Dr Rajiv Desai
An Educational Blog
DRUG ADDICTION
Drug Addiction:
_
Intravenous injection of heroin typically causes a rush within seven to eight seconds. This method of drug use provides the highest intensity and quickest onset of the initial rush but is also the most dangerous. Also, approximately 10% of new HIV infections worldwide are attributable to injecting drug use, often of an opiate such as heroin.
______
Prologue:
Drugs are fascinating because they change our awareness. The basic reason people take drugs is to vary their conscious experience. Seeking pleasure is a human trait and certain chemicals which give a feeling of high or pleasure have always been used by some people everywhere. Of course, there are many ways to alter consciousness, such as listening to music, dancing, exercising, day dreaming and participating in religious rituals etc. and the list suggests that changing consciousness is something people like to do. People use substances (drugs) to alter their mood, to cover up their sadness, to ease their heartbreak, to lighten their stress load, to blur their painful memories, to escape their hurtful reality, or to make their unbearable days or nights bearable. Almost all cultures have used psychoactive drugs to facilitate social interaction, to alter consciousness, and to heal.
As drug addiction became more widespread, celebrities became more comfortable discussing their drug use, and some of their statements may have fanned the flames of drug abuse and addiction. This quote from George Harrison of The Beatles about his drug use proves this point quite well: “Suddenly I felt the most incredible feeling come over me. It was something like a very concentrated version of the best feeling I’d ever had in my whole life. It was fantastic. I felt in love, not with anything or anybody in particular, but with everything. Everything was perfect, in a perfect light, and I had an overwhelming desire to go around the club telling everybody how much I loved them—people I’d never seen before.”
Humans have used psychoactive substances for as long as we have records and some of the largest corporations in the world are actively developing new ones for the future. There is no magic bullet that will suddenly make these compounds disappear from our society. If there were, the past century of ever-increasing penalties for possession and sale of recreationally used drugs, along with massive anti-drug “education” campaigns, would have reduced use. But they have not. The cultural positions of different drugs vary enough to preclude universal policies on how to deal with all illicit drugs. The drug menace is the illicit, non-medical use of limited number of substances which have the property of altering the mental state in ways that are considered by social norms and defined by statute to be inappropriate, undesirable, harmful threatening to the life of the user and to the society at large. Heroin, cocaine, opium, LSD and marijuana are some of the drugs abused. Generally, the youth seem to be the target of this drug menace and its abuse. Curiosity, peer pressure, and availability of drugs are the immediate causes of drug abuse amongst the youth. Prolonged use of drugs cripples the user’s judgement and thinking ability. This leads to a set of complex social, medical and psychological problems. Drug addiction remains one of society’s major public health problems, posing a significant threat to the health as well as the social and economic fabric of individuals, families, communities, and nations. Few diseases can compete with addiction in their capacity to generate misinformation, misjudgment, or misunderstanding.
Would you believe that nearly 90% of 45-year-olds in the United States have tried an illegal drug in their lifetime? Few people take their first dose of a drug with the hope of getting addicted. Yet millions are getting addicted to drugs worldwide. The drug trade has become a multibillion-dollar business gradually engulfing the globe controlled by drug lords and drug cartels who receive political support from Latin America to Afghanistan.
______
Note:
Drug in this article means psychoactive drug. Although this article is titled ‘Drug Addiction’, I am predominantly discussing illicit drug addiction as I have already discussed so called ‘Licit Drugs’ alcohol and nicotine (tobacco) in my earlier articles.
_____
Abbreviations and synonyms:
CB1R = type 1 cannabinoid receptor
DA = dopamine
DAT = dopamine transporter
GABA = γ -aminobutyric acid
GHB = γ -hydroxy butyrate
BDNF = brain-derived neurotrophic factor
CRF = corticotropin‐releasing factor
ACE = Adverse childhood experiences
MDA = 3,4-Methylenedioxyamphetamine
NSP = Needle and syringe program
OST = Opioid Substitution Therapy = Opioid replacement therapy (ORT)
CBD = cannabidiol
DMT = Dimethyltryptamine,
DOM = 2,5-Dimethoxy-4-methylamphetamine, known on the street as STP, standing for Serenity, Tranquillity and Peace
AMT = α-Methyltryptamine
DOI = 2,5-Dimethoxy-4-iodoamphetamine
GIRK = G protein–coupled inwardly rectifying K+
GPCR = G protein–coupled receptor
MOR = μ-opioid receptor
NAcc = nucleus accumbens
MSN = medium spiny neuron
nAChR = nicotinic acetylcholine receptor
NMDA = N-methyl-D-aspartate
PCP = phencyclidine
PFC = prefrontal cortex
SERT = serotonin transporter
THC = delta-9-tetrahydrocannabinol
VTA = ventral tegmental area
fMRI = functional magnetic resonance imaging
HIPP/PH = hippocampus/parahippocampal gyrus
PET = positron emission tomography
VS = ventral striatum
LSD = Lysergic acid diethylamide
MDMA = 3,4-methylenedioxymethamphetamine = ecstasy
SUD = substance use disorder
UNICEF = United Nations Children’s Fund
WHO = World Health Organization
UNODC = United Nations Office on Drugs and Crime
INCB = International Narcotics Control Board
Europol = European Union Agency for Law Enforcement Cooperation
NIH = National Institutes of Health
NIDA = The National Institute on Drug Abuse
_______
Addiction Glossary of Terms, Phrases, and Definitions:
Addiction: a brain disorder characterized by compulsive engagement in rewarding stimuli despite adverse consequences
addictive: behavior that is both rewarding and reinforcing
addictive drug: a drug that is both rewarding and reinforcing
dependence: an adaptive state associated with a withdrawal syndrome upon cessation of repeated exposure to a stimulus (e.g., drug intake)
drug sensitization or reverse tolerance: the escalating effect of a drug resulting from repeated administration at a given dose
drug withdrawal: symptoms that occur upon cessation of repeated drug use
physical dependence: dependence that involves persistent physical–somatic withdrawal symptoms (e.g., fatigue and delirium tremens)
psychological dependence: dependence that involves emotional–motivational withdrawal symptoms (e.g., dysphoria and anhedonia)
reinforcing stimuli: stimuli that increase the probability of repeating behaviors paired with them
rewarding stimuli: stimuli that the brain interprets as intrinsically positive, pleasurable and desirable or as something to approach
sensitization: an amplified response to a stimulus resulting from repeated exposure to it
substance use disorder – a condition in which the use of substances leads to clinically and functionally significant impairment or distress
tolerance: the diminishing effect of a drug resulting from repeated administration at a given dose
impulsivity: an inability to resist urges, deficits in delaying gratification, and unreflective decision-making. It is a tendency to act without foresight or regard for consequences and to prioritize immediate rewards over long-term goals.
positive reinforcement: the process by which presentation of a stimulus such as a drug increases the probability of a response like drug taking.
negative reinforcement: the process by which removal of a stimulus such as negative feelings or emotions increases the probability of a response like drug taking.
compulsivity: repetitive behaviors in the face of adverse consequences, and repetitive behaviors that are inappropriate to a particular situation. People suffering from compulsions often recognize that the behaviors are harmful, but they nonetheless feel emotionally compelled to perform them. Doing so reduces tension, stress, or anxiety.
snort: inhale the powdered form of an illegal drug through the nose
__
dopamine (DA): A neurotransmitter present in brain regions that regulate movement, emotion, motivation, and the feeling of pleasure.
GABA (gamma-amino butyric acid): A neurotransmitter in the brain whose primary function is to inhibit the firing of neurons.
locus ceruleus (LC): A region of the brain that receives and processes sensory signals from all areas of the body; involved in arousal and vigilance.
noradrenaline (NA): A neurotransmitter produced in the brain and peripheral nervous system; involved in arousal and regulation of blood pressure, sleep, and mood; also called norepinephrine.
nucleus accumbens (NAcc): A structure in the forebrain that plays an important part in dopamine release and stimulant action; one of the brain’s key pleasure centers.
prefrontal cortex (PFC): The frontmost part of the brain; involved in higher cognitive functions, including foresight and planning.
ventral tegmental area (VTA): The group of dopamine-containing neurons of midbrain that make up a key part of the brain reward system; key targets of these neurons include the nucleus accumbens and the prefrontal cortex
__
Conditioned place preference: A behavioural test for examining the rewarding properties of drugs. The preference of a particular environment associated with drug exposure is measured by comparing the time an animal spends in the compartment where the drug was previously administered compared to a control compartment.
Coupling efficiency: The efficiency with which a given G protein–coupled receptor can activate an effector.
DARPP-32: Dopamine and cAMP-regulated phosphoprotein. A key target protein for increased dopamine that plays a role in signaling the effects of many addictive drugs.
DeltaFosB (ΔFosB): A transcription factor that is induced in areas such as the NAcc in response to many addictive drugs, and thought to be involved in the long-term maintenance of addictive behaviour.
EC50: 50% effective concentration, i.e., the concentration of an agonist that produces 50% of the maximal effect.
Equilibrative nucleoside transporter ENT1: Transporter responsible for the re-uptake of adenosine.
Kir3/GIRK channels: One class of inwardly rectifying potassium channels; Kir3 are also termed G protein–coupled inwardly rectifying K+ channels.
Quantal content: The amount of neurotransmitter released by a single vesicle.
_______
_______
Introduction to drug addiction:
_
What is a drug?
There are various definitions of what a drug is. A drug is any substance (with the exception of food and water) which, when taken into the body, alters the body’s function either physically and/or psychologically. For the purposes of this article, we consider a ‘drug’ to be any chemical substance, natural or synthetic, that changes a person’s mental state and that may be used repeatedly by a person for that effect. Drugs may be legal (e.g. alcohol, caffeine and tobacco) or illegal (e.g. cannabis, ecstasy, cocaine and heroin).
The word licit means “within the law”. In other words, anything that is licit is allowed or legal. Licit drugs include alcohol, caffeine, and nicotine. It is legal to purchase and use these substances. Legal drug use includes prescription drugs that are used according to doctor’s instruction as well as by the person for whom it was prescribed. Legal drugs also include medicines used for an illness and over the counter drugs when used as directed. Illegal is an adjective, where it means not in accordance with laws. Illicit is another adjective that means against the law. It has connotations of immorality. Some people might know that the phrase “illicit drugs” refer to drugs that are “illegal” or “forbidden”. However, many people don’t realize that these drugs are not only illegal to use, but they are also illegal to sell and make. Illicit drugs are those that have been classified as illegal because they pose a threat to one’s health and in some cases, their life. They are also dangerous to society as well as the national and even global economy. Individual countries and places have different laws about different drugs, and there are also international treaties against some drugs.
Examples of illicit drugs include:
Heroin
Cocaine
Methamphetamine
Cannabis
LSD
Ecstasy
Psilocybin or magic mushrooms
PCP
In addition to being illegal, some drugs are classified into five categories, schedule I, II, III, IV, or V by the Controlled Substances Act (CSA) in the U.S. The drugs are classified on their deemed potential for abuse. Those drugs with high risk and no benefits are banned from medical practice and are considered to be Schedule I drugs. Of the drugs listed above heroin, methamphetamine, LSD, and ecstasy are considered to be Schedule I drugs. Schedule II drugs are also considered to be dangerous, particularly because they can create a physical and psychological dependence. These include methadone, oxycodone, morphine, and codeine. The classification of drugs continues with III, IV, and V, depending upon how dangerous it may be.
______
Drug abuse is a global phenomenon, affecting almost every country, but its extent and characteristics differ from region to region. Illicit drug abuse not only affects the health and lives of individuals but also undermines the political, social, and cultural foundation of all countries. Problems of drug dependence produce dramatic costs to all societies in terms of lost productivity, transmission of infectious diseases, family and social disorder, crime, and excessive utilization of health care. The picture is grim if the world statistics on the drugs scenario is taken into account. With a turnover of around $500 billion, it is the third largest business in the world, next to petroleum and arms trade. Drug addiction causes immense human distress, and the illegal production and distribution of drugs have spawned crime and violence worldwide. Today, there is no part of the world that is free from the curse of drug trafficking and drug addiction. Millions of drug addicts, all over the world, are leading miserable lives, between life and death.
_
Illicit drugs are only used by a minority of the world’s population, with between 3.5% and 5.7% having used an illicit substance at least once (United Nations Office on Drugs and Crime, 2010). Around 10–15% of these are classed as problematic users. Cannabis has the highest prevalence of use followed by amphetamine, cocaine and heroin. In the UK, problem drug use of Class A substances costs society £15.4 billion a year, of which £13.9 billion is attributable to criminal offences. The US Department of Justice National Drugs Intelligence Centre (2011) reported that the total impact of illicit substances on society amounted to over $193 billion, with crime and incarceration accounting for over $100 billion of these costs. Addiction exacts an “astoundingly high financial and human toll” on individuals and society as a whole. In the United States, the total economic cost to society is greater than that of all types of diabetes and all cancers combined. These costs arise from the direct adverse effects of drugs and associated healthcare costs (e.g., emergency medical services and outpatient and inpatient care), long-term complications (e.g., lung cancer from smoking tobacco products, liver cirrhosis and dementia from chronic alcohol consumption, and meth mouth from methamphetamine use), the loss of productivity and associated welfare costs, fatal and non-fatal accidents (e.g., traffic collisions), suicides, homicides, and incarceration, among others. Classic hallmarks of addiction include impaired control over substances or behavior, preoccupation with substance or behavior, and continued use despite adverse consequences. Habits and patterns associated with addiction are typically characterized by immediate gratification (short-term reward), coupled with delayed deleterious effects (long-term costs).
_
The impact of drugs and alcohol on children is particularly problematic, as adolescents are significantly more vulnerable than adults to substance abuse and to addiction. Also, because many of the molecular targets affected by drugs are involved with brain development, substance abuse during childhood and adolescence has the potential to be particularly deleterious. Indeed, it has been shown that children who begin using alcohol early in childhood (ages 14 or younger) are four times more vulnerable to becoming addicted to alcohol later in life than are those who begin drinking at 20 years of age or older. The younger you start using drugs or alcohol, the more likely you are to get addicted. Between ages 10-19, the prefrontal cortex (the part of the brain responsible for sizing up a situation, making good decisions, and controlling how we react to what we want and how we feel) is still developing. You’re more likely to experiment with substance use during this time because the prefrontal cortex isn’t done maturing and those substances could impact future brain development, making it easier to continue to use.
_
Current approaches aimed at reducing illicit drug use include prohibition of supply, education and treatment. Most countries and international agencies (such as the United Nations and World Health Organization), classify drugs according to how dangerous or harmful they are. For example, under the UK Misuse of Drugs Act 1971, drugs are segregated into three classes (A, B and C) which are meant to (i) reflect their relative harms and (ii) determine the penalties for possessing and trafficking each drug. In the USA drugs are classified into five schedules reflecting their ‘potential for abuse’. It has been argued that these systems have evolved in an unsystematic way according to social, political and historical concerns rather than being based on any scientific evidence. The International Day against Drug Abuse and Illicit Trafficking is observed annually on 26 June. The decision to mark the day was taken on 7 December 1987 via resolution 42/112 of the United Nations General Assembly in order to strengthen global action and cooperation to achieve its aim of making the international society free of drug abuse. This year’s theme ‘Health for Justice. Justice for Health’ emphasizes that justice and health are “two sides of the same coin” when it comes to addressing the problems associated with drugs. According to the United Nations, in order to create effective responses to tackle the problem of drugs, accountable institutions of criminal justice, health and social services should work together to provide integrated solutions.
______
Addiction is defined as a chronic, relapsing disorder characterized by compulsive drug seeking and use despite adverse consequences. It is considered a brain disorder, because it involves functional changes to brain circuits involved in reward, stress, and self-control, and those changes may last a long time after a person has stopped taking drugs. Addiction is a lot like other diseases, such as heart disease. Both disrupt the normal, healthy functioning of an organ in the body, both have serious harmful effects, and both are, in many cases, preventable and treatable. If left untreated, they can last a lifetime and may lead to death. The word “addiction” is derived from a Latin term for “enslaved by” or “bound to.” Anyone who has struggled to overcome an addiction — or has tried to help someone else to do so — understands why.
_
Addiction is a brain disorder characterized by compulsive engagement in rewarding stimuli despite adverse consequences. Despite the involvement of a number of psychosocial factors, a biological process – one which is induced by repeated exposure to an addictive stimulus – is the core pathology that drives the development and maintenance of an addiction. The two properties that characterize all addictive stimuli are that they are reinforcing (i.e., they increase the likelihood that a person will seek repeated exposure to them) and intrinsically rewarding (i.e., they are perceived as being inherently positive, desirable, and pleasurable). The disease of addiction is one of the least understood, and frequently misunderstood, of all chronic diseases. While it would be absurd to assert that other diseases of the brain such as schizophrenia or depression are due to weak will or moral character, it is still the prevailing opinion of many, including healthcare professionals, that drug addiction is about improper choices rather than improper brain function. Current scientific evidence has revealed that chemical addiction is a process that is caused by a malfunctioning cascade of neurotransmitters which is further exacerbated by drug use.
_
An addicted person’s impaired ability to stop using drugs or alcohol has to do with deficits in the function of the prefrontal cortex — the part of the brain involved in executive function. The prefrontal cortex has several important jobs: self-monitoring, delaying reward, and integrating whatever the intellect tells you. The difficulty also has to do with how the brain, when deprived of the drugs to which it is accustomed, reacts to stress. The response is usually exaggerated negative emotion, and even despair. In this setting, the strong association of learned environmental cues (for instance, smelling beer at a ball game or seeing the corner where the dealer can be found) exacerbates the craving for the substance. And the flood of intoxicating brain chemicals called neurotransmitters (chiefly dopamine) during drug use makes the brain relatively insensitive to “normal” sources of pleasure — say, a good conversation with a friend or a beautiful sunset. The brain science behind these observed and measurable processes in addiction helps to clarify the goals of treatment. Agonist medications (such as methadone and buprenorphine) can stabilize the craving brain while the planning and reasoning processes get back in shape.
_
Essentially, drugs and alcohol produce dopamine, a chemical associated with pleasure, to be released in the brain. Your brain will produce less dopamine as a response to the continual rush that substance use brings, which means you have to continue to use to feel good. Dopamine also interacts with the motivating and planning centers of the brain, meaning that the rush of pleasure that accompanies substance use makes your brain drive you to want and seek out drugs and alcohol. As you use larger amounts of substances or use more often, your brain programs more memories of a quick high and conditions itself to respond well to certain triggers, like the smell of beer or the sight of drug paraphernalia.
What is a trigger?
A trigger is anything that makes you feel the urge to go back to using drugs. It can be a place, person, thing, smell, feeling, picture, or memory that reminds you of taking a drug and getting high. A trigger can be something stressful that you want to escape from. It can even be something that makes you feel happy. People fighting addiction need to stay away from the people and triggers that can make them start using drugs again, just like people with breathing problems need to avoid smoke and dust.
________
Drug addiction, relating to both licit and illicit substances, is a chronic, relapsing disorder defined as compulsive drug seeking and taking that continues despite significant negative consequences. Addictive behaviours usually begin with a period of experimentation with a particular drug, the use of which escalates over repeated exposures associated with the appearance of tolerance; that is, an individuals’ hedonic (pleasure) set point increases and increasing amounts of the drug are needed to reach the “high” produced by earlier lower quantities. As an individual heads towards dependence, there is an increase in the motivation to obtain and continue using a drug and a loss of control in limiting drug intake. There is also a growing awareness of the emotional consequences associated with drug use and a link to environments associated with accessing or taking the drug. Following chronic drug use, many individuals go into withdrawal, usually through self-imposed abstinence, which may see the development of withdrawal syndromes in some patients. Withdrawal is also often associated with a negative emotional state with individuals displaying high levels of depression, stress, and anxiety. In the majority of individuals (up to 90%) this is followed by relapse resulting in a repetitive, cyclic drug taking pattern which displays a high degree of resistance to cessation of drug seeking. Consequently, the progression from casual drug use to an addicted state is commonly referred to as the cycle of addiction which consists of 3 main stages: (1) preoccupation and anticipation of the drug, (2) intoxication, usually in a binge-like fashion with loss of control, (3) withdrawal, usually associated with negative affect, and craving generally followed by relapse.
_
However, not all individuals who experiment with drugs of abuse go on to become addicted, indeed it is estimated that only 10 to 15 % of individuals who engage in drug taking will meet the criteria for addiction. Furthermore, an individual’s vulnerability to displaying addictive behaviours is highly complex and multifactorial being influenced by (epi)genetic, biological, and environmental factors. As a result, individuals who go on to display characteristic addictive behaviours may be influenced by factors mediating their vulnerability to initiate and engage in drug use which is further influenced by factors that mediate their shift from casual to compulsive drug use. Addiction also involves components of both compulsivity and impulsivity; for example, premature responding, as a measure of high impulsivity on attentional tasks, is associated with cocaine seeking and relapse. While drug use is associated with high impulsivity in humans and may further exacerbate the impulsive nature of an individual, evidence from human studies suggests that trait impulsivity may play a greater role in the influence over an individual’s predisposition to continue drug-seeking and -taking behaviours. This includes resistance to ceasing these behaviours during abstinence as treatment known to reduce impulsivity may aid in the prevention of relapse. Assessment of impulsivity in children and adolescents has been used to predict subsequent alcohol-related issues and drug use and smoking vulnerability, with analysis of high impulsivity in siblings of cocaine users suggesting a heritable basis. Impulsivity is also thought to precede compulsivity and it is the shift from impulsive to compulsive behaviours that is linked to the development of addiction in many individuals. Impulsivity can also be distinct from other behaviours such as anxiety, response to a novel environment, and some forms of stress response. However trait impulsivity appears to play greater role in the loss of control over some drugs such as cocaine compared to heroin, for example.
_
People who have stayed sober for a while, either because they were in jail or in treatment, should know that they are at a high risk of overdose if they relapse and take the same amount of drug they used to. Their cravings may not have decreased, but their tolerance has, meaning their body can’t handle usual doses of the drug anymore. Without immediate treatment, overdose often leads to death. This is why you often hear about people dying of an overdose soon after leaving rehab.
_
Due to the complex nature of drug addiction, our greatest understanding of the neurobiological aspects of processes mediating addictive behaviours have, to date, largely come from preclinical studies in animal models. Both humans and animals will voluntarily consume drugs of abuse and display preferences for environments associated with exposure to a drug, continued motivation to obtain a drug, an inability to limit or stop taking a drug despite adverse consequences, and a high incidence of relapse following withdrawal. Animal models can also be assessed based on genetic variability, which indicates an association of heritable factors such as impulsivity, with the predisposition to engage in drug-seeking behaviours as seen in the human situation. Of relevance, like humans, only a subset of animals exposed to a drug (~17%) will display addictive-like behaviours providing validity in the extrapolation of animal data to the human situation.
_
In thinking about the problem of addiction, and the development of animal models of addiction, it is important to remember that at some time many people experiment with a variety of potentially addictive drugs, but most do not become addicted. In other words, mere self-administration of a drug, by a human or by a non-human animal, is not tantamount to addiction. Indeed, the factors responsible for experimental or casual drug use may or may not be directly relevant to the problem of addiction. Drug-seeking and drug-taking in the addict may involve factors that are qualitatively different from those that motivate drug-taking in the nonaddict. The question of addiction specifically concerns (a) the process by which drug-taking behavior, in certain individuals, evolves into compulsive patterns of drug-seeking and drugtaking behavior that take place at the expense of most other activities, and (b) the inability to cease drug-taking, that is, the problem of relapse.
_
Addiction is a disorder of the brain’s reward system which arises through transcriptional and epigenetic mechanisms and develops over time from chronically high levels of exposure to an addictive stimulus (e.g., eating food, the use of cocaine, engagement in sexual activity, participation in high-thrill cultural activities such as gambling, etc.). DeltaFosB (ΔFosB), a gene transcription factor, is a critical component and common factor in the development of virtually all forms of behavioral and drug addictions. Two decades of research into ΔFosB’s role in addiction have demonstrated that addiction arises, and the associated compulsive behavior intensifies or attenuates, along with the overexpression of ΔFosB in the D1-type medium spiny neurons of the nucleus accumbens. Due to the causal relationship between ΔFosB expression and addictions, it is used preclinically as an addiction biomarker. ΔFosB expression in these neurons directly and positively regulates drug self-administration and reward sensitization through positive reinforcement, while decreasing sensitivity to aversion. Examples of drug and behavioral addictions include alcoholism, marijuana addiction, amphetamine addiction, cocaine addiction, nicotine addiction, opioid addiction, food addiction, video game addiction, gambling addiction, and sexual addiction. The only behavioral addiction recognized by the DSM-5 and the ICD-10 is gambling addiction.
______
______
In a broad sense, most addictions progress, in the same way, following the same steps:
- Experimentation- or the first time you try drugs or alcohol. Reasons for experimentation include curiosity, trying to fit in, or to deal with negative emotions like insecurity or sadness.
- Recreation- the stage where your drug use becomes more frequent — usually on weekends and up to a few times a month. You’ll associate this type of use with fun, thrill-seeking, or to conform to peer pressure. You likely won’t notice any negative consequences of doing so.
- Regular use or misuse- the point where you’re not truly addicted, but where drugs begin to become detrimental to your life. You may become uninterested in things that usually bring joy and focus on having fun purely through obtaining substances. This stage could include experiences like getting caught driving under influence of drug or being caught using or carrying drugs.
- Risky use or abuse- when you continue to use drugs despite severe consequences, like using funds set aside for bills on substances (or even borrowing or stealing money) or putting your social or romantic relationships at risk by continuing to use.
- Dependence- the point where drugs or alcohol have taken significant control of your life. While you may still have a job or social relationships, your performance at work has most likely declined, your friendships are probably restricted to other users, and there is usually significant tension at home. At this point, you are physically dependent, meaning your body has gotten used to a steady supply of drugs or alcohol.
- Addiction- the stage when you will do whatever you have to in order to get drugs or alcohol, regardless of the consequences. You are no longer seeking a high, but trying to avoid withdrawal.
With recreational drug use on the rise, it’s important to understand the risks involved with drugs that can lead to addiction. There is a very short amount of time between the experimental phase of recreational drug use and the next steps towards losing control. Based on statistics, recreational drug use is common among a wide range of ages and socioeconomic classes because addiction does not discriminate. Knowing the potential dangers of drug misuse can help educate others to prevent them from using drugs that could lead them down a dark path. Taking drugs recreationally may seem harmless, but it’s one step towards addiction. While some people can experiment with substances without losing control, there are many other factors involved in what makes someone more prone to addiction. Once the wheels towards addiction are set in motion, it’s hard to stop them. If you find yourself questioning whether or not your drug use is truly recreational, or whether or not you have reached the level of addiction with your drug use, consider taking an assessment at a treatment center to help stop addiction in its tracks with the help of trained professionals.
______
______
Substance abuse has a major impact on individuals, families, and communities. The effects of substance abuse are cumulative, significantly contributing to costly social, physical, mental, and public health problems. These problems include:
- Teenage pregnancy
- Human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS)
- Other sexually transmitted diseases (STDs)
- Domestic violence
- Child abuse
- Motor vehicle crashes
- Physical fights
- Crime
- Homicide
- Suicide
_
According to the National Institute on Drug Abuse, people begin taking drugs for a variety of reasons including:
- to feel good — feeling of pleasure, “high”
- to feel better — e.g., relieve stress
- to do better — improve performance
- curiosity and peer pressure
People with addictive disorders may be aware of their problem, but be unable to stop it even if they want to. The addiction may cause health problems as well as problems at work and with family members and friends. The misuse of drugs and alcohol is the leading cause of preventable illnesses and premature death.
_
Symptoms of substance use disorder are grouped into four categories:
- Impaired control: a craving or strong urge to use the substance; desire or failed attempts to cut down or control substance use
- Social problems: substance use causes failure to complete major tasks at work, school or home; social, work or leisure activities are given up or cut back because of substance use
- Risky use: substance is used in risky settings; continued use despite known problems
- Drug effects: tolerance (need for larger amounts to get the same effect); withdrawal symptoms (different for each substance)
Many people experience both mental illness and addiction. The mental illness may be present before the addiction. Or the addiction may trigger or make a mental disorder worse.
_
The National Institute on Drug Abuse indicates the following risk factors for developing drug abuse problems (typically seen in adolescence):
- Unstable home environment, often due to drug abuse or mental illness of the parent
- Poor relationship with parents
- Inadequate supervision over adolescent’s activities
- Use of drugs by friends / peers
- Permissive attitude towards their own drug use and the drug use of the adolescent
- Behavioral problems combined with poor parenting
- Poor achievement in school
- Apparent ambivalence or approval of drug use in the school, peer group or community
- Availability of drugs in the community, peer group or home
_
Drug use disorder facts:
- Drug abuse and addiction, now both grouped as substance or drug use disorder, is a condition characterized by a self-destructive pattern of using a substance that leads to significant problems and distress, which may include tolerance to or withdrawal from the substance.
- Drug use disorder is unfortunately quite common, affecting more than 8% of people in the United States at some point in their lives.
- Dual diagnosis refers to the presence of both a drug-use issue in addition to a serious mental health condition in an individual.
- People can abuse virtually any substance whose ingestion can result in a euphoric (“high”) feeling.
- Inhalants like household cleaners are some of the most commonly abused substances.
- While the specific physical and psychological effects of drug use disorder tend to vary based on the particular substance involved, the general effects of a substance use disorder involving any drug can be devastating.
- Although drug use disorders have no single cause, there are a number of biological, psychological, and social risk factors that can predispose a person to developing a chemical use disorder.
- Symptoms of a drug problem include recurrent drug use that results in legal problems, occurs in potentially dangerous situations, interfere with important obligations, results in social or relationship problems, tolerance, withdrawal symptoms, using a lot of the drug or for a long period of time, persistent desire to use the drug, unsuccessful efforts to stop using the drug, neglecting other aspects of life because of their drug use, and spending inordinate amounts of time or energy getting, using, or recovering from the effects of the drug.
- While the specific effects of drugs on the brain can somewhat vary depending on the drug that is being used, virtually every substance that is abused has an effect on the executive-functioning areas of the brain. Drugs particularly affect the brain’s ability to inhibit actions that the person would otherwise delay or prevent.
- Since there is no single test that can definitively diagnose someone with a chemical use disorder, health care professionals assess these disorders by gathering comprehensive medical, family, and mental health information, as well as securing a physical examination and lab tests to assess the sufferer’s medical state.
- Treatment options for substance abuse disorders remain largely underutilized by most people who suffer from these conditions.
- The primary goals of recovery are abstinence, relapse prevention, and rehabilitation.
- During the initial stage of abstinence, a person who suffers from chemical dependency may need detoxification treatment to help avoid or lessen the effects of withdrawal.
- Often, much more challenging and time-consuming than recovery from the physical aspects of addiction is psychological addiction.
- The treatment of dual diagnosis is more effective when treatment of the sufferer’s mental illness occurs in tandem with the treatment of the individual’s chemical dependency.
- Drug addiction increases the risk of a number of negative life stressors and conditions, particularly if left untreated.
- Episodes of remaining drug free (remission) and relapse characterize recovery from a substance use disorder.
__
What drug makes you angry?
A number of drugs are associated with antisocial and violent behavior. Some drugs, particularly when used to excess and/or used illegally, significantly increase the risk for aggressive behavior and the commission of acts of violence. Alcohol, anabolic steroids, benzodiazepines, methamphetamine and cocaine are key drugs that can escalate the development of aggression and violent behaviour.
How to stay safe from dangers of drugs:
Not taking drugs is the safest option. Most people who are offered drugs don’t accept. If you are in a situation you are pressured to take drugs the best thing to do is to remove yourself from the situation and surround yourself with people who don’t take drugs.
How long after taking drugs can one drive safely?
Drugs affect every person differently. The drug you use (strength, dose, how and how often you use it and other drugs) can affect how long it stays in your system. It can also be affected by you as an individual depending on your tolerance, age and gender, overall health, metabolism, mood and environment you are in. It is against the law for anyone to drive under the influence of a psychoactive drug (a drug that affects the mind or behaviour), and this includes alcohol.
_______
_______
Confusion and lack of consensus in terminology related to drug addiction:
The various definitions of the terms “misuse,” “addiction,” “abuse,” “physical dependence,” “psychological dependence,” “intoxication,” and “nonmedical” or “non-therapeutic use” have elements within each term that are consistently used across the classification and definition systems. Currently, a critical weakness is that distinct patterns of inappropriate use are typically grouped under ill-defined terms such as “misuse” or “abuse.”
_
Abuse definitions:
| Source | Definition |
| National Poison Data System | Intentional improper or incorrect use of a substance where the victim was likely attempting to achieve a euphoric or psychotropic effect. All recreational use of substances for any reason is included. |
| Researched Abuse, Diversion and Addiction-Related Surveillance | Use to get high; use in combination with other drugs to get high; use as a substitute for other drugs of abuse. |
| Federation of State Medical Boards | The use of any substance(s) for non-therapeutic purposes or use of medication for purposes other than those for which it is prescribed. |
| Institute of Medicine | Same as ICD-10 and DSM-IV. |
| Tufts Health Care Institute expert panel | Any use of an illegal drug; the intentional self-administration of a medication for a nonmedical purpose such as altering one’s state of consciousness, e.g., getting high. |
| National Institute on Drug Abuse | The use of a medication without a prescription, in a way other than as prescribed, or for the experience or feelings elicited. |
| American Medical Association – Council on Scientific Affairs, Panel on Alcoholism and Drug Abuse | The use of a psychoactive substance in a manner detrimental to the individual or society but not meeting criteria for substance or drug dependence. |
| Substance Abuse and Mental Health Services Administration | Nonmedical use of a substance for psychic effect, dependence, or suicide attempt or gesture. |
| US Food and Drug Administration | The nonmedical use of a drug, repeatedly or even sporadically, for the positive psychoactive effects it produces. |
| World Health Organization | Persistent or sporadic excessive drug use inconsistent with or unrelated to acceptable medical practice. |
Among the various definitions of “abuse,” the major characteristic that frequently appears is that the substance be used for nontherapeutic purposes to obtain psychotropic (e.g., euphoric, sedative, or anxiolytic) effects. Some definitions also require that use contradicts medical advice, that the medication is not taken as prescribed, or that there is harm to the user or to others associated with the use. One definition indicates that abuse can also be used to refer to illegal use of a substance.
_
“Addiction” is primarily defined as compulsive substance use that occurs despite personal harm or negative consequences. Many definitions also state that addiction is a chronic disease that may involve impaired control and craving. Two definitions also identify addiction as involving neurobiologic dysfunction.
Addiction definitions:
| Source | Definition |
| American Academy of Pain Medicine, American pain Society, American Society of Addiction Medicine | A primary, chronic, neurobiologic disease, with genetic, psychosocial, and environmental factors influencing its development and manifestations. It is characterized by behaviors that include one or more of the following: impaired control over drug use, compulsive use, continued use despite harm, and craving. |
| American Society of Addiction Medicine | A primary, chronic disease of brain reward, motivation, memory and related circuitry. Dysfunction in these circuits leads to characteristic biological, psychological, social and spiritual manifestations. This is reflected in an individual pathologically pursuing reward and/or relief by substance use and other behaviors. Addiction is characterized by inability to consistently abstain, impairment in behavioral control, craving, diminished recognition of significant problems with one’s behaviors and interpersonal relationships, and a dysfunctional emotional response. |
| Federation of State Medical Boards | Same as AAPM, APS, ASAM, 2001. |
| Institute of Medicine | Same as ICD-10 and DSM-IV. |
| Tufts Health Care Institute expert panel | Same as AAPM, APS, ASAM, 2001. |
| National Center on Addiction and Substance Abuse at Columbia University | Same as ICD-10 and DSM-IV-TR. |
| National Institute on Drug Abuse | A chronic, relapsing disease characterized by compulsive drug seeking and use despite serious adverse consequences, and by long-lasting changes in the brain. |
| American Medical Association – Council on Scientific Affairs, Panel on Alcoholism and Drug Abuse | A chronic disorder characterized by the compulsive use of a substance resulting in physical, psychological, or social harm to the user and continued use despite that harm. |
| US Food and Drug Administration | Same as AAPM, APS, ASAM, 2001. |
| University of Wisconsin Pain & Policy Studies Group | Refers to maladaptive pattern of behaviors and compulsive use of drugs despite harm. |
| World Health Organization | Repeated use of a psychoactive substance or substances, to the extent that the user (referred to as an addict) is periodically or chronically intoxicated, shows a compulsion to take the preferred substance (or substances), has great difficulty in voluntarily ceasing or modifying substance use, and exhibits determination to obtain psychoactive substances by almost any means. |
_
Physical and psychological dependence are defined separately by various classification systems. All definitions of “physical dependence” suggest that it is associated with withdrawal symptoms or a withdrawal syndrome and most indicate that it is a physiologic response to a drug that manifests due to rapid reduction in exposure or exposure to an antagonist. Some physical dependence definitions also include the development of tolerance to the effects of the substance.
Physical and psychological dependence definitions:
| Source | Definition – physical dependence |
| American Academy of Pain Medicine, American Pain Society, American Society of Addiction Medicine | A state of adaptation that is manifested by a drug class specific withdrawal syndrome that can be produced by abrupt cessation, rapid dose reduction, decreasing blood level of the drug, and/or administration of an antagonist. |
| Cheatle & Savage review | Same as AAPM, APS, ASAM, 2001. |
| Federation of State Medical Boards | Same as AAPM, APS, ASAM, 2001. |
| Tufts Health Care Institute expert panel | Same as AAPM, APS, ASAM, 2001. |
| National Institute of Drug Abuse | An adaptive physiological state that occurs with regular drug use and results in a withdrawal syndrome when drug use is stopped; often occurs with tolerance. Physical dependence can happen with chronic – even appropriate – use of many medications, and by itself does not constitute addiction. |
| American Medical Association – Council on Scientific Affairs, Panel on Alcoholism and Drug Abuse | A physiological state of adaptation to a drug or alcohol, usually characterized by the development of tolerance to drug effects and the emergence of a withdrawal syndrome during prolonged abstinence. |
| University of Wisconsin Pain & Policy Studies Group | The physical adaptation of the body to the presence of an opioid; it is characterized by signs of withdrawal when use of an opioid is stopped abruptly, or when an opioid antagonist is administered to an individual who was been on chronic opioid therapy. |
| World Health Organization | Tolerance and withdrawal symptoms. |
| Source | Definition – psychological dependence |
| Ballantyne & LaForge review | The psychological component of withdrawal, which comprises both unpleasant emotional effects (withdrawal anhedonia and dysphoria) and motivational effects (craving during withdrawal), the latter being partly mediated by physical withdrawal. |
| Cheatle & Savage review | A non-physiological attachment to the availability of the prescribed medication that may be a natural response to effective relief of distressing symptoms. |
| American Medical Association – Council on Scientific Affairs, Panel on Alcoholism and Drug Abuse | The emotional state of craving a drug either for its positive effect or to avoid negative effects associated with its absence. |
| University of Wisconsin Pain & Policy Studies Group | A behavioral pattern characterized by a compulsion to obtain a drug for mood altering effects. |
| World Health Organization | The experience of impaired control over drug use. |
__
Substance (drug) abuse vs. dependence vs. addiction:
Substance abuse, also known as drug abuse, is a patterned use of a drug in which the user consumes the substance in amounts or with methods which are harmful to themselves or others, and is a form of substance-related disorder According to WHO, substance abuse refers to the harmful or hazardous use of psychoactive substances, including alcohol and illicit drugs. Psychoactive substance use can lead to dependence and addiction. Substance abuse occurs when there is excessive use or misuse of a drug beyond its intended purpose or prescription. The most commonly abused substances are alcohol and prescription drugs. All use of illegal drugs is considered substance abuse. The most common reason for drug and alcohol abuse is the desire to achieve a certain feeling or sensation. Substance abuse, if not treated, often leads to dependence and/or addiction. Drug dependence on a substance develops when the brain’s neurons adapt to repeated drug exposure and only function normally in the presence of the drug. Drugs disrupt the balance of chemicals in the brain. The brain adapts by changing its natural chemical production. As it adapts, it becomes more tolerant to the substance. Over time, the brain begins to rely on the presence of the drug to function. When someone who is dependent stops taking the drug, the chemical balance is thrown off, and the person experiences symptoms of withdrawal. Dependence can be a warning sign for addiction, but it may simply be a sign of drug abuse. When the drug is withdrawn, several physiologic reactions occur. This is known as the withdrawal syndrome. In the case of illegal drugs or even medically administered drugs such as morphine, withdrawal can be very serious and the user will use the drug again to avoid the withdrawal syndrome. Dependence often leads to addiction.
Addiction of any kind is the display of compulsive behavior. Unlike dependence, addiction doesn’t affect every person who is repeatedly exposed to an addictive substance. A combination of genetic and environmental factors affects addiction risk. Like dependence, addiction is caused by physical changes in the brain. These changes affect the reward and motivation parts of the brain. They make people value the addictive substance and receive unrivaled pleasure or happiness when they consume the substance. In the case of drug and alcohol abuse, this compulsive behavior is reinforcing and rewarding to the user, in spite of the negative consequences of their behavior. A major feature of addiction is the loss of control when it comes to abstaining from the substance. Scientists have learned a great deal about the biochemical, cellular, and molecular bases of addiction; it is clear that addiction is a disease of the brain. When a person is addicted to a substance, the use of that substance targets certain cells in the brain which triggers a feeling of reward or satisfaction.
__
Psychoactive drugs are often associated with addiction or drug dependence. Dependence can be divided into two types: psychological dependence, by which a user experiences negative psychological or emotional withdrawal symptoms (e.g., depression) and physical dependence, by which a user must use a drug to avoid physically uncomfortable or even medically harmful physical withdrawal symptoms. Drugs that are both rewarding and reinforcing are addictive; these properties of a drug are mediated through activation of the mesolimbic dopamine pathway, particularly the nucleus accumbens. Not all addictive drugs are associated with physical dependence, e.g., amphetamine, and not all drugs that produce physical dependence are addictive drugs, e.g., caffeine. So it is possible for someone to be dependent on a drug but not addicted although addiction is often associated with dependence.
___
Figure below shows different brain areas involved in dependence and addiction to opioids.
Different parts of the brain are responsible for the addiction and dependence to heroin and opiates although significant overlap exists. Figure above shows the areas in the brain underlying the addiction to morphine (reward pathway) and those underlying the dependence to morphine (thalamus and brainstem). Thus, it is possible to be dependent on morphine, without being addicted to morphine. (Although, if one is addicted, they are most likely dependent as well.) This is especially true for people being treated chronically with morphine, for example, pain associated with terminal cancer. They may be dependent – if the drug is stopped, they suffer a withdrawal syndrome. But, they are not compulsive users of the morphine, and they are not addicted. Finally, people treated with morphine in the hospital for pain control after surgery are unlikely to become addicted; although they may feel some of the euphoria, the analgesic and sedating effects predominate. There is no compulsive use and the prescribed use is short-lived. That’s why you can be dependent on a drug but not addicted to it. For example, when a person drinks alcohol repeatedly for several days or weeks, the brain adapts to the presence of the substance. He or she becomes dependent on alcohol and relies on it to feel normal. When that person quits drinking, withdrawal symptoms occur. When people who are dependent on alcohol stop drinking, they will usually overcome withdrawal after seven days. Some people are unable to quit drinking because they have a disease called alcohol addiction that makes it difficult for them to stay sober. Tolerance is another phenomenon that’s closely associated with dependence. As people become more dependent on a drug, their tolerance tends to increase. High tolerance and dependency on a substance are warning signs for addiction, but they are not the sole indicators of addiction.
_____
In 1987, the authors of the Diagnostic and Statistical Manual (DSM) — the “bible” that lists official psychiatric diagnoses and their attributes — designated two acceptable substance-related diagnoses. They were “substance abuse” for short-term but potentially dangerous problems (e.g. college binge drinking), and “substance dependence” for the chronic, relapsing condition we typically call addiction. Unfortunately, both of these terms turned out to be inaccurate and actively harmful: This is why, in 2013, they were dropped from DSM-5 and replaced with a spectrum category called “substance use disorder,” which runs from mild to severe. In the case of opioids, the diagnosis is labeled “opioid use disorder,” and when it is “severe,” this corresponds with what most people call addiction. But the media and the public remain uninformed.
Instead, dependence is frequently used as a synonym for addiction, which causes numerous problems. Most importantly, depending on a drug to function without withdrawal symptoms is not itself pathological: This is a normal, physiological result of taking certain medications long-term. If “drug dependence” was the best way to define addiction, then people with diabetes would have “insulin addiction,” people with high blood pressure would have “antihypertensive addiction,” and everyone would have “food, water, and air addiction.” In contrast, addiction, as defined by the DSM and the National Institute on Drug Abuse, isn’t simply needing a substance. It is compulsive drug use that continues despite harm.
This definition accurately includes cocaine as addictive — even though it doesn’t involve significant physical illness during withdrawal — while accurately excluding appropriate use of medication in chronic disease. It also means that people stabilized on medications like methadone are not addicted — they don’t engage in compulsive use despite consequences — but merely dependent. (When opioids are taken in a steady, regular dose appropriate for a particular patient, that person will not be impaired and can safely drive, work, and parent). So confusing “dependence” and “addiction” spurs bias against the most effective known treatment for opioid addiction: long-term use of methadone or buprenorphine. Decades of research show that these medications dramatically reduce the risk of death, HIV infection, and recurrence of drug use. A recent review of the scientific literature (BMJ 2017) involving more than 100,000 patients found that death rates were two to three times lower for people in methadone or buprenorphine treatment, compared to people not taking medication. No other method — including abstinence-only residential rehab — has such strong support. Yet the common myth is that people taking these medications are “still addicted” and that residential treatment is a better option. Failure to understand that addiction is not dependence leads many — including family members and people with addiction themselves — to avoid lifesaving care. Remember taking drugs to treat addiction doesn’t mean you’re ‘still addicted’.
Philip Jenkins suggests that there are two issues with the term “drug abuse”. First, what constitutes a “drug” is debatable. For instance, GHB, a naturally occurring substance in the central nervous system is considered a drug, and is illegal in many countries, while nicotine is not officially considered a drug in most countries. Second, the word “abuse” implies a recognized standard of use for any substance. Drinking an occasional glass of wine is considered acceptable in most Western countries, while drinking several bottles is seen as an abuse. Strict temperance advocates, who may or may not be religiously motivated, would see drinking even one glass as an abuse. Some groups even condemn caffeine use in any quantity. Similarly, adopting the view that any (recreational) use of cannabis or substituted amphetamines constitutes drug abuse implies a decision made that the substance is harmful, even in minute quantities.
The phrase “drug abuse” also misleads. It derives from a term meaning “willful misconduct,” which basically labels addiction as a sinful choice. “Abuse” is also associated with harms to children and sexual assault: It’s not a word that belongs in medical lexicon. These may sound like academic distinctions, but they can have deadly implications. Labels affect even highly trained clinicians. One study, for example, found that doctoral and masters level therapists were significantly more likely to recommend punitive measures such as sending a court-ordered patient to jail for relapse when that person was labeled as a “substance abuser,” rather than as a “person with substance use disorder.” And research shows that harsh methods actually backfire in treating addiction.
____
Substance use disorder (SUD):
The substances involved tend to be members of the 10 classes of drug that typically cause substance-related disorders:
- Alcohol
- Antianxiety and sedative drugs
- Caffeine
- Cannabis (including marijuana and synthetic cannabinoids)
- Hallucinogens (including LSD, phencyclidine, and psilocybin)
- Inhalants (such as paint thinner and certain glues)
- Opioids (including fentanyl, morphine, and oxycodone)
- Stimulants (including amphetamines and cocaine)
- Tobacco
- Other (including anabolic steroids and other commonly abused substances)
These substances all directly activate the brain’s reward system and produce feelings of pleasure. The activation may be so strong that people intensely crave the substance. They may neglect normal activities to obtain and use the drug. Substance use disorders can develop whether or not a drug is legal, is socially acceptable, or has an accepted medical use (with or without a prescription).
The terms “addiction,” “abuse,” and “dependence” have traditionally been used in regard to people with substance use disorders. However, those terms are all too loosely and variably defined to be very useful and also are often used judgmentally. Thus, doctors now prefer to use the more comprehensive and less negative term “substance use disorder.”
Severe Substance Use Disorders (SUD) = drug addiction
____
Determining whether You’re Dependent or Addicted:
It’s easy to determine when people are dependent on a drug. If they stop taking the drug, they’ll experience noticeable withdrawal symptoms. But it isn’t always easy to determine if a person is addicted to a drug. For example, patients who receive opioids for severe cancer pain may be dependent on opioids. They’ll experience withdrawal if they suddenly stop receiving the medication. But they aren’t addicted if they aren’t compulsively seeking the medication despite obvious harms. Determining whether opioid-seeking behavior is caused by addiction or the desire for pain relief is complicated. If people aren’t experiencing noticeable consequences of prescription drug addiction, such as family problems or job loss, they probably aren’t addicted. You can determine if you’re addicted to a drug by analyzing your behaviors. If drug use is hurting your relationships, causing problems at school or work or getting you in trouble with law enforcement, you may be addicted. If you feel cravings or withdrawal when you quit a drug but you can prevent yourself from using the drug, you probably aren’t addicted.
_____
Caffeine dependence vs addiction:
Caffeine is a bitter psychoactive drug found in the beans, leaves, and fruits of plants, where it acts as a natural pesticide. It is found in a wide variety of products, including coffee, tea, soft drinks, candy, and desserts. In North America, more than 80% of adults consume caffeine daily (Lovett, 2005). Caffeine acts as a mood enhancer and provides energy. Although Health Canada lists caffeine as a safe food substance, it has at least some characteristics of dependence. People who reduce their caffeine intake often report being irritable, restless, and drowsy, as well as experiencing strong headaches, and these withdrawal symptoms may last up to a week. Most experts feel that using small amounts of caffeine during pregnancy is safe, but larger amounts of caffeine can be harmful to the fetus (Health Canada, 2014).
Within 24 hours of quitting the drug, your withdrawal symptoms begin. Initially, they’re subtle: The first thing you notice is that you feel mentally foggy, and lack alertness. Your muscles are fatigued, even when you haven’t done anything strenuous, and you suspect that you’re more irritable than usual. Over time, an unmistakable throbbing headache sets in, making it difficult to concentrate on anything. Eventually, as your body protests having the drug taken away, you might even feel dull muscle pains, nausea and other flu-like symptoms. This isn’t heroin, tobacco or even alcohol withdrawal. We’re talking about quitting caffeine, a substance consumed so widely (the FDA reports that more than 80 percent of American adults drink it daily) and in such mundane settings (say, at an office meeting or in your car) that we often forget it’s a drug—and by far the world’s most popular psychoactive one. With the publication of the 5th edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM), caffeine withdrawal was finally included as a mental disorder for the first time—even though its merits for inclusion are symptoms that regular coffee-drinkers have long known well from the times they’ve gone off it for a day or more.
Soon after you drink (or eat) something containing caffeine, it’s absorbed through the small intestine and dissolved into the bloodstream. Because the chemical is both water- and fat-soluble, it’s able to penetrate the blood-brain barrier and enter the brain. Structurally, caffeine closely resembles a molecule that’s naturally present in our brain, called adenosine (which is a byproduct of many cellular processes, including cellular respiration)—so much so, in fact, that caffeine can fit neatly into our brain cells’ receptors for adenosine, effectively blocking them off. Normally, the adenosine produced over time locks into these receptors and produces a feeling of tiredness. When caffeine molecules are blocking those receptors, they prevent this from occurring, thereby generating a sense of alertness and energy for a few hours. Additionally, some of the brain’s own natural stimulants (such as dopamine) work more effectively when the adenosine receptors are blocked, and all the surplus adenosine floating around in the brain cues the adrenal glands to secrete adrenaline, another stimulant.
For this reason, caffeine isn’t technically a stimulant on its own but a stimulant enabler: a substance that lets our natural stimulants run wild. In people who take advantage of this process on a daily basis (i.e. coffee/tea, soda or energy drink addicts), the brain’s chemistry and physical characteristics actually change over time as a result. The most notable change is that brain cells grow more adenosine receptors, which is the brain’s attempt to maintain equilibrium in the face of a constant onslaught of caffeine, with its adenosine receptors so regularly plugged (studies indicate that the brain also responds by decreasing the number of receptors for norepinephrine, a stimulant). This explains why regular coffee drinkers build up a tolerance over time—because you have more adenosine receptors, it takes more caffeine to block a significant proportion of them and achieve the desired effect.
This also explains why suddenly giving up caffeine entirely can trigger a range of withdrawal effects. The underlying chemistry is complex and not fully understood, but the principle is that your brain is used to operating in one set of conditions (with an artificially-inflated number of adenosine receptors, and a decreased number of norepinephrine receptors) that depend upon regular ingestion of caffeine. Suddenly, without the drug, the altered brain chemistry causes all sorts of problems, including the dreaded caffeine withdrawal headache.
The good news is that, compared to many drug dependences, the effects are relatively short-term. To kick the thing, you only need to get through about 7-12 days of symptoms without drinking any caffeine. During that period, your brain will naturally decrease the number of adenosine receptors on each cell, responding to the sudden lack of caffeine ingestion. If you can make it that long without a cup of tea or coffee, the levels of adenosine receptors in your brain reset to their baseline levels, and your dependence will be broken. Remember tea or coffee leads to dependence and not addiction. Nobody will steal money or destroy career or break relationship to get tea or coffee.
______
Can a person develop a Drug Addiction without ever being a Substance Abuser?
Absolutely. This happens quite often with certain prescription medications. Typically, a medication with an appreciable potential for addiction will be improperly prescribed – an opioid painkiller might be given for long-term chronic pain, for instance, when in reality, guidelines dictate that prescription opioids should only be given for acute, short-term pain. All drugs that carry a potential for addiction affect a person’s brain in a similar fashion, by disrupting its reward pathways. The use of the substance triggers an over-production of dopamine, the neurotransmitter responsible for feelings of pleasure. This flood of dopamine “trains” the person that the activity—the use of the drug—is a desirable activity that should be repeated. Over time, the brain stops producing dopamine naturally, and will only do so when the substance is used. The symptoms occur because without the drug, the person is incapable of feeling “good” or “normal”. The person is compelled by these feelings to do something…anything…to get the drug again. This can be the result of purposeful substance abuse, but it can also happen with certain medications, even if they are taken exactly as prescribed. Those same biochemical changes occur simply because of the way that a person’s brain reacts to the long-term use of the mediation.
______
Tolerance:
Tolerance is defined as a person’s diminished response to a drug that is the result of repeated use. People can develop tolerance to both illicit drugs and prescription medications. Tolerance is a physical effect of repeated use of a drug, not necessarily a sign of addiction. For example, patients with chronic pain frequently develop tolerance to some effects of prescription pain medications without developing an addiction to them.
There are 3 main types of tolerance:
- Acute, or short-term, tolerance is caused by repeated exposure to a drug over a relatively short period of time. Cocaine abuse often results in acute tolerance. Experiments have shown that after a first dose of cocaine, test subjects experience a euphoric high and an increase in heart rate and blood pressure. However, despite nearly doubling the levels of drug in the blood, a second dose of cocaine 40 minutes later does not result in a dose-dependent increase in the “positive” effects of the drug, including a further increase in heart rate or blood pressure.
- Chronic, or long-term, tolerance develops when an individual’s body adapts to constant exposure to a drug over weeks or months. People who regularly abuse prescription opioids build up chronic tolerance to the euphoric effects of these medications, leading many of them to increase the dosage taken or switch to more potent ways of taking these drugs, such as snorting or injecting.
- Learned tolerance may result from frequent exposure to certain drugs. For example, people who abuse alcohol for months or years often do not appear intoxicated to others. Experimental studies have shown that drinkers can compensate for the effects of alcohol on their coordination when they practice a task repeatedly while under the influence. However, this tolerance disappears if the task is altered.
Finally, most drugs have more than one effect, and tolerance does not necessarily develop equally to all effects. Abusers of illicit and prescription opioids, such as heroin or oxycodone, quickly develop tolerance to the euphoric high these drugs produce but not to the dangerous side effect of respiratory depression (slowed breathing rate). Opioid abusers who take large doses of these drugs to overcome tolerance and get high are frequently hospitalized—or even die—because they stop breathing.
_____
Withdrawal:
Withdrawal is the body’s reaction to abstaining from a substance upon which a person has developed a dependence syndrome. When dependence has developed, cessation of substance-use produces an unpleasant state, which promotes continued drug use through negative reinforcement; i.e., the drug is used to escape or avoid re-entering the associated withdrawal state. The withdrawal state may include physical-somatic symptoms (physical dependence), emotional-motivational symptoms (psychological dependence), or both. Chemical and hormonal imbalances may arise if the substance is not re-introduced. Psychological stress may also result if the substance is not re-introduced. Withdrawal symptoms can be severe. Patients experiencing withdrawal from these substances, especially prescription and illicit opioids, should seek immediate medical attention. Infants also suffer from substance withdrawal, known as Neonatal Abstinence Syndrome (NAS), which can have severe and life-threatening effects. Addiction to drugs and alcohol in expectant mothers not only causes NAS, but also an array of other issues which can continually affect the infant throughout his/her lifetime.
______
Relapse:
Relapse occurs when someone returns to substance use after a period of abstinence. It is a common setback among people recovering from addiction. In fact, many individuals in recovery experience more than one relapse in their lives. According to the National Institute on Drug Abuse, between 40 and 60 percent of people recovering from drug addiction relapse. Staying sober takes time, practice and commitment, and a relapse does not mean treatment has failed. A number of factors can increase the likelihood of relapse, including succumbing to triggers or failing to seek aftercare services upon completion of addiction treatment. In evaluating this phenomenon, stress is a key factor that influences relapse. The mind of the addicted person is affected in such a way that their coping mechanisms for stress are inadequate to prevent relapse. Hopefully, with better understanding of the causes for relapse, treatment will be more successful and the relapse rate will drop.
______
______
Psychoactive and recreational drugs:
_
Psychoactive drug:
A psychoactive drug is a chemical substance that changes brain function and results in alterations in perception, mood, consciousness, cognition, or behavior. These substances may be used medically; recreationally to purposefully improve performance or alter one’s consciousness; as entheogens for ritual, spiritual, or shamanic purposes; or for research. Some categories of psychoactive drugs, which have therapeutic value, are prescribed by physicians and other healthcare practitioners. Examples include anesthetics, analgesics, anticonvulsant and antiparkinsonian drugs as well as medications used to treat neuropsychiatric disorders, such as antidepressants, anxiolytics, antipsychotics, and stimulant medications. Some psychoactive substances may be used in the detoxification and rehabilitation programs for persons dependent on or addicted to other psychoactive drugs.
Psychoactive substances often bring about subjective (although these may be objectively observed) changes in consciousness and mood that the user may find rewarding and pleasant (e.g., euphoria or a sense of relaxation) or advantageous (e.g. increased alertness) and are thus reinforcing. Substances which are both rewarding and positively reinforcing have the potential to induce a state of addiction – compulsive drug use despite negative consequences. In addition, sustained use of some substances may produce physical or psychological dependence or both, associated with somatic or psychological-emotional withdrawal states respectively. Conversely, certain psychoactive drugs may be so unpleasant that the person will never use the substance again. This is especially true of certain deliriants (e.g. Jimson weed), powerful dissociatives (e.g. Salvia divinorum), and classic psychedelics (e.g. LSD, psilocybin), in the form of a “bad trip”.
In some cases the effects of psychoactive drugs mimic other naturally occurring states of consciousness. For instance, sleeping pills are prescribed to create drowsiness, and benzodiazepines are prescribed to create a state of relaxation. In other cases psychoactive drugs are taken for recreational purposes with the goal of creating states of consciousness that are pleasurable or that help us escape our normal consciousness. The use of psychoactive drugs, especially those that are used illegally, has the potential to create very negative side effects. This does not mean that all drugs are dangerous, but rather that all drugs can be dangerous, particularly if they are used regularly over long periods of time. Psychoactive drugs create negative effects not so much through their initial use but through the continued use, accompanied by increasing doses, that ultimately may lead to drug abuse.
It is a common belief that addiction is an overwhelming, irresistibly powerful force, and that withdrawal from drugs is always an unbearably painful experience. But the reality is more complicated and in many cases less extreme. For one, even drugs that we do not generally think of as being addictive, such as caffeine, nicotine, and alcohol, can be very difficult to quit using, at least for some people. On the other hand, drugs that are normally associated with addiction, including amphetamines, cocaine, and heroin, do not immediately create addiction in their users. Even for a highly addictive drug like cocaine, only about 15% of users become addicted (Robinson & Berridge, 2003; Wagner & Anthony, 2002). Furthermore, the rate of addiction is lower for those who are taking drugs for medical reasons than for those who are using drugs recreationally. Patients who have become physically dependent on morphine administered during the course of medical treatment for a painful injury or disease are able to be rapidly weaned off the drug afterward, without becoming addicts. Robins, Davis, and Goodwin (1974) found that the majority of soldiers who had become addicted to morphine while overseas were quickly able to stop using after returning home.
This does not mean that using recreational drugs is not dangerous. For people who do become addicted to drugs, the success rate of recovery is low. These drugs are generally illegal and carry with them potential criminal consequences if one is caught in possession of them and arrested. Drugs that are smoked may produce throat and lung cancers and other problems. Snorting (“sniffing”) drugs can lead to a loss of the sense of smell, nosebleeds, difficulty in swallowing, hoarseness, and chronic runny nose. Injecting drugs intravenously carries with it the risk of contracting infections such as hepatitis and HIV. Furthermore, the quality and contents of illegal drugs are generally unknown, and the doses can vary substantially from purchase to purchase. The drugs may also contain toxic chemicals.
_
An assortment of psychoactive drugs—street drugs and medications:
- cocaine
- crack cocaine
- methylphenidate (MPH)
- ephedrine
- MDMA (ecstasy)
- Peyote (mescaline)
- LSD blotter
- psilocybin mushroom (Psilocybe cubensis)
- Salvia divinorum
- diphenhydramine
- Amanita muscaria mushroom
- Tylenol 3 (contains codeine)
- codeine with muscle relaxant
- pipe tobacco
- bupropion
- cannabis
- hashish
_
Are Psychoactive Drugs and Psychotropic Drugs the Same?
The terms psychoactive drugs and psychotropic drugs are frequently used to mean the same thing. Some may consider psychotropic drugs to be prescription medications, rather than illegal or illicit drugs. For example, psychotropic drugs are frequently prescribed to treat certain mental health conditions. Depression, anxiety and other disorders are some reasons why people take these medications.
_
What are recreational drugs?
“Recreational drugs” is a loose term that refers to legal and illegal drugs that are used without medical supervision. Recreational drug use is the use of a psychoactive drug to induce an altered state of consciousness for pleasure, by modifying the perceptions, feelings, and emotions of the user. “Recreational drugs” is a misleading term. It suggests that drugs can be fun and safe. Nothing could be further from the truth. All drugs are nightmarish and dangerous. They alter our perception of reality and diminish our ability to reason, both of which endanger us. Drugs create psychological and physical dependence, both of which enslave us. Recreation is a legitimate need that requires legitimate activities, such as hobbies, exercise, conversation, music, dance, art, and literature. The use of substances for utilitarian purposes – such as the relief of fatigue or insomnia, or the control of appetite – is not understood as recreational.
One of the emerging trends in the last 20 years was the rising use of the so-called club drugs. Club drugs also called rave drugs, or party drugs tend to be used by teenagers and young adults at bars, nightclubs, concerts, and parties. Club drugs include GHB, flunitrazepam, ketamine, MDMA (Ecstasy), Methamphetamine, and LSD.
_
Characteristics of Recreational Drug Use:
It’s important to know if a person has jumped from recreational drug user to an addict. These are the characteristics of someone who is recreationally using;
- They use occasionally when it suits their needs but can say no when drugs are offered.
- They understand the potential problems that can arise from taking drugs recreationally.
- A recreational drug user will have good healthy relationships with those who wouldn’t normally use drugs.
- A recreational drug user doesn’t take drugs to numb themselves or attempt to be a better version of themselves.
- Drug use is not something that consumes their thoughts.
- When using drugs recreationally, they are conscious about the amount of money they’re spending.
A 2017 study found that recreational users viewed themselves as different from people who are habitual users. The recreational drug users used drugs because they valued the benefits that specific drugs seemed to offer while considering the risks to be manageable, worthwhile and/or minimal. Two important drivers lead people to take up recreational drug use: social networking and performance enhancement.
_
Characteristics of Recreational Drug use becoming an Addiction:
Recreationally using the drugs can lead to addiction. This is what the characteristics of a drug addict will look like:
- The recreational drug user may start to find any party they can attend as an excuse to “use drugs recreationally.” This will help them fall under the radar from the dependency they’re building.
- They may believe they are a better person when they’re using their drug of choice.
- They have a hard time saying no if drugs are offered to them.
- They build relationships with other users and are less interested in their healthy relationships.
- Their behavior will change and they’re more prone to arguing with people that they are normally harmonious with.
- They may start to choose recreational drug use over the things they used to care about. This can be masked as “choosing the party.”
- They begin to fixate on when and how they can become high again.
_
Psychoactive drugs affect consciousness by influencing how neurotransmitters operate at the synapses of the central nervous system (CNS). Some psychoactive drugs are agonists, which mimic the operation of a neurotransmitter; some are antagonists, which block the action of a neurotransmitter; and some work by blocking the reuptake of neurotransmitters at the synapse.
_
Depending on its method of action, a psychoactive substance may block the receptors on the post-synaptic neuron (dendrite), or block reuptake or affect neurotransmitter synthesis in the pre-synaptic neuron (axon). Stimulants, including caffeine, nicotine, cocaine and amphetamines, increase neural activity by blocking the reuptake of dopamine, norepinephrine, and serotonin in the CNS. Depressants, including, alcohol, barbiturates, and benzodiazepines, decrease consciousness by increasing the production of the neurotransmitter GABA and decreasing the production of the neurotransmitter acetylcholine. Opioids, including codeine, opium, morphine, and heroin, produce euphoria and analgesia by increasing activity in opioid receptor neurons.
Psychoactive drugs operate by temporarily affecting a person’s neurochemistry, which in turn causes changes in a person’s mood, cognition, perception and behavior. There are many ways in which psychoactive drugs can affect the brain. Each drug has a specific action on one or more neurotransmitter or neuroreceptor in the brain.
Drugs that increase activity in particular neurotransmitter systems are called agonists. They act by increasing the synthesis of one or more neurotransmitters, by reducing its reuptake from the synapses, or by mimicking the action by binding directly to the postsynaptic receptor. Drugs that reduce neurotransmitter activity are called antagonists, and operate by interfering with synthesis or blocking postsynaptic receptors so that neurotransmitters cannot bind to them.
Exposure to a psychoactive substance can cause changes in the structure and functioning of neurons, as the nervous system tries to re-establish the homeostasis disrupted by the presence of the drug. Exposure to antagonists for a particular neurotransmitter can increase the number of receptors for that neurotransmitter or the receptors themselves may become more responsive to neurotransmitters; this is called sensitization. Conversely, overstimulation of receptors for a particular neurotransmitter may cause a decrease in both number and sensitivity of these receptors, a process called desensitization or tolerance. Sensitization and desensitization are more likely to occur with long-term exposure, although they may occur after only a single exposure. These processes are thought to play a role in drug dependence and addiction.
_
Psychoactive drugs classification:
Drugs are classified chemically according to how they affect the brain and the body. Common classifications include stimulants, depressants, hallucinogens, and opioids. Additionally, the DEA legally classifies drugs into schedules (I, II, III, IV, and V) based on their medical use and potential for abuse and dependence.
_
Chemical Classifications of psychoactive drugs:
Diverse Chemical Substances cause Addiction:
- Opiates (morphine, heroin, oxycontin, vicodin)
- Cocaine
- Amphetamine and like drugs (methamphetamine, methylphenidate)
- MDMA (ecstasy)
- PCP (phencyclidine or angel dust; also ketamine)
- Marijuana (cannabinoids)
- Tobacco (nicotine)
- Alcohol (ethanol)
- Sedative/hypnotics (barbiturates, benzodiazepines)
Chemical Structures of some Drugs of Abuse:
Most drugs in the past were made from plants. These plants were grown and then processed into coca paste, opium, marijuana and other drugs. After further processing, these crude products yielded drugs like cocaine and heroin. Now in the 21st century, drugs such as Speed, Ecstasy, LSD and so forth are being made from chemicals.
_
Each of the psychoactive drug that act on the central nervous system and alter your feelings and perceptions can be classified according to their physical and psychological effects. The different drug types include the following:
_
As you can see in Table below, “Psychoactive Drugs by Class,” the four primary classes of psychoactive drugs are stimulants, depressants, opioids, and hallucinogens.
Psychoactive Drugs by Class:
| Mechanism | Symptoms | Drug | Dangers and Side Effects | Psychological Dependence | Physical Dependence | Addiction Potential |
| Stimulants:
Stimulants block the reuptake of dopamine, norepinephrine, and serotonin in the synapses of the CNS. |
Enhanced mood and increased energy | Caffeine | May create dependence | Low | Low | Low |
| Nicotine | Has major negative health effects if smoked or chewed | High | High | High | ||
| Cocaine | Decreased appetite, headache | Low | Low | Moderate | ||
| Amphetamines | Possible dependence, accompanied by severe “crash” with depression as drug effects wear off, particularly if smoked or injected | Moderate | Low | Moderate to High | ||
| Depressants:
Depressants change consciousness by increasing the production of the neurotransmitter GABA and decreasing the production of the neurotransmitter acetylcholine, usually at the level of the thalamus and the reticular formation. |
Calming effects, sleep, pain relief, slowed heart rate and respiration | Alcohol | Impaired judgment, loss of coordination, dizziness, nausea, and eventually a loss of consciousness | Moderate | Moderate | Moderate |
| Barbiturates and benzodiazepines | Sluggishness, slowed speech, drowsiness, in severe cases, coma or death | Moderate | Moderate | Moderate | ||
| Toxic inhalants | Brain damage and death | High | High | High | ||
| Opioids:
The chemical makeup of opioids is similar to the endorphins, the neurotransmitters that serve as the body’s “natural pain reducers.” |
Slowing of many body functions, constipation, respiratory and cardiac depression, and the rapid development of tolerance | Opium | Side effects include nausea, vomiting, tolerance, and addiction. | Moderate | Moderate | Moderate |
| Morphine | Restlessness, irritability, headache and body aches, tremors, nausea, vomiting, and severe abdominal pain | High | Moderate | Moderate | ||
| Heroin | All side effects of morphine but about twice as addictive as morphine | High | Moderate | High | ||
| Hallucinogens:
The chemical compositions of the hallucinogens are similar to the neurotransmitters serotonin and epinephrine, and they act primarily by mimicking them. |
Altered consciousness; hallucinations | Marijuana | Mild intoxication; enhanced perception | Low | Low | Low |
| LSD, mescaline, PCP, and peyote | Hallucinations; enhanced perception | Low | Low | Low |
____
Legal Classifications of Psychoactive Drugs in the U.S.
The Controlled Substances Act established five classifications, or schedules, for drugs regulated by law. According to the DEA, these classifications are broken down based on their potential for abuse and if they have a legitimate medical use:
- Schedule I include the drugs that have a high potential for abuse, that have no currently accepted medical use in treatment in the United States, and that there is a lack of accepted safety for use of the drug under medical supervision. Drugs such as cannabis, ecstasy, GHB, heroin, LSD, mescaline, and methaqualone are included in Schedule I.
- Schedule II includes drugs that have a high potential for abuse, have currently accepted medical use in treatment in the United States or currently accepted medical use with severe restrictions, and that the abuse of may lead to severe psychological or physical dependence. Drugs such as amphetamine, cocaine, fentanyl, hydromorphone oxycodone, methadone and hydrocodone are included in Schedule II.
- Schedule III includes drugs that have a potential for abuse less than the drugs or other substances in schedules I and II, have a currently accepted medical use in treatment in the United States, and that the abuse of may lead to moderate or low physical dependence or high psychological dependence. Drugs such as anabolic steroids, buprenorphine, and ketamine are included in Schedule III.
- Schedule IV includes drugs that have a low potential for abuse relative to the drugs or other substances in schedule III, have a currently accepted medical use in treatment in the United States, and that the abuse of may lead to limited physical dependence or psychological dependence relative to the drugs or other substances in schedule III. Drugs such as benzodiazepines, modafinil, and tramadol are included in Schedule IV.
- Schedule V includes drugs that have a low potential for abuse relative to the drugs or other substances in schedule IV, have a currently accepted medical use in treatment in the United States, and that the abuse of may lead to limited physical dependence or psychological dependence relative to the drugs or other substances in schedule IV. Drugs such as diphenoxylate (in combination with atropine), lacosamide, and pregabalin are included in Schedule V.
_____
Route of administration:
Psychoactive drugs are administered via oral ingestion as a tablet, capsule, powder, liquid, and beverage; via injection by subcutaneous, intramuscular, and intravenous route; via rectum by suppository and enema; and via inhalation by smoking, vaporization and insufflation (“snorting”). The efficiency of each method of administration varies from drug to drug. The psychiatric drugs fluoxetine, quetiapine, and lorazepam are ingested orally in tablet or capsule form. Alcohol and caffeine are ingested in beverage form; nicotine and cannabis are smoked or vaped; peyote and psilocybin mushrooms are ingested in botanical form or dried; and crystalline drugs such as cocaine and methamphetamine are usually insufflated (inhaled or “snorted”).
When you take a drug orally, many things can happen to it. It may be broken down in the stomach or in the intestine, or it may just precipitate and never be absorbed. Both the gastrointestinal acidity and the intestinal flora can play a role in drug stability. Drugs that traverse the stomach and intestine intact funnel into the portal vein that flows into the liver, which acts like a filter, either removing or breaking down toxins and drugs that get absorbed. Drug molecules that escape the liver enter the systemic circulation and may reach their site of action i.e. the brain. Most drugs are broken down in the liver.
____
Determinants of effects:
The theory of dosage, set, and setting is a useful model in dealing with the effects of psychoactive substances, especially in a controlled therapeutic setting as well as in recreational use. Dr. Timothy Leary, based on his own experiences and systematic observations on psychedelics, developed this theory along with his colleagues Ralph Metzner, and Richard Alpert (Ram Dass) in the 1960s.
Dosage:
The first factor, dosage, has been a truism since ancient times, or at least since Paracelsus who said, “Dose makes the poison.” Some compounds are beneficial or pleasurable when consumed in small amounts, but harmful, deadly, or evoke discomfort in higher doses.
Different Severities of Dependency:
In general, the longer people consume an addictive substance, the more dependent they’ll become. The method of abuse can also increase the severity of dependency. For example, injecting or snorting a drug may make a person more dependent than swallowing the same drug. Injecting or snorting a drug also decreases the time it takes to become addicted to the drug because the brain feels the full dose of the drug suddenly instead of gradually feeling a smaller dose over time.
Set:
Set means the unique biological, neurological, psychological and experiential qualities of the user. Set creates a personal vulnerability and selective responsivity to substances. Biologically, a person’s genetics (inherited DNA), as well as current brain neurochemistry or entire body physiology, can significantly influence the action of a psychoactive drug. The same quantity of drug may have orders of magnitude, more or less, in its impact. Moreover, repetitive use of a substance can produce central nervous system hyper- or hypo-reactivity to that agent. Psychologically and experientially, a history of trauma (from abuse, neglect, violence and torture, forced immigration, and natural disaster) induces great brain (and emotional) reactivity to many things, including drugs. Temperamental aspects of a personality—particularly a tendency to externalize, to hold others responsible for whatever, as well as dimensions of personality, such as passive or active, rebellious or conforming, the capacity to experience feelings or not, and accepting or denying reality—all influence the action of a substance.
Setting:
The third aspect is setting, which pertains to the surroundings, the place, and the time in which the experiences transpire. A historical story reveals what setting means. At the height of the Vietnam War, the Department of Defense came to realize that 20 percent of the soldiers were frequent users of the potent heroin they had easy access to. The DoD feared that upon their return they would continue their use, join the already too large population in the U.S. of those addicted to heroin. Norman Zinberg and his colleague Lee Robins were dispatched to Vietnam to assess the problem and try to predict the future for these soldiers. They were proven to be correct when they forecast a no greater rate of heroin use or dependence than existed in those who did not go to war. It was the soldiers’ setting—battling in a fierce, deadly, unpredictable guerrilla war in a country that did not want them and with little support from Americans back home, with ready access to cheap, powerful heroin to make the unbearable bearable—that led to their high rates of use. Today’s analogue, if only partial, is Iraq and Afghanistan, where studies show that as many of 30 percent of combat veterans return with PTSD, depression or traumatic brain injury (TBI). Their setting is inducing high rates of alcoholism and drug dependence.
This theory clearly states that the effects are equally the result of chemical, pharmacological, psychological, and physical influences. The model that Timothy Leary proposed applied to the psychedelics, although it also applies to other psychoactive drugs.
_____
_____
Responsible drug use:
The concept of “responsible drug use” is that a person can use drugs recreationally or otherwise with reduced or eliminated risk of negatively affecting other aspects of one’s life or other people’s lives. Advocates of this philosophy point to the many well-known artists and intellectuals who have used drugs, experimentally or otherwise, with few detrimental effects on their lives. Responsible drug use becomes problematic only when the use of the substance significantly interferes with the user’s daily life.
Responsible drug use advocates that users should not take drugs at the same time as activities such as driving, swimming, operating machinery, or other activities that are unsafe without a sober state. Responsible drug use is emphasized as a primary prevention technique in harm-reduction drug policies. Another issue is that the illegality of drugs in itself also causes social and economic consequences for those using them—the drugs may be “cut” with adulterants and the purity varies wildly, making overdoses more likely—and legalization of drug production and distribution would reduce these and other dangers of illegal drug use.
The fact that some people can use a drug responsibly and even beneficially does not imply that it is safe. We all know people who drink and take no harm from it, and we all know people whose lives have been wrecked by alcohol. However just because some people do not work to minimize risks and use a drug dangerously or to their own detriment does not mean that is true of everyone who tries it.
_____
_____
Commonly used illicit drugs:
Commonly used illegal drugs include marijuana, heroin, cocaine, amphetamines and methamphetamines and club drugs.
Here is the list of some of the most addictive types of illegal drugs:
- Marijuana
Although marijuana is the most benign types of drugs on this list, it certainly can cause changes in the brain to the point of addiction. Marijuana isn’t seen as being physically or chemically addictive, but many health experts agree that it can be psychologically addictive. Roughly 10 percent of people who use marijuana will become dependent on it, according to the National Institute on Drug Abuse. As the most commonly used illicit substance, marijuana is now legal in some states in the U.S., and it’s available in many others via prescription. Marijuana addiction can lead to mild withdrawal symptoms, such as irritability, sleep difficulties, restlessness, physical discomfort and decreased appetite. Long-term use of marijuana has been found to decrease the volume of grey matter in the brain, while a longitudinal study in New Zealand found that teens who started and continued using the drug regularly lost an average of 8 IQ points by mid-adulthood.
- Ecstasy
Ecstasy is the most popular type of club drug. Ecstasy, or the “love drug” was commonly used in the 1980s and is still part of the club scene. Users feel happy, loving, alert and focused, yet very relaxed when under its influence. Some users can also do without sleep for between 24-72 hours at a time. Ecstasy, also known as “E” or “X,” is a very seductive type of addiction, and many users have difficulty admitting that they would have trouble quitting it once they start using. Ecstasy’s active ingredient is MDMA (methylenedioxymethamphetamine), which is now popular in its pure form, known as “Molly.” Ecstasy and Molly and are commonly available as a capsule, tablet or powder. Ecstasy’s side effects include muscle cramps, blurred vision, increased heart rate, nausea, chills and hallucinations. Someone who has become addicted and experiences withdrawal symptoms may experience panic attacks, insomnia, psychosis, depression and paranoia. MDMA-related deaths do happen occasionally, but they rarely follow an overdose on ecstasy. Instead, moderate uses of the drug cause some users to suffer a fatal heat stroke, and the substance can amplify existing heart conditions for some users to the point of death.
- Methadone
Methadone is an opioid that is commonly prescribed to treat heroin or morphine addicts, as this pain reliever helps the user come down from those harder substances. Even though the risk of addiction is low when used as directed by a doctor in a clinical setting, many recreational users have been drawn to the substance and subsequently become addicted. Methadone generally comes in the form of tablets, powder and liquid. It shares some of the same effects as morphine, but is not quite as strong or addictive as that opiate. Methadone can slow or stop a user’s breathing, especially when someone first starts using the drug. Other short-term effects of methadone include itchiness, severe sweating, constipation, nausea, sexual dysfunction and even death. Long-term use can lead to lung and respiration problems. U.S. government statistics show that, as of 2015, methadone is the fastest-growing cause of narcotic-related deaths, possibly since it’s far less expensive than other prescription painkillers.
- Amphetamines
Not to be confused with methamphetamine, amphetamines (or “uppers”) create a rapid tolerance and intense cravings in users. They make users feel confident, energetic and euphoric, and they may be attractive for their appetite-curbing traits. Amphetamines are usually taken orally, but can be snorted or injected. This substance is featured in some legal drugs, although several street forms are also available. Amphetamine’s side effects include anxiety, nervousness, dry mouth, decreased appetite, headaches and weight loss. Long-term use of amphetamine can lead to panic attacks, psychotic episodes, acne or skin conditions, and convulsions. In 2012, more than 116,000 people were admitted into a rehab program in the U.S. for addiction to some form of amphetamine addiction.
- Cocaine
Cocaine, like many other drugs on this list, affects the amount of dopamine in a person’s brain and causes intense cravings for more of the substance. Snorting cocaine powder causes a rapid, intense high and builds up a tolerance quickly. Coming down from a cocaine high can cause depression, edginess and irregular sleeping and eating patterns. Cocaine use also carries the risk of heart attack, stroke, seizure and respiratory failure. Long-term use can lead to psychosis and hallucinations. Every month, somewhere between 1 million and 2 million Americans typically use cocaine. Annual cocaine deaths in the U.S. have hovered around 5,000 since 2011, according to the National Institute on Drug Abuse.
- Bath Salts
Bath salts are a synthetic type of drug that create a feeling of euphoria and are taken by injecting, snorting or smoking the substance. The effects can last for several hours, but users often re-dose and may stay up for several days. One of the main substances in bath salts, MDPV (methylenedioxypyrovalerone), was found to be nearly as addictive as methamphetamine. Bath salts are considered a cheap alternative to cocaine, ecstasy or methamphetamine. Bath salts often cause insomnia, agitation, hallucinations and even violent behavior upon first use. Long-term use can lead to kidney and liver damage, as well as a breakdown of skeletal muscle tissue.
- Methamphetamine
Methamphetamine affects the dopamine and norepinephrine levels in the brain, making the user alert and hyperactive. Meth releases massive amounts of dopamine into the brain and suppresses norepinephrine production. Users develop a tolerance quickly and develop cravings for more of the substance. Methamphetamine can be smoked, snorted or taken orally. It can also be dissolved in water or alcohol and then injected. Crystal meth is one of the most common forms of the drug, and is often considered a “club drug.” Meth usually suppresses the user’s appetite, and the high doesn’t wear off for 6 to 8 hours. Long-term meth use can cause memory loss, psychotic behavior, heart and brain damage, dangerous weight loss, tooth decay and gum recession.
- Heroin
Heroin users instantly get a “rush,” and after a time, cannot experience any good feelings without using it. Addicts get intense cravings while going through withdrawal. Heroin is a semi-synthetic substance that is extracted from the opium plant, making it a member of the opioid class of drugs. Heroin is generally taken via needle injection, although pure forms of the drug can be smoked or snorted. Many heroin users got their start by being prescribed a legal opioid painkiller and then craving a similar, likely stronger effect once the prescription ran out. Opioids such as heroin are responsible for nearly 20 percent of all admissions for drug and alcohol treatment in the U.S. In 2013, more than 8,000 Americans died from a heroin-related overdose. And in 2014, there were more than 10,000 such deaths.
- Crack Cocaine
Crack, also known as crack rocks, is the purest form of cocaine available and is smoked through a glass pipe. It causes the user’s brain to release large amounts of dopamine, which results in intense feelings of pleasure and a burst of energy for about 10 minutes. Some users become addicted to crack the first time they try it. Crack cocaine and powder cocaine have similar chemical compositions and effects, but crack causes a stronger, faster high, albeit one that lasts for a shorter amount of time.
______
Lacing:
Lacing is the act of adding one or more substances to another. Some street drugs are commonly laced with other chemicals for various reasons, but it is most commonly done so as to bulk up the original product or to sell other, cheaper drugs in the place of something more expensive. Individuals sometimes lace their own drugs with another substance to combine or alter the physiological or psychoactive effects.
Drugs may be sold to end users who are unaware they have been laced or are unaware what was used to lace them. At various points in the supply chain, in order to maximize profitability, many drugs are adulterated with cutting agents. A cutting agent is a chemical used to “cut” (dilute or adulterate) recreational drugs with something less expensive than the drug itself. The classical model of drug cutting refers to the way that illicit drugs were diluted at each stage of the chain of distribution. Substances with similar physical and/or chemical properties can be used so the end product most closely resembles what it is purported to be. Inert substances with similar physical properties can be used to increase weight without changing the look and feel. Less expensive or easier to obtain compounds with similar chemical properties may be used to lace heavily adulterated drugs while still maintaining some psychoactive potency.
