, isopropyl alcohol has greater lipophilic properties than ethyl alcohol and is less active against hydrophilic viruses (e.g., poliovirus). Generally, the antimicrobial activity of alcohols is significantly lower at concentrations below 50% and is optimal in the 60 to 90% range. Alcohols denature proteins by breaking the hydrogen bonds that link oppositely charged hydrogen and oxygen atoms on different parts of the chain-like molecules. They do this because they themselves form hydrogen bonds at these locations, causing the protein molecule to lose its shape. Their effectiveness depends on how concentrated they are. Ethanol, for example, works best against microorganisms at about 70% concentration, as it is easily absorbed by cells. At much higher concentrations, it coagulates proteins on the cell surface, preventing further penetration; microbes are often able to survive this, although they may be temporarily inactivated. In addition to denaturating proteins, these alcohols can have a dehydrating effect, and can also dissolve lipids — fats and oils — to some extent, which can damage cell membranes. Ethanol has a greater dehydrating effect, while isopropanol has a greater affinity for lipids. Several common bacteria can be killed off in less than two minutes with 70 percent ethanol, and 35 percent will slay some fungi in a minute flat. The stuff also kills many viruses, including HIV, but at low concentrations the job may take hours.
_
Ethanol-based soaps are becoming common in restaurants and are convenient because they do not require drying due to the volatility of the compound. Alcohol based gels have become common as hand sanitizers.
______
Alcohol thermometer:
The alcohol thermometer or spirit thermometer is an alternative to the mercury-in-glass thermometer and has similar functions. Unlike the mercury-in-glass thermometer, the contents of an alcohol thermometer are less toxic and will evaporate away fairly quickly. An organic liquid is contained in a glass bulb which is connected to a capillary of the same glass and the end is sealed with an expansion bulb. The space above the liquid is a mixture of nitrogen and the vapor of the liquid. For the working temperature range, the meniscus or interface between the liquid is within the capillary. With increasing temperature, the volume of liquid expands and the meniscus moves up the capillary. The position of the meniscus shows the temperature against an inscribed scale.
_____
Cooking with alcohol:
Many dishes incorporate alcoholic beverages into the food itself. Such dishes include coq au vin, chicken cacciatore, and boeuf bourguignon. More modern examples are beer grilled chicken and bratwursts boiled in beer. Adding beer, instead of water, to chili during cooking is popular. An overnight marinade of chicken, pork or beef in beer and spices is another example. Specialist cooking wines, liqueurs, vermouths and eaux de vie are widely used by professional chefs to enhance flavour in traditional and modern dishes. These are specially created to be an ingredient in cooking, not a beverage. As well as offering excellent value for money, they have a longer shelf life which avoids wastage. The addition of specialist cooking wines, liqueurs and vermouths adds flavour to finished meat and fish dishes; desserts benefit from the use of sweet or dry wines. In addition, the use of specialist cooking wine in marinades can tenderise meat and is of particular benefit to game dishes. Many chefs discourage serving the same alcoholic beverage with the meal that was cooked using it.
____
Alcohol stove:
A portable stove is a cooking stove specially designed to be portable and lightweight, as in camping, picnicking, backpacking, or other use in remote locations where an easily transportable means of cooking or heating is needed. Portable stoves can be used in diverse situations, such as for outdoor food service and catering and in field hospitals. The Trangia stove is a popular commercial alcohol stove using alcohol as fuel, which is available in many different models, from a single bare burner to an integrated expedition cooking system.
_
Preservative:
Alcohol is often used as a preservative for specimens in the fields of science and medicine.
_
Solvents:
Alcohols have applications in industry and science as reagents or solvents. Because of its relatively low toxicity compared with other alcohols and ability to dissolve non-polar substances, ethanol can be used as a solvent in medical drugs, perfumes, and vegetable essences such as vanilla. In organic synthesis, alcohols serve as versatile intermediates.
__________________
__________________
Discussion:
After having gone through alcohol in detail, I attempt to answer these questions in discussion segment.
Are we biologically primed to drink alcohol?
Are most studies on alcohol flawed?
Does alcohol help or harm?
What is the safe limit of alcohol consumption?
Is it moderate drinking or moderate life-style of moderate drinker that reduces cardiovascular mortality?
________
Are we biologically primed to drink alcohol?
Yes, but in small amount.
Photosynthesis created sugar from sun energy, CO2 and water releasing O2 in plants. Sun energy is extracted from sugar utilizing oxygen by animals including humans releasing CO2 & water. Alcohol is created by yeast and other microorganisms extracting sun energy from sugar without using oxygen releasing CO2. Animals and humans extract remaining sun energy from alcohol utilizing O2 and releasing CO2 & water. The released CO2 and water is recycled in photosynthesis. This proves role of alcohol in evolution of life on earth in last 3 billion years. All living organisms actually produce alcohol in small amounts by several pathways including humans. All ripe & over-ripe fruits that we eat daily have trace alcohol and microorganisms in our intestines generate 3 grams of alcohol daily. Alcohol preference appears to be an evolutionary inherited trait that came under positive selection in periods of mostly scarce resources for humans. Humans have evolved the necessary enzymatic functions that provide metabolic tolerance to low amounts of ethanol, thereby preventing intoxication. So there is a biological proclivity for low alcohol consumption by humans. There is no genetic biological mechanism to protect against high alcohol consumption as high concentrations of alcohol only became available in the last 10,000 years, a period too short to induce adequate evolutionary counter responses. Since humans have biological proclivity for small amount of alcohol consumption, alcohol cannot be classified as poison. Yes, it does become poison when you drink in excess amount.
________
Are most studies on alcohol flawed?
Yes. Most studies on alcohol are observational epidemiological studies and not double-blind randomized controlled studies (RCT).
Observational studies of alcohol vis-à-vis health:
There are two main groups of people that influence the outcomes of health vis-à-vis alcohol studies. There are people who are very health conscious and do whatever they can to be healthy, and those that do not care about their health and make food and lifestyle choices that are purely based on giving them pleasure. People who are health conscious tend to have better health than people who are not health conscious. They follow the health advice that has been generally given for many years; they smoke less, drink less alcohol, exercise more, take vitamins, eat less calories, eat less sugar, eat less refined processed foods, and eat more vegetables. Any one of these variables could be contributing to their good health, but from an observational study you can’t tell which one. Observational studies are full of confounding variables. You would need a controlled experiment to do that. Another problem with observational health studies is that the data collected is not very reliable. It is usually collected using alcohol frequency questionnaires. In these studies people are asked to recall what they drank in the last day, month, year, or even four years. Most people can’t remember what they drank last week; let alone what they drank three years ago. In an observational study, the investigators don’t attempt to control the behavior of the subjects: they simply collect data about what the subjects are doing on their own. Let’s watch the same group of people for decades, measure some things every once in a while, and see what happens to them. Then we can go back through the data and see if the people with a specific health issue had anything else in common. It’s easy to see that looking for statistical associations in data that already exists is far easier and cheaper than performing a randomized clinical trial. This huge pitfall of observational studies is often neglected: in large cohort studies, data is often self-reported, and self-reported data is often wildly inaccurate. “Correlation does not imply causation” means “Just because two things vary in a similar way over time doesn’t mean one is causing the other.” Since observational studies can only prove correlation, not causation, almost every article on health benefits of moderate alcohol use, which claims “X causes Y” is factually wrong. The only statements we can make from an observational study are “X associated with Y” or “X linked with Y”. Also, there are cases in which sampling bias and selection bias skew the results, and the cases in which the data is inaccurate; there is also the possibility that the truth is being stretched or broken…that the data is being misrepresented. Some scientists can have such a strong belief in what the outcome of their study will be that they become biased. Since there are so many confounding variables, you can make the outcome of a study say pretty much whatever you want it to say. Most studies will try and account for these variables, but it is almost impossible to know exactly how much of a part each one played in someone’s health. Some researchers will use a third variable to link two items when there is no direct link. A good example of this is saturated fat, cholesterol and heart disease. Many studies will claim to show that saturated fat causes heart disease even if the data in their data shows that people who ate more saturated fat had a lower incidence of heart disease. They do this by saying that saturated fat intake was associated with higher cholesterol, which is claimed to be a marker for heart disease. (Even though it has never been proven that high cholesterol causes heart disease) We need to start doing controlled experiments to find out which hypotheses about alcohol consumption result in healthy outcomes. However, RCTs are expensive—especially alcohol vis-à-vis health studies, which require alcohol consumption of large groups over extended periods. As a result, RCTs are infrequently done, especially in the alcohol vis-à-vis health field. Since alcohol vis-à-vis health RCTs are so rare; almost all alcohol vis-à-vis health headlines are based on observational studies. The overwhelming majority of alcohol vis-à-vis health headlines are from cohort studies, in which health data has been collected for years (or decades) from a fixed group of people, often with no specific goal in mind. Observational study only help making a hypothesis, it can neither prove nor disprove the hypothesis. 99% of health vis-à-vis alcohol studies are observational studies which actually don’t prove anything. When observational studies are portrayed as fact or truth, it becomes bad science.
_______
Does alcohol help or harm?
It does harm far greater than help.
Alcohol is widely used in our society. Most individuals who use alcohol drink in ways that do not increase risk for alcohol use problems. Some, however, drink in ways or at times during their life course that increase risk to themselves or others. Still others who use alcohol may derive a health benefit from its use. Defining precisely who is at risk for alcohol use problems and assessing the risks versus benefits of alcohol use are the first steps toward providing accurate public health information and designing effective interventions to reduce alcohol use problems.
_
The figure below shows factors affecting alcohol consumption and alcohol-related harms:
_
The impact of alcohol consumption on chronic and acute health outcomes in populations is largely determined by two separate but related dimensions of drinking:
•the total volume of alcohol consumed, and
•the pattern of drinking.
The context of drinking plays an important role in occurrence of alcohol-related harm, particularly associated with health effects of alcohol intoxication, and, on rare occasions, also the quality of alcohol consumed. Alcohol consumption can have an impact not only on the incidence of diseases, injuries and other health conditions, but also on the course of disorders and their outcomes in individuals.
_
As you go through this article, you would know that alcohol and mortality has J shaped relationship: mortality is lowest especially cardiovascular mortality among light drinkers as opposed to abstainers or heavy drinkers. Moderate drinking is associated with reduced cardiovascular mortality, increases insulin sensitivity, slower cognitive decline with age and improves bone mineral density. Of course, with heavy drinking, all these benefits vanish and alcohol related harm to health become manifested as seen in the figure below:
_
_
It is estimated that about one third of alcohol-related deaths are due to accidents (32%), and another 14% are from intentional injury.
_
Why low dose alcohol beneficial and high dose harmful?
Numerous mechanisms have been proposed to explain the benefit that light-to-moderate alcohol intake has on the heart, including an increase of high-density lipoprotein cholesterol, reduction in plasma viscosity and fibrinogen concentration, increase in fibrinolysis, decrease in platelet aggregation, improvement in endothelial function, reduction of inflammation, and promotion of antioxidant effects. However, high doses of alcohol lead to the induction of the P450 hepatic microsomal ethanol-oxidizing. Small amounts alcohol is not sufficient to induce P450. P450 is a class, or family, of liver enzymes whose main functions include catalyzing the metabolism of drugs and the oxidation of organic substances. This pathway generates free radicals that damage tissues and because the system consumes NADPH, the antioxidant glutathione cannot be regenerated, exacerbating the oxidative stress. These free radicals and reduced anti-oxidants cause alcohol-related diseases.
_
Alcohol is a bigger problem than other drugs:
Ethanol (simply called alcohol) is a psychoactive drug primarily found in alcoholic beverages. Alcohol is one of the most commonly abused drugs in the world (Meropol, 1996) often used for self-medication, and as recreational drug use. Results of the ISCD 2010 study ranked the levels of damage caused by drugs, in the opinion of drug-harm experts. When harm to self and others is summed, alcohol was the most harmful of all drugs considered, scoring 72% as seen in the figure below:
_
_
Alcohol is addictive:
Yes, alcohol can be addictive. The lifetime risk for alcohol dependence is about 10–15% for men and 5–8% for women. A JAMA psychiatry study of 2007 found that prevalence of lifetime alcohol dependence was 12.5% and only 24.1% of those with alcohol dependence were ever treated in America. International surveys conducted in the early 1980s showed prevalence of lifetime alcohol dependence of 8.8% to 23.0%. The NHS estimates that around 9% of men in the UK and 4% of UK women show signs of alcohol dependence. People with an addiction may have difficulty stopping by themselves, even if they want to, and even if other negative effects (such as financial or other personal problems) begin to outweigh the positive effects. Alcohol dependence can also cause major problems with friends, family, school, work, emotional and mental health, physical health, the law and money!
_
So in a nutshell, alcohol does cause harm far greater than potential benefits. Alcohol caused far more deaths than prevented. In other words, deaths due to heavy drinking, binge drinking, alcohol abuse and alcohol dependence far exceeds lives saved by light or moderate drinking. People who’ve heard that one drink a day might be good for the heart should also remember that just a bit more is known to increase the risk of 60 diseases and 14 cancers. Diseases related to heavy consumption of alcohol and alcoholism include stroke, alcoholic cardiomyopathy, several kinds of cancer, cirrhosis, and pancreatitis, as well as accidents, suicide, and homicide.
_______
What is the safe limit of alcohol consumption?
