Dr Rajiv Desai
An Educational Blog
CHIKUNGUNYA
CHIKUNGUNYA
Prologue:
Few years ago, I have not heard the name Chikungunya but now a days, I am treating plenty of Chikungunya cases in my medical practice in India. The hall mark of Chikungunya is presence of multiple cases in a family/ neighbourhood/ locality /village /township. Majority of patients have abrupt onset fever with severe joint pain (arthralgia) with/without joint swelling (arthritis). Even though majority recovered soon, some of them have chronic crippling arthritis lasting for months or years. Also, many patients of Chikungunya were erroneously diagnosed as typhoid/ malaria/ dengue and received wrong treatment. So I posted this comments on Chikungunya to educate masses.
Synonyms and abbreviations:
Vector = arthropod = mosquito
Chikungunya fever = CF
Chikungunya virus = CHIK-V
Chikungunya = chicken guinea = chicken gunaya = chickengunya
The disease was first described by Marion Robinson and W.H.R. Lumsden in 1955, following an outbreak in 1952 on the Makonde Plateau, along the border between Mozambique and Tanganyika (the mainland part of modern day Tanzania). The word Chikungunya is derived from Makonde language of Africa which means ‘that which bends up’ which is because the patient walks in stooped posture due to crippling polyarthritis. Chikungunya fever (CF) is a viral illness caused by arbovirus (ar=arthropod & bo=borne) transmitted by a bite of Aedes aegypti mosquito which also transmit dengue and yellow fever.
Chikungunya (CF) is an emerging vector-borne disease affecting millions of people in 20 countries belonging to Africa, south Asia, south-east Asia and Europe. CF affected 1.4 million people in India in the year 2006. There is a strong possibility of Chikungunya becoming a pandemic in future. Although not a killer disease, it causes chronic polyarthritis in some patients resulting in substantial disability to patients causing adverse socio-economic impact to the affected country.
It has been reported that the attack rate in susceptible populations may be as high as 40 to 85 percent and the ratio of symptomatic to asymptomatic patients (inapparent infections) is about 1.2 to 1 in one study. Another study done in La Reunion Island in the year 2006 showed that the clinical attack rate of 34 percent in the population; and the clinically inapparent infections in 16 percent of the population as compared to 50 percent in dengue fever.
CF is caused by Chikungunya virus (CHIK-V) which is a RNA virus of family Togaviridae and genus Alphavirus of size 60 to 70 nanometer and having a single strand RNA genome and transmitted to humans from a bite (bloody meal) of arthropod (vector/mosquito). The main virus reservoirs are monkeys, but other vertebrates can also be reservoirs including humans. In Africa, Chikungunya is spread via a sylvatic cycle in which the virus largely resides in other primates in between human outbreaks but in Asia, humans have been the main reservoir of the virus. Chikungunya virus is an Alphavirus closely related to the O’nyong’nyong virus, the Ross River virus in Australia, and the viruses that cause eastern equine encephalitis and western equine encephalitis.
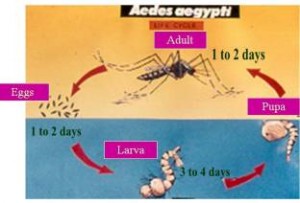
Aedes aegypti mosquito is a vector for CF. The CHIK-V has undergone mutation and therefore it can also be transmitted by Aedes albopictus (Asian tiger mosquito) which is wide spread and survives in temperate climate. It is possible for a person to have Chikungunya and Dengue fever together at the same time because the infected Aedes mosquito can carry both the viruses.
Female Aedes mosquito gets infected with virus after bloody meal from viremic vertebrate and the mosquito develops systemic infection in 7 days (extrinsic incubation period) following which the virus resides in the salivary glands of mosquito which transmits infection to vertebrate during subsequent bloody meal. The mosquito is unharmed during the viral infection of itself and the virus remains in salivary gland of mosquito as long as mosquito lives (about 2 weeks). The male Aedes mosquito does not bite humans, survives on plant nectar and dies within few days of mating.
The Aedes mosquito breeds in clean water collections in domestic setting like flower vases, air coolers, water containers, coconut shells, tyres etc and also on construction sites. A blood meal takes 2 to7 days to digest and 1 to 3 meals are needed to complete development of clutch of eggs.
The adult female Aedes mosquito rests during night and bites humans during day time. CF outbreaks occur in post-monsoon period when vector density is high. The Aedes mosquito is a localized insect and can travel only up to 200 meters from its habitat and therefore epidemic of CF occurs due to travel by infected human from affected area to unaffected area. There is no direct human to human transmission of disease and hence it is not a contagious disease.
Clinical presentation:
Incubation period is 2 to 4 days from the time of mosquito bite but can vary from 1 to 12 days. Viremia persists for 5 days from onset of illness. 92 % patients have fever which is abrupt onset, reaching 39 to 40 degree Celsius, associated by rigors and subsides in 3 days.