Drugs may also be laced with the end user being made aware of the lacing. In this case, rather than as an adulteration, the lacing is intended to make the product more desirable. Sometimes less potent, often less expensive drugs, are laced with a small amount of a more potent, often more expensive drug. This may be used to facilitate the ingestion of drugs or to allow the simultaneous ingestion of multiple drugs. Cigarettes laced with PCP allow users to take in the liquid PCP through smoking and some multi drug users report intentionally buying marijuana laced with methamphetamine.
_
Commonly laced drugs:
| Drug 1 | Drug 2 | Drug 3 | Poly drug name |
| Alcohol | Barbiturates | Geronimo | |
| Alcohol | Chloral hydrate | Mickey Finn | |
| Cannabis | Embalming fluid | Illy | |
| Cannabis | Formaldehyde | Clicker, dank | |
| Cannabis | PCP | Embalming fluid (optional) | Love boat (less known: fry sticks) |
| Crack-cocaine | Benzocaine | Fire | |
| Crack-cocaine | Procaine | Double rock | |
| LSD | Strychnine | Back breakers | |
| Heroin | Motion sickness medication | Polo | |
| Heroin | Scopolamineor strychnine | Spike | |
| PCP | Gasoline | Octane |
Cocaine has been cut with various substances ranging from flour and powdered milk to ground drywall and other common, easily obtainable substances. Most hard drugs are adulterated to some degree. Some street drugs can be as low as 10–15% of the active drug, with the other (85–90%) not necessarily being the cutting agent. In fact, a heroin sample of only 20% purity may have no cutting agents in it at all. The other 80% may be impurities produced in the manufacturing process and substances created as byproducts of this process and/or degradation of the drug if improperly stored.
_
Combining drugs:
Speedball:
Speedball (or powerball) is a mixture of cocaine (a stimulant) with heroin or morphine (an opioid), taken intravenously or by insufflation. Speedball is a dangerous mixture, often more so than the sum of the parts due to drug synergy. The original speedball used cocaine hydrochloride mixed with morphine sulfate, as opposed to heroin. Speedball may also use pharmaceutical opioids, benzodiazepines, or barbiturates along with stimulants. However, since opioids and sedative-hypnotics have different objective and subjective effects, stimulant-opioid mixtures are known by the slang term “set up”.
Combining drugs is dangerous because their combined effects on the CNS can increase dramatically and can lead to accidental or even deliberate overdoses. For instance, ingesting alcohol or benzodiazepines along with the usual dose of heroin is a frequent cause of overdose deaths in opiate addicts, and combining alcohol and cocaine can have a dangerous impact on the cardiovascular system.
______
______
Drug paraphernalia:
“Drug paraphernalia” is a term, to denote any equipment, product or accessory that is intended or modified for making, using, or concealing drugs, typically for recreational purposes. Drugs such as marijuana, cocaine, heroin, and methamphetamine are related to a wide range of paraphernalia. Paraphernalia generally falls into two categories: user-specific products and dealer-specific products.
User-specific products include glass hashish pipes, crack cocaine pipes, smoking masks, hashish bongs, cocaine freebase kits, syringes, roach clips for holding the burning end of a marijuana joint. Some stores sell items for growing hydroponic marijuana, such as guidebooks, fertilizer, and fluorescent grow-lights. The term “paraphernalia” also refers to items such as hollowed-out cosmetic cases or fake pagers when used to conceal illegal drugs, or products purported to cleanse an individual’s system of drug residues to increase the individual’s chance of passing a urine analysis for drug use.
Dealer-specific products are used by the drug sellers or traffickers for preparing drugs for distribution. Items such as digital scales, vials, and small zipper storage bags that can be used to sell crack, heroin, or marijuana fall into this category.
_____
_____
Vaping:
Vaping is the act of inhaling and exhaling the aerosol, often referred to as vapor, which is produced by an e-cigarette or similar device. The use of electronic cigarettes has reached heightened levels in recent years as they have gained in popularity and social acceptance. Tobacco smoke is highly toxic, carcinogenic, can create lung problems and produces many undesirable effects. Electronic cigarettes were developed to only deliver the psychoactive chemical in cigarettes, nicotine, through vaporizing dissolved nicotine and subsequently inhaling it. The use of e-cigarettes has not yet been definitively shown to be effective in stopping the use of nicotine. Using e-cigarettes, otherwise known as vaping, is not without its own risks, as other substances may be included in the vapor and the vapor itself can create lung problems, problems with immunity, and other medical problems. The most dangerous form of vaping is when people deliberately swap out the vaping liquid with synthetic street drugs such as spice, flakka, bath salts. Using E-Cigarettes that contain synthetic street drugs can potentially lead to drug addiction and other possible serious health concerns. Vaping marijuana continues to dramatically increase in popularity among teens. Vaping marijuana (THC oil) can be more dangerous than smoking the drug. This is because people often vape a higher concentration of THC which, in turn, intensifies the high and can increase the likelihood of addiction and adverse medical consequences.
______
______
Factors responsible for drug-related harm:
The effects of a drug, and how long they last, depend on a number of factors:
- the type and strength of drugs that you use
- how the drug was made — substances manufactured in home labs may contain bacteria, dangerous chemicals and other unsafe substances, and have an unknown strength. Even one dose may cause an overdose that leads to brain damage or death
- your physical characteristics (including height, weight, age, body fat and metabolism)
- the dose that you take
- how often and for how long you have been using drugs
- how you ingest the drug (by inhalation, by injection or orally). Compared with swallowing a drug, inhalation and injection are more likely to lead to overdose and dependence. If you are injecting drugs, sharing injecting equipment will increase your risk of contracting serious diseases such as hepatitis and HIV. It will also increase your risk of serious infection
- your mental health, mood and environment (that is, whether you are in a secure, happy place or an unsafe place) can affect the experience you have when taking drugs. If you have a mental health condition, drugs may exacerbate or complicate the symptoms of that condition
- whether you mix drugs, including alcohol. In particular, alcohol use may lead to high risk behaviour (such as drink driving) which can result in the serious injury or death of yourself or others.
- availability (how easily accessible is the substance and how this impacts upon use)
- legal situation (both the law and its implementation around use of the substance)
- social context (consequences of set, setting & social milieu on dangerousness)
- incapacitation (the effect of imprisonment or treatment on patterns of use – including the substitution of other drugs)
______
Hard drugs and soft drugs:
Drug harmfulness is the degree to which a psychoactive drug is harmful to a user and is measured in various ways, such as by addictiveness and the potential for physical harm. More harmful drugs are called “hard drugs”, and less harmful drugs are called “soft drugs”. The term “soft drug” is considered controversial by its critics as it may imply that soft drugs cause no or insignificant harm. The distinction between soft drugs and hard drugs is important in the drug policy of the Netherlands, where cannabis production, retail and use come under official tolerance, subject to certain conditions. The Dutch Opium Law contains two lists of drugs, List I and List II, that are colloquially considered to be lists of hard and soft drugs, respectively. According to the legal system of the Netherlands; selected soft drugs are tolerated legally while other hard drugs are illegal. Soft drugs can be tolerated in various ways whether it be total lack of regulation or some regulation, but still legal availability to the public. Other countries typically have more than two categories. For example, the United States has five schedules in the Controlled Substances Act, ranging from one through five. The United Kingdom has three classes in the Misuse of Drugs Act 1971: A, B and C.
______
Addictive potential of drugs:
For decades, researchers have ranked the most addictive drugs in the world. A variety of factors influence the addictiveness of a substance, such as the degree of tolerance a person develops after repeated use and the intensity of the drug’s withdrawal symptoms. The most addictive drugs can cause widespread addiction and public health problems. A number of researchers have conducted studies to rank the addictiveness of specific drugs using a variety of factors.
_
Main criteria that researchers use to determine the overall addictiveness of a drug include:
- How much harm does the drug cause?
- What is the street value of the drug?
- To what extent does the drug activate the brain’s dopamine system?
- How pleasurable do users report the drug to be?
- To what degree does the drug cause withdrawal symptoms?
- How likely or unlikely is it to get hooked on the drug?
- How easy or difficult is it to get off of the drug?
Researchers compare the survey results from active drug users which then assists those who study addiction in arriving at relatively sound theories about the overall addictiveness of various substances. Here is an example of how this analysis works in action. Comparing heroin and marijuana, research has shown us that, for the most part, heroin is more addictive than marijuana. Heroin has a higher street value. It actives the brain’s dopamine system on an entirely higher plane than marijuana does. It is conceived to produce a more powerful effect on the user. It can cause addiction after just one use. It creates far more painful withdrawal symptoms and is harder to get off than marijuana. So we can see that heroin is a more addictive, more dangerous, and overall more harmful drug than marijuana.
_
In the 1990s, Dr. Jack E. Henningfield of the National Institute on Drug Abuse and Dr. Neal L. Benowitz of the University of California at San Francisco each ranked the six most addictive drugs.
Rankings for addictiveness were based on five problem areas, including:
- Presence and severity of withdrawal symptoms
- Reinforcement
- Cravings and tolerance
- Rates of dependence and relapse
- Level of intoxication
Henningfield ranked nicotine as the most addictive substance, followed by heroin, cocaine, alcohol, caffeine and marijuana. He said that heroin caused the second most intense withdrawal symptoms, followed by nicotine, cocaine, caffeine and marijuana. According to Henningfield’s rankings, alcohol caused the highest level of intoxication, and it had the most serious withdrawal symptoms. Alcoholism can lead to delirium tremens, a severe form of alcohol withdrawal characterized by sudden and severe changes to the nervous system. Both addiction experts found that cocaine ranked highest for reinforcement, which is a measure of a substance’s ability to drive repeated use based on human and animal tests. Like Henningfield, Benowitz found that addiction to nicotine was the most common and that marijuana addiction was the least common.
_
In 2007, British psychiatrist David Nutt and a team of addiction experts investigated the most harmful drugs. In a study published in The Lancet, Nutt’s team assessed the harm, dependence and potential misuse associated with 20 drugs. Nutt and colleagues analyzed each substance based on physical and psychological dependency, physical harm and societal harms. Dependence was based on pleasurable effects, tolerance, withdrawal symptoms and the drug’s ability to influence repeated use.
According to Nutt and his team, the top five most addictive drugs are:
1.Heroin
2.Cocaine
3.Nicotine
4.Street methadone
5.Barbiturates
_
The diagram above shows the dependence potential and the relation between active and lethal dose of some psychoactive substances. Heroin and nicotine are highly addicting. LSD is least addicting.
_
Capture rates:
Capture rates enumerate the percentage of users who reported that they had become dependent to their respective drug at some point.
| Drug | % of users |
| Cannabis | 9% |
| Alcohol | 15.4% |
| Cocaine | 16.7% |
| Heroin | 23.1% |
| Tobacco | 31.9% |
As you can see, among illicit drugs heroin has highest capture rate.
______
Although all recreational drugs are dangerous, some can be more deadly than others. One way to determine how dangerous recreational drugs are is to calculate a safety ratio, based on the dose that is likely to be fatal divided by the normal dose needed to feel the effects of the drug. Drugs with lower ratios are more dangerous because the difference between the normal and the lethal dose is small. For instance, heroin has a safety ratio of 6 because the average fatal dose is only six times greater than the average effective dose. On the other hand, marijuana has a safety ratio of 1,000. This is not to say that smoking marijuana cannot be deadly, but it is much less likely to be deadly than is heroin. The safety ratios of common recreational drugs are shown in Table below:
Popular Recreational Drugs and Their Safety Ratios:
| Drug | Description | Safety ratio |
| Heroin | Strong depressant | 6 |
| GHB (Gamma hydroxy butyrate) | “Rave” drug, also used as a “date rape” drug | 8 |
| Isobutyl nitrite | Depressant and toxic inhalant | 8 |
| Alcohol | Active compound is ethanol | 10 |
| DXM (Dextromethorphan) | Active ingredient in over-the-counter cold and cough medicines | 10 |
| Methamphetamine | May be injected or smoked | 10 |
| Cocaine | May be inhaled or smoked | 15 |
| MDMA (methylenedioxymethamphetamine) | Very powerful stimulant | 16 |
| Codeine | Depressant | 20 |
| Methadone | Opioid | 20 |
| Mescaline | Hallucinogen | 24 |
| Benzodiazepine | Prescription tranquilizer | 30 |
| Ketamine | Prescription anaesthetic | 40 |
| DMT (Dimethyltryptamine) | Hallucinogen | 50 |
| Phenobarbital | Usually prescribed as a sleeping pill | 50 |
| Fluoxetine | Antidepressant | 100 |
| Nitrous oxide | Often inhaled from whipped-cream dispensers | 150 |
| Lysergic acid diethylamide (LSD) | Hallucinogenic drug | 1,000 |
| Marijuana (Cannabis) | Active ingredient is THC | 1,000 |
Drugs with lower safety ratios have a greater risk of brain damage and death.
_____
_____
Illicit drug usage correlation:
Is there any correlation between use of one illicit drug with another?
If you use one illicit drug, how likely are you to use another illicit drug?
The Pearson correlation coefficient is a measure of the strength of a linear association between two variables and is denoted by r. The Pearson correlation coefficient, r, can take a range of values from +1 to -1. A value of 0 indicates that there is no association between the two variables. A value greater than 0 indicates a positive association; that is, as the value of one variable increases, so does the value of the other variable. A value less than 0 indicates a negative association; that is, as the value of one variable increases, the value of the other variable decreases.
_
Figure above depicts the correlations among the usage of 18 legal and illegal drugs: alcohol, amphetamines, amyl nitrite, benzodiazepine, cannabis, chocolate, cocaine, caffeine, crack, ecstasy, heroin, ketamine, legal highs, LSD, methadone, magic mushrooms (MMushrooms), nicotine and volatile substance abuse (VSA). Usage is defined as having used the drug at least once during years 2005–2015. The colored links between drugs indicate the correlations with |r|>0.4, where |r| is the absolute value of the Pearson correlation coefficient.
Usage of some drugs is strongly correlated. For example, the consumption of seven illicit drugs (amphetamines, cannabis, cocaine, ecstasy, legal highs, LSD, and magic mushrooms) is correlated and the Pearson correlation coefficient r>0.4 in every pair of them; consumption of cannabis is strongly correlated (r>0.5) with usage of nicotine (tobacco), and heroin is correlated with cocaine (r>0.4). According to the concept common liability to addiction, a number of personal, social, genetic and environmental factors can lead to a generally increased interest in various drugs.
_____
_____
An Evolving Understanding of Substance Use Disorders:
Scientific breakthroughs have revolutionized the understanding of substance use disorders. For example, severe substance use disorders, commonly called addictions, were once viewed largely as a moral failing or character flaw, but are now understood to be chronic illnesses characterized by clinically significant impairments in health, social function, and voluntary control over substance use. Although the mechanisms may be different, addiction has many features in common with disorders such as diabetes, asthma, and hypertension. All of these disorders are chronic, subject to relapse, and influenced by genetic, developmental, behavioral, social, and environmental factors. In all of these disorders, affected individuals may have difficulty in complying with the prescribed treatment.
This evolving understanding of substance use disorders as medical conditions has had important implications for prevention and treatment. Research demonstrating that addiction is driven by changes in the brain has helped to reduce the negative attitudes associated with substance use disorders and provided support for integrating treatment for substance use disorders into mainstream health care. Moreover, research on the basic neurobiology of addiction has already resulted in several effective medications for the treatment of alcohol, opioid, and nicotine use disorders, and clinical trials are ongoing to test other potential new treatments.
- Well-supported scientific evidence shows that addiction to alcohol or drugs is a chronic brain disease that has potential for recurrence and recovery.
- Well-supported evidence suggests that the addiction process involves a three-stage cycle: binge/intoxication, withdrawal/negative affect, and preoccupation/anticipation. This cycle becomes more severe as a person continues substance use and as it produces dramatic changes in brain function that reduce a person’s ability to control his or her substance use.
- Well-supported scientific evidence shows that disruptions in three areas of the brain are particularly important in the onset, development, and maintenance of substance use disorders: the basal ganglia, the extended amygdala, and the prefrontal cortex. These disruptions: (1) enable substance-associated cues to trigger substance seeking (i.e., they increase incentive salience); (2) reduce sensitivity of brain systems involved in the experience of pleasure or reward, and heighten activation of brain stress systems; and (3) reduce functioning of brain executive control systems, which are involved in the ability to make decisions and regulate one’s actions, emotions, and impulses.
- Supported scientific evidence shows that these changes in the brain persist long after substance use stops. It is not yet known how much these changes may be reversed or how long that process may take.
- Well-supported scientific evidence shows that adolescence is a critical “at-risk period” for substance use and addiction. All addictive drugs, including alcohol and marijuana, have especially harmful effects on the adolescent brain, which is still undergoing significant development.
–Well-supported: when evidence is derived from multiple rigorous human and nonhuman studies;
–Supported: when evidence is derived from rigorous but fewer human and nonhuman studies.
All addictive substances have powerful effects on the brain. These effects account for the euphoric or intensely pleasurable feelings that people experience during their initial use of alcohol or other substances, and these feelings motivate people to use those substances again and again, despite the risks for significant harms.
_______
There are multiple ways in which genetic and environmental factors may result in variation in vulnerability to addiction (West, 2013). According to NIH (2010), genes account for approximately 50% of an individual’s risk of becoming addicted. Genetic vulnerability contributes to the risk of developing an addiction. Twin and adoption studies show that about 40% to 60% of susceptibility to addiction is hereditary. But behavior plays a key role, especially when it comes to reinforcing a habit.
Three attributes influence an individual’s disposition to engage in a specific behavior:
- Capability – the physical or psychological capacity to engage in behavior.
- Motivation – the mental process that guide behavior, both automatic (e.g. euphoria after ingesting cocaine) and reflective (e.g. attitude that marijuana is harmless).
- Opportunity – environmental factors that either promote or constrain behavior. Includes:
-The physical environment (e.g. ease of access to a substance).
-Social factors, such as peer attitudes (West, 2013).
-Although substance use at any age can progress to addiction, onset of use is highly predictive. Adolescents are quite vulnerable as their brains are still developing.
Environment’s Role:
Environment plays a major role in it as well. The interplay between an individual and his environment gives rise to behavior. There are many influences in one’s environment, including:
- Social network.
- Socioeconomic status.
- Stress.
- Parental involvement.
- Personal history, such as physical or sexual abuse, or neglect.
To combat addiction, exposure to environmental and internal factors that foster strong motivations to use must be reduced and countered with other motivators (West, 2013). From a harm reduction standpoint, delaying onset of use may be highly beneficial. For example, targeted prevention and outreach efforts toward adolescents and their networks, including family and teachers, have successfully demonstrated changes in attitudes and behaviors with respect to youth tobacco use (NIH, 2010).
________
________
Different types of addiction:
Addiction can be either behavioral or substance related. An intense feeling of emotional need or physical craving characterizes them both. Both types of addiction carry a number of other similarities, but behavioral addiction does not possess the same physical symptoms that accompany drug addiction. Experts disagree on the similarities and differences between the symptoms and consequences of the types of addictions.
_
- Drug Addiction
Drugs are addictive substances that change the way the body — the brain in particular — handles communication and processes information. Long-term drug use causes physical changes in the brain that lead to a substance use disorder. Different drugs affect the body differently. Stimulants, such as tobacco, cocaine or prescription amphetamines, stimulate the brain and nervous system, causing increased alertness. Depressants, such as alcohol, barbiturates and benzodiazepines, slow activity in the brain and nervous system, causing relaxation. Hallucinogens, such as LSD and PCP, drastically disrupt the way the brain and nervous system communicate, causing hallucinations.
Common drug addictions include:
Marijuana
Heroin
Cocaine/crack
Synthetic drugs such as bath salts and spice
_
- Prescription Drug Addiction
Prescription drugs are approved medications used to treat symptoms of diseases and other medical conditions. Even when used as prescribed, they can cause physical changes that can lead to addiction. When they’re used in any way other than as prescribed by a doctor, the likelihood of prescription drug addiction drastically increases.
Common drugs that cause prescription drug addiction include:
Opioids, including oxycodone and hydrocodone.
Benzodiazepines, such as alprazolam and diazepam
Amphetamines, dextroamphetamine and methylphenidate
Sedatives including zolpidem and eszopiclone
People often believe that if they take prescription drugs, they are safe from addiction. Many addictive prescription psychotropic drugs have labels on them warning of the risk of addiction.
An addiction to prescription psychotropic drugs can be formed for a number of reasons. Most often, it is because:
- The individual is taking the drug without a prescription
- The person is taking too much of the drug at one time
- The person has been using the drug for too long
- The individual is taking doses that are too close together
- The drug is being crushed and snorted, or mixed with liquid and injected
Any of these methods of taking prescription psychotropic drugs will eventually lead to addiction. These drugs are not at all safe; and even more so when they are being misused.
Prescription psychotropic drugs can lead to addiction the same way that other psychoactive drugs do. The body grows dependent upon the drugs as time goes on. Eventually, the person begins to feel as though they can’t live without them. In 2016, approximately 2.1 million Americans over the age of 11 suffered from addiction to opioids such as the prescription pain medications oxycodone, hydrocodone and the illegal drug heroin. Yet, 11.8 million people – nearly six times as many – reported misusing opioids, primarily prescription medications. Although it does not receive the same media attention as addiction, this startling figure highlights a serious yet often overlooked problem within our society: the issue of opioid misuse.
Myth: Using drugs like opioid painkillers are safe since they’re so commonly prescribed by doctors.
Fact: Short-term medical use of opioid painkillers can help to manage severe pain after an accident or surgery, for example. However, regular or longer-term use of opioids can lead to addiction. Misuse of these drugs or taking someone else’s medication can have dangerous—even deadly—consequences.
_
- Over-the-Counter (OTC) Medication addiction
Over-the-counter medicines that are commonly misused include dextromethorphan (DXM), a cough suppressant, and loperamide, an antidiarrheal. Products containing DXM can be sold as cough syrups, gel capsules, and pills that can look like candies. They are often misused by young people, who refer to the practice as “robotripping” or “skittling.” Loperamide is available in tablet, capsule, or liquid form. Both DXM and loperamide are opioids. DXM does not have effects on pain reduction or addiction and does not act on the opioid receptors. However, when taken in large doses, DXM can cause a depressant and hallucinogenic effect. Short-term effects of DXM misuse can range from mild stimulation to alcohol- or marijuana-like intoxication. Loperamide does not enter the brain; but when taken in large doses and combined with other substances, it may cause the drug to act in a similar way to other opioids. Loperamide misuse can cause euphoria, similar to other opioids, or lessen cravings and withdrawal symptoms, but other effects have not been well studied and reports are mixed.
Purple drank:
Purple drank is a name given to a recreational drug consisting of a soft drink mixed with prescription-strength cough syrup used in a manner inconsistent with its labelling. The cough syrup used in purple drank contains codeine and promethazine (not to be confused with dextromethorphan: DXM). The cough syrup, used in doses much higher than medically recommended, is typically mixed with ingredients such as the soft drinks Sprite, Mountain Dew, or Grape Fanta and optionally a Jolly Rancher hard fruit candy added, often for extra sweetness. The purplish hue of purple drank comes from dyes in the cough syrup. The amount of cough syrup used “can exceed up to 25 times the recommended dose.”
_
- Behavioral Addiction
As with drugs, certain behaviors cause brief feelings of happiness or euphoria. However, some long-term behaviors cause a person to lose control of their actions. People suffering from these addictions experience symptoms similar to those of drug addicts, including cravings, tolerance, withdrawal and relapse.
Common behavioral addictions include:
-1. Gambling
-2. Sex
-3. Eating
-4. Internet
-5. Shopping
-6. Video Games
The term behavioral addiction refers to a compulsion to engage in a natural reward – which is a behavior that is inherently rewarding (i.e., desirable or appealing) – despite adverse consequences. Preclinical evidence has demonstrated that marked increases in the expression of ΔFosB through repetitive and excessive exposure to a natural reward induces the same behavioral effects and neuroplasticity as occurs in a drug addiction. Reviews of both clinical research in humans and preclinical studies involving ΔFosB have identified compulsive sexual activity – specifically, any form of sexual intercourse – as an addiction (i.e., sexual addiction).Moreover, reward cross-sensitization between amphetamine and sexual activity, meaning that exposure to one increases the desire for both, has been shown to occur preclinically and clinically as a dopamine dysregulation syndrome; ΔFosB expression is required for this cross-sensitization effect, which intensifies with the level of ΔFosB expression. Reviews of preclinical studies indicate that long-term frequent and excessive consumption of high fat or sugar foods can produce an addiction (food addiction).
Gambling is a natural reward which is associated with compulsive behavior and for which clinical diagnostic manuals, namely the DSM-5, have identified diagnostic criteria for an “addiction”. In order for a person’s gambling behavior to meet criteria of an addiction, it shows certain characteristics, such as mood modification, compulsivity, and withdrawal. There is evidence from functional neuroimaging that gambling activates the reward system and the mesolimbic pathway in particular. Similarly, shopping and playing video games are associated with compulsive behaviors in humans and have also been shown to activate the mesolimbic pathway and other parts of the reward system. Based upon this evidence, gambling addiction, video game addiction, and shopping addiction are classified accordingly.
_
- Co-Occurring Disorders (vide infra)
Research indicates people who suffer from substance abuse disorders are very likely to suffer from co-occurring mental health disorders and vice versa.
Common co-occurring mental health disorders include:
Depression
Anxiety
Schizophrenia
Post-traumatic stress disorder
Eating disorders
Attention-deficit hyperactivity disorder
_
- Multiple addiction
Sexual addiction can be accompanied by other addictions and/or substance abuse. Multiple addiction means that multiple addictive behaviors exist as part of a single illness. These behaviors interact as reinforcements and become part of one another. They, in effect, become packages in which the whole is greater than the sum of the parts. A common combination is cocaine abuse, alcohol abuse, and sexual addiction. An individual can suffer from a behavioral addiction, a drug addiction and a mental health disorder all at the same time.
_
- Cross addiction:
In the simplest terms, cross addiction means you’ve traded one addiction for another. Cross addiction happens in many different ways. For example, a heroin addict might start abusing alcohol, or someone recovering from alcoholism starts abusing painkillers. Many cross-addicted people will use a substance that mimics their original addiction. For instance, a recovering cocaine addict may become addicted to prescription stimulants used to treat ADHD. Individuals with a cross addiction might also abuse seemingly innocent substances, such as over-the-counter sleep aids or prescription sedatives. Some even develop non-substance addictions to activities like excessive shopping, gambling, or sex.
In some cases, the person may have been sober for many years. After years of being sober, the person gets into an accident and a doctor prescribes a narcotic pain medication. Soon after being placed on the pain reliever, the person becomes addicted to the drug. Because the person is prone to addiction after having a prior addiction, they may quickly become addicted to another substance. On the other hand, a person may start abusing another substance while trying to recover from an addiction. It’s common for a person to abuse a substance that has similar effects to the original substance of abuse. For instance, a person who is addicted to heroin might start abusing prescription painkillers, or a person who was originally addicted to cocaine may abuse a different stimulant, such as a prescription amphetamine. Although cross addiction is common, not everyone who recovers from one addiction is necessarily going to develop another at some point.
If you have the disease of addiction, any other addicting drug also stimulate the part of the brain that regulates addiction and addictive behavior. The dopamine dysregulation in the reward system of the brain seen in addiction is not able to tell the difference between addictive drugs or different drugs are using similar mechanisms in the reward system. Therefore, if someone who has drug addiction is given another addictive drug for whatever reason, the individual with addiction may start abusing the second drug.
______
Similarities between Obesity and Drug Addiction:
Feeding is influenced by pleasure and reward, and obtaining food reward can powerfully motivate consumption. Nevertheless, hedonic mechanisms contributing to obesity remain poorly understood. In hyperphagic human patients with congenital leptin deficiency, activity in the dorsal and ventral striatum, core components of brain reward circuitries, is markedly increased in response to images of food, and leptin replacement therapy attenuates both striatal activity and self-reported “liking” of food. This suggests that the striatum plays an important role in hedonic aspects of feeding behavior. It was shown recently that activation of the striatum is blunted in obese individuals when compared with lean controls in response to highly palatable food. Moreover, hypofunctionality of the dorsal striatum and long-term weight gain is most pronounced in individuals with the TaqIA allele of the D2R gene locus that results in decreased striatal D2R expression, shown previously to be a predisposing factor to substance dependence disorders. Based on these and similar observations it has been proposed that deficits in reward processing may be an important risk factor for the development of obesity, and that obese individuals may compulsively consume palatable food to compensate for reward hyposensitivity. Importantly, it is presently unclear if deficits in reward processing are constitutive and precede obesity, or if excessive consumption of palatable food is sufficient to drive reward dysfunction and thereby contribute to diet-induced obesity.
A defining characteristic of overweight and obese individuals is the fact that they will continue to overeat despite the well-known negative health and social consequences. Indeed, many overweight individuals express a desire to limit their food consumption, yet struggle to control their intake and repeatedly consume past energy requirements. Development of feeding behavior that is insensitive to negative outcome is analogous to the compulsive drug-taking behavior seen in human drug addicts that is similarly impervious to negative consequences.
Recently an emphasis has been placed on the study of addiction-like behaviors as they relate to non-drug-related “reinforcers” such as food. Corwin and Babbs (2012) introduce the notion of binge eating in the context of addiction-like behaviors. Barson and colleagues (2012) consider the neurobiological mechanisms that control food intake, particularly excessive intake, and how these systems may be co-opted to control consumption of the commonly used drug alcohol. Finally, Michaelides and colleagues (2012) discuss the striking similarities between drug addiction and obesity in functional impairment in discrete brain regions and neurotransmitter circuits.
Obesity and drug addiction are major societal diseases. Aside from their direct effects on physical health, these disorders may be associated with significant and devastating mental health problems for those afflicted. They can also lead to dysfunctional relations for the affected individual both within the family and with coworkers and other members of society. In addition, sky-rocketing medical costs associated with treatment for drug addiction and obesity (especially for obesity-related complications such as type 2 diabetes and heart disease) affect all members of society. Obesity and drug addiction likely result from disturbances in ingestive behavior (Volkow and Wise 2005). Recent studies have documented the involvement of satiety and adiposity signals in drug addiction; for example, psychostimulants (i.e., cocaine and amphetamine) affect circulating levels of ghrelin and leptin (Kobeissy et al. 2008). Accordingly, food restriction indirectly (via its changes in circulating peptide and hormone concentrations) enhances drug seeking (Carr 2007), and ghrelin antagonists attenuate cocaine- and amphetamine-induced locomotor activity and conditioned place preference (CPP) in rats. These behaviors are paralleled by decreases in DA release in the nucleus accumbens (part of ventral striatum), a brain region heavily implicated in food and drug reward (Jerlhag et al. 2010). Aside from homeostatic mechanisms, ingestive behavior for both food and drugs of abuse is affected by nonhomeostatic mechanisms that are influenced by taste, pleasure, habits, social interactions, convenience, availability, and stress (Volkow and Wise 2005).
_______
Impulsive action and impulsive choice across substance and behavioral addictions: Cause or consequence? A 2014 study:
Substance use disorders are prevalent and debilitating. Certain behavioral syndromes (‘behavioral addictions’) characterized by repetitive habits, such as gambling disorder, stealing, shopping, and compulsive internet use, may share clinical, co-morbid, and neurobiological parallels with substance addictions. This review considers overlap between substance and behavioral addictions with a particular focus on impulsive action (inability to inhibit motor responses), and impulsive choice (preference for immediate smaller rewards to the detriment of long-term outcomes). Authors find that acute consumption of drugs with abuse potential is capable of modulating impulsive choice and action, although magnitude and direction of effect appear contingent on baseline function. Many lines of evidence, including findings from meta-analyses, show an association between chronic drug use and elevated impulsive choice and action. In some instances, elevated impulsive choice and action have been found to predate the development of substance use disorders, perhaps signifying their candidacy as objective vulnerability markers. Research in behavioral addictions is preliminary, and has mostly focused on impulsive action, finding this to be elevated versus controls, similar to that seen in chronic substance use disorders. Only a handful of imaging studies has explored the neural correlates of impulsive action and choice across these disorders. Future work should further explore whether the cognitive deficits identified are state or trait in nature: i.e. are evident before addiction perhaps signalling risk; or are a consequence of repetitive engagement in habitual behavior; and effects of novel agents known to modulate these cognitive abilities on various addictive disorders.
Highlights of this review:
- Behavioral addictions associated with impulsive actions.
- Findings are similar to those seen in chronic substance use disorders.
- Whether cognitive deficits are cause or effect remains unclear.
______
______
The Brain and Drug Addiction:
The American Society of Addiction Medicine defines addiction as “a primary, chronic disease of brain reward, motivation, memory, and related circuitry.” With the recent rise in opioid abuse and overdose, which has quickly become a national health epidemic, scientists are focused increasingly on understanding the science behind addiction and its effect on the brain, in hopes of finding new ways to treat and ultimately prevent the disease from occurring.
Addiction exerts a long and powerful influence on the brain that manifests in three distinct ways: craving for the object of addiction, loss of control over its use, and continuing involvement with it despite adverse consequences. While overcoming addiction is possible, the process is often long, slow, and complicated. It took years for researchers and policymakers to arrive at this understanding.
In the 1930s, when researchers first began to investigate what caused addictive behavior, they believed that people who developed addictions were somehow morally flawed or lacking in willpower. Overcoming addiction, they thought, involved punishing miscreants or, alternately, encouraging them to muster the will to break a habit. The scientific consensus has changed since then. Today we recognize addiction as a chronic disease that changes both brain structure and function. Just as cardiovascular disease damages the heart and diabetes impairs the pancreas, addiction hijacks the brain. Recovery from addiction involves willpower, certainly, but it is not enough to “just say no” — as the 1980s slogan suggested. Instead, people typically use multiple strategies — including psychotherapy, medication, and self-care — as they try to break the grip of an addiction.
Another shift in thinking about addiction has occurred as well. For many years, experts believed that only alcohol and powerful drugs could cause addiction. Neuroimaging technologies and more recent research, however, have shown that certain pleasurable activities, such as gambling, shopping, and sex, can also co-opt the brain.
_
The most complex body organ, the brain, is impacted by drug addiction in 3 central areas:
- The brain stem. This controls basic bodily functions, including breathing, sleeping, and heart rate.
- The cerebral cortex. This controls executive functions, such as decision-making, planning, and sensory information processing.
- The limbic system. This is the body’s emotional reward circuitry and controls our ability to experience pleasure and motivation for survival sustaining activities, which is activated by drugs of abuse (NIDA, 2014).
_
Neuroimaging in Drug Dependence:
In the past two decades, we have seen unprecedented advances in studying the human brain. Perhaps the most exciting has been the advent of structural and functional brain imaging techniques, which have revolutionized cognitive and behavioral neuroscience by allowing us a window into the brain activity underlying complex human behaviors. These technological advances have also led to the swift translation of basic neuroscience findings into more targeted therapies for clinical practice.
There is a wide variety of brain imaging techniques, which can be classified into three major categories: (1) nuclear medicine imaging techniques, including positron emission tomography (PET) and single photon emission computed tomography (SPECT); (2) magnetic resonance imaging (MRI) techniques including structural MRI, functional MRI (fMRI), and MR spectroscopy; and (3) electrophysiological imaging techniques, which include electroencephalography (EEG) and magnetoencephalography (MEG). Each of these techniques reveals a different aspect of brain structure and/or function, yielding a breadth of knowledge about the biochemical, electrophysiological, and functional processes of the brain; neurotransmitter activity; energy utilization and blood flow; and drug distribution and kinetics. Together they shed light on complex neuropsychological diseases, including drug addiction.
Neuroimaging traditionally has provided non-invasive anatomic views of the brain, but the applications of neuroimaging have expanded to include measurement of the concentrations of neurochemicals and specific proteins such as subtypes of neurotransmitter receptors or transporters, rates of metabolic pathways and blood flow, and the detection of functional or pharmacologic changes in the brain and evaluations of connections among brain regions. Over the past few years, the primary neuroimaging techniques used to study the effects of alcohol and other substances have been positron emission tomography (PET), magnetic resonance imaging (MRI), and magnetic resonance spectroscopy (MRS). Each approach has its own strengths and weaknesses, and there is the potential to utilize them synergistically.
_
The Role of Neurotransmitters in Addiction:
Neurons communicate via dendrites and axons, sending electrical impulses down the axon, converting them to chemical signals at the axon terminal, releasing neurotransmitters (chemical messengers) across synaptic gaps (narrow space between the axon terminal and the dendrite of another neuron), and attaching to the receiving neuron’s receptor site. The dendrite receives the neurotransmitter and converts it back to electrical signals. This process happens between billions of neurons in the brain. Communication between neurons functions to control behavior, cognition, mood, and movement (NIDA, 2013).
Drugs of abuse, whose chemical structures mimic natural neurotransmitters, interfere with normal neuronal processing, releasing neurotransmitters in excessive amounts, providing greater pleasure than naturally pleasing survival activities (e.g., eating or sex) and preventing normal chemical reuptake, meaning that an excessive amount of neurotransmitters are left in the synapse, ultimately affecting the behavior of other communicating neurons, which subjectively alters our mood. (NIDA, 2013).
The brain’s reward system is activated when an individual engages in survival activities, providing euphoric feelings and reinforcing behavior. When activated, information travels from the ventral tegmental area (VTA) to the nucleus accumbens and then to the prefrontal cortex (Van Wormer & Davis, 2013). The VTA is connected to both the nucleus accumbens and the prefrontal cortex via this pathway and it sends information to these structures via its neurons. The neurons of the VTA contain the neurotransmitter dopamine, which is released in the nucleus accumbens and in the prefrontal cortex.
Normal brain function, whether it is within the neo-cortex or the reward center, is a process involving appropriate nerve stimulation, transmission, and reception. How well that process works depends on having an adequate number of nerve synapses and the appropriate amount of neurotransmitters and receptors within that synapse. When an individual ingests a mood-altering substance, he or she is exogenously altering the amount of dopamine and other neurotransmitters that are present in the synapses of the NAcc, within the reward pathway.
Heroin for example, binds to the endorphin receptors of the brain. This in turn causes a decrease in the release of GABA, one of our inhibitory neurotransmitters, which modulates normal dopamine release. By inhibiting GABA, there is a corresponding increase in dopamine release, which leads to an increase in dopamine receptor stimulation. This fools the brain into thinking that an instinctual drive has just been satisfied.
Cocaine, on the other hand, has a more direct effect in that it acts as a dopamine reuptake inhibitor, much like the SSRIs inhibit the reuptake of serotonin. By blocking the reuptake of dopamine, cocaine use allows the dopamine molecule to remain within the synaptic gap for a longer time period, which in turn allows for more dopamine receptors to be stimulated. Ultimately, just like an opiate, cocaine fools the brain into believing it has just met an instinctual need.
Some drugs may have a more indirect effect on the reward pathway. Alcohol, for example, has its immediate site of action within the globus pallidus, which ultimately alters dopamine levels within the reward pathway. Essentially, all of the drugs of abuse exert their effects by influencing the amount of neurotransmitters within the reward pathway.
- Dopamine:
Dopamine plays a key role in the regulation of various physiological functions of normal brain including reward, locomotion, behavior, learning, and emotion. It is not then surprising that the dysregulation of the dopaminergic system has been linked to pathophysiology of many diseases, such as Alzheimer’s disease, schizophrenia, Parkinson’s disease, attention deficit hyperactivity disorder, depression and drug addiction, leading to the clinical use of drugs that target dopamine neurotransmission in the treatment of these disorders. The neurotransmitter dopamine is responsible for incentive, reward and motivation, and is a key neurotransmitter involved in addiction. Drugs of abuse activate reward pathways, releasing excessive dopamine. Dopamine surges produce:
- Euphoria.
- Strong behavioral reinforcement.
- Cravings or compulsions to perform certain behaviors.
The brain adjusts to such surges by reducing dopamine production and the number of receptors that can receive signals. Dopamine depletion, along with disruption in other neurotransmitters, reduces one’s ability to experience pleasure (NIDA, 2013). Dopamine depletion following cocaine use may account for binges, tolerance, and craving (Van Wormer & Davis, 2013).
- Serotonin:
Serotonin, the neurotransmitter involved in sleep, sensory experiences, and sense of well-being, may also play a key role in addiction. Decreased serotonin levels have been linked to behaviors associated with:
- Intoxication.
- Depression.
- Anxiety.
- Poor impulse control.
- Aggression.
- Suicidal behavior.
- Glutamate:
Another neurotransmitter, glutamate, the primary excitatory brain neurotransmitter stimulating brain cells to fire, is associated with learning and memory, and has been implicated in the perpetuation of addiction.
Research has demonstrated that glutamate, operating independently and interacting with the dopaminergic system, fosters the development and maintenance of addiction through:
- Reinforcement.
- Conditioning (cues in one’s daily routine become associated with use).
- Craving.
- Relapse (Tzschentke & Schmidt, 2003).
- GABA:
Gamma-aminobutyric acid (GABA) is the primary inhibitory neurotransmitter in the brain. Sedative-hypnotic drugs including alcohol, benzodiazepines, and barbiturates have long been hypothesized to modulate receptors in GABA systems. GABA binds with GABAA and GABAB receptors to inhibit neuronal activity. Substances of abuse can down regulate or up regulate the GABA system. GABAB receptors modulate substance reward and reinforcement behaviours. Disturbances to the GABA system may predate substance addiction. Compounds that target the GABA system may help in the treatment of addiction.
- Endogenous Opioids:
Endogenous opioids are morphinelike neurotransmitters. Considerable evidence shows that the endogenous opioid systems have roles in the positive reinforcing effects of opiates (e.g., heroin). The opioid system also appears to be important for the reinforcing effects of both alcohol and nicotine. For example, the opiate receptor antagonists naloxone and naltrexone reduce both alcohol and nicotine reinforcement in several animal models. Naltrexone has also shown success in decreasing alcohol consumption, frequency of relapse, and craving for alcohol in humans. These data suggest that interactions between mesolimbic dopamine and opioid systems are important in the addictive process.
_
The Primary Brain Regions involved in Substance Use Disorders:
The brain has many regions that are interconnected with one another, forming dynamic networks that are responsible for specific functions, such as attention, self-regulation, perception, language, reward, emotion, and movement, along with many other functions. There are three regions that are the key components of networks that are intimately involved in the development and persistence of substance use disorders: the basal ganglia, the extended amygdala, and the prefrontal cortex (see figure below). The basal ganglia control the rewarding, or pleasurable, effects of substance use and are also responsible for the formation of habitual substance taking. The extended amygdala is involved in stress and the feelings of unease, anxiety, and irritability that typically accompany substance withdrawal. The prefrontal cortex is involved in executive function (i.e., the ability to organize thoughts and activities, prioritize tasks, manage time, and make decisions), including exerting control over substance taking.
_
Figure below shows regions of the brain involved in the addiction cycle. The basal ganglia are near the top of the brain, the extended amygdala is near the bottom, and the prefrontal cortex is towards the front.
These brain areas and their associated networks are not solely involved in substance use disorders. Indeed, these systems are broadly integrated and serve many critical roles in helping humans and other animals survive. For example, when people engage in certain activities, such as consuming food or having sex, chemicals within the basal ganglia produce feelings of pleasure. This reward motivates individuals to continue to engage in these activities, thereby ensuring the survival of the species. Likewise, in the face of danger, activation of the brain’s stress systems within the extended amygdala drives “fight or flight” responses. These responses, too, are critical for survival. So these and other survival systems are “hijacked” by addictive substances.
_
The Basal Ganglia:
The basal ganglia are a group of structures located deep within the brain that play an important role in keeping body movements smooth and coordinated. They are also involved in learning routine behaviors and forming habits. Two sub-regions of the basal ganglia are particularly important in substance use disorders:
- The nucleus accumbens (part of ventral striatum), which is involved in motivation and the experience of reward, and
- The dorsal striatum, which is involved in forming habits and other routine behaviors.
The Extended Amygdala:
The extended amygdala and its sub-regions, located beneath the basal ganglia, regulate the brain’s reactions to stress-including behavioral responses like “fight or flight” and negative emotions like unease, anxiety, and irritability. This region also interacts with the hypothalamus, an area of the brain that controls activity of multiple hormone-producing glands, such as the pituitary gland at the base of the brain and the adrenal glands at the top of each kidney. These glands, in turn, control reactions to stress and regulate many other bodily processes.
The Prefrontal Cortex:
The prefrontal cortex is located at the very front of the brain, over the eyes, and is responsible for complex cognitive processes described as “executive function.” Executive function is the ability to organize thoughts and activities, prioritize tasks, manage time, make decisions, and regulate one’s actions, emotions, and impulses.
Some drugs like opioids also affect other parts of the brain, such as the brain stem, which controls basic functions critical to life, such as heart rate, breathing, and sleeping explaining why overdoses can cause depressed breathing and death.
______
The Addiction Cycle:
Addiction can be described as a repeating cycle with three stages. Each stage is particularly associated with one of the brain regions described above—basal ganglia, extended amygdala, and prefrontal cortex. Three-stage model draws on decades of human and animal research and provides a useful way to understand the symptoms of addiction, how it can be prevented and treated, and how people can recover from it. The three stages of addiction are:
- Binge/Intoxication, the stage at which an individual consumes an intoxicating substance and experiences its rewarding or pleasurable effects;
- Withdrawal/Negative Affect, the stage at which an individual experience a negative emotional state in the absence of the substance; and
- Preoccupation/Anticipation, the stage at which one seeks substances again after a period of abstinence.
The binge/intoxication stage is associated with the basal ganglia, the withdrawal/negative affect stage is associated with the extended amygdala, and the preoccupation/anticipation stage is associated with the prefrontal cortex.
Figure above shows three Stages of the Addiction Cycle and brain regions associated with them.
The three stages are linked to and feed on each other, but they also involve different brain regions, circuits (or networks), and neurotransmitters and result in specific kinds of changes in the brain. A person may go through this three-stage cycle over the course of weeks or months or progress through it several times in a day. There may be variation in how people progress through the cycle and the intensity with which they experience each of the stages. Nonetheless, the addiction cycle tends to intensify over time, leading to greater physical and psychological harm.
_
Each stage of addiction cycle is associated with the activation of specific neurobiological circuits and the consequential clinical and behavioral characteristics (Figure below).
During intoxication, drug-induced activation of the brain’s reward regions (in blue) is enhanced by conditioned cues in areas of increased sensitization (in green). During withdrawal, the activation of brain regions involved in emotions (in pink) results in negative mood and enhanced sensitivity to stress. During preoccupation, the decreased function of the prefrontal cortex leads to an inability to balance the strong desire for the drug with the will to abstain, which triggers relapse and reinitiates the cycle of addiction. The compromised neurocircuitry reflects the disruption of the dopamine and glutamate systems and the stress-control systems of the brain, which are affected by corticotropin-releasing factor and dynorphin. The behaviors during the three stages of addiction change as a person transitions from drug experimentation to addiction as a function of the progressive neuroadaptations that occur in the brain.
_
- Binge/Intoxication Stage: Basal Ganglia
The binge/intoxication stage of the addiction cycle is the stage at which an individual consumes the substance of choice. This stage heavily involves the basal ganglia and its two key brain sub-regions, the nucleus accumbens and the dorsal striatum. In this stage, substances affect the brain in several ways.
Addictive Substances “Hijack” Brain Reward Systems:
All addictive substances produce feelings of pleasure. These “rewarding effects” positively reinforce their use and increase the likelihood of repeated use. The rewarding effects of substances involve activity in the nucleus accumbens, including activation of the brain’s dopamine and opioid signalling system. Many studies have shown that neurons that release dopamine are activated, either directly or indirectly, by all addictive substances, but particularly by stimulants such as cocaine, amphetamines, and nicotine. In addition, the brain’s opioid system, which includes naturally occurring opioid molecules (i.e., endorphins, enkephalins, and dynorphins) and three types of opioid receptors (i.e., mu, delta, and kappa), plays a key role in mediating the rewarding effects of other addictive substances, including opioids and alcohol. Activation of the opioid system by these substances stimulates the nucleus accumbens directly or indirectly through the dopamine system. Brain imaging studies in humans show activation of dopamine and opioid neurotransmitters during alcohol and other substance use (including nicotine). Other studies show that antagonists, or inhibitors, of dopamine and opioid receptors can block drug and alcohol seeking in both animals and humans.
- Withdrawal/Negative Affect Stage: Extended Amygdala
The withdrawal/negative affect stage of addiction follows the binge/intoxication stage, and, in turn, sets up future rounds of binge/intoxication. During this stage, a person who has been using alcohol or drugs experiences withdrawal symptoms, which include negative emotions and, sometimes, symptoms of physical illness, when they stop taking the substance. Symptoms of withdrawal may occur with all addictive substances, including marijuana, though they vary in intensity and duration depending on both the type of substance and the severity of use. The negative feelings associated with withdrawal are thought to come from two sources: diminished activation in the reward circuitry of the basal ganglia and activation of the brain’s stress systems in the extended amygdala.
When used over the long-term, all substances of abuse cause dysfunction in the brain’s dopamine reward system. For example, brain imaging studies in humans with addiction have consistently shown long-lasting decreases in a particular type of dopamine receptor, the D2 receptor, compared with non-addicted individuals. Decreases in the activity of the dopamine system have been observed during withdrawal from stimulants, opioids, nicotine, and alcohol. Other studies also show that when an addicted person is given a stimulant, it causes a smaller release of dopamine than when the same dose is given to a person who is not addicted.
This stage of addiction involves a decrease in the function of the brain reward systems and an activation of stress neurotransmitters, such as CRF and dynorphin, in the extended amygdala. Together, these phenomena provide a powerful neurochemical basis for the negative emotional state associated with withdrawal. The drive to alleviate these negative feelings negatively reinforces alcohol or drug use and drives compulsive substance taking.
- Preoccupation/Anticipation Stage: Prefrontal Cortex
The preoccupation/anticipation stage of the addiction cycle is the stage in which a person may begin to seek substances again after a period of abstinence. In people with severe substance use disorders, that period of abstinence may be quite short (hours). In this stage, an addicted person becomes preoccupied with using substances again. This is commonly called “craving.” Craving has been difficult to measure in human studies.
This stage of addiction involves the brain’s prefrontal cortex, the region that controls executive function: the ability to organize thoughts and activities, prioritize tasks, manage time, make decisions, and regulate one’s own actions, emotions, and impulses. Executive function is essential for a person to make appropriate choices about whether or not to use a substance and to override often strong urges to use, especially when the person experiences triggers, such as stimuli associated with that substance (e.g., being at a party where alcohol is served or where people are smoking) or stressful experiences.
This stage of the addiction cycle is characterized by a disruption of executive function caused by a compromised prefrontal cortex. The activity of the neurotransmitter glutamate is increased, which drives substance use habits associated with craving, and disrupts how dopamine influences the frontal cortex. The over-activation of the Go system in the prefrontal cortex promotes habit-like substance seeking, and the under-activation of the Stop system of the prefrontal cortex promotes impulsive and compulsive substance seeking.
To recap, addiction involves a three-stage cycle—binge/intoxication, withdrawal/negative affect, and preoccupation/anticipation—that worsens over time and involves dramatic changes in the brain reward, stress, and executive function systems. Progression through this cycle involves three major regions of the brain: the basal ganglia, the extended amygdala, and the prefrontal cortex, as well as multiple neurotransmitter systems. The power of addictive substances to produce positive feelings and relieve negative feelings fuels the development of compulsive use of substances. The combination of increased incentive salience (binge/intoxication stage), decreased reward sensitivity and increased stress sensitivity (withdrawal/negative affect stage), and compromised executive function (preoccupation/anticipation stage) provides an often-overwhelming drive for substance seeking that can be unrelenting.
_
Different Classes of Substances affect the Brain and Behavior in Different Ways:
Although the three stages of addiction generally apply to all addictive substances, different substances affect the brain and behavior in different ways during each stage of the addiction cycle. Differences in the pharmacokinetics of various substances determine the duration of their effects on the body and partly account for the differences in their patterns of use. For example, nicotine has a short half-life, which means smokers need to smoke often to maintain the effect. In contrast, THC, the primary psychoactive compound in marijuana, has a much longer half-life. As a result, marijuana smokers do not typically smoke as frequently as tobacco smokers. Typical patterns of use are described for the major classes of addictive substances. However, people often use these substances in combination. Additional research is needed to understand how using more than one substance affects the brain and the development and progression of addiction, as well as how use of one substance affects the use of others.
_______
Pleasure principle:
The brain registers all pleasures in the same way, whether they originate with a psychoactive drug, a monetary reward, a sexual encounter, or a satisfying meal. In the brain, pleasure has a distinct signature: the release of the neurotransmitter dopamine in the nucleus accumbens, a cluster of nerve cells lying underneath the cerebral cortex. Dopamine release in the nucleus accumbens is so consistently tied with pleasure that neuroscientists refer to the region as the brain’s pleasure center:
_
Role of dopamine in worms:
- C. elegans (round worms) contain 4-8 dopamine neurons (depending on sex).
- Worms normally slow down when they encounter food (bacteria).
- This behavior is lost in worms upon ablation of these dopamine neurons.
- Thus, the use of dopamine in a neural circuit that controls motor responses to natural rewards goes back >1 billion years in evolution.
Role of dopamine in mammals:
- VTA dopamine neurons are “rheostats” of reward:
–Rewards activate the neurons
–Expectation of rewards activates the neurons
–Absence of expected rewards inhibits the neurons
–Unexpected rewards activate the neurons even more.
- Drugs directly and powerfully activate these neurons with no connection to purposeful behavior.
- This leads to a profound corruption of the brain’s reward mechanisms: drugs gradually, progressively, and insidiously replace natural rewards as the major shaper of behavior.
_
Early animal models showed that when a catheter containing cocaine was placed into the NAcc of a rat, the animal became addicted to the drug and learned to press a lever to get a dose of the drug. Once the animal was addicted, an electrical stimulus was connected to the lever that provided an ever-increasing shock each time the animal attempted to get his “fix.” In every case, the animals electrocuted themselves rather than cease the drug use. When this study was conducted again with food instead of a drug, the animals starved to death rather than endure the electrical stimulus. Finally, this study was replicated with the drug-containing catheter placed in the spinal cord, and no addictive behaviors were observed. The findings of this study included: (1) the drugs of abuse have a specific site of action in the brain; (2) this area of the brain must have a similar area in human beings (i.e., the instinctual brain); (3) no amount of unpleasant stimuli was great enough to get the animal to stop seeking the drug; and (4) this process was greater than other instinctual drives, including the drive to eat.
_
The addictive process manifests itself in human beings as the behaviors that we normally associate with being an addict (e.g., inability to control drug use, replacement of important activities by drug use). When the reward pathway is exogenously stimulated by drug use, it sends exaggerated signals to the prefrontal cortex, an area of the brain that control reasoning and judgment. This signal highjacks the prefrontal cortex into believing that, with drug use, an instinctual drive was just fulfilled and should be repeated. Unfortunately, while many people are able to experiment with psychoactive drugs with little or no adverse effects on repeated use, the person predisposed to addiction has malfunctioning satiation process, and therefore progresses into uncontrolled drug use.
_
A seemingly equivalent syndrome of addiction can occur with exposure to a wide variety of chemical substances or even rewarding activities, from cocaine to gambling to sex. The circuit that has received the most attention is referred to as the mesolimbic dopamine system, which involves dopamine neurons in the ventral tegmental area (VTA) of the midbrain innervating medium spiny neurons in the nucleus accumbens (NAcc, a part of ventral striatum). These VTA neurons also innervate many other forebrain regions, including hippocampus, amygdala, and prefrontal cortex (PFC).
_
Figure above shows brain areas involved in addiction: Originating from dopaminergic neurons located in the ventral tegmental area (VTA) of the midbrain this pathway projects to the nucleus accumbens (NAcc) (motivation), amygdala (mediates association of reward with cues and negative reinforcement), ventral pallidum, hippocampus (limbic system associated with memory and learning), and forebrain, in particular the prefrontal cortex (PFC). Addictive drugs provide a shortcut to the brain’s reward system by flooding the nucleus accumbens with dopamine. The hippocampus lays down memories of this rapid sense of satisfaction, and the amygdala creates a conditioned response to certain stimuli.
The prefrontal cortex contains both dopamine D1 and D2 receptors. D2 receptors have an approximately 10‐ to 100‐fold greater affinity for dopamine than D1 receptors and are therefore activated at lower dopamine concentrations. Under normal circumstances, the prefrontal cortex receives a low level, stable flow of dopamine owing to relatively slow, tonic firing of dopamine neurons in the ventral tegmental area (VTA) that project to the cortex. However, in response to an unexpected event, such as an extraordinary reward or very aversive event, dopamine neurons fire much more quickly. This phasic firing results in an abrupt, yet transient, increase in dopamine. The high levels of dopamine achieved during phasic firing are able to activate D1 receptors and are thought to be required for dopamine’s full rewarding effects. Drugs of abuse, particularly psychostimulants, mimic the high dopamine concentrations produced by phasic firing and thus activate both D1 and D2 receptors.
The nucleus accumbens (NAcc) is one output of the VTA projections. The nucleus accumbens itself consists mainly of GABAergic medium spiny neurons (MSNs). The NAcc is associated with acquiring and eliciting conditioned behaviors, and is involved in the increased sensitivity to drugs as addiction progresses. Overexpression of ΔFosB in the nucleus accumbens is a necessary common factor in essentially all known forms of addiction; ΔFosB is a strong positive modulator of positively reinforced behaviors.
Induction of Addiction:
The mesocorticolimbic dopamine system originates in the ventral tegmental area (VTA), which projects most notably to the nucleus accumbens (NAcc) and the prefrontal cortex (PFC). It is a defining commonality of all addictive drugs that they increase dopamine concentrations in target structures of the mesocorticolimbic projections. The release of dopamine from these projections is thought to play a crucial role in the induction of compulsive addictive behaviour. The precise role of dopamine in reinforcement and the modulation of reward-related behaviour remains controversial. Most experts in the field agree that some aspects of reward (e.g., euphoria/ pleasure) are dopamine-independent. In rats, for example, blockade of mesolimbic DA (dopamine) signalling with either systemic or intra-NAcc neuroleptic pre-treatment potentiated the sensitivity to nicotine’s rewarding properties. Also, dopamine-deficient mice display conditioned place preference for morphine. Moreover, it is important to realize that, once compulsive use has been established, addiction is thought to be largely dopamine-independent. Nonetheless, it is widely accepted that the induction of addiction crucially involves mesocorticolimbic dopamine.
_
Interactions of the Mesocortical and Mesolimbic Circuits in Drug Addiction:
The mesolimbic dopamine circuit, which includes the nucleus accumbens, amygdala, and hippocampus, has been traditionally associated with the acute reinforcing effects of a drug and with the memory and conditioned responses that have been linked to craving. It is also likely to be involved in the emotional and motivational changes seen in drug abusers during withdrawal. The mesocortical dopamine circuit, which includes the prefrontal cortex, orbitofrontal cortex, and anterior cingulate, is likely to be involved in the conscious experience of drug intoxication, drug incentive salience, drug expectation/craving, and compulsive drug administration. Because these circuits operate in parallel and interact with one another, it is likely that a given behavior involves, to a greater or lesser extent, their joint participation. The nature of these interactions affects response to the drug. The activation of these interacting circuits may be indispensable for maintaining the compulsive drug administration observed during bingeing and to the vicious circle of drug addiction.
In summary, much is known about the neurobiological circuitry of drug reward. The starting point for the reward circuit is the medial forebrain bundle, composed of myelinated fibers that bidirectionally connect the olfactory tubercle and nucleus accumbens with the hypothalamus and ventral tegmental area, and includes ascending monoamine pathways such as the mesocorticolimbic dopamine system. The initial action of drug reward is hypothesized to depend on dopamine release in the nucleus accumbens for cocaine, amphetamine, and nicotine, opioid peptide receptor activation in the ventral tegmental area (via dopamine activation) and nucleus accumbens (independent of dopamine activation) for opiates, and GABA systems in the nucleus accumbens and amygdala for alcohol. The nucleus accumbens is situated strategically to receive important limbic information from the amygdala, frontal cortex, and hippocampus that could be converted to motivational action via its connections with the extrapyramidal motor system. Thus, an early critical role of the nucleus accumbens is established for the acute reinforcing effects of drugs, with a supporting role of the central nucleus of the amygdala and ventral pallidum.
_
Mesocorticolimbic dopamine (DA) pathways, which arise from the midbrain ventral tegmental area (VTA), play a critical role in the mediation of reward. In particular, the VTA DA projection to the nucleus accumbens (NAcc) plays a prominent role in positive reinforcement, i.e. the recognition of rewards in the environment and promotion of goal-directed behavior (that is, ‘approach behaviour’) resulting in reward acquisition. Natural rewards such as food, sex and exercise and drugs of abuse including psychostimulants (such as cocaine and amphetamine), nicotine, alcohol, opiates and cannabinoids each increase NAcc DA and this neurochemical response contributes to subjective reward and positive reinforcement. Other components of the limbic system are also innervated by VTA DA neurons including the amygdala, hippocampus, orbitofrontal cortex and aspects of the prefrontal cortex (PFC). These regions are interconnected in complex circuits that involve excitatory (primarily glutamatergic) and inhibitory (primarily GABAegic) projections. In broad, simplistic terms amygdala circuits contribute to the formation of associative reward- and fear-related memories, hippocampal circuits are critical for declarative memory functions and frontal cortical circuits mediate control of executive functions. In turn, innervation of the NAcc by each of these circuits allows sensory and emotional information to be converted into motivational actions through the output to extrapyramidal motor systems. DA signalling in the dorsal striatum does not have a major influence in processing acute reward but plays a key role in the development of compulsive forms of reward seeking and consumption.
_
In the figure above, the brain on the left depicts dopaminergic afferents (light blue arrows) which originate in the ventral tegmental area (blue) and release dopamine in the nucleus accumbens (red) and many other limbic targets. Also shown are other monoaminergic nuclei — the noradrenergic locus coeruleus (green) and serotonergic dorsal raphe (yellow) — which modulate drug reward and other actions. The brain on the right highlights glutamatergic regions that are important for reward: medial prefrontal cortex (green), orbitofrontal cortex (yellow), anterior cingulate cortex (dark blue), thalamus (purple), hippocampus (orange), and amygdala (aqua), all of which send excitatory projections to the nucleus accumbens (red). Drugs of abuse alter this reward circuitry in complex ways, which lead to addiction.
_
Neural Circuits and Neurotransmitters in drug addiction:
There are many different drugs that are commonly abused in society, some being obtained legally such as alcohol, tobacco, and inhalants while others are obtained illegally, such as marijuana, amphetamine, cocaine, and heroin. Each drug has a differing chemical and pharmacological profile, can be administered via different routes, acts on different neurobiological systems, and undergoes different metabolic pathways. Nevertheless, all drugs appear to exert their initial effects on the mesocorticolimbic dopaminergic pathway which is heavily involved in reinforcement learning. Originating from dopaminergic neurons located in the ventral tegmental area (VTA) of the midbrain this pathway projects to the nucleus accumbens (NAcc) (motivation), amygdala (mediates association of reward with cues and negative reinforcement), ventral pallidum, hippocampus (limbic system associated with memory and learning), and forebrain, in particular the prefrontal cortex (PFC). The acute exposure to a drug results in a transient increase in the extracellular levels of dopamine in the NAcc and other projection sites, though the process via which this occurs may be dependent on the drug itself. For example, for alcohol, nicotine, opiates, cannabis, and inhalants this occurs via enhancement of dopamine release from presynaptic terminals primarily as a consequence of increased neuronal firing in the VTA. In comparison, for cocaine this occurs via the inhibition of presynaptic dopamine uptake by the dopamine transporter (DAT) or via actions on the vesicular monoamine transporter which actively reverses DAT function to elevate extracellular dopamine in the NAcc, which is the case for amphetamine. Following repeated exposure to a drug there is a progressive increase in basal levels of dopamine and the appearance of tolerance along with altered dopamine receptor expression. Should exposure to the drug cease, the levels of dopamine typically fall below normal baseline levels. Conditioned cues associated with drug taking can be sufficient to induce relapse and indeed these cues are powerful enough to activate dopaminergic brain regions in patients who regularly abuse cocaine.
However, the VTA contains a heterogeneous population of cells with approximately 65% being dopaminergic, 30% being gamma-aminobutyric acid (GABA)ergic, and 5% being glutamatergic. The primary afferents to the VTA are excitatory glutamatergic inputs from the PFC and inhibitory GABAergic inputs from medium spiny neurons (MSNs) in the NAcc, both of which can form feedback loops to regulate activity in this region though this can occur via different mechanisms. Drug-induced release of GABA, for example, may mediate local inhibitory feedback mechanisms by binding presynaptically to receptors expressed by MSNs themselves or enhance synaptic inhibition by binding postsynaptically at projection sites, thus causing disinhibition of downstream targets. This includes increasing dopamine release, as the firing rate of VTA neurons is under inhibitory control. The VTA also receives connections from regions such as the ventral pallidum, hippocampus, amygdala, lateral hypothalamus, and bed nucleus of the stria terminalis.
Aside from the VTA, the NAcc is believed to play a substantial role in mediating addictive behaviours. The NAcc is involved in the control of the motivational value of stimuli, reward reinforcement, and the mediation of impulsive choice. As well as dopaminergic inputs from the VTA, the NAcc also receives excitatory glutamatergic input from the PFC, amygdala, thalamus, and hippocampus thus serving as an interface between the limbic (processing of new and learnt information) and motor (task performance) pathways. Furthermore MSNs, the dominate cell type in the NAcc, can express either dopamine D1 receptors and thus form part of the direct pathway that results in neuronal excitation or D2 receptors and thus form part of the indirect pathway that results in neuronal inhibition. Consequently, the activation of these receptor subtypes and thus modulation of the direct and indirect pathways determine which signals are reinforced and which are suppressed. More recently human functional neuroimaging studies have identified that the PFC plays an important role in addiction. This is thought to occur, in part, via the PFCs ability to regulate the activity of neurons in reward associated nuclei (i.e., the NAcc and VTA) and its involvement in inhibitory control over behaviour, planning, and executing complex cognitive behaviours and executive function (i.e., awareness, decision making, and self-control). The PFC is also believed to play a pivotal role in mediating controlled drug intake with a transition from PFC to striatal control as drug use transfers into a compulsive behaviour. However, the highly integrated networks mediated by exposure to a drug of abuse and the different neurotransmitter systems they may act upon permit considerable crosstalk which acts to fine tune signal transmission, with the resultant outcome being driven by an integration of all incoming signals.
In addition to the involvement of select neural circuits, glutamate signaling has been recognized recently as an important response to numerous drugs of abuse including amphetamines, benzodiazepines, cocaine, ethanol, nicotine, and opiates (Cunha-Oliveira et al. 2008; Kalivas et al. 2009; Koob 2003). Disruption of normal glutamate transmission has been implicated in drug-dependent excito-toxicity, drug seeking, and reinstatement as well as reward and reinforcement (Kalivas et al. 2006, 2009; Knackstedt and Kalivas 2009). For many drugs of abuse, glutamate-opioid interactions are important determinants of addictive processes in the brain, and both stress and exposure to drugs of abuse engage the glutamatergic system at common neural sites (Fitzgerald et al. 1996). As with many addictive compounds, opiate abuse can lead to disturbances in excitatory amino acid signaling, particularly through homeostatic disruption of glutamate, a ubiquitous excitatory neurotransmitter in the nervous system (Cunha-Oliveira et al. 2008). As a result, numerous investigators have explored the nature of glutamate-opioid interactions in drug abuse in the hopes of better identifying potential therapeutic targets for the treatment of addiction.
_
Mechanism of drug addiction:
Drugs of abuse, despite diverse initial actions, produce some common effects on the ventral tegmental area (VTA) and nucleus accumbens (NAcc). Stimulants directly increase dopaminergic transmission in the NAcc. Opiates do the same indirectly: they inhibit GABA-ergic interneurons in the VTA, which disinhibits VTA dopamine neurons. Opiates also directly act on opioid receptors on NAcc neurons, and opioid receptors, such as D2 dopamine (DA) receptors, signal via Gi; hence, the two mechanisms converge within some NAcc neurons. The actions of the other drugs remain more conjectural. Nicotine appears to activate VTA dopamine neurons directly via stimulation of nicotinic cholinergic receptors on those neurons and indirectly via stimulation of its receptors on glutamatergic nerve terminals that innervate the dopamine cells. Alcohol, by promoting GABA receptor function, may inhibit GABA-ergic terminals in the VTA and disinhibit VTA dopamine neurons. It may similarly inhibit glutamatergic terminals that innervate NAcc neurons. Many additional mechanisms (not shown) are proposed for alcohol. Cannabinoid mechanisms are complex and involve the activation of cannabinoid CB1 receptors (which, similar to D2 and opioid receptors, are Gi-linked) on glutamatergic and GABAergic nerve terminals in the NAcc and on NAcc neurons themselves. Phencyclidine (PCP) may act by inhibiting postsynaptic NMDA glutamate receptors in the NAcc. Finally, evidence shows that nicotine and alcohol may activate endogenous opioid pathways and that these and other drugs of abuse (such as opiates) may activate endogenous cannabinoid pathways (not shown). PPT/LDT, peduncular pontine tegmentum/lateral dorsal tegmentum. Gi is the Gi alpha subunit of G protein that inhibits the production of cAMP from ATP and coupled to GPCR (vide infra).
_
Neurobiological substrates for the acute reinforcing effects of Drugs of Abuse:
_
“Natural” rewards (e.g., food and sex) and drugs of abuse mediate their reinforcing properties by targeting the meso-corticolimbic dopamine system, a brain circuit that is defined by projections from the ventral tegmental area to its major targets: the nucleus accumbens, a brain region involved in motor and limbic functions, and the prefrontal cortex, a brain region involved in decision making and executive functions (Koob 1992). Investigators increasingly recognize that most drugs of abuse share a common mechanism involving increases in extracellular concentrations of dopamine in the nucleus accumbens via activation of dopaminergic neurons in the ventral tegmental area (Willuhn et al. 2011). This working model predicts that dopamine release in response to drug-related stimuli will be enhanced over stimuli associated with natural reinforcers, which may result in aberrant goal-directed behaviors that contribute to drug addiction. Although dopamine is integral to the initial euphoric effects of several drugs of abuse (Di Chiara and Imperato 1988), several lines of evidence indicate that neural circuits outside the reward pathway become engaged and contribute to the initiation of drug-seeking activities (Goto and Grace 2005; Hyman et al. 2006).
All drugs of abuse, from nicotine to heroin, cause a particularly powerful surge of dopamine in the nucleus accumbens. The likelihood that the use of a drug or participation in a rewarding activity will lead to addiction is directly linked to the speed with which it promotes dopamine release, the intensity of that release, and the reliability of that release. Even taking the same drug through different methods of administration can influence how likely it is to lead to addiction. Smoking a drug or injecting it intravenously, as opposed to swallowing it as a pill, for example, generally produces a faster, stronger dopamine signal and is more likely to lead to drug misuse.
_____
Learning process:
Scientists once believed that the experience of pleasure alone was enough to prompt people to continue seeking an addictive substance or activity. But more recent research suggests that the situation is more complicated. Dopamine not only contributes to the experience of pleasure, but also plays a role in learning and memory — two key elements in the transition from liking something to becoming addicted to it.
According to the current theory about addiction, dopamine interacts with another neurotransmitter, glutamate, to take over the brain’s system of reward-related learning. This system has an important role in sustaining life because it links activities needed for human survival (such as eating and sex) with pleasure and reward. The reward circuit in the brain includes areas involved with motivation and memory as well as with pleasure. Addictive substances and behaviors stimulate the same circuit — and then overload it.
Repeated exposure to an addictive substance or behavior causes nerve cells in the nucleus accumbens and the prefrontal cortex (the area of the brain involved in planning and executing tasks) to communicate in a way that couples liking something with wanting it, in turn driving us to go after it. That is, this process motivates us to take action to seek out the source of pleasure.
______
Tolerance and compulsion:
Over time, the brain adapts in a way that actually makes the sought-after substance or activity less pleasurable. In nature, rewards usually come only with time and effort. Addictive drugs and behaviors provide a shortcut, flooding the brain with dopamine and other neurotransmitters. Our brains do not have an easy way to withstand the onslaught. Addictive drugs, for example, can release two to 10 times the amount of dopamine that natural rewards do, and they do it more quickly and more reliably. In a person who becomes addicted, brain receptors become overwhelmed. The brain responds by producing less dopamine or eliminating dopamine receptors — an adaptation similar to turning the volume down on a loudspeaker when noise becomes too loud. As a result of these adaptations, dopamine has less impact on the brain’s reward center. People who develop an addiction typically find that, in time, the desired substance no longer gives them as much pleasure. They have to take more of it to obtain the same dopamine “high” because their brains have adapted — an effect known as tolerance.
At this point, compulsion takes over. The pleasure associated with an addictive drug or behavior subsides — and yet the memory of the desired effect and the need to recreate it (the wanting) persists. It’s as though the normal machinery of motivation is no longer functioning. The learning process mentioned earlier also comes into play. The hippocampus and the amygdala store information about environmental cues associated with the desired substance, so that it can be located again. These memories help create a conditioned response — intense craving — whenever the person encounters those environmental cues. Cravings contribute not only to addiction but to relapse after a hard-won sobriety. A person addicted to heroin may be in danger of relapse when he sees a hypodermic needle, for example, while another person might start to drink again after seeing a bottle of whiskey. Conditioned learning helps explain why people who develop an addiction risk relapse even after years of abstinence.
______
It was once thought that surges of the neurotransmitter dopamine produced by drugs directly caused the euphoria, but scientists now think dopamine has more to do with getting us to repeat pleasurable activities (reinforcement) than with producing pleasure directly.
How does dopamine reinforce drug use?
Our brains are wired to increase the odds that we will repeat pleasurable activities. The neurotransmitter dopamine is central to this. Whenever the reward circuit is activated by a healthy, pleasurable experience, a burst of dopamine signals that something important is happening that needs to be remembered. This dopamine signal causes changes in neural connectivity that make it easier to repeat the activity again and again without thinking about it, leading to the formation of habits. Just as drugs produce intense euphoria, they also produce much larger surges of dopamine, powerfully reinforcing the connection between consumption of the drug, the resulting pleasure, and all the external cues linked to the experience. Large surges of dopamine “teach” the brain to seek drugs at the expense of other, healthier goals and activities.
Cues in a person’s daily routine or environment that have become linked with drug use because of changes to the reward circuit can trigger uncontrollable cravings whenever the person is exposed to these cues, even if the drug itself is not available. This learned “reflex” can last a long time, even in people who haven’t used drugs in many years. For example, people who have been drug free for a decade can experience cravings when returning to an old neighborhood or house where they used drugs. Like riding a bike, the brain remembers.
Why are drugs more addictive than natural rewards?
For the brain, the difference between normal rewards and drug rewards can be likened to the difference between someone whispering into your ear and someone shouting into a microphone. Just as we turn down the volume on a radio that is too loud, the brain of someone who misuses drugs adjusts by producing fewer neurotransmitters in the reward circuit, or by reducing the number of receptors that can receive signals. As a result, the person’s ability to experience pleasure from naturally rewarding (i.e., reinforcing) activities is also reduced. This is why a person who misuses drugs eventually feels flat, without motivation, lifeless, and/or depressed, and is unable to enjoy things that were previously pleasurable. Now, the person needs to keep taking drugs to experience even a normal level of reward—which only makes the problem worse, like a vicious cycle. Also, the person will often need to take larger amounts of the drug to produce the familiar high—an effect known as tolerance.
_
Mechanism of impaired dopamine signaling:
- There is increasing evidence in animal models and in humans that long-term exposure to drugs of abuse impairs dopamine neurons as well as dopamine signaling in the nucleus accumbens.
- This dampens natural reward and leaves the addict “unrewarded” (amotivational, depressed) without drug.
- This effect is mediated in part by actual physical shrinkage of VTA dopamine neurons in response to chronic drug administration.
Mechanism of shrinkage of VTA dopamine neurons:
Drugs of abuse decrease the size of VTA dopamine neurons by depriving the neurons of a crucial nerve growth factor, BDNF (brain-derived neurotrophic factor):
- Chronic drug exposure decreases BDNF signaling in the VTA.
- Loss of BDNF signaling mediates the decrease in VTA cell size and impairs reward behavior.
- Restoration of BDNF signaling prevents the ability of drug exposure to decrease the size of VTA neurons.
______
Presynaptic G Protein-Coupled Receptors: Gatekeepers of Addiction?
Drugs of abuse alter synaptic transmission, and these actions contribute to acute intoxication as well as the chronic effects of abused substances. Transmission at most mammalian synapses involves neurotransmitter activation of two receptor subtypes, ligand-gated ion channels that mediate fast synaptic responses and G protein-coupled receptors (GPCRs) that have slower neuromodulatory actions. The GPCRs represent a large proportion of neurotransmitter receptors involved in almost all facets of nervous system function. In addition, these receptors are targets for many pharmacotherapeutic agents. Drugs of abuse directly or indirectly affect neuromodulation mediated by GPCRs, with important consequences for intoxication, drug taking and responses to prolonged drug exposure, withdrawal and addiction. Among the GPCRs are several subtypes involved in presynaptic inhibition, most of which are coupled to the Gi/o class of G protein. There is increasing evidence that these presynaptic Gi/o-coupled GPCRs have important roles in the actions of drugs of abuse, as well as behaviors related to these drugs.
_
Receptors for various neurotransmitters, Dopamine (DA; D1- and D2-like receptors), Endocannabinoids (CB1 receptors), endogenous opioids (opioid receptor MOR) and glutamate (group II metabotropic glutamate (mGlu) receptors) are all GPCRs. G protein-coupled receptors (GPCRs; also known as transmembrane domain or TM receptors) are a large class of metabotropic receptors for neurotransmitters and hormones that couple to heterotrimeric G proteins. G proteins mediate a wide variety of cellular functions, including, but not limited to, altering the production of second messengers such as cyclic adenosine monophosphate (cAMP), mobilizing internal calcium stores, modulating ion channel function, altering neurotransmitter release, and influencing gene expression. Upon activation of a GPCR, the heterotrimeric G protein dissociates into α and βγ subunits, which then modulate the function of a diverse array of effector proteins to simultaneously influence many cellular functions (Latek et al., 2012). GPCRs are often classified by the G protein α subunits with which they prefer to interact. Gαi/o-coupled GPCRs are well-known modulators of neurotransmitter release. These receptors inhibit adenylyl cyclase to reduce production of the second messenger molecule cAMP. In addition to Gα-mediated effects, the Gβγ subunits liberated by GPCR activation can influence neuronal physiology via direct interactions with voltage-gated calcium channels, G protein-activated inward-rectifying potassium (GIRK) channels, and vesicular release machinery. In the context of the presynaptic axon terminal, each of these mechanisms can contribute to the inhibition of neurotransmitter release in response to GPCR activation
_
Preclinical models of drug abuse including investigator-administered passive drug exposure, conditioned place preference (CPP) and operant drug self-administration have been used to evaluate the multifaceted relationships between presynaptic GPCRs and drugs of abuse. Based on these studies, several prominent themes have emerged. First, GPCRs, particularly Dopamine (DA) receptors, are important mediators of the neurochemical and behavioral effects of drugs of abuse. Second, modulation of presynaptic GPCRs can alter neurochemical and behavioral responses to acute drug exposure in ways that would be predicted to either promote or constrain the rewarding and stimulating effects of a variety of abused drugs. Third, repeated exposure to drugs such as alcohol, cocaine, and nicotine produce long-lasting changes in the ability of some presynaptic GPCRs to modulate the release of neurotransmitters, particularly glutamate, in addiction-relevant circuits. Such drug-induced neuroadaptations are likely to play key roles in the transitions to problematic drug-related behaviors including escalation of drug taking and relapse following abstinence. Finally, pharmacological manipulation of presynaptic GPCRs can reduce seeking and taking of self-administered drugs in both rodent and non-human primate models, suggesting that targeting these receptors could be a viable therapeutic approach for treating addiction.
_
Classification of Addictive Drugs based on mechanism of signal transmission:
Addictive drugs are a chemically heterogeneous group with very distinct molecular targets. Moreover, an individual drug may have more than one molecular target. Here focus is on those mechanisms that are directly responsible for the increase in dopamine concentration. Three groups of addictive drugs are distinguished: (1) drugs that bind to G protein–coupled receptors (GPCRs)—this group includes the opioids, cannabinoids, and γ -hydroxy butyrate (GHB); (2) drugs that interact with ionotropic receptors or ion channels—this group includes nicotine, alcohol, and benzodiazepines; and (3) drugs that target monoamine transporters—this group comprises cocaine, amphetamine, and methylenedioxymetamphetamine (MDMA, ecstasy) (see table and figure below).
_
GPCRs that are of the Gi/o family inhibit neurons through post-synaptic hyperpolarisation and pre-synaptic regulation of the transmitter release. In the VTA, the action of these drugs is preferentially on the γ -aminobutyric acid (GABA) neurons that act as local inhibitory interneurons. They also inhibit glutamate release, but in the VTA their dominant mechanism of action is inhibition of GABA neurons leading to a net disinhibition of dopamine neurons and increased dopamine release. Addictive drugs that bind to ionotropic receptors and ion channels can have combined effects on dopamine neurons and GABA neurons, eventually leading to enhanced release of dopamine. Finally, addictive drugs interfering with monoamine transporters block the re-uptake of dopamine, or stimulate non-vesicular release of dopamine, causing an accumulation of extracellular dopamine in target structures.
_
All drugs of abuse interact initially with receptor or reuptake proteins. For example, opiates activate opioid receptors, and cocaine inhibits reuptake proteins for the monoamine neurotransmitters (which include dopamine, norepinephrine, and serotonin). These initial effects lead to alterations in the levels of specific neurotransmitters, or to different activation states of specific neurotransmitter receptors, in the brain. Opiate activation of opioid receptors, for example, leads to recruitment of inhibitory and related G proteins. This, in turn, leads to activation of K+ channels and inhibition of Ca2+ channels. Both are inhibitory actions, because more K+ flows out of the cell and less Ca2+ flows into the cell. Thus, the electrical properties of the target neurons are affected relatively rapidly by opiates. Recruitment of the inhibitory G protein also inhibits adenylyl cyclase, and reductions in cellular Ca2+ levels decrease Ca2+-dependent protein phosphorylation cascades, altering the activity of still additional ion channels. These effects, along with changes in many other neural processes within target neurons, contribute further to the acute effects of opiates. The sum of such changes presumably triggers the longer-term effects of the drugs that eventually lead to abuse, dependence, tolerance, and withdrawal.
_
In a nutshell
Mechanisms of primary effects of drugs:
- Intoxication via CNS G Protein-coupled receptors
-Marijuana
-Opioids
- Intoxication via direct central nervous system (CNS) toxicity
-Toxic inhalants and other highly lipophilic agents
- Psychostimulation (Agitated Delirium) mediated by multiple neurotransmitters (Epinephrine, Norepinephrine, Serotonin, Dopamine)
-Cocaine
-Methamphetamine
- Hallucinogenic effects mediated by Serotonin release (mediated at 5-HT-2A receptor)
-Ecstasy (MDMA)
-LSD
- Dissociation (“out-of-body”) mediated by NMDA Receptor mediated glutamate modulation
-Ketamine
-Phencyclidine (PCP)
-Dextromethorphan (DM)
- Sedation (with anxiolysis and amnesia) via Gamm-aminobutyric acid (GABA)
-Benzodiazepines
-Alcohol Intoxication
-Gamma Hydroxybutyrate (GHB)
_____
Drug induced dysfunction in the brain’s dopamine reward system:
When used over the long-term, all substances of abuse cause dysfunction in the brain’s dopamine reward system. For example, brain imaging studies in humans with addiction have consistently shown long-lasting decreases in a particular type of dopamine receptor, the D2 receptor, compared with non-addicted individuals (see figure below). Decreases in the activity of the dopamine system have been observed during withdrawal from stimulants, opioids, nicotine, and alcohol. Other studies also show that when an addicted person is given a stimulant, it causes a smaller release of dopamine than when the same dose is given to a person who is not addicted.
_
These PET scans compare the brain of an individual with a history of cocaine use disorder (middle and right) to the brain of an individual without a history of cocaine use (left). The person who has had a cocaine use disorder has lower levels of the D2 dopamine receptor (depicted in red) in the striatum one month (middle) and four months (right) after stopping cocaine use compared to the non-user. The level of dopamine receptors in the brain of the cocaine user are higher at the 4-month mark (right), but have not returned to the levels observed in the non-user (left).
__
Figure above shows relationship between dopamine (DA) D2 receptors in the brains of cocaine, alcohol, heroin and methamphetamine abusers.