Little agreement exists between countries on what is considered safe or sensible alcohol consumption, a comparison of drinking guidelines by British researchers has found. Psychologists from the University of Sussex looked at government advice on drinking in 57 countries, including all 27 EU member states. Dr Richard de Visser and Nina Furtwangler found a “remarkable lack of agreement” about what constitutes harmful or excessive alcohol consumption on a daily and weekly basis, and when driving. There was also no consensus on whether it was safe for women to drink as much as men, their study, published in Drug and Alcohol Review, found. Dr de Visser said: “We were surprised at the wide variation in guidelines. There is no international agreement about whether women should drink as much as men or only half as much. “In some countries, the weekly maximum is simply seven times the daily maximum, whereas in others there is an explicit statement that drinkers should have at least one alcohol-free day a week.” Calls have now been made for internationally-agreed standard definitions of alcohol units and consumption guidelines to help people drink responsibly. The research found that some countries referred to standard drinks but failed to define them in grams of ethanol. In addition, eight of the 27 EU member states did not have readily accessible guidelines. Among the countries that allowed drivers to have alcohol in their blood, there was a ten-fold variation between the least generous, Panama, and the most generous, United Arab Emirates. Dr de Visser acknowledged that guidelines have limited success in encouraging moderation. But he added: “Despite these caveats, it is important for people who do want to adhere to recommendations to drink responsibly, that there should be internationally-agreed standard definitions of alcohol units and consumption guidelines. “Agreed guidelines would be useful for international efforts to reduce alcohol-related harm by increasing people’s capacity to monitor and regulate their alcohol consumption.”
_
The people in the Danish study who had a 50-percent decreased chance of heart disease were drinking one alcoholic beverage per week. The importance of moderation is backed up in every study on this topic. A 2007 U.S. study focusing on men found that those who drank one to two drinks a day had fewer heart attacks than those who drank less and those who drank more. In 2001, a University of Buffalo team looked at the drinking habits of women who already had heart disease and found that those who had one drink per day were less likely to have heart attacks than those who drank nothing. In that study, wine was found to be more heart-healthy than liquor. The University of Buffalo scientists point out in their results that alcohol consumption increases a woman’s chances of developing breast cancer. That’s the problem with the healthy alcohol concept: It’s just not. Whatever benefits might be achieved by drinking between one and 14 alcoholic beverage per week, they’re outweighed by the downsides of alcoholism, cancer, liver disease, obesity and, yes, heart disease. While alcohol might reduce clogging of the arteries under certain circumstances, it almost always raises blood pressure, causes weight gain and boosts triglyceride levels in the blood, all risk factors for heart disease. Triglycerides are fatty substances than can build up in the liver if the body doesn’t break them down properly, and even small amounts of alcohol inhibit the body’s processing of triglycerides. The American Heart Association does not recognize alcohol intake as a legitimate heart-healthy activity. It advises against it, not only because alcohol is inherently unhealthy, but also because the AHA doesn’t believe the studies have proved that moderate alcohol consumption — and not the drinkers’ lifestyles — leads to healthier hearts. Even those scientists who published the studies do not recommend that any nondrinker start drinking to avoid heart disease.
_
Alcohol in the form of alcoholic beverages has been consumed by humans since pre-historic times, for a variety of hygienic, dietary, medicinal, religious, and recreational reasons. While infrequent consumption of alcohol in small quantities may be harmless or even beneficial, larger doses result in a state known as drunkenness or intoxication and, depending on the dose and regularity of use, can cause acute respiratory failure or death and with chronic use can cause severe health problems, such as liver and brain damage. As stated earlier, alcohol in small doses is harmless and can even be beneficial, but how many people can consume alcohol “responsibly” and “sensibly”?
_
My view:
One drink a day increased breast cancer risk by about 10 percent and two drinks increased it by 25 percent. So, the adverse effects of alcohol on the breast occur at the same levels of drinking that protect the heart. Also, if you are going to drive/fly a vehicle/ aircraft, you should not drink any alcohol for 24 hours before driving/flying. This is because alcohol effects linger on brain for 24 hours even after blood alcohol level has become zero. Also, about 20 % people who drink alcohol have alcohol use disorder. So there is no safe limit of alcohol consumption. All we have is low risk drinking. I define low risk drinking as less than 40 gm of alcohol per any day and less than 140 gm of alcohol per week for healthy men; and less than 30 gm of alcohol per any day and less than 70 gm of alcohol per week for healthy non-pregnant women. It’s important that both the daily and the weekly limits be considered. Anything above is high risk drinking with adverse health, social and legal consequences; and high probability of getting alcohol dependence. Remember, even low risk drinking leads to cancer, accidents, violence, injuries, drowning and dependence. There is no zero risk drinking.
_
1. If you don’t drink, there’s no need to start. Yes, there is biological proclivity for small amount alcohol consumption but that does not mean that everybody should drink alcohol as you never know when you cross limit and also there is potential for alcohol addiction. All of us have biological proclivity for sugar as it is essential for survival but when we over-consume sugar, we develop obesity and diabetes. For some people—especially pregnant women, people recovering from alcohol addiction, people with a family history of alcoholism, people with liver disease, and people taking one or more medications that interact with alcohol—the risks of drinking far outweigh the benefits. There are other ways to boost your heart health such as getting more exercise, staying at a healthy weight and eating healthy food.
2. If you do drink, drink in moderation—and choose whatever drink you like. Wine, beer, or spirits—each seems to have the same health benefits as long as it is low risk drinking.
3. Take a multivitamin with B complex and vitamin C daily if you drink to reduce alcohol toxicity.
_______
Is it moderate drinking or moderate life-style of moderate drinker that reduces cardiovascular mortality?
There is overwhelming evidence to show that death due to coronary heart disease is less in light to moderate drinker than heavy drinker or abstainer. Consumption of one or two drinks per day is associated with a reduction in the risk of coronary heart disease by approximately 30% to 50%. However, several caveats are to be considered before you recommend anybody to drink alcohol in moderate amount daily for health benefits:
a) The large numbers of observational epidemiological studies support a true protective effect of moderate consumption of alcohol. However, there are no double-blind randomized controlled studies on relationship between alcohol and heart. Observational study only help making a hypothesis, it can neither prove nor disprove the hypothesis.
b) The risk reduction of 30 to 50 % shown in various observational studies is relative risk reduction and not absolute risk reduction. The fact is that relative risk tells you nothing about actual risk. Outcomes that are presented in terms of relative risk reduction exaggerate the apparent benefits of alcohol. Relative risk is never a valid measure of safety when comparing drinker against non-drinker. One researcher calculated that 3 heart attacks can be prevented per 1000 person-years. So the absolute risk reduction is miniscule.
c) Physical dependence can develop from low-dose alcohol, opioids and benzodiazepines. The higher the dose used, the greater the duration of use, and the earlier age use began are predictive of worsened physical dependence and thus more severe withdrawal syndromes. Even for low level alcohol consumption, there is a risk for alcohol abuse and alcohol dependence; and nobody can predict with certainty who will become abuser and addict. Out of 100 heavy drinkers about 20 would become alcoholic and out of 100 low risk drinkers (light/moderate drinker), about 3 would become alcoholic; and only one fourth of all alcoholics would ever be treated. All the studies of alcohol benefit were conducted on light/moderate drinkers but 3 of 100 among them would become alcoholics with only one fourth treated for dependence and remaining would have reduction in life span by 10 years.
d) Light drinkers are the healthiest, wealthiest and fittest group as compared to non-drinkers or heavy drinkers who usually belong to working class, lower socio-economic group, having limited education and poorer health. Even though alcohol per se reduces coronary heart disease, one cannot overlook the fact that most light drinkers are healthier anyway as compared to non-drinkers or heavy drinkers or ex-drinkers.
e) There is no lower safe limit for cancer. Even consuming less than two standard drinks a day is estimated to cause around thousands of deaths due to cancer triggered by alcohol.
f) People are notorious for underestimating what they drink.
g) Low dose aspirin, healthy diet, maintaining ideal weight and regular exercise can decrease coronary risk similar to alcohol.
h) Abstainers are not a single group but have many sub-groups. Abstainers who never drank alcohol in their life had mortality risks similar to light drinkers. Abstainers who were former drinkers have higher mortality than light drinkers. Also, it doesn’t necessarily follow that those people’s mortality rates would fall if they began drinking. In fact people who were problem drinkers in the past might increase their mortality risk further by starting to drink again. Also, abstainers from lower socioeconomic group of society have higher mortality risk than light drinkers from higher socioeconomic group, where lower socioeconomic status could be one of the underlying causes for the mortality differences. In that case, starting to drink without changing a person’s socioeconomic status will not lower mortality rates.
i) People who are dependent on alcohol are three times more likely than those in the general population to be smokers; therefore likely to develop all hazards of smoking added to alcohol. In fact one study found that about 10% of the U.S. population is heavy smokers, but among alcoholics, 70% to 90% are heavy smokers.
j) Moderate alcohol intake is also associated with increased risk of violence, drowning, and injuries from falls and motor vehicle crashes. One cannot overlook it for cardiovascular benefit.
k) ADH enzyme has many variants. One quickly breaks down alcohol, the other does it more slowly. Moderate drinkers who have two copies of the gene for the slow-acting enzyme are at much lower risk for cardiovascular disease than moderate drinkers who have two genes for the fast-acting enzyme. It’s because the fast-acting enzyme breaks down alcohol before it can have a beneficial effect on HDL and clotting factors. So all moderate drinkers do not benefit from alcohol’s beneficial effects on heart. In fact, fast processors would have higher acetaldehyde with all its toxic effects including cirrhosis of liver.
l) Most of the physiologic benefit of moderate drinking is confined to ischemic cardiovascular conditions, such as CHD; in areas of the world where there is little mortality from cardiovascular diseases, and people under age 45 who have little ischemic cardiovascular mortality, alcohol provides little or no reduction in overall mortality. Rather, the relationship between intake and all-cause mortality assumes more of a direct, linear shape, with increasing consumption associated with higher overall mortality.
m) While alcohol might reduce clogging of the arteries under certain circumstances, it almost always raises blood pressure, causes weight gain and boosts triglyceride levels in the blood, all risk factors for heart disease.
_
In a nutshell, even though light to moderate drinking does reduce cardiovascular mortality, the evidence is not indisputable, objective and conclusive. There are many unattended confounding variables in alcohol mortality relationship and there are many flaws in alcohol mortality studies.
___________
Frequently asked questions: (FAQ):
_
How does alcohol affect a person?
Alcohol affects every organ in the body. It is a central nervous system depressant that is rapidly absorbed from the stomach and small intestine into the bloodstream. Alcohol is metabolized in the liver by enzymes; however, the liver can only metabolize a small amount of alcohol at a time, leaving the excess alcohol to circulate throughout the body. The intensity of the effect of alcohol on the body is directly related to the amount consumed.
_
Why do some people react differently to alcohol than others?
Individual reactions to alcohol vary, and are influenced by many factors; such as:
Age
Gender
Genetics
Physical health
Amount of food consumed before drinking
How quickly the alcohol was consumed.
Use of drugs or prescription medicines
Family history of alcohol problems
_
Is beer or wine safer to drink than liquor?
No. One 12-ounce beer has about the same amount of alcohol as one 5-ounce glass of wine, or 1.5-ounce shot of liquor. It is the amount of alcohol consumed that affects a person most, not the type of alcoholic drink.
_
What does moderate drinking mean?
According to the Dietary Guidelines for Americans, moderate alcohol consumption is defined as having up to 1 drink per day for women and up to 2 drinks per day for men. This definition is referring to the amount consumed on any single day and is not intended as an average over several days. However what is one drink varies from country to country. One drink in America is 14 gm ethanol, one drink in U.K. is 8 gm ethanol and one drink in Japan is 20 gm of ethanol.
_
What is excessive alcohol use?
Excessive alcohol use includes binge drinking, heavy drinking, high risk drinking, problem drinking, alcohol use disorder, any alcohol use by people under legal drinking age, and any alcohol use by pregnant/lactating women.
_____________
Alcohol myths:
There are so many stories around alcohol and drinking that it’s hard to know what to believe. Being informed about the facts is the best way to make sure that you drink safely.
_
Myth: Beer gets you less drunk.
Fact: An average pint of beer (ABV 5%), large glass of wine (250ml, ABV 11%) or a ‘large’ double vodka (70ml, ABV 38 to 40%) all have around 2.8 U.K. units of alcohol. This is what makes you drunk chemically, and the faster you drink the full 2.8 units, the higher your peak blood level. But there are a wide range of factors that can affect how drunk you feel including your expectations.
_
Myth: Your body develops a tolerance to alcohol, so you can safely drink more.
Fact: The more you drink the more damage your body will sustain and the greater the risks become. Tolerance can actually be seen as a warning sign that your body has started to be affected by alcohol dependence.
_
Myth: I’ve had one drink in an hour, so I’m safe to drive.
Fact: While it’s true that it takes one hour for men’s bodies to metabolize one U.K. drink, women wait at least an hour and a half, due to their unique physiology. Even then, you can’t trust your judgment once you’re buzzed; you’ll probably feel buzzed sooner than you think. People have trouble judging how seriously alcohol has affected them. That means many individuals who drive after drinking one drink think they can control a car – but they’re wrong. This can have deadly consequences.
_
Myth: Drinking alcohol is better than doing illegal drugs such as heroin and crystal meth.
Fact: Problematic use of any substance can lead to serious harms or trauma to individuals, families, and communities. It may seem like illegal drug problems are more serious because the media closely follows these stories and issues and because we tend to downplay the harms linked to alcohol, a legal product that is tightly woven into our culture. However, studies confirm that problematic alcohol use results in more harms – there are more than 50 ways that alcohol use leads to death – and is much more costly to society than all forms of illegal substance use combined. Alcohol is known to increase the risk of 60 diseases and 14 cancers.
_
Myth: You can drink and still be in control.
Fact: Alcohol impairs your judgment, which increases the likelihood that you will do something you’ll regret, such as having unprotected sex, being involved in crime, damaging property, accidents or being victimized by others.
_
Myth: If someone passes out after drinking, it’s best to let them sleep it off.
Fact: If a friend or a guest passes out, never leave them alone. Have someone call for medical assistance. Be sure to roll them onto their side, with their head on its side as well, until help comes.
_
Myth: Alcohol warms the body.