87 % patients have arthralgia (joint pain) which is worst in the morning followed by backache in 67 %. About 70 % patients have migratory polyarthritis with joint effusions affecting ankles, wrists, small joints of hand, knees, shoulders etc. Patients in acute stage complain bitterly of pain when asked to move. They characteristically lie still in the attitude of flexion. Pain on movement is worse in the morning, improved by mild exercise and exacerbated by strenuous exercise. Swelling may occur but fluid accumulation is uncommon.
Many patients have pedal oedema (swelling of both feet) in CF which is unexplained but could be peri-arthritis of ankles spreading up as cellulitis or fasciitis. I have seen many cases of Chikungunya having puffiness of face in acute stage which is unnecessarily investigated for renal or thyroidal disorders and the puffiness usually disappear in one week.
50 % patients have maculo-papular skin rash. Many patients and physicians confuse it with drug rash due to allergy to the medicines the patient took for fever and joint pain. Redness (erythema) of skin is another important finding. Skin rash is due to hypersensitivity vasculitis.
Besides these prominent symptoms, patients may have headache, vomiting, photophobia, muscle aches etc. and very rarely a patient may have encephalitis, uveitis, optic neuritis etc.
Occasionally, CF may manifest without fever and only with joint symptoms.
Pregnant women can pass virus to their fetus but only few new born will manifest with meningo-encephalitis. IgM, an antibody against CHIK-V, generally appears in blood between 4 and7 days after the onset of clinical illness and reaches maximum titers after 3 to 6 weeks. IgM, however, does not pass through the placental barrier. The body starts producing IgG antibodies around day 15 and it passes through the placenta and confers immunity to the fetus.
Sequelae:
Persistent arthritis, joint stiffness and tendonitis persist in 10 % patients for months to years. Occasional patient may show chronic destructive arthropathy and very occasionally show features of rheumatoid arthritis with low levels of rheumatoid factors.
Recovery:
Younger patients recover within 5 to 15 days; middle-aged patients recover in 1 to 2.5 months. Recovery is longer for the elderly. The severity of the disease as well as its duration is less in younger patients and pregnant women. In pregnant women, no untoward effects are noticed after the infection.
Recurrence:
An attack of CF gives life time immunity against CF just like chicken pox.
Death due to CF is very rare indeed but in elderly patients, severe CF may worsen underlying diseases which may cause death.
Laboratory Diagnosis:
The viremia persists for 4 to 5 days after onset of disease and therefore virus isolation and culture from blood in acute febrile state is possible. Also, RT-PCR test for viral RNA can be done on patient’s blood in acute febrile state. Both viral culture and RT-PCR test are gold standard for diagnosis of CF but not available in small towns and many cities.
IgM antibodies detection by Elisa test can give indirect evidence of acute CHIK-V infection. However, best results are obtained 10 to 14 days after onset of illness and the test should not be done in first week. Some patients get positive test after 6 to 12 weeks. A false positives can occur with infection via other related viruses such as O’nyong’nyong virus and Semliki Forest Virus. I have seen many clinically classical cases of CF having negative IgM test repeatedly proving limitation of this test. Also, four fold rise in IgG antibodies between acute and convalescent sera can be used for diagnosis.
Presence of leucopenia and platelet count less than 50000 per micro liter should alert possibility of co-existing Chikungunya with Dengue fever.
Differential diagnosis:
Any fever with joint pain with/without arthritis can be mistaken for CF including rheumatic fever, dengue, leptospirosis, malaria. Besides Chikungunya, true arthritis is a common accompaniment of several viral diseases like rubella, parvovirus B19 infection, hepatitis B; and occasional accompaniment of mumps, enterovirus, herpes virus, adeno virus etc. I have seen a case of chronic Chikungunya with polyarthritis and skin rash mimicking SLE.
Treatment in acute state:
There is no specific anti-viral medicine for CF. Bed rest is advised during acute state and the patient must avoid warm/heat fomentation to the affected joint as it may increase joint pain. The patient must maintain good hydration. Symptomatic treatment with NSAIDS is recommended with due precaution to avoid its GI side effects. Avoid aspirin in acute stages of disease.
I found Etoricoxib 90 mgs once daily most useful in adults. I also found that NSAIDS must be started as early as possible and must be continued despite resolution of arthritis. Sudden discontinuation of NSADIS because of apparent clinical recovery leads to relapse of joint symptoms in most cases. In case, arthralgia is refractory to NSAIDS, then, use hydroxychloroquine 200 mg or chloroquine 300 mg once a day orally for 4 weeks. I recommend short course of low dose corticosteroids in selected cases of CF with severe polyarthritis lasting for more than 1 week to prevent permanent damage to joints notwithstanding minor side effects of short course of corticosteroids.
Only paracetamol (acetaminophen) should be used when CF and dengue are present together as other NSAIDS affect platelet function and may precipitate bleeding.
Recent studies have shown promising results of use of Interferon-Alfa, ribavirin and 6 azarudine which can kill virus.
Treatment in chronic state:
As noted earlier, 10 % patients develop chronic osteoarticular problems due to persistence of CHIK-V in joint-macrophages and complement mediated joint damage. Even though NSAIDS produce relief in majority of cases, short course of corticosteroids may be very useful in selected cases.