_
These findings suggest that people addicted to substances experience an overall reduction in the sensitivity of the brain’s reward system (especially the brain circuits involving dopamine), both to addictive substances and also to natural reinforcers, such as food and sex. This is because natural reinforcers also depend upon the same reward system and circuits. This impairment explains why those who develop a substance use disorder often do not derive the same level of satisfaction or pleasure from once-pleasurable activities. This general loss of reward sensitivity may also account for the compulsive escalation of substance use as addicted individuals attempt to regain the pleasurable feelings the reward system once provided.
At the same time, a second process occurs during the withdrawal stage: activation of stress neurotransmitters in the extended amygdala. These stress neurotransmitters include corticotropin-releasing factor (CRF), norepinephrine, and dynorphin. Studies suggest that these neurotransmitters play a key role in the negative feelings associated with withdrawal and in stress-triggered substance use. In animal and human studies, when researchers use special chemicals called antagonists to block activation of the stress neurotransmitter systems, it has the effect of reducing substance intake in response to withdrawal and stress. For example, blocking the activation of stress receptors in the brain reduced alcohol consumption in both alcohol-dependent rats and humans with an alcohol use disorder. Thus, it may be that an additional motivation for drug and alcohol seeking among individuals with substance use disorders is to suppress overactive brain stress systems that produce negative emotions or feelings. Recent research also suggests that neuroadaptations in the endogenous cannabinoid system within the extended amygdala contribute to increased stress reactivity and negative emotional states in addiction.
The desire to remove the negative feelings that accompany withdrawal can be a strong motivator of continued substance use. This motivation is strengthened through negative reinforcement, because taking the substance relieves the negative feelings associated with withdrawal, at least temporarily. Of course, this process is a vicious cycle: Taking drugs or alcohol to lessen the symptoms of withdrawal that occur during a period of abstinence actually causes those symptoms to be even worse the next time a person stops taking the substance, making it even harder to maintain abstinence.
______
The role of corticotropin releasing factor and dynorphin in addiction:
The brain’s stress and reward systems are intricately linked. Moderate forms of stress, such as skydiving, can also activate the reward system. Excessive activation of the reward system, as in the case of excessive drug use, can also engage the brain’s stress system. As individuals who have become dependent on drugs lose normal function of aspects of their reward systems, they can gain activation of their stress system as well.
_
The driving force for negative reinforcement (where removal of an aversive stimulus, drug withdrawal, increases the probability of drug seeking and taking) is the negative emotional state of withdrawal mediated by stress‐related neurotransmitters, particularly corticotropin‐releasing factor (CRF) and dynorphin.
During acute stress, the peptide CRF is activated in the extended amygdala during withdrawal from abused substances that include alcohol, cocaine, cannabinoids, opioids, and nicotine. CRF antagonists decrease withdrawal‐induced anxiety‐like responses in animals, decrease the escalation associated with extended access to drugs of abuse, and decrease alcohol intake in alcohol‐dependent rats while having no effect on alcohol intake in nondependent rats.
_
During the development of dependence, not only a change in the function of neurotransmitters associated with the acute reinforcing effects of drugs (dopamine, opioid peptides, serotonin, GABA, and endocannabinoids) occurs but also recruitment of the brain stress system (CRF and norepinephrine) and dysregulation of the neuropeptide Y brain antistress system. Additionally, activation of the brain stress systems may not only contribute to the negative motivational state associated with acute abstinence but also may contribute to the vulnerability to stressors observed during protracted abstinence in humans. Another candidate for the aversive effects of drug withdrawal is the opioid peptide dynorphin. Dynorphin is an opioid peptide that acts primarily at kappa opioid receptors (KORs) and is generally associated with negative emotional states. Much evidence shows that dynorphin is increased in the nucleus accumbens in response to dopaminergic activation and, in turn, that overactivity of dynorphin systems can decrease dopaminergic function. Opioid agonists are aversive, and cocaine, opioid, and ethanol withdrawal is associated with increased dynorphin in the nucleus accumbens or amygdala. Dynorphin systems may also interact with the brain CRF systems and evidence shows that dynorphin drives CRF and CRF drives dynorphin.
_
Figure above shows neurocircuitry associated with the acute positive reinforcing effects of drugs of abuse and the negative reinforcement of dependence and how it changes in the transition from nondependent drug taking to dependent drug taking. Key elements of the reward circuit are dopamine and opioid peptide neurons that intersect at both the ventral tegmental area and nucleus accumbens and are activated during initial use and the early binge/intoxication stage. Key elements of the stress circuit are CRF and noradrenergic neurons that converge on GABA interneurons in the central nucleus of the amygdala and are activated during the development of dependence. DA, dopamine; NE, norepinephrine; GABA, -aminobutyric acid; CRF, corticotropin-releasing factor.
______
Drug use changes the Brain over Time:
- Dopamine levels increase
All addictive drugs affect brain pathways involving reward—that is, the dopamine system in the reward pathway. Within seconds to minutes of entering the body, drugs cause dramatic changes to synapses in the brain. By activating the brain’s reward circuitry, drugs deliver a jolt of intense pleasure.
- Synapse activity decreases
Drugs of abuse affect the brain much more dramatically than natural rewards, such as food and social interactions. To bring stimulation down to a more manageable level, the brain must try to adapt. One way the brain compensates is to reduce the number of dopamine receptors at the synapse. This down-regulation of D2 receptors might be why some people gradually develop addiction—the more individuals use drugs, the fewer D2 receptors they have, and the more they “need” drugs to feel normal. Others, who naturally have fewer D2 receptors, seem to be more prone to addiction—in other words, they are “instant addicts. In addition, sending neurons increase their number of dopamine transporters, more quickly clearing dopamine from the synapse. These changes make the brain less responsive to the drug, but they also decrease the brain’s response to natural rewards. Because of these changes, after the user has “come down,” they will need more of the drug next time they want to get high. This response is commonly referred to as “tolerance.”
- Brain connections are rewired
As the brain continues to adapt to the presence of the drug, regions outside of the reward pathway are also affected. Over time, brain regions responsible for judgment, decision-making, learning, and memory begin to physically change, making certain behaviors “hard-wired.” In some brain regions, connections between neurons are pruned back. In others, neurons form more connections. Once these changes take place, drug-seeking behavior becomes driven by habit, almost reflex. The drug user becomes a drug addict. After cocaine use, connections between neurons in the nucleus accumbens, part of the reward pathway, increase in number, size, and strength.
- Changes last long after use
Stopping drug use doesn’t immediately return the brain to normal. Some drugs have toxic effects that can kill neurons—and most of these cells will not be replaced. And while changes to connections between neurons in the brain may not be permanent, some last for months. Some research suggests the changes may even last for years. Long-lasting brain changes can make it challenging for addicts to stay drug-free. They often experience intense cravings, leading to relapse.
_____
Drug induced adaptations:
Despite the importance of numerous psychosocial factors, at its core, drug addiction involves a biological process: the ability of repeated exposure to a drug of abuse to induce changes in a vulnerable brain that drive the compulsive seeking and taking of drugs, and loss of control over drug use, that define a state of addiction. There are various types of molecular and cellular adaptations that occur in specific brain regions to mediate addiction-associated behavioral abnormalities. These include alterations in gene expression achieved in part via epigenetic mechanisms, plasticity in the neurophysiological functioning of neurons and synapses, and associated plasticity in neuronal and synaptic morphology mediated in part by altered neurotrophic factor signaling. Each of these types of drug-induced modifications can be viewed as a form of “cellular or molecular memory.”
- All drug-induced adaptations can be seen as types of “molecular or cellular memory:” the nerve cell undergoing such changes is different as a result of drug exposure and hence responds differently to that same drug, to other drugs, or to a host of other stimuli as a result.
- It is interesting that many, perhaps most, of the types of changes that have been associated with a state of addiction (e.g., altered gene transcription, epigenetics, synaptic and whole cell plasticity, and neuronal morphology and neurotrophic mechanisms) are also implicated in traditional forms of “behavioral memory” such as spatial memory, fear conditioning, and operant conditioning, among others.
- Among the brain regions affected by drugs of abuse are those that are key neural substrates for behavioral memory, including hippocampus, amygdala, and PFC. This coincides with the increasing realization that some of the most important features of addiction seen clinically (e.g., drug craving and relapse) reflect abnormalities in traditional memory circuits, with long-term memories of the drug experience serving as potent drivers of addiction pathology. Conversely, the brain’s reward regions (e.g., VTA and NAcc) potently influence behavioral memory.
Despite the fact that drugs of abuse have distinct chemical structures and act on distinct protein targets, it is striking that many prominent addiction-related adaptations are common to many, and in some cases all, drugs of abuse and likely contribute to shared features of an addiction syndrome. In contrast, many other drug-induced adaptations are specific to a given drug and may mediate more unique aspects of a given addiction.
_____
Drug-Induced Neuroplasticity:
The drug-induced release of dopamine triggers neuroplasticity (systematic changes in the synaptic signaling, or communication, between neurons in various reward regions of the brain). These neuroplastic changes are fundamental to learning and memory. Experience-dependent learning (such as that which occurs in repeated episodes of drug use) may invoke both long-term potentiation, in which the transmission of signals between neurons increases, and long-term depression, in which signal transmission decreases.
Neuroplastic changes triggered by drugs have been uncovered not only in the nucleus accumbens but also in the dorsal striatum (a region implicated in the encoding of habits and routines), the amygdala (a region involved in emotions, stress, and desires), the hippocampus (a region involved in memory), and the prefrontal cortex (a region involved in self-regulation and the attribution of salience. All these regions of the brain participate in the various stages of addiction, including conditioning and craving. These regions also regulate the firing of dopamine cells and the release of dopamine.
______
Repeated use of a substance “trains” the brain to associate the rewarding high with other cues in the person’s life, such as friends they drink or do drugs with, places where they use substances, and paraphernalia that accompany substance-taking. As these cues become increasingly associated with the substance, the person may find it more and more difficult not to think about using, because so many things in life are reminders of the substance.
Changes to two brain areas, the extended amygdala and the prefrontal cortex, help explain why stopping use can be so difficult for someone with a severe substance use disorder. The extended amygdala controls our responses to stress. If dopamine bursts in the reward circuitry in the basal ganglia are like a carrot that lures the brain toward rewards, bursts of stress neurotransmitters in the extended amygdala are like a painful stick that pushes the brain to escape unpleasant situations. Together, they control the spontaneous drives to seek pleasure and avoid pain and compel a person to action. In substance use disorders, however, the balance between these drives shifts over time. Increasingly, people feel emotional or physical distress whenever they are not taking the substance. This distress, known as withdrawal, can become hard to bear, motivating users to escape it at all costs. As a substance use disorder deepens in intensity, substance use is the only thing that produces relief from the bad feelings associated with withdrawal. And like a vicious cycle, relief is purchased at the cost of a deepening disorder and increased distress when not using. The person no longer takes the substance to “get high” but instead to avoid feeling low. Other priorities, including job, family, and hobbies that once produced pleasure have trouble competing with this cycle.
Healthy adults are usually able to control their impulses when necessary, because these impulses are balanced by the judgment and decision-making circuits of the prefrontal cortex. Unfortunately, these prefrontal circuits are also disrupted in substance use disorders. The result is a reduced ability to control the powerful impulses toward alcohol or drug use despite awareness that stopping is in the person’s best long-term interest. This explains why substance use disorders are said to involve compromised self-control. It is not a complete loss of autonomy—addicted individuals are still accountable for their actions—but they are much less able to override the powerful drive to seek relief from withdrawal provided by alcohol or drugs. At every turn, people with addictions who try to quit find their resolve challenged. Even if they can resist drug or alcohol use for a while, at some point the constant craving triggered by the many cues in their life may erode their resolve, resulting in a return to substance use, or relapse.
_
Addiction is associated with several types of long-lasting abnormalities, induced in brain reward regions by repeated exposure to drugs of abuse:
- Reduced responses to natural rewards.
- Sensitized responses to drugs of abuse and associated cues.
- Impaired cortical control over more primitive reward pathways.
______
Transcription Factors in Addiction:
The classic mechanism for regulation of gene expression is through the actions of transcription factors: proteins that, in response to cell signaling pathways, bind to specific sequences of DNA, generally in the promoter or enhancer regions of target genes, and increase or repress their expression by promoting or blocking the recruitment, respectively, of the RNA polymerase-II transcriptional complex. Transcription factors operate as part of large protein complexes, with their mechanisms of action eventually involving alterations in chromatin structure. Although neurons contain hundreds of transcription factors, studies of adaptations induced by drugs of abuse have focused primarily on a small subset.
_
DeltaFosB:
DeltaFosB – more commonly written as ΔFosB – is a truncated splice variant of the FOSB gene. ΔFosB has been implicated as a critical factor in the development of virtually all forms of behavioral and drug addictions. In the brain’s reward system, it is linked to changes in a number of other gene products, such as CREB and sirtuins. In the body, ΔFosB regulates the commitment of mesenchymal precursor cells to the adipocyte or osteoblast lineage.
In the nucleus accumbens, ΔFosB functions as a “sustained molecular switch” and “master control protein” in the development of an addiction. In other words, once “turned on” (sufficiently overexpressed) ΔFosB triggers a series of transcription events that ultimately produce an addictive state (i.e., compulsive reward-seeking involving a particular stimulus); this state is sustained for months after cessation of drug use due to the abnormal and exceptionally long half-life of ΔFosB isoforms. ΔFosB expression in D1-type nucleus accumbens medium spiny neurons directly and positively regulates drug self-administration and reward sensitization through positive reinforcement while decreasing sensitivity to aversion. Based upon the accumulated evidence, a medical review from 2014 argued that accumbal ΔFosB expression can be used as an addiction biomarker and that the degree of accumbal ΔFosB induction by a drug is a metric for how addictive it is relative to others.
Role in addiction:
Chronic addictive drug use causes alterations in gene expression in the mesocorticolimbic projection, which arise through transcriptional and epigenetic mechanisms. The most important transcription factors that produce these alterations are ΔFosB, cyclic adenosine monophosphate (cAMP) response element binding protein (CREB), and nuclear factor kappa B (NF-κB). ΔFosB is the most significant biomolecular mechanism in addiction because the overexpression of ΔFosB in the D1-type medium spiny neurons in the nucleus accumbens is necessary and sufficient for many of the neural adaptations and behavioral effects (e.g., expression-dependent increases in drug self-administration and reward sensitization) seen in drug addiction. ΔFosB overexpression has been implicated in addictions to alcohol (ethanol), cannabinoids, cocaine, methylphenidate, nicotine, opioids, phencyclidine, propofol, and substituted amphetamines, among others. ΔJunD, a transcription factor, and G9a, a histone methyltransferase, both oppose the function of ΔFosB and inhibit increases in its expression. Increases in nucleus accumbens ΔJunD expression (via viral vector-mediated gene transfer) or G9a expression (via pharmacological means) reduces, or with a large increase can even block, many of the neural and behavioral alterations seen in chronic drug abuse (i.e., the alterations mediated by ΔFosB).
_
ΔFosB also plays an important role in regulating behavioral responses to natural rewards, such as palatable food, sex, and exercise. Natural rewards, similar to drugs of abuse, induce gene expression of ΔFosB in the nucleus accumbens, and chronic acquisition of these rewards can result in a similar pathological addictive state through ΔFosB overexpression. Consequently, ΔFosB is the key mechanism involved in addictions to natural rewards (i.e., behavioral addictions) as well; in particular, ΔFosB in the nucleus accumbens is critical for the reinforcing effects of sexual reward. Research on the interaction between natural and drug rewards suggests that dopaminergic psychostimulants (e.g., amphetamine) and sexual behavior act on similar biomolecular mechanisms to induce ΔFosB in the nucleus accumbens and possess bidirectional reward cross-sensitization effects that are mediated through ΔFosB. This phenomenon is notable since, in humans, a dopamine dysregulation syndrome, characterized by drug-induced compulsive engagement in natural rewards (specifically, sexual activity, shopping, and gambling), has also been observed in some individuals taking dopaminergic medications.
_
Plasticity in cocaine addiction:
ΔFosB levels have been found to increase upon the use of cocaine. Each subsequent dose of cocaine continues to increase ΔFosB levels with no ceiling of tolerance. Elevated levels of ΔFosB leads to increases in brain-derived neurotrophic factor (BDNF) levels, which in turn increases the number of dendritic branches and spines present on neurons involved with the nucleus accumbens and prefrontal cortex areas of the brain. This change can be identified rather quickly, and may be sustained weeks after the last dose of the drug.
_
Mechanisms of dependence:
Psychological dependence:
Two factors have been identified as playing pivotal roles in psychological dependence: the neuropeptide “corticotropin-releasing factor” (CRF) and the gene transcription factor “cAMP response element binding protein” (CREB). The nucleus accumbens (NAcc) is one brain structure that has been implicated in the psychological component of drug dependence. In the NAcc, CREB is activated by cyclic adenosine monophosphate (cAMP) immediately after a high and triggers changes in gene expression that affect proteins such as dynorphin; dynorphin peptides reduce dopamine release into the NAcc by temporarily inhibiting the reward pathway. A sustained activation of CREB thus forces a larger dose to be taken to reach the same effect. In addition, it leaves the user feeling generally depressed and dissatisfied, and unable to find pleasure in previously enjoyable activities, often leading to a return to the drug for another dose.
In addition to CREB, it is hypothesized that stress mechanisms play a role in dependence. Koob and Kreek have hypothesized that during drug use, CRF activates the hypothalamic–pituitary–adrenal axis (HPA axis) and other stress systems in the extended amygdala. This activation influences the dysregulated emotional state associated with psychological dependence. They found that as drug use escalates, so does the presence of CRF in human cerebrospinal fluid. In rat models, the separate use of CRF inhibitors and CRF receptor antagonists both decreased self-administration of the drug of study. Other studies in this review showed dysregulation of other neuropeptides that affect the HPA axis, including enkephalin which is an endogenous opioid peptide that regulates pain. It also appears that µ-opioid receptors, which enkephalin acts upon, is influential in the reward system and can regulate the expression of stress hormones. Increased expression of AMPA receptors in nucleus accumbens MSNs is a potential mechanism of aversion produced by drug withdrawal.
Physical dependence:
Upregulation of the cAMP signal transduction pathway in the locus coeruleus by CREB has been implicated as the mechanism responsible for certain aspects of opioid-induced physical dependence. The temporal course of withdrawal correlates with LC firing, and administration of α2 agonists into the locus coeruleus leads to a decrease in LC firing and norepinephrine release during withdrawal. A possible mechanism involves upregulation of NMDA receptors, which is supported by the attenuation of withdraw by NMDA receptor antagonists. Physical dependence on opioids has been observed to produce an elevation of extracellular glutamate, an increase in NMDA receptor subunits NR1 and NR2A, phosphorylated CaMKII, and c-fos. Expression of CaMKII and c-fos is attenuated by NMDA receptor antagonists, which is associated with blunted withdrawal in adult rats, but not neonatal rats. While acute administration of opioids decreases AMPA receptor expression and depresses both NMDA and non-NMDA excitatory postsynaptic potentials in the NAcc, withdrawal involves a lowered threshold for LTP and an increase in spontaneous firing in the NAcc.
_____
_____
Reinforcement:
Reinforcement is a theoretical construct by which a stimulus (e.g., an unconditioned stimulus, such as the drug itself or drug withdrawal, or a conditioned stimulus, such as drugtaking paraphernalia) increases the probability of a response (e.g., continued use of the drug).
The brain reward system is critical for survival. The hedonic effects produced by eating, exercise and sexual activity provide important motivational effects that increase the likelihood of future engagement in these critical activities (e.g. positive reinforcement). The reward system is also essential for important negative hedonic responses in which aversive or unpleasant events (e.g. sickness, bodily harm) increase the likelihood of behaviors that will avoid or relieve these negative states (e.g. negative reinforcement).
Several sources of reinforcement may contribute to addiction. In positive reinforcement, a rewarding stimulus (e.g., drug-induced euphoria) directly increases the probability of a response (e.g., continued drug use). In negative reinforcement, the incentive for drug use is relief of a painful or unpleasant state (i.e., the physiological and motivational symptoms of withdrawal). In addition to their direct reinforcing effects, drugs can motivate behavior indirectly through environmental stimuli with which the drugs have become associated (i.e., conditioned reinforcement). For example, the locations where drugs are taken or the paraphernalia used for their administration may themselves elicit a druglike state of euphoria in the absence of the drug (i.e., conditioned positive reinforcement). Conversely, exposure to stimuli associated with periods of abstinence may produce symptoms of withdrawal (i.e., conditioned negative reinforcement).
_
Craving is due to reinforcing effects of drugs:
Most contemporary explanations of addiction suggest that addicts are motivated to take drugs (crave drugs) for one of two reasons. Drug craving is characterized by both the desire to experience the positive hedonic effects of the drug … and the desire to avoid aversive withdrawal symptoms. That is, it is generally thought that addicts are motivated to take drugs either for the pleasure drugs produce (basically to achieve remembered pleasure), or to avoid the unpleasant consequences of withdrawal.
_
Two factors that modulate behavior—reinforcement and neuroadaptation—contribute to the addictive process. Neuroadaptation refers largely to the processes by which initial drug effects are either enhanced (i.e., sensitization) or attenuated (i.e., counteradaptation) by repeated drug exposure. Drug-related responses (i.e., reinforcement) are modulated by the neuroadaptive changes that occur with drug exposure. Working together, these factors appear to motivate the initial, short-term (i.e., acute) response to a drug and the establishment of the long-term (i.e., chronic) craving for the drug that characterizes addiction. In addition, some neuroadaptive changes may be permanent, producing the persistent sense of discomfort during abstinence that leads to reinstatement of drug use (i.e., relapse).
_
Limitations of negative reinforcement models:
Despite the intuitive appeal of withdrawal avoidance models many authors have pointed out the short-comings of negative reinforcement models in general as explanations for addiction. For example, drugs that do not produce strong withdrawal syndromes, such as psychostimulants, can be highly addictive. Conversely, there are drugs that produce tolerance and withdrawal syndromes but do not support compulsive patterns of use. The latter compounds include some tricyclic antidepressants, anticholinergics and kappa opioid agonists. Thus, as put by Jaffe, “there is little correlation between the visibility or physiological seriousness of withdrawal signs and their motivational force”. Another problem for withdrawal-based explanations is that drug craving is often elicited by drug administration itself, in association with euphorigenic effects, at the moments when withdrawal symptoms should be at their weakest. Similarly, in animals trained to self-administer heroin, reinstatement of drug-taking behavior following extinction is more potently elicited by a priming injection of heroin, which elicits a drug-like effect, than by the injection of an opioid antagonist, which induces withdrawal signs. For human addicts, the prolonged cessation of drug use, during which time withdrawal symptoms decay, is by no means a guarantee of a cure, as relapse to compulsive use even long after withdrawal is over remains a major problem in addiction. In conclusion, although there is no doubt that under some circumstances the desire to avoid withdrawal can be a potent motive for drug use, for these and other reasons many authors have suggested that models of addiction based on the alleviation of withdrawal symptoms (whether “physical” or “psychological”) are neither necessary nor sufficient to explain compulsive drug-seeking and drug-taking behavior.
_
Limitations of drug pleasure (hedonic/positive reinforcement) models:
Drugs are addicting because they produce positive affective states that people label with words such as pleasure or euphoria, and these states are what addicts seek. This pleasure-seeking view of addiction is the simple common-sense view of addiction. People want drugs (are motivated to seek and take drugs) because they like drugs (because drugs give pleasure). In this view the motivation to take drugs (drug wanting) is directly attributable to the ability of drugs to produce pleasure, i.e. there is a necessary causal relationship between wanting drugs and liking drugs.
It is probably true that often people are initially motivated to take drugs because of the ability of drugs to produce positive affective states (and because their peers are doing it, and for many other complicated psychosocial reasons), but in the addict the association between the hedonic consequences of drug consumption and the ability of drugs and drug-related stimuli to motivate behavior often become dissociated, revealing that the relationship between the motivational force of drugs and their hedonic consequences may not be a necessary causal relationship. As Dews cautioned many years ago, “… it was supposed that the prediction of addiction liability was essentially equivalent to prediction of euphorigenic power. As with most self-evident ideas, the mere matter of there being essentially no evidence in favor of it, and much against it, had little effect on its acceptance”.
Perhaps the most compelling evidence against the idea that the ability of drugs to promote drug-taking is directly attributable to their subjective pleasurable effects comes from studies showing that subjective states are often poorly correlated with drug-taking.
First, drug-taking may increase dramatically over time as an addiction develops, but the pleasure induced by a given dose of a drug is not reported to increase. If addicts craved drugs in proportion to their ability to produce pleasure, then craving late in addiction ought not to be stronger then craving after the initial drug experience—but of course that is not the case.
Secondly, after pharmacological manipulations there is often a dissociation between the reported subjective effects of cocaine and cocaine-taking behavior. For example, Haney et al. reported recently that pergolide decreased cocaine’s cardiovascular effects, decreased ratings of its subjective effects (“high”, “stimulated”), increased ratings of “I want cocaine”, while having no effect whatsoever on cocaine self-administration behavior. Similarly, Haney et al. reported: “that even a 50% decrease in certain of cocaine’s subjective effects by ABT-431 … did not shift cocaine self-administration” . Along the same lines, Comer et al. reported that doses of intranasal and intravenous heroin that maintained the same “breakpoint” on a progressive ratio schedule resulted in very different subjective ratings of “high”.
Thirdly, it has been reported that people will work for low doses of morphine or cocaine that produce no subjective pleasure at all; doses that indeed produce no reported subjective effects of any kind. In summarizing their findings Lamb et al. concluded: “The reinforcing effects of morphine can occur in the absence of self-reported subjective effects and thus, do not appear to be causally related to drug-liking or euphoria”. These kinds of data are very important because they establish that the motivation to take drugs (drug wanting) is not always directly attributable to the subjective pleasurable effects of drugs (drug liking), and it is possible this is especially true in addicts. That is, one must consider the possibility that in addicts the subjective pleasurable effects and the motivational effects of drugs are merely correlated effects. They occur together most of the time, but they can be dissociated and there is no necessary causal relationship between them.
______
Incentive–sensitization hypothesis:
If compulsive drug-seeking and drug-taking behavior are often not motivated by either the desire to obtain pleasure or by the desire to relieve withdrawal, then what motivates addictive behavior in these instances? Why do addicts compulsively seek drugs? Researchers have attempted to address these questions by proposing the concept of “incentive–sensitization”. This focuses on sensitization, whereby drugs alter the reward circuitry to cause increased assignment of incentive salience to drug cues, effectively making drug-associated environmental stimuli more difficult to ignore and leading to intense drug craving and relapse. Pathological drug-induced changes in the reward circuitry further impair behavioral control.
The basic thesis of the incentive–sensitization view of addiction can be summarized in four points.
(1) Potentially addictive drugs share the ability to produce long-lasting adaptations in neural systems (i.e. addictive drugs change the brain).
(2) The brain systems that are changed include those normally involved in the process of incentive motivation and reward.
(3) The critical neuroadaptations for addiction render these brain reward systems hypersensitive (“sensitized”) to drugs and drug associated stimuli.
(4) The brain systems that are sensitized do not mediate the pleasurable or euphoric effects of drugs (drug “liking”), but instead they mediate a subcomponent of reward that researchers have termed incentive salience or “wanting”. It is the psychological process of incentive salience specifically that is responsible for instrumental drug-seeking and drug-taking behavior (drug “wanting”).
______
______
Addicted versus non-addicted brain:
“Even for the normal person, drugs change the brain just like they change the brain of the addict…But eventually, the inhibitory neurotransmitters of the normal person’s brain put on the brakes…and the persons stops drinking or drugging. Those brakes don’t work in the addict’s brain. They were made defective or they’ve burned out…”
~Dr. Akikur Mohammad, M.D., The Anatomy of Addiction
______
______
Common liability to addiction and gateway hypothesis:
Two competing concepts address the development of involvement with psychoactive substances: the “gateway hypothesis” (GH) and common liability to addiction (CLA). These are the theory of biological alterations in the brain due to an earlier drug use and the theory of similar attitudes across different drugs.
_
Gateway hypothesis (GH):
Gateway hypothesis means the use of a psychoactive drug can be coupled to an increased probability of the use of further drugs by possibly causing biological alterations in the brain due to the earlier drug use. Research concerned with the GH, during the 44 years since it was advanced (Kandel, 1975), has commanded substantial attention due to the high practical value that has been ascribed to the observation of a sequential order in drug use initiation. GH was predated by the similar “stepping-stone” theory that first appeared in the 1930s and assumed that consumption of a “soft” drug such as marijuana inexorably sets an individual on a trajectory to addiction to hard drugs. GH relaxes the inevitability assumption, but still posits that substance use starting with a licit substance and progressing to marijuana leads to use of other, “harder” drugs. Marijuana is thus designated the “gateway” drug in this progression, although originally, and sometimes still, this role has been assigned to alcohol and tobacco (Grunberg and Faraday, 2002; Kandel, 1975). Because it is frequently observed that “very few individuals who have tried cocaine and heroin have not already used marijuana; the majority have previously used alcohol or tobacco” (Kandel, 2003, p. 482), the conclusion is drawn (Kandel, 2002a) that “there is a progressive and hierarchical sequence of stages of drug use that begins with tobacco or alcohol, two classes of drugs that are legal, and proceeds to marijuana, and from marijuana to other illicit drugs, such as cocaine, methamphetamines, and heroin.
The gateway drug theory, or the idea that using some substances increase the probability of using more dangerous drug later in life, could point to the ways that recreational use leads to addiction. These substances are often used by children and young adults in a social atmosphere and are viewed as ‘a way to have fun,’ but using a “less dangerous” drug recreationally can often lead to using or becoming addicted to “harder” drugs.
The sequence of drug use initiation is thus the essence of the GH. Accordingly, it is drug use itself that is viewed as the cause of drug use development. Likewise, the “stages” are defined in a circular manner: a stage is said to be reached when a certain drug(s) is used, but this drug is supposed to be used only upon reaching this stage. In other words, the stage both is identified by the drug and identifies that drug. In effect, the drug is identical to the stage (“marihuana is a crucial stage . . .”) (Kandel, 1975). There is no process or organismic characteristic, separate from drug use per se, which is presumed to cause or underlie the supposed developmental staging indicated by, and identical to, drug milestones. Moreover, the notion of “stage” itself is redefined from its common meaning, such that the later stages are assumed to be reachable, albeit less frequently, before the earlier ones. This renders the GH incongruent with the conventional biological developmental framework (cf. stages of embryonic development).
Alterations in the brain:
Rats repeatedly injected with tetrahydrocannabinol – earlier in life – increased the self-administration of heroin (results based on 11 male rats), morphine (study based on 12 male rats) and also nicotine (34 rats). There were direct indications that the alteration consisted of lasting anatomical changes in the reward system of the brain. In mice nicotine increased the probability of later consumption of cocaine and the experiments permitted concrete conclusions on the underlying molecular biological alteration in the brain. The importance of these findings for the reward system in the human brain in relation to the liability to the use of further drugs has been pointed out in several reviews. The biological changes in mice correspond to the epidemiological observations in humans that nicotine consumption is coupled to an increased probability of later use of cannabis and cocaine. Animal studies suggest that caffeine can prime the teen brain for later drug use.
Examples of trends:
A study of drug use of 14,577 US 12th graders showed that alcohol consumption was associated with an increased probability of later use of tobacco, cannabis, and other illegal drugs. Adolescents who smoked cigarettes before age 15 were up to 80 times more likely to use illegal drugs. Large-scale longitudinal studies in the UK and New Zealand from 2015 and 2017 showed an association between cannabis use and an increased probability of later disorders in the use of other drugs. Students who regularly consume caffeinated energy drinks have a greater risk of alcohol use disorder, cocaine use and misuse of prescription stimulants. The elevated risk remains after accounting for prior substance use and other risk factors.
______
Common liability to addiction:
In contrast to the GH, which addresses only the order of drug use initiation, the concept of common (general) liability to addiction (CLA) involves mechanisms and biobehavioral characteristics that pertain to the entire course of development of the disorder and changes in the risk. The CLA concept also overlaps with the psychological and psychopathological constructs that have been previously used to explicate addiction and its mechanisms. Liability denotes a latent (unobservable) quantitative trait that, when measured, “would give us a graded scale of the degree of affectedness or of normality” (Falconer, 1965). These two latter broad phenotypic categories are divided by a latent threshold on the liability axis. An individual’s quantitative liability phenotype at any time point, above or below the threshold, represents a value within the norm of reaction of the genotype (Dobzhansky, 1951), the genetically determined distribution of all phenotypic values for a trait in an individual for all possible environmental conditions. A probability distribution that can be considered at each time point as well as within the entire developmental trajectory, the norm of reaction fluctuates across time in accordance with the ontogenesis of liability, the changing propensity to (risk for) or severity of the disorder.
Theoretically, the liability distribution in the population may range from the individual norms of reaction that do not include the disorder (at least, in the present range of environmental conditions) and thus totally resistant (resilient)—up to the phenotypes corresponding to the most severe fastest-developing disorder. The “gradations of normality” (the subthreshold liability phenotypes) correspond to variation in the risk (propensity), whereas “gradations of affectedness” (the suprathreshold phenotypes, which are likely to be assigned a clinical diagnosis) correspond to variation in severity, comprising the two parts of the liability distribution relative to the threshold. Applied to addiction (Conway et al., 2010; Vanyukov et al., 2003a), severity refers to the degree of maladaptive compulsive drug-seeking and using behavior displayed by an individual and corresponds to variation in liability above the diagnostic threshold. Propensity refers to the probability of the disorder onset and corresponds to liability variation below the diagnostic threshold. Variation in propensity may manifest as psychological/behavioral precursors of addiction. These precursors have been conceptualized as problem behavior (Jessor and Jessor, 1977), overlapping with the CLA (Vanyukov et al., 1994, 1996; Vanyukov and Tarter, 2000). This particularly concerns propensity mechanisms preceding drug involvement as well as its changes—the domain pertaining to the focus of the GH. The GH perspective has been presented as a “fundamental theoretical antithesis” (Kandel and Yamaguchi, 1999) to this concept. Such a juxtaposition is not, however, fully adequate, as the problem behavior and liability theories address mechanisms of addiction development, whereas the GH at best only describes a pattern of drug use initiation.
Whereas the “gateway” hypothesis does not specify mechanistic connections between “stages”, and does not extend to the risks for addictions, the concept of common liability to addictions incorporates sequencing of drug use initiation as well as extends to related addictions and their severity, provides a parsimonious explanation of substance use and addiction co-occurrence, and establishes a theoretical and empirical foundation to research in etiology, quantitative risk and severity measurement, as well as targeted non-drug-specific prevention and early intervention. The scientific discussion is dominated by these two concepts, which appear to cover almost all possible causal connections if appropriately combined.
_
According to the concept of similar attitudes across different drugs (common liability to addiction), a number of personal, social, genetic and environmental factors can lead to a generally increased interest in various drugs. The sequence of first-time use would then depend on these factors. Violations of the typical sequence of first-time drug usage give credit to this theory. For example, in Japan, where cannabis use is uncommon, 83.2% of the users of illicit drugs did not use cannabis first. The concept received additional support from a large-scale genetic analysis that showed a genetic basis for the connection of the prevalence of cigarette smoking and cannabis use during the life of a person.
On the other hand, results of a twin study presented indications that familial genetic and familial environmental factors do not fully explain these associations, and are possibly only relevant for sequences of some drugs. In 219 same-sex Dutch identical and non-identical twin pairs, one co-twin had reported cannabis use before the age of 18 whereas the other had not. In the cannabis group the lifetime prevalence of later reported use of party drugs was four times higher and the lifetime prevalence of later reported use of hard drugs was seven times higher than in the non-cannabis group. The authors concluded that at least family influences – both genetic and social ones – could not explain the differences. The study noted that, besides a potential causal role of cannabis use, non shared environment factors could play a role in the association such as differing peer affiliations that preceded the cannabis use.
Gene Expression altered by drug abuse support gateway hypothesis:
Irrespective of the presence or absence of genes that may increase an individual’s vulnerability to become addicted, human postmortem studies have shown that the expression of numerous genes is altered in the brain of addicted patients. Chronic cocaine use, for example, differentially alters the expression of up to 49 transcripts in the NAcc including those involved in signal transduction, synaptic function, and DNA to RNA processing. Similarly, significant upregulation of numerous transcripts, including glutamate receptors, have been reported using targeted microarrays on the VTA from cocaine overdose victims. Importantly changes to transcripts reported following chronic cocaine use correspond to altered protein expression in both of these studies. In support of the observations in humans, up to 295 genes were differentially regulated after 1 h of nicotine treatment in cultured neuron-like SH-SY5Y cells, including those involved in neural development, synaptic plasticity, neuronal survival, immune responses, and cellular metabolism. Indeed, genes affected by drugs of abuse can be subcharacterised into those relating to the extracellular matrix, synaptic plasticity and efficacy, receptors, ion channels and transporters, signal transduction, and cell death, among others.
______
______
Growing plants to produce drugs:
The production of drugs may be divided into three categories: (a) those processes which require only plant products, (b) those involving a semi-synthetic process where natural materials are partly changed by synthetic substances to produce the final product and (c) processes which use only manmade chemicals to produce consumable drugs. Examples of these three are (a) opium gathered in the fields for home use, (b) coca bush leaves processed to make cocaine and (c) narcotic or psychotropic drugs made entirely in the laboratory or factory.
Long before the world economy felt the impact of globalization of money, markets and products, illicit drugs moved internationally from producer countries in less developed areas of the world to consumer countries that were usually more developed. Production in rural areas was transported to and sold in other continents after enormous price increases along the way, providing high profit and risk incentive to traffickers. The end user has often been a poor person who buys drugs before the necessities of life.
Estimates of illicit drug production come from several sources. Systematic attempts to provide information about the amount of opiates or coca produced may employ high technology satellite mapping, ground surveys, agronomic characteristics or consumption figures. Political factors may also affect the process of preparing estimates. Experts have called the production estimate process one of making “best guesses”.
Many experts think that the first stage, when plants are grown in the fields or consumable drugs are produced in the laboratory, is the most vulnerable point in the chain of illicit production, distribution and consumption. The second major stage, the distribution phase, is also considered by some as an equally good intervention point for drug control purposes. However, the potential for easy movement, disguise and diversion of drug shipments and the vast numbers of shipments of small quantities of drugs decrease the yield of enforcement for each unit of intervention effort. The third stage of possible intervention is at the time of consumption. Here, a particularly vulnerable point is when drugs pass from dealers to consumers. This stage is often a target of law enforcement, especially if a strategy of “buy and bust” is followed.
Recently, emphasis has been placed on drug demand, mostly in public statements and commentary in the media. Whereas the obligations of parties to the conventions on drug control concerning reductions in illicit supply are clearly defined, implementation of demand-side obligations of States parties are not specified in the conventions and depend on the ability of States parties to carry out education, information, treatment and rehabilitation. To some observers, this emphasis in the treaty system gives it the appearance of favouring supply-side mechanisms. The consequences of this apparent supply-demand imbalance for bringing drug control into closer collaboration with human and social development programmes are not known.
Since some drugs are more available and used more often than others, the questions that arise are the following: what pharmacological properties of specific drugs, what personal characteristics of the users and what social or cultural factors in a given country influence the attractiveness of a drug? Or, asked another way, why do users want certain drugs as opposed to others and how does this influence their willingness to pay for them? Studies suggest that production and distribution of illicit drugs follow supply-demand principles with some allowance for the illegal nature of the product. In terms of their impact on global drug problems and their large-scale financial implications, opium-heroin and coca-cocaine are the primary drugs of current interest.
How much opium-heroin and coca-cocaine are produced and where? Illicit production figures are not precise, but gross amounts produced in various countries have been estimated. Based on the integration of information from nine country studies, an expert has noted that many variables detract from the precision of any attempt at assessment. Nevertheless, that study provides gross estimates of illicit drug production for coca, cocaine, opium, heroin and cannabis for major supplier countries.
Adding the gross estimates for these nine countries results in estimated opium production of 3,045 tonnes. This is not considered an estimate of world production, for two reasons: (a) some countries have not been included in these estimates (Afghanistan, for example, had an estimated cultivation of 19,470 hectares in 1992 and produced 640 tonnes of opium that year according to the United States Department of State); and (b) many unexamined assumptions have been made in preparing these estimates. For heroin, the comparable gross estimate for the nine-country production is 246 tonnes.
In contrast to opium production, coca leaf and cocaine production take place in relatively few countries. The estimates made by the above-cited commentator are not highly divergent from those provided for coca and cocaine by the Department of State. The approximate total for the three producer countries (Peru, Bolivia and Colombia) are coca leaf, 330,000 tonnes, and cocaine, 322 tonnes.
Several features of this picture are noteworthy: (a) the major production sources of drugs are quite varied, not limited to one or two producer countries or simply one region of the world; (b) according to 1992 GNP per capita data, major production of opium and coca takes place in less developed countries, many of which have considerable economic, agricultural, political and social problems; and (c) according to all estimates, the total amount of production is extremely high. If alcohol and tobacco production amounts were added to those of opium, cocaine, cannabis and psychotropic drugs to form an aggregated estimate of addictive substances production, the picture that emerges is one of enormous supply of these substances.
One commentator has described the illicit drug industry during the production phase, as “labor intensive, decentralized, growth-pole oriented, cottage-industry promoting, and foreign exchange earning desirable features of rural development in economically stagnating areas”. He has found agreement on the following points: 1) the production of marijuana, heroin, and cocaine/crack is increasing, especially cocaine/crack; 2) cocaine traffickers, now finding their supply substantially exceeding current market demand in the United States, are vigorously opening new markets in Canada, Great Britain, Western and Eastern Europe (with Spain and Italy as principal ports of entry for Europe); 3) the increasing supply of illicit drugs relative to current demand contributes to additional violence as international cartels and domestic gangs war over market turf, and 4) the policy instruments designed so far to curtail the demand for, suppress the traffic in, and control the supply of illicit drugs have not produced satisfactory results.
It should be noted that production of illicit drugs is often inexpensive. Labour costs are low and even if workers demand decent wages, the percentage of the total income required for wages and other expenses is still very low.
______
Distribution and illicit trafficking:
Illicit drug trafficking takes place in most countries of the world. Recognition of illegal importation and distribution, a criminal activity frequently involving foreigners, is politically less troublesome than purely domestic illicit production or consumption. The involvement of outsiders makes smuggling or illicit dealing appear less of a home-based problem. Few countries are immune to drug abuse problems. Indeed, in most countries, what were formerly thought of as safe places – religious, penal or educational institutions – have now been found to have some form of drug problems. For example, illicit traffic in drugs is now common in prisons because a significant percentage of inmates are drug abusers.
Individuals acting alone do not usually move significant quantities of drugs, hence the focus on control of supply is normally on organized groups or cartels. Traffic patterns tend to follow drug types and country of origin. Cocaine trafficking, for example, begins in the Andean region and spreads northward through Central America, Mexico and the Caribbean region to end-points in North America, Europe and elsewhere. Major heroin trafficking originates in South-west and South-east Asia with final processing of the consumable product close to the point of origin. The route of distribution may involve many countries and territories, such as Malaysia, Thailand, Hong Kong and China.
Interdiction and seizure of illicit drugs are the classic law enforcement control measures to reduce the supply of drugs. Drug smugglers make detection more difficult by converting opium into morphine and heroin (or coca leaf into cocaine) in or near the producing areas. This transformation process reduces the sheer bulk and weight of the goods to be transported. Refining stations are usually located in more remote and secure areas. In remote rural areas, movement of precursors and chemicals needed for processing the harvested plants (e.g. acetic anhydride) can take place with less potential for discovery. Methods of concealing drugs are constantly changed to avoid capture and seizure. According to one source, “many women in drug producing countries are growing, harvesting and processing drug crops. Women are also increasingly involved in drug trafficking and organized crime”.
Border controls are a major focus of interception efforts. However, with the increased flow of commercial traffic between countries and the free movement of goods in large regional trade blocks, the success rate of interdiction at national borders, low to begin with, may decrease further. Vigorous action by authorities in one area often leads to shifts in the pattern of illicit activity or to movement of the illegal activity to another area. While interception efforts may result in lengthening or altering the chain of illicit movement and increase the exposure of the illicit operation to seizure in a given area, unless the interdiction and seizure success rates are high, illicit shipments of drugs will likely continue. Those who get caught smuggling drugs are often low-level persons who can easily be replaced with new recruits. Poor persons already living on the margins of society stand to gain much and lose relatively little by smuggling. With very high profit margins and low seizure rates, interception efforts are not likely to stop illicit distribution. It is more probable that the pattern of smuggling and couriers will be changed to a safer profile. After a detailed review of interdiction, pointing out the adaptability of smugglers, the variety of their methods and the profits involved, one commentator, speaking of the United States, observed: “The recent past suggests that interdiction, even if it produces a high rate of seizures, will do little to decrease cocaine imports”.
The high-risk, high-gain nature of drug trafficking is well known. Profits from the drug traffic flow back into the coffers of sophisticated criminal organizations with financial interests in other illicit areas, such as prostitution and rackets. In some cases, drug dealing may be undertaken by political dissident groups that desire the money to support arms purchases, political insurgency or terrorism. For example, drug enforcement efforts are often hampered by insurgent groups which are engaged in bitter and violent struggles with criminal cartels for control of the drug trade. Hence, political conflicts within and between countries, often involving dissident groups, obstruct government action. Governments that are unable to control major insurgent movements representing a direct challenge to their authority are unlikely to be successful in controlling a drug trade that generates enormous amounts of money to buy influence or weapons. Nor will such governments find it easy to implement programmes of national development in the areas most vulnerable to production of illicit drug crops.
__
Figure below shows growing areas and trafficking routes of illicit drugs:
________
Overview of opium/heroin and coca/cocaine:
Most of the world’s opium is grown in Afghanistan, the Lao People’s Democratic Republic and Myanmar. Several other countries also produce opium but in lesser volume. The development of significant populations of users and addicts in these countries indicates serious social changes that make it even more difficult to reduce drug production. While any social problem may be highly resistant to change, drug use exerts powerful effects, influencing not only the brain processes that influence or control individual behavior but also, ultimately, the social milieu. A portion of the illicit drug production that originates in remote areas of developing countries is invariably diverted along the way from the intended consumer to local individuals. In many cases, the local population provides a stable consumer base for illicit production. The distinction between producer and consumer country is not a rigid one, and the traditional categories of producer and consumer countries is being replaced by the recognition that consumption is a major problem in producer countries as well. For example, in Myanmar, which is one of the largest producers of opium, officials have reported a steady increase in the abuse of opium and heroin since 1970. In Afghanistan, another large producer, the areas of opium poppy cultivation increased in 1992 although the extent of consumption and addiction is unknown. In Pakistan, there were an estimated 650,000 heroin abusers with no end in sight for the increases.
_
Afghan opium poppy cultivation drives record opiate production:
Total global opium production jumped by 65 per cent from 2016 to 2017, to 10,500 tons, easily the highest estimate recorded by UNODC since it started estimating global opium production at the beginning of the twenty-first century. A marked increase in opium poppy cultivation and a gradual increase in opium poppy yields in Afghanistan resulted in opium production in the country reaching 9,000 tons in 2017, an increase of 87 per cent from the previous year. Among the drivers of that increase were political instability, lack of government control and reduced economic opportunities for rural communities, which may have left the rural population vulnerable to the influence of groups involved in the drug trade. The surge in opium poppy cultivation in Afghanistan meant that the total area under opium poppy cultivation worldwide increased by 37 per cent from 2016 to 2017, to almost 420,000 ha. More than 75 per cent of that area is in Afghanistan. Overall seizures of opiates rose by almost 50 per cent from 2015 to 2016. The quantity of heroin seized globally reached a record high of 91 tons in 2016. Most opiates were seized near the manufacturing hubs in Afghanistan. Although not all terrorist groups depend on drug profits, some do. Without the proceeds of drug production and trafficking, which make up almost half of the Taliban’s annual income, the reach and impact of the Taliban would probably not be what it is today. Up to 85 per cent of opium cultivation in Afghanistan occurs in territory under some influence of the Taliban.
_
The coca leaf has been chewed by indigenous people in the Andes for centuries. The plant is grown primarily in Bolivia, Colombia and Peru, with Peru having the largest plant production. Smoking of coca paste, often mixed with tobacco or cannabis (basuco, pitillo etc.) is now frequent among the youth of Bolivia, Colombia and Peru. Cocaine is the principal active ingredient of the coca leaf, extracted from leaves and used to make other forms of the drug such as coca paste or crack. The largest single market for cocaine is the United States, which saw sharp increases in the 1980s. Deaths and injuries related to cocaine received widespread publicity, and high percentages of individuals arrested by the police tested positive for cocaine use. The enormous profits in the cocaine trade have fuelled the creation of new production centres and expansion into new markets as well as infiltration into legitimate businesses and political parties in a number of countries. The addictive nature of cocaine can lead to rapid escalation in frequency of use, amounts taken or use in combination with other drugs. Cocaine abuse has put a heavy burden on communities in many countries, frequently overloading welfare, treatment and law enforcement agencies.
_____
Figure below shows year 2016 cocaine cultivation, production, seizures and users worldwide.
Global cocaine manufacture in 2016 reached the highest level ever reported, with an estimated 1,410 tons being produced. Most of the world’s cocaine comes from Colombia while Africa and Asia are emerging as cocaine trafficking and consumption hubs.
The global seizure of pharmaceutical opioids in 2016 was 87 tons, roughly the same as the quantities of heroin seized that year. Seizures of pharmaceutical opioids – mainly tramadol in West and Central Africa, and North Africa accounted for 87 per cent of the global total in 2016. Countries in Asia, which had previously accounted for more than half of global seizures, reported just 7 per cent of the global total in 2016.
_____
Drug dealers: trust, gender and delivery:
- In global drug survey 2019, 57% respondents reported ever buying drugs (other than cannabis) from a dealer who identified as a woman. Delivery and pick are just as likely in most countries.
- The most common description of the main person that they obtained drugs from was a friend, with only 22% describing them solely as their drug supplier.
- Over 50% had known the main person they get drugs from for 3 or more years.
- Over a third of people reported that they usually take drugs with their supplier when purchasing, with 5% saying they usually flirt or have sex when they get their drugs.
- Overall rates of trust in their dealer with respect to them not becoming abusive or violent if a complaint was made was high, with respondents from Brazil, Scotland and Ireland perceiving their dealers the least trustworthy in this regard.
- Picking up your drugs or having them delivered are common in all countries with 40% indicating both were just as likely.
- Delivery of illegal drugs to order was most common in Brazil (47%), Scotland (39%), England (36%) and least common in Hungary and Norway (<10%).
______
United Nations Convention Against Illicit Traffic in Narcotic Drugs and Psychotropic Substances:
The United Nations Convention Against Illicit Traffic in Narcotic Drugs and Psychotropic Substances of 1988 is one of three major drug control treaties currently in force. It provides additional legal mechanisms for enforcing the 1961 Single Convention on Narcotic Drugs and the 1971 Convention on Psychotropic Substances. The Convention entered into force on November 11, 1990. As of February 2018, there are 190 Parties to the Convention. These include 185 out of 193 United Nations member states.
The 1988 Convention was introduced following the political and sociological developments in the 1970s and 1980s. The growing demand for cannabis, cocaine, and heroin for recreational purposes, mostly in the developed world, triggered an increase of illicit production in geographical areas where cannabis, coca, and opium had been traditionally cultivated. With the rising size of the illicit drug trade, international drug trafficking became a multibillion-dollar business dominated by criminal groups, providing grounds for the creation of the 1988 Convention and the consequential escalation of the war on drugs.
The Preamble notes that previous enforcement efforts have not stopped drug use, warning of “steadily increasing inroads into various social groups made by illicit traffic in narcotic drugs and psychotropic substances.” It cautions that the drug trade and related activities “undermine the legitimate economies and threaten the stability, security and sovereignty of States.”
The illegal drug trade or drug trafficking is a global black market dedicated to the cultivation, manufacture, distribution and sale of drugs that are subject to drug prohibition laws. Most jurisdictions prohibit trade, except under license, of many types of drugs through the use of drug prohibition laws. The United Nations Office on Drugs and Crime’s World Drug Report 2005 estimates the size of the global illicit drug market at US$321.6 billion in 2003 alone. With a world GDP of US$36 trillion in the same year, the illegal drug trade may be estimated as nearly 1% of total global trade. Consumption of illegal drugs is widespread globally and remains very difficult for local authorities to thwart its popularity.
_____
Consumption of drugs:
Trends in drug use and abuse are reflected in official reports to the United Nations and unofficial reports from a variety of sources. Parties to the 1961 Single Convention have an obligation to report to the United Nations, although an analysis of this reporting process over the past decade reveals disappointing results. The United Nations Secretariat indicates that the information provided by governments over the period 1983-1991 did not meet data collection objectives. Only 13 of the countries reported for each of the 9 years involved. Over this same period, 25 countries did not report at all. Information submitted was characterized by high variability from region to region and inconsistency within regions.
There were also major regional gaps in information in official reporting with respect to the nine-year period 1983-1991. The average percentages of countries actually reporting over this nine-year period were as follows: in Europe (74%), the Americas (51 %), the Near and Middle East (46%), Asia and the Pacific region (40%) and Africa (37%). In Africa, the region of the world where the fewest countries report to the United Nations, only about one-third of the countries have reported six or more times in the last nine years. The absence of systematic reporting for this region makes it even more vulnerable since trends that take place there may be unassessed or difficult to identify until long after they have occurred.
Qualitative information summarized by UNDCP indicates that most governments report a much higher prevalence of drug abuse among men than women. However, abuse among women is reported to be increasing, often attributed to their recent gains in entering the labour market. Although drug abuse is common among all age groups, it occurs more frequently among young adults. Increases were noted in illicit drug demand in most countries in the Americas and in eastern Europe, where it was attributed to the socioeconomic crisis affecting these regions and, in particular, high unemployment. Opening European borders between East and West also facilitated contact and communication between traffickers as well as others, increasing the number of transit routes for drugs and the potential number of drug consumers. During the reporting period, illicit demand for drugs increased in western Europe, with some exceptions.
Documents presented to the Commission on Narcotic Drugs indicate that an increase in drug abuse has taken place across most regions of the world, although the specific nature of this trend of increasing drug abuse varies by country and often within country. The regions where these trends for increasing abuse occur are Africa, Europe (especially eastern Europe) and the Americas (except for the Bahamas, Canada, Ecuador and the United States of America). In the Asian and Pacific region, a mixed trend emerged, with as many countries reporting stable or slight decreases as increases. In the Near and Middle East, increasing abuse was found in Egypt, Israel, Pakistan and the Syrian Arab Republic.
Several States reported overall decreasing patterns: Bahrain, Iran (Islamic Republic of), Kuwait, Qatar and Saudi Arabia.
_____
_____
Now I will discuss in detail major illicit addicting drugs:
_
Opioids: Opium, Morphine, Heroin, and Codeine:
Opioids are a group of analgesic agents commonly used in clinical practice. Opioids are chemicals that increase activity in opioid receptor neurons in the brain and in the digestive system, producing euphoria, analgesia, slower breathing, and constipation. Their chemical makeup is similar to the endorphins, the neurotransmitters that serve as the body’s “natural pain reducers.” Natural opioids are derived from the opium poppy, which is widespread in Eurasia, but they can also be created synthetically.
Opium is the dried juice of the unripe seed capsule of the opium poppy. It may be the oldest drug on record, known to the Sumerians before 4000 BC. Morphine and heroin are stronger, more addictive drugs derived from opium, while codeine is a weaker analgesic and less addictive member of the opiate family. When morphine was first refined from opium in the early 19th century, it was touted as a cure for opium addiction, but it didn’t take long to discover that it was actually more addicting than raw opium. When heroin was produced a few decades later, it was also initially thought to be a more potent, less addictive painkiller but was soon found to be much more addictive than morphine. Heroin is about twice as addictive as morphine, and creates severe tolerance, moderate physical dependence, and severe psychological dependence. The danger of heroin is demonstrated in the fact that it has the lowest safety ratio among all psychoactive drugs. Once administered, heroin (diamorphine or diacetylmorphine) is rapidly hydrolysed to 6-monoacetylmorphine (6-MAM) and then to the end-product morphine which binds to opiate receptors located throughout the mammalian nervous and gastrointestinal systems.
Brown Sugar is one of the most commonly used drugs. It is an adulterated form of Heroin – a derivative of opium. It is highly addictive in nature and is available in a powdered form in small vials. Brown sugar is around 20% heroin mixed with other impurities like chalk powder, rat poison, zinc oxide or even strychnine. Though the presence of such impurities makes the drug cheaper than heroin, it makes the users even more vulnerable to casualties, which might even lead to death.
_
Morphine is commonly considered to be the archetypal opioid analgesic and the agent to which all other painkillers are compared. There is evidence to suggest that as long ago as 3000 B.C. the opium poppy, Papaver somniferum, was cultivated for its active ingredients. It was, however, not until morphine was isolated from opium in 1805 by Sertürner that modern opioid pharmacology was truly born. In 1847 the chemical formula for morphine was deduced and this, coupled with the invention of the hypodermic needle in 1853, led to the more precise and widespread clinical use of morphine.
Though morphine is the most widely known extract of P. somniferum, four naturally occurring alkaloids (plant-derived amines) can be isolated from it: morphine, codeine, papaverine and thebaine. Following Sertürner’s isolation of morphine as the active component of the opium poppy, simple chemical manipulations of these basic opiate alkaloids began to yield a range of semi-synthetic opioids useful in clinical medicine (agents such as diamorphine, dihydrocodeine, buprenorphine, nalbuphine, naloxone and oxycodone). During the 20th century a number of synthetic opioids were also produced either by design or serendipitously. These synthetic compounds can be divided into four chemical groupings: the morphinan derivatives (levorphanol, butorphanol), the diphenylheptane derivatives (methadone, propoxyphene), the benzomorphan derivatives (pentazocine, phenazocine) and the phenylpiperidine derivatives (pethidine, alfentanil, fentanyl, sufentanil and remifentanil).
_
Classification of opioids by synthetic process:
| Naturally occurring compounds | Semi-synthetic compounds | Synthetic compounds |
| Morphine | Diamorphine (heroin) | Pethidine |
| Codeine | Dihydromorphone | Fentanyl |
| Thebaine | Buprenorphine | Methadone |
| Papaverine | Oxycodone | Alfentanil |
| Remifentanil | ||
| Tapentadol |
_
Opioids can also be classified according to their effect at opioid receptors. In this manner opioids can be considered as agonists, partial agonists and antagonists. Agonists interact with a receptor to produce a maximal response from that receptor (analgesia following morphine administration is an example). Conversely, antagonists bind to receptors but produce no functional response, while at the same time preventing an agonist from binding to that receptor (naloxone). Partial agonists bind to receptors but elicit only a partial functional response no matter the amount of drug administered (buprenorphine).
_
Opioid receptors:
The proteins that mediate the analgesic and other effects of opioid drugs and endogenous opioid peptides are known as opioid receptors. It is now understood that morphine and other opioid drugs act on an endogenous opioidergic system, which is not only involved in setting pain (nociceptive) threshold and controlling nociceptive processing but also participates in modulation of gastrointestinal, endocrine and autonomic function, as well as a possible role in cognition. Opioid receptors consist of a family of four closely-related proteins belonging to the large superfamily of G-protein coupled receptors. The three types of opioid receptors shown unequivocally to mediate analgesia in animal models are the mu (MOR), delta (DOR), and kappa (KOR) opioid receptor proteins while the novel NOP (nociceptin or orphanin FQ) receptor is considered to be a non-opioid branch of the opioid receptor family. Opioids can act at these receptors as agonists, antagonists or partial agonists. Opioid agonists bind to G-protein coupled receptors to cause cellular hyperpolarisation. Most clinically relevant opioid analgesics bind to MOP receptors in the central and peripheral nervous system in an agonist manner to elicit analgesia. There are now cDNA sequences for all four types of opioid receptors that are expressed in the brain of six species from three different classes of vertebrates.
Opioid receptors are a group of inhibitory G protein-coupled receptors with opioids as ligands. The endogenous opioids are dynorphins, enkephalins, endorphins, endomorphins and nociceptin. The opioid receptors are ~40% identical to somatostatin receptors (SSTRs). Opioid receptors are distributed widely in the brain, in the spinal cord, on peripheral neurons, and digestive tract.
_
Opioids have many effects on the brain, mediated through specific receptors (μ, κ, or δ). The key opioid receptor subtype is μ, which mediates ‘euphoria’, as well as respiratory depression, and is the main target for opioids (Lingford-Hughes & Nutt, 2003), while the κ receptor is involved in mood regulation. Drugs such as heroin and methadone are agonists, which stimulate the receptor. Buprenorphine is a partial agonist; that is, it occupies the receptor in the same way but only partially activates it. In addition, it is an antagonist at the κ receptor and therefore is less likely to lower mood compared with μ agonists.
Soon after injection (or inhalation), heroin metabolises into morphine and binds to opioid receptors. This is subjectively experienced as a euphoric rush, normally accompanied by a warm flush, dry mouth, and sometimes nausea, vomiting and severe itching. As the rush wears off, drowsiness, and slowing of cardiac function and breathing (sometimes to the point of death in an overdose), persist for several hours (National Institute on Drug Abuse [NIDA], 2005a). The effects of methadone are similar but more drawn out and therefore less intense (lasting up to 24 hours when taken orally as prescribed); however, this may be circumvented by illicit users who inject the drug.
_
Cellular mechanisms of action:
G-protein-coupled receptors, such as those for opioids, have no direct link with effector proteins; instead the message is relayed via a G-protein. Both classical opioid receptors (MOP/KOP/DOP) and the non-classical NOP opioid receptor couple to inhibitory G-proteins. Activation of opioid receptors, for example MOP with morphine leads to: (i) closing of voltage sensitive calcium channels (VSCC); (ii) stimulation of potassium efflux leading to hyperpolarization; and (iii) reduced cyclic adenosine monophosphate (cAMP) production via inhibition of adenylyl cyclase. Overall, this results in reduced neuronal cell excitability leading to a reduction in transmission of nerve impulses along with inhibition of neurotransmitter release.
_
Table below is a list of exogenous and endogenous classical opioid receptor ligands:
| Endogenous ligand | Receptor subtype
|
|||
| MOP
|
KOP
|
DOP
|
NOP
|
|
| β-endorphin | ✓✓✓ | ✓✓✓ | ✓✓✓ | × |
| Endomorphin 1/2 | ✓✓✓ | × | × | × |
| Leu-enkephalin | ✓ | × | ✓✓✓ | × |
| Met-enkephalin | ✓✓ | × | ✓✓✓ | × |
| Dynorphin A/B | ✓✓ | ✓✓✓ | ✓ | ✓ |
| N/OFQ | × | × | × | ✓✓✓ |
| Clinical Drugs | ||||
| Agonists | ||||
| Morphine | ✓✓✓ | ✓ | ✓ | × |
| Meperidine | ✓✓✓ | ✓ | ✓ | × |
| Diamorphine | ✓✓✓ | ✓ | ✓ | × |
| Fentanyl/remifentanil | ✓✓✓ | ✓ | × | × |
| Antagonist | ||||
| Naloxone | ✓✓✓ | ✓✓ | ✓✓ | × |
Table above shows endogenous opioid peptides, synthetic and semi-synthetic opioid agonists and antagonists, along with their selectivity for the different subtypes of opioid receptor.
N/OFQ = nociceptin orphanin FQ;
× = no affinity; ✓ = low affinity; ✓✓ = intermediate affinity; ✓✓✓ = high affinity.
_
Opioid-mediated analgesia:
Opioid receptors are distributed throughout the central nervous system and within peripheral tissue of neural and non-neural origin. Centrally, the periaqueductal grey (PAG), locus ceruleus and rostral ventral medulla show high concentrations of opioid receptors, and opioid receptors are also present in the substantia gelatinosa of the dorsal horn. Within the central nervous system, activation of MOP receptors in the midbrain is thought to be a major mechanism of opioid-induced analgesia. Here, MOP agonists act by indirectly stimulating descending inhibitory pathways which act upon the periaqueductal grey (PAG) and nucleus reticularis paragigantocellularis (NRPG) with the net effect of an activation of descending inhibitory neurons. This leads to greater neuronal traffic through the nucleus raphe magnus (NRM), increasing stimulation of 5-hydroxytryptamine and enkephalin-containing neurons which connect directly with the substantia gelatinosa of the dorsal horn. This in turn results in a reduction of nociceptive transmission from the periphery to the thalamus. Exogenous and endogenous opioids can also exert a direct inhibitory effect upon the substantia gelatinosa (in the dorsal horn) and peripheral nociceptive afferent neurones, reducing nociceptive transmission from the periphery. This series of cellular events and mechanisms produces much of the analgesic effect commonly seen following the administration of MOP agonists.
_
Drug Abuse/Addiction:
Excessive use of opioids leads to opioid addiction. Drug abuse and addiction are now considered as neurological pathology due to their effects on brain function. Neurological impairments observed in addiction reflect drug-induced neuronal dysfunction and neurotoxicity. The drugs of abuse directly or indirectly affect various neurotransmitter systems, particularly dopaminergic and glutamatergic neurons. The treatment of drug abuse and addiction is the most expensive of all the neuropsychiatric disorders associated with personality disorders and a diminished quality of life. Behavioral patterns of addiction include compulsive drug-seeking, persistent abuse of substances despite the often irreparable social consequences and deterioration of physical health, and the high probability of relapse even after prolonged drug-free periods.
The mechanisms underlying neurological disorder caused by opioid addiction are not clear yet. Neuronal basis of positive reinforcement relies on activation of dopaminergic neurons resulting in an increased dopamine release in the mesolimbic brain structures. Certain aspects of opioid dependence and withdrawal syndrome are also related to noradrenergic and serotonergic systems, as well as to both excitatory and inhibitory amino acid and peptidergic systems. An important role in neurochemical mechanisms of opioid reward, dependence and vulnerability to addiction has been ascribed to the activation of endogenous opioid peptides, particularly those acting via the MOR and KOR.
_
Opioid abuse leads to opioid tolerance in the nervous system.
Mechanisms of tolerance and withdrawal in opioid abuse:
- In response to long-term exposure to relatively high doses of exogenous opioids, cells internalize their mu and delta opioid receptors. Therefore, increased opioid levels and/or increased opioid potency are necessary to generate the same effect on fewer receptors (tolerance). Similarly, once the exogenous opioids are removed from the system, the remaining endogenous opioids are unable to sufficiently activate the small number of remaining receptors (withdrawal).
- Intracellular second-messenger systems mediating the activity of opioid receptors are down-regulated in the presence of high levels of potent exogenous opioids. Therefore, even the few remaining opioid receptors cannot generate the response they were capable of prior to the administration of exogenous opioids. Down-regulated second messengers include G-proteins and adenylyl cyclase/cAMP.
- Acute tolerance can be mediated by changes in the phosphorylation patterns of mu and delta opioid receptors.
In general, drug abuse induces adaptive changes in opioid receptors that occur following acute (e.g., desensitization and/or internalization) and chronic (e.g., adaptive tolerance and down-regulation) opioid administration.
In addition, opioid abuse may predispose an individual to opportunistic infections, such as hepatitis, bacterial pneumonia, tuberculosis, abscesses, CNS infections, endocarditis and even AIDS. One of the explanations for this phenomenon is that opioids suppress immune function including antimicrobial resistance, antibody production, monocyte-mediated phagocytosis, and neutrophil and monocyte chemotaxis.
_
Mechanism of long-term potential for relapse:
One of the most insidious features of opioid addiction is the tendency to relapse on the drug even weeks, months, or years after those addicted stop using and withdrawal symptoms disappear. The mechanism for this type of relapse is being studied intensely. Animal studies suggest 3 distinct conditions that reliably induce relapse:
- Stress
- Exposure to conditioned cues related to past drug use
- A dose of the previously administered drug or a drug with similar properties
There is evidence that long-term administration of opioids can permanently alter the density of dendritic spines in certain neurons, and these permanent changes may contribute to long-lasting vulnerability to relapse.
_
Means of administration:
Most persistent users follow a classic progression from sniffing (similar to the oral route) to “skin popping” (subcutaneous route) to “mainlining” (intravenous route), each step bringing a more intense experience and a higher addiction liability. With mainlining, the initial thrill is more immediate. Within seconds a warm glowing sensation spreads over the body, most intense in the stomach and intestines, comparable to sexual release. This intense “rush” is then followed by a deep sense of relaxation and contentment. The user is “high” and momentarily free. It is this initial state of intense pleasure that presumably brings the novice to repeat the experience, and it is this mode of administration that hastens a user on the way to drug tolerance and physical dependence. Soon the user finds that the effects are not quite there. Instead, his or her body is beginning to experience new miseries. At this juncture, the user “shoots” to avoid discomfort. The euphoria is gone. The individual now spends every waking moment in obtaining further supplies to prevent the inevitable withdrawal symptoms should supplies run out.
Habits are expensive. If indigent, the addict must spend all his or her time “hustling” for drugs—which means that the person must steal or raise money by other means such as prostitution, procuring, or small-time narcotics peddling. The addict always faces the danger of withdrawal, the danger of arrest, the danger of loss of available supply, and the danger of infection, of collapsed veins, or of death from overdosage. Very few individuals are still addicted by age 40. They have either died, somehow freed themselves from their addiction, or sought treatment.
_______
Cocaine:
Cocaine is an alkaloid derived from the leaves of the coca plant (Erythroxylon coca), a bush that is natural to Bolivia, Chile, and Peru along the western slopes of the Andes Mountains. Cocaine has a pronounced excitant action on the central nervous system and, in small doses, produces a pleasurable state of well-being associated with relief from fatigue, increased mental alertness, physical strength, and a reduction of hunger. In greater amounts, cocaine is an intoxicant that produces excitement, mental confusion, and convulsions. The Incas were acquainted with the ability of cocaine to produce euphoria, hyperexcitability, and hallucinations; the practice of chewing the coca leaf as part of religious ceremonials was an established custom at the time of the Spanish conquest in the 16th century. The natives who worked the mines high in the Andes chewed coca leaves for increased strength and endurance. In the late 19th and early 20th centuries, it was a primary constituent in many popular tonics and elixirs and, although it was removed in 1905, was one of the original ingredients in Coca-Cola. Today cocaine is taken illegally as a recreational drug. Cocaine is a powerful nervous system stimulant that can be taken intranasally, injected intravenously or smoked.
_
Do not confuse chocolate and cocaine:
Chocolate is a range of foods derived from cocoa (cacao), mixed with fat (e.g., cocoa butter) and finely powdered sugar to produce a solid confectionery. Chocolate comes from the species Theobroma cacao, commonly known as cacao. Cocaine comes from a bunch of different plants in the genus Erythroxylum, but mostly from the species Erythroxylum coca. It’s typically referred to as coca or coca leaf. So cacao (cocoa) and coca are two completely different plants with similar names. Coca (the source of cocaine) is still associated with a common household product, though: Coca-cola. In the late 19th century, the coca leaf was combined with the caffeinated kola nut (also in the mallow family along with chocolate) to form coca-kola. It was common at the time for “health products” to contain cocaine—the industry was not yet regulated and cocaine does, after all, make you feel very good for a short time, even if it harms your body. Eventually cocaine fell out of favor, and Coca-cola started using pre-processed, cocaine-free coca leaves to flavor the drink, relying only on sugar and caffeine content to provide a much milder kick.
_
As central nervous system stimulants, cocaine and amphetamine affect a number of neurotransmitter systems in the brain but exert their effects primarily via dopamine, which mediates reward. Cocaine blocks the presynaptic reuptake of dopamine, such that it is not removed from the intracellular space and leads to extended firing of postsynaptic neurons, resulting in physiological arousal. Amphetamines also increase the availability of dopamine but are thought to do so by triggering a presynaptic leakage. The acute subjective effects of cocaine are euphoria, increased energy, heightened alertness, sexual arousal, increased sociability and talkativeness. Physiologically there can be acute adverse effects on breathing, and the cardiovascular and central nervous systems: increased heart rate, blood pressure and body temperature, and pupil dilation. All these effects have near-immediate onset but also diminish quickly (after roughly 15–30 minutes if the drug is snorted and 5–10 minutes if smoked), as cocaine is metabolised rapidly by the body (NIDA, 2004). As acute effects wear off, users experience a rebound period (‘crash’), which may include restlessness, anxiety, agitation and insomnia. This can lead to the user bingeing on cocaine in an attempt to displace these negative effects. Chronic misuse of cocaine may lead to increased paranoia, inability to concentrate, sexual dysfunction and cognitive deficits.
_
Cocaine has a variety of adverse effects on the body. It constricts blood vessels, dilates pupils, and increases body temperature, heart rate, and blood pressure. It can cause headaches, abdominal pain, and nausea. Cocaine could cause blood pressure to rise, sometimes so much so that a stroke or heart attack would occur. Since cocaine also tends to decrease appetite, chronic users may become malnourished. The intensity and duration of cocaine’s effects, which include increased energy and reduced fatigue, depend on how the drug is taken. The faster the drug is absorbed into the bloodstream and delivered to the brain, the more intense the high. Injecting or smoking cocaine produces a faster, stronger high than snorting it. However, the faster the drug is absorbed, the faster the effects subside. The high from snorting cocaine may last 30 minutes, whereas the high from smoking “crack” cocaine may last only 10 minutes. In order to sustain the high, the user must administer the drug again, which may lead to frequent use, often in higher doses, over a short period of time.
Cocaine is habit-forming and may also be physically addicting in some individuals, but not to the extent of the opiates. Only certain persons display abstinence symptoms on withdrawal. Significant physiological tolerance does not develop. Chronic use is associated with severe personality disturbances, inability to sleep, loss of appetite, emaciation, an increased tendency to violence, and antisocial acts. When a toxic psychosis develops, it is characteristically accompanied by paranoid delusions. Hallucinations are prominent with continued use of cocaine, particularly the tactile hallucinations that give the impression that bugs are under the skin.
_
Mechanism of action:
In the brain, cocaine acts as a monoamine transporter blocker, with similar affinities for dopamine, serotonin, and norepinephrine transporters. Cocaine, and the dopamine transporter to which it binds, can be visualized in the human brain using positron emission tomography (PET) imaging (Figure below). The antagonism of the transporter proteins leaves more monoaminergic neurotransmitters available in the synaptic cleft to act upon presynaptic and postsynaptic receptors. It is widely accepted that the ability of cocaine to act as a reinforcer is due largely to its ability to block dopamine reuptake. Both D1 and D2 receptors have been implicated in the reinforcing effects of cocaine. Using PET to investigate the role of dopamine in the reinforcing effects of cocaine in humans it has been shown that the rate at which cocaine enters the brain and blocks the dopamine transporter is associated with the “high”, and not merely with the presence of the drug in the brain.
_
Figure below shows [11C] cocaine distribution in human brain at different time points after injection
_
Despite the evidence pointing to a dopaminergic mechanism for cocaine reward, dopamine may not be the sole mediator of the reinforcing properties of cocaine, since dopamine transporter knock-out mice – mice that have had the dopamine transporter gene silenced so that the transporter is not expressed, – continue to self-administer cocaine. The serotonergic system may influence the reinforcing properties of cocaine, because cocaine also facilitates serotonin transmission in the nucleus accumbens.
_
Tolerance and withdrawal:
In general, there appears to be little tolerance to the effects of cocaine, although there may be acute tolerance within a single session of repeated substance use. Cocaine withdrawal does not result in the severe symptoms that characterize opioid withdrawal, but it does induce a “post-high down”, which can contribute to further cocaine use or use of another drug.
Neurobiological adaptations to prolonged use:
Cognitive deficits associated with chronic use of cocaine have been noted, and such deficits reflect changes to the underlying cortical, subcortical and neuromodulatory mechanisms that underpin cognition – and also interfere directly with rehabilitative programmes. Individuals who are dependent on cocaine have specific defects of executive functions, e.g. decision-making and judgement, and this behaviour is associated with dysfunction of specific prefrontal brain regions. PET studies suggest that stimulation of the dopaminergic system secondary to chronic use of cocaine activates a circuit that involves the orbitofrontal cortex, cingulate gyrus, thalamus and striatum. This circuit is abnormal in people with cocaine dependence and it is hypothesized that this abnormality contributes to the intense desire to use cocaine, resulting in the loss of control over the drive to take more cocaine.
_______
Hallucinogens: Cannabis, Mescaline, and LSD:
The drugs that produce the most extreme alteration of consciousness are the hallucinogens, psychoactive drugs that alter sensation and perception and that may create hallucinations. The hallucinogens are frequently known as “psychedelics.” Drugs in this class include lysergic acid diethylamide (LSD, or “acid”), mescaline, and phencyclidine (PCP), as well as a number of natural plants including cannabis (marijuana), peyote, and psilocybin. The chemical compositions of classical psychedelics are similar to the neurotransmitters serotonin and epinephrine, and they act primarily as agonists by mimicking the action of serotonin at the synapses. The hallucinogens may produce striking changes in perception through one or more of the senses. The precise effects a user experiences are a function not only of the drug itself, but also of the user’s pre-existing mental state and expectations of the drug experience. In large part, the user tends to get out of the experience what he or she brings to it. The hallucinations that may be experienced when taking these drugs are strikingly different from everyday experience and frequently are more similar to dreams than to everyday consciousness.
A psychedelic experience (or ‘trip’) is a temporary altered state of consciousness induced by the consumption of psychedelic drugs (such as mescaline, LSD, psilocybin, and DMT Dimethyltryptamine). For example, the term acid trip refers to psychedelic experiences brought on by the use of LSD. The term “psychedelic” derives from Greek words essentially meaning “mind revealing”. Psychedelic experiences are interpreted in exploratory, learning, recreational, religious/mystical and therapeutic contexts.
Cannabis (marijuana) is the most widely used hallucinogen. Marijuana also acts as a stimulant, producing giggling, laughing, and mild intoxication. It acts to enhance perception of sights, sounds, and smells, and may produce a sensation of time slowing down. It is much less likely to lead to antisocial acts than that other popular intoxicant, alcohol. In recent years, cannabis has again been frequently prescribed for the treatment of pain and nausea, particularly in cancer sufferers, as well as for a wide variety of other physical and psychological disorders. Although the hallucinogens are powerful drugs that produce striking “mind-altering” effects, they do not produce significant physiological or psychological tolerance or dependence. While they are not strongly addictive and pose little physical threat to the body, their use is not advisable in any situation in which the user needs to be alert and attentive, exercise focused awareness or good judgment, or demonstrate normal mental functioning, such as driving a car, studying, or operating machinery.
_
Pharmacological classes of hallucinogens:
One possible way of classifying the hallucinogens is by their chemical structure and that of the receptors they act on. In this manner, the following categories are often used:
- Psychedelics (classical hallucinogen):
-Serotonergics (5-HT2A receptor agonists or classical psychedelics) such as mescaline from peyote (Lophophora williamsii)
-Indoles / Tryptamines such as psilocybin from “magic” mushrooms (Psilocybe)
-Ergolines such as lysergol from morning glory (Convolvulaceae)
-Lysergamides such as LSD (“acid”), derived from ergot (Claviceps purpurea)
-β-carbolines such as harmine, harmaline, and tetrahydroharmine (monoamine oxidase inhibitors or MAOIs, specifically reversible inhibitors of monoamine oxidase A or RIMAs) from B. caapi and P. harmala
-Complexly substituted tryptamines such as ibogaine from iboga (Tabernanthe iboga)
-Phenethylamines such as mescaline
-Empathogen–entactogens such as MDA
-Substituted methylenedioxyphenethylamines (serotonin releasing agents) such as MDMA (“ecstasy”)
-Cannabinoidergics (CB-1 receptor agonists or atypical psychedelics) such as THC from cannabis (Cannabis)
- Dissociatives (Dissociatives are a class of hallucinogen which distort perceptions of sight and sound and produce feelings of detachment – dissociation – from the environment and self):
-Antiglutamatergics (NMDA receptor antagonists or classical dissociatives) such as “laughing gas” (nitrous oxide) and ketamine
-Opioidergics (sometimes regarded as atypical psychedelics) (κ-Opioid receptor agonists or atypical dissociatives) such as salvinorin A from Salvia divinorum and pentazocine
- Deliriants:
-Anticholinergics (muscarinic acetylcholine receptor antagonists or classical deliriants) such as tropane alkaloids such as atropine from deadly nightshade (Atropa belladonna) and diphenhydramine (Benadryl)
-GABAergics (sometimes regarded as atypical dissociatives) (GABA receptor agonists, and some positive allosteric modulators of the GABA receptor, or atypical deliriants) such as muscimol from fly agaric (Amanita muscaria) and zolpidem
_
Physiological and psychological effects of hallucinogens:
The psychedelics are capable of producing a wide range of subjective and objective effects. However, there is apparently no reaction that is distinctive for a particular drug. Subjects are unable to distinguish among LSD, mescaline, and psilocybin when they have no prior knowledge of the identity of the drug ingested. These drugs induce a physiological response that is consistent with the type of effect expected of a central-nervous-system stimulant. Usually there is elevation of the systolic blood pressure, dilatation of the pupils, some facilitation of the spinal reflexes, and excitation of the sympathetic nervous system and the brain.
There is considerable difference in the potency of these drugs. A grown man requires about 500 milligrams of mescaline or 20 milligrams of psilocybin or only 0.1 milligram of LSD for full clinical effects when the substances are ingested orally. The active principle in the seeds of the morning glory is about one-tenth as potent as LSD. There are also differences in the time of onset and the duration of effects. Psilocybin acts within 20 to 30 minutes, and the effects last about five to six hours. LSD acts within 30 to 60 minutes, and the effects usually last eight to 10 hours, although occasionally some effects persist for several days. Mescaline requires two to three hours for onset, but the effects last more than 12 hours. All psychedelics presumably are lethal if taken in quantities large enough, but the effective dose is so low compared with the lethal dose that death has not been a factor in experimental studies. Physiological tolerance for these drugs develops quite rapidly—fastest for LSD, somewhat more slowly and less completely for psilocybin and mescaline. The effects for a particular dose level of LSD are lost within three days of repeated administration, but the original sensitivity is quickly regained if several days are allowed to intervene. Cross-tolerance has been demonstrated for LSD, mescaline, psilocybin, and certain of the lysergic acid derivatives. Tolerance to one of the drugs reduces the effectiveness of an equivalent dose of a second drug, thus suggesting a common mode of action for the group.
Most persons regard the experience with one of these drugs as totally removed from anything ever encountered in normal everyday life. The subjective effects vary greatly among individuals and, for a particular person, even from one drug session to the next. The variations seem to reflect such factors as the mood and personality of the subject, the setting in which the drug is administered, the user’s expectation of a certain kind of experience, the meaning for the individual of the act of taking the drug, and the user’s interpretation of the motives of the person administering the drug. Nevertheless, certain invariant reactions experienced by hallucinogen users stand out. The one most easily described by users is the effect of being “flooded” with visual experience, as much when the eyes are closed as when they are open. Light is greatly intensified; colours are vivid and seem to glow; images are numerous and persistent, yielding a wide range of illusions and hallucinations; details are sharp; perception of space is enhanced; and music may evoke visual impressions, or light may give the impression of sounds.
A second important aspect, which people have more difficulty describing, involves a change in the feelings and the awareness of the self. The sense of personal identity is altered. There may be a fusion of subject and object; legs may seem to shrink or become extended, and the body to float; space may become boundless and the passage of time very slow; and the person may feel completely empty inside or may believe that he is the universe. This type of reaction has been called depersonalization, detachment, or dissociation. Increased suspiciousness of the intentions and motives of others may also become a factor. At times the mood shifts. Descriptions of rapture, ecstasy, and an enhanced sense of beauty are readily elicited; but there can also be a “hellish” terror, gloom, and the feeling of complete isolation. For some people the experience is so disturbing that psychiatric hospitalization is required. Studies of performance on standardized tests show some reduction in reasoning and memory, but the motivation of the subject probably accounts for much of the performance decrement, since many people are uncooperative in this type of structured setting while under the influence of a drug.
_
What is a bad trip?
A bad trip is when people experience negative feelings while using hallucinogens. This may include feeling like they are losing control as well as anxious and paranoid. It can lead to panic attacks and extreme risky behaviours’ like jumping off high places or running across a busy road. It can feel like it will never end.
_
Are Hallucinogens truly Addictive?
Sometimes people will take hallucinogens thinking that they can do so safely. They assume that these types of drugs are not addictive. Therefore, they have nothing to worry about. Unfortunately, this is not at all accurate. There are hallucinogens that result in an addiction. There are also those drugs that experts believe don’t result in addiction. For example, LSD is a drug that is not thought to be physically addictive. Even so, taking LSD for a longer period of time will result in increased levels of tolerance. This in itself is an indicator of addiction. Even if hallucinogens are not believed to be physically addictive, they are psychologically addictive. When you become psychologically addicted to a drug, you believe you need it. Psychological addiction can produce physical addiction symptoms for all types of psychoactive drugs, including hallucinogens. Please don’t think that you’re safe if you take hallucinogens. These drugs are dangerous, and they do lead to addiction, in one form or another.