Fact: Alcohol is a vasodilator, meaning that it causes your blood vessels to dilate, particularly the capillaries under the surface of your skin. Thus, the volume of blood brought to the skin’s surface increases, making you feel warm. This overrides one of your body’s defenses against cold temperatures, constricting your blood vessels, thereby minimizing blood flow to your skin in order to keep your core body temperature up. While you may feel warmer from the extra blood warming your skin (where most of your “heat sensors” are located), this blood being brought close to the surface of your skin will be rapidly cool if you are in a cold environment (sometimes exacerbated by sweating as a result of this heat flush). The net effect being a rapid drop in core body temperature, often without you even realizing it as your skin will feel fairly warm, which makes it doubly dangerous to drink alcohol in extremely cold weather. You can observe this dilation effect when you see people who are slightly or fully intoxicated looking flushed. This effect is more extreme in some people than others. So if you’re one of those people who gets flushed quickly when drinking even small amounts of alcohol, you’ll likely see your core temperature drop even faster than most when drinking in frigid environments. This isn’t the only bad thing about drinking alcohol when cold. According to a study done by the Army Research Institute of Environmental Medicine, drinking alcohol in cold weather also reduces the body’s ability and tendency to shiver, taking away yet another method your body uses to help keep warm when it is cold. Alcohol metabolism does generate heat by ethanol-induced thermogenesis and activation of the Microsomal Ethanol-Oxidizing System (MEOS) system but heat generated is insufficient as compared to heat loss through vasodilatation & impaired shivering. Alcohol actually lowers your body temperature. Too much alcohol in very cold weather may even increase the risk of hypothermia. So, bottom line, the age old practice of drinking alcoholic beverages to keep the body warm in cold weather is the exact opposite of what you should do.
_
Myth: Alcoholics drink every day.
Fact: The issue is not how frequent or how much you drink but whether you have strong craving for alcohol, whether you have inability to limit drinking, whether you have withdrawal symptoms, whether you continue to drink despite objective evidence of harm and whether there is denial of excess drinking.
_
Myth: A cold shower, fresh air or hot coffee will sober someone up.
Fact: Black coffee and cold showers only produce wide-awake drunks. Only time will rid the body of alcohol. There is no known way of speeding the metabolic process of eliminating alcohol from the body. Your body can eliminate 100 mg of alcohol per kg body weight per hour.
_
Myth: I can save up my drinks for the weekend.
Fact: Saving up your units from the week and drinking them all at once could leave you with a nasty hangover in the morning and some embarrassing memories of the night before, as well as increasing your risk of injuries, fights and accidents. It amounts to binge drinking which is now part of alcohol use disorder. Drinking more than 40 gm of alcohol by men and 30 gm by women on any day is high risk drinking although total weekly consumption is within recommended limit.
_
Myth: Alcohol helps me sleep.
Fact: Alcohol may make you feel sleepy and reduce the time it takes to fall asleep, but the quality of sleep is often poor. Studies show that alcohol consumed as much as six hours before bedtime will increase wakefulness during the second half of your sleep, and keep you from getting the deep sleep you need. Alcohol impairs deep sleep and reduces REM sleep.
_
Myth: Exercise in gymnasium will undo alcohol harms.
Fact: Exercise may make you feel a little better after drinking, but it won’t undo the effects of alcohol on your body. In fact, sweating during exercise may make you more dehydrated, and so worsen your hangover. You are also likely to have low blood sugar levels after any evening’s drinking, meaning exercise will be a lot harder work.
_
Myth: Drinking beer gives you a beer belly.
Fact: It certainly can — but so can anything you consume in excess. That stereotypical beer-drinker’s gut is a sign you’re overdoing it on something, but not necessarily beer. Most beer bellies are just due to excessive calories from any source, beer among them. In India, people who drink beer habitually overeat; they start eating before beer, during beer and after beer and the food they eat is high calorie high carb high fat food. Even if they have not taken beer, they would develop pot belly.
_
Myth: Alcohol has nothing to do with Nutrition.
Fact: Actually, alcohol can block the absorption of certain nutrients, including the B vitamin folate. It’s thought that this may be one way alcohol increases the risk of certain cancers, including breast cancer. Women drinkers with the highest levels of folate were 90 percent less likely to develop breast cancer than those with the lowest levels. Alcohol also consumes thiamine and vitamin C during metabolism in liver. Not to mention, many alcoholics only drink alcohol and eat very little food.
_
Myth: Older Adults can drink like they did in college.
Fact: While there are some benefits to moderate alcohol consumption among older adults (namely for the heart and brain benefits mentioned above), aging tends to lower your body’s tolerance for alcohol. An older adult will typically feel the effects of alcohol more quickly than when they were younger, increasing the risk for falls, car crashes and other accidents. Additionally, certain medications can have bad interactions with alcohol, sometimes leading to deadly consequences. Examples of medications that may be dangerous when mixed with alcohol are aspirin, sleeping pills, pain medications, anti-anxiety drugs and antidepressants.
_
Myth: Alcohol is a stimulant.
Fact: Alcohol is a central nervous system depressant. Although the initial effects of alcohol may be euphoric and seem stimulating, the cumulative effect of alcohol actually depresses the brain. The ability to make good judgments and decisions are depressed first, followed by loss of coordination and motor functioning (slurring and staggering). If taken in high enough dose, alcohol can depress the central nervous system so much that breathing and heartbeat will cease.
_
Myth: I can stop drinking anytime I want to.
Fact: Maybe you can; more likely, you can’t. Either way, it’s just an excuse to keep drinking. The truth is, you don’t want to stop. Telling yourself you can quit makes you feel in control, despite all evidence to the contrary and no matter the damage it is doing.
_
Myth: I’m not an alcoholic because I have a job and I’m doing okay.
Fact: You don’t have to be homeless and drinking out of a brown paper bag to be an alcoholic. Many alcoholics are able to hold down jobs, get through school, and provide for their families. Some are even able to excel. But just because you’re a high-functioning alcoholic doesn’t mean you’re not putting yourself or others in danger. Over time, the effects will catch up with you.
______________
______________
The moral of the story: (Alcohol means ethanol unless specified otherwise)
_
1. Photosynthesis synthesized sugar from sun energy, carbon dioxide (CO2) and water releasing oxygen (O2) by plants. Many bacteria produce glucose by photosynthesis, just like plants. Sun energy is extracted from sugar utilizing O2 by animals including humans releasing CO2 & water. Alcohol is synthesized by yeast and other microorganisms extracting sun energy from sugar without using O2 releasing CO2. Animals and humans extract remaining sun energy from alcohol utilizing O2 and releasing CO2 & water. The released CO2 and water is recycled in photosynthesis. The most commonly accepted evolutionary scenario states that organisms first arose in an atmosphere lacking oxygen and therefore anaerobic fermentation by microorganisms is supposed to have evolved first and considered the most ancient pathway for obtaining energy. In other word, generation of alcohol by microorganisms is an important step of evolution of life on earth.
_
2. All living organisms actually produce alcohol in small amounts by several pathways including humans. Fermentation of fruit sugar by yeast during ripening generates alcohol. All ripe & over-ripe fruits that we eat daily have trace alcohol and microorganisms in our intestines generate 3 grams of alcohol daily. So scientifically there is no teetotaler in the world including deeply religious people who condemn alcohol use. However, endogenous generation of 3 gm alcohol in 24 hour is far less than body’s elimination rate of 7 to 8 gm per hour by liver and therefore it is undetectable in blood.
_
3. Alcohol preference appears to be an evolutionary inherited trait that came under positive selection in periods of mostly scarce resources for humans. Humans have evolved the necessary enzymatic functions that provide metabolic tolerance to low amounts of ethanol, thereby preventing intoxication. So there is a biological proclivity for low alcohol consumption by humans. There is no genetic biological mechanism to protect against high alcohol consumption as high concentrations of alcohol (distilled beverage) only became available in the last 2800 years, a period too short to induce adequate evolutionary counter responses.
_
4. Since humans have biological proclivity for small amount of alcohol consumption, alcohol cannot be classified as poison. Yes, it does become poison when you drink in excess amount.
_
5. Laboratory experiments have shown that in fruit flies and in rats; longevity is increased at very low concentrations of ethanol, but decreases rapidly with exposure to higher concentration. Interesting to note that longevity is also increased at low alcohol consumption in humans and it falls rapidly with higher consumption.
_
6. From fruit flies to elephants, if you give them a source of alcohol and sugar, they love it. Intentionally fermented beverages containing alcohol existed at least as early as the Neolithic period around 10,000 B.C. Throughout history, wine and other alcoholic beverages have been a source of pleasure and aesthetic appreciation in many cultures and enormous differences can be observed as to how different ethnic and cultural groups handle alcohol.
_
7. Both genes and culture contribute to alcohol use in humans.
_
8. Approximately 60% of the risk for alcohol use disorders is attributed to genes, as indicated by the fourfold higher risk for alcohol abuse and dependence in children of alcoholics (even if these children were adopted early in life and raised by non-alcoholics foster parents) and a higher risk in identical twins as compared to fraternal twins of alcoholics.
_
9. Alcoholism is more common in those people who are less sensitive to the motor, perceptual, and biochemical changes induced by alcohol due to genetic makeup. All follow-up studies have demonstrated that the need for higher doses of alcohol to achieve desired effects predicts future heavy drinking, alcohol problems, and alcohol use disorders.
_
10. Susceptibility to complications of alcoholism (e.g. liver cirrhosis, pancreatitis, cardiomyopathy, or psychosis due to brain damage) is influenced by genetic factors independent of those genetic factors influencing susceptibility to alcoholism itself; explaining the inconsistency with which medical complications occur in alcoholism.
_
11. Women usually achieve a higher blood alcohol content (BAC) than men after drinking the same amount of alcohol, and for the same level of BAC women are more susceptible to alcohol’s damaging effects than men. That is why all recommendations regarding safe alcohol consumption worldwide advise lower limit of alcohol intake for women. Even though women are more susceptible to alcohol related diseases, the percentage of alcohol-attributable deaths among men amount to 7.6 % of all global deaths compared to 4.0 % of all deaths among women. That is because lower total alcohol consumption per capita per year among female (8.9 liters) drinkers as compared to male (21.2 liters) drinkers worldwide.
_
12. Drinking is essentially a social act. Culture does determine drinking patterns and practices among people and nations. How we learn to drink and continue to drink is determined most by the drinking we observe, the attitudes about drinking we pick up, and the people we drink with. There is convincing historical and contemporary evidence to show that the adoption of ‘foreign’ drinks often involves the adoption of the drinking patterns, attitudes and behaviours of the foreign culture.
_
13. Beverage alcohol is commercially produced by fermentation of sugar (directly from fruits and/or by hydrolysis of starch of cereals/vegetables/fruits) by yeast (type of fungus) without using oxygen and alcohol content is further increased by distillation. Other means of increasing alcohol content are freeze-distillation by which water is frozen out and fortification where distilled beverage is added to fermented beverage. Industrial alcohol is produced by chemical methods without use of microorganisms.
_
14. Essence of alcohol metabolism in human body is no digestion, rapid absorption, no storage and prioritized oxidation to water& carbon dioxide in liver generating 7 Kcal energy from 1 gm alcohol. More than 50 % alcoholics derive 30 % energy (dietary calories) from burning alcohol in liver. You may think that since humans have innate ability to metabolize 7 to 8 gm alcohol per hour and since 1 gm alcohol gives 7 Kcal, consuming 7 to 8 gm alcohol hourly would generate 50 Kcal/hour and 1200 Kcal per day sufficient to cater to more than 50 % energy need of the body, then why not alcohol be classified as a nutrient just like sugar? However, alcohol generate excessive NADH in liver causing metabolic acidosis (lactic acid plus ketone bodies), hypoglycemia, hypertriglyceridemia, fatty liver, acetaldehyde toxicity depleting vitamins & anti-oxidants in liver followed by liver cell necrosis.
_
15. The pharmacologic and toxic effects of alcohol are different. The pharmacological effect (i.e., intoxication or drunkenness) is caused by high blood ethanol level and the toxic effect (e.g., flush, hangover, susceptibility to cancer and cirrhosis of liver) is caused by high acetaldehyde level. To reduce toxic effect (acetaldehyde) effects of alcohol, take vitamin C & B complex and N-Acetylcysteine (NAC) before and during alcohol intake. All these are freely available in any medical store.
_
16. The effects of alcohol on brain; be it pleasure, disinhibition, intoxication, poisoning, tolerance, withdrawal or dependence; depend upon inter-play of various neurochemicals like GABA, glutamate (NMDA), dopamine, norepinephrine, nicotinic acetylcholine and serotonin & various ion channels; acting through various receptors at various brain areas. Both genetic and cultural factors affect alcohol consumption and consequently action on these receptors on neurons. Variations in the genes of these target receptors may result in different alcohol-susceptible phenotypes. Alcohol intoxication means greater GABA and diminished NMDA receptor activity. Chronic regular alcohol intake leads to neuroadaptation in brain whereby GABA receptors are down-regulated and NMDA receptors are up-regulated resulting in tolerance to alcohol. It will now take more alcohol to produce the same effect as the first drink. Further neuroadaptation and involvement of reward system (dopamine plus endogenous opioids) lead to alcohol dependence (addiction). If the person now chooses to quit drinking, the body tries to return to its original state, in doing so causes a number of withdrawal symptoms & signs, due to diminished GABA with enhanced NMDA actions and decreased dopaminergic activity in the reward area.
_
17. One unit of alcohol = one standard drink = one drink = one shot
For all practical purposes, moderate drinking means up to 1 drink daily for women and 1to 2 drinks daily for men. Light drinking is greater than zero but below the moderate amounts. Anything above moderate drinking is heavy drinking. Binge drinking means five or more drinks [men], or four or more drinks [women], in about 2 hours; on any day in previous six months. However, different countries have different amount of alcohol in one drink from 6 gm in Austria to 14 gm in U.S. to 20 gm in Japan. This is unscientific, irrational and counter-productive as far as studies on harm vs. benefit by alcohol are considered. I therefore propose international alcohol unit equivalent to 10 grams of absolute alcohol.
One international unit (IU) = one international drink = 10 grams of absolute alcohol in any beverage.
I urge all nations to adjust their alcohol measurement in various beverages to international units (IU).
For example, a 750 ml beer bottle containing alcohol 5 % v/v contains 30 grams of absolute alcohol i.e. 3 IU—so that beer bottle label should mention that it contains 3 international unit of alcohol.