Public health measures:
Reducing vector (Aedes mosquitoes) population with minimizing vector-human contact (mosquito bite) is the best public health measure to control CF. Vector population can be controlled by removing all stagnant water sources in household and neighbourhood ; use of larvivorous fish (Gambusia and Guppy) in aquaria and garden pools and apply chemical larvicide to containers/ vases/ gutters. The contact of vector to humans can be minimized by wearing full-sleeve cloths, use of mosquito net, and spray of insecticide/ insect repellent in household. ‘Patients suffering from CF must be protected from mosquito bite to prevent spread of infection to others.’
Vaccination: There is no vaccine for CF available in world today. Past attempts have resulted in virus developing resistance to vaccine. Recently, scientists have developed a vaccine against CF by using ‘virus-like particles’ which is an empty outer protein-coat of virus that is able to stimulate immune system to produce protective antibodies against CHIK-V without replicating just like hepatitis B vaccine. Experiments were conducted on monkeys and vaccinated monkeys fought off infection. Also, the anti-Chikungunya antibodies produced by monkeys protected mice from lethal dose of virus.
Recent studies have shown that infecting mosquitoes by wolbachia bacteria make them more resistant to infection by viruses of Dengue and Chikungunya and therefore prevent Dengue and Chikungunya in humans. Researchers are developing genetically modified (GM) mosquitoes to combat the menace of vector-borne diseases by a genetic alteration in the mosquitoes that disrupts wing muscle development in female offspring, rendering them incapable of flights to bite humans. Male mosquitoes’ ability to fly is unaffected and they show no ill effects from carrying the gene. The technology is completely species-specific as the GM males will mate only with females of the same species.
THE MORAL OF THE STORY:
1) Chikungunya is easy to diagnose clinically in outbreaks but difficult to diagnose as a sporadic case.
2) Best way to prevent spread of Chikungunya during outbreak/epidemic is to prevent mosquito bite to the patients having Chikungunya during first five days of illness.
3) Elisa test available to detect IgM antibodies against Chikungunya virus must be done 10 to 14 days after onset of illness for laboratory confirmation.
4) Early judicious use of short course of low dose corticosteroids is very useful in selected cases of Chikungunya with severe refractory polyarthritis.
5) Mosquito control measures not only prevents Chikungunya but also prevents dengue, malaria, filariasis and yellow fever.
Dr. Rajiv Desai. MD.
March 1, 2010







It’s a shame you don’t have a donate button! I’d most certainly donate to this excellent blog! I guess for now i’ll settle for bookmarking and adding your RSS feed to my Google account. I look forward to brand new updates and will share this website with my Facebook group. Talk soon!|
Say, you got a nice article.Much thanks again. Really Great.
Being sensational is much easier than you think!
I am so happy to read this. This is the kind of manual that needs to be given and not the accidental misinformation thatis at the other blogs. Appreciate your sharing this greatest doc.Also visit my blog post marketing online
Aw, this was an extremely nice post. Spending some time and actual effort to produce a really good articleÖ but what can I sayÖ I hesitate a whole lot and don’t manage to get nearly anything done.
I will right away clutch your rss feed as I can not find youre-mail subscription link or e-newsletter service. Do you’ve any?Please permit me understand so that I could subscribe. Thanks.
An interesting discussion is worth comment. I do believe that you need to write more about this subject matter, it might not be a taboo subject but typically people do not speak about these topics. To the next! Kind regards.
I am truly happy to read this weblog posts which contains plenty of valuable data, thanks for providing these statistics.|
Very nice explaination sir
Spot on with this write-up, I truly think this website needs much more consideration. I?ll probably be again to read much more, thanks for that info.
Only wanna tell that this is extremely helpful, Thanks for taking your time to write this.
Only wanna tell that this is extremely helpful, Thanks for taking your time to write this.
“Hey There. I found your blog using msn. This is a very well written article. I’ll be sure to bookmark it and return to read more of your useful info. Thanks for the post. I will certainly comeback.”
Very interesting info !Perfect just what I was looking for! “It’s not the having, its the getting.” by Elizabeth Taylor.
We are laughing at our heroes but secretly we are definitely rooting for them too.
Good Morning, glad that i found on this in google. Thanks!
Appreciate you sharing, great post. Want more.
I enjoy the report
What’s up to all, the contents present at this site are truly awesome
for people knowledge, well, keep up the nice work fellows.
A round of applause for your blog post.Really looking forward to read more. Will read on…
Simply wanna state that this is handy , Thanks for taking your time to write this.
There’s definately a great deal to find out about this topic.
I really like all of the points you have
made.
Piece of writing writing is also a excitement, if
you be acquainted with after that you can write or else it is complex to write.
Very shortly this web page will be famous among all blogging users, due to
it’s fastidious articles
It works really well for me
I value the article post. Really Cool.
wow, awesome blog post.Really thank you! Fantastic.
“Say, you got a nice blog.Thanks Again. Really Cool.”