______
Lysergic acid diethylamide:
Lysergic acid diethylamide (LSD), also known as acid, is a hallucinogenic drug. Effects typically include altered thoughts, feelings, and awareness of one’s surroundings. Many users see or hear things that do not exist. Dilated pupils, increased blood pressure, and increased body temperature are typical. Effects typically begin within half an hour and can last for up to 12 hours. It is used mainly as a recreational drug and for spiritual reasons. LSD does not appear to be addictive, although tolerance may occur with use of increasing doses. Adverse psychiatric reactions are possible, such as anxiety, paranoia, and delusions. Distressing flashbacks might occur in spite of no further use, a condition called hallucinogen persisting perception disorder. Death is very rare as a result of LSD, though it occasionally occurs in accidents. The effects of LSD are believed to occur as a result of alterations in the serotonin system. As little as 20 micrograms can produce an effect. In pure form, LSD is clear or white in color, has no smell, and is crystalline. It breaks down with exposure to ultraviolet light.
Prior to the mid-1960s, LSD-type drugs were taken by several different types of persons including many who were respected, successful, and well-established socially. Intellectuals, educators, medical and mental health professionals, volunteer research subjects, psychiatric patients, theological students, and participants in special drug-centre communities were some of the first users of these hallucinogenic substances. Beginning in 1966, experimentation in most countries was severely restricted, and subsequent use was almost entirely of a black market type. LSD use has declined substantially, since the drug was replaced largely by cannabis and the amphetamines. Most users tend to be of the middle class—either college-educated young persons or people who have drifted to the fringe of society. Drug initiation is typically by way of a personal friend or acquaintance. Employers or teachers also have a powerful influence over subordinates and students in terms of drug acceptance. The user of LSD seems often to have an almost fanatic need to proselytize others to drug use. Those who have taken a hallucinogenic substance generally have had experience with other drugs prior to the LSD experience, and there is also a tendency on the part of those who take these drugs to repeat the drug experience and to experiment with other drugs. The special language, method of proselytizing, and psychological dependence surrounding the use of psychedelics bear striking resemblance to the context of narcotics addiction. The chronic LSD user tends to be introverted and passive. Motives for LSD use are many: psychological insight; expansion of consciousness; the desire to become more loving, more creative, open, religious; a desire for new experience, profound personality change, and simple “kicks.”
About 10 percent of people in the United States have used LSD at some point in their lives as of 2017, while 0.7 percent have used it in 2016. It was most popular in the 1960s to 1980s. LSD is typically either swallowed or held under the tongue. It is most often sold on blotter paper and less commonly as tablets or in gelatin squares. There are no known treatments for addiction, if it occurs.
_____
N-Methyl-D-aspartate (NMDA) receptor antagonists are a class of anesthetics that work to antagonize, or inhibit the action of, the N-Methyl-D-aspartate receptor. They are used as anesthetics for animals and humans; the state of anesthesia they induce is referred to as dissociative anesthesia. Several synthetic opioids function additionally as NMDA receptor antagonists, such as pethidine, levorphanol, methadone, dextropropoxyphene, tramadol and ketobemidone. Some NMDA receptor antagonists, such as ketamine, dextromethorphan (DXM), phencyclidine (PCP), methoxetamine (MXE), and nitrous oxide (N2O), are popular recreational drugs used for their dissociative, hallucinogenic, and euphoriant properties. When used recreationally, they are classified as dissociative drugs.
_______
Cannabis:
Cannabis, or marijuana, is the general term applied to Cannabis plants, when the plants are used for their pleasure-giving effects. Cannabis may grow to a height of about 5 meters (16 feet), but the strains used for drug-producing effects are typically short stemmed and extremely branched. The resinous exudate is the most valued part of the plant because it contains the highest concentration of tetrahydrocannabinol (THC), an active hallucinogenic principle associated with the plant’s potency. The terms cannabis and marijuana also encompass the use of the flowering tops, fruit, seeds, leaves, stems, and bark of the plant even though the potency of these plant parts is considerably less than that of the pure resin itself. Cannabis plants grow freely throughout the temperate zones of the world, but the content of the resin in the plant differs appreciably according to the geographic origin of the plant and the climate of the region in which the plant is grown. A hot, dry, upland climate is considered most favourable in terms of the potency of the plant. Careful cultivation is also considered to be an important factor in resin production. The prevention of pollination and the trimming of top leaves to produce dwarfing enhances the content of resin at plant maturity.
_
Types of cannabis preparations:
Hashish, charas, ghanja, bhang, kef, and dagga are other names that have been applied to various varieties and preparations of Cannabis. Hashish, named after the Persian founder of the Assassins of the 11th century (Ḥasan-e Ṣabbāḥ), is the most potent of the cannabis preparations, typically being at least twice as strong, but sometimes being as many as 10 times as strong, as marijuana. Very few geographic areas are capable of producing a plant rich enough in resins to produce hashish. Unless sifted and powdered, hashish appears in a hardened, brownish form with the degree of darkness indicating strength. It may be eaten in a confection or smoked, the water pipe often being used to cool the smoke. The effects are more difficult to regulate when hashish is either ingested as a confection or drunk. In India this resinous preparation is called charas.
Whereas hashish and charas are made from the pure resin, ghanja is prepared from the flowering tops, stems, leaves, and twigs, which have less resin and thus less potency. Ghanja is nevertheless one of the more potent forms of cannabis. It is prepared from specially cultivated plants in India and the flowering tops have a relatively generous resinous exudate. Ghanja is consumed much in the manner of charas.
Bhang is the least potent of the cannabis preparations used in India. It does not contain the flowering tops found in ghanja. As a result, bhang contains only a small amount of resin (5 percent). It is either drunk or smoked. When drunk, the leaves are reduced to a fine powder, brewed, and then filtered for use. Bhang is also drunk in Hindu religious ceremonials.
Marijuana is considered mild in comparison with other forms of Cannabis preparations, though it is similar in potency to the bhang used in India. Typically it is smoked, but occasionally it is brewed as a tea or baked into cakes. Marijuana varies considerably in potency. Today’s marijuana is 5 to 6 times stronger than it was just 20 years ago. The amount of THC in marijuana has been increasing steadily in recent decades, creating more harmful effects in some people.
_
Cannabis is the most widely produced and consumed illicit psychoactive substance worldwide. Following initiation, occasional cannabis use can progress to frequent use, abuse and dependence. About 1 in 10 occasional users becomes dependent, which is associated with physical, psychological, social and occupational consequences. Despite the increasing use of cannabis for medicinal purposes, associations with adverse health effects have been reported. These include increased risk for psychiatric outcomes, including psychosis, schizophrenia, schizotypal personality disorder and mania. Early cannabis use appears to moderate relationship between polygenic risk scores for schizophrenia and brain maturation.
In the United States several states passed legislation in the late 1970s and early ’80s to fund research on or to legalize the medicinal use of marijuana, though some of these statutes were later repealed or lapsed. Renewed decriminalization efforts in the 1990s led to the legalization of medicinal marijuana in more than a dozen states, including Alaska, Arizona, California, Colorado, Nevada, Oregon, and Washington. In 2001, however, the U.S. Supreme Court ruled against the use of marijuana for medical purposes. Later that year Canada passed legislation easing restrictions on medicinal marijuana. That country’s new regulations included licensing marijuana growers to produce the drug for individuals with terminal illnesses or chronic diseases. In 2009 U.S. attorney general Eric Holder issued a new set of guidelines for federal prosecutors in states where the medical use of marijuana was legalized. The policy shift mandated that federal resources were to be focused primarily on prosecuting illegal use and trafficking of marijuana, thereby rendering cases of medical use, in which those individuals in possession of the drug are clearly in compliance with state laws, less prone to excessive legal investigation. In 2012 the U.S. states of Colorado and Washington became the first in which citizens voted in favour of legalizing the recreational use of marijuana.
_
Mechanism of action of cannabis:
Cannabinoid receptors and their endogenous ligands are widely expressed throughout the brain, with particularly strong presence and influence in neuronal circuits such as the mesocorticolimbic pathways highly implicated in reward and addiction. CB1 receptor signaling influences the motivation for both natural and drug rewards. In comparison to most drugs of abuse CB1 receptors exert only modest influence on psychostimulant intake. The Endocannabinoid system (ECS) is comprised of G protein-coupled receptors, small neuromodulatory lipid ligands and biosynthetic and metabolic enzymes for the synthesis and degradation of the ligands, respectively. Two major types of cannabinoid receptor have been characterized and cloned: CB1 and CB2. CB1 receptors (CB1Rs) are the most abundant G protein-coupled receptor expressed in the adult brain, with particularly dense expression in regions with known involvement in reward, addiction and cognitive function including amygdala, cingulate cortex, prefrontal cortex (PFC), ventral pallidum, caudate putamen, nucleus accumbens (NAc), ventral tegmental area (VTA), lateral hypothalamus. CB2 receptors (CB2Rs) are mainly expressed by immune cells with recent evidence also suggesting CB2R expression in neurons, glia and endothelial cells in brain. CB1R and CB2R are coupled to similar transduction systems primarily through Gi or Go proteins. CB1Rs directly inhibit the release of GABA, glutamate and acetylcholine that produce widespread effects on neural signaling across many neurotransmitter systems.
_
The Cannabinoid Receptor type1 System (CB1) is activated by the neurotransmitter Anandamide and THC
THC’s chemical structure is similar to the brain chemical anandamide. Similarity in structure allows the body to recognize THC and to alter normal brain communication. Endogenous cannabinoids such as anandamide (see figure above) function as neurotransmitters because they send chemical messages between nerve cells (neurons) throughout the nervous system. They affect brain areas that influence pleasure, memory, thinking, concentration, movement, coordination, and sensory and time perception. Because of similarity to anandamide, THC is able to attach to molecules called cannabinoid receptors on neurons in these brain areas and activate them, disrupting various mental and physical functions and causing the effects described earlier. The neural communication network that uses these cannabinoid neurotransmitters, known as the endocannabinoid system, plays a critical role in the nervous system’s normal functioning, so interfering with it can have profound effects.
For example, THC is able to alter the functioning of the hippocampus and orbitofrontal cortex, brain areas that enable a person to form new memories and shift his or her attentional focus. As a result, using marijuana causes impaired thinking and interferes with a person’s ability to learn and perform complicated tasks. THC also disrupts functioning of the cerebellum and basal ganglia, brain areas that regulate balance, posture, coordination, and reaction time. This is the reason people who have used marijuana may not be able to drive safely and may have problems playing sports or engaging in other physical activities. People who have taken large doses of the drug may experience an acute psychosis, which includes hallucinations, delusions, and a loss of the sense of personal identity.
THC, acting through cannabinoid receptors, also activates the brain’s reward system, which includes regions that govern the response to healthy pleasurable behaviors such as sex and eating. Like most other drugs that people misuse, THC stimulates neurons in the reward system to release the signaling chemical dopamine at levels higher than typically observed in response to natural stimuli. This flood of dopamine contributes to the pleasurable “high” that those who use recreational marijuana seek.
_
CB1 Receptors show disruption in their function when flooded by external cannabinoid exposure. The result of the flooded CB1 receptors by THC is altered structure and function of brain regions that control emotion, thought, memory and social interaction as seen in the figure below:
These changes can persist well into adulthood and increase the risk for psychiatric illness as well as other drug addiction.
_
Physiological and psychological effects of cannabis:
The effects of the various drug preparations made from Cannabis are difficult to specify because of the wide variations in the potency of the various preparations of the plant. Hashish or charas would be expected to produce a greater degree of intoxication than marijuana or bhang. Whether the drug is smoked, drunk, eaten, or received as an administration of synthetic tetrahydrocannabinol (THC) can also determine the extent of effect. In general, hashish produces effects similar to those of mescaline or, in sufficient quantity, to those of LSD—extreme intoxication being more typical when the substance is swallowed. Marijuana, on the other hand, is more apt to produce effects at the opposite or mild end of the continuum from those of LSD. When smoked, physiological manifestations are apparent within minutes. These include dizziness, light-headedness, disturbances in coordination and movement, a heavy sensation in the arms and legs, dryness of mouth and throat, redness and irritation of the eyes, blurred vision, quickened heartbeat, tightness around the chest, and peculiarities in the sense of hearing such as ringing, buzzing, a feeling of pressure in the ears, or altered sounds. Occasionally drug use is accompanied by nausea and an urge to urinate or defecate. There is also a feeling of hunger that may be associated with a craving for sweets. Toxic manifestations are rare and include motor restlessness, tremor, ataxia, congestion of the conjunctivae of the eye, abnormal dilation of the pupil, visual hallucinations, and unpleasant delusions. Marijuana is not a typical drug of addiction. Use does not lead to physical dependence, and there are no withdrawal symptoms when the drug is discontinued. Psychological dependence does occur among certain types of users. Infrequently, a “cannabis psychosis” may occur, but generally this type of psychiatric reaction is associated only with heavy long-term use of hashish. Other effects of chronic hashish use are a debilitation of the will and mental deterioration.
Psychological manifestations are even more variable in response to drugs prepared from Cannabis. Alterations in mood may include giggling, hilarity, and euphoria. Perceptual distortions may also occur, involving space, time, sense of distance, and sense of the organization of one’s own body image. Thought processes may also become disorganized, with fragmentation, disturbances of memory, and frequent shifts of attention acting to disrupt the orderly flow of ideas. One may also experience some loss of reality contact in terms of not feeling involved in what one is doing; this may lead to considerable detachment and depersonalization. On the more positive side, there may be an enhancement in the sense of personal worth and increased sociability. Undesired subjective experiences include fear, anxiety, or panic. These effects vary considerably with practice and with the setting in which the drug is taken.
_
Cannabis use impairs memory, attention and motor coordination, with especially dangerous consequences on driving performance. Such effects may last for many hours after administration of the drug; the numerous metabolites of a single moderate dose of cannabis may require up to 4 weeks to be completely eliminated from the body (Maykut, 1985). The smoke from cannabis contains the same constituents as tobacco smoke; hence chronic cannabis smoking is associated with a range of respiratory tract disorders, including bronchitis, emphysema and cancers (Hashibe et al., 2005; Tashkin, 1990). It’s unlikely that a person will fail a drug test or get high from passive exposure by inhaling secondhand marijuana smoke. There aren’t any reports of teens and adults dying from using marijuana alone, but marijuana use can cause some very uncomfortable side effects, such as anxiety and paranoia and, in rare cases, extreme psychotic reactions. Marijuana use can lead to a substance use disorder, which can develop into an addiction in severe cases. No medications are currently available to treat marijuana use disorder, but behavioral support can be effective.
_
Brain endocannabinoid (EC) levels are increased by most drugs of abuse, though the nature of this effect differs between classes of drugs and across brain regions. The response contingency of drug exposure (volitional vs. response-independent) appears to influence brain EC production, suggesting contributions of both drug-related pharmacological effects and neural activity engaged by active drug-seeking. Chronic exposure to drugs of abuse generally results in impaired CB1 receptor function, loss of EC-mediated synaptic plasticity in addiction-related neural circuits, and negative affective states that can be ameliorated through pharmacologically enhanced EC tone. The ECS plays a strong role in modulating relapse-like behavior induced by conditioned cues or reward priming, and this is evident for both natural and drug rewards.
_____
Amphetamines:
Stimulants such as Methylphenidate and amphetamines are commonly prescribed for attention-deficit hyperactivity disorder (ADHD) and narcolepsy—uncontrollable episodes of deep sleep. Prescription stimulants increase alertness, attention, and energy. Stimulants enhance the effects of certain neurotransmitters in the brain, such as norepinephrine and dopamine. Dopamine affects feelings of pleasure. Norepinephrine affects blood vessels, blood pressure and heart rate, blood sugar, and breathing. People who use prescription stimulants report feeling a “rush” (euphoria) along with increased blood pressure and heart rate, increased breathing, decreased blood flow, increased blood sugar, opened-up breathing passages.
The amphetamine group includes:
- Dexamphetamine, commonly known as Dexies, which is used for medical purposes to treat conditions such as Attention Deficit Hyperactivity Disorder.
- Amphetamine sulphate, commonly known as whizz and goey, which comes as a powder or waxy paste.
- Methamphetamine, commonly known as speed, meth, ice, crystal, shards; which is a more potent form of amphetamine which can come with a crystal-like appearance, as a powder or waxy paste.
_
The amphetamines have been used to alleviate depression, fatigue, the hyperkinetic behaviour disturbances of children, postencephalitic parkinsonism, enuresis, nausea of pregnancy, and obesity. More recently, the amphetamines have been used in combination with one of the barbiturates, such as amobarbital or phenobarbital, to produce mood elevating effects. It is the effects of the amphetamines on mood that have led to their widespread abuse. A toxic psychosis with hallucinations and paranoid delusions may be produced by a single dose as low as 50 milligrams if no drug tolerance is present. Although the normal lethal dose for adult humans is estimated to be around 900 milligrams, habitual use may increase adult tolerance up to 1,000 milligrams per day. Amphetamines can be swallowed, injected, smoked or inhaled (snorted). The effects of amphetamines can last from four to eight hours. Sometimes a person may experience a hangover effect that can last up to three days.
_
Methamphetamine is a club drug known by many names, including ‘crystal meth’, ‘crank’ and ‘ice’. This drug is another amphetamine derivative and can be manufactured from ephedrine. As with all designer amphetamines, this drug is purported to produce feelings of euphoria, energy and a ‘high’. Methamphetamine is probably the most dangerous of the modern club drugs. Compared with nicotine and alcohol, it has significantly more serious psychic, physical and withdrawal symptoms. The dependence developed with methamphetamine is worse than that with alcohol or nicotine. As well, methamphetamine has significant cardiovascular effects due to its sympathomimetic properties. This drug can cause tachycardia, arrhythmia, hypertension (systemic, pulmonary), myocardial infarction and death.
Methamphetamine was used extensively by the Japanese during World War II, and by 1953 the habitual users of the drug in Japan numbered about 500,000 persons. This large-scale usage created such a serious social problem that the amphetamines were placed under governmental control in Japan in 1954. This Japanese experience provided the opportunity for systematic studies on chronic methamphetamine intoxication. One group of 492 addicts who had been institutionalized showed a 14 percent rate of chronic psychosis with evidence of permanent organic brain damage. In the language of the street, “Meth is death.” The amphetamines produce habituation, drug dependency, physiological tolerance, and toxic effects, but no physical addiction.
_
What is a ‘binge crash cycle’ on amphetamines?
Unlike regular and dependent users of other drugs such as alcohol and heroin, some regular users of amphetamines do not use every day. Rather, they are more likely to use continuously over several days to a week (sometimes called a binge). The effects of the drug may include feelings of euphoria, reduced appetite and inability to sleep. Of course, no-one can do without sleep indefinitely so this combined with inadequate nutrition results in exhaustion, paranoia, anxiety and depression. This is sometimes called a crash. To respond to the crash, the person might then start using again, and this can be commencement of the binge-crash cycle.
_
Ecstasy:
Ecstasy is the name given to methylenedioxymethamphetamine (MDMA). MDMA is a derivative of the compounds methamphetamine and amphetamine. Ecstasy has both stimulant and hallucinogenic properties. Ecstasy can cause stimulation similar to amphetamines, and in higher doses they can have hallucinogenic type effects. MDMA is a very strong stimulant that very successfully prevents the reuptake of serotonin, dopamine, and norepinephrine. It is so effective that when used repeatedly it can seriously deplete the amount of neurotransmitters available in the brain, producing a catastrophic mental and physical “crash” resulting in serious, long-lasting depression. MDMA also affects the temperature-regulating mechanisms of the brain, so in high doses, and especially when combined with vigorous physical activity like dancing, it can cause the body to become so drastically overheated that users can literally “burn up” and die from hyperthermia and dehydration. Ecstasy comes in tablet, capsule, crystal and powder form and is usually swallowed or snorted. The effects become apparent within 1 hour and last for up to six hours. The hangover effects may last for up to 24 hours.
Ecstasy does not always contain just MDMA. Ecstasy pills are often mixed with a variety of other substances including aspirin, caffeine and ketamine. Sometimes drugs containing no MDMA are sold as ecstasy. This makes it difficult for people to know what they are taking.
MDMA is the most common club drug being used and is probably the most recognized. This oral drug is an amphetamine derivative that is chemically related to both amphetamines and hallucinogens. An incidence study in the United States has found a 69% increase in use by college students from 1997 to 1999. Users state that they use this substance to increase sensory stimulation at raves and dance parties. Effects include increased positive mood and feelings of intimacy with others, and increased energy and stamina. Many of these raves and circuit parties start in the early hours of the morning and extend into the late afternoon. Patrons state that they ‘require’ the drug to enhance the experience and to be able to endure the long hours of the parties. However, they document that they develop a tolerance to the positive effects of the drug, and, hence, they do not use it regularly. There has been a great deal of concern regarding this drug because of the possible severe adverse systemic effects, as well as the number of documented deaths due to its use. In the United Kingdom, the death rate of 15 to 24-year-old users was found to be from 0.2 to 5.3 per 10,000. Severe systemic effects include hyperthermia, seizures, cardiac abnormalities (tachycardias), hyponatremia, rhabdomyolysis, acute renal failure and death. The majority of effects are due to the drug’s sympathomimetic properties. Due to the heat of the dance venues, as well as sympathetic effects, users experience polydipsia, and can develop severe hyponatremia and seizures.
______
Inhalants:
Mostly made up of everyday household items, these drugs cause brief feelings of euphoria. As the name suggests, inhalants are always inhaled as gases or fumes. The “highs” slightly differ from inhalant to inhalant, but most abusers are willing to huff whatever inhalant they can acquire.
Examples of inhalants include:
- Fumes of markers, paint, paint thinner, gasoline and glue
- Nitrous oxide
- Aerosol sprays
- Room deodorizers
Risks of Inhalant Abuse:
Inhalant abuse can have devastating effects, both immediate and in the long run:
- Loss of smell
- Brain damage
- Nosebleeds
- Weakness
- Euphoria
- Increased heart rate
- Loss of consciousness
- Hallucinations
- Slurred speech
______
New psychoactive substances (NPS):
New psychoactive substances (NPS) are a range of drugs that have been designed to mimic established illicit drugs, such as cannabis, cocaine, ecstasy and LSD. Manufacturers of these drugs develop new chemicals to replace those that are banned, which means that the chemical structures of the drugs are constantly changing to try to stay ahead of the law. New psychoactive substances (NPS) are being developed at an unprecedented rate. NPS have become a global phenomenon with 119 countries and territories from all regions of the world having reported one or more NPS. Up to December 2018, 888 substances have been reported to the UNODC Early Warning Advisory (EWA) on NPS by Governments, laboratories and partner organisations. NPS available on the market have similar effects as substances under international control such as cannabis, cocaine, heroin, LSD, MDMA (ecstasy) or methamphetamine. Looking at the effects of NPS that have been reported until December 2018, the majority are stimulants, followed by synthetic cannabinoid receptor agonists and classic hallucinogens. Based on the patterns of consumption identified up to now, the new psychoactive drugs can be considered companion drugs, used by people who have already taken other illegal drugs.
The United Nations describes NPS as: Any substance in pure form or in preparation that is not included in the 1961 Single Convention on Narcotic Drugs or the 1971 Convention on Psychotropic Substances but that may pose a threat to public health.
Other names of NPS:
Synthetic drugs, designer drugs, legal highs, herbal highs, party pills, synthetic cocaine, synthetic cannabis, herbal ecstasy, NBOMes, bath salts, plant fertiliser, herbal incense, room deodorisers, aphrodisiac tea, social tonics, new and emerging drugs (NEDs), drug analogues and research chemicals. These products can sometimes be marked ‘not for human consumption’.
A designer drug is a structural or functional analog of a controlled substance that has been designed to mimic the pharmacological effects of the original drug, while avoiding classification as illegal and/or detection in standard drug tests. Designer drugs include psychoactive substances that have been designated by the European Union as new psychoactive substances (NPS) as well as analogs of performance-enhancing drugs such as designer steroids. Some of these were originally synthesized by academic or industrial researchers in an effort to discover more potent derivatives with fewer side effects and were later co-opted for recreational use. Other designer drugs were prepared for the first time in clandestine laboratories. Because the efficacy and safety of these substances have not been thoroughly evaluated in animal and human trials, the use of some of these drugs may result in unexpected side effects.
_
UNODC have described six groups or families of emerging substances:
Phenethylamines, tryptamines, piperazines, cathinones, synthetic cannabinoids and a diverse group that covers other types of drugs known as other substances. The mechanism of action and effects of each one depends on their chemical structure and their intervention in specific areas of the CNS. Phenethylamines, piperazines and cathinones release catecholamines and inhibit the reuptake thereof. Synthetic cannabinoids are CB1 cannabinoid receptor agonists. Tryptamines are agonists or partial agonists of serotonin receptors 5HT2. Certain derivatives of phencyclidine and ketamine are NMDA glutamate receptor antagonists. The effects vary depending on the substance and its interaction points, but they are mainly psychostimulant, entactogenic, hallucinogenic and sedative in nature.
_
Tracy and colleagues provide a concise overview of the pharmacology and toxicology of four major Novel Psychoactive Substances categories:
-Stimulants (e.g. mephedrone)
-Cannabinoid NPS (SCRA or ‘Spice’)
-Hallucinogens (e.g. methoxetamine, the NBOMe series)
-Depressants (e.g. benzodiazepine and opioid like NPS such as flubromazepam and AH-7291).
_
Categories of NPS sold in the market
The main substance groups of NPS are aminoindanes (e.g. 5,6-methylenedioxy-2-aminoindane (MDAI)), synthetic cannabinoids (e.g. APINACA, JWH-018), synthetic cathinones (e.g. 4-methylethcathinone (4-MEC) and α-pyrrolidinopentiophenone (α –PVP)), phencyclidine-type substances (e.g. methoxetamine (MXE)), phenethylamines (e.g. 2C-E and 25H-NBOMe), piperazines (e.g. benzylpiperazine (BZP) and 1-(3-chlorophenyl) piperazine (mCPP)), plant-based substances (e.g. kratom (mitragyna speciosa Korth), salvia divinorum and khat (Catha edulis)), tryptamines (e.g. α-methyltryptamine (AMT)), and other substances (e.g. 1,3-dimethylamylamine (DMAA)).
_
Legal situation of NPS:
Since NPS are not controlled under the International Drug Control Conventions, their legal status can differ widely from country to country. Up to 2018, over 60 countries have implemented legal responses to control NPS, with many countries having used or amended existing legislation and others having used innovative legal instruments. Several countries where a large number of different NPS has rapidly emerged, have adopted controls on entire substance groups of NPS using a so-called generic approach, or have introduced analogue legislation that invokes the principal of “chemical similarity” to an already controlled substance to control substances not explicitly mentioned in the legislation. At the international level, up to March 2018, the Commission on Narcotic Drugs decided to place 39 NPS under international control. These control measures have to be implemented into the national legal framework of each country.
_
NPS is a challenge to Public Health
In general, consumption of psychoactive substances has always been a challenge to public health, given that the consequences affect not only the individual who takes them but also their entire setting and society as a whole.
In particular, the use of emerging drugs represents a significant public health problem because of several of the features characterizing them and primarily because:
- They are not illegal.
- They are easily synthesized.
- They are not safe for use.
- They are spread over new technology.
_______
_______
Brief history of drug addiction:
Psychoactive drug use can be traced to prehistory. Opium and its derivatives have been used for centuries, both in a medicinal and ‘recreational’ manner. Indeed, findings of fossilized opium poppy seeds dating as far back as 30,000 years ago suggest the use of opium by Neanderthal man. There is archaeobotanical evidence of the consumption of Ephedra and Cannabis in Neolithic and Bronze Age Europe (around 12,000 years ago); of entoptic imagery in Upper Palaeolithic artwork (produced during altered states of consciousness) (around 40,000 years ago); and fragmentary evidence of fermentation in the deep history of hominid consumption. Peruvian foraging societies were already chewing coca leaves 8,000 years ago, archaeological evidence has shown.
_
Historically, hallucinogens have been commonly used in religious or shamanic rituals. In this context they are referred to as entheogens, and are used to facilitate healing, divination, communication with spirits, and coming-of-age ceremonies. Evidence exists for the use of entheogens in prehistoric times, as well as in numerous ancient cultures, including Ancient Egyptian, Mycenaean, Ancient Greek, Vedic, Maya, Inca and Aztec cultures. One of the earliest recorded examples of the religious use of drugs is a substance that is called “soma” in the the Vedic literature of Hinduism or “haoma” in the sacred literature of Zoroastrianism. A drink made from soma-haoma bestowed alertness, strength, virility, insight, healing, and even immortality when it was drunk in ritual settings. Candidates for soma-haoma that have been proposed by scholars have included honey, opium, cannabis, and hallucinogenic mushrooms. The most likely candidate is ephedra, and modern Zoroastrian priests still prepare a ritual drink called haoma using ephedra or related plants. The Upper Amazon is home to the strongest extant entheogenic tradition; the Urarina of the Peruvian Amazon, for instance, continue to practice an elaborate system of ayahuasca shamanism, coupled with an animistic belief system. Shamans consume hallucinogenic substances in order to induce a trance. Once in this trance, shamans believe that they are able to communicate with the spirit world, and can see what is causing their patients’ illness. The Aguaruna of Peru believe that many illnesses are caused by the darts of sorcerers. Under the influence of yaji, a hallucinogenic drink, Aguaruna shamans try to discover and remove the darts from their patients.
_
A number of animals consume different psychoactive plants, animals, berries and even fermented fruit, becoming intoxicated, such as cats after consuming catnip. Traditional legends of sacred plants often contain references to animals that introduced humankind to their use. Animals and psychoactive plants appear to have co-evolved, possibly explaining why these chemicals and their receptors exist within the nervous system.
_
Alcohol has a long history of use and misuse throughout recorded history. Biblical, Egyptian and Babylonian sources record the history of abuse and dependence on alcohol. Fermented grain, fruit juice and honey have been used to make alcohol (ethyl alcohol or ethanol) for thousands of years. Fermented beverages existed in early Egyptian civilization, and there is evidence of an early alcoholic drink in China around 7000 B.C. In India, an alcoholic beverage called sura, distilled from rice, was in use between 3000 and 2000 B.C. The Babylonians worshiped a wine goddess as early as 2700 B.C. In Greece, one of the first alcoholic beverages to gain popularity was mead, a fermented drink made from honey and water. Greek literature is full of warnings against excessive drinking. Addictive substances have been available for thousands of years. However, addiction could not have begun until human beings developed agriculture (about 13,000 years ago). Prior to that time hunter-gatherer groups did not have access to addictive substances in sufficient quantities to cause addiction. Once humans became able to produce alcohol and grow other addictive substances (marijuana, opium, peyote) in larger quantities it then became possible for addiction to arise. Excessive alcohol misuse and drunkenness were recognized as causing social problems even thousands of years ago. However, the defining of habitual drunkenness as it was then known as and its adverse consequences were not well established medically until the 18th century.
_
Archaeological evidence from various places in the Americas suggest tobacco usage going back at least three or four thousand years. Tobacco was clearly used in social circumstances, and unlike alcohol, it’s certainly not about calories—you don’t need tobacco to survive. And yet it also seems to be the case that tobacco’s cultural usage tended toward diplomacy and ceremony. The offering of a tobacco pipe could be used, as in the eastern North American “calumet,” as a way to initiate diplomacy during war, or to provide a traveller with safe passage through a particular territory, social functions that don’t exactly equate with “recreation.”
_
Drug use in European American society was first acknowledged to be a “problem” in the mid-nineteenth century. By the 19th century, the medical profession was under pressure from unorthodox practitioners offering homeopathy, mesmerism, and other new “scientific” interventions that eschewed unpleasant standard treatments like blistering and bleeding. To retain their wealthy patients, physicians shifted towards managing symptoms rather than attempting dramatic but painful cures, and doctors increasingly prescribed opium. Opium used by William Cullen from the Edinburgh School of Medicine to demonstrate the centrality of the nervous system through animal experiments, was applied in treatment of wide variety of conditions, e.g. chronic respiratory disorders, malaria, syphilis, rheumatism, insomnia, anxiety, fatigue and alcoholism. Increased use of narcotics could be attributed primarily to the fact that only limited range of pharmaceuticals was available to the physicians.
At the same time also recreational opium use found its way to the society thanks to the large number of Chinese workers immigrating to America. It is estimated that almost 25% of them smoked it. Opium known for several thousand years as a folk medicine thus came into widespread use and it was often mixed with another New World import, tobacco.
In I805 morphine the active ingredient of opium was first isolated. Fifty years after the invention of the hypodermic syringe allowed administration of the drug in far more concentrated form, thus having a profound influence on the opiate problem. Although morphine can be smoked or eaten, injection is the preferred means till nowadays.
In 1898 heroin was produced from morphine. Originally it was believed to have all the therapeutic qualities of morphine without the most serious side effect. However, it was quickly showed the opposite.
The end of the nineteenth century also saw a dramatic increase in cocaine use, first introduced to Europe in the 16th century. Leaves of coca (Erythroxylum coca) had been chewed by the Aymara Indians of Peru for more than 1000 years without any evidence showing the coca plant’s potential for addiction. Also heart attacks and strokes were, and still are, uncommon in this group of drug-takers, because the physical constraints of leaf chewing restrict the amount of cocaine that can be introduced into the bloodstream.
The benign phase of cocaine consumption abruptly came to an end in 1884, when Freud published his famous paper praising cocaine as a miracle drug and recommended it same as a number of American physicians in the treatment of alcoholism and morphine addiction. Cocaine also quickly found wide acceptance as an effective local anesthetic agent, especially in ophthalmic surgery, in treatment of “wasting diseases”, e.g. dyspepsia, typhoid fever, kidney disease, hay fever, colds, and sinus conditions. Later the problem of cocaine abuse rose, because of its inappropriate medical application as a stimulant.
In the second half of the 19th century an awareness of physicians that alcohol distorts the view of reality was emerging. Up to present day otherwise persists the tension between medical view of addiction as a disease and a moral intolerance of intoxicants, weakening their self-restraint, impairing moral faculty, and damaging their soul. During the 20th century, many governments across the world initially responded to the use of recreational drugs by banning them and making their use, supply, or trade a criminal offense. A notable example of this was Prohibition in the United States, where alcohol was made illegal for 13 years. However, many governments, government officials and persons in law enforcement have concluded that illicit drug use cannot be sufficiently stopped through criminalization.
_
Historically an addiction was defined as a dependence on a psychoactive substance. This substance would alter the brain chemistry, activate neuronal circuits that underline reinforcement, as well as circuits that produce powerful emotional memories, and subsequently cause dependence. However, the number of addiction definitions has grown during the second half of the 20th century to include also so-called behavioral, soft, process or non-substance related addictions like gambling, compulsive sexual behaviors etc. Currently the addiction concept remains controversial, because there are explicit criteria for its definition missing. Sussman & Sussman (2011) in their systematic review analyzed 52 studies grappling with views of addiction and discovered that they include five common elements representing necessary and sufficient conditions for a psychological state or pattern of behavior to be an addiction:
- engagement in the behavior to achieve appetitive effects,
- preoccupation with the behavior,
- temporary satiation,
- loss of control and
- suffering negative consequences.
The precise concept of addiction based on a well confirmed, substantive theory covering all the phenomena has not been found anyway, and further empirical and theoretical work to develop it is necessary. The concept of addiction also differs from the view of clients and experts. Clients tend to define addiction in terms of needs, urges, and diminished control whereas expert focus more on the compulsive aspects of the behavior, the presence of physical dependence, and diminished control.
______
______
Statistics of drug addiction:
Substance use and substance use disorders are prevalent worldwide. Scientific evidence has consistently shown that alcohol, tobacco, and illegal drug use cause considerable morbidity and mortality. Results from the World Health Organization’s (WHO) World Mental Health (WMH) surveys of 17 countries reveal that substance use is pervasive throughout the world. Alcohol is used by 41% to 97% of adults in their lifetimes, and tobacco products are consumed by 17% to 74% of adults. In addition, cannabis is the illicit drug most commonly used, but use varies widely from a low rate of 0.3% in the People’s Republic of China to a high lifetime rate of 42% in the United States and New Zealand. Lifetime cocaine use ranges from less than 1% in some countries to 16.2% in the United States. These country-level variations highlight that substance use is fairly heterogeneous both within a region and across countries.
_
About 275 million people worldwide, which is roughly 5.6 per cent of the global population aged 15–64 years, used drugs such as cocaine, cannabis, other hallucinogens, opiates and sedative hypnotics at least once during 2016. Some 31 million of people who use drugs suffer from drug use disorders, meaning that their drug use is harmful to the point where they may need treatment. Initial estimations suggest that, globally, 13.8 million young people aged 15–16 years used cannabis in the past year, equivalent to a rate of 5.6 per cent. Roughly 450,000 people died as a result of drug use in 2015, according to WHO. Of those deaths, 167,750 were directly associated with drug use disorders (mainly overdoses). The rest were indirectly attributable to drug use and included deaths related to HIV and hepatitis C acquired through unsafe injecting practices. Opioids continued to cause the most harm, accounting for 76 per cent of deaths where drug use disorders were implicated. Persons Who Inject Drugs (PWID) — some 10.6 million worldwide in 2016 — endure the greatest health risks. More than half of them live with hepatitis C, and one in eight live with HIV. The U.N. estimates that illicit drug use causes over 200,000 deaths globally, most of them being in their mid 30’s. According to the World Health Organization’s report, approximately half of the total world population drinks alcohol.
_
As revealed in figure below, substance use is not a static phenomenon. In the late 1990s, the main drugs of problematic use as measured by treatment demand were cocaine in North and South America, cannabis in Africa, and opiates in Europe, Asia, and Oceania. These patterns have changed over time. In 2008, the treatment demand for abuse of cocaine in North and South America has decreased, but the demand for treatment has increased for abuse of amphetamines (including methamphetamines) in North and South America and for abuse of cannabis in South America. Likewise, the demand for treatment related to abuse of opiates has decreased in Europe, Asia, and Oceania in the past decade, whereas the demand for treatment is estimated to have increased for abuse of amphetamines (in Asia and Oceania), cannabis (in Europe and Oceania), and cocaine (in Europe). In Africa, the demand for treatment related to abuse of cannabis remains high, but the demand for treatment related to abuse of opiates also has increased.
Figure above shows main problem drugs as reflected in treatment demand, by region, from the late 1990s to 2008.
_
World Drug Report 2018:
Cannabis was the most widely consumed drug in 2016, with 192 million people using it at least once during the previous year. The global number of cannabis users continues to rise and appears to have increased by roughly 16 per cent in the decade to 2016, reflecting a similar increase in the world population. Drugs such as heroin and cocaine that have been available for a long time increasingly coexist with new psychoactive substances (NPS) and prescription drugs. A growing stream of pharmaceutical preparations of unclear origin destined for non-medical use, together with poly drug use and poly drug trafficking, is adding unprecedented levels of complexity to the drug problem.
The majority of people who use drugs are men, but women have specific drug use patterns, the Report finds. The prevalence of non-medical use of opioids and tranquillizers by women remains at a comparable level to that of men, if not actually higher. Women with substance use disorders are reported to have high rates of post-traumatic stress disorder and may also have experienced childhood adversity such as physical neglect, abuse or sexual abuse. Women continue to account for only one in five people in treatment. The proportion of females in treatment tends to be higher for tranquillizers and sedatives than for other substances. Drug use treatment and HIV prevention, treatment and care should be tailored to the specific needs of women.
While women who use drugs typically begin using substances later than men, once they have initiated substance use, women tend to increase their rate of consumption of alcohol, cannabis, cocaine and opioids more rapidly than men. This has been consistently reported among women who use those substances and is known as “telescoping”. Another difference is that women are more likely to associate their drug use with an intimate partner, while men are more likely to use drugs with male friends.
Women may not only be victims, but also active participants in the drug trade. Women play important roles throughout the drug supply chain. Criminal convictions of women who presided over international drug trafficking organizations — particularly in Latin America, but also in Africa — attest to this. Women’s involvement in opium poppy cultivation in Afghanistan and coca cultivation in Colombia is well documented, as is the role that women play in trafficking drugs, as drug “mules”. However, there is a lack of consistent data from Governments to enable a deeper understanding of those roles: 98 countries provided sex-disaggregated drug-related crime data to UNODC for the period 2012–2016. Of the people arrested for drug-related offences in those countries during that period, some 10 per cent were women. As suggested in several studies, women may become involved in drug trafficking to sustain their own drug consumption; however, as shown in other studies, some women involved in trafficking in drugs are victims of trafficking in persons, including trafficking for the purposes of sexual exploitation.
_
The National Institute of Drug Abuse (NIDA), National Institute on Alcohol Abuse and Alcoholism (NIAAA) and the Services Administration for Mental Health and Substance Abuse (SAHMSA) have devoted substantial resources to track patterns of drug use, abuse and its consequences for several decades. A detailed description of the methods and findings of these rich resources are beyond the scope of this article, but these data have had major impact on establishment of policy and prevention programs for drug use in the U.S. The most important ongoing descriptive study of drug use in American youth is the Monitoring the Future (MTF) survey. This survey, sponsored by NIDA since 1975, provides information on annual trends in adolescent substance use via an anonymous paper-and-pencil questionnaire in nationally-representative cross-sectional school-based samples of 8th, 10th and 12th graders (Johnston et al. 2011). MTF study conducted in 2010, included 46,482 participants (Johnston et al. 2011). The survey focuses on overall substance use rather than diagnostic information (i.e. abuse and dependence). Key findings from this study include increases in the overall rate of illicit drug use for all grades (Johnston et al. 2011). Older students in the study (12th graders) showed increases in the use of marijuana and high rates of alcohol use (Johnston et al. 2011). Information garnered from the MTF receives national attention and has helped to guide public policy related to substance use in the U.S.
_
Quick Facts on Drug Addiction in the U.S.
- According to the National Survey on Drug Use and Health (NSDUH), 19.7 million American adults (aged 12 and older) battled a substance use disorder in 2017.
- Almost 74% of adults suffering from a substance use disorder in 2017 struggled with an alcohol use disorder.
- About 38% of adults in 2017 battled an illicit drug use disorder.
- That same year, 1 out of every 8 adults struggled with both alcohol and drug use disorders simultaneously.
- In 2017, 8.5 million American adults suffered from both a mental health disorder and a substance use disorder, or co-occurring disorders.
- Drug abuse and addiction cost American society more than $740 billion annually in lost workplace productivity, healthcare expenses, and crime-related costs.
_
Substance use and global burden of disease:
Substance use problems are among the leading contributors to the global burden of disease. The magnitude of societal burden resulting from substance abuse is enormous. Substance abuse not only affects personal health and accomplishments, but also negatively affects the quality of life of abusers’ family members (e.g., financial security, mental health, social networks, and productivity) and the functioning of society at large (e.g., the criminal justice and health care systems). For example, in the United States, the direct and indirect economic cost to individual users, their families, and society was estimated to be $21.9 billion for heroin addiction and $184.6 billion for alcohol use problems per year. Indeed, problems associated with substance abuse are so pervasive that they can affect nearly every aspect of the abuser’s life. These problems may include: employment issues, injuries, violence, assaults, child neglect or abuse, incarceration, suicidal behaviors, psychiatric disorders, cognitive impairments, transmission of sexually transmitted diseases (e.g., HIV/AIDS), damage to multiple organs (e.g., respiratory, immune, digestive, cardiovascular, reproductive, and pancreatic systems), and mortality. In particular, substance use-related behaviors are a major contributor to the HIV/AIDS epidemic, either through sharing of injection equipment or substance use-related risky/unprotected sexual behavior.
_
Drug abuse in India, 2019:
Among adults (age 15+), 28.6% of the population (267 million) currently uses tobacco products in India. Alcohol is the second most common psychoactive substance used by Indians. Nationally, about 14.6% of the population between 10 and 75 year of age uses alcohol. In terms of absolute numbers, there are about 160 million persons who consume alcohol in the country. After Alcohol, Cannabis and Opioids are the next commonly used substances in India. About 2.8% of the population (31 million individuals) reports having used any cannabis product within the 2018. About 2.1% of the country’s population (22.6 million individuals) use opioids which includes Opium (or its variants like poppy husk known as doda/phukki), Heroin (or its impure form – smack or brown sugar) and a variety of pharmaceutical opioids. Nationally, the most common opioid used is Heroin (1.14%) followed by pharmaceutical opioids (0.96%) and Opium (0.52%). A sizeable number of individuals use Sedatives and Inhalants. About 1.08% of 10-75 year old Indians (approximately 11.8 million people) are current users of sedatives (non-medical, nonprescription use). Inhalants (overall prevalence 0.7%) are the only category of substances for which the prevalence of current use among children and adolescents is higher (1.17%) than adults (0.58%). Other categories of drugs such as, Cocaine (0.10%) Amphetamine Type Stimulants (0.18%) and Hallucinogens (0.12%) are used by a small proportion of country’s population.
Drug trafficking in India:
According to a 2018 report by United Nations-backed International Narcotics Control Board (INCB), India is one of the major hubs for illicit trading of drugs. The drugs range from cannabis to more recent prescription drugs like tramadol. According to an official of the Red Cross Drug Deaddiction and Rehabilitation Centre, Gurdaspur, “The geographical location of the district makes it prone to trafficking of many types of drugs. This affects not only the dealers but also the people, as the drugs are easily available and are cheaper.” These drugs reach into India through Punjab via the India-Pakistan border, or through a more circuitous route wherein they first reach Africa and then come to Delhi and Punjab. The rivers and streams along the border are preferred routes for smugglers to slide in drugs as they are not easily tracked by the Indian forces. Kashmir has also become a new source of drugs for Punjab. In Kashmir, cannabis is locally cultivated whereas heroin and cocaine enter the Valley through the Line of Control which is then transported to other regions.
India accounts for 1.62% of the world’s seizures of illegal drugs. Proximity to the largest producers of heroin and hashish – the Golden Triangle (Southeast Asia) and Golden Crescent (Afghanistan, Pakistan & Iran) is one of the main reasons for drug trafficking in India making its border vulnerable. Additionally, Nepal is a traditional source of cannabis. India is both a destination and a transit route for drug traffickers in these regions. As a consequence of smuggling of narcotic drugs across the border, Indian states bordering with neighbouring countries in Northeast, North and Western parts have been affected with narco – terrorism – a term to describe trafficking of narcotics by terrorist groups as a quid pro quo for the funds which are utilized to create terror in the form of assassination, extortion, hijacking, bombing, kidnapping and the general disruption of the government.
Drug abuse and Punjab:
Drug consumption in Punjab is three times the national average. Due to Punjab’s proximity to the border, the state serves as a transit route for smugglers for the distribution of drugs in the state and the rest of the country. Youth who are unemployed often resort to narcotics in the hope of forgetting their troubles. Sometimes, the youth try drugs for fun under the influence of their peers, which often results in addiction. The Punjabi music industry only exacerbates the problem, as glorification of drugs has become a trend. The problem was so severe that it prompted the Punjab government to set up a “culture commission” to tackle the “menace of vulgarity” and its complete eradication by monitoring songs. Drug abuse problems in women are increasing at a very fast rate. Despite the increasing number of drug addicts, not many women seek help. One reason for this is that women’s drug abuse problems are often stigmatized. Drug abuse and addiction in women is a source of constant anxiety for not only the women but for their families as well. Thus, the women are usually reluctant to access the treatment and rehabilitation.
The bane of drug abuse in Punjab has acquired the proportions of a pestilence that has shaken the entire society in the state. It is observed that in Punjab “drug abuse” is a raging epidemic, especially among the young. According to one survey, 66% of the school going students in the state consume “gutka” or tobacco; every third male and every tenth female student have taken to drugs on one pretext or another and seven out of ten college-going students are into drug abuse. A recent government study suggests that more than 860,000 young men in the state, between the ages of 15-35, take some form of drugs. Heroin is the most preferred, used by 53% of all addicts. But opium and synthetic drugs such as crystal methamphetamine are also common. It is astonishing how widespread the problem is. One estimate says that more than two-thirds of Punjab’s households have at least one addict in the family.
______
______
Why people take addicting drugs?
The following diagram shows the three major influences on an individual’s decisions about drug use. Addressing drug-related harm needs to consider the links between these different factors.
_
There are several reasons why drug usage soon gets changed to drug abuse. At a very basic level this happens because the person concerned feels a desperate need to deal with stress, to get a momentary high or to just ‘fit in’ with his or her peers, as happens in the case of youngsters. It soon reaches a stage where this need becomes much more than other needs in life and the person begins to believe their survival depends on those drugs. One of the major reasons for drug abuse – and this is especially applicable for youngsters doing drugs – is its presence, and at times glorification, in popular media such as television series and films. Quite often it so happens that doing drugs is romanticized and some fictional positive aspects of the same are shown. Thus it becomes a thrilling and seductive affair for youngsters who can be misguided easily because of their relative lack of experience in life. Education alone isn’t enough to help an addict get clean. But learning about the dangers of drugs can be an important step if you’re thinking about experimenting with heroin, marijuana or meth — or if you’re wondering whether you’re ready to seek help for addiction.
_
Apart from the case of beginning drug use via a prescription from a doctor, there are 4 main reasons people may try substances, according to NIDA:
- To feel good. Drugs may lure people with the appeal of:
-A euphoric high.
-Feelings of power.
-Increased confidence.
-Energy.
-Relaxation.
- To feel better. Someone with anxiety, high stress, or depression might turn to drugs to try and manage distressing symptoms.
- To do better. Some drugs have the reputation of improving athletic or academic performance, so people may see them as a way of getting ahead or even just keeping up.
- To fit in or experiment. People, adolescents especially, may use out of sheer curiosity or to try and impress their peers.
People who have an intensely good experience their first time using begin to learn that drugs can make them feel great, and the foundations of addiction are set. Not everyone responds the same way to drugs and alcohol, however.
_
Here is a list of important reasons why people use drugs:
- Experimenting
It is not uncommon for addiction to stem from a person being curious and experimenting with drugs or alcohol. It is a scenario that often starts with a young person using alcohol or marijuana out of curiosity. While it seems harmless, adolescents that experiment with drugs and alcohol are more likely to develop substance use disorder according to the National Institute on Drug Abuse.
- Family History/Genetics
If you have a family history of drug addiction, you may have a genetic predisposition to develop an addiction to drugs or alcohol. It is stated that about 50% – 60% of a person’s risk for addiction is linked to the genes they are born with along with other social factors.
- Prescription Drugs
There is a popular misconception that any medication prescribed by a doctor is safe. Unfortunately, that is not always the case. Doctors prescribe medications to alleviate symptoms of physical or mental health issues. However, many individuals are not properly educated on the risks that the medications may carry. Chronic pain is often managed through opioid medications, which are highly addictive. Dependent upon the amount used and other factors, someone may require a medical detox just to stop using opioids. Likewise, those suffering from anxiety and depression may be prescribed addictive medications to ease symptoms. Non-addictive medication and/or pain recovery services are often available.
- Loneliness
Addiction can start when an individual feel lonely or is isolated from the friends and family. They turn to drugs and alcohol thinking that it will fill a void that they have been living with. People lacking positive daily interaction may choose to use substances to feel happy or content. Additionally, users begin to alienate themselves further if they fear being judged or that help is not available to them.
- Peer Pressure
Peer pressure usually applies to adolescents or young adults. The need to fit in, on some level, is built into each and every one of us. Some people may feel the need to participate in potentially harmful activities to do so. The pressure of being around others who are abusing drugs or alcohol can push someone to follow suit. Drug use is in part the result of socialization. Children try drugs when their friends convince them to do it, and these decisions are based on social norms about the risks and benefits of various drugs as seen in the figure below.
Figure above shows use of various drugs by grade 12 students in 2005 in the U.S.
_
- Feel good/feel high
Drugs can make you feel good. People chase the high they once experienced. Ask anyone who has tried drugs and they will tell you that it is one of the best feelings of their life. The highs from drugs are so much more extreme than regular everyday joys because most drugs overload the pleasure sensors in your brain. Once a person feels this extreme pleasure, it’s common for that person to become hooked on a drug simply chasing the initial high they once felt. As we all know, this is a viscous cycle that is extremely difficult to break. The highs are equally as powerful as the lows felt when coming off of the drugs.
- Mental Health Disorders
Depression, anxiety, and PTSD can put individuals at higher risk of developing an addiction. Using substances to cope with difficult feelings may seem like an easier path for some. Though they may seem crippling at times, there is help available to anyone struggling with a mental health disorder. Non-narcotic medications are often available for most mental health disorders. It’s worth researching with a doctor to see if there is an alternative to addictive medications.
- Recreation
Many people use drugs or alcohol socially with friends or to “unwind” after a long day. They often see substances as a way to relax or clear their minds. Recreational drug users are still at risk to become addicted if their use becomes more frequent or they use highly addictive substances.
- Self-Medicating
The self-medication hypothesis began appearing in medical journals in the 1970s, as clinicians noticed that heroin addicts were using the drug to cope with problems such as stress and loneliness. The self-medication theory suggests that use develops as a way of coping with stress in the absence of adequate solutions and meaningful social relationships. The self-medication theory of addiction suggests that suffering is at the heart of addictive disorders (Khantzian, 2012). That is, individuals with deficits in emotion-regulation skills (i.e., skills relevant for modifying emotional reactions and tolerance for negative emotions) use drugs in an attempt to manage negative or distressing affective states. Alcohol is frequently used as a way of coping with social anxiety. The drinking removes, at least temporarily, the stress of anxiety. Mate (2010) suggests that addictive behaviors ultimately driven by our unwillingness to allow ourselves to really feel and experience pain, frustration, fear, and all the negative emotions that are part of being human. Instead, we choose the chemical shortcut to avoid those emotions and become trapped there. People struggling with any of a multitude of ailments may turn to drugs or alcohol to ease their pain. While some who take a hard line on addictions believe the self-medication theory is an excuse for irresponsible behavior, many in the medical profession find it useful to transition people from substances and behaviors that they are addicted to and are causing the problems to more controllable prescription medications that address the underlying problem directly. Depression, for example, can often be successfully treated with antidepressant medication, freeing the individual from seeking emotional comfort in their addiction.
- Boredom
People become bored and think drugs will help. Boredom is a big factor in drug abuse in teens and young adults. People in this age bracket generally don’t have bills, jobs and all the stresses that go along with adulthood. So it’s easier to become bored and want to try something new and exciting. Drug use is often thought of as a way to escape the mundane world and enter an altered reality.
- Stress
People think drugs will help relieve stress. Our modern world is full of new strains and stresses that humans have never experienced in the past. Although many things in life are now easier than ever, the burdens are also very high. Simply having a family, maintaining a household, and holding a job are huge stress factors. Some drugs are viewed as a means of relaxation – a way to calm the storm in your mind. Although drugs can be very effective at doing that, there can be serious side effects.
- Painful memories
People use drugs to cover painful memories in their past. Many people go through extremely traumatic events in their life, many times as children, and turn to drugs to cover the horrible memories. Children are extremely susceptible to trauma, whether physically or emotionally, and those feelings can haunt them into their adulthood. These people could benefit from working with psychologists to help repair their damaged mind. Drugs usually only deepen the issue.
- Cultural attitudes
The value that a person attaches to using drugs is strongly influenced by the community in which the person lives (Wilson, 2005). For example, students drink more on campuses that have a strong drinking culture, few alcohol-control policies on campus and easier access to alcohol through special promotions and low pricing by local stores and bars (Sher and Rutledge, 2007). Social norms help to define the circumstances in which it is appropriate to drink and how much alcohol should be consumed.
- Financial incentives
Evidence shows that people will stop using when the costs become too high (Dalrymple, 2006). Many of the states that have the lowest smoking rates are those that have been the most aggressive about indoor smoking laws and about state taxes that drive up the cost of cigarettes. In general, when cigarette’s price increases people smoke less. Increases in taxes on alcohol lead to reductions in alcohol consumption generally and reductions specifically in binge and other kinds of excessive drinking.
- Personality
Impulsivity is a personality trait that has often been identified as a risk factor for alcohol and other substance misuse (MacKillop, 2016). Addicted individuals assign lower values to delayed rewards than to immediate ones. The excessive preference for the immediate rewards despite longer-term consequences leads to problems with addiction.
- Grieving
The death of a loved one, such as a close friend or family member, or even a mentor who positively influenced a person, is emotionally devastating for people. Different people handle grief in different ways. Some people are able to seek counseling or work through grief on their own in healthy ways. Other people really struggle with emotional or physical loss, so they use drugs as a way of coping with grief in the short-term. However, this short-term coping mechanism may transition into a long-term dependence for some people.
- End of a Relationship
The end of a relationship is one of the most emotionally destructive events in a person’s life. When a relationship ends through a breakup or divorce, it can negatively impact self-confidence. This goes on to affect other areas of life including career, friendships, families and even one’s ability to find a purpose. If the person doesn’t have appropriate emotional support available to them, they may use drugs as a way of grieving the loss of their relationship.
- Instrumental drug use
The phrase `instrumental drug use’ has been used to denote drug use for reasons specifically linked to a drug’s effects (WHO, 1997). Examples of the instrumental use of amphetamine-type stimulants include vehicle drivers who report using to improve concentration and relieve tiredness, and people who want to lose weight (particularly young women), using these drugs to curb their appetite.
- Functional perspective
The most popular functions for drug use are to: relax (96.7%), become intoxicated (96.4%), keep awake at night while socializing (95.9%), enhance an activity (88.5%) and alleviate depressed mood (86.8%).
____
Below is a graphical representation of the risk factors for drug abuse:
Only a minority of people who use drugs ultimately become addicted — just as not everyone is equally at risk for the development of other chronic diseases. Susceptibility differs because people differ in their vulnerability to various genetic, environmental, and developmental factors. Many genetic, environmental, and social factors contribute to the determination of a person’s unique susceptibility to using drugs initially, sustaining drug use, and undergoing the progressive changes in the brain that characterize addiction. Factors that increase vulnerability to addiction include family history (presumably through heritability and child-rearing practices), early exposure to drug use (adolescence is among the periods of greatest vulnerability to addiction), exposure to high-risk environments (typically, socially stressful environments with poor familial and social supports and restricted behavioral alternatives and environments in which there is easy access to drugs and permissive normative attitudes toward drug taking), and certain mental illnesses (e.g., mood disorders, attention deficit–hyperactivity disorder, psychoses, and anxiety disorders). It is estimated that the most severe phenotypic characteristics of addiction will develop in approximately 10% of persons exposed to addictive drugs. Thus, although long-term exposure to drugs is a necessary condition for the development of addiction, it is by no means sufficient. Yet for those in whom there is progress to addiction, the neurobiological changes are distinct and profound.
_
For years, experts have debated if it was nature (biology/ genes) or nurture (upbringing/ environment) that determined whether someone will become addicted. Now, the prevailing view is that there is no one thing we can look at to predict someone’s risk of developing drug addiction—rather, the interaction of the person’s unique biology and environment both influence how the drug will impact a person’s susceptibility to becoming addicted. There is also gene/environment interaction in such way that individuals may self-select into different environments, e.g., they may seek out work environments where addictive substances are more readily available.
Biological factors impacting addiction account for between 40% and 60% of someone’s risk for addiction.
Possible biological factors include:
- Genes and epigenetics (the way environment impacts gene expression).
- Gender.
- Ethnicity.
- Stage of development.
The person’s developmental stage is particularly important, since teens who use drugs are much more likely to become addicted and remain addicted into adulthood.
Environmental factors include all situations and experiences a person lives through.
The most significant environmental influences include:
- Home environment.
- Family dynamics.
- Friends.
- School.
According to journalists, public officials, and even popular song writers, kids who drop out of school early are inviting disaster. Not only are they undermining their future earnings, but life on the streets paves the way to delinquency, drugs, and worse. Years-of-school is negatively correlated with illicit drug use. There is evidence that early drug use causes students to drop out of school, and, conversely, there is evidence that early success in school protects against later drug use. A study found that years-of-school predicts lower levels of illicit drug use after controlling for IQ and impulsivity.
_
What other factors increase the risk of addiction?
-Early Use.
Although taking drugs at any age can lead to addiction, research shows that the earlier a person begins to use drugs, the more likely he or she is to develop serious problems. This may be due to the harmful effect that drugs can have on the developing brain. It also may result from a mix of early social and biological risk factors, including lack of a stable home or family, exposure to physical or sexual abuse, genes, or mental illness. Still, the fact remains that early use is a strong indicator of problems ahead, including addiction.
-How the drug is taken.
Smoking a drug or injecting it into a vein increases its addictive potential. Both smoked and injected drugs enter the brain within seconds, producing a powerful rush of pleasure. However, this intense high can fade within a few minutes. Scientists believe this starkly felt contrast drives some people to repeated drug taking in an attempt to recapture the fleeting pleasurable state.
-Comorbid disorders.
Individuals with comorbid (i.e., co-occurring) mental health disorders such as depression, anxiety, attention-deficit/hyperactivity disorder (ADHD) or post-traumatic stress disorder are more likely to develop substance use disorders.
_____
Each person will have a number of biological and environmental, risk and protective factors. A risk factor is something that puts the individual in more danger of becoming addicted, while a protective factor is something that minimizes that danger.
Possible biological and environmental risk factors include:
- Family history of addiction.
- Family history of mental illness.
- Chaotic home life.
- Adverse childhood experiences (ACE) like neglect or physical, mental, or sexual abuse.
- Negative attitudes of parents and friends.
- Unsupportive community.
- Poor school achievement.
- Easy access to drugs and alcohol.
Possible biological and environmental protective factors are:
- No family history of addiction or mental illness.
- Good physical health.
- Supportive, involved family.
- Healthy relationships at home and in the community.
- Access to positive resources in the neighborhood like community groups, safe playgrounds, recreation centers, etc.
- Academic success.
- Strong impulse control.
Finally, the risk of addiction may be strongly impacted by the route of administration of the abused substance. Certain routes will produce stronger highs. For example, injecting opioids will produce a rapid intense euphoria that snorting or swallowing opioids can’t match. Intense highs that come on rapidly also tend to dissipate quickly, and the quicker comedown may further encourage drug abuse.
______
Factors that determine different pathways to substance use and substances use disorders:
Figure above shows the two main categories of factors conferring risk for substance use: genes and the environment. Genetic variants are like switches: they are either turned on or off, but their expression is influenced by experience (i.e., epigenetic modifications). Environmental factors are more like dials that are turned up or down, also depending on experience. Risk or adversity factors include child maltreatment, poverty, poorly equipped schools, dysfunctional families, discrimination and witnessing violence. Resiliency or protective factors include high-quality education, housing, health care, social attachments and parenting. The combination of switches and dials crosses a liability threshold that, when predominantly negative, primes the brain for substance use. The functional relationship between factors is not linear, nor is it static; it fluctuates throughout a lifespan. Some environmental influences confer resiliency and may attenuate the effects of genetic predispositions. Thus, psychosocial interventions and practices are of the utmost importance in determining final outcomes.
_____
Since most people do not become addicts, what is known about the ”non-addict” profile?
Dr. Robert B. Millman, director of the Alcohol and Drug Abuse Service at the Payne Whitney Psychiatric Clinic at the New York Hospital describes the best candidates for this group as ”those people who have strong families, often with religious backgrounds and who have good social relations.” Experts say that the youth who has positive relations with his peers and with adults is less likely to fall prey to drug addiction than the antiauthoritarian loner who is achieving below his potential.
Although no one can say with certainty which kind of family is most likely to produce an addict, many mental health experts have strong views on the subject. For instance, Leon Wurmser, a psychiatry professor and former director of the Alcohol and Drug Abuse Program at the University of Maryland School of Medicine, notes that the potentially addictive child may well have been physically abused by parents, who are often themselves dependent on drugs or alcohol. He notes that the child has often been lied to, shamed and humiliated by parents who act in a highly inconsistent manner. ”The mother may support something that the father strongly disapproves, or a parent may tell the child one thing today and the opposite tomorrow,” he says. This legacy of brutality ”leaves the child in a helpless rage,” Dr. Wurmser says. He does not view authority, which has been represented by the parents, as something which should be respected, but as capriciously cruel. The child can feel completely out of control and is racked by feelings of violence toward those around him. For him, the use of narcotics can be a way of trying to suppress the highly aggressive feelings that have resulted from his early trauma.
____
Now I will discuss some important factors in detail that may lead to drug addiction:
- Age:
Teen brain is more susceptible to addiction:
The brain continues to develop into adulthood and undergoes dramatic changes during adolescence. One of the brain areas still maturing during adolescence is the prefrontal cortex—the part of the brain that allows people to assess situations, make sound decisions, and keep emotions and desires under control. The fact that this critical part of a teen’s brain is still a work in progress puts them at increased risk for making poor decisions, such as trying drugs or continuing to take them. Introducing drugs during this period of development may cause brain changes that have profound and long-lasting consequences.
Figure below shows brain scans showing the healthy development of the brain from ages 5 to 20. The images are from the side and top views, with a focus on the prefrontal cortex.
As the brain matures, experiences prune excess neural connections while strengthening those that are used more often. Many scientists think that this process contributes to the steady reduction in gray matter volume seen during adolescence (depicted as the yellow to blue transition in the figure above). As environmental forces help determine which connections will wither and which will thrive, the brain circuits that emerge become more efficient. However, this is a process that can cut both ways because not all tasks are desirable. The environment is like an artist who creates a sculpture by chipping away excess marble; and just like bad artists can produce bad art, environments with negative factors (like drugs, malnutrition, bullying, or sleep deprivation) can lead to efficient but potentially harmful circuits that conspire against a person’s well-being.
The teenage years are a critical window of vulnerability to substance use disorders, because the brain is still developing and malleable (a property known as neuroplasticity), and some brain areas are less mature than others. The parts of the brain that process feelings of reward and pain—crucial drivers of drug use—are the first to mature during childhood. What remains incompletely developed during the teen years are the prefrontal cortex and its connections to other brain regions. The prefrontal cortex is responsible for assessing situations, making sound decisions, and controlling our emotions and impulses; typically, this circuitry is not mature until a person is in his or her mid-20s.
The adolescent brain is often likened to a car with a fully functioning gas pedal (the reward system) but weak brakes (the prefrontal cortex). Teenagers are highly motivated to pursue pleasurable rewards and avoid pain, but their judgment and decision-making skills are still limited. This affects their ability to weigh risks accurately and make sound decisions, including decisions about using drugs.
Adolescence represents a period of unique vulnerability for developing an addiction. In adolescence, the incentive-rewards systems in the brain mature well before the cognitive control center. This consequentially grants the incentive-rewards systems a disproportionate amount of power in the behavioral decision-making process. Therefore, adolescents are increasingly likely to act on their impulses and engage in risky, potentially addicting behavior before considering the consequences. Not only are adolescents more likely to initiate and maintain drug use, but once addicted they are more resistant to treatment and more liable to relapse.
Most individuals are exposed to and use addictive drugs for the first time during their teenage years. In the United States, there were just over 2.8 million new users of illicit drugs in 2013 (~7,800 new users per day); among them, 54.1% were under 18 years of age. In 2011, there were approximately 20.6 million people in the United States over the age of 12 with an addiction. Over 90% of those with an addiction began drinking, smoking or using illicit drugs before the age of 18.
For these reasons, adolescents are a major target for prevention messages promoting healthy, drug-free behavior and giving young people encouragement and skills to avoid the temptations of experimenting with drugs. Most teens do not escalate from trying drugs to developing an addiction or other substance use disorder; however, even experimenting with drugs is a problem. Drug use can be part of a pattern of risky behavior including unsafe sex, driving while intoxicated, or other hazardous, unsupervised activities.
____
- Adverse Childhood Experiences (ACE):
Adverse childhood experiences (ACEs) are various forms of maltreatment and household dysfunction experienced in childhood. The Adverse Childhood Experiences Study by the Centers for Disease Control and Prevention has shown a strong dose–response relationship between ACEs and numerous health, social, and behavioral problems throughout a person’s lifespan, including those associated with substance abuse.
Children’s neurological development can be permanently disrupted when they are chronically exposed to stressful events such as physical, emotional, or sexual abuse, physical or emotional neglect, witnessing violence in the household, or a parent being incarcerated or suffering from a mental illness. As a result, the child’s cognitive functioning or ability to cope with negative or disruptive emotions may be impaired. Over time, the child may adopt substance use as a coping mechanism, particularly during adolescence. Findings of the Adverse Childhood Experiences (ACE) study demonstrate that unrecognized adverse childhood experiences are a major factor underlying addiction. These adverse childhood experiences result in neurodevelopmental changes and emotional damage (Felitti, 2004). These experiences can predispose one to negative emotional states and create a strong motivation for seeking relief through psychoactive substance use which provides short-term benefit in the face of long-term risks.
A study of 900 court cases involving children who experienced abuse found that a vast amount of them went on to suffer from some form of addiction in their adolescence or adult life. This pathway towards addiction that is opened through stressful experiences during childhood can be avoided by a change in environmental factors throughout an individual’s life and opportunities of professional help. If one has friends or peers who engage in drug use favorably, the chances of them developing an addiction increases. Family conflict and home management is also a cause for one to become engaged in drug or alcohol use.
_______
- Addictive personality:
An addictive personality refers to a particular set of personality traits that make an individual predisposed to developing addictions. This hypothesis states that there may be common personality traits observable in people suffering from addiction. Alan R. Lang of Florida State University, author of an addiction study prepared for the United States National Academy of Sciences, said, “If we can better identify the personality factors, they can help us devise better treatment and can open up new strategies to intervene and break the patterns of addiction.”
Alan R Lang’s research found that, while there is no single set of traits that is definitive of an “addictive personality”, several “significant personality factors” exist, including:
-Impulsivity
-Sensation seeking
-Nonconformity combined with weak commitment to socially valued goals for achievement
-Social alienation and tolerance for deviance
-Heightened stress coupled with lack of coping skills.
Some claim the existence of “addictive beliefs” in people more likely to develop addictions, such as “I cannot make an impact on my world” or “I am not good enough”, which may lead to developing traits associated with addiction, such as depression and emotional insecurity. People who strongly believe that they control their own lives and are mostly self-reliant in learning information (rather than relying on others) are less likely to become addicted. However, it is unclear whether these traits are causes, results or merely associated coincidentally. For example, depression due to physical disease can cause feelings of hopelessness that are mitigated after successful treatment of the underlying condition, and addiction can increase dependence on others.
Most researchers in addiction today would caution against the idea of a single, generic personality that is prone to addiction. In fact, some seemingly disparate traits can lead different people to become addicted to drugs or alcohol, depending on other factors. While there are several different types of traits that can be recognized in individuals who develop substance use disorders, they are not all present in every person who becomes addicted. Therefore, the image that some people see of the socially outcast criminal is an inaccurate vision of the individual who becomes addicted to drugs or alcohol.
_______
- Stress and addiction:
Stress is a well-known risk factor in the development of addiction and in addiction relapse vulnerability. A series of population-based and epidemiological studies have identified specific stressors and individual-level variables that are predictive of substance use and abuse. Preclinical research also shows that stress exposure enhances drug self-administration and reinstates drug seeking in drug-experienced animals. The deleterious effects of early life stress, child maltreatment, and accumulated adversity on alterations in the corticotropin releasing factor and hypothalamic-pituitary-adrenal axis (CRF/HPA), the extrahypothalamic CRF, the autonomic arousal, and the central noradrenergic systems cause changes the corticostriatal-limbic motivational, learning, and adaptation systems that include mesolimbic dopamine, glutamate, and gamma-amino-butyric acid (GABA) pathways which underly the pathophysiology associated with stress-related risk of addiction.
______
- Genes and addiction:
Genetic makeup of a person may play some role in drug and alcohol abuse but there is no single gene which is associated with alcohol and drug abuse. Drug abuse is the result of a complex interplay between the genetic makeup of an individual, and social, biochemical, and environmental factors. It is usually assumed that the vulnerability of an individual to drug abuse is roughly 50% determined by genetic factors while another 50% is nongenetic factors. As a result, many genes involved in modification of neurotransmitter balance collectively play some role in making an individual susceptible to alcohol and drug abuse. Since a number of genes are involved, the effect of an individual gene in making a person vulnerable to alcohol or drug abuse may be modest. Moreover, repeated exposure of a drug to the human brain may also cause epigenetic changes such as histone modification (acetylation and methylation), DNA methylation, and modification of noncoding RNA. Like many drugs, drugs of abuse are also metabolized by various liver enzymes. Polymorphisms of genes causing modification of enzymatic activities of these enzymes are also linked to addiction as well as susceptibility of toxicity of certain abused drugs.
_
Addiction is a complex disease that is multifactorial and polygenic, thus it does not follow a clear Mendelian pattern of gene expression. Unlike disorders such as Down’s syndrome, no single gene has been identified that predisposes individuals to develop addictive behaviours. However, genetic background is believed to influence addiction liability with mutations in certain genes believed to increase an individual’s vulnerability to addictive behaviours should they engage in drug use. Twin and adoption studies indicate the heritability of genes that predispose an individual to becoming addicted ranges from 40% to 70% (alcohol: 50%, cocaine 60%, and opiates 70%). That is up to 70% of the risk for addictive behaviours can be attributed to heritable influences, with a 4–8-fold increase in the risk of developing an addictive behaviour if a first-degree relative has a substance abuse disorder. Another study found heritability estimates for addictions range between 40% (hallucinogens) to 70 % (cocaine). To date 1,500 genes have been linked to an “addiction” phenotype in humans which can further be classified as those related to the initial stages of experimentation, those related to neuroadaptations following continued exposure, and those that influence outcome including the age of onset and patterns of use. The influence of genetic background over addiction appears additive; the more mutations an individual has, the greater their vulnerability to becoming addicted with different genes contributing to addictive behaviours in different individuals is. However environment may also exert considerable influence over the development of addiction, which is further confounded by gene-environment interactions. Many psychiatric disorders including depression, stress, and anxiety coexist with substance abuse disorders, as such heritable factors that influence these disorders may be perpetuated by adverse environmental exposures which may act as a trigger to activate a genetic predisposition and influence behavioural outcome, that is, it increases the risk of substance use.
_
_
Twin Studies:
A traditional study paradigm used to identify the role of genetic factors in the etiology of a trait or disorder is the study of twins. Typically, a comparison is made between the prevalence of a disorder among twin pairs who possess identical genes (monozygotic or identical twins) and twin pairs who have only half of their genes in common (dizygotic or fraternal twins). For any disease, if the environment has no influence, monozygotic twins would always be concordant (similar) with respect to the disease. However, because both genetic and environmental factors play a role, it is generally not possible to discriminate among the many possible influences. Additionally, monozygotic twins are often raised in similar environments (e.g., they are dressed alike, often share friends, and copy each other’s behaviors) and often share environmental factors to a greater extent than dizygotic twins, which makes it difficult to discriminate between genetic and environmental influences (Helzer and Burnam, 1991).
Nonetheless, many twin studies have provided useful insight regarding the possible role that genetic factors play in the familial aggregation of drug abuse (Cloninger et al., 1981; Gurling et al., 1981; Hrubec and Omenn, 1981; Pedersen, 1981; Murray et al., 1983; Pickens et al., 1991). Studies performed on twins found that rarely did only one twin have an addiction. In most cases where at least one twin suffered from an addiction, both did, and often to the same substance. Cloninger and colleagues (1981) and others have found that monozygotic twins are about twice as likely as dizygotic twins (of the same sex) to be concordant for alcoholism. The highest twin correlations, however, were reported for nicotine and caffeine, based on a study of the Swedish twin registry (Pederson et al., 1981). The role of genetic factors in the etiology of drug abuse for monozygotic twins reared apart has been studied (Grove et al., 1990). Researchers examined the concordance for alcoholism, illicit drug abuse, and antisocial personality disorder among monozygotic twin pairs separated at birth and found that the heritability of illicit drug abuse exceeded that of alcoholism. Pickens and colleagues (1991) found that the drug abuse concordance rate was significantly greater for monozygotic twins than for dizygotic twins in males but not in females. Furthermore, illicit drug abuse has been found to be associated with conduct disorder in childhood and with antisocial personality in adulthood. The aggregate of these findings suggests that genetic factors explain some of the variance in the development of drug abuse and that a large proportion of the heritability of drug abuse in adulthood may be attributed to genetic factors that underlie the development of behavior problems in childhood (Cadoret et al., 1980; Grove et al., 1990).
The risk of lifetime cannabis use, defined as any use of cannabis during the lifetime, varies between individuals. Previous studies have shown that individual differences in lifetime cannabis use can be partly explained by genetic differences between individuals; a meta-analysis of twin studies reported significant heritability estimates of lifetime cannabis use of 48% for males and 40% for females. Shared environmental factors, such as cannabis availability and parental monitoring, also have a role accounting for 25 and 39% of the risk for males and females, respectively. Also, there is substantial overlap in the genetic risks underlying lifetime cannabis use and cannabis use disorder.
Adoption Studies:
The optimal study paradigm for discriminating the interaction of genetic and environmental factors in the development of a trait or disorder is cross-adoption studies, in which adoptees with biological vulnerability for drug abuse, for example, are reared in homes of non-drug-abusing adoptive parents, and adoptees whose biological parents lack a history of drug abuse are reared in homes of parents with drug abuse. Cross-adoption studies of children of alcoholics who were raised by nonalcoholic adoptive parents have shown a three- to fourfold increased risk for alcohol abuse and dependence compared to adoptees whose parents were not alcoholics (Schuckit et al., 1972; Goodwin et al., 1973; Cadoret et al., 1980; Bohman et al., 1981; Cloninger et al., 1981).
____
Epigenetics:
Our knowledge regarding the role of epigenetics in addictive behaviours is relatively new. A current hypothesis is that exposure to drugs of abuse results in stable epigenetic modifications that alter gene expression and neuroadaptive changes seen during the transition to, and maintenance of, an addicted state. It is also believed that these epigenetic changes act to perpetuate relapse following periods of abstinence. Of the possible epigenetic processes known DNA methylation and posttranslational modification of histones are currently the best understood. However, while both these processes have the ability to mediate downstream neuroadaptive changes, they do not appear mutually exclusive.
Addiction is often described as maladaptive neural plasticity in response to drugs of abuse, which results in long-term molecular alterations in key brain regions leading to life-long behavioral abnormalities. While there is much evidence supporting a strong genetic component of susceptibility to addiction, it is also thought that the addicted phenotype is a result of exposure to “risk factors,” including early life experiences and other environmental stimuli, that “prime” an organism to be more vulnerable to addiction. Because of the strong influence of external risk factors on the development of addiction, it has been proposed that epigenetic mechanisms regulate the long-term changes associated with this phenotypic priming and the subsequent addicted phenotype.
In its broadest definition, epigenetics is described as changes in gene expression that do not arise from changes to the DNA sequence; this generally involves alterations in histone modifications, DNA methylation, and noncoding RNAs (microRNAs and long noncoding RNAs). Each of these mechanisms can be altered in response to internal and external signals and provide a mechanism by which environmental stimuli can interact with an individual’s genome to influence cellular response and function, including neuroplasticity. The differing temporal effects of each mechanism are, in part, a result of their varying levels of stability – e.g., most histone modifications are exceptionally dynamic, whereas DNA methylation is less so.
With regards to addiction, epigenetic mechanisms alter gene expression in the following ways: 1) by changing the steady state expression of specific genes; 2) by priming genes for induction (sensitizing) or repression (desensitizing) in response to a stimulus (e.g., drug); or 3) regulating the expression of splice variants of specific genes that are sensitive to drugs of abuse.
To date, a majority of the work on the epigenetic mechanisms involved in addiction have focused on histone modifications in response to stimulants (e.g., cocaine) and, to a lesser extent, opiates (e.g., morphine) in the nucleus accumbens (NAcc), a key brain region involved in reward. Recently, work has expanded to other brain regions in the reward circuitry (see figure below) including the ventral tegmental area (VTA), prefrontal cortex (PFC), basolateral amygdala (BLA), and hippocampus (HPC) as seen in the figure below:
_
Figure above shows exposure to drugs of abuse results in epigenetic alterations throughout the brain reward circuitry. The major brain regions involved in mesolimbic reward pathway are depicted in the rodent brain: dopaminergic neurons (green) in the ventral tegmental area (VTA) project to the nucleus accumbens (NAcc), prefrontal cortex (PFC), amygdala (AMY) and hippocampus (HPC). The NAcc also receives glutamatergic (red) innervation from the PFC, AMY and HPC. While the mechanisms of action are specific for each drug, most drugs of abuse increase dopaminergic signaling from VTA to other regions of the reward circuitry.
Many studies investigating epigenetic mechanisms of addiction have focused on the NAcc as it is a major region of integration for rewarding stimuli. Altered epigenetic regulation of gene expression within the brain’s reward system plays a significant and complex role in the development of drug addiction. Addictive drugs are associated with three types of epigenetic modifications within neurons. These are (1) histone modifications, (2) epigenetic methylation of DNA at CpG sites at (or adjacent to) particular genes, and (3) epigenetic downregulation or upregulation of microRNAs which have particular target genes. As an example, while hundreds of genes in the cells of the nucleus accumbens (NAcc) exhibit histone modifications following drug exposure – particularly, altered acetylation and methylation states of histone residues – most other genes in the NAcc cells do not show such changes.
_
Transgenerational epigenetic inheritance:
Epigenetic genes and their products (e.g., proteins) are the key components through which environmental influences can affect the genes of an individual; they also serve as the mechanism responsible for transgenerational epigenetic inheritance, a phenomenon in which environmental influences on the genes of a parent can affect the associated traits and behavioral phenotypes of their offspring (e.g., behavioral responses to environmental stimuli). In addiction, epigenetic mechanisms play a central role in the pathophysiology of the disease; it has been noted that some of the alterations to the epigenome which arise through chronic exposure to addictive stimuli during an addiction can be transmitted across generations, in turn affecting the behavior of one’s children (e.g., the child’s behavioral responses to addictive drugs and natural rewards). The general classes of epigenetic alterations that have been implicated in transgenerational epigenetic inheritance include DNA methylation, histone modifications, and downregulation or upregulation of microRNAs.
_
Genome-wide association study of lifetime cannabis use based on a large meta-analytic sample of 32330 subjects from the International Cannabis Consortium, a 2016 study:
Cannabis is the most widely produced and consumed illicit psychoactive substance worldwide. Occasional cannabis use can progress to frequent use, abuse and dependence with all known adverse physical, psychological and social consequences. Individual differences in cannabis initiation are heritable (40–48%). The International Cannabis Consortium was established with the aim to identify genetic risk variants of cannabis use. Authors conducted a meta-analysis of genome-wide association data of 13 cohorts (N=32330) and four replication samples (N=5627). In addition, they performed a gene-based test of association, estimated single-nucleotide polymorphism (SNP)-based heritability and explored the genetic correlation between lifetime cannabis use and cigarette use using LD score regression. No individual SNPs reached genome-wide significance. Nonetheless, gene-based tests identified four genes significantly associated with lifetime cannabis use: NCAM1, CADM2, SCOC and KCNT2. Previous studies reported associations of NCAM1 with cigarette smoking and other substance use, and those of CADM2 with body mass index, processing speed and autism disorders, which are phenotypes previously reported to be associated with cannabis use. Furthermore, authors showed that, combined across the genome, all common SNPs explained 13–20% (P<0.001) of the liability of lifetime cannabis use. Finally, there was a strong genetic correlation (rg=0.83; P=1.85 × 10−8) between lifetime cannabis use and lifetime cigarette smoking implying that the SNP effect sizes of the two traits are highly correlated. This is the largest meta-analysis of cannabis GWA studies to date, revealing important new insights into the genetic pathways of lifetime cannabis use. Future functional studies should explore the impact of the identified genes on the biological mechanisms of cannabis use.
Conclusion:
Authors have performed the largest meta-analysis to date of GWASs investigating cannabis use phenotypes. With a sample of over 32000 individuals, the results implicate four genes as involved in lifetime cannabis use: NCAM1, CADM2, SCOC and KCNT2. The results illustrated that lifetime cannabis use is under the influence of many common genetic variants. The combined SNPs explained 13–20% of the phenotypic variation, and revealed a high degree of genetic sharing (r=0.83) with lifetime cigarette smoking. Future studies should investigate the impact of these genes on the biological mechanisms leading to lifetime cannabis use.
_______
_______
Drugs and Social Media:
Bloomberg says that the intersection between social media and drug use is “a double whammy,” where consumption of illegal substances is normalized and glamorized in high-definition pictures and videos. Drug use isn’t something that is limited to celebrities and strangers; now, friends (and even family members) can share a picture of a row of shot glasses, a joint of marijuana, or even harder and more dangerous drugs with hundreds of contacts, all at the click of a button. The instantaneousness of the connection also allows users and their dealers to stay in touch through instant messaging programs that are often part of social media platforms. To that end, a 2011 survey conducted by the National Center on Addiction and Substance Abuse at Columbia University found that teenagers who regularly use popular social media outlets (such as Facebook) were more likely to drink, use drugs, and buy tobacco than adolescents who either did not use social media or used it less. The founder and chairman of the National Center on Addiction and Substance Abuse cautions against making a simplistic connection between social media and drug use. Social media doesn’t cause drug use, Joseph Califano said, but there is the fear that services like Facebook, reddit, or 4chan will create “a new form of peer pressure” that will compel vulnerable teenagers into engaging in drug use. A spokesman for Facebook says the company removes any content that promotes illegal drug use or underage drinking based on whether users flag the content as objectionable.