31 ml of 40 % v/v whisky/rum/gin/vodka contains 1 international unit of alcohol.
_
18. People are notorious for underestimating what they drink and therefore going by people’s version of how much they drink would be underestimating how much they actually drink.
_
19. In homes or restaurants, to drink less, use tall narrow glasses or ones on which the alcohol level is pre-marked.
_
20. There is growing evidence that drinking large numbers of alcohol units over a relatively short period is likely to be far worse for your general health than spreading the same alcohol over a whole week, even though overall consumption is same.
_
21. Any amount/duration of alcohol consumption with any harm to any individual including self-harm is alcohol use disorder. The harm could be physical health, social, psychological, legal, educational, cognitive, work related and economic.
_
22. Chronic alcoholism (dependence/addiction) decreases life span by about 10 years.
_
23. Each year worldwide alcohol kills about 3.3 million people, more than AIDS, tuberculosis and violence combined.
_
24. Alcohol is more harmful than tobacco, marijuana (cannabis), cocaine, heroin, LSD, ecstasy, speed and other psychoactive drugs.
_
25. There is no rationale to consume alcohol for good sleep. In fact alcohol reduces number of sleep cycles, interferes with deep sleep and reduces REM sleep. Additionally alcohol being a diuretic will wake you up at night frequently to pass urine and relaxes muscles of body including throat muscles causing snoring & sleep apnea.
_
26. Modest alcohol consumption especially a glass of wine with healthy food does not lead to weight gain. However, I have seen many patients who over-eat high calorie food with modest alcohol consumption and therefore do become overweight with abdominal obesity.
_
27. Do not drink alcohol in cold weather to keep body warm. Alcohol induces feeling of warmth in skin but actually promotes heal toss resulting in lower core body temperature and may precipitate hypothermia. There are other ways to keep body warm in cold weather.
_
28. Even though moderate alcohol consumption in a non-diabetic individual does reduce risk of diabetes, moderate alcohol consumption in a diabetic patient worsens diabetes control.
_
29. Heavy drinking and binge drinking is associated with hypertension.
_
30. About 10% of all cancer cases in men and 3% of all cancer cases in women are attributable to current and former alcohol consumption. One drink a day increases breast cancer risk by about 10 percent and two drinks increase it by 25 percent. So, adverse effects of alcohol on the breast occur at the same level of drinking that protect the heart.
_
31. Light drinking protect against cognitive decline (dementia) while heavy drinking accelerate cognitive decline.
_
32. Moderate alcohol consumption does reduce risk of kidney stones by increasing urine output due to suppression of vasopressin (ADH). However, if water intake is not increased to replace water loss, you may get dehydrated. Dehydration leads to more concentrated urine, allowing substances to collect into kidney stones. In other words, you may simply drink excess water to reduce kidney stone risk rather than consume alcohol.
_
33. Pregnant women, breastfeeding women and women who are planning pregnancy must abstain from alcohol completely.
_
34. A study found that youth who start drinking before age 15 years are five times more likely to develop alcohol dependence or abuse later in life than those who begin drinking at or after age 21 years. Another study found that the odds of dependence decreased by 14% and the odds of abuse decreased by 8% with each increasing year of age of onset of use. Another study found that it is early drunkenness rather than an early age of first drink as a key risk factor for alcohol abuse and dependence in adulthood. Alcohol impacts adolescent brain differently than adult brain. The adolescent’s decreased response to the negative aspects of alcohol consumption (motor impairment, sedation, anxiety, and social depression) coupled with increased or altered response to the positive and rewarding effects of alcohol may promote excessive intake. The lower the age of first use of alcohol, higher is the probability of alcohol abuse and dependence. Alcohol is a major cause of antisocial behavior among adolescent. Adolescent drunkenness is associated with accidents, violence, injuries, suicides, alcohol poisoning, sexual promiscuity, risky sexual behaviors and poor school performance. Therefore legal drinking age of 21 years is reasonable. Legal drinking age need not correlate with marriage age and voting age.
_
35. Breathalyzer test by police to detect driving under influence of alcohol has many fallacies inherent in technique. Also, you cannot administer a preliminary breath test for 15 minutes after the subject eats, vomits, or put anything in their mouth. Also, most instruments require that the individual be tested twice at least two minutes apart. Therefore to use breathalyzer as a surrogate marker for blood alcohol content is unscientific and results of breathalyzer cannot be used to convict anybody of driving under influence of alcohol. Breathalyzer should be used only as a screening procedure and if positive, collect blood from subject for blood alcohol level.
_
36. If you are going to drive/fly a vehicle/ aircraft, you should not drink any alcohol for 24 hours before driving/flying. This is because alcohol effects linger on brain for 24 hours even after blood alcohol level has become zero. In other words, if you are driving or flying daily, you should become teetotaler.
_
37. There is no safe limit of alcohol consumption. All we have is low risk drinking. I define low risk drinking as less than 40 gm of alcohol per any day and less than 140 gm of alcohol per week for healthy men; and less than 30 gm of alcohol per any day and less than 70 gm of alcohol per week for healthy non-pregnant women. It’s important that both the daily and the weekly limits be considered. Anything above is high risk drinking with adverse health, social and legal consequences; and high probability of getting alcohol dependence. Remember, even low risk drinking leads to cancer, accidents, violence, injuries, drowning and dependence. There is no zero risk drinking.
_
38. Out of 100 heavy drinkers about 20 would become alcoholic and out of 100 light to moderate drinkers, about 3 would become alcoholic. Taking regular breaks from alcohol can help to break any habitual patterns of drinking you have unintentionally fallen into. Remember 60 % of dependence is genetic and 40 % environmental (age of onset of drinking, family, peers, media, neighborhood, culture, higher dose etc) and nobody can predict with certainty who will become an addict. Induction of the P450 hepatic microsomal ethanol-oxidizing system by high doses of alcohol results in more efficient clearing of alcohol and therefore person drinks more to get the same effects of the alcohol. High doses also lead to neuroadaptive changes and stimulation of reward system in the brain. That is why high doses of alcohol is far more likely than low dose to cause addiction, not to mention greater alcohol related diseases; when all other factors are the same.
_
39. Approximately one child in every four (28.6%) in the United States is exposed to alcohol abuse or dependence in the family. I do not have statistics from developing nations like India but it could not be better. 25 % children of alcoholic parents (one or both parent) become alcoholic as they grow up.
_
40. People who are dependent on alcohol are three times more likely than those in the general population to be smokers, and people who are dependent on tobacco are four times more likely than the general population to be dependent on alcohol. Twin studies proved that while initial exposure to alcohol and nicotine is environmentally influenced, persistence in using these substances is under strong shared genetic influence.
_
41. Almost 50 percent of unplanned sexual encounters involve alcohol, and 60 percent of sexually transmitted diseases including HIV are transmitted when alcohol is involved.
_
42. Out of all violent crimes each year, one in four report that offender has been drinking alcohol prior to committing the crime.
_
43. Drinking problems negatively affect family functioning, and family problems can cause you to drink excessively. Thus, drinking and family functioning are strongly and reciprocally linked.
_
44. The global alcoholic drinks industry is $1 trillion in 2014.
_
45. American statistics show that binge drinking cost federal, state, and local governments about 62 cents per drink in 2006, while federal and state income from taxes on alcohol totaled only about 12 cents per drink. In other words, income generated from alcohol sales to state via taxes is far less than expenditure the state incurs in management of alcohol related losses in productivity, health care, crime, and accidents. A 2003 EU study found that economic cost of alcohol to the state far exceeds economic benefit of tax revenue to state and jobs created by alcohol manufacturers and supply chain.
_
46. In addition to family, peers, media, culture and genetics; alcohol advertising and marketing have a significant impact on youth decisions to drink.
_
47. I do not recommend total prohibition of alcohol. Lower the age of first alcohol use & higher the dose of alcohol; greater the probability of alcohol abuse & dependence. Raising the legal drinking age to 21 years and making alcohol expensive would mitigate these two factors. Alcohol education, tobacco education and sex education should be integrated in school curriculum to reduce sexual promiscuity, sexual transmitted diseases including HIV, violence, accidents, addictions and diseases due to alcohol & tobacco abuse.
_
48. When responsible drinking becomes part of culture, alcohol related problems are less, and when responsible drinking is enforced using laws, alcohol related problems are more.
_
49. Even though light to moderate drinking does reduce cardiovascular mortality, the evidence is not indisputable, objective and conclusive. There are many unattended confounding variables in alcohol mortality relationship. Most studies on alcohol are flawed as they are observational epidemiological studies and not double-blind randomized controlled studies (RCT). The cardiovascular risk reduction of 30 to 50 % due to light/moderate drinking in various observational studies is relative risk reduction and not absolute risk reduction. Outcomes that are presented in terms of relative risk reduction exaggerate the apparent benefits of alcohol. Relative risk tells you nothing about actual risk. Read my article ‘Imitation Science’.
_
50. If you don’t drink, there is no need to start for cardiovascular benefits. Maximum 3 heart attacks are prevented in 1000 person years but for individuals under 50 years of age, 20 gm of alcohol per day increases all-cause mortality by 15-20%. Even assuming alcohol in small doses is harmless and can even be beneficial, how many people can consume alcohol “responsibly” and “sensibly”? Lifetime risk for alcohol dependence is about 10–15% for men and 5–8% for women. The World Health Organization estimates that there are 140 million people with alcoholism worldwide. Only one fourth of alcoholics would be treated and remaining three fourth would die 10 year prematurely due to alcoholism related diseases. Alcohol causes far more deaths than preventing it. In other words, deaths due to heavy drinking, binge drinking, alcohol abuse and alcohol dependence far exceeds lives saved by light to moderate drinking. In fact, moderate alcohol intake is also associated with increased risk of cancer, violence, drowning, injuries from falls and motor vehicle crashes and dependence. Low dose aspirin, regular exercise, healthy diet and maintaining ideal weight would also reduce cardiovascular mortality without problems related to alcohol use.
________________
Dr. Rajiv Desai. MD.
June 24, 2014
________________
Postscript:
Instead of drinking alcoholic beverages, humans can use alcohol as biofuel. Alcohol (ethanol) is a renewable domestically produced ‘fuel’ made from plant material, such as corn, sugar cane, grasses or even ocean kelp, which can reduce oil dependence and greenhouse gas emissions .We can easily use alcohol fuel to power domestic cars, diesel engines, trains, aircraft, small utility engines, generators to make electricity, heaters for our homes—and it can even be used to cook our food. Additionally locally produced ethanol supercharges regional economies. Instead of fuel expenditures draining capital away to gulf countries, each gallon of alcohol produces local income that gets recirculated many times. Every dollar of tax credit for alcohol generates up to six dollars in new tax revenues from the increased local business. Brazil and U.S. are using alcohol to cater their energy need. Why not rest of the world? Anyplace where there is sunlight, water and land can produce biofuel alcohol from plants.


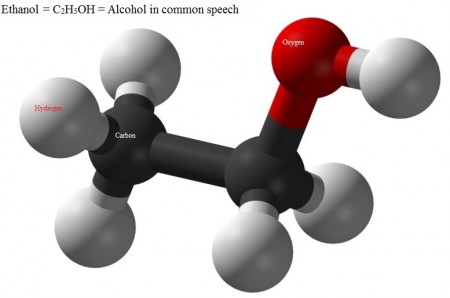
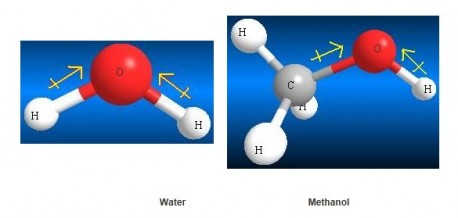
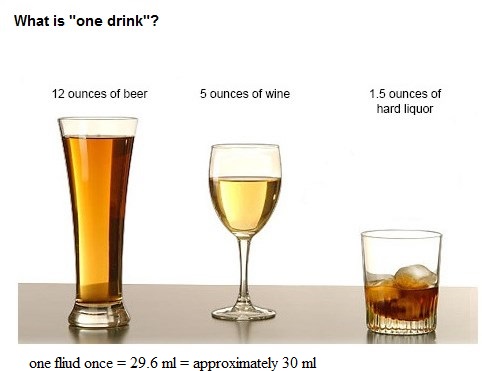
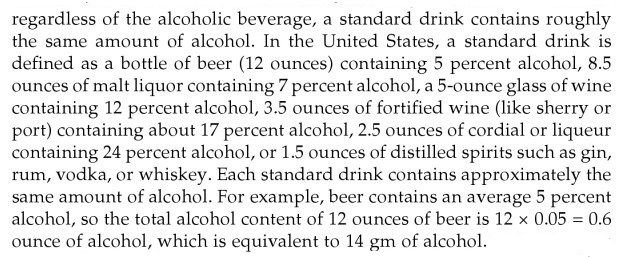
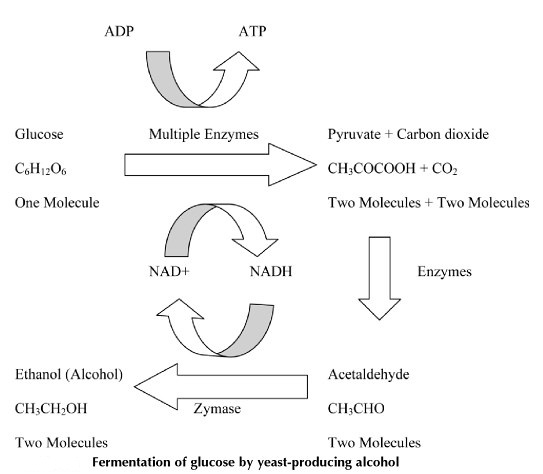
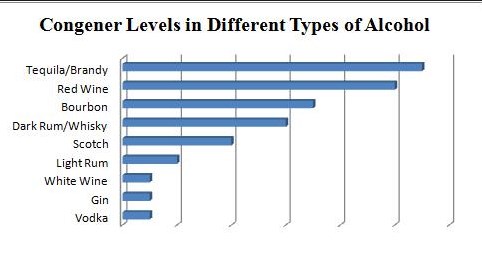
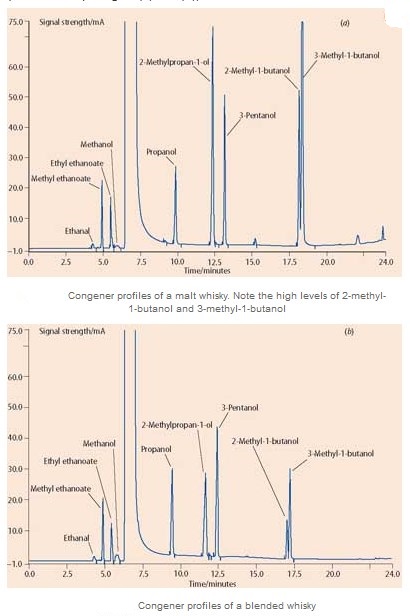
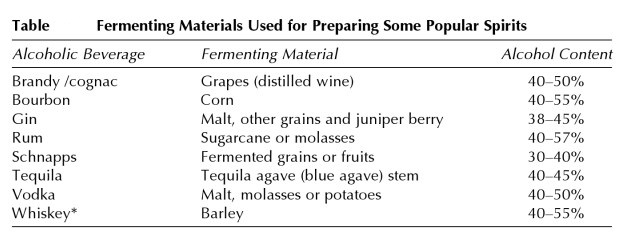
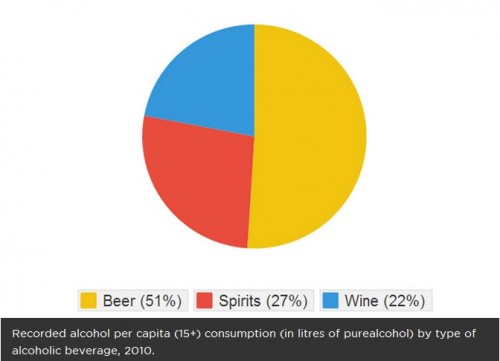

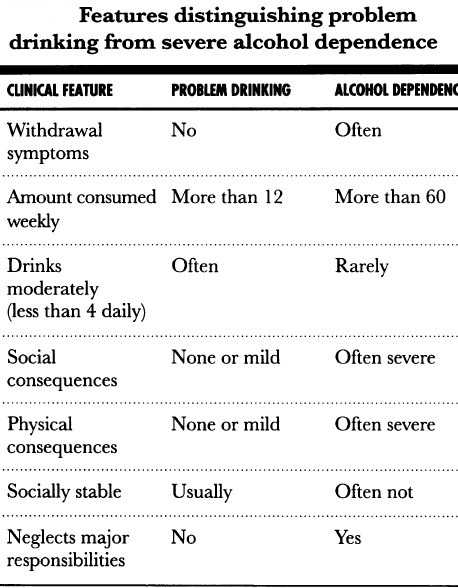
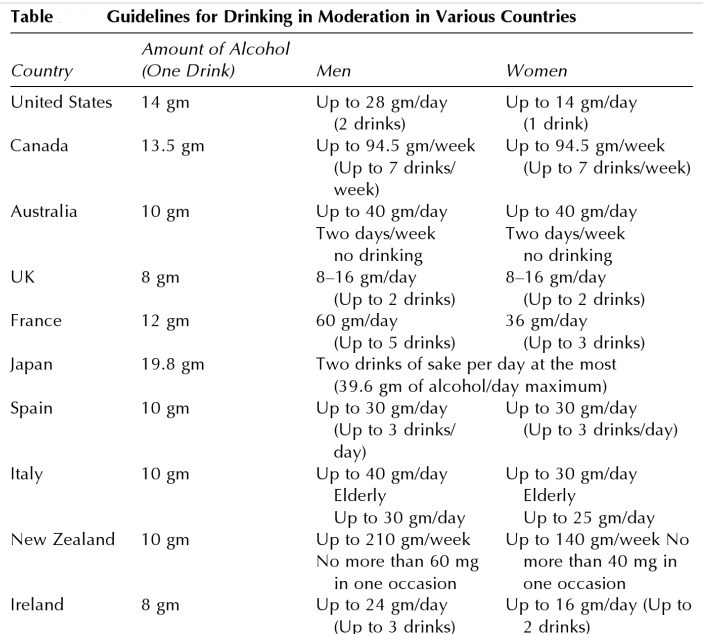
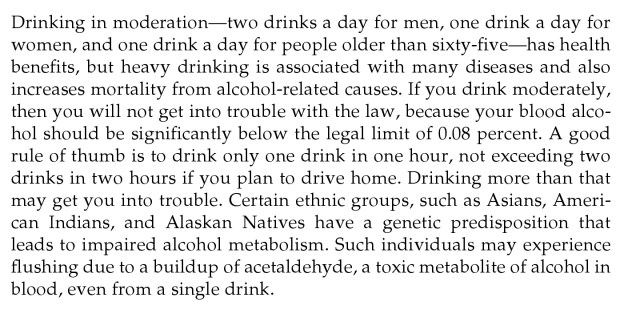
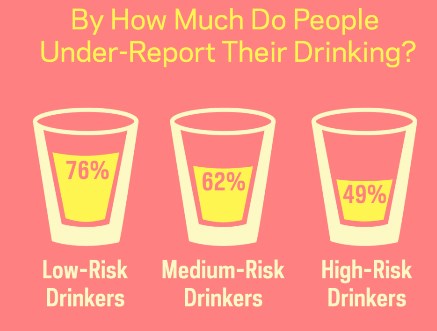
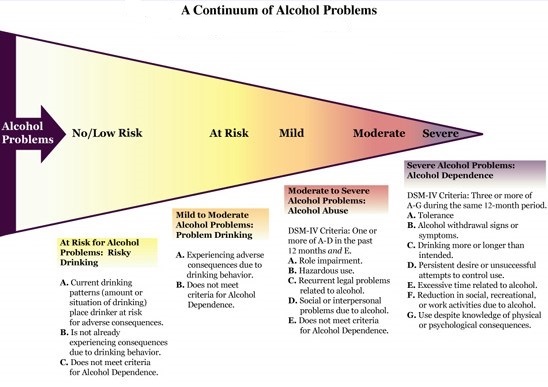
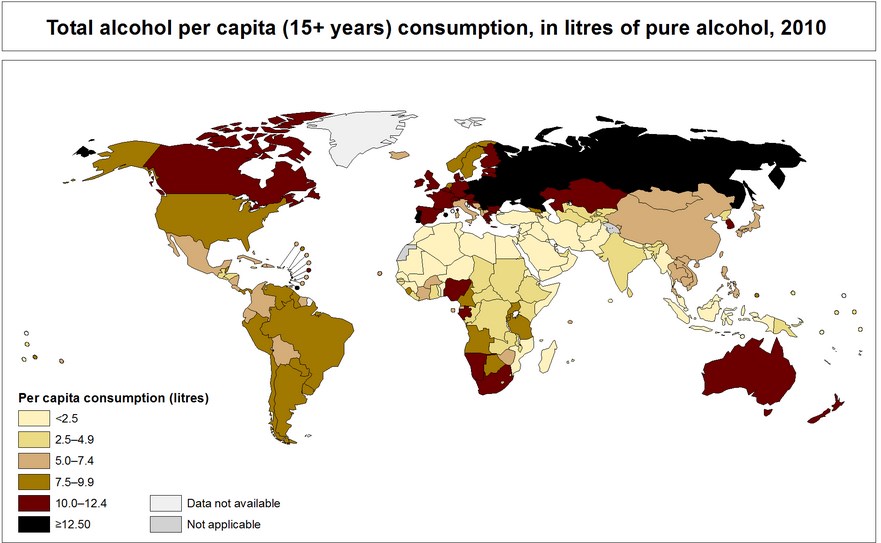
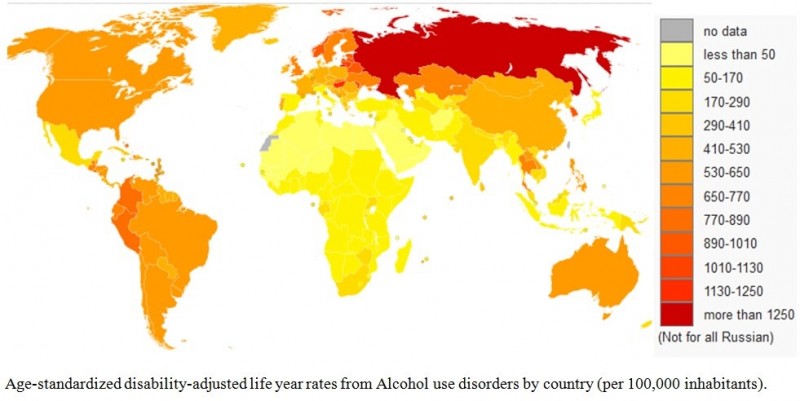
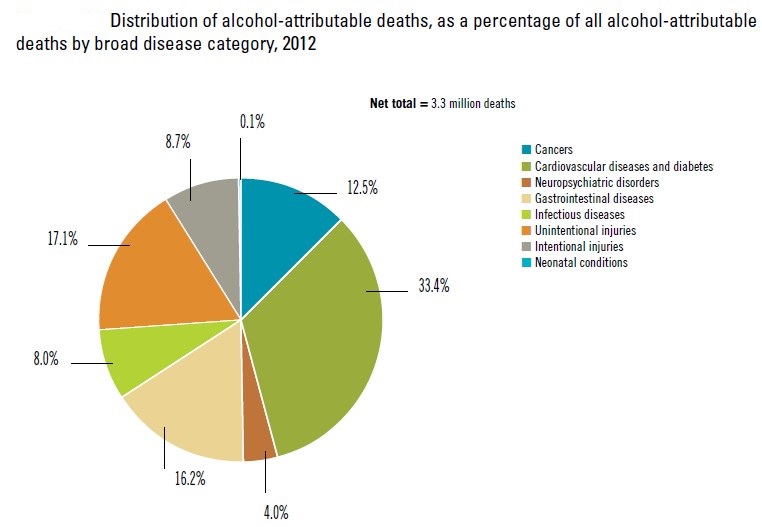
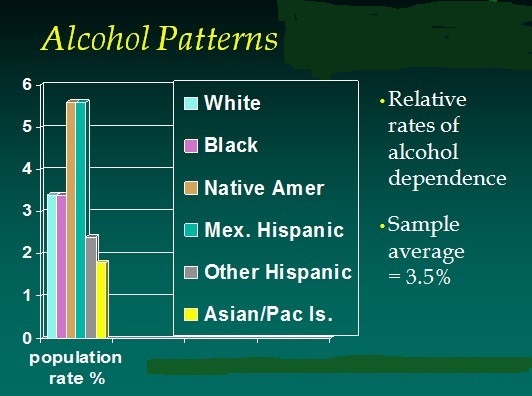
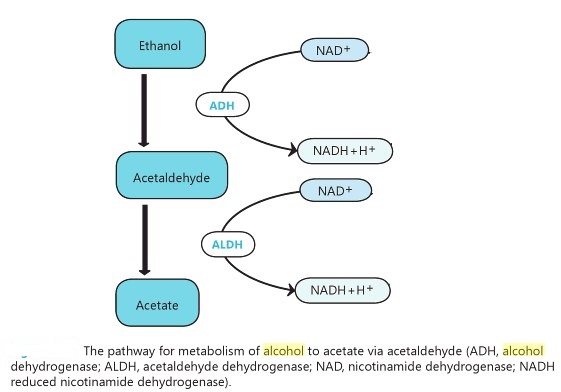
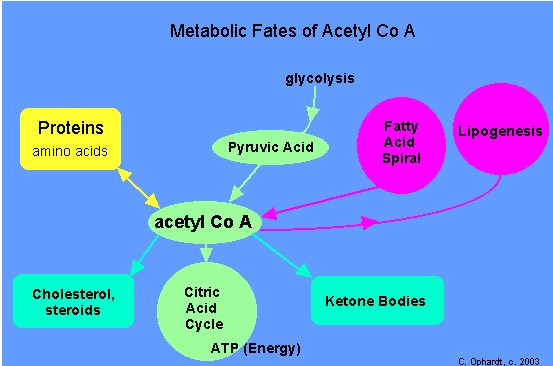
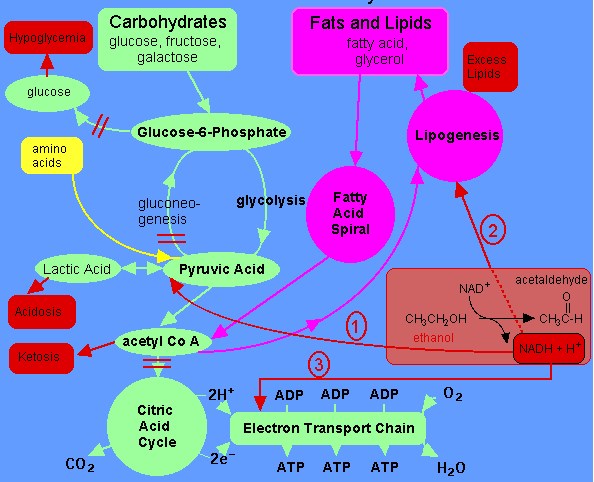
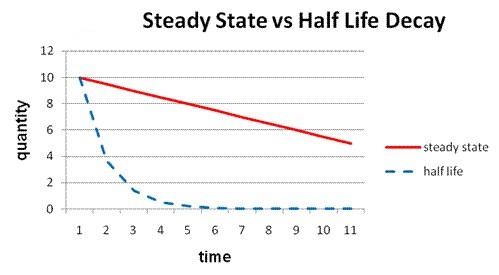
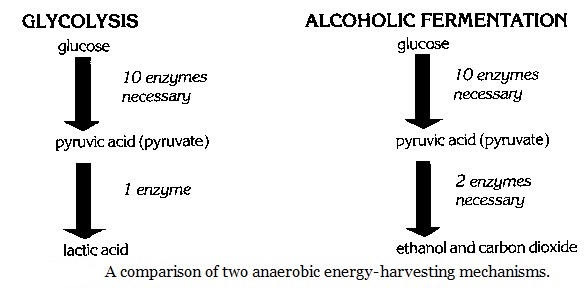
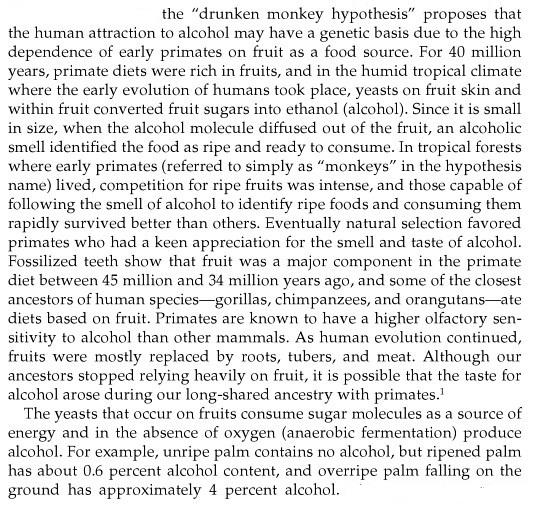

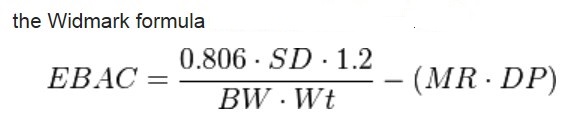
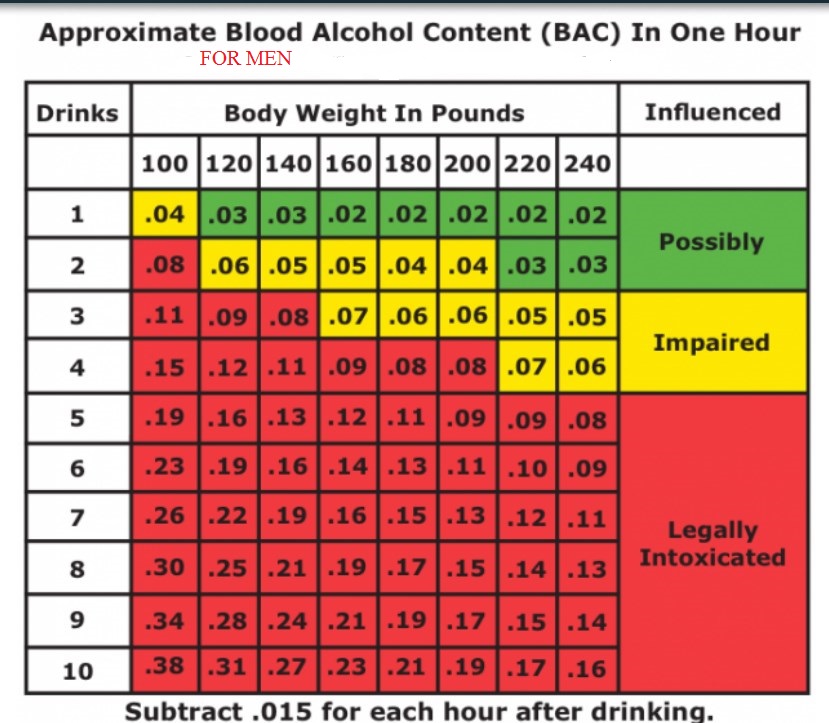