Facebook is, by far, the most popular social network that exists, and finding drugs on the platform is “easier than buying a cup of coffee,” according to the McAfee Institute. In Colorado, where the sale of recreational marijuana is limited to adults, a hidden Facebook group acted as a marketplace for high schoolers to buy and sell cannabis as well as synthetic marijuana, prescription drugs, methamphetamines, MDMA, and LSD. The group had 900 members in total, and 171 of them were students from 55 high schools and middle schools across a single metro area. Police were more interested in using the experience as a learning opportunity for parents, children, and educators about how an otherwise benign (and even beneficial) service like Facebook could be usurped by people looking to expose high schoolers to the drug trade. Nonetheless, police arrested one man on charges of distributing controlled substances, and Facebook closed down the group when investigators contacted the company.
A similar situation took place in Adelaide, Australia, where a local news organization discovered the existence of another “hidden” Facebook group, where the privacy settings are such that only the group’s members are aware of its existence, and joining the group happens by invitation only. The so-called “Adelaide street pharmacists” group had over 200 members, which Facebook shut down when alerted by the news organization. A criminologist at the University of Adelaide Law School explained that the group and others like it are examples of “social drug dealing,” where social media platforms (like Facebook) are becoming increasingly used by criminals of all colors, allowing drug dealers to hide in plain sight. The Internet is probably the primary mechanism for drug dealers because using social media and smartphones to conduct business is far quicker and more efficient than methods of the past. The same privacy settings that are meant to protect users’ confidential information are also used by drug dealers to cover their tracks and render themselves invisible among the millions of legitimate Facebook groups and pages. Criminals always exploit any form of technology and innovation they can, and social media is no exception. And the ubiquity of platforms like Facebook blur the line between the online world and real life, to the point where placing an “order” through a hidden Facebook group can result in drugs being delivered to a user’s front door. Pharmacies is a code word that is often used by drug smugglers to create seemingly legitimate groups to sell their products. Facebook may be the name that comes to mind when the term social media is used, but there are literally hundreds of platforms that allow users of all walks of life to connect, and drug dealers are attuned to all of them. The next wave of freelance narcotics is online and with millions of people having a smartphone in their hand, the marketplace is everywhere. All it takes is for a smartphone app to be social and location-based for a dealer to find a customer. Social media apps are increasingly likely to be used by young people to buy illegal drugs, research suggests. The study, from Royal Holloway, University of London, says drug users valued the convenience and speed of buying drugs via apps like Snapchat.
Drugs and internet:
The WWW enables relatively anonymous business transactions across the world 24 hours a day. So the fluidity of cyberspace is ideally suited for illicit drug transactions (Forman, 2006). Schifano et al. (2006) explored data from web pages regarding information of consumption, production and sale of psychoactive substances. The authors reported that 42% of the websites showed a clear anti-drug position, 30.1% did not clearly state their view, 17.9% showed a pro-drug approach and 10% a harm reduction approach. 9.1% of the websites offered detailed information about the technical procedures to synthesize and extract a range of variant recreational psychoactive compounds. Also “no prescription web sites” have begun to emerge, which allows people to acquire drugs without a prescription. Little is known on how to control the “no prescription web sites”, therefore strategies will be needed to examine these new trading strategies (Forman, 2006).
New technologies in general and the Internet in particular have become essential features that characterize the phenomenon known as the new psychoactive substances.
There are four basic reasons for which the Internet plays a key role in the new psychoactive substances:
- It facilitates the knowledge of their existence.
- It provides information about their performance.
- It is an instrument of trade.
- It is a place in which to share experiences with them.
The websites devoted to emerging drugs have features that make them particularly attractive, but these sites that advertise emerging drugs are commonly and perversely worded with the aim of avoiding any liability, clearly stating that the information supplied is about “indigenous uses and customs”, that the relevant substance “is not fit for human consumption” or it is only for external use.
_
Cyberbullying and Drug Abuse:
Although it is challenging to find exact statistics on drug abuse related to cyberbullying since it is a relatively new problem, we do know that substance use is strongly associated with trauma and co-occurring mental illnesses like depression and anxiety. And research does suggest that adolescents who have been bullied are twice as likely to use alcohol, marijuana, and cigarettes as teens who have not been bullied. Interestingly, those who are on the receiving end of bullying are not the only ones negatively affected by the act. Teens who bully their peers are also more likely to use alcohol, marijuana, and cigarettes compared to students who do not bully others.
_____
_____
Sex differences in drug addiction:
Women and men differ in various ways when it comes to addictions. Research has shown that women are more likely to be poly-substance dependent. It has been noted that a larger percentage of women abuse licit (legal) drugs such as tranquilizers, sedatives, and stimulants. On the other hand, men are more likely to abuse illicit (illegal) drugs such as cocaine, meth, and other street drugs. Research suggests that women addicts more frequently have a family history of drug abuse. When asked to describe their onset of addictions, women more frequently describe their addiction as sudden where as men describe them as gradual. Females have a higher percentage of fatty tissues and a lower percentage of body water than men. Therefore, women have slower absorption rates of drug substances and higher concentration in bloodstream. Women addicts are known to be at greater risk for fatty liver disease, hypertension, anemia, and other disorders.
_
Current scientific consensus is that fundamental differences exist in brain structure and function between men and women possibly in response to sexually selective evolutionary pressures (Cahill, 2014a). Brain differences between sexes have been shown in terms of neurodevelopmental trajectories (Lenroot et al., 2007), structural morphometry (Clayton and Collins, 2014; Luders et al., 2009; Peelle et al., 2012; Watanabe et al., 2013), connectivity (Cahill, 2014b; Duarte-Carvajalino et al., 2012; Gong et al., 2015; Ingalhalikar et al., 2014), and molecular biology (Al Nadaf et al., 2010; Cahill, 2006; Jazin and Cahill, 2010; Wu et al., 2014).
_
Patients with substance use disorder (SUD) demonstrate sex differences in many natural history features, including age of first use, rate of drug consumption escalation, quantity consumed, affect, and behavior (Becker et al., 2012; Eaton et al., 2012; Hernandez-Avila et al., 2004). Additionally, sex differences in substance use disorders exist across etiological factors, prevalence rates, pharmacokinetics, pharmacodynamics, self-administration behavior, hormonal influences, associated health risks, treatment outcomes, and medication response (Anker and Carroll, 2011; Becker and Koob, 2016; Cooper et al., 2016; Hasin and Grant, 2015; Oberleitner et al., 2015; Smith et al., 2016). These fundamental sex differences in neurobiology and clinical course suggest interactions between neurophysiology, sex, and disease process. Although results of single-sex studies may, at times, generalize to both sexes (Sechzer et al., 1994), it is important to include and appropriately analyze both sexes to fully characterize this disease process. Inclusion and appropriate statistical methods can prevent reporting of an overall effect that may be true for only one sex, or reporting no effect when there may be opposing effects between sexes (Wetherington, 2007).
_
Because many studies that included women and used an analytically appropriate approach discovered significant sex by SUD interactions on brain structure (81.3% that stratified and 31.3% that used an interaction term), it suggests that sex significantly modulates SUD pathophysiology. Such modulation may be mediated by sex hormones or menstrual cycle, endophenotypes that predate disease, neurobehavioral mechanisms associated with socialized gender roles, co-morbidities, or stress responses known to differ in women compared to men (Becker et al., 2012; Brady and Randall, 1999; Chaplin et al., 2008; Hagemann et al., 2011). SUD is a chronic relapsing-remitting disease that is difficult to treat; if sex-specific patterns of altered brain structure and function can be identified, it could lead to different treatments in women and overall improvement in clinical management. As one example of this approach, Cosgrove and colleagues (Cosgrove et al., 2012) have documented key sex differences in the function of nicotinic receptors in abstinent smokers, providing a neurochemical explanation for why nicotine replacement treatments fail to work as well in women compared to men smokers (Smith et al., 2016).
_____
_____
Effects of common illicit drugs:
A drug can have psychological, emotional and physical effects and can change the behaviour of the person taking the drug. These behavioural changes are not the same for everyone. The effect of any drug will depend on the drug: what effect it has on the central nervous system; the amount taken; how it is taken; how often; for how long; if it is taken with other drugs the person: age, weight, sex, tolerance, past experiences, mood, personality, the expectations and what the person wants to happen from using the drug the environment: what the community or society expects, allows and excuses as a result of using the drug; the place; the presence of other people; noise levels, and so forth.
_
Short-Term Health Effects of Drug Abuse:
The National Institute on Drug Abuse (NIDA) describes several short-term health effects of using addicting substances:
- Marijuana: drowsiness and relaxation, impairment of attention, coordination, judgment and short-term memory, increased heart rate and appetite.
- Prescription medications: cardiovascular failure, coma, decreased respiration, drowsiness and relaxation, irregular heartbeat, nausea, seizures, severely increased body temperature.
- Cocaine: decreased appetite and sleep, dilated pupils, increased blood pressure, body temperature and heart rate, nausea.
- Hallucinogens: decreased appetite, depression, distortions in perception, dizziness, increased blood pressure, body temperature and heart rate, nausea, paranoia, tremors.
- Inhalants: coma, confusion, dizziness and lightheadedness, hallucinations, headaches, heart failure, loss of coordination, nausea, seizures, suffocation.
- Heroin: alternating states of wakefulness and drowsiness, clouded thinking, decreased respiration, dry mouth, nausea.
Long-Term Health Effects of Drug Abuse:
Additionally, the NIDA lists the following potential conditions that can develop as the result of long-term substance abuse:
- Marijuana: anxiety, bronchitis, chronic cough, depression and schizophrenia.
- Prescription medications: anxiety, paranoia,
- Cocaine: anxiety, digestive problems, insomnia, irritability, panic attacks, paranoia.
- Hallucinogens: flashbacks, Hallucinogen Persisting Perception Disorder.
- Inhalants: muscle spasms and other permanent motor impairment, liver and kidney damage.
- Heroin: collapsed veins, abscesses, infection of heart lining and valves, arthritis, diseases transmitted through the blood such as HIV and Hepatitis C.
_
Side Effects of Illegal Drugs Abuse:
Illicit drug abuse carries with it several side effects that affect the user both in the short term and long term. While the effects of illegal drugs are as broad as the types of substances that constitute the category, there are some general side effects that cut across all illegal drugs. For a person with illegal drug addiction, understanding the possible side effects of using these substances can act as a deterrent to continuing taking them. For a person who may have once taken an illicit drug, these side effects can work as a warning sign to not go down that road again. Illegal drugs effects can be devastating to a person with illicit drug addiction. Hence the need for anyone exposed to illicit substances to take them seriously.
Short-term Side Effects of Illegal Drugs:
Decreased breathing: Most illicit substances act on the Central Nervous System, the center involved in the regulation of vital functions such as breathing. When a person takes an illicit drug, their breathing might become depressed and this could lead to hypoxia (oxygen deprivation) and further to more serious complications.
Impaired judgment: When a person is high on illicit drugs, they may not be able to make sound decisions. This can lead to risky behavior such as having sex with multiple partners with no protection, driving under the influence, or getting into criminal acts. When a person takes illegal drugs, they expose themselves to such situations to deadly effect.
Poor coordination: Another short-term side effect that cuts across most illicit substances, poor hand-eye coordination can be dangerous. If a person on illicit drugs is operating machinery, for instance, this lack of coordination might lead to an accident. Poor coordination can also lead to injurious falls and other similar accidents.
Inattention: While some illegal drugs increase attention, once a person gets addicted, the effect is almost always the contrary. As the person is now constantly seeking the next high, their ability to focus on anything dwindles. They may also get restless, which will also affect their ability to pay attention.
Increased heart rate: If the illicit drug taken is a stimulant, this will raise the heart rate. An example is cocaine, which quickly raises the heart rate when taken. While this might not be fatal under normal circumstances, if a person has a heart defect, this could trigger a heart attack.
Coma: If a person overdoses, the result could be a coma. Comas often happen to drug addicts and can last for anything from a few hours to weeks. This happens because most addicts at some point are unable to control their drug intake, leading to consumption of dangerously high doses that ultimately lead to a coma.
Long-term Side Effects of Illegal Drugs:
Addiction: Continued use of an illicit drug leads to tolerance, then dependence, then addiction. An addict is a described as a person who functions at the mercy of illicit drugs. Such a person has no life and spends their every waking moment either getting high or looking for the next high. This long-term effect can destroy a person’s life and livelihood.
Brain damage: Substances with psychoactive properties cross the blood-brain barrier and impact the brain. When this happens consistently, neurotoxicity occurs which ultimately leads to cell necrosis. Brain damage arising in this manner is permanent and can lead to more complications such as memory loss, permanent loss of coordination, among others.
Figure above shows brain positron emission tomography images that compare brain metabolism in a healthy individual and a cocaine addict.
Malnutrition: As a person entrapped in a drug addiction focuses on drug seeking actions, neglect of basic needs tends to occur. Such a person will not have nutritious meals, and this will lead to malnutrition. Over time, this will lead to a depressed immune system and expose the person to opportunistic diseases such as TB and HIV.
Suicidal thoughts: When a person finds themselves addicted to illicit substances, they could lose hope. At this point, suicidal thoughts and ideation might creep in as they try to escape the maze they are in. These thoughts become more pronounced over time as the addiction gets worse. Getting timely help for the addiction can help prevent these thoughts from escalating.
Chronic insomnia: As most psychoactive illicit drugs affect the CNS, which also regulates sleep, prolonged use can rewire these pathways and render the sleep hormone melatonin useless. Chronic insomnia that results can prove to be resistant to mild sleep medication and lead the person to take stronger sleeping pills, which in themselves also represent a danger to the person.
Death: Over time, illicit drug use can lead to death. This could happen as a drug overdose, or because of the combination of all these side effects that culminate in a fatal outcome. Quitting illegal drugs early is, therefore, a life and death situation that any person taking them should consider.
_____
Oxidative Stress and Drugs of Abuse:
Several evidences support a role for oxidative stress in the toxicity induced by many drugs of abuse in different organs, such as the brain, heart, liver or kidneys. This leads to oxidation of important cellular macromolecules, and may culminate in cell dysfunction and death. There is evidence for oxidative damage and depletion of antioxidants upon exposure to drugs of abuse, especially amphetamines, cocaine and opiates. The sources of oxidative stress induced by drugs of abuse include oxidative metabolism of drugs, oxidative metabolism of monoamines by monoamine oxidases or by auto-oxidation, mitochondrial dysfunction, excitotoxicity, microglial activation, inflammation, hyperthermia and the effects of drug interactions. The oxidative stress serves as a relevant mechanism contributing for the cytotoxicity of drugs of abuse and for behavioral changes associated with drug addiction. Increase in the levels of oxidants compared to antioxidant defence systems leads to oxidation of proteins, phospholipids or DNA, leading to cell dysfunction and, eventually, to cell death.
______
______
Diagnosis of drug addiction:
_
Drug addiction is often used as a synonym for what the DSM-5 describes as severe substance use disorder, a culmination of symptoms that fall into four categories:
- Impaired control
- Social impairment
- Risky use
- Pharmacological criteria
Medical professionals use these criteria to diagnose and treat substance use disorders based on a person’s behavior over a 12-month period. Substance use disorders are then broken down into specific drug types such as opioid use disorders, alcohol use disorders and more.
_
To determine a substance use disorder diagnosis, professionals analyze a collection of behavioral factors over a 12-month period:
- A substance is frequently used for longer periods of time or higher dosages than originally intended.
- Efforts to control or lesson substance use are unsuccessful.
- A significant amount of time is spent on obtaining, using and dealing with the effects of substances.
- A heightened urge or desire to regularly use substances is present.
- Regular drug use prevents completion of obligations at home, school, or work.
- Recurrent substance use despite continued social or relationship issues related to drug use and its effects.
- A reduction or abandonment of valuable or important social activities in favor of drug use.
- Substance use taking place during dangerous situations or times (driving, caring for children, etc.).
- Continued substance use despite underlying medical or physical issues that are exacerbated by the drug.
- Development of a tolerance, which can involve:
- An increased dosage amount to achieve the desired effects.
- Decreased effects or response to the same amount of a particular substance.
A person does not have to meet all of these points to have an addiction. For example, some drugs do not create physical tolerance or withdrawal symptoms. Also, addiction does not always result in a loss of employment, etc. Everyone’s addiction will look slightly different.
As a diagnostic biomarker, ΔFosB expression could be used to diagnose an addiction in humans, but this would require a brain biopsy and therefore is not used in clinical practice.
___
Addiction is an all-consuming disease, using much of an individual’s time, energy and resources. There are many physical, mental and emotional signs of addiction. If you are experiencing a combination of these signs, treatment may be a stepping stone for long-term recovery. Looking for signs and symptoms of drug abuse can be the first step toward identifying an addiction:
- Unintentional weight loss
- Loss of sleep
- Skin problems (lesions, scratch marks, rashes, pimples, bruises, or needle marks at an intravenous injection site)
- Cool, unnaturally pale skin
- Bloodshot eyes
- Unusual odors (may be chemical smells or strong body odors)
- Tremors or loss of motor coordination
- Slurred speech
- Frequent nausea
- Irregular heart rate
- Shallow breathing
Many of the neurological processes and brain structures involved in addiction are also used in cognitive tasks like reasoning, learning and memory. With heavy drug use, you may find that you have difficulty learning or remembering information or that you lose focus when you’re trying to concentrate on a task. In addition to short-term physical and psychological impacts, long-term drug use can also alter your mental health.
Mental impacts of Drug Use:
Drugs affect the way a person thinks, feels, behaves and how they look. But substance use disorders are often accompanied by co-occurring mental health disorders like anxiety or depression. Some people may use drugs as a form of self-medication for these issues, while other people may develop a mental health disorder after taking substances. Either way, it’s important to look out for psychological and behavioral changes in someone who might be struggling with addiction:
- Anxiety
- Restlessness
- Uncharacteristic lying
- Confusion
- Memory loss or blackouts
- Stealing money or medications
- Irregular sleep patterns
- Self-isolation
- Depression
- Mood swings
- Unusual personality changes or mood swings
- Failure at school or on the job
- Increased secrecy
- Legal problems
When a person is struggling with both a mental illness and substance use disorder, it can be difficult to identify the issues and treat them both. Many treatment facilities focus solely on the symptoms of substance use, without treating the mental health issues that may contribute to addiction. Finding a center that specializes in co-occurring disorder treatment can help identify the roots of a substance use disorder and equip patients with the tools they need for lifelong recovery.
_
Warning signs of commonly abused drugs:
Marijuana: Glassy, red eyes; loud talking, inappropriate laughter followed by sleepiness; loss of interest, motivation; weight gain or loss.
Stimulants (including amphetamines, cocaine, crystal meth): Dilated pupils; hyperactivity; euphoria; irritability; anxiety; excessive talking followed by depression or excessive sleeping at odd times; may go long periods of time without eating or sleeping; weight loss; dry mouth and nose.
Inhalants (glues, aerosols, vapors): Watery eyes; impaired vision, memory and thought; secretions from the nose or rashes around the nose and mouth; headaches and nausea; appearance of intoxication; drowsiness; poor muscle control; changes in appetite; anxiety; irritability; lots of cans/aerosols in the trash.
Hallucinogens (LSD, PCP): Dilated pupils; bizarre and irrational behavior including paranoia, aggression, hallucinations; mood swings; detachment from people; absorption with self or other objects, slurred speech; confusion.
Heroin: Contracted pupils; no response of pupils to light; needle marks; sleeping at unusual times; sweating; vomiting; coughing, sniffling; twitching; loss of appetite.
_
Warning signs of commonly abused prescription drugs:
Opioid painkillers (including oxycodone, hydrocodone): Drooping eyes, constricted pupils even in dim light, sudden itching or flushing, slurred speech; drowsiness, lack of energy; inability to concentrate, lack of motivation, decline in performance at work or school; neglecting friendships and social activities.
Anti-anxiety medications, sedatives, and hypnotics (including alprazolam, diazepam, zolpidem): Contracted pupils; drunk-like, slurred speech, difficulty concentrating, clumsiness; poor judgment, drowsiness, slowed breathing.
Stimulants (including Amphetamine/dextroamphetamine, Methylphenidate): Dilated pupils, reduced appetite; agitation, anxiety, irregular heartbeat, high body temperature; insomnia, paranoia.
_
Serious medical Side Effects of Drug Use:
Different drugs affect the body and brain in unique ways. However, there are many similarities in the way drug addiction can damage the body and cause life-threatening symptoms. Some of the most severe side effects may include:
- Insomnia
- Loss of appetite and weight loss
- An abnormally slow or rapid heart rate
- Slow or rapid breathing
- Increased blood pressure
- Heart attack
- Stroke
- Respiratory distress
- Fever
- Muscle spasms
- Seizures
- Increased risk of accidental injuries
- Exposure to blood-borne diseases (for IV drug users)
_
Table below shows toxidromes caused by drug overdose:
_
Physical dependence on a drug can cause serious withdrawal symptoms if a person suddenly stops using the substance or severely reduces the dose. The withdrawal process itself can be uncomfortable and dangerous. Some of the classic signs of withdrawal include tremors, cold sweats, involuntary movements (e.g., jerking, twitching, or shaking), nausea and vomiting, muscle cramps and bone pain. Because withdrawal can be dangerous, proper medical detox can be a life-saving step in recovery.
_______
Differences between Drug Side Effects and Addiction Symptoms:
Many drugs, whether legal or illegal, have side effects. These are unpleasant, unintended and sometimes dangerous effects that occur in addition to the desired effects of the drug. When a person uses drugs, she may experience several different types of side effects, even if she uses the recommended dosage. Because some drugs’ side effects can be similar to symptoms of addiction, it’s important to recognize the differences between the two.
Common drug Side Effects:
Side effects of drugs vary widely from mild to severe, and can occasionally be life-threatening. As the National Institute on Drug Abuse lists, some of the most common side effects for different types of drugs include:
The risks and side effects of drug use should be weighed against any potential benefits to ensure users are not experiencing unnecessary complications. Most of the time, side effects from drugs are unwanted. They are sometimes unrelated to the main effect of the drug, and can lessen the overall worth of using it. For people who struggle with drug abuse, though, negative side effects may not be enough to make them stop abusing the drug.
Additionally, some of the side effects of drug abuse are similar to symptoms of addiction.
Some drug addictions have the following drug-specific symptoms:
- Marijuana: memory loss, concentration problems, increased appetite, paranoia
- Benzodiazepines: drowsiness, depression, decreased breathing and blood pressure
- Stimulants: decreased appetite, irritability, insomnia, weight loss, increased heart rate, blood pressure and temperature
- Opioids: depression, decreased breathing, confusion
Since several of these symptoms are similar or identical to these drugs’ side effects, it can be difficult to distinguish between them. It can therefore be helpful to know the specific symptoms of addiction.
Following symptoms are common to all types of addiction, regardless of the substance:
- Need to use the drug regularly
- Inability to stop using the drug
- Maintaining a supply of the drug
- Spending a lot of money on the drug, even when doing so is financially unwise
- Doing whatever it takes to acquire the drug
- Using the drug as a coping mechanism for personal problems
- Engaging in dangerous behavior while using the drug
- Allowing the drug abuse to consume large amounts of time and energy
Another common sign of addiction is isolation. An addict may try to hide the negative behavior from friends and family by isolating himself and making up excuses for his absences. Additionally, addicts may experience severe mood swings and have withdrawal symptoms that make them depressed, anxious and irritable when they stop using the substance. Likewise, beginning the substance use again can cause a sudden shift into a happy and positive mood.
Distinguishing between drug Side Effects and Addiction Symptoms:
It’s not always easy to tell when a person is struggling with an addiction since the side effects of many drugs are similar to the symptoms of addiction. A person experiencing the negative effects of a drug may mistake his symptoms for an addiction, or a person who thinks his drug abuse is under control may assume that the side effects he experiences are normal for the drug, and thus may ignore key signs of addiction. Because of these similarities it’s important to keep your healthcare provider informed of your use habits and any effects – expected or unexpected – so he or she may be able to objectively identify warning signs of addiction and dosage needs.
______
Uncommon Adverse Effects of Commonly Abused Illicit Drugs:
The negative effects of drug use are numerous, and many are well documented in the medical literature. Illicit drug use should be considered in the differential diagnosis of many clinical presentations, especially in patients with positive drug screens or a history of substance abuse, because the list of known deleterious effects is growing. There are an increasing number of case reports involving uncommon adverse effects of commonly abused illicit drugs (Table below).
_
Uncommon Adverse Effects of Illicit Drug Use:
| Drug | Uncommon effect | Treatment |
| Cocaine | Leukopenia
Positive autoimmune markers Vasculitis Reticular, purpuric lesions |
Cocaine cessation
Treatment of any superimposed infection |
| Heroin | Acute kidney injury
Rhabdomyolysis Dark urine Fatigue Myalgia Stiffness Transverse myelitis Bowel/bladder dysfunction Loss of deep tendon reflexes Low back pain Muscle spasms Paraplegia Paresthesias Sensory loss |
Heroin cessation
Aggressive rehydration for rhabdomyolysis and acute kidney injury Corticosteroid therapy for transverse myelitis |
| Marijuana | Cannabinoid hyperemesis syndrome
Abdominal pain Hyperemesis Intermittent severe nausea |
Marijuana cessation
Temporary relief through compulsive bathing in hot water |
Common acute manifestations of marijuana abuse include euphoria, conjunctival injection, and xerostomia. Cannabinoid hyperemesis syndrome is a lesser-known outcome of chronic marijuana use. Recently, clinical criteria have been proposed to aid in the diagnosis of cannabinoid hyperemesis syndrome. The condition occurs in susceptible individuals and leads to intermittent severe nausea, hyperemesis, and abdominal pain. A unique finding of this syndrome is temporary relief through compulsive bathing in hot water. Definitive treatment of cannabinoid hyperemesis syndrome requires cessation of marijuana use.
Well-known adverse effects of cocaine use include cardiovascular manifestations (e.g., myocardial infarction, arrhythmias), psychiatric conditions (e.g., psychosis, paranoia), and neurologic findings (e.g., headache, stroke, seizures). Recently, however, many cocaine users have presented to health care facilities with an unusual clinical triad of leukopenia, positive autoimmune markers, and dermatologic manifestations. This unusual presentation has been linked to the adulteration of cocaine with levamisole, an anthelmintic agent currently used in veterinary medicine. Although it is uncertain why levamisole is added to cocaine, it is undetectable by most street tests for the purity of cocaine, making it useful when a person is trying to “cut” or dilute the drug. Levamisole has also been theorized to increase the euphoria associated with cocaine use. This problem will likely become more recognized, because the Centers for Disease Control and Prevention reported that 69 percent of all cocaine seized in 2009 contained this adulterant. Patients who use cocaine containing levamisole often have impressive reticular, purpuric lesions on the ears and extremities due to underlying vasculitis. Assuming there are no superimposed infections, the effects often resolve with the cessation of use of the adulterated cocaine and supportive care.
Acute heroin intoxication is known to cause euphoria, miosis, xerostomia, bradycardia, hypotension, and respiratory depression. Less common effects include transverse myelitis and rhabdomyolysis with subsequent acute kidney injury. The underlying mechanism of these effects is not known, and the patient’s description of symptoms may be vague, leading to a delay in clinical recognition. Denial of drug use may further hinder recognition. Prompt treatment of transverse myelitis and rhabdomyolysis is imperative to minimize any long-term sequelae. Transverse myelitis should be treated with corticosteroids. Rhabdomyolysis is treated with aggressive rehydration to prevent kidney injury.
Because of the social implications related to illicit drugs, patients may conceal their use of these substances, further complicating a difficult diagnosis. Promptly beginning the cessation discussion is an important aspect in the overall treatment of adverse effects from illicit drug use. Family physicians are often the first to recognize serious drug abuse. They can be especially helpful to these patients by remaining actively involved in their care as the patients receive comprehensive, multidisciplinary treatment for substance abuse and addiction.
_______
When to see a doctor:
If your drug use is out of control or causing problems, get help. The sooner you seek help, the greater your chances for a long-term recovery. Talk with your primary doctor or see a mental health professional, such as a doctor who specializes in addiction medicine or addiction psychiatry, or a licensed alcohol and drug counselor.
Make an appointment to see a doctor if:
- You can’t stop using a drug
- You continue using the drug despite the harm it causes
- Your drug use has led to unsafe behavior, such as sharing needles or unprotected sex
- You think you may be having withdrawal symptoms after stopping drug use
Staging an intervention:
People struggling with addiction usually deny that their drug use is problematic and are reluctant to seek treatment. An intervention presents addict with a structured opportunity to make changes before things get even worse and can motivate someone to seek or accept help. An intervention should be carefully planned and may be done by family and friends in consultation with a doctor or professional such as a licensed alcohol and drug counselor, or directed by an intervention professional. It involves family and friends and sometimes co-workers, clergy or others who care about the person struggling with addiction. During the intervention, these people gather together to have a direct, heart-to-heart conversation with the person about the consequences of addiction and ask him or her to accept treatment.
When to seek emergency help:
Seek emergency help if you or someone you know has taken a drug and:
- May have overdosed
- Shows changes in consciousness
- Has trouble breathing
- Has seizures or convulsions
- Has signs of a possible heart attack, such as chest pain or pressure
- Has any other troublesome physical or psychological reaction to use of the drug
_____
Assessing for Co-Occurring Disorders:
Alcohol and drug use may contribute to or arise in association with a physical or mental health disorder. According to the National Alliance on Mental Illness, approximately 20.2 million adults in the U.S. have some sort of substance use disorder. Of those 20.2 million, more than 50% of them have a co-occurring mental illness. Untreated medical or mental health problems can complicate the recovery trajectory—sometimes prompting a person to relapse into addictive behaviors. So diagnosing and treating a co-occurring disorder is as important as treating the drug or alcohol addiction. Diagnosis of disorders that occur alongside an addiction is typically done in the same manner as diagnosing the addiction. In addition to obtaining feedback from the person seeking treatment, the clinician may perform tests, obtain the patient’s medical history, observe the person’s symptoms, consult the DSM-5, and use clinical judgment to determine whether the person has a co-occurring disorder. Of all the tools at the clinician’s disposal, observation of symptoms will be the most useful in diagnosing a co-occurring disorder. Here are a few disorders that may be diagnosed during or after an addiction assessment, and the symptoms associated with them:
- Depression: Symptoms include fatigue, loss of energy, excessive sleeping or insomnia, inability to concentrate, depressed mood, loss of appetite or excessive appetite, and suicidal ideation.
- Anxiety: Symptoms include difficulty controlling worry, restlessness, difficulty concentrating, muscle tension, irritability, and sleep disturbances.
- Post-traumatic stress: Symptoms include mentally re-experiencing the trauma, hyper-arousal, dissociation, cognitive and behavioral avoidance, and emotional numbing.
- Psychosis: Symptoms include visual and auditory hallucinations, delusions, disorganized speech, and catatonic behavior.
- Liver disease: Signs of liver disease include jaundice, itching, easy bruising, edema, mental confusion, fatigue, vague abdominal pain, loss of appetite, and weakness.
- Kidney disease: Symptoms include lethargy, shortness of breath, weakness, edema, metabolic acidosis, high potassium levels, uremia, and anemia.
- Malnutrition: Symptoms include fatigue, dizziness, weight loss, irritability, bone or joint pain, bloated abdomen, edema, brittle nails, dry skin, hair loss, changes in skin and hair color, slow wound healing, loss of appetite, and sunken temples.
_____
_____
Drug Testing:
A drug test is primarily performed to confirm the presence of one or more illegal or prescription drugs in a person’s urine, blood, saliva, hair, or sweat. The test is performed by using the samples such as urine, hair, blood, saliva, and others. Among these urine sample is the most widely preferred owing to the advantages it offers, such as lower test cost, availability of more sample, and availability of point-of-care tests. Drug testing offers a critical adjunct to clinical care and substance use. The most often tested drugs include marijuana, opioids, cocaine, morphine, and others. Urine testing is the most common type of drug screening. Drug tests are increasingly being adopted by sports organizations, employers, forensic purposes, and several other applications.
The drugs most often tested for include:
- Marijuana
- Opioids, such as heroin, codeine, oxycodone, morphine, hydrocodone, and fentanyl
- Amphetamines, including methamphetamine
- Cocaine
- Steroids
- Barbiturates, such as phenobarbital and secobarbital
- Phencyclidine (PCP)
Drug testing is also known as drug screen, drugs of abuse testing, substance abuse testing, toxicology screen, tox screen, sports doping tests etc. Drug screening is used to find out whether or not a person has taken a certain drug or drugs. It may be used for:
- Employment. Employers may test you before hiring and/or after hiring to check for on-the-job drug use.
- Sports organizations. Professional and collegiate athletes usually need to take a test for performance-enhancing drugs or other substances.
- Legal or forensic purposes. Testing may be part of a criminal or motor vehicle accident investigation. Drug screening may also be ordered as part of a court case.
- Monitoring opioid use. If you’ve been prescribed an opioid for chronic pain, your health care provider may order a drug test to make sure you are taking the right amount of your medicine.
_
There are limits to urine drug tests. Most drugs are metabolized by the body and may not be detected after a certain period of time. Additionally, the urine specimen can be tampered with and falsified. Hair strand analysis is a more reliable way to test for the presence of drugs. It is less invasive, and most drugs can still be detected as long as 90 days after use, and hair from any part of the body can be collected for analysis. The analyses of hair strands can form a more complete picture of a person’s drug use over time. Blood, saliva, and sweat may also be tested for drug use. The detection period, though, is very short. Typically, these tests are used when urine or hair testing is not available or practical. For example, police officers conduct onsite saliva tests to determine the amount of alcohol a person has recently consumed.
Drug screening tests cannot be used to determine if a person has a drug or alcohol addiction, however. They are typically used in the addiction assessment process to determine the type of drugs a person is using. It is best to talk to a doctor or clinician to determine whether you have an addiction.
_
Urine vs. hair analysis:
Department of Transportation in the U.S. currently recognizes only urinalysis as a drug test method, allowing employers to require additional test methods as part of employer hiring practices. However, a growing number of trucking company employers, including Trucking Alliance carriers, require a second drug test, a hair analysis, as part of their pre-employment truck driver hiring policies. Here, a lab technician will cut off a small portion of your hair for testing (typically, the first inch and a half of hair nearest the root will be tested). Hair strand testing looks for two things: the presence of a drug and something called a metabolite that carries a record of the drug. When a person consumes drugs, the drugs enter the blood stream. The blood then metabolizes, or processes the drugs and produces a metabolite. Hair follicles use blood for nourishment, and the presence of drugs and the metabolites are absorbed into the hair follicle. As hair grows it passes a record of drug use through the follicle into the hair strands. Hair strand testing can detect traces of illegal substances from as recently as 10 days to as far back as 90 days (using a typical 1 1/2-inch hair sample) from their use or ingestion. Using urinalysis alone missed nine out of 10 illegal drug users, according to the Alliance survey. Cocaine was the most prevalent drug that tested positive, followed by opioids and marijuana. Applicants who failed or refused the hair test were disqualified for employment at these companies, but likely obtained the same job elsewhere, at companies that administer only a urinalysis.
_
The DrugWipe is a test used to wipe surfaces for traces of drug residue. It may also be used for sweat or saliva testing of individuals. Law enforcement at the roadside can quickly screen suspected drivers of being under the influence of an illegal drug by using the DrugWipe. DrugWipe was named a finalist in the 2011 Cygnus Law Enforcement Group Innovation Awards competition. The DrugWipe 6s (saliva only) test was entered under the category of ‘Traffic Enforcement’.
Saliva testing is used in random roadside drug testing. It is used to detect the presence of THC (the active component in cannabis) and amphetamine type stimulants including methylamphetamine (‘speed’ or ‘ice’) and MDMA (‘ecstasy’), which are, after alcohol, the drugs of greatest concern in relation to road safety. A roadside saliva screening test takes around five minutes. Where a positive result is obtained, the driver is required to undertake a second saliva test or provide a blood sample to confirm the presence of the prescribed drug. In most cases, the confirmatory saliva test takes around 30 minutes.
MDMA can be detected in saliva for approximately 24 hour after use, cocaine can be detected in the saliva for up to 1 day after use and Delta-9 tetrahydrocannabinol (THC) (the active component in cannabis) can be detected in saliva for up to 4 hours after use. However this all depends on the amount and potency used, and a person’s metabolism rate.
_
So prevalent is drug use that all healthcare professionals, wherever they practice, should be able to identify and carry out a basic assessment of people who use drugs. Many people who misuse drugs do not present to drug treatment services, with perhaps 50% of people who misuse drugs not seeking treatment; however this represents a significant improvement on the position in the UK in the early 1990s, when perhaps only 20% of people who misused drugs sought treatment. Of those who do not seek treatment for their drug misuse, a proportion may nevertheless present to other medical services, the criminal justice system and social care agencies. Many will not be seeking help for their drug problems and many, for example some of those primarily misusing cocaine or cannabis, may not be aware of the potentially harmful effects of their drug use. It is probable that those who present to services for drug treatment have the greatest number of problems (Best et al., 2006b).
_
An improved diagnostic evaluation instrument for substance abuse patients: The Addiction Severity Index:
The Addiction Severity Index (ASI) is a structured clinical interview developed to fill the need for a reliable, valid, and standardized diagnostic and evaluative instrument in the field of alcohol and drug abuse. The ASI may be administered by a technician in 20 to 30 minutes producing 10-point problem severity ratings in each of six areas commonly affected by addiction. Analyses of these problem severity ratings on 524 male veteran alcoholics and drug addicts showed them to be highly reliable and valid. Correlational analyses using the severity ratings indicated considerable independence between the problem areas, suggesting that the treatment problems of patients are not necessarily related to the severity of their chemical abuse. Cluster analyses using these ratings revealed the presence of six subgroups having distinctly different patterns of treatment problems. The authors suggest the use of the ASI to match patients with treatments and to promote greater comparability of research findings.
______
______
Adverse impact of drug addiction:
_
Adverse consequences of psychoactive substances and their mechanisms of action:
In the majority of cases, people use psychoactive substances because they expect to benefit from their use, whether through the experience of pleasure or the avoidance of pain. The benefit is not necessarily gained directly from the psychoactive action of the substance. Someone drinking beer with colleagues may be more motivated by the feeling of fellowship this brings than by the psychoactive effect of the ethanol. However, the psychoactive effect is nevertheless present, and is usually at least peripherally involved in the decision to use. In spite of the real or apparent benefits, the use of psychoactive substances also carries with it the potential for harm, whether in the short term or long term. Such harm can result from the cumulative amount of psychoactive substance used, for example, the toxic effect of alcohol in producing liver cirrhosis. Harmful effects can also result from the pattern of use, or from the form or medium in which it is taken (see figure below). Pattern of use is of obvious importance – for instance, in the case of deaths due to overdose – not only in terms of the amount on a particular occasion, but also in terms of the context of use (e.g. heroin use accompanied by heavy alcohol use). The form or medium of use may also be crucially important. Most of the adverse health effects of tobacco smoking, for instance, come not from the nicotine itself, but from the tars and carbon monoxide which are released when nicotine is taken in cigarette form. Similarly, the adverse effects from taking the drug by injection are evident in the case of heroin use.
The main harmful effects due to substance use can be divided into four categories (see figure below).
First there are the chronic health effects. For alcohol this includes liver cirrhosis and a host of other chronic illnesses; for nicotine taken in cigarette form, this includes lung cancer, emphysema and other chronic illnesses. Through the sharing of needles, heroin use by injection is a main vector for transmission of infectious agents such as HIV and hepatitis C virus. Second there are the acute or short-term biological health effects of the substance. Notably, for drugs such as opioids and alcohol, these include overdose. Also classed in this category are the casualties due to the substance’s effects on physical coordination, concentration and judgement, in circumstances where these qualities are demanded. Casualties resulting from driving after drinking alcohol or after other drug use feature prominently in this category, but other accidents, suicide and (at least for alcohol) assaults are also included. The third and fourth categories of harmful effects comprise the adverse social consequences of the substance use: acute social problems, such as a break in a relationship or an arrest, and chronic social problems, such as defaults in working life or in family roles. These last categories are important in relation to alcohol and many illicit drugs, but are poorly measured and mostly excluded from measurements of health effects such as in the Global Burden of Disease (GBD).
_
Mechanisms relating psychoactive substance use to health and social problems are depicted in figure below:
_
The probability of the occurrence of these categories of harmful effects also depends on how much of the substance is used, in what forms, and with what patterns of use. These aspects of use may be thought of as linked to the different kinds of health and social problems by three main mechanisms of action (see figure above). One mechanism concerns the direct toxic effects of the substance, either immediate (e.g. poisoning) or cumulative over time (e.g. cirrhosis). A second mechanism concerns the intoxicating or other psychoactive effects of the substance. A traffic accident may result, for instance, from the fact that a car driver is under the influence of sedatives. A retail store employee may be intoxicated at work after using cannabis, and because of this, may be fired by the manager. The third mechanism concerns addiction on the substance. At the heart of this concept is the idea that the user’s control over and volition about use of the drug has been lost or impaired. The user is no longer choosing to use simply because of the apparent benefits; the use has become habitual, and cravings to reuse mean that the user feels that the habit is no longer under control. The user’s dependence is thus seen as propelling further use despite adverse consequences which might have deterred others who are not dependent, from further use.
The link between substance use and harm in a particular case may, of course, involve more than one of the three mechanisms. Benzodiazepines may be involved in a case of suicide, for instance, both through the user’s despair over the disruption brought to his or her life by dependence on the drugs, and as the actual means of suicide through overdose. However, the mechanisms can also operate alone. It is important to keep in mind, moreover, that dependence is not the only mechanism potentially linking substance use to health and social harm.
______
Drug abuse impact everybody:
The American statistics given below can be extrapolated for rest of the world although other nations have different patterns of drug abuse and different socioeconomic conditions:
- Drug Abuse is costly:
Drug abuse is a major public health problem that impacts society on multiple levels. Directly or indirectly, every community is affected by drug abuse and addiction, as is every family. Drugs take a tremendous toll on our society at many levels.
-Substance abuse costs U.S. more than $484 Billion in 2003. The costs of drug abuse are as substantial as compared to other Chronic Conditions: e.g. Diabetes costs society $131.7 billion annually and Cancer costs society $171.6 billion annually. This includes health care expenditures, lost earnings, and costs associated with crime and accidents. This is an enormous burden that affects all of society – those who abuse these substances, and those who don’t.
-In 2013, abuse of tobacco, alcohol, prescription, and illicit drugs is economically taxing to the United States, annually costing approximately $137 billion in direct health care expenses. Cost estimates that include crime and lost work productivity balloon to over $600 billion dollars, equivalent to 17.1% of the U.S. federal budget.
Taking into account the staggering costs associated with criminal justice, treatment and loss of productivity, we estimate that the real cost of America’s drug epidemic exceeds $1 trillion, says Kumar Cidambi, CEO of the Center for Network Therapy (CNT), New Jersey’s first licensed outpatient facility for the treatment of all substances of abuse. He estimates that the cost will surely rise without changes in policies that promote criminalization and restrict funding for treatment.
- Drug Abuse is a major Public Health Problem:
Many of America’s top medical problems can be directly linked to drug abuse:
-Cancer: Tobacco contributes to 11-30% of cancer deaths.
-Heart Disease: Researchers have found a connection between the abuse of tobacco, cocaine, MDMA (ecstasy), amphetamines, and steroids and the development of cardiovascular diseases. Tobacco is responsible for approximately 30% of all heart disease deaths each year.
-HIV/AIDS: Approximately one-third of AIDS cases reported in 2000 (11,635) and most cases of hepatitis C (approximately 25,000 in 2001) in the United States are associated with injection drug use.
-Approximately half of pediatric AIDS cases (4,700 reported through 2002) result from injection drug use or sex with injection drug users by the child’s mother.
- Many of America’s top social problems also relate to or impact drug abuse:
-Drugged Driving: The National Highway Traffic Safety Administration estimates that drugs are used by approximately 10 to 22 percent of drivers involved in crashes, often in combination with alcohol.
-Violence: At least half of the individuals arrested for major crimes including homicide, theft, and assault were under the influence of illicit drugs around the time of their arrest.
-Stress: Exposure to stress is one of the most powerful triggers of substance abuse in vulnerable individuals and of relapse in former addicts.
-Child Abuse: At least two-thirds of patients in drug abuse treatment centers say they were physically or sexually abused as children.
_
Drug abuse impacts the individual, family, and community.
Everybody knows someone who is affected by drug abuse.
- Individual:
-Adolescence: This is a time period of high vulnerability to drug abuse and other risk taking behaviors.
-Mental Illness: People with mental illness are particularly at risk for problems related to substance abuse.
-Consequences of Substance Abuse: These can include illness, injuries, and death. Each year approximately 40 million debilitating illnesses or injuries occur among Americans as the result of their use of tobacco, alcohol, or another addictive drug. In 2000, approximately 460,000 deaths were attributable to illicit drug abuse and smoking in the U.S.
- Families can be destroyed by drug abuse:
According to the National Center on Addiction and Substance Abuse at Columbia University, families facing substance abuse and addiction frequently face the following consequences.
-Families with substance abusers typically face more financial pressure as these individuals are at greater risk for job instability, long-term unemployment, and accidents or injuries at work.
-Substance abuse in the family increases the likelihood of unhappy marriages and divorce.
-Male alcohol and drug abuse are associated with an increased risk of partner violence, which also increases the likelihood that children in the household will engage in substance use as well as a result of the stress and trauma of witnessing violence at home.
-Children of substance abusers are often neglected or abused. Adults with substance use disorders are 4.2 times more likely to report neglectful behavior and 2.7 times more likely to report abusive behavior toward their children.
When a family member is suffering from addiction, other members of the family typically adopt certain behaviors, thoughts, and attitudes to cope with the destructive impact of the drug abuse. These coping strategies may seem like the only way to deal with the addiction, but in fact, are often very unhealthy and harmful.
- Community:
-Homelessness: 31% of America’s homeless suffer from drug abuse or alcoholism.
-Crime: As many as 60% of adults in Federal prisons are there for drug-related crimes.
-Education: Children with prenatal cocaine exposure are more likely (1.5 times) to need special education services in school. Special education costs for this population are estimated at $23million per year.
-The Workplace: In 1997, illicit drug users were more likely than others to have missed 2 or more days of work in the past month and to have worked for three or more employers in the past year.
_______
The figure below shows harm to users and harm to others by drugs:
______
Dependence on drugs can create a number of dangerous and damaging complications, including:
- Getting a communicable disease. People who are addicted to a drug are more likely to get an infectious disease, such as HIV, either through unsafe sex or by sharing needles.
- Other health problems. Drug addiction can lead to a range of both short-term and long-term mental and physical health problems. These depend on what drug is taken.
- Accidents. People who are addicted to drugs are more likely to drive or do other dangerous activities while under the influence.
- Suicide. People who are addicted to drugs die by suicide more often than people who aren’t addicted.
- Family problems. Behavioral changes may cause marital or family conflict and custody issues.
- Work issues. Drug use can cause declining performance at work, absenteeism and eventual loss of employment.
- Problems at school. Drug use can negatively affect academic performance and motivation to excel in school.
- Legal issues. Legal problems are common for drug users and can stem from buying or possessing illegal drugs, stealing to support the drug addiction, driving while under the influence of drugs or alcohol, or disputes over child custody.
- Financial problems. Spending money to support drug use takes away money from other needs, could lead to debt, and can lead to illegal or unethical behaviors.
______
Club drugs and erectile function: Far from sexual ecstasy:
The use of these agents is on the rise, especially among young individuals who attend ‘raves’ and ‘circuit parties’. The four most common ‘club drugs’ include 3,4-methylenedioxymethamphetamine (MDMA: ‘ecstasy’), gamma-hydroxybutyrate (GHB), ketamine (‘Special K’) and methamphetamine (‘crystal meth’, ‘crank’, ‘ice’). Their effects on sexual function is described below.
MDMA:
The sympathomimetic effects of the synthetic amphetamine cause systemic vasoconstriction. It is hypothesized that this is one factor in the drug’s role in erectile dysfunction in young, otherwise healthy, users. The negative effects of these club drugs on sexual dysfunction have been indirectly determined by the frequent concomitant use of ‘Vitamin V’ (Viagra). Users report episodes of erectile dysfunction and state that sildenafil is taken as an adjunct to prevent sexual failure.
GHB:
GHB is another club drug that is gaining popularity. This drug was sold in health food stores due to its purported anabolic, muscle-building effects. The Food and Drug Administration in the United States pulled this drug from retail markets in 1991. This compound is structurally similar to the central inhibitory neurotransmitter gamma-aminobutyric acid. GHB is reported to increase feelings of euphoria, relaxation and sexuality in users. Participants describe the intoxication from GHB to be similar to alcohol intoxication or the hypnotic intoxication associated with sedatives. However, many adverse effects of GHB have been documented. In regular users, loss of consciousness was reported by 66%, overdose by 28% and amnesia by 13%. Systemic side effects include nausea, vomiting, dizziness, confusion, drowsiness, respiratory depression, bradycardia and hypotension. GHB is known to have effects on the central neurotransmitter, dopamine. GHB is normally found in the human brain, especially in the basal ganglia. It primarily acts to inhibit dopamine release in vivo, but, in some instances, may have the paradoxical effect of stimulating dopamine release. Dopamine has been documented to be a central initiator of erectile function. If GHB inhibited dopamine release, it would be associated with erectile dysfunction; however, if GHB stimulated dopamine release, then this effect may explain the subjective feelings of increased sexuality in GHB users. The more alarming aspect of GHB is its effect on sexual behaviour. GHB in its liquid form can be mixed with alcohol, masking its taste. Due to its amnestic qualities, as well as causing an increase in sexual feeling, it has been implicated as a ‘date rape’ drug.
Methamphetamine:
Its effects on sexual function are multiple. Again, due to the sympathomimetic properties of amphetamines, which cause vasoconstriction, vascular erectile dysfunction can ensue. As well, methamphetamine has been demonstrated to induce central dopamine depletion and neurotoxicity. As previously mentioned, dopamine has been found to be a central initiator of sexual function. Interestingly, one study examined the use of apomorphine as a neuroprotectant in methamphetamine-induced neurotoxicity. Apomorphine, a dopamine agonist used in the treatment of erectile dysfunction, was found to protect nerves from the detrimental effects of methamphetamine. Thus, it appears that dopamine depletion may be another pathway that causes erectile dysfunction in methamphetamine users.
Ketamine:
Ketamine is a derivative of phencyclidine, a known psychotropic recreational drug. Anaesthetists commonly use this drug for induction of anaesthesia. Ketamine is reported to produce analgesia and amnesia. Ketamine is documented to cause vivid, technicolour visual, auditory, and proprioceptive hallucinations. This effect is the allure of ketamine as a recreational drug. As with the other club drugs, ketamine has many systemic effects. This drug has been shown to directly stimulate the central nervous system, leading to increased sympathetic nervous system outflow. Thus, ketamine’s hemodynamic effects include tachycardia, hypertension, arrhythmia and an increase in the cardiac index. The vasoconstriction caused by ketamine could potentially lead to vascular erectile dysfunction.
Club Drugs and sexual behavior:
Besides the concern of the physiological effects of many of these drugs on peripheral vasculature and erections, these drugs can affect sexual decision-making and risk-taking behaviour. The behaviour and the sexual choices of gay and bisexual men using club drugs at circuit parties has been examined. In one study, 295 gay or bisexual men were screened. Of these men, 80% had used MDMA, 66% ketamine, 43% methamphetamine, 29% GHB, 14% sildenafil and 12% poppers (amyl nitrate); 53% had used four or more drugs. Unprotected anal intercourse with partners of unknown HIV serostatus or opposite HIV serostatus was reported in 21% of men who were HIV-positive and 9% of men who were HIV-negative. This alarming rate of high risk behaviour was found to be higher than those reported without the use of club drugs.
Another concern relates to the illicit use of sildenafil due to the side effects of the recreational drugs. The use of nitrates is a known contraindication to the concomitant use of sildenafil. One study demonstrated that some men were using sildenafil with amyl nitrate, putting themselves at cardiovascular risk.
Many of the club drugs have significant sympathomimetic effects that cause significant vasoconstriction, which can lead to erectile dysfunction. Also, many of these drugs have central and neurotoxic effects (GHB, methamphetamine), which may have effects on neurotransmitters involved in the central initiation of the erectile pathway. More worrisome is the increase in high risk sexual behaviour and sexual assault. Young adults need to be informed of the risks that these drugs pose to their sexual health. As well, when assessing young adults who present with sexual dysfunction, the use of club drugs should be included in the sexual history. Counselling patients regarding the effects of these drugs should be a part of the treatment of erectile dysfunction in club drug users.
________
Cocaine – the “perfect heart-attack drug”:
The powdered form of cocaine is either inhaled through the nose (snorted) and absorbed through nasal tissue, or dissolved in water and injected into the bloodstream. Crack is a form of cocaine that has been processed to make a rock crystal that can be smoked. Even so-called recreational cocaine users may have higher blood pressure, stiffer arteries and thicker heart muscle walls than non-users — all of which can cause a heart attack. An Australian study presented at the American Heart Association’s Scientific Sessions in 2012 was the first to document these cardiovascular abnormalities in seemingly healthy regular cocaine users long after the immediate effects of cocaine have worn off. Researchers – who called cocaine “the perfect heart attack drug” – showed how users had higher rates of multiple factors associated with higher risks of heart attack and stroke:
- 30 percent to 35 percent increase in aortic stiffening;
- 8 mm Hg higher systolic blood pressure; and
- 18 percent greater thickness of the heart’s left ventricle wall.
Cocaine is the illegal drug most often associated with visits to U.S. hospital emergency departments. Cocaine use has been associated with chest pain and myocardial infarction. In 2011, it was involved in an estimated 40.3 percent of illicit drug-related emergency department visits (505,224 visits), versus about 36.4 percent (455,668 visits) for marijuana and about 20.6 percent (258,482 visits) for heroin.
______
Drug use and viral infections:
People who engage in drug use or high-risk behaviors associated with drug use put themselves at risk for contracting or transmitting viral infections such as human immunodeficiency virus (HIV) and hepatitis. This is because some viruses spread through blood or other body fluids. It happens primarily in two ways: (1) when people inject drugs and share needles or other drug equipment and (2) when drugs impair judgment and people have unprotected sex with an infected partner. This can happen with both men and women. Drug use and addiction have been inseparably linked with HIV/AIDS since AIDS was first identified as a disease. According to the CDC, one in 10 HIV diagnoses occur among people who inject drugs. In 2016, injection drug use (IDU) contributed to nearly 20 percent of recorded HIV cases among men—more than 150,000 patients. Among females, 21 percent (about 50,000) of HIV cases were attributed to IDU. Additionally, women who become infected with a virus can pass it to their baby during pregnancy, regardless of their drug use. They can also pass HIV to the baby through breastmilk.
If you inject drugs, you are at risk for getting or transmitting HIV and hepatitis B and C if you share needles or equipment (or “works”) used to prepare drugs, like cotton, cookers, and water. This is because the needles or works may have blood in them, and blood can carry HIV. You should not share needles or works for injecting silicone, hormones, or steroids for the same reason.
______
Drugs, work place and employment:
The workplace is part of the community, reflecting its strengths and weaknesses. With an estimated 30 per cent of the world’s labour force not productively employed and young people seeking jobs faster than they are created, the ranks of the unemployed, and their problems, continue to increase. Drug abuse occurs frequently in the same age groups as those without productive work, increasing the vulnerability of this segment of the population to social problems.
Drug abuse represents difficult problems for employers because they are under competitive pressure to increase output. At the same time, these employers must respond to critical human resource issues to continue in business. Illicit drugs as well as alcohol and tobacco create significant problems in the workplace, according to recent studies and reports. Prescription drug problems, i.e. legal drugs used in unwise fashion or with unexpected results, are a major concern to employers, workers and enterprise representatives.
Work tasks that require higher level judgement, constant attention, immediate memory and fine motor skills are easily disrupted by drugs. Safety-sensitive jobs with immediate responsibility for the welfare of others are particularly vulnerable to drug impairment. Illicit and licit drugs may increase response time, disrupt fine motor skills and cause mood changes. Cocaine and other stimulants have the potential to induce compulsive use, disrupting work and family life. Drug abusers have more absenteeism, accidents on the job, medical claims and lost productivity than non-users. Drug problems have a costly impact on the workplace as well as the community. Employers and workers alike are concerned about the consequences of drug and alcohol abuse. According to one expert, “alcohol and drug involvement in accidents, and the impact on such employment indicators as absenteeism, turnover, medical claims, safety risk and lost productivity, confirm that there are direct costs involved with drug or alcohol use in the workplace”.
Productivity losses are calculated as work that would be reasonably expected to have been done if not for drug use (a loss of potential income and output and therefore GDP) as a result of a reduction in the supply or effectiveness of the workforce. Lost productivity in the United States as a result of labour non-participation is significant: $120 billion (or 0.9 per cent of GDP) in 2011, amounting to 62 per cent of all drug-related costs. Similar studies in Australia and Canada identified losses of 0.3 per cent of GDP and 0.4 per cent of GDP, respectively. In those two countries, the cost of lost productivity was estimated to be 8 and 3 times higher, respectively, than health-related costs due to morbidity, ambulatory care, physician visits and other related consequences.
The high costs of drug abuse can be reduced by careful pre-employment appraisal, supervision on the job, periodic prevention efforts and occasional interventions as required.
______
Drugs and poverty:
Throughout history, illicit drug use has often been linked to poverty. This is true around the world. For example, according to a study published in Drugs: Education, Prevention and Policy, poor proficiency in English, lower educational status and low economic status were associated with illicit drug use in Canada. The same is likely true in the United States.
Although rural and urban poor are alike in that they must constantly seek the essentials of daily living, they have basically different kinds of involvement in drug problems. Rural poverty is more related to the supply of illicit drugs and urban poverty is more related to both dealing and demand. Illicit growth provides income for farmers willing to take risks for the higher gain than obtained from licit crops. Poverty may change perspective so that immediate money with a risk is preferable to stable but delayed income with less risk. Because of the size of the shadow economy created by illicit drug money, the absorption of drugs and drug money into the fabric of society and the degree of dependence of many social and economic sectors on this relatively new income, drugs have a social significance far beyond that reflected in statistics on production, consumption or impact. Persons with marginal incomes often spend money on drugs, alcohol or tobacco instead of food, clothes and shelter. With dependence-producing drugs, sporadic use may deteriorate into regular or compulsive use, reinforcing consumption and guaranteeing a market for the supplier. The poorest 20 per cent of the population represent nearly one-half of the drug abusers, primarily heroin addicts, according to the National Survey of Drug Abuse. It has also been found that the poor often spend a greater percentage of their income on drugs than middle- or upper-income persons, and at a much greater cost to their families. A country expert on Pakistan has found that the “bulk of consumer expenditures on heroin are made by lower income groups, while the income generated by the heroin industry mainly flows to upper- and middle-income groups “. Drug traffickers do not normally put their illicit profits into productive enterprises. Nor is employment in the illicit drugs industry a significant means of putting money back into the community.
Studies show that drug abuse leads to poverty and family breakdown. According to a survey in India, weekly expenditure on drugs amounted to $13 and total expenditure ranged between US $250–$25,000. In families disrupted by drug abuse, poverty is often transmitted from parents to children.
________
Drugs and crime:
The connection between drugs and crime is reflected in at least three types of crimes:
- Drug‐defined crimes, such as the possession, use, or sale of controlled substances, which violates drug laws.
- Crimes committed by drug users to get money to buy more drugs or crimes committed by persons under the influence of drugs.
- Organized criminal activities, such as money laundering and political corruption, in support of the drug trade.
_
More than half of the economic cost of alcohol and other drugs is due to crime. A substance abuser is 18 times more likely to be involved in illegal activity than someone who does not abuse alcohol or other drugs. Many violent crimes have been linked to the mind-altering effects of drugs. Substance abusers often commit thefts to support their drug habits. Drugs and alcohol have been linked to domestic violence and sexual assault. At colleges, 75% of date rapes are alcohol-related. Among jailed sex offenders, 43% say they were under the influence of drugs or alcohol at the time of their crime.
_
The National Center for Victims of Crime reports that according to these 1997 Bureau of Justice statistics:
- 29 percent of inmates incarcerated in state prisons were using drugs when they committed crimes of violence
- 36 percent of inmates in state prisons were using drugs when they committed crimes involving the theft or damage of property
- 41.9 percent of inmates in state prisons were using drugs when they committed crimes involving drugs
- 22.4 percent of inmates in state prisons were using drugs when they committed crimes involving weapons
_
Whether illicit drug use should be considered a crime, a disease, a social disorder or some mixture of these is debated in many countries. Often, public policy is ambivalent about the nature of addiction, with social attitudes towards drug abuse reflecting uncertainty about what causes abuse and who is ultimately responsible.
A continuum exists in relation to accepted social status and crime. At one end is law-abiding behaviour and at the other, criminal activity. Between these two extremes are found deviant behaviour and delinquency. Many marginal persons who use drugs do not go on to become delinquents or criminals. If progression along this continuum does not take place within a country, the concept of progression is even less applicable across cultures. What is marginal or deviant in one culture may be tolerated or even considered to be part of the mainstream in another.
_
The complex connection between drug use, delinquency and crime has been discussed by experts for decades. Substance use and delinquent behaviour are often related, especially as either drug use or delinquency become more serious. Early sexual activity is strongly related to delinquency and drug abuse. Girls who have been pregnant report increased prior use of alcohol and other drugs. Youth who do not feel a strong attachment to their parents are more likely than others to use drugs and become delinquent.
One aspect of this connection between drugs and crime is temporal causation: which is cause and which is effect? In the case of individual addicts, drug use may precede crime or the reverse. After examination of groups, researchers in the United States have concluded that many variations exist but that some delinquency or crime often precedes addiction. They have found that involvement in property crime generally precedes the addiction career. After addiction occurs, property crime increases and narcotic use is further increased. One expert found that during “… periods of curtailed narcotics use produced by treatment, property crime levels are significantly reduced and become extremely low after termination of the addiction career”.
Researchers have found a close connection between drug abuse, criminal behaviour and social attitudes. Review of the crime/drugs literature supports three notions: heroin addicts are usually deeply involved in crime; daily opiate use increases criminality several fold; and many heroin abusers are not interested in obtaining treatment although drug treatment programs do reduce the criminality of addicts while they are in treatment.
Whether causality is involved in these relationships is not clear. Illicit drug use, delinquency and crime are best seen as closely interrelated behaviours, especially when they occur in contact with the supply of illicit drugs. Drugs and crime cannot be considered separately, in isolation from each other, especially if they emerge from a common set of circumstances. The close connection between drug use and criminal behaviour is supported by many studies. A national survey in the United States examined the relationship between drug use and criminal behaviour. Results show that “drug use is a strong correlate of being booked for a criminal offence, but age is the more important correlate of criminal involvement. There were few differences in models predicting violent as opposed to property crime, although minority status was a more important predictor of violent crime, and poverty was a more important predictor of property crime”.
_
A number of terrorists and organized criminal gangs are involved in or have close ties to the illicit drug trade. The link between the two is often money and power. One commentator cites an example of terrorists and drug dealers joining forces as follows: “Colombian political terrorists … finance much of their operations through the drug trade, which has caused some “conventional” drug barons to explode in retribution”. Colombia has emerged as a center of trafficking in cocaine, blending highly organized social and economic interests with an underground specializing in drug crime. Organized crime is not restricted to one area of the world. In Italy, faced with a socially entrenched, long-standing criminal element, authorities have enacted laws against the Mafia to seize and confiscate property illegally acquired. Aimed at depriving organized crime of their supply of money, these laws are reported to have had a positive impact.
Political changes may affect smuggling patterns, organized crime and drug abuse. A study of the effects of opening the borders within the European Union has raised the issues of drug trafficking, terrorism and computer crime. In the past, close links existed between terrorist groups in several European countries. Fewer control points between member countries of the European Union may make it more difficult to maintain adequate security. In the countries of the former Soviet Union and with the opening of eastern Europe, major changes are taking place in social controls, rules and laws. New frontiers tempt smugglers of drugs and other merchandise.
_
Drug use and violence:
Compared with alcohol, there are relatively few sources of data on patterns of drug use and violence in the U.S. These sources and studies provide the following picture: (1) In 1989, 60 percent of arrestees for violent offenses tested positive for at least one illegal drug, about the same fraction as those arrested for public order offenses, slightly less than those arrested for property crimes and sex offenses, and, as expected, far less than those arrested for drug offenses. (2) Users of certain drugs commit violent crimes at higher individual annualized frequencies than do nonusers, and violent crime frequency increases with drug use frequency. (3) The risk of drug-related homicide varies by place, from perhaps 10 percent of all homicides nationwide, to a third or more in certain cities, to more than 70 percent in high-risk areas of some cities as well as over time, in ways that vary from area to area.
_______
Drugs and environment:
The illicit manufacture and disposal of drugs and pharmaceuticals cause significant environmental contamination, owing to the precursor chemicals required for manufacture, the manufacturing process itself and the active ingredient or substance. Disposal introduces those substances into the environment in sewage, from where they can enter sediment, surface and ground water and the tissues of vegetation and aquatic organisms. As a result, wildlife and humans can be chronically exposed to very low doses of drugs and the chemicals used in their illicit manufacture. That results in costs to individuals and to Governments, as they are responsible for ensuring public health.
Illicit cultivation of both coca bush and opium poppy has often resulted in the clearance of forests—in the case of illicit cultivation of coca bush, primarily in Bolivia, Colombia and Peru. Since coca growers want to avoid police and military detection, they select remote and difficult terrain to clear. According to a recent report, “coca farmers cut down forests on steep hillsides subject to erosion, instead of expanding cultivation of rich alluvial soil on the valley floors”. An expert from Peru’s National Agrarian University, states that coca cultivation may have resulted in deforestation of 700,000 hectares in the Amazon region. The situation in Bolivia has similarities to that in Peru. Opium poppy cultivation has historically taken place in South-East Asia, where hill tribe farmers have cleared enormous amounts of rain forest to support their slash-and-bum agricultural system, using the new land for poppy growth and then subsequently moving to find more fertile land. More recently, significant poppy growth has taken place outside South-East and South-West Asia. In the tropical and high mountain forest regions of Latin America, opium poppy cultivators are planting crops on fragile land that is isolated from population centers, thereby reducing visibility and possibility of detection. Cannabis is even more widely grown than either opium or coca. Cannabis growers typically try to use the most fertile soils to produce the biggest crop, often abandoning fields after runoff and erosion have taken place.
Some devastating effects of illicit cultivation of cannabis plant, coca bush and opium poppy on biodiversity are the loss, degradation and fragmentation of the forests, and the loss of areas where food could be grown. In addition to the deforestation caused by illicit crop cultivation, chemicals used for the processing of illicit drugs can be harmful to biodiversity, both in the immediate area and downstream, as a result of chemical run-off. There can also be negative effects associated with the aerial spraying of crops. Chemicals used to process plants are often simply thrown on the ground or into streams or rivers. In speaking of Bolivia, an expert has stated that lime, sodium carbonate, sulfuric acid, kerosene, acetone and hydrochloric acid used in the processing range from being moderately toxic to extremely destructive of the environment. Around 30,000 tons of toxic chemicals are flushed down the waterways each year, and this does not count what the police confiscate and also characteristically discard in the country’s waterways. Nor does it count the 200,000 tons of annually discarded contaminated coca leaves thrown about and left to leach into the soil. A Peruvian official has concluded that the extensive use of chemicals to process drugs and the practice of disposing of them by the quickest means possible have been responsible for the killing off of species of fish and aquatic plants in the Huallaga River. Other experts, relying on United States government studies, have concluded that cocaine processors in the Andean region” dump each year 10 million liters of sulfuric acid, 16 million liters of ethyl ether, 8 million liters of acetone, and from 40 to 770 million liters of kerosene, depending on how much is recycled. The processors simply pour these dangerous chemicals on to the ground, and they quickly end up in the region’s rivers”. The chemical wastes alter water pH, reduce oxygen and lead to acute poisoning of fish and plants with possible genetic mutations in some species.
Finally, the emergence of illicit drug cultivation and manufacture in residential areas brings with it concern about reduced quality of life for residents, neighbourhood decay and property damage resulting from child endangerment, criminal activity and explosions.
______
Drugs and economy:
Illicit traffic in drugs generates enormous profits. Funds are obtained in or converted into an international currency and then moved into financial centers which can electronically transfer the money around the world. The process of moving the money makes its origins indistinguishable from those of legitimately obtained currency. Shell, ghost or front operations are used in this process, as are businesses which handle large amounts of cash.
It was estimated that sales of cocaine, heroin and cannabis amount to approximately $122 billion per year in the United States and Europe, of which 70 per cent or as much as $85 billion per year, could be available for laundering and investment. Given the magnitude of these estimates, the economies of the countries involved are likely to be overwhelmed by drug money. In the case of countries whose economy is dependent on commodities, such as is the case with Colombia and its coffee exports, sharp falls in the world price of the commodity may increase the importance of drug money to the national economy. The $85 billion per year estimated from illicit trafficking in heroin, cocaine and cannabis makes it larger than the GNP of three-fourths of the 207 economies of the world. This amount is larger than the GNP of Poland or Portugal and slightly smaller than that of Hong Kong.
The importance of production of illicit drugs to an economy will vary significantly from country to country. As noted earlier, income from the drug trade is exorbitant in some nations. Speaking of Colombia, a country expert estimates that businessmen of the illegal drugs industry would have “huge combined drug and capital income relative to the size of the country’s economy”. He further states that “between 1976 and 1986 gross private fixed investment ranged from $1.6 to $3.7 billion and averaged $2.8 billion, figures that clearly indicate that the illegal businessmen had the capacity to invest in Colombia an amount as large as what official data attributes to the whole private sector of the country”. This view of the impact of the drug trade is not atypical. The United States Office of Technology Assessment has found that in Bolivia, the coca economy annually generates as much foreign exchange (roughly $600 million) as all other exports combined. It has also found that a significant number of persons are employed in the coca economy: 7 per cent of the labour force in 1990, although this figure is significantly less than the 20 per cent estimated to have been employed in coca in the late 1980s.
The economic costs of drug abuse can be categorized as direct and indirect. Direct costs involve increased costs of police, courts, military, treatment programs, welfare payments to drug addicts and their families, as well as increased security measures by businesses. Indirect economic costs include the displacement of legal industries; diminished control over the economy; spending money for drugs and inappropriate use of money gained from drug sales; and fiscal problems related to the inability to tax the drug economy. Concerning displacement of legal industries due to the cocaine trade, commentators have found that the cocaine industry in a developing country can create such a high inflow of foreign exchange that dollars become cheap relative to the local currency. This reduces the competitiveness of local products in both foreign and domestic markets.
Because money generated by illicit activities does not normally enter into the formal economic process of a country, macroeconomic planning is not possible for these funds. Hence, a source of serious error is introduced into estimates of national income and expenditure. In speaking of the need for improved information on the illegal sector, a country expert has concluded that “large financial flows are not accounted for and the enormous sums generated by the opiate industry fail to show up in investment rates. This allows a general conclusion that most investment has been unproductive and used for speculative purposes. However, an increasing part of the GNP is produced outside official accounts and thus outside intervention possibilities. This inevitably contributes to skewed macro-planning”. Moreover, control over expenditures is reduced when governments have to devote resources to protect the financial and banking systems against subversion through additional banking regulation, increased reporting and other anti-money-laundering measures.
A very important indirect cost of the drug industry is a result of the fact that governments are not able to tax it. In such a case, governments have no choice but to increase taxes on those who can be expected to pay. However, the externalities of the drug industry, i.e. the hidden economic and social costs of illicit drug production and trafficking, cannot be charged back to those involved. They are, therefore, an added burden to the law-abiding population. Experts consider cocaine a good example of market failure, a situation where markets encourage behaviour that is unprofitable for society and discourage behaviour that is better for development: Market failure occurs when there is a difference between the costs of an action for an individual and the cost of that action for society. In the case of cocaine, market failure occurs -the market encourages cocaine production even though it may be bad for society -because the roughly 5% to 15% of the national population involved in the cocaine industry do not bear many of the costs they impose on society. This situation of market failure applies not only to cocaine production and trafficking but also to the production and sales of other illicit drugs.
_______
Drug-affected driving:
The abuse of drugs affects perception, attention, cognition, coordination and reaction time, among other neurological functions, which affect safe driving. According to roadside survey studies from Canada, the USA, Australia and various European countries, cannabis is often the illicit drug most commonly used prior to driving. After alcohol, cannabis is the substance most frequently detected in seriously and fatally injured drivers. Research has found that habitual cannabis use is linked to a 9.5-fold greater risk of driving accidents, cocaine and benzodiazepines increase the risk 2-10 times, amphetamines or multiple drug use increase the risk 5-30 times, and alcohol in combination with drugs increases the risk of getting seriously injured or killed while driving by a factor of 20-200. That increased risk also has consequences for passengers and others on the road, who may become victims of drug-affected driving. The Road Safety Report of the World Health Organization stated that amphetamine was responsible for 51% of the drug-related traffic accidents, followed by marijuana (22%), cocaine (14%) and opioids (13%).
The effects of specific drugs on driving skills differ depending on how they act in the brain. For example, marijuana can slow reaction time, impair judgment of time and distance, and decrease coordination. Drivers who have used cocaine or methamphetamine can be aggressive and reckless when driving. Certain kinds of prescription medicines, including benzodiazepines and opioids, can cause drowsiness, dizziness, and impair cognitive functioning (thinking and judgment). All of these effects can lead to vehicle crashes.
_______
_______
Evolution of drug addiction:
In order to truly understand addiction, we have to look at the evolution of the human brain. Human beings, being highly evolved, have an incredibly large neo-cortex compared with other living beings. This neo-cortex can be described as our “new” or “thinking” brain. However, we still share with other beings an “old” or “instinctual” brain that controls all of our involuntary functions, including our instinctual drives (e.g., hunger, sex, and nurturing). It is in this old or instinctual brain that the pathophysiology of addiction resides, an area within the limbic system that controls our moods, a reward pathway within the medial forebrain bundle that includes the nucleus accumbens (NA) and the ventral tegmental area (VTA).
_
The use of psychoactive substances is one of the most perplexing human behaviours. Some substances cause immeasurable harm to individuals and societies (e.g. heroin) or impose a tremendous social burden in the form of preventable chronic illnesses (e.g. tobacco), while others appear to be mostly harmless and are widely enjoyed by people around the world (e.g. coffee and chocolate). Historically, a broad range of psychosocial, behavioural and neurobiological theories seeking to understand drug phenomena are unified by the notions of reward and reinforcement (Thorndike 1911). According to these theories, recreational drugs reward and/or reinforce consumption, often via hedonic effects (Wise & Rompre 1989; Everitt & Robbins 2005; Kalivas 2005; Koob & Le Moal 2005; Nestler 2005).
_
According to the ‘conventional’ evolutionary perspective, the human propensity for substance use is the product of a ‘mismatch’ between emotional mechanisms that evolved in a past without pure drugs or direct routes of drug administration, and the occurrence of these phenomena in the contemporary environment (Tooby & Cosmides 1990; Nesse 1994; Nesse & Berridge 1997; Smith 1999). Consequently, psychoactive substances can ‘short-circuit’ the adaptive functions of positive emotions and instead ‘directly stimulate the brain mechanisms that regulate pleasure’ (Nesse 1994). Nesse & Berridge (1997) contend that ‘drugs of abuse create a signal in the brain that indicates, falsely, the arrival of a huge fitness benefit’. Similarly, drugs are used to block painful feelings or affect states, short-circuiting the adaptive functions of negative emotions. The conventional evolutionary explanation for human substance-using phenomena is based on the assumption that the human central nervous system is inherently vulnerable to psychotropic substances. Accordingly, the conventional view tends to focus on pathological rather than mundane substance use.
Contrary view:
Mammals have shared a co-evolutionary relationship with psychotropic plant substances that is millions of years old. This ‘deep time’ relationship is self-evident both in the extant chemical–ecological adaptations that have evolved in mammals to metabolize psychotropic plant substances and in the structure of plant defensive chemicals that have evolved to mimic the structure, and interfere with the function, of mammalian neurotransmitters.
Allelochemicals that mimic mammalian neurotransmitters are evidence of a deep-time relationship between psychotropic plants and mammals. Chemical analogs of mammalian neurotransmitters— psychoactive substances—were ubiquitous in the ancestral environment, as they are nowadays, in the form of plant allelochemicals: toxic metabolites deployed by plants to dissuade herbivores and pathogens (Johns 1990; Wink 1993). Over hundreds of millions of years, plants have evolved allelochemicals that mimic the structure of mammalian neurotransmitters (NTs), and bind at receptors in the nervous systems of plant predators (Wink 1993, 1998a, 1998c). This process is demonstrated in the structure–function relationship between ergot alkaloids & the neurotransmitters serotonin, dopamine and noradrenaline. In this case, the ergot alkaloid has evolved a single molecular structure that binds to any of three monoamine neurotransmitter receptors. Ergot alkaloids interfere with the central nervous system (CNS) neurotransmission of grazing animals, exerting a range of effects from vasoconstriction to hallucination (Wink 1998b).
This molecular co-evolutionary relationship between plants and their mammalian predators, the allelochemical–CNS phenomenon, represents evidence that psychotropic substances were a recurrent feature of the ancestral environment, and had been so for a great deal of time before the emergence of hominids. The allelochemical–CNS phenomenon is not idiosyncratic, but encompasses many of the known CNS-signaling pathways to the extent that, with the exception of alcohol, allelochemicals constitute all of the most commonly used psychotropic substances (see table below). Moreover, it is noteworthy that the discovery of several mammalian neurotransmitter (NT) systems has followed observations of the psychotropic effects of allelochemicals and of their site of action in the CNS. As Deakin (1980: 40) has observed, ‘the development of the opiate receptor concept begged the teleological question of the reason the brain contains a set of receptors for substances derived from plants’. Other receptor systems named for their allelochemical NT analogs are the nicotinic & muscarinic cholinomimetics, and the recently described cannabinoid system (Ameri 1999).
_
Examples of allelochemicals that interfere with mammalian neurotransmission:
_
Over the approximately 200 million-year evolutionary history of Mammalia, plants have evolved chemical defenses—neurotransmitter substitutes—that interfere with CNS-signaling processes in plant predators. In turn, mammals have evolved ‘counter adaptations’ to manage plant chemicals—functional mechanisms that have been interpreted conventionally as performing a defensive role against toxins. Plants have evolved neurotransmitter analogs to target the mammalian CNS, and that adaptations such as the cytochrome P-450 mechanism have evolved specifically to metabolize plant allelochemicals. The focus of contrary view is the origin of mundane and ubiquitous human substance-using behavior: why people everywhere choose to seek out substances in the first instance, not to explain why a minority go on to gross, habitual substance use.
_
Emerging insights from plant evolutionary ecology and the genetics of hepatic enzymes, particularly cytochrome P450, indicate that animal and hominid taxa have been exposed to plant toxins throughout their evolution. Specifically, evidence of conserved function, stabilizing selection, and population-specific selection of human cytochrome P450 genes indicate recent evolutionary exposure to plant toxins, including those that affect animal nervous systems.
_
Evolutionary biologists studying plant–herbivore interactions have convincingly argued that many plant secondary metabolites, including alkaloids such as nicotine, morphine and cocaine, are potent neurotoxins that evolved to deter consumption by herbivores (Karban & Baldwin 1997; Roberts & Wink 1998). On the other hand, neurobiology’s reward model sees interactions between drugs and the nervous system as rewarding and reinforcing. Hence, in their current forms, neurobiology’s reward model and evolutionary biology’s punishment model appear to be incompatible. This incompatibility is the paradox of drug reward. Resolving the paradox of human drug use will require new neurobiological models, or new interpretations of neurobiological reward theory, that are consistent with insights from evolutionary ecology.
________
________
Drug addiction in Special populations:
Research studies increasingly show that certain groups of people may be more vulnerable to drug abuse than members of the general population. These groups are sometimes referred to as “special populations” because their health concerns are unique and should be taken into consideration during addiction treatment. Addiction is a chronic condition that does not discriminate. It affects people of all ages, genders, races, social classes, educational backgrounds, and family structures. Addiction can affect us all, but some people may be particularly vulnerable to developing maladaptive, compulsive patterns of substance abuse compared to the general population.
______
Drug addiction in teens:
Drug abuse is a complex phenomenon, which has various social, cultural, biological, geographical, historical and economic aspects. The disintegration of the old joint family system, absence of parental love and care in modern families where both parents are working, decline of old religious and moral values etc. lead to a rise in the number of adolescent drug addicts who take drugs to escape hard realities of life. The processes of industrialization, urbanization and migration have led to loosening of the traditional methods of social control rendering an individual vulnerable to the stresses and strains of modern life. The fast-changing social milieu, among other factors, is mainly contributing to the proliferation of drug abuse, both of traditional and of new psychoactive substances. The introduction of synthetic drugs and intravenous drug use leading to HIV/AIDS has added a new dimension to the problem. Drug use, misuse or abuse is also primarily due to the nature of the drug abused, the personality of the individual and the addict’s immediate environment.
Kastner and Silbereisen demonstrated that drug abuse among adolescents is clearly related to the developmental pressures. They ascertained that the use of drugs can assume developmental relevance in 6 ways:
- A deliberate violation of social norms
- Testing whether the adolescent is able to behave like an adult.
- Excessive and ritualized behaviour in the sense of testing one’s limits.
- A lack of self control and thus an indicator of “underdevelopment.”
- An age related life-style, aimed at peer group integration.
- An emergency reaction to age-related every day stress, thus a developmentally relevant coping strategy.
_
Why Teenagers experiment with Drugs?
Some reasons why teens use drugs include stress, boredom, and peer pressure.
- Boredom
One of the most common reasons that teenagers begin experimenting with drugs and alcohol is that they are simply bored and have no deeper interests. They see drugs and alcohol as a pastime to be explored.
- Bonding Experience
Many teenagers, usually around freshman year in high school, are shy and have trouble making friends (especially at a new school with older students). They turn to drugs and alcohol to help them feel more confident or to bond with a social group that is known for using these substances. This isn’t the same as direct peer pressure; it stems from the need to bond and make friends.
- Depression
Some teens turn to drugs and alcohol as a form of escapism. When they are sad or depressed, they see these substances as a way to forget and feel happier. It’s their attempt to self-medicate.
- Curiosity
Curiosity is a natural part of life and teenagers are not immune to the urge. Many teens begin experimenting with drugs and alcohol simply because they are curious and want to know what it feels like.
- Weight Loss
Female teenagers often turn to harder drugs—such as cocaine—for a quick way to lose weight. During high school especially, young girls become more body-conscious and may become desperate to slim down and attract the attention of popular boys. These young ladies may also be struggling with a co-occurring eating disorder, such as anorexia or bulimia.
- Stress
During high school many teenagers are overly stressed with a packed schedule of advanced classes and extracurricular activities. A lack of coping skills can lead us to seek out an artificial method of coping with stress. They then turn to drugs such as marijuana in order to relax.
- Low Self-Esteem
In teenagers, especially between the ages of fourteen and sixteen, low self-esteem due to physical appearance or lack of friends can lead to self-destructive behavior. The media, bullies, and often family put pressure on teenagers to act and look a certain way, and they lose confidence in themselves if they don’t meet those high standards. Drugs and alcohol seem like an easy way to escape this reality.
- Enhanced Experiences
Drugs and alcohol are often used to enhance certain experiences. Cocaine and Amphetamine are commonly used to enhance energy and focus when they feel like they can’t do something on their own and need a little help. Ecstasy can be used for a lack of inhibition and enhanced sexual experience. Marijuana and alcohol are often used to relax and be more comfortable in social situations.
- Peer Pressure
The classic tale of peer pressure is the reason they experiment with drugs and alcohol. This peer pressure happens most often between the ages of sixteen and eighteen, when teenagers begin to think “everyone else is doing it,” so they should too.
- Now or never
Teenagers often feel a social imperative to experiment and experience all that they can while they are still young. They feel like it is a “now or never” situation. They have to try drugs now, before they become adults and have responsibilities.
- Genetics
If there is a family history of drug addiction or alcoholism, teenagers may be genetically predisposed to experiment with drugs and alcohol and become addicted.
_____
Party Culture:
Partying among teens and young adults may have been viewed as relatively normal behavior in previous generations, yet these days, given the considerable dangers associated with various drugs and drug behaviors, the risks are far greater. Today’s “party culture” is more likely to involve prescription medications combined with alcohol and other drugs, the consequences of which can be very harmful, particularly because people between the ages of 12 and 18 have bodies and minds that are still developing.
What Are Pharm Parties?
In recent years, prescription drug use has escalated so much so that it currently ranks second only to marijuana use among young adults. The combination of increased accessibility of prescription drugs, the misconception that prescription drugs are safer than other drugs, and the social acceptability of using prescription drugs has created the perfect storm for prescription drug misuse and abuse. A particularly worrying new trend among young people is sharing prescription and over-the-counter medications to get high. Teens gather to have a “pharm party”—also sometimes referred to as “Skittles parties”—where they each bring prescription drugs and contribute to a mixture of pills thrown into a bowl. These bowls and baggies of random pills mixed together are often referred to as “trail mix.” Teenagers pass around the bowl and each person takes a handful of the drugs to get high.