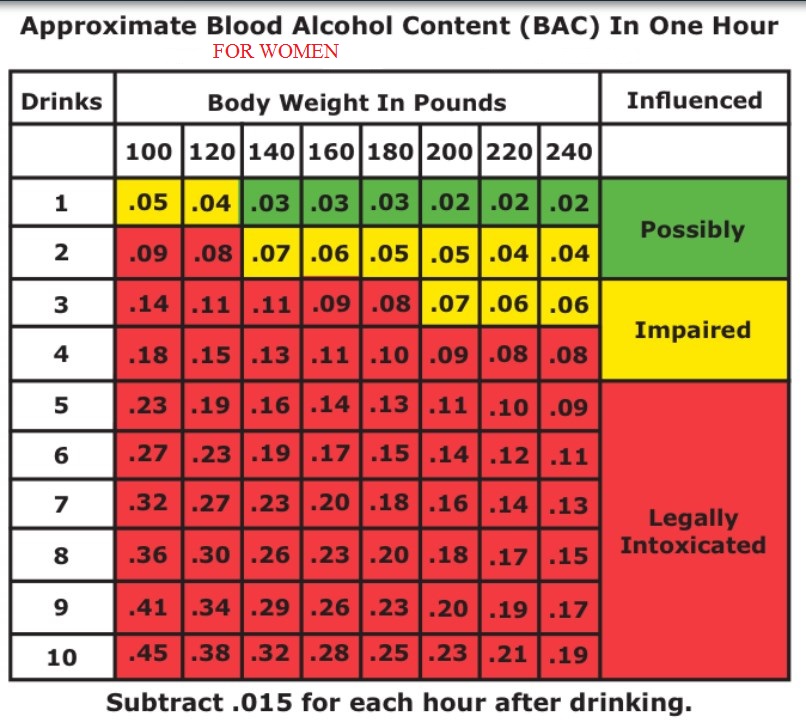
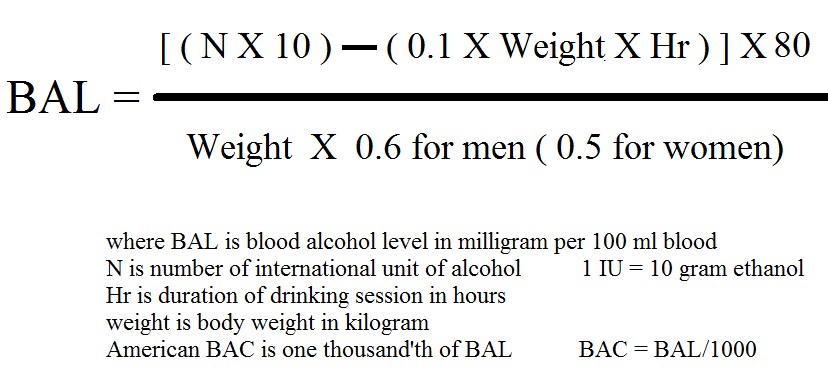

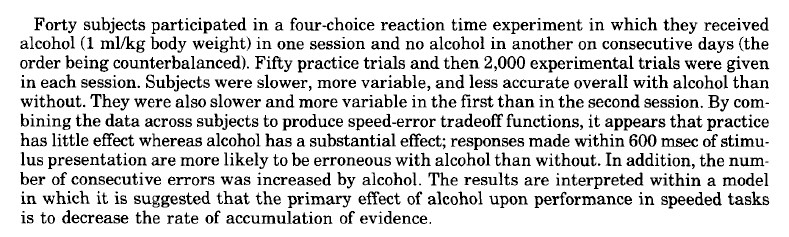

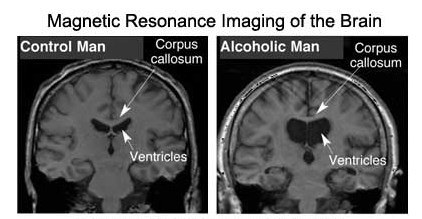
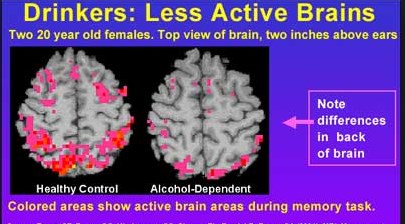
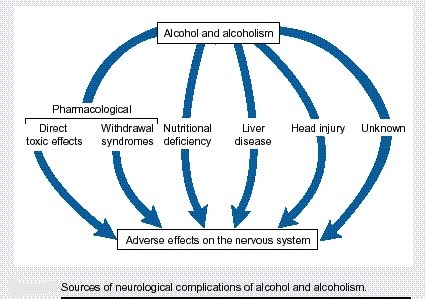
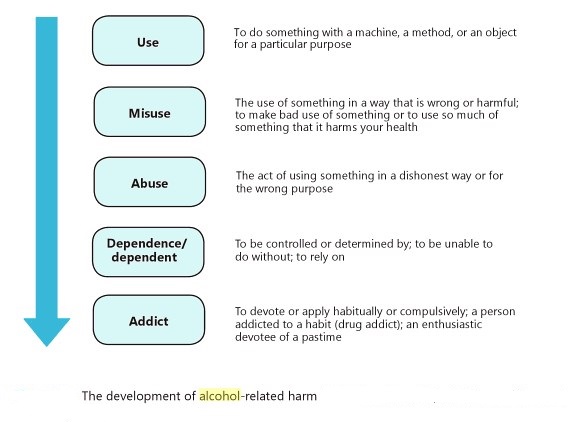
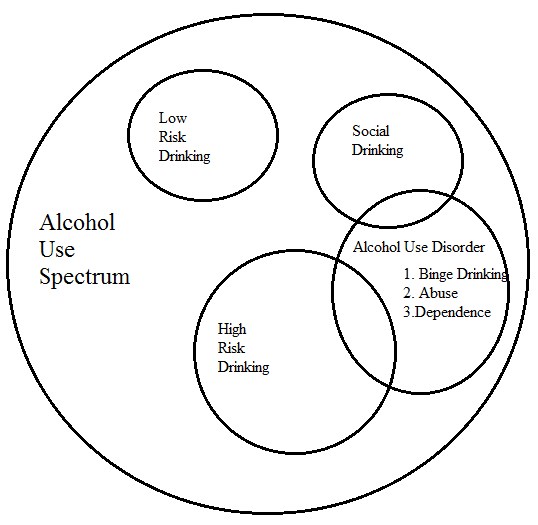
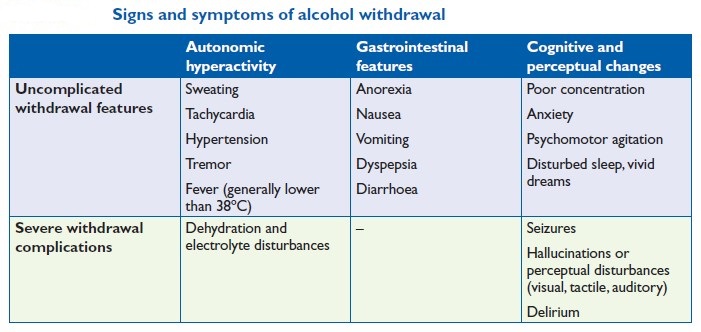
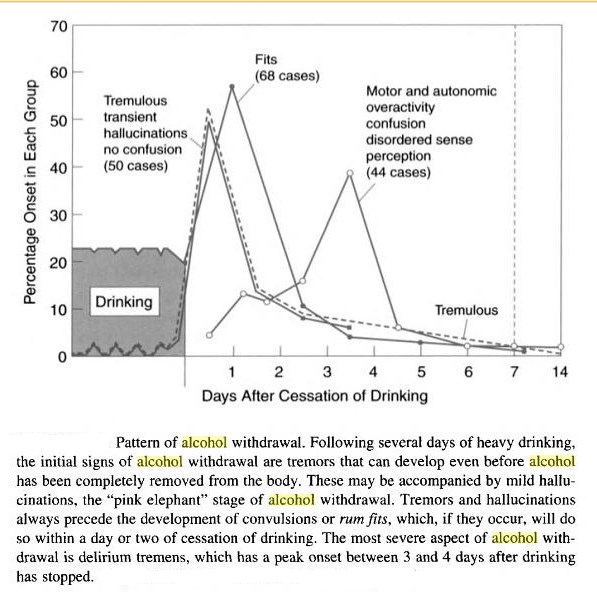
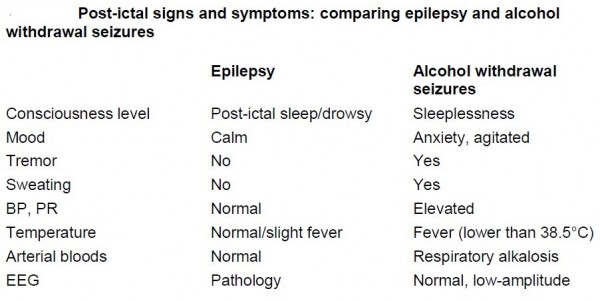
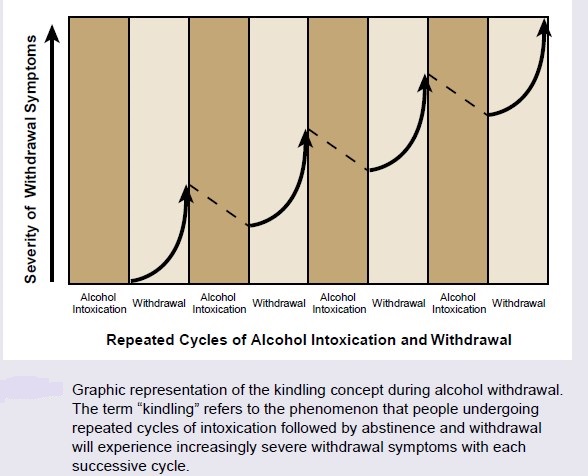
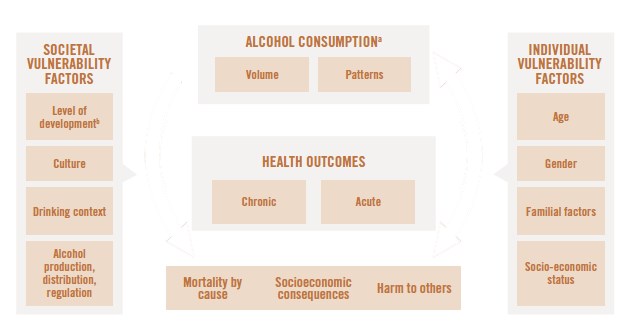
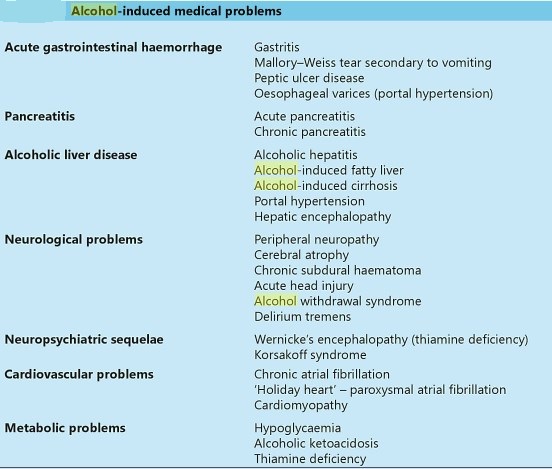
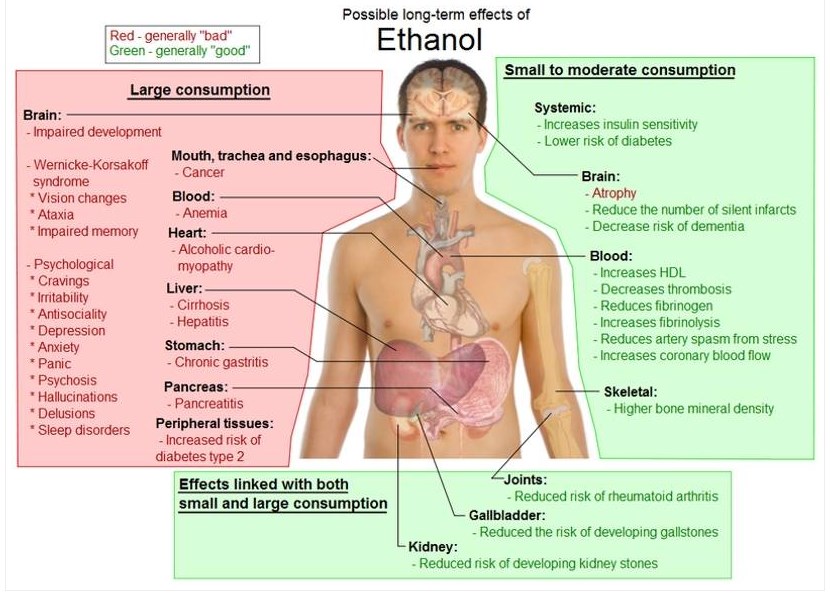
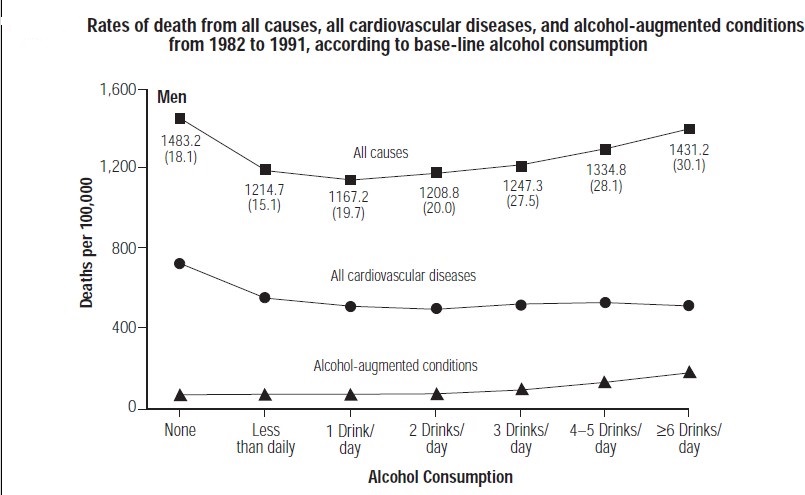
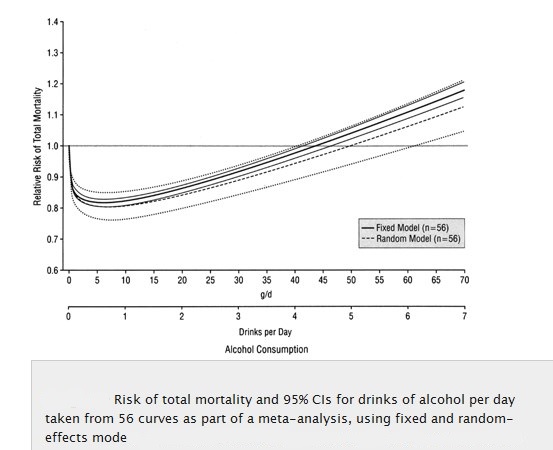
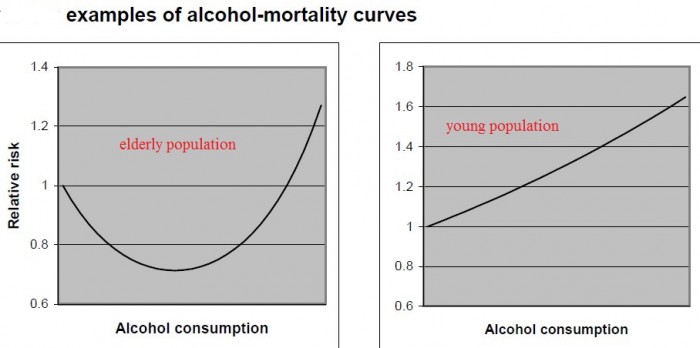
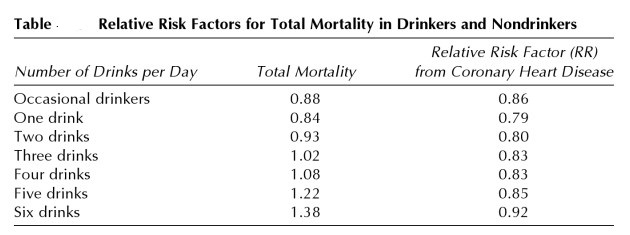
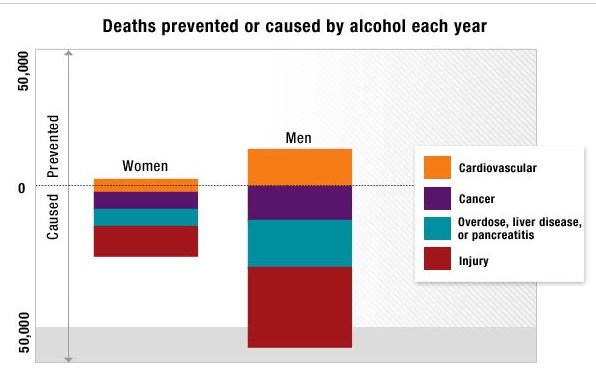
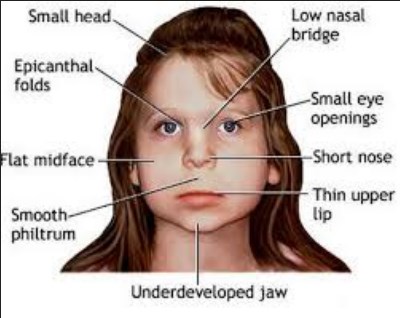
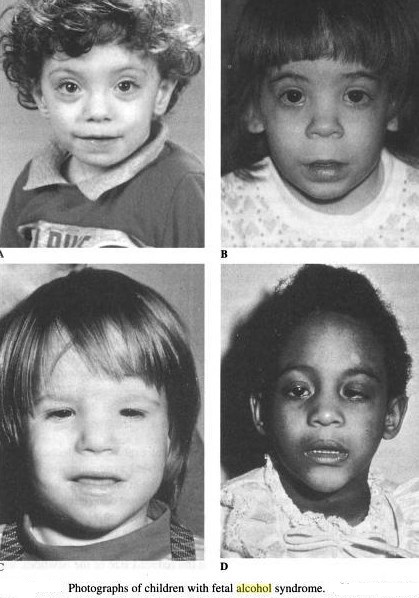
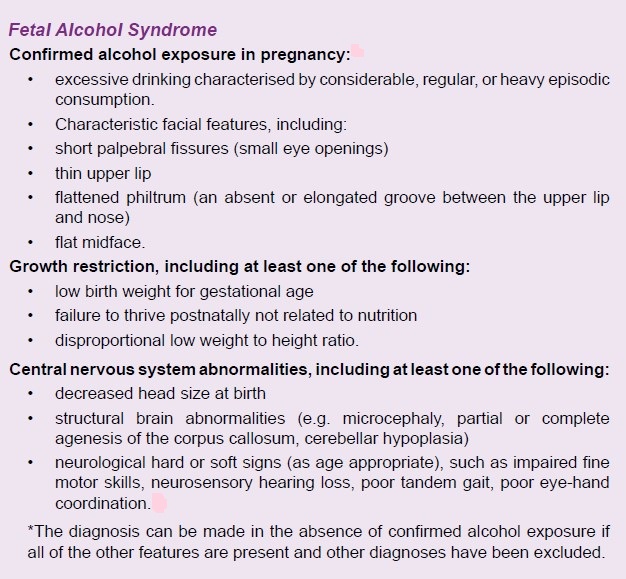
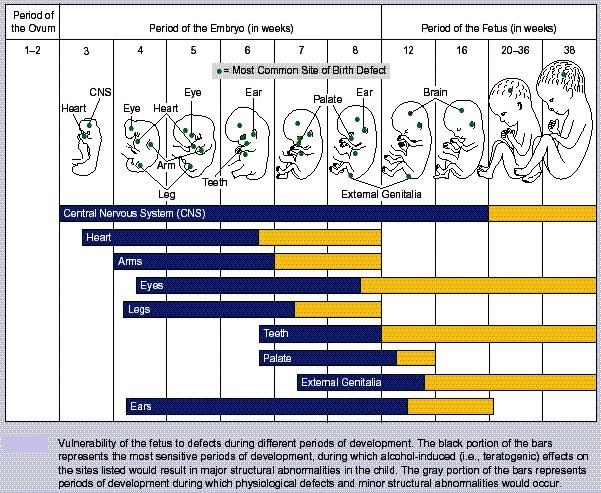
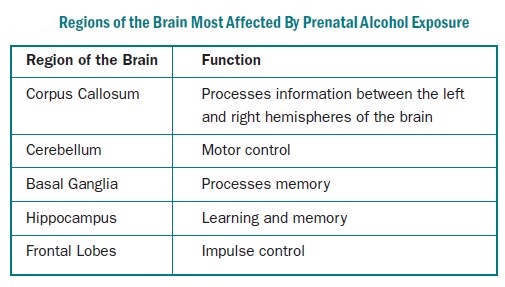
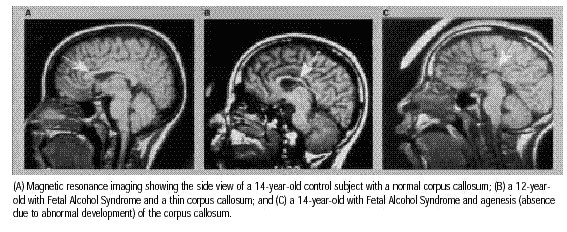
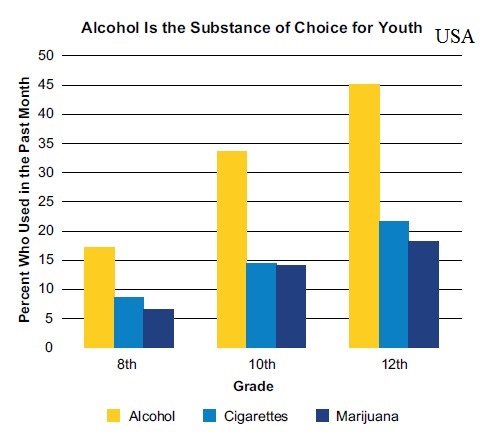
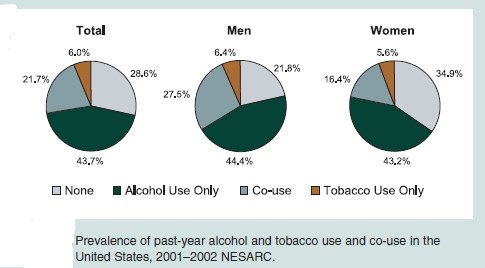
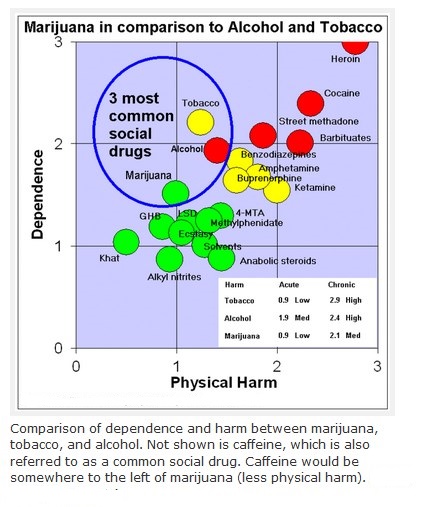
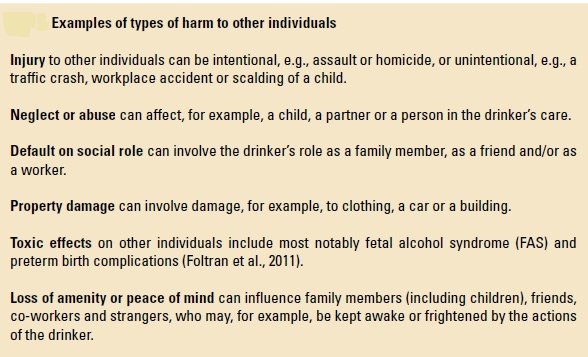
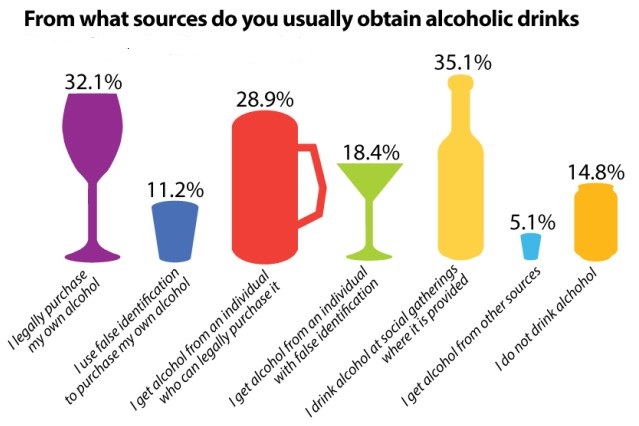
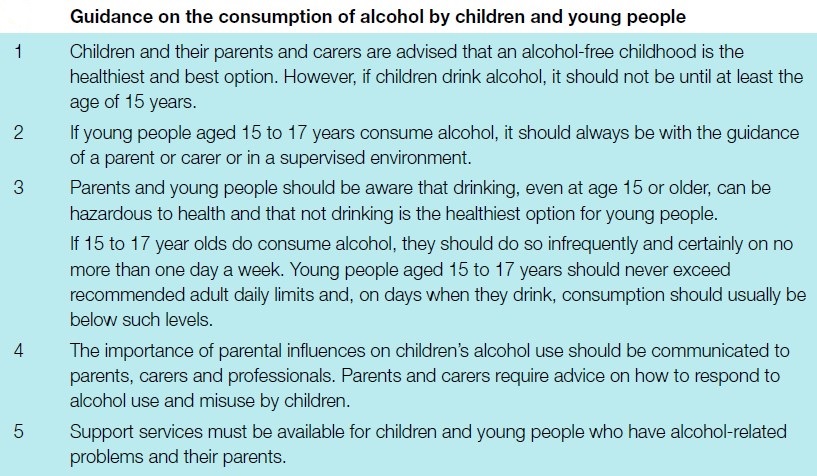
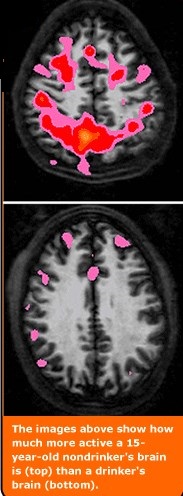
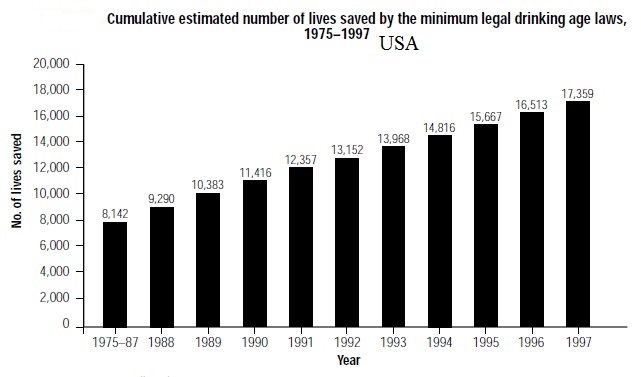
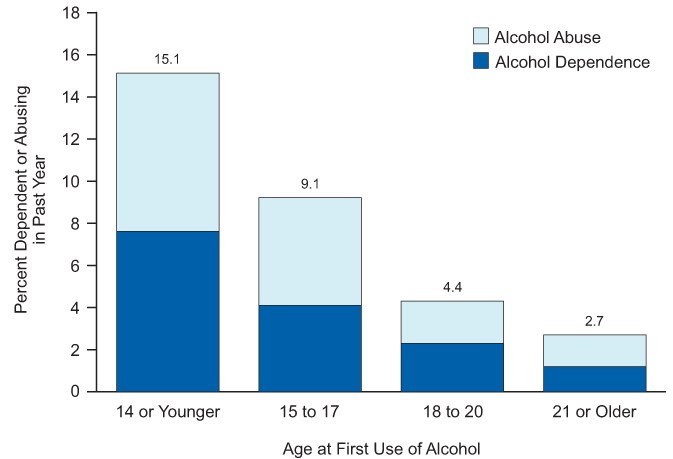
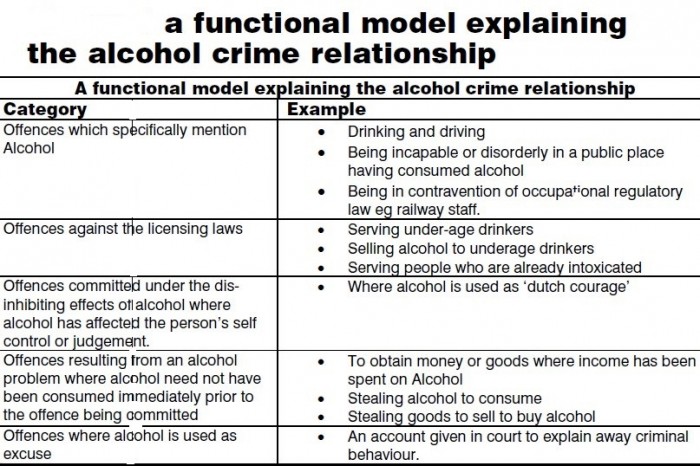
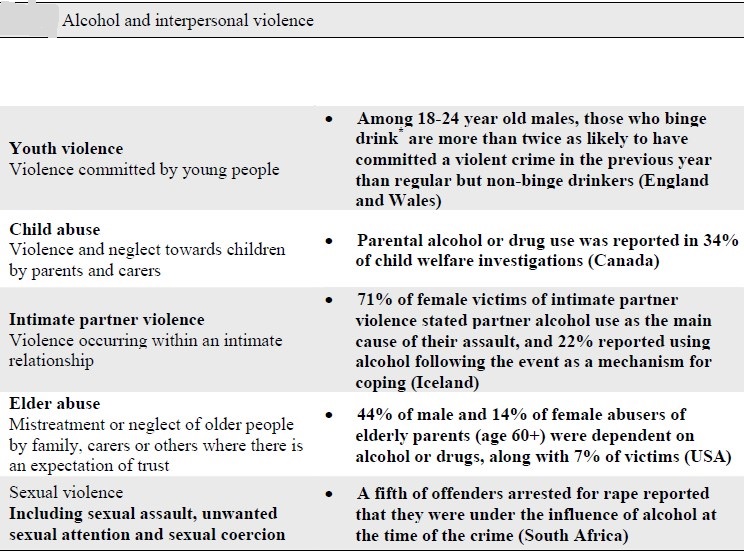
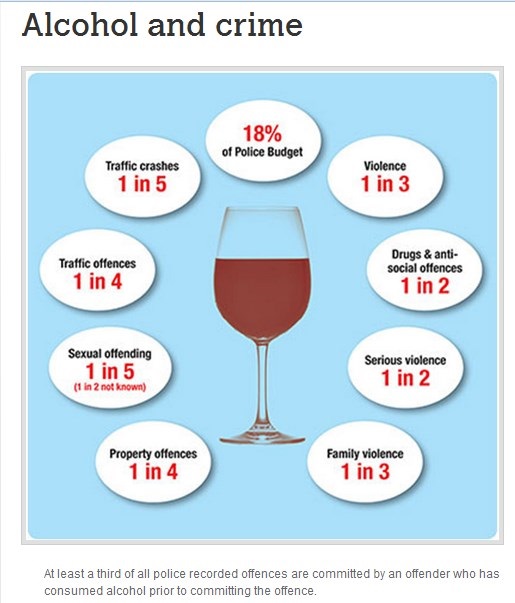
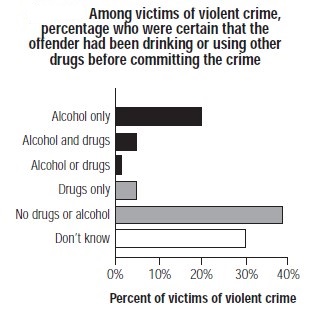
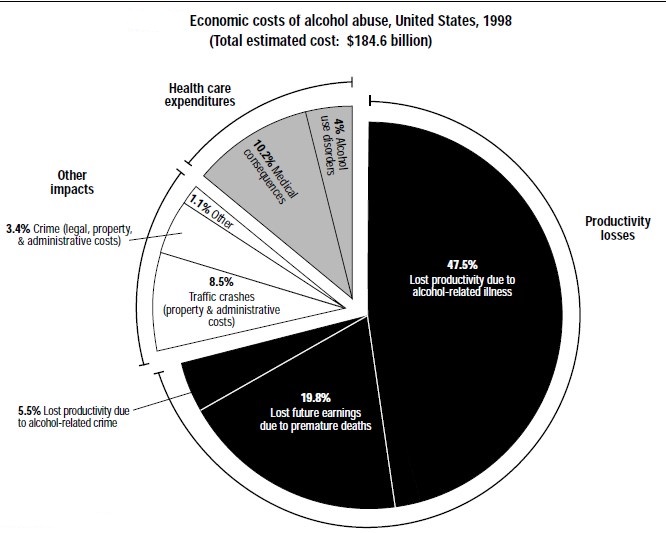
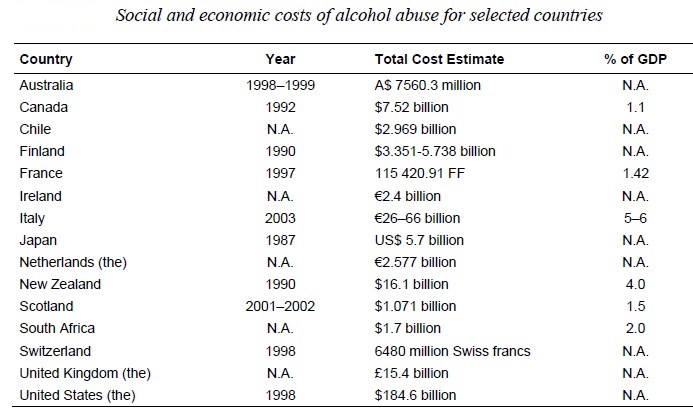
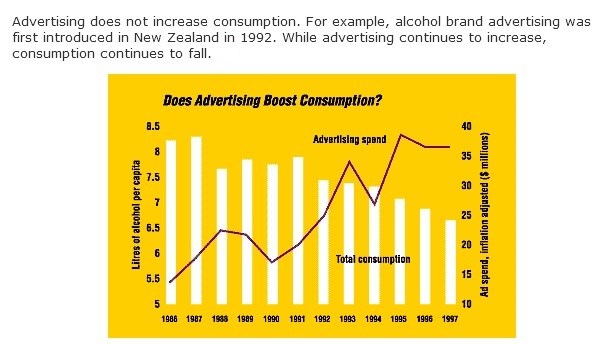

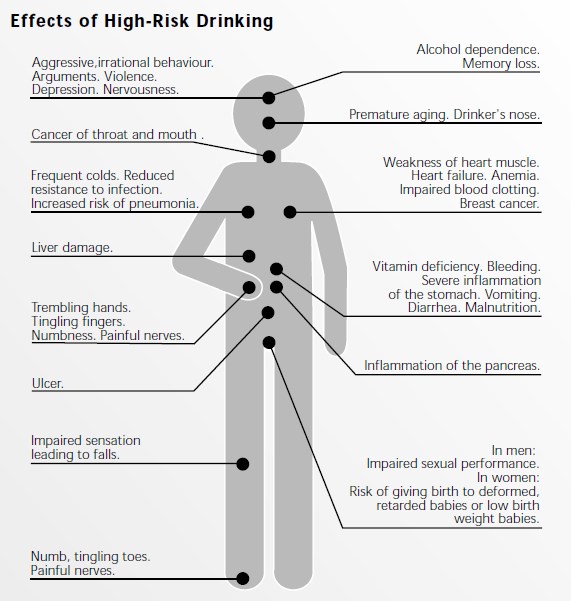
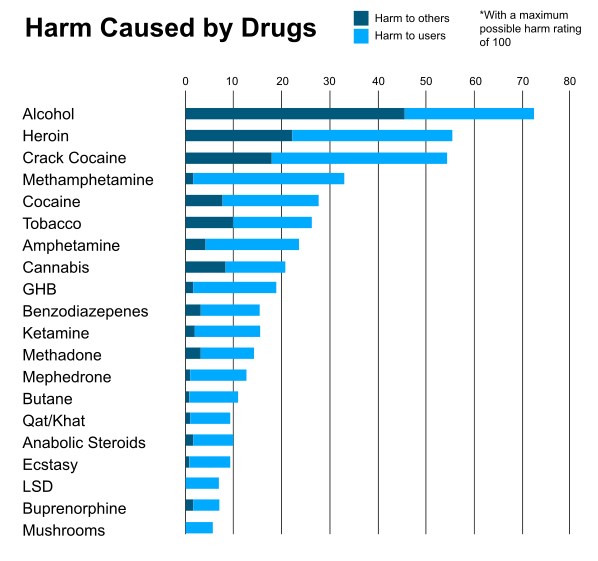
I’m impressed, I must say. Seldom do I encounter a blog that’s both educative and interesting, and without a doubt, you’ve hit the nail on the head. The issue is something that too few men and women are speaking intelligently about. I am very happy that I stumbled across this during my search for something regarding this.
The very next time I read a blog, Hopefully it won’t disappoint me just as much as this particular one. I mean, I know it was my choice to read through, however I genuinely thought you’d have something helpful to say. All I hear is a bunch of complaining about something you could possibly fix if you weren’t too busy looking for attention.
Major thankies for the blog article.Really thank you! Much obliged.
This is a topic which is near to my heart… Thank you! Where are your contact details though?
It’s hard to search out educated people on this matter, but you sound like you recognize what you’re speaking about! Thanks
Yes, this is a Good one
If you gamble a few rounds you might get a couple of bucks, but try a little longer and it’s all absent. The clients can play here all these video games and win for themselves fantastic sums of real money.
I really prize your work , Great post.
some truly interesting details you have written.
Your home is valueble for me. Thanks!…
A big thank you for your blog.Really thank you! Cool.