Today’s party culture may include abusing the following substances:
- Cough medicine: When taken in large amounts, the main ingredient in cough medicine (dextromethorphan, or DXM) can cause serious reactions, like nausea, vomiting, increased heart rate and blood pressure, impaired motor function, and numbness.
- Prescription drugs: Taking prescription drugs in ways other than prescribed by your doctor can be very dangerous and can ultimately lead to addiction. Young adults between the ages of 18 and 25 were the biggest abusers of prescription painkillers, ADHD stimulants, and anti-anxiety drugs. In 2014, more than 1,700 young people died from a prescription drug overdose.
- Inhalants: Sniffing the fumes or inhaling the aerosol from household items such as paint thinners, certain glue bottles, computer cleaning dusters, or nitrous oxide canisters can cause damage to the brain and other organs.
- Marijuana: Marijuana use can lead to problems with learning and memory and can make it more difficult for you to solve problems. It distorts perception and can impair your coordination, which can increase your risk of accidents or injury.
_____
Common risk factors for teen drug abuse include:
- A family history of substance abuse
- A mental or behavioral health condition, such as depression, anxiety or attention-deficit/hyperactivity disorder (ADHD)
- Impulsive or risk-taking behavior
- A history of traumatic events, such as experiencing a car accident or being a victim of abuse
- Low self-esteem or feelings of social rejection
_____
Social and Cultural Consequences of Adolescent Substance Abuse:
Adolescent drug abuse is one of the major areas of concern in adolescent and young people’s behavior. The use of substances may compromise an adolescent’s mental and emotional development by interfering with how young people approach and experience interactions. In addition, adolescents are at serious risk for a number of direct and indirect consequences, including the following:
- Traffic Accidents
- School-Related Problems
- Risky Sexual Practices
- Delinquent Behavior
- Juvenile Crime
- Developmental Problems
- Physical and Mental Consequences
- Infections —Increase in incidences of HIV, hepatitis B and C
- Violence
- Future Use Disorders
_____
Which Drugs are commonly Abused by Teens?
Illegal drugs may seem like the biggest threat to teens, but in fact, teenagers abuse both legal and illegal substances. According to the American Academy of Child & Adolescent Psychiatry, the most commonly abused illegal drugs include:
- Marijuana
- Stimulants like meth and cocaine
- Hallucinogenic drugs like LSD, PCP and Ecstasy
- Heroin and other opiates
The most widely abused legal drugs among adolescents include:
- Alcohol
- Prescription drugs
- Over-the-counter medications, like cough syrup, anti-allergy medications, caffeine pills or laxatives
- Inhalants like solvent, glue or paint fumes
Some of these drugs, like alcohol, heroin, cocaine, marijuana and prescription painkillers, have a higher potential for abuse and addiction than others, but all of these substances are dangerous to developing teens and may lead to destructive, addictive behavior.
____
Steps parents can take to curb teen drug use:
- Talk openly about the dangers of both illegal and prescription drug use with your kids. Providing a safe and open environment to talk about these issues can make a real difference in the likelihood that they’ll use or abuse drugs.
- Lay down rules and consequences. Your teen should understand that using drugs comes with specific consequences. But don’t make hollow threats or set rules that you cannot enforce—and make sure your spouse agrees and is prepared to enforce the rules. Remind your teen that taking someone else’s prescription or sharing theirs with others is illegal.
- Monitor your teen’s activity. Know where your teen goes and who they hang out with. It’s also important to routinely check potential hiding places for drugs—in backpacks, between books on a shelf, in DVD cases or make-up cases. Monitor your teen’s use of the Internet to check for illegal online purchases.
- Keep prescription medicines in a safe place, avoid stockpiling them, and dispose of any unused prescription medicines. Monitor your prescription refills carefully.
- Encourage other interests and social activities. Expose your teen to healthy hobbies and activities, such as team sports and after-school clubs.
- Talk to your child about underlying issues. Drug use can be the result of other problems. Is your teen having trouble fitting in? Has there been a recent major change, like a move or split causing stress?
- Get help. Teenagers often rebel against their parents but if they hear the same information from a different authority figure, they may be more inclined to listen. Try a sports coach, family doctor, therapist, or drug counselor.
_______
College Drug Abuse:
College students make up one of the largest consumer groups of drugs. Open attitudes toward drug abuse, high anxiety during test time, newfound personal freedom, and frequent partying can easily be incentives to try or use substances. The National Library of Medicine National Institutes of Health reports 37% of college students have used an illicit drug (Opioids, Stimulants, Benzodiazepines, Cannabinoids, Barbiturates) and abused alcohol on a regular basis.
College Marijuana Abuse:
Marijuana is frequently misused to relieve college-related stress, at the cost of risking academic progress and school-related responsibilities. The percentage of college students who abuse Marijuana increased from 3.7% in 1999 to 4.6% in 2015 in the U.S. Marijuana is by far the most widely used illicit drug among college students, with 1 in 22 college students using it on a regular basis. Marijuana use is not limited to any specific group of college students. For example, Marijuana use is common in male college lacrosse players according to a NCAA study.
Unique risks come with marijuana in addition to its illegal statuses in some states, including:
- Impaired short-term memory
- Poor motor skills
- Risk of incarceration if used in a state which prohibits use
- Lowered school performance
- Reduced decision making
- Weight gain (extreme hunger called “the munchies” encourages increased appetite after marijuana use)
College Synthetic Marijuana Abuse:
The interest in Marijuana use also puts individuals at risk of exposure to Synthetic Marijuana with dangerous side effects. Also known as Spice or K2, Synthetic Marijuana blends are synthetic chemicals that are legal in the United States but can be extremely harmful. The Synthetic Marijuana is a popular substance among college students who want to feel similar effects to Marijuana, but who don’t want the legal risks. This chemical is easy to obtain and is available in edibles, drinks, or can be smoked. According to some studies, as many as 1 in 10 college students admit to regular Synthetic Marijuana use. However, using Synthetic Marijuana can be very dangerous, possibly even deadly. Side effects include:
- Anxiety
- Heart attacks
- Hallucinations
- Paranoia
- Seizures
- Kidney damage
- High blood pressure
College Stimulant Abuse:
Illegal stimulants like Cocaine and prescription stimulants like Amphetamine are very commonly abused among college students because of the dopamine they cause the brain to release and the added mental focus they can temporarily provide. Stimulants are classes of chemicals that alert the central nervous system to enhance the functions of the brain.
Common symptoms of stimulant abuse are:
- Heightened energy
- Decreased appetite
- Talkativeness
- Nervous excitedness
- Weight loss
- Euphoria
Consequences of College Drug Abuse:
College students who abuse drugs risk poor academic functioning in a time where they are developing skills for the real world. They need the ability to focus while maintaining a healthy lifestyle for success. Drug abuse can render them unsuccessful in college and create:
- Nausea
- Drug tolerances and addiction
- Spending too much money on drugs
- Experimentation with other substances
- Risky behavior
- Aggressive behavior
- Cravings
- Feeling guilt or shame
- Increased substance use
- Accepting attitudes toward drug abuse
Other consequences, like declining health, financial strain, and family fights can impact a student’s life for the long term.
______
Research links Adolescent Substance Use to Adult Brain Volumes:
Researchers found that higher levels of alcohol, cigarette, and marijuana use before age 19 correlated with smaller gray matter volume in two brain areas. The amygdala was smaller in youths who had reported higher use of the substances at ages 12 to 15. The pars opercularis, a subregion of the inferior frontal gyrus, was smaller in those who reported higher use of the substances at ages 16 to 18. The location and timing of the observed associations parallel the staged maturation of the adolescent brain, in which emotional circuits come fully online prior to cognitive circuits. The amygdala is part of the limbic system, which matures earlier and is strongly implicated in emotional responses, especially fear. The pars opercularis is part of a forebrain circuit that matures later and supports the ability to refrain from impulsive behaviors. Less gray matter in an area may indicate that it contains fewer neurons, which suggests a reduced capacity to shape behavior. Dr. Windle and colleagues say that relatively low gray matter volume in the two areas may be a contributing cause or an effect of substance use, depending on whether it was already present before the adolescents used the substances, in which case it may have rendered them more likely to become users or continue using after an initial exposure; or came about because the drugs inhibited the developmental expansion of gray matter volume in the affected areas. Both etiologies might also pertain. To resolve the issue, researchers will need to conduct a longitudinal study in which they obtain brain images before adolescence, collect substance use data throughout adolescence, and obtain follow-up images after adolescence.
______
Effects of marijuana on the adolescent brain:
While several studies have compared the effects of marijuana use on brain structure and function in smokers versus nonsmokers, few have looked at whether the age at which a person starts smoking cannabis comes into play. Staci Gruber (McLean Hospital, Harvard Medical School) investigated whether the age of onset of marijuana use affects neurocognitive performance, brain function, and brain structure. In fMRI studies, late‐onset smokers had activation patterns that were more similar to control, nonsmokers than to early‐onset smokers. Adolescents who began smoking earlier (before 16 years of age) smoked nearly twice as often and more than 2.5 times as much as those who began smoking later. Earlier age of onset was also associated with poorer performance on measures of executive function than late age of onset.
Marijuana users also exhibit differences from controls in brain volume, mass, and shape. There are regional differences in cerebral cortical thickness compared with nonusers and differences in density and in gyrification, a measure of the folding of the cortex in the gray matter that has been related to poor performance on attentional tasks. Among early‐onset smokers, significant reductions in white matter integrity have been observed by diffusion tensor imaging compared with images from late‐onset smokers and nonsmokers. This difference in white matter integrity was associated with higher self‐reported impulsivity among early‐onset smokers, but not among late‐onset smokers or nonsmoking controls, although the causality of this relationship is not fully understood.
Susan Weiss noted both the importance of determining the effects of marijuana on the developing brain, given its increasing prevalence and availability to adolescents, and the lack of consistency in the field. For example, a large longitudinal study in New Zealand reported that persistent cannabis use was associated with a decline in IQ; however, twin studies failed to observe this connection. Studies of the effects of marijuana on brain structure are also mixed. Gaps in knowledge include whether the effects of marijuana are reversible with abstinence; how varying doses, strains, and potency of cannabis affect outcomes; whether there are gender‐specific effects; and how the age of onset influences cannabis effects.
______
Adolescent Brain Cognitive Development (ABCD) study:
The adolescent brain is highly susceptible to being altered by experiences like substance use. However, there is much we have yet to learn about how these experiences influence brain development, how they promote or interfere with later health outcomes, or even what healthy brain development looks like. A large longitudinal study beginning in early adolescence could help us understand the normal variability in adolescent brain and cognitive development and tease apart the many factors that influence it. Recent advances in neuroimaging, informatics, and genetics technologies have made it feasible to conduct a study of sufficient size and scope to answer many outstanding questions. At the same time, several Institutes across the NIH recognized the value of collaborating in such a project because of its ability to address the role of biological, environmental, and behavioral factors like gender, pubertal hormones, sports participation, and social/economic disparities on brain development as well as their association with the emergence and progression of substance use and mental illness including suicide risk. Thus, the Adolescent Brain Cognitive Development (ABCD) study was created to answer the most pressing public health questions of our day.
Substance use does not exist in a vacuum; it is entwined with mental and physical health and with our social systems in myriad complex ways, as is neurodevelopment. Thus, even as the ABCD study was being conceived, the CRAN Institute Directors realized that it would have to address a wide range of questions about genetic influences and environmental exposures on neurodevelopment during the second decade of life. Other Institutes, Centers, and Offices across the NIH similarly recognized the value of the proposed cohort for addressing pressing questions in their own priority areas. Answers to these questions could inform policies and practices to improve public health in a variety of ways (see table below).
_
The ABCD study is a collaborative trans-NIH venture, bringing together a wide range of scientific research agendas and expertise, to answer some of the most pressing public health questions of our day. The collaboration continues to expand, with involvement now of the NIH Office of Research on Women’s Health, the Centers for Disease Control and Prevention-Division of Adolescent and School Health, and the National Institute of Justice. The study will yield important insights into mechanisms and causal relationships that have previously proved elusive, inform the development of new prevention and treatment strategies, and give rise to new research areas we cannot yet anticipate. The massive data resource ABCD will create will be utilized by the entire scientific community for decades to come; the study will release curated, anonymized data annually to the research community (along with the computational workflows used to produce the data), which will allow scientists from all over the world to conduct analyses, pool resources, and find the answers to unforeseen questions about adolescent brain development and factors that interact with it. And in addition to data about perturbed developmental trajectories, ABCD will also generate valuable benchmarks for normal structural and functional neurodevelopment during the transition from childhood into young adulthood, a lasting contribution to medicine. ABCD will thus inform not only mental health and substance use researchers but also educators, parents, physicians, and policymakers—everyone with a stake in the health of our nation’s youth.
_______
MRI brain scans may help identify risks, prevent adolescent substance abuse: a 2017 study:
Neuroimaging of the brain using technologies such as magnetic resonance imaging, or MRIs, increasingly is showing promise as a technique to predict adolescent vulnerability to substance abuse disorders, researchers conclude in a new analysis. The findings are of importance, researchers say, because underage alcohol and drug use is increasingly being recognized as a public health and social problem, with long-term consequences that include poorer academic performance, neurocognitive deficits and psychosocial problems. Youth who begin drinking before age 15 have four to six times the rate of lifetime alcohol dependence than those who do not drink by age 21, researchers noted in this analysis, which was recently published in Current Opinion in Behavioral Sciences.
Structural and neural alterations in the brain from drug and alcohol abuse have now been well established. It’s also becoming clear that some of these alterations can exist before any substance abuse, and often are found in youth who have a family history of alcohol and drug use disorders. These familial risk factors can play a role in future substance abuse, along with environmental risk factors such as peer influence, personality and psychosocial interactions. Family history of alcohol-use disorder is a strong predictor of substance abuse, as it raises the risk for the development of alcohol-use disorder in adolescents by three to five times. Neuroimaging studies show significant overlap in brain scans between those with a family history of alcohol- and substance-use disorders and youth who begin using substances during adolescence.
Some of the findings in youth with family history of alcohol- and substance-use disorder include a smaller volume of limbic brain regions, sex-specific patterns of hippocampal volume, and a positive association of familial risk with “nucleus accumbens” volume in the brain. Other risk factors for adolescent substance use that have been identified include poorer performance on executive functioning tasks of inhibition and working memory, smaller brain volumes in reward and cognitive control regions, and heightened response to rewards.
______
______
Drug addiction in pregnant women:
Here are some of the most common reasons for drug addiction during pregnancy:
- Age
Perhaps the biggest reason for substance abuse during pregnancy is that a woman’s reproductive years (age 15 to 44) coincide with a time in life when a person is most likely to seek out new experiences and begin abusing drugs. Adolescents and young adults are biologically wired to take risks and experiment with tobacco, alcohol, prescription pills, and illicit drugs. This puts women of childbearing age at an increased risk of addiction. Studies show that pregnant teens are more likely to abuse drugs compared to older women.
- Unplanned pregnancy
About 45 percent of pregnancies in the United States are unintended or mistimed, meaning either the pregnancy was not desired or it occurred earlier than desired. Unplanned pregnancies are a risk factor for exposure to drugs and alcohol due to a late recognition of pregnancy and delayed access to antenatal care. When a pregnancy is unplanned, the woman may continue risky consumption of alcohol and drugs without realizing she is carrying a baby.
- Prescription medicines
Some of the drugs that may be prescribed during pregnancy, such as benzodiazepines (sleeping pills), are highly addictive. In addition, prenatal exposure to benzos such as diazepam is associated with birth defects including facial clefts and cardiac malformations. In pregnant women, treatment with any medication needs to be carefully monitored to ensure the mother does not become dependent and no harm is caused to the baby.
- Inability to quit
Most women want to do what’s best for their baby. They realize that quitting tobacco, alcohol, or drugs is an important step towards a healthy birth. Yet, changing behaviors is not easy. Not all women are able to stop smoking, drinking, or using drugs when they find out they are expecting. Women who are daily smokers, heavy drinkers, and long-term drug abusers find it the hardest to quit. In fact, studies show that only 1 in 3 women who smoked before pregnancy is able to quit in the prenatal period. Abstinence rates for alcohol and illicit drugs are slightly more encouraging, but relapse rates in the postpartum period remain high.
- Underestimation of risk
Any chemical that enters a pregnant woman’s body, whether it is prescribed by a physician or used illegally for recreational purposes, can harm the fetus. However, not every woman who is expecting understands the risks of tobacco, alcohol, and drug abuse for herself and her baby. Some women are under the false impression that light drinking is okay, believing that only binge drinking is harmful to the baby. According to the CDC, no type or amount of alcohol is safe for pregnant women.
- Fear of consequences
It is mandatory for obstetricians to report substance abuse in pregnant women. Many expectant mothers are aware of the risks of drugs and alcohol but avoid seeking treatment for their addiction because they are afraid of the legal ramifications. Some women fear they will be judged and criticized by friends, family, and healthcare providers. Some women are afraid they may lose custody of their children or be evicted from their home if their addiction is discovered. The threat of institutionalization or incarceration keeps many pregnant women from seeking treatment for substance abuse.
- Postpartum depression
Pregnancy and the birth of a child is associated with many biological and lifestyle changes for a woman. Many women struggle to cope with and adapt to the new phase of their lives and suffer from depression as a result. Postpartum depression, commonly known as baby blues, affects an estimated 15 percent of new mothers. Feelings of anxiety, sadness, and exhaustion make it difficult for the mother to care for herself and her baby. Studies show that women with postpartum depression are at a high risk of substance abuse. In fact, substance abuse and depression are risks for each other and both have a substantial negative impact on maternal and infant health.
_
Statistics of drug addiction in pregnancy:
Substance use disorders are most prevalent in adolescents and young adults. This puts women of childbearing age (15 to 44 years old) at greatest risk of developing an addiction. Based on this demographic, women who are pregnant or could soon become pregnant are at high risk of substance abuse. In fact, according to a nationwide survey in U.S. on drug use in 2012, almost 16 percent of pregnant women smoked cigarettes, 8.5 percent drank alcoholic beverages, and nearly 6 percent used illicit drugs. According to the Substance Abuse and Mental Health Services Administration (SAMHSA), 5.4 percent of pregnant women between ages 15 and 44 are current users of illicit drugs. In pregnant teens (age 15 to 17), the rate of drug abuse is much higher at almost 15 percent. Tobacco use is also prevalent during pregnancy and 1 in 14 pregnant women smokes cigarettes. One study found nearly 9 percent of women in the age group of 20 to 29 years reported recent use of ecstasy. It is evident that substance use disorders are rampant during pregnancy. One study found that about 20% of pregnant women 24-years-old and younger screened positive for marijuana. However, this study also found that women were about twice as likely to screen positive for marijuana use via a drug test than they state in self-reported measures. This suggests that self-reported rates of marijuana use in pregnant females may not be an accurate measure of marijuana use. Another study found that substance abuse during pregnancy is more prevalent than commonly realized, with up to 25% of gravidas using illicit drugs. In fact, substance abuse is more common among women of reproductive age than among the general population. There is little information available on the extent of substance use, other than tobacco, among pregnant women in low-income and middle-income countries.
_
Caffeine during pregnancy:
Caffeine is a stimulant and is present in tea, coffee, sodas, energy drinks, and some headache medications, in varying amounts. The data on maternal caffeine consumption during pregnancy and fetal safety is conflicting. What we do know is that pregnant women metabolize caffeine slower than non-pregnant women and caffeine is transmitted across the placenta from the mother to the baby. Studies suggest that one to two cups of coffee a day are safe, but intake of more than 300 mg per day may be associated with adverse outcomes such as spontaneous abortion, growth restriction, congenital malformations, and stillbirth. A typical 8-ounce serving of coffee has about 135 mg of caffeine. Another study found that a 100 mg dose of caffeine per day from all sources during pregnancy is associated with an elevated risk of miscarriage. Research shows that high caffeine intake is associated with impaired fetal growth and low birth weight. There is a linear increase in risk. For every additional 100 mg of caffeine (1 cup of coffee or 2 cups of tea) per day, there is a 3 percent increase in low birth weight. Pregnant women who drink more than 8 cups of coffee a day are at increased risk of stillbirth. Fetal exposure to moderate to high levels of caffeine has been linked to childhood obesity.
_
Maternal drug addiction harm to Growing Baby:
It is well known that there are several serious health consequences for the developing fetus from maternal substance abuse. Some of the most common prenatal effects of various drugs include miscarriage, preterm labor, low birth weight, and a number of developmental problems and birth defects. Pregnant women with addictions is a high-risk group that requires intensive obstetric and neonatal care.
_
Illicit drug use by pregnant women can cause serious health problems for the unborn baby. Here is a list of some illicit drugs and the effects they can have on a fetus:
- Amphetamines: The use of these drugs has been linked to heart defects in babies born to women who used them. These drugs taken during pregnancy may increase the risk of placental problems as well as miscarriage and preterm birth. These babies may also be of low birth weight. Amphetamines are often sold as a street drug, but the main ingredient in amphetamines can be found in many over-the-counter diet pills.
- Cocaine: Cocaine use can cause contractions of the uterus, which might lead to bleeding complications or premature labor. Cocaine can cause stillbirth, miscarriage, preterm birth, growth retardation, and birth defects in babies.
- Marijuana: Women who smoke marijuana during their pregnancies might have babies with problems, including impaired fetal growth. Marijuana increases the risk of having a miscarriage, preterm birth, a baby with low birth weight, developmental delays, and even learning problems. These smaller babies are more likely to have health problems than are babies born to women who did not use marijuana. Some women report using marijuana to treat severe nausea associated with their pregnancy; however, there is no research confirming that this is a safe practice, and it is generally not recommended. Women considering using medical marijuana while pregnant should not do so without checking with their health care providers. Animal studies have shown that moderate concentrations of THC, when administered to mothers while pregnant or nursing, could have long-lasting effects on the child, including increasing stress responsivity and abnormal patterns of social interactions. Animal studies also show learning deficits in prenatally exposed individuals. Human research has shown that some babies born to women who used marijuana during their pregnancies display altered responses to visual stimuli, increased trembling, and a high-pitched cry, which could indicate problems with neurological development. In school, marijuana-exposed children are more likely to show gaps in problem-solving skills, memory, and the ability to remain attentive.
- Narcotics: Drugs such as heroin can cause growth problems, premature labor, and a fetal syndrome of narcotic withdrawal after birth. In addition, sudden infant death syndrome (SIDS) is more likely among babies whose mothers used narcotics during pregnancy.
- Tranquilizers: Tranquilizers including Valium have been associated with birth defects. Mothers who engage in heavy use during pregnancy can also have babies who undergo withdrawal symptoms after birth.
- Glues and solvents: Women who sniff fumes during pregnancy may suffer a miscarriage or preterm labor and birth. They can have babies with birth defects including low weight, short height, joint and limb problems, heart defects, and abnormal facial features.
- Ecstasy: Pregnant women who use this drug might have babies with long-term learning and memory problems.
_
Neonatal Abstinence Syndrome (NAS):
A baby who has been exposed to an illicit substance during fetal life because the mother was regularly using it can be born with a dependence on the substance. This is known as neonatal abstinence syndrome. Maternal abuse of drugs such as opioids (for example, oxycodone, codeine), heroin, and methadone can cause NAS in a newborn infant. It can also be caused by exposure to alcohol, benzodiazepines (sleeping pills), and antidepressants (SSRIs) in the womb. Babies who receive one or more of these drugs before delivery from their mothers are born with a dependence on the drugs. After birth, when they no longer get the drugs, it results in a postnatal withdrawal syndrome.
During the period 2000-2012, the incidence of NAS in the United States increased by 383 percent. In 2013, there were 6 cases of NAS reported per 1,000 births, up from 1.5 in 1999. Treatment for NAS often requires pharmacological intervention with medications such as methadone and morphine in up to 70 percent of infants. The treatment protocol can extend for several weeks, depending on the severity of the withdrawal, which in turn depends on the duration of in utero drug exposure.
_
Many women are aware of the risks of alcohol and drugs during pregnancy and want to quit but are unable to do so on their own. Some pregnant drug and alcohol abusers avoid seeking addiction treatment for fear of legal issues. Expectant mothers fear there will be consequences regarding custody of other children or other legal ramifications. Social stigma and the fear of being criticized and judged by healthcare providers, friends, and family also prevents some pregnant women from going to drug rehab.
According to the American College of Obstetrics and Gynecology (ACOG), the threat of incarceration prevents many women from seeking prenatal care and this is ineffective in reducing drug and alcohol abuse in expectant mothers. There is no specific criminal law for drug abuse during pregnancy, but in some states, substance use during pregnancy is equivalent to child abuse. Laws mandate obstetricians report substance abuse in their patients. Pregnant drug abusers may be persecuted for child neglect, endangerment, mistreatment, and abuse. Legally mandated drug testing and reporting and fear of legal consequences, such as incarceration, commitment, loss of child custody, and loss of housing, leads many pregnant drug abusers to disengage from even routine prenatal care, putting themselves and their babies at considerable risk.
Studies have found that medication-assisted treatment with methadone therapy for opioid-addicted pregnant women is associated with reduced fetal morbidity, improved maternal health, and better utilization of prenatal care. Treatment for substance abuse during pregnancy is significantly more effective than at other times in a woman’s life. Pregnancy may be a window of opportunity to intervene for substance abuse problems (Weiner and Larsson 1987). It may be the first time that a woman has sought medical care (Woods 1993). Denial—a concern whenever questions are asked about substance abuse—may be less common during pregnancy. Pregnant women as a group are invested in the health of their babies and can no longer deny that their alcohol or drug abuse is hurting anyone but themselves. Women in recovery have reported that they wanted help during pregnancy but didn’t know how to ask (McElaney 1991). Pregnant women report that they consider health care providers one of their best sources of information, and are likely to comply with advice given (Minor and Van Dort 1982). This makes the prenatal setting the ideal place for discussion of substance abuse.
_
Breastfeeding and postpartum substance use:
Breastfeeding has the potential to be a useful tool for substance use in the postpartum period. Breastfeeding is the only available intervention shown to reduce NAS severity in opioid-exposed newborns. Breastfeeding might also be protective for postpartum relapse. For example, among breastfeeding smokers, 10% stop breastfeeding because of smoking, and over half of recent or current smokers reported that smoking affected their infant feeding decision. In addition, non-current smokers are more likely to initiate and continue breastfeeding compared to current smokers. Therefore, the promotion of breastfeeding might prevent or delay postpartum relapse.
While studies evaluating the potential role of breastfeeding as an intervention for substance use postpartum are limited, the rationale for such interventions is clear. Lactation reduces the HPA response to physical stress. A behavior that promotes relaxation and reduces stress would be helpful to women with substance use disorders since psychosocial stress increases cravings. While hormones released during lactation may mediate stress reduction, such hormones have other properties that may help women cope with addiction. Considerable attention has been dedicated to oxytocin, a hormone released during delivery and lactation. Oxytocin administration is under investigation for treatment of drug and alcohol use disorders. In addition, lactation is positively associated with cognitive and motor development in the infant. It is well known that stable attachment among children increases resiliency and protects against the development of addiction later in life. Thus, an intervention that promotes lactation and intimacy through skin-to-skin contact may enhance stable attachment, and have the intergenerational benefit of protecting offspring from the development of addictive and other problematic behaviors.
On the other hand, woman who abuse drugs while breastfeeding creates problems for baby. One study suggests that moderate amounts of THC find their way into breast milk when a nursing mother uses marijuana. Some evidence shows that exposure to THC through breast milk in the first month of life could result in decreased motor development at 1 year of age.
_______
_______
Drug addiction in LGBT (lesbian, gay, bisexual, and transgender) community:
According to 2015 data from the National Survey on Drug Use and Health, adults defined as “sexual minority” (in this survey, meaning lesbian, gay, or bisexual) were more than twice as likely as heterosexual adults (39.1 percent versus 17.1 percent) to have used any illicit drug in the past year. Nearly a third of sexual minority adults (30.7 percent) used marijuana in the past year, compared to 12.9 percent of heterosexual adults, and about 1 in 10 (10.4 percent) misused prescription pain relievers, compared to 4.5 percent of heterosexual adults. Both cross-sectional and longitudinal studies have shown that sexual minority youth (e.g., those who identify as lesbian, gay or bisexual or experience same-sex attractions and/or relationships) are more likely to use drugs than heterosexual youth (Corliss et al., 2010; Garofalo et al., 1998; Marshal et al., 2008; Russell et al., 2002). A meta-analysis found that the odds of substance use among sexual minority youth are nearly twice that of heterosexual youth (Marshal et al., 2008). Furthermore, sexual minority youth were 1.56 times more likely to report past 30-day marijuana use, and were 2.58 times more likely to report lifetime marijuana use, compared to their heterosexual peers (Marshal et al., 2008).
An Institute of Medicine (2011) report on sexual minority health disparities noted that the reasons for higher levels of substance use, including marijuana use, among sexual minority youth are largely unknown. However, the stigma related to sexual orientation is frequently cited as a risk factor for health disparities between sexual minority and heterosexual populations. Several studies have documented associations between various stigma-related stressors and substance use among sexual minority youth (Coker et al., 2010), including gay-related stressful life events (e.g., identity disclosure; Rosario et al., 1996), victimization at school (Bontempo and D’Augelli, 2002), and verbal/physical abuse (Savin-Williams, 1994).
______
______
Dual diagnosis:
The combination of mental illness and substance use disorder is often called “concurrent disorders” or “co-occurring disorders”, and in the United States, “dual diagnosis”. It might surprise you to learn that mental health issues and substance abuse often occur together. When this happens, these are called co-occurring disorders. Occasionally, substance abuse can lead to a mental health problem. However, this is usually a rarer situation. More often than not the mental health condition appears first. If you’ve never had a mental illness (such as bipolar disorder, anxiety or depression), then it’s difficult for you to understand the emotional and often physical pain it can cause. Many people use drugs and alcohol in an attempt to help themselves feel better because it actually relieves some of the pain they experience due to their mental illnesses. There are a lot of examples of how people use drugs and alcohol to cope with mental illnesses. Some of these might include:
- A veteran who uses drugs to deal with symptoms of PTSD
- A young person who drinks to avoid feeling stressed out or anxious
- A college student who uses stimulant drugs to deal with depression
- An overwhelmed mom who uses drugs to help with bipolar disorder symptoms
- A teenager who smokes marijuana to help with symptoms of an eating disorder
What’s really concerning is the fact that mental illnesses so often go undiagnosed. Someone can be living with anxiety or depression for years without knowing that they have them. The best way to treat co-occurring disorders is to do so together. In the past, people with these conditions would be treated for them separately. This was found to be ineffective. After going to drug detox, those individuals can actually choose a good drug detox facility that addresses both issues at the same time.
_
Drug addiction is more common among people with mental disorders than among the general population. For example, people with mental disorders are more likely to be alcohol dependent at some stage in their lives than people without a mental illness. Conversely, drug-dependent people are more likely to suffer from mental disorders than non-dependent people. For instance, people who are dependent on alcohol, tobacco, or cocaine are more likely to suffer from depression than non-dependent people. This indicates either a common basis for both afflictions, or an interaction of effects at some level. Drug use may either bring about mental illness, or it may be a way of easing some of the symptoms of a mental disorder or the side effects of medication. Also, since many drugs produce effects typical of some mental illnesses, drug dependence and mental illness may have the same neurobiological causes. To make the situation more complicated, the co-occurring disorders also affect each other. When a mental health problem goes untreated, the substance abuse problem usually gets worse. And when alcohol or drug abuse increases, mental health problems usually increase too.
_
Co-occurring substance abuse problems and mental health issues are more common than many people realize.
According to reports published in the Journal of the American Medical Association:
- Roughly 50 percent of individuals with severe mental disorders are affected by substance abuse.
- 37 percent of alcohol abusers and 53 percent of drug abusers also have at least one serious mental illness.
- Of all people diagnosed as mentally ill, 29 percent abuse either alcohol or drugs.
_
Psychedelics and mental illnesses in long-term users:
Most psychedelics are not known to have long-term physical toxicity. However, entactogens such as MDMA that release neurotransmitters may stimulate increased formation of free radicals possibly formed from neurotransmitters released from the synaptic vesicle. Free radicals are associated with cell damage in other contexts, and have been suggested to be involved in many types of mental conditions including Parkinson’s disease, senility, schizophrenia, and Alzheimer’s. Research on this question has not reached a firm conclusion. The same concerns do not apply to psychedelics that do not release neurotransmitters, such as LSD, nor to dissociatives or deliriants. No clear connection has been made between psychedelic drugs and organic brain damage. However, hallucinogen persisting perception disorder (HPPD) is a diagnosed condition wherein certain visual effects of drugs persist for a long time, sometimes permanently, although science and medicine have yet to determine what causes the condition. A large epidemiological study in the U.S. found that other than personality disorders and other substance use disorders, lifetime hallucinogen use was not associated with other mental disorders, and that risk of developing a hallucinogen use disorder was very low.
_
Link between marijuana use and psychiatric disorders:
Several studies have linked marijuana use to increased risk for psychiatric disorders, including psychosis (schizophrenia), depression, anxiety, and substance use disorders, but whether and to what extent it actually causes these conditions is not always easy to determine. The amount of drug used, the age at first use, and genetic vulnerability have all been shown to influence this relationship. The strongest evidence to date concerns links between marijuana use and substance use disorders and between marijuana use and psychiatric disorders in those with a preexisting genetic or other vulnerability.
Recent research has found that people who use marijuana and carry a specific variant of the AKT1 gene, which codes for an enzyme that affects dopamine signaling in the striatum, are at increased risk of developing psychosis. The striatum is an area of the brain that becomes activated and flooded with dopamine when certain stimuli are present. One study found that the risk of psychosis among those with this variant was seven times higher for those who used marijuana daily compared with those who used it infrequently or used none at all. Another study found an increased risk of psychosis among adults who had used marijuana in adolescence and also carried a specific variant of the gene for catechol-O-methyltransferase (COMT), an enzyme that degrades neurotransmitters such as dopamine and norepinephrine. Marijuana use has also been shown to worsen the course of illness in patients who already have schizophrenia. Marijuana can produce an acute psychotic reaction in non-schizophrenic people who use marijuana, especially at high doses, although this fades as the drug wears off.
_
Schizophrenia & substance use:
At some point in their lives, many people with schizophrenia abuse substances (street drugs, over-the-counter drugs and /or alcohol). Recent studies have shown that about half of all people with schizophrenia also have problems with drugs and alcohol, and up to 90% of people with schizophrenia are addicted to nicotine. People living with schizophrenia and other psychotic disorders tend to use substances that are affordable, easily accessible and readily available, such as alcohol, cannabis and nicotine. Prescription drugs like tranquilizers and sleep medication may also be misused. Research has shown that people with schizophrenia and other mental disorders often use drugs and alcohol for the same reasons as everyone else – to feel better or different, to relax and have fun, and to be part of a group. Other reasons for drug use include curiosity or experimentation, to relieve stress, to overcome boredom, and to cope with symptoms of mental illness.
_
Depression and substance use:
Depression is a mental illness frequently co-occurring with substance use. The relationship between the two disorders is bi-directional, meaning that people who abuse substances are more likely to suffer from depression, and vice versa. People who are depressed may drink or abuse drugs to lift their mood or escape from feelings of guilt or despair. But substances like alcohol, which is a depressant, can increase feelings of sadness or fatigue. Conversely, people can experience depression after the effects of drugs wear off or as they struggle to cope with how the addiction has impacted their life. Roughly one-third of adults who have a substance use disorder also suffer from depression. Among individuals with recurring major depression, roughly 16.5 percent have an alcohol use disorder and 18 percent have a drug use disorder. Because drug use symptoms can imitate the symptoms of depression, it can be difficult to diagnose depression when a person is actively using. Depression can look different depending on the person experiencing the disorder.
______
______
Drug addiction in Street children:
According to UNICEF, 100 million children live and work on the streets of the cities of the world: 40 million in Latin America, 25-30 million in Asia, and 10 million in Africa. India has the largest number of street children in the world. Though, India is largely still rural, urbanization is taking place rapidly, leading to fast growth of slums and shanty towns. All these factors have resulted in an explosion of street children in the country. 18 million children lived and worked in India’s slums qualifying to be the street children. According to WHO estimates, up to 90% of the world’s street children abuse some kind of drugs. Street children in many developing countries are a high risk group for substance misuse, in particular solvent abuse. Drawing on research in Kenya, Cottrell-Boyce argues that “drug use amongst street children is primarily functional – dulling the senses against the hardships of life on the street – but can also provide a link to the support structure of the ‘street family’ peer group as a potent symbol of shared experience.” Various studies show that 90 % of the Delhi street children are addicted to drugs.
_____
Drug addiction in Musicians:
In order to maintain high-quality performance, some musicians take chemical substances. Some musicians take drugs or alcohol to deal with the stress of performing. As a group they have a higher rate of substance abuse. The most common chemical substance which is abused by pop musicians is cocaine, because of its neurological effects. Stimulants like cocaine increase alertness and cause feelings of euphoria, and can therefore make the performer feel as though they in some ways ‘own the stage’. One way in which substance abuse is harmful for a performer (musicians especially) is if the substance being abused is inhaled. The lungs are an important organ used by singers, and addiction to cigarettes may seriously harm the quality of their performance.
_____
Drug addiction in physicians:
Drug availability and occupational stress help explain why physicians have the highest rate of opiate addiction of any group. Physicians have high rates of abuse of alcohol and mood-altering prescription drugs. Charles Winick, a sociologist at the City College of New York, has linked availability and stress to high rates of drug dependence among physicians, particularly psychiatrists and surgeons.
_____
Drug addiction in Legal Professionals:
More recently, attorneys and other legal professionals have been identified as a high-risk group for substance use disorders. In large-scale national survey studies of professionals, individuals in legal professions have reported higher rates of problematic drinking behaviors when compared to other populations. A recent survey of legal professionals indicated that 36.4% of respondents had scores on the Alcohol Use Disorders Identification Test, version C (AUDIT-C), consistent with problematic drinking; in comparison, AUDIT-C scores consistent with problematic drinking have been self-reported by only 15.4% of surgeons. Legal professionals have also reported or presented personality characteristics and personality disorders that may be linked to greater propensity for substance use disorders. A 2008 study of personality profiles among attorneys found that antisocial and narcissistic personality configurations (as measured by the Millon Clinical Multiaxial Inventory-III; MCMI-III) were present among 17.6% and 11.7% of attorneys in the sample (respectively), as compared to a national epidemiological survey that estimated antisocial and narcissistic personality disorders among 3.2% and 6.2% of the population (respectively). Both antisocial personality disorder and narcissistic personality disorder are significantly correlated with addiction and substance use disorders. Given the unique factors of the legal profession that can involve increased alcohol consumption as part of professional networking and socializing, as well as high levels of stigma associated with the professional and political costs of seeking treatment, there has been an increased focus on the provision of treatment services specific to legal professionals.
_____
Drug addiction in sports:
There has been a worldwide increase in the use of recreational or social drugs, creating management problems for sports governing bodies and their medical advisers. These recreational drugs are addictive in nature but their consumption has nothing to do with performance enhancement or “cheating”. In sports in which safety of the participants is a major issue, such as horse racing, motor racing, and motor cycle racing, the governing bodies are appropriately more concerned about any impairment of performance that could put the participant, and other competitors, at risk. In this context, there is a good case to include all the recreational drugs listed as prohibited substances by governing bodies of high speed/high risk sports (including alcohol at an agreed threshold).
The IOC first introduced the monitoring of cannabinoids in the1980s, justifying their action on the basis that sports personalities were role models and that the use of marijuana brought sport into disrepute. This was slightly different from their approach to alcohol, which was only screened at the request of the governing body when athlete safety was an issue. Individual sporting bodies have therefore had the option of whether to include cannabis and alcohol on their banned list. A sport in which both alcohol and cannabis are banned is skiing; originally their use was prohibited in the high-risk disciplines ski jumping, downhill racing, and freestyle aerials.
A variety of recreational drugs are commonly used in society and have the potential for abuse by sportsmen and women. They include:
- IOC banned drugs:
Stimulants:
-Amphetamines (including methamphetamine)
-Cocaine
-MDMA, MDA and MDEA (ecstasy-like drugs)
Narcotic analgesics:
-Opiates (heroin, morphine, pethidine)
- IOC monitored (not generally prohibited) drugs:
-Cannabinoids
-Alcohol
- Substances that are not screened at all by the IOC:
-LSD (lysergic acid diethylamide)
-PCP (phencyclidine)
-Ketamine
-Tiletamine
-Gamma hydroxybutyrate
______
Drug addiction in disabled:
People with physical disabilities experience substance use disorders at 2 to 4 times the rate of the general population. A disability and lack of support can easily discourage someone’s happiness and sense of purpose in life, creating depressing states. Co-occurring disorders, like depression, anxiety, and unhealed trauma, are especially common among disabled, leading many to seek a false sense of comfort with harmful substances. Individuals with mental and physical disabilities battle unique stressors, such as social perspectives of seeing them as outsiders, an inability to qualify for certain careers, access to certain benefits, and an inability to participate in a number of activities to the extent they would like. Individuals with disabilities are more likely to be unemployed; disabled adults 25 and older are less likely to have completed high school and more likely to live in poverty. They are more likely to be victims of violent crimes and suffer health conditions like obesity and smoking. All of these factors contribute to high rates of substance use seen in the disabled community. In the United States, 54 million people experience some form of a disability, of which roughly 9% (a total of 4.7 million adults) have both a substance use disorder and a co-existing disability.
Patients with disabilities often use prescription medications to battle painful conditions, many of which have high potential for addiction. Prescription opioids in particular are effective pain relievers, yet are highly addictive and can easily be abused. People with disabilities are more likely to abuse opioids, but less likely to get the treatment they deserve. Opioids are so highly addictive that even individuals that closely follow short-term prescriptions can quickly get hooked, a risk that only goes up the longer the prescription is for. Once a disabled individual develops an addiction to prescription opioids, they will often end up switching over to cheaper and more readily available drugs such as heroin when their prescription runs out. This risk is heightened among the disabled, who are often under greater mobility and financial restrictions than the general population. These factors, combined with the fact that opioid addiction is by far the most likely form of addiction to end in overdose and death, make disability and addiction to opioids a growing cause for concern.
_______
_______
Is drug addiction a disease or choice?
Many people don’t understand why or how other people become addicted to drugs. They may mistakenly think that those who use drugs lack moral principles or willpower and that they could stop their drug use simply by choosing to. In reality, drug addiction is a complex disease, and quitting usually takes more than good intentions or a strong will. Drugs change the brain in ways that make quitting hard, even for those who want to. In the past, addiction was viewed as stemming from an individual’s moral failing and weakness of will (NIH, 2010). With the advances in scientific research, biological theories of addiction as a “brain disease” are now widely accepted; however, this point of view is still controversial. Many prefer to characterize it as a condition that requires continued management, rather than a disease, as it promotes the idea that addiction can be managed through behavioral changes and that the individual is ultimately in control of the condition.
_
The disease model is supported by the changes that occur in the brain as a result of continued substance use. Through a process of adaptation, the brain attempts to adapt to the presence of a substance in effort to function normally. The disease model asserts that while initial choice to use the substance may have been voluntary, over time behavioral choice is lessened as these neurobiological changes occur.
Not only do these changes modify one’s initial response to a substance, they regulate:
- The development of craving.
- The distress associated with periods of abstinence (which is a key factor in relapse).
_
Role of brain in addiction (vide supra):
In the healthy brain, dopamine is released in response to natural rewards, such as food or exercise, as a way of saying, “that was good.” But drugs hijack dopamine pathways, teaching the brain that drugs are good, too. For example, some drugs have a structure similar to other chemical messengers in the brain, allowing them to bind to brain cells and release dopamine. Therefore, taking a drug produces a euphoric feeling, which in turn strongly reinforces drug-using behavior. Drugs release two to 10 times the amount of dopamine that natural rewards release. How much is released depends on the type of drug; amphetamines, for example, release more dopamine than cocaine. As a result, the increased and sometimes constant influx of dopamine means feelings of reward, motivation or pleasure are also increased. But if substance use continues, the brain produces less dopamine and/or reduces the number of brain structures that receive dopamine. Thus, dopamine’s impact on the reward network diminishes, along with the individual’s ability to experience pleasure. This explains why individuals who chronically abuse drugs or alcohol begin to appear lethargic, unmotivated and depressed, and report a lack of pleasure in things that were once pleasurable. To counter this, they increase their substance use in an attempt to feel the same pleasure they used to. This only exacerbates the problem, creating a vicious cycle of needing to take the drug in order to regain dopamine levels, then later needing to increase the dose, and so on, an effect known as tolerance. While short-term use may only produce small, transient effects in the brain, prolonged substance use changes the brain in fundamental ways that reinforce continued use, such as the strengthening of memory circuits associated with drug taking. Cues that are social (such as being around substance-using friends), geographic (former favorite bars), and physical (experiencing stress) in nature become strongly associated with the drug. These have a powerful impact on the brain — no matter if that person has been abstinent for 15 days or 15 years — and can trigger a relapse. Brain changes from chronic drug or alcohol use can persist years after a person quits. This is why individuals risk relapse even after long periods of abstinence, and despite a relapse’s potentially devastating effects. More importantly, this is why treatment depends on the type of drug and the individual characteristics of the patient. Understanding the brain’s role in addiction can help reduce negative perceptions and attitudes of those struggling with substance use disorders.
_
The National Institute on Drug Abuse (NIDA), the Substance Abuse and Mental Health Services Administration (SAMHSA), and the National Institutes of Health (NIH) all similarly describe addiction as a long-term and relapsing condition characterized by the individual compulsively seeking and using drugs despite adverse consequences.
These organizations call addiction a disorder or a disease because:
- Addiction changes how the brain responds in situations involving rewards, stress, and self-control.
- These changes are long-term and can persist well after the person has stopped using drugs.
Comparing substance addiction to heart disease may help illustrate why it is defined as a disease by so many:
- Both addiction and heart disease disturb the regular functioning of an organ in the body – the heart for heart disease and the brain for addiction.
- They both can lead to a decreased quality of life and increased risk of premature death.
- Addiction and many types of heart disease are largely preventable by engaging in a healthy lifestyle and avoiding poor choices.
- They are both treatable to prevent further damage.
Furthermore, since addiction is marked by periods of recovery and symptom recurrence (relapse), it resembles other diseases like hypertension and type-2 diabetes. These diseases are lifelong conditions that require continual effort to manage. Symptoms will likely return during periods where treatment compliance is low or absent, and symptoms will likely diminish when compliance to treatment begins again in earnest.
_
Scientists are now able to portray addiction as a medical disease with physiological and molecular changes thanks to the scientific and technological advances that have occurred over the past decade. Remarkable progress has revolutionized our understanding of the neurobiology of addiction and the way we treat it.
- Why do some people become addicted and others do not?
Addiction has a significant genetic component. In fact, it is estimated that 40–60% of the vulnerability to addiction can be attributed to genetic factors. These estimates of heredity include the percentage of the variance attributed to genetic factors by themselves as well as the percentage of the variance that is attributed to gene-environment interactions. Genotypic vulnerability for addiction is often suggested to reflect both variability in metabolism of the drug and variability in the sensitivity to the reinforcing effects of the abused substance. However, addiction-prone and addiction-resistant phenotypes may also reflect sensitivity to the various stressors and alternative reinforcers in an individual’s environment. As we gain knowledge of the individual differences in genes and the gene environment interactions that make a person more vulnerable to addiction, we will be able to tailor interventions for those at high risk.
- Why does addiction begin most frequently during adolescence?
Experimentation with drugs and alcohol often starts in adolescence, and so does the process of addiction. This could reflect normal adolescent-specific behaviors (risk-taking, novelty-seeking, response to peer pressure) that increase the probability of someone experimenting with drugs and alcohol, and perhaps could also reflect the incomplete development of brain regions involved in the processes of executive control and motivation (for example, myelination of frontal lobe regions). In adolescence, the incentive-rewards systems in the brain mature well before the cognitive control center. This consequentially grants the incentive-rewards systems a disproportionate amount of power in the behavioral decision-making process. Therefore, adolescents are increasingly likely to act on their impulses and engage in risky, potentially addicting behavior before considering the consequences. Furthermore, preclinical studies indicate that the neuroadaptations that occur in adolescents exposed to certain drugs such as nicotine or cannabinoids are different from those that occur during adulthood. Much research is currently focused on finding out whether the sensitivity to neuroadaptations during adolescence generalizes to other drugs and to alcohol, and whether this phenomenon could underlie the greater vulnerability to addiction in individuals who start using alcohol, nicotine and marijuana early in life. Better knowledge of the adolescent brain, its normal functioning and how it responds to social stressors and reinforcers will allow us to develop strategies to engage adolescents in productive and creative ways that will minimize their chances of experimenting with drugs.
- Why do addicted people often have other mental illnesses?
Individuals suffering from a variety of different disorders (such as depression, anxiety disorder, ADHD and schizophrenia) are at a much higher risk of abusing drugs and alcohol. Similarly, substance abusers and addicted individuals have a higher prevalence of mental disorders than the rest of the population. These robust comorbidities are likely to reflect overlapping environmental, genetic and neurobiological factors that influence substance abuse and mental illness. Comorbidities may emerge, in certain instances, when individuals afflicted by a mental disorder attempt to self-medicate (for example, when individuals with depression or schizophrenia use nicotine and alcohol). A more controversial interpretation, for which there is still not sufficient evidence, is the possibility that early exposure to certain drugs of abuse might increase the vulnerability to other mental disorders, particularly in those genotypes that confer increased susceptibility.
- What are the neural consequences of environmental risks?
Drug availability is the most obvious environmental factor that influences addiction. Indeed, increased availability of cocaine and methamphetamine has contributed to the recent epidemics of addiction to these drugs. Low socioeconomic class and poor parental support are two other factors that are consistently associated with a propensity to self-administer drugs, and stress might be a common feature of these environmental factors. The mechanisms responsible for stress-induced increases in vulnerability to drug use and to relapse in those addicted are not yet well understood. However, there is evidence that corticotropin-releasing factor (CRF) might play a linking role through its effects on the mesocorticolimbic dopamine system and the hypothalamic-pituitary–adrenal axis. Additional preclinical studies have provided tantalizing insights on how environmental factors affect the brain and how these, in turn, affect the behavioral responses to drugs of abuse. For example, in nonhuman primates, social status affects dopamine (DA) D2 receptor expression in the brain; low status decreases expression and increases the propensity for cocaine self-administration. Also, animal studies have shown that an increase in DA D2 receptors in the nucleus accumbens markedly decreases drug consumption, and this could provide a mechanism by which a social stressor modifies the propensity to self-administer drugs. If we understand the neurobiological consequences underlying the adverse environmental factors that increase the risks for drug use and for addiction, we will be able to develop interventions to counteract these changes
- How can we repair the brain circuits disrupted by drugs?
The adaptations in the brain from chronic drug exposure seem to be long-lasting and implicate multiple brain circuits (reward, motivation, learning, inhibitory control, executive function). This suggests that new interventions for drug addiction should include strategies that enhance the saliency value of natural reinforcers (including social support), strengthen inhibitory control and executive function, decrease conditioned responses and improve mood if disrupted. An interesting approach is the development of medications that act synergistically with an effective behavioral intervention. Although not yet evaluated for addiction, a proof of principle for such a concept has been recently established in a report showing that D-cycloserine administration facilitates the extinction of fear in phobic individuals through the pharmacological strengthening of the relearning events triggered during a desensitization session.
- What is volition and how do drugs disrupt it?
Remarkable scientific advances have emerged in the neuroscience of addiction that offer new insights into how chronic drug use affects the inner workings of the brain and how this leads to the aberrant behavioral manifestations of addiction. We have learned how some drugs and alcohol can disrupt volitional mechanisms by hijacking the brain mechanisms involved in seeking natural reinforcement and weakening brain mechanisms that inhibit these processes. This new knowledge has started to provide explanations of why the addicted person relapses even in the face of dire consequences such as loss of a child’s custody or incarceration. However, despite these advances in understanding the neuroplastic changes to drugs and alcohol, addicted individuals continue to be stigmatized by the pernicious yet enduring popular belief that their affliction stems from voluntary behavior. The loss of behavioral control in the addicted individual should spur a renewed discussion of what constitutes volition, challenge us to identify the neurobiological substrates that go haywire, and influence our evolving strategies to direct our efforts to prevent and treat substance abuse and addiction more effectively.
- Why is will power often not enough?
The initial and early decisions to use substances reflect a person’s free or conscious choice. However, once the brain has been changed by addiction, that choice or willpower becomes impaired. Perhaps the most defining symptom of addiction is a loss of control over substance use.
- Are people with Addiction responsible for their actions?
People with addiction should not be blamed for suffering from the disease. All people make choices about whether to use substances. However, people do not choose how their brain and body respond to drugs and alcohol, which is why people with addiction cannot control their use while others can. People with addiction can still stop using – it’s just much harder than it is for someone who has not become addicted.
_
The idea that substance addiction is a disease is not, however, universal. Some would argue that addiction is not a disease because:
- Addiction is not transmissible or contagious.
- Addiction is not autoimmune, hereditary, or degenerative.
- Addiction is self-acquired, implying the person gives the condition to himself.
Proponents of this way of thinking put much more emphasis on the social and environmental factors of addiction—one proponent claims that addictions may be “cured” by locking addicts in a cell where there is no access to substances—instead of on the brain changes that occur as a result of substance abuse. Some schools of thought view treatment for addiction as little more than the individual making the decision to stop using. Specific aspects of these opinions are hard to refute. For example, it is true that most substance abuse begins with a decision (although in many cases substance use began with a prescription from a doctor for a real medical problem and evolved into abuse). But while no one forced an addicted person to begin misusing a substance, it’s hard to imagine someone would willingly ruin their health, relationships, and other major areas of their lives. Surely, if overcoming addiction were as easy as simply choosing to stop, the problem of addiction would be much easier to address and relapse would not be as common. It should be noted that the “addiction is a choice” view is largely relegated to individuals and small groups. There are few, if any, nationally recognized substance abuse-focused organizations whose views have not evolved to understanding addiction as a disorder or disease. In fact, the NIH views the idea that addiction is a moral failing as an outdated, ill-informed relic of the past. The American Psychiatric Association (APA) no longer uses “addiction” as a term or diagnosis. Instead, the APA adopted the phrase “substance use disorder” as a way to describe problems related to “compulsive and habitual” substance use. The change was made specifically to avoid confusion surrounding the term addiction and it’s “uncertain” definition, as well as the negative stigma attached to the word.
_
Is current medical consensus about addiction as disease wrong?
From everyday experience we know that not everyone who tries or uses drugs and alcohol gets addicted, that of those who do many quit their addictions and that people don’t all quit with the same ease—some manage on their first attempt and go cold turkey; for others it takes repeated attempts; and others still, so-called chippers, recalibrate their use of the substance and moderately use it without becoming re-addicted.
But there is also strong scientific evidence that most people recover from addiction on their own and that things are not as simple as the medical model implies.
- Canadian psychologist, Bruce K. Alexander, argues the disease model makes one of two claims:
- Claim A: All or most people who use heroin or cocaine beyond a certain minimum amount become addicted.
- Claim B: No matter what proportion of the users of heroin and cocaine become addicted, their addiction is caused by exposure to the drug.
Alexander (2001) argues that historical and clinical evidence fails to support this view. He states that during the 19th century, opiate consumption in America and England was more prevalent than it is now, but less than 1% of the population became dependent or addicted and the numbers were declining at the end of the century even before certain laws were passed restricting use. In the United Kingdom, Alexander notes, heroin was widely used as a medication for chronic pain, cough, and diarrhea. In 1972, British physicians prescribed large doses of heroin, yet British statistics showed a surprisingly low number of people who’d become addicted to heroin as a result (Trebach,1982: p. 83). This challenges the disease theory, in addition to the assertion that exposure to certain substances will result in addiction in most people.
- Do Substances cause Addiction?
Reference to research on self-administration of drugs by laboratory animals is often used as an argument to support the construct of substance-induced addiction. In the 1960s, researchers at the University of Michigan created devices that allowed rats to self-administer drugs by pressing a lever. These types of experiments were conducted throughout the 1970s and demonstrated that rats, mice, monkeys, and other mammals will self-inject large doses of heroin, cocaine, amphetamines, and other drugs (Woods, 1978), seemingly proving that these substances are irresistibly addicting.
In the 1970s, Alexander and associates conducted the Rat Park study. Alexander posited that addiction was not substance-dependent, and that the evidence for opiate addiction seen in laboratory rats was attributable to living conditions rather than to the drugs’ addictive properties (Alexander, 2001). To prove his premise, Alexander built Rat Park, a housing colony approximately 200 times more spacious than a regular laboratory cage, with half dozen rats of both sexes living with ample provision of food, toys, and space for socializing, mating and raising litters. Experiments conducted in Rat Park indicated that rats who were living in a better environment had little appetite for morphine (Alexander, 2001). Rats that had been forced to consume morphine hydrochloride daily for nearly two months were brought to Rat Park and given the opportunity to choose between tap or morphine-laced water. Alexander (2001) reports that the rats for the most part chose plain water. Control groups of rats isolated in small cages consumed more morphine in this and subsequent experiments.
Alexander believes that the Rat Park experiments demonstrate that animal self-administration studies provide no empirical evidence for the theory of substance-induced addiction.
Two major science journals, Science and Nature, rejected Alexander’s results, but they were later accepted and published in Pharmacology Biochemistry and Behavior. Further studies showed mixed results. One of those studies found that both caged and “park” rats showed a decreased preference for morphine, suggesting a genetic difference. Another found that while social isolation can influence levels of heroin self-administration, isolation is not a necessary condition for heroin or cocaine injections to be reinforcing. Other studies reinforced the “Rat Park” findings showing that environmental enrichment reduced cocaine seeking behavior in mice and that environmental enrichment can eliminate already established addiction-related behaviors. Furthermore, removing mice from enriched environments has been shown to increase vulnerability to cocaine addiction and exposure to complex environments during early stages of life produce dramatic changes in the reward systems of the brain that result in reduced reactivity to drugs of abuse.
- In 1974 sociologist Lee Robins conducted an extensive study of U.S. servicemen addicted to heroin returning from Vietnam. While in Vietnam, 20 percent of servicemen became addicted to heroin, and one of the things Robins wanted to investigate was how many of them continued to use it upon their return to the U.S. and how many remained addicted. What she found was that the remission rate was surprisingly high: only around 7 percent used heroin after returning to the U.S., and only about 1-2 percent had a relapse, even briefly, into addiction. The vast majority of addicted soldiers stopped using on their own.
- In The Biology of Desire: Why Addiction Is Not a Disease, Marc Lewis, a neuroscientist and former drug addict, argues that addiction is “uncannily normal,” and he offers what he calls the learning model of addiction, which he contrasts to both the idea that addiction is a simple choice and to the idea that addiction is a disease. Lewis acknowledges that there are undoubtedly brain changes as a result of addiction, but he argues that these are the typical results of neuroplasticity in learning and habit formation in the face of very attractive rewards. In reviewing a number of case studies, Lewis argues that most addicts don’t think they are sick (and this is good for their recovery) and that the stories of people who have overcome their addiction, instead of impotence and disease, speak of a journey of empowerment and of rewriting one’s life narrative. That is, addicts need to come to know themselves in order to make sense of their addiction and to find an alternative narrative for their future. In turn, like all learning, this will also “re-wire” their brain.
- Taking a different line, in his book Addiction: A Disorder of Choice, Harvard University psychologist Gene Heyman also argues that addiction is not a disease but sees it, unlike Lewis, as a disorder of choice. Heyman presents powerful evidence not only that just about 10 percent of people who use drugs get addicted and only around 15 percent of regular alcohol drinkers become alcoholics but also that around 80 percent of addicts overcome their addiction on their own by the age of 30. They do so because the demands of their adult life, like keeping a job or being a parent, are incompatible with their drug use and are strong incentives for kicking a drug habit. Most people quit problematic drug use as they get older often without treatment. This is about people finding purposes that come to outweigh the importance of drug use for them as they mature.
In Addiction: A disorder of choice Gene Heyman makes a case for drug addiction to be a result of natural processes involving voluntary (i.e., operant) behavior, specifically choice. This approach stands in stark contrast to the current received view, at least as promulgated by the National Institute on Drug Abuse (NIDA) and the National Institute on Alcohol Abuse and Alcoholism (NIAAA), that drug abuse is a disease, specifically, “Addiction is a chronic, often relapsing brain disease…similar to other chronic, relapsing diseases, such as diabetes, asthma, or heart disease….” (NIDA, 2008).
Heyman seals the fate of the now discredited notion that compulsive, involuntary craving is a characteristic of drug addiction: both that it is a reliable feature and that it somehow indicates that a disease has developed. “Craving” has been dropped from the DSM as a diagnostic feature of drug dependence, but it is still invoked as being relevant, especially to relapse. But as Heyman notes, if most drug abusers suffer cravings when they quit, then craving cannot be that important in producing relapse because about three-quarters of those who are dependent quit permanently. Heyman also summarizes sound empirical evidence indicating that reports of craving and actual drug taking may be uncorrelated. He does note, however, that the question remains as to why anyone would voluntarily engage in behavior like incessant drug seeking, given its deleterious effects. Heyman argues for the possibility that normal choice processes are at the root of drug abuse. That is, he makes the case that while people do not choose to be drug addicts, they do make choices that lead to addiction. He argues that choice always involves the selection of the better current option, and that under certain circumstances drugs have advantages over other outcomes in that they provide immediate pleasure, their negative effects are delayed, they are not particularly subject to satiation, and they can undermine the value of other options. These advantages, of course, raise the question: Why isn’t everyone a drug addict? Heyman’s principal response to this question is that people differ in how they frame a sequence of choices. With lucid examples, he shows convincingly that overall benefit across a series of choices can be maximized by not choosing the immediately (local, in his terms) better option. A key preventative therefore is framing drug taking not locally but across a series of choices, that is, globally.
To sum up, Heyman’s book is provocative in two major ways. First, it develops a very compelling case that drug abuse should not be considered a disease. The several lines of evidence he presents accumulate and complement each other, building a virtually overwhelming argument in favor of his contention. Certainly, at the very least, research-funding and treatment agencies should not be “putting all their eggs” in the disease basket. Second, Heyman presents a reasonable suggestion that drug abuse can be considered as illustrating choice patterns that are appropriate in the short term, appropriate in the sense that they are predictable from what is known about choice. Those patterns are, however, not appropriate in the global, long-term, rational sense. This viewpoint offers several potential avenues for the remediation of drug abuse. One is simply to bring to bear alternatives that are more powerful in directing choice than are those operating when drug abuse is occurring, so that the basics of choice, for example generalized matching, can operate to retard drug abuse rather than promote it. This approach is what characterizes many of the relatively successful treatment approaches now being used. A second approach, one that is less adequately understood, has to do with “reframing” choice so that longer term consequences exert their effects.
All above studies and findings might seem contrary to what we are used to thinking. And, it is true, there is substantial evidence that addicts often relapse. But most studies on addiction are conducted on patients in treatment, and this skews the population sample. Most addicts never go into treatment, and the ones who do are the ones, the minority, who have not managed to overcome their addiction on their own. What becomes apparent is that addicts who can take advantage of alternative options do, and do so successfully, so there seems to be a choice, albeit not a simple one, involved here as there is in Lewis’s learning model—the addict chooses to rewrite his life narrative and overcomes his addiction.
______
______
Prevention of drug addiction:
The best way to prevent an addiction to a drug is not to take the drug at all. If your doctor prescribes a drug with the potential for addiction, use care when taking the drug and follow the instructions provided by your doctor. Doctors should prescribe these medications at safe doses and amounts and monitor their use so that you’re not given too great a dose or for too long a time.
Drug checking:
Drug checking or pill testing, as it is known in the Southern Hemisphere, is a way to reduce the harm from drug consumption by allowing users to find out the content and purity of substances that they intend to consume. This empowers users to make safer choices: to avoid more dangerous substances, to use smaller quantities, and to avoid dangerous combinations. Drug checking services have developed over the last twenty-five years in twenty countries and are being considered in more countries, although attempts to implement them in some countries have been hindered by local laws. Drug checking initially focused on MDMA users in electronic dance music events but the services have broadened as drug use has become more complex. A range of analysis techniques are in use by drug checking service. The most common are reagent testing, Fourier transform infrared spectroscopy, ultraviolet-visible spectroscopy, Raman spectroscopy, and gas chromatography mass spectroscopy. Developing technologies include nuclear magnetic resonance spectroscopy and ion-trap mass spectroscopy.
Alternative development:
Although the conceptual connection between drug abuse and development has been weak, an operational linkage between the two can be traced back to the early 1970s. At that time, crop substitution to provide sufficient income to replace opium poppies was carried out with pilot projects. Early experiences were frustrating. Each substitute crop brought new problems: selection of the substitutes; gaining experience in planting, care and harvesting; and other difficulties associated with processing, storage and marketing. Officials recognized that agricultural diversification was needed and commercial support was required for production. To survive, development projects had to become more diversified and regional in nature. Poppy-growing regions of Asia needed regional development programs and the promotion of agroprocessing, the generation of new employment and the introduction of activities in entirely new economic sectors and services, as well as the development of basic infrastructure, especially in transport and communications. These programs also sometimes required the creation of alternative living conditions acceptable to the local populations. What began as crop substitution broadened into integrated rural development and has now further evolved into alternative development as a means of drug abuse prevention and control.
Alternative development is an approach to policy formulation and implementation that takes into account the economic and social structures that influence illicit drug supply. This approach recognizes that in order to achieve long-run success it is necessary to integrate into the social mainstream peasants, producers and traffickers. The aim, therefore, is to combine development for drug abuse prevention and control with broader, mainstream development efforts. Alternative development programs assist governments in finding alternative socioeconomic strategies and extending them to farmers engaged in the production of drug-producing crops that the governments want to eliminate. These programs may also serve to ease, and thus help encourage, the transition of an entire country from an economic dependency on narcotics production and/or trafficking to a non-narcotics-based development strategy. As broad as these programs are, there is no single approach to alternative development suited to all countries where it may be used. Each country needs a carefully tailored strategy to fit its situation. Alternative development differs from mainstream development in that it not only indicates a process of change to strengthen the legal economy but also sets an additional goal, directing change so as to prevent or exclude illicit activities.
_____
_____
Drug abuse education:
Education is the principal means of preventing drug abuse. In addition to educational institutions, other settings are important for the contributions they make to learning and socialization. Home, workplace and religious institutions, to name three examples, are settings for the education of young and old alike. Most officials support the full integration of drug abuse education into mainstream institutions, whether public and private, religious or secular. Drug education is the planned provision of information, resources, and skills relevant to living in a world where psychoactive substances are widely available and commonly used for a variety of both medical and non-medical purposes, some of which may lead to harms such as overdose, injury, infectious disease (such as HIV or hepatitis C), or addiction.
An issue, often unstated, is whether, to have real impact on the drug problem, society or the individual should be the initial target for change. Seeking the root causes focuses on the social conditions that lead persons to engage in drug abuse. Slow and indirect, education is often seen as producing its results only over the long run, involving parents and making gradual social changes to reduce experimentation, occasional or regular drug use. The short-term approach (to control the supply of drugs) and the long-term demand reduction approach by education are two ends of a continuum which are often placed in opposition to each other. In reality, both are essential parts of a comprehensive view of prevention of drug abuse.
Approaches to education about drugs may be grouped conceptually into a threefold typology: (a) the chosen educational strategy or approach (direct, alternative or indirect and selective); (b) the target group and (c) the type of activity and teaching materials used. Depending on the target group, a direct substance-centered approach may be used. It is possible to make the environment of the individuals involved the target, although this is not frequently done. Also, educational activities may be carried out by adults, teachers, specialist educators, youth leaders, parents or peers.
_
The mass media have been used in many different types of campaigns and programs. However, the objectives of mass communication efforts have often been unclear and lacking in specific outcome goals. They are based on the assumption that peoples’ knowledge, attitudes and behaviour can be influenced in a desired direction. Television, radio, newspapers, posters, brochures – all of these may reach a large number of persons. The overall effect of their use on various target groups in many different countries has not been evaluated. There are examples of inquiries into the success of mass media efforts. Specialized communication techniques have recently been examined from the standpoint of the potential for reducing drug demand and promoting alternative development. The dramatic success of child immunization campaigns in developing countries may provide useful ideas for the drug abuse field. Applicability of similar techniques to drug abuse education has been the subject of some speculation. Qualitative audience research and focus groups have been proposed as a means of obtaining a better understanding of the common underlying causes of drug abuse in various groups. Further study of the impact of the mass media on attitudes and behaviour in a variety of social and cultural contexts is needed.
_____
_____
Measures against drug addiction:
The global drug problem has 3 major themes, which are clearly discernible in most countries around the world: concern about young people and drugs; concern about addiction; and concern about the effects of the illegal production, trafficking, and selling of drugs. Two major policy and programming approaches are used to deal with these concerns about drug use: the criminal justice model and the public health model.
_
War on drugs:
In 1972, United States President Richard Nixon announced the commencement of the so-called “War on Drugs”. Later, President Reagan added the position of drug czar to the President’s Executive Office. In 1973, New York introduced mandatory minimum sentences of 15 years to life imprisonment for possession of more than 113 grams (4 oz) of a so-called hard drug, called the Rockefeller drug laws after New York Governor and later Vice President Nelson Rockefeller. Similar laws were introduced across the United States. California’s broader ‘three strikes and you’re out’ policy adopted in 1994 was the first mandatory sentencing policy to gain widespread publicity and was subsequently adopted in most United States jurisdictions. This policy mandates life imprisonment for a third criminal conviction of any felony offense. A similar ‘three strikes’ policy was introduced to the United Kingdom by the Conservative government in 1997. This legislation enacted a mandatory minimum sentence of seven years for those convicted for a third time of a drug trafficking offense involving a class A drug.
It’s a war without a clear enemy. Anything waged against a shapeless, intangible noun can never truly be won — President Clinton’s drug czar Gen. Barry McCaffrey said as much in 1996. And yet, within the past 40 years, the U.S. government has spent over $2.5 trillion dollars fighting the War on Drugs till 2009. Despite the ad campaigns, increased incarceration rates and a crackdown on smuggling, the number of illicit drug users in America has risen over the years and now sits at 19.9 million Americans. And a large portion of their supply makes its way into the country through Mexico. As you probably know, however, the fight is far from over. In fact, it’s likely that you know someone intimately who either has a current problem with drugs or is recovering from an addiction to drugs. Even if you don’t, you may hear news about drug cartels in Mexico and Columbia, killing residents in order to stay in business creating and selling illicit drugs to willing buyers.
_
Drug policy:
A drug policy is the policy, usually of a government, regarding the control and regulation of drugs considered dangerous, particularly those that are addictive. Governments try to combat drug addiction with policies that address both the demand and supply of drugs, as well as policies that mitigate the harms of drug abuse, and for medical treatment. Demand reduction measures include prohibition, fines for drug offenses, incarceration for persons convicted for drug offenses, treatment (such as voluntary rehabilitation, coercive care, or supply on medical prescription for drug abusers), awareness campaigns, community social services, and support for families. Supply side reduction involves measures such as enacting foreign policy aimed at eradicating the international cultivation of plants used to make drugs and interception of drug trafficking. Policies that help mitigate drug abuse include needle exchange and drug substitution programs, and free facilities for testing a drug’s purity. Drugs subject to control vary from jurisdiction to jurisdiction. For example, heroin is regulated almost everywhere; substances such as qat, codeine are regulated in some places, but not others. Most jurisdictions also regulate prescription drugs, medicinal drugs not considered dangerous but that can only be supplied to holders of a medical prescription, and sometimes drugs available without prescription but only from an approved supplier such as a pharmacy, but this is not usually described as a “drug policy”.
_
Drugs and the law:
The law is different in every country. A drug can be legal in one country and illegal in another. For instance, in Ecuador, cannabis is allowed. But in the United States of America it is illegal to have cannabis in most states. In the United Arab Emirates, alcohol is not allowed. But in the United States, adults are allowed to have alcohol. Some drugs are only legal if you have permission (a “prescription”) from a doctor to have them. If a person is caught by the police with controlled drugs they are not allowed to have, they may be taken to court. Court cases may result in fines (when one is required to pay a large sum of money to the government). One may be sent to prison. In some countries, execution is a punishment for drug possession. It is important to know what the law says about drugs in your area.
_
Harm reduction:
Harm reduction, or harm minimization, is a range of public health policies designed to lessen the negative social and/or physical consequences associated with various human behaviors, both legal and illegal. Harm reduction policies are used to manage behaviors such as recreational drug use and sexual activity in numerous settings that range from services through to geographical regions. Critics of harm reduction typically believe that tolerating risky or illegal behaviour sends a message to the community that such behaviours are acceptable and that some of the actions proposed by proponents of harm reduction do not reduce harm over the long term.
Harm reduction seeks to minimize the harm that can occur through the use of various drugs, whether legal (e.g., alcohol and nicotine), or illegal (e.g., heroin and cocaine). For example, people who inject illicit drugs can minimize harm to both themselves and members of the community through proper injecting technique, using new needles and syringes each time, and proper disposal of all injecting equipment. Needle-exchange programs reduce the likelihood of users of heroin and other drugs sharing the syringes and using them more than once. Syringe-sharing can lead to infections such as HIV or hepatitis C, which can spread from user to user through the reuse of syringes contaminated with infected blood. Needle and syringe program (NSP) and Opioid Substitution Therapy (OST) outlets in some settings offer basic primary health care. Opioid replacement therapy (ORT), or opioid substitution therapy (OST), is the medical procedure of replacing an illegal opioid, such as heroin, with a longer acting but less euphoric opioid; methadone or buprenorphine are typically used and the drug is taken under medical supervision. Another approach is Heroin assisted treatment, in which medical prescriptions for pharmaceutical heroin (diacetylmorphine) are provided to heroin-dependent people.
In some countries, there has been a move toward harm reduction by health services, where the use of illicit drugs is neither condoned nor promoted, but services and support are provided to ensure users have adequate factual information readily available, and that the negative effects of their use be minimized. Such is the case of Portuguese drug policy of decriminalization, which achieved its primary goal of reducing the adverse health effects of drug abuse.
__
Discrimination against drug addicts:
Discrimination against drug addicts is a form of discrimination against individuals who suffer from a drug addiction. In the process of stigmatization, drug addicts are stereotyped as having a particular set of undesirable traits, in turn causing other individuals to act in a fearful or prejudicial manner toward them. Drug use discrimination also leads to many users being secretive about drug use. As it relates to healthcare stigmatizing attitudes surrounding drug use can cause barriers to treatment uptake and engagement. In some of its manifestations, discrimination against drug addicts involves a violation of human rights.
Drug abusers are often depicted as human beings who are not capable of staying drug free and are often addressed using derogatory terms. The reasoning for not helping patients seek the treatments needed are often due to the terms used to identify them, such as “crackhead” or “junkie”. The name calling and stigma places a sense of shame for drug users for a disease that takes control of them physically and psychologically. Discrimination against drug abusers is very common in the workplace, and the most familiar example happens when employers give random drug test to see if the employee will pass it.
______
______
Arguments for legalization of marijuana: Medical Marijuana:
Many articles have been written on the subject of Cannabis drugs, but data that definitively outlines benefits and harms is often conflicting or inconclusive. Some research has suggested that marijuana is a very mild substance that requires considerable practice before its full (desired) effects are achieved. Alcohol clearly appears more potent and far more deleterious. From the point of view of those who favour the legalization of marijuana, the drug is a mild hallucinogen that bears no similarity to the narcotics. They feel that the evidence clearly indicates that marijuana is not a stepping-stone to heroin and that its use is not associated with major crimes. As a means of reducing tension and achieving a sense of well-being, they believe that it is probably more beneficial and considerably safer than alcohol. The debate over the use of marijuana and the harsh penalties that are imposed are perceived by users as a greater threat to society than would be a more rational and realistic approach to drug use.
_
The term medical marijuana refers to using the whole, unprocessed marijuana plant or its basic extracts to treat symptoms of illness and other conditions. The U.S. Food and Drug Administration (FDA) has not recognized or approved the marijuana plant as medicine. Because the marijuana plant contains chemicals that may help treat a range of illnesses and symptoms, many people argue that it should be legal for medical purposes. In fact, a growing number of states have legalized marijuana for medical use. Currently, the two main cannabinoids from the marijuana plant that are of medical interest are THC and CBD. THC can increase appetite and reduce nausea. THC may also decrease pain, inflammation (swelling and redness), and muscle control problems. Unlike THC, CBD is a cannabinoid that doesn’t make people “high.” These drugs aren’t popular for recreational use because they aren’t intoxicating. It may be useful in reducing pain and inflammation, controlling epileptic seizures, and possibly even treating mental illness and addictions.
_
Some studies have suggested that medical marijuana legalization might be associated with decreased prescription opioid use and overdose deaths, but researchers don’t have enough evidence yet to confirm this finding. For example, one study found that Medicare Part D prescriptions filled for all opioids decreased in states with medical marijuana laws. Another study examined Medicaid prescription data and found that medical marijuana laws and adult-use marijuana laws were associated with lower opioid prescribing rates (5.88 percent and 6.88 percent lower, respectively). Additionally, one NIDA-funded study suggested a link between medical marijuana legalization and fewer overdose deaths from prescription opioids. These studies, however, are population-based and can’t show that medical marijuana legalization caused the decrease in deaths or that pain patients changed their drug-taking behavior. A more detailed NIDA-funded analysis showed that legally protected medical marijuana dispensaries, not just medical marijuana laws, were also associated with decreased prescription opioid use and overdose deaths. Additionally, some data suggests that medical marijuana treatment may reduce the opioid dose prescribed for pain patients, while another recent NIH-funded study suggests that cannabis use appears to increase the risk of developing and opioid use disorder. NIDA is funding additional studies to determine the link between medical marijuana use and the use or misuse of opioids for specific types of pain, and also its possible role for treatment of opioid use disorder.
_______
Arguments against legalization of marijuana:
The new legalization initiatives bear the risk of unintended consequences. Legalizing the production and consumption of cannabis for nonmedical uses not only frees users from fear of the police and stops the current criminal traffic in the substance, it may, more fundamentally, call into question the basic principles of international drug policy, which focus on limiting all drug use to therapeutic, medically supervised purposes. It may, in other words, unravel the international medical drug supply system.
_
A large proportion of individuals who use cannabis go on to use other illegal drugs. The increased risk of progression from cannabis use to other illicit drugs use among individuals with mental disorders underscores the importance of considering the benefits and adverse effects of changes in cannabis regulations and of developing prevention and treatment strategies directed at curtailing cannabis use in these populations. One study indicates that about 40% of individuals with lifetime cannabis use progressed to other illicit drug use, highlighting the potential dangers of policies that may increase the availability of cannabis, at least for the fraction of individuals at risk for other illicit drug use. Furthermore, psychiatric comorbidity is a strong predictor of the association between cannabis use and progression to other illicit drug use. There is a need to consider the health benefits and adverse effects of changes in cannabis regulation that expand access to this substance, and for the development of prevention and intervention efforts targeted at cannabis users with co-occurring mental disorders.
_
Unintentional Marijuana ingestions by Young Children is associated with legalization. One observational study portrays a trend of increasing unintentional marijuana ingestions by young children over the past 5 years. States with at least some form of legalized marijuana seem to be preferentially affected. This may be attributable to higher levels of accidental ingestions or other factors, including more ready disclosure by caregivers in states with legalized marijuana.
_
Although many states have legalized marijuana for medical use, the scientific evidence to date is not sufficient for it to gain U.S. Food and Drug Administration (FDA) approval, for two main reasons.
First, there have not been enough clinical trials showing that marijuana’s benefits outweigh its health risks. The FDA requires carefully conducted studies (clinical trials) in hundreds to thousands of patients to determine benefits and risks.
Second, to be considered a legitimate medicine, a substance must have well-defined and measurable ingredients that are consistent from one unit to the next (such as a pill or injection). This consistency allows doctors to determine the dose and frequency. As the marijuana plant contains hundreds of chemical compounds that may have different effects and that vary from plant to plant, evaluating the whole plant as a medicine is difficult.
However, synthetic THC-based drugs to treat nausea caused by chemotherapy and increase appetite in patients with extreme weight loss caused by AIDS are already FDA-approved and prescribed. In addition, the FDA recently approved Epidiolex®, the first medicine derived from the marijuana plant itself. Epidiolex® is made using CBD, a non-psychoactive ingredient in the plant, and has shown efficacy in treating two rare and severe forms of epilepsy in children.
Note:
Tetrahydrocannabinol (THC) and cannabidiol (CBD) are the two primary cannabinoids that occur naturally in the Cannabis sativa plant, most commonly known as cannabis. Both of these substances interact with the cannabinoid receptors found in the human body and brain, but they differed dramatically in their effects. CBD is non-psychoactive which means that it will not get the user high. Because of this trait, CBD appears more frequently than THC in dietary and natural supplements.
_____
_____
Arguments for prohibition of drugs:
Health:
That illicit drugs are inherently harmful substances is attested by the very nomenclature of the ‘harm reduction’ movement. Taking as an example the disproportionate harms of heroin, European mortality ranges from 1 to 4 deaths for every 100 opiate users per annum but worldwide is most usually around 2% per annum. In Australia, 83% of Australians aged 14 and over drink alcohol, and for the 10% estimated to be problem drinkers the 3,500 deaths per year from alcohol would represent just 0.22 lives per hundred, even before recognising that alcohol deaths are not all self-inflicted. In 2005, there were 14,900 tobacco deaths per year predominantly afflicting the age-group which had 43% of Australia’s 11,388,000 population smoking tobacco in 1965, yielding 0.3 lives per hundred mortality per year. The protest that alcohol is harmful yet legal, therefore illegal drugs should similarly be legal (and harmful) ignores the fact that the legal drugs already cause more than enough harm to want to add a new battery of even more harmful but now legal drugs.
Illicit drugs are illicit precisely because they present inordinate mortality or morbidity via their use. By comparison, the current costs of law enforcement, which has so dramatically maintained levels of illicit drug use so much below that of licit drug use, and which has thereby contained their health harms, will be far outweighed by the exponential increases in healthcare costs as drug use increases under the legalization/ regulation paradigm – as with alcohol or tobacco there is an inverse relationship between reducing the cost of the drug and the resulting increases in use and harms. Many of the deaths from using cannabis, other than from car accidents while intoxicated or violence and aggression while withdrawing, are more likely to figure in the longer term, just as it is with tobacco, where both nicotine overdose and cannabis overdose are both extremely rare.
The Success of Prohibition:
Prohibition has a successful track record suppressing illicit drug use since it was introduced 100 years ago in that licit drugs have current (last 12 months) user rates as high as 80-90% in populations over 14 years of age, and tobacco has historically had current use rates up to 60% of adult populations, the percentages currently using illicit drugs in OECD countries are generally below 1% of the population excepting cannabis where most are between 3% and 10%, with six countries between 11% and 17%. A 2001 Australian study, of 18- to 29-year-olds by the NSW Bureau of Crime Statistics and Research suggests that prohibition deters illicit drug use. 29% of those who had never used cannabis cited the illegality of the substance as their reason for never using the drug, while 19% of those who had ceased use of cannabis cited its illegality as their reason. Controls and prohibitions help to keep prices higher, and higher prices help keep use rates relatively low, since drug use, especially among young people, is known to be sensitive to price. Legalizing drugs will make drugs cheaper and thus increase use as with the experience of cheaper crack cocaine in the US.
The view that prohibition makes a prohibited item lucrative for criminals is indeed correct, after all this is an inherent dynamic that drives criminality. But capitulating to illicit drug use on these grounds makes no more sense than capitulating to those who continue to traffic in human lives, a more expensive business because of its illegality and therefore more lucrative for the criminal, but necessary for the rights of vulnerable citizens.
The idea that criminals will be put out of business by legalization fails to recognize that the most productive recruiting pool to illicit drug use has always been amongst secondary school-aged young people, an age group that would still be prohibited from buying drugs even in a regulated framework, as with alcohol or tobacco. Consequently, criminal effort will be more concentrated on this vulnerable age group even more so than currently. Further, a large number of studies have shown that criminal careers are embarked on before the onset of drug use, while drug use intensifies this criminal behaviour.
The argument that drug addicts are forced into crime by prohibition should first and foremost highlight the fact that this argument presupposes and underlines the addictive nature of illicit drugs (which legalization proponents often downplay), addictive enough to create a viable criminal supply industry. Secondly, the harms of increased drug use would be a consequence of legalization and its cheaper prices, far outweigh the current crime harms of prohibition.
Drug legalization advocates spuriously claim that US prisons are overflowing with people convicted for only simple possession of marijuana. This claim is aggressively pushed by groups seeking to relax or abolish marijuana laws. A more accurate view is that the vast majority of inmates in prison for marijuana have been found guilty of more than simple possession. They were convicted for drug trafficking, or for marijuana possession along with other offences. Many of those in prison for marijuana entered a guilty plea to a marijuana charge to avoid a more serious charge. In the US, just 1.6 percent of the state inmate population were held for offences involving only marijuana, and less than one percent of all state prisoners (0.7 percent) were incarcerated with marijuana possession as the only charge. An even smaller fraction of state prisoners were first time offenders (0.3 percent). The numbers on the US federal prisons are similar. In 2001, the overwhelming majority of offenders sentenced for marijuana crimes were convicted for trafficking and only 63 served time for simple possession.
Freedom from the Consequences of Drugs:
The notion that illicit drug use is a victimless crime and that everyone should be free to do what they want with their body disregards the web of social interactions that constitute human existence. Affected by an individual’s illicit drug use are children, parents, grandparents, friends, colleagues, work, victims of drugged drivers, crime victims, elder abuse, sexual victims, patients made sicker by medical marijuana etc. Illicit drug use is no less victimless than alcoholism. Taking as an example the effect of illicit drug use on children, in 2007 one in every nine children under the age of 18 in the United States lived with at least one drug dependent or drug abusing parent. 2.1 million children in the United States live with at least one parent who was dependent on or abused illicit drugs. Parental substance dependence and abuse can have profound effects on children, including child abuse and neglect, injuries and deaths related to motor vehicle accidents, and increased odds that the children will become substance dependent or abusers themselves.
The idea that one should always have the freedom to do whatever one wants without regard to the common good is belied by the plethora of social agreements which make a society cohesive. Notably, democracy limits the freedom of individuals, particularly the freedom of individuals who are not in accord with the majority beliefs as to what promotes the common good. Therefore any democratic society that deems the use of a certain drug to present unacceptable harm to the individual user, to present unacceptable harm to the users’ surrounding community or to transfer too great a burden to the community will seek legislation which will curb that particular freedom of the individual user. The argument that illicit drug use is an unalienable human right rests on a faulty assumption of individual freedom that fails to balance freedom with responsibility to others in the community.
Regarding the freedom of choice of those addicted to a drug, it is important to recognize that addiction is defined as compulsive by its very nature and that addictions curb individual freedom. Likewise, the proposal that addictive drugs should be legalized, regulated and opened to free market dynamics is immediately belied by the recognition that the drug market for an addict is no longer a free market – it is clear that they will pay any price when needing their drug.
Libertarians argue that only drug dealers should be fought and not the drug users themselves. But this rests on the fundamental error that big-time drugs smugglers and dealers hawk illicit drugs to new consumers. This is most often not the case. Rather it is the users themselves that are mostly responsible for recruiting new users through networks of friends or relatives demonstrating that users need to be targeted as the recruiters of new drug use, and that an emphasis on early rehabilitation for young users is the best answer to curbing widespread dealing. Sweden’s mandatory rehabilitation program has resulted in the lowest drug use levels in the developed world.
_______
Arguments against prohibition of drugs:
Prohibition does not discourage drug use:
It has been suggested that drug law reform could reduce the use of hard drugs as it has in countries such as the Netherlands. According to a 2009 annual report by the European Monitoring Centre for Drugs and Drug Addiction, the Dutch are among the lowest users of marijuana or cannabis in Europe, despite the Netherlands’ policy on soft drugs being one of the most liberal in Europe, allowing for the sale of marijuana at “coffee shops”, which the Dutch have allowed to operate for decades, and possession of less than 5 grams (0.18 oz). British Crime Survey statistics indicated that the proportion of 16- to 24-year-olds using cannabis decreased from 28% a decade ago to 21%, with its declining popularity accelerating after the decision to downgrade the drug to class C was announced in January 2004. The BCS figures, published in October 2007, showed that the proportion of frequent users in the 16–24 age group (i.e. who were using cannabis more than once a month), fell from 12% to 8% in the past four years. American teenagers are drinking and smoking less and doing fewer drugs than their predecessors in more than 40 years of tracking. Use of marijuana is down among 8th- and 10th-graders, though it is flat among high school seniors, according to the annual Monitoring the Future survey of American teens.
_
Failed prohibition:
Since the 1960s, approaches to drug use have tended to involve criminalization and interfering with supply through policing, customs controls, and education (Nutt et al 2007). Politicians frequently respond to drug use not by suggesting divergent policies, but by persisting with those in existence whilst calling for more intense, prohibitive, and punitive measures (Des Jarlais 1995). To be sure, incarceration in prisons or drug detention centres of people who use drugs – but have committed no other crime – policies which are known to contribute to the increased transmission of HIV, hepatitis, and tuberculosis, receive more fervent support than ever (Global Commission on Drug Policy 2011; Global Commission on Drug Policy 2012; Kerr and Wood 2008). People who use drugs are seen to be “deserving punishment rather than deserving health care” (Des Jarlais et al 1995: 1579).
Globally, criminalisation of and punitive approaches to drug use continue to be implemented, in spite of there being little evidence to suggest that these policies have yielded positive results. In spite of its popularity, it is stressed that prohibitionism has failed to curb or diminish drug use and associated problems, failing even by its own metrics and standards; the astronomical numbers of people who use drugs speak for themselves, where estimates point to strikingly high levels of global drug use. The United Nations Office on Drugs and Crime estimate that in 2009, 149-272 million people (3.3-6.1% of the global populace aged 15-64) “used illicit substances at least once in the previous year” (UNODC 2011: 13). Though downward trends in global cocaine and heroin use are noted, these are offset by increasing nonmedical/illicit usage of synthetic and prescription drugs (UNODC 2011). Between 15 and 39 million people are defined as ‘problem drug users’, having dependency issues or being people who inject drugs (UNODC 2011).
_
Failure of war on drugs:
The ‘war on drugs’ approach of criminalising supply and consumption has been an unequivocal failure. Eduardo Porter writing in the New York Times (July 3 2012) gave the shocking statistic that a gram of pure cocaine from an average, local dealer now costs 74% less than it did 30 years ago. This demonstrates that banning a drug does not impact the availability by pricing consumers out of the market. One of the biggest flaws in the war on drugs is the counter-productive nature of law enforcement. Once the market in any illegal drug is established, law enforcement interventions actually increase violence. A systematic review of the effect of law enforcement on drug violence for the International Journal of Drug Policy showed that in that, in 14 out of 15 studies, law enforcement interventions not only failed to decrease violence, but led to more violence. Dan Werb et al (2011) state this is due to the resulting conflict to takeover when top figures are removed by investigations, and by ‘target hardening’, where organisations become increasingly militarised due to constant threat from rivals or the authorities. The real danger is that this law enforcement effect gradually influences the newly formed criminal organisations supplying drugs, turning them into serious, hardened organised crime structures. If this is the case, policy makers will succeed in creating organised crime, with the resulting fear and fallout, where none existed.
Global Commission on Drug Policy, an organization launched by former Presidents of Brazil, Colombia and Mexico (and whose accomplished 19-member board includes former U.N. Secretary General Kofi Annan, Pakistani feminist activist Asma Jehangir, and, yes, Sir Richard Branson), declared that the “global war on drugs has failed, with devastating consequences for individuals and societies around the world.” Four decades ago, policy makers imagined creating a drug free world through “harsh law enforcement action” that cracked down on drug production and distribution. But the resulting “vast expenditures on criminalization and repressive measures directed at producers, traffickers and consumers” have only led to an expansion of the trade, higher rates of drug consumption, and has created — as seen in places like Mexico or Afghanistan — deadly, volatile new arenas for an illicit industry to sow mayhem.
The report outlines some of the unintended consequences of a near half century of global anti-drug policies. A few:
- The growth of a ‘huge criminal black market’, financed by the risk-escalated profits of supplying international demand for illicit drugs.
- Geographical displacement, often known as ‘the balloon effect’, whereby drug production shifts location to avoid the attentions of law enforcement.
- The perception and treatment of drug users, who are stigmatized, marginalized and excluded.
The commission advocates decriminalizing drug use by those who do no harm to others. Countries that have adopted measures that treat drug users as patients — and not criminals — have, for example, drastically lower rates of HIV-positive needle-users. The public health consequences for decades of ineffective policies are stark and can’t be ignored. Governments, the report says, need to stop fretting over false dichotomies of “tough or soft, repressive or liberal” policies and think up a flexible approach that both minimizes “health and social harms” and maximizes “individual and national security.” A vital cog of this is decriminalizing and perhaps even legalizing certain drugs, particularly cannabis, and taxing their production and sale.
______
______
Calls for legalization, relegalization or decriminalization:
The terms relegalization, legalization, and decriminalization are used with very different meanings by different authors, something that can be confusing when the claims are not specified. Here are some variants:
- Sales of one or more drugs (e.g., marijuana) for personal use become legal, at least if sold in a certain way.
- Sales of an extracts with a specific substance become legal sold in a certain way, for example on prescription.
- Use or possession of small amounts for personal use do not lead to incarceration if it is the only crime, but it is still illegal; the court or the prosecutor can impose a fine. (In that sense, Sweden both legalized and supported drug prohibition simultaneously.)
- Use or possession of small amounts for personal use do not lead to incarceration. The case is not treated in an ordinary court, but by a commission that may recommend treatment or sanctions including fines. (In that sense, Portugal both legalized and supported drug prohibitions).
In the 2010s, movements have grown around the world proposing the relegalization and decriminalization of drugs. For instance, there is a movement for cannabis legalization in Canada, as well as the Marijuana Party of Canada. Drug liberalization policies are often supported by proponents of liberalism and libertarianism on the grounds of individual freedom. There are also growing counter movements. Prohibition of drugs is supported by proponents of conservative values but also by many other types of NGO’s that are not linked to conservative political parties. A growing number of NGO organizations in many countries have joined the international network World Federation Against Drugs. WFAD members support the United Nations narcotics conventions.
______
______
Decriminalization and treatment of drug addict is better than incarceration:
It is high time the drug users were seen as patients, not criminals. Unfortunately, our laws and policies are not adequately geared up to treat the drug users as victims. Many youngsters get attracted to drug consumption for various reasons. Rather than putting them in jails, we should focus on giving them medical and psychosocial aid. The drug problem cannot be checked only by supply control or law enforcement. Those affected should get adequate help, support and treatment and not be treated as criminals. Even the United Nations lately has been telling all the countries to amend laws so that using drugs is not seen as a criminal act.
The goal of social policy is to reduce potential harms. However, punitive enforcement drug policies have made it difficult to see potentially dangerous drugs with the same lens as potentially dangerous foods, tobacco and alcohol. Evidence-based treatment for drug addiction reduces health and social consequences e.g. crime, HIV/AIDS and economic burden.
According to the World Health Organization, there is a cost savings of US$7 for every US$1 spent on treatment. Treatment is cost-effective in developed and developing countries. The use of punitive laws with incarceration as a control measure and lengthy custodial sentences for minor drug offences have led to over-representation of drug users in prisons. Various reviews have also reported drug use and injections in prisons although their occurrence is often denied. Denial is the chain that prevents addicts from seeking treatment. Billions have been spent over the years on incarceration and rehabilitation centers.
_
Decriminalization versus legalization:
Decriminalization does not mean legalization.
Decriminalization refers to drug use and possession offences, and not the sale or supply of drugs. It focuses on drug users, not drug suppliers. The objective is to provide users with a more humane and healthcare response to their drug use. Whilst there is no universal definition of decriminalization, and even confusion sometimes, in essence it means the removal of criminal penalties for drug use or possession either by law or by practice. The penalties could be civil e.g. fines or diversion of offenders to educational or treatment options.
On the other hand, legalization is akin to that of the currently legal drugs e.g. tobacco and alcohol which have limitations on their sale.
Evidence for decriminalization:
Policies should be based on evidence. Numerous studies have concluded that the “war on drugs” failed to deter drug addiction but instead deterred drug addicts from seeking treatment and inhibited harm reduction efforts.
The global research evidence on the impact of decriminalization of drug use include:
- Reduction in costs to society, especially the criminal justice system
- Reduction in social costs to individuals, including improvement to education and employment prospects
- Does not increase drug use
- Does not increase other crime
- May, in some jurisdictions, widen contact with the criminal justice system.
_
Portugal’s experience:
In 2001, Portugal decriminalized the use of all drugs. Whilst the possession and use of drugs remained illegal, the offence changed from criminal, in which the offender could be sent to prison, to an administrative one. The Health Ministry had oversight over treatments for drug addiction, which are accessible to everyone free-of-charge with substantial aftercare to reintegrate addicts back into society.
Decriminalization reduced the heroin abuse with the Health Ministry’s estimate that heroin users numbered about 25,000 in 2017 compared to 100,000 in 2001. The reported rate of drug-related deaths is the second lowest in the European Union together. There was also a continuous decrease in the numbers of drug-related HIV/AIDS.
_
Opioid-epidemic-incarceration-income-study:
In counties across the United States, when incarceration rates rise and household incomes fall, drug-related deaths increase, according to a study published in the medical journal Lancet Public Health. The study found that, from 1983 to 2014, when there was a large decrease in average household income — a drop of nearly a third — there was an associated 12.8% increase in drug-related deaths in the county. Average increases of 7,018 jail admissions per 100,000 people and 255 prison admissions per 100,000 people were associated with a 1.5% and a 2.6% increase in the county’s death rate from drug use, respectively, the study found.
If we’re incarcerating people because we don’t like the negative effects of drugs, what this study shows is it’s counterproductive. It’s a strong argument for decriminalization of hard drugs as opposed to criminalization, which actually makes a lot of sense, given that the definition that we use of addiction is the continued obsessive-compulsive use of drugs despite negative consequences. So imprisoning people — giving them negative consequences to get them to stop using drugs — is not going to work by the very definition we’re using of addiction. The impact of incarceration on individuals and families can be devastating leading to an increased incidence of homelessness, unemployment, divorce, and recidivism. Individuals who have been incarcerated are more likely to be substance users and have a higher risk of premature death. Economic deprivation is also a known risk factor for substance abuse and early death. It seems plausible, therefore, that both rates of incarceration and impoverishment might contribute to changes in mortality from drug use. The results highlight the need to evaluate current approaches towards the issues associated with incarceration.
______
______
Treatment of drug addiction:
_
Principles of Drug Addiction Treatment:
- Addiction is a complex but treatable disease that affects brain function and behavior. Drugs alter the brain’s structure and how it functions, resulting in changes that persist long after drug use has ceased. This may help explain why abusers are at risk for relapse even after long periods of abstinence.
- No single treatment is appropriate for everyone. Matching treatment settings, interventions, and services to an individual’s particular problems and needs is critical to his or her ultimate success.
- Treatment needs to be readily available. Because drug-addicted individuals may be uncertain about entering treatment, taking advantage of available services the moment people are ready for treatment is critical. Potential patients can be lost if treatment is not immediately available or readily accessible.
- Effective treatment attends to multiple needs of the individual, not just his or her drug abuse. To be effective, treatment must address the individual’s drug abuse and any associated medical, psychological, social, vocational, and legal problems.
- Remaining in treatment for an adequate period of time is critical. The appropriate duration for an individual depends on the type and degree of his or her problems and needs. Research indicates that most addicted individuals need at least 3 months in treatment to significantly reduce or stop their drug use and that the best outcomes occur with longer durations of treatment.
- Counseling—individual and/or group—and other behavioral therapies are the most commonly used forms of drug abuse treatment. Behavioral therapies vary in their focus and may involve addressing a patient’s motivations to change, building skills to resist drug use, replacing drug-using activities with constructive and rewarding activities, improving problem solving skills, and facilitating better interpersonal relationships.
- Medications are an important element of treatment for many patients, especially when combined with counseling and other behavioral therapies. For example, methadone and buprenorphine are effective in helping individuals addicted to heroin or other opioids stabilize their lives and reduce their illicit drug use. Also, for persons addicted to nicotine, a nicotine replacement product (nicotine patches or gum) or an oral medication (bupropion or varenicline), can be an effective component of treatment when part of a comprehensive behavioral treatment program.
- An individual’s treatment and services plan must be assessed continually and modified as necessary to ensure it meets his or her changing needs. A patient may require varying combinations of services and treatment components during the course of treatment and recovery. In addition to counseling or psychotherapy, a patient may require medication, medical services, family therapy, parenting instruction, vocational rehabilitation and/or social and legal services. For many patients, a continuing care approach provides the best results, with treatment intensity varying according to a person’s changing needs.
- Many drug-addicted individuals also have other mental disorders. Because drug abuse and addiction—both of which are mental disorders—often co-occur with other mental illnesses, patients presenting with one condition should be assessed for the other(s). And when these problems co-occur, treatment should address both (or all), including the use of medications as appropriate.
- Medically assisted detoxification is only the first stage of addiction treatment and by itself does little to change long-term drug abuse. Although medically assisted detoxification can safely manage the acute physical symptoms of withdrawal, detoxification alone is rarely sufficient to help addicted individuals achieve long-term abstinence. Thus, patients should be encouraged to continue drug treatment following detoxification.
- Treatment does not need to be voluntary to be effective. Sanctions or enticements from family, employment settings, and/or the criminal justice system can significantly increase treatment entry, retention rates, and the ultimate success of drug treatment interventions.
- Drug use during treatment must be monitored continuously, as relapses during treatment do occur. Knowing their drug use is being monitored can be a powerful incentive for patients and can help them withstand urges to use drugs. Monitoring also provides an early indication of a return to drug use, signaling a possible need to adjust an individual’s treatment plan to better meet his or her needs.
- Treatment programs should assess patients for the presence of HIV/AIDS, hepatitis B and C, tuberculosis, and other infectious diseases, as well as provide targeted risk-reduction counseling to help patients modify or change behaviors that place them at risk of contracting or spreading infectious diseases. Targeted counseling specifically focused on reducing infectious disease risk can help patients further reduce or avoid substance-related and other high-risk behaviors. Treatment providers should encourage and support HIV screening and inform patients that highly active antiretroviral therapy (HAART) has proven effective in combating HIV, including among drug-abusing populations.
______
Types of drug treatment programs:
- Residential treatment:
Residential treatment involves living at a facility and getting away from work, school, family, friends, and addiction triggers while undergoing intensive treatment. Inpatient drug abuse rehab allows an addict to fully focus on his or her recovery in an intensive treatment environment. Residential treatment can last from a few days to several months. Most American programs follow a traditional 28–30 day program length. The length is based solely upon providers’ experience. 70% to 80% of American residential alcohol treatment programs provide 12-step support services. These include, but are not limited to AA, Narcotics Anonymous, Cocaine Anonymous and Al-Anon. One recent study suggests the importance of family participation in residential treatment patient retention, finding “increased program completion rate for those with a family member or significant other involved in a seven-day family program.”
Long-Term Treatment:
In some cases, long-term residential treatment for drug abuse is necessary for some to develop their readiness for reintegration into their daily lives. Drug addicts who have already attended a standard treatment program but have relapsed may respond better to therapeutic communities. These treatment centers often involve a 6- to 12-month stay. They focus on helping addicts re-socialize by developing socially productive lives while maintaining personal accountability.
The National Institute on Drug Abuse notes that drug treatment programs that last less than 90 days have limited effectiveness, but many people benefit from longer treatment periods and several different levels of treatment. It is common for addicts to attend short-term inpatient treatment programs but later transition into a longer-term outpatient treatment program.
- Day treatment/Partial hospitalization:
Partial hospitalization is for people who require ongoing medical monitoring but wish to still live at home and have a stable living environment. These treatment programs usually meet at a treatment center for 7 to 8 hours during the day, then you return home at night.
- Outpatient treatment:
Not a live-in treatment program, these outpatient programs can be scheduled around work or school. You’re treated during the day or evening but don’t stay overnight. The major focus is relapse prevention. Outpatient drug abuse treatment can guide some people through all stages of their recovery. However, some recovering individuals will fare better using outpatient treatment as a step-down level of care after completing an inpatient program.
- Sober living communities:
Living in a sober house normally follows an intensive treatment program such as residential treatment. You live with other recovering addicts in a safe, supportive, and drug-free environment. Sober living facilities are useful if you have nowhere to go or you’re worried that returning home too soon will lead to relapse.
______
Drug rehabilitation:
Drug rehabilitation is the process of medical or psychotherapeutic treatment for dependency on psychoactive substances such as alcohol, prescription drugs, and street drugs such as marijuana, cocaine, heroin or amphetamines. The general intent is to enable the patient to confront substance dependence, if present, and cease substance abuse to avoid the psychological, legal, financial, social, and physical consequences that can be caused, especially by extreme abuse. Treatment includes medication for depression or other disorders, counseling by experts and sharing of experience with other addicts.
______
Five Steps of drug addiction Treatment:
- Detoxification: Usually the first step is to purge your body of drugs and manage withdrawal symptoms.
- Behavioral counseling: Individual, group, and/or family therapy can help you identify the root causes of your drug use, repair your relationships, and learn healthier coping skills.
- Medication-assisted treatment: Medication may be used to manage withdrawal symptoms, prevent relapse, or treat any co-occurring mental health condition such as depression or anxiety.
- Evaluation and treatment for co-occurring disorders.
- Long-term plan for relapse prevention: Long-term follow-up can help to prevent relapse and maintain sobriety. This may include attending regular in-person support groups or online meetings to help keep your recovery on track.
Every patient has different treatment needs, so it is important to have a specialized treatment plan. Some people may resist drug treatment and refuse to go to a rehabilitation facility. If necessary, family members, employers or the criminal justice system can require them to get treatment.
_____
Treatments currently available for addiction include both pharmacological interventions as well as behavioral methods. With the variety of brain regions available as targets from treatment, most of these pharmacological interventions aim to accomplish three things: reduce drug craving, increase cognitive control and/or decrease the enhanced stress reactivity and negative moods. Medications that are aimed at attenuating the drug cravings include naltrexone, methadone, varenicline, bupropion, baclofen, amisulpride, and aripiprazole (Konova et al. 2013; Young et al. 2014; Hermann et al. 2006; Myrick et al. 2010). Treatments that aim to increase cognitive control in order to normalize performance include N-acetylcysteine and modafinil (Schmaal et al. 2012; Schmaal et al. 2014). Some of these medications, specifically varenicline and modafinil, were shown to both attenuate craving and improve cognitive performance (Wheelock et al. 2014; Goudriaan et al. 2013). Additionally, antidepressants are used to improve negative moods which are associated with addiction and which significantly contribute to relapse.
_
Imaging studies have corroborated the role of dopamine in the reinforcing effects of drugs of abuse in human beings and have extended traditional views of dopamine involvement in drug addiction. These findings suggest multicomponent strategies for the treatment of drug addiction that include strategies to (1) decrease the reward value of the drug of choice and increase the reward value of nondrug reinforcers, (2) weaken conditioned drug behaviors, (3) weaken the motivational drive to take the drug, and (4) strengthen frontal inhibitory and executive control (see table below).
The table above shows synopsis of pharmacological interventions in drug addiction.
_
Types of behavioral therapy include:
- Cognitive-behavioral therapy, which seeks to help patients to recognize, avoid and cope with situations in which they are most likely to relapse.
- Multidimensional family therapy, which is designed to support recovery of the patient by improving family functioning.
- Motivational interviewing, which is designed to increase patient motivation to change behavior and enter treatment.
- Motivational incentives, which uses positive reinforcement to encourage abstinence from the addictive substance.
_
Behavioral approaches to abstinence include motivation enhancement, cognitive bias modification and virtual reality trainings (Wiers et al. 2015b; Son et al. 2015). Neuromodulatory interventions include neurofeedback and transcranial magnetic stimulation. Recently investigated treatment includes the use of real time fMRI neurofeedback where participants are shown the activation of certain regions and asked to manipulate the activation in a certain direction (Li et al. 2013). The use of neuroimaging techniques in capturing treatment effects may provide insight into neurobiological mechanisms of the treatment in the pathology of addiction, which is a unique benefit over behavioral outcome measures of treatment. In addition, neuroimaging may be more sensitive than behavioral measures in detecting effects of treatment (Linden 2012). Repetitive transcranial magnetic stimulation (rTMS) is a noninvasive brain stimulation technique that has been assessed in a growing number of studies for its therapeutic potential in treating addiction.
_____
Family-Based Approaches:
Family-based approaches to treating adolescent substance abuse highlight the need to engage the family, including parents, siblings, and sometimes peers, in the adolescent’s treatment. Involving the family can be particularly important, as the adolescent will often be living with at least one parent and be subject to the parent’s controls, rules, and/or supports. Family-based approaches generally address a wide array of problems in addition to the young person’s substance problems, including family communication and conflict; other co-occurring behavioral, mental health, and learning disorders; problems with school or work attendance; and peer networks. Research shows that family-based treatments are highly efficacious; some studies even suggest they are superior to other individual and group treatment approaches. Typically offered in outpatient settings, family treatments have also been tested successfully in higher-intensity settings such as residential and intensive outpatient programs.
_____
Substance Abuse Services:
Substance abuse services are also most effective when combined with services that aid a recovering individual in managing other aspects of their life. Substance abuse services can be found through private- and public-funded treatment programs. Using specific substance abuse services, such as substance use monitoring or pharmacotherapy, may be a required part of your long-term treatment program. Some services also offer counseling and individual therapy to patients who have finished a residential treatment program but still need regular support. Substance abuse services are also most effective when combined with services that aid a recovering individual in managing other aspects of their life. These services include:
- Medical services.
- HIV/AIDS services.
- Financial services.
- Family services.
- Vocational services.
- Mental health services.
- Educational services.
- Legal services.
- Childcare services.
- Housing/transportation services.
_______
Drug Abuse Hotline:
Cravings can happen anytime. They don’t always occur at convenient times, such as during a therapy appointment or a 12-step meeting. Much of the time, the urge to get drunk or high is pretty inconvenient, and occurs when there’s no one around to talk to about the craving while waiting for it to pass. This is when a drug abuse hotline can be most helpful. When you are fighting off the urge to relapse, immediate help is essential. You may not have the luxury of waiting for a therapist, sponsor, close friend or family member to call you back. There may be no self-help meetings nearby at that specific time. You need help immediately – and there’s nothing more immediate than a phone call to a drug abuse hotline.
In addition to the immediate gratification, you get:
- Anonymity. Everything you say on the phone to your drug abuse hotline operator stays between you and the person on the other end of the line.
- No charge. You pay nothing to call a toll-free drug abuse hotline and you can talk as long as you need to about your cravings or what happened that made you want to relapse.
- Connection to treatment resources. Staff members at drug abuse hotlines are knowledgeable about the different types of addiction treatment available. If you have relapsed or fear that you are going to, the counselor you call at the drug abuse hotline can help to determine what kind of treatment will help you to avoid falling back into an active addiction.
______
Computer-based interventions:
New technologies of drug addiction assessment, treatment, and research, such as computer-based methodologies, appear to be cost-effective, efficacious, and accessible. For example, drug-dependent individuals reported being more responsive to a computer-based HIV/AIDS information program than a standard counsellor-led intervention. Computer-based interventions were also found to increase new mothers’ motivation for abstinence and have similar levels of alliance building as therapist interventions. However, it needs to be noted that computer-based therapies may not be suited to all patients; some may prefer and respond better to an interaction with a therapist who is in the same room, while others may not be used to computer-based technologies which may cause them to focus on the operation and delivery of the treatment and be less engaged with the program’s content (Magura, 2000). Another consideration is whether the present circumstances of the patient require an immediate intervention by the therapist, for example, when they are an immediate danger to themselves or to others. In these situations the physical presence of the therapist would be more appropriate.
______
Telehealth in drug addiction:
Telehealth involves the use of technologies such as telephone-based services, videoconferencing, texting, smartphone applications and web-based tools to provide care over a distance without requiring patients to travel to a clinic or provider’s office. For some, the term telemedicine is considered the clinical use of technology while telehealth refers to a more widespread approach that includes products or services aimed directly at consumers. More recently, these terms are used interchangeably.
Telehealth Applications for drug addiction:
A variety of electronic delivery methods are increasing the use of telehealth in addiction treatment and recovery including:
- Telephone-based support: One of the earliest methods of delivering telehealth services, telephone-based care has been used to provide continuing care for substance use disorders. Study results for telephone-based continuing care generally show better results than traditional continuing care.
- Videoconferencing: Videoconferencing occurs through secure portals on personal computers or dedicated telemedicine equipment. Studies on videoconferencing for addiction services have found equivalent results and patient satisfaction compared with care provided in person or by video. Meta-analyses of videoconferencing for psychiatry services have found similar positive results.
- Texting: Texting is the transmission of short electronic messages between mobile devices. Positive results have been attributed to texting interventions using mobile device apps. Text messaging-based addiction treatment is inexpensive and has the potential to be widely accessible in real time.
- Mobile apps: A mobile app is a software application developed specifically for use on computing devices such as smartphones and tablets. An early analysis that examined several studies on mobile device use in overall health care determined it is too early to generalize the effectiveness of this technology. However, research on one smartphone app found reduced risky drinking days and higher abstinence rates than usual care. Research on another mobile app showed reduced hazardous drinking days and drinks per day.
- Web-based treatment supports: Patients access web-based services over a network connection. These applications are typically “asynchronous,” meaning that people can access them any time, at their convenience. Overall, web-based telemedicine services have been found to be more effective at reducing alcohol consumed per week than comparison conditions.
- Virtual reality: Virtual reality allows an individual to explore and interact with a computer-generated experience that simulates a real-life environment. Research using virtual reality has shown that drug-dependent people react with strong cravings to specific cues (e.g., cigarette packs, liquor bottles) as well as environments or settings (e.g., bar, party) that are associated with drug use. The ability to bring forth feelings of cravings could mean that virtual reality has the potential to be successfully used in treatment, though this has not yet been rigorously demonstrated.
______
Substitution therapy:
_
Approximately 10% of new HIV infections worldwide are attributable to injecting drug use, often of an opiate such as heroin. Opioid substitution therapy supplies illicit drug users with a replacement drug, a prescribed medicine such as methadone or buprenorphine, which is usually administered orally in a supervised clinical setting. The effectiveness of this therapy is recognized in developed countries, where the provision of opioid substitutes to opiate-dependent people is a fundamental component of the response to the dual public health problems of injecting drug use and HIV transmission. However, better prevention of HIV transmission among and from injecting drug users is still needed, especially in resource-poor settings.
Despite the evidence of effectiveness, it is estimated that only 8% of injecting drug users globally currently receive opioid substitution therapy – even less in developing countries. There is substantial global inequity in access – for example, 90% of injecting drug users in the United Kingdom of Great Britain and Northern Ireland and 69% in Australia are receiving such therapy; compared with 3% in China and India, and none in the Russian Federation, where opioid substitution therapy is not available.
_
Harm reduction for opiate dependency involves prescribing agents that will occupy the opiate receptors much like their opiate addict’s drug of choice, at a dose that will prevent the induction of withdrawal symptoms. It is also believed that by maintaining the saturation of the opiate receptor with an opiate agonist, the euphoric effects or heroin are blunted when taken at the same time. The underlying philosophy of harm reduction is to maintain the individual in a dependent state, but to a drug that is legal (less need to commit crimes to support habit), requires only 1 dose per day (increases functionality and ability to hold a job), administered orally (less risk of HIV or hepatitis infection), and has a less euphorogenic activity (lower risk of diversion and abuse).
Methadone:
The mainstay of this approach has been the drug methadone. Methadone is not without its problems in that, although it has a long half-life and is less euphorogenic than heroin, it can still be abused. It can also cause respiratory depression and other opiate-related side effects, including death by overdose. Because of these risks, methadone is very tightly controlled, and regulated pursuant to the Drug Abuse Treatment Act. Currently, only clinics registered as a methadone maintenance program can dispense methadone for maintenance of opiate addiction. In an attempt to expand the harm reduction model, the FDA has amended the Drug Abuse Treatment Act to allow greater access to opiate replacement therapy. Rather than limit opiate replacement access only to methadone clinics, the amendment allows qualifying physicians to prescribe approved narcotic drugs in schedule III, IV, and V for the treatment of opiate dependence. There are, however, specific requirements that the drug and practitioner have to meet.
Buprenorphine:
The newest agent to be investigated for opiate replacement therapy is the drug buprenorphine. Buprenorphine is a partial mu receptor agonist, meaning it has less intrinsic activity for the mu receptor than a full agonist, and also a kappa receptor antagonist. Buprenorphine has high affinity and slow dissociation from the mu receptor sites. Since buprenorphine has both opiate agonist and antagonist properties, it is believed to have a much lower abuse potential than methadone, yet still able to occupy the opiate receptor site. It is further believed that due to its combined agonist/antagonist properties, there is a ceiling at which the drug is no longer capable of inducing a euphoric response. In fact, it is believed that at higher doses, the antagonist properties will create a dysphoric response. Finally, due to its long duration of action, less-than-daily dosing of buprenorphine may be appropriate.
In the context of harm reduction, buprenorphine is expected to be a safer agent, with less potential for diversion and abuse. While buprenorphine’s safety profile is preferable to that of methadone, it is not without any risk of abuse. One approach to combat the diversion and abuse is combining buprenorphine with naloxone, an opiate antagonist that will induce withdrawal symptoms when injected. Naloxone has very limited oral bioavailability and should not interfere with buprenorphine’s effects when ingested orally.
According to the National Institute on Drug Abuse (NIDA), patients stabilized on adequate, sustained doses of methadone or buprenorphine can keep their jobs, avoid crime and violence, and reduce their exposure to HIV and Hepatitis C by stopping or reducing injection drug use and drug-related high-risk sexual behavior.
_
A 2018 study concluded that Heroin-assisted treatment is more effective for people with opioid dependence who continue intravenous heroin while on methadone maintenance or who are not enrolled in treatment. Despite a higher risk, it should be considered for treatment resistance under medical supervision.
______
Stimulant maintenance:
Stimulant maintenance is the medical practice of prescribing stimulant drugs such as cocaine or amphetamines to people who are dependent on these drugs. Supporters of stimulant maintenance believe that prescription offers legal alternatives to people who would otherwise be purchasing impure drugs in unknown potency and concentration, unnecessarily risking their health and supporting an illegal market that fuels organized crime. This practice is being tried in Canada for methamphetamine addicts.
_____
Other Medications:
Naltrexone is a long-acting opioid antagonist with few side effects. It is usually prescribed in outpatient medical conditions. Naltrexone blocks the euphoric effects of alcohol and opiates. Naltrexone cuts relapse risk during the first three months by about 36%. However, it is far less effective in helping patients maintain abstinence or retaining them in the drug-treatment system (retention rates average 12% at 90 days for naltrexone, average 57% at 90 days for buprenorphine, average 61% at 90 days for methadone).
Ibogaine is a hallucinogenic drug promoted by certain fringe groups to interrupt both physical dependence and psychological craving to a broad range of drugs including narcotics, stimulants, alcohol, and nicotine. To date, there have never been any controlled studies showing it to be effective, and it is not accepted as a treatment by physicians, pharmacists, or addiction specialists. There have also been several deaths related to ibogaine use, which causes tachycardia and long QT syndrome. The drug is an illegal Schedule I controlled substance in the United States, and the foreign facilities in which it is administered from tend to have little oversight, and range from motel rooms to one moderately-sized rehabilitation center.
A few antidepressants have been proven to be helpful in the context of smoking cessation/nicotine addiction, these medications include bupropion and nortriptyline. Bupropion inhibits the re-uptake of nor-epinephrine and dopamine and has been FDA approved for smoking cessation, while nortriptyline is a tricyclic antidepressant which has been used to aid in smoking cessation but it has not been FDA approved for this indication.
Acamprosate, disulfiram and topiramate (a novel anticonvulsant sulphonated sugar) are also used to treat alcohol addiction. Acamprosate has shown effectiveness for patients with severe dependence, helping them to maintain abstinence for several weeks, even months. Disulfiram (also called Antabuse) produces a very unpleasant reaction when drinking alcohol that includes flushing, nausea and palpitations. It is more effective for patients with high motivation and some addicts use it only for high-risk situations. Patients who wish to continue drinking or may be likely to relapse, should not take disulfiram as it can result in the disulfiram-alcohol reaction, which is very serious and can even be fatal.
Nitrous oxide, also sometimes known as laughing gas, is a legally available gas used for purposes that include anaesthesia during certain dental and surgical procedures, as well as food preparation and the fueling of rocket and racing engines. Substance abusers also sometimes use the gas as an inhalant. Like all other inhalants, it’s popular because it provides consciousness-altering effects while allowing users to avoid some of the legal issues surrounding illicit or illegal drugs of abuse. Abuse of nitrogenous oxide can produce significant short-term and long-term damage to human health, including a form of oxygen starvation, called hypoxia, brain damage, and a serious vitamin B12 deficiency that can lead to nerve damage. Although dangerous and addictive in its own right, nitrogenous oxide has been shown to be an effective treatment for a number of addictions.
Varenicline is a prescription medication used to treat nicotine addiction. It reduces both craving for and decreases the pleasurable effects of cigarettes and other tobacco products. It is a high-affinity partial agonist for the α4β2 nicotinic acetylcholine receptor subtype (nACh) that leads to the release of dopamine in the nucleus accumbens when activated, and therefore, has the capacity to reduce the feelings of craving and withdrawal caused by smoking cessation.
Since addiction involves abnormalities in glutamate and GABAergic neurotransmission, receptors associated with these neurotransmitters (e.g., AMPA receptors, NMDA receptors, and GABAB receptors) are potential therapeutic targets for addictions. N-acetylcysteine, which affects metabotropic glutamate receptors and NMDA receptors, has shown some benefit in preclinical and clinical studies involving addictions to cocaine, heroin, and cannabinoids. It may also be useful as an adjunct therapy for addictions to amphetamine-type stimulants, but more clinical research is required.
ΔFosB inhibitors (drugs or treatments that oppose its action or reduce its expression) may be an effective treatment for addiction and addictive disorders. Current medical reviews of research involving lab animals have identified a drug class – class I histone deacetylase inhibitors – that indirectly inhibits the function and further increases in the expression of accumbal ΔFosB by inducing G9a expression in the nucleus accumbens after prolonged use. These reviews and subsequent preliminary evidence which used oral administration or intraperitoneal administration of the sodium salt of butyric acid or other class I HDAC inhibitors for an extended period indicate that these drugs have efficacy in reducing addictive behavior in lab animals that have developed addictions to ethanol, psychostimulants (i.e., amphetamine and cocaine), nicotine, and opiates; however, as of 2015 however, few clinical trials involving human addicts and any HDAC class I inhibitors have been conducted to test for treatment efficacy in humans or identify an optimal dosing regimen.
_____
Prognosis for Substance Abuse:
Individuals who suffer from substance abuse tend to be more successful in recovery when they are highly motivated to be in treatment, are actively engaged in their own recovery, and receive intensive treatment services. Prognosis for substance abuse recovery is further improved by being able to easily access community-based social supports.
_____
Naloxone for heroin overdose:
Fatal heroin overdose among injection drug users (IDUs) is a rapidly growing public health problem, representing one of the highest causes of preventable death in U.S. areas where heroin injection is widespread. The epidemiology of morbidity and mortality associated with overdose has been gaining overdue attention. Analysis suggests that overdose incidents typically take place with other users present and that death occurs 1–3 hours after the initial injection. This allows ample opportunity for medical intervention to prevent fatalities through the administration of naloxone, a safe and effective opiate antagonist. A generically-manufactured agent, naloxone is a Class 3 substance that is typically injected but can also be nasally-administered to a victim of an opiate overdose. This substance lacks any psychoactive or addictive qualities; it merely blocks the effects of opiates without any potential for abuse. On standing orders of a physician, first responders routinely administer naloxone through injection when summoned to the scene of drug overdose. Side effects associated with naloxone treatment for opiate overdose are generally rare. An initial dose of 400 to 2000 micrograms (0.4mg to 2mg) of naloxone may be given intravenously and may, if required, be repeated at 2 to 3 minute intervals in opioid overdosage of adults (known or suspected). The diagnosis of opioid-related toxicity should be reconsidered if there is still failure to respond after a total of 10mg of naloxone has been administered. If intravenous administration is impracticable, naloxone may be administered by the intramuscular or subcutaneous route. The duration of action of some opioids (including dextropropoxyphene, dihydrocodeine and methadone) may exceed that of naloxone. In these circumstances, an intravenous infusion of naloxone will provide sustained antagonism of the opioid and obviate the need for repeated injections.
Too often, timely medical attention is not provided to victims of opiate overdose. Witnesses may fail to summon help for fear of legal repercussions to self or to the victim, or mistrust of the medical system. Equipping drug users with naloxone for administration in the event of an overdose has been introduced in several areas in the United States as well as internationally, with positive results. Naloxone distribution programs have been associated with a drastic reduction in the number of overdose deaths in a community.
______
Exercise as a Treatment for Drug Addiction:
Physical activity, and specifically exercise, is a potential non-pharmacological treatment for addiction that targets systems implicated in both early and late stages of the addiction process and has secondary health benefits (e.g., prevention of obesity and secondary diseases such as diabetes). Mechanistically, physical activity and exercise activate the same reward pathway as drugs of abuse, through increases in dopamine concentrations and dopamine receptor binding (Greenwood et al., 2011; MacRae et al., 1987). These effects may be particularly beneficial at preventing drug use and reducing initial vulnerability to drug use. Physical activity and exercise also decrease glutamate in the striatum (Guezennec et al., 1998), which may protect against overstimulation of glutamatergic receptors following chronic drug exposure. Exercise may also influence brain plasticity through mechanisms centered on remodeling of chromatin at regions that are implicated in drug addiction (Gomez-Pinilla et al., 2011; Chase and Sharma, 2012; Kumar et al., 2005; Sadri-Vakili et al., 2010; Vassoler et al., 2013; Wan et al., 2011).
Despite promising results, certain exercise conditions may be either ineffective or lead to detrimental effects. Exercise itself can also become addictive for some individuals, which is not surprising given that it activates many of the same circuits as drugs of abuse. Such evidence underscores the importance of developing a complete understanding of the exercise parameters that produce a beneficial response. Future studies are also needed to characterize the neurobiological mechanisms by which exercise, alone or in combination with other treatments, exerts its efficacy as a function of stage of the addiction process. For example, the beneficial effects of exercise may be augmented during withdrawal if combined with a low dose of a dopamine agonist (i.e., to reduce the likelihood of adverse side effects), and following prolonged abstinence when combined with a glutamate receptor antagonist (i.e., to further block glutamatergic signaling that is heightened at this time). Such a neurobiological-behavioral response pattern or “finger-print” would enable us to identify conditions that produce the most efficacious response, as well as enable us to understand which of its properties can be harnessed to develop even more efficacious treatments.
_____
Drug vaccines:
Research indicates that vaccines which utilize anti-drug monoclonal antibodies can mitigate drug-induced positive reinforcement by preventing the drug from moving across the blood–brain barrier; however, current vaccine-based therapies are only effective in a relatively small subset of individuals. As of November 2015, vaccine-based therapies are being tested in human clinical trials as a treatment for addiction and preventative measure against drug overdoses involving nicotine, cocaine, and methamphetamine.
Addictive drugs are small molecules that are not highly immunogenic. Though the immune system does not readily produce good antibodies directed against addictive drugs, this hurdle is being addressed. Active vaccination strategies conjugate the addictive drug to adenovirus capsid proteins, which are highly immunogenic. Cocaine vaccine is developed by conjugating the cocaine analog GNE to adenovirus that has been denatured so that it cannot replicate. The vaccine, dAd5GNE, can engender high anticocaine antibody titers in both rodent and nonhuman primate models. The vaccine prevents cocaine distribution in the brain in rodent models, even with frequent administration and at very high doses. It also reduces cocaine self‐administration in nonhuman primates. A phase 1 clinical trial is underway in human cocaine users. Participants receive 6 monthly injections of either conjugate vaccine or placebo. The study will investigate the ability of three different vaccine doses to produce anticocaine antibodies and will assess safety.
In passive immunization approaches, expression of a gene that encodes an anticocaine antibody is delivered to the liver using an adeno‐associated virus vector. Transfection with the AAvrh.10 vector containing this anticocaine antibody gene can produce high, persistent anticocaine antibody titers following a single administration to animals. In mice, AAvrh.10 reduced cocaine levels in the brain and reduced cocaine‐induced hyperactivity for periods of months after the transfection.
____
Gene therapy:
Gene therapy for addiction is an active area of research. One line of gene therapy research involves the use of viral vectors to increase the expression of dopamine D2 receptor proteins in the brain.
_____
Chemogenetics in addiction:
Ion channels are switches through cell membranes that can control the passage of small electrical ions into and out of the cell. When activated or inhibited by drugs, these switches can increase or decrease the cell’s function. Scientists are using such switches to develop a variety of new ways for manipulating neurons to study the brain and to ultimately correct malfunctioning brain activity associated with addiction and other diseases. Optogenetics, for example, uses light to activate light-sensitive ion channels to manipulate neurons. Chemogenetics, however, uses designer chemicals and engineered ion channels that exclusively respond to these chemicals to alter neuronal activity.
Magnus et al. designed chemogenetic ion channels that improve currently available systems and are activated by the clinically used antismoking drug varenicline. They engineered a ligand-binding domain less responsive to endogenous signals and identified agonists that function at nanomolar concentrations. The combination of drug and introduced channels transiently silenced neurons, with slow but effective washout, and induced behavioral changes in animal models after brain administration.
______
Deep brain stimulation in addiction:
While optogenetics has proven to be a useful tool in the laboratory, it is currently less feasible as a treatment in humans. Deep brain stimulation (DBS) involves sending electrical impulses to specific areas of the brain via implanted electrodes. DBS is currently used in the treatment of a number of neurological conditions, especially Parkinson’s disease, but also epilepsy and OCD.
Meaghan Creed (University of Geneva) uses DBS to depotentiate synapses in the nucleus accumbens. DBS has been shown to be effective in abolishing some of the neurological and behavioral effects of cocaine in mice. The background for this work comes from findings that addictive drugs alter both the quality and the quantity of synaptic transmission in the D1 receptor expressing spiny neurons of the nucleus accumbens. These changes persist long after the drug is out of the system.
_______
_______
Beneficial aspects of psychoactive drugs:
Most of the psychoactive drugs now prohibited in modern societies have had medical uses in history. In natural plant drugs like opium, coca, cannabis, mescaline, and psilocybin, the medical history usually dates back thousands of years and through a variety of cultures. Psychedelics such as LSD and psilocybin (the main ingredient in most hallucinogenic mushrooms) are the subject of renewed research interest because of their therapeutic potential. They could ease a variety of difficult-to-treat mental illnesses, such as chronic depression, post-traumatic stress disorder, and alcohol dependency. MDMA (Ecstasy) has been used for cognitive enhancement in people with Parkinson’s disease, and has shown potential in treating posttraumatic stress disorder. Any psychoactive drug that is consumed in excess can be harmful. However, there are some types of these drugs that actually do have some benefits.
People who frequently use psychoactive drugs say that they use them because they:
- Allow them to be more sociable
- Give them enjoyment or pleasure
- Improve their state of mind
- Relieve their pain
- Relieve their depression or anxiety
- Help them feel more relaxed
- Relieve their stress
- Help them lose weight
- Provide more energy
- Improve sleep
- Improve memory, attention and concentration
Even so, it must be stated that any time a psychoactive drug is misused, there are consequences. The abuse of psychotropic drugs can provide all of these and other benefits. However, those benefits are quite likely to be short-lived. With ongoing abuse, the negative effects of these drugs are likely to become much more pronounced. This is true whether a drug is considered to be socially acceptable, or whether it is prescribed or illegal.
According to Janet D. Lapey, M.D., of Concerned Citizens For Drug Prevention, “Due to a placebo effect, a patient may erroneously believe a drug is helpful when it is not. This is especially true of addictive, mind-altering drugs like marijuana. A marijuana withdrawal syndrome occurs, consisting of anxiety, depression, sleep and appetite disturbances, irritability, tremors, diaphoresis, nausea, muscle convulsions, and restlessness. Often, persons using marijuana erroneously believe that the drug is helping them combat these symptoms without realizing that actually marijuana is the cause of these effects. Therefore, when a patient anecdotally reports a drug to have medicinal value, this must be followed by objective scientific studies.”
The US Drug Enforcement Administration also says:
“There is a growing misconception that some illegal drugs can be taken safely. For example, savvy drug dealers have learned how to market drugs like Ecstasy to youth. Some in the Legalization Lobby even claim such drugs have medical value, despite the lack of conclusive scientific evidence.”
_______
Hallucinogens fall into several different classes, as broadly defined by pharmacological mechanism of action, and chemical structure. These include psychedelics, entactogens, dissociatives, and other atypical hallucinogens. Although these classes do not share a common primary mechanism of action, they do exhibit important similarities in their ability to occasion temporary but profound alterations of consciousness, involving acute changes in somatic, perceptual, cognitive, and affective processes. Such effects likely contribute to their recreational use. However, a growing body of evidence indicates that these drugs may have therapeutic applications beyond their potential for abuse.
Summary of hallucinogens and potential clinical applications:
Psychedelics:
These are a group of serotonergic agonists that are currently classified as Schedule I substances. Some, including psilocybin, peyote (mescaline) and the DMT containing admixture ayahuasca, have been used for hundreds to thousands of years for religious purposes by indigenous cultures (Guerra-Doce, 2015). Preliminary evidence indicates one or more of these may be useful in treating cluster headache (Sewell et al., 2006), substance use disorders (Bogenschutz et al., 2015; Johnson et al., 2014; Krebs & Johanesen, 2012; Savage & McCabe, 1973), end-of-life anxiety and potentially depression (Carhart-Harris et al., 2016; Gasser et al., 2014; Grob et al., 2010), and obsessive compulsive disorder (Moreno et al., 2009).
Entactogens:
These are a group of Schedule I monoamine releasers and reuptake inhibitors known for their ability to evoke a sense of emotional openness and connection (Nichols, 1986). MDMA in particular has shown potential therapeutic benefits in post-traumatic stress disorder (PTSD; Mithoefer et al., 2011, 2012), and is being evaluated as a treatment for social anxiety in adults with autism spectrum disorders (Danforth et al., 2015), and end-of-life anxiety.
Dissociatives:
These are a group of glutamatergic NMDAe antagonists that are either unscheduled (DXM and N2O), or restricted but available for use as anesthetics (ketamine), and whose additional therapeutic uses are currently being explored in a variety of areas including depression (Abdallah et al., 2015a; Nagele et al., 2015; Nguyen et al., 2014), and substance use disorders (Krupitsky et al. 1992; 2007; Krupitsky & Grinenko, 1997; 1998).
Atypical:
These are a group of unrelated, pharmacologically distinct substances with some hallucinogenic properties, exhibiting diverse mechanisms of action, legal status, and therapeutic potentials. Ibogaine (Schedule I, US) acts as a serotonin 2A agonist, MOR g agonist, KOR h antagonist, and NMDA antagonist, displaying potentials as an anti-addiction agent, particularly for opioids (Alper et al., 1999; Schenberg et al., 2014). The unscheduled KOR agonist Salvinorin A exhibits preclinical evidence for potential in treating addiction (Butelman & Kreek, 2015; Freeman et al., 2014). The CB 1 receptor agonist THC is the main psychoactive chemical in cannabis, and has recognized therapeutic utility for nausea and vomiting due to chemotherapy, chronic neuropathic or cancer pain, and spasticity due to multiple sclerosis (Whiting et al., 2015). Many other cannabinoids and terpenes are present in whole plant cannabis and are being explored for their own therapeutic purposes (e.g., Devinsky et al., 2014). Cannabis and cannabinoids are currently undergoing a major shift in legal status, and range from Schedule I to unscheduled.
_
Psychedelic microdosing:
Psychedelic microdosing is a practice to use sub-threshold doses of psychedelic drugs in an attempt to improve creativity, boost physical energy level, emotional balance, increase performance on problems-solving tasks and to treat anxiety, depression and addiction. A microdose is usually a tenth of an active dose of psychedelic drugs. This practice has become more widespread in the 21st century. In 2018, a group of scientists at Imperial College London announced a self-blinding study recruiting volunteers across the globe via Internet, using questionnaires and games to evaluate psychological well-being and cognitive function effects of psychedelic microdosing.
_
Psychedelic therapy:
Psychedelic therapy refers to therapeutic practices involving psychedelic drugs, oftentimes utilizing serotonergic psychedelics such as LSD, psilocybin, DMT, MDMA, mescaline, and 2C-B. Psychedelic therapy, in contrast to conventional psychiatric medication taken by the patient regularly or as-needed, patients generally remain in an extended psychotherapy session during the acute psychedelic activity with additional sessions both before and after in order to help integrate experiences with the drug.
Psychedelic substances which may have therapeutic uses include psilocybin (the main active compound found in magic mushrooms), LSD, and mescaline (the main active compound in the peyote cactus). Although the history behind these substances has hindered research into their potential medicinal value, scientists are now able to conduct studies and renew research that was halted in the 1970s. Some research has shown that these substances have helped people with such mental disorders as obsessive-compulsive disorder, post-traumatic stress disorder, alcoholism, depression, and cluster headaches. Some of the well known particular psychedelic substances that have been used to this day are: LSD, DMT, psilocybin, mescaline, 2C-B, 2C-I, 5-MeO-DMT, AMT, ibogaine and DOM. In general, however, the drugs remain poorly understood. Their effects are strongly dependent on the environment in which they are given and on the recipient’s state of mind.
_
Concord Prison Experiment:
The Concord Prison Experiment was designed to evaluate whether the experiences produced by the psychoactive drug psilocybin, derived from psilocybin mushrooms, combined with psychotherapy, could inspire prisoners to leave their antisocial lifestyles behind once they were released. How well it worked was to be judged by comparing the recidivism rate of subjects who received psilocybin with the average for other Concord inmates. The failure of the Concord Prison Experiment to generate a reduction in recidivism rates should not be interpreted as proof of the lack of value of psychedelics as adjuncts to psychotherapy in criminals. Rather, the failure of the Concord Prison Experiment should finally put to rest the myth of psychedelic drugs as magic bullets, the ingestion of which will automatically confer wisdom and create lasting change after just one or even a few experiences. Personality change may be made more likely after a cathartic and insightful psychedelic experience, though only sustained hard work after the drug has worn off will serve to anchor and solidify any movement toward healing and behavior change. Psychedelic drug experiences are not sufficient in and of themselves to produce lasting change.
_
Psychedelics and Creativity:
Psychedelics such as LSD and psilocybin are often said to increase creativity. This claim is complex to evaluate — Psychedelics produce other effects that may be mistaken for creativity and creativity itself is hard to measure. Most of the empirical studies that reported increases in creativity after hallucinogen use are old and used methods that would not be accepted in modern psychopharmacology. After decades of disinterest, scientists are again attending to possible beneficial effects of psychedelics (Vollenweider and Kometer, 2010). For example, recent trials of psychedelics in patients with obsessive compulsive disorder, drug dependence, and anxiety have occurred or are underway (New York University, 2010; Grob et al., 2011; Bogenschutz et al., 2015; Johnson et al., 2014) and articles have called for research into psychedelics’ effects on creativity (Sessa, 2008). It is therefore timely to examine the literature on how this difficult-to-understand class of drugs might act as cognitive enhancers and improve creativity (Lanni et al., 2008).
An association of psychedelics and creativity has been noted in a broad range of nonscientific publications. This includes well-known cases of creative individuals who attribute breakthroughs in their work to use of psychedelics, such as Nobel laureate Kerry Mullis (1998) and author Ken Kesey (1996). Architect Kiyo Izumi used LSD for inspiration when designing a hospital in Saskatchewan (Edginton, 2010). Society’s encounter with LSD is believed to have led to innovative albums like the Beach Boys’ Pet Sounds and the Beatles’ Revolver and movies like Easy Rider (DeRogatis, 2003; Benshoff, 2001). Study of illustrator Robert Crumb’s work suggests considerable influence of psychedelics on his style (Jones, 2007). More broadly, Markoff (2005) has argued that the hallucinogen-oriented counterculture had a profound, if difficult to quantify, influence on the early personal computing industry. Along with qualitative descriptions of hallucinogen effects, these anecdotes suggest that psychedelics may facilitate creativity (Sessa, 2008; Dobkin de Rios and Janiger, 2003; ten Berge, 1999; ten Berge, 2002; Krippner, 1985).
However, qualitative impressions are not always confirmed when quantitative assessments are made and there are reasons to be skeptical about the perceived effects of psychedelics on creativity. Objective tests consistently find hallucinogen-induced impairments in other cognitive domains and these impairment are often accompanied by the erroneous belief that the impaired abilities are enhanced (Hollister, 1968). It is not clear if we should expect creativity to be an exception to this pattern of objective impairments with subjective feelings of improvement. In fact, the “seeming clarity and portentous quality” of thought during hallucinogen effects can include things that later seem trivial to the same person (Jaffe, 1990), which seems consistent with an impaired sense of significance. Even when there are persisting feelings of profound significance after the drug wears off, McGlothlin (1962) points out that the impressively powerful acute effects of psychedelics might lead to a halo effect and exaggerated estimation of benefits.
Psychedelics have unique and powerful effects and yet, only have religious and experimental use. The reported effects of psychedelics on creativity suggest other potential socially important uses for these drugs. Yet controlled research on psychedelics and creativity is lacking and available results are unimpressive. Rather than looking to this limited literature for answers, it may be more informative to conduct qualitative research to document how individuals use psychedelics to enhance their creativity or gain other perceived benefits. Ultimately, creativity may not be the most appropriate construct for characterizing either the acute or long-term changes that people often report after psychedelic exposure. Hallucinogen-induced feelings of creativity may be an inconsistent by-product of more fundamental cognitive changes, such as alterations in activation of representations or changes in Bayesian inference. Research on the effects of these drugs using these paradigms may provide insights into the drugs’ sometime profound impact on individuals.
_
Psychedelics and Mysticism:
The claim has been made that the experience facilitated by psychedelic drugs, such as LSD, psilocybin, and mescaline, can be similar or identical to the experience described by the mystics of all ages, cultures, and religions. There is a long and continuing history of the religious use of plants that contain psychedelic substances. In some instances, such natural products were ingested by a priest, shaman, or witch doctor to induce a trance for revelatory purposes; sometimes they were taken by groups of people who participated in sacred ceremonies. For example, the dried heads of the peyote cactus, whose chief active ingredient is mescaline, were used by the Aztecs at least as early as 300 B.C. and are currently being employed by over fifty thousand Indians of the Native American Church as a vital part of their religious ceremonies. Both ololiuqui, a variety of morning-glory seed, and certain kinds of Mexican mushrooms (called teonanacatl, “flesh of the gods “) were also used for divinatory and religious purposes by the Aztecs. These practices have continued to the present among remote Indian tribes in the mountains of the state of Oaxaca, in Mexico. Modern psychopharmacological research has shown the active chemicals to be psilocybin in the case of the mushrooms, and several compounds closely related to LSD in the case of ololiuqui. Amanita muscaria, the mushroom that has been used for unknown centuries by Siberian shamans to induce religious trances, does not contain psilocybin. The most important psychologically active compound from this mushroom has not yet been isolated, but promising work is in progress. Other naturally occurring plants, which are used by various South American Indian tribes in a religious manner for prophecy, divination, clairvoyance, tribal initiation of male adolescents, or sacred feasts are: cohoba snuff, made from the pulverized seeds of Piptadenia; the drink vinho de Jurumens, made from the seeds of Mimosa hostilis; and the drink caapi, made from Banisteriopsis. These last three products contain various indolic compounds that are all closely related to psilocybin, both structurally and in their psychic effects (bufotenine, dimethyl-tryptamine, and harmine, respectively). Both LSD and psilocybin contain the indolic ring, and mescaline may be metabolized to an indole in the body.
Some of the researchers who have experimented with synthesized mescaline, LSD, or psilocybin have remarked upon the similarity between drug-induced and spontaneous mystical experiences because of the frequency with which some of their subjects have used mystical and religious language to describe their experiences.
______
Cognitive enhancement by psychoactive drugs:
Cognitive enhancement can be defined as the use of drugs and/or other means with the aim to improve the cognitive functions of healthy subjects in particular memory, attention, creativity and intelligence in the absence of any medical indication. Currently, it represents one of the most debated topics in the neuroscience community. Human beings always wanted to use substances to improve their cognitive functions, from the use of hallucinogens in ancient civilizations in an attempt to allow them to better communicate with their gods, to the widespread use of caffeine under various forms (energy drinks, tablets, etc.), to the more recent development of drugs such as stimulants and glutamate activators. In the last ten years, increasing attention has been given to the use of cognitive enhancers, but up to now there is still only a limited amount of information concerning the use, effect and functioning of cognitive enhancement in daily life on healthy subjects.
Some might argue that seeking to improve ourselves is a human trait, and therefore cognitive enhancement is nothing more than our application of new scientific approaches to meet our age-old desire for self-improvement and development. However, others argue that artificially enhancing one’s cognitive abilities is unfair and gives an unbeatable advantage to the richer populations who will have more ready access to the drugs (Butcher, 2003; Cakic, 2009). The issue of cognitive enhancement has even been likened to the steroid debate in sports (Cakic, 2009).
One of the most popular drugs under consideration for cognitive enhancement was originally developed to treat attention deficit-hyperactivity disorder (ADHD). Methylphenidate (MPH) is currently the most commonly prescribed medications for the treatment of ADHD (Challman and Lipsky, 2000; Spiller et al., 2013). MPH is a psychostimulant, related to amphetamine and cocaine and exerts its effects by blocking the transporters that reuptake dopamine and norepinephrine into the presynaptic neuron following their release; thus, it increases the levels or prolongs the availability of these neurotransmitters in the synapses to exert effects on postsynaptic neurons (Kuczenski and Segal, 2005). The dangers of cognitive enhancement with stimulants like MPH lie in their potential effects on the regulation of dopamine and norepinephrine (see figure below). At optimal doses, dopamine binds to higher-affinity D1-like receptors, and norepinephrine binds to α2 receptors, leading to an increase in prefrontal cortical signal-to-noise ratio and enhancing the flow of information and strengthening neuronal communication (Arnsten and Li, 2005). When the levels of dopamine and norepinephrine rise beyond the optimal levels, they begin to activate dopamine D2-class receptors and noradrenergic α1 and β receptors, which leads to weakening of the signal-to-noise ratio via activation of neurons that may not be involved in the current task (Arnsten and Li, 2005; Arnsten, 2009b). This nonspecific activation impairs attentional selectivity and results in a manifestation of locomotor hyperactivity, distractability and poor impulse control.
_
Relationship of dopamine/norepinephrine to prefrontal cortex function:
At lower than optimal levels, the PFC is underactive, and the individual suffers from symptoms of ADHD (impulsivity, poor judgment, inattentiveness, motor hyperactivity). As levels rise, the function improves, until cognition and executive function reaches peak performance at optimal levels of dopamine/norepinephrine. As levels of the neurotransmitters continue to rise past the optimal point, cognition again becomes impaired, with the individual showing distractability, impulsivity, stereotypical behaviors and cognitive inflexibility.
_
Levels of dopamine and norepinephrine in a normal, healthy brain are not universal and they may vary slightly over time within the same individual based on season, time of day, or activity (Otter and Nurmand, 1980; Petrović et al., 1980). Currently, there is no reliable method for determining optimal levels of these neurotransmitters in living human brains; thus, predicting how a certain dose of MPH will affect a particular person is largely an educated approximation. It is also possible that, although many studies found no overt cognitive differences between the effects of low-dose MPH on normal individuals and ADHD patients, molecular or cellular differences may exist that await detection by the development of more advanced technology. Thus, one must examine the research on MPH as a cognitive enhancer and studies using normal individuals with caution.
_
MPH is currently most often abused and sold on the black market among adolescents, particularly in high schools and on college campuses (Goodman, 2010; Franke et al., 2011). Students look for the medication when they have exams, or need to stay awake for long hours, in order to boost their energy and memory. This rather commonplace usage among adolescents is particularly frightening in light of the developmental timeline of the prefrontal cortex. This brain region, the center of control of judgment, behavioral inhibition and emotion, logical thinking and decision making, does not finish developing until young adulthood; in humans this falls around the end of the second decade or the beginning of the third decade of life (Casey et al., 2008). During adolescent development, the levels of norepinephrine and dopamine surge and wane to allow for maturation of the executive control and reward pathways (Kanitz et al., 2011). Introducing a substance that alters dopamine and norepinephrine levels, such as MPH, might disrupt the maturation of the prefrontal cortex and have lasting behavioral consequences.
_
Performance enhancement at the cost of potential brain plasticity: neural ramifications of nootropic drugs in the healthy developing brain, a 2014 study:
Cognitive enhancement is perhaps one of the most intriguing and controversial topics in neuroscience today. Currently, the main classes of drugs used as potential cognitive enhancers include psychostimulants (methylphenidate (MPH), amphetamine), but wakefulness-promoting agents (modafinil) and glutamate activators (ampakine) are also frequently used. Pharmacologically, substances that enhance the components of the memory/learning circuits—dopamine, glutamate (neuronal excitation), and/or norepinephrine—stand to improve brain function in healthy individuals beyond their baseline functioning. In particular, non-medical use of prescription stimulants such as MPH and illicit use of psychostimulants for cognitive enhancement have seen a recent rise among teens and young adults in schools and college campuses. However, this enhancement likely comes with a neuronal, as well as ethical cost. Altering glutamate function via the use of psychostimulants may impair behavioral flexibility, leading to the development and/or potentiation of addictive behaviors. Furthermore, dopamine and norepinephrine do not display linear effects; instead, their modulation of cognitive and neuronal function maps on an inverted-U curve. Healthy individuals run the risk of pushing themselves beyond optimal levels into hyperdopaminergic and hypernoradrenergic states, thus vitiating the very behaviors they are striving to improve. Finally, recent studies have begun to highlight potential damaging effects of stimulant exposure in healthy juveniles. This review explains how the main classes of cognitive enhancing drugs affect the learning and memory circuits, and highlights the potential risks and concerns in healthy individuals, particularly juveniles and adolescents. Authors emphasize the performance enhancement at the potential cost of brain plasticity that is associated with the neural ramifications of nootropic drugs in the healthy developing brain.
_
Does treatment of ADHD with stimulant medications like MPH increase risk of substance abuse later in life?
Prescription stimulants are effective at treating attention disorders in children and adolescents, but concerns have been raised that they could make a young person more vulnerable to developing later substance use disorders. On balance, the studies conducted so far have found no differences in later substance use for ADHD-affected children who received treatment versus those that did not. This suggests that treatment with ADHD medication does not affect (either negatively or positively) an individual’s risk for developing a substance use disorder.
________
Drug use can have social benefits, and acknowledging this could improve rehabilitation, a 2018 study:
Illicit drug use is often framed in terms of risk and antisocial or criminal behaviour. But drug use is often a highly social activity. For many people, the pleasure of using drugs is about social connection as much as it is about the physical effects. A new study aiming to understanding the social benefits of drug use may help us to improve responses to risky or harmful drug taking.
Pleasure is an obvious part of drug use and the short-term physical benefits are well known. Drugs can produce a “high”, give people energy, make them feel good, reduce stress and aid sleep. The social benefits of drug use are more complex to quantify. But there are now numerous studies showing people use alcohol or other drugs in social settings such as bars, clubs and parties to enhance their interactions with others through increased confidence, greater sociability and less anxiety. For some people this leads to longer-term benefits such as stronger bonds with friends. This was shown in recent Australian studies where young people reported cultural gains from drug use, such as strengthening social ties and gaining access to social networks that offered a form of cultural capital. “Party drugs” are those which, as the name suggests, are generally used in a dance party or nightclub setting. This set of drugs often includes MDMA (ecstasy), cocaine, ketamine, gamma hydroxybutyrate (GHB), methamphetamine (speed) or crystal methamphetamine (crystal meth or ice). Studies have shown people generally use party drugs to give them energy, help them socialise and have fun.
At La Trobe University, authors recently conducted a study which explored party drug use – including use of crystal meth – among Australian gay and bisexual men who are living with HIV. Consistent with what authors know about party-drug use, they found the men in this study almost always used party drugs socially – at nightclubs and dance parties or to facilitate sexual pleasure. More surprisingly, they also found men who were occasional or regular users of party drugs reported significantly better social outcomes than non-users on a range of measures including a higher level of resilience, less experience of HIV-related stigma, and a greater sense of support from other people living with HIV as well as from their gay and bisexual friends. This is important because all of these outcomes are strongly associated with greater emotional well-being among people living with HIV.
Authors are not claiming this study shows drug-use (in any form) has a direct impact on longer-term well-being. It’s also possible people who are resilient and socially connected are more likely than others to be part of social circles in which drug use is common. But this study does encourage authors to consider the social losses some people might encounter if they stop drug use. Friendship, connection, intimacy and sex are fundamental to humanity. If these are strongly tied to the social circles in which a person consumes drugs, their social and emotional well-being may suffer if they cease drug use. For people living with HIV, who may have experienced HIV-related stigma or rejection by sexual partners, access to social and sexual networks in which they feel accepted may be part of the appeal of party drugs.
How this can help responses to drug use:
Research that explores people’s social experiences of drug use can usefully inform harm minimisation or drug cessation programs. While the physical effects of a drug may pose risks, the social settings in which drugs are consumed are not necessarily damaging or dangerous. In fact, they may be quite the opposite, providing a source of friendship, support and happiness for users. It might be tempting to denounce this with the assertion that the potential health risks undermine any claims to benefit – or that friendships generated through drug use are not genuine. But sense of community and friendship has been successfully harnessed in drug and alcohol harm minimisation campaigns such as the “Take Care of Your Mates” campaigns directed toward young people. Focusing on the social settings in which drug use occurs may also be useful for strategies to reduce other risks. For example, campaigns to promote safer sex among gay men who use crystal meth have focused on venues and parties where “sex on drugs” is common. Understanding the potential social benefits of drug use may also enhance drug rehabilitation programs. Strategies to help people rebuild social ties, friendships and support networks could be important in supporting long term cessation of drug use.
______
Psychedelic drugs promote neural plasticity in rats and flies, a 2018 study:
Psychedelic drugs may have mind-altering powers in the physical sense, too. A new study has found psychedelics, specifically DOI, DMT, and LSD, can change brain cells in rats and flies, making neurons more likely to branch out and connect with one another. The work supports the theory that psychedelics could help to fight depression, anxiety, addiction, and post-traumatic stress disorder.
The idea that depression stems from imbalanced brain chemistry remains popular, but recent studies have revealed evidence that depression manifests as structural changes in brain circuits or atrophy in parts of the brain. This doesn’t mean neurons die off during depression, but that neurites retract. Neurites are the sections — either axons or dendrites — of a neuron that project out to bridge the gap between two neurons at the synapse to facilitate communication. One of the hallmarks of depression is that the neurites in the prefrontal cortex — a key brain region that regulates emotion, mood, and anxiety — those neurites tend to shrivel up. These brain changes also appear in cases of anxiety, addiction, and post-traumatic stress disorder.
In their paper, Olson and colleagues tested psychedelics. In both test tube and animal experiments, the psychedelics showed functional and structural changes like those promoted by ketamine in cortical neurons. Psychedelics increased both the density of dendritic spines and the density of synapses. Some psychedelics tested, including LSD, proved to be more potent and efficacious than ketamine in promoting neurite growth. The researchers did not do any human experiments, but experiments in both vertebrates and invertebrates showed psychedelics produced similar effects across species. This indicates the biological mechanisms that respond to psychedelics have remained the same across eons of evolution and that psychedelics will likely have the same brain growth (neural plasticity) effects in humans.
Olson and colleagues also set out to test how these psychedelics promoted neural plasticity, meaning they explored which biological pathways psychedelics activate that lead to neural growth. Ketamine’s neural plasticity effects were previously shown to be dependent on a protein called brain-derived neurotrophic factor (BDNF). When the researchers blocked BDNF signaling, psychedelics lost their ability to promote neurite growth. BDNF binds to a receptor, called TrkB, that is part of a signaling pathway that includes mTOR, which is known to play a key role in the production of proteins necessary for the formation of new synapses. When the researchers experimented by inhibiting mTOR, it also completely blocked the psychedelics’ ability to promote neurite growth. Olson thinks identifying the signaling pathways at play in psychedelic-induced brain changes will help future research identify compounds that could be developed into depression treatments.
Although most psychedelics aren’t considered to be addictive in the same way that cocaine is, they do produce hallucinations. Olson doesn’t expect psychedelics to become prescription drugs for depression. “But a compound inspired by psychedelics very well could,” he says.
______
______
Why are intelligent (high IQ) people more likely to abuse drugs?
No mathematician has ever published more papers than Paul Erdos. The 20th century mathematician was brilliant, eccentric, and prolific, publishing a record 1,525 papers. By the age of four, Erdos could calculate the number of seconds someone had lived if they gave him their age. He contributed to a wide variety of mathematical disciplines, including discrete mathematics, probability theory, Ramsey theory, graph theory, and others. He worked 19-hour days. And he loved amphetamines. When Ronald Graham, a concerned friend and fellow mathematician, bet him $500 that he couldn’t stay off his drug of choice for a month, Erdos accepted and easily won the challenge. When the 30 days was up, Erdos said to Graham, “You’ve showed me I’m not an addict. But I didn’t get any work done. I’d get up in the morning and stare at a blank piece of paper. I’d have no ideas, just like an ordinary person. You’ve set mathematics back a month.” Erdos resumed taking amphetamines and did so for every day of his life until his death 17 years later.
_
Addiction is a complex issue that has multiple influences, including intelligence. Many specialists have considered the connection between addiction and intelligence, trying to gauge how they are related. The results of various studies have been surprising: high intelligence has been more commonly linked to addiction, rather than low intelligence. But why? Doctors, scientists, and those who study addiction have struggled to understand why this correlation exists. After all, why would intelligent people more likely to turn to drugs? Most people understand the risks associated with drugs and many argue that intelligent people would be more likely to avoid those risks. The downsides of drug abuse are so clear that one would imagine smarter folks would stay away from them. The research suggests otherwise. Numerous studies have documented the relationship between intelligence and substance abuse. This relationship should be a negative one. After all, recreational drugs can damage your health, addiction costs huge amounts of money, and the legal consequences can be dire. But in fact, intelligence and substance abuse have a positive relationship: intelligent individuals are more likely to abuse drugs than less intelligent individuals. However, the mechanism for this correlation has been difficult to pin down.
_
Evidence for a link between intelligence and substance abuse:
A study conducted on nearly 8,000 people measured their IQ scores at ages 5 and 10. Then, the study followed up with these individuals at ages 16 and 30. Individuals from this group with higher IQ scores were more likely to use cannabis, cocaine, ecstasy, amphetamines, heroin or a combination of these drugs. Women with IQ scores in the top third, for instance, were more than twice as likely to have used cannabis or cocaine by 30 than those in the bottom third. Men with high IQs were nearly twice as likely to have taken amphetamines and 65% more likely to have taken ecstasy compared with men who scored less. The same relationship exists for alcohol consumption. Even accounting for religion, social class, parental education, and satisfaction with life, intelligence has been found to be the second-greatest predictor of alcohol consumption, the first being gender.
Another study found that there is a clear monotonic association between childhood general intelligence and adult consumption of psychoactive drugs. “Very bright” individuals (with IQs above 125) are roughly three-tenths of a standard deviation more likely to consume psychoactive drugs than “very dull” individuals (with IQs below 75).
_
It’s clear that there is some kind of positive relationship between substance abuse and intelligence, but why does this relationship exist? Why would more intelligent people who should ostensibly know better practice such a risky habit?
Correlation is Not Causation:
While many studies seem to point to high intelligence as a factor in substance abuse and drug addiction, one study released in 2016 suggests this data is correlation not causation. In short, persons with higher IQs are more likely to experience factors that contribute to addiction, such as peer pressure, stress, anxiety, negative emotions, difficulty socializing, and high pressure to perform well in jobs or school. This contributes to an increased rate of self-medication, of using substances as a reward, and of trauma or stress which contribute to addiction. The same study reviewed over a dozen clinical reviews of drug use in teens, finding that once other factors were taken out of the equation, teens being prone to drug use did not change based on IQ tests.
So, why is there a Correlation between IQ and Drug Addiction?
While no similar study of adult drug use has been performed, it remains true that adults with high intelligence tend to be more prone to drug abuse and addiction. For example, some estimates suggest that over 21% of doctors and lawyers qualify as problem drinkers or drug users. And 20% or more students in professions like medicine abuse drugs like MPH and cocaine. In these cases, addiction can easily be traced to stress, the need to perform, and high amounts of pressure from parents, job boards, and patients or clients. Doctors, lawyers, and students use drugs to self-medicate, to unwind or reward themselves for a job well done, and to increase performance – all of which can easily lead to addiction. As a result, many people eventually become high-functioning addicts who perform reasonably well in work and school functions, sometimes even outperforming colleagues. At the same time, they use substances to destress or to boost performance and eventually need the substance to perform well or at all.
Other explanations:
Variety of hypotheses have been postulated to explain this seemingly paradoxical correlation. These ideas are hard to test, but give a good range of concerns that potentially influence addiction.
These hypotheses argue that intelligent people who abuse drugs:
-Are easily bored – As a result, they look for new and novel things to push their mind. Drugs, being a dangerous and risky thing, entertain and even challenge their minds.
-Try to fuel their creative fires – Intelligence and creativity are highly linked and the myth that drug use helps fuel creative genius has been spread for centuries. Unfortunately, this may lead intelligent people to try drugs.
While these are among the most popular explanations, there are a variety of more in-depth and well-studied theories that may better explain why intelligent people suffer from such an unfortunately high rate of addiction.
- You’re more likely to have a high IQ if you grow up in a socioeconomically advantageous environment — there’s less stress, better access to education, better healthcare, and other factors that facilitate the growth of intelligence. This kind of environment shields people from the downsides of drug use. People growing up in socioeconomically disadvantaged environments can’t afford drug treatment, highly capable lawyers, or the funding their habit requires without resorting to unsavory activities, so they’re exposed to the dangers of drug use far more frequently. An intelligent person might look at their (wealthy) peers, see that their real-life evidence experience doesn’t back up the messaging of anti-drug campaigns and therefore feel more comfortable taking recreational drugs. This theory is corroborated by the fact that — out of nearly all other drugs — individuals with higher IQs are less likely to smoke cigarettes. The downsides of cigarette smoking are so patently obvious that it’s more reasonable for an affluent person to avoid it than, say, cannabis or ecstasy.
- Evolutionary psychologist Satoshi Kanazawa has a different theory: The Savanna-IQ Interaction hypothesis.
Life evolves to become better adapted to a certain environment. Giraffes have long necks so they can see predators, dogs spin around in circles before they lie down to check their surroundings, and some birds migrate to avoid the winter. These adaptations are positively selected for because the creatures that possess them are more likely to survive and reproduce. However, environments are dynamic; the entire spectrum of useful behaviors can’t be hard-wired into animals. The Savanna hypothesis contends that general intelligence evolved as an adaptation to solve evolutionarily novel problems; that is, the unexpected challenges of the environment.
The Savanna hypothesis suggests that outside of the savanna — Homo sapiens’s “natural” environment — general intelligence would be selected for, since there are more evolutionarily novel experiences than evolutionarily familiar experiences, or situations in which we have a hard-wired response to. It would also stand to reason that humans who were both intelligent and inclined to try novel things would leave the savanna and become biologically successful across the globe. So, the humans that left the savanna and succeeded outside of it would be both intelligent and inclined to try new things, such as drugs. This hypothesis proposes this link between intelligence and novelty is why intelligent people do drugs; The fact that drugs are unhealthy would be less relevant than the fact that drugs are a more novel experience than, say, being charged by a predator, a scenario for which we have a hard-wired response to.
Criticisms of the Savanna-IQ Interaction hypothesis:
Kanazawa hypothesis has been popular in the media, but it has also attracted some criticism from other scientists. First, the association between intelligence and seeking novelty may be more easily explained. Other research has shown that variations in the dopaminergic system are associated with corresponding variations in novelty-seeking (or openness to experience) and intelligence. Another criticism of the Savanna-IQ Interaction hypothesis is that intelligence likely evolved long before humans began traveling outside of the savanna and migrating across the globe. There’s also the fact that humans have been consuming drugs for thousands of years, suggesting that their use might not be so novel after all. There are numerous other points of contention against the hypothesis, but very few other proposals have been able to satisfactorily explain why intelligent people seek out novel experiences like substance abuse.
- Self-Medication, Depression, and Anxiety: Both anxiety and depression are strongly linked to higher intelligence, and both contribute to increased substance use. Abusers suffering from depression or anxiety, especially without a diagnosis, may be using substances to self-medicate, treating symptoms such as constant stress and worry or to relax and alleviate symptoms of depression. At the same time, those with high intelligence are often high-achievers and therefore less likely or willing to admit when something is wrong to seek out professional health and treatment. Data shows that while substance use disorders average at around 8.02% for the general population, they average at 32% or higher for persons with mood disorders like anxiety, depression, or bipolar disorder. So, the fact that persons with high intelligence are more prone to mood disorders makes many innately more vulnerable to substance addiction.
- Intelligence may be linked to Emotional Instability: High intelligence can greatly contribute to emotional instability, inability to socialize, and a lack of empathy. While each of these problems can change depending on the person, classical intelligence, as measured by an IQ test, often contributes to isolationism, instable social relationships, and social awkwardness. This can result in a lack of emotional intelligence, as well as feeling isolated, lonely, and left out. Low emotional intelligence is a significant predictor of both alcohol-related problems and drug-related problems. Drugs present an easy social lubricant, which many use to overcome barriers presented by a racing mind or overthinking – enabling them to act or be normal around others. This is especially true for those in turbulent houses or those who have experienced traumatic events such as family death or divorce – who would be prone to social awkwardness due to higher level of intelligence. Such people use substances just to be in social situations and therefore prone to substance addiction.
It may simply be that intelligent people are more easily bored and that drug use is the easiest way to alleviate boredom, or that intelligent people find more utility in their drug experiences and can incorporate lessons learned from altered states into their worldview.
Can drug addiction lower IQ?
Long term use of hard drugs (Methamphetamine, Heroin, Cocaine, etc.,) can wear down the body and brains ability to maintain homeostasis, which can severely hinder cognitive behaviour and lower IQ, but the human brain is resilient and able to rewire when the substances that were chemically altering it, are abandoned. Heavy, long-term marijuana use beginning in the teens can possibly lead to lower IQ, a provocative new study shows. Frequent, continued use of marijuana starting before age 18 was associated with an eight-point decline in IQ in the study. The decline was not seen in users who started smoking pot in early adulthood or later in life. The findings suggest that long-term marijuana use can cause long-term harm to some thinking abilities, such as intelligence, memory, and attention span, and that teens are uniquely vulnerable, researchers say.
In a nutshell:
High IQ individuals are more likely to abuse drugs than low IQ individuals and chronic drug abuse may lower IQ transiently as long as brain is addicted to drugs.
______
______
Moral of the story:
_
- Humans have used psychoactive substances for as long as we have records and changing consciousness is something people like to do. In fact, psychoactive drug use can be traced to prehistory based on archaeological evidence.
_
- The disease of addiction is one of the least understood, and frequently misunderstood, of all chronic diseases. Addiction is a disorder of the brain’s reward system which arises through transcriptional and epigenetic mechanisms and develops over time from chronically high levels of exposure to an addictive stimulus (e.g., eating food, the use of cocaine, engagement in sexual activity, participation in gambling, etc.). The two properties that characterize all addictive stimuli are that they are reinforcing (i.e., they increase the likelihood that a person will seek repeated exposure to them) and intrinsically rewarding (i.e., they are perceived as being inherently positive, desirable, and pleasurable). DeltaFosB (ΔFosB), a gene transcription factor, is a critical component and common factor in the development of virtually all forms of behavioral and drug addictions. Two decades of research into ΔFosB’s role in addiction have demonstrated that addiction arises along with compulsive behavior due to overexpression of ΔFosB in the D1-type medium spiny neurons of the nucleus accumbens in the brain.
_
- Addiction can be either behavioral or substance (drug) related. Common behavioral addictions include: Gambling, Sex, Food, Smartphone, Internet, Video Games and Shopping addiction. All addictive objects have powerful effects on the brain. These effects account for the euphoric or intensely pleasurable feelings that people experience during their initial use of these objects, and these feelings motivate people to use those objects again and again, despite the risks for significant harms. Addiction manifests in three distinct ways: craving for the object of addiction, loss of control over its use, and continuing involvement with it despite adverse consequences.
_
- Substance abuse, also known as drug abuse, is a patterned use of a psychoactive drug in which the user consumes the substance in amounts or with methods which are harmful to themselves or others. Substance abuse, if not treated, often leads to dependence and/or addiction. The most commonly abused substances are alcohol and prescription drugs. Opioids are so highly addictive that even individuals that closely follow short-term prescriptions can quickly get hooked, a risk that only goes up the longer the prescription is for. All use of illicit drugs is considered substance abuse. Virtually every substance that is abused has an effect on the executive-functioning areas of the brain.
_
- Drug Addiction is defined as a chronic, relapsing brain disorder characterized by compulsive drug seeking, craving and use that continues despite adverse consequences. The user (addict) is periodically or chronically intoxicated, has impaired control over drug use, has compulsive patterns of drug-seeking and drug-taking behavior that take place at the expense of most other activities, exhibits determination to obtain drug by almost any means, and high probability of relapse even after prolonged drug-free periods.
_
- It is important to remember that at some time many people experiment with a variety of potentially addictive drugs, but most do not become addicted. In other words, mere self-administration of a drug is not tantamount to addiction. Only a minority of people who use drugs ultimately become addicted. Susceptibility differs because people differ in their vulnerability to various genetic, environmental, and developmental factors. It is estimated that only 10 to 15 % of individuals who engage in drug taking will become addicted. Even for a highly addictive drug like cocaine, only about 15% of users become addicted. Furthermore the rate of addiction is lower for those who are taking drugs for medical reasons than for those who are using drugs recreationally.
_
- Cross addiction means you’ve traded one addiction for another. Cross addiction happens in many different ways. For example, a heroin addict might start abusing alcohol, or someone recovering from alcoholism starts abusing painkillers. If you have the disease of addiction, any other addicting drug also stimulate the part of the brain that regulates addiction and addictive behavior. The dopamine dysregulation in the reward system of the brain seen in addiction is not able to tell the difference between addictive drugs or different drugs are using similar mechanisms in the reward system. Therefore, if someone who has drug addiction is given another addictive drug for whatever reason, that individual may start abusing the second drug.
_
- Tolerance is defined as a person’s diminished response to a drug that is the result of repeated use. People can develop tolerance to both illicit drugs and prescription medications. Tolerance is a physical effect of repeated use of a drug, not necessarily a sign of addiction. Most drugs have more than one effect, and tolerance does not necessarily develop equally to all effects. Abusers of illicit and prescription opioids, such as heroin or oxycodone, quickly develop tolerance to the euphoric high these drugs produce but not to the dangerous side effect of respiratory depression. Opioid abusers who take large doses of these drugs to overcome tolerance and get high are frequently hospitalized—or even die—because they stop breathing.
People who have stayed sober for a while, either because they were in jail or in treatment, should know that they are at a high risk of overdose if they relapse and take the same amount of drug they used to. Their cravings may not have decreased, but their tolerance has, meaning their body can’t handle usual doses of the drug anymore. That is why you often hear about people dying of an overdose soon after leaving rehab.
_
- Drug addiction and drug dependence are not same. Dependence affect every person who is repeatedly exposed to substances that may cause dependence. Unlike dependence, addiction doesn’t affect every person who is repeatedly exposed to an addictive substance. Drug dependence on a substance develops when the brain’s neurons adapt to repeated drug exposure and only function normally in the presence of the drug. Drug dependence is associated with withdrawal symptoms or a withdrawal syndrome which is a physiologic response to a drug that manifests due to rapid reduction in exposure of drug or exposure to an antagonist. Areas in the brain underlying the addiction to morphine are mesolimbic reward pathway particularly nucleus accumbens while those underlying the dependence to morphine are thalamus and brainstem. Morphine can cause addiction as well as dependence. High tolerance and dependency on a substance are warning signs for addiction, but they are not the sole indicators of addiction. Although, if one is addicted, they are most likely dependent as well. Not all addictive drugs are associated with physical dependence, e.g., amphetamine, and not all drugs that produce physical dependence are addictive drugs, e.g., caffeine. It is possible to be dependent on drug, without being addicted to drug e.g. caffeine.
It’s easy to determine when people are dependent on a drug. If they stop taking the drug, they’ll experience noticeable withdrawal symptoms. But it isn’t always easy to determine if a person is addicted to a drug. You can determine if you’re addicted to a drug by analyzing your behaviors. If drug use is hurting your relationships, causing problems at school or work, or getting you in trouble with law enforcement, you may be addicted. If you feel cravings or withdrawal when you quit a drug but you can prevent yourself from using the drug, you probably aren’t addicted.
Distinguishing between drug Side Effects and Addiction Symptoms is not always easy to tell when a person is struggling with an addiction since the side effects of many drugs are similar to the symptoms of addiction. A person experiencing the negative effects of a drug may mistake his symptoms for an addiction, or a person who thinks his drug abuse is under control may assume that the side effects he experiences are normal for the drug, and thus may ignore key signs of addiction.
_
- A psychoactive drug is a chemical substance that changes brain function and results in alterations in perception, mood, consciousness, cognition, or behavior. These substances may be used medically; as recreational drug to purposefully improve performance and/or alter one’s consciousness, without medical supervision; as entheogens for ritual, spiritual, or shamanic purposes; and for research. Psychoactive drugs alter consciousness by influencing how neurotransmitters operate at the synapses of the central nervous system (CNS). All psychoactive drugs interact initially with receptor or reuptake proteins. These initial effects lead to alterations in the levels of specific neurotransmitters, or to different activation states of specific neurotransmitter receptors in the brain. Common classification includes stimulants, depressants, hallucinogens, and opioids. Psychotropic drugs are psychoactive drugs that are used as prescription medications.
_
- Recreation is a legitimate need that requires legitimate activities, such as hobbies, exercise, conversation, music, dance, literature and other arts. Recreational drug use is the use of a psychoactive drug to induce an altered state of consciousness for pleasure, by modifying the perceptions, feelings, and emotions of the user, without medical supervision. Recreational drugs often bring about subjective (although these may be objectively observed) changes in consciousness and mood that the user may find rewarding and pleasant (e.g., euphoria or a sense of relaxation) or advantageous (e.g. increased alertness) and are thus reinforcing. Recreational drugs alter our perception of reality and diminish our ability to reason, both of which endanger us. There is a very short amount of time between the experimental phase of recreational drug use and the next steps towards losing control. Recreational drug use may lead to dependence and/or addiction.
_
- The concept of “responsible drug use” is that a person can use drugs recreationally or otherwise with reduced or eliminated risk of negatively affecting other aspects of one’s life or other people’s lives. Many well-known artists and intellectuals have used drugs, experimentally or otherwise, with few detrimental effects on their lives. The fact that some people can use a drug responsibly and even beneficially does not imply that it is safe. We all know people who drink alcohol and take no harm from it, and we all know people whose lives have been wrecked by alcohol.
_
- Factors that increase vulnerability to drug addiction include family history (presumably through heritability and child-rearing practices), early exposure to drug use (adolescence is among the periods of greatest vulnerability to addiction), exposure to high-risk environments (typically, socially stressful environments with poor familial and social supports and restricted behavioral alternatives and environments in which there is easy access to drugs and permissive normative attitudes toward drug taking), and certain mental illnesses (e.g., mood disorders, attention deficit–hyperactivity disorder, psychoses, and anxiety disorders). Drug availability is the most obvious environmental factor that influences addiction. Indeed, increased availability of cocaine and methamphetamine has contributed to the recent epidemics of addiction to these drugs.
_
- Impulsive action (inability to inhibit motor responses), and impulsive choice (preference for immediate smaller rewards to the detriment of long-term outcomes) are associated with drug addiction. Impulsivity is thought to precede compulsivity and it is the shift from impulsive to compulsive behaviors that is linked to the development of addiction.
_
- Children’s neurological development can be permanently disrupted when they are chronically exposed to stressful events such as physical, emotional, or sexual abuse, physical or emotional neglect, witnessing violence in the household, or a parent being incarcerated or suffering from a mental illness. As a result, the child’s cognitive functioning or ability to cope with negative or disruptive emotions may be impaired. Over time, the child may adopt substance use as a coping mechanism, particularly during adolescence. seeking relief through psychoactive substance use which provides short-term benefit in the face of long-term risks.
_
- Experimentation with drugs and alcohol often starts in adolescence, and so does the process of addiction. This could reflect normal adolescent-specific behaviors (risk-taking, novelty-seeking, response to peer pressure) that increase the probability of someone experimenting with drugs and alcohol. In adolescence, the incentive-rewards systems in the brain mature well before the cognitive control center (prefrontal cortex). This consequentially grants the incentive-rewards systems a disproportionate amount of power in the behavioral decision-making process. Therefore, adolescents are increasingly likely to act on their impulses and engage in risky, potentially addicting behavior before considering the consequences. Adolescents are more likely to experiment with substance use because their prefrontal cortex is not mature and those substances could impact future development of prefrontal cortex, making it easier to continue to use. Not only are adolescents more likely to initiate and maintain drug use, but once addicted they are more resistant to treatment and more liable to relapse.
_
- All drugs of abuse, from nicotine to heroin, cause a particularly powerful surge of dopamine in the nucleus accumbens of brain through various mechanisms. The likelihood that the use of a drug will lead to addiction is directly linked to the speed with which it promotes dopamine release, the intensity of that release, and the reliability of that release. Even taking the same drug through different methods of administration can influence how likely it is to lead to addiction. Smoking a drug or injecting it intravenously, as opposed to swallowing it as a pill, for example, generally produces a faster, stronger dopamine signal and is more likely to lead to drug addiction. By activating the brain’s reward circuitry, drugs deliver a jolt of intense pleasure. Dopamine not only contributes to the experience of pleasure, but also plays a role in learning and memory — two key elements in the transition from liking something to becoming addicted to it. Dopamine also interacts with the motivating and planning centers of the brain, meaning that the rush of pleasure that accompanies substance use makes your brain seek out more drug. As you use larger amounts of drugs or use more often, your brain programs more memories of a quick high and conditions itself to respond well to certain triggers.
Addictive drugs can release two to 10 times the amount of dopamine that natural rewards do, and they do it more quickly and more reliably. Drugs of abuse affect the brain much more dramatically than natural rewards, such as food and social interactions. So brain receptors become overwhelmed. To bring stimulation down to a more manageable level, the brain tries to adapt. One way the brain compensates is to reduce the number of dopamine receptors at the synapse. In addition, sending neurons increase their number of dopamine transporters, more quickly clearing dopamine from the synapse. All drug addictions have consistently shown long-lasting decreases in a particular type of dopamine receptor, the D2 receptor in brain reward systems. This down-regulation of D2 receptors might be why some people gradually develop addiction—the more individuals use drugs, the fewer D2 receptors they have, and the more they “need” drugs to feel normal. Others, who naturally have fewer D2 receptors from the beginning, seem to be more prone to addiction—in other words, they are “instant addicts. Also when an addicted person is given a drug, it causes a smaller release of dopamine than when the same dose is given to a person who is not addicted. These findings suggest that people addicted to substances experience an overall reduction in the sensitivity of the brain’s reward system (especially the brain circuits involving dopamine), both to addictive substances and also to natural reinforcers, such as food and sex. This is because natural reinforcers also depend upon the same reward system and circuits. This impairment explains why those who develop a substance use disorder often do not derive the same level of satisfaction or pleasure from once-pleasurable activities. Hijack of pleasure circuit in brain by drug addiction causes brain adaptations that often lead to the person becoming less and less able to derive pleasure from other things they once enjoyed, like food, sex, or social activities. This general loss of reward sensitivity may also account for the compulsive escalation of substance use as addicted individuals attempt to regain the pleasurable feelings the reward system once provided. As the brain continues to adapt to the presence of the drug, regions outside of the reward pathway are also affected. Over time, brain regions responsible for judgment, decision-making, learning, and memory begin to physically change, making certain behaviors “hard-wired.” At the same time, a second process occurs during the withdrawal stage: activation of stress neurotransmitters in the extended amygdala. These stress neurotransmitters include corticotropin-releasing factor (CRF), norepinephrine, and dynorphin. These neurotransmitters play a key role in the negative feelings associated with withdrawal and in stress-triggered substance use. Long-lasting brain changes can make it challenging for addicts to stay drug-free. They often experience intense cravings, leading to relapse. Many of the neurological processes and brain structures involved in addiction are also used in cognitive tasks like reasoning, learning and memory. With heavy drug use, you may find that you have difficulty learning or remembering information or that you lose focus when you’re trying to concentrate on a task.
_
- A defining characteristic of obese individuals is the fact that they will continue to overeat despite the well-known negative health and social consequences. Development of feeding behavior that is insensitive to negative outcome is analogous to the compulsive drug-taking behavior seen in human drug addicts that is similarly impervious to negative consequences. There is striking similarities between drug addiction and obesity in functional impairment in discrete brain regions and neurotransmitter circuits i.e. decrease in dopamine release in the nucleus accumbens, a brain region heavily implicated in food and drug reward. Feeding is influenced by pleasure and reward, and obtaining food reward can powerfully motivate consumption. Deficits in reward processing may be an important risk factor for the development of obesity, and that obese individuals may compulsively consume palatable food to compensate for reward hyposensitivity.
_
- In positive reinforcement, a rewarding stimulus (e.g., drug-induced euphoria and pleasure) directly increases the probability of a response (e.g., continued drug use). In negative reinforcement, the incentive for drug use is relief of a painful or unpleasant state (i.e., the physiological and motivational symptoms of withdrawal). However compulsive drug-seeking and drug-taking behavior are not all the time motivated by either the desire to obtain pleasure or by the desire to relieve withdrawal. What motivates addictive behavior in these instances? Researchers have attempted to address this question by proposing the concept of “incentive–sensitization”. This focuses on sensitization, whereby drugs alter the reward circuitry to cause increased assignment of incentive salience to drug cues, effectively making drug-associated environmental stimuli more difficult to ignore and leading to intense drug craving and relapse.
_
- Addiction is often described as maladaptive neural plasticity in response to drugs of abuse, which results in long-term molecular alterations in key brain regions leading to behavioral abnormalities. Many genes involved in modification of neurotransmitter balance collectively play some role in making an individual susceptible to drug abuse. Twin and adoption studies indicate the heritability of genes that predispose an individual to becoming addicted ranges between 40% (hallucinogens) to 70% (cocaine). Since a number of genes are involved, the effect of an individual gene in making a person vulnerable to drug abuse may be modest. Like many drugs, drugs of abuse are also metabolized by various liver enzymes. Polymorphisms of genes causing modification of enzymatic activities of these liver enzymes is also linked to addiction as well as susceptibility of toxicity of certain abused drugs. Moreover, repeated exposure of a drug to the human brain may also cause epigenetic changes such as histone modification (acetylation and methylation), DNA methylation, and modification of noncoding RNA. Epigenetic changes are the key components through which environmental influences can affect the genes of an individual. Although there is strong genetic component of susceptibility to addiction, there is also strong influence of external risk factors on the development of addiction, therefore it has been postulated that epigenetic mechanisms acquired through environment regulate the long-term changes associated with addicted phenotype. Also, altered epigenetic regulation of gene expression within the brain’s reward system due to drug exposure per se plays a significant and complex role in the development of drug addiction, for example histone modifications in response to stimulants (e.g., cocaine) and, to a lesser extent, opiates (e.g., morphine) in the nucleus accumbens (NAcc). Epigenetic mechanisms play a central role in the pathophysiology of drug addiction; additionally it has been noted that some of the alterations to the epigenome which arise through chronic exposure to addictive stimuli during an addiction can be transmitted across generations, in turn affecting the behavior of one’s children. It is called transgenerational epigenetic inheritance.
_
- Irrespective of the presence or absence of genes that may increase an individual’s vulnerability to become addicted, human post-mortem studies have shown that the expression of numerous genes is altered in the brain of addicted patients. Chronic cocaine use, for example, differentially alters the expression of up to 49 transcripts in the NAcc including those involved in signal transduction, synaptic function, and DNA to RNA processing. Similarly, significant upregulation of numerous transcripts, including glutamate receptors, have been reported using targeted microarrays on the VTA from cocaine overdose victims. In support of the observations in humans, up to 295 genes were differentially regulated after 1 h of nicotine treatment in cultured neuron-like SH-SY5Y cells, including those involved in neural development, synaptic plasticity, neuronal survival, immune responses, and cellular metabolism. SH-SY5Y is a human derived cell line used in scientific research. Indeed, genes affected by drugs of abuse can be sub-characterized into those relating to the extracellular matrix, synaptic plasticity and efficacy, receptors, ion channels and transporters, signal transduction, and cell death, among others. All these show strong biological basis for drug addiction irrespective of genetic vulnerability.
_
- Two competing concepts address the development of involvement with psychoactive substances: the “gateway hypothesis” (GH) and common liability to addiction (CLA). The former is the theory of biological alterations in the brain due to an earlier drug use (gateway drugs like alcohol, nicotine and cannabis) and the latter is the theory of similar attitudes across different drugs. According to the concept of similar attitudes across different drugs (common liability to addiction), a number of personal, social, genetic and environmental factors can lead to a generally increased interest in various drugs. The scientific discussion is dominated by these two concepts, which appear to cover almost all possible causal connections if appropriately combined.
_
- Psychedelic drugs are neither magic bullets, nor confer wisdom/creativity. However animal experiments showed that psychedelics make neurons more likely to branch out and connect with one another and thereby supports the theory that psychedelics could help to fight depression, anxiety, addiction, and post-traumatic stress disorder.
_
- Cognitive enhancement can be defined as the use of drugs and/or other means with the aim to improve the cognitive functions of healthy subjects in particular memory, attention, creativity and intelligence in the absence of any medical indication. Cognitive enhancement is perhaps one of the most intriguing and controversial topics in neuroscience today. Currently, the main classes of drugs used as potential cognitive enhancers include psychostimulants (methylphenidate (MPH), amphetamine), but wakefulness-promoting agents (modafinil) and glutamate activators (ampakine) are also frequently used. Pharmacologically, substances that enhance the components of the memory/learning circuits—dopamine, glutamate (neuronal excitation), and/or norepinephrine—stand to improve brain function in healthy individuals beyond their baseline functioning. In particular, non-medical use of prescription stimulants such as MPH and illicit use of psychostimulants for cognitive enhancement have seen a recent rise among teens and young adults in schools and college campuses. MPH is currently most often abused and sold on the black market among adolescents, particularly in high schools and on college campuses. Students look for the medication when they have exams, or need to stay awake for long hours, in order to boost their energy and memory. This rather commonplace usage among adolescents is particularly frightening in light of the harm drugs cause to development of prefrontal cortex. Three points against their use are as follows:
-1. Introducing a substance that alters dopamine and norepinephrine levels, such as MPH, might disrupt the maturation of the prefrontal cortex affecting the learning and memory circuits, and have lasting behavioral consequences.
-2. Altering glutamate function via the use of psychostimulants may impair behavioral flexibility, leading to the development and/or potentiation of addictive behaviors.
-3. Healthy individuals run the risk of pushing themselves beyond optimal levels into hyperdopaminergic and hypernoradrenergic states, thus vitiating the very behaviors they are striving to improve. As levels of the neurotransmitters continue to rise past the optimal point, cognition becomes impaired with the individual showing distractability, impulsivity, hyperactivity, inattentiveness, stereotypical behaviors and cognitive inflexibility.
_
- Drug harmfulness is the degree to which a psychoactive drug is harmful to a user and is measured in various ways, such as by addictiveness and the potential for physical/psychological/social harm. More harmful drugs are called “hard drugs”, and less harmful drugs are called “soft drugs”. Heroin, morphine, and cocaine are most addictive while cannabis and LSD are less addictive. Safety ratio is the ratio of dose that is likely to be fatal to normal dose needed to feel the effects of the drug. Drugs with lower safety ratios are more dangerous because the difference between the normal and the lethal dose is small. Accordingly, heroin and cocaine are most dangerous while cannabis and LSD are least dangerous. Interesting to note that highly addictive illicit drugs are also most dangerous. Heroin and cocaine are hard drugs, and LSD and cannabis are soft drugs.
_
- Use of several drugs like amphetamines, cannabis, cocaine, ecstasy, legal highs, LSD, and magic mushrooms is highly correlated. That means if you use any one of them, you are likely to use another also. Additionally, consumption of cannabis is strongly correlated with usage of nicotine (tobacco), and heroin is correlated with cocaine. Combining drugs is dangerous because their combined effects on the CNS can increase dramatically and can lead to overdose as well as other dangerous complications.
_
- Most hard drugs are adulterated to some degree. Some street drugs can be as low as 10–15% of the active drug. Drug checking or pill testing is a way to reduce the harm from drug consumption by allowing users to find out the content and purity of substances that they intend to consume. This empowers users to make safer choices: to avoid more dangerous substances, to use smaller quantities, and to avoid dangerous combinations. A range of analysis techniques are in use by drug checking service.
_
- The growing demand for cannabis, cocaine, and heroin for recreational purposes, mostly in the developed world, triggered an increase of illicit production in geographical areas where cannabis, coca, and opium had been traditionally cultivated. Devastating effects of illicit cultivation of cannabis plant, coca bush and opium poppy on biodiversity are the loss, degradation and fragmentation of the forests, and the loss of areas where food could be grown. In addition to the deforestation caused by illicit crop cultivation, chemicals used for the processing of illicit drugs can be harmful to biodiversity, both in the immediate area and downstream, as a result of chemical run-off.
_
- With the rising size of the illicit drug trade, international drug trafficking became a multibillion-dollar business dominated by criminal groups. With a turnover of around $500 billion, illicit drug business it is the third largest business in the world, next to petroleum and arms trade. Profits from the drug traffic flow back into the coffers of sophisticated criminal organizations with financial interests in other illicit areas, such as prostitution, racketeering and money laundering.
_
- Sales of cocaine, heroin and cannabis amount to approximately $122 billion per year in the United States and Europe, of which 70 per cent or as much as $85 billion per year, could be available for laundering and investment. And this amount is larger than the GNP of three-fourths of the 207 economies of the world. Because money generated by illicit drug activities does not normally enter into the formal economic process of a country, macroeconomic planning is not possible for these funds. Hence, a source of serious error is introduced into estimates of national income and expenditure. The hidden economic and social costs of illicit drug production and trafficking cannot be charged back to those involved and therefore, they are an added burden to the law-abiding population.
_
- Governments that are unable to control major insurgent or terrorist movements are unlikely to be successful in controlling a drug trade that generates enormous amounts of money to buy influence or weapons for these insurgent or terrorist groups.
_
- More than 75 per cent of opium poppy cultivation area is in Afghanistan. A marked increase in opium poppy cultivation and increase in opium poppy yields in Afghanistan resulted in opium production in the country reaching 9,000 tons in 2017. Up to 85 per cent of opium cultivation in Afghanistan occurs in territory under some influence of the Taliban. Without the proceeds of drug production and trafficking, which make up almost half of the Taliban’s annual income, the reach and impact of the Taliban would probably not be what it is today.
_
- Drugs reach into Indian state of Punjab via the India-Pakistan border. Drug consumption in Punjab is three times the national average of India as drugs are easily available and cheaper in Punjab. More than two-thirds of Punjab’s households have at least one addict in the family.
_
- About 275 million people worldwide i.e. roughly 5.6 per cent of the global population used illicit drugs at least once during 2016, and out of them 31 million suffer from illicit drug addiction, and out of them 10.6 million inject illicit drugs. Cannabis was the most widely consumed drug in 2016, with 192 million people using it at least once during the year. Roughly 450,000 people died as a result of illicit drug abuse in 2015 worldwide. Opioids continued to cause the most harm, accounting for 76 per cent of deaths where drug use disorders were implicated.
_
- The probability of drug addiction among LGBT community is twice that of heterosexual youths/adults.
_
- Of all people diagnosed as mentally ill, 29 percent abuse either alcohol or drugs. Co-occurring substance abuse problems and mental health issues are more common than many people realize. Co-occurring disorders also affect each other. When a mental health problem goes untreated, the substance abuse problem usually gets worse. And when alcohol or drug abuse increases, mental health problems usually increase too.
_
- People with physical disabilities experience substance use disorders at 2 to 4 times the rate of the general population.
_
- About 100 million children live and work on the streets of the cities of the world and up to 90% of the world’s street children abuse some kind of drugs.
_
- Drug availability and occupational stress help explain why medical professionals have high rate of opiate addiction, abuse of alcohol and mood-altering prescription drugs.
_
- Quite puzzlingly high IQ individuals are more likely to abuse drugs than average individuals. This is so because intelligent people are more easily bored and that drug use is the easiest way to alleviate boredom, or intelligent people find more utility in their drug experiences and can incorporate lessons learned from altered states into their worldview, or intelligent people are unable to socialize and drugs present an easy social lubricant enabling them to act or be normal around others. On the other hand, chronic drug abuse may lower IQ till brain recovers from drug addiction.
_
- The Internet is probably the primary mechanism for drug dealers because using social media and smartphones to conduct business is far quicker and more efficient than methods of the past. The next wave of freelance narcotics is online and with millions of people having a smartphone in their hand, the marketplace is everywhere. Social media apps are increasingly used by young people to buy illegal drugs due to privacy, convenience and speed of buying drugs.
_
- The problems associated with substance abuse are so pervasive that they can affect nearly every aspect of the abuser’s life. These problems may include: employment issues, injuries, violence, assaults, child neglect or abuse, incarceration, suicidal behaviors, psychiatric disorders, cognitive impairments, transmission of sexually transmitted diseases (e.g., HIV/AIDS), damage to multiple organs (e.g., respiratory, immune, digestive, cardiovascular, reproductive, and pancreatic systems) and mortality. In particular, substance use-related behaviors are a major contributor to the HIV/AIDS epidemic, either through sharing of needles or other drug equipment or substance use-related risky/unprotected sexual behavior. One in 10 HIV diagnoses occur among people who inject drugs. One in eight persons who inject drugs live with HIV. Illicit drugs carry with them potential criminal consequences if one is caught in possession of them and arrested. Drugs that are smoked may produce throat and lung cancers and other problems. Snorting (“sniffing”) drugs can lead to a loss of the sense of smell, nosebleeds, difficulty in swallowing, hoarseness, and chronic runny nose.
_
- Drug abuse and addiction cost American society more than $1 trillion annually in lost workplace productivity, healthcare expenses, and crime-related costs. The cost will continue to rise due to policies that promote criminalization of drug use and restrict funding for treatment.
_
- Drug addiction is expensive. If poverty-stricken, the addict must spend all his or her time “hustling” for drugs—which means that the person must steal or raise money by other means such as prostitution, procuring, or small-time narcotics peddling. The addict always faces the danger of withdrawal, the danger of arrest, the danger of loss of available supply, and the danger of infection, of collapsed veins, or of death from overdosage. Very few individuals are still addicted by age 40. They have either died, somehow freed themselves from their addiction, or sought treatment.
_
- Drug use has often been linked to poverty. Poor are more likely to abuse drugs and drug abuse leads to poverty. Persons with marginal incomes often spend money on drugs, alcohol or tobacco instead of food, clothes and shelter. Poor are more likely to be involved in drug production and trafficking.
_
- The close connection between drug use and criminal behavior is supported by many studies. Whether drugs caused criminal behavior or whether criminal behavior cause drug abuse is a matter of debate. Large number of studies have shown that criminal careers are embarked on before the onset of drug use, while drug use intensifies this criminal behaviour. A drug abuser is 18 times more likely to be involved in illegal activity than someone who does not abuse drugs. Heroin addicts are usually deeply involved in crime; daily opiate use increases criminality several fold. Many violent crimes have been linked to the mind-altering effects of drugs. Substance abusers often commit thefts to support their drug habits. Drugs and alcohol have been linked to domestic violence and sexual assault. Women may become involved in drug trafficking to sustain their own drug consumption; and some women involved in drug trafficking are victims of sex trafficking.
_
- The abuse of drugs affects perception, attention, cognition, coordination and reaction time, among other neurological functions, which affect safe driving. After alcohol, cannabis is the substance most frequently detected in seriously and fatally injured drivers. Mild to moderate increase in accident risk is associated with the use of most of the drugs.
_
- About 16 percent of pregnant women smoked cigarettes, 8.5 percent drank alcoholic beverages, and nearly 6 percent used illicit drugs in the U.S. There is little information available on the extent of substance use, other than tobacco, among pregnant women in low-income and middle-income countries. Several serious health consequences for the developing fetus result from maternal substance abuse including miscarriage, preterm labor, low birth weight, and a number of developmental problems and birth defects. Treatment for substance abuse during pregnancy is significantly more effective than at other times in a woman’s life but not all women are able to stop smoking, drinking, or using drugs when they find out they are expecting.
_
- Everyone should know that caffeine in tea/coffee is a licit psychoactive drug which can cause dependence. About one to two cups of coffee or two to four cups of tea per day are probably safe in pregnancy, but intake of more than 300 mg caffeine per day may be associated with adverse outcomes such as spontaneous abortion, growth restriction, congenital malformations, and stillbirth.
_
- A drug test is primarily performed to confirm the presence of one or more illegal or prescription drugs in a person’s urine, blood, saliva, hair, breath or sweat. Hair strand analysis is a more reliable way to test for the presence of drugs. It is less invasive, and most drugs can still be detected as long as 90 days after use, and hair from any part of the body can be collected for analysis. Using urinalysis alone missed nine out of 10 illegal drug users. Drug screening tests cannot be used to determine if a person has a drug addiction. As a diagnostic biomarker, ΔFosB expression could be used to diagnose addiction in humans, but this would require a brain biopsy and therefore not used in clinical practice.
_
- Opioid substitution therapy supplies illicit drug users with a replacement drug, a prescribed medicine such as methadone or buprenorphine, which is usually administered orally in a supervised clinical setting. A recent review of the scientific literature involving more than 100,000 patients found that death rates were two to three times lower for people in methadone or buprenorphine treatment, compared to people not taking medication. No other method — including abstinence-only residential rehab — has such strong support. Despite the evidence of effectiveness, it is estimated that only 8% of injecting drug users globally currently receive opioid substitution therapy. Patients stabilized on adequate, sustained doses of methadone or buprenorphine can keep their jobs, avoid crime and violence, and reduce their exposure to HIV and Hepatitis C by stopping or reducing injection drug use and drug-related high risk sexual behavior. Remember taking drugs to treat addiction doesn’t mean you’re ‘still addicted’. Long-term use of methadone or buprenorphine for opioid addiction is not addiction but merely dependence.
_
- Relapse occurs when someone returns to substance use after a period of abstinence. Between 40 and 60 percent of people recovering from drug addiction relapse.
_
- If you are in a situation you are pressured to take drugs, the best thing to do is to remove yourself from the situation and surround yourself with people who don’t take drugs. The best way to prevent an addiction to a drug is not to take the drug at all.
_
- A large proportion of individuals who use cannabis go on to use other illegal drugs. Also there have not been enough clinical trials showing that marijuana’s benefits outweigh its health risks. I therefore do not support legalization of cannabis just like alcohol and tobacco. The protest that alcohol & tobacco are harmful yet legal, therefore illegal drugs should similarly be legal (and harmful) ignores the fact that the legal drugs already cause more than enough harm to want to add a new battery of even more harmful but now legal drugs. Tobacco use due to nicotine addiction is a greater problem for the world than poverty, terrorism and corruption. Even low to moderate alcohol consumption leads to cancer, accidents, violence, injuries, drowning and dependence. In my view, it is time to review legalization of alcohol and tobacco.
_
- Prohibition means manufacture, storage, transportation, sale, possession, and consumption of any drug is banned legally. Legalization is removal of prohibition. Prohibition does deter illicit drug use. Prohibition helps to keep prices higher, and higher prices help keep use rates relatively low, since drug use especially among young people is known to be sensitive to price. Legalizing drugs will make drugs cheaper and thus increase its use. The harms of increased drug use as a consequence of legalization far outweigh harms of prohibition.
_
- Decriminalization means drug user is seen as a patient and not a criminal. Decriminalization does not mean legalization. Decriminalization refers to drug use and possession offences, and not the sale or supply of drugs. It focuses on drug users, not drug suppliers. Drug suppliers and traffickers are criminals but not drug user. Decriminalization of drugs makes a lot of sense, given that the definition we use of addiction is the continued obsessive-compulsive use of drugs despite negative consequences. So imprisoning people, giving them negative consequences to get them to stop using drugs, is not going to work by the very definition we’re using of addiction. Portuguese drug policy of decriminalization has reduced the heroin abuse with heroin users numbered about 25,000 in 2017 compared to 100,000 in 2001. The reported rate of drug-related deaths is the second lowest in the European Union together. There is also a continuous decrease in the numbers of drug-related HIV/AIDS. I support decriminalization of drug user worldwide no matter hard drug or soft drug. Incarceration in prisons or drug detention centers of people who use drugs but have committed no other crime contribute to increased transmission of HIV, hepatitis, and tuberculosis. The impact of incarceration on individuals and families can be devastating leading to increased incidence of homelessness, unemployment, divorce, and recidivism. Remember there is a cost savings of US$7 for every US$1 spent on treatment of drug addicts. Evidence-based treatment for drug addiction reduces health and social consequences e.g. crime, HIV/AIDS and economic burden. Everybody should treat drug addict as patient and not criminal, provided he/she has committed no other crime.
_
- Alcohol prohibition in India is in force in the states of Bihar, Gujarat, Mizoram and Nagaland as well as in the Union Territory of Lakshadweep. I support decriminalization of alcohol users in these states. I strongly oppose incarceration in prisons for alcohol users provided they committed no other rime under the influence of alcohol or otherwise. Alcohol addict should be treated as a patient and not criminal. Alcohol users who are not addicts may be fined but not imprisoned in these states. How can you take away the liberty of an individual merely on the ground that he/she consumed alcohol or any other drug for that matter? It is outrageous to say the least and draconian to say the most.
_
- In the past, drug addiction was viewed as stemming from an individual’s moral failing and weakness of will. There is current medical consensus that portrays drug addiction as a disease or disorder rather than moral failing. People with addiction should not be blamed for suffering from the disease. All people make choices about whether to use substances. However, people do not choose how their brain rewires and adapts to drugs and alcohol, that is why people with addiction cannot control their use while others can and that is why they willingly ruin their health, relationships, and other major areas of their lives.
But there is also strong scientific evidence that most people recover from addiction on their own and that things are not as simple as the medical model of drug addiction as disease imply. Only 10 to 15 percent of people who use drugs get addicted and around 80 percent of addicts overcome their addiction on their own by the age of 30. They do so because the demands of their adult life, like keeping a job or being a parent, are incompatible with their drug use and are strong incentives for kicking a drug habit. Most people quit problematic drug use as they get older often without treatment. This is about people finding purposes that come to outweigh the importance of drug use for them as they mature. Most studies on addiction are conducted on patients in treatment, and this skews the population sample. In fact, most addicts never go into treatment, and the ones who do are the ones, the minority, who have not managed to overcome their addiction on their own. The fact that majority of drug addicts kick addiction on their own without treatment proves role of will power rewiring brain and reverting expression of numerous genes to normality. As discussed in previous paragraphs, drugs like cocaine and nicotine do alter expression of genes in brain in addiction and these altered expressions of genes need to be reverted back to normality in de-addiction.
Researchers have analyzed the biological effects of meditation, yoga, breathing exercises, Qi gong and Tai Chi. Together the studies show that these mind-body exercises appear to suppress the expression of genes and genetic pathways that promote inflammation. Meditation is found to alter levels of gene-regulating machinery and reduced levels of pro-inflammatory genes, which in turn correlated with faster physical recovery from a stressful situation. Inflammation can temporarily boost the immune system, and can be protective against infection and injury, but in today’s society, stress is primarily psychological, the body’s inflammatory response can become chronic and can impair both physical and mental health.
In a nutshell, human mind through sheer will power and meditation can alter expression of genes. This is sensational.
_
- Chemical analogs of mammalian neurotransmitters— psychoactive substances—were ubiquitous in the ancestral environment, as they are nowadays, in the form of plant allelochemicals. Animals and psychoactive plants appear to have co-evolved, possibly explaining why these chemicals and their receptors exist within the nervous system. Over the approximately 200 million-year evolutionary history of Mammalia, plants have evolved chemical defenses—neurotransmitter substitutes—that interfere with CNS-signaling processes in plant predators. In turn, mammals have evolved ‘counter adaptations’ such as the cytochrome P-450 mechanism evolved specifically to metabolize plant allelochemicals. Evolutionary biologists studying plant–herbivore interactions have convincingly argued that many plant secondary metabolites, including alkaloids such as nicotine, morphine and cocaine, are potent neurotoxins that evolved to deter consumption by herbivores. On the other hand, neurobiology’s reward model sees interactions between drugs and the nervous system as rewarding and reinforcing. Hence, in their current forms, neurobiology’s reward model and evolutionary biology’s punishment model appear to be incompatible. This incompatibility is the paradox of drug reward. Resolving the paradox of human drug use will require new neurobiological models, or new interpretations of neurobiological reward theory, that are consistent with insights from evolutionary ecology.
In biology, coevolution occurs when two or more species reciprocally affect each other’s evolution. In the context of evolutionary biology, coevolution refers to the evolution of at least two species, which occurs in a mutually dependent manner. Coevolution functions by reciprocal selective pressures on two or more species, analogous to an arms race in an attempt to outcompete each other. Classic examples include predator-prey, host-parasite, and other competitive relationships between species. While the process of coevolution generally only involves two species, multiple species can be involved. Moreover, coevolution also results in adaptations for mutual benefit. An example is the coevolution of flowering plants and associated pollinators (e.g., bees, birds, and other insect species).
Hominids have coevolved with plants for millions of years; the skulls of ancient hominids reflect the nature of the plant species they ate, while more recently we domesticated plants to suit our needs, leading to a dramatic cultural shift from hunter‐gatherer to agricultural societies. Our deep relationship with, and understanding of, plants has enabled us to harness their nutritional, medicinal, and aesthetic benefits. The domestication of particular plant taxa has genetically modified those taxa and intensified human contact with specific plants and their endogenous bioactive allelochemicals (secondary plant compounds).
In my view, had there been no similarities between plant allelochemicals and human neurotransmitters, there would be no pleasure obtained from consumption of these plants by humans and consequently humans would not cultivate these plants on such large scales, for example, enhanced cultivation of cannabis, coca, and opium plants. In other words, besides food and sex, pleasure-reward system in human ancestors have evolved to feel pleasure from these plant allelochemicals so that human ancestors endeavor to work for survival of these plant species. The entire agriculture sector is based on obtaining food for our survival, and that food also utilize the same reward system in brain and therefore we cultivate plants for fruits, vegetables and cereals. Our species propagates and plants’ species also propagate. Therefore human plant coevolution results in adaptations for mutual benefit and not necessarily predator-prey relationship to outcompete each other. Plants give us oxygen for our survival and we give them carbon dioxide for their survival.
The problem is that some humans go overboard, that give rise to drug addiction and obesity, through similar mechanism of dysfunction of reward system. And we pay price for going overboard, morbidity and mortality of drug addiction and obesity. I think I resolved the paradox of drug reward for humans.
______
Dr. Rajiv Desai. MD.
July 30, 2019
_____
Postscript:
Due to severe stress of multiple civil and criminal litigations out of matrimonial dispute, I had consumed alprazolam and alcohol on regular basis for few years in 1990s. On hindsight it was a mistake as it did not relieve any stress but worsened the situation and I somehow managed to survive.
______


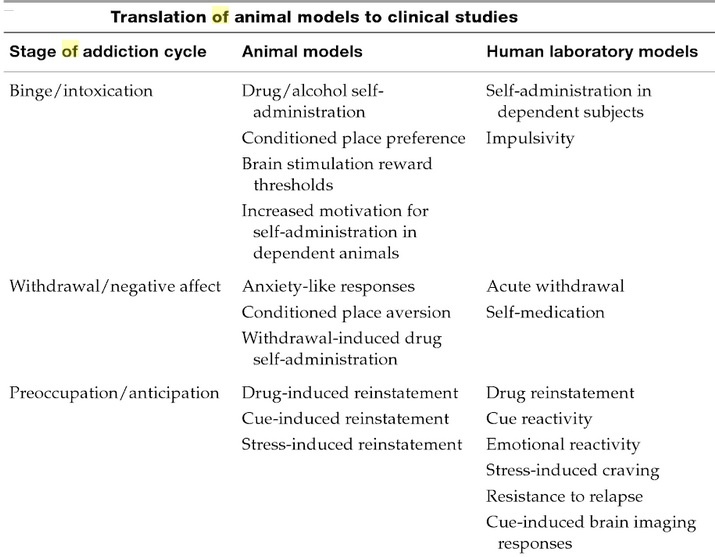
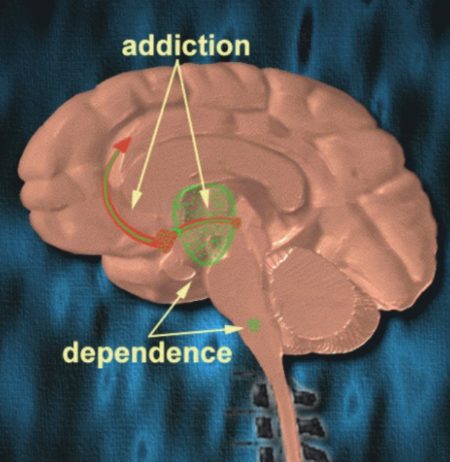

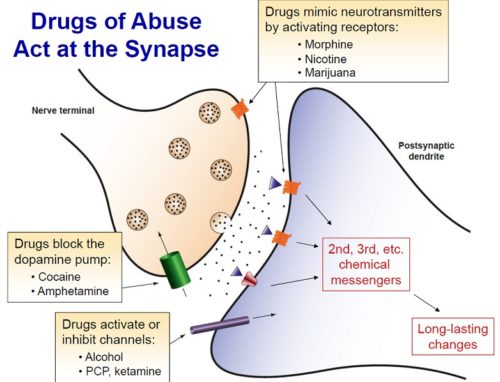
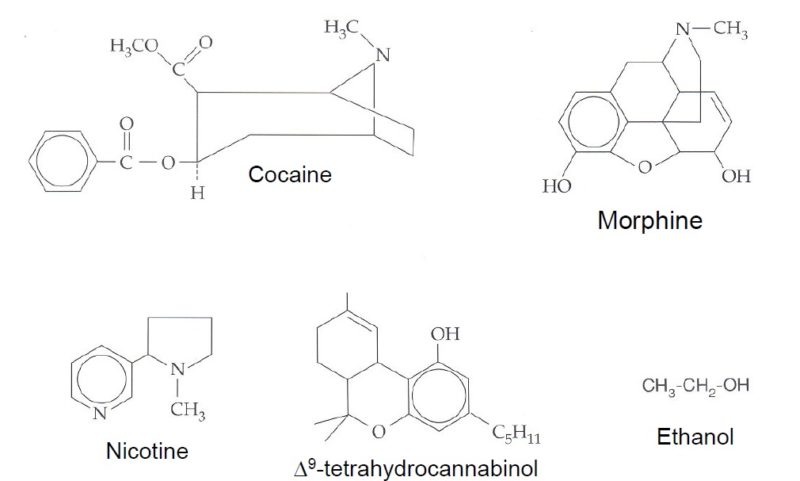
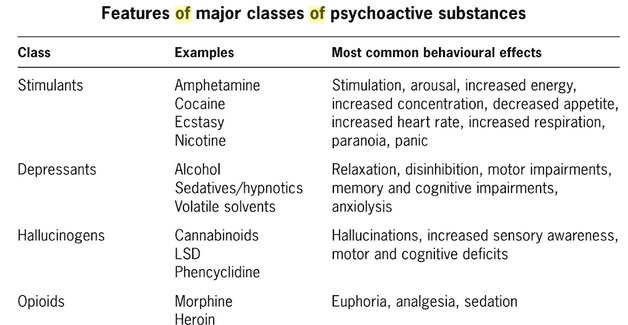
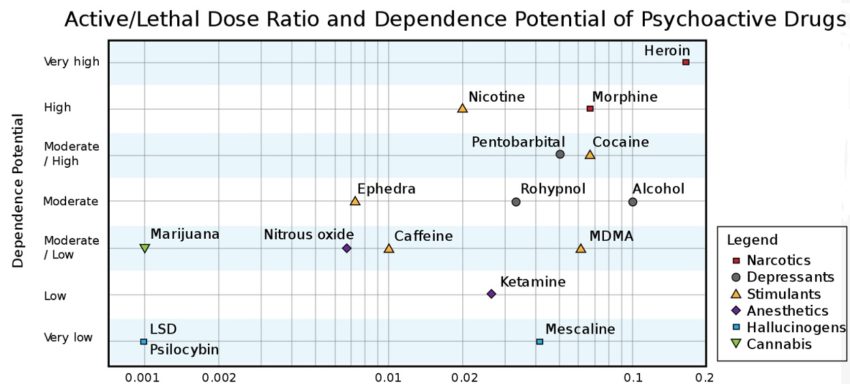
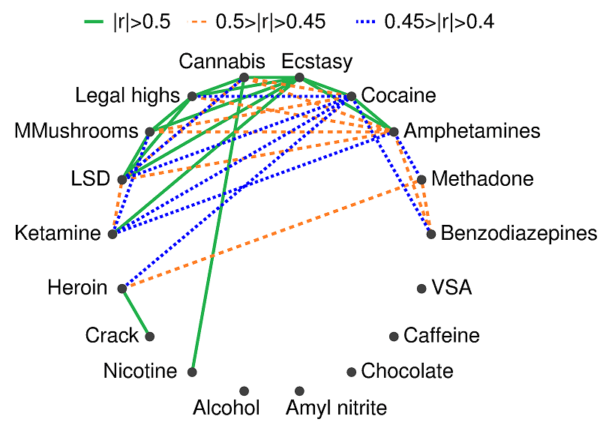
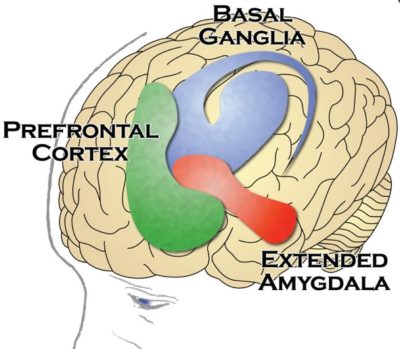
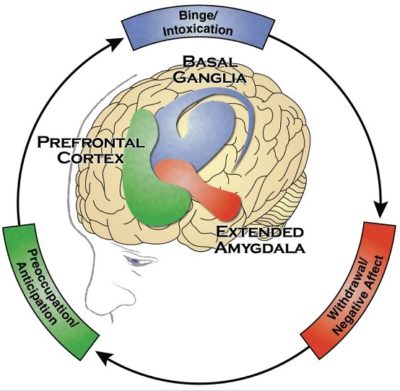
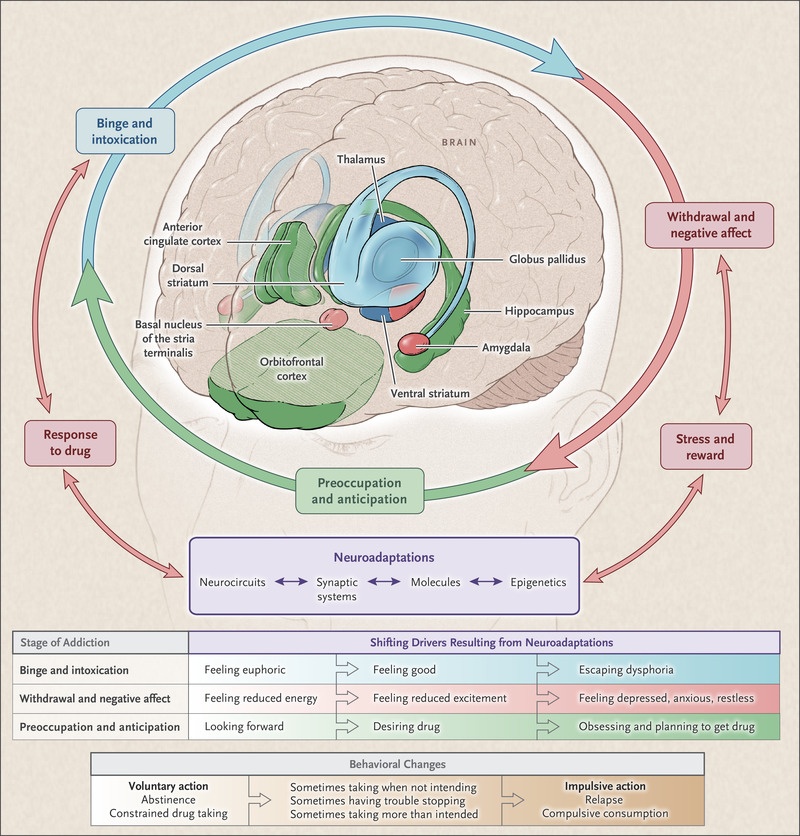
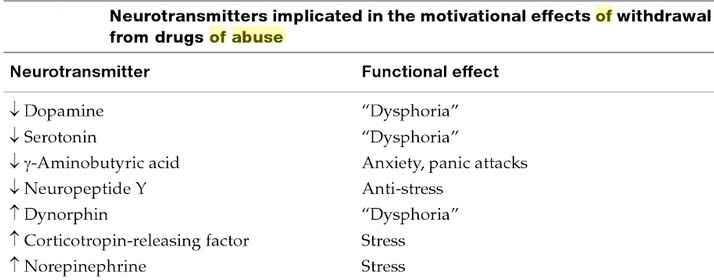
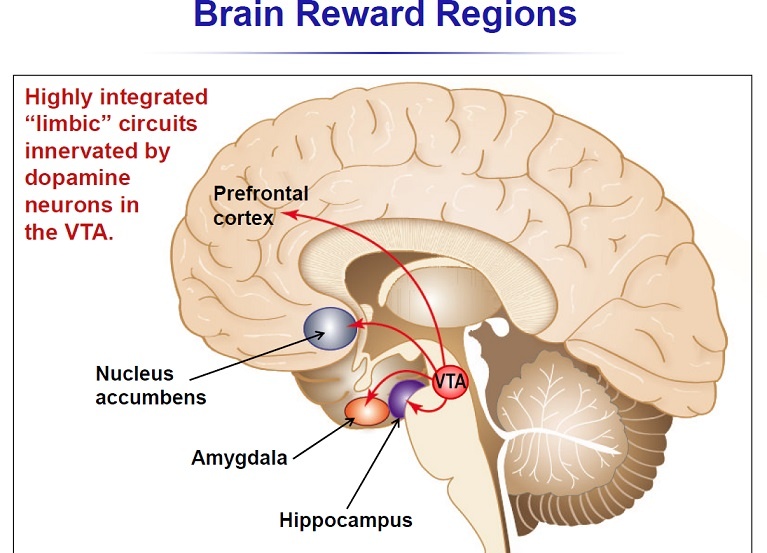
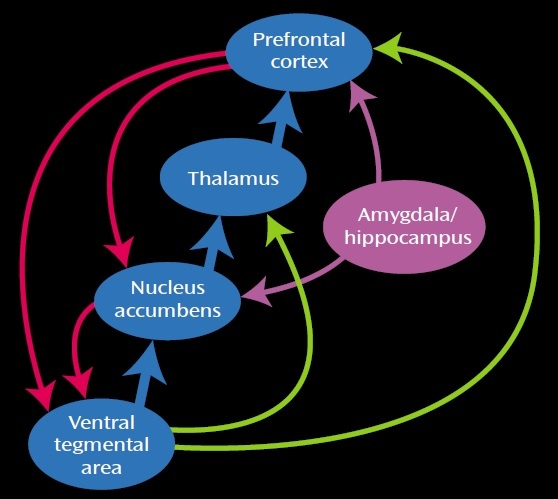
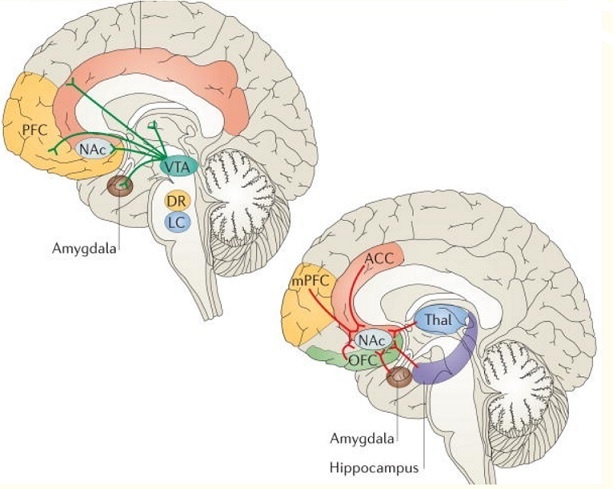
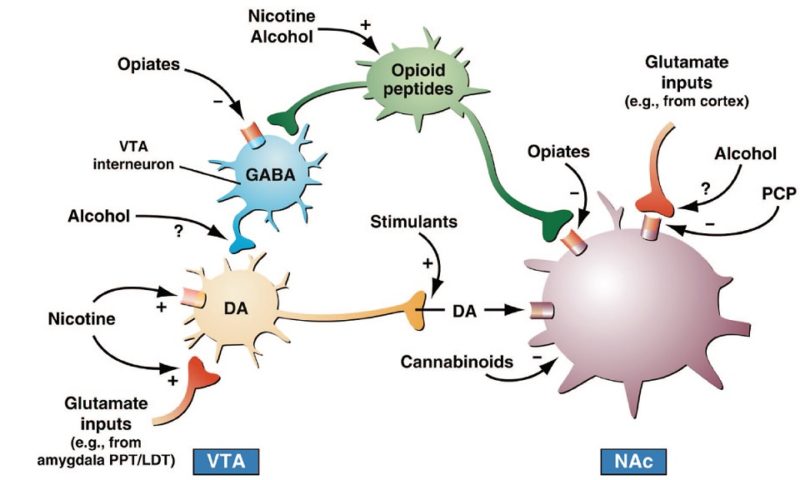
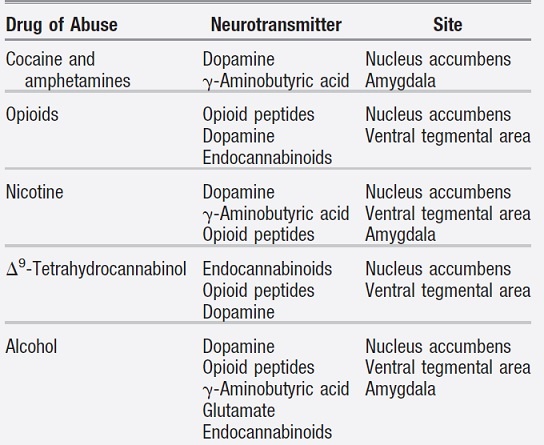
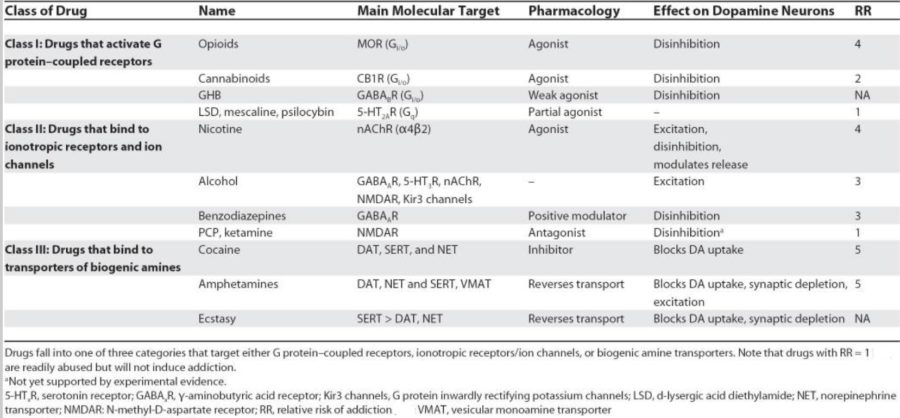
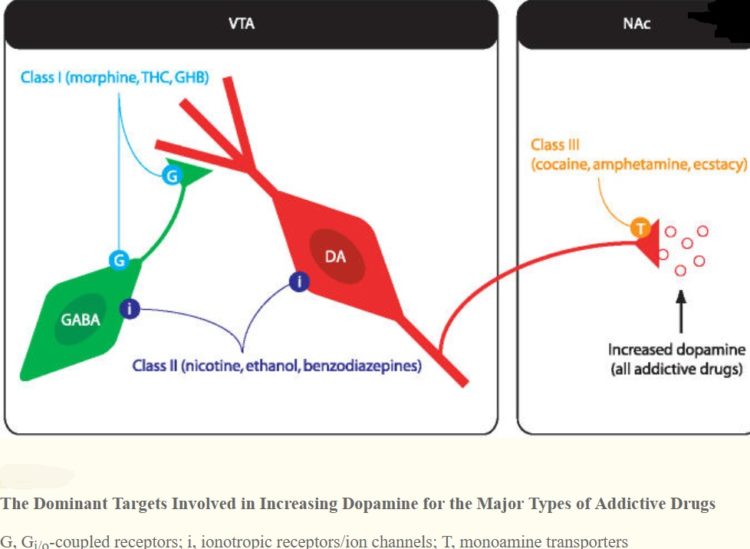
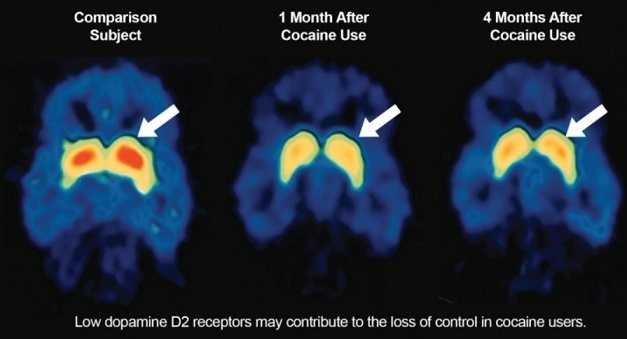
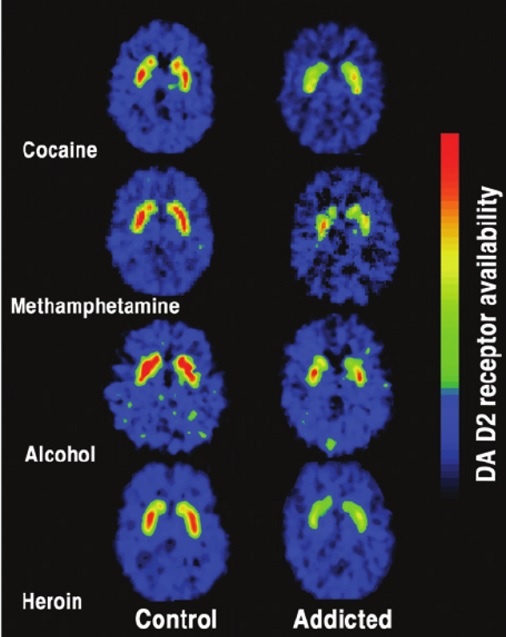
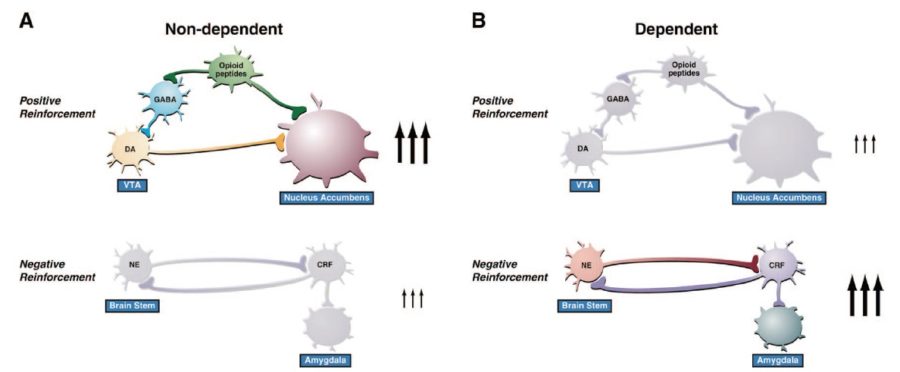
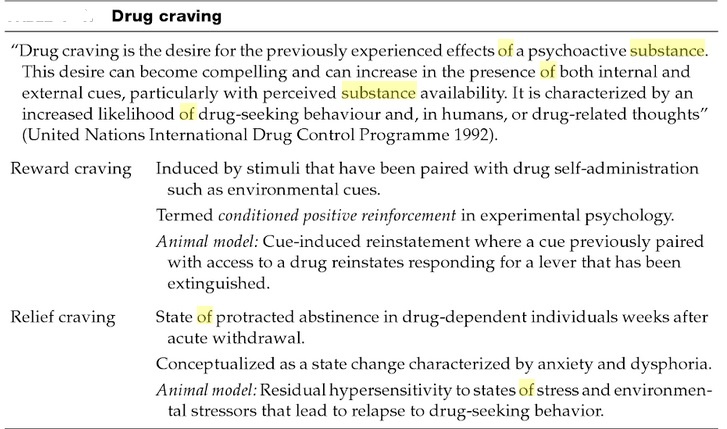
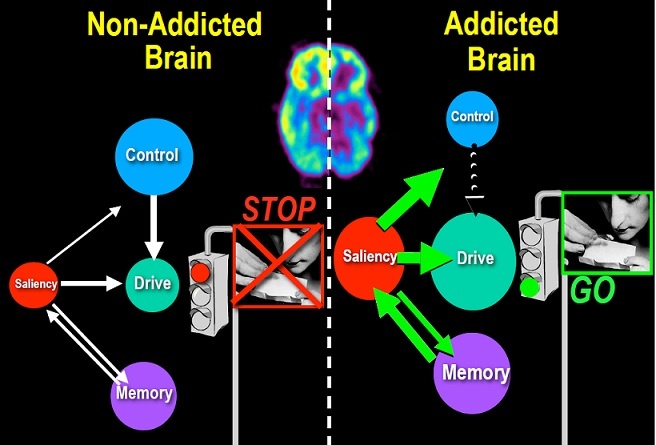

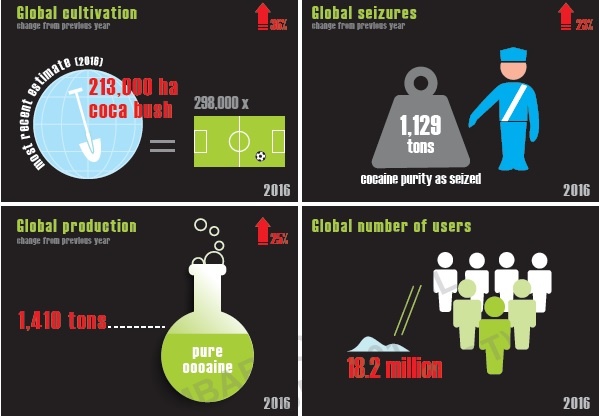
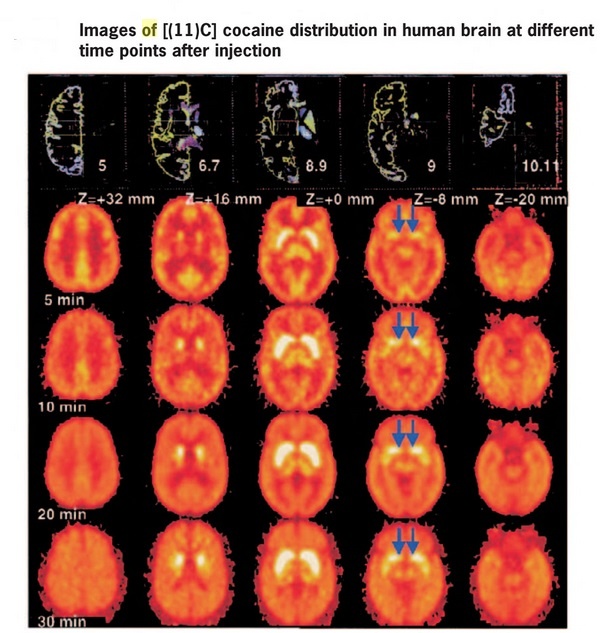

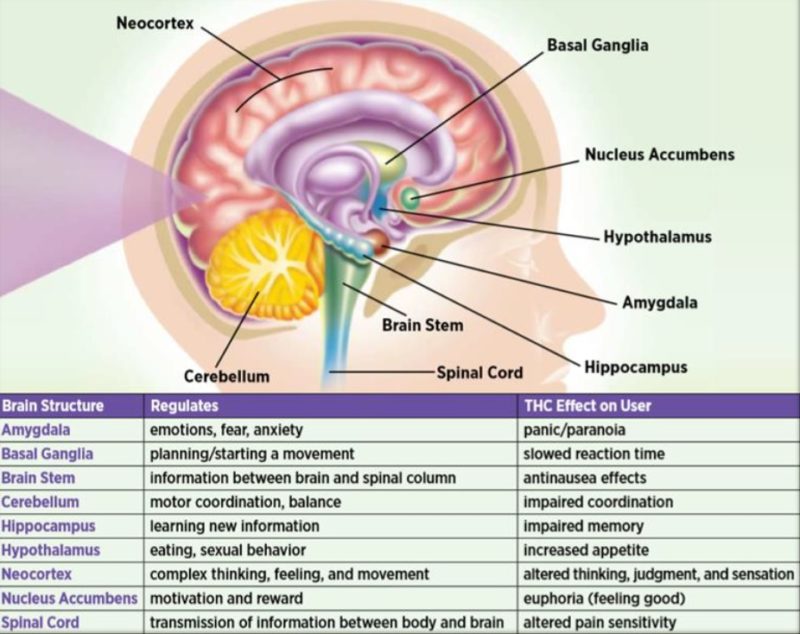
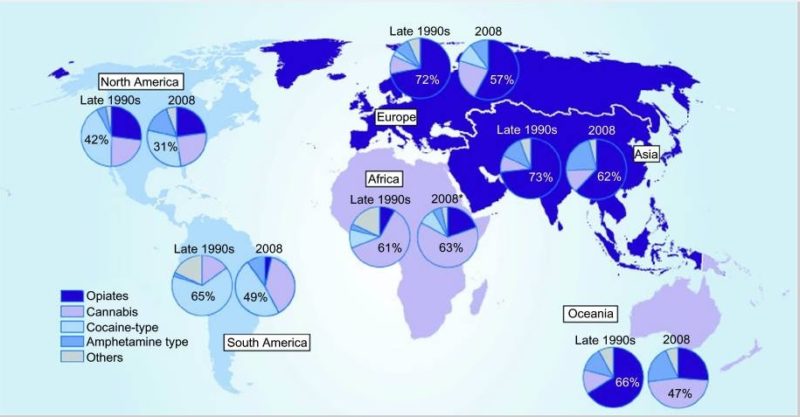
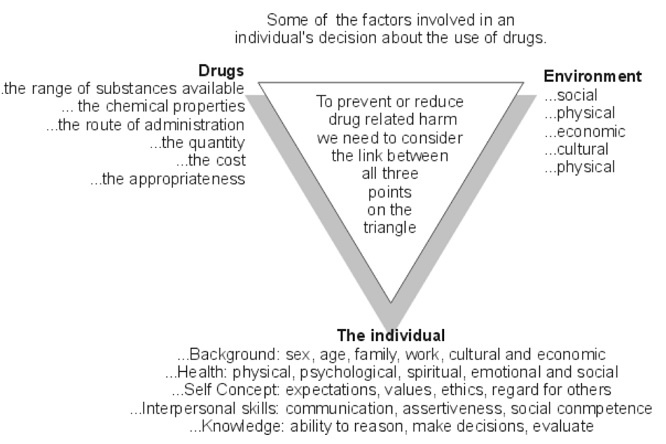
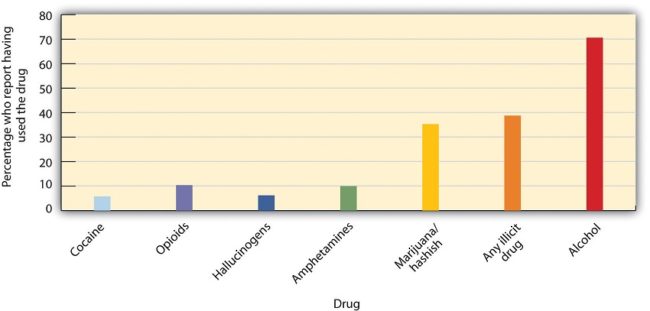
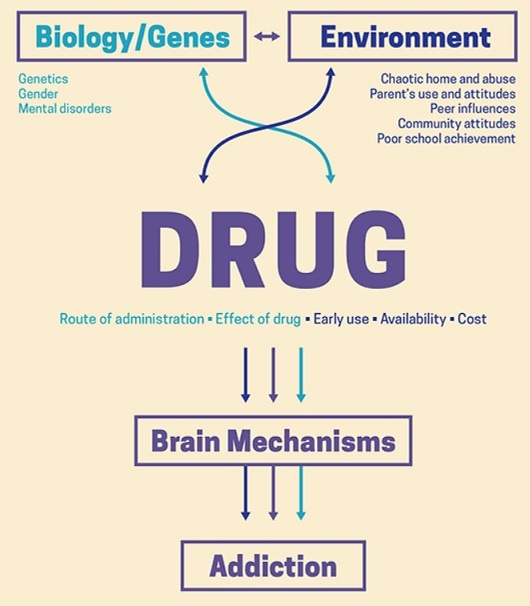
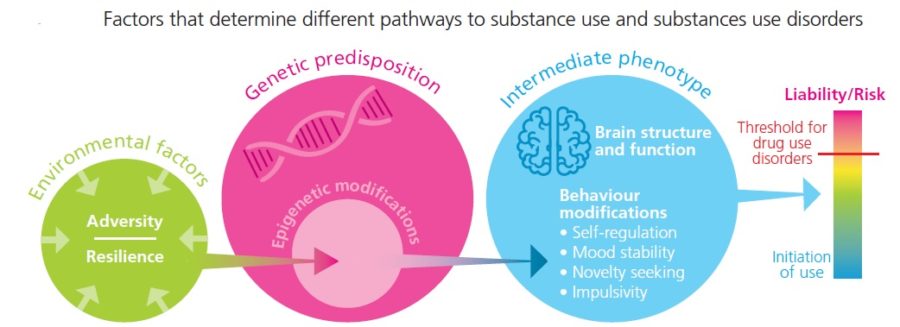
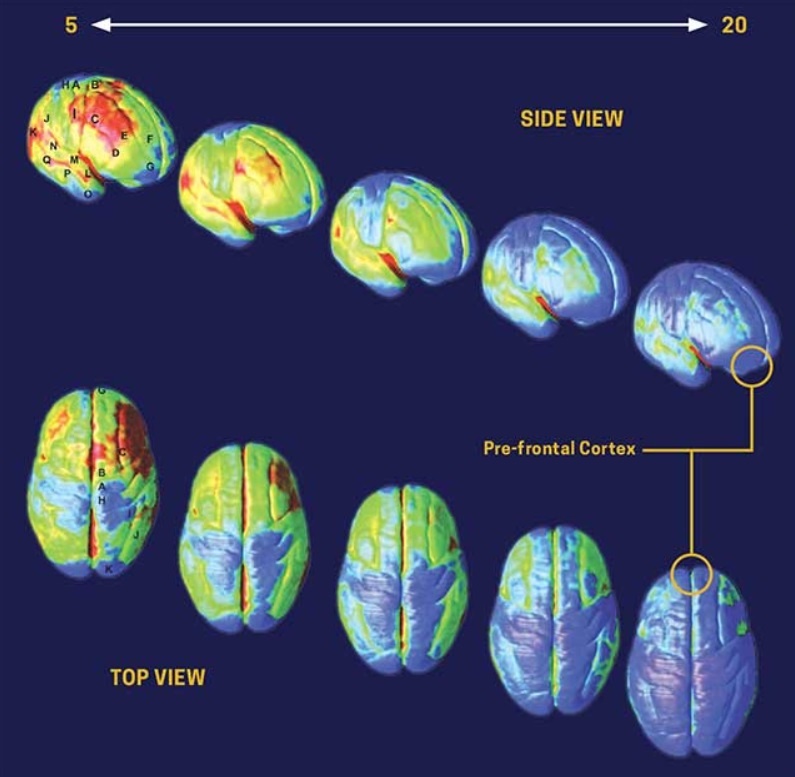
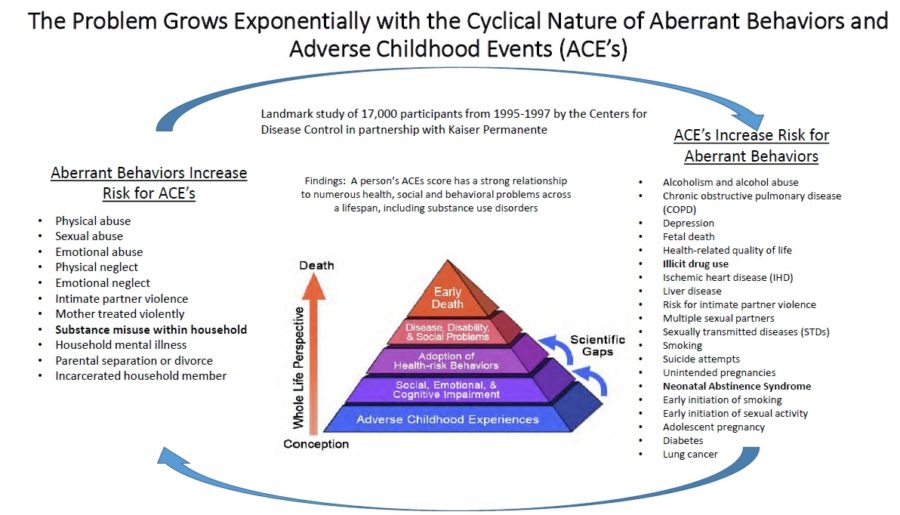
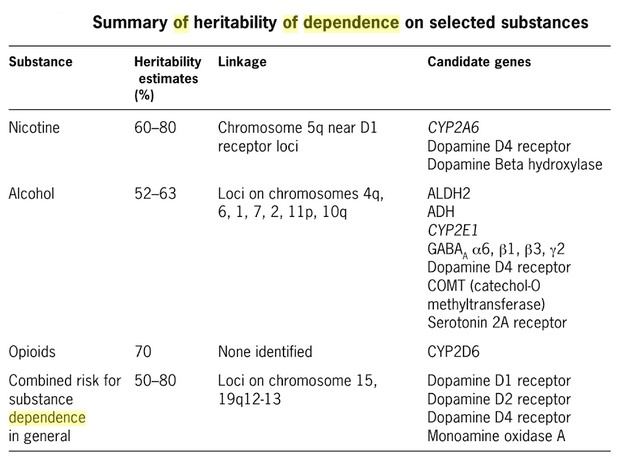
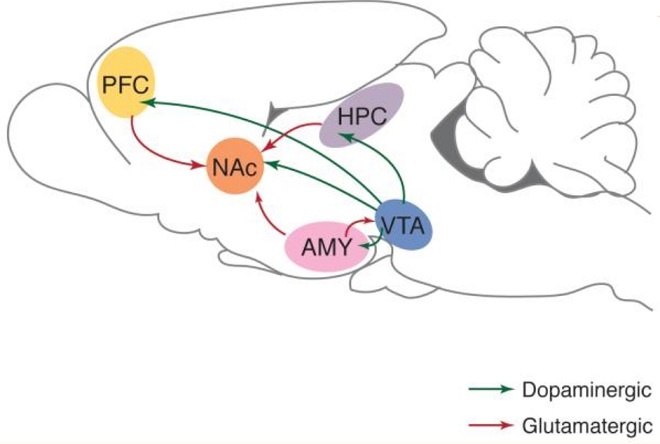
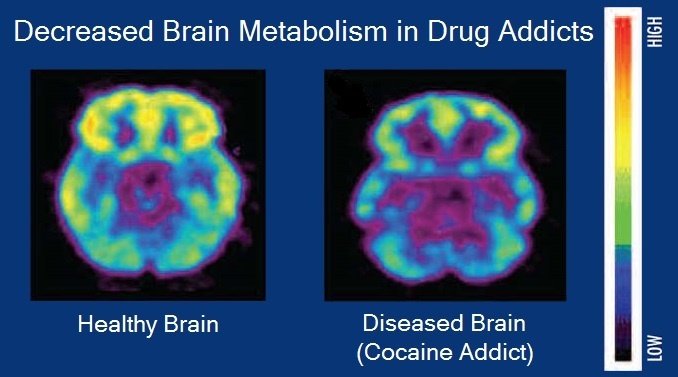
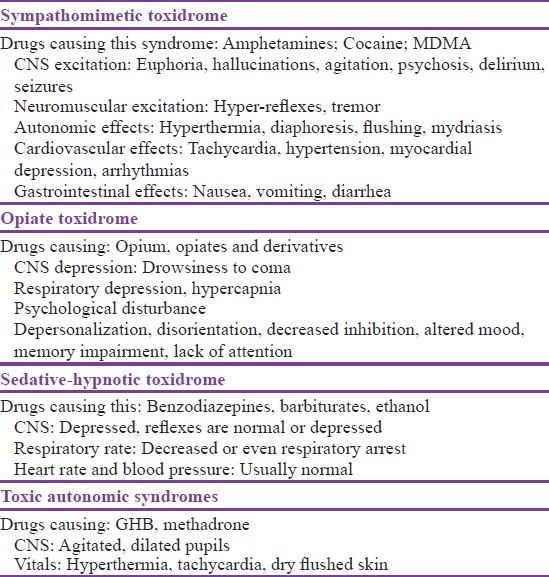
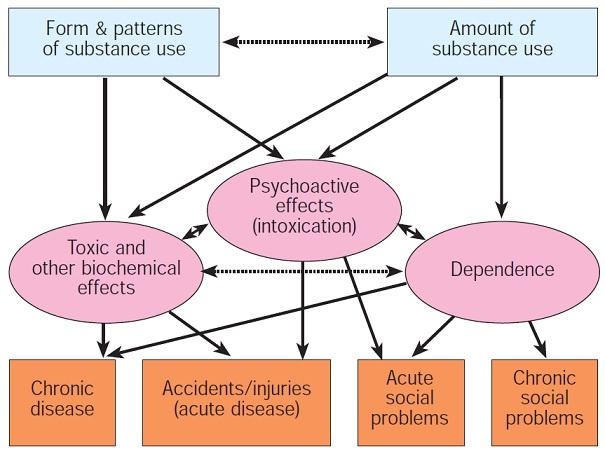
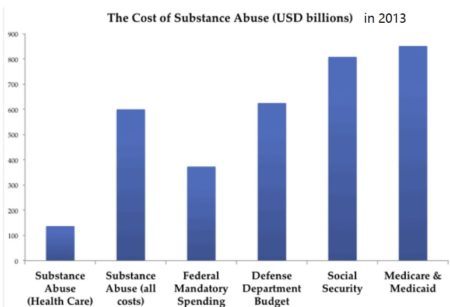
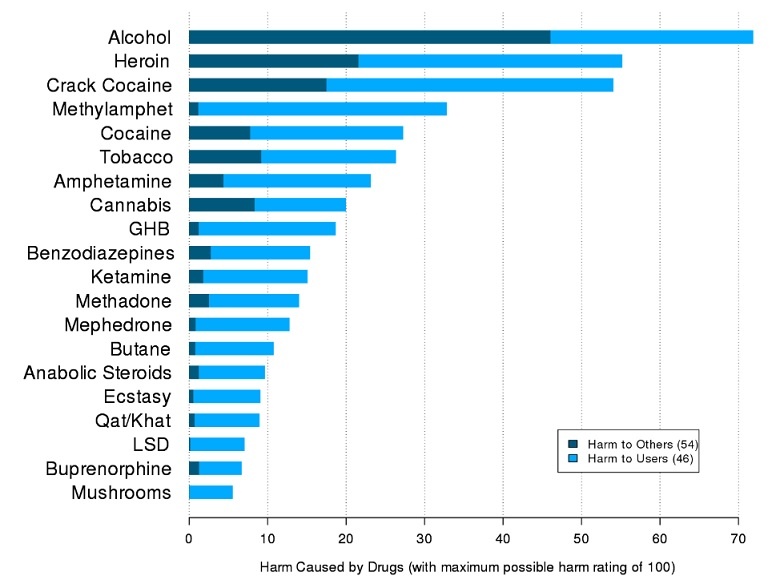
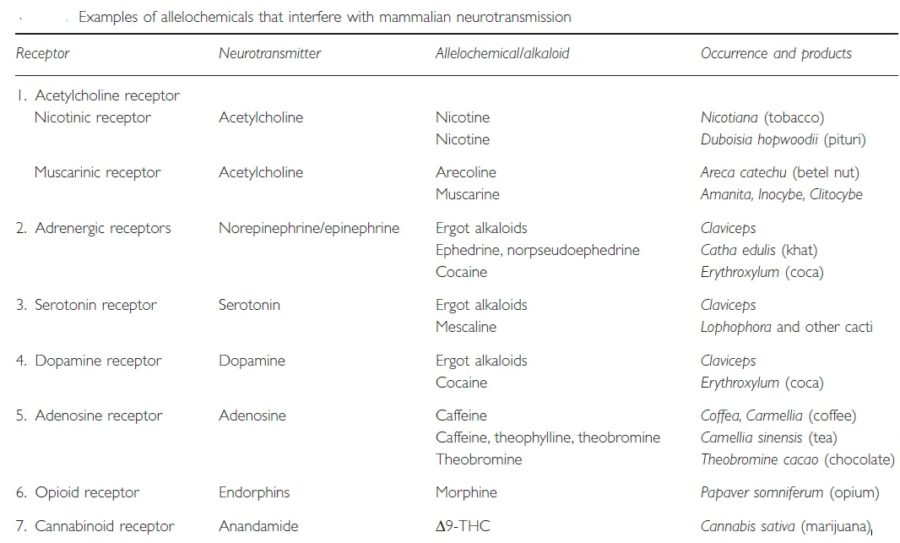
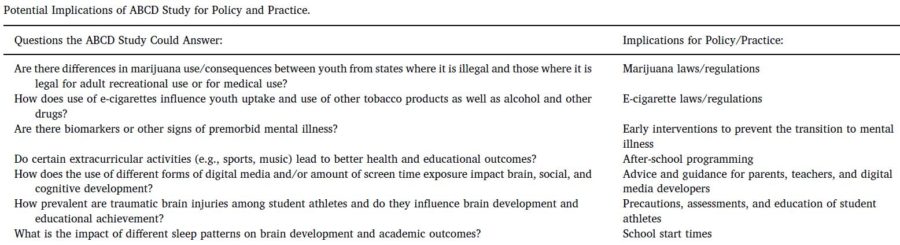
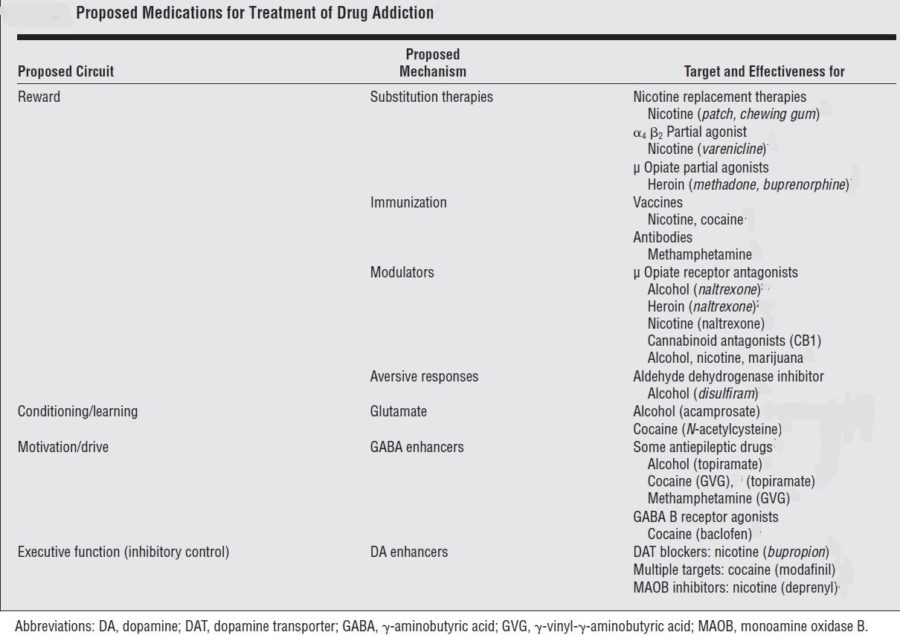
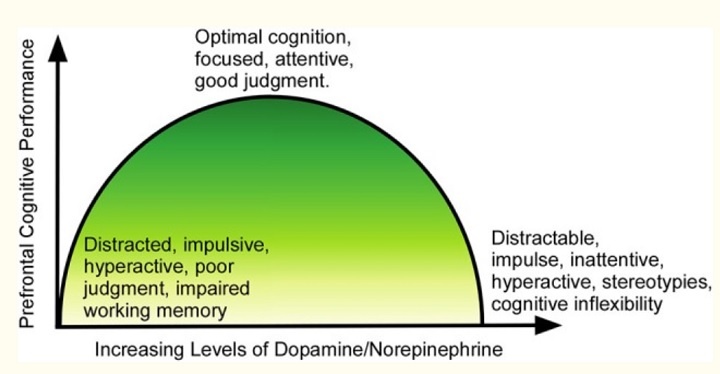
Hello mates, how is the whole thing, and what you want to say concerning this piece of writing, in my view its genuinely awesome in favor of me.|
Thank you so much for generously providing all of this information on a website that is free to the public at your own cost. It really is superb!
I am sure this article has touched all the internet users, its really really good paragraph on building up new webpage.|
I needed to thank you for this excellent read!! I absolutely loved every little bit of it. I have got you book marked to look at new things you post…
Thanks for the blog post.Really thank you! Fantastic.
I need to to thank you for this great read!! I absolutely enjoyed every bit of it. I have you saved as a favorite to look at new stuff you postÖ
Good answer back in return of this matter with real arguments and explaining everything concerning that.
You made a few good points there. I did a search on the theme and found a good number of persons will have the same opinion with your blog.
I agree with you
Fastidious answer back in return of this question with real arguments
and describing the whole thing regarding that.
This blog DRUG ADDICTION – Dr Rajiv Desai has helped me a lot with my dog.
Also, I used this training course https://s96.me/dog-training-course and now
my dog follows everything I ask. Kiss you All!
As the admin of this web page is working, no question very quickly it will be well-known, due to its feature contents.|